*NURSING > EXAM > Rasmussen College: NUR 2755 Exam 1 (002) MDC IV Latest 2021/2022,100% CORRECT (All)
Rasmussen College: NUR 2755 Exam 1 (002) MDC IV Latest 2021/2022,100% CORRECT
Document Content and Description Below
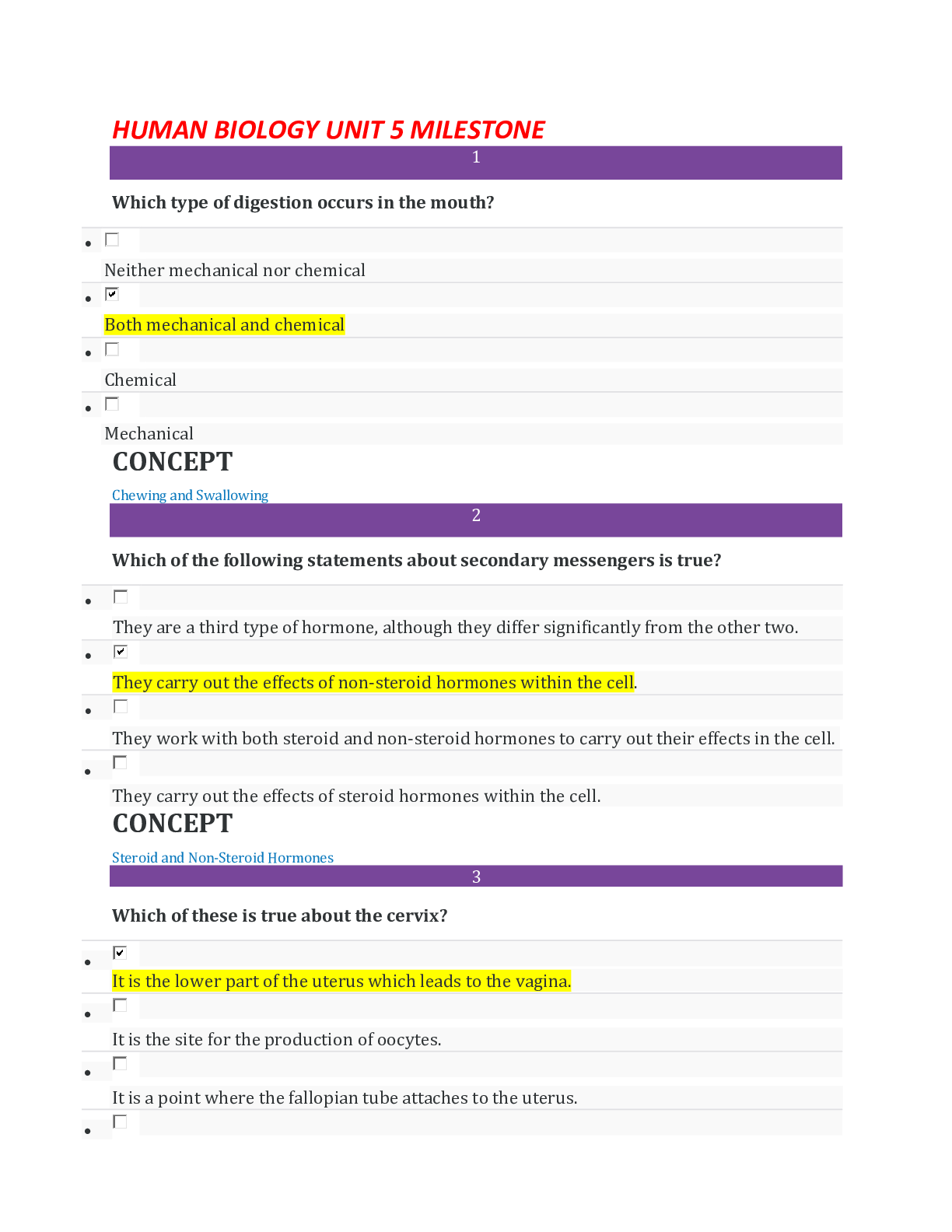
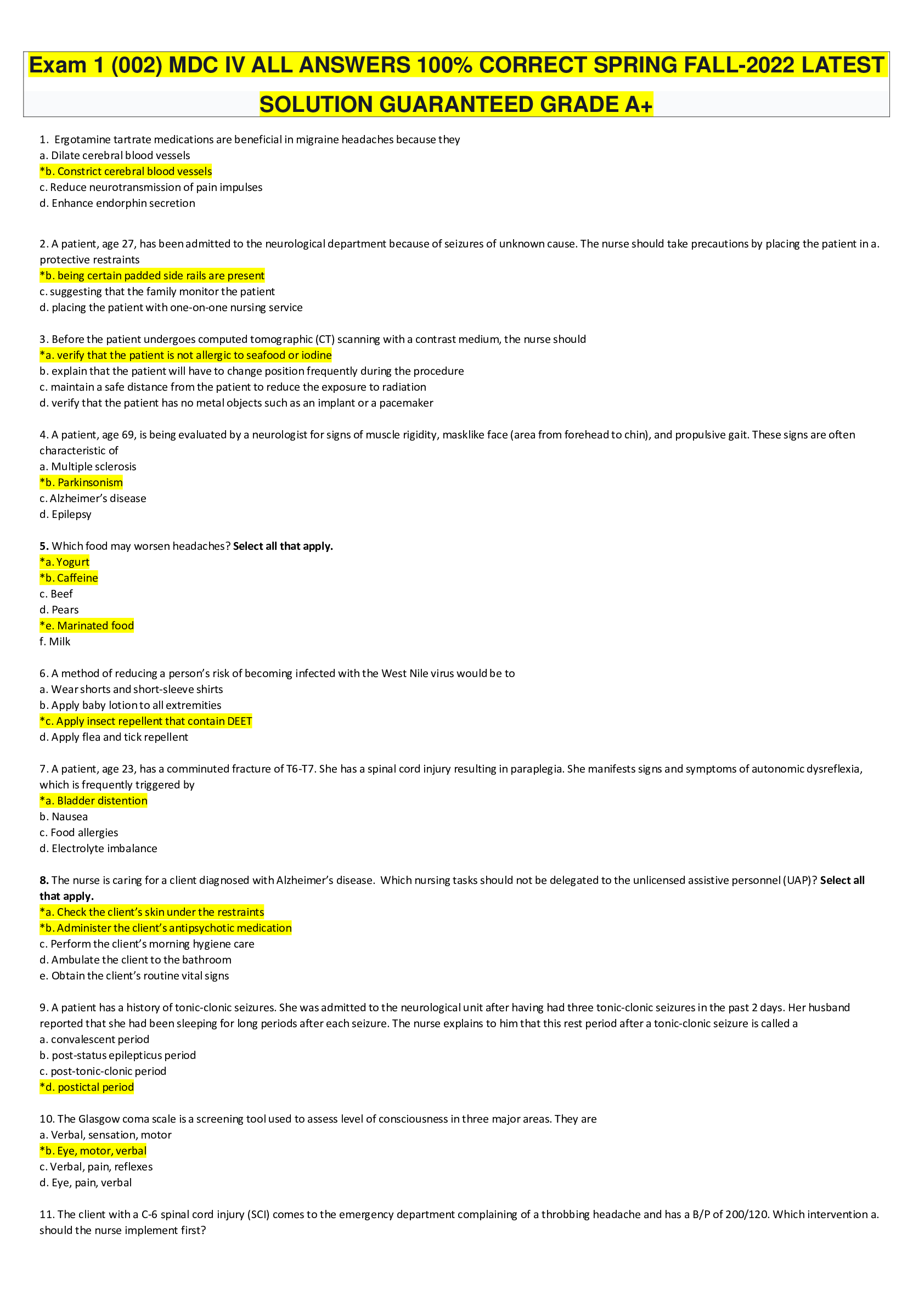
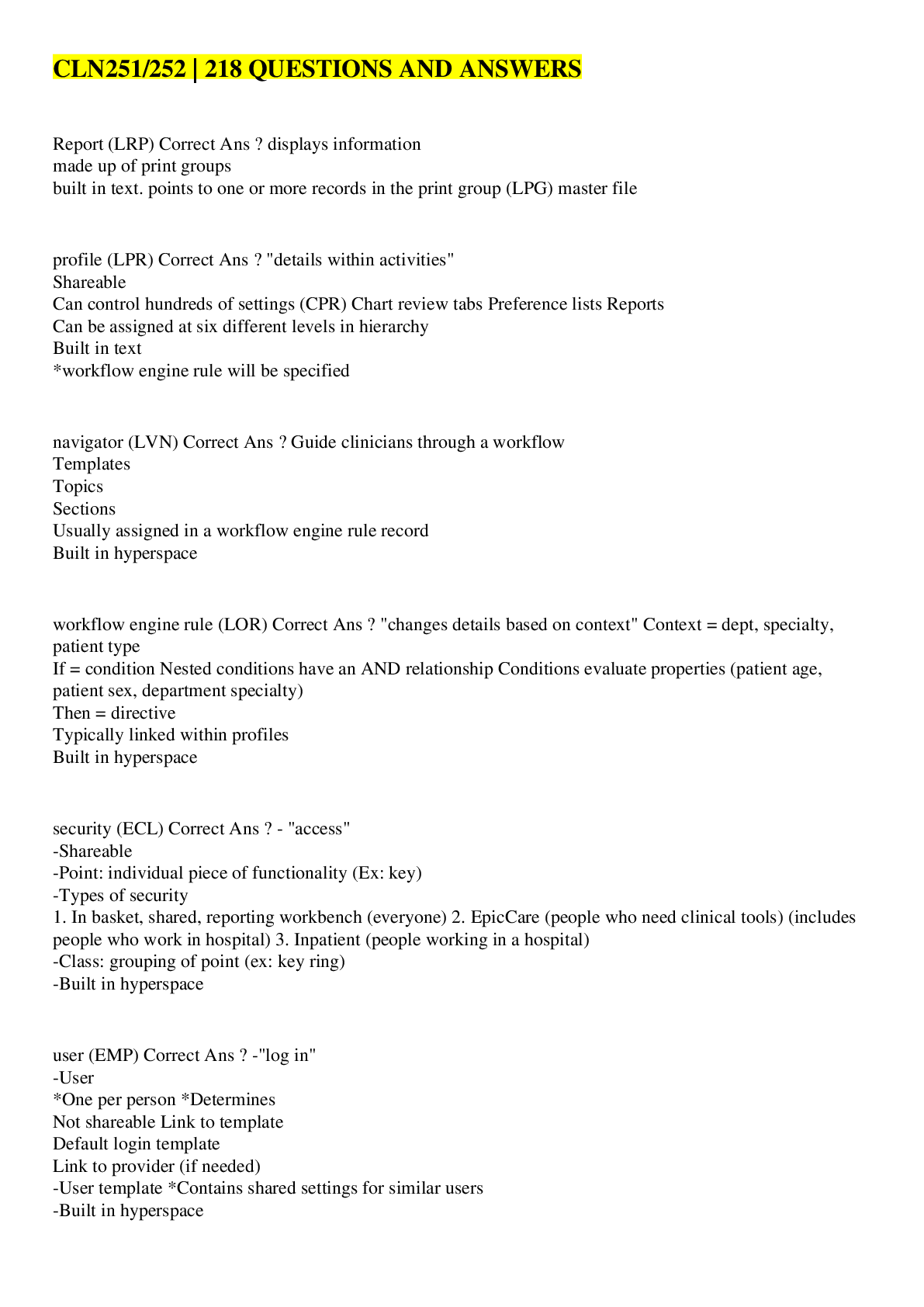
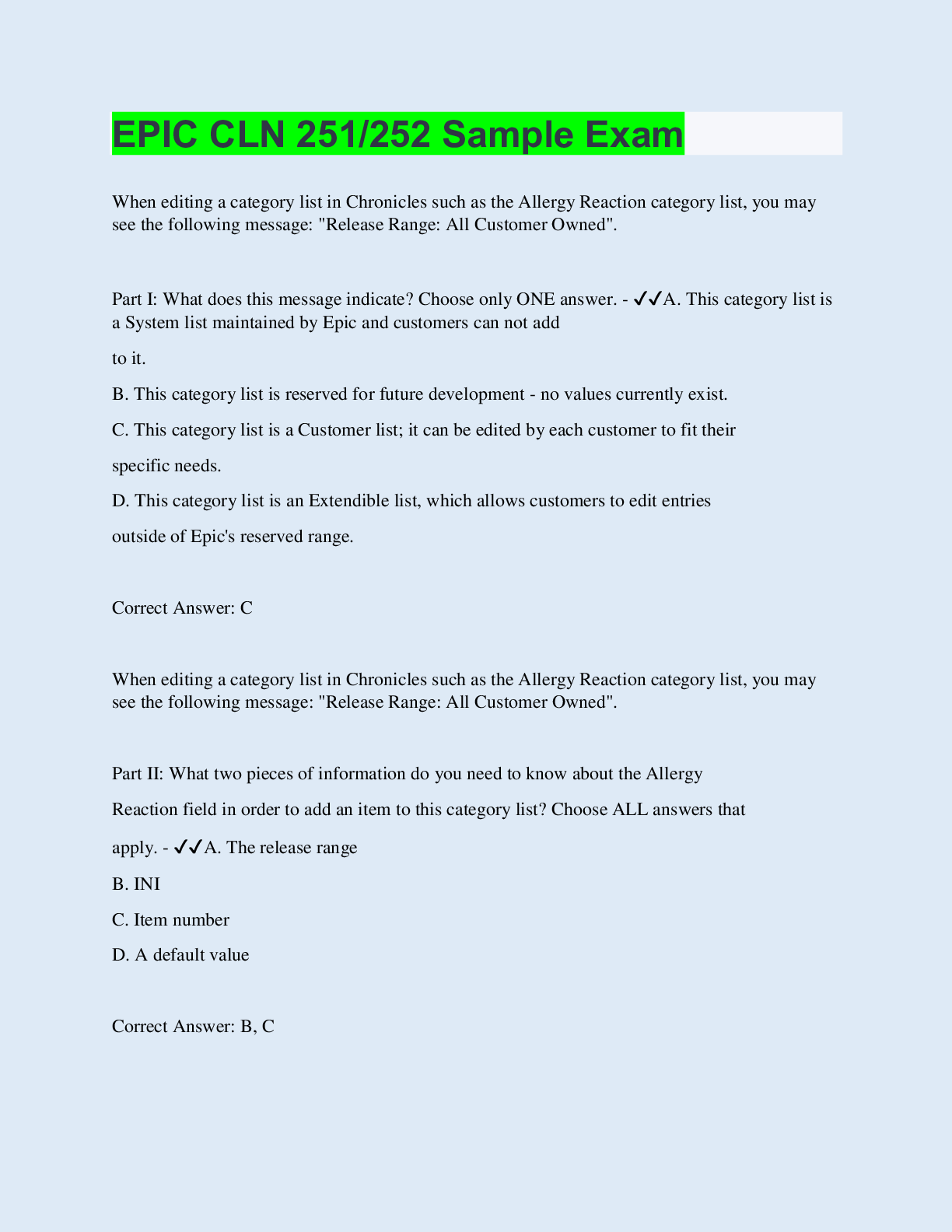
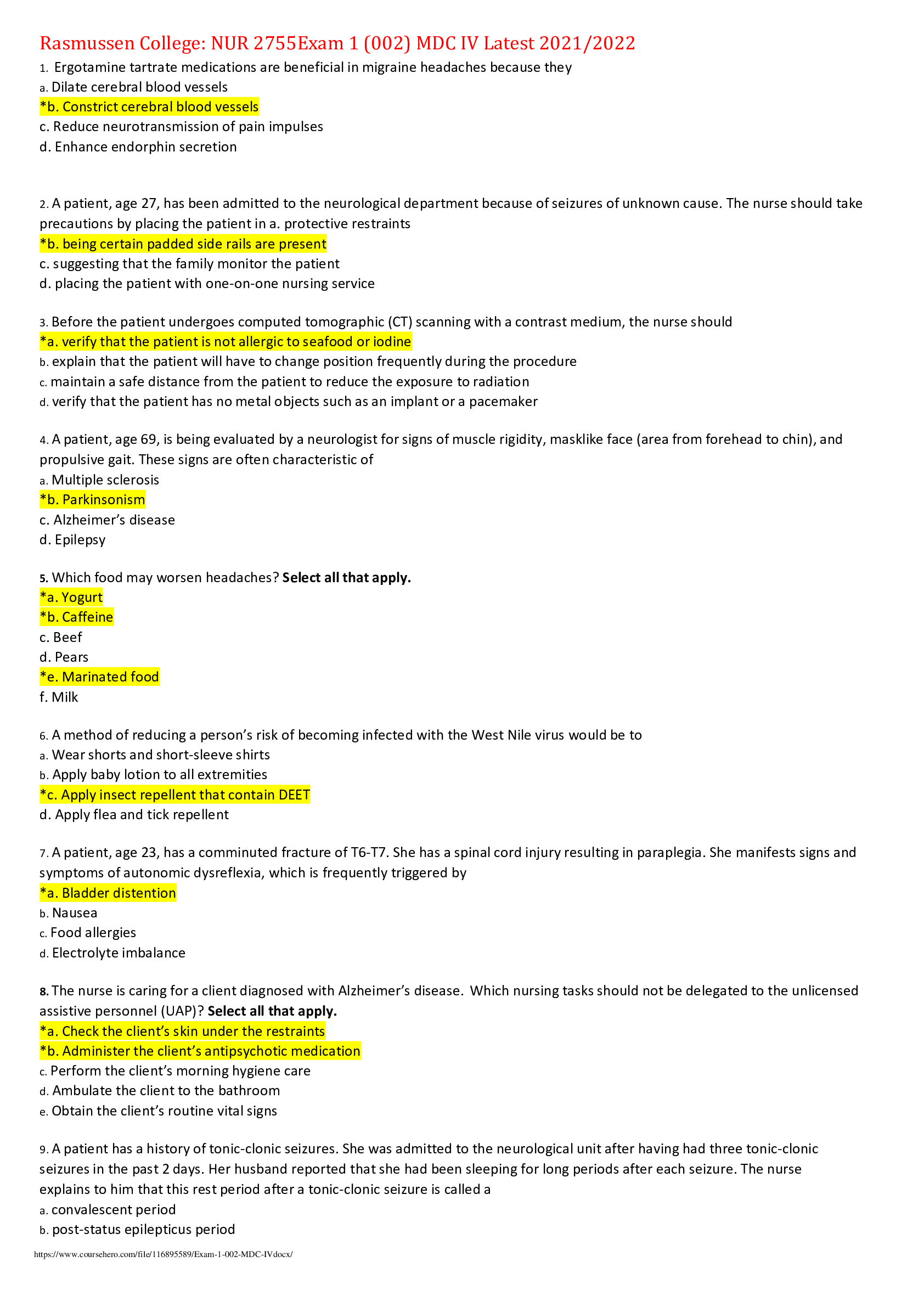
Rasmussen College: NUR 2755Exam 1 (002) MDC IV Latest 2021/2022 1. Ergotamine tartrate medications are beneficial in migraine headaches because they a. Dilate cerebral blood vessels *b. Constrict c... erebral blood vessels c. Reduce neurotransmission of pain impulses d. Enhance endorphin secretion 2. A patient, age 27, has been admitted to the neurological department because of seizures of unknown cause. The nurse should take precautions by placing the patient in a. protective restraints *b. being certain padded side rails are present c. suggesting that the family monitor the patient d. placing the patient with one-on-one nursing service 3. Before the patient undergoes computed tomographic (CT) scanning with a contrast medium, the nurse should *a. verify that the patient is not allergic to seafood or iodine b. explain that the patient will have to change position frequently during the procedure c. maintain a safe distance from the patient to reduce the exposure to radiation d. verify that the patient has no metal objects such as an implant or a pacemaker 4. A patient, age 69, is being evaluated by a neurologist for signs of muscle rigidity, masklike face (area from forehead to chin), and propulsive gait. These signs are often characteristic of a. Multiple sclerosis *b. Parkinsonism c. Alzheimer’s disease d. Epilepsy 5. Which food may worsen headaches? Select all that apply. *a. Yogurt *b. Caffeine c. Beef d. Pears *e. Marinated food f. Milk 6. A method of reducing a person’s risk of becoming infected with the West Nile virus would be to a. Wear shorts and short-sleeve shirts b. Apply baby lotion to all extremities *c. Apply insect repellent that contain DEET d. Apply flea and tick repellent 7. A