*NURSING > STUDY GUIDE > Maternal Child Exam 1 study guide/ Concept Guide for Week 3 test-chapters: 2, 3, 4, 5, 6, 7, 8, 9, 1 (All)
Maternal Child Exam 1 study guide/ Concept Guide for Week 3 test-chapters: 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 ; (Nursing, Obstetrics, Test 1, Fetal heart rate, fetal heart tones) / 100% GUARANTEED.
Document Content and Description Below
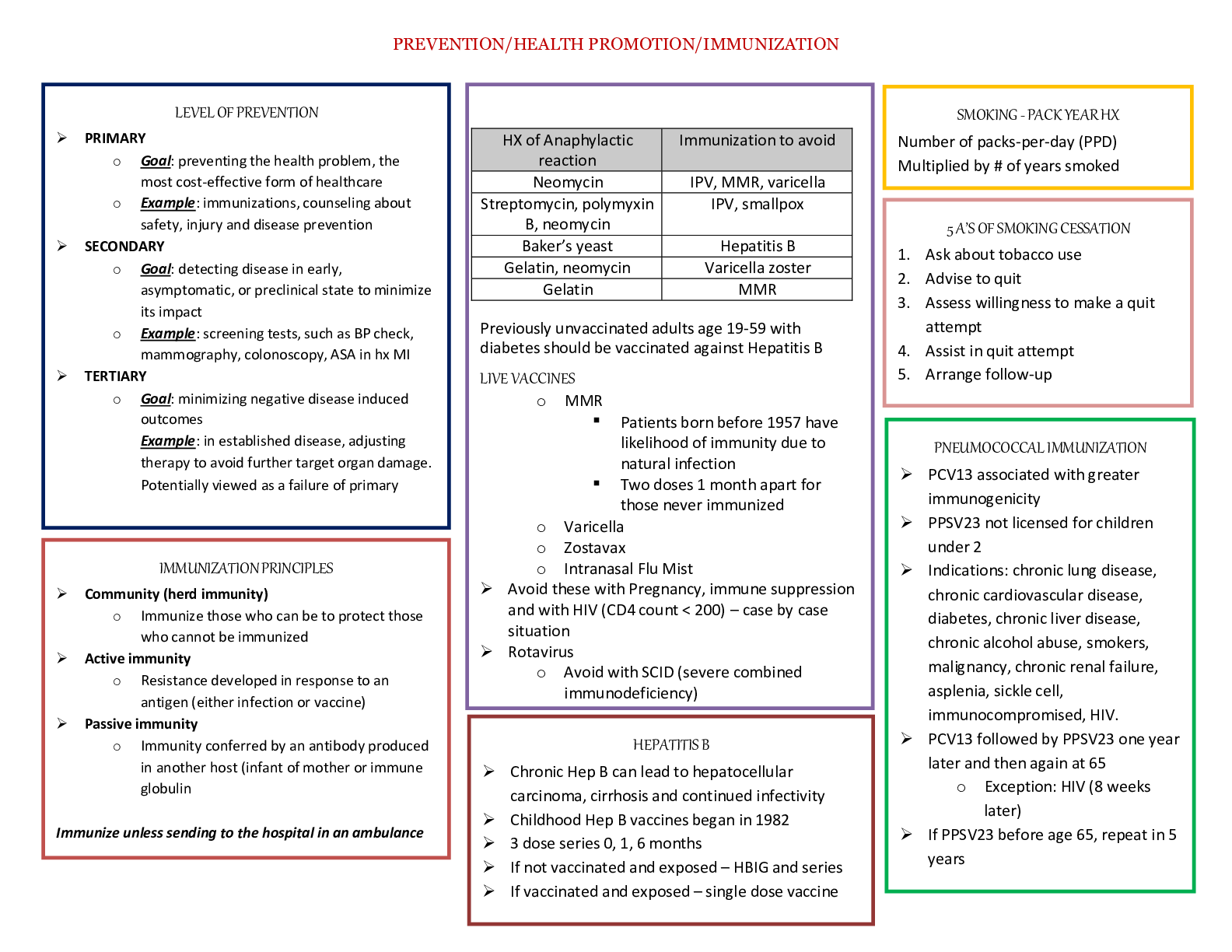
Maternal Child Exam 1 study guide Concept Guide for Week 3 test-chapters: 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 • Nutrition in all 3 trimesters o special needs diets ▪ caloric intake increases on... ly slightly and requires only a 300 kcal/day increase from prepregnant needs. (normal ranges from 1200-2400 cal/day) ▪ In the first trimester, the average maternal weight gain is 1 to 2.5 kg, and thereafter the recommended weight gain for a woman of normal weight is approximately 0.4 kg per week. For overweight women, the recommended weekly weight gain during the second and third trimesters is 0.3 kg; for underweight women, it is 0.5 kg. ▪ Dairy products are a great source of protein and include eggs, milk, cheese, and yogurt. Other protein sources: soy milk and soy cheese, beans, legumes, peanut butter ▪ Calcium is essential for maintaining bone and tooth mineralization and calcification. During pregnancy, calcium must be available to the fetus for the growth and development of the skeleton and teeth. ▪ Calcium foods: dairy, legumes, dark green leafy vegetables, dried fruits, and nuts. o vitamins pregnancy ▪ calcium requirement: 1,300 mg/day ▪ Vit D requirement: 600 IU (15mcg) ▪ The iron RDA for prepregnant women ages 14 to 18 is 15 mg/day, for women age 19 and older, 18 mg/day, and for pregnant women, this amount increases to 27 mg/day, starting by 12 weeks of gestation o Fluid intake recommendations ▪ pregnant women should have an intake of eight to ten (8-oz) glasses of fluid per day. o Folic acid ▪ Increased estrogen alters the absorption and metabolism of folic acid, producing susceptibility for folic acid deficiency. Folic acid deficiency can cause neural tube defects (NTDs), including spina bifida, cleft lip and palate, and anencephaly. ▪ folic acid helps to regulate red blood cell development and facilitates the oxygen- carrying capacity of the blood, produces DNA and RNA and helps to maintain normal brain function and to stabilize mental and emotional health. ▪ minimum of 800 mcg/day of folic acid is recommended ▪ Foods that are rich in folic acid include dark leafy greens, asparagus, broccoli, citrus fruits, beans, peas and lentils, avocado, okra, Brussels sprouts, seeds and nuts, fortified breakfast cereals, and calf liver. • Prenatal o 1st movements ▪ AKA ‘quickening’, usually felt by the mother between 17-20 weeks o domestic abuse ▪ During pregnancy, the reported incidence of physical abuse ranges from 4% to 30% (CDC, 2013a), and up to 45% of victims of intimate partner abuse before pregnancy continue to be abused during the pregnancy ▪ Ask if mother feels safe going home ▪ Always report suspected abuse o recreation drug use ▪ Women may use a number of defenses to emotionally deal with abuse. One method may involve the use of recreational drugs. it is estimated that approximately 3% of pregnant women use nonprescription drugs such as cocaine, amphetamines, heroin, marijuana, or ecstasy. Illegal or recreational drug use can have a number of detrimental effects on maternal and fetal health during pregnancy-see chart below: • o nausea and vomiting ▪ Nausea and vomiting of pregnancy, or “morning sickness,” occurs because of high levels of hCG and relaxation of the stomach, esophagus, and gastroesophageal sphincters. o hormonal changes ▪ Estrogen and progesterone are the major hormones produced by the placenta during pregnancy. The effect of estrogen is one of “growth”; the effect of progesterone is one of “maintenance.” ▪ Estrogen prompts hyperplasia and hypertrophy (growth of cells in number and size) during pregnancy. Because of the effects of estrogen, breast tissue enlarges and becomes functional and the uterus expands, a process that allows for stretching of the muscles to accommodate the growing fetus. Estrogen also enhances uterine contractility to prepare the muscles for labor. ▪ Progesterone enables the pregnancy to thrive by its relaxation effect on the smooth muscle. Progesterone causes vasodilation and an increased blood flow to all body tissues, it slows the gastrointestinal tract to ensure absorption of essential nutrients for fetal development, and it relaxes the uterine muscle to prevent the onset of labor until term. o Fundal heights ▪ Fundal height should match the woman’s gestational age. Example: if she is 17 weeks pregnant fundal height should measure 17cm o Chadwick's sign : discoloration, or bluish purple hue, that appears on the cervix, vagina, and vulva-early sign of pregnancy o Goodell's sign: cervical softening o Signs and symptoms that a women should report ▪ 1st trimester: Severe vomiting, Abdominal