Health Care > QUESTIONS & ANSWERS > Western Governors University PSYCH C487 Psych Exam TestBank - 150 Questions and Rationale (All)
Western Governors University PSYCH C487 Psych Exam TestBank - 150 Questions and Rationale
Document Content and Description Below
1. The nurse is planning care with a Mexican-American client who is diagnosed with depression. The client believes in “mal ojo” (the evil eye), and uses treatment by a root healer. The nurse sh... ould do which of the following? 1. Avoid talking to the client about the root healer. 2. Explain to the client that Western medicine has a scientific, not mystical, basis. 3. Explain that such beliefs are superstitious and should be forgotten. 4. Involve the root healer in a consultation with the client, physician and nurse. 1. 4. RATIONALE: Including the root healer gives credibility and respect to the client’s cultural beliefs. Avoiding talking about the healer demonstrates either ignorance or disregard for the client’s cultural values. Negative comparison of root healing with Western medicine not only denigrate the client’s beliefs, but are likely to alienate him or her and cause them to end treatment. TEST-TAKING STRATEGY: #4 is more “collaborative”, involves more teamwork….it’s something that would happen in a perfect NCLEX world! 2. After a period of unsuccessful treatment with Elavil (amitriptyline), a woman diagnosed with depression is switched to Parnate (tranylcypromine). Which statement by the client indicates the client understands the side effects of Parnate? 1. “I need to increase my intake of sodium.” 2. “I must refrain from strenuous exercise.” 3. “I must refrain from eating aged cheese or yeast products.” 4. “I should decrease my intake of foods containing sugar.” 2. 3. RATIONALE: Cheese and yeast products contain tyramine which the client should avoid to prevent a negative interaction with Parnate, a monoamine oxidase (MAO) inhibitor. Sodium will not interact with Parnate and neither exercise nor sugar needs to be limited. 3. A client is scheduled for the first electroconvulsive therapy (ECT) treatment in the morning. The client has been unable to sleep, but at 10 p.m. refused to take Restoril as the nurse suggested. The client is still unable to sleep at 11:15 p.m. In what order should the nurse do the following? 1. Sit quietly with the client 2. Encourage the use of Restoril. 3. Offer use of MP3 player with relaxing music. 4. Discuss specific concerns. RATIONALE: The client is likely anxious about the procedure. The nurse should first spend time with the client and then discuss the client’s concerns Question Answer/Rationale about the procedure. Next, the nurse could suggest the client listen to relaxing music. The use of the sleeping medication would only be considered as a last resort since it might interfere with the effectiveness of the seizure required for the treatment. TEST-TAKING STRATEGY: The most therapeutic thing to do would be just to sit with him….and get him to reveal his specific concerns. Giving him meds would be last – you would try non-medication efforts first. 4. The client is receiving 6 mg of selegiline transdermal system (Emsam) every 24 hours for major depression. The nurse should judge teaching about Emsam to be effective when the client makes which statement? 1. “I need to avoid using the sauna at the gym.” 2. “I can cut the patch and use a smaller piece.” 3. “I need to wait until the next day to put on a new patch if it falls off.” 4. “I might gain at least 10 lb from Emsam.” 4. 1. RATIONALE: Selegiline transdermal system is the first transdermal monoamine oxidase inhibitor. The client on Emsam needs to avoid exposing the application site to external sources of direct heat, such as saunas, heating lamps, electric blankets, heating pads, heated water beds, and prolonged direct sunlight because heat increases the amount of selegiline that is absorbed, resulting in elevated serum levels of selegiline. Cutting the patch and using a smaller piece will result in a decreased amount of medication absorption, most likely leading to a worsening of the symptoms of depression. The client should apply a new patch as soon as possible if one falls off to ensure an adequate amount of medication absorption. Emsam is not associated with significant weight gain, although a weight gain of 1 to 2 lb (2.2 to 4.4 kg) is possible. 5. A client has been taking 30 mg of duloxetine hydrochloride (Cymbalta) twice daily for 2 months because of depression and vague aches and pains. While interacting with the nurse, the client discloses a pattern of drinking a 6-pack of beer daily for the past 10 years to help with sleep. What should the nurse do first? 1. Refer the client to the dual diagnosis program at the clinic. 2. Share the information at the next interdisciplinary treatment conference. 3. Report the client’s beer consumption to the physician. 4. Teach the client relaxation exercises to perform before bedtime. 5. 3. RATIONALE: The nurse should report the client’s beer consumption to the physician. Duloxetine should not be administered to a client with renal or hepatic insufficiency because the medication can elevate liver enzymes and, together with substantial alcohol use, can cause liver injury. Referring the client to the dual diagnosis program, sharing information at the next interdisciplinary treatment conference, and teaching the client relaxation exercises are helpful interventions for the nurse to implement. However, reporting the findings to the physician is most important. 6. A client was admitted to the inpatient unit 3 days ago with a flat affect, psychomotor retardation, anorexia, hopelessness, and suicidal ideation. The physician prescribed 75 mg of venlafaxine extended release (Effexor XR) to be given every 6. 2. RATIONALE: The client’s sudden improvement and decrease in anxiety most likely indicates that the client is relieved because he has made the decision to kill himself and may now have the energy to complete the suicide. Symptoms of severe depression do not suddenly abate because Question Answer/Rationale morning. The client interacted minimally with the staff and spent most of the day in his room. As the nurse enters the unit at the beginning of the evening shift, the client is smiling and cheerfully greets the nurse. He appears to be relaxed and joins the group for community meeting before supper. What should the nurse interpret as the most likely cause of the client’s behavior? 1. The Effexor is helping the client’s symptoms of depression significantly. 2. The client’s sudden improvement calls for close observation by the staff. 3. The staff can decrease their observation of the client. 4. The client is nearing discharge due to the improvement of his symptoms. most antidepressants work slowly and take 2 to 4 weeks to provide a maximum benefit. The client will improve slowly due to the medication. The sudden improvement in symptoms does not mean the client is nearing discharge and decreasing observation of the client compromises the client’s safety. 7. The nurse is conducting an intake interview with an Asian American female who reports sadness, physical and mental fatigue, anxiety, and sleep disturbance. Prior to the client’s time with the physician, it is important for the nurse to obtain information about the client’s use of which of the following? Select all that apply. 1. Tea. 2. Herbal medicine. 3. Breathing exercise. 4. Massage. 5. Folk healer. 7. 1, 2, 5. RATIONALE: It is important for the nurse to obtain information about the client’s use of tea, herbal medicine, and a folk healer because the information is critical to the safe prescription of psychotropic medication. Breathing exercises, massage, and acupuncture are also traditional therapies used by the Asian American population, but do not interfere with the use of medications. 8. The client is taking 50 mg of lamotrigine (Lamictal) daily for bipolar depression. The client shows the nurse a rash on his arm. What should the nurse do? 1. Report the rash to the physician. 2. Explain that the rash is a temporary adverse effect. 3. Give the client an ice pack for his arm. 4. Question the client about recent sun exposure. 8. 1. RATIONALE: The nurse should immediately report the rash to the physician because lamotrigine can cause Stevens-Johnson syndrome, a toxic epidermal necrolysis. The rash is not a temporary adverse effect. Giving the client an ice pack and questioning the client about recent sun exposure are irresponsible nursing actions because of the possible seriousness of the rash. TEST-TAKING STRATEGY: Calling the MD is almost NEVER the right answer – but in this case, the rash could be a very serious adverse effect. KNOW WHICH MEDS CAN RESULT IN STEVENS-JOHNSON SYNDROME! 9. The nurse is reviewing the laboratory report with the client’s lithium level taken that morning prior to administering the 5 9. 2. RATIONALE: The nurse should hold the 5 p.m. dose of lithium because a level of 1.8 mEq/ L can cause adverse reactions, including diarrhea, Question Answer/Rationale p.m. dose of lithium. The lithium level is 1.8 mEq/ L. The nurse should: 1. Administer the 5 p.m. dose of lithium. 2. Hold the 5 p.m. dose of lithium. 3. Give the client 8 oz (236 mL) of water with the lithium. 4. Give the lithium after the client’s supper. vomiting, drowsiness, muscle weakness, and lack of coordination, which are early signs of lithium toxicity. The nurse should report the lithium level to the physician, including any symptoms of toxicity. Administering the 5 p.m. dose of lithium, giving the client the lithium with 8 oz (236 mL) of water, or giving it after supper would result in an increase of the lithium level, thus increasing the risk of lithium toxicity. TEST-TAKING STRATEGY: KNOW YOUR LITHIUM LEVELS! 10. A nurse is conducting a psychoeducational group for family members of clients hospitalized with depression. Which family member’s statement indicates a need for additional teaching? 1. “My husband will slowly feel better as his medicine takes effect over the next 2 to 4 weeks.” 