patient, age 23, has a comminuted fracture of T6-T7. She has a spinal cord injury resulting in paraplegia. She manifests signs and symptoms of autonomic dysreflexia, which is frequently triggered by *a. Bladder distention b. Nausea c. Food allergies d. Electrolyte imbalance 8. The nurse is caring for a client diagnosed with Alzheimer’s disease. Which nursing tasks should not be delegated to the unlicensed assistive personnel (UAP)? Select all that apply. *a. Check the client’s skin under the restraints *b. Administer the client’s antipsychotic medication c. Perform the client’s morning hygiene care d. Ambulate the client to the bathroom e. Obtain the client’s routine vital signs 9. A patient has a history of tonic-clonic seizures. She was admitted to the neurological unit after having had three tonic-clonic seizures in the past 2 days. Her husband reported that she had been sleeping for long periods after each seizure. The nurse explains to him that this rest period after a tonic-clonic seizure is called a a. convalescent period b. post-status epilepticus period c. post-tonic-clonic period *d. postictal period 10. The Glasgow coma scale is a screening tool used to assess level of consciousness in three major areas. They are a. Verbal, sensation, motor *b. Eye, motor, verbal c. Verbal, pain, reflexes d. Eye, pain, verbal 11. The client with a C-6 spinal cord injury (SCI) comes to the emergency department complaining of a throbbing headache and has a B/P of 200/120. Which intervention a. should the nurse implement first? b. Place the client on a telemetry unit c. Complete a neurological assessment *d. Insert an indwelling urinary catheter e. Request a STAT CT scan on the head This study source was downloaded by 100000802531269 from CourseHero.com on 07-23-2022 11:38:45 GMT -05:00 12. Important nursing measures needed when feeding a hemiplegic patient include: Select all that apply. a. Mixing liquids and solid foods together b. Taking the patient’s dentures out to prevent choking *c. Offering small bites of food *d. Checking the affected side of mouth for food accumulation e. Elevating the patient to no more than 30 degrees *f. Adding a thickening agent to liquids 13. If a patient with a head injury has drainage from the nose or ears, which nursing intervention would be appropriate? a. Cleanse the ear or nose with a soft cotton-tipped swab b. Gently suction the nasal cavity *c. Allow the patient to wipe the nose or ears, but not blow the nose or place anything in the external ear d. Place a pressure dressing over the ear 14. A patient has recently suffered a stroke with left-sided weakness. She has problems with choking, especially when she drinks thin liquids. What nursing interventions would be most helpful in assisting this patient to swallow safely? a. Having her avoid all liquids *b. Instructing her to tuck her chin when swallowing c. Giving her sips of water with each bite d. Having her turn her head to the left 15. A patient, age 52, is brought to the emergency department by ambulance after she hit her head on her bathroom sink and fell unconscious to the floor. Which assessment should the nurse perform first? a. History of health problems *b. Patency of airway c. Neurological status d. Status of bodily functions 16. The patient, injured in an automobile accident, is being evaluated in the emergency department for possible head injury. Which test should not be done if there is an indication of increased intracranial pressure? a. CT scan b. MRI scan *c. Lumbar puncture d. Electroencephalogram 17. A patient’s neurological status deteriorates over hours, and a craniotomy is performed to evacuate the hematoma. Which nursing intervention is indicated to help decrease the threat of increased intracranial pressure? *a. Elevate the head of the bed 30 degrees b. Cluster nursing interventions to provide uninterrupted periods of rest c. Teach him to cough and deep breathe to prevent the necessity for suctioning d. Teach him to hold his breath and bear down while repositioning in bed 18. A patient has been injured in a motorcycle accident and is presenting with signs and symptoms of increased intracranial pressure. What is the most significant sign or symptom of increased intracranial pressure? a. Pupil changes b. Ipsilateral paralysis