cramping and vaginal spotting or bleeding, any signs of infection- chills, fever, malaise, and anorexia, burning on urination ▪ 2nd tri: headache, vision changes, elevated blood pressure, edema, change in vaginal discharge, uterine contractions, absence of fetal movements ▪ 3rd tri: vaginal bleeding with or without abdominal pain, uterine contractions, absence of fetal movements o Cardiovascular changes ▪ As growth of the fetus exerts pressure on the diaphragm, the maternal heart is pushed upward and laterally to the left ▪ Cardiac hypertrophy results from the increased blood volume and cardiac output - the woman may experience palpitations, chest pain, shortness of breath, or a decreased tolerance to activity o Musculoskeletal changes ▪ As the pregnancy progresses, the abdominal wall weakens, and the rectus abdominis muscles separate (diastasis recti) to accommodate the growing uterus. As the weight of the uterus shifts upward and outward, a lumbar lordosis (anterior convexity of the lumbar spine) develops. Low back pain usually accompanies this physiological change. ▪ Relaxin, a hormone produced by the placenta, along with the action of progesterone, causes a relative laxity of the ligaments. The pubis symphysis separates at approximately 28 to 30 weeks gestation. These changes, coupled with the change in the maternal center of gravity, result in an unsteady gait and a greater tendency toward falls. ▪ Pregnant women frequently complain of sharp pain in the lower abdominal quadrants or in the groin area. Most often, the pain is related to stretching and hypertrophy of the round ligaments that support the uterus (round ligament pain) ▪ The activity of calcitonin, coupled with adequate nutrition, protects the maternal skeleton from a loss of bone density despite an increase in the turnover of bone mass. ▪ cramping in the lower extremities and calves, especially at night- caused by poor circulation and imbalances in calcium and phosphorus. o Fetal Heart Tones ▪ The fetal heart rate (FHR) is heard most clearly directly over the fetal upper back (the maternal right or left lower abdominal quadrants) in a vertex presentation. The intensity of the fetal heart tones (FHT) varies according to the fetal position (Fig. 9- 7). With a breech presentation, the fetal heart tones may be best heard in the patient's right or left upper abdominal quadrants. ▪ The normal heart rate for a fetus is approximately 110 to 160 beats per minute (bpm). ▪ With the Doppler stethoscope, FHT may be auscultated by 10 to 12 weeks or by 17 to 19 weeks with the fetal stethoscope. o Skin changes during pregnancy ▪ Estrogen, progesterone, and alpha-melanocyte-stimulating hormones cause many changes in the appearance, structure, and function of the integumentary system. ▪ pigmentation changes related to estrogen. Moles (nevi), freckles, and recent scars may darkenor multiply. The nipples, areolae, axillae, vulvar area, and perineum also darken in color. ▪ The linea alba, a light line that extends from the umbilicus to the mons pubis (and sometimes upward to the xiphoid process), darkens, becoming the linea nigra ▪ Melasma gravidarum, also known as chloasma, forms the “mask of pregnancy”. This dark, blotchy brownish pigmentation change occurs around the hairline, brow, nose, and cheeks and often gives the appearance of “raccoon eyes.” ▪ During pregnancy the skin becomes photosensitive, and sunburn may occur in a shorter exposure time than usual for the individual. ▪ Increased adrenal steroid levels can cause striae gravidarum, or “stretch marks,” on the breasts, buttocks, thighs, and abdomen ▪ Increased levels of estrogen during pregnancy may cause • Angiomas, also called “vascular spiders,” are tiny, bluish, end-arterioles that occur on the neck, thorax, face, and arms. They may appear as star-shaped or branched structures that are slightly raised and do not blanch with pressure • Palmar erythema is a condition characterized by color changes over the palmar surfaces of the hands- presents as a diffuse, reddish-pink mottling of the palms. • Fertilization process o After completion of the first meiotic division, the secondary oocyte is expelled from the ovary during ovulation. The oocyte then makes its way to the infundibulum (funnel-shaped passage) at the end of the fallopian tube and passes into the ampulla of the tube. Sperm must undergo a process called capacitation, whereby a glycoprotein coat and seminal proteins are removed from the surface of the sperm's acrosome (the caplike structure surrounding the head of the sperm). The sperm become more active during this process of capacitation, which takes about 7 hours and usually occurs in the fallopian tube but may begin in the uterus. Once a sperm penetrates through the zona pellucida, a reaction takes place to prevent fertilization by other sperm. The oocyte then undergoes its second meiotic division and forms a mature oocyte and secondary polar body. The nucleus of the mature oocyte becomes the female pronucleus. The sperm loses its tail within the cytoplasm of