2. “My wife will need to take her antidepressant medicine and go to group to stay well.” 3. “My son will only need to attend outpatient appointments when he starts to feel depressed again.” 4. “My mother might need help with grocery shopping, cooking, and cleaning for a while.” 10. 3. RATIONALE: Additional teaching is needed for the family member who states her son will only need to attend outpatient appointments when he starts to feel depressed again. Compliance with medication and outpatient follow-up are key in preventing relapse and rehospitalization. The statements expressing expectations of feeling better as medication takes effect, needing medicine and group therapy to stay well, and needing help with grocery shopping, cooking, and cleaning for a while indicate the families’ understanding of depression, medication, and follow-up care. 11. The nurse is distinguishing between delusions experienced by a client diagnosed with major depression with psychotic features and the delusions of a client diagnosed with schizophrenia. The essential difference is: 1. Major depression delusions are more likely to be negative than schizophrenic delusions. 2. Major depression delusions clear up less quickly than schizophrenic delusions. 3. Major depression delusions are more likely than schizophrenic delusions to require long-acting depot antipsychotic medication given intramuscularly. 4. Major depression delusions are more mood congruent than schizophrenic delusions. 11. 4. RATIONALE: Delusions occurring in schizophrenia tend to be more mood incongruent and more bizarre than delusions experienced with depression. Schizophrenic delusions clear up less quickly and are more likely to require depot antipsychotic medication, which are administered intramuscularly. Delusions in major depression match the client’s mood, are somewhat more reality based, and tend to resolve once the client is properly medicated. 12. A 16-year-old client is prescribed 10 mg of paroxetine (Paxil) at bedtime for major depression. The nurse should instruct the client and parents to monitor the client closely for which adverse effect? 12. 4. RATIONALE: The nurse closely monitors the client taking paroxetine for the development of agitation, which could lead to self-harm in the form of a suicide attempt. Headache, nausea, and fatigue are transient adverse effects of paroxetine. Question Answer/Rationale 1. Headache. 2. Nausea. 3. Fatigue. 4. Agitation. 13. The nurse is assessing the outcomes of care for a client who has an Axis I diagnosis of major depression. Following the initiation of treatment, arrange the symptoms in chronological order from the one that improves first to the one that improves last. 1. Self esteem 2. Sleep 3. Energy level 4. Appetite RATIONALE: When beginning medication treatment, the client will initially notice an improvement in sleep, followed by an improvement in appetite which leads to an increase in energy level. Behavioral treatment is most likely to affect self-esteem and since the decline in self-esteem generally occurs over months or years, it will likely take longer than a few days to improve. 14. A client who has had three episodes of recurrent endogenous depression within the past 2 years states to the nurse, “I want to know why I’m so depressed.” Which of the following statements by the nurse is most helpful? 1. “I know you’ll get better with the right medication.” 2. “Let’s discuss possible reasons underlying your depression.” 3. “Your depression is most likely caused by a brain chemical imbalance.” 4. “Members of your family seem very supportive of you.” 14. 3. RATIONALE: Endogenous depression (depression coming from within the person) is biochemical in nature. The biologic theory of depression indicates a neurotransmitter imbalance involving serotonin, norepinephrine, and possibly dopamine. Reactive depression is caused by the occurrence of something happening outside the body, such as the death of a loved one or another significant loss. Stating that the client will improve with the right medication or that family members seem supportive does not address the client’s immediate concerns of not knowing the cause of the depression. Discussing possible reasons for the client’s depression is nontherapeutic because the depression is endogenous and biochemically based TEST-TAKING STRATEGY: Look at the word “endogenous” in the question. If that word weren’t there, this may not be the right answer! #1 dismisses his concerns. #2 might be too “deep” for him at this time. #4 sounds like you just want his family to help, and don’t want to get involved. ALSO - #3 is actually the only one that answers his question! 15. A client diagnosed with major depression spends most of the day lying in bed with the sheet pulled over his head. Which of 15. 2. RATIONALE: The nurse should initiate brief, frequent contacts throughout the day to let the client know that he is important to the nurse. Question Answer/Rationale the following approaches by the nurse is most therapeutic? 1. Wait for the client to begin the conversation. 2. Initiate contact with the client frequently. 3. Sit outside the client’s room. 4. Question the client until he responds. This will positively affect the client’s self-esteem. The nurse’s action conveys acceptance of the client as a worthwhile person and provides some structure to the seemingly monotonous day. Waiting for the client to begin the conversation with the nurse is not helpful because the depressed client resists interaction and involvement with others. Sitting outside of the client’s room is not productive and not necessary in this situation. If the client were actively suicidal, then a one-on-one client-to-staff assignment would be necessary. Questioning the client until he responds would overwhelm him because he could not meet the nurse’s expectations to interact. TEST-TAKING STRATEGY: You wouldn’t ever “question” someone. If you wait for him to talk, he might never talk. Sitting outside his room wouldn’t help. Keep letting him know you’re there (#2). 16. The client exhibits a flat affect, psychomotor retardation, and depressed mood. The nurse attempts to engage the client in an interaction but the client does not respond to the nurse. Which response by the nurse is most appropriate? 1. “I’ll sit here with you for 15 minutes.” 2. “I’ll come back a little bit later to talk.” 3. “I’ll find someone else for you to talk with.” 4. “I’ll get you something to read.” 16. 1. RATIONALE: The most appropriate action is for the nurse to remain with the client even if the client does not engage in conversation with the nurse. A client with severe depression may be unable to engage in an interaction with the nurse because the client feels worthless and lacks the necessary energy to do so. However, the nurse’s presence conveys acceptance and caring, thus helping to increase the client’s self-worth. Telling the client that the nurse will come back later, stating that the nurse will find someone else for the client to talk with, or telling the client that the nurse will get her something to read conveys to the client that she is not important, reinforcing the client’s negative view of herself. Additionally, such statements interfere with the client’s development of a sense of security and trust in the nurse. TEST-TAKING STRATEGY: #2, 3, and 4 all dismiss his issue. #1 is the only one that offers him help at that time. He might open up if he knows you’re available to him. 17. After a few minutes of conversation, a female client who is depressed wearily asks the nurse, “Why pick me to talk to? Go talk to someone else.” Which of the following replies by the nurse is best? 1. “I’m assigned to care for you today, if you’ll let me.” 2. “You have a lot of potential, and I’d like to help you.” 3. “I’ll talk to someone else later.” 4. “I’m interested in you and want to help you.” 17. 4. RATIONALE: The nurse tells the client that the nurse is interested in her to increase the client’s sense of importance, worth, and self-esteem. Also, stating that the nurse wants to help conveys to the client that she is worthwhile and important. Telling the client that the nurse is assigned to care for her is impersonal and implies that the client is being uncooperative. Telling the client that the nurse is there because the client has potential for improvement will not help the client with low self-esteem because most people develop a sense of self-worth through accomplishment. Simply saying Question Answer/Rationale that the client has a lot of potential will not convince her that she is worthwhile. Telling the client that the nurse will talk to someone else later is not client-focused and does not address the client’s question or concern. TEST-TAKING STRATEGY: #4 just sounds like the “perfect NCLEX answer”. #1 and #3 are a bit rude…and #2 implies that he isn’t letting you help. 18. A client is receiving paroxetine (Paxil) 20 mg every morning. After taking the first three doses, the client tells the nurse that the medication upsets his stomach. Which of the following instructions should the nurse give to the client? 1. “Take the medication an hour before breakfast.” 2. “Take the medication with some food.” 3. “Take the medication at bedtime.” 4. “Take the medication with 4 oz of orange juice.” 18. 2. RATIONALE: Nausea and gastrointestinal upset is a common, but usually temporary, side effect of paroxetine (Paxil). Therefore, the nurse would instruct the client to take the medication with food to minimize nausea and stomach upset. Other more common side effects are dry mouth, constipation, headache, dizziness, sweating, loss of appetite, ejaculatory problems in men, and decreased orgasms in women. Taking the medication an hour before breakfast would most likely lead to further gastrointestinal upset. Taking the medication at bedtime is not recommended because Paxil can cause nervousness and interfere with sleep. Because orange juice is acidic, taking the medication with it, especially on an empty stomach, may lead to nausea or increase the client’s gastrointestinal upset. 