Health Care > Summary > Summary Rasmussen College - PN 2 PN2 Exam #2 Study Guide (complete latest guide) (All)
Summary Rasmussen College - PN 2 PN2 Exam #2 Study Guide (complete latest guide)
Document Content and Description Below
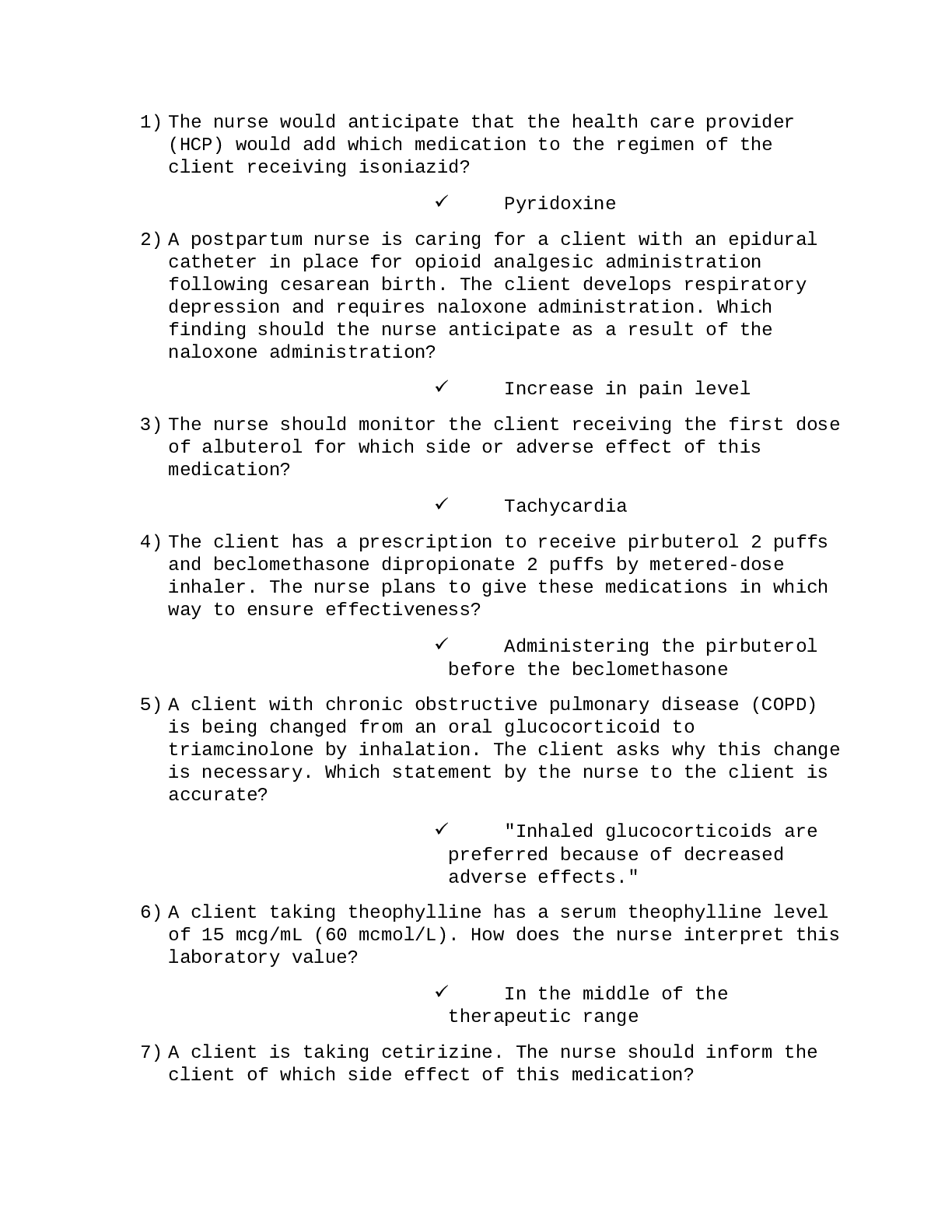
PN2 Exam 2 Study Guide. ASTHMA • Characterized by exacerbations of acute airway inflammation • Airway obstruction occurs d/t bronchoconstriction, mucous, or inflammation when exposed to trigger Cl... inical Manifestations: • High pitched, wheezing lung sounds • Cough • SOB • Chest tightness • Worsens at night or when triggers are present Medications: • Short Acting= Albuterol, Proventil, Ventoli • Long Acting= Serevent • Corticosteroids= Serevent, Advair Education: • Avoid triggers • Stop/avoid smoking • Teach which inhaler is rescue Exacerbation Interventions: • Give short-acting beta agonist • IV corticosteroids depending on severity • O2 via nasal cannula • High-fowler’s position • Calm atmosphere Questions: If a pt. is having an asthma attack how would you expect it to affect their VS? • At first RR increased then decreased as attack progresses • Tachycardia >120 • Decreased BP If you give a pt. Albuterol, what type of side effects would you expect to see? • Increased HR • Tremors What are rescue medications for Asthma? • Short-acting beta agonists (Albuterol) EPITAXIS • Nose bleed – d/t trauma, allergies, drug use • Most frequent ED complaint Interventions & Treatment: • Anterior portion of nose = apply direct pressure for 5-10 while leaning forward • Apply silver nitrate • Apply lidocaine/ep with cotton pledge for 5-10 minutes • Nasal packing for 2-5 days • Educate on prevention – Vaseline, humidifiers COPD • Chronic obstructive pulmonary disease – emphysema & chronic bronchitis • Causes= air pollution, occupation, smoking Primary Symptoms: • Cough • Sputum production • DOE – Dyspnea On Exertion Clinical Manifestations: • Wheezes or crackles heard in lungs • Prolonged expiratory phase • Distant heart sounds • Orthopneic position • Barrel chest • Use of accessory muscles • Weight loss (dyspnea with eating) • Late phase= clubbing to nails, right-sided HF, chronic cyanosis Medications: • Avoid frequent use of cough suppressants (antitussives) because coughing is a protective mechanism • Limit narcotic use d/t respiratory depression can worsen hypercapnia • Beta-Adrenergic Agonists: Albuterol, formoterol • Anticholinergics: Atrovent, Spiriva • Corticosteroids: short course only • Methylxanthines: Theophylline (limited) Interventions & Education: • Pursed lipped breathing • Controlled coughing • Controlled O2 therapy (1-2 L) • Low sodium diet • Diaphragmic breathing • Conserve energy • Small frequent meals • Increase fluids • BiPAP RAYNAUD’S DISEASE • Bilateral vasospasms; peripheral artery occlusive disease triggered by cold & stress Clinical Manifestations: • Pain & cyanosis followed by redness and pain (when warmed up) • Pain is intermittent, extremities are numb & cold & may have swelling/ulcerations