NURS MISC Urosepsis Case Study Jean Kelly age 82,100% CORRECT
Document Content and Description Below
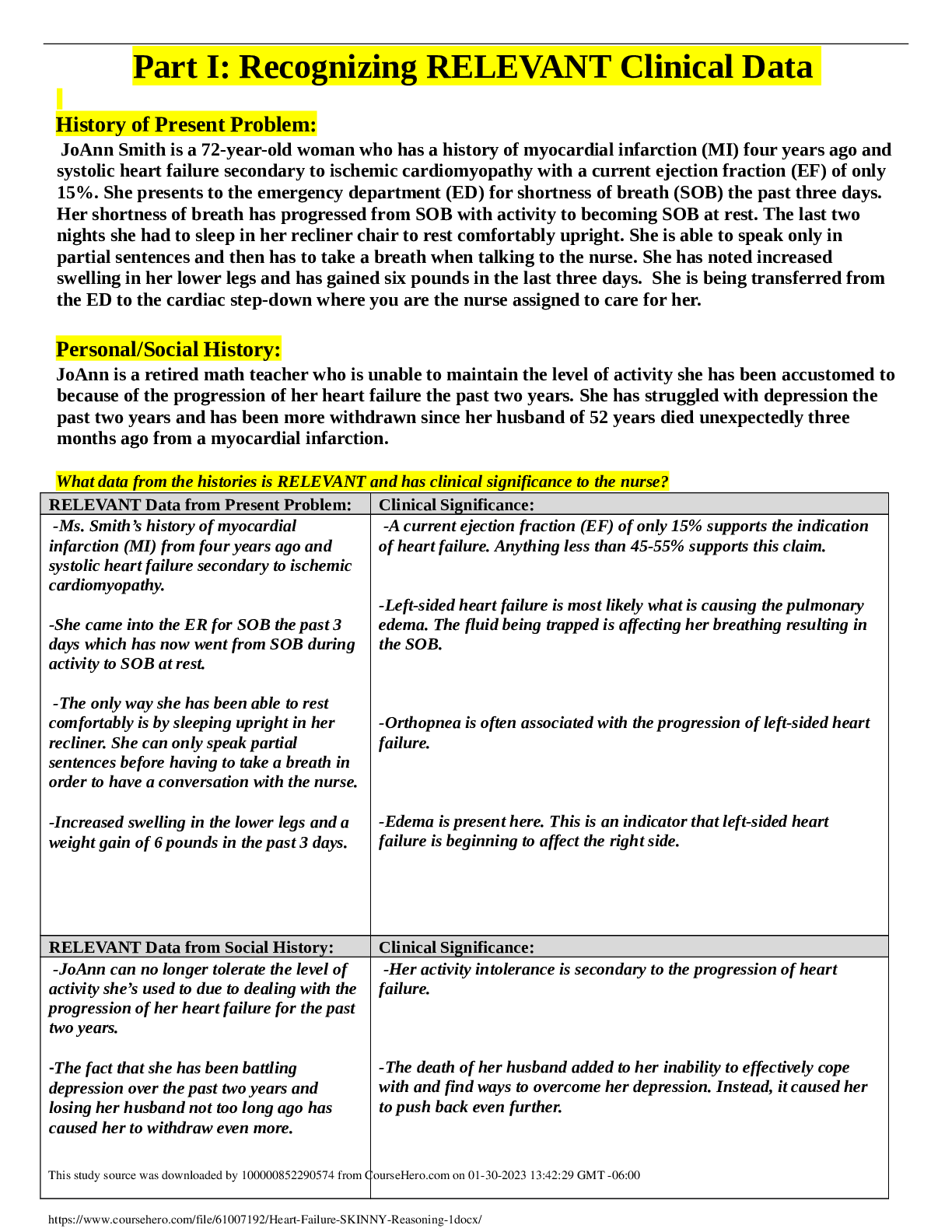
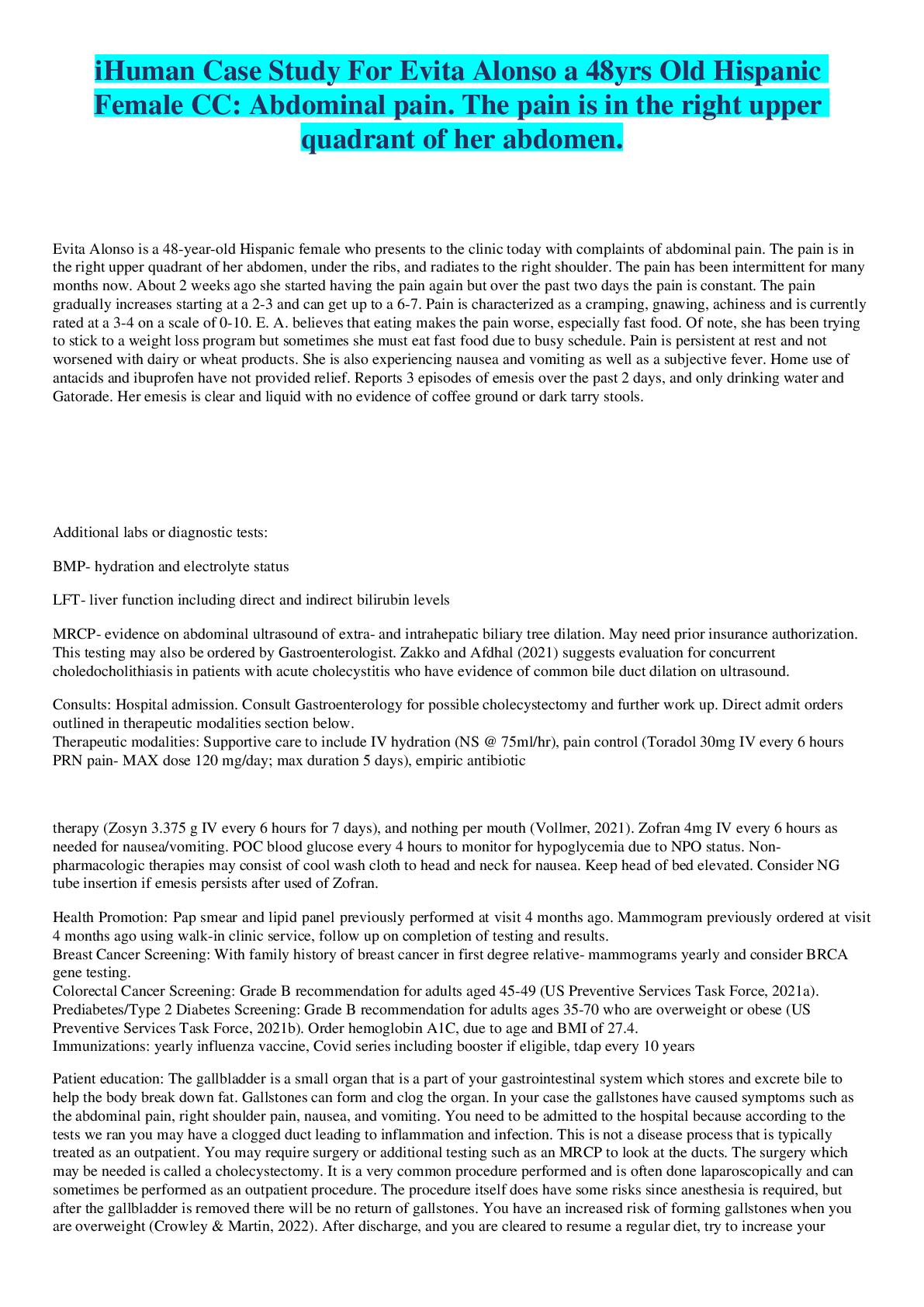
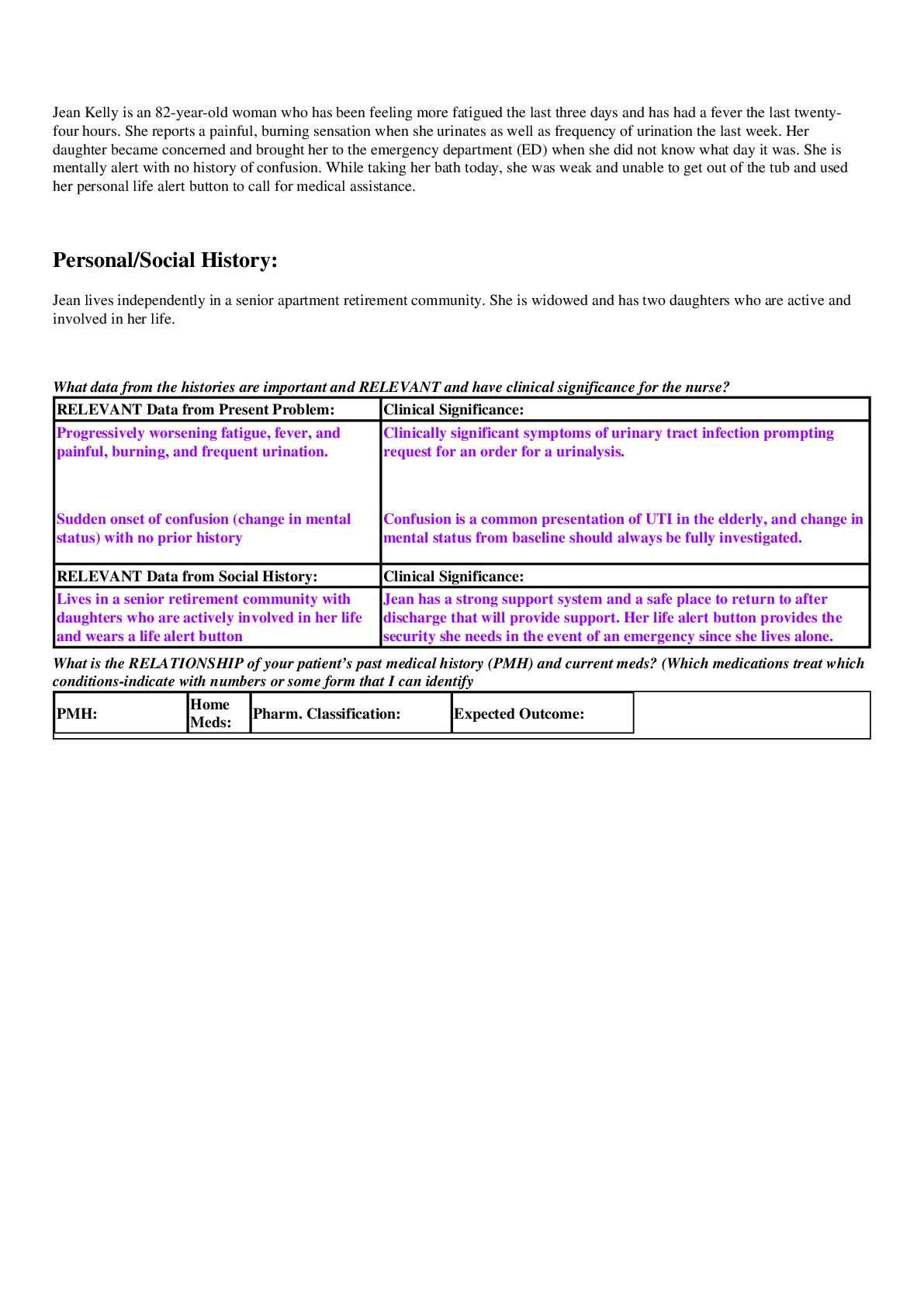
NURS MISC Urosepsis Case Study Jean Kelly age 82 Jean Kelly is an 82-year-old woman who has been feeling more fatigued the last three days and has had a fever the last twenty-four hours. She report... s a painful, burning sensation when she urinates as well as frequency of urination the last week. Her daughter became concerned and brought her to the emergency department (ED) when she did not know what day it was. She is mentally alert with no history of confusion. While taking her bath today, she was weak and unable to get out of the tub and used her personal life alert button to call for medical assistance. Personal/Social History: Jean lives independently in a senior apartment retirement community. She is widowed and has two daughters who are active and involved in her life. What data from the histories are important and RELEVANT and have clinical significance for the nurse? RELEVANT Data from Present Problem: Clinical Significance: Progressively worsening fatigue, fever, and painful, burning, and frequent urination. Sudden onset of confusion (change in mental status) with no prior history Clinically significant symptoms of urinary tract infection prompting request for an order for a urinalysis. Confusion is a common presentation of UTI in the elderly, and change in mental status from baseline should always be fully investigated. RELEVANT Data from Social History: Clinical Significance: Lives in a senior retirement community with daughters who are actively involved in her life and wears a life alert button Jean has a strong support system and a safe place to return to after discharge that will provide support. Her life alert button provides the security she needs in the event of an emergency since she lives alone. What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medications treat which conditions-indicate with numbers or some form that I can identify PMH: Home Meds: Pharm. Classification: Expected Outcome: Diabetes type 2 1. Allopurinol 100 mg PO 1. Antigout agent 1. Decreased production of uric acid to reduce gout flares 2. Reduce platelet aggregation and clumping to prevent clotting 3. Reduces and controls blood glucose levels 4. Reduces cholesterol/ blood lipid levels 5. Reduces blood pressure 6. Reduces blood pressure 7. Reduces BP through diuresis 8. Replaces K in the body lost through diuresis Hyperlipidemia bid 2. ASA 81 mg PO daily 3. Pioglitazone 15 mg PO daily 4. Simvastatin 20 mg PO daily 5. Metoprolol 25 mg PO bid 6. Lisinopril 10 mg PO daily 7. Furosemide 