the oocyte and then enlarges to become the male pronucleus. Fusion of pronuclei of both the oocyte and sperm create a single zygote containing the diploid number of chromosomes. The zygote is genetically unique in that it contains half of its chromosomes from the mother and half from the father. o After conception, the fertilized ovum, or zygote, remains in the ampulla for 24 hours and then, propelled by ciliary action, travels toward the uterus. During this time, cleavage (mitotic cell division of the zygote) occurs. By 3 to 4 days after fertilization, there are approximately 16 cells. The zygote is now called a morula and enters the uterus. Once the morula enters the uterus, fluid passes through the zona pellucida into the intercellular spaces of the inner cell mass and forms a large fluid-filled cavity. The morula is now called a blastocyst and contains an inner mass of cells called the embryoblast. The embryo develops from the embryoblast and contains an outer cell layer called the trophoblast. The chorion and placenta develop from the trophoblast. The uterus secretes a mixture of lipids, mucopolysaccharides, and glycogen that nourishes the blastocyst. The zona pellucida degenerates approximately 5 to 6 days after fertilization. This process allows the blastocyst to adhere to the endometrial surface of the uterus • GTPAL o G Gravida o T Number of Term pregnancies o P Number of Preterm deliveries o A Number of Abortions, both spontaneous and induced o L Number of Living children • Naegel’s Sign (rule?) o Naegele's rule is used to calculate the Expected Date of Birth (EDB)— Expected Date of Delivery (EDD). This calculation is based on the first day of the woman's last normal period. 7 days are added to the LMP, 3 months subtracted, and where necessary a year added. For example, if the woman's LMP was June 8, 2014 o Add 7 days = June 15, 2014 o Subtract 3 months = March 15, 2014 o Add a year = March 15, 2015; EDB = March 15, 2015 o (An alternative way is to add 7 days and then add 9 months + year where needed.) • Preconception counseling o purpose of it o goal o Gestational diabetes • Prenatal testing – blood work completed o A screening test: ▪ Identifies patients at increased risk for developing a disorder or disease ▪ Identifies patients who need diagnostic testing o A diagnostic test: ▪ Confirms the presence of a disorder or disease o Non-stress test ▪ nonstress test (NST) may be ordered to provide an evaluation of the FHR in response to fetal movement and/or uterine activity. A reactive test (the desirable result), is one in which the heart rate accelerates by at least 15 beats per minute for at least 15 seconds, with at least three “acceleration episodes” in a 20-minute period of monitoring ▪ It is important to remember that a reactive nonstress test is only an indicator of the fetus's present condition rather than a test that can be used to predict future fetal well-being. o Stress test ▪ The contraction stress test (CST) evaluates the FHR response to uterine contractions. ▪ The test is considered negative (normal) if there is no evidence of late or significant variable decelerations. A positive CST (abnormal) is one in which there are late decelerations with 50% of contractions, even if the frequency is less than three in 10 minutes. CSTs are evaluated according to the presence or absence of late FHR decelerations. A late deceleration, associated with fetal hypoxia, is one that begins at the peak of the contraction and persists after the conclusion of the contraction. ▪ Contraindications: Patients who have experienced third trimester bleeding from placenta previa or marginal abruptio placentae, women who have had extensive uterine surgery (including c-section), those at high risk for preterm labor, and those with PROM are not candidates for a CST o Toxoplasmosis ▪ Associated with consumption of infested undercooked meat and poor hand washing after handling cat litter. Fetal infection occurs if the mother acquires toxoplasmosis after conception and passes it to the fetus via the placenta. Most infants are asymptomatic at birth but develop symptoms later. • Maternal Effects o Flu-like symptoms in the acute phase. • Fetal/Neonatal Effects o Miscarriage likely in early pregnancy. In neonates, CNS lesions can result in hydrocephaly, microcephaly, chronic retinitis, and seizures. Retinochoroiditis may appear in adolescence or adulthood. o Quad(ruple) Marker Screen ▪ Done between 15-20weeks gestation ▪ SCREENS (tests tells you how likely it is your baby will have a defect) for Down syndrome and trisomy 18, which are chromosomal abnormalities, as well as neural tube defects, such as spina bifida. ▪ If it is abnormal, doctor can offer a DIAGNOSTIC test that would confirm any abnormality o Lab screening done by trimesters (more info on page 286) ▪ First trimester combined screen: Nuchal translucency (NT) testing + pregnancy- associated plasma protein-A (PAPP-A) + free beta-human chorionic gonadotropin (free β-hCG) • NT: Fetal ultrasound examination performed between 11 and 