*NURSING > Presentation > NR 566 Week 6 Grand Rounds Presentation Part 1 – MENOPAUSE {GRADED A+} (All)
NR 566 Week 6 Grand Rounds Presentation Part 1 – MENOPAUSE {GRADED A+}
Document Content and Description Below
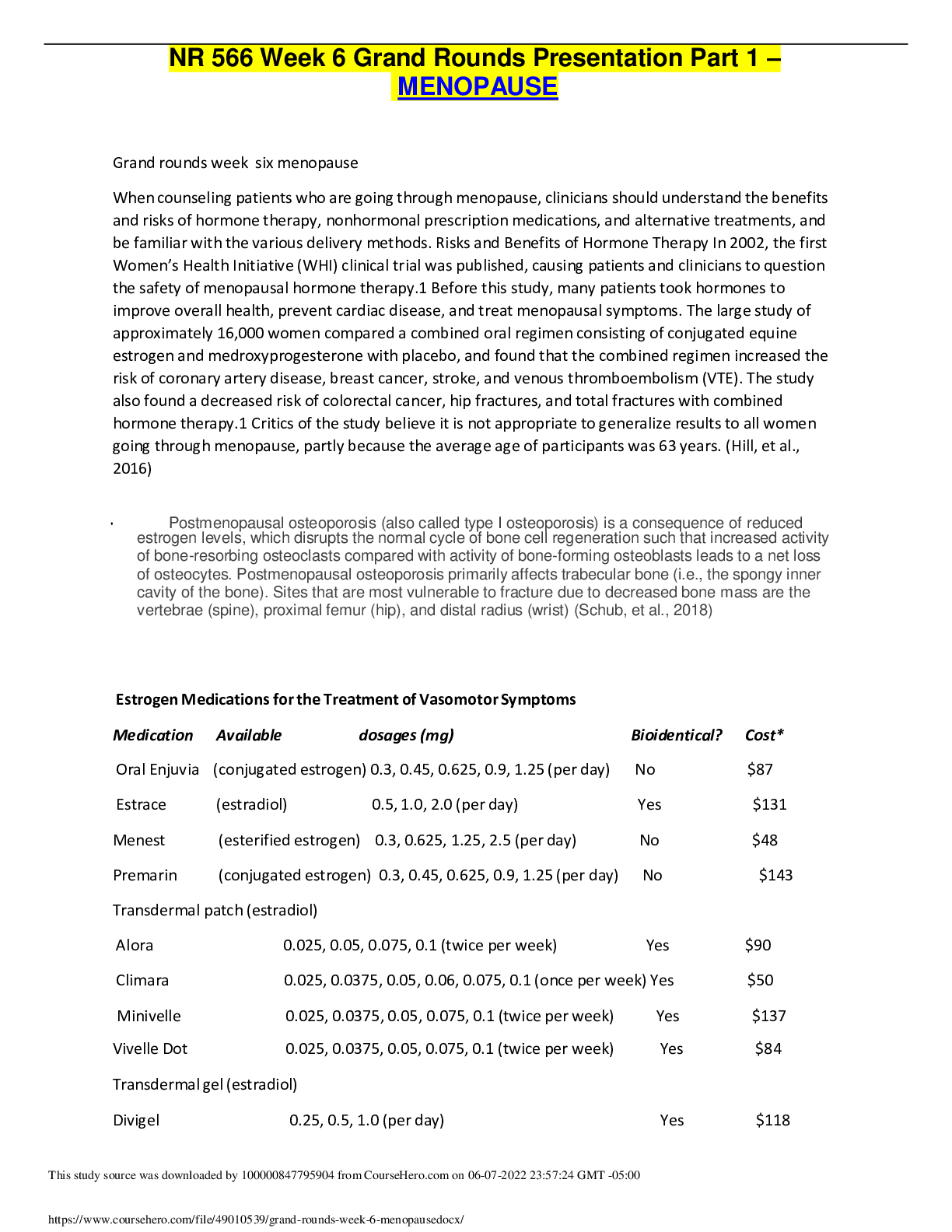
NR 566 Week 6 Grand Rounds Presentation Part 1 – MENOPAUSE Grand rounds week six menopause When counseling patients who are going through menopause, clinicians should understand the benefits and... risks of hormone therapy, nonhormonal prescription medications, and alternative treatments, and be familiar with the various delivery methods. Risks and Benefits of Hormone Therapy In 2002, the first Women’s Health Initiative (WHI) clinical trial was published, causing patients and clinicians to question the safety of menopausal hormone therapy.1 Before this study, many patients took hormones to improve overall health, prevent cardiac disease, and treat menopausal symptoms. The large study of approximately 16,000 women compared a combined oral regimen consisting of conjugated equine estrogen and medroxyprogesterone with placebo, and found that the combined regimen increased the risk of coronary artery disease, breast cancer, stroke, and venous thromboembolism (VTE). The study also found a decreased risk of colorectal cancer, hip fractures, and total fractures with combined hormone therapy.1 Critics of the study believe it is not appropriate to generalize results to all women going through menopause, partly because the average age of participants was 63 years. (Hill, et al., 2016) • Postmenopausal osteoporosis (also called type I osteoporosis) is a consequence of reduced estrogen levels, which disrupts the normal cycle of bone cell regeneration such that increased activity of bone-resorbing osteoclasts compared with activity of bone-forming osteoblasts leads to a net loss of osteocytes. Postmenopausal osteoporosis primarily affects trabecular bone (i.e., the spongy inner cavity of the bone). Sites that are most vulnerable to fracture due to decreased bone mass are the vertebrae (spine), proximal femur (hip), and distal radius (wrist) (Schub, et al., 2018) Estrogen Medications for the Treatment of Vasomotor Symptoms Medication Available dosages (mg) Bioidentical? Cost* Oral Enjuvia (conjugated estrogen) 0.3, 0.45, 0.625, 0.9, 1.25 (per day) No $87 Estrace (estradiol) 0.5, 1.0, 2.0 (per day) Yes $131 Menest (esterified estrogen) 0.3, 0.625, 1.25, 2.5 (per day) No $48 Premarin (conjugated estrogen) 0.3, 0.45, 0.625, 0.9, 1.25 (per day) No $143 Transdermal patch (estradiol) Alora 0.025, 0.05, 0.075, 0.1 (twice per week) Yes $90 Climara 0.025, 0.0375, 0.05, 0.06, 0.075, 0.1 (once per week) Yes $50 Minivelle 0.025, 0.0375, 0.05, 0.075, 0.1 (twice per week) Yes $137 Vivelle Dot 0.025, 0.0375, 0.05, 0.075, 0.1 (twice per week) Yes $84 Transdermal gel (estradiol) Divigel 0.25, 0.5, 1.0 (per day) Yes $118 Elestrin 0.52 (per day; adjust dosage based on response) Yes $109 Estrogel 0.75 (per day) Yes $126 Transdermal spray (estradiol) Evamist 1.53 per spray (start with 1 spray per day, adjust up to 3 sprays per day based on response) Yes $118 Vaginal (estradiol) Femring 0.05, 0.10 (for 90 days) Yes $355 (Hill, et al., 2016) Hormone replacement therapy may increase the risk of heart attack, stroke, breast cancer, and blood clots in the lungs and legs. Tell your doctor if you smoke and if you have or have ever had breast lumps or cancer; a heart attack; a stroke; blood clots; high blood pressure; high blood levels of cholesterol or fats; or diabetes. If you are having surgery or will be on bedrest, talk to your doctor about stopping estrogen and progestin at least 4 to 6 weeks before the surgery or bedrest.