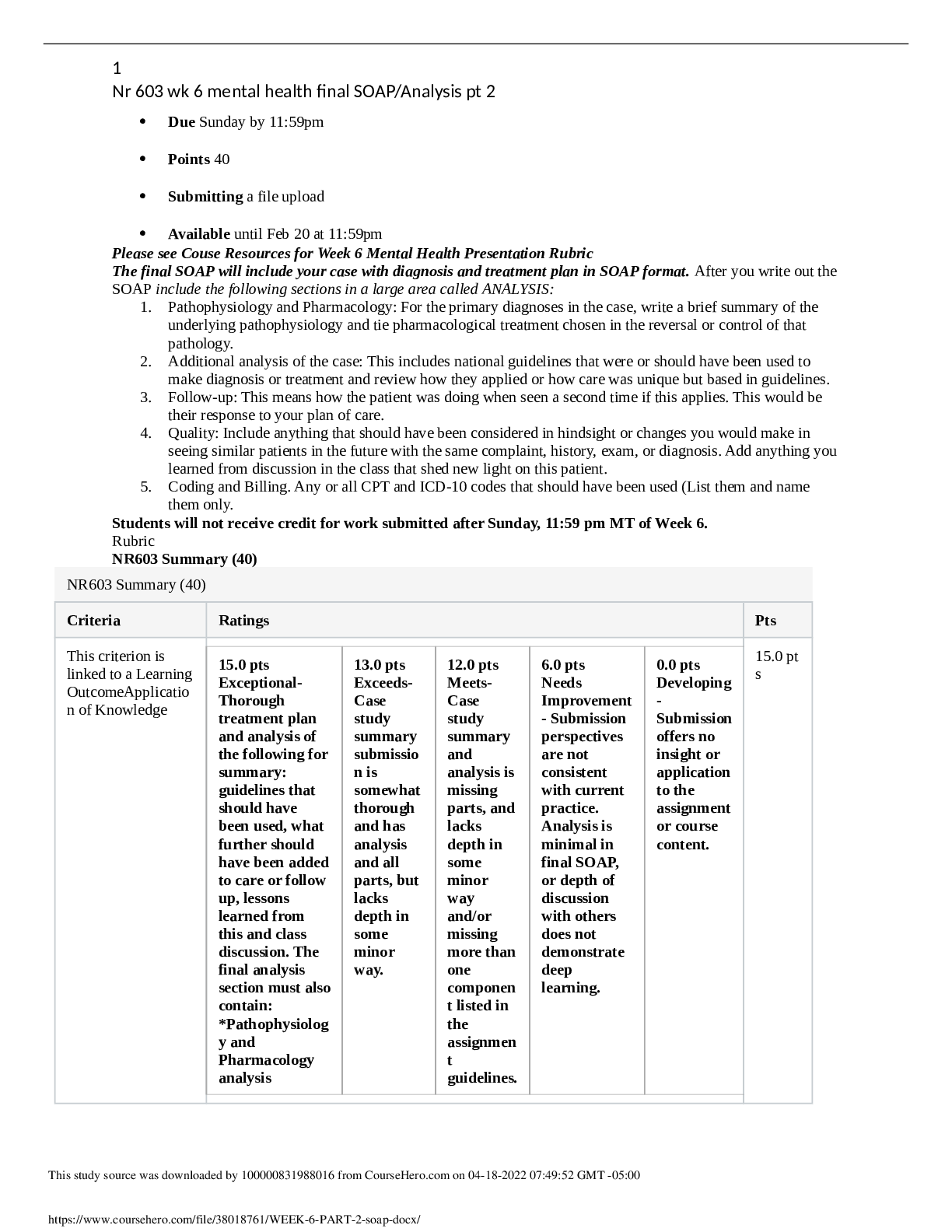
Summary NR 509 Week 5 Abdominal Pain SOAP Note
Document Content and Description Below
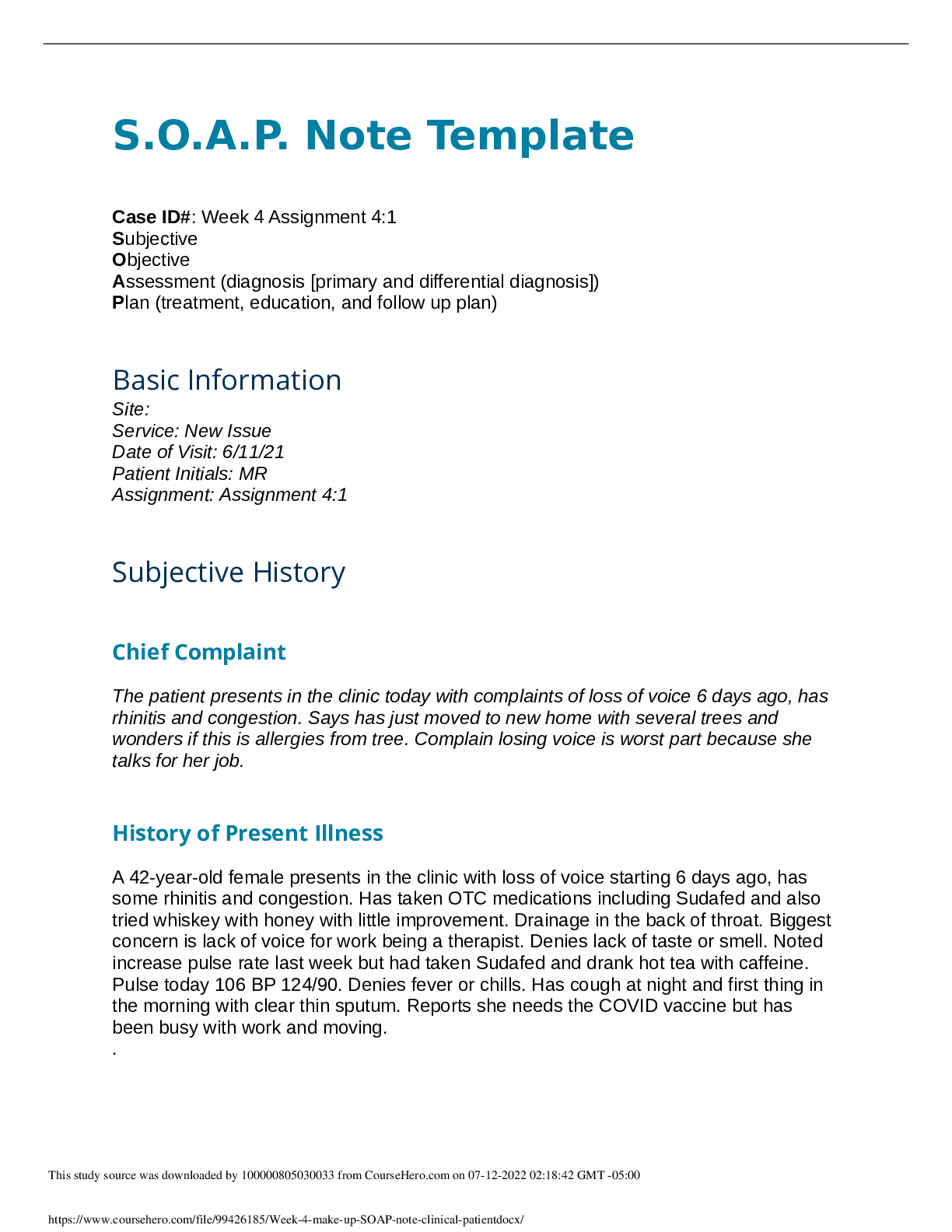
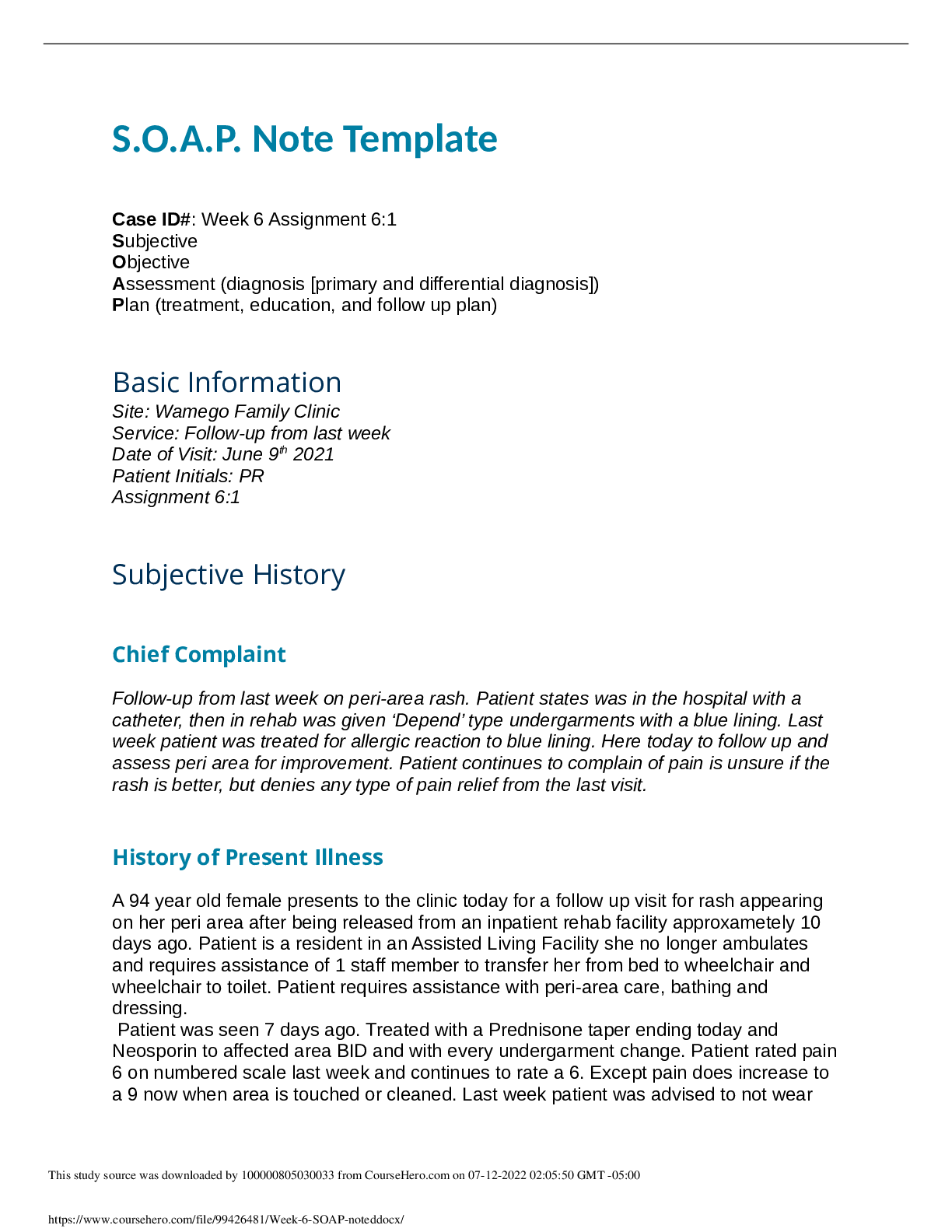
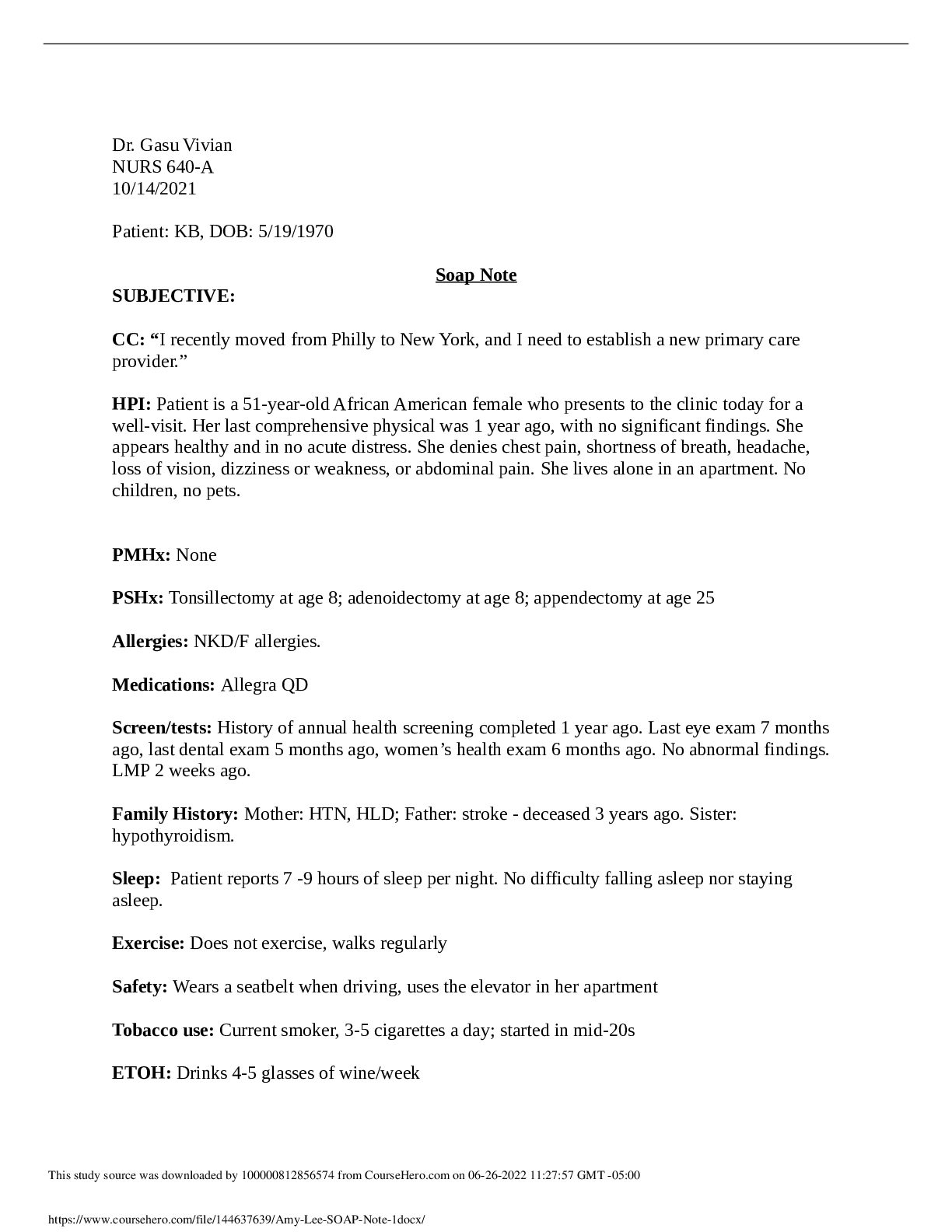
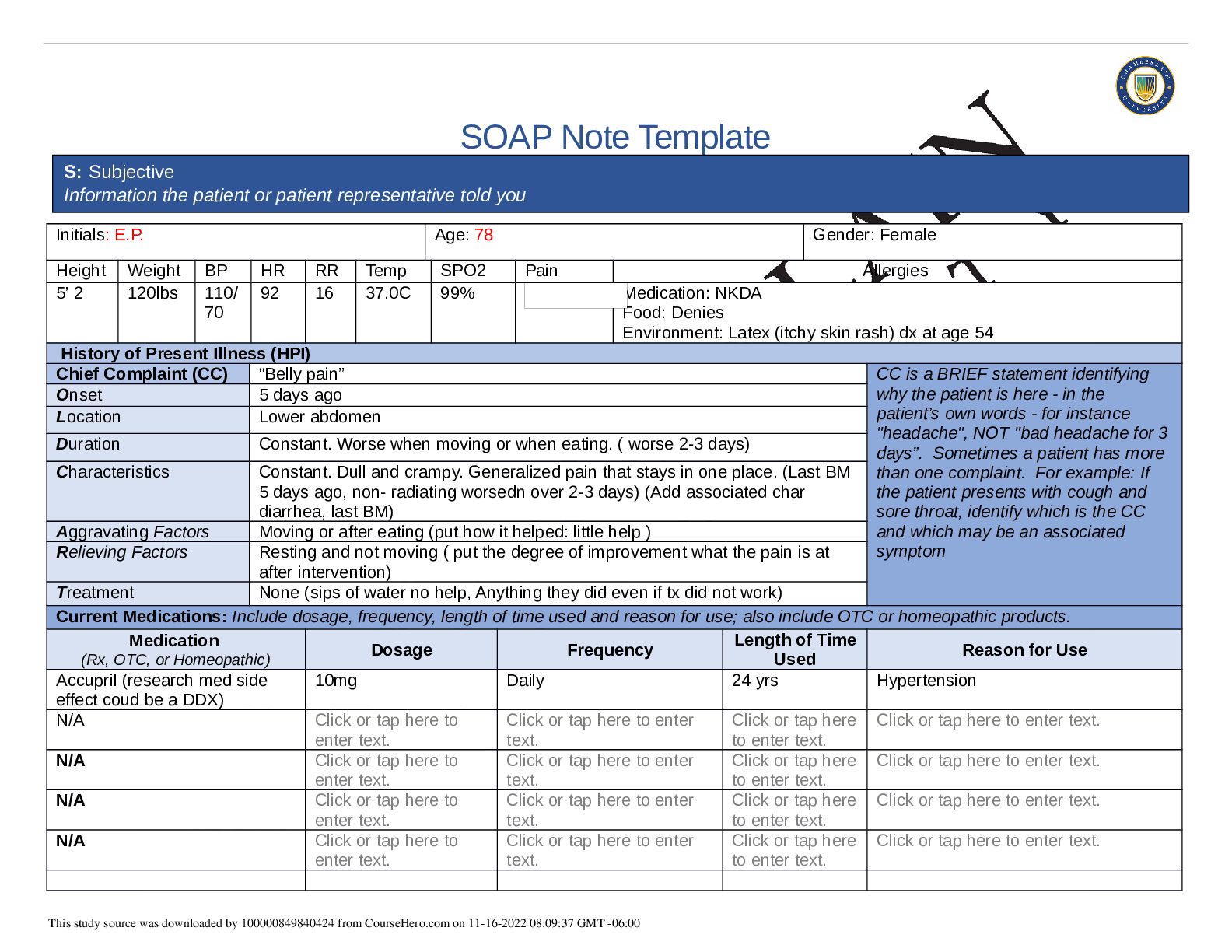
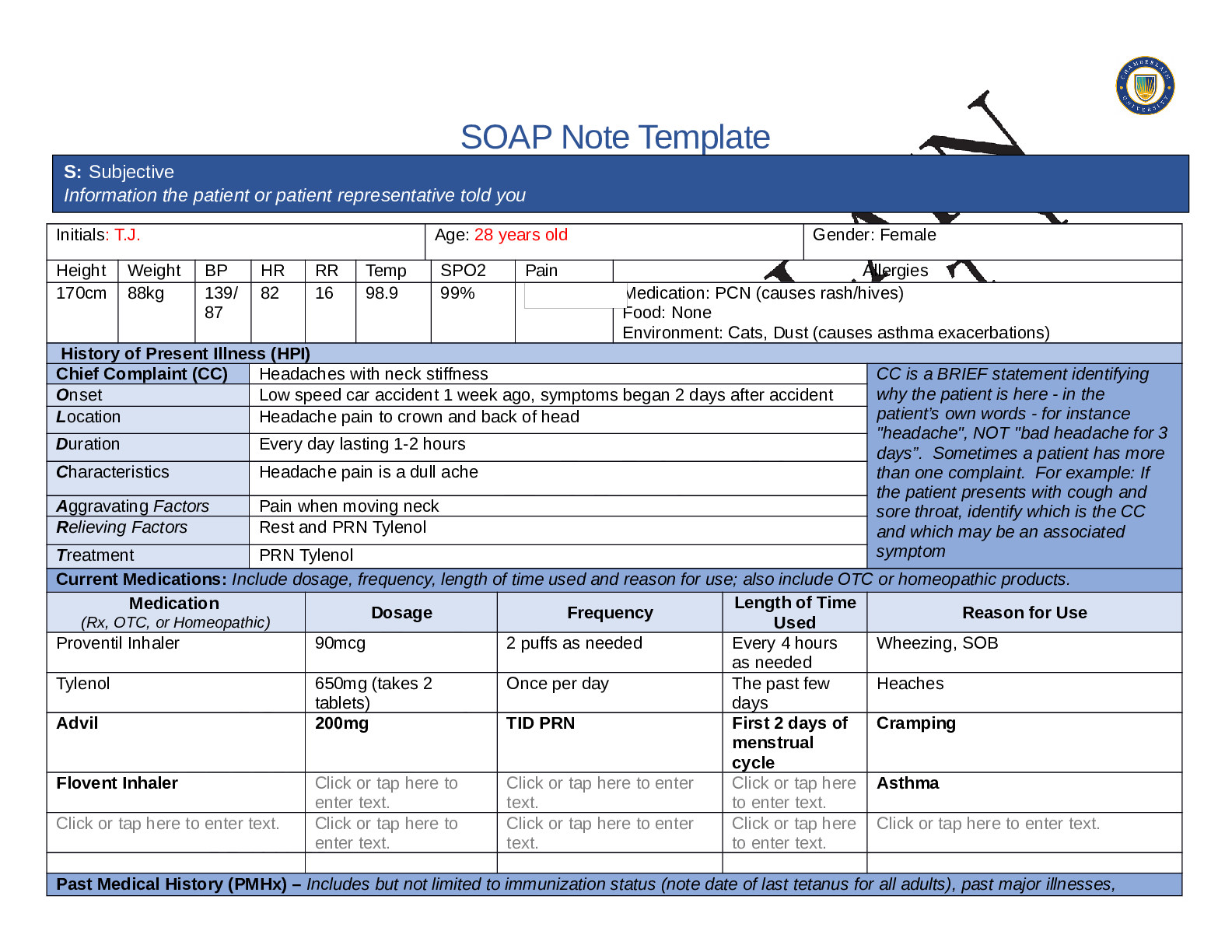
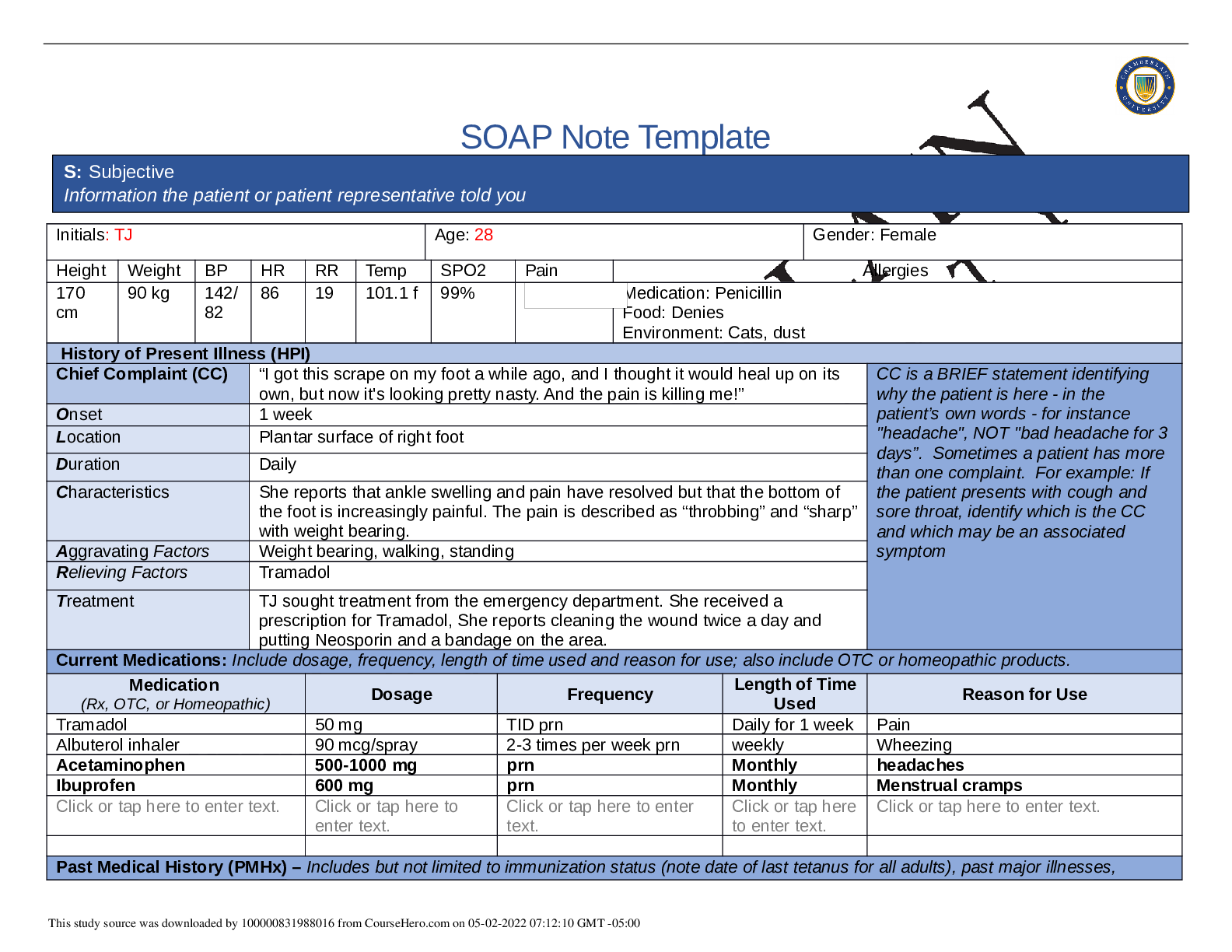
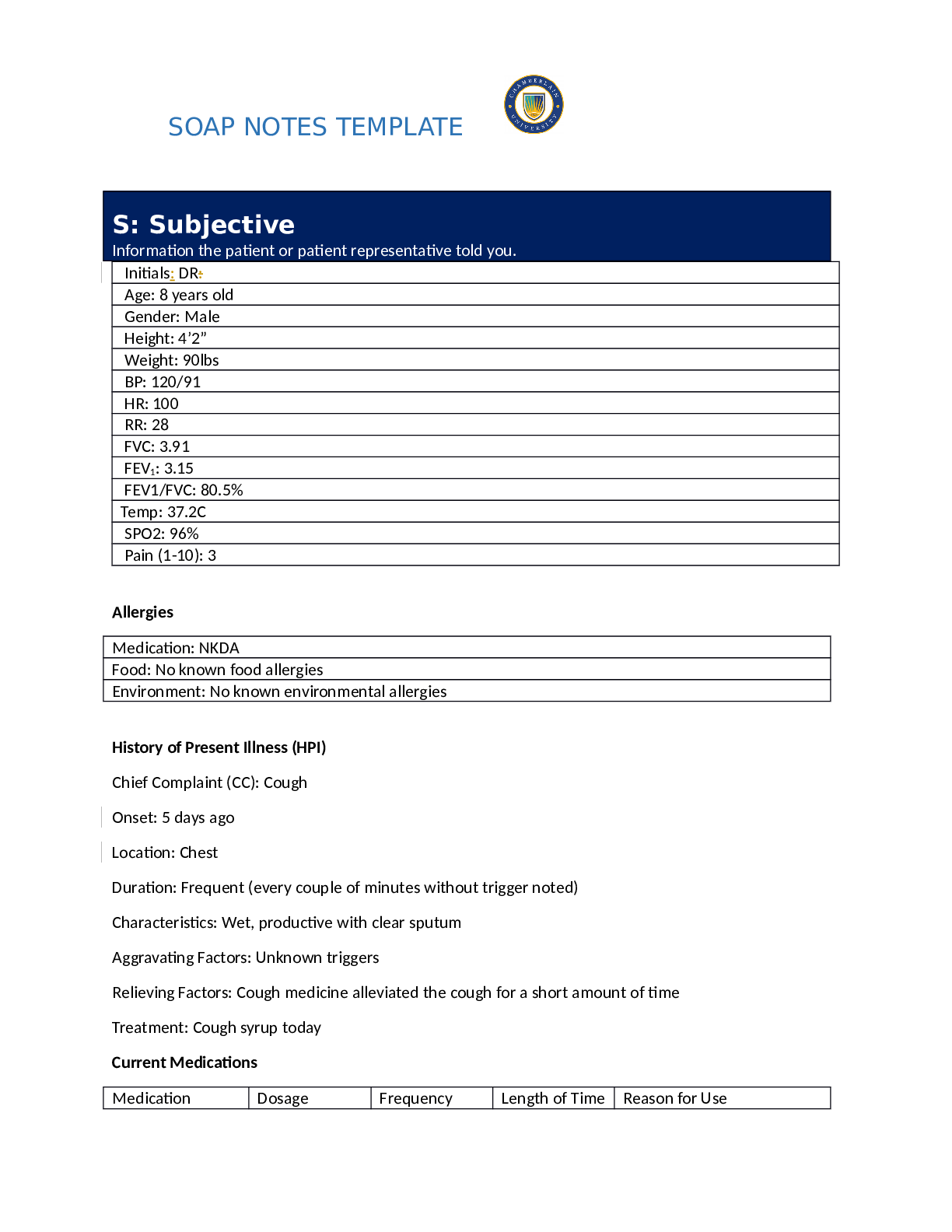
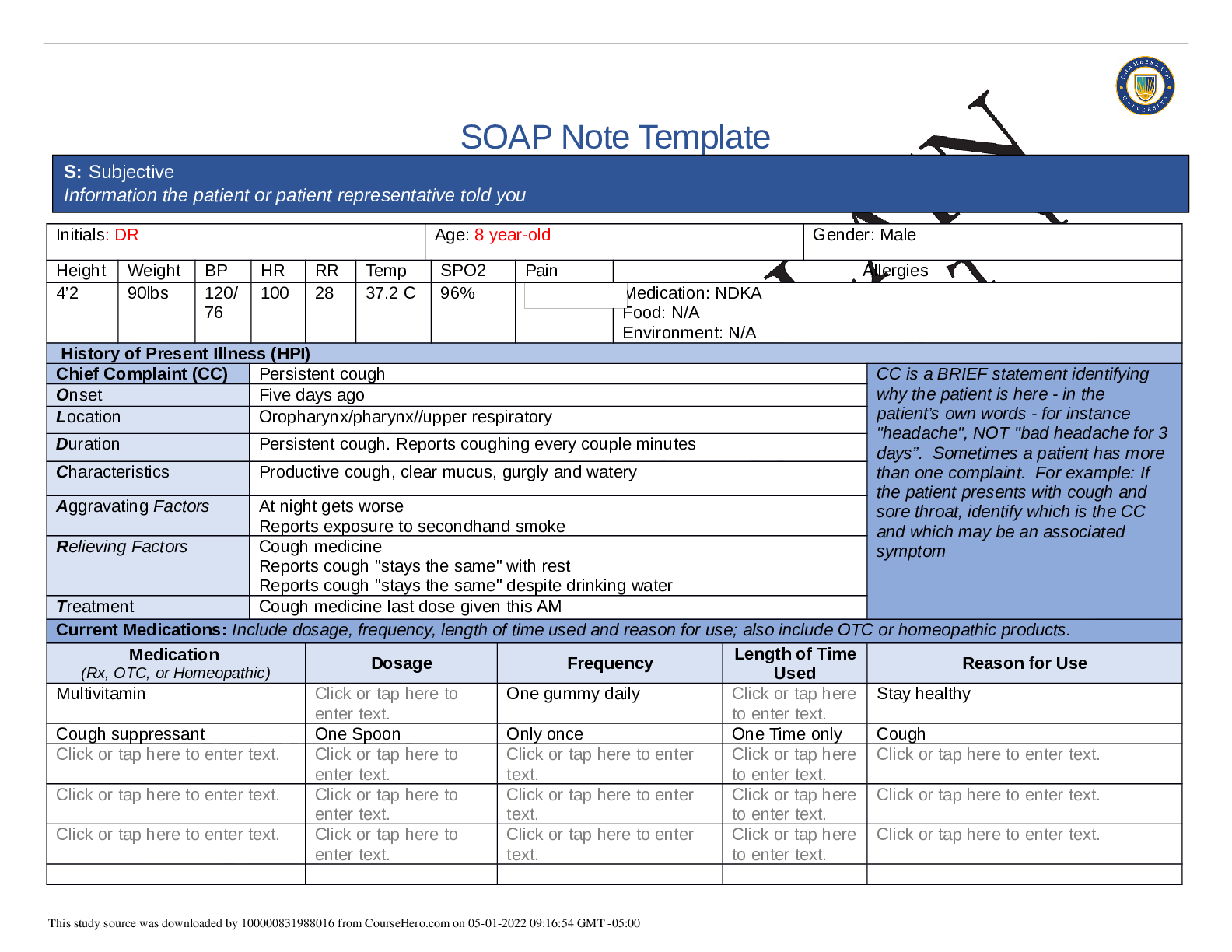
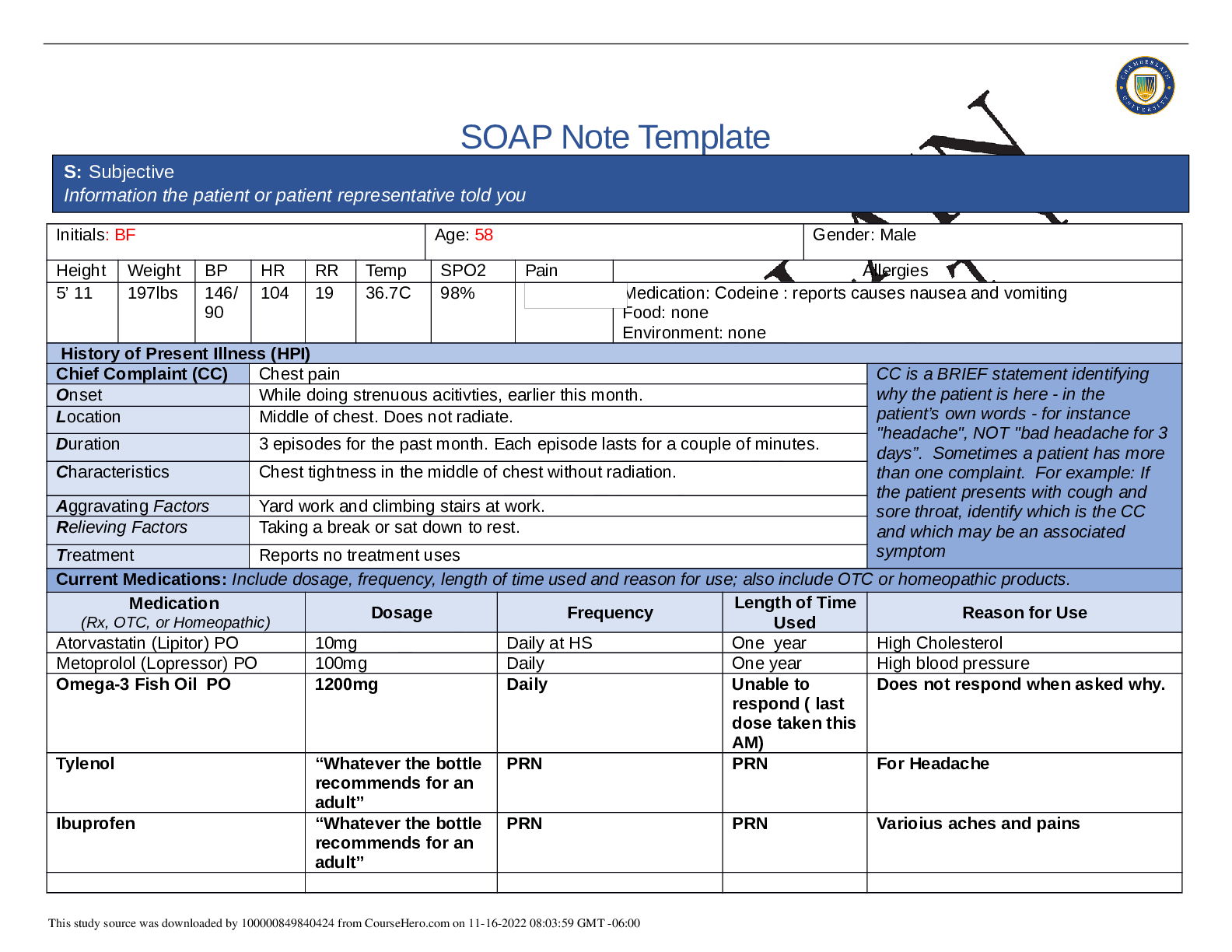
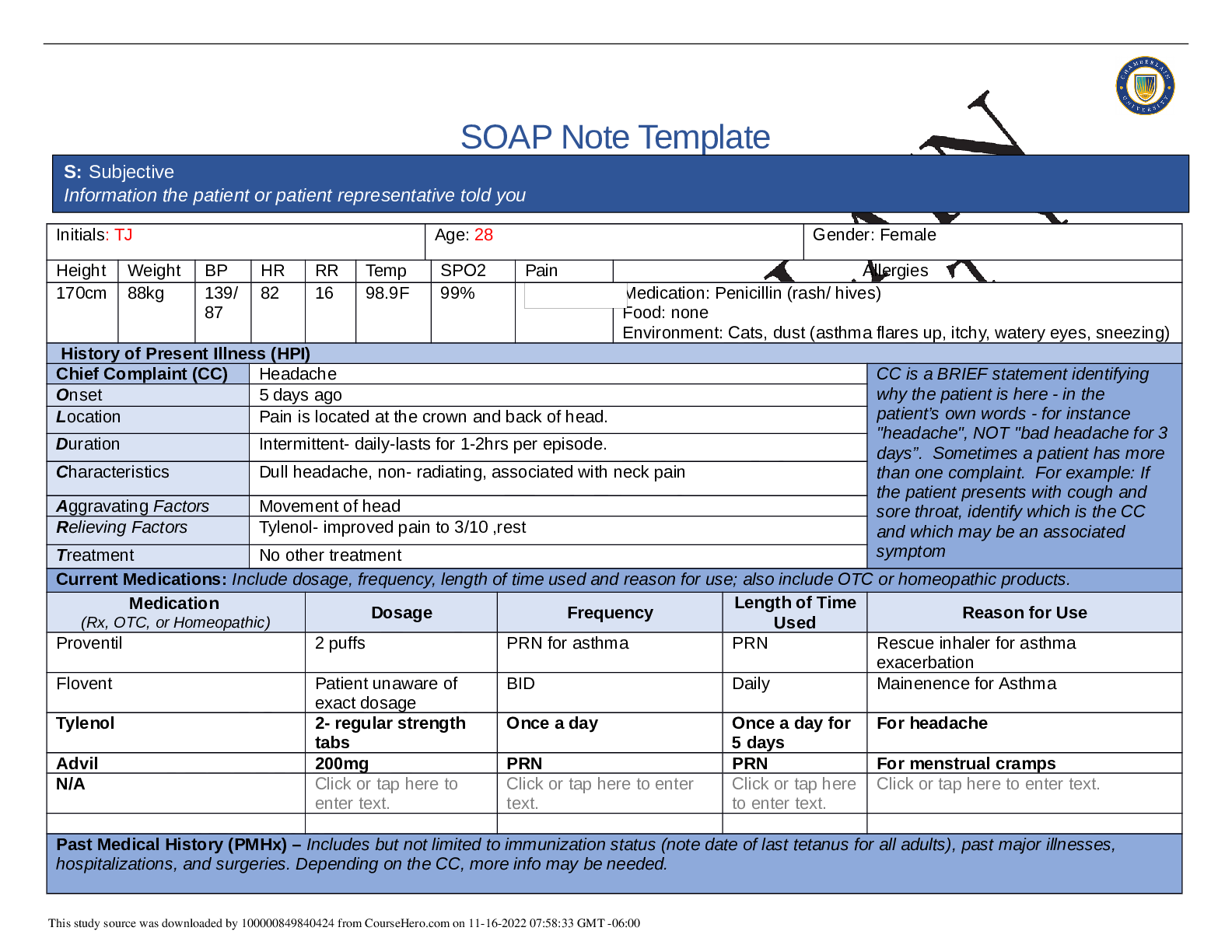
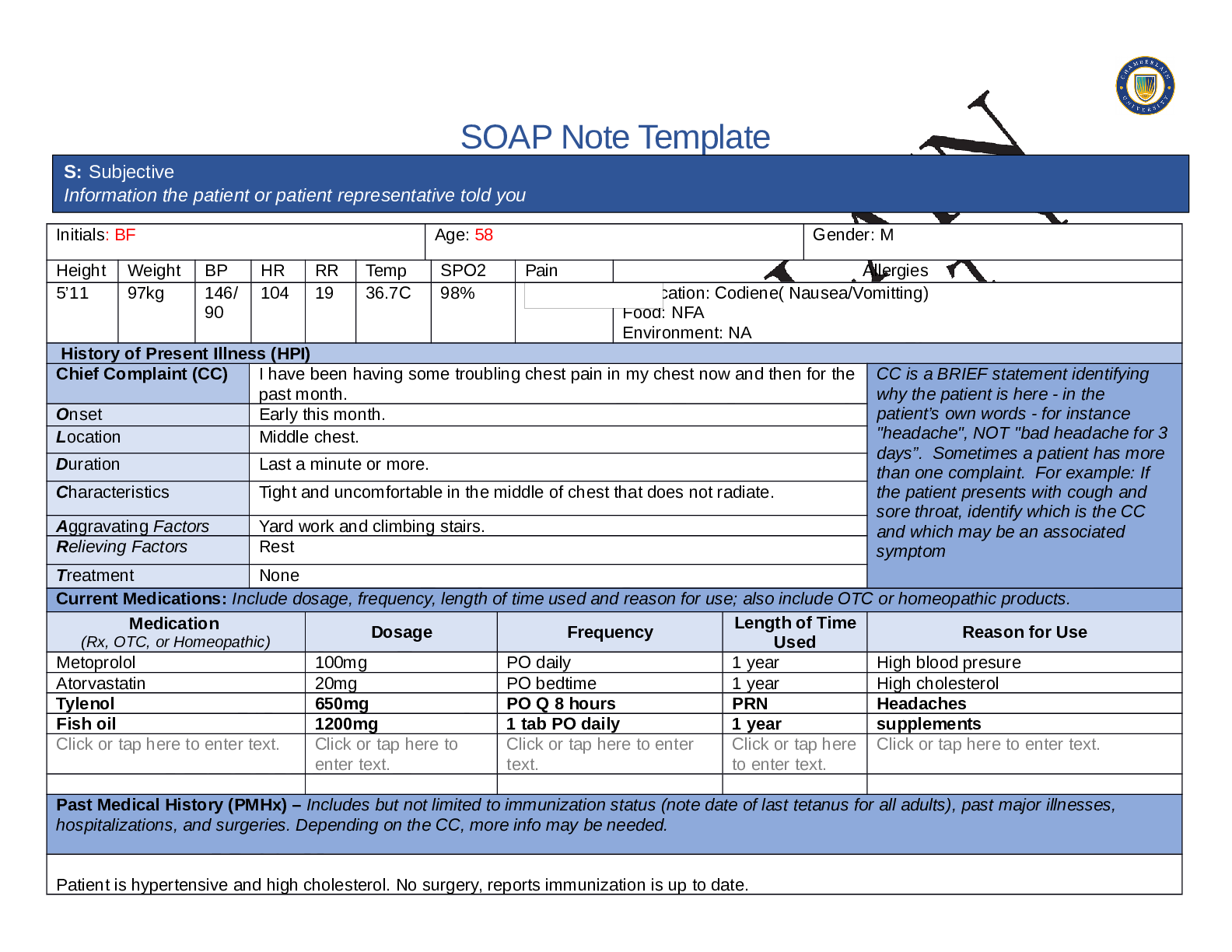
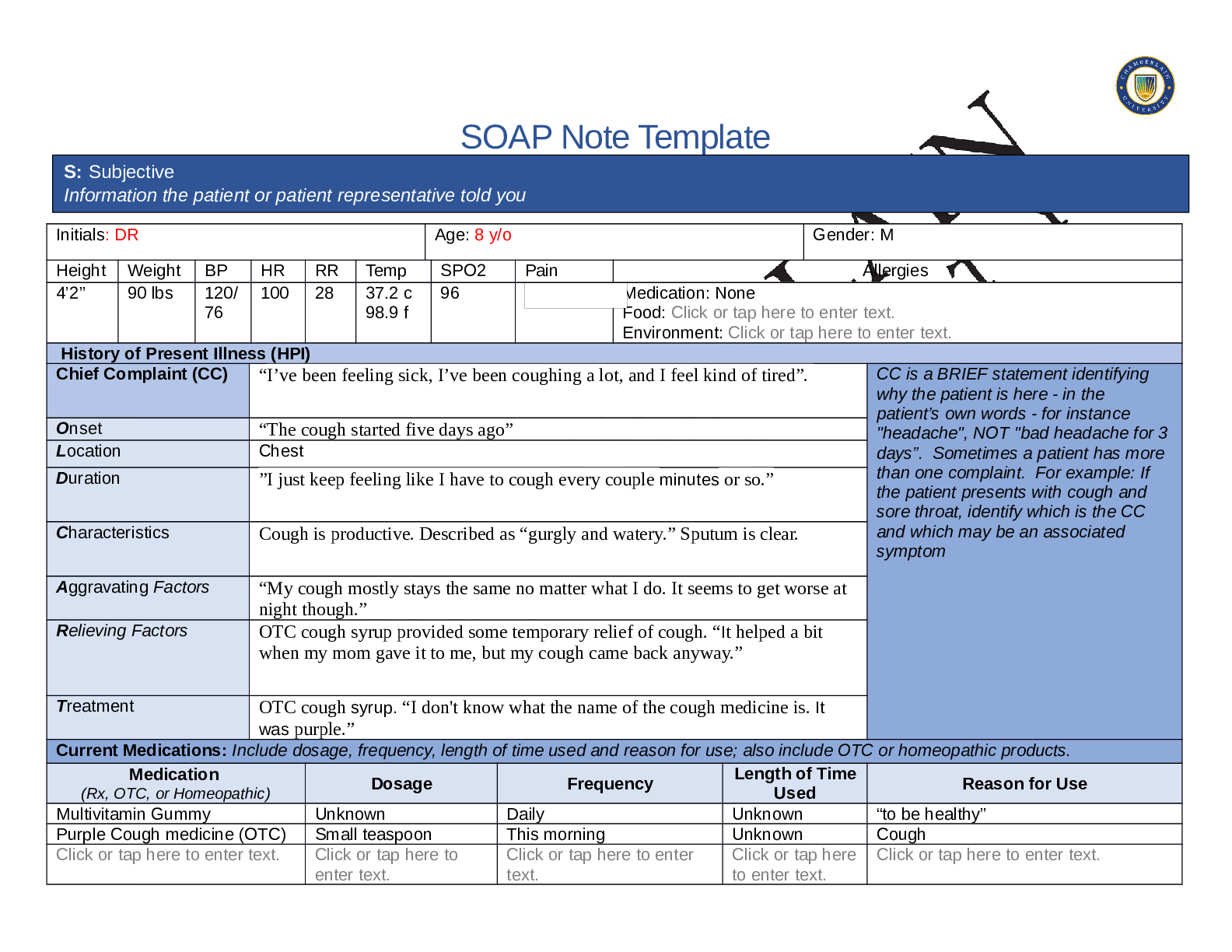
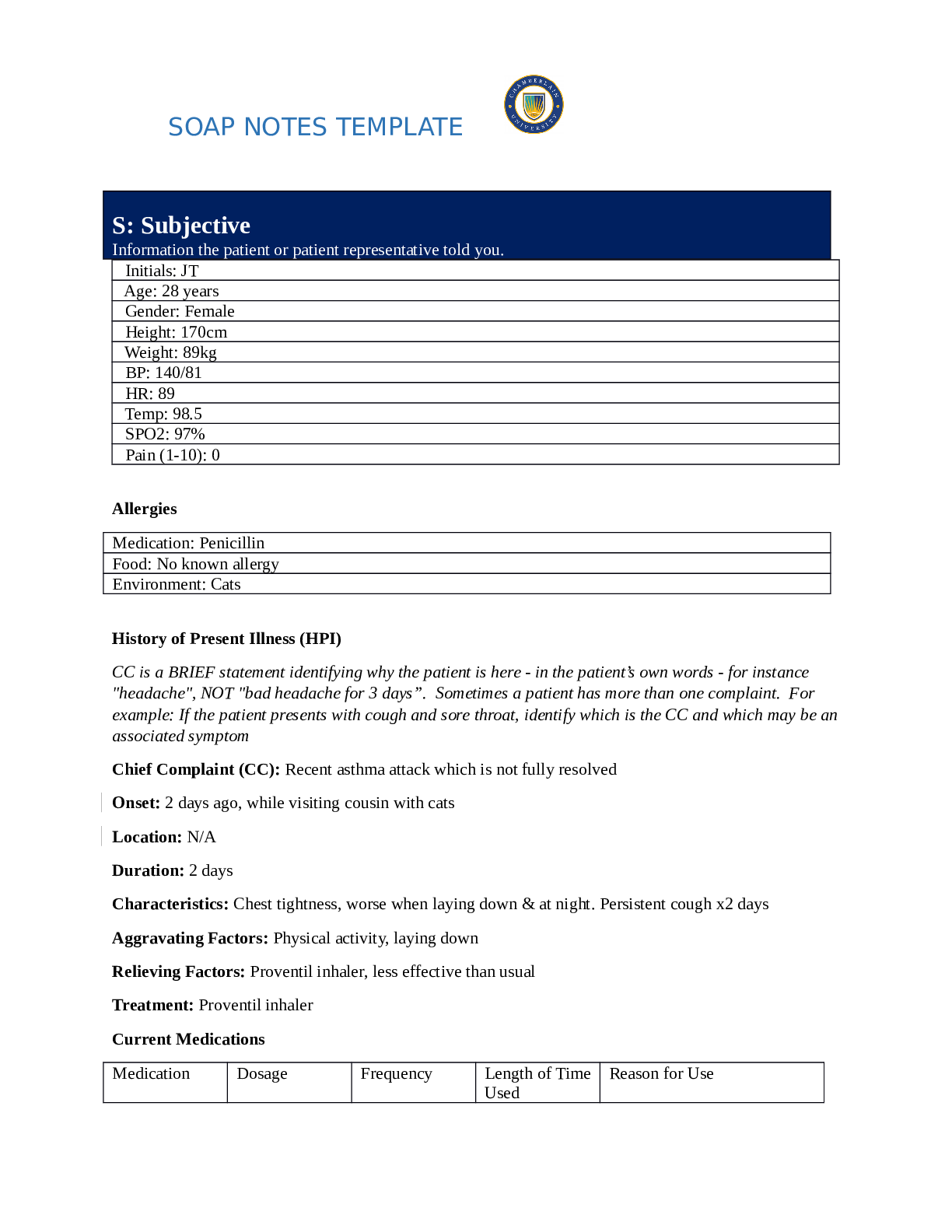
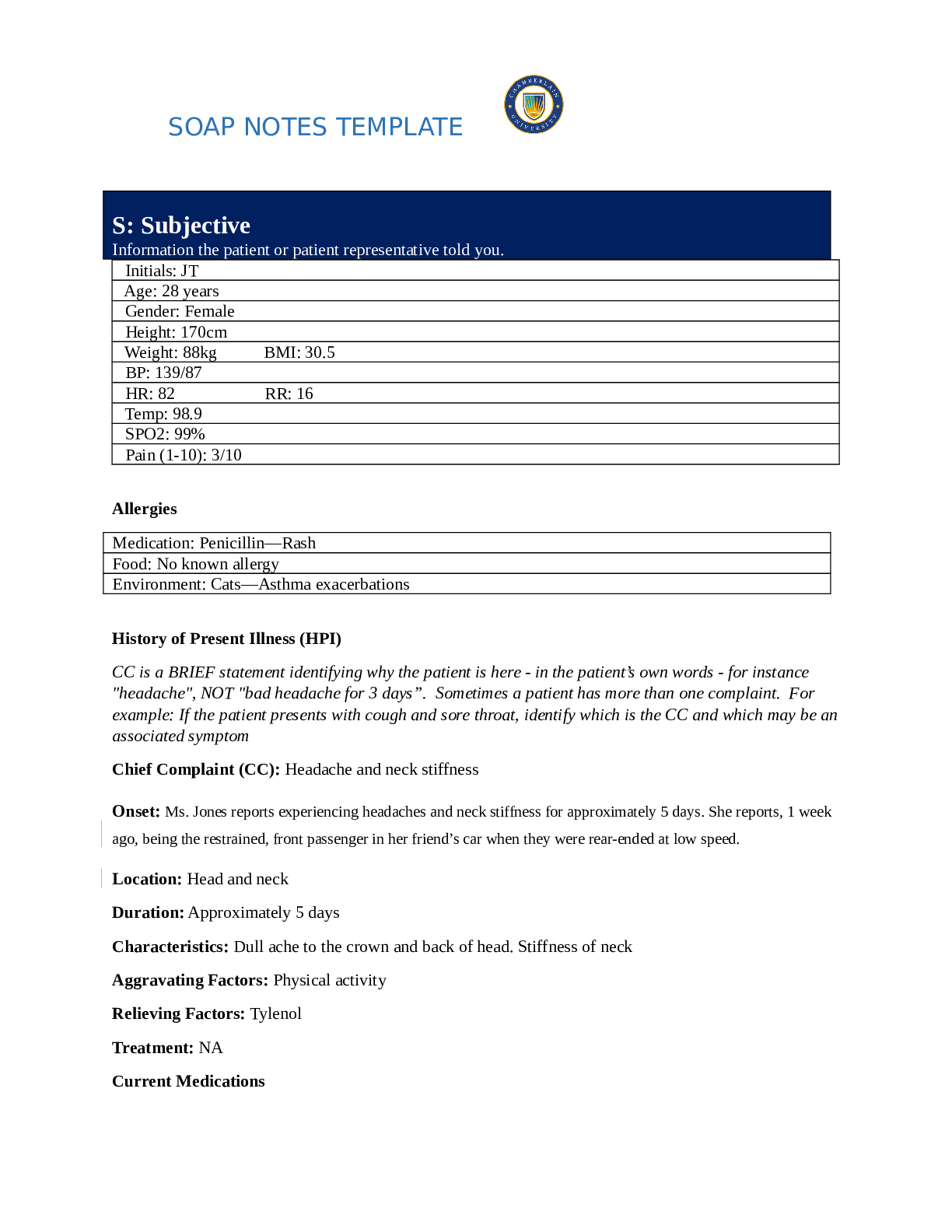
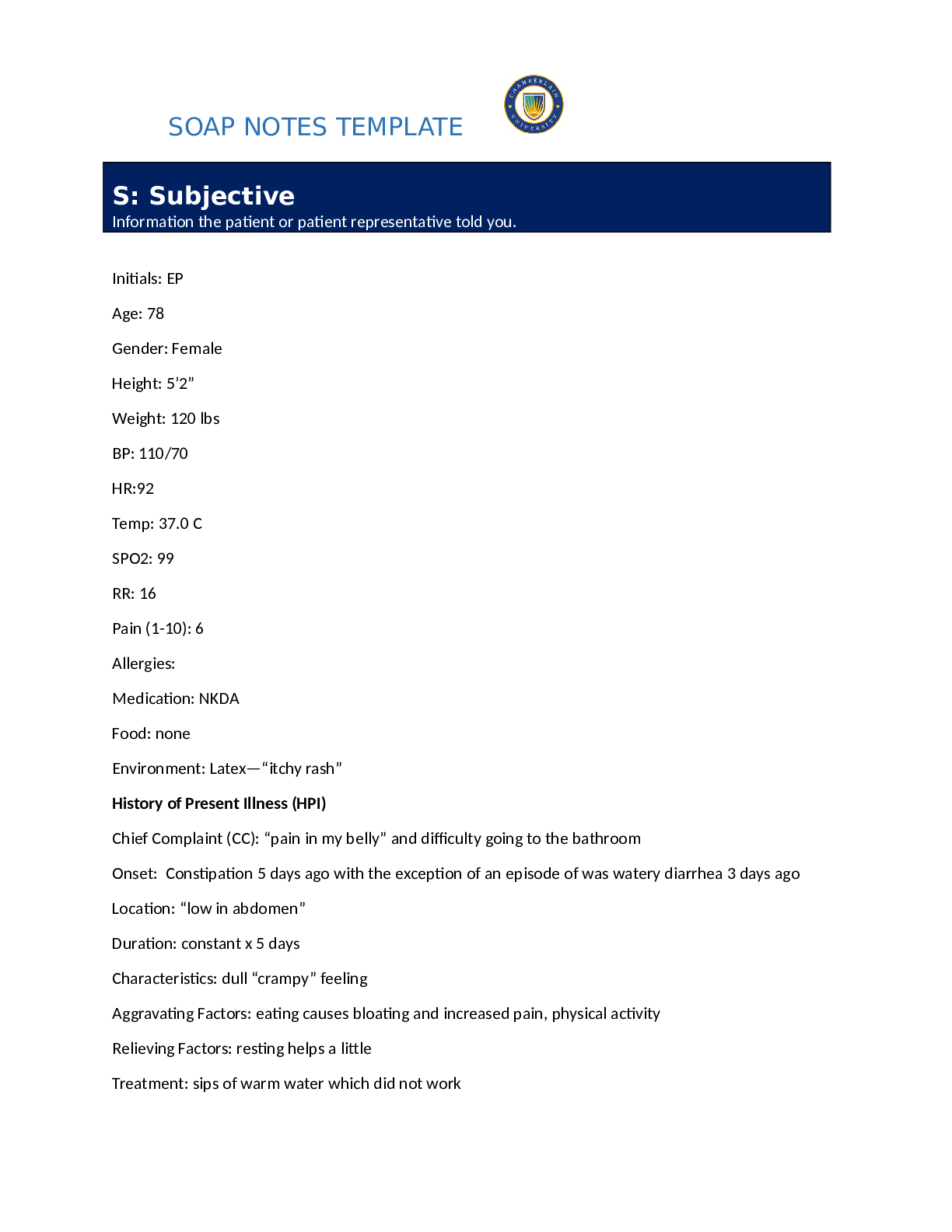
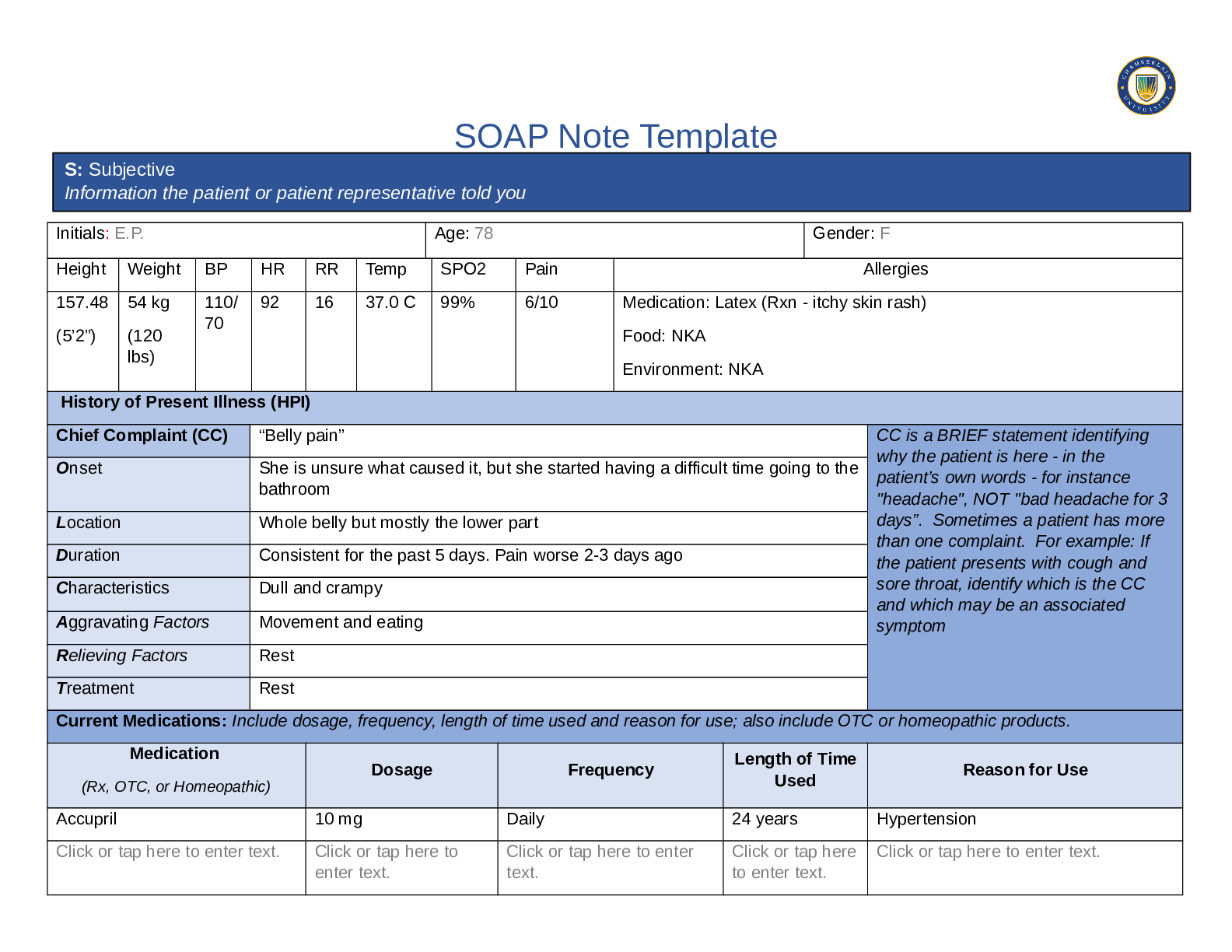
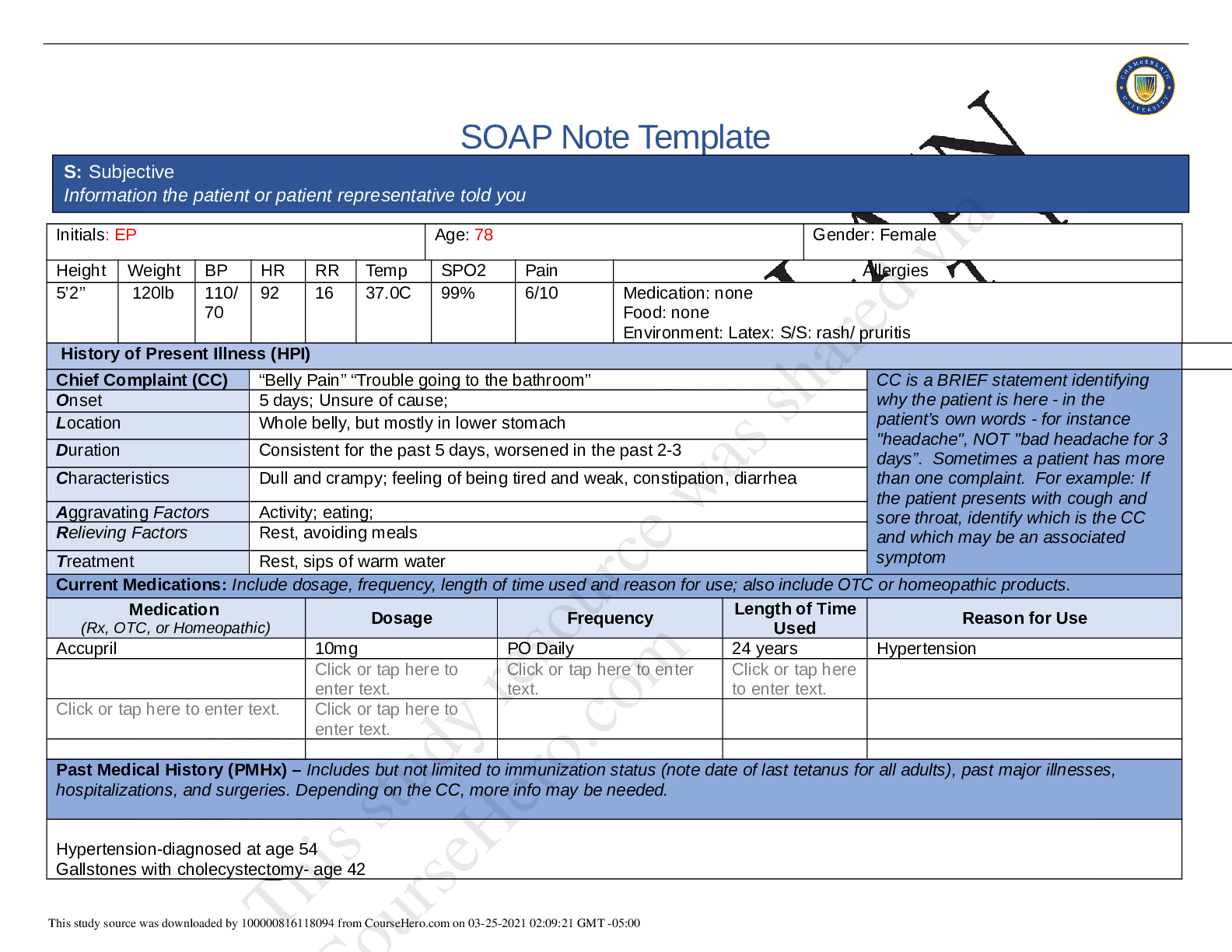
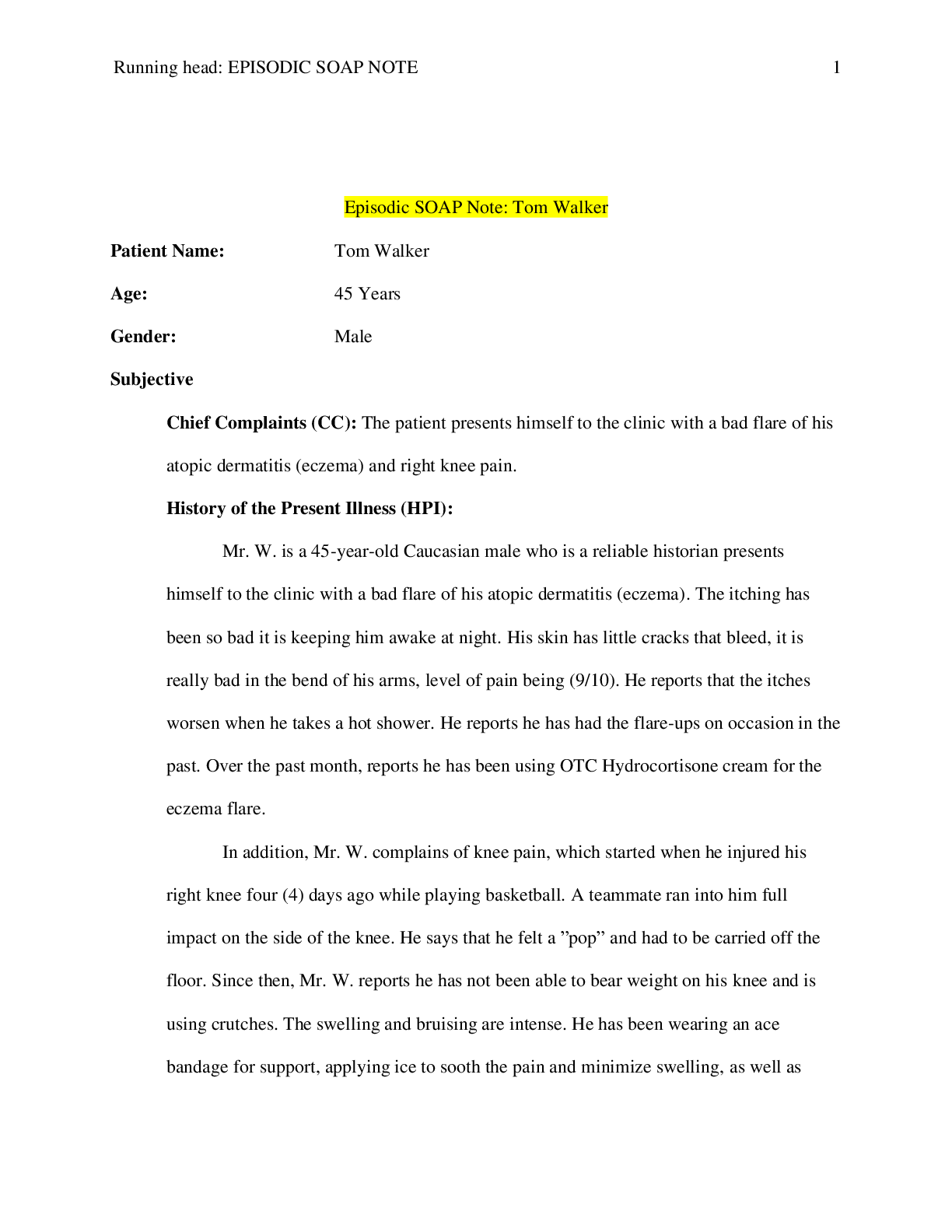
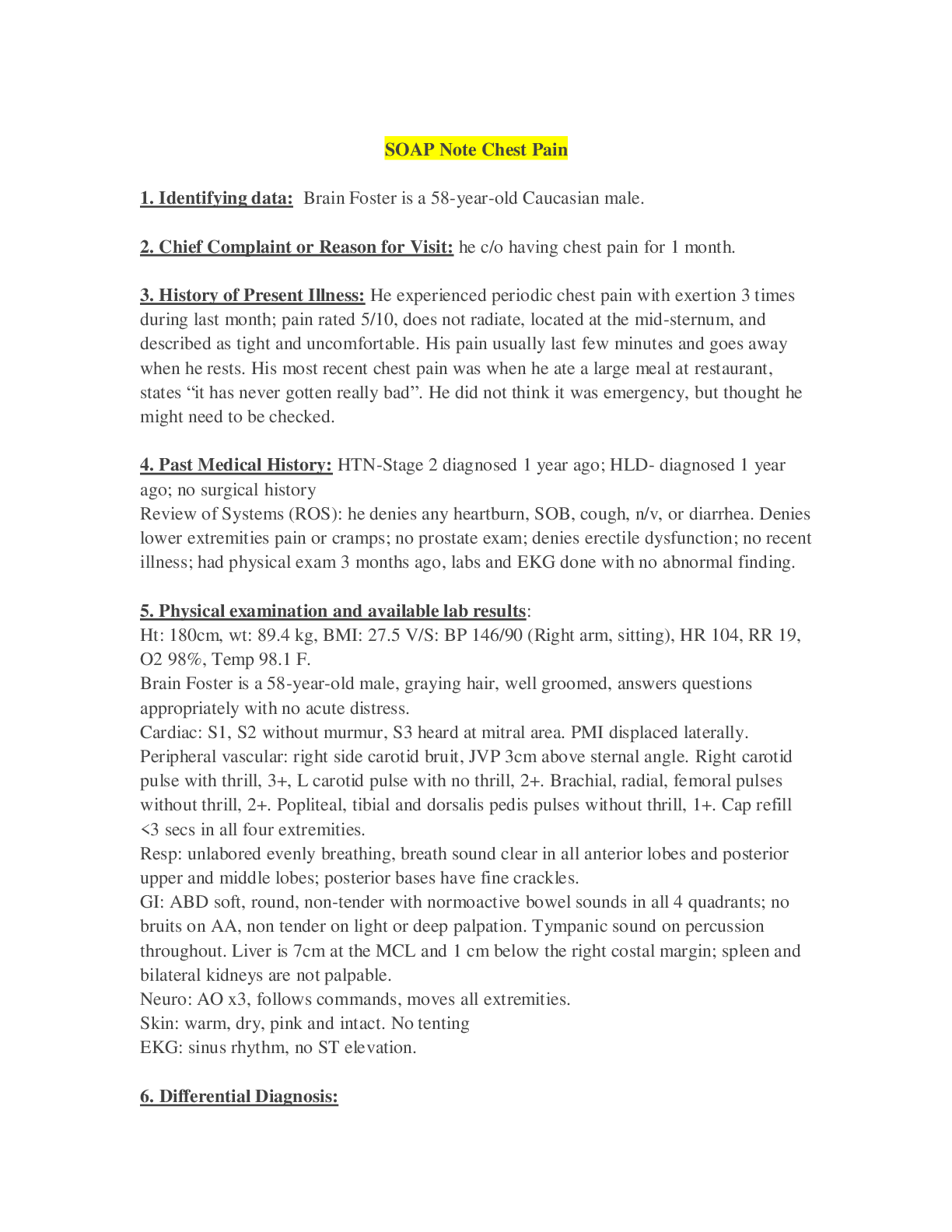
SOAP Note Template Initials: E.P. Age: 78 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 5’ 2 120lbs 110/ 70 92 16 37.0C 99% Medication: NKDA Food: Denies Environment: Latex (... itchy skin rash) dx at age 54 History of Present Illness (HPI) Chief Complaint (CC) “Belly