14 weeks of pregnancy. Increased NT (>3 mm), elevated maternal serum free β-hCG and reduced PAPP-A suggest aneuploidy (e.g., trisomy 13 [Patau syndrome], trisomy 18 [Edwards’ syndrome], and trisomy 21 [Down syndrome] and Turner's syndrome [gonadal dysgenesis]). • When these findings are present, offer genetic counseling, and chorionic villus sampling, or amniocentesis. • When combined screening results are all negative, offer second trimester maternal serum alpha-fetoprotein testing to screen for neural tube defects. ▪ Second trimester: Maternal serum α-fetoprotein (MSAFP) screening • May be performed between 14th and 22nd weeks of pregnancy but most accurate during the 16th to 18th weeks. Higher than normal levels may be indicative of an open neural tube defect but may also result from incorrect dates, multiple gestation, or fetal demise. • Lower than normal levels may indicate that the woman is at risk for trisomy 18 or trisomy 21. ▪ Triple screen: maternal serum alpha-fetoprotein (MSAFP) + unconjugated estriol (uE3) + free beta-human chorionic gonadotropin (free β-hCG) Quadruple screen: Triple screen biochemical markers plus measurement of inhibin A • Lower than normal levels of unconjugated estriol and higher than normal levels of free β-hCG and inhibin-A (included in the quadruple screen) may indicate that a woman is at risk for trisomy 18 or trisomy 21. • Pregnancy female organs and structure o Vagina, uterus, cervix, ovaries, fallopian tubes • Fetal development (good chart on page 204) o Week 1: Fertilization occurs and the blastocyst is superficially implanted by the end of the first week. o Week 2: The yolk sac develops, the amniotic cavity appears, and the embryoblast differentiates into the bilaminar embryonic disk. Implantation of the blastocyst is completed. o Week 3: Characterized by the appearance of a primitive streak, the development of the notochord, and differentiation of the three germ layers: embryonic ectoderm (outer layer, gives rise to skin, teeth, and glands of the mouth and nervous system), endoderm (inner layer, gives rise to epithelium of the respiratory, digestive, and genitourinary tracts), and mesoderm (lies between the ectoderm and endoderm; gives rise to the connective tissue) o Week 4: four limb buds and a closed otic vesicle (later develops into labyrinth of inner ear) are present, development of the nervous system is well under way. A thickened portion of the ectoderm develops into the neural plate. The top portion will differentiate into the neural tube, which forms the central nervous system (brain and spinal cord) and the neural crest, which will develop into the peripheral nervous system. Later, the eye and inner ear develop as projections of the original neural tube. o Week 8: clear distinction between the upper and lower limbs; the external genitals are well developed, main organ systems have also begun to develop by the end of 8 weeks. Except for the cardiovascular system, however, there is minimal function of most of the organ systems. o Week 9 (fetal period)-12: The fetal head is half the length of the crown–rump length at the beginning of the ninth week. The face is recognizably human at 10 weeks. Body growth increases, and as a result, the crown–rump length more than doubles by the twelfth week. Head growth does not keep pace with body growth and slows considerably by the 12th week but remains proportionately large as compared with the rest of the body. Ossification centers appear in the skeleton. The intestines leave the umbilical cord and enter the abdomen. The external genitalia differentiate and are distinguishable by week 12. At 9 weeks, the liver serves as the major site for red blood cell production (erythropoiesis). However, by 12 weeks, the spleen begins to take over this process. Urine production commences between 9 and 12 weeks. o Weeks 13-16: Ossification of the skeleton takes place, and the bones become clearly visible on ultrasound examination. The external genitalia are recognizable by 12 to 14 weeks, the ovaries are differentiated, and the primordial (primitive) ovarian follicles are present by 16 weeks. o Weeks 17-20: Growth continues but slows during this period. Maternal awareness of fetal movements (quickening) is frequently reported during this time. The skin is now covered with a thick, cheese-like material called vernix caseosa that protects the fetal skin from exposure to the amniotic fluid. By 20 weeks, hair appears on the eyebrows and head. Fine downy hair (lanugo) is usually present by 20 weeks and covers all parts of the body except the palms, soles, or areas where other types of hair are usually found. Subcutaneous deposits of brown fat, used by the newborn for heat production, help to make the skin less transparent in appearance. The fetal uterus is formed at 18 weeks in females, and in males, the testes have begun to descend but are still located in the abdominal wall. o Weeks 21-25: The fetus gains much weight during this time. Rapid eye movements begin at 21 weeks. By 24 weeks, the fetus has