*NURSING > EXAM REVIEW > NR 283 Pathophysiology Exam 1 Concepts to Review,100% CORRECT (All)
NR 283 Pathophysiology Exam 1 Concepts to Review,100% CORRECT
Document Content and Description Below
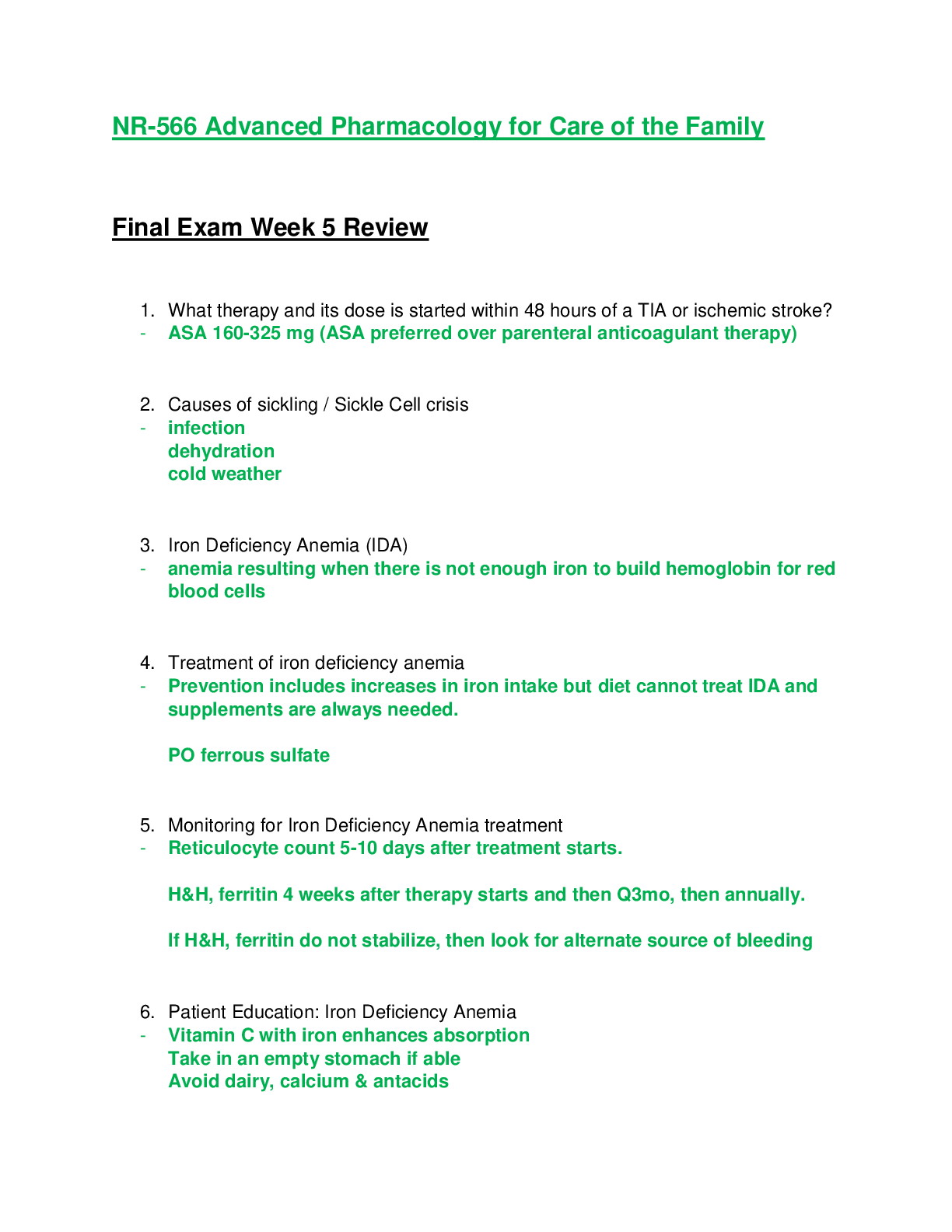
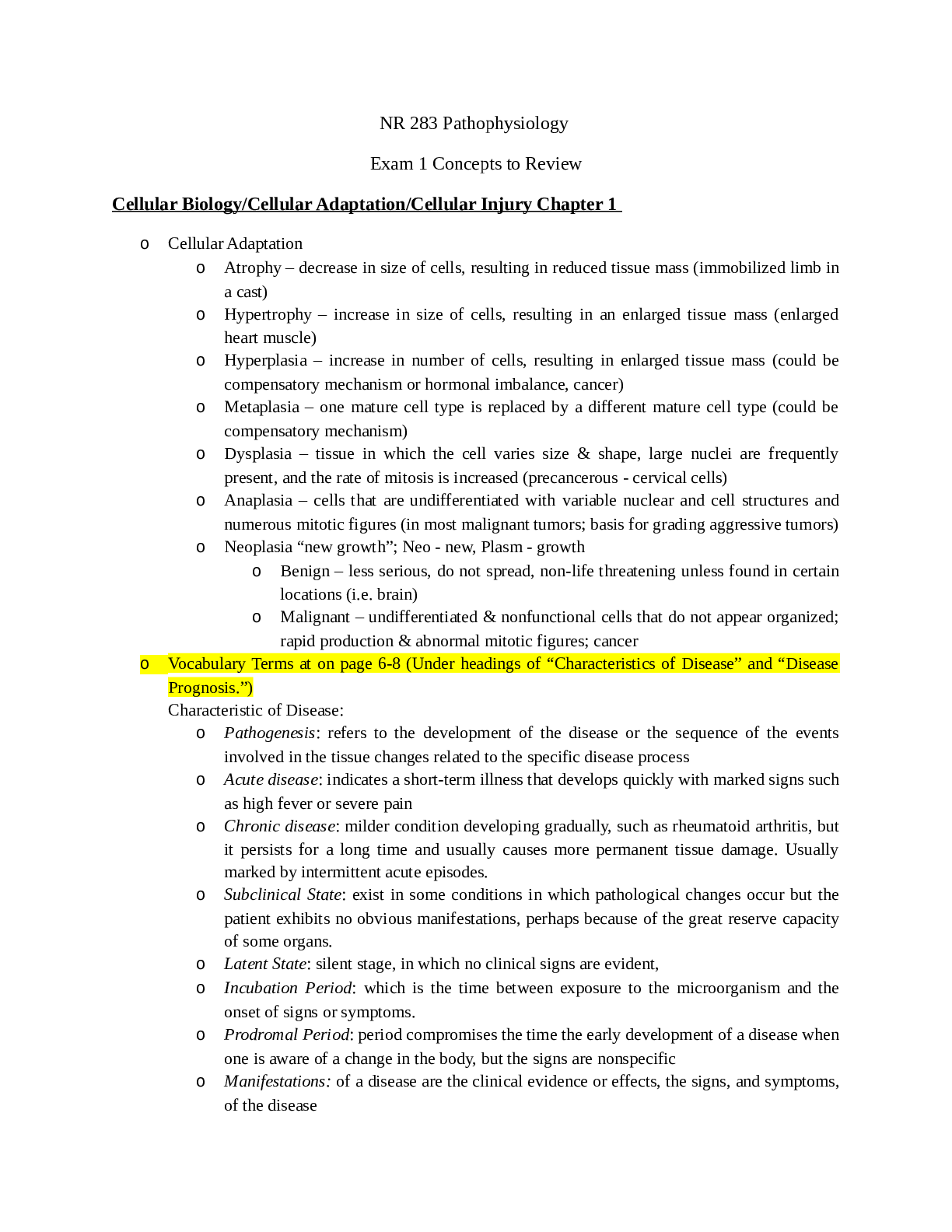
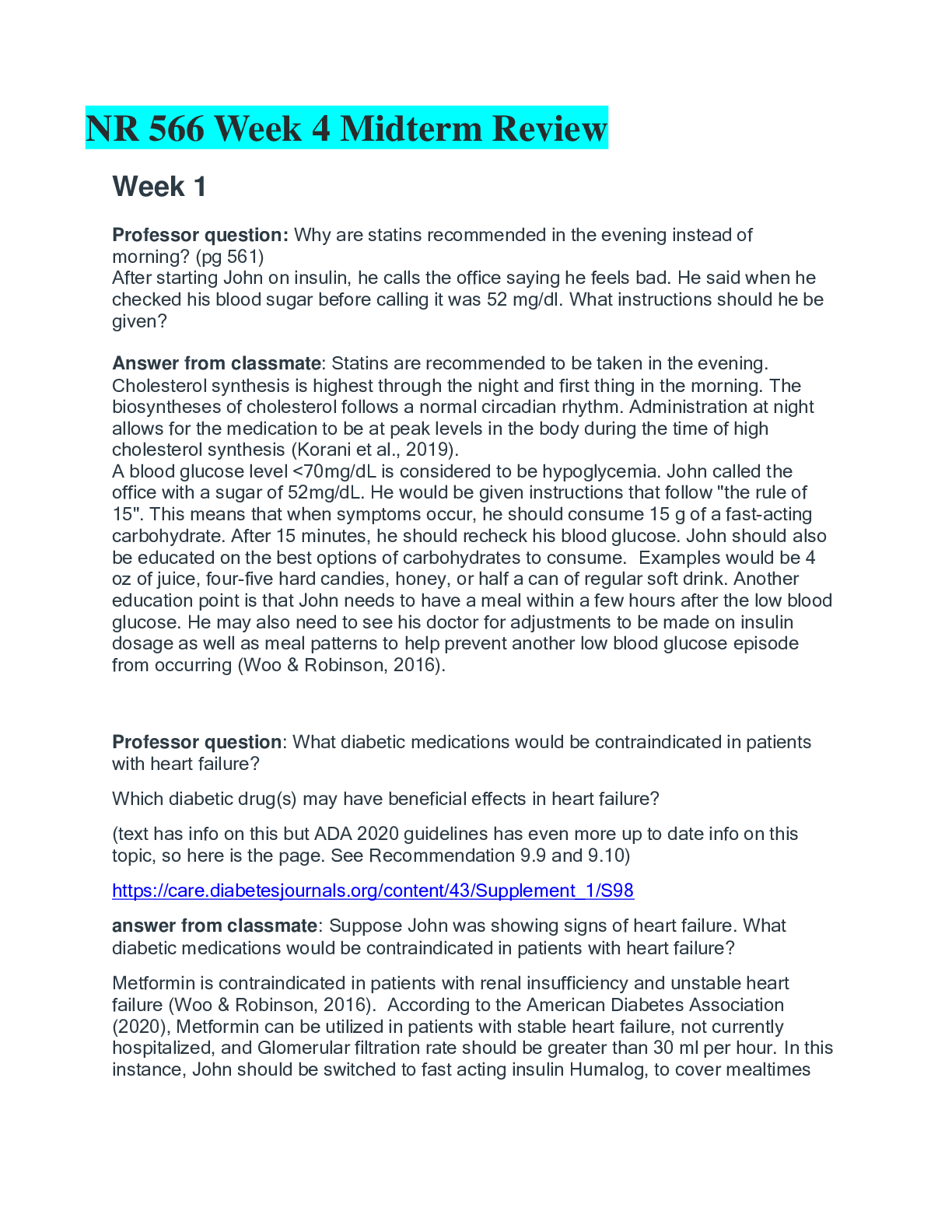
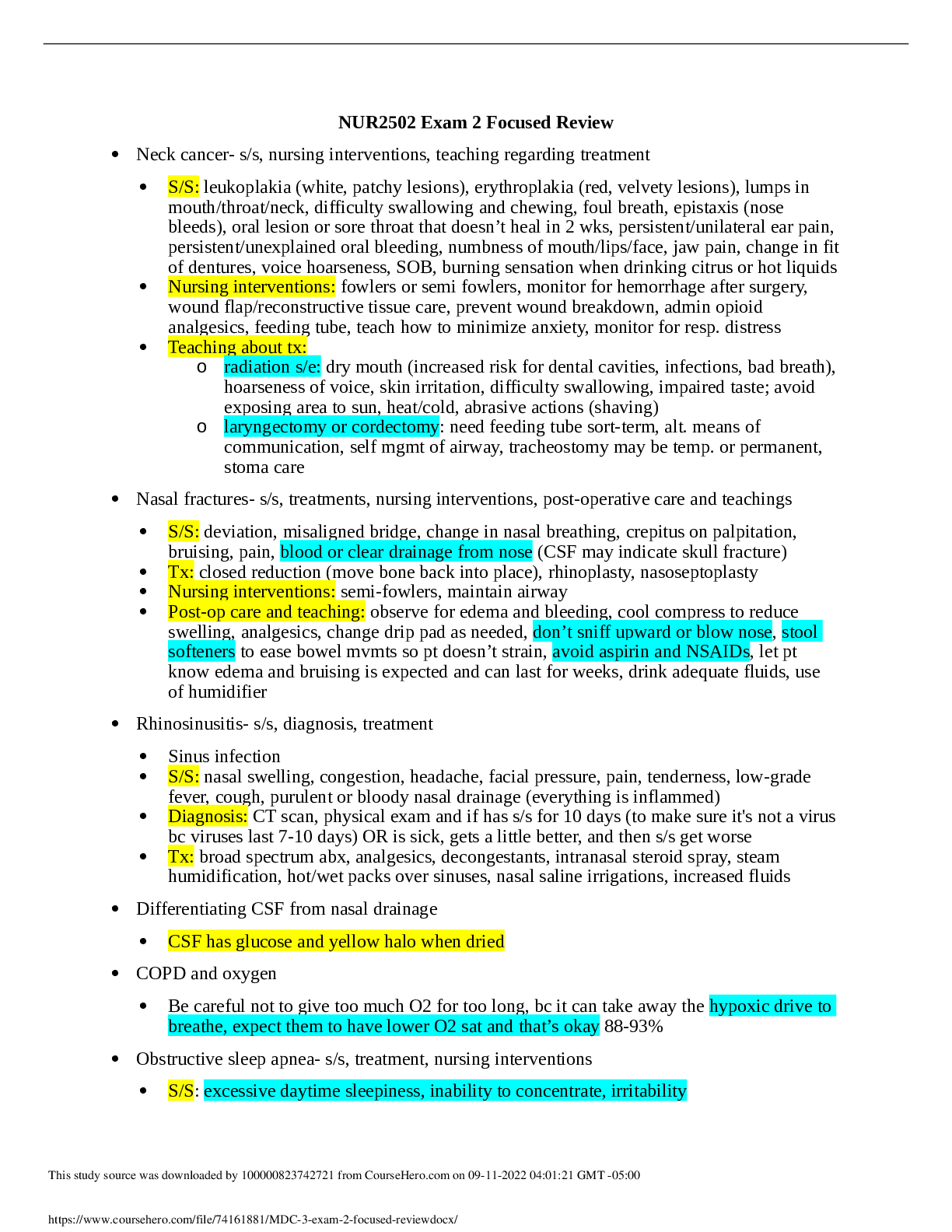
NR 283 Pathophysiology Exam 1 Concepts to Review Cellular Biology/Cellular Adaptation/Cellular Injury Chapter 1 o Cellular Adaptation o Atrophy – decrease in size of cells, resulting in r... educed tissue mass (immobilized limb in a cast) o Hypertrophy – increase in size of cells, resulting in an enlarged tissue mass (enlarged heart muscle) o Hyperplasia – increase in number of cells, resulting in enlarged tissue mass (could be compensatory mechanism or hormonal imbalance, cancer) o Metaplasia – one mature cell type is replaced by a different mature cell type (could be compensatory mechanism) o Dysplasia – tissue in which the cell varies size & shape, large nuclei are frequently present, and the rate of mitosis is increased (precancerous - cervical cells) o Anaplasia – cells that are undifferentiated with variable nuclear and cell structures and numerous mitotic figures (in most malignant tumors; basis for grading aggressive tumors) o Neoplasia “new growth”; Neo - new, Plasm - growth o Benign – less serious, do not spread, non-life threatening unless found in certain locations (i.e. brain) o Malignant – undifferentiated & nonfunctional cells that do not appear organized; rapid production & abnormal mitotic figures; cancer o Vocabulary Terms at on page 6-8 (Under headings of “Characteristics of Disease” and “Disease Prognosis.”) Characteristic of Disease: o Pathogenesis: refers to the development of the disease or the sequence of the events involved in the tissue changes related to the specific disease process o Acute disease: indicates a short-term illness that develops quickly with marked signs such as high fever or severe pain o Chronic disease: milder condition developing gradually, such as rheumatoid arthritis, but it persists for a long time and usually causes more permanent tissue damage. Usually marked by intermittent acute episodes. o Subclinical State: exist in some conditions in which pathological changes occur but the patient exhibits no obvious manifestations, perhaps because of the great reserve capacity of some organs. o Latent State: silent stage, in which no clinical signs are evident, o Incubation Period: which is the time between exposure to the microorganism and the onset of signs or symptoms. o Prodromal Period: period compromises the time the early development of a disease when one is aware of a change in the body, but the signs are nonspecific o Manifestations: of a disease are the clinical evidence or effects, the signs, and symptoms, of the disease o Local: found at the site of the problem o Systemic: general indicators of illness o Signs: objective indicators of disease that are obvious to someone other than the affected individual. Can be local or systemic o Symptoms: subjective feelings, such as pain or nausea o Lesion: term used to describe a specific local change in the tissue. Can be microscopic o Syndrome: a collection of signs and symptoms, often affecting more than one organ, that usually occur together in response to a certain condition o Diagnostic tests: laboratory tests that assist in the diagnosis of a specific disease o Remission: is a period or condition in which the manifestations of the disease subside, either permanently or temporarily o Exacerbations: is a worsening in the severity of the disease or in its signs/symptoms o Precipitating Factor: condition that triggers an acute episode o Complications: are new secondary or additional problems that arise after the original disease begins o Therapy/ therapeutic interventions: treatment measures used to promote recovery or slow the progress of a disease. Ex: surgery, drugs, physiotherapy, therapies, behavior modifications o Sequelae: the potential unwanted outcomes of the primary condition, such as paralysis following recovery from stroke o Convalescence or rehabilitation: period of recovery and return to the normal healthy state, may last days or months Disease Prognosis: o Prognosis: probability or likelihood for recovery or other outcomes o Morbidity: indicates the disease rate within a group o Mortality: indicate the