nderstanding Pathophysiology 7th Edition Test Bank
Document Content and Description Below
Understanding Pathophysiology 7th Edition Test Bank Chapter 1. Cellular Biology MULTIPLE CHOICE 1. A student is observing a cell under the microscope. It is observed to have supercoiled DNA... with histones. Which of the following would also be observed by the student? a. A single circular chromosome b. A nucleus c. Free-floating nuclear material d. No organelles ANS: B The cell described is a eukaryotic cell, so it has histones and a supercoiled DNA within its nucleus; thus, the nucleus should be observed. A single circular chromosome is characteristic of prokaryotic cells, which do not have histones. Free-floating nuclear material describes a prokaryotic cell, which would not have a distinct nucleus. Eukaryotic cells have membrane bounded cellular components called organelles. No organelles describes a prokaryotic cell. 2. A nurse is instructing the staff about cellular functions. Which cellular function is the nurse describing when an isolated cell absorbs oxygen and uses it to transform nutrients to energy? a. Metabolic absorption b. Communication c. Secretion d. Respiration ANS: D The ability of the cell to absorb oxygen refers to the cells function of respiration. The ability of the cell to function within a society of cells refers to its function of communication. The ability of the cell to take in nutrients refers to the cells function of metabolic absorption. The ability of the cell to synthesize new substances and secrete these elsewhere refers to the cells function of secretion. 3. A eukaryotic cell is undergoing DNA replication. In which region of the cell would most of the genetic information be contained? a. Mitochondria b. Ribosome c. Nucleolus d. Nucleus ANS: C The region of the cell that contains genetic material, including a large amount of ribonucleic acid, most of the DNA, and DNA-binding proteins, is the nucleolus. The mitochondria is the site of cellular respiration. The ribosomes are involved in manufacturing of proteins within the cell. The nucleus contains the nucleolus, and it is the nucleolus that contains genetic material. 4. The fluid mosaic model for biologic membranes describes membrane behavior. According to this model, which of the following float singly or as aggregates in the fluid lipid bilayer? a. Peripheral membrane proteins b. Integral membrane proteins c. Glycoproteins d. Cell adhesion molecules ANS: B Integral membrane proteins float freely in the fluid lipid bilayer. Peripheral membrane proteins are not embedded in the layer, but reside at the surface. Glycoproteins act as cell surface markers. Cell adhesion molecules are on the outside of the membrane and allow cells to hook together. 5. Which of the following can bind to plasma membrane receptors? a. Oxygen b. Ribosomes c. Amphipathic lipids d. Ligands ANS: D Ligands are specific molecules that can bind with receptors on the cell membrane. Oxygen moves by diffusion; it does not bind to receptors. Ribosomes make proteins and are not involved in binding. Amphipathic lipids are a portion of the cell membrane. 6. A nurse is reviewing a report from a patient with metastatic cancer. What finding would support the diagnosis of metastatic cancer? Alterations in extracellular matrix that include: a. Decreased fibronectin b. Increased collagen c. Decreased elastin d. Increased glycoproteins ANS: A Reduced amounts of fibronectin are found in some types of cancerous cells, allowing cancer cells to travel, or metastasize. Collagen provides strength, and its breakdown is associated with osteoarthritis, not cancer. Elastin is found in the lungs and allows tissues to stretch; it is not associated with cancerous cells. Decreased, not increased, glycoproteins are associated with cancerous cells. 7. Which form of cell communication is used to relate to other cells in direct physical contact? a. Cell junction b. Gap junction c. Desmosomes d. Tight junctions ANS: A Cell junctions hold cells together and permit molecules to pass from cell to cell. Gap junctions allow communication from the inside of one cell to the inside of another. Desmosomes are not involved in communication, but allow cells to hold together. Tight junctions are barriers that prevent movement of some substances and leakages of others. 8. Pancreatic beta cells secrete insulin, which inhibits secretion of glucagon from neighboring alpha cells. This action is an example of which of the following signaling types? a. Paracrine b. Autocrine c. Neurohormonal d. Hormonal ANS: A Paracrine signaling involves the release of local chemical mediators that are quickly taken up, destroyed, or immobilized, as in the case of insulin and the inhibition of the secretion of glucagon. When cells produce signals that they themselves respond to, autocrine signaling is used. Neurohormonal signaling involves secretion of hormones into the bloodstream by neurosecretory hormones. Hormonal signaling involves specialized endocrine cells that secrete hormone chemicals released by one set of cells that travel through the tissue through the bloodstream to produce a response in other sets of cells. 9. In cellular metabolism, each enzyme has a high affinity for a: a. Solute b. Substrate c. Receptor d. Ribosome ANS: B Each enzyme has a high affinity for a substrate, a specific substance converted to a product of the reaction. Solutes are small particles that pass through the cell membrane. A receptor is a site on the cell wall that allows transport into the cell. Ribosomes are located inside the cell and are not related to the work of enzymes. 10. An athlete runs a marathon, after which his muscles feel fatigued and unable to contract. The athlete asks the nurse why this happened. How should the nurse respond? A deficiency in can cause impaired muscle contraction. a. GTP b. AMP c. ATP d. GMP ANS: C The cell uses ATP for muscle contraction. when it is deficient, impaired muscle contraction results. GTP is involved in cell signaling, not muscle contraction. AMP is not involved in muscle contraction. GMP is not involved in muscle contraction. 11. Which phase of catabolism produces the most ATP? a. Digestion b. Glycolysis c. Oxidation d. Citric acid cycle ANS: D Most of the ATP is generated during the citric acid cycle. Larger molecules are broken down into smaller units during digestion; no ATP is produced during this cycle. During glycolysis, two molecules of ATP are produced from each glucose molecule, but the most ATP is produced during the citric acid cycle. Oxidation is part of the glycolysis process and ATP is produced, but more ATP is produced during the citric acid cycle. 12. A nurse is teaching the staff about the three phases of cellular catabolism. Which of the following should the nurse include? a. Digestion, glycolysis and oxidation, and the citric acid cycle b. Diffusion, osmosis, and mediated transport c. S phase, G phase, and M phase d. Metabolic absorption, respiration, and excretion ANS: A Digestion, glycolysis and oxidation, and the citric acid cycle are the three phases of cellular catabolism. Diffusion, osmosis, and mediated transport are parts of the movement of fluids in and out of cells. The S, G, and M phases are phases of cellular division, not catabolism. Metabolic absorption, respiration, and excretion are functions of the cell. 13. A runner has depleted all the oxygen available for muscle energy. Which of the following will facilitate his continued muscle performance? a. Electron-transport chain b. Aerobic glycolysis c. Anaerobic glycolysis d. Oxidative phosphorylation ANS: C When no oxygen is available, anaerobic glycolysis occurs. The electron-transport chain is part of the citric acid cycle. Aerobic glycolysis involves the presence of oxygen. Oxidative phosphorylation is the mechanism by which the energy produced from carbohydrates, fats, and proteins is transferred to ATP. It is not part of muscle performance. 14. The faculty member asked the student to identify the appropriate term for the movement of small, electrically uncharged molecules through a semipermeable barrier. Which answer indicates the nursing student understood the teaching? a. Osmosis b. Diffusion c. Hydrostatic pressure d. Active transport ANS: B Diffusion is the movement of a solute molecule from an area of greater solute concentration to an area of lesser solute concentration. Osmosis is the movement of water across a semipermeable membrane from a region of higher water concentration to one of lower concentration. Hydrostatic pressure is the force of fluid against a cell membrane. Within the vascular system, this pressure is the blood pressure. In active transport, molecules move up a concentration gradient. This process requires energy. 15. A nurse is teaching a patient about fluid and electrolytes. Which of the following indicates the teaching was successful regarding electrolytes? Electrolytes are: a. Small lipid-soluble molecules b. Large protein molecules c. Micronutrients used to produce ATP d. Electrically charged molecules ANS: D Electrolytes are electrically charged molecules. Electrolytes are not lipid soluble. Electrolytes are not made up of protein. Electrolytes do not have a role in the production of ATP. 16. A nurse is reading a chart and sees the term oncotic pressure. The nurse recalls that oncotic pressure (colloid osmotic pressure) is determined by: a. Concentration of sodium b. Plasma proteins c. Hydrostatic pressure d. Availability of membrane transporter proteins ANS: B Oncotic pressure is determined by the effect of colloids or plasma proteins. The concentration of sodium plays a role in tonicity. Hydrostatic pressure is the force within a vessel. Membrane transporter proteins are involved in active transport within a concentration gradient. 17. A patient has a body fluid of 300 mOsm/kg. This lab result is measuring: a. Osmolality b. Osmolarity c. Osmotic pressure d. Oncotic pressure ANS: A Osmolality measures the number of milliosmoles per kilogram of water, or the concentration of molecules per weight of water. Osmolarity measures the number of milliosmoles per liter of solution, or the concentration of molecules per volume of solution. Osmotic pressure is the amount of hydrostatic pressure required to oppose the osmotic movement of water. Oncotic pressure is from plasma proteins, not body fluids. 18. In teaching a patient with cirrhosis, which information should the nurse include regarding cholesterol? a. Cholesterol decreases the membrane fluidity of the erythrocyte, which reduces its ability to carry oxygen. b. Cholesterol decreases the membrane fluidity of erythrocytes, which reduces its ability to carry hemoglobin. c. Cholesterol increases the membrane fluidity of erythrocytes, which allows binding of excess glucose. d. Cholesterol increases the membrane fluidity of erythrocytes, which prolongs its life span beyond 120 days. ANS: A In cirrhosis, the cholesterol content of the red blood cells plasma membrane increases, causing a decrease in membrane fluidity that seriously affects the cells ability to transport oxygen. In cirrhosis, for example, the cholesterol content of the red blood cells plasma membrane increases, causing a decrease in membrane fluidity that seriously affects the cells ability to transport oxygen, not hemoglobin; the hemoglobin carries the oxygen. In cirrhosis, for example, the cholesterol content of the red blood cells plasma membrane increases, causing a decrease in membrane fluidity that seriously affects the cells ability to transport oxygen; it does not bind excess glucose. In cirrhosis, for example, the cholesterol content of the red blood cells plasma membrane increases, causing a decrease in membrane fluidity that seriously affects the cells ability to transport oxygen. It does not prolong the life of the RBC and could decrease it. 19. A nurse is discussing the movement of fluid across the arterial end of capillary membranes into the interstitial fluid surrounding the capillary. Which process of fluid movement is the nurse describing? a. Hydrostatic pressure b. Osmosis c. Diffusion d. Active transport ANS: A Blood reaching the capillary bed has a hydrostatic pressure of 25 to 30 mm Hg, which is sufficient force to push water across the thin capillary membranes into the interstitial space. Osmosis involves the movement of fluid from an area of higher concentration to an area of lower concentration. It does not involve pressure or force. It is related to hydrostatic pressure. Diffusion is the passive movement of a solute from an area of higher solute concentration to an area of lower solute concentration. Active transport involves movement up a concentration gradient. 20. A patient who has diarrhea receives a hypertonic saline solution intravenously to replace the sodium and chloride lost in the stool. What effect will this fluid replacement have on cells? a. Cells will become hydrated. b. Cells will swell or burst. c. Cells will shrink. d. Cells will divide. ANS: C The hypertonic saline will cause fluid to leave the intracellular space and enter the vascular space, causing cells to shrink. Intravenous hypertonic solutions lead to cell dehydration. Intravenous hypertonic solutions cause fluid to leave cells; thus, they would shrink, not swell. Intravenous hypertonic solutions do not affect cellular division. 21. A nurse is teaching a patient with diabetes how glucose is transported from the blood to the cell. What type of transport system should the nurse discuss with the patient? a. Active-mediated transport (active transport) b. Active diffusion c. Passive osmosis d. Passive-mediated transport (facilitated diffusion) ANS: D A well-known passive-mediated transport system is that for glucose in erythrocytes (red blood cells). The transport of glucose does not require energy, so active-mediated transport is not correct. The transport of glucose does not require energy, so active diffusion is not correct. Osmosis involves the movement of water. 22. How are potassium and sodium transported across plasma membranes? a. By passive electrolyte channels b. By coupled channels c. By adenosine triphosphate enzyme (ATPase) d. By diffusion ANS: C A carrier mechanism in the plasma membrane mediates the transport of ions and nutrients. The best-known pump is the Na+-K+dependent ATPase pump. Electrolyte movements require energy and do not move passively. Enzymes, not electrolytes, are passed via coupled channels. Electrolytes are not transported by diffusion. 23. Why is potassium able to diffuse easily in and out of cells? a. Because potassium has a greater concentration in the intracellular fluid (ICF) b. Because sodium has a greater concentration in the extracellular fluid (ECF) c. Because the resting plasma membrane is more permeable to potassium d. Because there is an excess of anions inside the cell ANS: C The resting membrane is more permeable to potassium because potassium is more easily transported inward. Potassium is greater in concentration in the ICF, but this is not why it is transported more easily. Sodium does have a greater concentration, but this is not why potassium moves easily when the membrane potential is at rest. It is cations, not anions, that are involved in membrane potential activity. 24. The ion transporter that moves Na+ and Ca2+ simultaneously in the same direction is an example of which of the following types of transport? a. Biport b. Uniport c. Antiport d. Symport ANS: D When ions are transported in one direction, it is termed symport. There is no such term as biport. Uniport refers to the movement of a single molecule. Antiport refers to movement of molecules in the opposite direction. 25. During which process can lysosomal enzymes be released to degrade engulfed particles? a. Endocytosis b. Pinocytosis c. Phagocytosis d. Exocytosis ANS: C Engulfment of particles occurs by phagocytosis. Endocytosis involves the formation of vesicles to facilitate movement into the cell. Pinocytosis is a type of endocytosis in which fluids and solute molecules are ingested through formation of small vesicles. Exocytosis occurs when coated pits invaginate and internalize ligand-receptor complexes in coated vesicles. 26. A nurse is teaching the staff about cholesterol. Which information should be taught? The cellular uptake of cholesterol depends on: a. Active-mediated transport b. The antiport system c. Receptor-mediated endocytosis d. Passive transport ANS: C The cellular uptake of cholesterol depends on receptor-mediated endocytosis. The cellular uptake of cholesterol depends on receptor-mediated endocytosis; it is not dependent on active-mediated transport. The cellular uptake of cholesterol depends on receptor-mediated endocytosis; it is not a part of the antiport system. The cellular uptake of cholesterol depends on receptor-mediated endocytosis; it requires energy and is not passive in transport. 27. Some cancer drugs work during the cell cycle phase where nuclear and cytoplasmic division occurs. What is this cell cycle phase called? a. G1 b. S c. M d. G2 ANS: C The M phase includes both nuclear and cytoplasmic division. The G1 phase includes the period between the M phase and the start of DNA synthesis. The S phase include synthesis of DNA in the cell nucleus. The G2 phase includes RNA and protein synthesis. 28. What causes the rapid change in the resting membrane potential that initiates an action potential? a. Potassium gates open, and potassium rushes into the cell, changing the membrane potential from negative to positive. b. Sodium gates open, and sodium rushes into the cell, changing the membrane potential from negative to positive. c. Sodium gates close, allowing potassium into the cell to change the membrane potential from positive to negative. d. Potassium gates close, allowing sodium into the cell to change the membrane potential from positive to negative. ANS: B When the threshold is reached, the cell will continue to depolarize with no further stimulation. The sodium gates open, and sodium rushes into the cell, causing the membrane potential to reduce to zero and then become positive (depolarization). Sodium is involved in creating the action potential, not potassium. The sodium gate must be open, not closed. The sodium channel must be open; this is not affected by a change in the potassium gate. 29. A cell is isolated, and electrophysiology studies reveal that the resting membrane potential is 70 millivolts. The predominant intracellular ion is Na+, and the predominant extracellular ion is K+. With voltage change, which of the following would result in an action potential? a. K+ rushing into the cell b. Na+ rushing into the cell c. Na+ rushing out of the cell d. K+ rushing out of the cell ANS: A With voltage change, potassium rushes into the cell. Potassium, not sodium, rushes into the cell. Potassium, not sodium, is involved in the process, and potassium moves into the cells, not out. Potassium rushes into the cell, not out. 30. A nurse is teaching the staff about platelet-derived growth factor. Which information should the nurse include? Platelet-derived growth factor (PDGF) stimulates the production of: a. Platelets b. Epidermal cells c. Connective tissue cells d. Fibroblast cells ANS: C Different types of cells require different growth factors; for example, PDGF stimulates the production of connective tissue cells. The factor stimulates the production of connective tissue, not platelets. The factor stimulates the production of connective tissue, not epidermal cells. The factor stimulates the production of connective tissue, not fibroblast cells. 31. The phase of the cell cycle during which the centromeres split and the sister chromatids are pulled apart is referred to as: a. Anaphase b. Telophase c. Prophase d. Metaphase ANS: A Anaphase begins when the centromeres split and the sister chromatids are pulled apart. During telophase, the final stage, a new nuclear membrane is formed around each group of 46 chromosomes, the spindle fibers disappear, and the chromosomes begin to uncoil. During prophase, the first appearance of chromosomes occurs. Metaphase occurs when two centrioles located at opposite poles of the cell pull the chromosomes to opposite sides of the cell. 32. What is the role of cytokines in cell reproduction? a. Provide growth factor for tissue growth and development b. Block progress of cell reproduction through the cell cycle c. Restrain cell growth and development d. Provide nutrients for cell growth and development ANS: A Cytokines play a major role in the regulation of tissue growth and development. Cytokines help overcome intracellular braking mechanisms that restrain cell growth. Cytokines promote cell growth, not restrain it. Cytokines regulate growth; they do not provide nutrients. 33. A biopsy of the lung bronchi revealed ciliated epithelial cells that are capable of secretion and absorption. These cells are called columnar epithelium. a. Simple b. Ciliated simple c. Stratified d. Pseudostratified ciliated ANS: B Ciliated simple columnar epithelium are found in the lungs. Simple columnar epithelium are found from the stomach to the anus. Stratified columnar epithelium are found in the linings of epiglottis, part of pharynx, anus, and male urethra. Pseudostratified ciliate columnar epithelium is found in the linings of large ducts of some glands (parotid, salivary), male urethra, respiratory passages, and eustachian tubes of ears. 34. The nurse would be correct in identifying the predominant extracellular cation as: a. Sodium b. Potassium c. Chloride d. Glucose ANS: A The predominant extracellular cation is sodium. Potassium is the predominant intracellular cation. Chloride is an anion. Urea is a nonelectrolyte. Glucose is a nonelectrolyte. 35. The student is reviewing functions of the cell. The student would be correct in identifying the primary function of the nerve cell as: a. Sensory interpretation b. Conductivity c. Maintenance of homeostasis d. Communication ANS: B Conduction as a response to a stimulus is manifested by a wave of excitation; an electrical potential that passes along the surface of the cell to reach its other parts. Conductivity is the chief function of nerve cells. Nerve cells assist with sensory interpretation, but their primary function is conductivity. Nerve cells assist with maintenance of homeostasis, but their primary function is conductivity. Nerve cells assist with communication, but their primary function is conductivity. Chapter 2. Genes and Genetic Diseases MULTIPLE CHOICE 1. A nurse recalls the basic components of DNA are: a. Pentose sugars and four phosphate bases b. A phosphate molecule, deoxyribose, and four nitrogenous bases c. Adenine, guanine, and purine d. Codons, oxygen, and cytosine ANS: B DNA has three basic components: the pentose sugar molecule, deoxyribose; a phosphate molecule; and four types of nitrogenous bases. DNA contains four nitrogenous bases, not phosphate bases. Adenine and quinine are purines and are only a portion of the components of DNA. DNA synthesizes body protein, of which a codon is a component. 2. Which of the following mutations have the most significant effect on protein synthesis? a. Base pair substitutions b. Silent mutations c. Intron mutations d. Frameshift mutations ANS: D The frameshift mutation involves the insertion or deletion of one or more base pairs of the DNA molecule. They alter the amino acid sequence. The base pair substitution is a type of mutation in which one base pair replaces another. Silent mutations do not change amino acids or protein synthesis. Intron mutations are part of RNA sequencing. 3. The base components of DNA are: a. A, G, C, and U b. P, G, C, and T c. A, G, C, and T d. X, XX, XY, and YY ANS: C The four base components of DNA are cytosine, thymine, adenine, and guanine and are commonly represented by their first letters: A, C, T, and G. The four base components of DNA are cytosine, thymine, adenine, and guanine and are commonly represented by their first letters: A, C, T, and G. U is not included. The four base components of DNA are cytosine, thymine, adenine, and guanine and are commonly represented by their first letters: A, C, T, and G. P is not included. X, XX, XY and YY are components of human chromosomes. 4. A DNA strand has a region with the sequence ATCGGAT. Which of the following would be a complementary strand? a. CGATACGT b. TAGCCTAG c. TUGCCTUG d. UAGCCUAG ANS: B The consistent pairing of adenine with thymine and of guanine with cytosine is known as complementary base pairing; thus, A complements to T and C to G and vice versa throughout the strand. A complements to T; thus, the first letter must be a T. U does not represent a complement in the sequence. U does not represent a complement in the sequence. 5. A biologist is explaining how RNA directs the synthesis of protein. Which process is the biologist describing? a. Termination b. Transcription c. Translocation d. Translation ANS: D In translation, RNA directs the synthesis of a polypeptide, interacting with transfer RNA (tRNA), a cloverleaf-shaped strand of about 80 nucleotides. At a termination signal, translation and polypeptide formation cease. This does not involve synthesis of protein. Transcription is the process by which DNA specifies a sequence of messenger RNA (mRNA). Translocation is the interchange of genetic material between nonhomologous chromosomes. 6. When homologous chromosomes fail to separate during meiosis, which of the following occurs? a. Neurofibromatosis b. Nondisjunction c. Polyploidy d. Conjoined twins ANS: B Nondisjunction is an error in which homologous chromosomes or sister chromatids fail to separate normally during meiosis or mitosis. Neurofibromatosis is a dominant disorder. It is not due to chromosome failure during meiosis. Polyploidy occurs when a euploid cell has more than the diploid number of chromosomes. Conjoined twins are not due to chromosome failure during meiosis. 7. A cell that does not contain a multiple of 23 chromosomes is called a cell. a. diploid b. euploid c. polyploid d. haploid ANS: C A polyploid cell is one in which a euploid cell has more than the diploid number of chromosomes. A diploid cell is when the somatic cell nucleus has 46 chromosomes in 23 pairs. A euploid cell is a cell with multiples of the normal number of chromosomes. A haploid cell has only one member of each chromosome pair, for a total of 23 chromosomes. 8. A 20-year-old pregnant female gives birth to a stillborn child. Autopsy reveals that the fetus has 92 chromosomes. What term may be on the autopsy report to describe this condition? a. Biploidy b. Triploidy c. Tetraploidy d. Aneuploidy ANS: C Tetraploidy is a condition in which euploid cells have 92 chromosomes. Biploidy is a euploid cell with 2 times more chromosomes, or 46. Triploidy is a zygote that has three copies of each chromosome, rather than the usual two. Aneuploidy is when an aneuploid cell does not contain a multiple of 23 chromosomes. 9. The condition in which an extra portion of a chromosome is present in each cell is called: a. Reciprocal translocation b. Partial trisomy c. Inversion d. Down syndrome ANS: B Partial trisomy is a condition in which only an extra portion of a chromosome is present in each cell. A reciprocal translocation occurs when breaks take place in two different chromosomes and the material is exchanged. An inversion occurs when two breaks take place on a chromosome, followed by the reinsertion of the missing fragment at its original site, but in inverted order. Down syndrome is an aneuploidy of the twenty-first chromosome. 10. After a geneticist talks to the patient about being a chromosomal mosaic, the patient asks the nurse what that means. How should the nurse respond? You may genetic disease(s). a. Only be a carrier of the b. Have a mild form of the c. Have two d. Be sterile as a result of the ANS: B A chromosomal mosaic means the body has two or more different cell lines, each of which has a different karyotype; thus, the person has a mild form of the disease. Mosaics are not only carriers; they have the disease. Mosaics have two different lines but not two different diseases. Mosaics are not sterile. 11. The nurse is teaching staff about the most common cause of Down syndrome. What is the nurse describing? a. Paternal nondisjunction b. Maternal translocations c. Maternal nondisjunction d. Paternal translocations ANS: C The most common cause of Down syndrome is maternal nondisjunction. Down syndrome is not related to paternal nondisjunction. Down syndrome is related to the maternal side, but not due to translocation. Down syndrome is not related to paternal abnormalities. 12. A patient wants to know the risk factors for Down syndrome. What is the nurses best response? a. Fetal exposure to mutagens in the uterus b. Increased paternal age c. Family history of Down syndrome d. Pregnancy in women over age 35 ANS: D The primary risk for Down syndrome is pregnancy in women over 35. Down syndrome is a trisomy and not due to fetal exposure. Paternal age is not a risk factor in Down syndrome. Down syndrome is a chromosomal abnormality and is not related to family history. 13. A 13-year-old girl has a karyotype that reveals an absent homologous X chromosome with only a single X chromosome present. What medical diagnosis will the nurse observe on the chart? a. Down syndrome b. Cri du chat syndrome c. Turner syndrome d. Fragile X syndrome ANS: C A condition with the presence of a single X chromosome and no homologous X or Y chromosome, so the individual has a total of 45 chromosomes, is known as Turner syndrome. Down syndrome is a change in one arm of a chromosome. Cri du chat syndrome is due to a chromosome deletion. Fragile X syndrome is due to a break or a gap in a chromosome. 14. An XXY person asks the nurse what this genetic disorder is called. What is the nurses best response? This disorder is syndrome. a. Turner b. Klinefelter c. Down d. Fragile X ANS: B Individuals with at least two X chromosomes and one Y chromosome in each cell (47 XXY karyotype) have a disorder known as Klinefelter syndrome. A condition with the presence of a single X chromosome and no homologous X or Y chromosome, so the individual has a total of 45 chromosomes, is known as Turner syndrome. Down syndrome is a trisomy. Fragile X syndrome is due to a break or a gap in a chromosome, not an extra chromosome. 15. A patient has severe mental retardation caused by a deletion of part of chromosome 5. What genetic disorder will the nurse see documented in the chart? a. Prader-Willi syndrome b. Down syndrome c. Cri du chat syndrome d. Trisomy X ANS: C Cri du chat syndrome means cry of the cat and describes the characteristic cry of the affected child. Another symptom of the disorder is mental retardation. Prader-Willi syndrome is characterized by short stature, obesity, and hypogonadism. Down syndrome does cause mental retardation, but is due to chromosome 21, not chromosome 5. Trisomy X can result in mental retardation, but is due to an extra X chromosome. 16. A couple has three offspring: one child with an autosomal dominant disease trait and two who are normal. The father is affected by the autosomal dominant disease, but the mother does not have the disease gene. What is the recurrence risk of this autosomal dominant disease for their next child? a. 50% b. 33% c. 25% d. Impossible to determine ANS: A For each child with an autosomal dominant disease parent there is a 1 in 2, or 50%, risk. The risk is 50%. The risk is 50%. The risk can be determined and the risk is 50%. 17. An aide asks the nurse why people who have neurofibromatosis will show varying degrees of the disease. Which genetic principle should the nurse explain to the aide? a. Penetrance b. Expressivity c. Dominance d. Recessiveness ANS: B Expressivity is the extent of variation in phenotype associated with a particular genotype. For neurofibromatosis, a variety of manifestations occur among individuals. The penetrance of a trait is the percentage of individuals with a specific genotype who also exhibit the expected phenotype. Dominance refers to observable traits and risk of transmission. Recessiveness refers to silent strains with reduced risk of occurrence. 18. When a patient asks what causes cystic fibrosis, how should the nurse respond? Cystic fibrosis is caused by an gene. a. X-linked dominant b. X-linked recessive c. Autosomal dominant d. Autosomal recessive ANS: D Cystic fibrosis is an autosomal recessive disorder. Cystic fibrosis is not X linked, but autosomal. Cystic fibrosis is not X linked, but recessive. Cystic fibrosis is not dominant. 19. A 15-year-old female is diagnosed with Prader-Willi syndrome. This condition is an example of: a. Gene imprinting b. An autosomal recessive trait c. An autosomal dominant trait d. A sex-linked trait ANS: A Prader-Willi is an example of gene imprinting. Prader-Willi is not an autosomal recessive trait, but due to gene imprinting. Prader-Willi is not an autosomal dominant train, but due to gene imprinting. Prader-Willi is not a sex-linked trait, but due to gene imprinting. 20. A patient, age 9, is admitted to a pediatric unit with Duchenne muscular dystrophy. When planning care the nurse recalls the patient inherited this condition through a trait. a. Sex-linked dominant b. Sex-influenced c. Sex-limited d. Sex-linked recessive ANS: D Duchenne muscular dystrophy is a relatively common X-linked recessive disorder. Duchenne is a recessive trait, not dominant. Duchenne is a sex-linked, not sex-influenced, trait. Duchenne is a sex-linked, not sex-limited, trait. 21. A child is born with blue eyes (bb). The childs mother has blue eyes and the father has brown eyes. Which of the following represents the father? a. Bb b. Bb c. BB d. Bbb ANS: B The father would need to have one b and one B because blue eyes are recessive and the father has a dominant eye color. bb is incorrect because, with this description, the father could not have brown eyes. BB would describe the fathers brown eyes, but without a b he could not father a blue-eyed child. The father would have only two, not three. 22. A child is diagnosed with cystic fibrosis. History reveals that the childs parents are siblings. Cystic fibrosis was most likely the result of: a. X inactivation b. Genomic imprinting c. Consanguinity d. Obligate carriers ANS: C Consanguinity refers to the mating of two related individuals, and the offspring of such matings are said to be inbred. Consanguineous matings produce a significant increase in recessive disorders and are seen most often in pedigrees for rare recessive disorders. X inactivation occurs when one X chromosome in the somatic cells of females is permanently inactivated. Genomic imprinting is related to methylation and other changes. Obligate carriers are those who have an affected parent and affected children and, therefore, must themselves carry the mutation. 23. A 12-year-old male is diagnosed with Klinefelter syndrome. His karyotype would reveal which of the following? a. XY b. XX c. XYY d. XXY ANS: D A person with Klinefelter syndrome has an XXY karyotype. An XY is a normal male. An XX is a normal female. An XYY is an aneuploid karyotype. 24. To express a polygenic trait: a. Genes must interact with the environment. b. Several genes must act together. c. Multiple mutations must occur in the same family. d. Penetrance must occur. ANS: B Polygenic traits are those that result from several genes acting together. When environmental factors influence the expression of the trait, the term multifactorial inheritance is used. When multiple mutations occur in the same family, the mechanism most likely responsible is termed germline mosaicism. Penetrance of a trait is the percentage of individuals with a specific genotype who also exhibit the expected phenotype. 25. What is the diagnosis of a 13-year-old female who has a karyotype that reveals an absent homologous X chromosome with only a single X chromosome present? Her features include a short stature, widely spaced nipples, reduced carrying angle at the elbow, and sparse body hair. a. Down syndrome b. Cri du chat syndrome c. Turner syndrome d. Klinefelter syndrome ANS: C Turner syndrome is characterized by short stature, female genitalia, webbed neck, shieldlike chest with underdeveloped breasts and widely spaced nipples, and imperfectly developed ovaries. Down syndrome is characterized by distinctive characteristics: low nasal bridge, epicanthal folds, protruding tongue, and low-set ears. Cri du chat syndrome is characterized by low birth weight, severe mental retardation, microcephaly (smaller than normal head size), and heart defects. Klinefelter syndrome is characterized by small testes, some development of the breasts, sparse body hair, and long limbs. 26. A normal male and a female carrier for red-green color blindness mate. Given that red-green color blindness is an X-linked recessive trait, what is the likelihood of their children being affected? a. 25% b. 50% c. Females most affected; no males affected d. Males most affected; no females affected ANS: D Because a single copy of an X-linked recessive gene will cause disease in a male, whereas two copies are required for disease expression in females, more males are affected by X-linked recessive diseases than are females. Males are more often affected at a greater than 25% rate. Males are more often affected at a greater than 50% rate. Males are most often affected. 27. The gradual increase in height among the human population over the past 100 years is an example of: a. A polygenic trait b. A multifactorial trait c. Crossing over d. Recombination ANS: B The gradual increase in height is an example of multifactorial traits influenced by genes and also by environment. Polygenic traits result from several genes acting together. Crossing over is an abnormal chromosome structure. Recombination results from new arrangements of alleles. 28. When discussing DNA replication, which enzyme is most important? a. RNA polymerase b. Transfer RNA c. Messenger RNA d. DNA polymerase ANS: D DNA polymerase is the primary enzyme involved in replication. It adds bases to the new DNA strand and performs proofreading functions. It is DNA polymerase, not RNA polymerase, that is most important for DNA replication. It is DNA polymerase, not transfer RNA, that is most important for DNA replication. It is DNA polymerase, not messenger RNA, that is most important for DNA replication. 29. The regions of the heterogeneous nuclear RNA that must be spliced out to form functional RNA are called: a. Promoter sites b. Introns c. Exons d. Anticodon ANS: B Introns are spliced from the mRNA before the mRNA leaves the nucleus. A promoter site is a sequence of DNA that specifies the beginning of a gene. In eukaryotes, many RNA sequences are removed by nuclear enzymes; the sequences that are left to code for proteins are called exons. In translation, RNA directs the synthesis of a polypeptide, a cloverleaf-shaped strand of about 80 nucleotides. The tRNA molecule has a site where an amino acid attaches. The three-nucleotide sequence at the opposite side of the cloverleaf is called the anticodon. 30. A 5-year-old male presents with mental retardation and is diagnosed with fragile X syndrome. When the parents ask what caused this, how should the geneticist respond? This was most probably caused from: a. Translocation b. Inversion c. Nondisjunction d. Duplication at fragile sites ANS: D Unaffected transmitting males have been shown to have more than about 50 repeated DNA sequences near the beginning of the fragile X gene. Translocation effects do not result in mental retardation. Inversions have no physical effects. Fragile X is not related to nondisjunction. 31. A 50-year-old male was recently diagnosed with Huntington disease. Transmission of this disease is associated with: a. Penetrance b. Recurrence risk c. Expressivity d. Delayed age of onset ANS: D A key feature of Huntington disease is its delayed age of onset such that symptoms are not seen until 40 years of age or later. The penetrance of a trait is the percentage of individuals with a specific genotype who also exhibit the expected phenotype. Recurrence risk is the percentage of family members that will inherit the disease. Expressivity is the extent of variation in phenotype associated with a particular genotype. 32. Mutations that do not change the amino acid sequence and thus have no consequence are termed mutations. a. Frameshift b. Spontaneous c. Silent d. Missense ANS: C Silent mutations do not change the amino acid sequence and have no consequences. Frameshift mutation involves the insertion or deletion of one or more base pairs of the DNA molecule. They alter the amino acid sequence. Spontaneous mutations occur in the absence of exposure to a mutagen and produce changes in amino acid sequence. Missense mutations, a form of base pair substitution, alter amino acids, which produce a change (i.e., the sense) in a single amino acid. 33. A nurse is reviewing the pedigree chart. When checking for a proband, what is the nurse looking for? a. The person who is first diagnosed with a genetic disease b. The individual who has a disease gene but is phenotypically normal c. The phenotype of genetic material d. The codominance ANS: A The pedigree chart summarizes family relationships and shows which members of a family are affected by a genetic disease. The pedigree begins with the proband. The person who has a disease gene but is phenotypically normal is a carrier. The phenotype is the result of both genotype and environment; it is not a proband. Codominance is not represented by proband, but it occurs when the heterozygote is distinguishable from both homozygotes. 34. Which of the following disorders is manifested primarily in males? a. Cystic fibrosis b. Neurofibromatosis c. Muscular dystrophy d. Klinefelter syndrome ANS: C Muscular dystrophy is manifested primarily in males. Cystic fibrosis is manifested in males and females. Neurofibromatosis is manifested in males and females. Klinefelter syndrome is manifested in males and females. Chapter 3. Epigenetics and Disease 1. Genetic disorders that involve a single gene trait are characterized by: A) multifactorial gene mutations. B) chromosome rearrangements. C) Mendelian patterns of transmission. D) abnormal numbers of chromosomes. 2. In addition to having a 50% chance of inheriting an autosomal dominant disorder from an affected parent, such a disorder is characterized by: A) aneuploidy of genes in all cells. B) deficiencies in enzyme synthesis. C) affected X transmission to daughters. D) varied gene penetration and expression. 3. Autosomal recessive disorders are characterized by: A) age of onset later in life. B) abnormal protein structure. C) inborn errors of metabolism. D) one in two risk of a carrier child. 4. When a male child inherits an X-linked disorder from his heterozygous carrier mother, A) his sons will be carriers. B) his father has the disorder. C) some of his sisters will be carriers. D) his daughters will have the disorder. 5. Multifactorial inheritance disorders, such as cleft palate, are often caused by during fetal development. A) multiple gene mutations B) dominant gene expression C) X-linked crossover problem D) polyploidy of chromosomes 6. The newborn has the distinctive physical features of trisomy 21, Down syndrome, which includes: A) upward slanting of eyes. B) large, protruding ears. C) thin lips and small tongue. D) long fingers with extra creases. 7. Aneuploidy of the X chromosome can result in a monosomy or polysomy disorder. The manifestations of monosomy X, Turner syndrome, differ from polysomy X disorders in numerous ways that include: A) short-stature female individual.. B) mental retardation. C) enlarged breasts. D) early onset puberty. 8. A teratogenic environmental agent can cause birth defects when: A) inherited as a recessive trait. B) intense exposure occurs at birth. C) disjunction occurs during meiosis. D) retained during early pregnancy. 9. Fetal alcohol syndrome (FAS) is unlike other teratogens in that the harmful effects on the fetus: A) directly result in liver damage. B) extend throughout the pregnancy. C) is most noticeable in adulthood. D) cause death in early childhood. 10. Prenatal diagnosis methods include the use of ultrasonography for identifying abnormalities. A) cytogenic B) skeletal C) chromosomal D) a-fetoprotein 11. A woman who is a carrier for which of the following diseases possesses the greatest likelihood of passing the disease to her future children when heterozygous pairing exists? A) Phenylketonuria (PKU) B) Tay-Sachs disease C) Neurofibromatosis D) Cystic fibrosis 12. Which of the following statements is true of autosomal recessive disorders? A) Onset is typically late in childhood or early in adulthood. B) Symptomatology is less uniform than with autosomal dominant disorders. C) Mitochondrial DNA is normally the site of genetic alteration. D) Effects are typically the result of alterations in enzyme function. 13. The parents of a newborn infant are relieved that their baby was born healthy, with the exception of a cleft lip that will be surgically corrected in 10 or 12 weeks. Which of the nurses following statements to the parents best conveys the probable cause of the infants cleft lip? A) Though you are both healthy, you likely both carry the gene for a cleft lip. B) Provided one of you had the gene for a cleft lip, your baby likely faced a 50/50 chance of having one. C) Your childs cleft lip likely results from the interplay between environment and genes. D) A cleft lip can sometimes result from taking prescription drugs, even when theyre taken as ordered. 14. Which of the following practitioners is most likely to be of assistance in the early care of an infant with a cleft lip? A) Lactation consultant B) Respiratory therapist C) Occupational therapist D) Social worker 15. A 41-year-old woman has made the recent decision to start a family, and is eager to undergo testing to mitigate the possibility of having a child with Down syndrome. Which of the following tests is most likely to provide the data the woman seeks? A) Genetic testing of the woman B) Genetic testing of the woman and the father C) Prenatal blood tests D) Ultrasonography 16. Genetic testing has revealed that a male infant has been born with an extra X chromosome. What are the most likely implications of this finding? A) The child is unlikely to survive infancy B) The child is likely to have no manifestations of this chromosomal abnormality C) The child will have significant neurological and cognitive defects D) The child will be unable to reproduce 17. Which of the following variables determine the extent of teratogenic drug effects? Select all that apply. A) Maternal health history B) Molecular weight of the drug C) Stage of pregnancy when the drug was taken D) Duration of drug exposure E) Fetal blood type 18. A woman who has just learned that she is pregnant for the first time has sought advice from her healthcare provider about the safe use of alcohol during pregnancy. What advice should the clinician provide to the woman? A) Its likely best to eliminate alcohol from your diet while youre pregnant. B) Moderation in alcohol use is critical while you are pregnant. C) You should limit yourself to a maximum of one drink daily while youre pregnant. D) You should drink no alcohol until you are in your second trimester. 19. Which of the following health problems may be identified by a TORCH screening test? A) Rubella and herpes B) Tenovaginitis and human papillomavirus C) Rhinovirus and Ormond disease D) Chlamydia and rickets 20. Ultrasonography is most likely to detect which of the following fetal abnormalities? A) Neural tube defects B) Skeletal abnormalities C) Chromosomal defects D) Single-gene disorders Answer Key 1. C 2. D 3. C 4. C 5. A 6. A 7. A 8. D 9. B 10. B 11. C 12. D 13. C 14. A 15. C 16. B 17. B, C, D 18. A 19. A 20. B Chapter 4. Altered Cellular and Tissue Biology MULTIPLE CHOICE 1. A report comes back indicating that muscular atrophy has occurred. A nurse recalls that muscular atrophy involves a decrease in muscle cell: a. Number b. Size c. Vacuoles d. Lipofuscin ANS: B Atrophy is a decrease or shrinkage in cellular size. Hyperplasia is an increase in the number of cells. Vacuoles are membrane-bound vesicles within the cell that contain cellular debris and hydrolytic enzymes. Lipofuscin is the yellow-brown age pigment. 