20 mg PO daily 8. Potassium chloride 20 mEq PO daily 2. Antiplatelet/salicylate 3. Thiazolidinedione/anti diabetic 4. Antihyperlipidemic 5. Beta blocker Hypertension (HTN) Gout 6. Ace inhibitor 7. Loop diuretic 8. K supplement One disease process often influences the development of other illnesses. Based on your knowledge of pathophysiology, (if applicable), which disease likely developed FIRST that then initiated a “domino effect” in their life? ● Circle what PMH problem started FIRST • DMII ● Underline what PMH problem(s) FOLLOWED as dominoes • HTN, HLD (probably coexisted), Gout • Wasn’t exactly sure when Gout could have happened as it not necessarily linked to her other comorbidities Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 101.8 F/38.8 C (oral) Provoking/Palliative: Nothing/Nothing P: 110 (regular) Quality: Ache R: 24 (regular) Region/Radiation: Right flank BP: 102/50 Severity: 5/10 O2 sat: 98% room air Timing: Continuous The nurse recognizes the need to validate his/her concern of fluid volume deficit and performs a set of orthostatic VS and obtains the following: Position: HR: BP: Supine 110 102/50 Standing 132 92/42 What VS data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: Temp of 101.8F Indicative of fever, systemic sign of infection Pulse of 110 Tachycardia, heart is beating faster - could be sign of anxiety or compensation of some sort Respirations of 24 Tachypnea could also be a sign of anxiety or compensation BP 102/50 In combination with tachycardia, probably indicative of fluid volume deficit in which heart beats faster to maintain pressure with the decreased blood volume Orthostatic BP changes Orthostatic hypotension defined as a systolic change of at least 20 between supine and standing which she demonstrates. Indicative of many things but given her vitals and s/s, this is consistent with fluid volume deficit GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Pink, warm and dry, no edema, heart sounds regular-S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented x2-is not consistently oriented to date and place, c/o dizziness when she sits up GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants GU: Dysuria and frequency of urination persists, right flank tenderness to gentle palpation SKIN: Skin integrity intact, lips dry, oral mucosa tacky dry What assessment data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: Disorientation, dizziness Dysuria, frequency persist; flank pain and tenderness upon palpation Lips and oral mucosa tacky dry Orthostatic hypotension confirmed with BP measurements and her dizziness with position changes confirms this. She is not sure of the time/place which family reports is not her baseline and should be investigated