relative number of deaths resulting from a particular disease o Autopsy: examination of all or part of the body by a pathologist o Epidemiology: science of tracking the pattern or occurrence of disease o Occurrence: tracked by two factors o Incidence: the number of new cases in a given population noted within a stated time frame. o Prevalence: number of new and old or existing cases within a specific population and time frame. o Epidemics: occur when there are a higher than expected number of cases of an infectious disease within a given area o Pandemics: higher numbers of cases in many regions of the globe o Communicable: disease or infections that can be spread from one person to another o Notifiable/ Reportable: disease must be reported by the physician to certain designated authorities. o Types of tissue necrosis o Liquefaction Necrosis – dead cells liquify due to certain cell enzymes (ex. brain tissue dies or cavity/ulcer development in affected area) o Coagulative Necrosis – cell proteins are altered or denatured (ex. MI due to lack of oxygen) o Fat Necrosis – fatty tissue breaks down into fatty acids in the presence of infection or certain enzymes o Caseous Necrosis – form of coagulation necrosis; thick, yellowish, “cheesy” substance (ex. Tuberculosis) o Infarction - area of dead cells resulting from lack of oxygen (ex. MI) o Gangrene – necrotic tissue due to lack or loss of blood supply followed by invasion of bacteria o Seven Steps for Health 1. Be a nonsmoker and avoid second-hand smoke. 2. Eat 5 to 10 servings of vegetables and fruit a day. Choose high-fiber, lower-fat foods. If you drink alcohol, limit your intake to one to two drinks a day. 3. Be physically active on a regular basis. This will also help you to maintain a healthy body weight. 4. Protect yourself and your family from the sun. 5. Follow cancer screening guidelines. 6. Visit your doctor or dentist if you notice any change in your normal state of health. 7. Follow health and safety instructions at home and at work when using, storing, and disposing of hazardous materials. Genetics Chapter 21 • Congenital: Meaning o Genetic & inherited disorders present at birth • Teratogens: Meaning and types o Agents that cause damage during embryonic or fetal development o Types: ▪ Physical agents ▪ Metabolic conditions ▪ Infections ▪ Drugs & Chemicals • Genetic Diseases - know where these examples fall under inheritance; chance of inheritance as it applies to X-linked, autosomal dominant, and autosomal recessive, characteristics, and risk factors if applicable. o Down syndrome: Chromosomal Disorder (Trisomy 21) ▪ Inheritance? • No ▪ Characteristics: • Small head, round face, flat facial profile • Slanted eyes and epicanthic fold • Large tongue, high-arched palate • Small hands, single palmar crease • Short stature • Muscles tend to be hypotonic; loose joints • Delayed developmental stages • Cognitive impairment ranges from mild to major • Delayed or incomplete sexual development • Males infertile • Females have lower rate of conception ▪ Risk factors? • Maternal age o Turner’s Syndrome or Monosomy Occurs when only one sex chromosome, the x chromosome is present. This person has only 45 chromosomes, resulting in a variety of physical abnormalities and lack of ovaries. ▪ Inheritance? • Most cases are not inherited ▪ Chance of Inheritance? • Women with syndrome who conceive naturally have 30% chance of having a fetus with Turner Syndrome ▪ Characteristics • Short stature and webbed neck • Delayed puberty • Infertility • Heart defects • Certain learning disabilities ▪ Risk Factors o Marfan’s: Autosomal Dominant Disorder ▪ Inheritance? • Yes ▪ Chance of inheritance? • Affected parent has a 50% probability of passing the disorder on to each child regardless of gender ▪ Characteristics: • Skeletal deformities like pectus excavatum and abnormal curvature of the thoracic spine • Aorta is wider and more fragile leading to leakage of the aortic valve or tears to the aortic wall ▪ Risk factors? • o Huntington’s: Autosomal Dominant Disorder ▪ Inheritance? • Yes ▪ Chance of inheritance? • Affected parent has a 50% probability of passing the disorder on to each child regardless of gender ▪ Characteristics: • Difficulty swallowing • Strange and uncontrolled movements that are either slow or wild and jerking ▪ Risk factors? • Developed later in life (30-40 y.o.) o Color Blindness: X-Linked Recessive Disorders ▪ Inheritance? • Yes, may appear to skip generations ▪ Chance of inheritance? • Carrier females have a 50% chance of producing an affected male child and an equal chance of producing a carrier female child in each pregnancy ▪ Characteristics: • ▪ Risk factors? • Fam. Hx o Hemophilia: X-Linked Recessive Disorder ▪ Inheritance? • Yes, may appear to skip generations ▪ Chance of inheritance? • Carrier females have a 50% chance of producing an affected male child and an equal chance of producing a carrier female child in each pregnancy ▪ Characteristics: • Prolonged bruising ▪ Risk factors? • o Duchenne’s Muscular Dystrophy: X-Linked Recessive Disorder ▪ Inheritance? • Yes, may appear to skip generations ▪ Chance of inheritance? • Carrier females have a 50% chance of producing an affected male child and an equal chance of producing a carrier female child in each pregnancy ▪ Characteristics: • ▪ Risk factors? • o Cystic Fibrosis: Autosomal Recessive Disorders ▪ Inheritance? • Yes ▪ Chance of inheritance? • 25% that the child will be born with the unaffected genotype • 50% that the child will be born with the carrier genotype • 25% that the child will be born with the affected or disease genotype ▪ Characteristics: • ▪ Risk factors? • o Turner Syndrome: Chromosomal Disorder (Monosomy X) ▪ Inheritance? • No ▪ Characteristics: • Short stature • Webbed neck ▪ Risk factors? • o Klinefelter’s Syndrome: Chromosomal Disorder (Polysomy X) ▪ Inheritance? • No ▪ Characteristics: • Small testes and do not produce sperm • Develop breast tissue ▪ Risk factors? • Chapter 2 • What controls sodium balance o the sodium-potassium pump or active transport, resulting in sodium levels that are high in extracellular fluids and low inside the cell • Causes of Edema o Increased Capillary Hydrostatic Pressure o Loss of Plasma Proteins o Obstructions of the Lymphatic Circulation o Increased Capillary Permeability • Electrolytes found in intracellular fluid and extracellular fluid o Intracellular: Potassium o Extracellular: Sodium Chloride • Types of edema (localized, generalized, pitting) o Pitting edema – excess fluid moved aside when fingers pressed into tissue o Generalized – increase in body weight o Localized – central to one specific area • Hypervolemia (S/S, causes) o Increase in blood volume • Hypovolemia (Dehydration) (S/S, causes) o Fluid deficit in the excess vascular compartment o Dehydration – insufficient body fluid resulting from adequate intake or excessive loss of fluids or a combination of both ▪ S/S • Vomiting/ Diarrhea (Loss of electrolytes, nutrients, water) • Excessive sweating (Loss of sodium & water) • Diabetic ketoacidosis (Loss of fluid, electrolytes, glucose in urine) • Insufficient water intake in elderly or unconscious person • Use of concentrated formula (infant) • Hypernatremia (S/S, causes) < 142 mEq/L o Ingestion of large amounts of sodium w/o proportionate water intake o Loss of water faster than the loss of water o Cause: ▪ Specific causes include the following: • Insufficient ADH, which results in a large volume of dilute urine (diabetes insipidus) • Loss of the thirst mechanism • Watery diarrhea • Prolonged periods of rapid respiration o S/S: ▪ Thirst: tongue & mucosa are dry & sticky ▪ Weakness ▪ Lethargy ▪ Agitation ▪ Edema ▪ Elevated blood pressure ▪ Decreased U/O due to ADH secretion • Hyponatremia (S/S, causes) > 135 mEq/L o Direct loss of sodium from the body o An excess of water in the extracellular compartment resulting in dilution of sodium o Cause: ▪ Losses from excessive sweating, vomiting, and diarrhea ▪ Use of certain diuretic drugs combined with low-salt diets ▪ Hormonal imbalances such as insufficient aldosterone, adrenal insufficiency, and excess ADH secretion (SIADH or syndrome of inappropriate antidiuretic hormone secretion) ▪ Early chronic renal failure ▪ Excessive water intake o S/S: ▪ Anorexia, nausea, cramps ▪ Fatigue, lethargy, muscle weakness ▪ Headache, confusion, seizures ▪ Decreased blood pressure • Hyperkalemia (S/S, causes) < 5 mEq/L o Causes: ▪ Renal failure ▪ Deficit of aldosterone ▪ Use of “potassium-sparing” diuretic drugs, which prevent potassium from being excreted in adequate amounts ▪ Leakage of intracellular potassium into the extracellular fluids in patients with extensive tissue damage such as traumatic crush injuries or burns ▪ Displacement of potassium from cells by prolonged or severe acidosis o S/S: ▪ Arrhythmias, cardiac