(HRT,2019) Hormone therapy has been the primary treatment for menopausal symptoms. However, because of the health risks associated with hormone therapy, many women cannot or choose not to use hormone therapy.9–11 Approximately 51% of women use CAM and more than 60% perceive it be effective for menopausal symptoms.9 However, the majority of women using CAM do not discuss it with their health care providers.9 Women often report feeling confused about their options and rely on the internet as their primary source of information.11,12 It is imperative that physicians engage in shared decision making with women regarding treatment options, including CAM, for menopausal symptoms. This type of patient-centered integrated approach can potentially reduce the risk for under treatment and adverse events.(Johnson et al., 2019) Hypnosis, a mind-body therapy that involves a deeply relaxed state of focused attention, individualized mental imagery, and suggestion,17 has been investigated for menopausal symptom management. Two randomized clinical trials of 5 sessions of hypnotherapy for hot flashes among breast cancer survivors demonstrated a clinically meaningful (≥69%) reduction in hot flash severity and frequency. 18,19 These results are comparable to pharmacological intervention.(Johnson et al., 2019) Hypnosis has been recommended by the North American Menopause Society, and others, for the treatment of menopausal symptoms and poses little risk.(Johnson et al., 2019) Cognitive Behavioral Therapy In CBT, the therapist and the client work together to identify unhelpful patterns of thinking and behaviour. For example, someone might only notice the negative things that happen to them and not notice the positive things This is sometimes called a “vicious circle” of thoughts, feelings and behaviours. CBT is an action-oriented psychological intervention that has been used to treat hot flashes, depression, and other menopausal symptoms. CBT is a time-limited treatment that focuses on changing cognitive appraisals and behavior choices to alter symptoms. CBT may include education, motivational interviewing, relaxation, paced breathing, and other strategies to improve symptoms.26 Mann et al26 compared the effects of a 6-week CBT intervention to usual care (eg, standard follow-up care) among 96 female breast cancer survivors and found hot flash interference was reduced on average 52%. Women receiving usual care reported a 25% decrease in hot flash interference. Hot flash frequency was reduced by 38% in both groups, 38% indicating CBT was no better than usual care for reducing the frequency of hot flashes.26 In a second RCT, 65% of women receiving a 4-week CBT intervention and 21% of a no-treatment control group, reported clinically significant improvements (eg, 2-point change on a 10-point numerical rating scale) in hot flush interference.27 CBT did not demonstrate a clinically significant reduction (eg, 50%) in hot flash frequency.27 Both of these trials used objective and subjective measures for hot flash frequency.26,27 In a pilot study of 39 women randomized to CBT or waitlist control, there was a statistically significant reduction in hot flash distress, but not in interference or frequency of hot flashes/night sweats, in the immediate treatment group.28 The authors reported a 48% positive treatment effect for the 17 women who completed the CBT program, but it is unclear how that effect was calculated.28 In addition, there is some evidence to suggest that CBT may reduce mild depression in