2. During childhood, the thymus decreases in size, and this is referred to as atrophy. a. Physiologic b. Pathologic c. Disuse d. Neurogenic ANS: A A normal decrease in cell size is physiologic atrophy. When cell size decrease due to disease, it is termed pathologic atrophy. When cells undergo disuse, the cells shrink in size, and this is disuse atrophy. Neurogenic atrophy is injury or disease affecting the nerves that connect to the muscle. 3. When planning care for a cardiac patient, the nurse knows that in response to an increased workload, cardiac myocardial cells will: a. Increase in size b. Decrease in length c. Increase in excitability d. Increase in number ANS: A Organ cells respond to increased workload by increasing in size, much as a muscle when it is exercised. Organ cells increase in size with increased workload; they do not decrease in length. A deficiency of electrolytes or minerals could lead to an increase in excitability; it is not due to increased workload. Increase in cell numbers is referred to as hyperplasia and is not related to increased workload. 4. A 55-year-old male with a 30-year history of smoking is examined for respiratory disturbance. Examination of his airway (bronchial) reveals that stratified squamous epithelial cells have replaced the normal columnar ciliated cells. This type of cellular adaptation is called: a. Anaplasia b. Hyperplasia c. Metaplasia d. Dysplasia ANS: C Metaplasia is the reversible replacement of one mature cell type by another, sometimes a less differentiated cell type. Anaplasia is loss of cellular differentiation. Hyperplasia is an increase in the number of cells resulting from an increased rate of cellular division. Dysplasia refers to abnormal changes in the size, shape, and organization of mature cells. 5. When planning care for the pregnant patient, the nurse will recall that the mammary glands enlarge as a consequence of: a. Compensatory hyperplasia b. Hormonal hyperplasia c. Hormonal anaplasia d. Compensatory anaplasia ANS: B An increase in the mammary glands during pregnancy is a result of hormonal changes. The number of mammary cells increases in response to increased hormone levels. Hyperplasia is correct, but it is not a compensatory response, but a hormonal response. Hormonal is correct, but the growth is due to an increased number of cells, not enlargement. Compensatory is not correct, nor is anaplasia, a reversal to more immature cells. Mammary enlargement is a normal response. 6. A 24-year-old female presents with excessive menstrual bleeding. The physician identified endometrial changes that are due to hormonal imbalances. These cellular changes would be referred to as: a. Dysplasia b. Pathologic dysplasia c. Hyperplasia d. Pathologic hyperplasia ANS: D Because the changes are due to an imbalance, they would be considered pathologic hyperplasia. The endometrial changes were not abnormal in size and shape; thus, it is not dysplasia. The description of alteration in hormone levels is pathologic. Hyperplasia is not as accurate as pathologic because there is an imbalance of hormone levels. 7. A 55-year-old male is diagnosed with hepatocellular cancer secondary to hepatitis C. If the cancerous region of the liver were removed, the remaining cells would undergo: a. Pathologic hyperplasia b. Pathologic metaplasia c. Compensatory hyperplasia d. Compensatory aplasia ANS: C Compensatory hyperplasia is an adaptive mechanism that enables certain organs to regenerate. The cells become compensatory and would not be pathologic. Metaplasia is the reversible replacement of one mature cell type by another, sometimes less differentiated, cell type. Aplasia is not a compensatory mechanism. 8. A 40-year-old female is diagnosed with cervical cancer after a Pap smear. Which of the following cellular changes would the nurse most likely see on the report? a. Metaplasia b. Atrophy c. Hypertrophy d. Dysplasia ANS: D When cervical cells become cancerous, they have undergone dysplasia, a change in the size and shape of cells. The cells have changed; they have not been replaced, so metaplasia is not the correct choice. The cells have not decreased in size; therefore, atrophy is incorrect. The cells have not increased in size; therefore, they have not hypertrophied. 9. A 75-year-old male presents with chest pain on exertion. The chest pain is most likely due to hypoxic injury secondary to: a. Malnutrition b. Free radicals c. Ischemia d. Chemical toxicity ANS: C The cardiac cells are deprived of oxygen leading to ischemia, a reduction in blood supply to tissues. The cells are deprived of oxygen; they are not malnourished. Free radicals are electrically uncharged atoms or groups of atoms that have an unpaired electron. Chemical toxicity is not a factor in the chest pain; the pain is related to a lack of oxygen. 10. A patient has a heart attack that leads to progressive cell injury that causes cell death with severe cell swelling and breakdown of organelles. What term would the nurse use to define this process? a. Adaptation b. Pathologic calcification c. Apoptosis d. Necrosis ANS: D Necrosis is the sum of cellular changes after local cell death. Cellular adaptation is a reversible, structural, or functional response to both normal or physiologic conditions and adverse or pathologic conditions. Calcification is an accumulation of calcium salts. Apoptosis is an active process of cellular self-destruction. 11. Sodium and water accumulation in an injured cell are a direct result of: a. Decreased ATP production b. Karyorrhexis c. Ribosome detachment d. Dehydration ANS: A A reduction in ATP levels causes the plasma membranes sodium-potassium (Na+-K+) pump and sodium-calcium exchange to fail. Sodium and water can then enter the cell freely. Karyorrhexis means fragmentation of the nucleus into smaller particles or nuclear dust. Ribosome detachment reduces protein synthesis. Dehydration leads to loss of sodium and water. 12. The early dilation (swelling) of the cells endoplasmic reticulum results in: a. Increased aerobic metabolism b. Failure of DNA c. Reduced protein synthesis d. Decreased Na+-K+ pump function ANS: C Early dilation of the endoplasmic reticulum causes the ribosomes to detach from the rough endoplasmic reticulum, reducing protein synthesis. Aerobic metabolism is a normal process and would not lead to swelling. Cellular swelling will not alter cellular DNA. A reduction, not an increase, in the Na+-K+ pump leads to an intracellular accumulation of sodium and calcium and diffusion of potassium out of the cell. Sodium and water can then enter the cell freely, and cellular swelling results. 13. A 52-year-old male suffered a myocardial infarction secondary to atherosclerosis and ischemia. Once oxygen returned to the damaged heart, reperfusion injury occurred as a result of: a. Free radical formation b. Vacuolation c. Increased metabolic state d. Lipid acceptor proteins ANS: A Reperfusion injury results from radicals that cause further membrane damage and mitochondrial calcium overload. Vacuolation leads to cellular swelling and is not associated with reperfusion. Lactic acid increases as a result of damage due to necrosis, and necrosis would interfere with reperfusion, not initiate it. Lipid acceptor proteins bind with triglycerides to create fatty liver, and they do not affect the myocardium. 14. A family presents to their primary care provider reporting headache, nausea, weakness, and vomiting. Which of the following would be the most likely explanation for these symptoms? a. Lead exposure b. Carbon monoxide poisoning c. Ethanol exposure d. Mercury poisoning ANS: B Symptoms related to carbon monoxide poisoning include headache, giddiness, tinnitus (ringing in the ears), nausea, weakness, and vomiting. Although nausea and vomiting can occur with lead exposure, lead toxicity is primarily manifested by convulsions and delirium and, with peripheral nerve involvement, wrist, finger, and sometimes foot paralysis. Ethanol exposure has CNS effects and would not affect the whole family. Mercury poisoning is manifested by CNS effects and would not lead to nausea and vomiting. 15. A common pathway of irreversible cell injury involves increased intracellular: a. Sodium b. Potassium c. Magnesium d. Calcium ANS: D Irreversible cellular injury is due to increased intracellular calcium and loss of calcium steady state. It is calcium, not sodium, that is involved in cellular injury. It is calcium, not potassium, that is involved in cellular injury. It is calcium, not magnesium, that is involved in cellular injury. 16. A 50-year-old male sustained a closed head injury as a result of a motor vehicle accident. CT scan revealed a collection of blood between the inner surface of the dura mater and the surface of the brain. Which type of injury will the nurse be caring for? a. Subdural hematoma b. Epidural hematoma c. Contusion d. Abrasion ANS: A A subdural hematoma occurs when blood is between the inner surface of the dura mater and the surface of the brain; it can result from blows, falls, or sudden acceleration/deceleration of the head. An epidural hematoma is a collection of blood between the inner surface of the skull and the dura; it is most often associated with a skull fracture. A contusion is bleeding into the skin or underlying tissues. An abrasion (scrape) results from removal of the superficial layers of the skin caused by friction between the skin and injuring object. 17. A 20-year-old male presents to the emergency department with a jagged sharp-force injury that is longer than it is deep. Which type of wound will the nurse be caring for? a. Stab wound b. Incised wound c. Puncture wound d. Chopping wound ANS: B An incised wound is a cut that is longer than it is deep. A stab wound is a penetrating sharp-force injury that is deeper than it is long. A puncture wound is without sharp edges and is made with an instrument like a nail. Heavy, edged instruments (axes, hatchets, propeller blades) produce wounds with a combination of sharp and blunt force characteristics. 18. A 30-year-old female presents with a gunshot wound to the head. The wound has seared edges and a deep penetration of smoke and gunpowder fragments. This wound would be documented as a(n) wound. a. Exit b. Intermediate range entrance c. Contact range entrance d. Indeterminate range entrance ANS: C Contact range entrance wound is a distinctive type of wound when the gun is held so the muzzle rests on or presses into the skin surface; in addition to the hole, there is searing of the edges of the wound from flame and soot or smoke on the edges of the wound. It is unlikely it is an exit wound since there is only one wound and it has seared edges and gunpowder fragments. Intermediate range entrance wound is surrounded by gunpowder tattooing or stippling. Indeterminate range entrance wound occurs when flame, soot, or gunpowder does not reach the skin surface, but the bullet does. 19. A 15-year-old female presents to the ER following a physical assault. She has internal damage to the neck with deep bruising. X-ray reveals fractures of the hyoid bone and tracheal and cricoid cartilage. Which of the following most likely caused her injuries? a. Chemical asphyxiation b. Choking asphyxiation c. Ligature strangulation d. Manual strangulation ANS: D Squeezing of the neck as with strangulation would fraction the hyoid bone. Chemical asphyxiation would lead to breathing problems but would not result in fracture. Choking asphyxiation would lead to swelling of tissues but would not result in fracture. In ligature strangulation, the mark on the neck is horizontal without the inverted V pattern seen in hangings. It would not lead to fracture. 20. A 55-year-old male has swelling of the feet. Which of the following aided in development of swelling? a. Increased ATP b. Chloride movement out of the cell c. Na+ movement into the cell d. Decreased oncotic pressure ANS: C When sodium and water enter the cell freely, cellular swelling, as well as early dilation of the endoplasmic reticulum, results. Decreased ATP would lead to swelling, not increased ATP. Chloride movement out of the cell would affect muscle contraction and does not lead to swelling. Increased oncotic pressure would not affect swelling. 21. A 35-year-old female is diagnosed with multiple myeloma. Biopsy of the tumor reveals Russell bodies, and laboratory testing reveals kidney dysfunction. Which substance should the nurse monitor as it is accumulating in the patients body? a. Glycogen b. Protein c. Pigment d. Melanin ANS: B Russell bodies occur due to excess aggregates of protein. Excess glycogen would affect blood glucose and this is not related to Russell bodies. Increased pigment would not lead to kidney dysfunction. Melanin accumulates in epithelial cells (keratinocytes) of the skin and retina. It is an extremely important pigment because it protects the skin against long exposure to sunlight. 22. A newborn male is diagnosed with albinism based on skin, eye, and hair appearance. Which finding will support this diagnosis? a. Increased melanin b. Increased hemoproteins c. Inability to convert tyrosine to DOPA (3,4 dihydroxyphenylalanine) d. Inability to convert bile to bilirubin ANS: C The person with albinism is unable to convert tyrosine to DOPA, an intermediate in melanin biosynthesis. An increase in melanin would cause skin to be darker. Hemoprotein accumulations in cells are caused by excessive storage of iron, which is transferred to the cells from the bloodstream. An inability to convert bile to bilirubin would not lead to albinism. 23. A 23-year-old male develops a black eye following a fight. When the aide asks the nurse why this occurred, the nurses best response is that the bruising is due to an accumulation of: a. Transferrin b. Bilirubin c. Albumin d. Hemosiderin ANS: D Hemosiderin is responsible for the color changes in a black eye. Transferrin is a transport protein responsible for iron transport. Bilirubin is the normal, yellow-to-green pigment of bile derived from the porphyrin structure of hemoglobin. Albumin is the protein in the serum, responsible for cellular integrity. 24. Liquefactive necrosis occurs in the brain because: a. Debris is not digested by hydrolases b. Of protein denaturation c. It is rich in hydrolytic enzymes and lipids d. Ischemia results in chemical injury ANS: C Liquefactive necrosis is due to enzymatic action and because cells of the brain are rich in enzymes. Liquefactive necrosis is not due to hydrolases. Protein denaturation occurs primarily in the kidneys. Liquefactive necrosis is due to enzymatic reaction and not to hypoxia. 25. A 2-year-old swallowed watch batteries. Following ingestion, kidney function was impaired, and the heart began to fail. Which of the following was the most likely cause? a. Karyorrhexis b. Coagulative necrosis c. Ammonia accumulation d. Caseous necrosis ANS: B Coagulative necrosis occurs primarily in the kidneys, heart, and adrenal glands and commonly results from hypoxia. Karyorrhexis means fragmentation of the nucleus into smaller particles or nuclear dust. Ammonia accumulation is not associated with this toxicity. Caseous necrosis results from tuberculosis pulmonary infection. 26. A group of prison inmates developed tuberculosis following exposure to an infected inmate. On examination, tissues were soft and granular (like clumped cheese). Which of the following is the most likely cause? a. Coagulative necrosis b. Liquefactive necrosis c. Caseous necrosis d. Autonecrosis ANS: C Caseous necrosis results from tuberculosis pulmonary infection. Coagulative necrosis occurs primarily in the kidneys, heart, and adrenal glands and commonly results from hypoxia. Liquefactive necrosis results from ischemic injury to neurons and glial cells in the brain. Autonecrosis is a process of cellular self-digestion and is not due to infection such as tuberculosis. 27. A 50-year-old female became infected with Clostridium bacteria and died a week later. Examination of her red blood cells revealed lysis of membranes. Which of the following was the most likely cause of her death? a. Fat necrosis b. Wet gangrene c. Gangrenous necrosis d. Gas gangrene ANS: D Gas gangrene is a special type of gangrene caused by infection of injured tissue by one of many species of Clostridium. Fat necrosis is cellular dissolution caused by powerful enzymes, called lipases, that occur in the breast, pancreas, and other abdominal structures. It is not due to infection. Wet gangrene develops when neutrophils invade the site, causing liquefactive necrosis. It is not due to infection. Gangrenous necrosis is due to death of tissue and results from severe hypoxic injury, not infection. 28. While reading a textbook, the student reads the term, apoptosis. The student recalls that apoptosis is a condition in which cells program themselves to: a. Atrophy b. Die c. Regenerate d. Age ANS: B In apoptosis, cells are programmed to die. In apoptosis, cells do not atrophy; they die. In apoptosis, cells do not regenerate; they die. In apoptosis, cells do not age; they die. 29. A 50-year-old male intravenous drug user is diagnosed with hepatitis C. Examination of the liver reveals cell death secondary to: a. Fat necrosis b. Physiologic apoptosis c. Pathologic apoptosis d. Pyknosis ANS: C With hepatitis C, the liver will demonstrate apoptosis that is pathologic. Fat necrosis occurs with enzymatic action due to lipases. Apoptosis is not a normal physiological process. Pyknosis occurs when the nucleus shrinks and becomes a small, dense mass of genetic material. 30. What principle should the nurse remember when trying to distinguish aging from diseases? a. It is difficult to tell the difference because both processes are believed to result from cell injury. b. It is easy to tell normal processes from abnormal processes. c. Disease, unlike aging, has a genetic component. d. Aging is defined as exceeding life expectancy, but not maximal life span. ANS: A It is difficult to differentiate between aging and disease because both occur secondary to cellular aging. It is not easy to differentiate normal processes from abnormal because aging appears as a normal process. Disease and aging have a possible genetic component. Aging is a time-dependent loss of structure and function that proceeds slowly and in such small increments that it appears to be the result of the accumulation of small, imperceptible injuries. It is not a time period outside of life expectancy. 31. When a nurse observes muscle stiffening occurring within 6 to 14 hours after death, the nurse should document this finding as present. a. Livor mortis b. Gangrene c. Algor mortis d. Rigor mortis ANS: D Rigor mortis occurs within 6 hours after death and is evidence by muscle stiffening. Livor mortis is a purple discoloration. Gangrene refers to death of tissue and results from severe hypoxic injury and does not lead to stiffening. Algor mortis is postmortem reduction of body temperature. 32. When the nurse is checking the urinalysis, the finding that would alert the nurse to cellular injury is the presence of: a. Slight glucose b. Excessive protein c. Blood d. Urea ANS: B The presence of protein in the urine in significant amounts indicates cellular injury and altered cellular function. Glucose should not normally be present in the urine, but its presence is not indicative of altered cellular function, but of excess glucose in the blood. Blood should not normally be present in the urine, but its presence indicates kidney alteration and not cellular injury. Urea is an expected substance in the kidney. 33. An 86-year-old female patient has the wasting syndrome of aging, making her vulnerable to falls, functional decline, disease, and death. The nurse knows this patient is experiencing: a. Frailty b. Sarcopenia c. Somatic death d. Cellular aging ANS: A Frailty leaves the individual vulnerable to falls, disease, and death. Sarcopenia is loss of muscle mass. It is associated with aging, but is not as severe as frailty. Somatic death is death of the whole person. Cellular aging occurs at the cellular level and is characteristic of aging, including cell atrophy, decreased function, and loss of cells. 34. Confirmation of somatic death is based on: a. Presence of algor mortis b. Presence of livor mortis c. Complete cessation of respiration and circulation d. Change in skin color to pale yellow ANS: C The most notable manifestations are complete cessation of respiration and circulation. Algor mortis is postmortem reduction of body temperature and is not confirmation of somatic death. Chapter 5. Fluids and Electrolytes, Acids and Bases MULTIPLE CHOICE 1. A nurse is reviewing lab reports. The nurse recalls blood plasma is located in which of the following fluid compartments? a. Intracellular fluid (ICF) b. Extracellular fluid (ECF) c. Interstitial fluid d. Intravascular fluid ANS: D Blood plasma is the intravascular fluid. ICF is fluid in the cells. ECF is all the fluid outside the cells. Interstitial fluid is fluid between the cells and outside the blood vessels. 2. A 35-year-old male weighs 70 kg. Approximately how much of this weight is ICF? a. 5 L b. 10 L c. 28 L d. 42 L ANS: D The total volume of body water for a 70-kg person is about 42 L. 5 L is incorrect because a 70-kg person has about 42 L of body water. 10 L is incorrect because a 70-kg person has about 42 L of body water. 28 L is incorrect because a 70-kg person has about 42 L of body water. 3. While planning care for elderly individuals, the nurse remembers the elderly are at a higher risk for developing dehydration because they have a(n): a. Higher total body water volume b. Decreased muscle mass c. Increase in thirst d. Increased tendency towards developing edema ANS: B The elderly are at higher risk for dehydration due to a decrease in muscle mass. The elderly have a decrease in total body water, not an increase. The elderly have a decrease in thirst. The elderly may develop edema, but this does not lead to dehydration. Cognitive Level: Comprehension 100 4. Which of the following patients should the nurse assess for a decreased oncotic pressure in the capillaries? A patient with: a. A high-protein diet b. Liver failure c. Low blood pressure d. Low blood glucose ANS: B Liver failure leads to lost or diminished plasma albumin production, and this contributes to decreased plasma oncotic pressure. A high-protein diet would provide albumin for the maintenance of oncotic pressure. Low blood pressure would lead to decreased hydrostatic pressure. Decreased glucose does not affect oncotic pressure. Cognitive Level: Comprehension 101 5. Water movement between the ICF and ECF compartments is determined by: a. Osmotic forces b. Plasma oncotic pressure c. Antidiuretic hormone d. Buffer systems ANS: A Osmotic forces determine water movement between the ECF and ICF compartments. Oncotic pressure pulls water at the end of the capillary, which makes it move between intra and extra as interstitial is considered extra. The antidiuretic hormone regulates water balance which would make water move between the intra and extra. Buffer systems help regulate acid balance. Cognitive Level: Comprehension 101 6. An experiment was designed to test the effects of the Starling forces on fluid movement. Which of the following alterations would result in fluid moving into the interstitial space? a. Increased capillary oncotic pressure b. Increased interstitial hydrostatic pressure c. Decreased capillary hydrostatic pressure d. Increased interstitial oncotic pressure ANS: D Increased interstitial oncotic pressure would attract water from the capillary into the interstitial space. Increased capillary oncotic pressure would attract water from the interstitial space back into the capillary. Increased interstitial hydrostatic pressure would attract movement of water from the interstitial spaces into the capillary. Decreased capillary hydrostatic pressure would move water into the capillaries. Cognitive Level: Comprehension 101 7. When planning care for a dehydrated patient, the nurse remembers the principle of water balance is closely related to balance. a. Potassium b. Chloride c. Bicarbonate d. Sodium ANS: D Because water follows the osmotic gradients established by changes in salt concentration, water balance is tied to sodium balance. Because water follows the osmotic gradients established by changes in salt concentration, water balance is tied to sodium balance, not potassium. Because water follows the osmotic gradients established by changes in salt concentration, water balance is tied to sodium balance, not chloride. Because water follows the osmotic gradients established by changes in salt concentration, water balance is tied to sodium balance, not bicarbonate. Cognitive Level: Comprehension 103 8. A 70-year-old male with chronic renal failure presents with edema. Which of the following is the most likely cause of this condition? a. Increased capillary oncotic pressure b. Decreased interstitial oncotic pressure c. Increased capillary hydrostatic pressure d. Increased interstitial hydrostatic pressure ANS: C Increased capillary hydrostatic pressure would facilitate increased movement from the capillary to the interstitial space, leading to edema. Increased capillary (plasma) oncotic pressure attracts water from the interstitial space back into the capillary. Decreased interstitial oncotic pressure would keep water in the capillary. Increased interstitial hydrostatic pressure would facilitate increased water movement from the interstitial space into the capillary. Cognitive Level: Comprehension 100 9. A 10-year-old male is brought to the emergency room (ER) because he is incoherent and semiconscious. CT scan reveals that he is suffering from cerebral edema. This type of edema is referred to as: a. Localized edema b. Generalized edema c. Pitting edema d. Lymphedema ANS: A Cerebral edema is a form of localized edema. Generalized edema is manifested by a more uniform distribution of fluid in interstitial spaces. Pitting edema is due to a pit left in the skin. Lymphedema is due to swelling in interstitial spaces, primarily in the extremities. Cognitive Level: Comprehension 102 10. A nurse is teaching the staff about antidiuretic hormone (ADH). Which information should the nurse include? Secretion of ADH is stimulated by: a. Increased serum potassium b. Increased plasma osmolality c. Decreased renal blood flow d. Generalized edema ANS: B ADH is secreted when plasma osmolality increases or circulating blood volume decreases and blood pressure drops. ADH is secreted when plasma osmolality increases, not by an increase in potassium. ADH is secreted when plasma osmolality increases; it is not affected by decreased renal blood flow. Edema does not affect the secretion of ADH. Cognitive Level: Comprehension 104 11. Which statement by the staff indicates teaching was successful concerning aldosterone? Secretion of aldosterone results in: a. Decreased plasma osmolality b. Increased serum potassium levels c. Increased blood volume d. Localized edema ANS: C Aldosterone promotes renal sodium and water reabsorption and excretion of potassium, thus, increasing blood volume. Aldosterone secretion would cause increased plasma osmolality. Secretion of aldosterone decreases potassium levels because it causes potassium excretion. Secretion of aldosterone does not promote the development of localized edema; it affects blood volume. Cognitive Level: Comprehension 104 12. A 25-year-old male is diagnosed with a hormone-secreting tumor of the adrenal cortex. Which finding would the nurse expect to see in the lab results? a. Decreased blood volume b. Decreased blood K+ levels c. Increased urine Na+ levels d. Increased white blood cells ANS: B Aldosterone is secreted from the adrenal cortex. It promotes renal sodium and water reabsorption and excretion of potassium, leading to decreased potassium levels. Blood volume actually increases with aldosterone secretion. Aldosterone promotes sodium reabsorption, leading to normal or decreased Na+ levels. Aldosterone is not associated with white blood cells. Cognitive Level: Comprehension 103 13. A patient has been searching on the Internet about natriuretic hormones. When the patient asks the nurse what do these hormones do, how should the nurse respond? Natriuretic hormones affect the balance of: a. Calcium b. Sodium c. Magnesium d. Potassium ANS: B Natriuretic hormones are sometimes called a third factor in sodium regulation. Natriuretic hormones are a factor in sodium balance, not calcium. Natriuretic hormones are a factor in sodium balance, not magnesium. Natriuretic hormones are a factor in sodium balance, not potassium. Cognitive Level: Comprehension 103 14. A 5-year-old male presents to the ER with delirium and sunken eyes. After diagnosing him with severe dehydration, the primary care provider orders fluid replacement. The nurse administers a hypertonic intravenous solution. Which of the following would be expected? a. Symptoms subside quickly b. Increased ICF volume c. Decreased ECF volume d. Intracellular dehydration ANS: D A hypertonic solution would cause fluid to move into the extracellular space, leading to intracellular dehydration. With this solution, his symptoms will not subside quickly because his cells will lose fluid. His intracellular volume will decrease, not increase. His extracellular volume will increase, not decrease. Cognitive Level: Comprehension 106 15. Which of the following patients is the most at risk for developing hypernatremia? A patient with: a. Vomiting b. Diuretic use c. Dehydration d. Hypoaldosteronism ANS: C Dehydration leads to hypernatremia because an increase in sodium occurs with a net loss in water. Vomiting leads to hyponatremia. Diuretic use would lead to sodium loss. Hypoaldosteronism leads to hyponatremia. Cognitive Level: Comprehension 106 16. The most common cause of pure water deficit is: a. Renal water loss b. Hyperventilation c. Sodium loss d. Insufficient water intake ANS: A The most common cause of water loss is increased renal clearance of free water as a result of impaired tubular function. Hyperventilation can cause water loss, but it is not the most common cause. Sodium loss leads to hyponatremia, not pure water deficit. Insufficient water intake causes hypernatremia, not water deficit. Cognitive Level: Comprehension 106 17. Hyperlipidemia and hyperglycemia are associated with: a. Hypernatremia b. Hypertonic hyponatremia c. Hypokalemia d. Acidosis ANS: B Hypertonic hyponatremia develops with hyperlipidemia, hyperproteinemia, and hyperglycemia. Increases in plasma lipids displace water volume and decrease sodium concentration. Hyperlipidemia and hyperglycemia are associated with hyponatremia, not hypernatremia. Hyperlipidemia and hyperglycemia are associated with hyponatremia, not hypokalemia. Hyperlipidemia and hyperglycemia are associated with hyponatremia, not acidosis. Cognitive Level: Comprehension 107 18. A 52-year-old diabetic male presents to the ER with lethargy, confusion, and depressed reflexes. His wife indicates that he does not follow the prescribed diet and takes his medication sporadically. Lab results indicate hyperglycemia. Which assessment finding is most likely to occur? a. Clammy skin b. Decreased sodium c. Decreased urine formation d. Metabolic alkalosis ANS: B Hypertonic hyponatremia develops with hyperglycemia. Increases in plasma lipids displace water volume and decrease sodium concentration, leading to the symptoms described. The patient is experiencing symptoms of hyponatremia and hyperglycemia, not hypernatremia and hypoglycemia. The patient will have increased ECF and would have increased urine formation. Metabolic acidosis would occur, not alkalosis. Cognitive Level: Comprehension 107 19. When taking care of a patient with hyperkalemia, which principle is priority? Hyperkalemia causes a(n) in resting membrane potential with excitability of cardiac muscle. a. Increase; increased b. Decrease; increased c. Increase; decreased d. Decrease; decreased ANS: A Hyperkalemia causes an increase in resting membrane potential and increased excitability of cardiac muscle. Hyperkalemia does cause an increased excitability of cardiac muscle, but the result is an increase in resting membrane potential. Hyperkalemia does cause an increase in resting membrane potential, but the result is an increase in excitability of cardiac muscle. Hyperkalemia causes an increase in resting membrane potential and increased excitability of cardiac muscle. Cognitive Level: Comprehension 110 20. Which of the following patients is most prone to hypochloremia? A patient with: a. Hypernatremia b. Hypokalemia c. Hypercalcemia d. Increased bicarbonate intake ANS: D Hypochloremia is the result of elevated bicarbonate concentration, as occurs in metabolic alkalosis. Hypochloremia is the result of hyponatremia, not hypernatremia. Hypochloremia is the result of hyponatremia, not hypokalemia. Hypochloremia is the result of hyponatremia, not hypercalcemia. Cognitive Level: Comprehension 106 21. Which of the following conditions would cause the nurse to monitor for hyperkalemia? a. Excess aldosterone b. Acute acidosis c. Insulin usage d. Metabolic alkalosis ANS: B In acidosis, ECF hydrogen ions shift into the cells in exchange for ICF potassium and sodium; hyperkalemia and acidosis therefore often occur together. Acidosis causes hyperkalemia, not excess aldosterone. Insulin would help treat hyperkalemia, not cause it. It is acidosis, not alkalosis, that leads to hyperkalemia. Cognitive Level: Comprehension 110 22. Which organ system should the nurse monitor when the patient has long-term potassium deficits? a. Central nervous system (CNS) b. Lungs c. Kidneys d. Gastrointestinal tract ANS: C Long-term potassium deficits lasting more than 1 month may damage renal tissue, with interstitial fibrosis and tubular atrophy. Long-term potassium deficits damage the kidneys, not the CNS. Long-term potassium deficits damage the kidneys, not the lungs. Long-term potassium deficits damage the kidneys, not the gastrointestinal tract. Cognitive Level: Comprehension 108 23. A 42-year-old female presents to her primary care provider reporting muscle weakness and cardiac abnormalities. Laboratory tests indicate that she is hypokalemic. Which of the following could be the cause of her condition? a. Respiratory acidosis b. Constipation c. Hypoglycemia d. Primary hyperaldosteronism ANS: D Primary hyperaldosteronism, with excessive secretion of aldosterone from an adrenal adenoma (tumor) also causes potassium wasting. Acidosis is related to hyperkalemia, not hypokalemia. Constipation can occur with hypokalemia but does not cause it. Hypoglycemia is not related to muscle weakness. Cognitive Level: Comprehension 108 24. A 19-year-old male presents to his primary care provider reporting restlessness, muscle cramping, and diarrhea. Lab tests reveal that he is hyperkalemic. Which of the following could have caused his condition? a. Primary hyperaldosteronism b. Acidosis c. Insulin secretion d. Diuretic use ANS: B During acute acidosis, hydrogen ions accumulate in the ICF and potassium shifts out of the cell to the ECF, causing hyperkalemia. Primary hyperaldosteronism is associated with hypokalemia, not hyperkalemia. Insulin secretion helps reduce potassium levels in the cell, not cause it. Diuretics would cause hypokalemia, not hyperkalemia. Cognitive Level: Comprehension 110 25. A 60-year-old female is diagnosed with hyperkalemia. Which assessment finding should the nurse expect to observe? a. Weak pulse b. Excessive thirst c. Oliguria d. Constipation ANS: C Hyperkalemia is manifested by oliguria. Hypokalemia is manifested by a weak pulse; it is not caused by hyperkalemia. Hypokalemia is manifested by excessive thirst. Diarrhea, not constipation, is a manifestation of hyperkalemia. Cognitive Level: Comprehension 110 26. Which of the following buffer pairs is considered the major plasma buffering system? a. Protein/fat b. Carbonic acid/bicarbonate c. Sodium/potassium d. Amylase/albumin ANS: B The carbonic acid/bicarbonate buffer pair operates in both the lung and the kidney and is a major extracellular buffer. Protein and fat are nutrients not related to the buffering system. Sodium and potassium are electrolytes for fluid and electrolyte balance, not the major plasma buffering system for acid-base balance. Amylase is a carbohydrate enzyme, and albumin is a protein; neither is a buffering system. REF: pp. 111-112 27. A nurse recalls regulation of acid-base balance through removal or retention of volatile acids is accomplished by the: a. Buffer systems b. Kidneys c. Lungs d. Liver ANS: C The volatile acid is carbonic acid (H2CO3), which readily dissociates into carbon dioxide (CO2) and water (H2O). The CO2 is then eliminated by the lungs. Buffer systems are throughout the body and operate in the extracellular and intracellular systems. The kidneys release hydrogen ions, not volatile acids. The liver does not regulate acid-base balance. Cognitive Level: Comprehension 111 28. Physiologic pH is maintained around 7.4 because carbonic acid and bicarbonate exist in a ratio of: a. 20:1 b. 1:20 c. 10:2 d. 2:10 ANS: A Normal carbonic acid to bicarbonate ratio is 20:1. Normal carbonic acid to bicarbonate ratio is 20:1. Normal carbonic acid to bicarbonate ratio is 20:1. Normal carbonic acid to bicarbonate ratio is 20:1. Cognitive Level: Comprehension 110 29. Which patient is most prone to metabolic alkalosis? A patient with: a. Retention of metabolic acids b. Hypoaldosteronism c. Excessive loss of chloride (Cl) d. Hyperventilation ANS: C When acid loss is caused by vomiting, renal compensation is not very effective because loss of Cl stimulates renal retention of bicarbonate, leading to alkalosis. Retention of metabolic acids would lead to acidosis, not alkalosis. Hypoaldosteronism leads to hyponatremia and does not cause alkalosis. Hyperventilation leads to respiratory alkalosis, not metabolic alkalosis. Cognitive Level: Comprehension 113 30. Which patient should the nurse assess for both hyperkalemia and metabolic acidosis? A patient diagnosed with: a. Diabetes insipidus b. Pulmonary disorders c. Cushing syndrome d. Renal failure ANS: D Renal failure is associated with hyperkalemia and metabolic acidosis. Diabetes insipidus results in hypernatremia. Pulmonary disorders are a cause of respiratory acidosis or alkalosis but do not affect hyperkalemia. Cushing syndrome results in hypernatremia. Cognitive Level: Comprehension 113 31. For a patient experiencing metabolic acidosis, the body will compensate by: a. Excreting H+ through the kidneys b. Hyperventilating c. Retaining CO2 in the lungs d. Secreting aldosterone ANS: B In an attempt to compensate for metabolic acidosis, the lungs hyperventilate to blow off CO2. It is the lungs hyperventilating that would compensate for metabolic acidosis, not the kidneys. CO2 retention would increase the acidotic state. Aldosterone would conserve water, but does not help compensate for acidosis. REF: pp. 112-113 32. Which finding would support the diagnosis of respiratory acidosis? a. Vomiting b. Hyperventilation c. Pneumonia d. An increase in noncarbonic acids ANS: C Respiratory acidosis occurs with hypoventilation, and pneumonia leads to hypoventilation. Vomiting leads to loss of acids and then to alkalosis. Hyperventilation leads to respiratory alkalosis, not acidosis. Metabolic acidosis is caused by an increase in noncarbonic acids. Cognitive Level: Comprehension 114 33. A 54-year-old male with a long history of smoking complains of excessive tiredness, shortness of breath, and overall ill feelings. Lab results reveal decreased pH, increased CO2, and normal bicarbonate ion. These findings help to confirm the diagnosis of: a. Respiratory alkalosis b. Metabolic acidosis c. Respiratory acidosis d. Metabolic alkalosis ANS: C A decreased pH indicates acidosis. With increased CO2, it is respiratory acidosis. The decreased pH indicates acidosis, not alkalosis. It is acidosis, but the bicarbonate is normal, so it cannot be metabolic. The decreased pH indicates acidosis, not alkalosis. Cognitive Level: Comprehension 114 34. For a patient with respiratory acidosis, chronic compensation by the body will include: a. Kidney excretion of H+ b. Kidney excretion of HCO3 c. Prolonged exhalations to blow off CO2 d. Protein buffering ANS: A The kidneys excrete H+ to compensate for respiratory acidosis. The kidneys do not excrete HCO3 to compensate; this would increase acidosis. Prolonged exhalations would not be effective for compensation, especially in a chronic state. Protein buffering is intracellular and will not be effective enough to compensate for respiratory acidosis. Cognitive Level: Comprehension 114 35. A 55-year-old female presents to her primary care provider and reports dizziness, confusion, and tingling in the extremities. Blood tests reveal an elevated pH, decreased PCO2, and slightly decreased HCO3. Which of the following is the most likely diagnosis? a. Respiratory alkalosis with renal compensation b. Respiratory acidosis with renal compensation c. Metabolic alkalosis with respiratory compensation d. Metabolic acidosis with respiratory compensation ANS: A With an elevated pH, the diagnosis must be alkalosis. Since the PCO2 is low, it is likely respiratory with a slight decrease in HCO3 indicating renal compensation. With an elevated pH, the diagnosis must be alkalosis, not acidosis. With an elevated pH, the diagnosis must be alkalosis. Since the PCO2 is low, it is likely respiratory since the HCO3 is decreased. With an elevated pH, the diagnosis must be alkalosis. Cognitive Level: Comprehension 115 36. Outcomes of laboratory tests include an elevated level of natriuretic peptides. Which organ is the priority assessment? a. Lungs b. Heart c. Liver d. Brain ANS: B Elevated natriuretic peptides indicate problems with the heart or the vasculature. Elevated natriuretic peptides indicate problems with the heart or the vasculature, not the lungs. Elevated natriuretic peptides indicate problems with the heart or the vasculature, not the liver. Elevated natriuretic peptides indicate problems with the heart or the vasculature, not the brain. Cognitive Level: Comprehension 103 MULTIPLE RESPONSE 1. A 60-year-old male with a 30-year history of smoking is diagnosed with a hormone-secreting lung tumor. Further testing indicates that the tumor secretes ADH. Which of the following assessment findings should the nurse expect? (Select all that apply.) a. Confusion b. Weakness c. Nausea d. Muscle twitching e. Weight loss ANS: A, B, C, D Secretion of ADH leads to water intoxication with symptoms of cerebral edema, with confusion and convulsions; weakness; nausea; muscle twitching; headache; and weight gain, not loss. Cognitive Level: Comprehension 107 2. The nurse would anticipate the patient with syndrome of inappropriate ADH (SIADH) to demonstrate which of the following symptoms? (Select all that apply.) a. Weakness b. Nausea c. Headache d. Weight loss e. Muscle twitching ANS: A, B, C, E Weakness, nausea, muscle twitching, headache, and weight gain, not loss, are common symptoms of chronic water accumulation. Chapter 6. Innate Immunity: Inflammation and Wound Healing MULTIPLE CHOICE 1. A public health nurse is teaching the community about health promotion. Which information should the nurse include for innate immunity? Innate immunity is gained: a. Following an illness b. At birth c. Via injection of specific antibodies d. In adulthood ANS: B Innate immunity is present at birth. Innate immunity is present at birth and does not require an illness. Innate immunity is present at birth and does not require injection. Innate immunity is present at birth. Cognitive Level: Comprehension 119 2. Which statement indicates teaching was successful regarding collectins? Collectins are produced by the: a. Kidneys b. Bowel c. Lungs d. Integument ANS: C Collectins are produced by the lungs. Collectins are produced by the lungs, not the kidneys. Collectins are produced by the lungs, not the bowel. Collectins are produced by the lungs, not the integument. Cognitive Level: Comprehension 119 3. A 20-year-old male received a knife wound to the arm during an altercation. Which of the following types of immunity was compromised? a. Innate immunity b. Inflammatory response c. Adaptive immunity d. Specific immunity ANS: A The epithelial cells of the skin are a part of innate immunity. The inflammatory response is not a type of immunity. Adaptive immunity is represented by the normal flora of the bowel. Specific immunity is a type of adaptive immunity and is not associated with a break in skin integrity. Cognitive Level: Comprehension 120 4. Biochemical secretions that trap and kill microorganisms include: a. Hormones b. Neurotransmitters c. Earwax d. Gastric acid ANS: C Epithelial cells secrete several substances that protect against infection, including earwax. Hormones do not contain biochemical secretions that trap and kill microorganisms. Neurotransmitters carry important messages, but they do not contain biochemical secretions. Gastric acid helps break down food into its component parts, but does not contain biochemical secretions. Cognitive Level: Comprehension 120 5. A 25-year-old female presents to her primary care provider reporting vaginal discharge of a white, viscous, and foul-smelling substance. She reports that she has been taking antibiotics for the past 6 months. Which finding will the nurse most likely see on the microorganism report? a. Clostridium difficile overgrowth b. Decreased Lactobacillus c. Streptococcus overgrowth d. Decreased Candida albicans ANS: B Diminished colonization with Lactobacillus that occurs as a result of prolonged antibiotic treatment increases the risk for vaginal infections, such as vaginosis. Clostridium difficile occurs in the colon, not the vagina. Streptococcus overgrowth will occur in the mouth. Candida albicans occurs in the colon, not the vagina. Cognitive Level: Comprehension 120 6. When an aide asks the nurse what is a purpose of the inflammatory process, how should the nurse respond? a. To provide specific responses toward antigens b. To lyse cell membranes of microorganisms c. To prevent infection of the injured tissue d. To create immunity against subsequent tissue injury ANS: C One purpose of the inflammatory process is to prevent infection and further damage by contaminating microorganisms. Specific response toward antigens is a part of the complement system that assists in the inflammatory response, but not its purpose. Lysis of cell membranes is part of the process of phagocytosis, which removes foreign material, but this is not the purpose of the inflammatory response. Immunity cannot be achieved against future tissue injury. Cognitive Level: Comprehension 121 7. A child fell off the swing and scraped the right knee. The injured area becomes painful. What else will the nurse observe upon assessment? a. Vasoconstriction at injured site b. Decreased RBC concentration at injured site c. Pale skin at injured site d. Edema at injured site ANS: D Increased vascular permeability and leakage of fluid out of the vessel cause edema at the site of injury. Vasodilation occurs, not vasoconstriction. Increased RBCs come to the site, not fewer. Redness occurs, not paleness, during inflammation. Cognitive Level: Comprehension 121 8. A nurse recalls the mast cell, a major activator of inflammation, initiates the inflammatory response through the process of: a. Chemotaxis b. Endocytosis c. Degranulation d. Opsonization ANS: C Degranulation of mast cells is a major cellular component of inflammation. Chemotaxis is the process of white cell migration. Endocytosis is a part of phagocytosis and is not a factor in mast cell response. Opsonization is part of phagocytosis and is not a factor in mast cell response. Cognitive Level: Comprehension 127 9. Which of the following individuals would be at greatest risk for an opportunistic infection? a. 18-year-old with diabetes b. 70-year-old with congestive heart failure c. 24-year-old who is immunocompromised d. 30-year-old with pneumonia ANS: C Opportunistic microorganisms can cause disease if the individuals defenses are compromised. An 18-year-old with diabetes would not be immunocompromised and would not be at risk. A 70-year-old with congestive heart failure would not be immunocompromised and would not be at risk. A 