arrest ▪ Nausea, diarrhea ▪ Muscle weakness, paralysis beginning in the legs ▪ Paresthesias – fingers, toes, face, tongue ▪ Oliguria ▪ Acidosis – serum pH > 35 • Hypokalemia (S/S, causes) > 3.5 mEq/L o Causes: ▪ Excessive losses from the body due to diarrhea ▪ Diuresis associated with certain diuretic drugs; patients with heart disease who are being treated with certain diuretic drugs such as furosemide may have to increase their intake of potassium in food or take a potassium supplement because hypokalemia may increase the toxicity of heart medications such as digitalis ▪ The presence of excessive aldosterone or glucocorticoids in the body (in Cushing syndrome, in which glucocorticoids have some mineralocorticoid activity, retaining sodium and excreting potassium) ▪ Decreased dietary intake, which may occur with alcoholism, eating disorders, or starvation ▪ Treatment of diabetic ketoacidosis with insulin o S/S: ▪ Cardiac arrhythmias, cardiac arrest ▪ Anorexia, nausea, constipation ▪ Fatigue, muscle twitch (tetany), weakness, leg cramps ▪ Shallow respirations, paresthesias ▪ Postural hypotension, polyuria, nocturia ▪ Alkalosis – serum pH < 7.45 • Hypercalcemia (S/S, causes) < 10 mEq/L o Causes: ▪ Uncontrolled release of calcium ions from the bones due to neoplasms; malignant bone tumors may directly destroy the bone, and some tumors, such as bronchogenic carcinoma, may secrete PTH in excess of body needs ▪ Hyperparathyroidism ▪ Immobility, which may decrease stress on the bone, leading to demineralization ▪ Increased intake of calcium due either to excessive vitamin D or to excess dietary calcium ▪ Milk-alkali syndrome, associated with increased milk and antacid intake, which may also elevate serum calcium levels o S/S: ▪ Apathy, lethargy ▪ Anorexia, nausea, constipation ▪ Polyuria, thirst ▪ Kidney stones ▪ Arrhythmias, prolonged strong cardiac contractions, increased blood pressure • Hypocalcemia (S/S, causes) > 8 mEq/L o Causes: ▪ Hypoparathyroidism—decreased parathyroid hormone results in decreased intestinal calcium absorption ▪ Malabsorption syndrome—resulting in decreased intestinal absorption of vitamin D or calcium ▪ Deficient serum albumin ▪ Increased serum pH—resulting in alkalosis o S/S: ▪ Tetany—involuntary skeletal muscle spasm, carpopedal spasm, laryngospasm ▪ Tingling fingers ▪ Mental confusion, irritability ▪ Arrhythmias, weak heart contractions • Sodium imbalances o Found in Neuro • Potassium imbalances o Found in Heart • Acid/base balance o Essential to homeostasis o Normal serum pH range 7.35 – 7.45 • High Risk Population for dehydration o Elderly & Infants • Insensible fluid loss o Urine o Feces o Skin (perspiration) o Exhaled air • Causes for Dehydration in the elderly o Decrease water intake • Fluid regulation (Hydrostatic Pressure, Osmotic Pressure) o Hydrostatic Pressure pushes fluid o Osmotic Pressure pulls fluid • Normal level for pH o Normal serum pH 7.35 – 7.45 Chapter 5, 6 and 7 • Anaphylaxis o Severe, life-threatening, systemic hypersensitivity reaction resulting in decreased blood pressure, airway obstruction, and severe hypoxia. • Erythrocyte sedimentation rate (ESR) o Elevated plasma proteins increase the rate at which red blood cells settle in a sample o General indicator of inflammation (along with C-reactive protein) • Roles of the types of White blood cells (Leukocytes) o Neutrophils – Phagocytosis; nonspecific defense; active in inflammatory process o Basophils – Bind IgE, releases histamine in anaphylaxis o Eosinophils – Participate in allergic responses and defense against parasites o Monocytes – Migrate from the blood into tissues to become macrophages o T lymphocytes – cell-mediated immunity • Hypersensitivity o Allergic reactions are unusual and sometimes harmful immune responses to normally harmless substances • Signs and Symptoms of inflammation o Local signs ▪ Pain, swelling, redness, & warmth • Bacterial: purulent exudate • Viral: serous, clear exudate o Systemic signs ▪ Fever (possible) ▪ Fatigue & weakness ▪ Headache ▪ Nausea • Types of Hypersensitivity reactions (4 Types) o Allergic Reactions (immediate inflammation & pruritis) ▪ Hay fever; Anaphylaxis o Cytotoxic Hypersensitivity (cell lysis & phagocytosis) ▪ ABO blood incompatibility o Immune Complex Hypersensitivity (inflammation; vasculitis) ▪ Autoimmune disorders • Systemic Lupus • Erythematosus • Glomerulonephritis o Cell-Mediated / Delayed Hypersensitivity (delayed inflammation) ▪ Contact dermatitis: transplant rejection • Tests for immunity o Antigen identification o Antibody titer (measure levels of serum immunoglobulins) o Indirect Coomb’s Test (detects Rh blood incompatibility) o Elisa (detects HIV antibodies; used for several other diseases) o MHC typing (tissue matching before transplantation procedure) • Opportunistic Infections o Microbes that are not pathogenic under normal circumstances but may cause disease if they are transferred to another location in the body, if the balance among the species is not maintained or if the boy’s defenses are impaired. • Systemic versus local signs and symptoms o Local S&S ▪ Inflammation (pain, tenderness, swelling, redness, & warmth) ▪ Bacterial: purulent exudate / pus ▪ Viral: serous, clear exudates o Systemic S&S ▪ Fever, fatigue & weakness, headache, nausea ▪ Severe infections: nervous system may be affected, confusion / disorientation, seizures (convulsions), or loss of consciousness • Active vs Passive Immunity o Active Immunity: develops when the person’s own body develops antibodies or T cells in response to a specific antigen introduced into the body ▪ Takes a few weeks but lasts for years due to T & B Cells ▪ 2 forms • Active Natural (direct exposure to an antigen – chickenpox) • Active Artificial (vaccine injection – measles) o Passive Immunity: when antibodies are transferred from one person to another ▪ Effective immediately, but temporary protection ▪ 2 forms • Passive Natural (mother to fetus via placenta) • Passive Artificial (injection of antibodies from one person/animal into a second person) • Innate Immunity o Gene specific and is related to ethnicity • Humoral Immunity vs Cellular Immunity o Humoral Immunity – antibodies are produced to protect the body o Cellular Immunity – lymphocytes are programmed to attack nonself cells to protect the body • B cells o Responsible for production of antibodies o Humoral immunity o Mature in bone marrow ▪ Proceed to the spleen and lymphoid tissue o Plasma cells ▪ Produce antibodies o B memory cells ▪ Can quickly form clone of plasma cells • T cells o From the bone marrow stem cells o Further differentiation in thymus o Cell-mediated immunity o Cytotoxic T killer cells o Helper T cells o Memory T cells • Memory cells o Memory B cells o Memory T cells • Autoimmune definition o The immune system no longer recognizes itself from nonself and begins to attack its own cells / structures or organs • Most common cause of death in AIDS o Secondary infections ▪ Lungs – Pneumocystis carinii & Tuberculosis • Blood Transfusion Reaction o A reaction that will destroy the RBC (hemolysis) • Virus Replication o Trick the cells to create more • Bacterial Replication o Binary Fission ▪ A division of the cell that produces 2 daughter cells identical to the parent bacterium • Aerobic metabolism vs Anaerobic metabolism o Anaerobic metabolism – absence of oxygen o Aerobic metabolism – presence of oxygen • Sterile areas in the body (mostly the lungs and the bladder) o Skin: Blood, CSF o Nose; Pharynx: Lungs o Mouth; Colon; Rectum o Vagina: Uterus; Fallopian Tubes; Ovary o Distal Urethra & Perineum: Kidneys & Bladder • Nosocomial Definition o Infections that occur in the hospital care facilities ▪ Hospitals ▪ Nursing homes ▪ Doctor’s offices ▪ Dental offices • Carrier Definition o Persons who have a subclinical form of infection that is very mild, with few or no manifestations • Universal Precautions o Basic guidelines by which all blood, body fluids, and wastes are considered “infected” in any client regardless of the client’s apparent condition • Bacteremia o Presence of bacteria in the blood • Culture and Sensitivity tests o Culture – organisms grown in a specific medium o Sensitivity – Kirby Bauer & Minimum Inhibitory Concentration (MIC) ▪ Determine which drug therapy will be effective against the pathogen • Antiseptic versus Disinfectant o Antiseptics – antimicrobial chemicals designed to be used on living tissue (isopropyl 8alcohol 70%) o Disinfectants – chemical solutions designed to be used on nonliving surfaces that are known to destroy microorganisms or their toxins on inanimate objects (glutaraldehyde) • Types of Isolation for communicable diseases o Contact o Airborne o Droplet Chapter 20 Study Guide 1. 