c. Vomiting *d. Decrease in the level of consciousness 19. The three components of Cushing's response are: Select all that apply. a. Increased pulse rate b. Increased blood pressure *c. Widened pulse pressure *d. Bradycardia *e. Increased systolic blood pressure f. Uncontrolled thermoregulation 20. A patient, age 69, is being evaluated by a neurologist for signs of muscle rigidity, masklike face (area from forehead to chin), and propulsive gait. These signs are often characteristic of a. Multiple sclerosis *b. Parkinsonism c. Alzheimer’s disease d. Epilepsy 21. A patient has a head injury and is presenting with signs and symptoms of increased intracranial pressure. Which nursing intervention would be helpful in reducing this pressure? *a. Place the neck in a neutral position to promote venous drainage b. Suction hourly to stimulate the cough reflex c. Add extra blankets to keep the patient warm d. Turn the patient frequently to prevent skin impairment This study source was downloaded by 100000802531269 from CourseHero.com on 07-23-2022 11:38:45 GMT -05:00 22. A patient has been diagnosed with organic brain pathology. He is presenting with signs and symptoms of total or partial loss of the ability to recognize familiar objects or people through sensory stimulation. This condition is called a. Apraxia *b. Agnosia c. Aphasia d. Dysphagia 23. Myasthenia gravis (MG) is an autoimmune disease of the neuromuscular junction characterized by the fluctuating weakness of certain skeletal muscle groups. The use of intravenous immune globulin a. increases anxiety and depression *b. reduces the production of acetylcholine antibodies c. removes the antibodies produced by the autoimmune response d. increases the production of acetylcholine antibodies 24. As the result of a stroke, a patient has difficulty discerning the position of his body without looking at it. In the nurse’s documentation, which would best describe the patient’s inability to assess spatial position of his body? a. Agnosia *b. Proprioception c. Apraxia d. Sensation 25. Which body system would the nurse choose to closely monitor in a patient diagnosed with Guillain-Barré