30-year-old with pneumonia would not be immunocompromised and would not be at risk. Cognitive Level: Comprehension 120 10. The directional migration of leukocytes along a chemical gradient is termed: a. Chemotaxis b. Endocytosis c. Margination d. Diapedesis ANS: A Chemotaxis is the process by which leukocytes undergo directed migration. Endocytosis is a form of engulfment and a part of phagocytosis. Margination occurs when leukocytes adhere to endothelial cells in the walls of vessels. Diapedesis is the emigration of the cells through cell junctions that have loosened in response to inflammatory mediators. Cognitive Level: Comprehension 131 11. A 20-year-old male shoots his hand with a nail gun while replacing roofing shingles. Which of the following cell types would be the first to aid in killing bacteria to prevent infection in his hand? a. Eosinophils b. Neutrophils c. Leukotrienes d. Monocytes ANS: B Neutrophils are the predominant phagocytes in the early inflammatory site, arriving within 6 to 12 hours after the initial injury. Eosinophils help limit and control inflammation. Leukotrienes are activators of the inflammatory response. Monocytes enter much later and replace leukocytes. Cognitive Level: Comprehension 129 12. The predominant phagocyte of early inflammation is the: a. Eosinophil b. Neutrophil c. Lymphocyte d. Macrophage ANS: B Neutrophils are the predominant phagocytes in the early inflammatory site, arriving within 6 to 12 hours after the initial injury. Eosinophils help limit and control inflammation, but they are not the prominent phagocyte. Lymphocytes are part of the innate immune response. Macrophages kill microorganisms. Cognitive Level: Comprehension 129 13. A 25-year-old female experiences a headache and takes aspirin for relief. A nurse recalls aspirin relieves the headache by: a. Decreasing leukotriene production b. Increasing histamine release c. Decreasing prostaglandin production d. Increasing platelet-activating factor ANS: C Aspirin is a prostaglandin inhibitor. Aspirin inhibits prostaglandins; it does not affect leukotriene production. Aspirin inhibits prostaglandins; it does not affect histamine release. Aspirin does not play a role in the platelet activating factor; this is a leukotriene response. Cognitive Level: Comprehension 129 14. Which factor will help the nurse differentiate leukotrienes from histamine? a. Site of production b. Vascular effect c. Chemotactic ability d. Time of release ANS: D Leukotrienes are released slower and longer than histamine. Leukotrienes and histamine are produced from mast cells. Leukotrienes and histamine have similar vascular effects. Leukotrienes and histamine have similar chemotactic ability. Cognitive Level: Comprehension 129 15. A 25-year-old male is in a car accident and sustains a fracture to his left femur with extensive soft tissue injury. The pain associated with the injury is related to: a. Histamine and serotonin b. Kinins and prostaglandins c. Vasoconstriction d. Immune complex formation ANS: B Prostaglandins cause increased vascular permeability, neutrophil chemotaxis, and pain by direct effects on nerves. Kinins also promote pain. Prostaglandins produce pain; histamine promotes vasodilation. Prostaglandins produce pain, not vasoconstriction. Prostaglandins produce pain, not the immune complex. Cognitive Level: Comprehension 129 16. The complement, clotting, and kinin systems share which of the following characteristics? a. Activation of a series of proenzymes b. Phagocytosis initiation c. Granulocyte production d. Activated by interferon ANS: A The complement system, the clotting system, and the kinin system are normally in inactive forms, but can activate in a series as proenzymes and are involved in the inflammatory process. The complement system, the clotting system, and the kinin system do not play a role in phagocytosis, but do play a role in the inflammatory response as proenzymes. The complement system, the clotting system, and tje kinin system do not play a role in granulocyte production, but they function as proenzymes in the inflammatory response. The complement system, the clotting system, and the kinin system are not activated by interferon, but are activated by enzymatic action. Cognitive Level: Comprehension 122 17. Which statement indicates teaching was successful regarding the classic pathway of the complement system? The classic pathway of the complement system is activated by: a. Histamine b. Antigen-antibody complexes c. Leukotrienes d. Prostaglandins ANS: B The classic pathway of the complement system is activated by antibodies of the immune system. The classic pathway of the complement system is activated by antibodies, not by histamine. The classic pathway of the complement system is activated by antibodies, not by leukotrienes. The classic pathway of the complement system is activated by antibodies, not by prostaglandins. Cognitive Level: Comprehension 123 18. A patient has researched bradykinin on the Internet. Which information indicates the patient understands the functions of bradykinin? Bradykinin is involved in: a. Increasing vascular permeability b. Vasoconstricting blood vessels c. Stimulating the clotting system d. Increasing degradation of prostaglandins ANS: A Bradykinin increases vascular permeability. Bradykinin increases vascular permeability; it does not promote vasoconstriction. Bradykinin increases vascular permeability; it does not stimulate clotting. Bradykinin promotes pain; thus, it does not degrade prostaglandins but supports them. Cognitive Level: Comprehension 124 19. After teaching the staff about the clotting system, which statement indicates teaching was successful? The end product of the clotting system is: a. Plasmin b. Fibrin c. Collagen d. Factor X ANS: B The end product of the clotting system is fibrin. Plasmin activates the complement cascade. Collagen plays a factor in wound healing. Factor X is a first step in the clotting system. Cognitive Level: Comprehension 124 20. A 5-year-old male is diagnosed with a bacterial infection. Cultures of the bacteria revealed lipopolysaccharides on the bacterial cell surface. Which of the complement pathways would be activated in this case? a. Classical pathway b. Lectin pathway c. Alternative pathway d. Kinin pathway ANS: C The alternative pathway is activated by several substances found on the surface of infectious organisms, such as those containing lipopolysaccharides. The classical pathway is primarily activated by antibodies that are proteins of the acquired immune system. The lectin pathway is similar to the classic pathway but is independent of antibody. It is activated by several plasma proteins. The kinin pathway is involved in coagulation. Cognitive Level: Comprehension 124 21. An 8-year-old female presents with edema of the cutaneous and mucosal tissue layers. Her mother reports that the condition is recurrent and seems to occur more often during stressful situations. The child is diagnosed with hereditary angioedema. Which of the following is deficient in this child? a. C1 esterase inhibitor b. Carboxypeptidase c. Neutrophils d. Plasmin ANS: A A genetic defect in C1 esterase inhibitor (C1 INH deficiency) results in hereditary angioedema. Hereditary angioedema is due to C1 esterase inhibitor. Carboxypeptidase degrades kinins. Hereditary angioedema is due to C1 esterase inhibitor, not a disorder of neutrophils. Plasmin is not associated with hereditary angioedema, but is associated with clots. Cognitive Level: Comprehension 124 22. A nurse is preparing to teach on the subject of opsonins. Which information should the nurse include? Opsonins are molecules that: a. Are composed of fatty acids b. Regulate inflammation c. Degranulate mast cells d. Enhance phagocytosis ANS: D Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. Opsonins are not composed of fatty acids; they are antibodies. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. They do not regulate inflammation; mast cells do. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized; they do not react with mast cells. Cognitive Level: Comprehension 122 23. A 10-year-old male is diagnosed with a parasite. Which lab result should the nurse check for a response to the parasite? a. Monocytes b. Eosinophils c. Neutrophils d. Macrophages ANS: B Eosinophils serve as the bodys primary defense against parasites. Monocytes are not the bodys primary defense against parasite; eosinophils are. Monocytes are phagocytic. Neutrophils are phagocytic; they are not the bodys defense against parasites. Macrophages are not active against parasites; they act as long-term defense against infections. Cognitive Level: Comprehension 131 24. A 65-year-old female is diagnosed with metastatic breast cancer. She has developed muscle wasting. Which of the following substances would be produced in large quantities to eliminate the tumor cells and cause muscle wasting? a. Interleukin-6 b. Eosinophils c. Tumor necrosis factor d. Platelets ANS: C Tumor necrosis factor causes muscle wasting. Interleukin-6 stimulates growth and differentiation of blood cells. Eosinophils are stimulated for parasites. Platelets stimulate clotting. Cognitive Level: Comprehension 127 25. When phagocytes begin to stick avidly to capillary walls, which process is occurring? a. Margination b. Exudation c. Integration d. Emigration ANS: A Both leukocytes and endothelial cells secrete substances that increase adhesion, or stickiness, causing the leukocytes to adhere more avidly to the endothelial cells in the walls of the capillaries and venules in a process called margination. Exudation is the process of pus formation and does not result in stickiness. Integration occurs in cells but is not a major function and does not lead to stickiness. Emigration is similar to diapedesis and is not associated with increased stickiness. Cognitive Level: Comprehension 131 26. An infant develops a fever secondary to a bacterial infection. Which of the following most likely triggered the fever? a. Interleukin-1 b. Interleukin-6 c. Interleukin-10 d. Interferons (INFs) ANS: A Interleukin-1 is responsible for fever production. Interleukin-6 stimulates growth and differentiation of blood cells. Interleukin-10 helps decrease the immune response. INFs are members of a family of cytokines that protect against viral infections. Cognitive Level: Comprehension 126 27. A 54-year-old male intravenous (IV) drug user is diagnosed with chronic hepatitis C. Testing revealed that he is a candidate for treatment. Which of the following could be used to treat his condition? a. Interleukin-1 b. Interleukin-6 c. Interleukin-10 d. INFs ANS: D INFs are members of a family of cytokines that protect against viral infections. Interleukin-1 is responsible for fever production. Interleukin-6 stimulates growth and differentiation of blood cells. Interleukin-10 helps decrease the immune response. Cognitive Level: Comprehension 127 28. A 35-year-old male is diagnosed with lobar pneumonia (lung infection). Which of the following exudates would be present in highest concentration at the site of this advanced inflammatory response? a. Serous b. Purulent c. Hemorrhagic d. Fibrinous ANS: D Fibrinous exudates occur in the lungs of individuals with pneumonia. Serous fluid is watery fluid, as in a blister. Purulent is characterized by an abscess, such as pus. Hemorrhagic occurs when the exudates are filled with erythrocytes. Cognitive Level: Comprehension 132 29. During inflammation, the liver is stimulated to release plasma proteins, collectively known as: a. Opsonins b. Acute phase reactants c. Antibodies d. Phagolysosome ANS: B The synthesis of many plasma proteins by the liver is increased during inflammation. These proteins, which can be either proinflammatory or antiinflammatory in nature, are referred to as acute phase reactants. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. Antibodies are proteins of the immune system. Phagolysosome destroys bacterium. Cognitive Level: Comprehension 133 30. A 3-year-old is making play cakes in a sandbox and is eating the play cakes. The sand was also being used by cats as a litter box and was contaminated with toxoplasmosis. Which of the following would most likely also be present? a. Granuloma formation b. Degranulation c. Blood clots d. Exudate production ANS: A Infections caused by bacteria such as toxoplasmosis can result in granuloma formation. Degranulation is a part of mast cell destruction. Blood clots are not expected with chronic inflammation. Exudate production is pus formation. Cognitive Level: Comprehension 134 31. A 12-year-old male is fighting with another child when he receives a puncture wound from a pencil. The school nurse cleans and bandages the wound. After about 1 week, the wound would be in which phase of healing? a. Debridement b. Primary intention c. Resolution d. Maturation ANS: C Resolution occurs when repaired tissue is approaching close to normal. Debridement is the scraping away of dead tissue and is not a phase of wound healing. Primary intention is the stage of healing of wounds that are closely proximated. Maturation is the result of severe wounds which would begin several weeks after injury and may take 2 years. Cognitive Level: Comprehension 134 32. The macrophage secretion that stimulates procollagen synthesis and secretion is: a. Angiogenesis factor b. Matrix metalloproteinase c. Vascular endothelial growth factor d. Transforming growth factor-beta ANS: D Macrophages secrete transforming growth factor-beta to stimulate fibroblasts to secrete the collagen precursor procollagen. Chapter 7. Adaptive Immunity MULTIPLE CHOICE 1. Which of the following is responsible for initiating clonal selection? a. T cells b. B cells c. Antigens d. Lymphocytes ANS: C The lymphocytes remain dormant until an antigen initiates clonal selection. T cells are part of the immune response, but do not initiate clonal selection. B cells are antibodies. Lymphocytes are released into the circulation as immature cells that react with antigens. Cognitive Level: Comprehension 144 2. After teaching the students about B cells, which statement indicates teaching was successful? B cells are originally derived from cells of the: a. Bone marrow b. Lymph nodes c. Gut-associated lymphoid tissue d. Thymus ANS: A B cells are derived from the bone marrow. B cells are derived from the bone marrow, not the lymph nodes. B cells are derived from the bone marrow, not the gut-associated lymphoid tissue. B cells are derived from the bone marrow, not the thymus. Cognitive Level: Comprehension 147 3. A 6-year-old female is diagnosed with a bacterial infection of the respiratory system. Which of the following will most likely try to fight the antigen? a. Antibodies b. Cytotoxic T cells c. Self-antigens d. Helper T cells ANS: A Antibodies are produced by plasma cells that mature from lymphocytes, called B lymphocytes (B cells), in response to an antigen. Antibodies are produced by plasma cells that mature from lymphocytes, called B lymphocytes (B cells), in response to an antigen. Cytotoxic T cells do not respond to antigens. Antibodies are produced by plasma cells that mature from lymphocytes, called B lymphocytes (B cells), in response to an antigen. Self-antigens do not respond to antigens. Antibodies are produced by plasma cells that mature from lymphocytes, called B lymphocytes (B cells), in response to an antigen. Helper T cells do not respond to antigens. Cognitive Level: Comprehension 147 | p. 149 4. When the immunoglobulin crosses the placenta, what type of immunity does the fetus receive? a. Active b. Passive c. Innate d. Cell-mediated ANS: B Maternal antibodies that pass across the placenta into the fetus before birth provide passive systemic immunity. Maternal antibodies that pass across the placenta into the fetus before birth provide passive systemic immunity, not active immunity. Maternal antibodies that pass across the placenta into the fetus before birth provide passive systemic immunity, not innate immunity. Maternal antibodies that pass across the placenta into the fetus before birth provide passive systemic immunity, not cell-mediated immunity. Cognitive Level: Comprehension 145 5. An immunologist has isolated a molecule from the human body to study. It is found to react with antibodies on B cells. Further testing reveals that the molecule is large and chemically diverse. What type of molecule is the immunologist studying? a. Antigen b. Immunogen c. Epitope d. Paratope ANS: A Antibodies react with antigens. Antibodies react with antigens, not immunogen. Antibodies react with antigens, not epitopes. Antibodies react with antigens, not paratopes. Cognitive Level: Comprehension 147 6. Which statement indicates a correct understanding of antibodies? The most abundant class of antibody in the serum is: a. IgG b. IgM c. IgA d. IgE ANS: A IgG is the most abundant class of immunoglobulins, constituting 80% to 85% of the immunoglobulins in the blood. IgG is the most abundant class of immunoglobulins, not IgM. IgG is the most abundant class of immunoglobulins, not IgA. IgG is the most abundant class of immunoglobulins, not IgE. Cognitive Level: Comprehension 147 7. The predominant antibody of a typical primary immune response is: a. IgG b. IgM c. IgA d. IgE ANS: B IgM is the largest immunoglobulin and is the first antibody produced during the initial, or primary, response to antigen. IgM, not IgG, is the largest immunoglobulin and is the first antibody produced during the initial, or primary, response to antigen. IgM, not IgA, is the largest immunoglobulin and is the first antibody produced during the initial, or primary, response to antigen. IgM, not IgE, is the largest immunoglobulin and is the first antibody produced during the initial, or primary, response to antigen. Cognitive Level: Comprehension 147 8. An immunology nurse is caring for a patient. While planning care, which principle will the nurse remember? The primary role of IgA1 is to prevent infections in the: a. Blood b. Kidneys c. Lungs d. Mucous membranes ANS: A IgA1 is found predominantly in the blood. IgA1 is found predominantly in the blood, not the kidneys. IgA1 is found predominantly in the blood, not the lungs. IgA1 is found predominantly in the blood, not the mucous membranes. Cognitive Level: Comprehension 147 9. A 23-year-old pregnant female visits her primary care provider for her final prenatal checkup. The primary care provider determines that the fetus has developed an infection in utero. Which of the following would be increased in the fetus at birth? a. IgG b. IgA c. IgM d. IgD ANS: C IgM is synthesized early in neonatal life, and its synthesis may be increased as a response to infection in utero. IgM, not IgG, is synthesized early linlinfee,oannadtaits synthesis may be increased as a response to infection in utero. IgM, not IgA, is synthesized early in neonatal life, and its synthesis may be increased as a response to infection in utero. IgM, not IgD, is synthesized early in neonatal life, and its synthesis may be increased as a response to infection in utero. Cognitive Level: Comprehension 149 10. Which portion of the antibody is responsible for the biologic functions of antibodies? a. Heavy chain b. Variable region c. Fc portion d. Epitope ANS: C The Fc portion is responsible for most of the functions of antibodies. The Fc portion is responsible for most of the functions of antibodies, not the heavy chain. The Fc portion is responsible for most of the functions of antibodies, not the variable region. The Fc portion is responsible for most of the functions of antibodies, not the epitope. Cognitive Level: Comprehension 149 11. An experiment is carried out to characterize newly discovered immunoglobulins. Specificity of the amino acids within the immunoglobulin could be determined by studying the: a. C region of the light chain b. C region of the H chain c. Complementary-determining region (CDR) d. Framework regions ANS: C The amino acid differences are clustered into three areas in the variable region. These three areas are called CDRs. The amino acid differences are clustered into three areas in the variable region. These three areas are called CDRs, not the C region of the light chain. The amino acid differences are clustered into three areas in the variable region. These three areas are called CDRs, not the C region of the H chain. The amino acid differences are clustered into three areas in the variable region. These three areas are called CDRs, not the framework regions. Cognitive Level: Comprehension 149 12. A 20-year-old female is applying for nursing school and is required to be tested for immunity against several illnesses. Testing that looks at which of the following would be the best to determine immunity? a. Culture and sensitivity b. Agglutination c. Precipitation d. Titer ANS: D The amount of antibody in a serum sample is referred to as the titer; a higher titer indicates more antibodies. Culture and sensitivity determine the type of organism that causes an infection, and sensitivity identifies the antibody it is sensitive to. The amount of antibody in a serum sample is referred to as the titer, not agglutination. The amount of antibody in a serum sample is referred to as the titer, not precipitation. Cognitive Level: Comprehension 155 13. A 10-year-old male is stung by a bee while playing in the yard. He experiences a severe allergic reaction and has to go to the ER. The nurse providing care realizes this reaction is the result of: a. Toxoids b. IgA c. IgE d. IgM ANS: C IgE is normally at low concentrations in the circulation. It has very specialized functions as a mediator of many common allergic responses. IgE, not toxoids, is the mediator of common allergic response. IgE, not IgA, is the mediator of common allergic response. IgE, not IgM, is the mediator of common allergic response. Cognitive Level: Comprehension 151 14. A 25-year-old female has sexual relations with her boyfriend. Later she is told that the boyfriend is infected with Neisseria gonorrhoeae. Testing reveals that she does not have the disease. How is it possible that she did not contract the disease? a. Antibodies covered sites of attachment. b. She was vaccinated against it. c. Platelets provided protection. d. IgE was released. ANS: A Some bacteria, such as Neisseria gonorrhoeae that causes gonorrhea, must attach to specific sites on urogenital epithelial cells. Antibodies may protect the host by covering sites on the microorganism that are needed for attachment, thereby preventing infection. The patient did not contract the disease because antibodies covered sites of attachment, not because of vaccination. The patient did not contract the disease because antibodies covered sites of attachment, not because of platelets. The patient did not contract the disease because antibodies covered sites of attachment, not because of IgE release. Cognitive Level: Comprehension 150 15. Which of the following characteristics is shared by both the secretory and systemic immune systems? a. Lymphocytic paths of migration b. Neutralization following antigen-antibody binding c. Timing of response d. Location of response ANS: B Direct effects result from the binding of antibody directly to a harmful antigen or infectious agent. These include inhibition of processes that are necessary for infection, such as the reaction of an infectious agent with a particular cell in the body or neutralization of harmful bacterial toxins. The effect of the immune system is neutralization, not lymphocytic paths of migration. The effect of the immune system is neutralization, not timing of response. The effect of the immune system is neutralization, not location of response. Cognitive Level: Comprehension 150 16. A patient has done research on monoclonal antibodies on the Internet. Which statement indicates a correct understanding? Pure monoclonal antibodies are produced by: a. T lymphocytes b. Bone marrow c. Laboratories d. Fetuses ANS: C Monoclonal antibodies are produced in the laboratory from one B cell that has been cloned; thus, the entire antibody is of the same class, specificity, and function. Monoclonal antibodies are produced in the laboratory, not by T lymphocytes. Monoclonal antibodies are produced in the laboratory, not by the bone marrow. Monoclonal antibodies are produced in the laboratory, not by the fetus. Cognitive Level: Comprehension 155 17. An experiment is designed to determine specific cell types involved in cell-mediated immune response. The experimenter is interested in finding cells that attack cells that have specific antigens. Which cells should be isolated? a. Lymphokine-producing cells b. Cytotoxic T cells c. Helper T cells d. Macrophages ANS: B Cell-mediated immunity is driven by T-cytotoxic (Tc) cells that attack antigens directly and destroy cells that bear foreign antigens. Cell-mediated immunity is driven by T-cytotoxic (Tc) cells, not lymphokine-producing cells, that attack antigens directly and destroy cells that bear foreign antigens. Cell-mediated immunity is driven by T-cytotoxic (Tc) cells, not helper T cells, that attack antigens directly and destroy cells that bear foreign antigens. Cell-mediated immunity is driven by T-cytotoxic (Tc) cells, not macrophages, that attack antigens directly and destroy cells that bear foreign antigens. Cognitive Level: Comprehension 144 18. Which of the following statements indicates more teaching is needed regarding secondary lymph organs? is/are a secondary lymph organ. a. The spleen b. Peyer patches c. Adenoids d. The liver ANS: D The liver is not a secondary lymph organ. The spleen is a secondary lymphoid organ. Peyer patches are a secondary lymph organ. The adenoids are a secondary lymph organ. Cognitive Level: Comprehension 155 19. After a patient is exposed to a specific antigen, B cells will differentiate into: a. B cytotoxic cells b. Clonal equivalents c. Plasma cells d. Bursal cells ANS: C The B cell differentiates into plasma cells. The B cell differentiates into plasma cells, not B cytotoxic cells. The B cell differentiates into plasma cells, not clonal equivalents. The B cell differentiates into plasma cells, not bursal cells. Cognitive Level: Comprehension 158 20. A macrophage was isolated and analyzed for major histocompatibility complex. Which of the following would be expected? a. MHC I only b. MHC II only c. MHC I and II d. Neither MHC I or MHC II ANS: C MCH I and II would be expected. MCH I and II would be expected. MCH I and II would be expected. Both MCH I and II would be expected. Cognitive Level: Comprehension 157 21. A cell that is produced in the thymus and interacts with MHC class II molecules would have which of the following surface proteins? a. CD4 b. CD8 c. Th1 d. Superantigen ANS: A CD4-positive Th cells are restricted to interactions with cells presenting antigen by MHC class II molecules. CD4-positive Th, not CD8, cells are restricted to interactions with cells presenting antigen by MHC class II molecules. CD4-positive Th, not Th1, cells are restricted to interactions with cells presenting antigen by MHC class II molecules. CD4-positive Th, not superantigen, cells are restricted to interactions with cells presenting antigen by MHC class II molecules. Cognitive Level: Comprehension 158 22. A 6-month-old infant is brought to the pediatrician for recurrent colds. The child is fed formula, and the other family members have not been ill. The primary care provider tells the mother that the childs immune system is not yet competent, but will be about 60% of an adult system around age months. a. 3 b. 6 c. 9 d. 12 ANS: D The child has an immune system of about 60% of the adult by age 12 months. The child has an immune system of about 60% of the adult by age 12 months, not 3 months. The child has an immune system of about 60% of the adult by age 12 months, not 6 months. The child has an immune system of about 60% of the adult by age 12 months, not 9 months. Cognitive Level: Comprehension 164 23. A 5-month-old child is admitted to the hospital with recurring respiratory infections. A possible cause of this condition is: a. Hypergammaglobulinemia b. Increased maternal IgG c. Immune insufficiency d. Decreased maternal antibody breakdown, resulting in hyposensitivity ANS: C Normal human infants are immunologically immature when born, with deficiencies in antibody production, phagocytic activity, and complement activity, especially components of alternative pathways. Normal human infants are immunologically immature when born. They do not posses hypergammaglobulinemia. Possessing increased maternal IgG would not lead to recurring infections. The recurrent infections are due to decreased immunity, not maternal antibody breakdown. Cognitive Level: Comprehension 164 24. Which patient will develop active immunity? A patient who: a. Has natural exposure to an antigen or receives an immunization b. Receives preformed antibodies or T cells from a donor c. Has T cells that become B cells d. Receives immunoglobulin ANS: A Active immunity occurs after either natural exposure to an antigen or after immunization. Active immunity occurs after either natural exposure to an antigen or after immunization, not with preformed antibodies. Active immunity occurs after either natural exposure to an antigen or after immunization, not when T cells become B cells. Active immunity occurs after either natural exposure to an antigen or after immunization, not when the patient receives immunoglobulins. Cognitive Level: Comprehension 144 25. A 16-year-old is bitten by a rabid dog while jogging in the park. Upon admission to the emergency department, the nurse will administer which of the following to help prevent infection? a. Cytotoxic T cells b. Helper T cells c. Macrophages d. Immune globulin ANS: D Unvaccinated individuals who are exposed to particular infectious agents often will be given immune globulins, which are prepared from individuals who already have antibodies against that particular pathogen. The patient would be given immune globulin, not cytotoxic T cells. The patient would be given immune globulin, not helper T cells. The patient would be given immune globulin, not macrophages. Cognitive Level: Comprehension 145 26. Self-antigens do not meet the requirements for immunogenicity because they lack which of the following? a. Foreignness b. Size c. Quantity d. Virulence ANS: A A self-antigen that fulfills all the criteria listed above except foreignness does not normally elicit an immune response. A self-antigen fulfills all the criteria listed above except foreignness. They possess size. A self-antigen fulfills all the criteria listed above except foreignness. They possess quantity. Virulence is not a factor. Cognitive Level: Comprehension 145 27. A patient has a disease state that results from the secretion of toxins by bacteria. Which medical diagnosis will the nurse see documented on the chart? a. Malaria b. Tetanus c. Smallpox d. Hepatitis ANS: B Some bacteria secrete toxins that harm individuals. For instance, specific bacterial toxins cause the symptoms of tetanus or diphtheria. Tetanus, not malaria, is due to toxin secretion. Tetanus, not smallpox, is due to toxin secretion. Tetanus, not hepatitis, is due to toxin secretion. Cognitive Level: Comprehension 150 MULTIPLE RESPONSE 1. While planning care for an elderly patient, the nurse remembers that increased age is associated with (select all that apply): a. Increased T cell function b. Decreased immune function c. Increased production of antibodies d. Decreased numbers of circulating immune complexes e. Decreased ability to fight infection ANS: B, D, E Increased age is associated with diminished T cell function, decreased immune function, diminished production of antibody responses, decreased circulating immune complexes, and decreased ability to fight infection. Cognitive Level: Comprehension 164 2. When a patient asks about secondary lymph organs, how should the nurse respond? Secondary lymph organs include (select all that apply): a. Spleen b. Peyer patches c. Adenoids d. Liver e. Bone marrow f. Appendix ANS: A, B, C, F The secondary lymphoid organs include the spleen, lymph nodes, adenoids, tonsils, Peyer patches (intestines), and the appendix. The liver and bone marrow are not secondary lymph organs. Cognitive Level: Comprehension 155 3. Direct effects of antibodies include (select all that apply): a. Neutralization b. Agglutination c. Precipitation d. Phagocytosis e. Division ANS: A, B, C Directly, antibodies can affect infectious agents or their toxic products by neutralization (inactivating or blocking the binding of antigen to receptors), agglutination (clumping insoluble particles that are in suspension), or precipitation (making a soluble antigen into an insoluble precipitate). Indirectly, antibodies activate components of innate resistance, including complement and phagocytes. Antibodies are generally a mixed population of classes, specificities, and capacity to provide the functions listed above. Chapter 8. Alterations in Immunity 1. The mediators involved in type I hypersensitivity allergic responses are released from: A) mast cells. B) plasma cells. C) monocytes. D) arachidonic acid. 2. A genetically determined hypersensitivity to common environmental allergens causes reactions, such as: A) atopic; urticaria. B) autoimmune; diarrhea. C) IgM-mediated; infections. D) delayed; poison ivy rash: 3. Mismatched blood transfusion reaction with hemolysis of blood cells is an example of type II, mediated hypersensitivity reaction. A) T-cell B) antibody C) leukotriene D) complement 4. Type III hypersensitivity immune responses can be harmful when immune complex deposits in tissue activate that can directly damage area tissues. A) inflammation B) autoantibodies C) cytotoxic cells D) immunoglobulins 5. The mechanism by which humans recognize self-cells from non-self (antigens)-cells is . A) autoimmunity B) self-tolerance C) non-self anergy D) immunocompatibility 6. Organ rejection is a complication of organ transplantation caused by recipient immune cells: A) destroying the host T cells. B) attack on the donor cells. C) combining with grafts HLA. D) being recognized as foreign. 7. The leading cause of death for people with HIV is opportunistic . A) leukemia B) tuberculosis C) pneumonia D) toxoplasmosis 8. Wasting syndrome, an AIDS-defining illness, is characterized by involuntary weight loss of at least 10% of baseline body weight in the presence of: A) diarrhea. B) hypermetabolism. C) weakness and fever. D) glucose intolerance. 9. The window period of HIV infection refers to the period of time between infection and: A) transmission. B) seroconversion. C) initial symptoms. D) antibody screening. 10. HIV-positive persons that display manifestations of laboratory category 3 or clinical category C are considered to have: A) zero viral load. B) seroconversion. C) complete remission. D) AIDS-defining illnesses. 11. Contact with poison ivy has resulted in intense pruritus, erythema, and weeping on a patients forearm. Which of the following processes resulted in the patients signs and symptoms? A) IgE-mediated mast cell degranulation B) Formation of antigen-antibody complexes C) Cytokine release by sensitized T cells D) Formation of antibodies against cell surface antigens 12. A patient with a long history of hay fever has recently begun a series of immunotherapy (allergy shots). How will this treatment potentially achieve a therapeutic effect? A) By blocking cytokine release from sensitized mast cells B) By preventing mast cells from becoming sensitized C) By causing T cells to be sequestered in the thymus for longer periods D) By stimulating production of IgG to combine with antigens 13. A patient with a diagnosis of cirrhosis has experienced an acute rejection of a donor liver. Which of the following cells is central to the rejection of the patients transplanted organ? A) Natural killer cells B) Mast cells C) T cells D) Neutrophils 14. A patient with a diagnosis of aplastic anemia has undergone allogenic bone marrow transplantation. Which of the following signs and symptoms would most clearly suggest the existence of graft-versus-host disease (GVHD)? A) Shortness of breath, audible crackles, and decreasing PaO2 B) Presence of a pruritic rash that has begun to slough off C) Development of metabolic acidosis D) Diaphoresis, fever, and anxiety 15. A patient has developed pericarditis after developing acute glomerulonephritis, a development that may be attributable to the presence of similar epitopes on group A, b- hemolytic streptococci and the antigens in the patients heart tissue. Which of the following has most likely accounted for this patients autoimmune response? A) Breakdown of T-cell anergy B) Release of sequestered antigens C) Superantigens D) Molecular mimicry 16. A 70-year-old female patient has had her mobility and independence significantly reduced by rheumatoid arthritis. Which of the following processes likely contributed to the development of her health problem? A) Delayed-type hypersensitivity (DTH) reaction B) Proliferation of cytotoxic T cells C) Failure of normal self-tolerance D) Deletion of autoreactive B cells 17. Which of the following would constitute a normal assessment finding in a neonate? A) Minimal or absent levels of IgA and IgM B) Absence of plasma cells in the lymph nodes and spleen C) Undetectable levels of all immunoglobulins D) Absence of mature B cells with normal T-cell levels and function 18. A patient was diagnosed as HIV positive several years ago. Which of the following blood tests is most clinically useful for determining the stage and severity of her disease? A) Plasma levels B) CD4+ cell counts C) Viral load D) White blood cell count with differential 19. A patient has been admitted to the hospital for the treatment of HIV infection, which has recently progressed to overt AIDS. Which of the following nursing actions should the nurse prioritize when providing care for this patient? A) Frequent neurologic vital signs and thorough skin care B) Hemodynamic monitoring and physical therapy C) Careful monitoring of fluid balance and neurologic status D) Astute infection control and respiratory assessments 20. Shortly after being diagnosed with HIV, a patient has begun highly active antiretroviral therapy (HAART). What is the primary goal of the patients drug regimen? A) To limit the latent period of HIV B) To slow the progression of the disease C) To minimize opportunities for transmission D) To prevent seroconversion Answer Key 1. A 2. A 3. B 4. A 5. B 6. B 7. B 8. A 9. B 10. D 11. C 12. D 13. C 14. B 15. D 16. C 17. A 18. B 19. D 20. B Chapter 9. Infection and Defects in Mechanisms of Defense MULTIPLE CHOICE 1. When a patient asks the nurse what hypersensitivity is, how should the nurse respond? Hypersensitivity is best defined as: a. A reduced immune response found in most pathologic states b. A normal immune response to an infectious agent c. An excessive or inappropriate response of the immune system to a sensitizing antigen d. Antigenic desensitization ANS: C Hypersensitivity is an altered immunologic response to an antigen that results in disease or damage to the individual. Hypersensitivity is not a reduced immune response. Hypersensitivity is not a normal response to an infectious agent. Antigenic desensitization is performed to decrease hypersensitivity. Cognitive Level: Comprehension 165 2. A 5-year-old female takes a hike through the woods during a school field trip. Upon returning home, she hugs her father, and he later develops poison ivy. Which of the following immune reactions is he experiencing? a. IgE-mediated b. Tissue specific c. Immune complex d. Cell-mediated ANS: D Secondary contact activates a type IV cell-mediated reaction that causes dermatitis. The fathers response is a secondary, cell mediated, not a primary type IgE mediated. The fathers response is secondary, not tissue specific. The fathers response is a type IV, not an immune complex response. Cognitive Level: Comprehension 189 3. When the maternal immune system becomes sensitized against antigens expressed by the fetus, what type of immune reaction occurs? a. Autoimmune b. Anaphylaxis c. Alloimmune d. Allergic ANS: C Alloimmunity can be observed during immunologic reactions against transfusions, transplanted tissue, or the fetus during pregnancy. Autoimmunity is a disturbance in the immunologic tolerance of self-antigens. The most rapid and severe immediate hypersensitivity reaction is anaphylaxis. An allergic response occurs related to exposure to an allergen. Cognitive Level: Comprehension 190 4. While planning care, a nurse recalls seasonal allergic rhinitis is expressed through: a. IgE-mediated reactions b. Tissue-specific reactions c. Antigen-antibody complexes d. Type II hypersensitivity reactions ANS: A Seasonal allergic rhinitis is expressed through IgE-mediated reactions. Tissue-specific reaction is an autoimmune reaction. Antigen-antibody reactions are type III and are organ specific. Type II hypersensitivity reactions are tissue specific. Cognitive Level: Comprehension 190 5. A patient presents with poison ivy on the extremities, face, and buttocks. This condition is an example of: a. Anaphylaxis b. Serum sickness c. Delayed hypersensitivity d. Viral disease ANS: C The response to poison ivy is a delayed hypersensitivity because it takes up 72 hours to develop. Anaphylaxis is immediate. Serum sickness-type reactions are caused by the formation of immune complexes in the blood and their subsequent generalized deposition in target tissues. Poison ivy is not a viral disease. Cognitive Level: Comprehension 190 6. A 10-year-old male is stung by a bee while playing in the yard. He begins itching and develops pain, swelling, redness, and respiratory difficulties. He is suffering from: a. Immunodeficiency b. Autoimmunity c. Anaphylaxis d. Tissue-specific hypersensitivity ANS: C Anaphylaxis occurs within minutes of reexposure to the antigen and can be either systemic (generalized) or cutaneous (localized). Immunodeficiency is a decrease in the immune response. Autoimmunity is a disturbance in the immunologic tolerance of self-antigens. Tissue-specific reaction is an autoimmune reaction. Cognitive Level: Comprehension 190 7. When a patient presents at the emergency department for an allergic reaction, the nurse recognizes the most severe consequence of a type I hypersensitivity reaction is: a. Urticaria b. Hives c. Anaphylaxis d. Antibody-dependent cell-mediated cytotoxicity (ADCC) ANS: C The most rapid and severe immediate hypersensitivity type I reaction is anaphylaxis. Urticaria, or hives, is a dermal (skin) manifestation of allergic reactions. Hives and urticaria are similar responses. ADCC is a mechanism that involves natural killer (NK) cells. Antibodies on the target cell are recognized by Fc receptors on the NK cells, which release toxic substances that destroy the target cell. Cognitive Level: Comprehension 190 8. When histamine is released in the body, which of the following responses would the nurse expect? a. Bronchial dilation b. Edema c. Vasoconstriction d. Constipation ANS: B Increased vascular permeability leads to edema and is a direct response to histamine. Histamine produces bronchoconstriction. Histamine produces vasodilation. Histamine does not produce constipation; it increases gastric acidity. Cognitive Level: Comprehension 190 9. Which information would indicate more teaching is needed regarding hypersensitivity reactions? Type hypersensitivity reactions involve an antibody response. a. I b. II c. III d. IV ANS: D Type IV reactions are mediated by T lymphocytes and do not involve antibodies. Type I reactions involve antibody responses. Type II reactions involve antibody responses. Type III reactions involve antibody responses. Cognitive Level: Comprehension 195 10. A 10-year-old male presents to his primary care provider reporting wheezing and difficulty breathing. History reveals that both of the childs parents suffer from allergies. Which of the following terms would be used to classify the child? a. Desensitized b. Atopic c. Hyperactive d. Autoimmune ANS: B Atopic individuals are genetically predisposed to the development of allergies. Desensitization is a term used to describe the process of reducing the severity to allergies. Hypersensitivity is an altered immunologic response to an antigen that results in disease or damage to the individual. Autoimmunity is a disturbance in the immunologic tolerance of self-antigens. Cognitive Level: Comprehension 201 11. A 30-year-old female presents to her primary care provider reporting fatigue, excessive sweating, and increased appetite. Physical examination reveals protruding eyes, and laboratory testing reveals hyperthyroidism secondary to autoantibody production. This disorder falls into the category of type hypersensitivity. a. I b. II c. III d. IV ANS: B The patient is experiencing type II hypersensitivity. In hyperthyroidism, autoantibody binds to and activates receptors for thyroid-stimulating hormone (TSH) (a pituitary hormone that controls the production of the hormone thyroxine by the thyroid). The patient is experiencing a type II reaction, not type I, which is the most common type of allergic reaction. The patient is experiencing a type II reaction, not type III, which is not organ specific. The patient is experiencing a type II reaction; type IV is a delayed reaction. Cognitive Level: Comprehension 193 12. A 30-year-old male is having difficulty breathing and has been spitting blood. He reports that he began experiencing this reaction after cleaning his pigeons cages. Testing reveals he is suffering from allergic alveolitis. Which of the following is he experiencing? a. Serum sickness b. Raynaud phenomenon c. Antibody-dependent cytotoxicity d. Arthus reaction ANS: D The Arthus reaction is a model of localized or cutaneous reactions. Serum sicknesstype reactions are caused by the formation of immune complexes in the blood and their subsequent generalized deposition in target tissues. Typically affected tissues are the blood vessels, joints, and kidneys. Raynaud phenomenon is a condition caused by the temperature-dependent deposition of immune complexes in the capillary beds of the peripheral circulation. Antibody-dependent cytotoxicity is a type II form. Cognitive Level: Comprehension 193 13. A nurse recalls an example of an immune-complex-mediated disease is: a. Bronchial asthma b. Contact dermatitis c. Serum sickness d. Rheumatoid arthritis ANS: C Immune-complex disease can be a systemic reaction, such as serum sickness and related to type III reactions. Bronchial asthma is not an immune-complex mediated disease and related to type I reactions. Contact dermatitis is related to type IV reactions. Rheumatoid arthritis is related to type IV reactions. Cognitive Level: Comprehension 193 14. Several prisoners are experiencing symptoms of tuberculosis. A tuberculin reaction test was ordered. This test is an example of type hypersensitivity. a. I b. II c. III d. IV ANS: D Tuberculosis testing is an example of type IV hypersensitivity. Tuberculosis testing is an example of type IV hypersensitivity, not type I. Tuberculosis testing is an example of type IV hypersensitivity, not type II. Tuberculosis testing is an example of type IV hypersensitivity, not type III. Cognitive Level: Comprehension 196 15. When a nurse cares for a patient with systemic lupus erythematosus (SLE), the nurse remembers this disease is an example of: a. Autoimmunity b. Alloimmunity c. Homoimmunity d. Alleimmunity ANS: A SLE is the most common, complex, and serious of the autoimmune disorders. SLE is an autoimmune disorder, not alloimmune. SLE is an autoimmune disorder not homoimmune. SLE is an autoimmune disorder not alleimmune. Cognitive Level: Comprehension 197 16. A 30-year-old female complains of fatigue, arthritis, rash, and changes in urine color. Laboratory testing reveals anemia, lymphopenia, and kidney inflammation. Assuming a diagnosis of SLE, which of the following is also likely to be present? a. Anti-LE antibodies b. Antinuclear antibodies c. Antiherpes antibodies d. Anti-CMV antibodies ANS: B The presence of antinuclear antibodies is a diagnostic criterion for SLE. The presence of antinuclear antibodies is a diagnostic criterion for SLE. It would be positive LE. The presence of antinuclear antibodies is a diagnostic criterion for SLE, not antiherpes. The presence of antinuclear antibodies is a diagnostic criterion for SLE, not anti-CMV. Cognitive Level: Comprehension 198 17. A 40-year-old female is diagnosed with SLE. Which of the following findings would be considered a symptom of this disease? a. Gastrointestinal ulcers b. Decreased glomerular filtration rate c. Rash on trunk and extremities d. Photosensitivity ANS: D Photosensitivity is one of the 11 common clinical findings in SLE. Gastrointestinal ulcers are not a finding in SLE. Proteinuria is a symptom of SLE. A rash on the face is a symptom, but not a rash on the body. Cognitive Level: Comprehension 198 18. What is the chance that two siblings share both HLA haplotypes, making them a good match for an organ transplant from one to the other? a. 100% b. 75% c. 50% d. 25% ANS: D Odds dictate that children will share one haplotype with half their siblings and either no haplotypes or both haplotypes with a quarter of their siblings. Thus, the chance of finding a match among siblings is much higher (25%) than the general population. 