*NURSING > CASE STUDY > NURSING 556 Part I: Small Bowel Obstruction Mary O’Reilly, 55 years old Case Study (GRADED A) (All)
NURSING 556 Part I: Small Bowel Obstruction Mary O’Reilly, 55 years old Case Study (GRADED A)
Document Content and Description Below
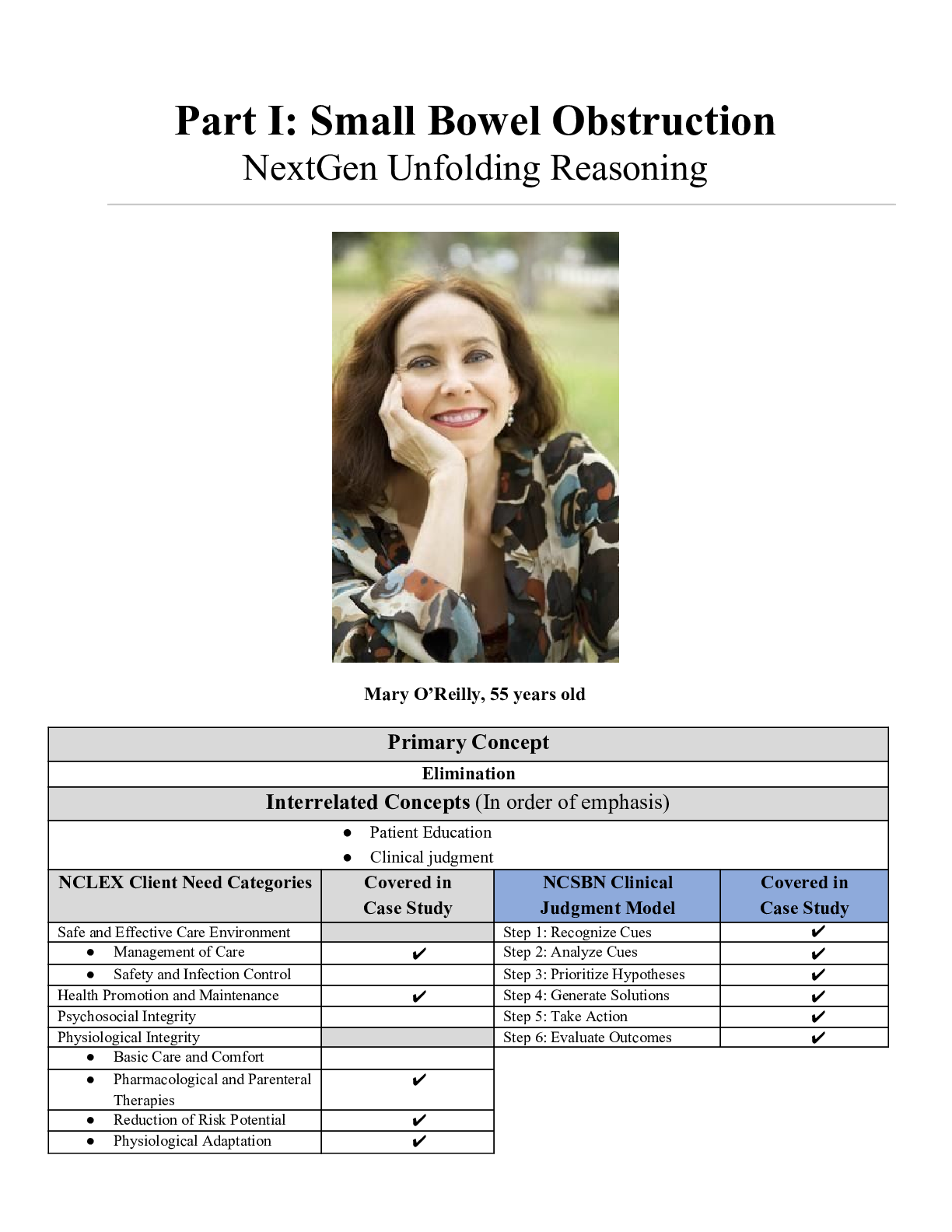
Part I: Small Bowel Obstruction NextGen Unfolding Reasoning Mary O’Reilly, 55 years old Primary Concept Elimination Interrelated Concepts (In order of emphasis) ● Patient Education �... � Clinical judgment NCLEX Client Need Categories Covered in Case Study NCSBN Clinical Judgment Model Covered in Case Study Safe and Effective Care Environment Step 1: Recognize Cues ✔ ● Management of Care ✔ Step 2: Analyze Cues ✔ ● Safety and Infection Control Step 3: Prioritize Hypotheses ✔ Health Promotion and Maintenance ✔ Step 4: Generate Solutions ✔ Psychosocial Integrity Step 5: Take Action ✔ Physiological Integrity Step 6: Evaluate Outcomes ✔ ● Basic Care and Comfort ● Pharmacological and Parenteral Therapies ✔ ● Reduction of Risk Potential ✔ ● Physiological Adaptation ✔ Present Problem: Part I: Initial Nursing Assessment Mary O’Reilly is a 55-year-old woman with a prior history of partial colectomy w/colostomy and small bowel obstruction three months ago that resolved with bowel rest and required no surgical intervention. Three days ago Mary developed a sudden onset of sharp generalized abdominal pain with nausea, vomiting and decreased output from her colostomy bag. She has had two small glasses of water today. Mary is admitted to the medical/surgical unit and you will be the nurse caring for her. You receive the following highlights of report from the emergency department (ED) nurse: ● CT of her abdomen/pelvis revealed high-grade small bowel obstruction. ● Lactate 2.8, WBC 14.7, Sodium 143, Potassium 3.7, Creatinine 1.35 ● An NG was placed and she is on low intermittent suction. She had NG output of 225 mL of bile green liquid. ● Received hydromorphone 0.5 mg IV for pain one hour ago. Abdominal pain decreased from 9/10 to 3/10 and she is resting more comfortably. ● Abd. is firm, slightly distended, with tympanic bowel sounds. ● Initial HR/BP was 102 and 92/48. ● Most recent vital signs: T: 99.8 (o) P: 78 (reg) R: 18 BP: 108/52 after 1000 mL 0.9% NS bolus 20 g. peripheral IV in left forearm. What data from the history are RELEVANT and must be NOTICED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: - Partial colectomy w/ colostomy - Small bowel obstruction 3 months ago - Sudden onset of sharp pain with N/V, decreased output from colostomy bag - Small bowel obstruction - Lactate 2.8 (HIGH) - WBC 14.7 (HIGH) - Creatinine 1.35 (HIGH) - Indicates patient cannot excrete normally due to partial colectomy - Highly likely that current problem is a small bowel obstruction since she has a history of it - S/S indicate small bowel obstruction. S/S also indicate pt may have electrolyte imbalances d/t obstructed digestion - CT reveals pt does, indeed, have an SBO - Normal = 0.5-1. High levels may indicate Type B lactic acidosis d/t regional ischemia. - Normal = 4-11K. High WBC’s may indicate infection and/or physical or emotional stress. - Normal = 07-1.2. Elevated creatinine levels signify impaired kidney function or kidney disease. Dehydration can also cause this, which is supported by patient’s recent vomiting. 1. WHY is your patient receiving these home medications? Draw lines to connect the medication to the problem it is most likely treating. (NCLEX: Pharmacologic and Parenteral Therapies) Past Medical History: Home Medications: 1. COPD 1-Umeclidinium-vilanterol 62.5/25 mcg inhaler 1 puff 2. Paroxysmal atrial daily fibrillation 2-Aspirin 81 mg PO daily 3. Coronary artery disease 2-Furosemide 20 mg PO 4. Diverticulitis daily 5. Small bowel obstruction 3-Lisinopril 5 mg PO daily 6. Partial colectomy 3-Metoprolol 25 mg PO BID w/colostomy 3-Simvastatin 20 mg PO 7. Non-dilated cardiomyopathy-EF 25% daily 1-Albuterol 0.083% neb solution 3 mL every 6 