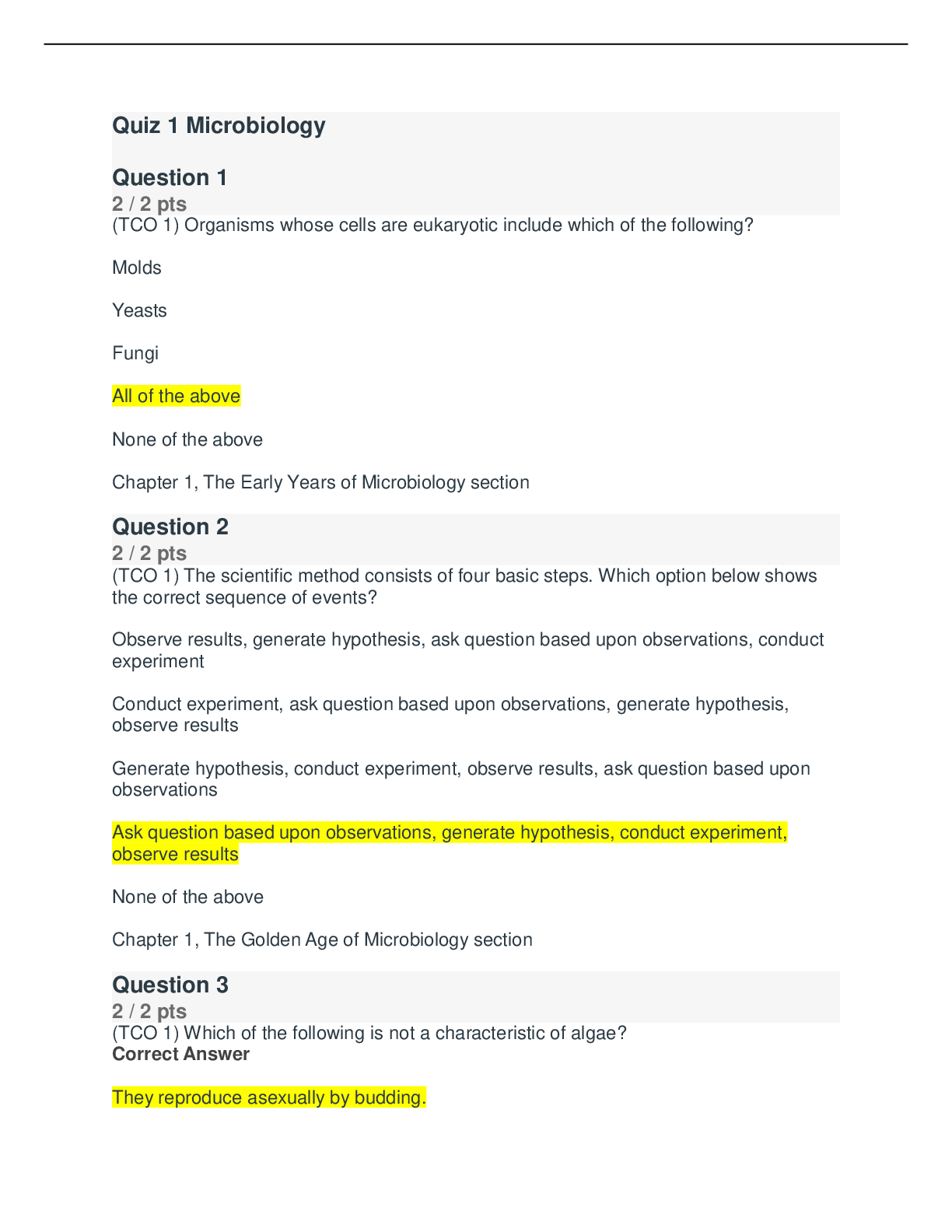
*NURSING > Summary > Chamberlain College of Nursing - NURSING NR603 Week 5 APEA Predictor Assignment Part 1 Already Grade (All)
Chamberlain College of Nursing - NURSING NR603 Week 5 APEA Predictor Assignment Part 1 Already Graded A
Document Content and Description Below
Week 5: APEA Predictor Assignment - Part 1 Chief complaint: 52-year-old African American male presented to the office with chief complaint of voiding difficulty and pain. HPI: “I been having some... dribbling and discomfort pain after peeing for some time now. I have been going to the bathroom more often since I do not feel like I have finish peeing all the way. The reason I am here today is because last night, I noticed a small amount of blood in my semen after having intercourse with my wife. I did not want to come, but this is really scaring me and my wife said this is not normal.” Patient Medical History: Current treatment for diabetes, hyperlipidemia, hypertension, erectile dysfunction Childhood illnesses: Varicella, common cold Patient surgical history: Hernia repair Hospitalizations: None Immunization: Up to date on all vaccinations Allergies: NKDA Current medications: Metformin 500 mg BID daily, Atorvastatin 20mg at bedtime, Amlodipine 10 mg daily and Cialis 10mg PRN. Family History: Children are healthy. Mother has diabetes and cholesterol. Father has HTN, BHP, and hyperlipidemia. Brother: BPH, PGM: Deceased unknown causes and PGF: erectile dysfunction died at 73 from heart attack. Lifestyle: In monogamous married relationship with his wife of 20 years. The patient works at the local High school as a math teacher. Due to the COVID-19 quarantine, he has been working from home, lives a sedentary lifestyle, increase his weight and food intakes. PE: Height 5’11’, Weight 234 pounds Vital signs: BP 151/94, Temp. 97.8, P 86, Oxygen sat 99% on room air. General: African-America male. Alert, oriented, cooperative. Pt appears unease and changing positions in chair every couple of minutes. Skin: Skin warm, moist, intact. Skin color dark brown skin tone without cyanosis or pallor. HEENT: Head norno-cephalic. Hair thin coarse hair with a bald circular spot on back of head. Eyes: Sclera clear, conjunctive: white, PERRLA. EOMs intact with no AV nicking noted. Nose: Nares patent without exudate. Sinuses non-tender to palpation. Nasal septum without deviation. This study source was downloaded by 100000831988016 from CourseHero.com on 04-22-2022 05:41:40 GMT -05:00 https://www.coursehero.com/file/80210702/NR603-Week-5-APEA-Predictor-Assignment-Part-1docx/ Throat: Oropharynx most without lesion or exudate. Teeth in need of repair. Gums swollen and red. Tongue midline, pink, smooth without lesion. Lungs: Lungs clear bilaterally to auscultation without labored breathing. Chest symmetrical without rashes or lesions noted. CV: Heart S1 and S2 noted without murmurs, noted. No parasternal lifts, heaves, and thrills. Peripheral pulses equally bilaterally. PMI 5th ICS displaced 4cm laterally. Trace edema in lower extremities. Abdomen: Abdomen round, soft without bowel sounds noted on all four quadrants. Rationale in the identified body system: Based on the National Institute Diabetic and Digestive and diabetes and digestive and kidney disease (NIDDK), men over 40-year-old with associated risk factor and family history of benign prostatic hyperplasia are prevalence of developing urological conditions. Urology was selected as the body system based on the patient chief compliant of dribbling, discomfort pain after voiding and the presence of blood after intercourse, which are all signs and symptoms of the three-differential diagnosis. The patient also has associated risk factors such as diabetes, hyperlipidemia, hypertension, erectile dysfunction, age, obesity, lack of physical exercise and African American descent (NIDDK, 2021a). Differential Diagnosis: For proper diagnosis and treatment, it is essential to be able to differentiate and identify the origins of each condition using the patient’s physical exam, medical history, and chief complaint. The following are the three differential diagnoses. 