100% is too high; the chance is 25%. 75% is too high; the chance is 25%. 50% is too high; the chance is 25%. Cognitive Level: Comprehension 199 19. When a nurse notices that a patient has type O blood, the nurse realizes that anti- antibodies are present in the patients body. a. A only b. B only c. A and B d. O ANS: C Type O individuals have both anti-A and anti-B antibodies. Type O individuals have both A and B antibodies. Type O individuals have both A and B antibodies. Type O individuals will have A and B antibodies, but not O. Cognitive Level: Comprehension 198 20. In addition to matching ABO antigens, a blood transfusion must also be matched for: a. HLA type b. Rh antigen c. Immunoglobulins d. Platelet compatibility ANS: B Blood transfusions must also be matched for the Rh antigen. Blood transfusions do not need to be matched to HLA. Blood transfusions do not need to be matched to immunoglobulins. Blood transfusions do not need to be matched to platelet compatibility. Cognitive Level: Comprehension 198 21. A 15-year-old male suffers from severe hemorrhage following a motor vehicle accident. He is given a blood transfusion, but shortly afterward the red blood cells are destroyed by agglutination and lysis. Which of the following blood type-transfusion type matches would cause this? a. A-A b. B-O c. AB-O d. A-AB ANS: D A person with type A blood also has circulating antibodies to the B carbohydrate antigen. If this person receives blood from a type AB or B individual, a severe transfusion reaction occurs, and the transfused erythrocytes are destroyed by agglutination or complement-mediated lysis. Type A can receive type A blood. Type B can receive type O. Type AB can accept type O. Cognitive Level: Comprehension 198 22. When an immunologist teaches about the relationship that benefits the organism but causes no harm to the host, the immunologist is describing which of the following? a. Symbiosis b. Mutualism c. Commensalism d. Pathogenicity ANS: C Commensalism benefits only the microorganism; there is no harm to the human. Parasitic microorganisms establish symbiosis with another species in which the parasite benefits at the expense of the other species. Mutualism benefits the human and the microorganism. Pathogenicity benefits the microorganism, but harms the human. (Opportunism is the situation that occurs when benign microorganisms become pathogenic because of decreased human-host resistance.) Cognitive Level: Comprehension 166 23. The microorganisms that make up the normal human flora are important for: a. Regulating inflammation b. Secreting bacteriostatic substances c. Activating white blood cells d. Preventing the colonization and multiplication of pathogens ANS: D Normal flora are provided with nutrients from ingested food, and in exchange they produce enzymes that produce antibacterial factors that prevent colonization by pathogenic microorganisms. Normal flora prevent colonization of pathogens; they do not regulate inflammation. Normal flora prevent colonization of pathogens; they do not secrete bacteriostatic substances. Normal flora prevent colonization of pathogens; they do not activate white blood cells. Cognitive Level: Comprehension 166 24. When bacterial pathogens enter a patients body, they can defend themselves from an immune response by: a. Producing capsules b. Phagocytosis c. Retreating d. Developing antibodies ANS: A Bacterial survival and growth depend on the effectiveness of the bodys defense mechanisms and on the bacteriums ability to resist these defenses. Many pathogens devise ways of preventing destruction by the inflammatory and immune systems by producing thick capsules of carbohydrate or protein. Bacteria do not produce phagocytosis. Bacteria do not retreat. Bacteria do not develop antibodies. Cognitive Level: Comprehension 168 25. A person is given an attenuated antigen as a vaccine. When the person asks what was given in the vaccine, how should the nurse respond? The antigen is: a. Alive, but less infectious b. Mutated, but highly infectious c. Normal, but not infectious d. Inactive, but infectious ANS: A Attenuated vaccines are alive, but less infectious. Attenuated vaccines are alive, not mutated or highly infectious. Attenuated vaccines are normal, but mutated doesnt relate to the answer. Attenuated vaccines are alive, but less infectious; they are not inactive. Cognitive Level: Comprehension 177 26. An immunologist is discussing endotoxin production. Which information should the immunologist include? Endotoxins are produced by: a. Gram-negative bacteria b. Gram-positive bacteria c. Gram-negative fungi d. Gram-positive fungi ANS: A Endotoxins are produces by gram-negative bacteria. Endotoxins are produced primarily by gram-negative bacteria, not gram-positive. Endotoxins are produced primarily by gram-negative bacteria, not gram-negative fungi. Endotoxins are produced primarily by gram-negative bacteria, not gram-positive fungi. Cognitive Level: Comprehension 171 27. A 5-year-old male becomes ill with a severe cough. Histologic examination reveals a bacterial infection, and further laboratory testing reveals cell membrane damage and decreased protein synthesis. Which of the following is the most likely cause of this illness? a. Endotoxin b. Exotoxin c. Hemolysis d. Septicemia ANS: B Exotoxins are enzymes that can damage the plasma membranes of host cells or can inactivate enzymes critical to protein synthesis, and endotoxins activate the inflammatory response and produce fever. Endotoxins released by blood-borne bacteria cause the release of vasoactive enzymes that increase the permeability of blood vessels. Hemolysis is the breakdown of red cells. Septicemia is the growth of bacteria in the blood. Cognitive Level: Comprehension 171 28. A 50-year-old female experiences decreased blood pressure, decreased oxygen delivery, cardiovascular shock, and subsequent death. A complication of endotoxic shock is suspected. Which of the following is the most likely cause? a. Gram-positive bacteria b. Fungi c. Gram-negative bacteria d. Virus ANS: C Symptoms of gram-negative septic shock are produced by endotoxins. Once in the blood, endotoxins cause the release of vasoactive peptides and cytokines that affect blood vessels, producing vasodilation, which reduces blood pressure, causes decreased oxygen delivery, and produces subsequent cardiovascular shock. Gram-positive bacteria typically do not produce endotoxins and thus do not manifest in shock. Fungi do not produce the endotoxic shock symptoms described. Viruses do not produce symptoms of shock. Cognitive Level: Comprehension 171 29. After studying about viruses, which information indicates the student has a good understanding of viruses? Viruses: a. Contain no DNA or RNA b. Are capable of independent reproduction c. Replicate their genetic material inside host cells d. Are easily killed by antimicrobials ANS: C Virus replication depends totally on their ability to infect a permissive host cell, a cell that cannot resist viral invasion and replication. Viruses contain both DNA and RNA. Viruses are incapable of independent reproduction. Viruses cannot be killed by antimicrobials. Cognitive Level: Comprehension 171 30. A patient has chicken pox. How does the varicella replicate? a. With the host cell DNA b. Using host cell DNA polymerase c. Using reverse transcriptase d. In the cytoplasm ANS: D Generally, all RNA viruses replicate their genetic material in the cytoplasm of the infected cell. Generally, all RNA viruses replicate their genetic material in the cytoplasm of the infected cell, not the host cell DNA. Generally, all RNA viruses replicate their genetic material in the cytoplasm of the infected cell, not the polymerase. Generally, all RNA viruses replicate their genetic material in the cytoplasm of the infected cell, not using reverse transcriptase. Cognitive Level: Comprehension 171 31. A 25-year-old female reports having unprotected sexual intercourse with several men. Blood tests reveal that she is positive for human papillomavirus. What else should the nurse assess for? a. Vaginal discharge b. Liver failure c. Breast cancer d. Warts ANS: D Direct contact with papillomavirus can lead to warts. Direct contact with papillomavirus can lead to warts, not vaginal discharge. Direct contact with papillomavirus can lead to warts, not liver failure. Direct contact with papillomavirus can lead to warts, not breast cancer. Cognitive Level: Comprehension 172 32. After studying about fungi, which information indicates a correct understanding of fungi? Fungi causing deep or systemic infections: a. Are easily treated with penicillin b. Are extremely rare c. Never occur with other infections d. Are commonly opportunistic ANS: D Diseases caused by fungi are called mycoses. Mycoses can be opportunistic. Diseases caused by fungi are called mycoses. Mycoses can be opportunistic and are not treatable with penicillin. Diseases caused by fungi are called mycoses. Mycoses can be opportunistic and are common. Diseases caused by fungi are called mycoses. Mycoses can be opportunistic and occur with other infections. Cognitive Level: Comprehension 174 33. When trying to distinguish between an infectious disease and noninfectious disease, what is the hallmark symptom for most infectious diseases? a. Fever b. Jaundice c. Vomiting d. Pain ANS: A The hallmark of most infectious diseases is fever. The hallmark of most infectious diseases is fever, not jaundice. The hallmark of most infectious diseases is fever, not vomiting. The hallmark of most infectious diseases is fever, not pain. Cognitive Level: Comprehension 175 34. Which information indicates a correct understanding of viral vaccines? Most viral vaccines contain: a. Active viruses b. Attenuated viruses c. Killed viruses d. Viral toxins ANS: B Viral vaccines contain live viruses that are weakened (attenuated). Viral vaccines contain live viruses that are weakened (attenuated), not active. Viral vaccines contain live viruses that are weakened (attenuated), not killed. Viral vaccines contain live viruses that are weakened (attenuated), not toxins. Cognitive Level: Comprehension 187 35. Which information indicates a good understanding of bacterial vaccines? Most bacterial vaccines contain: a. Active bacteria b. Synthetic bacteria c. Dead bacteria d. Bacterial toxins ANS: C Vaccines are biological preparations of weakened or dead pathogens that when administered stimulate production of antibodies or cellular immunity against the pathogen without causing disease. Vaccines are biological preparations of weakened or dead pathogens, not active bacteria. Vaccines are biological preparations of weakened or dead pathogens, not synthetic bacteria. D Vaccines are biological preparations of weakened or dead pathogens, not bacterial toxins. Cognitive Level: Comprehension 178 36. A nurse recalls bacteria become resistant to antimicrobials by: a. Proliferation b. Attenuation c. Specialization d. Mutation ANS: D Antibiotic resistance is usually a result of genetic mutations that can be transmitted directly to neighboring microorganisms by plasmid exchange. Antibiotic resistance is a result of mutations, not proliferation, which is increased growth. Antibiotic resistance is a result of genetic mutations, not attenuation. Antibiotic resistance is a result of genetic mutations, not specialization. Cognitive Level: Comprehension 176 37. What common symptom should be assessed in individuals with immunodeficiency? a. Anemia b. Recurrent infections c. Hypersensitivity d. Autoantibody production ANS: B The clinical hallmark of immunodeficiency is a propensity to unusual or recurrent severe infections. The type of infection usually reflects the immune system defect. Anemia is not a manifestation of immunodeficiency. Hypersensitivity is not a symptom of immunodeficiency. Autoantibody production is not a symptom of immunodeficiency. Chapter 10. Stress and Disease MULTIPLE CHOICE 1. After teaching about stress, which information indicates a correct understanding of stress? a. It worsens but does not cause disease. b. It can be viewed as transactional. c. It is a psychologic, rather than biologic, event. d. It is a passive event. ANS: B Stress has come to be defined by most as a transactional concept. There is a relationship between stress and disease. Stress is both a psychologic and a biologic event. Stress is an active, rather than a passive, event. Cognitive Level: Comprehension 208 2. Selye reported several structural changes in rats exposed to repeated stressors. These included: a. Hypertrophy of the thymus gland b. Ulceration in the gastrointestinal system c. Atrophy of the cortex in the adrenal gland d. Fight or flight response ANS: B Selye found the development of bleeding ulcers in response to stress. Selye found atrophy, not hypertrophy, of the thymus gland. Selye found enlargement of the cortex, rather than atrophy. The flight or fight response was part of the general adaptation syndrome, not a structural change. Cognitive Level: Comprehension 204 3. A female student is driving to school when another driver nearly hits her. Her heart begins beating harder and faster as she becomes aroused and scared. Which of the following stages of the general adaptation syndrome is she experiencing? a. Alarm stage b. Stage of resistance c. Adaptation d. Exhaustion ANS: A The alarm stage is manifested by arousal of the bodys defenses. The stage of resistance is the second step. Adaptation is a part of resistance. Exhaustion marks the breakdown of compensatory mechanisms. Cognitive Level: Comprehension 204 4. Exhaustion occurs if stress continues and is not successful. a. Fight or flight b. Alarm c. Adaptation d. Arousal ANS: C Exhaustion occurs if adaptation is not successful. Exhaustion occurs if adaptation is not successful, not fight or flight. Alarm is part of the adaptation process, but it is adaptation that prevents exhaustion. Arousal is the recognition of stress. Cognitive Level: Comprehension 205 5. A male student arrives at school to find that he has an exam for which he is unprepared. Which of the following would be expected? a. Decreased lipolysis b. Bronchoconstriction c. Decreased cortisol release d. Increased glucagon release ANS: D The student would experience increased glucagon release to supply glucose. Increased lipolysis would occur, not decreased. Bronchodilation would occur, not constriction. The student would experience increased cortisol release. Cognitive Level: Comprehension 206 | p. 211 6. A 10-year-old female is arriving at a national spelling bee contest. Her heart starts beating faster and harder, and she begins to sweat. Which of the following is she experiencing? a. Anticipatory response b. Homeostasis c. Reactive response d. Exhaustion stage ANS: A Anticipation of experiencing these events produces a physiologic stress response. Homeostasis is a steady state. Reactive response occurs following a stressful event; the student is anticipating a stressful event. Exhaustion stage is the final stage of the stressful response. Cognitive Level: Comprehension 207 7. Which of the following hormones activates adrenergic receptors? a. Oxytocin b. Prolactin c. Epinephrine d. Somatotropin ANS: C Epinephrine activates adrenergic receptors. Oxytocin activates receptors in the uterus. Prolactin does not activate adrenergic receptors. Somatotropin activates protein and carbohydrate metabolism. Cognitive Level: Comprehension 209 8. A 35-year-old male is diagnosed with a hormone-secreting tumor of the adrenal medulla. He experiences elevated blood pressure, pupil dilation, goose bumps, and increased anxiety. Which of the following hormones is the predominant one released by the tumor? a. Antidiuretic hormone b. Acetylcholine c. Norepinephrine d. Cortisol ANS: C Norepinephrine regulates blood pressure and promotes arousal, increased vigilance, increased anxiety, and other protective emotional responses. Antidiuretic hormone regulates urine output. Acetylcholine will not result in an increase in blood pressure. Cortisol regulates glucocorticoids. Cognitive Level: Comprehension 209 9. Stress induces sympathetic stimulation of the adrenal medulla. This causes the secretion of catecholamines, which include: a. Epinephrine and aldosterone b. Norepinephrine and cortisol c. Epinephrine and norepinephrine d. Cortisol and aldosterone ANS: C The catecholamines are epinephrine and norepinephrine. The catecholamines are epinephrine and norepinephrine, not aldosterone. The catecholamines are epinephrine and norepinephrine, not cortisol. The catecholamines are epinephrine and norepinephrine, not cortisol and aldosterone. Cognitive Level: Comprehension 209 10. A nurse recalls stress-induced stimulation of the adrenal cortex causes it to secrete: a. Estrogen b. Cortisol c. Parathyroid hormone d. Adrenocorticotropin hormone (ACTH) ANS: B The adrenal cortex secretes cortisol. The adrenal cortex secretes cortisol, not estrogen. The adrenal cortex secretes cortisol, not parathyroid hormone. The adrenal cortex secretes cortisol, not ACTH. Cognitive Level: Comprehension 210 11. Stress-induced catecholamine release from the adrenal medulla may result in: a. Decreased blood flow to the brain b. Elevated blood pressure c. Increased glycogen synthesis in the liver d. Decreased muscle contraction resulting from energy depletion ANS: B Catecholamine release results in elevated blood pressure. Catecholamine release results in increased blood flow to the brain. Catecholamine release results in increased glucose production, not glycogen synthesis. Catecholamine release results in increased muscle contraction. Cognitive Level: Comprehension 209 12. A 50-year-old female is diagnosed with a hormone-secreting tumor of the adrenal cortex. Which of the following would be expected? a. Decreased blood pressure b. Increased lipogenesis of face and trunk c. Increased lipogenesis of extremities d. Decreased gastric secretion ANS: B Increased release of cortisol leads to increased lipogenesis of face and trunk. Increased release of cortisol leads to increased blood pressure. Increased release of cortisol leads to lipolysis, not lipogenesis, of the extremities. Increased release of cortisol leads to increased gastric secretion. Cognitive Level: Comprehension 206 | p. 211 13. A 30-year-old male develops poison ivy after mowing the lawn near the woods. His primary care provider prescribes a synthetic cortisol. How will the cortisol relieve his symptoms? a. Suppressing Th1 cell activity b. Increasing cytokine secretion c. Suppressing natural killer cell activity d. Increasing Th2 activity ANS: A Cortisol suppresses Th1 responses. Cortisol does not increase cytokine secretion. Cortisol does not suppress natural killer cell activity. Cortisol suppresses Th2 activity. Cognitive Level: Comprehension 213 14. When assessing the effects of elevated -endorphins in a patient, which of the following should the nurse monitor? a. Peripheral vasoconstriction b. Hyperglycemia c. Pain inhibition d. Decreased immune cell activity ANS: C Elevated -endorphins activate endorphin (opiate) receptors on peripheral sensory nerves leading to pain relief or analgesia. Elevated -endorphins activate endorphin (opiate) receptors on peripheral sensory nerves leading to pain relief or analgesia, not vasoconstriction. Elevated -endorphins activate endorphin (opiate) receptors on peripheral sensory nerves leading to pain relief or analgesia, not hyperglycemia. Elevated -endorphins activate endorphin (opiate) receptors on peripheral sensory nerves leading to pain relief or analgesia, not decreased immune cell activity. Cognitive Level: Comprehension 214 15. A 10-year-old male was physically abused for the previous 4 years. He reports feeling stressed all the time and frequently gets ill. Which of the following hormones is most likely suppressed in this child? a. Endorphins b. Growth hormone c. Prolactin d. Cortisol ANS: B Increased levels of growth hormone are associated with psychological stimuli associated with stress and, thus, increase the chance of becoming ill. Increased levels of growth hormone are associated with psychological stimuli associated with stress; endorphins do not affect this. Increased levels of growth hormone are associated with psychological stimuli associated with stress; prolactin does not affect this. Increased levels of growth hormone are associated with psychological stimuli associated with stress; cortisol does not affect this. Cognitive Level: Comprehension 219 16. After teaching about coping, which information indicates a correct understanding? Coping is best defined as the process of: a. Adjusting to disease b. Preventing psychological distress c. Mediating anger d. Managing stressful challenges ANS: D Coping is the process of managing stressful challenges that tax the individuals resources. Coping is the process of managing stressful challenges that tax the individuals resources; it is not adjusting to disease. Coping is the process of managing stressful challenges that tax the individuals resources; it is not preventing psychological distress. Coping is the process of managing stressful challenges that tax the individuals resources; it is not mediating anger. Cognitive Level: Comprehension 217 MULTIPLE RESPONSE 1. When teaching about the stress-age syndrome, what information should the nurse include? (Select all that apply.) a. Decreased cortisol secretion b. Increased thyroxine c. Immunodepression d. Increased catecholamine secretion e. Hypercoagulation of the blood f. Free radical damage ANS: B, C, D, E, F The stress-age syndrome includes alterations in the excitability of structures of the limbic system and hypothalamus; rise of the blood concentration of catecholamines, ADH, ACTH, and cortisol; decrease in testosterone, thyroxine, and others; alterations of opioid peptides; immunodepression and pattern of chronic inflammation; alterations in lipoproteins; hypercoagulation of the blood; and free radical damage of cells. Cognitive Level: Comprehension 218 2. When dealing with repression in patients, which of the following assessment findings are associated with repression? (Select all that apply.) a. Decreased monocyte counts b. Increased eosinophil counts c. Decreased serum glucose d. Increased pulse rates e. Increased medication reactions ANS: A, B, E Repression was associated with lower monocyte counts, higher eosinophil counts, higher serum glucose, and more self-reported medication reactions in medical outpatients. It is not associated with increased pulse rates and glucose increases, rather than decreases. Chapter 11. Biology of Cancer MULTIPLE CHOICE 1. A patient has a tissue growth that was diagnosed as cancer. Which of the following terms best describes this growth? a. Neoplasm b. Lipoma c. Meningioma d. Hypertrophy ANS: A A neoplasm is a cancerous growth. Lipomas are benign growths. A meningioma is a benign tumor. Hypertrophy refers to tissue overgrowth, but not cancer. Cognitive Level: Comprehension 222 2. Which information indicates a nurse understands characteristics of malignant tumors? a. Grows slowly b. Has a well-defined capsule c. Has a high mitotic index d. Is well-differentiated ANS: C Malignant tumors have a high mitotic index. Malignant tumors grow rapidly. Malignant tumors are not encapsulated. Malignant tumors are poorly-differentiated. Cognitive Level: Comprehension 223 3. A nurse is discussing preinvasive epithelial tumors of glandular or squamous cell origin. What is the nurse describing? a. Tumor in differentiation b. Dysplastic c. Cancer in situ d. Cancer beyond (meta) situ ANS: C Early stage growths that are localized to the epithelium and have not invaded are called cancer in situ. Cancer in situ is early stage growth and not a tumor in differentiation. Cancer in situ is early stage growth and may contain dysplastic cells, but dysplastic cells do not define cancer in situ. Cancer in situ is early stage growth, and cancer beyond situ is more mature growth. Cognitive Level: Comprehension 223 4. A 25-year-old male develops a tumor of the breast glandular tissue. What type of tumor will be documented on the chart? a. Carcinoma b. Adenocarcinoma c. Sarcoma d. Lymphoma ANS: B Tumors that arise from or form ductal or glandular structures are named adenocarcinomas. Cancers arising in epithelial tissue are called carcinomas. Cancers arising from mesenchymal tissue (including connective tissue, muscle, and bone) usually have the suffix sarcoma. Cancers of lymphatic tissue are called lymphomas. Cognitive Level: Comprehension 223 5. A 30-year-old female is diagnosed with cancer. Testing reveals that the cancer cells have spread to local lymph nodes. A nurse realizes this cancer would be documented as stage: a. 1 b. 2 c. 3 d. 4 ANS: C Cancer that has spread to regional structures, such as lymph nodes, is stage 3. Cancer confined to the organ of origin is stage 1. Cancer that is locally invasive is stage 2. Cancer that has spread to distant sites, such as a liver cancer spreading to lung or a prostate cancer spreading to bone, is stage 4. Cognitive Level: Comprehension 244 6. An oncologist is discussing when a cancer cell loses differentiation. Which of the following is the oncologist describing? a. Autonomy b. Anaplasia c. Pleomorphic d. Metastasis ANS: B Anaplasia is the loss of differentiation. The loss of differentiation is anaplasia, not autonomy. Malignant cells are pleomorphic. A malignant tumors ability to spread far beyond the tissue of origin is metastasis. Cognitive Level: Comprehension 223 7. A primary care provider is attempting to diagnose cancer and is looking for a tumor marker. Which of the following could be a possible marker? a. Red blood cells b. Apoptotic cells c. Enzymes d. Neurotransmitters ANS: C Tumor markers include hormones, enzymes, genes, antigens, and antibodies. Tumor markers include hormones, enzymes, genes, antigens, and antibodies, but not red blood cells. Tumor markers include hormones, enzymes, genes, antigens, and antibodies, but not apoptotic cells. Tumor markers include hormones, enzymes, genes, antigens, and antibodies, but not neurotransmitters. Cognitive Level: Comprehension 225 8. A 52-year-old male with hepatitis C recently developed hepatic cancer. Which of the following markers should be increased? a. Alpha-fetoprotein (AFP) b. Catecholamines c. Prostate-specific antigen d. Homovanillic acid ANS: A Liver and germ cell tumors secrete a protein known as AFP. Liver and germ cell tumors secrete a protein known as AFP, not catecholamines. Prostate tumors secrete prostate-specific antigen. Homovanillic acid is a catecholamine marker. Cognitive Level: Comprehension 225 9. Which information should the nurse include when teaching about angiogenic factors? In cancer, angiogenic factors stimulate: a. Release of growth factors b. Tumor regression c. Apoptosis d. New blood vessel growth ANS: D Cancers can secrete multiple factors that stimulate new blood vessel growth, which is called angiogenesis. Cancers can secrete multiple factors that stimulate new blood vessel growth called angiogenesis, not release of growth factors. Cancers can secrete multiple factors that stimulate new blood vessel growth called angiogenesis, not tumor regression. Apoptosis is cell death. Cognitive Level: Comprehension 235 10. A patient has been researching telomere caps on the Internet. Which statement indicates the patient has a good understanding? Presence of telomere caps gives cancer cells: a. The ability to divide over and over again b. Clonal distinction c. Limited mitosis d. Mutation abilities ANS: A The presence of telomere caps gives cancer cells the ability to divide over and over. The presence of telomere caps does not give cells clonal distinction. Telomeres allow division over and over; thus, cancer cells have unlimited mitosis. Mutation capability is a characteristic of cancer cells, but this property is not related to telomeres. REF: pp. 235-236 11. Which of the following indicates a nurse understands a proto-oncogene? A proto-oncogene is best defined as a(n) gene. a. Normal b. Altered c. Inactive d. Tumor-suppressor ANS: A In its normal, nonmutant state, an oncogene is referred to as a proto-oncogene. A proto-oncogene is a normal gene, not an altered gene. A proto-oncogene is a normal gene, not an inactive gene. A proto-oncogene is a normal gene, not a tumor-suppressor gene. Cognitive Level: Comprehension 229 12. Of the following genetic lesions that cause cancer, which is the most common? a. Insertions b. Deletions c. Point mutations d. Amplification ANS: C Several types of genetic events can activate oncogenes. The most common are small scale changes in DNA called point mutations. Several types of genetic events can activate oncogenes. The most common are small scale changes in DNA called point mutations, not insertions. Several types of genetic events can activate oncogenes. The most common are small scale changes in DNA called point mutations, not deletions. Several types of genetic events can activate oncogenes. The most common are small scale changes in DNA called point mutations, not amplification. Cognitive Level: Comprehension 229 13. A 45-year-old female was recently diagnosed with cervical cancer. She reports a sexual history that includes 43 partners. Which of the following is the most likely cause of her cancer? a. Herpes virus b. Rubella virus c. Human papillomavirus (HPV) d. Hepatitis B virus ANS: C The presence of HPV is a factor in cervical cancer. The presence of HPV is a factor in cervical cancer, not herpes. The presence of HPV is a factor in cervical cancer, not rubella. The presence of HPV is a factor in cervical cancer, not hepatitis B. Cognitive Level: Comprehension 241 14. A 30-year-old male with HIV is diagnosed with Epstein-Barr virus. After 2 months, the virus is still active. Based upon the Epstein-Barr virus, which of the following cancers is most likely to develop in this patient? a. B cell lymphoma b. Kaposi sarcoma c. T cell leukemia d. T cell lipoma ANS: A Epstein-Barr virus is associated with B cell lymphoma. Kaposi sarcoma is associated with HIV. Retroviruses are associated with leukemia. Lipomas are not associated with HIV. Cognitive Level: Comprehension 241 15. A 45-year-old male presents with persistent, severe stomach pain. Testing reveals a peptic ulcer. Further laboratory tests reveal the presence of Helicobacter pylori. Which of the following is of concern for this patient? a. Gastric cancer b. Leukemia c. Lung cancer d. Adenocarcinoma of the colon ANS: A The presence of Helicobacter pylori is associated with gastric cancer. The presence of Helicobacter pylori is associated with gastric cancer, not leukemia. The presence of Helicobacter pylori is associated with gastric cancer, not lung cancer. The presence of Helicobacter pylori is associated with gastric cancer, not colon cancer. Cognitive Level: Comprehension 241 16. Which statement indicates the patient has a correct understanding of metastasis? The most common route of metastasis is through the blood vessels and: a. Lung tissue b. Body cavities c. Lymphatics d. Connective tissues ANS: C The most common route of metastasis is through the lymphatics. The most common route of metastasis is through the lymphatics, not lung tissue. The most common route of metastasis is through the lymphatics, not the body cavity. The most common route of metastasis if through the lymphatics, not connective tissues. Cognitive Level: Comprehension 242 17. A nurse is giving an example of inflammation as an etiology for cancer development. What is the best example the nurse should give? a. Pneumonia and lung cancer b. Ulcerative colitis and colon cancer c. Prostatic hypertrophy and prostate cancer d. Hypercholesteremia and leukemia ANS: B Individuals with a 10+ year history of ulcerative colitis have a 30-fold increase in developing colon cancer. There is no relationship between pneumonia and lung cancer, but there is a relationship between ulcerative colitis and colon cancer. There is no relationship between prostatic hypertrophy and cancer of the prostate, but there is a relationship between ulcerative colitis and colon cancer. There is no relationship between hypercholesteremia and leukemia, but there is a relationship between ulcerative colitis and colon cancer. Cognitive Level: Comprehension 240 18. A patient asks when adjuvant chemotherapy is used. How should the nurse respond? Adjuvant chemotherapy treatment is used: a. As the primary treatment b. Before radiation therapy c. After surgical removal of a tumor d. In cancer with little risk of metastasis ANS: C Adjuvant chemotherapy is given after surgical excision of a cancer with the goal of eliminating micrometastases. Adjuvant chemotherapy is given after surgery, not as the primary treatment. Adjuvant chemotherapy is given after surgery, not before radiation therapy. Adjuvant chemotherapy is given after surgery and is indicated in the treatment of individuals with metastasis. REF: pp. 248-249 MULTIPLE RESPONSE 1. Brachytherapy is being used to treat cancer in a patient. What type of cancers responds well to brachytherapy? (Select all that apply.) a. Heart b. Cervix c. Head d. Neck e. Lung ANS: B, C, D Radiation sources can be temporarily placed into body cavities through a delivery method termed brachytherapy. Brachytherapy is useful in the treatment of cervical, prostate, and head and neck cancers. Chapter 12. Cancer Epidemiology MULTIPLE CHOICE 1. Which statement indicates the patient has a good understanding of cancer risk factors? The most important environmental risk factor for cancer is exposure to: a. Ultraviolet (UV) radiation b. Radon c. Estrogen d. Cigarette smoke ANS: D Cigarette smoking is carcinogenic and remains the most important cause of cancer. UV radiation is an important risk factor, but cigarette smoking remains the most important cause of cancer. Radon plays a role as a risk factor for cancer, but cigarette smoking remains the most important cause of cancer. Estrogen plays a role in the risk factors of cancer, but cigarette smoking remains the most important cause of cancer. Cognitive Level: Comprehension 261 2. When an oncologist is discussing the degree to which an organisms development is contingent on its environment, which of the following is the oncologist explaining? a. Transgenerational inheritance b. Epigenetics c. Histone modification d. Developmental plasticity ANS: D Developmental plasticity is the degree to which an organisms development is contingent on its environment. Transgenerational inheritance is the heritable transmission to future generations of environmentally caused phenotypes. Epigenetics is the role of genes in development and disease. Histone modifications are changes in genetic acetylation. Cognitive Level: Comprehension 260 3. When a patient asks what types of cancers are associated with tobacco use, how should the nurse respond? a. Squamous and small cell adenocarcinomas b. Sarcoma and adenoma c. Melanoma and lymphoma d. Basal cell and lipoma ANS: A Tobacco use is associated with squamous and small cell adenocarcinomas. Tobacco use is associated with squamous and small cell adenocarcinomas, not sarcoma and adenoma. Tobacco use is associated with squamous and small cell adenocarcinomas, not melanoma and lymphoma. Tobacco use is associated with squamous and small cell adenocarcinomas, not basal cell and lipoma. Cognitive Level: Comprehension 261 4. Chromosome aberrations and mutations in cells that were not directly irradiated are referred to as: a. Bystander effects b. Lethal mutation c. Delayed reproductive death d. Genetic instability ANS: A The directly irradiated cells also can lead to genetic effects in so-called bystander cells or innocent cells. This is termed bystander effects. Lethal mutations occur when cells cannot reproduce, and this is not related to bystander effects. Lethal mutation and delayed reproductive death are similar phenomenon and are not related to bystander effects. Genetic instability is related to chromosomal instability. Cognitive Level: Comprehension 274 5. A 50-year-old female develops skin cancer on her head and neck following years of sunbathing. Which of the following cancers is the most likely? a. Lymphoma b. Adenoma c. Basal cell carcinoma d. Leukemia ANS: C Basal cell is related to UV radiation primarily from the sun. Lymphoma is not related to sunbathing. Adenoma is not related to sunbathing. Leukemia is not related to sunbathing. Cognitive Level: Comprehension 274 6. A 25-year-old male nursing student recently learned how diet can alter the chances of developing cancer. He tries to minimize his risks of developing the disease by ordering his steak: a. Rare b. Medium c. Medium-well d. Well done ANS: A The nursing student should order the steak rare, as the most relevant carcinogens produced by cooking are found in well-done charbroiled beef. The nursing student should order the steak rare, not medium, as the most relevant carcinogens produced by cooking are found in well-done charbroiled beef. The nursing student should order the steak rare, not medium-well, as the most relevant carcinogens produced by cooking are found in well-done charbroiled beef. The nursing student should order the steak rare, not well-done, as the most relevant carcinogens produced by cooking are found in well-done charbroiled beef. Cognitive Level: Comprehension 262 7. Which of the following compounds has been shown to increase the risk of cancer when used in combination with smoking? a. Alcohol b. Steroids c. Antihistamines d. Hypnotics ANS: A Tobacco use and alcohol use are known etiologic factors in head and neck cancers. It is alcohol, not steroids, and tobacco that have been identified as etiologic factors in cancer. It is alcohol, not antihistamines, and tobacco that have been identified as etiologic factors in cancer. It is alcohol, not hypnotics, and tobacco that have been identified as etiologic factors in cancer. Cognitive Level: Comprehension 261 8. A 25-year-old female was diagnosed with cervical cancer. History reveals she had many sexual partners, which she indicates is too many to count. Which of the following is most likely to have caused her cancer? a. HPV-16 b. HPV-18 c. HPV-31 d. HPV-45 ANS: A HPV-16, in most countries, accounts for 50% to 60% of cervical cancer cases. HPV-18 accounts for 10% to12% of cervical cancer cases. HPV-31 accounts for 4% to 5% of cervical cancer cases. HPV-45 accounts for 4% to 5% of cervical cancer cases. Cognitive Level: Comprehension 282 9. A nurse recalls physical activity was shown to reduce the risk of which of the following types of cancer? a. Prostate b. Lung c. Bone d. Colon ANS: D Physical activity reduces the risk for breast and colon cancers. Physical activity reduces the risk for breast and colon cancers, but not prostate. Physical activity reduces the risk for breast and colon cancers, but not lung. Physical activity reduces the risk for breast and colon cancers, but not bone. Cognitive Level: Comprehension 278 10. A 65-year-old male was recently diagnosed with cancer. He is retired from construction work. Which of the following cancers is he likely to develop secondary to occupational hazards? a. Mesothelioma b. Bladder cancer c. Prostate cancer d. Bone cancer ANS: A One notable occupational factor is asbestos, which increases the risk of mesothelioma, lung cancer, and possibly others. The cancer secondary to occupational hazards is mesothelioma, not bladder cancer. The cancer secondary to occupational hazards is mesothelioma, not prostate cancer. The cancer secondary to occupational hazards is mesothelioma, not bone cancer. Cognitive Level: Comprehension 278 11. A patient asks why indoor pollution is worse than outdoor pollution. How should the nurse respond? Indoor pollution is considered worse than outdoor pollution because of cigarette smoke and: a. Fireplace wood smoke b. Radon c. Benzene d. Chlorine ANS: B Indoor pollution is related to cigarette smoke and radon. Indoor pollution is related to cigarette smoke and radon, not fireplace smoke. Indoor pollution is related to cigarette smoke and radon, not benzene. Indoor pollution is related to cigarette smoke and radon, not chlorine. Cognitive Level: Comprehension 268 12. A water test recently revealed arsenic levels above 200 g/L. Which of the following cancers would be most likely to develop in those who consistently drank the water? a. Liver b. Skin c. Colon d. Kidney ANS: B Evidence indicates an increased risk of bladder, skin, and lung cancers following consumption of water with high levels of arsenic. Evidence indicates an increased risk of bladder, skin, and lung cancers, not liver, following consumption of water with high levels of arsenic. Evidence indicates an increased risk of bladder, skin, and lung cancers, not colon, following consumption of water with high levels of arsenic. Evidence indicates an increased risk of bladder, skin, and lung cancers, not kidneys, following consumption of water with high levels of arsenic. Cognitive Level: Comprehension 278 13. When an oncologist is teaching about how radiation induces genomic instability, which of the following should the oncologist discuss? a. Increasing hypersensitivity b. Facilitating new mutations c. Promoting cell death d. Enhancing mitosis ANS: B Radiation induces genomic instability because it facilitates new mutations. Radiation does not promote hypersensitivity. Radiation may promote cell death, but this is not its role in inducing genomic instability. Radiation does not enhance mitosis but halts it. Cognitive Level: Comprehension 274 14. Which of the following patients would be at greatest risk for basal cell carcinoma? a. Dark complexion, light eyes, underweight b. Light complexion, dark eyes, overweight c. Medium complexion, light eyes, smoker d. Light complexion, light eyes, fair hair ANS: D Individuals at risk for basal cell carcinoma are light complected and have light eyes and fair hair. Individuals at risk for basal cell carcinoma are light complected and have light eyes and fair hair. Individuals at risk for basal cell carcinoma are light complected and have light eyes and fair hair. Individuals at risk for basal cell carcinoma are light complected and have light eyes and fair hair. Cognitive Level: Comprehension 274 15. The role of physical activity in the prevention of colon cancer is identified by which of the following? a. It increases fluid loss leading to thirst and increased fluid intake, hydrating the colon. b. It increases blood supply thereby increasing oxygen to the colon. c. It increases gut motility thereby decreasing the time the bowel is exposed to mutagens. d. It increases the secretion of hydrochloric acid thereby killing mutants. ANS: C Physical activity increases gut motility thereby decreasing exposure to mutagens. Physical activity increases fluid loss, but this does not prevent mutagens. Physical activity increases blood supply to the colon, but this does not prevent mutagens. Physical activity does not increase hydrochloric acid. Cognitive Level: Comprehension 278 MULTIPLE RESPONSE 1. A 50-year-old female confirms chronic alcohol intake. This practice places the patient at risk for cancer in which organs? (Select all that apply.) a. Larynx b. Esophagus c. Liver d. Lung e. Brain f. Breast ANS: A, B, C, F Chronic alcohol consumption is a strong risk factor for colorectal cancer and cancer of the oral cavity, pharynx, hypopharynx, larynx, esophagus, liver, and breast. It is not associated with lung or brain cancer. Chapter 13. Cancer in Children and Adolescents MULTIPLE CHOICE 1. While planning care for children with cancer, which information should the nurse remember? Most childhood cancers originate from the: a. Placenta b. Environment c. Mesodermal germ layer d. Neural tube ANS: C Most childhood cancers originate from the mesodermal germ layer that gives rise to connective tissue, bone, cartilage, muscle, blood, blood vessels, gonads, kidney, and the lymphatic system. Most childhood cancers originate from the mesodermal germ layer, not the placenta. Most childhood cancers originate from the mesodermal germ layer, not the environment. Neural tubes are generally not associated with cancer. Cognitive Level: Comprehension 288 2. A child was recently diagnosed with cancer. The diagnosis suggests it is an embryonic tumor. Which of the following characterizes this type of cancer? a. Commonly occurring b. Often seen in adults c. Composed of mature, differentiated cells d. Usually manifested around age 5 ANS: D These types of cancers usually manifest around age 5. These types of cancers are not commonly occurring. These types of cancers are not commonly seen in adults. These types of cancers are composed of undifferentiated cells. Cognitive Level: Comprehension 288 3. A nurse is preparing to teach the most common malignancy in children. Which malignancy should the nurse discuss? a. Leukemia b. Neuroblastoma c. Wilms tumor d. Retinoblastoma ANS: A The most common malignancy in children is leukemia, accounting for one third. Tumors of the nervous system are the second most common. Wilms tumor is less frequently occurring. Retinoblastoma is less frequently occurring. Cognitive Level: Comprehension 288 4. A 3-year-old female was diagnosed with Wilms tumor. This disease is a tumor of the: a. Kidney b. Brain c. Bone marrow d. Liver ANS: A Wilms tumor is a tumor found in the kidney. Wilms tumor is a tumor found in the kidney, not the brain. Wilms tumor is a tumor found in the kidney, not the bone marrow. Wilms tumor is a tumor found in the kidney, not the liver. Cognitive Level: Comprehension 288 5. A couple brings their child to his primary care provider for a checkup. The child has Down syndrome, and the couple is concerned about other diseases that could afflict the child. The primary care provider explains that young children with Down syndrome are at higher risk for developing: a. Nephroblastoma b. Rhabdomyosarcoma c. Leukemia d. Retinoblastoma ANS: C One of the more recognized syndromes is the association of trisomy 21, Down syndrome, and with an increased susceptibility to acute leukemia. One of the more recognized syndromes is the association of trisomy 21, Down syndrome, and with an increased susceptibility to acute leukemia, not nephroblastoma. One of the more recognized syndromes is the association of trisomy 21, Down syndrome, and with an increased susceptibility to acute leukemia, not rhabdomyosarcoma. One of the more recognized syndromes is the association of trisomy 21, Down syndrome, and with an increased susceptibility to acute leukemia, not retinoblastoma. Cognitive Level: Comprehension 290 6. A newborn male is born with heart failure. Three weeks later he receives a heart transplant. Which of the following is he at the highest risk for developing? a. Leukemia b. Liver cancer c. Pancreatic cancer d. Burkitt lymphoma ANS: A Organ transplant places the child at risk for leukemia. Organ transplant places the child at risk for leukemia, not liver cancer. Organ transplant places the child at risk for leukemia, not pancreatic cancer. Organ transplant places the child at risk for leukemia, not Burkitt lymphoma. Cognitive Level: Comprehension 290 7. A 40-year-old female developed adenocarcinoma of the vagina. Which of the following is the most likely cause of her cancer? a. Rb gene mutation b. Prenatal exposure to diethylstilbestrol (DES) c. Prenatal exposure to solvents d. Prenatal exposure to radiation ANS: B The patient with adenocarcinoma of the vagina experienced prenatal exposure to DES. The patient with adenocarcinoma of the vagina experienced prenatal exposure to DES, not Rb gene mutation. The patient with adenocarcinoma of the vagina experienced prenatal exposure to DES, not solvents. The patient with adenocarcinoma of the vagina experienced prenatal exposure to DES, not radiation. Cognitive Level: Comprehension 291 8. A 16-year-old male with aspirations of becoming a bodybuilder spends 3 hours a day in the gym. Five years later he develops hepatocellular carcinoma. Which of the following is the most likely cause of the cancer? a. Immunosuppressive agents b. Cytotoxic agents c. Anabolic steroids d. A viral infection ANS: C A history of anabolic steroids places the patient at risk for hepatocellular carcinoma. A history of anabolic steroids, not immunosuppressive agents, places the patient at risk for hepatocellular carcinoma. A history of anabolic steroids, not cytotoxic agents, places the patient at risk for hepatocellular carcinoma. A history of anabolic steroids, not a viral infection, places the patient at risk for hepatocellular carcinoma. Cognitive Level: Comprehension 291 9. The most common tissue type of cancer occurring after adolescence is: a. Sarcoma b. Squamous cell c. Carcinoma d. Neuromas ANS: C The most common tissue type after adolescence is carcinoma. The most common tissue type after adolescence is carcinoma, not sarcoma. The most common tissue type after adolescence is carcinoma, not squamous cell. The most common tissue type after adolescence is carcinoma, not neuromas. Cognitive Level: Comprehension 288 MULTIPLE RESPONSE 1. When an aide asks why carcinomas rarely occur in childhood, how should the nurse respond? (Select all that apply.) a. Carcinomas cannot develop in an immunosuppressed environment. b. Carcinomas need a long time from exposure to occurrence. c. Carcinomas are due to environmental exposures. d. Carcinomas occur primarily in secondary sexual organs. e. Carcinomas are mesodermal. ANS: B, C Carcinomas rarely occur in children because these cancers most commonly result from environmental carcinogens and require a long period from exposure to the appearance of the carcinoma. Chapter 14. Structure and Function of the Neurologic System MULTIPLE CHOICE 1. When a patient asks what the somatic nervous system controls, how should the nurse respond? It controls: a. The heart b. The spinal cord c. Skeletal muscle d. Smooth muscle organs ANS: C The somatic nervous system consists of pathways that regulate voluntary motor control, the skeletal muscle system. The somatic nervous system does not control the heart; the autonomic nervous system controls the heart. The somatic nervous system does not control the spinal cord; the central nervous system (CNS) does. The somatic nervous system does not control the smooth muscle organs; the autonomic system does. Cognitive Level: Comprehension 293 2. A nurse is preparing to teach about nerves. Which information should the nurse include? The axon leaves the cell body at the: a. Axon hillock b. Nissl body c. Node of Ranvier d. Myelin sheath ANS: A The axon hillock is the cone-shaped process where the axon leaves the cell body. The Nissl body is involved in protein synthesis. Axons branch at the node of Ranvier. The myelin sheath covers the entire membrane. Cognitive Level: Comprehension 295 3. When a student asks in which region of the neuron do nerve impulses travel the fastest, how should the nurse respond? The: a. Large axon b. Axon hillock c. Cell body d. Dendrites ANS: A Large axons transmit impulses at a faster rate. The axon hillock has a low threshold level. The cell body is not the fastest. The dendrites carry impulses toward the cell body, but not as quickly as large axons. Cognitive Level: Comprehension 295 4. A neurologist is teaching the staff about motor neurons. Which information should be included? Motor neurons are structurally classified as neurons. a. Unipolar b. Pseudounipolar c. Bipolar d. Multipolar ANS: D A motor neuron is typically multipolar. Unipolar neurons are found in the retina. Pseudounipolar neurons have one process; the dendritic portion of each of these neurons extends away from the CNS, and the axon portion projects into the CNS. Bipolar neurons are found in the eye. Cognitive Level: Comprehension 295 5. An experiment looking at an isolated neuron revealed a sensory nerve with one process containing a dendritic portion extending away from the CNS and an axon extending toward the CNS. Which of the following classifications would this neuron fall into? a. Bipolar b. Multipolar c. Pseudounipolar d. Interpolar ANS: C Pseudounipolar neurons have one process; the dendritic portion of each of these neurons extends away from the CNS, and the axon portion projects into the CNS. Bipolar neurons have two distinct processes arising from the cell body. Multipolar neurons are the most common and have multiple processes capable of extensive branching. A motor neuron is typically multipolar. Interpolar is not a type of neuron. Cognitive Level: Comprehension 295 6. A cell was isolated from the CNS. A researcher revealed that its main function was to clear cellular debris. What type of cell is the researcher studying? a. Astrocyte b. Ependymal cell c. Microglia d. Schwann cell ANS: C Microglia remove debris (phagocytosis) in the CNS. Astrocytes are neuroglial cells and do not have phagocytic properties. Ependymal cells are neuroglial cells and do not have phagocytic properties. Schwann cells help form the myelin sheath in the peripheral nervous system (PNS). Cognitive Level: Comprehension 296 7. Which answer indicates a nurse understands regeneration of neurons? Neurons that have the capacity for regeneration include: a. Unmyelinated neurons in the brain b. Myelinated neurons in the spinal cord c. Myelinated peripheral neurons d. Postganglionic motor neurons ANS: C Regeneration is limited to myelinated fibers and generally occurs only in the PNS. Regeneration does not occur in unmyelinated neurons. Regeneration does not occur in myelinated neurons in the spinal cord. Regeneration does not occur in postganglionic motor neurons. Cognitive Level: Comprehension 297 8. When a presynaptic neuron is stimulated in a patients body by an electrical current, neurotransmitters are released from the: a. Synapse b. Synaptic bouton c. Synaptic cleft d. Receptor ANS: B When an impulse originates in a presynaptic neuron, the impulse reaches the vesicles, where chemicals (neurotransmitters) are stored in the synaptic bouton. Neurons are not physically continuous with one another. The region between adjacent neurons is called a synapse. The synaptic cleft is the space between the neurons. Neurotransmitters attach to the receptor. Cognitive Level: Comprehension 297 9. An aide asks a nurse what neurotransmitters interact with. Which response is the nurses best answer? Neurotransmitters interact with the postsynaptic membrane by binding to a: a. Receptor b. Nissl body c. Glial cell d. Neurofibril ANS: A Neurotransmitters bind to a receptor. The Nissl body is involved in protein synthesis. Neurotransmitters bind to receptors, not glial cells. Neurofibrils provide support for the neuron. REF: pp. 297-298 10. If a neurons membrane potential is held as close to the threshold potential by excitatory postsynaptic potentials (EPSPs), the neuron is said to be: a. Hyperpolarized b. Facilitated c. Integrated d. Inhibited ANS: B Facilitation refers to the effect of EPSP on the plasma membrane potential. The postsynaptic neurons plasma membrane may be inhibited, which is called hyperpolarized. When the neurons membrane potential is held close to the threshold potential the neuron is facilitated, not integrated. When the neurons membrane potential is held close to the threshold potential, the neuron is facilitated, not inhibited. Cognitive Level: Comprehension 298 11. A 20-year-old male was brought to the emergency room (ER) for severe burns. He requested something for the excruciating pain he was experiencing. Blocking which of the following neurotransmitters would reduce his pain? a. Enkephalin b. Dopamine c. Acetylcholine d. Substance P ANS: D Substance P is a neurotransmitter in pain transmission pathways. Blocking the release of substance P by morphine reduces pain. The opiates morphine and heroin bind to endorphin and enkephalin receptors on presynaptic neurons and reduce pain by blocking the release of neurotransmitters. Dopamine is a neurotransmitter involved in activity. Acetylcholine plays a role in nerve conduction presynaptically. Cognitive Level: Comprehension 298 12. A 19-year-old male college student reports to his primary care provider that he cannot stay awake in class regardless of how much sleep he gets. A drug that stimulates which of the following areas would best treat his problem? a. Corpora quadrigemina b. Reticular activating system c. Cerebellum d. Hypothalamus ANS: B The reticular activating system is responsible for wakefulness. The reticular activating system is responsible for wakefulness, not the corpora quadrigemina. The reticular activating system is responsible for wakefulness, not the cerebellum. The reticular activating system is responsible for wakefulness, not the hypothalamus. Cognitive Level: Comprehension 299 13. A 32-year-old female suffers from severe brain damage following a motor vehicle accident. After rehabilitation she notices that her thought processes and goal-oriented behavior are impaired. Which area does the nurse suspect is damaged? a. Thalamus b. Limbic c. Prefrontal d. Occipital ANS: C The prefrontal area is responsible for goal-oriented behavior (e.g., ability to concentrate), short- term or recall memory, the elaboration of thought, and inhibition on the limbic areas of the CNS. The prefrontal area is responsible for goal-oriented behavior, not the thalamus. The prefrontal area is responsible for goal-oriented behavior, not the limbic system. The prefrontal area is responsible for goal-oriented behavior, not the occipital area. Cognitive Level: Comprehension 301 14. A neurologist is teaching about the region responsible for motor aspects of speech. Which area is the neurologist discussing? a. Wernicke area b. Broca area c. Primary speech area d. Insula ANS: B The Broca area is responsible for the motor aspects of speech. The Broca area is responsible for the motor aspects of speech, not the Wernicke area. The Broca area is responsible for the motor aspects of speech, not the primary speech area. The Broca area is responsible for the motor aspects of speech, not the insula. Cognitive Level: Comprehension 301 15. A patient is looking at a picture of the brain and points to the convolutions on the surface of the cerebrum. The nurse should tell the patient these are called: a. Sulci b. Fissures c. Reticular formations d. Gyri ANS: D The surface of the cerebrum (cerebral cortex) is covered with convolutions called gyri, which greatly increase the cortical surface area and the number of neurons. The surface of the cerebrum (cerebral cortex) is covered with convolutions called gyri, not sulci, which greatly increase the cortical surface area and the number of neurons. The surface of the cerebrum (cerebral cortex) is covered with convolutions called gyri, not fissures, which greatly increase the cortical surface area and the number of neurons. The surface of the cerebrum (cerebral cortex) is covered with convolutions called gyri, not the reticular formation, which greatly increase the cortical surface area and the number of neurons. Cognitive Level: Comprehension 299 16. A 45-year-old male was previously diagnosed with Parkinson disease. He has impaired fine repetitive motor movements. Which of the following areas does the nurse suspect is most likely damaged? a. Basal ganglia b. Prefrontal area c. Hippocampus d. Temporal lobe ANS: A The basal ganglia system is believed to exert a stabilizing effect on motor movements. Parkinson disease and Huntington disease are conditions associated with defects of the basal ganglia. They are characterized by various involuntary or exaggerated motor movements. It is the basal ganglia system, not the prefrontal area, that is affected in Parkinson disease. It is the basal ganglia system, not the hippocampus, that is affected in Parkinson disease. It is the basal ganglia system, not the temporal lobe, that is affected in Parkinson disease. Cognitive Level: Comprehension 303 17. A neurologist is teaching about the location of the primary visual cortex in the brain. Which area is the neurologist discussing? a. Frontal lobe b. Temporal lobe c. Occipital lobe d. Parietal lobe ANS: C The visual cortex is located in the occipital lobe. The visual cortex is located in the occipital lobe, not the frontal lobe. The visual cortex is located in the occipital lobe, not the temporal lobe. The visual cortex is located in the occipital lobe, not the parietal lobe. Cognitive Level: Comprehension 301 18. A nurse is preparing to teach about functions to maintain homeostasis and instinctive behavioral patterns. Which area of the brain is the nurse discussing? a. Thalamus b. Medulla c. Cerebellum d. Hypothalamus ANS: D The hypothalamus functions to maintain a constant internal environment and instinctive behavioral patterns. It is the hypothalamus, not the thalamus, that maintains homeostasis. The thalamus serves also as a relay center for information from the basal ganglia and cerebellum to the appropriate motor area. The medulla controls reflex activities, such as heart rate, respiration, blood pressure, coughing, sneezing, swallowing, and vomiting. It is the hypothalamus that maintains homeostasis. The cerebellum is responsible for reflexive, involuntary fine-tuning of motor control, for maintaining balance and posture through extensive neural connections. Cognitive Level: Comprehension 304 19. When a nurse is teaching about the transverse fiber tract that connects the two cerebral hemispheres, what term should the nurse use? a. Peduncle b. Corpus callosum c. Basal ganglia d. Pons ANS: B The corpus callosum connects the two cerebral hemispheres and is essential in coordinating activities between hemispheres. The corpus callosum, not the peduncle, connects the two cerebral hemispheres and is essential in coordinating activities between hemispheres. The peduncle is made up of efferent fibers of the corticospinal, corticobulbar, and corticopontocerebellar tracts. The corpus callosum connects the two cerebral hemispheres and is essential in coordinating activities between hemispheres. The basal ganglia is a portion of the pyramidal system. The corpus callosum, not the pons, connects the two cerebral hemispheres and is essential in coordinating activities between hemispheres. The pons (bridge) is easily recognized by its bulging appearance below the midbrain and above the medulla. Cognitive Level: Comprehension 303 20. A student nurse asks the nurse what controls reflex activities concerned with heart rate and blood pressure. What is the nurses best response? These reflex activities are controlled by the: a. Medulla oblongata b. Pons c. Midbrain d. Cerebrum ANS: A The medulla oblongata controls reflex activities, such as heart rate, respiration, blood pressure, coughing, sneezing, swallowing, and vomiting. The medulla oblongata, not the pons, controls heart rate and blood pressure. The medulla oblongata, not the midbrain, controls heart rate and blood pressure. The midbrain is primarily a relay center for motor and sensory tracts, as well as a center for auditory and visual reflexes. The medulla oblongata controls reflex activities, such as heart rate and blood pressure. The cerebrum plays a role in the transfer of information. Cognitive Level: Comprehension 304 21. A 12-year-old presents with hydrocephalus. Blockage of which of the following would cause this condition? a. Cerebral aqueduct b. Inferior colliculi c. Red nucleus d. Tegmentum ANS: A Blockage of the cerebral aqueduct leads to hydrocephalus. Blockage of the cerebral aqueduct, not the inferior colliculi, leads to hydrocephalus. Blockage of the cerebral aqueduct, not the red nucleus, leads to hydrocephalus. Blockage of the cerebral aqueduct, not the tegmentum, leads to hydrocephalus. Cognitive Level: Comprehension 304 22. A patient presents with altered respiratory patterns following head trauma. Based upon the symptoms, which of the following areas does the nurse suspect is injured? a. Cerebrum b. Cerebellum c. Midbrain d. Reticular formation ANS: D The reticular formation is a large network of diffuse nuclei that control vital reflexes, such as those controlling cardiovascular function and respiration. The reticular formation, not the cerebrum, controls respiration. The reticular formation, not the cerebellum, controls respiration. The reticular formation, not the midbrain, controls respiration. Cognitive Level: Comprehension 299 23. A nurse recalls characteristics of upper motor neurons include: a. Directly innervating muscles b. Influencing and modifying spinal reflex arcs c. Cell bodies located in the gray matter of the spinal cord d. Dendritic processes extending out of the CNS ANS: B Upper motor neurons are completely contained within the CNS. Their primary roles are controlling fine motor movement and influencing/modifying spinal reflex arcs and circuits. Upper motor neurons are completely contained within the CNS. Their primary roles are controlling fine motor movement and influencing/modifying spinal reflex arcs and circuits. They do not innervate muscles. Upper motor neurons are completely contained within the CNS. Their primary roles are controlling fine motor movement and influencing/modifying spinal reflex arcs and circuits. Lower motor neurons interact with gray matter. Dendrites are part of neurons. Cognitive Level: Comprehension 306 24. A nurse is teaching about the area of the spinal cord that contains cell bodies involved in the autonomic nervous system. Which of the following area is the nurse discussing? a. Anterior horn b. Ventral horn c. Lateral horn d. Dorsal horn ANS: C The lateral horn contains cell bodies within the autonomic nervous system. The anterior horn contains the nerve cell bodies for efferent pathways that leave the spinal cord by way of spinal nerves. The ventral horn contains the nerve cell bodies for efferent pathways that leave the spinal cord by way of spinal nerves. The dorsal horn contains sensory neurons. Cognitive Level: Comprehension 305 25. A neurologist is teaching about sensory pathways. Which information should the neurologist include? Sensory pathways in the spinal cord include the: a. Corticospinal tract b. Pyramids c. Spinothalamic tract d. Anterior column ANS: C The spinothalamic tract carries nerve impulses from the spinal cord to the thalamus in the diencephalon. The spinothalamic tract carries impulses; the corticospinal tract carries motor impulses. The pyramids assist with motor movements. The anterior column carries nerve impulses. Cognitive Level: Comprehension 305 26. A nurse is discussing the membrane that separates the cerebellum from the cerebrum. What term should the nurse use to describe this membrane? a. Tentorium cerebelli b. Falx cerebri c. Arachnoid membrane d. Temporal lobe ANS: A The tentorium cerebelli, a common landmark, is a membrane that separates the cerebellum below from the cerebral structures above. The tentorium cerebelli separates the cerebellum, not the falx cerebri. The tentorium cerebelli separates the cerebellum, not the arachnoid membrane. The tentorium cerebelli separates the cerebellum, not the temporal lobe. Cognitive Level: Comprehension 308 27. What term should the nurse use when talking about the outermost membrane surrounding the brain? a. Dura mater b. Arachnoid mater c. Pia mater d. Falx cerebri ANS: A The dura mater is the outer layer of the brain. The arachnoid is a spongy, weblike structure that loosely follows the contours of the cerebral structures. The pia mater adheres to the contours of the brain. The falx cerebri dips between the two cerebral hemispheres along the longitudinal fissure. Cognitive Level: Comprehension 307 28. Cerebrospinal fluid (CSF) can accumulate around the brain when there is injury to the sites of CSF reabsorption, which are called the: a. Arachnoid villi b. Epidural foramina c. Lateral apertures d. Choroid plexuses ANS: A CSF is reabsorbed through a pressure gradient between the arachnoid villi and the cerebral venous sinuses. The site of CSF absorption is the arachnoid villi, not the epidural foramina. The site of CSF absorption is the arachnoid villi, not the lateral apertures. The site of CSF absorption is the arachnoid villi, not the choroid plexuses. Cognitive Level: Comprehension 309 29. A nurse remembers the brain receives approximately % of the cardiac output. a. 80 b. 40 c. 20 d. 10 ANS: C The brain receives approximately 20% of the cardiac output. The brain receives 20%, not 80%, of the cardiac output. The brain receives 20%, not 40%, of the cardiac output. The brain receives 20%, not 10%, of the cardiac output. Cognitive Level: Comprehension 310 30. The ensures collateral blood flow from blood vessels supplying the brain. a. Carotid arteries b. Basal artery c. Circle of Willis d. Vertebral arteries ANS: C The circle of Willis ensures collateral blood circulation in the brain. The circle of Willis ensures collateral blood circulation. The carotid arteries supply the brain. The circle of Willis, not the basal artery, ensures collateral blood circulation in the brain. The circle of Willis, not the vertebral arteries, ensures collateral blood circulation in the brain. Cognitive Level: Comprehension 310 31. Which cell type is the nurse discussing? A cell that is involved in forming the blood-brain barrier is the: a. Microglia b. Schwann cell c. Oligodendrocyte d. Astrocyte ANS: D Astrocytes are involved in forming the blood-brain barrier. The microglia remove debris (phagocytosis) in the CNS. Schwann cells provide structural support and nutrition for the neurons. Oligodendrocytes form the myelin sheaths. Cognitive Level: Comprehension 311 32. When a patients vagus nerve is stimulated, what does the nurse expect to observe? a. Increased gastrointestinal activity b. Increased heart rate c. Pupil constriction d. Vasoconstriction ANS: A Stimulation of the vagus nerve increases gastrointestinal activity. Stimulation of the vagus nerve increases gastrointestinal activity and it decreases heart rate. Stimulation of the vagus nerve increases gastrointestinal activity and causes pupil dilation. Stimulation of the vagus nerve increases gastrointestinal activity and leads to vasodilation. Cognitive Level: Comprehension 321 33. A 40-year-old male suffers from head trauma that affects cranial nerve I. Which of the following symptoms would the nurse expect? a. Visual disturbances b. Loss of sense of smell c. Loss of ability to taste d. Hearing disturbances ANS: B Cranial nerve I controls the sense of smell. Visual disturbances are associated with cranial nerve II. Cranial nerve VII is related to tasting. Cranial nerve VIII is related to hearing. Cognitive Level: Comprehension 315 34. Which neurotransmitter is released when a patients parasympathetic motor neurons are stimulated? a. Epinephrine b. Serotonin c. Acetylcholine d. Substance P ANS: C Parasympathetic motor neurons release acetylcholine. Adrenergic motor neurons release epinephrine. Serotonin is associated with the brain. Substance P is a neurotransmitter in pain transmission pathways. Blocking the release of substance P by morphine reduces pain. Cognitive Level: Comprehension 317 35. Which action will occur when a patients -1 receptors are stimulated? a. Dilation of the coronary arteries b. Vasoconstriction of arteries c. Increase in the strength of myocardial contraction d. Decrease in the rate of myocardial contraction ANS: C Stimulation of -1 receptors results in increased strength of myocardial contraction. -1 receptor stimulation does not affect the coronary arteries. -1 receptor simulation leads to dilation. -1 receptor stimulation leads to increased rate of contraction. Cognitive Level: Comprehension 319 36. A patient begins taking a new drug that causes pupil dilation, vasoconstriction, decreased gastrointestinal motility, and goose bumps. Which of the following receptors are activated? a. Alpha 1 b. Alpha 2 c. Beta 1 d. Beta 2 ANS: A Alpha 1 stimulation leads to pupil dilation. Alpha 2 stimulation leads to inhibition of intestinal secretions. Beta 1 stimulation leads to miosis or pupillary constriction. Beta 2 stimulation leads to pupillary constriction. Cognitive Level: Comprehension 319 37. When a student asks which type of nerves transmit nerve impulses at the fastest rate, what is the best response by the nurse? a. Large, non-myelinated b. Small, myelinated c. Large, myelinated d. Small, non-myelinated ANS: C Large and myelinated nerves transmit impulses at the fastest rate. Myelinated nerves transmit the fastest, not non-myelinated. Large nerves transmit the fastest, not small. Large, myelinated impulses transmit the fastest, not small non-myelinated nerves. Cognitive Level: Comprehension 295 38. Which of the following patients has the best chance of recovery from nerve injury? A patient with a(n): a. Torn nerve b. Crushed nerve c. Injury located closer to the cell body of the nerve d. Injury located closer to the synapse ANS: B Crush injuries to the nerve provide the greatest opportunity for recovery. Torn or cut injuries may never recover. A location closer to the cell body of the nerve may lead to cell death. A location closer to the synapse may not recover and may scar. Cognitive Level: Comprehension 297 39. The nurse is assessing the patient with a pen light. The integrity of which cranial nerve is being evaluated? a. Olfactory b. Vagus c. Oculomotor d. Trigeminal ANS: C In evaluating the oculomotor nerve, the pupils are examined for size, shape, and equality; pupillary reflex tested with a pen light (pupils should constrict when illuminated); and ability to follow moving objects. Olfactory is assessed using smells. Vagus is assessed using the ophthalmoscope. The trigeminal is assessed with a safety pin and hot and cold objects for sensations of pain, touch, and temperature. Cognitive Level: Comprehension 315 MULTIPLE RESPONSE 1. Which of the following is a neuroglial cell? (Select all that apply.) a. Astrocyte b. Oligodendrocyte c. Neuron d. Ependymal cell e. Melanocyte ANS: A, B, D Neuroglial cells include astrocytes, oligodendrocytes, and ependymal cells. Neurons and melanocytes are not neuroglial cells. Chapter 15. Pain, Temperature, Sleep, and Sensory Function MULTIPLE CHOICE 1. A patient asks the nurse where nociceptors can be found. How should the nurse respond? One location in which nociceptors can be found is the: a. Skin b. Spinal cord c. Efferent pathways d. Hypothalamus ANS: A Nociceptors are pain receptors and can be found in the skin. Nociceptors are not located in the spinal cord. Nociceptors are not located in efferent, but afferent pathways. Nociceptors are not located in the hypothalamus, but can be found in the meninges. Cognitive Level: Comprehension 326 2. A nurse is discussing an individuals conditioned or learned approach or avoidance behavior in response to pain. Which system is the nurse describing? a. Sensory-discriminative system b. Affective-motivational system c. Sensory-motivational system d. Cognitive-evaluative system ANS: B The affective-motivational system determines an individuals conditioned avoidance behaviors and emotional responses to pain. The sensory-discriminative system is mediated by the somatosensory cortex and is responsible for identifying the presence, character, location, and intensity of pain. The sensory-motivational system is not a system in the response to pain. The cognitive-evaluative system overlies the individuals learned behavior concerning the experience of pain and can modulate perception of pain. Cognitive Level: Comprehension 326 3. When a neurologist explains how pricking a finger with a needle provides minimal pain while cutting the finger with a knife provides more severe pain, what theory is being described? a. Gate control theory b. Neuromatrix theory c. Specificity theory d. Neuromodulation ANS: C The specificity theory of pain proposes that the intensity of pain is directly related to the degree of associated tissue injury. The gate control theory of pain suggests pain transmission is modulated by a balance of impulses conducted to the spinal cord, where cells in the substantia gelatinosa function as a gate that regulates the nociceptive (pain) transmission to higher centers in the central nervous system (CNS). The neuromatrix theory proposes that the brain produces patterns of nerve impulses drawn from various inputs, including genetic, psychological, and cognitive experiences. Neuromodulators of pain are found in the pathways that mediate information about painful stimuli throughout the nervous system. Cognitive Level: Comprehension 324 4. A 5-year-old female breaks her leg after falling from a merry-go-round. Which of the following would be released from the midbrain to modulate her pain? a. -Endorphin b. Enkephalin c. Endomorphin d. Dynorphin ANS: D Dynorphins are the most potent of the endogenous opioids, binding strongly to receptors to impede pain signals. -endorphins produce the greatest sense of exhilaration, as well as substantial natural pain relief. Enkephalins are natural opioids. Endomorphins have analgesic effects. Cognitive Level: Comprehension 327 5. A 15-year-old female scrapes her knee while playing soccer and complains of sharp and well- localized pain. Which of the following should the nurse document to most accurately characterize her pain? a. Chronic pain b. Referred pain c. Somatic pain d. Visceral pain ANS: C Somatic pain is superficial, arising from the skin. It is typically well localized and described as sharp, dull, aching, or throbbing. Chronic pain has been defined as lasting for more than 3 to 6 months. Referred pain is felt in an area removed or distant from its point of origin; the area of referred pain is supplied by the same spinal segment as the actual site of pain. Visceral pain is pain in internal organs and lining of body cavities and tends to be poorly localized with an aching, gnawing, throbbing, or intermittent cramping quality. Cognitive Level: Comprehension 327 6. A nurse should document on the chart that chronic pain is occurring when the patient reports the pain has lasted longer than: a. 1 month b. 3 to 6 months c. 1 year d. 2 to 3 years ANS: B Chronic or persistent pain has been defined as lasting for more than 3 to 6 months. One month is too short a time period to be classified as chronic pain. Chronic or persistent pain has been defined as lasting for more than 3 to 6 months; 1 year is too long. Chronic or persistent pain has been defined as lasting for more than 3 to 6 months; 2 to 3 years is too long. Cognitive Level: Comprehension 328 7. A 50-year-old male cut his hand off while working in a sawmill. Several years later he still sporadically feels pain in the absent hand. What type of pain should the nurse document in the chart? a. Neuropathic pain b. Visceral pain c. Phantom limb pain d. Chronic pain ANS: C The qualities we normally feel from the body, including pain, also can be felt in the absence of inputs from the body, such as is noted with phantom limb pain. Neuropathic pain is initiated or caused by a primary lesion or dysfunction in the nervous system. Visceral pain refers to pain in internal organs and lining of body cavities. Chronic pain lasts more the 3 to 6 months and is not associated with loss of a limb. Cognitive Level: Comprehension 329 8. When planning care for a child in pain, which principle should the nurse remember? The pain threshold in children is that of adults. a. Higher than b. Lower than c. The same as d. Not related to ANS: B The pain threshold in children is lower than that of adults. The pain threshold in children is lower, not higher, than that of adults. The pain threshold in children is lower, not the same, as that of adults. The pain threshold in children is lower than that of adults. Cognitive Level: Comprehension 330 9. When the nurse is taking a patients temperature, which principle should the nurse remember? Regulation of body temperature primarily occurs in the: a. Cerebrum b. Brainstem c. Hypothalamus d. Pituitary gland ANS: C Temperature regulation (thermoregulation) is mediated primarily by the hypothalamus. Temperature regulation (thermoregulation) is mediated primarily by the hypothalamus, not the cerebrum. Temperature regulation (thermoregulation) is mediated primarily by the hypothalamus, not the brainstem. Temperature regulation (thermoregulation) is mediated primarily by the hypothalamus, not the pituitary gland. Cognitive Level: Comprehension 330 10. When the nurse is discussing the patients cyclical temperature fluctuation occurring on a daily basis, what term should the nurse use? a. Thermogenesis cycle b. Thermoconductive phases c. Adaptive pattern d. Circadian rhythm ANS: D Internal temperature varies in response to activity, environmental temperature, and daily fluctuation (circadian rhythm). Temperature fluctuation is related to circadian rhythm, not thermogenesis cycle. Temperature fluctuation is related to circadian rhythm, not thermoconductive phases. Temperature fluctuation is related to circadian rhythm, not adaptive pattern. Cognitive Level: Comprehension 330 11. A nurse wants to teach about one of the primary organs responsible for heat production. Which organ should the nurse include? a. Pancreas b. Liver c. Adrenal gland d. Heart ANS: C The adrenal gland is one of the organs responsible for heat production because thyroxine acts on the adrenal medulla causing the release of epinephrine into the bloodstream. Epinephrine causes vasoconstriction that increases metabolic rates, thus increasing heat production. The pancreas does not play a role in heat production; the adrenal gland does as it releases epinephrine. which increases metabolic rates and increases heat production. The liver does not play a role in heat production; the adrenal gland does as it releases epinephrine, which increases metabolic rates and increases heat production. The heart does not play a role in heat production; the adrenal gland does as it releases epinephrine, which increases metabolic rates and increases heat production. Cognitive Level: Comprehension 330 12. Which statement by a patient indicates teaching was successful for heat loss? Heat loss from the body via convection occurs by: a. Evaporation of electromagnetic waves b. Transfer of heat through currents of liquids or gas c. Dilation of blood vessels bringing blood to skin surfaces d. Direct heat loss from molecule-to-molecule transfer ANS: B Convection occurs by transfer of heat through currents of gases or liquids, exchanging warmer air at the bodys surface with cooler air in surrounding space. Convection occurs by transfer of heat through gases or liquids, not electromagnetic waves. Convection occurs by transfer of heat through gases or liquids, not dilation of blood vessels bringing blood to skin surfaces. Convection occurs by transfer of heat through gases or liquids, not direct heat loss from molecule-to-molecule transfer. Cognitive Level: Comprehension 331 13. For evaporation to function effectively as a means of dissipating excess body heat, which one of the following conditions must be present? a. Moisture b. Fever c. Pyrogens d. Trauma ANS: A Moisture must be present because heat is lost through evaporation from the surface of skin and lining of mucous membranes, a major source of heat reduction connected with increased sweating in warmer surroundings. Fever is not required for evaporation to occur, but moisture is. Pyrogens are heat producers and do not assist with evaporation, but moisture is required. Trauma is not a portion of the evaporative process of heat loss. Cognitive Level: Comprehension 331 14. A 25-year-old female received a prescription for a weight loss pill. One effect of the pills is to increase the release of epinephrine. Which of the following would be expected to also occur? a. Decreased vascular tone b. Increased skeletal muscle tone c. Increased heat production d. Decreased basal metabolic rate ANS: C Epinephrine causes vasoconstriction, stimulates glycolysis, and increases metabolic rates, thus increasing heat production. Epinephrine increases vascular tone, but this does not lead to heat production. Epinephrine does not increase skeletal muscle tone. Epinephrine increases metabolic rate. Cognitive Level: Comprehension 330 15. When a patient has a fever, which of the following thermoregulatory mechanisms is activated? a. The bodys thermostat is adjusted to a lower temperature. b. Temperature is raised above the set point. c. Bacteria directly stimulate peripheral thermogenesis. d. The bodys thermostat is reset to a higher level. ANS: D Fever (febrile response) is a temporary resetting of the hypothalamic thermostat to a higher level in response to endogenous or exogenous pyrogens. Fever is the result of the bodys attempt to raise temperature, not adjust it to a lower level. When fever occurs, the temperature is raised, but the rise is due to a reset of the thermostat. Bacteria do not stimulate peripheral thermogenesis, but their endotoxins do. Cognitive Level: Comprehension 331 16. A patient has researched exogenous pyrogens on the Internet. Which information indicates the patient has a good understanding? Exogenous pyrogens are: a. Interleukins b. Endotoxins c. Prostaglandins d. Corticotropin-releasing factors ANS: B Exogenous pyrogens are endotoxins. Exogenous pyrogens are endotoxins, not interleukins. Exogenous pyrogens are endotoxins, not prostaglandins. Exogenous pyrogens are endotoxins, not corticotropin-releasing factors. Cognitive Level: Comprehension 331 17. Hikers are attempting to cross the Arizona desert with a small supply of water. The temperatures cause them to sweat profusely and become dehydrated. The hikers are experiencing: a. Heat cramping b. Heat exhaustion c. Heat stroke d. Malignant hyperthermia ANS: B Heat exhaustion results from prolonged high core or environmental temperatures, which cause profound vasodilation and profuse sweating, leading to dehydration, decreased plasma volumes, hypotension, decreased cardiac output, and tachycardia. Symptoms include weakness, dizziness, confusion, nausea, and fainting. Heat cramping is severe, spasmodic cramps in the abdomen and extremities that follow prolonged sweating and associated sodium loss. Heat cramping usually occurs in those not accustomed to heat or those performing strenuous work in very warm climates. Heat stroke is a potentially lethal result of an overstressed thermoregulatory center. With very high core temperatures (>40 C; 104 F), the regulatory center ceases to function, and the bodys heat loss mechanisms fail. Malignant hyperthermia is a potentially lethal complication of a rare inherited muscle disorder that may be triggered by inhaled anesthetics and depolarizing muscle relaxants. Cognitive Level: Comprehension 332 18. A 10-year-old male sneaks into a meat freezer at the local supermarket. Fearing he will get caught if he comes out, he decides to stay in there for several hours until the store closes. While in the cooler his body is most likely experiencing: a. Increased respirations b. Ischemic tissue damage c. CNS excitation d. Increased cellular metabolism ANS: B Hypothermia (marked cooling of core temperature) produces depression of the central nervous and respiratory systems, vasoconstriction, alterations in microcirculation, coagulation, and ischemic tissue damage. Hypothermia does not lead to increased respirations; it leads to ischemia. Hypothermia does not lead to CNS excitation; it leads to ischemia. Hypothermia does not lead to increased cellular metabolism; it leads to ischemia. Cognitive Level: Comprehension 333 19. Which finding indicates the patient is having complications from heat stroke? a. Mild elevation of core body temperatures b. Cerebral edema and degeneration of the CNS c. Spasmodic cramping in the abdomen and extremities d. Alterations in calcium uptake ANS: B Symptoms of heat stroke include high core temperature, absence of sweating, rapid pulse, confusion, agitation, coma, and complications include cerebral edema and degeneration of the CNS. Characteristics of heat stroke include cerebral edema and degeneration of CNS, not mild elevation of core body temperature. Characteristics of heat stroke include cerebral edema and degeneration of the CNS, not cramping. Characteristics of heat stroke include cerebral edema and degeneration of the CNS, not alterations in calcium uptake. Cognitive Level: Comprehension 332 20. For which patient would the primary care provider order therapeutic hypothermia? A patient with: a. Malnutrition b. Hypothyroidism c. Reimplantation surgery d. Parkinson disease ANS: C Therapeutic hypothermia is seen with reimplantation surgery. Therapeutic hypothermia is seen with reimplantation surgery, not malnutrition. Therapeutic hypothermia is seen with reimplantation surgery, not hypothyroidism. Therapeutic hypothermia is seen with reimplantation surgery, not Parkinson disease. Cognitive Level: Comprehension 333 21. A patient is undergoing a sleep lab test. When the sleep lab worker notices EEG patterns with brain activity similar to the normal awake pattern, which phase of sleep is occurring? a. Non-rapid eye movement (REM) b. Fast wave c. REM d. Delta wave ANS: C REM sleep is called paradoxical sleep because the EEG pattern is similar to the normal awake pattern and the brain is very active with dreaming. Non-REM sleep does not produce EEG patterns similar to the normal awake pattern. Fast wave sleep does not produce EEG patterns similar to the normal awake pattern. Delta wave sleep does not produce EEG patterns similar to the normal awake pattern. Cognitive Level: Comprehension 333 22. A patient asks when most dreams occur. What is the nurses best response? Most dreams occur during sleep. a. Non-REM b. Alpha wave c. REM d. Delta wave ANS: C Dreams occur during REM sleep. Dreams occur during REM sleep, not non-REM sleep. Dreams occur during REM sleep, not alpha wave sleep. Dreams occur during REM sleep, not delta wave sleep. Cognitive Level: Comprehension 13 | p. 19 | p. 33 23. During the sleep cycle, when does loss of temperature control occur? a. Non-REM sleep b. Light sleep c. REM sleep d. Delta wave sleep ANS: C Loss of temperature control occurs during REM sleep. Loss of temperature control occurs during REM sleep, not non-REM sleep. Loss of temperature control occurs during REM sleep, not light sleep. Loss of temperature control occurs during REM sleep, not delta wave sleep. Cognitive Level: Comprehension 333 24. A patient asks the nurse how often REM sleep occurs. How should the nurse respond? About every minutes. a. 15 b. 30 c. 60 d. 90 ANS: D REM sleep occurs every 90 minutes. REM sleep occurs every 90 minutes, not every 15. REM sleep occurs every 90 minutes, not every 30. REM sleep occurs every 90 minutes, not every 60. Cognitive Level: Comprehension 333 25. A 52-year-old male enters a sleep study to gather information about his sleep disturbances. He reports that his wife will not let him sleep in the bed with her until he stops snoring so loudly. He also reports feeling tired a lot through the day. When the nurse checks the chart, what is the most likely diagnosis? a. Insomnia b. Obstructive sleep apnea syndrome (OSAS) c. Somnambulism d. Jet-lag syndrome ANS: B OSAS generally results from upper airway obstruction recurring during sleep with excessive snoring and multiple apneic episodes that last 10 seconds or longer. Insomnia is the inability to fall or stay asleep and may be mild, moderate, or severe. It does not involve snoring. Somnambulism is sleep-walking. Jet-lag syndrome is a disorder of waking and sleeping and does not involve snoring. Cognitive Level: Comprehension 334 26. A 14-month-old child suffers from sudden apparent arousals in which she expresses intense fear or other emotion. Her mother reports that she seems to wake screaming, but that she is difficult to waken completely. The child most likely suffers from: a. Night terrors b. Parasomnia c. Somnambulism d. Enuresis episodes ANS: A Night terrors are characterized by sudden apparent arousals in which the child expresses intense fear or emotion. Parasomnia is unusual behaviors during sleep. Somnambulism is sleep-walking. Enuresis episodes are bed wetting. Cognitive Level: Comprehension 334 27. The ophthalmologist is teaching about the structure of the eye that prevents light from scattering in the eye. What structure is the ophthalmologist describing? a. Iris b. Pupil c. Choroid d. Retina ANS: C The choroid is the deeply pigmented middle layer that prevents light from scattering inside the eye. The iris is a part of the choroid and contains the pupil, which lets light into the eye. The pupil allows light to enter the eye. The retina is the innermost layer of the eye. Cognitive Level: Comprehension 335 28. A 50-year-old diabetic patient experiences visual disturbances and decides to visit his primary care provider. After examination, the primary care provider tells the patient that the cells that allow him to see are degenerated. Which of the following structures is most likely damaged? a. Lens b. Pupil c. Cornea d. Retina ANS: D The retina is the innermost layer of the eye, converting light energy into nerve impulses. Light entering the eye is focused on the retina by the lens. The pupil allows light to enter the eye. The cornea is the portion of the sclera in the central anterior region that allows light to enter the eye. Cognitive Level: Comprehension 335 29. A young child presents to the ophthalmologist for visual difficulties secondary to eye deviation. One of the childs eyes deviates outward, thereby decreasing the visual field. Which of the following diagnoses is most likely? a. Entropia b. Extropia c. Diplopia d. Nystagmus ANS: B The deviation of the eye outward is extropia. The deviation of the eye inward is entropia. Diplopia is double vision. Nystagmus is an involuntary unilateral or bilateral rhythmic movement of the eyes. Cognitive Level: Comprehension 336 30. A patient has increased intraocular pressure. Which diagnosis will the nurse observe on the chart? a. Glaucoma b. Ocular degeneration c. Diplopia d. Nystagmus ANS: A Glaucoma is the result of increased intraocular pressure. Ocular degeneration results in changes in vision, but not intraocular pressure. Diplopia is double vision. Nystagmus is an involuntary unilateral or bilateral rhythmic movement of the eyes. Cognitive Level: Comprehension 336 31. A 70-year-old male presents to his primary care provider reporting loss of vision. He reports that he has hypertension and smokes cigarettes. Which of the following disorders is most likely causing his visual loss? a. Presbyopia b. Macular degeneration c. Strabismus d. Amblyopia ANS: B Age-related macular degeneration (AMD) is a severe and irreversible loss of vision and a major cause of blindness in older individuals. Hypertension and cigarette smoking are risk factors. Presbyopia is a condition associated with aging in which the patient experiences reduced near vision. In strabismus, one eye deviates from the other when the person is looking at an object. In amblyopia, vision is reduced in the affected eye caused by cerebral blockage of the visual stimuli. Cognitive Level: Comprehension 336 32. Which group of people is most prone to red-green color blindness? a. Males b. Females c. Elderly persons d. Children ANS: A Color blindness affects 8% of the male population and 0.5% of the female population. Color blindness occurs most often in males, not females. Color blindness occurs most often in males, not the elderly. Color blindness occurs most often in males, not children. Cognitive Level: Comprehension 337 33. A 35-year-old female presents with watering and severely reddened eyes. She reports being very sensitive to light. Her primary care provider determined it was viral conjunctivitis caused by: a. Secondary bacterial infections