hours PRN Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment: T: 99.5 F/37.5 C (oral) Provoking/Palliative: No change in position or movement influences pain P: 94 (regular) Quality: cramping R: 16 (regular) Region/Radiation: Generalized abdomen BP: 118/64 Severity: 5/10 O2 sat: 98% room air Timing: continuous What VS data are RELEVANT and must be NOTICED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: Continuous abdominal cramping (5/10) 99.5 Temp The continuous abdominal cramping pain are signs of small bowel obstruction. The temperature is not a high temperature but could be a low grade fever and potentially become high if the bowel obstruction gets worse or infection is present, the latter of which can lead to peritonitis. Current Head to Toe Nursing Assessment: GENERAL SURVEY: Pleasant, calm, body tense, grimacing, appears uncomfortable NEUROLOGICAL: Alert & oriented to person, place, time, and situation (x4); muscle strength 5/5 in both upper and lower extremities bilaterally. HEENT: Head normocephalic with symmetry of all facial features. PERRLA, sclera white bilaterally, conjunctival sac pink bilaterally. Lips, tongue, and oral mucosa tacky dry RESPIRATORY: Breath sounds clear with equal aeration on inspiration and expiration in all lobes anteriorly, posteriorly, and laterally, non-labored respiratory effort on room air. CARDIAC: No edema, heart sounds regular S1S2, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refill. Heart tones audible and regular, S1 and S2 noted over A-P-T-M cardiac landmarks with no abnormal beats or murmurs. No JVD noted at 30-45 degrees. ABDOMEN: Abdomen round, firm, and generalized abdominal tenderness. BS tympanic in upper quadrants, hypoactive in lower quadrants GU: Voiding without difficulty, urine clear/dark amber INTEGUMENTARY: Skin pink, warm, dry, intact, normal color for ethnicity. No clubbing of nails, cap refill <3 seconds, Hair soft-distribution normal for age and gender. Skin integrity intact, skin turgor elastic, no tenting present. What assessment data is RELEVANT and must be RECOGNIZED as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential Reduction of Risk Potential/Health Promotion & Maintenance) RELEVANT Assessment Data: Clinical Significance: Abdomen round, firm, and generalized This assessment shows early signs of a bowel obstruction. Since the nurse can abdominal tenderness. BS tympanic in hear the bowel sounds in the lower quadrants, then that means the obstruction upper quadrants, hypoactive in lower has not caused cessation of movement yet. quadrants. Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: Patient is probably in pain as evidenced by reports of grimacing, body tension, and appearing uncomfortable. She’s probably also extremely worried and stressed out since she has multiple serious conditions and had a recent SBO 3 months ago. The nurse should speak to the patient in a calm, soft voice. S/he should explain every procedure performed that may be new to the patient, and keep her updated with regards to future treatment plans. After treating her physiological issues, the nurse should then take some time to engage the patient in conversation and actively listen to her concerns. Offering a back rub and/or holding her hand will show that she matters to the nurse. Part II: Put it All Together to Think Like a Nurse 1. What is the pathophysiology of the priority problem? (NCLEX Management of Care/Physiologic Adaptation) Priority Problem: Pathophysiology of Problem in OWN Words: Small Bowel Obstruction A small bowel obstruction is when a physical or nonphysical issue (twisting of intestines or decreased peristalsis) in the intestines causes blockage of the movement of stool, thereby obstructing proper elimination. Typical S/S include: abdominal pain and distention, N/V, malaise, anorexia, and severe constipation. 