syndrome? a. CNS b. GI *c. Respiratory d. Cardiovascular 26. In assessing a patient with suspected Bell’s palsy, what clinical manifestations might be present? *a. Inability to wrinkle forehead and pucker lips b. Inability to touch nose with finger with eyes closed c. Symmetric facial expressions d. Excruciating lighting-like shock in lips 27. The patient received a preoperative dose of lorazepam (Ativan) 20 minutes ago. The safety precaution the nurse should take in regard to this drug is to: a. monitor respiratory status *b. raise bed rails c. elevate the head of the bed 30 degrees d. take seizure precautions 28. The nurse warns the patient that, in order to retard the growth of microorganisms, the operating room is kept at a temperature of to degrees. a. 60; 65 *b. 66; 70 c. 71; 74 d. 75; 77 29. The nurse clarifies that the difference between regional anesthesia and procedural sedation anesthesia is that procedural sedation anesthesia uses: *a. IV sedation and regional anesthesia b. general anesthesia and IV sedation c. alternative medicine herbs and regional anesthesia d. IV sedation and local anesthesia 30. During the course of surgery, a patient exhibits tachycardia, diaphoresis, and rising body temperature. The priority intervention by the circulating nurse is to: a. continue to monitor the patient for any further changes in condition b. note the patient’s oxygen saturation and blood pressure c. ask the scrub nurse to verify the assessment findings *d. alert the anesthesiologist and surgeon immediately 31. The nurse explains that the person responsible for verifying that the consent form is signed and that the surgical site is marked is the: a. Scrub nurse b. Surgeon c. Anesthesiologist *d. Circulating nurse 32. The LPN/LVN is in the patient’s room while the charge nurse is obtaining the patient’s signature on the surgical consent form. The patient states, “I didn’t really understand what my surgeon explained, but I trust him completely.” Which response by the charge nurse is correct? *a. “I need to contact your surgeon so your questions can be answered.” b. “I can answer any questions that you might have regarding your surgery.” c. “As long as you are comfortable, then you may sign the consent form.” d. “Maybe we should call your surgeon to be sure it is okay to sign the consent.” 