b. Cytomegalovirus c. Herpes virus d. Adenovirus ANS: D Viral conjunctivitis is caused by an adenovirus and is manifested by symptoms of watering, redness, and photophobia. Bacterial infections are not manifested by photophobia. Cytomegalovirus infections are not manifested by photophobia. Adenovirus infections are not manifested by photophobia. Cognitive Level: Comprehension 338 34. A nurse is teaching about the structure that connects the middle ear with the pharynx. Which structure is the nurse describing? a. Organ of Corti b. Eustachian tube c. Semicircular canal d. Auditory canal ANS: B The Eustachian tube connects the middle ear to the pharynx. The organ of Corti contains the hair cells. The semicircular canal is one of the three bones of the labyrinth. The auditory canal leads to the middle ear. Cognitive Level: Comprehension 338 35. The most common form of sensorineural hearing loss in the elderly is: a. Conductive hearing loss b. Acute otitis media c. Presbycusis d. Mnire disease ANS: C Presbycusis is the most common form of sensorineural hearing loss in elderly people. Conductive hearing loss does not occur as frequently as presbycusis. Otitis media is an infection in the middle ear and is not defined as a hearing loss. Mnire disease leads to vertigo, not hearing loss. Cognitive Level: Comprehension 340 36. A 15-year-old female is diagnosed with an outer ear infection. Which of the following is most likely to cause this infection? a. Haemophilus b. Streptococcus pneumonia c. Moraxella catarrhalis d. Escherichia coli ANS: D The most common causes of acute infections are bacterial microorganisms including Pseudomonas, Escherichia coli, and Staphylococcus aureus. The most common causes of acute infections are bacterial microorganisms including Pseudomonas, Escherichia coli, and Staphylococcus aureus, not Haemophilus. The most common causes of acute infections are bacterial microorganisms including Pseudomonas, Escherichia coli, and Staphylococcus aureus, not Streptococcus. The most common causes of acute infections are bacterial microorganisms including Pseudomonas, Escherichia coli, and Staphylococcus aureus, not Moraxella catarrhalis. Cognitive Level: Comprehension 340 37. The nurse would expect the patient with an alteration in proprioception to experience vertigo which is manifested by: a. Headache b. Light sensitivity c. A sensation that the room is spinning d. Loss of feeling in the lips ANS: C Alterations in proprioception are manifested by a sensation that the room is spinning. Alterations in proprioception are manifested by a sensation of spinning, not headache. Alterations in proprioception are manifested by a sensation that the room is spinning. Light sensitivity does not occur. Alterations in proprioception are manifested by a sensation that the room is spinning. Loss of feeling in the lips does not occur. Cognitive Level: Comprehension 341 38. Which system modulates a patients perception of pain? a. Sensory-discriminative system b. Affective-motivational system c. Cognitive-evaluative system d. Reticular-activating system ANS: C The cognitive-evaluative system overlies the individuals learned behavior concerning the experience of pain and can modulate perception of pain. The sensory-discriminative system is mediated by the somatosensory cortex and is responsible for identifying the presence, character, location, and intensity of pain. The affective-motivational system determines an individuals conditioned avoidance behaviors and emotional responses to pain. The reticular-activating system does not play a role in the perception of pain. Cognitive Level: Comprehension 326 MULTIPLE RESPONSE 1. While planning care for infants, which principles should the nurse remember? (Select all that apply.) Infants have problems with thermoregulation because they: a. Cannot conserve heat b. Do not shiver c. Rarely sweat d. Have decreased metabolic rates e. Have excess subcutaneous fat ANS: A, B Infants cannot conserve heat; thus, they have a problem with thermoregulation because of their small size. Infants are unable to shiver, do have the ability to sweat, have an increased metabolic rate, and have little subcutaneous fat. Cognitive Level: Comprehension 330 COMPLETION 1. Fever of unknown origin (FUO) is characterized by a fever of F or greater ANS: 101 FUO iosf agrfeavteerr than 38.3 C (101 F) that remains undiagnosed after three days of hospital investigation or two or more outpatient visits. Chapter 16. Alterations in Cognitive Systems, Cerebral Hemodynamics, and Motor Function MULTIPLE CHOICE 1. A neurologists explains that arousal is mediated by the: a. Cerebral cortex b. Medulla oblongata c. Reticular activating system d. Cingulate gyrus ANS: C Arousal is mediated by the reticular activating system, which regulates aspects of attention and information processing and maintains consciousness. Arousal is mediated by the reticular activating system; the cerebral cortex affects movement. Arousal is mediated by the reticular activating system; the medulla oblongata controls things such as hiccups and vomiting. Arousal is mediated by the reticular activating system; the cingulate gyrus plays other roles in response. Cognitive Level: Comprehension 347 2. A 20-year-old male suffers a severe closed head injury in a motor vehicle accident. He remains in a vegetative state (VS) 1 month after the accident. Which of the following structures is most likely keeping him in a vegetative state? a. Cerebral cortex b. Brainstem c. Spinal cord d. Cerebellum ANS: B When a person loses cerebral function, the reticular activating system and brainstem can maintain a crude waking state known as a VS. Cognitive cerebral functions, however, cannot occur without a functioning reticular activating system. A VS is associated with the brainstem, not the cerebral cortex. A VS is associated with the brainstem, not the spinal cord. A VS is associated with the brainstem, not the cerebellum. Cognitive Level: Comprehension 347 3. A 16-year-old male took a recreational drug that altered his level of arousal. Physical exam revealed a negative Babinski sign, equal and reactive pupils, and roving eye movements. Which of the following diagnosis will the nurse most likely see on the chart? a. Psychogenic arousal alteration b. Metabolically induced coma c. Structurally induced coma d. Structural arousal alteration ANS: B Persons with metabolically induced coma generally retain ocular reflexes even when other signs of brainstem damage are present. Psychogenic arousal activation demonstrates a general psychiatric disorder. Structurally induced coma is manifested by asymmetric responses. Structural arousal alteration does not have drug use as its etiology. Cognitive Level: Comprehension 348 4. The breathing pattern that reflects respirations based primarily on carbon dioxide (CO2) levels in the blood is: a. Cheyne-Stokes b. Ataxic c. Central neurogenic d. Normal ANS: A Cheyne-Stokes respirations occur as a result of CO2 levels in the blood. Ataxic breathing occurs as a result of dysfunction of the medullary neurons. Central neurogenic patterns occur as a result of uncal herniation. Normal respirations are based on the levels of oxygen (O2) in the blood. Cognitive Level: Comprehension 349 5. A 45-year-old female presents to the emergency room (ER) reporting excessive vomiting. A CT scan of the brain reveals a mass in the: a. Skull fractures b. Thalamus c. Medulla oblongata d. Frontal lobe ANS: C Vomiting is due to disruptions in the medulla oblongata. Vomiting is due to disruptions in the medulla oblongata. Skull fractures can result in vomiting, but would not be related to the mass. Vomiting is due to disruptions in the medulla oblongata, not the thalamus, which controls other things such as temperature. Vomiting is due to disruption in the medulla oblongata, not the frontal lobe. The frontal lobe deals with emotions. Cognitive Level: Comprehension 351 6. A teenage boy sustains a severe closed head injury following an all-terrain vehicle (ATV) accident. He is in a state of deep sleep that requires vigorous stimulation to elicit eye opening. How should the nurse document this in the chart? a. Confusion b. Coma c. Obtundation d. Stupor ANS: D Stupor is a condition of deep sleep or unresponsiveness from which the person may be aroused or caused to open eyes only by vigorous and repeated stimulation. Confusion is the loss of the ability to think rapidly and clearly and is characterized by impaired judgment and decision making. Coma is a condition in which there is no verbal response to the external environment or to any stimuli; noxious stimuli such as deep pain or suctioning do not yield motor movement. Obtundation is a mild to moderate reduction in arousal (awakeness) with limited response to the environment. Cognitive Level: Comprehension 349 7. A 50-year-old male suffers a severe head injury when his motorcycle hits a tree. His breathing becomes deep and rapid but with normal pattern. What term should the nurse use for this condition? a. Gasping b. Ataxic breathing c. Apneusis d. Central neurogenic hyperventilation ANS: D Central neurogenic hyperventilation is a sustained, deep, rapid, but regular, pattern (hyperpnea) of breathing. Gasping is a pattern of deep all-or-none breaths accompanied by a slow respiratory rate. Ataxic breathing is completely irregular breathing that occurs with random shallow and deep breaths and irregular pauses. Apneusis is manifested by a prolonged inspiratory pause alternating with an end-expiratory pause. Cognitive Level: Comprehension 350 8. When a student asks what can cause dilated, fixed pupils, what is the nurses best response? Dilated fixed pupils can be caused by: a. Brainstem hypoxia b. Cerebral contusions c. Compression of the hypothalamus d. Spinal shock ANS: A Dilated fixed pupils are caused by brainstem hypoxia. Dilated fixed pupils are caused by brainstem hypoxia, not cerebral contusions. Dilated fixed pupils are caused by brainstem hypoxia, not compression of the hypothalamus. Dilated fixed pupils are caused by brainstem hypoxia, not spinal shock. Cognitive Level: Comprehension 362 9. An attorney spoke to the nurses regarding brain death. Which statement indicates the nurses understood brain death? For legal purposes, brain death is defined as: a. Cessation of brain function b. Lack of cortical function c. A VS d. Death of the brainstem ANS: A Brain death occurs when there is cessation of function of the entire brain, including the brainstem and cerebellum. Brain death occurs when there is cessation of function of the entire brain; lack of cortical function is not enough to define brain death. A VS is complete unawareness of the self or surrounding environment and complete loss of cognitive function. Brain death occurs when there is cessation of function of the entire brain, including the brainstem and cerebellum, not just the brainstem. Cognitive Level: Comprehension 352 10. When thought content and arousal level are intact but a patient cannot communicate, the patient has: a. Cerebral death b. Locked-in syndrome c. Dysphagia d. Cerebellar motor syndrome ANS: B Locked-in syndrome occurs when the individual cannot communicate through speech or body movement but is fully conscious, with intact cognitive function. Locked-in syndrome occurs when the individual cannot communicate through speech or body movement but is fully conscious, with intact cognitive function. In cerebral death the person is in a coma with eyes closed. Dysphagia is difficulty speaking Cerebellar motor syndrome is characterized by problems with coordinated movement. Cognitive Level: Comprehension 353 11. A 10-year-old female was brought to the ER following a sudden onset of convulsions. The primary care provider thinks that she experienced an explosive, disorderly discharge of cerebral neurons referred to as: a. Reflex b. Seizure c. Inattentiveness d. Brain death ANS: B An explosive disorderly discharge of neurons is a seizure. A reflex is an expected response. Inattentiveness is a form of neglect. Brain death is a cessation of function. Cognitive Level: Comprehension 354 12. A 30-year-old female had a seizure that started with her fingers and progressive1y spread up her arm and then extended to her leg, with no loss of consciousness. How should the nurse chart this? a. Myoclonic seizure b. Tonic-clonic seizure c. Focal motor seizure d. Atonic seizure ANS: C A focal motor seizure involves the extremities and the patient does not experience loss of consciousness. A myoclonic seizure involves symmetrical movements of selected extremities. A tonic-clonic seizure involves all body parts and loss of consciousness. An atonic seizure is without muscle tone. Cognitive Level: Comprehension 356 13. A 20-year-old male was at the supermarket when he fell to the ground. Bystanders reported that he lost consciousness and his body tensed up then relaxed, then tensed and relaxed several times. He most likely was experiencing a(n): a. Partial seizure b. Absence seizure c. Myoclonic seizure d. Tonic-clonic seizure ANS: D A tonic-clonic seizure involves repeated contraction and relaxation. A partial seizure involves only one body part. An absence seizure is without movement. A myoclonic seizure is a simple seizure with minimal jerking present. Cognitive Level: Comprehension 356 14. When a patient has a peculiar sensation that immediately precedes a seizure, what term should the nurse use to describe this sensation? a. Prodroma b. Agnosia c. Spasm d. Aura ANS: D An aura is a peculiar sensation that immediately precedes a seizure. A prodroma is a manifestation that occurs hours preceding a seizure. Agnosia is an inability to recognize objects. A spasm is a jerking action. Cognitive Level: Comprehension 356 15. A patient has memory loss of events that occurred before a head injury. What cognitive disorder does the nurse suspect the patient is experiencing? a. Selective memory deficit b. Anterograde amnesia c. Retrograde amnesia d. Executive memory deficit ANS: C Retrograde amnesia is manifested by loss of memory of past personal history memories or past factual memories. In selective memory deficit, the person reports inability to focus attention and has failure to perceive objects and other stimuli. Anterograde amnesia is a loss of the ability to form new memories. Executive memory deficit involves the failure to stay alert and oriented to stimuli. Cognitive Level: Comprehension 353 16. A 65-year-old male recently suffered a cerebral vascular accident. He is now unable to recognize and identify objects by touch because of injury to the sensory cortex. How should the nurse document this finding? a. Hypomimesis b. Agnosia c. Dysphasia d. Echolalia ANS: B Agnosia is the failure to recognize the form and nature of objects. Hypomimesis is a disorder of communication. Dysphasia is an impairment of comprehension of language. Echolalia is the ability to repeat. Cognitive Level: Comprehension 356 17. A 75-year-old female suffers a stroke and now has difficulty writing and production of language. This condition is most likely caused by occlusion of the: a. Anterior communicating artery b. Posterior communicating artery c. Circle of Willis d. Middle cerebral artery ANS: D Occlusion of the left middle cerebral artery leads to the inability to find words and difficulty writing. Occlusion of the left middle cerebral artery, not the anterior communicating artery, leads to the inability to find words and difficulty writing. Occlusion of the left middle cerebral artery, not the posterior communicating artery, leads to the inability to find words and difficulty writing. Occlusion of the left middle cerebral artery, not the circle of Willis, leads to the inability to find words and difficulty writing. Cognitive Level: Comprehension 357 18. A patient with an addiction to alcohol checked into a rehabilitation center. He experiences delirium, inability to concentrate, and is easily distracted. From which of the following is he most likely suffering? a. Acute confusional state b. Echolalia c. Dementia d. Dysphagia ANS: A Delirium and the inability to concentrate are characteristics of acute confusional state. Echolalia is the repeating of words and phrases. Dementia is characterized by loss of recent and remote memory. Dysphagia is difficulty speaking. Cognitive Level: Comprehension 357 19. A nurse thinks a patient may be experiencing dementia. Which assessment finding will most help support this diagnosis? a. Violent behavior b. Hyperactivity c. Depression d. Loss of recent and remote memory ANS: D Dementia is characterized by loss of recent and remote memory. Dementia is characterized by loss of memory. Patients with dementia may demonstrate aggressive behavior, but this is not its manifestation. Dementia is characterized by loss of memory, not hyperactivity. Dementia is characterized by loss of memory, not depression. Cognitive Level: Comprehension 357 20. The progress notes read: the cerebellar tonsil has shifted through the foramen magnum due to increased pressure within the posterior fossa. The nurse would identify this note as a description of herniation. a. Supratentorial b. Central c. Cingulated gyrus d. Infratentorial ANS: D In infratentorial herniation, the cerebellar tonsil shifts through the foramen magnum because of increased pressure within the posterior fossa. Supratentorial herniation involves temporal lobe and hippocampal gyrus shifting from the middle fossa to posterior fossa. Central herniation is a type of supratentorial herniation and is the straight downward shift of the diencephalon through the tentorial notch. Gyrus herniation occurs when the cingulate gyrus shifts under the falx cerebri. Little is known about its clinical manifestations. Cognitive Level: Comprehension 363 21. The patient is experiencing an increase in intracranial pressure. This increase results in: a. Brain tissue hypoxia b. Intracranial hypotension c. Ventricular swelling d. Expansion of the cranial vault ANS: A Brain tissue hypoxia occurs as a result of increased intracranial pressure as it places pressure on the brain. Increased intracranial pressure leads to intracranial hypertension. Ventricular swelling may lead to increased intracranial pressure, but increased pressure does not lead to ventricular swelling. Expansion of the cranial vault may lead to increased intracranial pressure, but increased pressure does not lead to expansion of the vault. Cognitive Level: Comprehension 361 22. A compensatory alteration in the diameter of cerebral blood vessels in response to increased intracranial pressure is called: a. Herniation b. Vasodilation c. Autoregulation d. Amyotrophy ANS: C Autoregulation is the compensatory alteration in the diameter of the intracranial blood vessels designed to maintain a constant blood flow during changes in cerebral perfusion pressure. Herniation is the downward protrusion of the brainstem. Vasodilation is an enlargement in vessel diameter and a part of autoregulation, but the vessels should not dilate in the presence of increased intracranial pressure. Amyotrophy is involved with the anterior horn cells of the spinal cord and not related to autoregulation. Cognitive Level: Comprehension 361 23. The primary care provider states that the patient has vasogenic edema. The nurse realizes vasogenic edema is clinically important because: a. It usually has an infectious cause. b. The blood-brain barrier is disrupted. c. Increased intracranial pressure (ICP) is excessively high. d. It always causes herniation. ANS: B Vasogenic edema is clinically important because the blood-brain barrier (selective permeability of brain capillaries) is disrupted, and plasma proteins leak into the extracellular spaces. Vasogenic does not have an infectious cause. ICP is increased, but not more so than other forms of edema. Vasogenic edema disrupts the blood-brain barrier, but it does not always cause herniation. Cognitive Level: Comprehension 362 24. A 51-year-old male is admitted to the neurological critical care unit with a severe closed head injury. All four extremities are in rigid extension, his forearm is hyperpronated, and his legs are in plantar extension. How should the nurse chart this condition? a. Decorticate posturing b. Decerebrate posturing c. Caloric posturing d. Excitation posturing ANS: B The description is of a patient in decerebrate posturing. The patient is in decerebrate posturing, not decorticate. The patient is in decerebrate posturing, not caloric. The patient is in decerebrate posturing, not excitation. Cognitive Level: Comprehension 372 25. A 20-year-old male is admitted to the neurological critical care unit with a severe closed head injury. When an intraventricular catheter is inserted, the ICP is recorded at 24 mm Hg. How should the nurse interpret this reading? This reading is: a. Higher than normal b. Lower than normal c. Normal d. Borderline ANS: A Normal ICP is 5 to 15 mm Hg; at 24 mm Hg, the patients is higher than normal. Normal ICP is 5 to 15 mm Hg; at 24 mm Hg, the patients is higher than normal, not lower. Normal ICP is 5 to 15 mm Hg; the patients is higher than normal. Normal ICP is 5 to 15 mm Hg; at 24 mm Hg, the patients is higher than normal, not borderline. Cognitive Level: Comprehension 361 26. A 70-year-old female is being closely monitored in the neurological critical care unit for a severe closed head injury. After 48 hours, her condition begins to deteriorate. Her pupils are small and sluggish, pulse pressure is widening, and she is bradycardic. These clinical findings are evidence of what stage of intracranial hypertension? a. Stage 1 b. Stage 2 c. Stage 3 d. Stage 4 ANS: C Stage 3 is characterized by decreasing levels of arousal or central neurogenic hyperventilation, widened pulse pressure, bradycardia, and pupils that become small and sluggish. Stage 1 is characterized by an ICP that may not change because of the effective compensatory mechanisms, and there may be few symptoms. Stage 2 is characterized by subtle and transient symptoms, including episodes of confusion, restlessness, drowsiness, and slight pupillary and breathing changes. Stage 4 is characterized by cessation of cerebral blood flow. Cognitive Level: Comprehension 362 27. An infant is diagnosed with noncommunicating hydrocephalus. What is an immediate priority concern for this patient? a. Metabolic edema b. Interstitial edema c. Vasogenic edema d. Ischemic edema ANS: B An immediate concern for the infant with noncommunicating hydrocephalus is interstitial edema. Interstitial edema, not metabolic edema, is seen most often with noncommunicating hydrocephalus. Interstitial edema, not vasogenic edema, is seen most often with noncommunicating hydrocephalus. Interstitial edema, not ischemic edema, is seen most often with noncommunicating hydrocephalus. Cognitive Level: Comprehension 363 28. An adult has hydrocephalus. When the patient asks the nurse what caused this, how should the nurse respond? Hydrocephalus in adults is most often caused by: a. Overproduction of CSF b. Intercellular edema c. Elevated arterial blood pressure d. Defective CSF reabsorption ANS: D Hydrocephalus occurs because of defective reabsorption of the fluid. Hydrocephalus can occur because of overproduction of CSF, but in adults it occurs most often because of defective reabsorption of the fluid. Hydrocephalus is not due to intercellular edema. Hydrocephalus does not occur due to elevated arterial blood pressure. Cognitive Level: Comprehension 363 29. A 16-year-old male fell off the bed of a pickup truck and hit his forehead on the road. He now has resistance to passive movement that varies proportionally with the force applied. He is most likely suffering from: a. Spasticity b. Gegenhalten c. Rigidity d. Dystonia ANS: B Gegenhalten is manifested by resistance to passive movement that varies in direct proportion to force applied. Spasticity is manifested by a gradual increase in tone causing increased resistance until tone suddenly reduces. Rigidity is manifested by muscle resistance to passive movement of a rigid limb that is uniform in both flexion and extension throughout the motion. Dystonia is manifested by sustained involuntary twisting movement. Cognitive Level: Comprehension 364 30. A patient has paralysis of both legs. What type of paralysis does the patient have? a. Paraplegia b. Quadriplegia c. Infraparaplegia d. Paresthesia ANS: A Paraplegia is the paralysis of both legs. Quadriplegia is the paralysis of all four extremities. Infraparaplegia is not a description of paralysis. Paresthesia is a loss of sensation, not paralysis. Cognitive Level: Comprehension 366 31. A patient has excessive movement. What disorder will the nurse see documented on the chart? a. Hypokinesia b. Akinesia c. Hyperkinesia d. Dyskinesia ANS: C Excessive movement is the definition of hyperkinesia. Hypokinesia is decreased movement. Akinesia is loss of movement. Dyskinesia is abnormal movement. Cognitive Level: Comprehension 369 32. Which principle should the nurse remember while planning care for a patient with spinal shock? Spinal shock is characterized by: a. Loss of voluntary motor function with preservation of reflexes b. Cessation of spinal cord function below the lesion c. Loss of spinal cord function at the level of the lesion only d. Temporary loss of spinal cord function above the lesion ANS: B Spinal shock is the complete cessation of spinal cord function below the lesion. The reflexes are not preserved in spinal shock. Spinal shock is the complete cessation of spinal cord function below the lesion, not at the lesion only. Spinal shock is the complete cessation of spinal cord function below the lesion. Cognitive Level: Comprehension 366 33. A 40-year-old male complains of uncontrolled excessive movement and progressive dysfunction of intellectual and thought processes. He is experiencing movement problems that begin in the face and arms that eventually affect the entire body. The most likely diagnosis is: a. Tardive dyskinesia b. Huntington disease c. Hypokinesia d. Alzheimer disease ANS: B Huntington disease is manifested by chorea, abnormal movement that begins in the face and arms, eventually affecting the entire body. There is progressive dysfunction of intellectual and thought processes. Tardive dyskinesia is manifested by rapid, repetitive, stereotypic movements. Most characteristic is continual chewing with intermittent protrusions of the tongue, lip smacking, and facial grimacing. Hypokinesia is loss of voluntary movement despite preserved consciousness and normal peripheral nerve and muscle function. Alzheimer disease is manifested by cognitive deficits and not movement problems; motor impairments will occur in the later stages. Cognitive Level: Comprehension 369 34. A nurse notes that a patient walks with the leg extended and held stiff, causing a scraping over the floor surface. What type of gait is the patient experiencing? a. Spastic gait b. Cerebellar gait c. Basal ganglion gait d. Scissors gait ANS: A An individual who walks with the leg extended and held stiff, causing a scraping over the floor surface, is experiencing a spastic gait. A cerebellar gait is wide-based with the feet apart and often turned outward or inward for greater stability. A basal ganglion gait occurs when the person walks with small steps and a decreased arm swing. A scissors gait is associated with bilateral injury and spasticity. The legs are abducted so they touch each other. Cognitive Level: Comprehension 372 35. A male patient complains of tiring easily, has difficulty rising from a sitting position, and cannot stand on his toes. The nurse would expect a diagnosis of: a. Parkinson disease b. Hypotonia c. Huntington disease d. Paresis ANS: B Individuals with hypotonia tire easily (asthenia) or are weak. They may have difficulty rising from a sitting position, sitting down without using arm support, and walking up and down stairs, as well as an inability to stand on their toes. Individuals with Parkinson disease have rigidity and stiffness. Symptoms of Huntington disease include irregular, uncontrolled, and excessive movement. Paresis, or weakness, is partial paralysis with incomplete loss of muscle power. Cognitive Level: Comprehension 364 MULTIPLE RESPONSE 1. A nurse recalls neural systems basic to cognitive functions include systems. (Select all that apply.) a. Attentional b. Memory and language c. Affective d. Sensory and motor e. Tactile ANS: A, B, C The neural systems that are essential to cognitive function are: (A) attentional systems that provide arousal and maintenance of attention over time; (B) memory and language systems by which information is communicated; and (C) affective or emotive systems that mediate mood, emotion, and intention. The sensory, motor, and somatic systems are not involved. The tactile system is not involved in cognitive functioning. Cognitive Level: Comprehension 353 2. The nurse is explaining clinical manifestations of alterations in the extrapyramidal system. The nurse would correctly include (select all that apply): a. Little or no paralysis of voluntary movement b. Normal or slightly increased tendon reflexes c. Positive (present) Babinski d. Presence of tremor e. Rigidity in muscle tone ANS: A, B, D, E The patient will experience little or no paralysis of voluntary movement. The patient will experience normal or slightly increased deep tendon reflexes. Babinski will be negative (absent). Tremor will be present. Rigidity of muscle tone occurs intermittently. Chapter 17. Disorders of the Central and Peripheral Nervous Systems and Neuromuscular Junction MULTIPLE CHOICE 1. A neurologist is teaching about brain injuries. Which information should the neurologist include? The most severe diffuse brain injury caused by rotational acceleration is most likely to be located the brainstem. a. More peripheral to b. In the central portion of c. Throughout d. Distal to ANS: A The most severe axonal injuries are located more peripheral to the brainstem. These injuries occur peripherally to the brainstem, not in the central portion. These injuries occur peripherally to the brainstem, not throughout the brainstem. These injuries occur peripherally to the brainstem, not distal to the stem. Cognitive Level: Comprehension 381 2. A nurse is preparing to teach staff about the most common type of traumatic brain injury. Which type of traumatic brain injury should the nurse discuss? a. Penetrating trauma b. Diffuse axonal injury c. Focal brain injury d. Concussion ANS: D A concussion is the most common type of traumatic brain injury. Penetrating trauma is due to such items as bullets and is not the most common type of brain injury. Diffuse axonal injury is due to rotation and is not as common as concussions. Focal brain injury is not as common as concussions. Cognitive Level: Comprehension 377 3. A 15-year-old male suffered diffuse brain injury after wrecking an all-terrain vehicle. He had momentary confusion and retrograde amnesia after 5 to 10 minutes. His injury could be categorized as: a. Grade I b. Grade II c. Grade III d. A mild concussion ANS: B Grade II is manifested as momentary confusion and retrograde amnesia after 5 to 10 minutes. Grade I is manifested by confusion and disorientation with momentary amnesia. Grade III is manifested by confusion and retrograde amnesia from impactalso anterograde amnesia. A mild concussion does not result in memory loss. Cognitive Level: Comprehension 379 4. A 25-year-old male was in an automobile accident. At impact, his forehead struck the windshield. In this situation, a nurse recalls the coup injury would occur in the region. a. Frontal b. Temporal c. Parietal d. Occipital ANS: A Coup injuries move forward and affect the frontal region of the brain. Coup injuries affect the frontal region of the brain as the brain moves forward, not to the side or temporal region. Coup injuries affect the frontal region of the brain as the brain moves forward, not to the middle or parietal region. Contrecoup injuries affect the rear or occipital region. Cognitive Level: Comprehension 379 5. While planning care for a patient with an extradural hematoma, which principle should the nurse remember? The main source of bleeding in extradural (epidural) hematomas is: a. Arterial b. Venous c. Capillary d. Sinus ANS: A An artery is the source of bleeding in 85% of extradural hematomas. An artery, not a vein, is the source of bleeding in 85% of extradural hematomas. An artery, not a capillary, is the source of bleeding in 85% of extradural hematomas. The sinus is not the source of bleeding in extradural hematomas; it is arterial. REF: pp. 379-380 6. A 69-year-old male with a history of alcohol abuse presents to the emergency room (ER) after a month-long episode of headaches and confusion. Based on his alcoholism, a likely cause of his neurologic symptoms is: a. Concussion b. Chronic subdural hematoma c. Epidural hematoma d. Subacute subdural hematoma ANS: B Chronic subdural hematomas are commonly found in persons who abuse alcohol and develop over weeks to months. A concussion is more acute, and chronic subdural hematomas are more commonly found in persons who abuse alcohol. It is a chronic subdural hematoma that occurs in alcoholics, not an epidural. Subacute subdural hematomas present with confusion, but these occur sooner than the chronic subdural associated with alcoholism. Cognitive Level: Comprehension 380 7. A 15-year-old male was struck by a motor vehicle and suffered a traumatic brain injury. Paramedics found him unconscious at the scene of the accident. During the ambulance ride, he regained consciousness and was able to maintain a conversation with the medical staff. Upon arrival to hospital, he was alert and oriented. Physical exam reveals confusion and impaired responsiveness. What is the probable nature of his brain injury based on this history? a. Mild concussion b. Subdural hematoma c. Extradural (epidural) hematoma d. Mild diffuse axonal injury ANS: C Individuals with extradural hematomas lose consciousness at injury; one-third then become lucid for a few minutes to a few days. Mild concussion is characterized by immediate but transitory confusion that lasts for one to several minutes, possibly with amnesia for events preceding the trauma. Subdural hematomas begin with headache, drowsiness, restlessness or agitation, slowed cognition, and confusion. These symptoms worsen over time and progress to loss of consciousness, respiratory pattern changes, and pupillary dilation. Individuals with mild diffuse axonal injury display decerebrate or decorticate posturing and may experience prolonged periods of stupor or restlessness. Cognitive Level: Comprehension 380 8. Which assessment finding by the nurse characterizes a mild concussion? a. A brief loss of consciousness b. Significant behavioral changes c. Retrograde amnesia d. Permanent confusion ANS: C Mild concussion is characterized by immediate but transitory confusion that lasts for one to several minutes, possibly with amnesia for events preceding the trauma. Individuals with extradural hematomas lose consciousness at injury; one-third then become lucid for a few minutes to a few days. Persons with diffuse brain injury demonstrate behavioral changes. Individuals with a mild concussion experience transient not permanent confusion. Cognitive Level: Comprehension 381 9. A 39-year-old male suffers a severe brain injury when he falls off a building while working. CT scan reveals that he has a basilar skull fracture. Based upon his injuries, what major complication should the nurse observe for in this patient? a. Hematoma formation b. Meningeal infection c. Increased intracranial pressure (ICP) d. Cognitive deficits ANS: B Individuals with basilar skull fractures should be observed for meningitis and other complications. Individuals with basilar skull fracture are at risk for meningitis due to the open fracture, not hematoma. Individuals with basilar skull fracture are at risk for meningitis due to the open fracture, not increased ICP. Individuals with basilar skull fracture are at risk for meningitis due to the open fracture, not cognitive deficits. Cognitive Level: Comprehension 381 10. A 65-year-old female loses her balance while walking in the woods, causing her to fall and hit her head. She loses consciousness and is in a coma for 5 days. She is diagnosed as having diffuse brain injury. Which of the following would most likely occur in this patient? a. Complete loss of vision b. Arrhythmia c. Blunted affect d. Meningitis infection ANS: C Individuals who experience diffuse brain injury experience agitation, impulsiveness, blunted affect, social withdrawal, and depression. Individuals who experience diffuse brain injury may experience visual impairments, but do not experience loss of vision. Individuals who experience diffuse brain injury may experience paralysis, but do not experience arrhythmias. Individuals with basilar skull fractures experience meningitis, not those with diffuse brain injury. Cognitive Level: Comprehension 381 11. A 10-year-old male was climbing on a house and fell. He suffered a severe brain injury. His Glasgow Coma Scale (GCS) was 5 initially and 7 after 1 day. He remained unconscious for 2 weeks, then was confused and suffered from anterograde amnesia. Which of the following is he most likely experiencing? a. Mild diffuse brain injury b. Moderate diffuse brain injury c. Severe diffuse brain injury d. Postconcussive syndrome ANS: B In moderate diffuse axonal injury, the score on the GCS is 4 to 8 initially and 6 to 8 by 24 hours and the person is confused and suffers a long period of posttraumatic anterograde and retrograde amnesia. Individuals who experience diffuse brain injury experience agitation, impulsiveness, blunted affect, social withdrawal, and depression. In severe diffuse axonal injury, the person experiences immediate autonomic dysfunction that disappears in a few weeks. Increased ICP appears 4 to 6 days after the injury. In postconcussive syndrome the individual experiences headache, nervousness or anxiety, irritability, insomnia, depression, inability to concentrate, forgetfulness, and fatigability. Cognitive Level: Comprehension 381 12. are most at risk of spinal cord injury from minor trauma. a. Infants b. Men c. Women d. The elderly ANS: D Elderly people are particularly at risk from minor trauma that results in serious spinal cord injury because of preexisting degenerative vertebral disorders. It is the elderly, not infants, who are at risk for minor trauma that results in serious spinal cord injury because of preexisting degenerative vertebral disorders. Males are at greatest risk for major spinal cord injury. It is the elderly that are most at risk for injury with minor trauma. Males, not females, are at greatest risk for major spinal cord injury. It is the elderly that are most at risk for injury with minor trauma. Cognitive Level: Comprehension 382 13. An initial assessment finding associated with acute spinal cord injury is the injury. a. Pain below the level of b. Loss of autonomic reflexes above c. Loss of voluntary control below d. Hyperactive spinal reflexes below ANS: C Normal activity of the spinal cord cells at and below the level of injury ceases because of loss of the continuous tonic discharge from the brain or brainstem and inhibition of suprasegmental impulses immediately after cord injury, thus causing spinal shock. Pain would not be present below the level of the injury because activity of the cells below the level of injury ceases. Autonomic reflexes above the injury remain intact. Activity of the cells below the level of injury cease; thus, hyperactive spinal reflexes below the injury will not occur. Cognitive Level: Comprehension 383 14. When a patient asks how bad the injuries will be from a spinal injury, what is the nurses best response? It is difficult to know the full extent of the injury because of: a. Incomplete transection of the spinal cord b. Swelling within the spinal cord c. Necrosis of the spinal cord d. Free radical injury and scarring of the glial cells ANS: B Cord swelling increases the individuals degree of dysfunction, so it is hard to distinguish functions permanently lost from those temporarily impaired. It is swelling, not incomplete transection, that leads to the difficulty knowing the full extent of injury in the spinal column. It is swelling, not necrosis, that leads to the difficulty knowing the full extent of injury in the spinal column. It is swelling, not free radical injury and scarring, that leads to the difficulty knowing the full extent of injury in the spinal column. Cognitive Level: Comprehension 383 15. A 20-year-old male is brought to the emergency room (ER) for treatment of injuries received in a motor vehicle accident. A spinal cord injury is suspected. What two regions should the nurse assess as they are most likely to be damaged? a. Cervical and thoracic regions b. Thoracic and lumbar regions c. Lumbar and sacral regions d. Cervical and lumbar regions ANS: D Vertebral injuries in adults occur most often at cervical and lumbar regions as these are the most mobile portions of the vertebral column. Vertebral injuries in adults occur most often at cervical and lumbar regions, rather than the cervical and thoracic, as these are the most mobile portions of the vertebral column. Vertebral injuries in adults occur most often at cervical and lumbar regions, rather than the thoracic and lumbar, as these are the most mobile portions of the vertebral column. Vertebral injuries in adults occur most often at cervical and lumbar regions, rather than the lumbar and sacral, as these are the most mobile portions of the vertebral column. Cognitive Level: Comprehension 382 16. A 33-year-old male is brought to the ER for treatment of injuries received in a motor vehicle accident. An MRI reveals an injury of the cervical cord. Cord swelling in this region may be life threatening because: a. Increased ICP may occur. b. Reflexes will be disrupted. c. Diaphragm function may be impaired. d. Bladder emptying will not occur. ANS: C In the cervical region, cord swelling may be life threatening because it may impair the diaphragm function. Increased ICP does not occur with cord injury, but cord swelling may be life threatening because it may impair the diaphragm function. Reflexes may be disrupted, but the cord swelling may be life threatening because it may impair the diaphragm function. Bladder emptying may not occur, but the cord swelling may be life threatening because it may impair the diaphragm function. Cognitive Level: Comprehension 383 17. A 15-year-old male is brought to the ER for treatment of injuries received in a motor vehicle accident. An MRI reveals spinal cord injury, and his body temperature fluctuates markedly. The most accurate explanation of this phenomenon is that: a. He developed pneumonia. b. His sympathetic nervous system has been damaged and thermal control disturbed. c. He has a brain injury. d. He has septicemia from an unknown source. ANS: B The patient experiences disturbed thermal control because the sympathetic nervous system is damaged. The hypothalamus cannot regulate body heat through vasoconstriction and increased metabolism; therefore, the individual assumes the temperature of the air. The patient may develop pneumonia, but the temperature fluctuation is due to disturbed thermal control because the sympathetic nervous system is damaged. The hypothalamus cannot regulate body heat through vasoconstriction and increased metabolism; therefore, the individual assumes the temperature of the air. The patient may have a brain injury, but thermal control is affected because the sympathetic nervous system is damaged. The hypothalamus cannot regulate body heat through vasoconstriction and increased metabolism; therefore, the individual assumes the temperature of the air. The patient exhibits disturbed thermal control, not because of septicemia, but because the sympathetic nervous system is damaged. The hypothalamus cannot regulate body heat through vasoconstriction and increased metabolism; therefore, the individual assumes the temperature of the air. Cognitive Level: Comprehension 383 18. Six weeks ago a female patient suffered a T6 spinal cord injury. She then developed a blood pressure of 200/120, a severe headache, blurred vision, and bradycardia. What does the nurse suspect the patient is experiencing? a. Extreme spinal shock b. Acute anxiety c. Autonomic hyperreflexia d. Parasympathetic areflexia ANS: C The patient is experiencing autonomic hyperreflexia, which is manifested by paroxysmal hypertension (up to 300 mm Hg, systolic), a pounding headache, blurred vision, sweating above the level of the lesion with flushing of the skin, nasal congestion, nausea, piloerection caused by pilomotor spasm, and bradycardia (30 to 40 beats/min). The patient in extreme spinal shock experiences paralysis and flaccidity in muscles, absence of sensation, loss of bladder and rectal control, transient drop in blood pressure, and poor venous circulation. The patient may experience acute anxiety, but the symptoms of elevated blood pressure with severe headache is due to autonomic hyperreflexia. It is autonomic hyperreflexia, not parasympathetic areflexia, that produces paroxysmal hypertension (up to 300 mm Hg, systolic), a pounding headache, blurred vision, sweating above the level of the lesion with flushing of the skin, nasal congestion, nausea, piloerection caused by pilomotor spasm, and bradycardia (30 to 40 beats/min). Cognitive Level: Comprehension 385 19. A 20-year-old female suffered from spinal cord injury that resulted from a motor vehicle accident. She had spinal shock lasting 15 days and is now experiencing an uncompensated cardiovascular response to sympathetic stimulation. What does the nurse suspect caused this condition? a. Toxic accumulation of free radicals below the level of the injury b. Pain stimulation above the level of the spinal cord lesion c. A distended bladder or rectum d. An abnormal vagal response ANS: C The described symptoms indicate autonomic hyperreflexia and are due to a distended bladder or rectum. The described symptoms indicate autonomic hyperreflexia and are due to a distended bladder or rectum, not the accumulation of free radicals. The described symptoms indicate autonomic hyperreflexia and are due to a distended bladder or rectum, not pain stimulation. The described symptoms indicate autonomic hyperreflexia and are due to a distended bladder or rectum, not an abnormal vagal response. Cognitive Level: Comprehension 385 20. A 50-year-old male presents with low back pain. He denies trauma and says he just woke up and it was hurting. An MRI reveals that the vertebra at L5 slid forward relative to those above and below it. Which of the following conditions will be documented on the chart? a. Degenerative disk disease b. Spondylolysis c. Spondylolisthesis d. Spinal stenosis ANS: C Spondylolisthesis occurs when there is forward displacement of the deficient vertebra. Degenerative disk disease is a pathophysiological cause of spondylolisthesis, but is not the definition of forward displacement. Spondylolysis is a structural defect of the spine. Spinal stenosis is a narrowing of the spinal canal. Cognitive Level: Comprehension 387 21. The majority of intervertebral disk herniations occur between which vertebral levels (cervical, C; thoracic, T; lumbar, L; sacral, S)? a. C1 to C3 b. T1 to T4 c. T12 to L3 d. L4 to S1 ANS: D The most common discs affected by herniation are the lumbosacral disksthat is, L5-S1 and L4- L5. Cervical herniation can occur, but the most common discs affected by herniation are the lumbosacral disksthat is, L5-S1 and L4-L5. The most common discs affected by herniation are the lumbosacral disksthat is, L5-S1 and L4- L5. The most common discs affected by herniation are the lumbosacral disksthat is, L5-S1 and L4- L5. Cognitive Level: Comprehension 387 22. A 30-year-old white male recently suffered a cerebrovascular accident. Which of the following is the most likely factor that contributed to his stroke? a. Age b. Gender c. Diabetes d. Race ANS: C The most likely contributing factor to the patients stroke is that he has diabetes with a fourfold increase in stroke incidence and an eightfold increase in stroke mortality. Age greater than 65 years is contributing factor. Men are affected, but for the 30-year-old, his type 2 diabetes