2. What body system(s) will you assess most thoroughly based on the primary/priority problem? Identify correlating specific nursing assessments. (NCLEX Reduction of Risk Potential/Physiologic Adaptation) PRIORITY Body System: PRIORITY Nursing Assessments: Gastrointestinal Bowel sounds Elimination (I/O of urine, output of colostomy bag) Fluid and electrolytes Palpation and auscultation of the abdomen 3. What nursing priority(ies) and goal will guide how the nurse RESPONDS to formulate a plan of care? (NCSBN: Step 4 Generate solutions/Step 5: Take action/NCLEX Management of Care) Nursing PRIORITY: To maintain baseline VS, labs in normal range, overall patient stability. GOAL of Care: To reduce/prevent any exacerbations or other conditions from occurring. Nursing Interventions: Rationale: Expected Outcome: 1. The nurse will administer prescribed pain meds PRN. 2. The nurse will monitor VS q 30 minutes and labs. 3. The nurse will conduct physical assessments q 30 minutes. 4. The nurse will administer prescribed IV fluids as ordered. 1. Maintaining an acceptable pain level by the patient and not chasing the pain. 2. Vital signs and labs can help indicate if an infection or another condition is occurring. 3. Monitoring for any change will assist in reducing any exacerbations of the pt’s condition. Abdominal pain and appearance are of particular importance since sudden, acute pain and abdominal firmness can be signs of an SBO complication. 4. Maintaining hydration will assist in keeping VS and labs in normal range, while reducing the risk of exacerbating pt’s condition. 1. Pt will remain comfortable with little to no pain, while keeping cortisol and glucose levels stable. 2. Pt’s VS and lab will remain stable with baseline. 3. Pt’s condition will remain stable from any complications or exacerbations. 4. Pt’s VS and labs will remain stable in normal range, while reducing the risk of any complications in pt’s condition. 4. What is the worst possible/most likely complication(s) to anticipate based on the primary problem? (NCLEX: Reduction of Risk Potential/Physiologic Adaptation) Worst Possible/Most Likely Complication to Anticipate: Peritonitis, tissue death caused by decreased blood supply leading to perforation and leaking of intestinal contents into peritoneum and developing an infection. Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: 1. Continue with NG suctioning to prevent obstruction from worsening. 2. Prepare the patient for surgery 1. Assessment of abdomen because a rigid-board like abdomen is a classic sign of peritonitis. 2. Assessment of abdomen for a distension 1. Place the patient on NPO per HCP orders. 2. Administer hypertonic IV fluids (3% aimed at relieving the obstruction. due to decreased peristalsis and increased fluid. 3. Auscultate bowel sounds, diminished bowel sounds is an indication. 4. Palpation of abdomen because rebound tenderness is indicative of movement of peritoneal fluid. 5. Assess the patient’s pain level since a sudden, acute increase in pain (especially with movement) is indicative of peritonitis. 6. Assess I/O because significantly less urine output or none at all can be a sign of peritonitis. NS, D51/2, D5NS, D5LR) per HCP orders. 3. Administer broad-spectrum antibiotics per HCP orders. 4. Position the patient in semi-fowlers STAT. 5. Administer non-opioid pain medications per HCP orders. 5. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: Relieve the patient’s anxiety and fear. PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse 1. The nurse will encourage the patient to share her fears and concerns. 2. The nurse will actively listen to the patient and use open ended questions with the patient. Physical comfort measures 3. The nurse will educate the patient on orders including diagnostic tests and procedures. 4. The nurse will provide a quiet and relaxing environment provided the circumstances. 5. The nurse will assess the patient’s pain level on her hourly rounds. 1. By encouraging the patient to share her fears and concerns the nurse is able to take interventions to educate the patient and help relieve those fears. 