33. During the course of surgery, a patient exhibits tachycardia, diaphoresis, and rising body temperature. The priority intervention by the circulating nurse is to: a. continue to monitor the patient for any further changes in condition b. note the patient’s oxygen saturation and blood pressure Thci.s astsukdythsoeurscecrwuasbdnowunrlsoeadteod bvye1r0if0y00t0h80e25a3s1s2e6s9sfmromenCtoufirsnedHienrog.csom on 07-23-2022 11:38:45 GMT -05:00 *d. alert the anesthesiologist and surgeon immediately 34. The nurse explains that the person responsible for verifying that the consent form is signed and that the surgical site is marked is the: a. Scrub nurse b. Surgeon c. Anesthesiologist *d. Circulating nurse 35. The LPN/LVN is in the patient’s room while the charge nurse is obtaining the patient’s signature on the surgical consent form. The patient states, “I didn’t really understand what my surgeon explained, but I trust him completely.” Which response by the charge nurse is correct? *a. “I need to contact your surgeon so your questions can be answered.” b. “I can answer any questions that you might have regarding your surgery.” c. “As long as you are comfortable, then you may sign the consent form.” d. “Maybe we should call your surgeon to be sure it is okay to sign the consent.” 36. The nurse determines that the patient demonstrates an understanding of preoperative teaching with which responses? Select all that apply. *a. “I will need to sign a consent form before I am given my medications prior to my surgery.” *b. “The surgeon will want me to ambulate as soon as possible after my surgery.” *c. “My nurse will want me to take the deepest breaths I can tolerate following my surgery.” *d. “I may experience some constipation if I am taking much pain medication after my surgery.” e. “The general anesthesia will prevent me from having pain for the first 24 hours after surgery.” 