pain” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset 5 days ago Location Lower abdomen Duration Constant. Worse when moving or when eating. ( worse 2-3 days) Characteristics Constant. Dull and crampy. Generalized pain that stays in one place. (Last BM 5 days ago, non- radiating worsedn over 2-3 days) (Add associated char diarrhea, last BM) Aggravating Factors Moving or after eating (put how it helped: little help ) Relieving Factors Resting and not moving ( put the degree of improvement what the pain is at after intervention) Treatment None (sips of water no help, Anything they did even if tx did not work) Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Accupril (research med side effect coud be a DDX) 10mg Daily 24 yrs Hypertension N/A Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. N/A Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. N/A Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. N/A Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. S: Subjective Information the patient or patient representative told you This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:00:22 GMT -05:00 Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Last Bowel movement 5 days ago. No gastrointestinal history. Menopausal. Reports 3 pregnancies but Last colonoscopy: 10yrs ago reports, results were negative. 2 colonoscopy’s total. Surgical history includes: Cholecystectomy at age 42 and one C-section at 40 with her last pregnancy. Denies other hospitalizations. No recent travel outside of USA in last few years. Hx: Stomach virus a few years ago for 24hrs. Last flu vaccine 2 years ago. Refuses flu vaccine at this visit. Unable to recall date of last tetanus but states is currently up to date at this time. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. ( add if pt is happy? , add sexual history with BF, ) Born SF, grew up in Korean towen. Widow married 50 yrs. Jennifer lawyer, tim son director. Retired nurse working at a rehabilitation clinic. Hobbies include gardening, walking a lot. Water aerobics 2-3 times a week. Started Pilates recently for exercise. Lives with daughter Jennifer with good relationship, daughter is driver. Widow but has a significant other. Denies history or present tobacco use. Reports first alcoholic drink on 13th birthday. Drinks one glass of white wine every Sunday filled in a normal glass of wine. Avoids caffeinated drinks but ocassinally has chamomille