19. The physician orders fluoxetine (Prozac) orally every morning for a 72-year-old client with depression. Which transient adverse effect of this drug requires immediate action by the nurse? 1. Nausea. 2. Dizziness. 3. Sedation. 4. Dry mouth. 19. 2. RATIONALE: The presence of dizziness could indicate orthostatic hypotension, which may cause injury to the client from falling. Nausea, sedation, and dry mouth do not require immediate intervention by the nurse. 20. Which of the following statements by a client taking trazodone (Desyrel) as prescribed by the physician indicates to the nurse that further teaching about the medication is needed? 1. “I will continue to take my medication after a light snack.” 2. “Taking Desyrel at night will help me to sleep.” 3. “My depression will be gone in about 5 to 7 days.” 4. “I won’t drink alcohol while taking Desyrel.” 20. 3. RATIONALE: Symptom relief can occur during the 1st week of therapy, with optimal effects possible within 2 weeks. For some clients, 2 to 4 weeks is needed for optimal effects. The client’s statement that the depression will be gone in 5 to 7 days indicates to the nurse that clarification and further teaching is needed. Trazodone should be taken after a meal or light snack to enhance its absorption. Trazodone can cause drowsiness, and therefore the major portion of the drug should be taken at bedtime. The depressant effects of central nervous system depressants and alcohol may be potentiated by this drug. 21. A 62-year-old female client with severe depression and psychotic symptoms is scheduled for electroconvulsive therapy 21. 3. RATIONALE: The nurse should explain that ECT is a safe treatment and that the client is given an ultra– short-acting anesthetic to induce sleep Question Answer/Rationale (ECT) tomorrow morning. The client’s daughter asks the nurse, “How painful will the treatment be for Mom?” The nurse should respond by saying which of the following? 1. “Your mother will be given something for pain before the treatment.” 2. “The physician will make sure your mother doesn’t suffer needlessly.” 3. “Your mother will be asleep during the treatment and will not be in pain.” 4. “Your mother will be able talk to us and tell us if she’s in pain.” before ECT and a muscle relaxant to prevent musculoskeletal complications during the convulsion, which typically lasts 30 to 60 seconds to be therapeutic. Atropine is given before ECT to inhibit salivation and respiratory tract secretions and thereby minimize the risk of aspiration. Medication for pain is not necessary and is not given before or during the treatment. Some clients experience a headache after the treatment and may request and be given an analgesic such as acetaminophen (Tylenol). Telling the daughter that the physician will ensure that the client does not suffer needlessly would not provide accurate information about ECT. This statement also implies that the client will have pain during the treatment, which is untrue. 22. A client who experienced sleep disturbances, feelings of worthlessness, and an inability to concentrate for the past 3 months was fired from her job a month ago. The client tells the nurse, “My boss was wonderful! He was understanding and a really nice man.” The nurse interprets the client’s statement as representing the defense mechanism of reaction formation. Which of the following would be the best response by the nurse? 1. “But, I don’t understand, wasn’t he the one who fired you?” 2. “Tell me more about having to work while not being able to sleep or concentrate.” 3. “It must have been hard to leave a boss like that.” 4. “It sounds like he would hire you back if you asked.” 22. 2. RATIONALE: Option 1 casts doubt on the client’s perception, which is likely to increase the client’s anxiety and make the client feel defensive. Options 3 & 4 further the client’s unrealistic perception of the situation. Option 2 focuses on the client and her feelings which is the most effective approach to help her realistically consider her situation and decrease the anxiety that led the client to use the defense mechanism of reaction formation. 23. During a group session, a client who is depressed tells the group that he lost his job. Which of the following responses by the nurse is best? 1. “It must have been very upsetting for you.” 2. “Would you tell us about your job.” 3. “You’ll find another job when you’re better.” 4. “You were probably too depressed to work.” 23. 1. RATIONALE: By stating, “It must have been very upsetting for you,” the nurse conveys empathy to the client by recognizing the underlying meaning of a painful occurrence. The nurse’s statement invites the client to verbalize feelings and thoughts and lets the client know that the nurse is listening to and respects the client. Telling the client to talk about the job disregards the client’s feelings and is nontherapeutic for the depressed client because of underlying feelings of worthlessness and guilt that are commonly present. Telling the client that he will find another job when he is better or that he was probably too depressed to work is inappropriate because it disregards the client’s feelings and may promote additional feelings of failure and inadequacy in the client. Question Answer/Rationale 24. During an interaction with the nurse, a client states, “My husband has supported me every time I’ve been hospitalized for depression. He’ll leave me this time. I’m an awful wife and mother. I’m no good. Nothing I do is right.” Based on this information, which of the following nursing diagnoses should the nurse identify when developing the client’s plan of care? 1. Impaired social interaction related to unsatisfactory relationships as evidenced by withdrawal. 2. Chronic low self-esteem related to lack of self-worth as evidenced by negative statements. 3. Risk for self-directed violence related to feelings of guilt as evidenced by statements of suicidal ideation. 4. Ineffective coping related to hospitalizations as evidenced by impaired judgment. 24. 2. RATIONALE: The client’s negative thinking and statements are directly related to the psychopathology of depression. The client’s views and feelings about herself reflect low self-esteem. Although Impaired social interaction, Risk for self-directed violence, and Ineffective coping are possible nursing diagnoses, there are insufficient data to support these diagnoses. Further assessment is needed to identify supportive data. 25. A male client who is very depressed exhibits psychomotor retardation, a flat affect, and apathy. The nurse observes the client to be in need of grooming and hygiene. Which of the following nursing actions is most appropriate? 1. Explaining the importance of hygiene to the client. 2. Asking the client if he is ready to shower. 3. Waiting until the client’s family can participate in the client’s care. 4. Stating to the client that it’s time for him to take a shower. 25. 4. RATIONALE: The client with depression is preoccupied, has decreased energy, and cannot make decisions, even simple ones. Therefore, the nurse presents the situation, “It’s time for a shower,” and assists the client with personal hygiene to preserve his dignity and self-esteem. Explaining the importance of good hygiene to the client is inappropriate because the client may know the benefits of hygiene but is too fatigued and preoccupied to pay attention to self-care. Asking the client if he is ready for a shower is not helpful because the client with depression commonly cannot make even simple decisions. This action also reinforces the client’s feeling about not caring about showering. Waiting for the family to visit to help with the client’s hygiene is inappropriate and irresponsible on the part of the nurse. The nurse is responsible for making basic decisions for the client until the client can make decisions for himself. 26. A client who is depressed states, “I’m an awful person. Everything about me is bad. I can’t do anything right.” Which of the following responses by the nurse is most therapeutic? 1. “Everybody around here likes you.” 2. “I can see many good qualities in you.” 3. “Let’s discuss what you’ve done correctly.” 4. “You were able to bathe today.” 26. 4. RATIONALE: By saying, “You were able to bathe today,” the nurse is pointing out a visible accomplishment or strength, thereby increasing the client’s feelings of self-worth and self-esteem. Stating that “everybody around here likes you” or discussing what the client has done correctly is inappropriate because although the client may agree with the nurse, the client still may be depressed. Stating that the nurse sees many good qualities in the client is not helpful because a person’s feeling of self-worth is generally determined by accomplishments. Intellectual understanding does Question Answer/Rationale not help the client with severe depression. Additionally, the nurse cannot talk a client out of depression because major depression is endogenous and biochemical in nature. Medication should restore the neurotransmitter balance and relieve the depression. 27. When developing the teaching plan for the family of a client with severe depression who is to receive electroconvulsive therapy (ECT), which of the following information should the nurse include? 1. Some temporary confusion and disorientation immediately after a treatment is common. 2. During an ECT treatment session, the client is at risk for aspiration. 3. Clients with severe depression usually do not respond to ECT. 4. The client will not be able to breathe independently during a treatment. 27. 