37. The anesthesiologist provides which type of anesthesia that requires both inhalation and IV administration routes. *a. General b. Regional c. Specific d. Preoperative 38. Which nursing interventions would be appropriate after a wound evisceration? a. Place the patient in high Fowler’s position b. Give the patient fluids to prevent shock c. Replace the dressing with sterile fluffy pads *d. Apply a warm, moist normal saline sterile dressing 39. Which early postoperative observation is abnormal and should be reported immediately? *a. Emesis that is red b. Complaint of feeling cold c. Nausea d. Complaint of pain 40. What nursing interventions will minimize the effects of venous stasis? a. Pillows under the knee in a position of comfort b. Sitting with feet flat on the floor *c. Early ambulation d. Gentle leg massage 41. The nurse is assisting with the sponge and instrument count in the operating room. The operative phase in which the nurse is assisting is called the a. Perioperative phase b. Preoperative phase *c. Intraoperative phase d. Postoperative phase 42. Sudden chest pain combined with dyspnea, cyanosis, and tachycardia is an indication of a. Hypovolemic shock b. Dehiscence c. Atelectasis *d. Pulmonary embolus 43. In preparing the patient for abdominal surgery, the Unlicensed Assistive Personnel can perform which interventions? Select all that apply. *a. Vital signs b. Insertions of Nasogastric tube (NGT) *c. Enema *d. Height and weight e. Obtain operative consent f. Sterile gowning This study source was downloaded by 100000802531269 from CourseHero.com on 07-23-2022 11:38:45 GMT -05:00 44. The nurse is assessing the level of consciousness in a client with a head injury who has been unresponsive for the last eight hours. Using the Glasgow Coma Scale, the nurse notes that the client opens the eyes only as a response to pain, responds with sounds that are not understandable, and has abnormal extension of the extremities. What should the nurse do? Glasgow Coma Scale Parameter Finding Score Eye opening Spontaneously 4 To speech 3 To pain 2 Do not open 1 Best verbal response Oriented 5 Confused 4 Inappropriate speech 3 Incomprehensible sounds 2 No verbalization 1 Best motor response Obeys