2. Define the following terms: i. neoplasm: A neoplasm or tumor is a cellular growth that is no longer responding to normal body controls. Cells continue to reproduce when there is no need for them. This excessive growth deprives other cells of nutrients. Many neoplasms are unable to function as normal tissue cells because they consist of atypical (abnormal) or immature cells. ii. benign: Benign tumors usually consist of differentiated cells that reproduce at a higher-than-normal rate. The benign tumor is often encapsulated and expands but does not spread. It is usually freely moveable on palpation. Tissue damage results from compression of adjacent structures such as blood vessels. A benign tumor is not considered life threatening unless it is in an area such as the brain where the pressure effects can become critical. iii. malignant: Malignant tumors are usually made up of undifferentiated, nonfunctional cells that do not appear organized. The cells tend to reproduce more rapidly than normal and often show abnormal mitotic figures. These cells have lost cellular connections with each other, and reproduction is not inhibited in the presence of other similar cells. Tumor cells infiltrate or spread into surrounding tissue and may easily metastasize or break away to spread to other organs and tissues iv. carcinoma: malignant tumor of epithelial tissue v. sarcoma: malignant tumor of connective tissue vi. anaplasia: A grade IV tumor that is undifferentiated with cells varying in size and shape (anaplasia); this type of tumor is considered highly malignant and likely to progress quickly. 2. Name three specific pathophysiologic changes that occur in the formation of malignant tumors. • Cells have altered genetics leading to initial immune response • Inner cells may die (necrosis) leading to further local inflammation and infection • Some secrete growth factors that stimulate blood vessel growth (angiogenesis) 3. Identify the correct nomenclature for both benign and malignant tumors in the following tissues/organs: Benign Tumor Malignant Tumor Pancreas Islet celladenoma, insulinoma, gastrinoma Islet cell carcinoma Fat Lipoma Liposarcoma Bone Osteoma Osteosarcoma Liver Adenoma Adenocarcinoma Cartilage Chondroma Chondrosarcoma Skin Lipomas, hemangiomas, moles, warts Basal cell carcinoma, squamous cell carcinoma, melanoma 4. Compare and contrast benign and malignant tumors using the following chart: Benign Tumors Malignant Tumor Cells Similar to normal cells Differentiated Mitosis fairly normal Varied in size/shape with large nuclei Many undifferentiated Mitosis increased & atypical Growth Relatively slow Expanding mass Frequently encapsulated Rapid growth Cells not adhesive, infiltrate tissue No capsule Spread Remains localized Invades nearby tissues or metastasizes to distant sites thru blood & lymph vessels Systemic effects Rare Often present General prognosis Not life threatening unless in certain locations such as brain Life threatening by tissue destructions and spread of tumors 5. Identify the warning signs of cancer. • Unusual bleeding or discharge anywhere in the body • Change in bowel or bladder habits • A change in a wart or mole • A sore that does not heal • Unexplained weight loss • Anemia or low hemoglobin and persistent fatigue • Persistent cough or hoarseness without reason 6. A tumor is a space-occupying mass that produces predictable local effects as it enlarges. Describe the consequences that could result from the following effects: i. compression of blood vessels: ischemia, necrosis, and areas of inflammation around the tumor; potential for infection ii. compression or obstruction of a tube or duct: blockage of secretion or normal flow of air (bronchi), food (GI tract), blood, or lymph de- pending on location iii. compression of nerves: pain and loss of function iv. erosion of blood vessels and other structures: hemorrhage, inflammation, necrosis v. invasion and replacement of normal tissue: loss of normal tissue function 7. Malignant tumors also have generalized systemic effects. Outline the factors that contribute to the development of the following systemic manifestations: i. weight loss and cachexia: (cachexia is severe tissue wasting) Contributing factors include anorexia, fatigue, pain, stress, and the increased demands placed on the body by reproducing tumor cells (nutrient trapping), altered carbohydrate and protein metabolism, and cachectic factors produced by macrophages in response to the tumor. This in turn leads to added fatigue and weakness and tissue breakdown. ii. anemia (decreased hemoglobin): Common problem resulting from anorexia and decreased food intake, chronic bleeding with iron loss, and bone marrow depression. Anemia decreases the oxygen available to cells, leading to fatigue and poor tissue regeneration. iii. systemic infections: Infections such as pneumonia occur frequently as host resistance declines. Tissue breakdown develops, and the immune system is less effective. The host's immobility contributes to infection in the lungs because of stasis of secretions in the lungs and a weaker cough effort. iv. bleeding: May occur because the tumor cells may erode the blood vessels or cause tissue ulceration. Bone marrow depression and hypoproteinemia may contribute to poor clotting. Chronic bleeding is common in the digestive tract, where the mucosa fails to regenerate quickly. Chronic blood loss leads to iron-deficiency anemia 8. Define and describe paraneoplastic syndrome. -Additional problems associated with certain tumors, such as bronchogenic carcinoma in the lungs. Tumor cells release substances that affect neurologic function or blood clotting or have hormonal effects. Example: the cells of a bronchogenic carcinoma may produce adrenocorticotropic hormone, leading to the manifestations of Cushing syndrome in the patient. This syndrome may confuse the diagnosis of cancer, complicate the monitoring and treatment of the patient, and cause change in body image. 9. Explain how the following diagnostic tools can assist in the detection and diagnosis of cancer: i. blood tests: important both as an indicator of a problem and in monitoring the effects of chemotherapy and radiation. Hemoglobin and erythrocyte counts may be low—a general sign of cancer. In some types of cancer, such as leukemia, the cell characteristics are diagnostic when confirmed by a bone marrow examination. Therapy frequently results in thrombocytopenia, erythrocytopenia, and leukopenia, and these may limit treatment if cell counts fall too low. ii. tumor markers: Are substances, enzymes, antigens, or hormones produced by some neoplastic cells. These tumor cell markers can be used to screen high-risk individuals, confirm a diagnosis, or monitor the clinical course of a malignancy. Examples include carcinoembryonic antigen for colon cancer, human chorionic gonadotropin for testicular cancer, alpha-fetoprotein for hepatocellular cancer, CA125 for ovarian cancer, and prostate specific antigen for prostate cancer. iii. x-ray, ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT or CAT scan): methods of examining changes in tissues or organs iv. biopsy and histologic and cytologic examinations: Cytologic tests are used to screen high-risk individuals, confirm a diagnosis, or follow a clinical course and monitor change. Histologic and cytologic examinations are used to evaluate biopsies of suspicious masses and check sloughed cells in specific tissues (exfoliative cytology). This is the only dependable confirmation of malignancy. 10. Describe how malignant cells spread from the original tumor to distant sites in the body. What is this called? -Metastasis means spread to distant sites by blood or lymphatic channels. In this case the tumor cells erode into a vein or lymphatic vessel, travel through the body, and eventually lodge in a hospitable environment to reproduce and create one or more secondary tumors 11. Distinguish between the grading and staging of neoplasms. -Staging is based on: • Size of the primary tumor • Extent of involvement of regional lymph nodes • Spread of the tumor 12. Differentiate between an initiating factor and a promoter in relation to carcinogenesis. -Initiating factors or procarcinogens cause the first irreversible changes in the cell DNA. Genetic changes or exposure to an environmental risk may cause this first mutation. This initial change does not create an active neoplasm. -Exposure to promoters later causes further changes in DNA, resulting in less differentiation and an increased rate of mitosis. Dysplasia or anaplasia may be evident at this time. This process may lead to development of the tumor. Promoters include hormones and environmental chemicals. The prolonged time interval and multiple factors involved complicate efforts by researchers to establish risk factors for many cancers. 