1. RATIONALE: The family needs to be informed that some confusion and disorientation will occur as the client emerges from anesthesia immediately after ECT, to lessen their fear and anxiety about the procedure. The nurse will assist the client with reorientation (time, person, and place) and will give clear, simple instructions. The client may need to lie down after ECT because of the effects of the anesthesia. Informing the family that there is a danger of aspiration during ECT is inappropriate and unnecessary. The risk of aspiration occurring during ECT is minimal because food and fluids are withheld for 6 to 8 hours before the treatment. In addition, the client receives atropine to inhibit salivation and respiratory tract secretions. Telling the family that the client will not be able to breathe independently during ECT may frighten them unnecessarily. If asked, the nurse should inform the family that the anesthesiologist mechanically ventilates the client with 100% oxygen immediately before the treatment. The client with severe depression responds to ECT. Usually, ECT is used for those who are severely depressed and not responding to pharmacotherapy and for those who are highly suicidal. 28. Which of the following comments indicates that a client understands the nurse’s teaching about sertraline (Zoloft)? 1. “Zoloft will probably cause me to gain weight.” 2. “This medicine can cause delayed ejaculations.” 3. “Dry mouth is a permanent side effect of Zoloft.” 4. “I can take my medicine with St. John’s wort.” 28. 2. RATIONALE: Sertraline, like other selective serotonin reuptake inhibitors (SSRIs), can cause decreased libido and sexual dysfunction such as delayed ejaculation in men and an inability to achieve orgasm in women. SSRIs do not typically cause weight gain but may cause loss of appetite and weight loss. Dry mouth is a possible side effect, but it is temporary. The client should be told to take sips of water, suck on ice chips, or use sugarless gum or candy. St. John’s wort should not be taken with SSRIs because a severe reaction could occur. 29. The client with recurring depression will be discharged from the psychiatric unit. Which suggestion to the family is best to help them prepare for the client’s return home? 1. Discourage visitors while the client is at home. 2. Provide for a schedule of activities outside the home. 3. Involve the client in usual at-home activities. 29. 3. RATIONALE: It is best to involve the client in usual at-home activities as much as the client can tolerate them. Discouraging visitors may not be in the client’s best interest because visits with supportive significant others will help reinforce supportive relationships, which are important to the client’s self-worth and self-esteem. Providing for a schedule of activities outside the home may be overwhelming for the client initially. Involving the client in Question Answer/Rationale 4. Encourage the client to sleep as much as possible. planning for outside activities would be appropriate. Encouraging the client to sleep as much as possible is nontherapeutic and promotes withdrawal from others. 30. A client with major depression is to be discharged home tomorrow. When preparing the client’s discharge plan, which of the following areas is most important for the nurse to review with the client? 1. Future plans for going back to work. 2. A conflict encountered with another client. 3. Results of psychological testing. 4. Medication management with outpatient follow-up. 30. 4. RATIONALE: Medication management with outpatient follow-up is of vital importance to discuss with the client before discharge. The nurse teaches and clarifies any questions related to medication and outpatient treatment. The client also has the opportunity to voice feelings related to medication and treatment. The goal is to assist the client in making a successful transition from hospital to home with optimal functioning outside the hospital for as long as possible. The nurse may also need to assist with decreasing any anxiety the client may have related to discharge. Discussing future plans for returning to work or employment is not as immediate a concern as assisting with medication and treatment compliance. Noncompliance with medication is a primary cause of relapse in a client with a psychiatric disorder. Reviewing a conflict the client had encountered with another client is not appropriate or therapeutic at this time unless the client brings it to the nurse’s attention. The conflict should have been dealt with and resolved when it occurred. Reviewing the results of psychological testing is the responsibility of the physician if he chooses. 31. A client with major depression and psychotic features is admitted involuntarily to the hospital. He will not eat because his “bowels have turned to jelly,” which the client states is punishment for his wickedness. The client requests to leave the hospital. The nurse denies the request because commitment papers have been initiated by the physician. Which of the following should the nurse identify as a criterion for the client to be legally committable? 1. Evidence of psychosis. 2. Being gravely disabled. 3. Risk of harm to self or others. 4. Diagnosis of mental illness. 31. 2. RATIONALE: Criteria for commitment include being gravely disabled and posing a harm to self or others. This client is not threatening to harm himself in the form of suicide or to harm others. The client is gravely disabled because of his inability to care for himself– namely, not eating because of his delusion. Evidence of psychosis or psychotic symptoms or diagnosis of a mental illness alone does not make the client legally eligible for commitment. 32. The client who has been taking venlafaxine (Effexor) 25 mg P.O. three times a day for the past 2 days states, “This medicine isn’t doing me any good. I’m still so depressed.” Which of the following responses by the nurse is most appropriate? 32. 3. RATIONALE: The client needs to be informed of the time lag involved with antidepressant therapy. Although improvement in the client’s symptoms will occur gradually over the course of 1 to 2 weeks, typically it takes 2 to 4 weeks to get the full effects of the medication. This information Question Answer/Rationale 1. “Perhaps we’ll need to increase your dose.” 2. “Let’s wait a few days and see how you feel.” 3. “It takes about 2 to 4 weeks to receive the full effects.” 4. “It’s too soon to tell if your medication will help you.” will help the client be compliant with medication and will also help in decreasing any anxiety the client has about not feeling better. The client’s dose may not need to be increased; it is too early to determine the full effectiveness of the drug. Additionally, such a statement may increase the client’s anxiety and diminish self-worth. Telling the client to wait a few days discounts the client’s feelings and is inappropriate. Although it is too soon to tell whether the medication will be effective, telling this to the client may cause the client undue distress. This statement is somewhat negative because it is possible that the medication will not be effective, possibly further compounding the client’s anxiety about not feeling better. 33. The client states to the nurse, “I take citalopram (Celexa) 40 mg every day like my physician prescribed. I have also been taking St. John’s wort 750 mg daily for the past 2 weeks.” Which of the following indicate that the client is developing serotonin syndrome? Select all that apply. 1. Confusion. 2. Restlessness. 3. Constipation. 4. Diaphoresis. 5. Ataxia. 33. 1, 2, 3, 5, 6. RATIONALE: Serotonin syndrome can occur if a selective serotonin reuptake inhibitor is combined with a monoamine oxidase inhibitor, a tryptophan-serotonin precursor, or St. John’s wort. Signs and symptoms of serotonin syndrome include mental status changes, such as confusion, restlessness or agitation, headache, diaphoresis, ataxia, myoclonus, shivering, tremor, diarrhea, nausea, abdominal cramps, and hyperreflexia. Constipation is not associated with serotonin syndrome. 34. When teaching the client with atypical depression about foods to avoid while taking phenelzine (Nardil), which of the following should the nurse include? 1. Roasted chicken. 2. Salami. 3. Fresh fish. 4. Hamburger. 34. 2. RATIONALE: Phenelzine is a monoamine oxidase inhibitor (MAOI). MAOIs block the enzyme monoamine oxidase, which is involved in the decomposition and inactivation of norepinephrine, serotonin, dopamine, and tyramine (a precursor to the previously stated neurotransmitters). Foods high in tyramine– those that are fermented, pickled, aged, or smoked– must be avoided because, when they are ingested in combination with MAOIs, a hypertensive crisis occurs. Some examples include salami, bologna, dried fish, sour cream, yogurt, aged cheese, bananas, pickled herring, caffeinated beverages, chocolate, licorice, beer, Chianti, and alcohol-free beer. 35. A client is taking phenelzine (Nardil) 15 mg P.O. three times a day. The nurse is about to administer the 1 p.m. dose when the client tells the nurse that about having a throbbing headache. Which of the following should the nurse do first? 1. Give the client an analgesic ordered p.r.n. 2. Call the physician to report the symptom. 35. 4. RATIONALE: The nurse should first take the client’s vital signs because the client could be experiencing a hypertensive crisis, which requires prompt intervention. Signs and symptoms of a hypertensive crisis include occipital headache, a stiff or sore neck, nausea, vomiting, sweating, dilated pupils and photophobia, nosebleed, tachycardia, bradycardia, and constricting chest pain. Giving this client an analgesic without taking his vital signs first is Question Answer/Rationale 3. Administer the client’s next dose of phenelzine. 4. Obtain the client’s vital signs. inappropriate. After the client’s vital signs have been obtained, then the nurse would call the physician to report the client’s complaints and vital signs. Administering the client’s next dose of phenelzine before taking his vital signs could result in a dangerous situation if the client is experiencing a hypertensive crisis. 36. A female client with severe depression and weight loss has not eaten since admission to the hospital 2 days ago. Which of the following approaches should the nurse include when developing this client’s plan of care to ensure that she eats? 1. Serving the client her meal trays in her room. 2. Sitting with the client and spoon-feeding if required. 3. Calling the family to bring the client food from home. 4. Explaining the importance of nutrition in recovery. 