fingernails, and the lungs have begun to secrete surfactant o Weeks 26-29: A fetus may survive if born during this time because the lungs can breathe air, and the central nervous system can regulate body temperature and direct rhythmic breathing. The eyelids are open, the toenails are evident, and subcutaneous fat is present under the skin. Erythropoiesis occurs in the spleen but ends at 28 weeks when the bone marrow takes over that function. o Weeks 30-34: pupillary light reflex is present. o Weeks 35-40: the fetus has a strong hand grasp reflex and orientation to light. • Placenta o Role ▪ prepare the breasts structurally for lactation by promoting growth of the ducts and secretory cells. ▪ responsible for providing oxygenation, nutrition, waste elimination, and hormones necessary to maintain the pregnancy ▪ plays an important role in protecting the fetus from pathogens and in preventing maternal rejection of the pregnancy. o risk factors for poor placental perfusion ▪ Any time blood flow to placenta is compromised: preeclampsia, placenta previa, infarction, retroplacental hematoma, septal cysts, calcification, thrombosis, tumors, villous edema, acute and chronic villitis, and umbilical cord abnormalities ▪ Certain physical positions also inhibit blood flow such as lifting from a supine position or doing the Valsalva maneuver (holding your breath) o Fetal circulation ▪ There are three shunts unique to fetal circulation: 1. Some blood circulates through the liver, but most bypasses the liver through the ductus venosus and enters the inferior vena cava. 2. Blood from the superior vena cava enters the right atrium, passes through the foramen ovale, through the right ventricle, and into the aorta supplying blood to the head and upper and lower extremities. 3. Blood returning from the head enters the right atrium and then flows through the right ventricle and into the pulmonary artery. Most of this blood bypasses the lungs through the ductus arteriosus. A small amount of blood flows through the pulmonary circulation, back into the right atrium, right ventricle, and then into the aorta. ▪ Blood travels through the fetus in a unique way. The umbilical cord contains three vessels: two arteries and one vein. Blood flows through the vein from the placenta to the fetus. A small amount of blood flows through the liver and then empties into the inferior vena cava. Most of the blood bypasses the liver and then enters the inferior vena cava by way of the ductus venosus, a vascular channel that connects the umbilical vein to the inferior vena cava. The blood then empties into the right atrium, passes through the foramen ovale (an opening in the septum between the right and left atria) into the left atrium, then moves into the left ventricle and on into the aorta. From the aorta, blood travels to the head, upper extremities, and lower extremities. Blood returning from the head enters the superior vena cava, then the right atrium and the right ventricle before entering the pulmonary artery. Most of the blood that enters the pulmonary artery bypasses the lungs and enters the aorta through the ductus arteriosus, a vascular channel between the pulmonary artery and descending aorta. The remaining blood flows to the pulmonary circulation to support lung development. The blood then returns through the pulmonary vein to the left atrium, the left ventricle, to the aorta, and returns to the placenta through the two arteries. Most of the blood in the lower extremities enters the internal iliac artery and the umbilical arteries to the placenta to be reoxygenated and recirculated. Some of the blood in the lower extremities passes back to the ascending vena cava and is mixed with oxygenated blood from the placenta without being oxygenated. • discomforts of pregnancy-nausea, vomiting, fatigue, urinary frequency, nocturia, dyspepsia, gum bleeding, dependent edema, leg varicosities, SOB, numbness/tingling of fingers, supine hypotensive syndrome, flatulence, constipation, insomnia, leg cramps, round ligament pain, nasal congestion, back pain, ptyalism (hypersalivation), leukorrhea (vaginal discharge) o nursing education ▪ nausea, acid reflux: eat small frequent meals and avoid ‘trigger foods’, remain in upright position after eating ▪ fatigue: take naps, get daily exercise ▪ nasal congestion: take hot showers, use humidifier ▪ vaginal discharge: wear cotton underwear, avoid tight clothing, use panty liner ▪ urinary frequency: encourage kegel exercises ▪ constipation: encourage high-fiber diet, increase fluids, get exercise, avoid straining ▪ leg cramps: dorsiflex the foot (point toes toward belly), get adequate calcium and phosphorus ▪ edema/leg varicosities: raise legs several times a day, avoid crossing legs, use compression stockings ▪ flatulence: avoid chewing gum/swallowing air, and gassy foods ▪ insomnia: encourage relaxation ▪ round ligament pain: take a warm bath, apply heat, support uterus with pillow ▪ SOB: maintain good posture, stretch arms above head o nursing interventions ▪ Administer antiemetic, IV