tea. -Reports only drinking 2 glasses of water daily, reports typical meal is toast or banana or peach for breakfast, skips lunch, and dinner is a protein with rice. Reports vegetable intake every other day. Reports usually has a bowel movement every day or every other day. Reports diarrhea episode prior to being constipated for the last 5 days. ( ask depression, 24hr diet recall, enjoys food in her culture.) Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Father:Deceased at age 82, obesity, hx Heartburn, HTN, hypercholesterolemia Mother:Deceased at 88, hx of HTN and DM 2. Maternal grandparents: CAD, DM2, HTN Paternal grandparents: hx obesity, CVA , HTN Husband:passed away at 82 yrs old from a fall, resulting in brain hemorrhage Brother(Christopher)81yr old – prostate cancer, HTN, hypercholesterolemia. Brother (Michael) 80 -HTN Daughter ( Jennifer)-age 46- healthy Son 48- healthy (Add if history of colon cancer? Denies family colon ca history.) Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:00:22 GMT -05:00 Constitutional Skin HEENT ☒Fatigue less energy for past week. ☐Weakness denies ☐Fever/Chills denies ☐Weight Gain denies ☒Weight Loss reports “ I don’t think so” ☐Trouble Sleeping denies ☐Night Sweats denies ☐Other: Click or tap here to enter text. ☐Itching denies ☐Rashes denies ☐Nail Changes denies ☒Skin Color Changes flushed face (cheeks) ☒Other: Reports Occassional dryness ☐Diplopia denies ☐Eye Pain denies ☐Eye redness denies ☐Vision changes denies ☐Photophobia denies ☐Eye discharge denies ☐Earache denies ☐Tinnitus denies ☐Epistaxis denies ☐Vertigo denies ☐Hearing Changes denies ☐Hoarseness denies ☐Oral Ulcers denies ☐Sore Throat denies ☐Congestion denies ☐Rhinorrhea denies ☐Other: Click or tap here to enter text. Respiratory Neuro Cardiovascular ☐Cough denies ☐Hemoptysis denies ☐Dyspnea denies ☐Wheezing denies ☐Pain on Inspiration denies ☐Sputum Production ☐Other: Click or tap here to enter text. ☐Syncope or Lightheadedness denies ☐Headache denies ☐Numbness denies ☐Tingling denies ☐Sensation Changes ☐Speech Deficits denies ☐Other: Click or tap here to enter text. ☐Chest pain denies ☐SOB denies ☐Exercise Intolerance denies ☐Orthopnea denies ☐Edema denies ☐Murmurs denies ☐Palpitations denies ☐Faintness denies ☐OC Changes denies ☐Claudications denies ☐PND denies ☐Other: Click or tap here to enter text. MSK GI GU PSYCH ☒Pain 6/10 lower abdominal pain ☐Stiffness