menopause comparable to placebo.27,29 To date, no RCTs of CBT have demonstrated clinically significant improvements in hot flash frequency, but may be beneficial in reducing hot flash distress and interference and other psychological symptoms (eg, depression) associated with menopause. CBT has been recommended by the North American Menopausal Society for reducing the bothersomeness of vasomotor symptoms, but not for frequency.24 Mindfulness-Based Stress Reduction Yoga Aromatherapy Wild Yam Black Cohosh (Cimicifuga racemosa) Dong Quai Maca Menopause is a process in the climacteric period, characterized by a reduction in ovarian activity, a fall in the fertility rate, and a range of symptoms including irregular menstruation intervals. Most women enter menopause in their 40s, but this can vary from one individual to another. Although there are many factors affecting the age of menopause onset, there is no general agreement on them. Studies have shown many factors to affect the age of menopause, such as the mother’s age at menopause, the age at menarche, gestational age, use of oral contraceptives, irregular menstrual cycle, number of pregnancies, body mass index, use of tobacco and alcohol, physical activity, unilateral oophorectomy, serum lead levels, consumption of polyunsaturated fat, socioeconomic status and educational level. During this period, hormonal and biochemical changes give rise to various symptoms in the woman’s body. In menopause period, physical, psychological, social and sexual changes have a negative effect on quality of life in women. Recently, different measures have been used to assess women’s quality of life in this period of change. The purpose of this review was to examine the factors affecting the onset age of menopause and the measures of quality of life related to menopause. Excess thyroid hormone affects many different organ systems (table 2). Commonly reported symptoms are palpitations, fatigue, tremor, anxiety, disturbed sleep, weight loss, heat intolerance, sweating, and polydipsia. Frequent physical findings are tachycardia, tremor of the extremities, and weight loss.2 CFS, also known as myalgic encephalomyelitis (ME), is an LTC with significant and unpredictable symptoms and uncertain duration.6 Often referred to as ME/CFS in leading literature, new descriptors are under discussion.16 However, the NICE guidelines descriptor of CFS/ME will be the term applied in this article. As CFS/ME is heterogeneous in nature and without medical or diagnostic markers, those with the illness are frequently disbelieved, despite the dramatic changes to functional abilities and emotional well-being.17 GPs are likely to have up to 40 patients experiencing symptoms, and upward of 50% will need input from specialist services. Chronic fatigue syndrome • Menopause refers specifically to the last menstrual period but is rarely used as a diagnosis in itself because it is impossible to know at the time if a menstrual period is the last one; therefore ‘postmenopause’ tends to be used more than ‘menopause’. age and amenorrhea are sufficient clinical indicators for the routine diagnosis of menopause • biochemical measurements, hormonal tests and ultrasound tests were not found useful in routine practice of diagnosis of menopause and perimenopause. • One of the goals of health for all is to improve the quality of life.[9] “Quality of life” is people's perception of their position in the social and cultural life, with regard to their goals and standards.[10,11] Various studies have reported the negative effect of menopause on the quality of life.