fluids, reposition client • Amniotic fluid o Purpose ▪ Amniotic fluid is vital for fetal growth and development. It cushions the fetus and protects against mechanical injury, helps the fetus to maintain a normal body temperature, allows for symmetrical fetal growth, prevents adherence of the amnion to the fetus, and aids in fetal musculoskeletal development by providing freedom of movement. It is essential for normal fetal lung development. o Oligohydramnios ▪ decreased amniotic fluid o Polyhydramnios ▪ Increased amniotic fluid o Newborn cord (umbilical cord) ▪ Used for blood flow to and from baby • medications used in pregnancy and nursing interventions o prenatal supplements o preterm labor meds and treatment ▪ Tocolysis is the use of medications (“tocolytics”) to inhibit uterine contractions ▪ Women at risk for preterm labor may benefit from progesterone supplementation: Micronized progesterone vaginal gel or suppositories (every night from weeks 16 to 20 through 36) may reduce preterm labor, especially in women with a history of preterm birth and a short CL verified by vaginal ultrasound ▪ progesterone supplementation o pre-eclampsia treatment ▪ Preeclampsia is a pregnancy-specific systemic syndrome clinically defined as an increase in blood pressure (i.e., systolic and diastolic blood pressures greater than or equal to 140 and greater than or equal to 90 mm Hg, respectively, occurring twice, 4 hours apart) after 20 weeks’ gestation accompanied by proteinuria (excretion of greater than or equal to 300 mg protein/24 hours o Rhogam- Rh(D)-negative woman: Check for Rh antibodies and if negative, 300 mcg of Rho(D) immune globulin (RhoGAM) is prescribed at 28–32 weeks’ gestation. • Female health concerns, education and nursing interventions o Dysmenorrhea- painful menstruation that interferes with daily activities ▪ relaxation and breathing techniques, the use of heat to reduce uterine contractions and increase blood flow to the uterine tissues, exercise or rest, and the use of nonsteroidal anti-inflammatory drugs to inhibit the synthesis of prostaglandin o Emergency contraception ▪ Plan B-does not cause miscarriage o Self-breast exams ▪ Should be done monthly, convenient to do in the shower o Contraception – both non hormonal and hormone ▪ Non hormonal-abstinence, condoms, contraceptive sponge, coper IUD, tube tying ▪ Hormonal: oral contraception (synthetic estrogen), transdermal patch, vaginal ring, IUD, depo shot, subdermal implant o HPV treatment ▪ Several topical chemical agents are available for the treatment of external genital warts. These include trichloroacetic acid (TCA) or bichloroacetic acid (BCA) and podophyllin resin (provider administered) and podofilox gel or solution 0.5% (Condylox), sinecatechins ointment 15% (Veregen) (green tea extract), and imiquimod cream 5% (Aldara, Zyclara), which are patient administered. Cryotherapy (freezing), CO2 laser surgery, electrosurgery, and surgical removal are other treatment options, depending on the severity of the lesions and resistance to treatment • problems during pregnancy, s/s, risk factors, nursing interventions, treatment education o Abruption ▪ Placental abruption (abruptio placentae) is the premature separation of a normally implanted placenta from the decidual lining of the uterus after 20 weeks’ gestation. An abruption results in hemorrhage between the uterine wall and the placenta. There are three grades: • Grade 1: Slight vaginal bleeding and some uterine irritability are usually present. Maternal blood pressure is unaffected, and the maternal fibrinogen level is normal. The fetal heart rate pattern is normal. • Grade 2: External uterine bleeding is absent to moderate. The uterus is irritable and tetanic, or very frequent contractions may be present. Maternal blood pressure is maintained, but the pulse rate may be elevated and postural blood volume deficits may be present. The fibrinogen level may be decreased. The fetal heart rate pattern often shows signs of fetal compromise. • Grade 3: Bleeding is moderate to severe but may be concealed. The uterus is tetanic and painful. Maternal hypotension is frequently present, and fetal death has occurred. Fibrinogen levels are often reduced or are less than 150 mg/dL; other coagulation abnormalities (e.g., thrombocytopenia and factor depletion) are present. ▪ Risk factors include maternal hypertension (chronic, gestational, preeclampsia/eclampsia), cigarette smoking, multiparity, abortions (spontaneous, elective), illicit drug use (cocaine, methamphetamine), short fetal umbilical cord, maternal abdominal trauma, rupture of the membranes, and uterine leiomyoma (fibroids) located behind the placenta ▪ S/S: The classic presenting sign is third-trimester bleeding associated with severe abdominal pain. Other signs include uterine tenderness and abdominal or back pain, a boardlike abdomen and no vaginal bleeding, abnormal contractions and increased uterine tone, fetal compromise as evidenced by late fetal heart rate (FHR) decelerations, bradycardia and lack of