further to be sure it is just part of the presentation of the UTI Consistent with UTI, flank tenderness and pain can possibly be indicative of kidney involvement/spread of infection beyond the urethra/bladder Dry mucous membranes is consistent with dehydration/fluid volume deficit Lab Results: What lab results are RELEVANT and must be recognized as clinically significant by the nurse? Complete Blood Count (CBC): Current: High/Low/WNL? Previous: WBC (4.5-11.0 mm 3) 13.2 High 8.8 Hgb (12-16 g/dL) 14.4 WNL 14.6 Platelets (150-450x 103/µl) 246 WNL 140 Neutrophil % (42-72) 93 High 68 Band forms (3-5%) 2 Low 1 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: WBC and Hgb WBC is increasing while Hgb remains stable. This means infection and likely rules out any sort of major traumatic blood loss contributing to fluid volume deficit. WBC worsening Hgb stable Stable Worsening Same - moving towards normal value Platelets WNL but rose significantly from last draw. Can be a sign of infection; rising platelets in the setting of infection known as reactive thrombocytosis Neutrophil Increasing neutrophil count is a sign of infection as the body produces more to fight the existing infection. Band forms Similar to neutrophils, considered neutrophils in their early form and altered counts can indicate infection or risk of infection Basic Metabolic Panel (BMP): Current: High/Low/WNL? Previous: Sodium (135-145 mEq/L) 140 WNL 138 Potassium (3.5-5.0 mEq/L) 3.8 WNL 3.9 Glucose (70-110 mg/dL) 184 High 128 BUN (7 - 25 mg/dl) 35 High 14 Creatinine (0.6-1.2 mg/dL) 1.5 High 1.1 RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Glucose Elevated BUN and Creatinine Patient is a type II diabetic and her body is likely responding to the stress of illness and fever with increased insulin demands These are indicative of kidney function and rising levels mean there is an impairment in kidney functioning and that the kidneys are not filtering/producing urine effectively Worsening Worsening Misc. Labs: Current: High/Low/WNL? Previous: Magnesium (1.6-2.0 mEq/L) 1.8 WNL 1.9 Lactate (0.5-2.2 mmol/L) 3.2 High n/a RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Lactate Lactate is indicative of sepsis due to organ hypoperfusion and considered critical with a value >2 Worsening Urine Analysis (UA): Current: ABNL/WNL? Previous: Color (yellow) Yellow WNL Yellow Clarity (clear) Cloudy ABNL Clear Specific Gravity (1.015-1.030) 1.032 ABNL 1.010 Protein (neg) 2+ ABNL 1+ Glucose (neg) Neg WNL Neg Ketones (neg) Neg WNL Neg Bilirubin (neg) Neg WNL Neg Blood (neg) Neg WNL Neg Nitrite (neg) Pos ABNL Pos LET (Leukocyte Esterase) (neg) Pos ABNL Pos MICRO: RBC’s (<5) 1 WNL 0 WBC’s (<5) >100 ABNL 3 Bacteria (neg) LARGE ABNL Few Epithelial (neg) Few ABNL Few RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Cloudy urine Can be a sign of infection Increased concentration of urine likely due to fluid deficit Seen in DM II and UTI All indicative of UTI; nitrites indicate presence of bacteria while LET and WBC demonstrate presence of WBC trying to attack infection Worsening Elevated spec grav Worsening Protein in the urine Worsening Nitrites, LET, WBC, Bacteria, epithelial Worsening Lab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Lactate Value: 3.2 Critical Value: 2 Lactate is a major sepsis marker demonstrating hypoperfusion of systemic organs Immediately notify provider of critical value. Assess vital signs including BP, HR, temp to give to provider. Assess for other s/s of systemic infection such as fever. Perform sepsis screen based on hospital protocol and notify sepsis team. Enact orders as prescribed including fluid replacement, cultures (1st) and administration of broad spectrum antibiotics. Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Creatinine Value: 1.5 Critical Value: Hospital dependent, usually >2-2.5 Creatinine is indicative of kidney function and elevated creatinine level means that the kidneys are not able to effectively keep up with filtration demands and therefore substances usually filtered out are Strict I&O, monitor urine quality and characteristics. Administer fluids as ordered. Assess ability to urinate (may need foley for incontinence if confused and also needing strict I&O - refer to hospital policy, foley criteria) accumulating in the blood Clinical Reasoning Begins… 1. What is the primary problem that your patient is most likely presenting? • Patient initially developed a urinary tract infection, but based on presenting data, it seems that this has progressed to a systemic level and is indicative of sepsis. 2. What is the underlying cause/pathophysiology of this primary problem? • In Jean’s case, the underlying cause would be an untreated UTI which therefore spread beyond the bladder and urethra likely to the kidneys causing systemic septic effects on the body. According to our text, “Severe sepsis is defined as a systemic inflammatory response related to an infection such as pneumonia, with dysfunction or failure of one or more organs (e.g., renal insufficiency, ARDS, or disseminated intravascular coagulation)” (Honan, pg. 305). Collaborative Care: Medical Management Care Provider Orders: Rationale: Expected Outcome: Establish peripheral IV 0.9% Establishes circulatory access for the initiation of treatment Fluid support to maintain BP and resuscitate fluid loss from dehydration Reduction of fever, antipyretic Broad spectrum antibiotic while specific cultures are pending Pain management (flank