36. 2. RATIONALE: A depressed client commonly is not interested in eating because of the psychopathology of the disorder. Therefore, the nurse must take responsibility to ensure that the client eats, including spoon-feeding the client (placing the food on the spoon, putting the food near the client’s mouth, and asking her to eat) if necessary. Serving the client her tray in her room does not ensure that she will eat. Calling the family to bring the client food from home usually is allowed, but it is still the nurse’s responsibility to ensure that the client eats. Explaining the importance of nutrition in recovery is not helpful. The client may intellectually know that eating is important but may not be interested in eating or want to eat. 37. After administering a prescribed medication to a client who becomes restless at night and has difficulty falling asleep, which of the following nursing actions is most appropriate? 1. Sitting quietly with the client at the bedside until the medication takes effect. 2. Engaging the client in interaction until the client falls asleep. 3. Reading to the client with the lights turned down low. 4. Encouraging the client to watch television until the client feels sleepy. 37. 1. RATIONALE: To promote adequate rest (6 to 8 hours per night) and to eliminate hyposomnia, the nurse should sit with the client at the bedside until the medication takes effect. The presence of a caring nurse provides the client with comfort and security and helps to decrease the client’s anxiety. Engaging the client in interaction until the client falls asleep, reading to the client, or encouraging the client to watch television may be too stimulating for the client, consequently increasing rather than decreasing the client’s restlessness. 38. Which of the following behaviors exhibited by a client with depression should lead the nurse to determine that the client is ready for discharge? 1. Interactions with staff and peers. 2. Sleeping for 4 hours in the afternoon and 4 hours at night. 3. Verbalization of feeling in control of self and situations. 4. Statements of dissatisfaction over not being able to perform at work. 38. 3. RATIONALE: The client who verbalizes feeling in control of self and situations no longer feels powerless to affect an outcome but realizes that one’s actions can have an impact on self and situations. It is common for the client with depression to feel powerless to affect an outcome and to feel a lack of control over a situation. Although interacting with staff and peers is a positive action, the client could be conversing in a negative or nontherapeutic manner. Sleeping 4 hours in the afternoon and 4 hours at night is evidence of symptomatology and does not indicate improvement or recovery. Verbalizing dissatisfaction over not being able to perform at work indicates that the client is most likely focusing on shortcomings and powerlessness. Question Answer/Rationale 39. The client with major depression and suicidal ideation has been taking bupropion (Wellbutrin) 100 mg P.O. four times daily for 5 days. Assessment reveals the client to be somewhat less withdrawn, able to perform activities of daily living with minimal assistance, and eating 50% of each meal. At this time, the nurse should monitor the client specifically for which of the following behaviors? 1. Seizure activity. 2. Suicide attempt. 3. Visual disturbances. 4. Increased libido. 39. 2. RATIONALE: The nurse must monitor the client for a suicide attempt at this time when the client is starting to feel better because the depressed client may now have enough energy to carry out an attempt. Bupropion inhibits dopamine reuptake; it is an activating antidepressant and could cause agitation. Although bupropion lowers the seizure threshold, especially at doses greater than 450 mg/ day, and visual disturbances and increased libido are possible adverse effects, the nurse must closely monitor the client for suicide attempt. As the client with major depression begins to feel better, the client may have enough energy to carry out an attempt. 40. Which of the following outcomes should the nurse include in the initial plan of care for a client who is exhibiting psychomotor retardation, withdrawal, minimal eye contact, and unresponsiveness to the nurse’s questions? 1. The client will initiate interactions with peers. 2. The client will participate in milieu activities. 3. The client will discuss adaptive coping techniques. 4. The client will interact with the nurse. 40. 4. RATIONALE: In the initial plan of care, the most appropriate outcome would be that the client will interact with the nurse. First, the client would begin interacting with one individual, the nurse. The nurse would gradually assist the client to engage in interactions with other clients in one-on-one contacts, progressing toward informal group gatherings and eventually taking part in structured group activities. The client needs to experience success according to the client’s level of tolerance. Initiating interactions with peers occurs when the client can gain a measure of confidence and selfesteem instead of feeling intimidated or unduly anxious. Discussing adaptive coping techniques is an outcome the client may be able to reach when symptoms are not as severe and the client can concentrate on improving coping skills. 41. When preparing a teaching plan for a client about imipramine (Tofranil), which of the following substances should the nurse tell the client to avoid while taking the medication? 1. Caffeinated coffee. 2. Sunscreen. 3. Alcohol. 4. Artificial tears. 41. 3. RATIONALE: Imipramine, a tricyclic antidepressant, in combination with alcohol will produce additive central nervous system depression. Although caffeinated coffee is safe to use when the client is taking imipramine, it is not recommended for a client with depression who may be experiencing sleep disturbances. Imipramine may cause photosensitivity so the client would be instructed to use sunscreen and protective clothing when exposed to the sun. Reduced lacrimation may occur as a side effect of imipramine. Therefore, the use of artificial tears may be recommended. 42. The client with depression who is taking imipramine (Tofranil) states to the nurse, “My doctor wants me to have an electrocardiogram (ECG) in 2 weeks, but my heart is fine.” Which response by the nurse is most appropriate? 42. 1. RATIONALE: Telling the client that ECGs are done routinely for all clients taking imipramine, a tricyclic antidepressant, is an honest and direct response. Additionally, it provides some reassurance for the client. Commonly, a client with depression will ruminate, leading needlessly to Question Answer/Rationale 1. “It’s routine practice to have ECGs periodically because there is a slight chance that the drug may affect the heart.” 2. “It’s probably a precautionary measure because I’m not aware that you have a cardiac condition.” 3. “Try not to worry too much about this. Your doctor is just being very thorough in monitoring your condition.” 4. “You had an ECG before you were prescribed imipramine and the procedure will be the same.” increased anxiety. Tricyclic antidepressants may cause tachycardia, ECG changes, and cardiotoxicity. Telling the client that it’s probably a precautionary measure because the nurse is not aware of a cardiac condition instills doubt and may cause undue anxiety for the client. Telling the client not to worry because the doctor is very thorough dismisses the client’s concern and does not give the client adequate information. Explaining that the client had an ECG before initiating therapy with imipramine and that the procedure will be the same does not answer the client’s question. 43. When assessing a client who is receiving tricyclic antidepressant therapy, which of the following should alert the nurse to the possibility that the client is experiencing anticholinergic effects? Analyze 1. Tremors and cardiac arrhythmias. 2. Sedation and delirium. 3. Respiratory depression and convulsions. 4. Urine retention and blurred vision. 43. 4. RATIONALE: Anticholinergic effects, which result from blockage of the parasympathetic (craniosacral) nervous system, include urine retention, blurred vision, dry mouth, and constipation. Tremors, cardiac arrhythmias, and sexual dysfunction are possible side effects, but they are caused by increased norepinephrine availability. Sedation and delirium are not anticholinergic effects. Sedation may be a therapeutic effect because many clients with depression experience agitation and insomnia. Delirium, typically not a side effect, would indicate toxicity, especially in elderly clients. Respiratory depression, convulsions, ataxia, agitation, stupor, and coma indicate tricyclic antidepressant toxicity. 44. A client with depression who is taking doxepin (Sinequan) 100 mg P.O. at bedtime has dizziness on arising. Which of the following suggestions is most appropriate? 1. “Try taking a hot shower.” 2. “Get up slowly and dangle your feet before standing.” 3. “Stay in bed until you are feeling better.” 4. “You need to limit the fluids you drink. 44. 2. RATIONALE: Doxepin and other tricyclic antidepressants may cause postural hypotension, especially in the morning. Postural hypotension occurs because the tricyclic antidepressant inhibits the body’s natural vasoconstrictive reaction when a person stands. The nurse regularly monitors the client’s vital signs, both lying and standing. The nurse should instruct the client to rise slowly and dangle his feet before standing. Advising the client to take a hot shower is detrimental to the client’s safety. Heat causes vasodilation, which could further exacerbate the dizziness, placing the client at risk for falls and subsequent injury. Telling the client to stay in bed until he is feeling better is not helpful and is impractical. The client with depression would rather stay in bed and withdraw from others. Placing the client on fluid restriction is detrimental to the client with depression whose fluid and food intake may be inadequate. 