variability on the electronic fetal monitor, and fetal demise. ▪ Interventions: • Hospitalization, IV placement, Labwork • Betamethasone may be given to the woman to promote fetal lung maturity when delivery is not imminent. • Rh(D)-negative patients should receive RhoGAM to prevent isoimmunization. • Continuous evaluation of intake and output, electronic fetal monitoring • C-section • Nursing care is centered on continuous maternal–fetal assessment, with ongoing information and emotional support for the patient and her family. o Previa - Placenta previa is an implantation of the placenta in the lower uterine segment, near or over the internal cervical os ▪ Risk factors: prior cesarean birth or previous abortions with curettage, large placental mass as seen in multiple gestations, diabetes, and erythroblastosis fetalis. Other risk factors include smoking, cocaine use, a prior history of placenta previa, closely spaced pregnancies, African or Asian ethnicity, and maternal age greater than 40 years ▪ S/S: painless vaginal bleeding-bright red ▪ Tx: Stabilization involves the administration of IV fluids and a laboratory work-up. A blood type and crossmatch should be obtained in anticipation of the need for a transfusion. Administer rhogam if appropriate. The patient is placed on bedrest and the fetus is continuously assessed by electronic fetal monitoring. If time permits, betamethasone (a long-acting corticosteroid) may be administered (to the woman) to promote fetal lung maturity. Labor that cannot be halted, fetal compromise, and life-threatening maternal hemorrhage are indications for immediate delivery regardless of gestational age ▪ Nursing intervention: Nurses can help decrease anxiety by speaking calmly to the patient and her support persons; carefully explaining her condition (using pictures, images, and other resources of the health-care team); describing planned interventions and why they are being performed; providing preparatory educational videotapes and reading materials regarding pregnancy, childbirth, infant care, and postpartum self-care; and offering reassurances and instructions for home care o Preterm labor- Preterm labor (PTL) is defined as cervical changes and regular uterine contractions occurring between 20 and 37 weeks of pregnancy. ▪ Risk factors: History of preterm birth, especially in the second trimester, Preterm premature rupture of the membranes (PPROM), Uterine or cervical anomalies, Multiple gestation, Hypertensive disorders of pregnancy, Diabetes, Low prepregnancy weight, Clotting disorders, Bacterial infections, Fetal anomalies, Uterine overdistension (e.g., multiple gestation, hydramnios), bleeding, especially in the second trimester or in more than one trimester, Late or no prenatal care, Alcohol or drug use, Smoking, Cervical injury (e.g., related to surgery or elective abortion, Diethylstilbestrol (DES) exposure, Trauma including intimate partner violence, Non-Hispanic African American race, Maternal age extremes (i.e., less than 16 years or greater than 40 years), Low socioeconomic and educational status, Stress, Long working hours with long periods of standing, Periodontal disease ▪ S/S: backache, pelvic aching, menstrual-like cramps, increased vaginal discharge, pelvic pressure, urinary frequency, and intestinal cramping with or without diarrhea. ▪ Criteria to meet preterm labor: • A gestation of 20 to 37 weeks • Documented persistent uterine contractions (4 every 20 minutes or 8 in 1 hour) • Documented cervical effacement of 80% or greater • Cervical dilation of more than 0.4 in. (1 cm) or a documented change in dilation ▪ Tx: Tocolysis is the use of medications (“tocolytics”) to inhibit uterine contractions, delivery of baby. antenatal corticosteroids for improvement of neonatal outcomes ▪ Nursing interventions: administer medications, educate mother on what is happening, continuous fetal monitoring, monitor moms vitals, position mom on her side for better placenta perfussion o Hyperemesis-extreme vomiting o Preeclampsia- Preeclampsia is a pregnancy-specific systemic syndrome clinically defined as an increase in blood pressure (i.e., systolic and diastolic blood pressures greater than or equal to 140 and greater than or equal to 90 mm Hg, respectively, occurring twice, 4 hours apart) after 20 weeks’ gestation accompanied by proteinuria (excretion of greater than or equal to 300 mg protein/24 hours ▪ Risk factors: Primigravida, Age extremes, Pregestational diabetes, Preexisting hypertension, renal disease, or collagen disease, Multiple gestation, Fetal hydrops, Hydatidiform mole, Preeclampsia in a previous pregnancy, Family history, Obesity, Periodontal disease, Antiphospholipid antibody syndrome, Rh incompatibility, African American ethnicity, Pregnancies that result from donor insemination, oocyte donation, embryo donation ▪ S/S: high BP, proteinuria ▪ Tx: delivery is only cure, may be managed at home for minor cases ▪ Nursing interventions: If the woman's blood pressure and laboratory test results indicate that her care may be safely