pain) and reduces anxiety IV access obtained to start treatment NS 1000 mL IV bolus Acetaminophen 650 mg BP will increase and be maintained within normal range Ceftriaxone 1g IVPB…after blood/urine cultures obtained Temperature will drop Morphine 2 mg IV push every 2 hours prn-pain Will begin to fight causative bacterial agents in the body Patient will remain relaxed and report improvement in pain level PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: What is the reason you are doing this action ● Establish peripheral IV 1 You have to establish venous access before initiating any treatment so this would come first. Given patient’s deteriorating BP it would be important to next administer fluids to provide support before other treatments. Antibiotics would be next to stop infection as soon as possible. Morphine would be next to provide pain management as patient last reported flank pain as 5/10. Acetaminophen would be last to bring down patient’s temperature and while this is a priority, her BP and cardiovascular status take priority. ● 0.9% NS 1000 mL IV 2 bolus ● Acetaminophen 650 mg 5 ● Ceftriaxone 1g 3 IVPB…after blood/urine cultures obtained ● Morphine 2 mg IV 4 push every 2 hours prn-pain Medication Dosage Calculation: Medication/Dose: Mechanism of Action: Volume/time frame to Safely Administer: Nursing Assessment/Considerations: Ceftriaxone 1g IVPB Third-gen cephalosporin antibiotic 50 ml Assess history of allergies to penicillins or other cephalosporins. Complete full dose of antibiotics. Nurse should obtain cultures prior to administration of any therapy. Binds to bacterial cell membranes to inhibit cell wall synthesis. Hourly rate IVPB: 30 mins Side effects include diarrhea, abdominal upset, oral/vaginal candidiasis. Monitor for signs of infusion reaction such as difficulty breathing, laryngeal edema, wheezing (anaphylaxis) or more moderate reaction signs such as urticaria and pruritus. Notify provider immediately. Collaborative Care: Nursing diagnosis (just the first part) 3. What nursing priority will guide your plan of care? (if more than one-list in order of PRIORITY) • Maintaining adequate hemodynamic stability • Patient is septic and hypotensive with labs demonstrating a deterioration in renal function; it is important to continually assess the patient’s vitals, pulses, and administer orders as prescribed to ensure that further complications do not arise from worsening sepsis/organ damage 4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome: Close monitoring of vitals especially BP and pulse, and urine output Antibiotic infusions as ordered Initiate fall precautions Monitor for signs of organ dysfunction, progression of instabilty Monitoring this will be indicative of