Education: • Stop smoking • Exercise • Control stress • Avoid extreme temperatures ALLERGIC RHINITIS Prevention: • Remove carpet • Keep pets out of house or out of bedrooms • Wash linens in hot water • Avoid heat & humidity • Avoid feather pillows • Avoid cigarette smoke Medications: • Fexofenadine (Allergra) = non-drowsy • Pseudoephedrine (Sudafed) = non-drowsy • Diphenhydramine (Benadryl) = drowsy CYSTIC FIBROSIS • An inherited, recessive, chronic, progressive, and frequently fatal disease of the body’s exocrine mucus producing glands • Primarily affects the respiratory, digestive, and intestinal systems and pancreas • Each parent passes the recessive gene to a child Possible Complications: • Lung abscesses • Chronic bronchitis • Honeycomb lung • Bronchiectasis • Chronic pancreatitis • Malabsorption • Cor pulmonale Clinical Manifestations: • Apical crackles • Frequent infections • Purulent secretions • Productive cough • Wheezing • Dyspnea • Recurrent infections • Bronchiectasis • Infiltrates • Scarring (CXR) • Increased chest circumference • Hyper-resonance with percussion • Clubbing • Gassiness • Diabetes • Pancreatic insufficiency • Pancreatitis • Meconium ileus • Diarrhea • Abnormal sweat Cl concentrations • Infertility Treatment: • Referral to regional CF center • Focus: clearance and reduction of lower airway secretions, prevention & treatment of respiratory infections, pancreatic enzyme replacement and adequate PO intake, psychosocial support. • Surgery-lung transplant, long wait-list Interventions: • Pancreatic Enzymes (may need replacement) • Bulky, foul-smelling stools (malabsorption) • Give adequate salt • TF/parenteral nutrition • Daily weight • Iron supplements PNEUMONIA • Acute or chronic infection of one or both lungs caused by bacteria or virus Risk Factors: • Increased age • Immunocompromised • Diabetes • CHF • Active malignancies • Chronic diseases (i.e. sickle cell anemia) Clinical Manifestations: • Fever/chills • Productive or dry cough • Tachycardia • Cyanosis • Joint pain/aches • Hypotension • Headache • Mood swings • Anorexia • Pleuritic chest pain • Dyspnea • Crackles in lungs Diagnostics: • CBC • Chest x-ray Treatment: • Antibiotics • Possible O2 • Pneumonia vaccine • Rest & fluids • Incentive spirometer, cough & deep breathing BUERGER’S DISEASE • Occlusive disease mostly in small/medium arteries • Associated with clot formation and fibrosis of vessel wall Cause/Education: • Smoking – especially young male smokers • Stopping smoking will stop disease progression Clinical Manifestations: • Thickened nail beds • Intermittent claudication • Cramps in legs after exercise • Blackish ulcerations on skin • Extreme sensitivity to hot & cold • Pain in digits • Weak/thread peripheral pulses Diagnostics: • Plethysmograph studies of the digits (early stages) • Doppler U/S • Arteriograms - extent of disease process ANEMIA • Low hemoglobin (RBC) level • 1st cause = blood loss/hemorrhage • 2nd cause = decreased RBC production d/t malnutrition, renal