managed at home, the nurse must make certain that the patient fully understands the signs and symptoms associated with a worsening of the condition. o HELLP- Hemolysis and Elevated Liver enzymes and Low Platelet levels. It is a rare (5% of women with preeclampsia), serious complication of preeclampsia that can manifest itself at any time during pregnancy and the puerperium. It causes rapidly deteriorating liver function and thrombocytopenia. ▪ S/S: This pathological process progresses to the development of a subcapsular hepatic hematoma and subsequent liver rupture. Other maternal signs and symptoms include malaise with influenza-like complaints, nausea or vomiting, headache, shoulder pain, and bruising or hematuria, epigastric pain ▪ Tx: Therapy for HELLP syndrome centers on improving the platelet count by transfusion of fresh-frozen plasma or platelets and delivery as soon as feasible by vaginal or cesarean birth. Intrapartum nursing care involves continuous maternal– fetal monitoring. Measurement of central venous pressure or pulmonary arterial wedge pressure (Swan–Ganz catheter) may be required to monitor fluid status accurately when pulmonary edema or acute renal failure is present o Hyperthyroidism ▪ S/S: (appear in normal pregnancy: heat intolerance, diaphoresis, fatigue, anxiety, emotional lability, tachycardia, and a wide pulse pressure). However, weight loss, tachycardia greater than 100 beats per minute, and diffuse goiter (enlargement of the thyroid gland) are clinical features suggestive of hyperthyroidism ▪ Tx: Treatment for hyperthyroidism includes the use of antithyroid medications such as the thioamides, propylthiouracil (PTU—the drug of choice), or methimazole (Tapazole) ▪ Nursing Interventions: When caring for patients with hyperthyroidism, it is important that the nursing assessment include the maternal pulse rate (less than 100 bpm), reflexes (2+ to 3+), weight gain, and fetal growth. Patient education should focus on complications of antithyroid therapy (i.e., purpuric skin rash, pruritus, fever, and nausea) and dietary needs (i.e., increased calories and protein) o Gestational Diabetes including Complications to newborn- GDM is an impairment in carbohydrate metabolism that first manifests during pregnancy. ▪ Risk factors: Women older than age 25 years, Obesity, Insulin resistance, Polycystic ovary syndrome, History of pregnancy-related diabetes mellitus, History of a large for gestational age infant, hydramnios, stillbirth, miscarriage, or an infant with congenital anomalies during a previous pregnancy, Family history of type 2 diabetes (first-degree relative), Ethnicity ▪ infant at risk for: macrosomia (large body size), congenital anomalies, birth trauma, perinatal asphyxia, respiratory distress syndrome, hypoglycemia, hypocalcemia, cardiomyopathy, hyperbilirubinemia, and polycythemia. ▪ Risk for mother: also increases the risk for cesarean birth and maternal preeclampsia. Preeclampsia is a condition associated with a decreased blood supply to the maternal organs and to the developing fetus and may result in preterm birth, premature rupture of membranes, maternal organ damage, thrombocytopenia, IUGR, and an altered acid-base balance in the fetus o Ectopic pregnancy- fertilized egg implants outside the uterine cavity. Implantation may occur in the fallopian tube (99%), on the ovary, on the cervix, on the outside of the fallopian tube, on the abdominal wall, or on the bowel ▪ Risk factors: History of sexually transmitted infections or pelvic inflammatory disease, Prior ectopic pregnancy, Previous tubal, pelvic, or abdominal surgery, Endometriosis, Current use of exogenous hormones (e.g., estrogen and progesterone), Use of an intrauterine device, In vitro fertilization or other method of assisted reproduction, In utero diethylstilbestrol (DES) exposure with abnormalities of the reproductive organs ▪ S/S: vaginal bleeding, a missed period, or abdominal tenderness or pain ▪ Tx: Methotrexate, a chemotherapeutic drug and folic acid inhibitor that stops cell production and destroys remaining trophoblastic tissue, is used in the management of uncomplicated, non–life-threatening ectopic pregnancies. Salpingectomy (removal of the ruptured fallopian tube) by laparotomy (surgical procedure in which the abdomen is opened to visualize the abdominal organs) o IUGR- intrauterine growth restriction also known as fetal growth restriction, refers to the inability of a fetus to achieve full growth potential while in utero ▪ Risk factors: IUGR may be related to genetic factors, congenital anomalies, infection, multiple gestation, maternal malnutrition, environmental toxins, placental factors, and maternal vascular disease related to medical conditions ▪ Tx: centers on ensuring fetal well-being and determining the optimal timing for delivery - [Show More]
Last updated: 1 year ago
Preview 1 out of 16 pages
 (1).png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 23, 2021
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
Oct 23, 2021
Downloads
0
Views
26



.png)