unable to assess ☐Crepitus unable to assess ☐Swelling denies ☐Limited ROM ☐Redness unable to assess ☐Nausea/Vomiting denies ☐Dysphasia denies ☒Diarrhea Reports diarrhea prior to constipation. ☒Appetite Change 5 days ago due to abdominal pain ☐Urgency denies ☐Dysuria denies ☐Burning denies ☐Hematuria denies ☐Polyuria denies ☐Nocturia denies ☐Stress denies ☒Anxiety anxious about abd pain ☐Depression denies ☐Suicidal/Homicidal Ideation denies This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:00:22 GMT -05:00 ☐Misalignment unable to asses ☐Other: Click or tap here to enter text. ☐Heartburn denies ☐Blood in Stool denies ☒Abdominal Pain 6/10 pain. Started 5 days ago. Constant. Dull & crampy . ☒Excessive Flatus Reports “gassier” ☐Food Intolerance denies ☐Rectal Bleeding denies ☒Other: Constipation (Last bowel movement was 5 days ago), oblong mass palpated in LLQ, fecal mass in rectal vault. ☐Incontinence denies ☒Other: decreased urination. ☐Memory Deficits denies ☐Mood Changes denies ☐Trouble Concentrating denies ☐Other: Click or tap here to enter text. GYN ☐Rash denies ☐Discharge denies ☐Itching denies ☐Irregular Menses denies ☐Dysmenorrhea denies ☐Foul Odor denies ☒Amenorrhea Menopause ☒LMP: 20years ago at age 54 ☐Contraception denies ☐Other:Click or tap here to enter text. O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:00:22 GMT -05:00 Body System Positive Findings Negative Findings General Cheeks are flushed. Appears stable but uncomfortable and grimacing at times. Appears anxious and breaks eye contact by looking away. Alert and oriented, pleasant,answered questions appropriately. Sitting on exam table and able to follow directions to lie down and sit up . Dressed appropriately. Skin Facial flushing. Old abdomen scars noted upon inspection: 6cm scar in RUQ and 10cm scar at midline in suprapubic region. Normal skin turgor, no tenting. Mucous membranes pink and moist. HEENT Click or tap here to enter text. Symmetrical face and head. Nasal and oral mucus membranes pink and moist. Respiratory Click or tap here to enter text. Breath sounds clear and unlabored. Able to speak full sentenced without difficulty. Neuro Click or tap here to enter text. Click or tap here to enter text. Cardiovascular Click or tap here to enter text. S1, S2, no murmurs, gallops, or rubs.; no S3 or S4 sounds.no lower extremity edema. Aortic width: 2cm with no lateral pulsation. Musculoskeletal Click or tap here to enter text. NEED TO ADD ALL THE NORMAL EXAM FINDINGS TOO. Gastrointestinal Abdominal: 6cm scar in RUQ and 10cm scar at midline in suprapubic region. Scattered dullness over LLQ. Palpated (deep) – firm, oblong mass (2x4cm) in LLQ with guarding, distention, and signs of pain. Digital rectal exam: fecal mass in rectal vault. Abdomen: Abdominal exam reveals no dicoloraion, normoactive bowel sounds in all quadrants; no bruits; no friction sounds;tympany in all areas except over LLQ; abd soft in all quadrants, no CVA tenderness, liver span 7cm at the midclavicular line, no hernias. Rectal exam: No hemorrhoids, no fissures, or ulcerations; strong sphincter tone. Genitourinary Urine is dark yellow Kidneys and bladder no palpable. Urine clear, normal odor. Urinalysis:Negative for WBC, Ketones, blood,protein, or nitrates. pH: 6.5 (acidic). Psychiatric This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:00:22 GMT -05:00 Problem List 1. Abdominal pain 6 Decreased fiber intake 11 N/A 2 Constipation 7 Fecal mass i [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 02, 2022
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
May 02, 2022
Downloads
0
Views
73





.png)