13. Identify eight risk factors for developing cancer, and include at least one example of each. -Genetic Factors: Leukemia is caused by chromosomal abnormalities -Viruses: hepatitis cancer is caused by hepatitis virus -Radiation: skin cancer is caused by sun exposure -Chemicals: lung cancer is caused by asbestos or nickel -Biologic Factors: colon cancer is caused by ulcerative colitis -Age: many cancers are more common in older people - Diet: colon cancer is caused by a diet high in fat -Hormones: endometrial cancer is caused by estrogen 14. Explain why individuals who have incompetent immune systems are at a higher risk for developing malignancies. -The immune system appears to offer protection by reacting to changes in the membranes of some tumor cells, which are seen as “foreign.” The immune response includes both cell- mediated and humoral immunity. Cytotoxic T lymphocytes, natural killer cells, and macrophages are involved in immune surveillance and the destruction of “foreign” or abnormal cells. Temporary or long-term immunodeficiency has been shown to increase the risk of cancer. For example, HIV infection or AIDS decreases the number of T lymphocytes. 15. Identify the four conventional treatment measures employed in the treatment of cancer. Why are they often used in combination rather than singly? -Surgery -Chemotherapy -Immunotherapy -Radiation Sometimes these treatment options are combined depending on the type of cancer. Not all cancer cells are sensitive to radiation or chemotherapy. Solid tumors are frequently removed by surgery, which is then followed by chemotherapy or radiation (or both) if the tumor cells are sensitive to these therapies. Immunotherapy stimulates the patient's immune system to target the cancer and attack it. 16. Treatment for cancer may be curative, palliative, or prophylactic. Explain the circumstances when each of these treatments may be used. -Curative if the tumor is small and localized. -Palliative if the cancer is advanced. Palliative treatment is intended to reduce the manifestations and complications related to the cancer and to prolong life. For example, decreasing the size of a tumor may lessen the pressure on a nerve, relieving pain, or reduce pressure on the esophagus or bronchus. -Adjuvant therapy is additional prophylactic (preventative) treatment used in cancers that are known to metastasize early in their development, producing secondary tumors that are too small to be detected (micrometastases) 17. Explain how radiotherapy is effective in treating some types of cancer. -Radiation is most effective on cells undergoing DNA synthesis or mitosis; therefore it destroys the more rapidly dividing cells in the body, both tumor cells and normal cells (radiosensitive cells). -Radiation may be used before surgery to shrink a tumor or destroy loose surface cells, or may be begun after healing of the surgical site (approximately 6 weeks). 18. Identify the mechanisms of action of antineoplastic medications. -A combination of two to four drugs, each from a different classification, is given to a patient at periodic intervals. The classifications include antimitotics, antimetabolites, alkylating agents, and antibiotics. The drugs interfere with protein synthesis and DNA replication at different points in the tumor cell cycle, thus destroying the cells. A cell cycle is essentially a mini life cycle of growth and reproduction. The choice of drugs and the timing sequence depend on the cell cycle of the particular tumor cell. So each type of cancer is matched to a specific drug treatment. When each drug acts at a different point in the cell cycle, the maximum number of malignant cells can be destroyed. 19. Identify adverse effects that commonly occur during both radiotherapy and chemotherapy, and explain why they happen. -Bone marrow depression -Vomiting -Cells are damaged -Fibrosis in the lungs 20. What is a biologic response modifier? How are these agents useful in the treatment of some types of cancer? -Biologic response modifiers are agents that augment the natural immune response in the body to improve surveillance and removal of abnormal cells. 21. Explain the three potential goals of gene therapy in the treatment of cancer. • Replace mutated genes with a healthy copy of the gene • Inactivate a mutated gene • Introduce a new gene 23. What is the most common form of skin cancer? -Basal cell carcinoma [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 25, 2021
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Oct 25, 2021
Downloads
0
Views
36




.png)