45. The MD orders mirtazapine (Remeron) 30 mg P.O. at bedtime for a client with depression. The nurse should: 1. Give the medication as ordered. 2. Question the physician’s order. 45. 1. RATIONALE: The nurse should give the medication as ordered. Mirtazapine is given once daily, preferably at bedtime to minimize the risk of injury resulting from postural hypotension and sedative effects. The usual dosage ranges from 15 to 45 mg. There is no reason to question the Question Answer/Rationale 3. Request to give the medication in the morning. 4. Give the medication in three divided doses. physician’s order. The nurse should administer the medication as ordered. Requesting to give the medication in three divided doses is inappropriate and demonstrates the nurse’s lack of knowledge about the drug. 46. A client taking mirtazapine (Remeron) is sad about a 20 lb weight gain over the past 3 months. The client says, “I stopped taking my Remeron 15 days ago. I don’t want to get depressed again, but I feel bad about my weight.” Which response by the nurse is most appropriate? 1. “Focusing on diet and exercise alone should control your weight.” 2. “Your depression is much better now, so your medication is helping you.” 3. “Look at all the positive things that have happened to you since you started Remeron.” 4. “I hear how difficult this is for you and will help you approach the doctor about it.” 46. 4. RATIONALE: The nurse should express concern for the client and offer to help the client speak with the physician which will lend support to the client’s concerns. The client who has stopped the medication must be taken seriously because medication non-compliance could result in a recurrence of symptoms of depression. Telling the client to focus on diet and exercise ignores the client’s feelings and subtly implies the weight gain is the client’s fault. Pointing out that the medication has helped and that positive things have happened since the depression lifted may be true, but it does not address the client’s current feelings or needs. 47. When developing a teaching plan for a client about medications prescribed for depression, which of the following is most important for the nurse to include? 1. Pharmacokinetics of the medication. 2. Current research related to the medication. 3. Management of common adverse effects. 4. Dosage regulation and adjustment. 47. 3. RATIONALE: Compliance with medication therapy is crucial for the client with depression. Medication noncompliance is the primary cause of relapse among psychiatric clients. Therefore, the nurse needs to teach the client about managing common adverse effects to promote compliance with medication. Teaching the client about the medication’s pharmacokinetics may help the client to understand the reason for the drug. However, teaching about how to manage common adverse effects to promote compliance is crucial. Current research about the medication is more important to the nurse than to the client. Teaching about dosage regulation and adjustment of medication may be helpful, but typically the physician, not the client, is the person in charge of this aspect. 48. The client with severe major depression has been taking Lexapro 10 mg (escitalopram) daily for the past 2 weeks. Which of the following should the nurse monitor most closely at this time? 1. Suicidal ideation. 2. Sleep. 3. Appetite. 4. Energy level. 48. 1. RATIONALE: After about 2 weeks of medication therapy, the nurse should expect improvements in sleep, appetite and energy though mood may not have improved significantly yet. The increased energy related to better sleep and food intake gives the client the ability to act on thoughts to harm self (suicide) since the depressed mood has not completely lifted. Question Answer/Rationale 49. A client taking paroxetine (Paxil) 40 mg P.O. every morning tells the nurse that her mouth “feels like cotton.” Which of the following statements by the client necessitates further assessment by the nurse? 1. “I’m sucking on ice chips.” 2. “I’m using sugarless gum.” 3. “I’m sucking on sugarless candy.” 4. “I’m drinking 12 glasses of water every day.” 49. 4. RATIONALE: Dry mouth is a common, temporary side effect of paroxetine. The nurse needs to further assess the client’s water intake when the client states she is drinking lots of water. Excessive intake of water could be harmful to the client and could lead to electrolyte imbalance. Dry mouth is caused by the medication, and drinking a lot of water will not eliminate it. Sucking on ice chips or using sugarless gum or candy is appropriate to ease the discomfort of dry mouth associated with paroxetine 50. The client with depression has been consistent with taking 12.5 mg of paroxetine (Paxil) extended release daily. The nurse judges the client to be benefiting from this drug therapy when the client demonstrates which of the following behaviors? Select all that apply. 1. Takes 2-hour evening naps daily. 2. Completes homework assignments. 3. Decreases pacing. 4. Increases somatization. 5. Verbalizes feelings. 50. 2, 3, 5. RATIONALE: Symptoms of depression include depressed mood, anhedonia, appetite disturbance, sleep disturbance, psychomotor disturbance, fatigue, feelings of worthlessness, excessive or inappropriate guilt, decreased concentration, and recurrent thoughts of death or suicide. Paroxetine is a selective serotonin reuptake inhibitor antidepressant that also can be used to treat anxiety. Improved concentration, verbalization of feelings, and decreased agitation or pacing are signs of improvement. Taking 2-hour evening naps daily is still a sign of fatigue or lack of energy, and the increased use of somatization (bodily complaints) could be signs of continued symptoms of depression. 51. A client with major depression has sleep & appetite disturbances, a flat affect and is withdrawn. He has been taking fluvoxamine (Luvox) 50 mg twice daily for 5 days. Which is most important to report to the next shift? 1. Client’s flat affect. 2. Client’s interacting with a visitor. 3. Client sleeping from 11 p.m. to 6 a.m. 4. Client spending the entire evening in her room. 51. 3. RATIONALE: The most important behavior to report to the next shift is that the client was able to sleep from 11 p.m. to 6 a.m. This indicates that improvement in the symptoms of depression is occurring as a result of pharmacologic therapy. The nurse would expect to observe improvement in sleep, appetite, and psychomotor behavior first before improvement in cognitive symptoms. The client’s flat affect is still a symptom of depression. The fact that the client had a visitor is not as important as changes in the client’s behavior. Spending the evening in the room is a continuation of the client’s withdrawn behavior and is important to report but not as important as the improvement in sleep. 52. Which of the following is the best predictor of a client’s favorable response to the choice of an antidepressant? 1. The drug’s side effect profile. 2. The client’s age at diagnosis. 3. The cost of the medication. 4. A favorable response by a family member. 52. 4. RATIONALE: A favorable response by a family member to a medication and a previous response to medication are good predictors of a favorable client response to a medication because the illness is genetic and hereditary. Although the side effects of the drug, the client’s age at diagnosis, and the cost of the medication are important factors to consider when choosing antidepressant therapy, this information does not necessarily predict how a client will respond to a specific drug. Question Answer/Rationale 53. A nurse is educating a client who has dysthymia about possible treatment for the disorder. Which response by the nurse is most appropriate? 1. “Antidepressants, particularly the SSRI group, offer you the best treatment for your dysthymia.” 2. “Doctors recommend that clients with dysthymia receive electroconvulsive therapy (ECT) to treat their disorder.” 3. “Because you have a mild, though long-lasting dysthymic mood, psychotherapy can usually bring improvement with less likelihood of the need for medication.” 4. “Since your dysthymia indicates a long-lasting mild depression, long-term psychoanalysis is best for you.” 53. 3. RATIONALE: Dysthymia is a milder, persistent type of depression in which sufferers are able to minimally carry on their work (Option 3). Options 1 and 2 are treatments used for occurrences of major depression with ECT being used as a last resort when several medications fail. Psychoanalysis is a very involved, long-term treatment rarely used now due to its cost and the long period of treatment required for results. Bipolar Disorder 54. A client is brought to the hospital by police & admitted involuntarily. She is diagnosed with bipolar disorder, manic phase. The MD orders lithium 300 mg three times a day. The client refuses her morning dose of lithium. The nurse should next: 1. Force the client to take the lithium because of the client’s involuntarily admission status. 2. Contact the physician to change the lithium order to be given intramuscularly. 3. Inform the client that she retains the right to refuse medication despite her involuntary admission. 4. Tell the client that certain privileges will be revoked if she does not take the medication. 54. 3. RATIONALE: The only right the client loses because of her involuntary admission is the right to leave the hospital whenever she wishes. Forcing the client to take medication and revoking privileges are punitive and coercive. Lithium is not given intramuscularly. 55. A young adult diagnosed with bipolar disorder has been managing the disorder effectively with meds and treatment for several years. She suddenly becomes manic. The nurse reviews the medication record. Which of these may have contributed to the development of his manic state? 1. Elavil (amitriptyline). 2. Prednisone. 3. BuSpar (buspirone). 4. Neurotonin (gabapentin). 55. 