2. By actively listening and using open ended questions the nurse is participating in therapeutic communication with the patient. This will aid the nurse with the 1st intervention. 3. By educating the patient the nurse is able to relieve the patient’s anxiety by decreasing what is unknown by the patient. 4. A quiet and relaxing environment will help with the patient’s discomfort by decreasing stimuli that would add the anxiety. 5. Although the patient is calm, she appears uncomfortable and in pain. Thus, the nurse should ask her to honestly rate her pain level so relief measures can be implemented. 1. The patient will verbalize feelings of reduced fear and anxiety. 2. The patient will develop a sense of trust with the nurse. 3. The patient will have a clear idea of her treatment regime, reducing any unnecessary stress and physical discomfort. 4. The patient will verbally report a lower level of pain using a 0/10 scale. 5. The patient will be able to rest more easily. Collaborative Care: Medical Management 6. State the rationale and expected outcomes for the medical plan of care. (NCLEX Pharm. and Parenteral Therapies) Care Provider Orders: Rationale: Expected Outcome: 1. NPO w/ice chips 1. In case the patient needs to have surgery to fix the issue. 1. The patient will not feel thirsty, maintain adequate hydration with lowered risk of aspiration during surgery. 2. 0.9% NS IV 100 mL/hour 2. Since the patient is NPO, the patient would need to be hydrated as well. So the NS keeps a continuous flow of hydration. 2. The patient will remain hydrated for the duration 3. Hydromorphone 0.25-0.5 mg IV every 2 hours PRN pain 3. This is for the pain that the obstruction is causing. . 3. The patient will not complain of pain. 4. NG low intermittent suction (LIS) 4. To help decompress the air and fluid from the bowel. 4. Tube will not adhere to the gut wall; fluid will not build up in intestines, thereby preventing vomiting. 5. Hold all home meds while NPO 5. In case the patient needs to have surgery. Lowers risk of aspiration of pills and ensures anesthesia can be administered without interacting with other meds. 5. Patient is adequately prepared for surgery 6. Assess colostomy output every 4 hours 6. The nurse does not want the patients bag to become full of stool because it could leak and cause skin breakdown 6. The patient’s colostomy bag will not become irritated around the skin or become too full. 7. Basic metabolic panel (BMP) in morning 7. BMP shows the electrolytes. The nurse can see if the patient is having an electrolyte imbalance, especially if the patient just came back from surgery, NPO, and/or has been vomiting. 7. The nurse will find the patient to have slight electrolyte imbalances due to the suctioning, NPO, and from the decreased bowel sounds. 8. Complete blood count (CBC) in morning 8. The nurse would want to look at the WBC to see if there is an infection or the H&H is high due to dehydration. 8. The nurse will find the patient to be within normal limits if the obstruction was caught in time. 9. Lactate in morning 9. The nurse will want to monitor the patient’s lactate because of the suction from the NGT or if the patient was vomiting. 9. The lactate may be more basic due to the suctioning from the NGT. 10. Consult general surgery 10. Due to the signs and symptoms present, the nurse could see that a bowel obstruction is happening. The surgeon can then come and consult the patient and proceed to the plan of care. 10. The surgeon will want to perform surgery on the patient to correct the obstruction. 7. Which orders do you implement first? Why? Care Provider Orders: Order of Priority: Rationale: ● NPO w/ice chips ● Consult general surgery ● 0.9% NS IV 100 mL/hour ● Hydromorphone 0.25-0.5 mg IV every 2 hours PRN pain ● NG low intermittent suction (LIS) ● Hold all home meds while NPO 1. NG low intermittent suction (LIS) 2. Hydromorphone 0.25-0.5 mg IV every 2 hours PRN pain 3. 