mellitus contributes to a fourfold increase in stroke incidence and an eightfold increase in stroke mortality. Blacks are affected more than whites, and it is this patients diabetes that places him at risk. Cognitive Level: Comprehension 389 23. Which of the following would increase a patients risk for thrombotic stroke? a. Hyperthyroidism b. Hypertension c. Anemia d. Dehydration ANS: D Dehydration is a risk factor because it increases blood viscosity and decreases cerebral perfusion. Hyperthyroidism would lead to increased blood pressure but does not place the patient at risk for thrombotic stroke. Hypotension, not hypertension is a risk factor for thrombotic stroke. Anemia would decrease a persons risk for thrombotic stroke. Cognitive Level: Comprehension 389 24. Of the following groups, who are at highest risk for a cerebrovascular accident (CVA)? a. Blacks over 65 years of age b. Whites over 65 years of age c. Blacks under 65 years of age d. Whites under 65 years of age ANS: A The individuals at highest risk for cerebrovascular accident would be blacks over 65. Blacks are at greater risks than whites. Older adults are at greater risk than younger adults. Older adults are at greater risks than younger adults, and blacks are at greater risks than whites. Cognitive Level: Comprehension 389 25. A 72-year-old male demonstrates left-sided weakness of upper and lower extremities. The symptoms lasted 4 hours and resolved with no evidence of infarction. The patient most likely experienced a(n): a. Stroke in evolution b. Arteriovenous malformation c. Transient ischemic attack d. Cerebral hemorrhage ANS: C When symptoms resolve with complete recovery, it is a transient ischemic attack. A stroke in evolution is an impending stroke, and symptoms would not resolve. An arteriovenous malformation is an abnormal arrangement of blood vessels that could lead to stroke, but is not a disorder in itself. Cerebral hemorrhage would not resolve. Cognitive Level: Comprehension 389 26. A major contributing process in CVAs is the development of atheromatous plaques in cerebral circulation. These most commonly form: a. In the larger veins b. Near capillary sphincters c. In cerebral arteries d. In the venous sinuses ANS: C Atheromatous plaques (stenotic lesion) form at branchings and curves in the cerebral circulation. Over 20 to 30 years, atheromatous plaques (stenotic lesion) form at branchings and curves in the cerebral circulation, primarily the arteries. Over 20 to 30 years, atheromatous plaques (stenotic lesion) form at branchings and curves in the cerebral circulation, not in the sphincters Over 20 to 30 years, atheromatous plaques (stenotic lesion) form at branchings and curves in the cerebral circulation, primarily in the arterial vessels. Cognitive Level: Comprehension 389 27. A 60-year-old female with a recent history of head trauma and a long-term history of hypertension presents to the ER for changes in mental status. MRI reveals that she had a hemorrhagic stroke. What does the nurse suspect caused this type of stroke? a. Rheumatic heart disease b. Thrombi c. Aneurysm d. Hypotension ANS: C The primary causative factor of a hemorrhagic stroke is an aneurysm. The primary causative factor of a hemorrhagic stroke is an aneurysm, not thrombi, which would lead to thrombotic stroke. A thrombi would lead to a CVA from blockage, but not to a hemorrhagic stroke. Hypertension, not hypotension, would lead to a hemorrhagic stroke. Cognitive Level: Comprehension 389 28. A 75-year-old male experienced a lacunar stroke. When looking through the history of the patients chart, which of the following would the nurse expect to find? a. An embolus b. Hypertension c. A hemorrhage d. An aneurysm ANS: B A lacunar stroke is associated with hypertension. A lacunar stroke is associated with hypertension, not an embolus. A lacunar stroke is associated with hypertension, not hemorrhage. A lacunar stroke is associated with hypertension, not an aneurysm. Cognitive Level: Comprehension 389 29. A 25-year-old male died from a gunshot wound to the heart. Upon autopsy, abnormalities in the media of the arterial wall and degenerative changes were detected. Which of the following most likely accompanied this finding? a. Fusiform aneurysm b. Saccular aneurysm c. Arteriovenous malformation d. Thrombotic stroke ANS: B Saccular aneurysms (berry aneurysms) occur frequently (in approximately 2% of the population) and likely result from congenital abnormalities in the media of the arterial wall and degenerative changes. Fusiform aneurysms (giant aneurysms) occur as a result of diffuse arteriosclerotic changes and are found most commonly in the basilar arteries or terminal portions of the internal carotid arteries. Arteriovenous malformation (AVM) is a tangled mass of dilated blood vessels creating abnormal channels between the arterial and venous systems. Thrombotic stroke would show signs of necrotic tissue, not degenerative changes. Cognitive Level: Comprehension 390 30. A 48-year-old female presents at the ER reporting an acute severe headache, nausea, photophobia, and nuchal rigidity. What does the nurse suspect caused these signs and symptoms? a. Diffuse brain injury b. Subarachnoid hemorrhage c. Epidural hematoma d. Classic concussion ANS: B With subarachnoid hemorrhage, meningeal irritation occurs, leading to nuchal rigidity. Diffuse brain injury is not associated with nuchal rigidity. Epidural hematoma is not associated with nuchal rigidity. Classic concussion is not associated with nuchal rigidity. Cognitive Level: Comprehension 390 31. A cause of hydrocephalus in subarachnoid hemorrhage is: a. Scarring of meninges and impairment of CSF resorption b. Choroid plexus injury c. Impairment of CSF flow through the ventricles d. Vasoconstriction related to carbon dioxide (CO2) changes in the cerebral circulation ANS: A A primary cause of hydrocephalus is impairment of CSF resorption that allows fluid to accumulate. A primary cause of hydrocephalus is impairment of CSF resorption that allows fluid to accumulate, not injury to the choroid plexus. A primary cause of hydrocephalus is impairment of CSF resorption. Flow of fluid through the ventricles could be affected, but it is the lack of resorption that leads to hydrocephalus. Vasoconstriction could lead to increased ICP, but it is the impairment of CSF resorption that allows fluid to accumulate. Cognitive Level: Comprehension 391 | p. 394 32. A 65-year-old male suffers a subarachnoid hemorrhage secondary to uncontrolled hypertension. He appears drowsy and confused with pronounced focal neurologic deficits. This condition is grade: a. I b. II c. III d. IV ANS: C With grade III, the patient experiences drowsiness and confusion with or without focal neurologic deficits and pronounced meningeal signs. With grade I, neurologic status is intact with mild headache and slight nuchal rigidity. With grade II, neurologic deficit is evidenced by cranial nerve involvement and moderate to severe headache with more pronounced meningeal signs (e.g., photophobia, nuchal rigidity). With grade IV, the patient is stuporous with pronounced neurologic deficits (e.g., hemiparesis, dysphasia) and nuchal rigidity. Cognitive Level: Comprehension 392 33. A 25-year-old female presents to her primary care provider reporting fever, headache, nuchal rigidity, and decreased consciousness. She was previously treated for sinusitis. Which of the following is the most likely diagnosis? a. Aseptic meningitis b. Bacterial meningitis c. Fungal meningitis d. Nonpurulent meningitis ANS: B Bacterial meningitis can occur secondary to sinusitis and is manifested by fever, tachycardia, chills, and a petechial rash with a severe throbbing headache, severe photophobia, and nuchal rigidity. The clinical manifestations of aseptic meningitis are milder than bacterial meningitis and are not associated with a previous infection such as sinusitis. Fungal meningitis presents as dementia. Nonpurulent meningitis is the same as aseptic and is milder and not associated with conditions such as sinusitis. Cognitive Level: Comprehension 394 34. A neurologist is teaching about encephalitis. Which information should the neurologist include? Most causes of encephalitis are: a. Bacterial b. Viral c. Fungal d. Toxoid ANS: B Most causes of encephalitis are viral. Most causes of encephalitis are viral, not bacterial. Most causes of encephalitis are viral, not fungal. Most causes of encephalitis are viral, not toxoid. Cognitive Level: Comprehension 395 35. A 15-month-old child from Pennsylvania was brought to the ER for fever, seizure activity, cranial palsies, and paralysis. Which of the following diagnosis will be documented in the chart? a. Eastern equine encephalitis b. Venezuelan encephalitis c. St. Louis encephalitis d. West Nile encephalitis ANS: A The symptoms indicate encephalitis, and given the residence of the child and the symptoms, the diagnosis is Eastern equine encephalitis. Venezuelan occurs in Texas, Florida, and the South. St. Louis occurs in Canada and the Pacific coast. West Nile occurs throughout the United States, but primarily affects the elderly. Cognitive Level: Comprehension 395 36. A 23-year-old female begins having problems with tiredness, weakness, and visual changes. Her diagnosis is multiple sclerosis (MS). What is occurring in the patients body? a. Depletion of dopamine in the central nervous system (CNS) b. Demyelination of nerve fibers in the CNS c. The development of neurofibril webs in the CNS d. Reduced amounts of acetylcholine at the neuromuscular junction ANS: B The pathophysiology of MS includes demyelination of nerve fibers. Depletion of dopamine is related to Parkinson disease. The development of neurofibrils is related to Alzheimer disease. Myasthenia gravis is due to decreased amounts of acetylcholine at the junction. Cognitive Level: Comprehension 397 37. When a patient asks, What is the cause of multiple sclerosis? how should the nurse reply? The cause of MS seems to be an interaction between: a. Vascular and metabolic factors b. Bacterial infection and the inflammatory response c. Autoimmunity and genetic susceptibility d. Neurotransmitters and inherited genes ANS: C Multiple sclerosis is due to an interaction between the autoimmune response and genetics. Multiple sclerosis is an autoimmune disorder. Multiple sclerosis is an autoimmune disorder that is thought to have developed secondary to a viral infection, not bacterial. Multiple sclerosis is not related to a neurotransmitter dysfunction. Cognitive Level: Comprehension 397 38. A patient is admitted with amyotrophic lateral sclerosis (ALS). Which classic assessment findings will support the diagnosis of ALS? a. Progressive dementia b. Muscle weakness and atrophy c. Severe paresthesias d. Autonomic dysfunctions ANS: B ALS is manifested by muscle weakness and atrophy. ALS is not manifested by dementia, but by muscle weakness and atrophy. ALS is not manifested by paresthesias, but by muscle weakness and atrophy. ALS is manifested by muscle weakness and atrophy. Cognitive Level: Comprehension 398 39. Which statement by a patient indicates teaching was successful regarding myasthenia gravis? Myasthenia gravis results from: a. Viral infection of skeletal muscle b. Atrophy of motor neurons in the spinal cord c. Demyelination of skeletal motor neurons d. Autoimmune injury at the neuromuscular junction ANS: D Myasthenia gravis is a disorder resulting from autoimmune injury at the neuromuscular junction. Myasthenia gravis is a disorder resulting from autoimmune injury at the neuromuscular junction, not from a viral infection. Myasthenia gravis is a disorder resulting from autoimmune injury at the neuromuscular junction. It is not due to motor neuron atrophy, but a lack of acetylcholine. MS is due to demyelination of skeletal motor neurons, not myasthenia gravis. Chapter 18. Alterations of Neurologic Function in Children MULTIPLE CHOICE 1. The nurse is assessing a 2-month-old infant. Which reflex of infancy will disappear first? a. Stepping b. Rooting c. Palmar grasp d. Moro reflex ANS: A The stepping reflex should no longer be obtainable at 6 weeks. The rooting reflex should no longer be obtainable at 4 months. The palmar grasp should no longer be obtainable at 6 months. The Moro reflex should no longer be obtainable at 3 months. Cognitive Level: Comprehension 410 2. A 10-month-old infant presents for a well-baby visit. Which of the following reflexes should be present at this age? a. Stepping b. Sucking c. Landau d. Palmar grasp ANS: C The Laundau reflex would be present up until 24 months. The stepping reflex should no longer be obtainable at 6 weeks. The sucking reflex should have disappeared by 10 months. The palmar grasp should no longer be obtainable at 6 months. Cognitive Level: Comprehension 410 3. The parents ask, During infancy, what is the fastest growing part of the body? How should the nurse respond? a. Spinal cord b. Limb bones c. Head d. Vertebral column ANS: C The head is the fastest growing part of the body during infancy. The head, not the spinal cord, is the fastest growing part of the body during infancy. The head, not the limb bones, is the fastest growing part of the body during infancy. The head, not the vertebral column, is the fastest growing part of the body during infancy. Cognitive Level: Comprehension 409 4. A nurse is preparing to teach about the most common defects of neural tube closure. Which one should the nurse discuss? a. Anterior b. Posterior c. Lateral d. Superior ANS: B Posterior neural tube defects are the most common. Posterior, not anterior, neural tube defects are most common. Posterior, not lateral, neural tube defects are most common. Posterior, not superior, neural tube defects are most common. Cognitive Level: Comprehension 411 5. An infant has an anterior midline defect of neural tube closure. What term will the nurse observe written on the chart? a. Anencephaly b. Myelodysplasia c. Cyclopia d. Hydrocephalus ANS: C Cyclopia is an example of an anterior midline defects that may cause brain and face abnormalities. In anencephaly, the soft, bony component of the skull and part of the brain are missing. Myelodysplasia is a posterior neural tube disorder. Hydrocephalus is associated with accelerated head growth. Cognitive Level: Comprehension 410 6. What nutrient should the nurse encourage a woman in the early stages of pregnancy to consume to prevent neural tube defects? a. Protein b. Iron c. Vitamin D d. Folic acid ANS: D Folic acid deficiency during early stages of pregnancy increases the risk for neural tube defects. Protein does not lead to neural tube defects; folic acid does. Iron does not lead to neural tube defects; folic acid does. Vitamin D does not lead to neural tube defects; folic acid does. Cognitive Level: Comprehension 410 7. A newborn child has a herniation of brain and meninges through a defect in the occipital area of the skull. What will the pediatrician call this condition? a. Encephalocele b. Meningocele c. Myelomeningocele d. Craniosynostosis ANS: A An encephalocele refers to a herniation or protrusion of brain and meninges through a defect in the occipital region of the skull, resulting in a saclike structure. A meningocele is a saclike cyst of meninges filled with spinal fluid, a mild form of posterior neural tube closure defect. These can occur throughout the cervical, thoracic, and lumbar spine areas. A myelomeningocele is a hernial protrusion of a saclike cyst (containing meninges, spinal fluid, and a portion of the spinal cord with its nerves) through a defect in the posterior arch of a vertebra in the lower spine. Craniosynostosis is the premature closure of one or more of the cranial sutures (saggital, coronal, lambdoid, metopic) during the first 18 to 20 months of the infants life. Cognitive Level: Comprehension 411 8. A newborn child has a hernial protrusion of a saclike cyst through a defect in the posterior arch of a vertebra. This condition is referred to as: a. Craniosynostosis b. Meningocele c. Encephalocele d. Myelomeningocele ANS: D A myelomeningocele is a hernial protrusion of a saclike cyst (containing meninges, spinal fluid, and a portion of the spinal cord with its nerves) through a defect in the posterior arch of a vertebra in the lower spine. Craniosynostosis is the premature closure of one or more of the cranial sutures (saggital, coronal, lambdoid, metopic) during the first 18 to 20 months of the infants life. A meningocele, a saclike cyst of meninges filled with spinal fluid, is a mild form of posterior neural tube closure defect. These can occur throughout the cervical, thoracic, and lumbar spine areas. An encephalocele refers to a herniation or protrusion of brain and meninges through a defect in the occipital region of the skull, resulting in a saclike structure. Cognitive Level: Comprehension 412 9. A 19-month-old boy developed a premature closure of one or more of the cranial sutures. Which diagnosis will the nurse observe on the chart? a. Craniosynostosis b. Congential hydrocephalus c. Microcephaly d. Acrania ANS: A Craniosynostosis is the premature closure of one or more of the cranial sutures. Congenital hydrocephalus is characterized by enlargement of the cerebral ventricles. Microcephaly is lack of brain growth with retarded mental and motor development. In acrania, the cranial vault is almost completely absent; an extensive defect of the vertebral column often is present. Cognitive Level: Comprehension 413 10. A baby is stillborn after 6 hours of labor. Autopsy reveals hydrocephalus caused by cystic dilation of the fourth ventricle and aqueductal compression. Which of the following is the most likely diagnosis? a. Congenital hydrocephalus b. Microcephaly c. Dandy-Walker deformity d. Macewen sign ANS: C The Dandy-Walker malformation is a congenital defect of the cerebellum characterized by a large posterior fossa cyst, which communicates with the 4th ventricle, and an atrophic upwardly rotated cerebellar vermis. Congenital hydrocephalus is characterized by enlargement of the cerebral ventricles. Microcephaly is lack of brain growth with retarded mental and motor development. Macewen sign is characterized by separation of the cranial sutures with a resonant sound when the skull is tapped. Cognitive Level: Comprehension 414 11. The parents of an infant born with true microcephaly ask what caused this. How should the nurse respond? True microcephaly can be caused by: a. Viral infection b. An autosomal recessive gene c. Fetal trauma d. Hydrocephalus ANS: B True (primary) microcephaly is usually caused by an autosomal recessive genetic or chromosomal defect. Viral infections can lead to microcephaly, but is not the true cause. Fetal trauma can lead to microcephaly, but is not the true cause. Hydrocephalus does not lead to microcephaly. Cognitive Level: Comprehension 413 12. An infant is diagnosed with congenital hydrocephalus. Which of the following characteristics would the nurse expect to find? a. Enlarged ventricles b. Decreased cerebrospinal fluid (CSF) production c. Increased resorption of CSF d. Smaller than average head circumference ANS: A Congenital hydrocephalus is characterized by enlargement of the cerebral ventricles. Increased, not decreased, CSF production would lead to hydrocephalus. Decreased resorption of CSF would lead to hydrocephalus, not increased CSF. An infant with congenital hydrocephalus would have increased head circumference. Cognitive Level: Comprehension 415 13. An aide asks what the most common type of cerebral palsy is. What is the nurses best response? a. Ataxic b. Dystonic c. Spastic d. Mixed ANS: C Spastic cerebral palsy accounts for approximately 70% to 80% of cerebral palsy cases. Ataxic cerebral palsy accounts for 5% to 10% of cerebral palsy cases. Dystonic cerebral palsy accounts for 10% to 20% of cerebral palsy cases. Mixed cases accounts for 13% of cerebral palsy cases. Cognitive Level: Comprehension 415 14. A child is diagnosed with cerebral palsy, characterized by extreme difficulty in fine motor coordination and purposeful movement. Which of the following types of cerebral palsy is the child experiencing? a. Ataxic b. Dystonic c. Spastic d. Mixed ANS: B Dystonic cerebral palsy is associated with extreme difficulty in fine motor coordination and purposeful movements. Ataxic cerebral palsy manifests with gait disturbances and instability. The infant with this form of cerebral palsy may have hypotonia at birth, but stiffness of the trunk muscles develops by late infancy. Spastic cerebral palsy is associated with increased muscle tone, persistent primitive reflexes, hyperactive deep tendon reflexes, clonus, rigidity of the extremities, scoliosis, and contractures. Mixed cerebral palsy may have symptoms of each of the disorders. Cognitive Level: Comprehension 415 15. Which of the following diseases does the nurse screen for in all newborns? a. Epilepsy b. Tay-Sachs disease c. Pica d. Phenylketonuria (PKU) ANS: D All newborns are screened for PKU. All newborns are screened for PKU, not epilepsy. All newborns are screened for PKU, not Tay-Sachs. All newborns are screened for PKU, not pica. Cognitive Level: Comprehension 416 16. Parents of a 3-month-old infant bring him to the emergency room (ER) after he has had a seizure. He has muscle rigidity, and the parents report they are of Jewish ancestry. For what genetic disease should this infant be screened? a. Juvenile myoclonic epilepsy b. Congenital encephalopathy c. Tay-Sachs disease d. PKU ANS: C Perhaps the best known of the lysosomal storage disorders is Tay-Sachs disease, an autosomal recessive disorder related to a deficiency of the enzyme hexosaminidase A (HEX A). Approximately 80% of individuals diagnosed are of Jewish ancestry. The infant should be screened for Tay-Sachs, due to the Jewish ancestry, not epilepsy. The infant should be screened for Tay-Sachs, due to the Jewish ancestry, not encephalopathy. All children are screened for PKU, but children of Jewish ancestry should be screened for Tay- Sachs. Cognitive Level: Comprehension 416 17. A child is brought to the ER. Initial examination documents the following assessment findings: tissue ischemia, anemia, and an apparent decrease in normal growth rate. Which of the following poisons should the nurse determine to be the most likely cause? a. Ethyl alcohol b. Lead c. Mercury d. Carbon monoxide ANS: B High blood levels of lead occur in lead poisoning. If lead poisoning is untreated, lead encephalopathy results and is responsible for serious and irreversible neurological damage. The child is experiencing symptoms of lead poisoning, not ethyl alcohol. The child is experiencing symptoms of lead poisoning, not mercury. The child is experiencing symptoms of lead poisoning, not carbon monoxide. Cognitive Level: Comprehension 418 18. To prevent Reye syndrome in infants, which of the following instructions should the nurse give to parents? a. Breast-feed infants as long as possible. b. Treat fevers with acetaminophen, not aspirin. c. Lock up hazardous cleaning agents. d. Remove lead paint from the home. ANS: B Reye syndrome is associated with treating fever with aspirin. Reye syndrome is associated with aspirin use and is not related to breast-feeding. It is important to lock up hazardous cleaning agents, but aspirin is the contributing factor for Reye syndrome. Removing lead paint is important, but lead is not associated with Reye syndrome. Cognitive Level: Comprehension 418 19. A child presents to his primary care provider with disorientation, delirium, aggressiveness, and stupor. His parents report that he was recently ill with an upper respiratory infection, which they treated with aspirin. Which of the following is the most likely diagnosis? a. Epilepsy b. Reye syndrome c. Tay-Sachs d. PKU ANS: B The manifestations of the Reye syndrome are disorientation, delirium, aggressiveness and combativeness, central neurological hyperventilation, shallow breathing, hyperactive reflexes, and stupor. It is associated with the taking of aspirin. Epilepsy is manifested by jerking motions. Tay-Sachs is manifested by exaggerated startle to loud noise, seizures, developmental regression, dementia, and blindness. PKU is manifested by brain damage. Cognitive Level: Comprehension 418 20. A child was recently diagnosed with varicella, for which her parents gave her aspirin. The child is now in a coma, is hyperventilating, and has decorticate rigidity. Pupil response is within normal limits. The child is diagnosed with Reye syndrome at stage: a. 1 b. 2 c. 3 d. 4 ANS: C Stage 3 is manifested by obtundation, coma, hyperventilation, and decorticate rigidity. Stage 1 is manifested by vomiting, lethargy, and drowsiness. Stage 2 is manifested by disorientation, delirium, aggressiveness and combativeness, central neurological hyperventilation, shallow breathing, hyperactive reflexes, and stupor. Stage 4 is manifested by deepening coma, decerebrate rigidity, loss of ocular reflexes, large fixed pupils, and divergent eye movements. Cognitive Level: Comprehension 418 21. A 3-year-old has bacterial meningitis. What should the nurse expect to find on the lab report for the most common cause of this bacterial meningitis? a. Haemophilus influenzae b. Neisseria meningitidis c. Streptococcus pneumonia d. Escherichia coli ANS: B The most common cause of bacterial meningitis in children under 5 is Neisseria meningitidis. Haemophilus influenzae formerly was the most common cause of bacterial meningitis but vaccines have decreased this. The most common cause is now Neisseria meningitidis. Streptococcus pneumonia can cause meningitis, but the most common cause of bacterial meningitis in children under 5 is Neisseria meningitidis. Escherichia coli is the most common cause of meningitis in the newborn, but the most common cause of bacterial meningitis in children under 5 is Neisseria meningitidis. Cognitive Level: Comprehension 418 22. A nurse is teaching the staff about viral meningitis. Which information should the nurse include? Viral meningitis: a. Is always sudden in onset b. Often occurs with measles, mumps, or herpes c. Is effectively treated with antibiotics d. Causes increased sugar in the CSF ANS: B Viral meningitis may result from a direct infection of a virus, or it may be secondary to disease, such as measles, mumps or herpes. Onset may be sudden or gradual. Treatment is symptomatic; antibiotics are not used. Glucose in the CSF is normal. Cognitive Level: Comprehension 418 23. A 3-year-old African-American child was diagnosed with sickle cell disease. She is now suffering from meningitis. Which is the most likely microorganism the nurse will find on the lab report? a. Virus b. Haemophilus influenzae type B c. Streptococcus pneumonia d. Neisseria meningitidis ANS: C 1 in every 24 children with sickle cell disease develops pneumococcal meningitis by the age of 4 years. 1 in every 24 children with sickle cell disease develops pneumococcal meningitis by the age of 4 years, not a virus. 1 in every 24 children with sickle cell disease develops pneumococcal meningitis by the age of 4 years, not Haemophilus influenzae. 1 in every 24 children with sickle cell disease develops pneumococcal meningitis by the age of 4 years not Neisseria meningitidis. Cognitive Level: Comprehension 418 24. When should be the best time for the nurse to assess for the vomiting and headache that are symptoms of a brain tumor in children? a. Morning b. Early afternoon c. As the sun goes down and darkness begins d. During the middle of the night ANS: A Headache and vomiting occur more commonly in the morning. Vomiting is not preceded by nausea and may become projectile. Headache and vomiting occur more commonly in the morning, not the early afternoon. Headache and vomiting occur more commonly in the morning, not as the sun goes down. Headache and vomiting occur more commonly in the morning, not at night. Cognitive Level: Comprehension 419 25. A nurse recalls the most frequent location of a neuroblastoma is: a. Retroperitoneal region b. Mediastinum c. Cervical ganglion d. Lung ANS: A 65% of neuroblastomas occur in the retroperitoneal region. 15% of neuroblastomas occur in the mediastinum. 4% of neuroblastomas occur in the cervical ganglion. Neuroblastomas do not occur in the lung. Cognitive Level: Comprehension 421 26. A nurse is preparing to teach about brain tumors. Which information should the nurse include? The most common type of brain tumor in children is: a. Neuroblastoma b. Astrocytoma c. Meningioma d. Glioma ANS: B Astrocytoma is the most common type of brain tumor in children. Astrocytoma is the most common type of brain tumor in children, not neuroblastoma. Astrocytoma is the most common type of brain tumor in children, not meningioma. Astrocytoma is the most common type of brain tumor in children, not glioma. Cognitive Level: Comprehension 419 27. When a nurse is asked where the most common location of brain tumors in children is found, how should the nurse respond? a. In the area always above the cerebellum b. In the posterior fossa c. In the cerebrum d. In the ventricular lining ANS: B Two-thirds of all pediatric brain tumors are found in the posterior fossa. Two-thirds of all pediatric brain tumors are found in the posterior fossa, not above the cerebellum. Two-thirds of all pediatric brain tumors are found in the posterior fossa, not in the cerebrum. Two-thirds of all pediatric brain tumors are found in the posterior fossa, not in the ventricular lining. Cognitive Level: Comprehension 419 28. A 10-year-old male presents with headache and seizures. CT scan reveals a tumor that is located near the optic chiasm. Which of the following is the most likely tumor type? a. Astrocytoma b. Craniopharyngioma c. Ependymoma d. Medulloblastoma ANS: B A craniopharyngioma originates from the pituitary gland or hypothalamus. Symptoms include headache, seizures, diabetes insipidus, early onset of puberty, and growth delay. Astrocytomas are located on the surface of the right or left cerebellar hemisphere and cause unilateral symptoms (occurring on the same side as the tumor), such as head tilt, limb ataxia, and nystagmus. Ependymoma develops in the fourth ventricle and arises from the ependymal cells that line the ventricular system. Because both tumors are located in the posterior fossa region along the midline, presenting signs and symptoms are similar and are usually related to hydrocephalus and increased intracranial pressure. Medulloblastoma occurs as an invasive malignant tumor that develops in the vermis of the cerebellum and may extend into the fourth ventricle. Cognitive Level: Comprehension 421 MULTIPLE RESPONSE 1. A newborn child is diagnosed with a vertebral arch defect, spina bifida. This condition would lead the nurse to suspect the child may have which of the following as well? (Select all that apply) a. Type II Chiari malformation b. Myelomeningocele c. Meningocele d. Acrania e. Craniosynostosis ANS: B, C When meningocele and myelomeningocele occur, they are related to an accompanying vertebral defect that allows the protrusion of the neural tube contents. When meningocele and myelomeningocele occur, they are related to an accompanying vertebral defect that allows the protrusion of the neural tube contents. Type II Chiari malformation is a complex malformation of the brain stem and cerebellum in which the cerebellar tonsils are displaced downward into the cervical spinal canal. This does not occur through a spina bifida. In acrania, the cranial vault is almost completely absent; an extensive defect of the vertebral column often is present. Craniosynostosis is the premature closure of one or more of the cranial sutures. Chapter 19. Mechanisms of Hormonal Regulation MULTIPLE CHOICE 1. A nurse recalls direct stimulation of the insulin-secreting cells of the pancreas by the autonomic nervous system is an example of control. a. Negative feedback b. Positive feedback c. Neural d. Substrate-level dependent ANS: C Direct stimulation of the insulin-secreting cells of the pancreas by the autonomic nervous system is a form of neural control. Stimulation of the insulin cells of the pancreas by the autonomic nervous system is a form of neural control and is not regulated as a form of negative feedback. Negative feedback works like a thermostat. Stimulation of the insulin cells of the pancreas by the autonomic nervous system is a form of neural control and is not regulated as a form of positive feedback. Stimulation of the insulin cells of the pancreas by the autonomic nervous system is a form of neural control and is not substrate-level dependent. Cognitive Level: Comprehension 427 2. A nurse is teaching staff about protein hormones. Which information should the nurse include? One of the protein hormones is: a. Thyroxine (T4) b. Aldosterone c. Testosterone d. Insulin ANS: D Protein hormones are also water-soluble hormones, and insulin is a part of this group. Thyroxine is a lipid soluble hormone and is not a protein hormone. Aldosterone is a lipid soluble hormone and is not a protein hormone. Testosterone is a lipid soluble hormone and is not a protein hormone. Cognitive Level: Comprehension 427 3. A 45-year-old female has elevated thyroxine production. Which of the following would accompany this condition? a. Increased thyroid-releasing hormone (TRH) b. Increased anterior pituitary stimulation c. Decreased T4 d. Decreased thyroid-stimulating hormone (TSH) ANS: D Secretion of TSH stimulates the synthesis and secretion of thyroid hormones. Increasing levels of T4 and T3 then feed back negatively on the pituitary and hypothalamus to inhibit TRH and TSH synthesis. With increased thyroxine production, TRH will be decreased. Increased thyroxine would lead to decreased anterior pituitary stimulation. Thyroxine is T4; its level will be elevated. Cognitive Level: Comprehension 427 4. An endocrinologist isolated a new hormone and found it to be a water-soluble amine. Which of the following is most like this new hormone? a. Growth hormone (GH) b. Luteinizing hormone (LH) c. Antidiuretic hormone (ADH) d. Epinephrine ANS: D An example of a water-soluble amine is epinephrine. GH is a water-soluble hormone but is a peptide. LH is water-soluble hormone but is a polypeptide. ADH is water-soluble hormone but is a polypeptide. Cognitive Level: Comprehension 427 5. When insulin binds to its receptors on muscle cells, an increase in glucose uptake by the muscle cells occurs. This is an example of a effect by a hormone. a. Pharmacologic b. Permissive c. Biphasic d. Direct ANS: D Direct effects are the obvious changes in cell function that result specifically from stimulation by a particular hormone as is true with insulin. Pharmacologic effects are the result of high doses of a drug. Permissive effects are less obvious hormone-induced changes that facilitate the maximal response or functioning of a cell. Biphasic effects are twofold effects. Cognitive Level: Comprehension 429 6. A 30-year-old male was diagnosed with hypothyroidism. Synthesis of which of the following would decrease in this patient? a. Corticosteroid B globulin b. Sex hormone-binding globulin c. Thyroid-binding globulin d. Albumin ANS: C TH is transported in the blood in bound and free forms. Most of the TH is transported bound to thyroxine-binding globulin (TBG); thus, if TH is low, the patient would also be low in TBG. Thyroid-binding globulin is decreased with hypothyroidism, not corticosteroid B globulin. Thyroid-binding globulin is decreased with hypothyroidism, not sex hormone-binding globulin. Thyroid-binding globulin is decreased with hypothyroidism, not albumin. Cognitive Level: Comprehension 428 7. A patient has high levels of hormones. To adapt to the high hormone concentrations, the patients target cells have the capacity for: a. Negative feedback b. Positive feedback c. Down-regulation d. Up-regulation ANS: C High concentrations of hormone decrease the number of receptors; this is called down- regulation; thus, the cell can adjust its sensitivity to the concentration of the signaling hormone. Adaptation to high hormone concentration is the process of down-regulation. Negative feedback regulates hormone release. Adaptation to high hormone concentration is the process of down-regulation. Positive feedback regulates some forms of hormone release. Up-regulation is a response to low concentrations of hormone, thus increasing the number of receptors per cell. Cognitive Level: Comprehension 429 8. A patient has researched lipid-soluble hormones on the Internet. Which information indicates the patient has a good understanding? Lipid-soluble hormone receptors cross the plasma membrane by: a. Diffusion b. Osmosis c. Active transport d. Endocytosis ANS: A Lipid-soluble hormones cross the plasma membrane by diffusion. Lipid-soluble hormones cross by diffusion, not osmosis. Lipid-soluble hormones cross by diffusion, not active transport. Lipid-soluble hormones cross by diffusion, not endocytosis. Cognitive Level: Comprehension 431 9. When a patient asks about target cell receptors, which is the nurses best response? Target cell receptors for most water-soluble hormones are located in the: a. Cytosol b. Cell membrane c. Endoplasmic reticulum d. Nucleus ANS: B Water-soluble hormones bind to cell surface receptors. Water-soluble hormones bind to cell surface receptors, not cytosol. Water-soluble hormones bind to cell surface receptors, not endoplasmic reticulum. Water-soluble hormones bind to cell surface receptors, not the nucleus. Cognitive Level: Comprehension 427 10. When the endocrinologist asks the staff how the releasing hormones that are made in the hypothalamus travel to the anterior pituitary, how should the staff reply? Via the: a. Vessels of the zona fasciculata b. Chromophils c. Median eminence d. Hypophysial portal system ANS: D Neurons in the hypothalamus secrete releasing hormones into veins that carry the releasing hormones directly to the vessels of the adenohypophysis via the hypophysial portal system, thus bypassing the normal circulatory route. Zona fasciculata secretes abundant amounts of cortisol from the adrenal gland. Chromophils are the secretory cells of the adenohypophysis. The median eminence is a part of the posterior pituitary, not the anterior. Cognitive Level: Comprehension 433 11. An aide asks the nurse what activates tyrosine. What is the nurses best response? a. GH b. PRL c. Insulin d. Estrogen ANS: C Insulin receptor binding activates tyrosine kinase autophosphorylation and sends a cascade of signals to activate glucose transporters. Insulin binding, not growth hormone, activates tyrosine. Insulin, not PRL, activates tyrosine. Insulin, not estrogen, activates tyrosine. Cognitive Level: Comprehension 430 12. A nurse recalls prolactin-inhibiting factors target tissue is the: a. Hypothalamus b. Anterior pituitary c. Mammary glands d. Posterior pituitary ANS: B Prolactin-inhibiting factor (PIF) inhibits prolactin secretion by the anterior pituitary. PIF inhibits prolactin secretion by the anterior pituitary, not the hypothalamus. PIF inhibits prolactin secretion by the anterior pituitary, not the mammary glands. PIF inhibits prolactin secretion by the anterior pituitary, not the posterior pituitary. Cognitive Level: Comprehension 444 13. When a staff member asks the nurse which gland secretes ADH and oxytocin, how should the nurse respond? a. Anterior pituitary b. Posterior pituitary c. Hypothalamus d. Pineal gland ANS: B The posterior pituitary secretes ADH, which also is called vasopressin, and oxytocin. The anterior pituitary secretes ACTH, melanocyte-stimulating hormone (MSH), somatotropic hormones (GH, prolactin), and glycoprotein hormonesfollicle-stimulating hormone (FSH), LH, and TSH. The hypothalamus secretes PRF, which stimulates secretion of prolactin; PIF (dopamine), which inhibits prolactin secretion; TRH, which affects release of thyroid hormones; GH-releasing hormone (GHRH), which stimulates the release of GH; somatostatin, which inhibits the release of GH; gonadotropin-releasing hormone (GnRH), which facilitates release FSH and LH; corticotropin-releasing hormone (CRH), which facilitates the release of ACTH and endorphins; and substance P, which inhibits ACTH release and stimulates release of a variety of other hormones. The pineal gland secretes melatonin. Cognitive Level: Comprehension 444 14. If a patients posterior pituitary is removed, which hormone would the nurse expect to decrease? a. PRF b. ADH c. ACTH d. GH ANS: B The hormones ADH and oxytocin are released from the posterior pituitary gland. PRF is released by the hypothalamus. ACTH is released by the anterior pituitary. GH is released by the hypothalamus. Cognitive Level: Comprehension 435 15. Which principle should the nurse include while planning care for a patient with an ADH problem? ADH release from the posterior pituitary is stimulated by: a. Low blood pressure sensed by baroreceptors in the kidneys b. High serum osmolarity sensed by osmoreceptors in the hypothalamus c. Low osmolality sensed by osmoreceptors in the kidneys d. High concentration of potassium sensed by chemoreceptors in the carotid body ANS: B As plasma osmolality increases, these osmoreceptors are stimulated, the rate of ADH secretion increases, more water is reabsorbed from the kidney, and the plasma is diluted back to its set- point osmolality. ADH release is stimulated by high serum osmolality, not lowered blood pressure. ADH release is stimulated by high serum osmolality, not low osmolality. ADH release is stimulated by high serum osmolality, not high concentrations of potassium. Cognitive Level: Comprehension 435 16. A patient wants to know why ADH is important in the body. What is the nurses best response? ADH is important in: a. The bodys water balance and urine concentration b. Maintaining electrolyte levels and concentrations c. Follicular maturation d. Regulation of metabolic processes ANS: A ADH is important in the bodys water balance and its ability to concentrate urine. ADH aids in water balance, not electrolyte levels. ADH aids in water balance, not follicular maturation. ADH aids in water balance, not metabolic processes. Cognitive Level: Comprehension 429 17. If a patient had a problem with the hypothalamus, which of the following hormones would be affected? a. ACTH b. Oxytocin c. ADH d. TSH ANS: B The hypothalamus secretes oxytocin. The anterior pituitary secretes ACTH. The posterior pituitary secretes ADH. The anterior pituitary secretes TSH. Cognitive Level: Comprehension 431 18. A nurse is teaching the staff about oxytocin. Which information should the nurse include? Target cells for oxytocin are located in the: a. Renal tubules b. Thymus c. Liver d. Uterus ANS: D Oxytocin causes uterine contraction and lactation in women and may have a role in sperm motility in men. Oxytocin does not stimulate the renal tubules; it stimulates the uterus. Oxytocin does not stimulate the thymus; it stimulates the uterus. Oxytocin does not stimulate the liver; it stimulates the uterus. Cognitive Level: Comprehension 435 19. A 50-year-old male patient is deficient in ADH production. Which of the following assessment findings would the nurse expect to find? a. Increased blood volume b. Increased urine osmolality c. Increased urine volume d. Increased arterial vasoconstriction ANS: C With deficient ADH, the kidneys would not concentrate urine leading to increased urine output. Blood volume would decrease with increased renal excretion of fluid. Urine osmolality would decrease. Arteries would dilate with deficient ADH production. REF: pp. 434-435 20. A 70-year-old female has brittle bones secondary to osteoporosis. Her primary care provider prescribes calcitonin to: a. Activate vitamin D b. Stimulate osteoclastic activity c. Inhibit calcium resorption from bones d. Promote thyroid hormone release ANS: C Calcitonin lowers serum calcium levels by inhibition of bone-resorbing osteoclasts. Calcitonin inhibits bone-resorbing osteoclasts; it does not activate vitamin D. Calcitonin inhibits bone-resorbing osteoclasts; not stimulate it. Calcitonin inhibits bone-resorbing osteoclasts; it does not promote thyroid hormone release. Cognitive Level: Comprehension 14 | p. 17 | p. 435 21. Which nutrient would the nurse encourage the patient to consume for thyroid hormone synthesis? a. Zinc b. Sodium c. Iodine d. Calcium ANS: C Iodine is necessary for the synthesis of thyroid hormone. Iodine, not zinc, is necessary for synthesis of thyroid hormone. Iodine, not sodium, is necessary for synthesis of thyroid hormone. Iodine, not calcium, is necessary for synthesis of thyroid hormone. Cognitive Level: Comprehension 436 22. A nurse is reviewing lab results. Which of the following lab results would slow down the rate of parathyroid hormone secretion? a. Increased serum calcium levels b. Decreased serum calcium levels c. Decreased levels of TSH d. Increased levels of TSH ANS: A An increase in serum calcium inhibits parathyroid hormone (PTH) secretion. An increase, not a decrease, in serum calcium inhibits PTH secretion. Thyroid-stimulating hormone would not affect PTH secretion. Thyroid-stimulating hormone would not affect PTH secretion. Cognitive Level: Comprehension 16 | p. 17 | p. 437 23. A 40-year-old male undergoes surgery for a PTH-secreting tumor in which the parathyroid is removed. Which of the following would the nurse expect following surgery? a. Increased serum calcium b. Decreased bone formation c. Decreased calcium reabsorption in the kidney d. Increased calcitonin ANS: C PTH also acts on the kidney to increase calcium reabsorption and to decrease phosphate reabsorption. Removal of the PTH-secreting tumor would result in decreased calcium reabsorption in the kidney, not increased serum calcium. Removal of the PTH-secreting tumor would result in decreased calcium reabsorption in the kidney, not decreased bone formation. Removal of the PTH-secreting tumor would result in decreased calcium reabsorption in the kidney, not increased calcitonin. Cognitive Level: Comprehension 437 24. A nurse is teaching a patient about insulin. Which information should the nurse include? Insulin is primarily regulated by: a. Metabolic rate b. Serum glucose levels c. Prostaglandins d. Enzyme activation ANS: B Insulin secretion is promoted when blood levels of glucose rise. Insulin secretion is not based on metabolic rate but on blood levels of glucose. Insulin secretion is not based on prostaglandins but on blood levels of glucose. Insulin secretion is not based on enzyme activation but on blood levels of glucose. Cognitive Level: Comprehension 437 25. A 30-year-old male is diagnosed with a hormone-secreting tumor of the pancreas alpha cells. Which of the following would the nurse expect to be most likely increased in this patient? a. Amylin b. Glucagon c. Insulin d. Somatostatin ANS: B Glucagon is produced by the alpha cells of the pancreas. Amylin is secreted by the beta cells. Insulin is secreted by the beta cells. Somatostatin is produced by the delta cells. Cognitive Level: Comprehension 439 26. A nurse recalls insulin has an effect on which of the following groups of electrolytes? a. Sodium, chloride, phosphate b. Calcium, magnesium, potassium c. Hydrogen, bicarbonate, chloride d. Potassium, magnesium, phosphate ANS: D Insulin facilitates the intracellular transport of potassium (K+), phosphate, and magnesium. Insulin facilitates the intracellular transport of potassium (K+), phosphate, and magnesium, not sodium and chloride. Insulin facilitates the intracellular transport of potassium (K+), phosphate, and magnesium, not calcium. Insulin facilitates the intracellular transport of potassium (K+), phosphate, and magnesium, not hydrogen, bicarbonate, and chloride. Cognitive Level: Comprehension 439 27. A student asks the instructor which of the following is the most potent naturally occurring glucocorticoid. How should the instructor respond? a. Aldosterone b. Testosterone c. Cortisol d. Prolactin ANS: C The most potent naturally occurring glucocorticoid is cortisol. The most potent naturally occurring glucocorticoid is cortisol, not aldosterone. The most potent naturally occurring glucocorticoid is cortisol, not testosterone. The most potent naturally occurring glucocorticoid is cortisol, not prolactin. Cognitive Level: Comprehension 441 28. A patient wants to know what can cause ACTH to be released. How should the nurse respond? a. High serum levels of cortisol b. Hypotension