response to therapy. Nurse is responsible for watching BP status after fluid bolus and alerting provider of changes in case additional support is needed. Patient’s blood pressure will normalize and be maintained after fluid bolus. Nurse is responsible for obtaining cultures beforehand and then administering antibiotics. Nurse should assess for any allergies and monitor patient closely for any infusion reactions. Fighting the infection and preventing a reaction will promote continued hemodynamic stability. Patient will receive broad spectrum antibiotics while cultures are pending without complication. Because of hemodynamic instability, patient is dizzy with position changes (orthostatic hypotension) and should have no-slip socks, a bed alarm, and a fall risk bracelet on at all times. Patient will not fall during admission. MODS can be a severe complication of sepsis and hemodynamic instability due to organ hypoperfusion. Close monitoring of I&O, especially urine output, renal function, and respiratory status are important to trend so that early changes can be caught and addressed. Patient will not develop multi organ failure as a complication. 5. What body system(s) will you most thoroughly assess based on the primary/priority concern? • Cardiovascular: BP monitoring and HR to determine response to treatment • Renal: urine output both in terms of infection and overall renal function in the setting of sepsis 6. What is the worst possible/most likely complication to anticipate?(don’t say death) • MODS (multiorgan dysfunction) due to continued septic shock and systemic organ hypoperfusion leading to organ failure 7. What nursing assessment(s) will you need to initiate to identify this complication EARLY if it develops? • Systemic monitoring of organ systems; perform thorough head to toe assessments. Monitor urine output closely and trend data. Monitor breathing pattern and auscultate lungs for changes. Monitor heart rate, rhythm, and blood pressure and track changes. Monitor body temperature and intervene as appropriate and ordered (i.e. tylenol or cool washcloths to keep patient comfortable). Signs of MODS would be worsening orientation/mental status, oliguria, tachypnea, rising lactate levels. 8. What nursing interventions will you initiate if this complication develops? • Immediately notifying the provider; fluid support, administering oxygen as needed, frequent vitals monitoring - providers orders will guide therapy. MODS is severe and life threatening. Patient will likely need ventilation and support from administration of pressors to maintain BP. 9. What psychosocial needs will this patient and/or family likely have that will need to be addressed? • Jean is fortunate in that she has a strong support system and a safe home. Patient and family should always be updated regarding her condition and the pathophysiology behind it (in a manner they can understand) to reduce anxiety. Given her age, it is important that Jean understand sepsis and that she should see a doctor any time she experiences any changes from her baseline. She had urinary pain and frequency for three days prior to admission. 