0.9% NS IV 100 mL/hour 4. Hold all home meds while NPO 5. NPO w/ice chips 6. Consult general surgery 1. Stomach decompression and the removal of stomach content takes priority due to the ABC approach. Unremoved stomach content can lead to aspiration of stomach contents. 2. Managing the patients pain and keeping it at an acceptable level should be the next priority to keep the patient comfortable. 3. Patient is exhibiting signs of dehydration; amber urine, and lips, tongue, and oral mucosa are tacky dry so keeping the patient hydrated is important. 4. Holding all medications should be done next to avoid any interruptions if surgery is required. 5. Providing ice chips is a comfort measure that should be done throughout the shift. 6. Consulting the general surgeon can take place after ABD management and comfort measures have taken place since the patient is not in need of immediate surgery. Lab Results: Part II: Interpreting Diagnostic Data Complete Blood Count (CBC) WBC HGB PLTs % Neuts Bands Current: 12.2 11.9 145 84 0 Yesterday: 14.7 12.2 158 89 0 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: - WBC’s decreased - Increased WBC can indicate inflammation, infection, or hemorrhage. Even though the WBC’s have reduced, it may not be a sign of improvement. All worsening - Hemoglobin decreased - The patient's decreased hemoglobin may indicate internal bleeding from the SBO, and may ultimately lead to rupture of the bowels. - Platelets decreased - Decreased platelets can also be an indication of hemorrhage. - Neutrophils decreased - Neutrophils are a good indicator of infection; however, the neutrophils are still very high. Basic Metabolic Panel (BMP) Na K Gluc. Creat. Current: 142 3.5 142 0.95 Yesterday: 143 3.9 152 1.29 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: - K - Glucose - Creat. - Potassium WNL - The decreasing glucose level is also good. This is most likely occurring because of the NPO orders placed. - Decreased creatinine is probably because of the IV fluids adequately hydrating the patient. Improving Misc. Lactate Current: 0.9 Most Recent: 2.8 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? (NCSBN: Step 1 Recognize cues/NCLEX Reduction of Risk Potential Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: Lactate This could be a possible indication of improved circulation and oxygen perfusion in the obstructed small intestines. Surgical intervention may not be necessary at this time. Improving Part III: Evaluation: Three Hours Later… 1. The nurse evaluates the patient by assessing after implementing the plan of care. Interpret clinical data to determine if the patient status is improving, declining, or reflects no change. (NCSBN: Step 6 Evaluate outcomes/NCLEX: Management of Care) RELEVANT Assessment Data: Clinical Significance: Improving-Declining No Change: Firm/rigid Abdomen Temperature 101.7 (HIGH) This assessment data shows that the patient’s obstruction most likely ruptured. The rigid/firm abdomen and high temperature are classic signs of peritonitis. This is an emergency. Declining Pulse: 118 RR: 24 2. Has the overall status of your patient improved, declined, or remain unchanged? If your patient has not improved, what other interventions need to be considered by the nurse? (NCSBN: Step 6 Evaluate outcomes/NCLEX: Management of Care) Overall Status: Additional Interventions to Implement: Expected Outcome: Declining - Inform MD STAT of sudden, acute decline in status - Raise HOB if down to prevent aspiration of any residual stomach contents and give patient bag to vomit in. - MD made aware of declining condition and further interventions requested under his/her guidance. - Patient’s airway will not be physically obstructed - Continuously watch vitals. Pulse may continue to rise; BP may lower; temperature is very high, which is a sign of infection. Act appropriate with fluctuation (e.g. administer Tylenol for fever per MD orders, assistive O2 if Sat drops below 92%) - Patient’s vitals will remain stable. If not, further