2. RATIONALE: The use of prednisone or other steroids can initiate a manic state in a bipolar client even if he is well controlled on medication. The other medications would decrease the client’s depression, mood swings, and anxiety, making him calmer rather than more agitated. Question Answer/Rationale 56. The client with acute mania has been admitted to the inpatient unit voluntarily. The nurse approaches the client with medication to be taken orally as ordered by the physician. The client states, “I don’t need that stuff.” Which response by the nurse is best? 1. “You can’t refuse to take this medication.” 2. “If you don’t take it orally, I’ll give you a shot.” 3. “The medication will help you feel calmer.” 4. “I’ll get you some written information about the medication.” 56. 3. RATIONALE: The nurse should concisely explain the benefit of the medication to the client to increase the possibility of compliance. The client has the right to refuse treatment, which in this instance is the medication. If the client was under involuntary commitment and the hospital had received a court order to treat, the client would have to comply with taking the medication and the physician would usually order the medication to be give intramuscularly if the oral medication was refused. The nurse would not threaten the client by stating that a shot will be given when there is no physician order and court order to treat. Giving written medication information to a client with acute mania is poor nursing judgment because a client with acute mania cannot benefit from written information due to his impaired ability to focus and concentrate. 57. A nurse observes a male client who is hyperactive and intrusive sitting very close to a female client with his arm around her shoulders. The nurse hears the male client tell a sexually explicit joke. The nurse approaches the client and asks him to walk down the hallway. Which of the following statements by the nurse should benefit the client? 1. “She will not want to be around you with that kind of talk.” 2. “Telling sexual jokes and touching others is not permitted here.” 3. “You need to be careful about what you say to other people.” 4. “I think a time-out in your room would be appropriate now.” 57. 2. RATIONALE: The nurse clearly informs the client about behavior that is unacceptable on the unit, such as voicing jokes with sexual content and touching others. Setting limits on behavior provides safety and security to the client and conveys to the client that he is worthy of help. Saying “she will not want to be around you with that kind of talk” and “you need to be careful about what you say to others” does not clearly inform the client about behaviors that are unacceptable and implies that the client can control behaviors if he chooses. A time-out in the client’s room does not inform the client about the inappropriateness of his behaviors and could be interpreted by the client as punitive as well as diminishing his self-esteem. 58. A client states to a nurse, “Hey sweetie, you’re looking good today.” Which of the following responses by the nurse is best? 1. “Thank you for being so kind and thoughtful.” 2. “I know you are only teasing me.” 58. 3. RATIONALE: The nurse states her identity and purpose for being on the unit to clarify any misperception by the client. Saying “thank you for being so kind,” “I know you are only teasing me,” or “I am not here to receive compliments from clients” are nontherapeutic statements and do not clarify Question Answer/Rationale 3. “My name is Molly, and I am a nurse on the unit today.” 4. “I am not here to receive compliments from clients.” the nurse’s identity and purpose. 59. A client with acute mania fails to respond to a nurse’s interventions to decrease his agitation. The nurse has attempted to defuse the client’s anger, but the client refuses to participate in interventions that would lower anxiety. Which action should the nurse take next? 1. Seclude the client. 2. Restrain the client. 3. Medicate the client. 4. Control the client. 59. 3. RATIONALE: The nurse should medicate the client who does not respond to verbal interventions and whose anxiety is escalating. This will reduce the client’s anxiety and agitation and prevent harm or injury to the client and others. Seclusion, restraint, and controlling the client are a last resort and require a physician’s order and close assessment for when the orders can be discontinued. 60. The client with mania is irritable and insulting to a nursing assistant. The nursing assistant states, “I can’t believe Mark is so rude. Shouldn’t he be overly happy?” Which of the following responses by the nurse should help the nursing assistant understand the client’s behavior? 1. “It’s our responsibility to listen to him even though we might not like what he’s saying.” 2. “We must reprimand Mark for doing that because there is no reason for him to behave like that.” 3. “I will go and speak to him about his behavior and make sure he understands that he needs to control what he is saying.” 4. “I know it’s difficult but Mark is a client whose irritable mood is a symptom of his mania.” 60. 4. RATIONALE: The nurse should help the nursing assistant understand the client’s behavior by stating that his irritable mood is a symptom of mania. Not all clients with mania are euphoric or have an expansive mood. Saying, “It’s our responsibility to listen to him even though we might not like what he’s saying” does not help the nursing assistant understand the client with mania. Reprimanding the client for his behavior or asking him to control his behavior are inappropriate actions and show poor nursing judgment and a lack of understanding of the manic client. 61. Which milieu activity should the nurse recommend to a client with acute mania? Select all that apply. 1. Scheduled rest periods. 2 2. Relaxation exercises. 3. Listening to soft music. 4. Watching television. 5. Aerobic exercises. 61. 1, 2, 3, 5. RATIONALE: Scheduled rest periods, relaxation exercises, and listening to soft music are activities that reduce environmental stimuli for the client who is hyperactive, talkative, easily distracted, irritable, and angry. Aerobic exercise is also beneficial to discharge some of the client’s need to be active. Watching television is not therapeutic because it would stimulate the client with acute mania. 62. A nurse is assessing a client experiencing hypomania who wants to stop her mood stabilizing medication because she is “feeling good,” has a high energy level and thinks she is 62. 3. RATIONALE: Reminding the client of past consequences of stopping the medication may help her realize the risks of stopping the medication again. Options 1 and 4 encourage the client’s misperception that she only Question Answer/Rationale productive at work. Which response by the nurse is most appropriate? 1. “Maybe you really don’t need your medication anymore.” 2. “If you stop your medication, your behavior will quickly spiral out of control.” 3. “I believe you were hospitalized the last time you stopped your medication.” 4. “Why don’t you cut your medication dosage in half for a while and see how you respond?” needs medication when she feels depressed or manic rather than recognizing that her mood stabilizer can prevent her from experiencing those extreme highs and lows. Option 2 describes what will happen if she stops her medication, but if the client had recognized the consequences, she wouldn’t be contemplating stopping the medication. 63. The client with acute mania is prescribed 600 mg of lithium (lithium carbonate) P.O. three times per day. The physician also orders 5 mg of haloperidol (Haldol) P.O. at bedtime. Which action should the nurse take? 1. Administer the medication as ordered. 2. Question the physician about the order. 3. Administer the Haldol, but not the lithium. 4. Consult with the nursing supervisor before administering the medications. 63. 1. RATIONALE: The nurse should administer the medication as ordered. Lithium has a clinical response lag time of 1 to 2 weeks. Haloperidol is prescribed temporarily to produce a neuroleptic effect until the lithium starts to produce a clinical response. Haldol is usually discontinued when the lithium starts to take effect. 64. The client with an Axis I diagnosis of bipolar disorder, manic phase, states to the nurse, “I’m the Queen of England. Bow before me.” The nurse interprets this statement as important to document as which of the following areas of the mental status examination? 1. Psychomotor behavior. 2. Mood and affect. 3. Attitude toward the nurse. 4. Thought content. 64. 4. RATIONALE: The client’s statement, “I’m the Queen of England. Bow before me,” is an example of a grandiose delusion and refers to thought content of the mental status examination. Examples of psychomotor behavior to be documented would include excited, typically exaggerated and repetitive physical movements and excessive talking and gesturing. Mood is a subjective state, and affect is an observable expression of emotion. Mood is what a client tells you she is feeling, and affect is what you see the client feeling. For example, the client may state that she feels sad or happy in reference to mood. Affect refers to the display of physical emotion, commonly described as “appropriate” or “flat.” Attitude toward the nurse refers to the client’s behavior in the presence of the nurse during the mental status examination (pleasant and cooperative, irritable and guarded). 65. The client is laughing and telling jokes to a group of clients. Suddenly, the client is crying and talking about a death in the family. A moment later, the client is laughing and joking again. The nurse should: 1. Call the psychiatrist for an order for Ativan as needed. 65. 4. RATIONALE: Decreasing external stimuli is the intervention most likely to decrease the emotional lability and minimize its effect on other clients. While the client is displaying emotional lability, this behavior has not reached the level where involuntary isolation (seclusion) or physical restraint is needed. The client is not totally out of control Question Answer/Rationale 2. Place the client in seclusion and call the psychiatrist for an order for the seclusion. 