command 6 Localizes pain 5 Withdraws from pain 4 Abnormal flexion 3 Abnormal extension 2 No motor response 1 Interpretation: Best score = 15; worst score = 3; 7 or less generally indicates coma; changes from baseline are most important a. to arouse the patient b. Reposition the client with extremities in normal alignment *c. Chart the client’s level of consciousness as coma d. Notify the healthcare provider (HCP) 45. A client arrives in the emergency department with an ischemic stroke. Because the healthcare team is considering administering tissue plasminogen activator (t-PA), the nurse should first: a. Ask what medications the client is taking b. Complete the history and health assessment *c. Identify the time of onset of the stroke d. Determine if the client is scheduled for any surgical procedures 46. During the first 24 hours after thrombolytic treatment for an ischemic stroke, the primary goal is to control the client’s: a. Pulse b. Respirations *c. Blood pressure d. Temperature 47. A client with Parkinson’s disease is prescribed levodopa (l-dopa) therapy. Improvement in which area indicates effective therapy? a. Mood *b. Muscle rigidity c. Appetite d. Alertness 48. A client with multiple sclerosis (MS) is receiving baclofen. The nurse determines that the drug is effective when it: a. Induces sleep b. Stimulates the client’s appetite *c. Relieves muscular spasticity d. Reduces the urine bacterial count 49. When planning care for a client with myasthenia gravis, the nurse understands that the client is at highest risk for: *a. Aspiration b. Bladder dysfunction c. Hypertension d. Sensory loss 50. The client who is to receive general anesthesia has a serum potassium level of 5.8 mEq/L. What should be the nurse’s first response? a. Call the operating room to cancel surgery b. Send the client to surgery c. Make a note on the client’s record *d. Notify the surgeon This study source was downloaded by 100000802531269 from CourseHero.com on 07-23-2022 11:38:45 GMT -05:00 [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 23, 2022
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Jul 23, 2022
Downloads
0
Views
40