10. How can the nurse address these psychosocial needs? • The nurse can act as a support person and educator for both patient and family and can explain the treatment plan and answer questions as appropriate. Evaluation: Evaluate the response of your patient to nursing and medical interventions during your shift. All physician orders have been implemented that are listed under medical management. Two Hours Later… Current VS: Most Recent: T: 101.4 F/38.6 C (oral) T: 101.8 F/38.8 C (oral) P: 116 (regular) P: 110 (regular) R: 22 (regular) R: 24 (regular) BP: 98/50 BP: 102/50 O2 sat: 98% room air O2 sat: 98% room air GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort CARDIAC: Color flushed. Skin is warm and dry centrally, but upper/lower extremities are mottled in appearance and cool to touch, heart sounds regular-S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented x2-is not consistently oriented to date and place GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four quadrants GU: No urine output the past two hours. SKIN: Skin integrity intact 1. What clinical data are RELEVANT and must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: Temp 101.4 Pulse 116 BP 98/50 RR 22 Patient still has a fever with little reduction. Still demonstrating tachycardia with worsening blood pressure. Tachypnic though oxygen saturation is within normal limits. RELEVANT Assessment Data: Clinical Significance: Cool, mottled extremities. NO URINE OUTPUT. Still disoriented. The fact that the patient is oliguric is a sign of worsening sepsis and renal system deterioration. The provider should be notified immediately of the patient’s lack of response to treatment thus far. Her cool extremities demonstrate that her cardiac output is not able to meet the demands of her whole body based on fluid volume deficit and is being reserved for her more vital areas (core). 1. Has the status improved or not as expected to this point? • Status has worsened and the provider should be contacted for additional orders to provide more hemodynamic support to the patient to preserve organ function. 2. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? • Provider needs to be notified. Plan of care should continue as is to provide continued hemodynamic support to the patient. 