1. Benign Prostatic Hyperplasia (BPH) (N40.0) 2. Acute Prostatitis (N41.0) 3. Malignant neoplasm of prostate (C61) The prostate is a walnut-shaped gland that produces prostate fluid to aid in the transfer of semen. Prostate fluid is an essential component in a man’s fertility. The urethra is the mode that transfer semen and urine out of the body through the penis (NIDDK, 2018). Benign prostatic hyperplasia, acute prostatitis and malignant neoplasm are all abnormal conditions of the prostate that originate from different origins. Many of the sign and symptoms along with risk factors of these conditions may overlap making it difficult to diagnose. Understanding the pathophysiology and knowing the risk factors, demographics, occurrences, and clinical presentation of each condition can assist in narrowing the diagnose for proper treatment. Pathophysiology: Benign prostatic hyperplasia (BPH) is characterized by increase proliferation of epithelial cell and smooth muscle with the prostatic resulting in hyperplasia and an enlargement of prostate (Lokeshwar, S. D., el. at, 2019). As the prostate gland enlarges it presses against the urethra decreasing urine and prostate fluid flow. The pressure thickens and weakens the bladder wall decreasing ability to completely empty out the bladder resulting in urine residue (NIDDK, This study source was downloaded by 100000831988016 from CourseHero.com on 04-22-2022 05:41:40 GMT -05:00 https://www.coursehero.com/file/80210702/NR603-Week-5-APEA-Predictor-Assignment-Part-1docx/ 2021b). BPH is a progressive condition. Unlike BPH, acute prostatitis (AP) is an inflammation of the prostate and possible surrounding areas is usually caused by bacteria. AP usually appears suddenly and last for a short period of time (NIDDK, 2021a). Malignant neoplasm of prostate / prostate cancer (PC) is a progressive condition like BPH. MNOP are prostate glands cells that mutate into cancer cells known as adenocarcinoma. These cancer cells form small clumps and can spread to other surrounding area such as the bladder, rectum or seminal vesicles and even enter the blood stream and lymphatic system (Salih, F.A.M, Mustafa, M., el. at, 2016). Risk factors: BPH associated risk factor included non-modifiable and modifiable risk factors. Non-modifiable risk factors include male age, genetics, and race. Modifiable risk factors include metabolic syndrome, obesity, diabetes, diet, physical activity, and inflammation. BPH associated risk factor consent more of modifiable risk factors, which are based on individual lifestyle choice such as physical inactivity and diet leading to obesity or metabolic syndrome, and proper management of diabetes (Lim, K.B, 2017). Unlike AP, risk factors are mostly associated with mode of transportation or malformation, such foreign antigens entering the prostate or obstruction/decreased of fluid exiting the body such as urine via the penis though the urethra. The following are associated risk factors of AP, such as phimosis, unprotected vaginal/anal intercourse, intraprostatic ductal reflux, indwelling catheter, urinary tract infection, sexual abuse, transurethral biopsy/surgery, and congenital abnormality of the ureter (Davis, N.G., & Silberman M., 2020). PC has non-modifiable and modifiable risk factors like BPH such as age, family