disease, or bone marrow suppression • 3rd cause = destruction of RBC/abnormal RBC structure (sickle cell anemia=crescent shaped) Clinical Manifestations: • Fatigue • Weakness • Tachycardia • Hypotension • Hypoxia, SOB • Pallor • Chest pain Diagnostics: • Full CBC • Iron studies & Serum B12 • Haptoglobin & Erythropoietin • Bone Marrow Aspiration Treatment: • Iron replacement PO/IV • Vitamin B12 IM/PO • Folic Acid PO (green leafy veggies, liver, fruits, cereal) • Erythropoietin • RBC infusion • O2 administration (especially in sickle cell) • Hemodynamic & cardiac monitoring TONSILLITIS • History of otitis media, hearing difficulties, sore throat w/ swallowing Clinical Manifestations: • Sore throat, change/loss of voice • Reddened tonsils • Swollen/tender neck lymph nodes • Fever • White/yellow coating on tonsils • Snoring Diagnostics: • Throat culture for group A strep. & bacterial infection • CT if infection present to see if it spread to neck region • Pre-op CBC to assess for anemia/infections Tonsillectomy Education: • Report= signs of hemorrhage, fever, excessive vomiting, unrelieved pain, excessive coughing or swallowing • Drink minimum 8 glasses of water a day • Soft foods for first few days • Avoid smoking & heavy lifting • No gargling – can irritate surgical site AORTIC ANEURYSM • Permanent bulging and stretching of an artery – dilated 2x or greater in size • Most common = Abdominal Aortic Aneurysm (AAA) Risk Factors: • Hypertension = #1 risk • Smoking • Hyperlipidemia AAA Clinical Manifestations: • Nausea/vomiting • Back pain d/t pressure on spinal nerves • Pulsation in upper abdominal midline • Auscultation of a bruit at aneurysm site – DO NOT palpate Thoracic Aorta Clinical Manifestations: • Severe back pain-compression of surrounding tissues • Bronchial obstruction & hoarseness • Dyspnea & dysphasia • Aphonia-r/t pressure on laryngial nerve • Pulsating mass about suprasternal notch Diagnostics: • X-ray to identify the location of the mass • CT scan • Duplex Ultrasonography • Transesophageal Echocardiography - thoracic aneurysms Treatment: • Anti-hypertensives • Anti-anxiety medications • Surgery for aneurysms >6cm or are rapidly growing • Aneurysms <6cm monitor with ultra sound every 6 months HEMOPHILIA • Hereditary bleeding disorder resulting in deficient clotting factors (VII, IX, & X) • Hemophilia A= VII deficient, from mothers to sons • Hemophilia B= Christmas disease, from mothers to sons • Hemophilia C= IX deficient, autosomal recessive • Von Willebrand’s disease Clinical Manifestations: • Joint & muscle pain • Hemorrhages • Bruises easily Complications: • Untreated joint bleeding can cause permanent damage Diagnostics: • Platelet levels • Factor assay tests • Coagulation tests .......................................continued [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 16, 2020
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Dec 16, 2020
Downloads
0
Views
58





NSG110 AMERICANS RATE NURSES HIGHEST ON HONESTY, ETHICAL STANDARDS.png)
.png)