interventions will be performed to maintain stability. - Administer PRN pain medication as ordered, request MD up dosage and/or increase frequency if pain does not subside with administration - Patient reports a tolerable pain level, ideally <5/10. Situation: Name/age: Mary O’Reilly, 55 years old BRIEF summary of primary problem: pt admitted with complaints of sharp abdominal pain with N/V and decreased colostomy bag output spanning over 3 days. Diagnosis of small bowel obstruction as indicated by CT scan. Patient was initially stabilized upon admittance to the med-surg floor, but is now experiencing a sudden decline. She is currently experiencing 10/10 abdominal pain, is diaphoretic, and her abdomen is firm and rigid. Background: Primary problem/diagnosis: Small bowel obstruction RELEVANT past medical history: Partial colectomy with colostomy RELEVANT background data: Small bowel obstruction 3 months ago that required no surgical intervention. Assessment: Vital signs: T 101.7F, P 118, R 24 (HIGH), BP 139/88, O2 98%, pain 10/10 RELEVANT body system nursing assessment data: GI: firm, rigid abdomen with localized 10/10 pain; nausea Integ: chills, pale, diaphoretic RELEVANT lab values:. K 3.5 (trending down, WNL) Creatinine 0.95 (trending down, WNL) Lactate 0.9 (trending down, WNL) Recommendation: Suggestions to advance plan of care: MD intervention STAT as pt may have perforation with possible peritonitis, CT of abdomen, increase hydromorphone dosage and/or frequency STAT, paracentesis if necessary Radiology: Abdominal CT Results: Clinical Significance: Probable perforated small bowel with free intraperitoneal air. Results indicate a life-threatening situation as perforation of the bowel can lead to peritonitis and/or ischemia and necrosis of abdominal tissue. 3. Based on the current status of your patient, what are the CURRENT nursing priorities and plan of care? (Management of Care) CURRENT Nursing PRIORITY: Ensure the patient is stabilized for surgery by preventing deficient fluid volume and infection. PRIORITY Nursing Interventions: Rationale: Expected Outcome: 1. The nurse will administer hypertonic IV fluids per HCP orders. 2. The nurse will administer broad-spectrum antibiotics per HCP orders. 3. 4. The nurse will monitor the patient’s WBC count. 4. The nurse will assess VS qh, noting progressive hypertension, tachycardia, tachypnea and fever. 1. A hypertonic solution will remove fluid out of the cells and into the vascular space, combating the fluid loss caused by the inflammatory response. 2. This is a prophylactic measure for infections. 3. A WBC count of 20,000 or higher would indicate the presence of an infection. 4. Those findings would indicate septic shock caused by an infection. 1. The patient will not develop hypovolemia. 2. The patient will not develop an infection as evidenced by showing no VS or labs indicating an infection. 3. Patient’s WBC count will remain steady or decrease to WNL. 5. Patient’s vitals will remain stable. 4. To develop clinical judgment, reflect on your thinking by answering the following questions: What did you do well in this case study? What knowledge gaps did you identify? Applied knowledge learned about SBO in pediatrics and MSIII to determine the main issues and possible complications with this patient. Analyzing laboratory values, I need to improve in that aspect. What did you learn? How will you apply learning caring for future patients? Interventions that could be used during the care of a patient with SBO. As well as interventions performed, their significance and purpose. Performing interventions for the current needs of a patient but also in anticipation of what the patient’s condition may escalade to, in this case surgery. [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 25, 2022
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Aug 25, 2022
Downloads
0
Views
28









 Correct Study Guide, Download to Score A.png)
 Correct Study Guide, Download to Score A.png)