history, ethnicity, obesity, gender (male), persistently elevated testosterone levels, hypertension, and agent orange exposure (Leslie, W. S., et, al., 2020). Demographics and Occurrences: The prevalence of men affected by BPH increases with age. Up to 50% of men over 50-year-old and up 80% of men over 80 years old experience BPH symptoms. Studies have demonstrated that black men are at greater prevalence of BPH than those of white descent. Male relative and/or brother with BPH have great incident of having BPH (Lokeshwar, S. D., el. at, 2019). Prostatitis true incidence is unknow, however there is a peak incidence in men between the ages of 20 to 40 and men older than 70-year-old. The most common cause of prostatitis is Escherichia coli ascending into the urethra and infecting the prostate (Coker, T.J., Dierfeldt D.M., 2016). PC is the second most common malignant cancer and the sixth leading cause of death in men resulting in 256,000 death worldwide. After the age of 50 the risk of cancer increases rapidly, six in every ten cases of PC are men over the age of 65. Incidence of PC are rare before the age of 40. African American descent and men from Caribbean island North America, Australia, northwestern Europe are along the most common to develop PC. Family history of PC doubles and those with brothers are at risk greater risk than those with father of PC. The greater the number of relatives with PC, the higher the risk of BPH especially the younger the relative (Salih, F.A.M, Mustafa, M., el. at, 2016 / ACS, 2021). The patient has a brother with a history of BHP and his is not within the peak incidence for prostatitis nor does he have a history of PC. Presentation: Clinical presentation of BHP mimic symptoms of lower urinary tract infection such as nocturia, frequency, dysuria, weak or interrupted stream, difficulty initiating micturition, urgency and difficulty emptying after micturition. Prostatitis typically present abruptly and with fever unlike This study source was downloaded by 100000831988016 from CourseHero.com on 04-22-2022 05:41:40 GMT -05:00 https://www.coursehero.com/file/80210702/NR603-Week-5-APEA-Predictor-Assignment-Part-1docx/ BHP. Other symptoms may include malaise, dysuria pelvic pain, myalgias, suprapubic tenderness and fullness, chills, pain (genital, groin, lower abdomen, or lower back area), nausea, vomiting, and body aches. Both BHP and prostatitis have overlapping symptoms such as urinary frequency and hesitancy, weak or interrupted stream, and pain after urination (Davis, N.G., & Silberman M., 2020 /NIDDK, 2021b /Lokeshwar, S. D., el. at, 2019). As per PC initially there are not early symptoms and men who are diagnosed with PC are symptomatic men who may present with lower urinary tract symptoms, visible hematuria and/or erectile dysfunction. Late symptoms may include paralysis from the spinal metastases, fatigue due to anemia, renal failure, and bone pain (Leslie, W. S., et, al., 2020/ Merriel, S.W.D., Funston, G., el. at, 2018). Diagnostic Testing: Diagnosing of BHP include patient and family history, laboratory studies (PSA levels), physical exam including a DRE, urinalysis, cystoscopy, and diagnostic imaging such as an ultrasound or MRI of the prostate (Lokeshwar, S. D., el. at, 2019/NIDDK, 2021). Diagnosing of prostatitis included patient and family history, urinalysis, and urine culture (Davis, N.G., & Silberman M., 2020). Diagnostic testing for PC is not routinely tested unless there is sufficient warrant to test for PC. Testing may include DRE, PDS levels biopsy, GleasonSore and staging (Salih, F.A.M, Mustafa, M., el. at, 2016). Several overlapping and similar symptoms make it difficult to differentiate one condition from the other. The