3. Ignore the client’s behavior in order not to give the client too much attention. 4. Ask the client to come to a quiet area to talk to the nurse individually. 66. A client with acute mania exhibits euphoria, pressured speech, and flight of ideas. The client has been talking to the nurse nonstop for 5 minutes and lunch has arrived on the unit. Which of the following should the nurse do next? 1. Excuse self while telling the client to come to the dining room for lunch. 2. Tell the client he needs to stop talking because it’s time to eat lunch. 3. Do not interrupt the client but wait for him to finish talking. 4. Walk away and approach the client in a few minutes before the food gets cold. 66. 1. RATIONALE: The nurse would excuse herself, showing respect and regard for the client, while telling the client to come to the dining room for lunch. Acutely manic clients need clear, concise comments and directions. Telling the client that he needs to stop talking because it’s lunchtime is disrespectful and does not give the client directions for what he needs to do. Using the familiar skill of waiting without interrupting until the person pauses would not be effective with the very talkative, manic client. Walking away and approaching the client after a few minutes before the food gets cold is not helpful because the client would probably continue talking. 67. A female client with acute mania brings six suitcases and three shopping bags of personal belongings on admission to the unit. When informed that some of the suitcases and bags need to be returned home with her husband because of a lack of storage space, the client begins to use profanity against the nurse. Which of the following responses by the nurse is most therapeutic? 1. “You’re acting inappropriately.” 2. “I won’t tolerate your talking to me like that.” 3. “Swearing and profanity are unacceptable here.” 4. “We don’t want to put you in seclusion yet.” 67. 3. RATIONALE: By stating to the client, “Swearing and profanity is unacceptable here,” the nurse is setting limits in a nonpunitive manner for behavior that is inappropriate or threatening to other clients and staff. Setting limits helps the client regain self-control, prevents alienation from others, and preserves self-esteem. It is common for the irritable manic client to misperceive the nurse’s and other’s statements and intentions, feel threatened, and respond in a manner that is out of character for the client when not in a manic phase. Stating that the client is acting very inappropriately, that the nurse will not tolerate the client’s swearing and profanity, or threatening to put the client in seclusion is threatening and punitive and thus nontherapeutic. 68. The husband of a client who is experiencing acute mania and is swearing and using profanity apologizes to the nurse for his wife’s behavior. Which of the following replies by the nurse is most therapeutic? 1. “This must be difficult for you.” 2. “It’s okay. We’ve heard worse.” 3. “How long has she been like this?” 68. 1. RATIONALE: Stating that this must be difficult for the husband conveys empathy and understanding and offers him the opportunity to voice his feelings to the nurse. Telling the husband that it is okay and that the nurse has heard worse is inappropriate and minimizes the impact of the wife’s illness on the husband. Asking about the length of the client’s illness or telling the husband that his wife needs some medication ignores the husband’s feelings, thereby minimizing his self-respect. Question Answer/Rationale 4. “She needs some medication.” 69. The nurse overhears a client with acute mania who is euphoric and flirtatious attempting to be sexually inappropriate with other clients by talking about a sexual exploit to a group of clients seated at a table. Which of the following should the nurse do next? 1. Continue walking down the hall, ignoring the conversation. 2. Speak to the client later in private while saying nothing at this time. 3. Tell the client others may not want to hear about sex, and invite him to play a game of ping-pong. 4. Inform the client that if he continues to talk about sex no one will want to be around him. 69. 3. RATIONALE: Telling the client that others may not want to hear about sex and inviting him to play a game of ping-pong with the nurse informs the client that even though his behavior is unacceptable, the nurse considers him worthy of help. The client’s thoughts and actions are out of control, and directing him to an activity with the nurse is an appropriate way of regaining control. The nurse is responsible for providing safety and security to this client and others on the unit. Continuing to walk down the hall while ignoring the conversation does nothing to meet the needs of this or other clients. Doing so also diminishes trust in the nurse. Speaking to the client later in private while saying nothing at the time allows the client to continue his provocative behavior instead of focusing his energy toward productive activity. Informing the client that if he continues to talk about sex, no one will want to be around him is not helpful because his behavior is a symptom of his illness and the statement diminishes his self-worth. 70. The client with acute mania states to the nurse, “I’m the prince of peace and can save the world. Those against me will find me and take me to another world. They will come. I know it.” The client is beginning to scan the room and starts to repeat his delusion. Which of the following responses by the nurse is most therapeutic? 1. “Describe the people who will come.” 2. “The staff and I will protect you.” 3. “You are not the prince of peace. Your name is Joe.” 4. “Let’s walk around the unit for a while.” 70. 4. RATIONALE: The nurse suggests an activity such as walking around the unit to distract the client from the paranoid grandiose delusion that could result in loss of control. This action interrupts the client’s anxious state and helps to redirect energy and focus on an activity based in reality. The focus must be on the underlying need or feeling of the delusion and not on the content. Asking the client to describe the people who will come challenges the client and forces the client to cling to the delusion. Stating that the nurse and staff will protect the client conveys agreement with the client’s belief system, reinforcing the client’s delusion. Telling the client that he is not the prince of peace and repeating his name challenges the client and his present belief system. Doing so may lead to decreased trust in the nurse and an aggressive response, or it may force the client to defend his beliefs. 71. A client with bipolar disorder, manic phase, is scheduled for a chest radiograph. Before taking the client to the radiology department, the nurse should: 1. Give a thorough explanation of the procedure. 2. Explain the procedure in simple terms. 3. Call security to be on standby for possible problems. 4. Cancel the appointment until the client can go unescorted. 71. 2. RATIONALE: The nurse needs to explain the procedure in simple terms because the client in a manic phase has difficulty concentrating, is easily distracted, and can misinterpret what the nurse states. Giving a thorough explanation of the procedure is not helpful and can confuse the client. Calling security to be on standby is inappropriate. If the nurse judges that the client might elope or become agitated, the nurse should schedule the appointment for another time. Canceling the appointment until the client can go unescorted is impractical and may not follow unit or hospital policy Question Answer/Rationale and the client’s treatment plan. 72. A client exhibiting euphoria, hyperactivity, and distractibility cannot remain seated at mealtimes long enough to eat an adequate amount of food. When developing the client’s plan of care, the nurse anticipates providing the client with “finger food” to eat while moving about the unit. Which of the following foods should the nurse include in the client’s plan of care? 1. Bacon, lettuce, and tomato sandwich. 2. Cheeseburger. 3. Ice cream cone. 4. Cut-up vegetables. 72. 2. RATIONALE: The nurse needs to provide the client who cannot sit long enough to eat adequate amounts of “finger foods,” or food that can be held and eaten while moving. High-protein and high-carbohydrate foods, such as a cheeseburger or peanut butter sandwich, are best for the hyperactive client to help maintain body weight. A bacon, lettuce, and tomato sandwich would not provide the client with adequate protein and carbohydrates. Additionally, this type of sandwich is difficult to carry around and can be dropped easily. An ice cream cone, although high in calories, would not provide the client with adequate protein. Cut-up vegetables are a poor selection because, although they are high in vitamins, they are low in protein, which is necessary for building and repairing body cells and tissues, and low in carbohydrates, which are needed for energy. 73. The client with bipolar disorder, manic phase, appears at the nurse’s station wearing a transparent shirt, miniskirt, high heels, 10 bracelets, and 8 necklaces. Her makeup is overdone and she is not wearing underwear. A pair of inverted underpants is on her head. The nurse should: 1. Tell the client to dress appropriately while out of her room. 2. Ask the client to put on hospital pajamas until she can dress appropriately. 3. Instruct the client to go to her room and change clothes. 4. Escort the client to h [Show More]
Last updated: 1 year ago
Preview 1 out of 43 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 05, 2022
Number of pages
43
Written in
Additional information
This document has been written for:
Uploaded
May 05, 2022
Downloads
0
Views
40

.png)

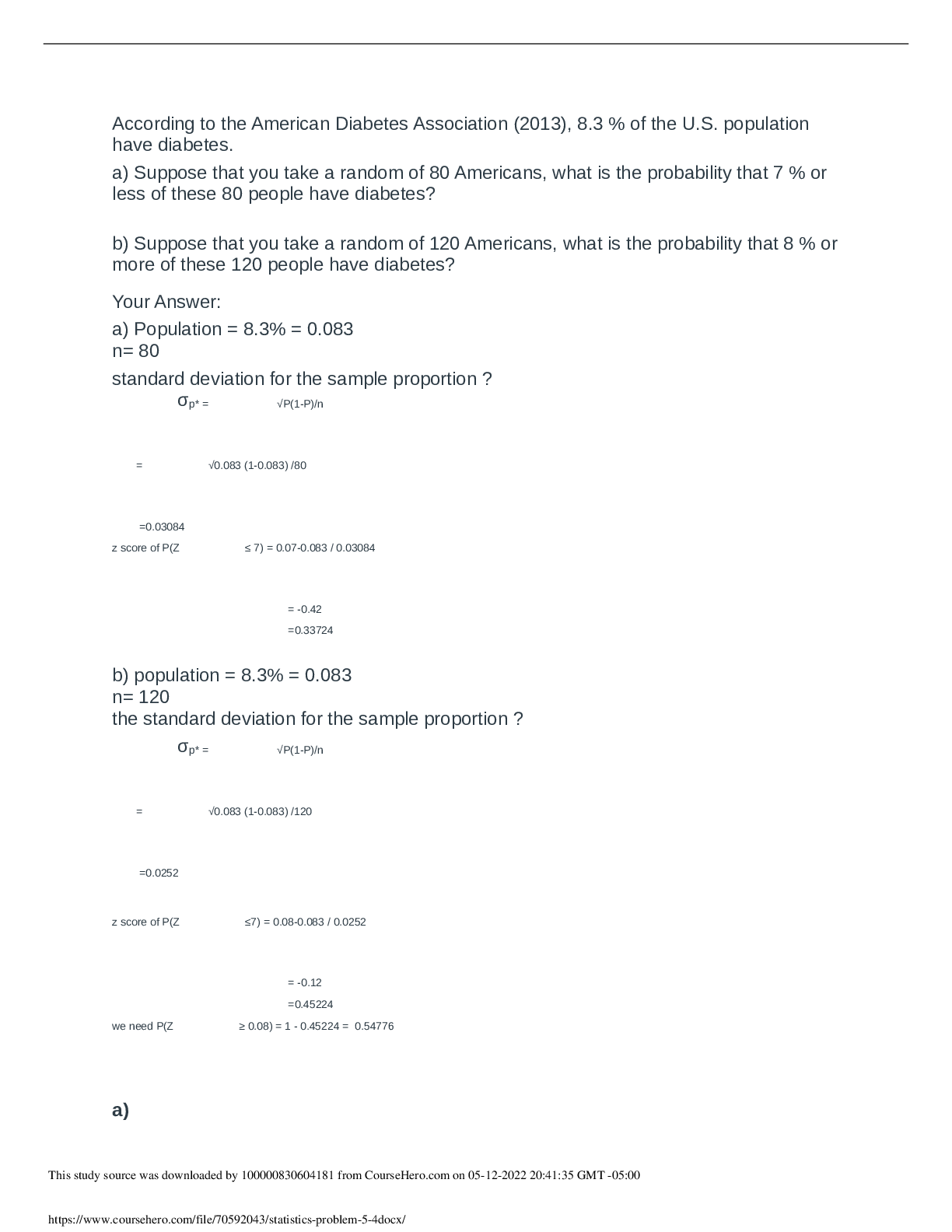
.png)
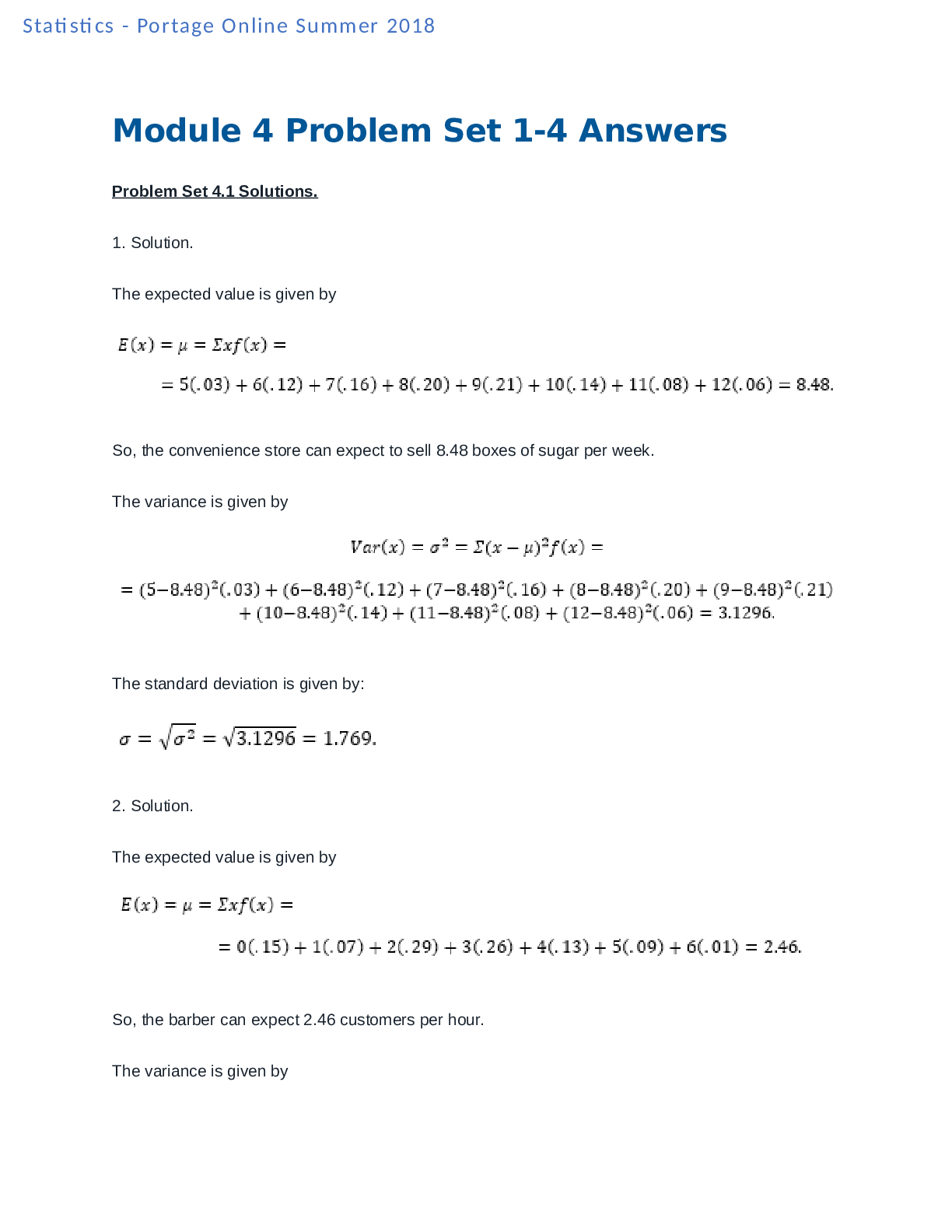
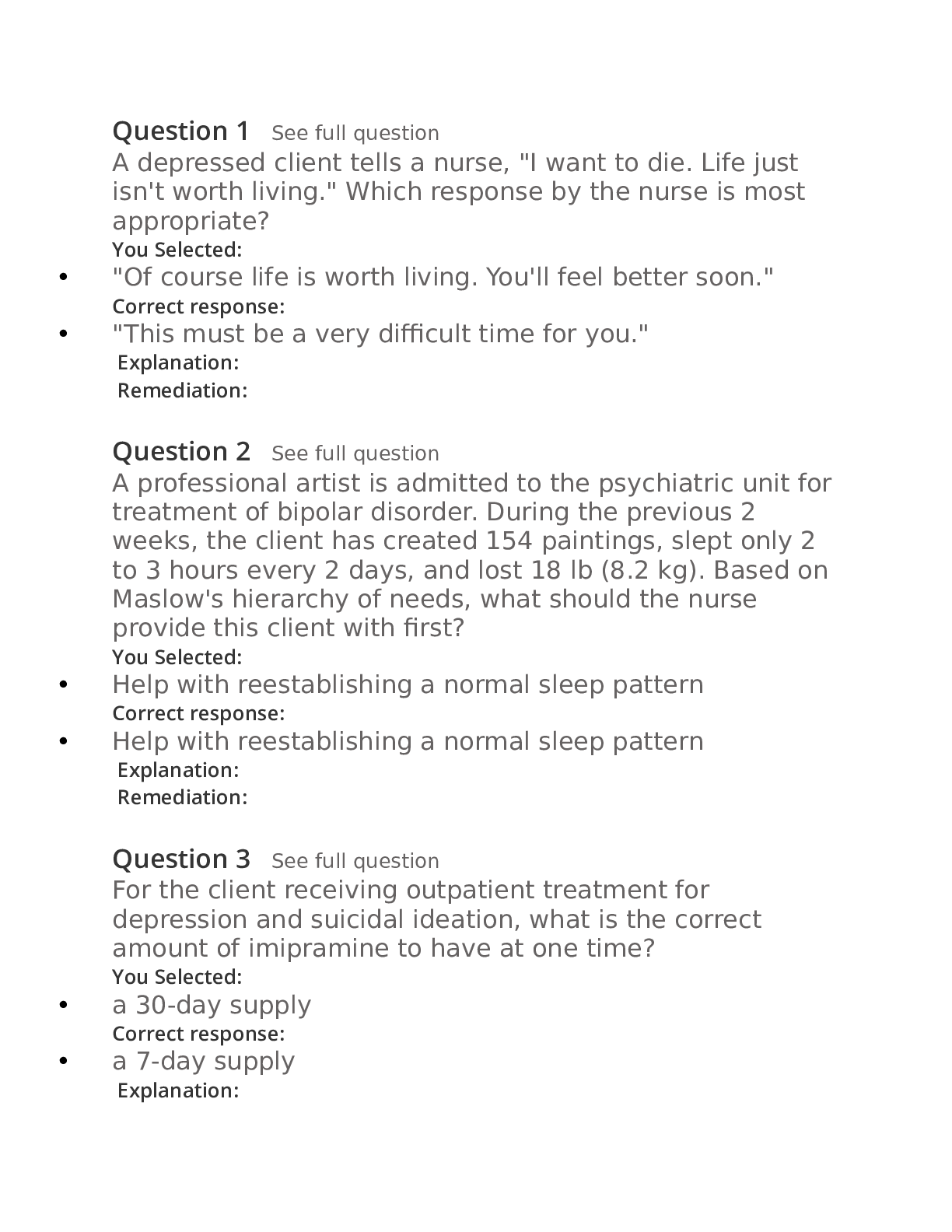

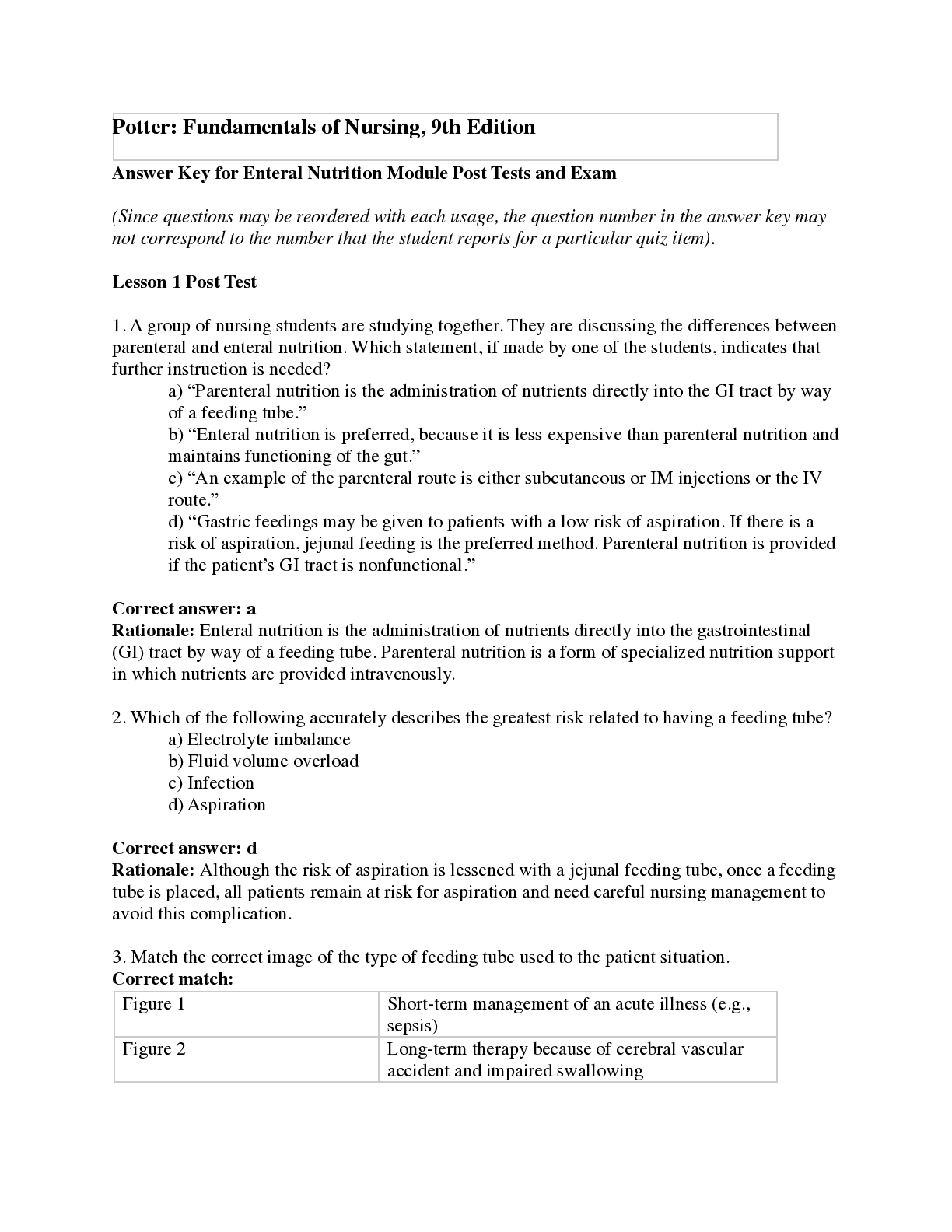
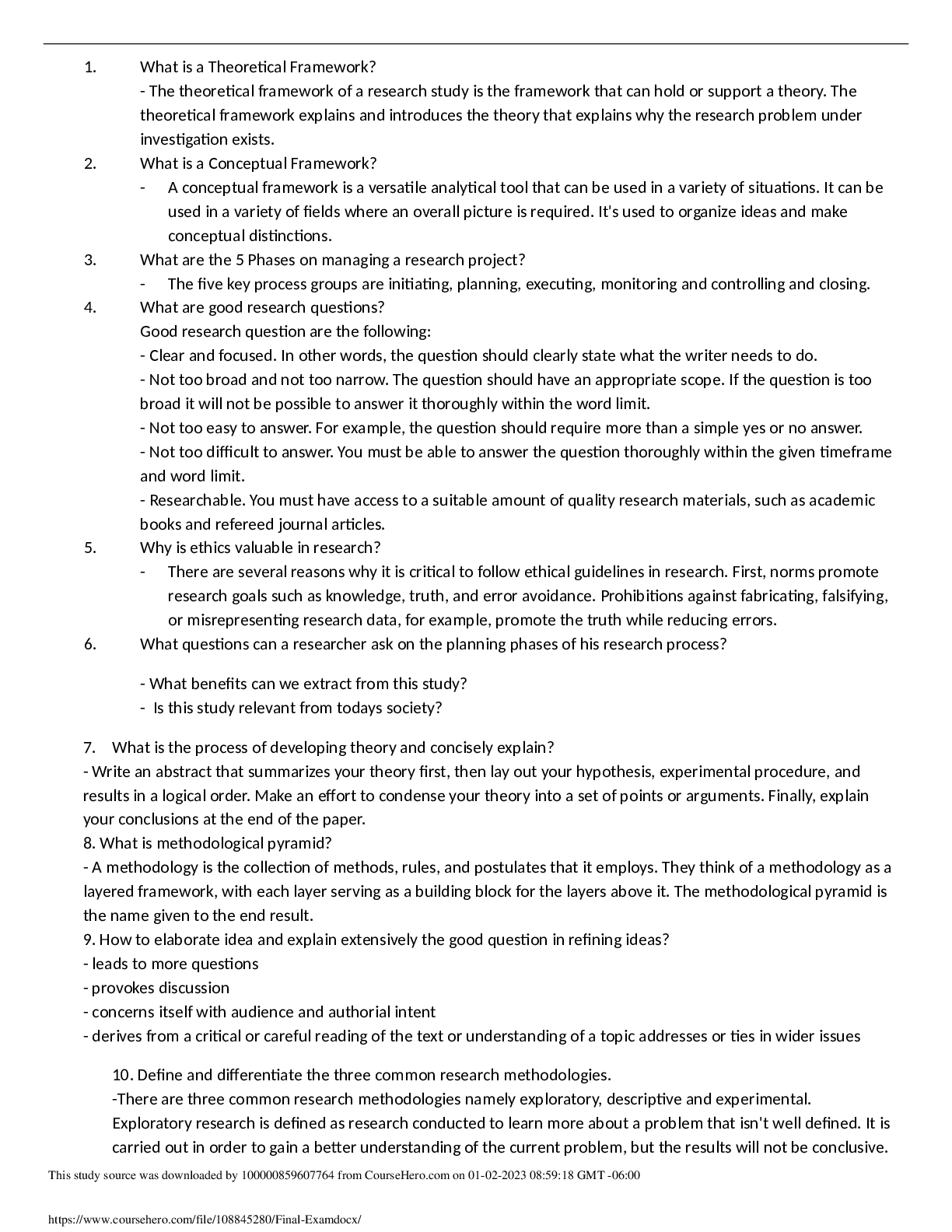
.png)
.png)
.png)
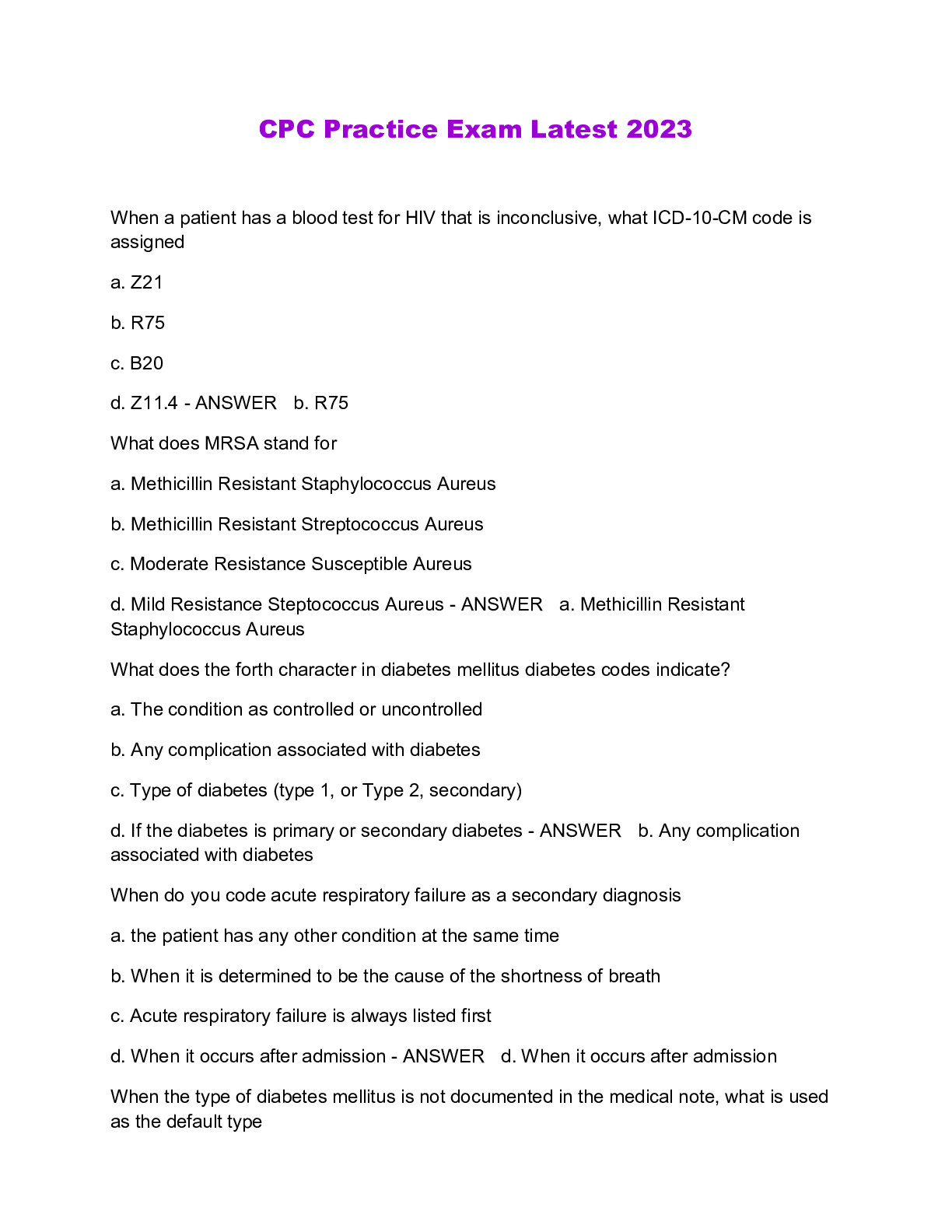
.png)


.png)

.png)