[12,13,14] Although hormone therapy is the standard treatment for the early symptoms of menopause, due to its side effects such as the risk for embolism and breast cancer,[4] using these combinations routinely is not considered appropriate. Using nonmedicinal methods for preventing the symptoms of menopause and improving the quality of life has been emphasized. Some studies have evaluated the effect of different educational and counseling methods,[10,15,16] participating in physical activities,[4,11,17,18] using medical plants containing phytoestrogens and isoflavones and using food supplements such as soy,[19] licorice,[6] red clover,[20] and fish oil[21] to improve and enhance the quality of life in menopausal women; but no review has been conducted on these studies in Iran so far. Hence, the present study was conducted to systematically review the conducted studies for introducing strategies to improve the quality of life in menopausal women. REFERENCES Ceylan, B., & Özerdoğan, N. (2015). Factors affecting age of onset of menopause and determination of quality of life in menopause. Journal of Turkish Society of Obstetric and Gynecology, 12(1), 43–49. doi: 10.4274/tjod.79836 Estrogen and Progestin (Hormone Replacement Therapy). (2019). AHFS Consumer Medication Information, 1. Retrieved from https://search-ebscohost- com.chamberlainuniversity.idm.oclc.org/login.aspx? direct=true&db=l0h&AN=78170237&site=ehost-live&scope=site Hill, D. A., Crider, M., & Hill, S. R. (2016). Hormone Therapy and Other Treatments for Symptoms of Menopause. American Family Physician, 94(11), 884–889. Retrieved from https://search-ebscohost-com.chamberlainuniversity.idm.oclc.org/login.aspx? direct=true&db=mdc&AN=27929271&site=eds-live&scope=site Johnson, A., Roberts, L., & Elkins, G. (2019). Complementary and Alternative Medicine for Menopause. Journal of Evidence-Based Integrative Medicine, 24. doi: 10.1177/2515690x19829380 Kariman, N., Taebi, M., Abdolahian, S., Ozgoli, G., & Ebadi, A. (2018). Strategies to improve menopausal quality of life: A systematic review. Journal of Education and Health Promotion, 7(1), 93. doi: 10.4103/jehp.jehp_137_17 Leo, S. D., Lee, S. Y., & Braverman, L. E. (2016). Hyperthyroidism. The Lancet, 388(10047), 906–918. doi: 10.1016/s0140-6736(16)00278-6 (2014). National Collaborating Centre for Women's and Children's Health (UK). Menopause: Full Guideline. London: National Institute for Health and Care Excellence (UK); 2015 Nov 12. (NICE Guideline, No. 23.) 5, Diagnosis of perimenopause and menopause.Available from: https://www.ncbi.nlm.nih.gov/books/NBK343466/ Practice Bulletin No. 141. Obstetrics & Gynecology, 123(1), 202–216. doi: 10.1097/01.aog.0000441353.20693.78 Roberts, D. (2018). Chronic fatigue syndrome and quality of life. Patient Related Outcome Measures, Volume 9, 253–262. doi: 10.2147/prom.s155642 Schub, T. B., & Schiebel, D. F. (2018). Menopause: Osteoporosis. CINAHL Nursing Guide. Retrieved from https://search-ebscohost-com.chamberlainuniversity.idm.oclc.org/login.aspx? direct=true&db=nup&AN=T701135&site=eds-live&scope=site Watts, N. B. (2018). Postmenopausal Osteoporosis: A Clinical Review. Journal of Womens Health, 27(9), 1093–1096. doi: 10.1089/jwh.2017.6706 What medication can you take to help with menopause symptoms ? Venlafexine when should you worry if you have post menopausal bleeding ? always have it checked do you have to worry about getting pregnant after menopause? [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 04, 2022
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Jan 04, 2022
Downloads
0
Views
73

.png)


.png)



.png)