pathophysiology pathway of the three differential diagnoses can all cause dripping and discomfort pain due to obstruction or inflammation blocking or decreasing urethra diameter. BPH and PC can cause a narrowing of the urethra causing dripping and discomfort pain due to obstruction, which is the patient chief complaint. AP can cause narrowing of the urethral decreasing urine flow, dripping and pain, however the patient does not complian of decreasing urine, but increase in frequency (NIDDK, 2021b/ (Lokeshwar, S. D., el. at, 2019/Salih, F.A.M, Mustafa, M., el. at, 2016).BHP and CA have similar associated risk factors such as obesity, family history, male gender, and African American descent, which make it a greater probability than AP. AP is mostly caused by bacteria infection and typically presented abruptly with fever along with other symptoms such as nausea, fatigue, chills, suprapubic tenderness, or fullness. (Davis, N.G., & Silberman M., 2020 /NIDDK, 2021b /Lokeshwar, S. D., el. at, 2019/Leslie, W. S., et, al., 2020/ Merriel, S.W.D., Funston, G., el. at, 2018). Diagnostic testing can also help distinguishe between the three differential diagnoses and can be achieved based on the patient conditions. BPH can be distinguished by voiding obstruction symptoms, a negative urine culture, nontenders and enlargement of the prostate, while bacterial prostatitis can be distinguished by a positive urine culture. PC can be distinguished by DRE for the presence of nodules on the prostate. The patient does not have fever and a negative urine culture can rule out bacterial prostatitis. A DRE without the presence nodules can assist in ruling out PC. After a proper diagnose is made and treatment plan can be created based on the results (Coker TJ, Dierfeldt DM., 2026). What do you suspect is the correct diagnosis, what is your justification, and what plan would you propose? This study source was downloaded by 100000831988016 from CourseHero.com on 04-22-2022 05:41:40 GMT -05:00 https://www.coursehero.com/file/80210702/NR603-Week-5-APEA-Predictor-Assignment-Part-1docx/ References American Cancer Society. (2021). Prostate Cancer Risk Factors. Retrieved from https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/risk-factors.html Coker TJ, Dierfeldt DM. (2026). Acute bacterial prostatitis: Diagnosis and management. American Family Physician. Retrieved from https://www.aafp.org/afp/2016/0115/p114.html Davis, N.G., & Silberman M. (2020). Bacterial Acute Prostatitis. StatPearls Treasure Island. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK459257/ Leslie, S.W., Soon-Sutton, T.L., Sajjad H, etal. (2020). Prostate Cancer. StatPearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK470550/ Lim K. B. (2017). Epidemiology of clinical benign prostatic hyperplasia. Asian journal of urology, 4(3), 148–151. https://doi.org/10.1016/j.ajur.2017.06.004 Lokeshwar, S. D., Harper, B. T., Webb, E., Jordan, A., Dykes, T. A., Neal, D. E., Jr, Terris, M. K., & Klaassen, Z. (2019). Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Translational andrology and urology, 8(5), 529–539. https://doi.org/10.21037/tau.2019.10.01 Merriel, S.W.D, Funston. G. & Hamilton, W. (2018). Prostate cancer in Primary care. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6133140/ National Institute of Diabetic and Digestive and Kidney Diseases (NIDDK). (2021a). Prostatitis: Inflammation of the prostate. Retrieved from https://www.niddk.nih.gov/healthinformation/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate National Institute of Diabetic and Digestive [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 22, 2022
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Apr 22, 2022
Downloads
0
Views
71


.png)