3. Based on your current evaluation, what are your nursing priorities and plan of care? • Priority is still to achieve and maintain hemodynamic stability through the plan of care which includes careful monitoring of vitals, urine output (I&O), administration of antibiotics and fluids, and monitoring for signs of complications such as MODS (including oliguria and tachypnea which patient is demonstrating). Given patient condition after first round of orders, she may require pressor support. Because you have not seen the level of improvement you were expecting in the medical interventions, you decide to update the physician and give the following SBAR: Situation: Jean Kelly (Age 82) admitted for sepsis secondary to UTI. Has been given a 1L fluid bolus and 1G ceftriaxone. BP is not improving and patient is now oliguric. Background: History of DMII, HLD, and HTN. Admitted after 3 days of UTI symptoms and acutely altered mental status when she could not get out of the bathroom. Has not responded to initial orders and BP, HR, urine output, RR continue to deteriorate. Assessment: Cool, mottled extremities. Fever at 101.4. Last BP 92/50. Pulse 116. Oriented to self but not time or place. Oral membranes dry and tacky. Oliguric over last two hours. Recommendation: Patient likely requires additional support. Additional fluid boluses recommended and if hemodynamic stability is not achieved then pressors may be needed. Try additional fluids first. The physician agrees with your concerns and decides to repeat the 0.9% NS bolus of 1000 mL and insertion of Foley catheter. After one hour this has completed and you obtain the following set of VS: Current VS: Most Recent: T: 100.6 F/38.1 C (oral) T: 101.4 F/38.6 C (oral) P: 92 (regular) P: 116 (regular) R: 20 (regular) R: 22 (regular) BP: 114/64 MAP: 81 BP: 94/48 MAP: 63 O2 sat: 98% room air O2 sat: 98% room air Current Assessment: GU: 200 mL cloudy urine in bag 1. Has the status of the patient improved or not as expected to this point? • Patient has definitely improved. 2. What data supports this evaluation assessment? • 200mL of urine output, increasing blood pressure, pulse within normal range, as well as decrease in fever and respiratory rate. 3. What health promotion needs does your patient need addressed? • Gerontological considerations for infection - Jean should be aware that the elderly are more susceptible to infections and complications which can occur faster in them. It is important to seek a provider as soon as there is a change in baseline. Always better to be safe. [Show More]
Last updated: 1 year ago
Preview 1 out of 21 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 22, 2022
Number of pages
21
Written in
Additional information
This document has been written for:
Uploaded
Sep 22, 2022
Downloads
0
Views
34