c. Hypoglycemia d. Stress ANS: D Stress increases ACTH secretion. ACTH regulates the release of cortisol from the adrenal cortex. It is not stimulated by high serum levels. Hypotension does not stimulate ACTH. Hypoglycemia does not stimulate ACTH. Chapter 20. Alterations of Hormonal Regulation Test Bank MULTIPLE CHOICE 1. A nurse is discussing endocrine system dysfunction with a patient. Which statement indicates the patient understood? Endocrine system dysfunction can result from hyposecretion, hypersecretion, or from: a. Abnormal receptor activity b. Abnormal hormone levels c. Increased synthesis of second messengers d. Extracellular electrolyte alterations ANS: A Dysfunction may result from abnormal cell receptor function or from altered intracellular response to the hormone-receptor complex. Abnormal hormone levels can occur, but are not the cause. Intracellular storage of hormones would not lead to dysfunction; receptor function does. Extracellular electrolyte alterations may result from dysfunction, but it is not a cause. Cognitive Level: Comprehension 448 2. An aide asks the nurse what is the most common cause of elevated levels of antidiuretic hormone (ADH) secretion. How should the nurse respond? a. Autoimmune disease b. Cancer c. Pregnancy d. Heart failure ANS: B The most common cause of elevated levels of ADH is cancer. The most common cause of elevated levels of ADH is cancer, not autoimmune disorders. The most common cause of elevated levels of ADH is cancer, not pregnancy. The most common cause of elevated levels of ADH is cancer, not heart failure. Cognitive Level: Comprehension 449 3. A 54-year-old patient with pulmonary tuberculosis (lung infection) is evaluated for syndrome of inappropriate ADH secretion (SIADH). Which of the following electrolyte imbalances would be expected in this patient? a. Hyponatremia b. Hyperkalemia c. Hypernatremia d. Hypokalemia ANS: A Hyponatremia occurs due to increased water reabsorption by kidneys. Hyperkalemia does not occur, but hyponatremia occurs due to increased water reabsorption. Sodium levels are lowered, with hyponatremia they are not elevated. Hypokalemia does not occur; SIADH is a problem of sodium. Cognitive Level: Comprehension 449 4. A 44-year-old patient with pulmonary tuberculosis (lung infection) is evaluated for SIADH. Which of the following assessment findings would be expected in this patient? a. Peripheral edema b. Tachycardia c. Low blood pressure d. Concentrated urine ANS: D Clinical manifestations of SIADH include urine that is inappropriately concentrated with respect to serum osmolarity. Peripheral edema is not a symptom of SIADH; concentrated urine is. Tachycardia is not a symptom of SIADH, but confusion and lethargy are. Low blood pressure is not a symptom of SIADH, but gastrointestinal symptoms and dyspnea are. Cognitive Level: Comprehension 449 5. A nurse is caring for a patient with SIADH. What severe complication should the nurse assess for? a. Stroke b. Diabetes insipidus c. Neurologic damage d. Renal failure ANS: C When the hyponatremia of SIADH becomes severe, 110 mEq/L to 115 mEq/L, confusion, lethargy, muscle twitching, convulsions, and severe and sometimes irreversible neurologic damage may occur. Stoke is not associated with SIADH, but confusion and convulsions do occur. Diabetes insipidus is not associated with SIADH, as it is manifested by increased urine output and in SIADH urine output decreases. Neurological failure, not renal failure, occurs in SIADH. Cognitive Level: Comprehension 449 6. A 22-year-old male is admitted to the intensive care unit with a closed head injury sustained in a motorcycle accident. The injury has caused severe damage to the posterior pituitary. Which of the following complications should the nurse anticipate? a. Dilutional hyponatremia b. Dehydration from polyuria c. Cardiac arrest from hyperkalemia d. Metabolic acidosis ANS: B Diabetes insipidus is a well-recognized complication of closed head injury and is manifested by polyuria leading to dehydration. The patient will experience hypernatremia, not hyponatremia. Electrolytes other than sodium are typically not affected with diabetes insipidus. Acidosis is not associated with diabetes insipidus. Cognitive Level: Comprehension 449 7. While planning care for a patient from general anesthesia, which principle should the nurse remember? A side effect of some general anesthetic agents is diabetes insipidus. a. Neurogenic b. Nephrogenic c. Psychogenic d. Allogenic ANS: B General anesthetics can lead to nephrogenic diabetes insipidus. General anesthetics can lead to nephrogenic, not neurogenic, diabetes insipidus; neurogenic diabetes may be due to primary brain tumors, hypophysectomy, aneurysms, thrombosis, infections, and immunologic disorders and head injury. General anesthetics can lead to nephrogenic, not psychogenic, diabetes insipidus; psychogenic is due to ingestion of large quantities of fluid. General anesthetics can lead to nephrogenic, not allogenic, diabetes insipidus. Cognitive Level: Comprehension 449 8. Diabetes insipidus, diabetes mellitus (DM), and SIADH share which of the following assessment manifestations? a. Polyuria b. Edema c. Vomiting and abdominal cramping d. Thirst ANS: D All three share thirst as a common clinical manifestation. SIADH does not have polyuria as a clinical manifestation. Insipidus does not have edema as a clinical manifestation. SIADH is manifested by gastrointestinal symptoms, the other two are not. Cognitive Level: Comprehension 449 9. A 50-year-old male patient presents with polyuria and extreme thirst. He was given exogenous ADH. For which of the following conditions would this treatment be effective? a. Neurogenic diabetes insipidus b. Psychogenic diabetes insipidus c. Nephrogenic diabetes insipidus d. SIADH ANS: A Neurogenic diabetes insipidus is caused by the insufficient secretion of ADH; thus, exogenous ADH would be useful in the treatment of this disorder. Psychogenic diabetes insipidus is due to increased intake of water and would not respond to exogenous ADH. ADH is high in nephrogenic diabetes insipidus; thus, exogenous ADH would be contraindicated. SIADH is manifested by high levels of ADH; thus, exogenous administration of ADH would be contraindicated. Cognitive Level: Comprehension 449 10. A 25-year-old male presents with fatigue, constipation, and sexual dysfunction. Tests reveal all pituitary hormones are normal and no masses are present. The nurse suspects the most likely cause of his symptoms is a dysfunction in the: a. Anterior pituitary b. Posterior pituitary c. Pars intermedia d. Pituitary stalk ANS: D When pituitary hormones are normal, dysfunction in the action of hypothalamic hormones are most commonly related to interruption of the connection between the hypothalamus and pituitary, the pituitary stalk. Pituitary hormones are normal so the dysfunction cannot be in the anterior pituitary. Pituitary hormones are normal, so the dysfunction cannot be in the posterior pituitary. Pituitary hormones are normal, so the dysfunction cannot be in the pars intermedia. Cognitive Level: Comprehension 450 11. A 15-year-old female presents with breast discharge, dysmenorrhea, and excessive excitability. Tests reveal that all her pituitary hormones are elevated. What does the nurse suspect as the most likely cause for these assessment findings? a. A pituitary adenoma b. Hypothalamic hyposecretion c. Hypothalamic inflammation d. Pheochromocytoma ANS: A Hormonal effects of pituitary adenomas include hypersecretion from the adenoma, itself, and hyposecretion from surrounding pituitary cells; in this case prolactin would be elevated with the manifestation of menstrual irregularities and secretion from the breast. These symptoms are indicative of hypersecretion, not hyposecretion. These symptoms are indicative of hypersecretion, not hypothalamic inflammation, which would lead to hyposecretion. Pheochromocytoma is a tumor of the adrenal gland and would be manifested by elevated blood pressure. Cognitive Level: Comprehension 450 12. What common neurologic disturbances should the nurse assess for in a patient with a pituitary adenoma? a. Coma b. Visual disturbances c. Confused states d. Breathing abnormalities ANS: B The clinical manifestations of pituitary adenomas are visual changes including visual field impairments (often beginning in one eye and progressing to the other) and temporary blindness. Coma is not associated with pituitary adenoma, visual disturbances are. Confused states are not associated with pituitary adenoma, visual disturbances are. Breathing abnormalities are not associated with pituitary adenoma, visual disturbances are. Cognitive Level: Comprehension 451 13. A 35-year-old female with Graves disease is admitted to a medical-surgical unit. While the nurse is reviewing the lab tests, which results would the nurse expect to find? a. High levels of circulating thyroid-stimulating antibodies b. Ectopic secretion of thyroid-stimulating hormone (TSH) c. Low circulating levels of thyroid hormones d. Increased circulation of iodine ANS: A Graves disease results from a form of Type II hypersensitivity in which there is stimulation of the thyroid by autoantibodies directed against the TSH receptor. The thyroid-stimulating antibodies stimulate TSH receptors; it is not an ectopic secretion. Graves disease is manifested by elevated levels of thyroid hormones. Iodine deficiency leads to goiter, but not Graves disease. REF: pp. 454-455 14. While checking the lab results for a patient with Graves disease, the nurse would check the T3 level to be abnormally: a. Low b. High c. Variable d. Absent ANS: B T3 levels are elevated in Graves disease. T3 levels are elevated in Graves disease. T3 levels are elevated in Graves disease, not variable. T3 levels are elevated in Graves disease, not absent. Cognitive Level: Comprehension 454 15. A 35-year-old female with Graves disease is admitted to a medical-surgical unit. Which of the following symptoms would the nurse expect to find before treatment? a. Weight gain, cold intolerance b. Slow heart rate, rash c. Skin hot and moist, rapid heart rate d. Constipation, confusion ANS: C Symptoms of Graves disease include heat intolerance and increased tissue sensitivity to stimulation by the sympathetic division of the autonomic nervous system. Weight loss, rather than weight gain, and heat intolerance would result. Tachycardia, not slow heart rate, would occur. Diarrhea would occur as opposed to constipation. Cognitive Level: Comprehension 454 16. Visual disturbances are a common occurrence in patients with untreated Graves disease. The endocrinologist explains to the patient that the main cause of these complications is: a. Decreased blood flow to the eye b. Orbital edema and protrusion of the eyeball c. TSH neurotoxicity to retinal cells d. Local lactic acidosis ANS: B Visual disturbances with Graves disease include orbital fat accumulation, inflammation, and edema of the orbital contents resulting in exophthalmos (protrusion of the eyeball), periorbital edema, and extraocular muscle weakness leading to diplopia (double vision). Blood flow to the eye is not an effect, but visual changes occur. Functional abilities of the eye results from hyperactivity of the sympathetic system. Lactic acid is not involved with visual changes in the eye. Cognitive Level: Comprehension 455 17. A 25-year-old female with Graves disease is admitted to a medical-surgical unit. Palpation of her neck would most likely reveal: a. A normal-sized thyroid b. A small discrete thyroid nodule c. Multiple discrete thyroid nodules d. Diffuse thyroid enlargement ANS: D A patient with Graves disease would reveal stimulation of the gland causing diffuse thyroid enlargement. In Graves disease, the thyroid will be enlarged, not normal sized. In Graves disease, the entire gland will be enlarged, not just a small nodule. In Graves disease, the entire gland will be enlarged, not multiple discrete nodules. Cognitive Level: Comprehension 455 18. A 22-year-old female has a low level of TSH. What condition does the nurse expect the patient is experiencing? a. Primary hypothyroidism b. Secondary hypothyroidism c. Autoimmune hypothyroidism d. Atypical hypothyroidism ANS: B Causes of secondary hypothyroidism are related to either pituitary or hypothalamic failure, which would be evident by low levels of TSH. Primary hypothyroidism would be evident by elevated levels of TSH. Autoimmune hypothyroidism would be evident by elevated TSH. Atypical hypothyroidism would be evident by normal or elevated TSH. Cognitive Level: Comprehension 456 19. While planning care for a patient with hypothyroidism, which principle should the nurse remember? The basal metabolic rate is unusually with hypothyroidism. a. High b. Low c. Steady d. Variable ANS: B The metabolic rate with hypothyroidism is low. The metabolic rate with hypothyroidism is low, not high. The metabolic rate with hypothyroidism is low, not steady. The metabolic rate with hypothyroidism is low, not variable. Cognitive Level: Comprehension 456 20. A 3-year-old male was diagnosed with congenital hypothyroidism. The parents ask the nurse if left untreated what will happen. What is the nurses best response? If left untreated, the child would have: a. Mental retardation and stunted growth b. Increased risk of childhood thyroid cancer c. Hyperactivity and attention deficit disorder d. Liver, kidney, and pancreas failure ANS: A Cognitive disability varies with the severity of congenital hypothyroidism and the length of delay before treatment is initiated. Cognitive disability varies with the severity of congenital hypothyroidism and the length of delay before treatment is initiated. There is not an increased risk for thyroid cancer. Cognitive disability varies with the severity of congenital hypothyroidism and the length of delay before treatment is initiated. There is not a risk for hyperactivity and attention deficit disorder. Cognitive disability varies with the severity of congenital hypothyroidism and the length of delay before treatment is initiated. There is not a risk for liver, kidney, and pancreas failure. Cognitive Level: Comprehension 457 21. A 30-year-old male was diagnosed with thyroid carcinoma. The lab tests the nurse would most likely find are T3 and T4 levels. a. High b. Low c. Normal d. Variable ANS: C Most individuals with thyroid carcinoma have normal T3 and T4 levels and are therefore euthyroid. Most individuals with thyroid carcinoma have normal T3 and T4 levels and are therefore euthyroid, not hyperthyroid. Most individuals with thyroid carcinoma have normal T3 and T4 levels and are therefore euthyroid, not hypothyroid. Most individuals with thyroid carcinoma have normal T3 and T4 levels and are therefore euthyroid, not variable in their levels. Cognitive Level: Comprehension 457 22. What problem should the nurse assess for in a patient with chronic hyperparathyroidism? a. Seizure disorders b. Vitamin D malabsorption c. Hyponatremia d. Osteoporosis and pathologic fractures ANS: D Excessive osteoclastic and osteocytic activity resulting in bone resorption may cause pathologic fractures, kyphosis of the dorsal spine, and compression fractures of the vertebral bodies. Pathologic fractures are associated with chronic hyperparathyroidism, not a seizure disorder. Pathologic fractures are associated with chronic hyperparathyroidism, not vitamin D malabsorption. Pathologic fractures are associated with chronic hyperparathyroidism, not hyponatremia. Cognitive Level: Comprehension 457 23. A 45-year-old female with Graves disease underwent surgical removal of her thyroid gland. During the postoperative period, her serum calcium was low. The most probable reason for her low serum calcium is: a. Hyperparathyroidism secondary to Graves disease b. Myxedema secondary to surgery c. Hypoparathyroidism caused by surgical injury to the parathyroid glands d. Hypothyroidism resulting from lack of thyroid replacement ANS: C Hypoparathyroidism is most commonly caused by damage to the parathyroid glands during thyroid surgery. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands during thyroid surgery, not secondary to Graves disease. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands during thyroid surgery, not due to myxedema. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands during thyroid surgery; it does not result from the lack of thyroid replacement. Cognitive Level: Comprehension 458 24. A 30-year-old female with Graves disease is admitted to a hospital unit for the surgical removal of her thyroid gland. During the postoperative period, the nurse notes that the patients serum calcium is low. The nurse should observe the patient for which of the following signs/symptoms? a. Muscle weakness and constipation b. Laryngeal spasms and hyperreflexia c. Abdominal pain and fever d. Anorexia, nausea, and vomiting ANS: B Symptoms of low calcium are associated with tetany, a condition characterized by muscle spasms, hyperreflexia, clonic-tonic convulsions, and laryngeal spasms. Symptoms of low calcium are associated with tetany, a condition characterized by muscle spasms, hyperreflexia, clonic-tonic convulsions, and laryngeal spasms. It does not involve muscle weakness and constipation. Symptoms of low calcium are associated with tetany, a condition characterized by muscle spasms, hyperreflexia, clonic-tonic convulsions, and laryngeal spasms. It does not cause abdominal pain. Symptoms of low calcium are associated with tetany, a condition characterized by muscle spasms, hyperreflexia, clonic-tonic convulsions, and laryngeal spasms. It does not cause anorexia, nausea, or vomiting. Cognitive Level: Comprehension 458 25. When a patient wants to know what most commonly causes hypoparathyroidism, how should the nurse reply? It is most commonly caused by: a. Pituitary hyposecretion b. Parathyroid adenoma c. Parathyroid gland injury d. Hypothalamic inactivity ANS: C Hypoparathyroidism is most commonly caused by damage to the parathyroid glands. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands, not pituitary hyposecretion. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands, not parathyroid adenoma. Hypoparathyroidism is most commonly caused by damage to the parathyroid glands, not inactivity of the hypothalamus. Cognitive Level: Comprehension 458 26. A 25-year-old male presents to his primary care provider reporting changes in facial features. CT scan reveals a mass on the anterior pituitary, and lab tests reveal severely elevated growth hormone (GH). Which of the following would the nurse also expect to find? a. Decreased IGF-1 b. Hypotension c. Sexual dysfunction d. Height increases ANS: C In addition to elevated levels of GH, sexual dysfunction in men can occur. In addition to elevated levels of GH, sexual dysfunction in men can occur, and IGF-1 increases. In addition to elevated levels of GH, sexual dysfunction in men can occur, not hypotension. In addition to elevated levels of GH, sexual dysfunction in men can occur, and overgrowth of bone occurs but not an increase in height. Cognitive Level: Comprehension 452 27. A 30-year-old male presents to his primary care provider reporting visual disturbances. CT reveals a pituitary tumor and lab tests reveal elevated prolactin. He is diagnosed with prolactinoma. Which of the following treatments would the nurse help implement? Administering: a. Dopaminergic agonists b. Calcium c. Insulin d. Radiation ANS: A Dopaminergic agonists (bromocriptine and cabergoline) are the treatment of choice for prolactinomas. Calcium is used to treat parathyroid disease. Insulin is used to treat diabetes. Radiation is used to treat GH. Cognitive Level: Comprehension 453 28. A 12-year-old female is newly diagnosed with type 1 DM. When the parents ask what causes this, what is the nurses best response? a. A familial, autosomal dominant gene defect b. Obesity and lack of exercise c. Immune destruction of the pancreas d. Hyperglycemia from eating too many sweets ANS: C The most common cause of type 1 DM is a slowly progressive autoimmune T cell-mediated disease that destroys the beta cells of the pancreas. The most common cause of type 1 DM is a slowly progressive autoimmune T cell-mediated disease that destroys the beta cells of the pancreas; it is not due to a gene defect. Although obesity can contribute to diabetes, the most common cause of type 1 DM is a slowly progressive autoimmune T cell-mediated disease that destroys the beta cells of the pancreas. Eating too many sweets does not contribute to the development of diabetes; the most common cause of type 1 DM is a slowly progressive autoimmune T cell-mediated disease that destroys the beta cells of the pancreas. Cognitive Level: Comprehension 459 29. A 12-year-old male is newly diagnosed with type 1 DM. Which of the following tests should the nurse prepare the patient to best confirm the diagnosis? a. Fasting plasma glucose levels b. Random serum glucose levels c. Genetic testing d. Glycosylated hemoglobin measurements ANS: A Fasting blood glucose levels are most beneficial in confirming the diagnosis of diabetes. Random serum levels are not as accurate as fasting. Genetic testing may be important for future determination, but it does not confirm the diagnosis. Glycosylated testing measures glucose control over time. Cognitive Level: Comprehension 18 | p. 435 | p. 462 30. An 11-year-old male is newly diagnosed with type 1 DM. Which classic symptoms should the nurse assess the patient for? a. Recurrent infections, visual changes, fatigue, and paresthesias b. Polydipsia, polyuria, polyphagia, and weight loss c. Vomiting; abdominal pain; sweet, fruity breath; dehydration; and Kussmaul breathing d. Weakness, vomiting, hypotension, and mental confusion ANS: B Classic symptoms of type 1 DM include polydipsia, polyuria, polyphagia, and weight loss. Recurrent infections and visual changes are complications of diabetes. Vomiting, abdominal pain, and sweet breath are signs of diabetic ketoacidosis. Weakness, hypotension, and mental confusion are signs of hypoglycemia. Cognitive Level: Comprehension 461 31. A 19-year-old female with type 1 DM was admitted to the hospital with altered consciousness and the following lab values: serum glucose 500 mg/dl (high) and serum K+ 2 (low). Her parents state that she has been sick with the flu for a week. The diagnosis is hyperosmolar hyperglycemia nonketotic syndrome (HHNKS). What relationship do these values have with her insulin deficiency? a. Increased glucose utilization causes the shift of fluid from the intravascular to the intracellular space. b. Decreased insulin causes hyperglycemia and osmotic diuresis. c. Increased glucose and fatty acid metabolism stimulates renal diuresis and electrolyte loss. d. Increased insulin use results in protein catabolism, tissue wasting, and electrolyte loss. ANS: B Because the amount of insulin required to inhibit fat breakdown is less than that needed for effective glucose transport, insulin levels are sufficient to prevent excessive lipolysis and ketosis. Volume is depleted, not increased. Electrolyte loss does occur, but it is not due to fatty acids and glucose metabolism, it is due to insufficient insulin. Insulin is decreased, not increased. Cognitive Level: Comprehension 465 32. A nurse is reviewing lab results for glycosylated hemoglobin (hemoglobin A1c) levels. A nurse recalls the purpose of this test is to: a. Measure fasting glucose levels. b. Monitor long-term serum glucose control. c. Detect acute complications of diabetes. d. Check for hyperlipidemia. ANS: B Glycosylated hemoglobin refers to the permanent attachment of glucose to hemoglobin molecules and reflects the average plasma glucose exposure over the life of a red blood cell (approximately 120 days). Glycosylated hemoglobin does not measure fasting, but glucose control over time. Glycosylated hemoglobin does not identify complications, but could provide data if the patient is at risk. Glycosylated does not check for hyperlipidemia. Cognitive Level: Comprehension 459 33. When a patient asks what causes hyperglycemia in type 2 DM, how should the nurse respond? Hyperglycemia is a result of: a. Insulin deficiency b. Hyperinsulinemia c. Glucagon deficiency d. Liver dysfunction ANS: B Type 2 diabetes is due to hyperinsulinemia and insulin resistance. Type 1 is due to insulin deficiency; type 2 is due to insulin resistance. Type 2 diabetes is due to hyperinsulinemia and insulin resistance, not glucagon deficiency. Type 2 diabetes is due to hyperinsulinemia, not liver dysfunction. Cognitive Level: Comprehension 462 34. A 19-year-old female with type 1 DM was admitted to the hospital with the following lab values: serum glucose 500 mg/dl (high), urine glucose and ketones 4+ (high), and arterial pH 7.20 (low). Her parents state that she has been sick with the flu for a week. Which of the following statements best explains her acidotic state? a. Increased insulin levels promote protein breakdown and ketone formation. b. Her uncontrolled diabetes has led to renal failure. c. Low serum insulin promotes lipid storage and a corresponding release of ketones. d. Insulin deficiency promotes lipid metabolism and ketone formation. ANS: D With insulin deficiency, lipolysis is enhanced, and there is an increase in the amount of nonesterified fatty acids delivered to the liver. The consequence is increased glyconeogenesis contributing to hyperglycemia and production of ketone bodies (acetoacetate, hydroxybutyrate, and acetone) by the mitochondria of the liver at a rate that exceeds peripheral use. Insulin is deficient, not increased. The patient is in acidosis, not renal failure. Insulin is low, but the ketones are the result of fatty acid breakdown due to lack of insulin, not because of lipid storage. Cognitive Level: Comprehension 465 35. A 13-year-old male who uses insulin to control his type 1 diabetes experiences hunger, lightheadedness, tachycardia, pallor, headache, and confusion during gym class. The most probable cause of these symptoms is: a. Hyperglycemia resulting from incorrect insulin administration b. Dawn phenomenon caused by eating a snack before gym class c. Hypoglycemia caused by increased exercise d. Somogyi effect caused by insulin sensitivity ANS: C The boy is experiencing hypoglycemia due to increased glucose utilization with exercise. The boy is experiencing hypoglycemia, not hyperglycemia. The boy is experiencing hypoglycemia, not dawn phenomenon, which occurs as an early morning rise in blood glucose concentration with no hypoglycemia during the night. The Somogyi effect is a combination of hypoglycemia with rebound hyperglycemia. Cognitive Level: Comprehension 465 36. A 55-year-old female is admitted to the medical unit for complications of long-term, poorly controlled type 2 DM. Which of the following would the nurse expect to find in addition to elevated glucose? a. Atherosclerosis b. Metabolic alkalosis c. Elevated liver enzymes d. Anemia ANS: A Macrovascular disease (lesions in large and medium sized arteries) increases morbidity and mortality and increases risk for accelerated atherosclerosis. Acidosis, rather than alkalosis, would occur in this patient. Elevated enzymes do not occur, but atherosclerosis does. Anemia would not be expected, but atherosclerosis is. Cognitive Level: Comprehension 468 37. When a staff member asks the nurse what causes the chronic complications of DM such as microvascular and macrovascular disease, how should the nurse respond? These complications are primarily related to: a. Pancreatic changes b. Hyperglycemia c. Ketone toxicity d. Hyperinsulinemia ANS: B The underlying cause of the micro and macro diseases associated with diabetes is due to hyperglycemia. The underlying cause of the micro and macro diseases is related to hyperglycemia, not pancreatic changes. The underlying cause of the micro and macro diseases is related to hyperglycemia, not ketone toxicity. The underlying cause of the micro and macro diseases is related to hyperglycemia, not hyperinsulinemia. Cognitive Level: Comprehension 465 38. A nurse checks lab results as both Cushing syndrome and Addison disease can manifest with elevated levels of: a. ADH b. Cortisol c. Adrenocorticotropic hormone (ACTH) d. Aldosterone ANS: C Cushing syndrome and Addison are related to elevated levels of ACTH. Cushing syndrome and Addison are related to elevated levels of ACTH, not ADH. Cushing syndrome and Addison are related to elevated levels of ACTH, not cortisol. Cushing syndrome and Addison are related to elevated levels of ACTH, not aldosterone. Cognitive Level: Comprehension 469 39. Which of the following alterations would the nurse expect to find in a patient with untreated Cushing disease or syndrome? a. Bradycardia b. Tachypnea c. Hyperkalemia d. Hypertension ANS: D With elevated cortisol levels, vascular sensitivity to catecholamines increases significantly, leading to vasoconstriction and hypertension. Tachycardia is more likely than bradycardia due to increased sensitivity to catecholamines. Tachypnea does not occur; the patient experiences hypertension. Hyokalemia, not hyperkalemia, occurs. Cognitive Level: Comprehension 470 40. When a nurse is assessing the physical features of individuals with Cushing syndrome, these findings will include: a. Weight loss and muscle wasting b. Truncal obesity and moon face c. Pallor and swollen tongue d. Depigmented skin and eyelid lag ANS: B Weight gain is the most common feature and results from the accumulation of adipose tissue in the trunk, facial, and cervical areas. These characteristic patterns of fat deposition have been described as truncal obesity, moon face, and buffalo hump. Weight gain, not loss, is the most common feature of Cushing syndrome. Pallor is not associated with Cushing syndrome. The skin of the patient with Cushing syndrome is bronze in color. Cognitive Level: Comprehension 469 41. A 35-year-old female took corticosteroid therapy for several months. Which of the following would the nurse expect to find? a. Renal toxicity b. Episodes of hypoglycemia c. Hypotension d. Type 2 DM ANS: D Overt DM develops in approximately 20% of individuals with hypercortisolism. Diabetes develops, not renal toxicity. Hypoglycemia does not occur; hyperglycemia does. Hypertension, not hypotension, occurs; hypotension occurs with Addison. Cognitive Level: Comprehension 470 42. A nurse is preparing to teach a patient about Addison disease. Which information should the nurse include? The most common cause of Addison disease is: a. An autoimmune reaction b. Dietary deficiency of sodium and potassium c. Cancer d. Viral infection of the pituitary gland ANS: A Addison disease is caused by autoimmune mechanisms that destroy adrenal cortical cells and is more common in women. Chapter 21. Obesity and Disorders of Nutrition 1. The adipocytes in adipose tissue not only serve as a storage sites, they also: A) produce linoleic fatty acid. B) synthesize triglycerides. C) increase glucagon release. D) degrade fat-soluble vitamins. 2. Protein contains nitrogen. A negative nitrogen balance represents: A) more protein consumed than excreted. B) a reduced need for nitrogen as protein. C) more nitrogen excreted than consumed. D) less use of nitrogen for protein synthesis. 3. Natural appetite suppression mechanisms, necessary for food intake control, include : A) ketoacid deficiency. B) cholecystokinin storage. C) decreased blood glucose. D) leptin receptor stimulation. 4. Body weight should be used in combination with other measurements to establish if a person is underweight or overweight. Obesity is indicated by: A) female body fat of 20% and 30%. B) body mass index (BMI) of 30 to 40. C) relative body weight of 70% to 100%. D) abdominal fat/ hip ratio of 0.8 to 1.0. 5. A patient with upper body obesity also has central fat distribution. This body fat configuration places the patient at greater risk for than a patient with lower body obesity. A) osteoporosis B) renal disease C) cardiometabolic disorders D) chronic anemia 6. As the problem of childhood and adolescent obesity increases, an increase in the incidence of is occurring in this obese population. A) type 2 diabetes mellitus B) attention deficit disorder C) juvenile rheumatoid arthritis D) antibiotic-resistant bacterial infections 7. A diet deficient in calories and protein causes marasmus, which is characterized by: A) discolored hair. B) bradycardia. C) enlarged liver. D) pitting edema. 8. Protein-calorie malnutrition with loss of lean tissues and muscle mass results in: A) respiratory muscle stimulation. B) excessive blood cell production. C) diarrhea. D) increased cardiac contractility. 9. Similarities between girls or women with anorexia nervosa and bulimia nervosa include: A) periodontal disease. B) low estrogen level. C) electrolyte imbalances. D) enlarged parotid gland. 10. Both binge-eating and bulimia nervosa patients consume excessive amounts of foods secretively. A major difference is that binge-eaters: A) remain overweight. B) eat when not hungry. C) are substance abusers. D) experience depression. 11. A large, high-calorie meal has resulted in the intake of far more energy than a person requires. What will the individuals body do with the excess carbohydrates provided by this meal? A) Convert them into glucose and store them in the liver and muscles B) Excrete most of the excess polysaccharides through the kidneys C) Convert the carbohydrates into amino acids in preparation for long-term storage D) Create structural proteins from some of the carbohydrates and store the remainder as triglycerides 12. Which of the following patients is most likely to be in positive nitrogen balance? A) A patient who is receiving treatment for sepsis B) A patient whose diagnosis of pneumonia is causing a fever C) A woman who has been admitted to the hospital in early labor D) A patient who sustained extensive burns in a recent industrial accident 13. In addition to facilitating bowel movements, a diet that is high in fiber confers which of the following benefits? A) Lowering cholesterol and blood glucose B) Removing toxins and metabolic byproducts C) Lowering blood pressure and resting heart rate D) Increasing intestinal absorption of vitamins and minerals 14. Which of the following statements best conveys the endocrine function of adipose tissue? A) Adipose tissue antagonizes the effects of insulin on cell membranes. B) Adipose tissue produces ghrelin, which stimulates both appetite and eating. C) Adipose tissue produces and secretes cholecystokinin (CCK), which stimulates the hypothalamic feeding center. D) Adipose tissue produces leptin, which mediates body weight. 15. Chronic inflammation as a result of excess adipose tissue is implicated in the etiology of which of the following health problems? A) Osteoporosis B) Type 2 diabetes C) Rheumatoid arthritis D) Systemic lupus erythematosus (SLE) 16. A public health nurse has noted a significant increase in the number of school-aged children who are obese. Which of the following factors is most significant predictor of childhood obesity? A) Low socioeconomic status B) Low self-esteem C) Having obese parents D) Living in a rural or inner-city neighborhood 17. Which of the following measures should a school nurse prioritize in the treatment and prevention of childhood obesity? A) Group cognitive therapy B) Use of selective serotonin-reuptake inhibitors (SSRIs) C) Education on exercise and nutrition D) High-protein, low-carbohydrate diet 18. Which of the following characteristics distinguishes kwashiorkor from marasmus? A) Impairment of immune function B) Lack of dietary fat intake C) High intake of carbohydrates D) Impaired pigment synthesis 19. A frail, 87-year-old female patient has been admitted to a hospital after a fall and has been diagnosed with failure to thrive. Which of the following laboratory values would suggest that the patient may be experiencing malnutrition? A) Low prealbumin B) High C-reactive protein C) High bilirubin D) Low fasting blood sugar 20. Which of the following assessments should be prioritized in the care of a patient with anorexia nervosa? A) Serum electrolyte levels B) Chest auscultation C) White blood cell count with differential D) Blood pressure monitoring Answer Key 1. B 2. C 3. D 4. B 5. C 6. A 7. B 8. C 9. C 10. A 11. A 12. C 13. A 14. D 15. B 16. C 17. C 18. C 19. A 20. D Chapter 22. Structure and Function of the Hematologic System MULTIPLE CHOICE 1. A primary care provider is talking about plasma proteins synthesized by lymphocytes in the lymph nodes. What is the primary care provider describing? a. Antibodies b. Albumins c. Clotting factors d. Complement proteins ANS: A Antibodies are produced by plasma cells in the lymph nodes and other lymphoid tissues. Albumins are specific types of plasma proteins. Clotting factors describe a function of plasma proteins. Complement proteins are a type of plasma proteins. Cognitive Level: Comprehension 480 2. While reviewing lab results, the nurse recalls the most abundant cells in the blood are: a. Leukocytes b. Lymphocytes c. Erythrocytes d. Thrombocytes ANS: C Erythrocytes (red blood cells) are the most abundant cells of the blood, occupying approximately 48% of the blood. Erythrocytes, not leukocytes, are the most abundant cells in the blood. Erythrocytes, not lymphocytes, are the most abundant cells in the blood. Erythrocytes, not thrombocytes, are the most abundant cells in the blood. Cognitive Level: Comprehension 480 3. An adult patients blood sample is analyzed in a laboratory. Assuming a normal sample, which type of white blood cell accounts for the highest percentage? a. Neutrophils b. Eosinophils c. Basophils d. Lymphocytes ANS: A Neutrophils constitute about 55% of the total leukocyte count in adults. The eosinophils, which have large, coarse granules, constitute only 1% to 4% of the normal leukocyte count in adults. Basophils make up less than 1% of the leukocytes. Lymphocytes constitute approximately 36% of the total leukocyte count. Cognitive Level: Comprehension 480 4. A group of cells isolated in the laboratory have membrane-bound granules in their cytoplasm and they show phagocytic activity. Which of the following cells is most similar? a. Monocyte b. Macrophage c. Lymphocyte d. Eosinophils ANS: D Eosinophils, which have large, coarse granules, are capable of ameboid movement and phagocytosis. Monocytes help fight infection. Macrophages are mature monocytes. Lymphocytes are the primary cells of the immune response. Cognitive Level: Comprehension 480 5. While planning care for a patient with inflammation, which principle will the nurse remember? The predominant phagocyte of early inflammation is the: a. Eosinophil b. Lymphocyte c. Macrophage d. Neutrophil ANS: D Neutrophils are the chief phagocytes of early inflammation. Eosinophils ingest antigen-antibody complexes and are induced by IgE-mediated hypersensitivity reactions to attack parasites. Most lymphocytes transiently circulate in the blood and eventually reside in lymphoid tissues as mature T cells, B cells, or plasma cells. Macrophages migrate out of the vessels in response to infection or inflammation, but are not the early responders. Cognitive Level: Comprehension 480 6. A patient has researched white blood cells on the Internet. Which statement indicates the patient has a good understanding? contain preformed granules of vasoactive amines. a. Neutrophils b. Eosinophils c. Monocytes d. Basophils ANS: D Basophils have cytoplasmic granules that contain vasoactive amines (e.g., histamine) and an anticoagulant (heparin). Their function is similar to tissue mast cells. Neutrophils are the chief phagocytes of early inflammation. Eosinophils ingest antigen-antibody complexes and are induced by IgE-mediated hypersensitivity reactions to attack parasites. Monocytes do not have amines, and their job it to help fight infection. Cognitive Level: Comprehension 480 7. A nurse recalls that monocytes are blood cells that mature (differentiate) into: a. Macrophages b. Neutrophils c. Eosinophils d. Mast cells ANS: A Macrophages are mature monocytes. Monocytes mature into macrophages, not neutrophils. Monocytes mature into macrophages, not eosinophils. Monocytes mature into macrophages, not mast cells. Cognitive Level: Comprehension 481 8. A nurse is teaching the staff about platelets. Which information should the nurse include? In addition to playing a role in hemostasis, platelets have the ability to: a. Stimulate bone marrow production of erythrocytes b. Release biochemical mediators of inflammation c. Undergo cell division in response to bleeding d. Activate a humoral response ANS: B Platelets contain cytoplasmic granules capable of releasing proinflammatory biochemical mediators when stimulated by injury to a blood vessel. Platelets assist with inflammation; they do not produce erythrocytes. Platelets assist with inflammation; they do not undergo cell division in response to bleeding. Platelets assist with inflammation; they do not activate the humoral response. Cognitive Level: Comprehension 481 9. While planning care for a newborn, the pediatric nurse recalls the main site of hematopoiesis in the fetus is the: a. Bone marrow b. Liver c. Lymph nodes d. Spleen ANS: D The spleen is the largest of the lymphoid organs and is the site of fetal hematopoiesis. The spleen, not the bone marrow, is the site of fetal hematopoiesis. The spleen, not the liver, is the site of fetal hematopoiesis. The spleen, not the lymph nodes, is the site of fetal hematopoiesis. Cognitive Level: Comprehension 482 10. A 45-year-old female undergoes a splenectomy to remove a tumor. Which of the following assessment finding is most likely to occur following surgery? a. Leukocytosis b. Hypoglycemia c. Decreased red blood cell count d. Decreased platelets ANS: A Leukocytosis often occurs after splenectomy. Elevated levels of leukocytes, not hypoglycemia, occur after splenectomy. Elevated levels of leukocytes, not decreased levels of red blood cells, occur after splenectomy. Elevated levels of leukocytes, not decreased platelets, occur after splenectomy. Cognitive Level: Comprehension 482 11. During an infection, the nurse assesses the lymph nodes. Lymph nodes enlarge and become tender because: a. Lymphocytes are rapidly dividing. b. Edema accumulates within the fibrous capsule. c. Microorganisms are accumulating. d. The nodes are not functioning properly. ANS: A During an infection, the rate of proliferation of lymphocytes within the nodes is so great that the nodes enlarge and become tender. Edema may be present, but the tenderness is due to proliferation of lymphocytes. The tenderness is not due to the microorganisms, but to the proliferation of lymphocytes. The tenderness is due to the normal function of the gland in response to the proliferation of lymphocytes. Cognitive Level: Comprehension 482 12. After birth, red blood cells are normally made only in the: a. Liver b. Spleen c. Bone marrow d. Kidney ANS: C Red blood cells are produced in the bone marrow. Red blood cells are produced in the bone marrow, not the liver. Red blood cells are produced in the bone marrow, not the spleen. Red blood bells are produced in the bone marrow, not the kidney. Cognitive Level: Comprehension 485 13. A nurse is discussing a cell that can differentiate into any tissue type. Which term is the nurse describing? a. Hematopoietic b. Pluripotent c. Blastocyst d. Progenitor ANS: B A pluripotent cell can grow into different kinds of tissue: blood, nerves, heart, bone, and so forth. A pluripotent cell, not a hematopoietic cell, can grow into different kinds of tissue: blood, nerves, heart, bone, and so forth. A pluripotent cell can grow into different kinds of tissue: blood, nerves, heart, bone, and so forth. A blastocyst is an embryonic cell. A pluripotent cell can grow into different kinds of tissue: blood, nerves, heart, bone, and so forth. A progenitor becomes a hematologic cell. Cognitive Level: Comprehension 485 14. A hematologist is discussing hematopoiesis. Which information should be included? participate in hematopoiesis. a. Colony-stimulating factors (CSFs) b. Eosinophils c. Basophils d. Neutrophils ANS: A Several cytokines participate in hematopoiesis, particularly CSFs (or hematopoietic growth factors). Several cytokines participate in hematopoiesis, particularly CSFs (or hematopoietic growth factors); eosinophils do not play a role in hematopoiesis. Several cytokines participate in hematopoiesis, particularly CSFs (or hematopoietic growth factors); basophils do not play a role in hematopoiesis. Several cytokines participate in hematopoiesis, particularly CSFs (or hematopoietic growth factors); neutrophils do not play a role in hematopoiesis. Cognitive Level: Comprehension 485 15. An unstable type of hemoglobin that cannot bind with oxygen is termed: a. Deoxyhemoglobin b. Oxyhemoglobin c. Methemoglobin d. Glycosylated hemoglobin ANS: C Without reactivation, the Fe3+-containing hemoglobin (methemoglobin) cannot bind oxygen. Deoxyhemoglobin is reactivated hemoglobin whose oxygen has been released. Binding of oxygen to ferrous iron temporally oxidizes Fe2+ to Fe3+ as in oxyhemoglobin. Glycosylated hemoglobin is glucose bound to hemoglobin. Cognitive Level: Comprehension 487 16. A staff member wants to know where the greatest proportion of iron is located. How should the nurse respond? The greatest proportion of total body iron is located in the: a. Erythrocytes b. Spleen pulp c. Bone marrow d. Liver tissue ANS: A Approximately 67% of total body iron is bound to heme in erythrocytes (hemoglobin) and muscle cells (myoglobin). Approximately 67% of total body iron is bound to heme in erythrocytes (hemoglobin) and muscle cells (myoglobin), not the spleen pulp. Approximately 67% of total body iron is bound to heme in erythrocytes (hemoglobin) and muscle cells (myoglobin), not the bone marrow. Approximately 67% of total body iron is bound to heme in erythrocytes (hemoglobin) and muscle cells (myoglobin), not the liver tissue. Cognitive Level: Comprehension 487 17. A student asks the instructor about recycled iron. What information should the instructor share? Recycled iron from macrophages is delivered to the bone marrow bound to: a. Ferritin b. Hemoglobin c. Hemosiderin d. Transferrin ANS: D Iron is transported in the blood bound to transferrin. Iron is transported in the blood bound to transferrin, ferritin is the storage form of iron. Iron is transported in the blood bound to transferrin, hemoglobin carries oxygen. Iron is transported in the blood bound to transferrin, hemosiderin is also a storage form of iron. Cognitive Level: Comprehension 488 18. A nurse is preparing to teach about erythropoietin. Which information should the nurse include? Erythropoietin is produced in the: a. Liver b. Bone marrow c. Kidneys d. Spleen ANS: C Erythropoietin is produced in the kidneys. Erythropoietin is produced in the kidneys, not the liver. Erythropoietin is produced in the kidneys, not the bone marrow. Erythropoietin is produced in the kidneys, not the spleen. Cognitive Level: Comprehension 486 19. Which condition will cause a patient to secrete erythropoietin? a. Low blood pressure b. Hypercarbia c. Inflammation d. Hypoxia ANS: D Hypoxia stimulates production of erythropoietin. Hypoxia, not low blood pressure, stimulates production of erythropoietin. Hypoxia, not hypercarbia, stimulates production of erythropoietin. Hypoxia, not inflammation, stimulates production of erythropoietin. Cognitive Level: Comprehension 486 20. After erythrocytes have circulated for about 120 days, they are removed by macrophages, which are mainly in the: a. Liver b. Spleen c. Appendix d. Bone marrow ANS: B Aged or damaged erythrocytes are removed from the bloodstream by macrophages of the MPS chiefly in the spleen. Aged or damaged erythrocytes are removed from the bloodstream by macrophages of the MPS chiefly in the spleen, not the liver. Aged or damaged erythrocytes are removed from the bloodstream by macrophages of the MPS chiefly in the spleen, not the appendix. Aged or damaged erythrocytes are removed from the bloodstream by macrophages of the MPS chiefly in the spleen, not the bone marrow. Cognitive Level: Comprehension 482 21. Which electrolyte will the nurse check to ensure normal platelet functioning? a. Sodium b. Potassium c. Magnesium d. Calcium ANS: D Calcium is necessary for many of the intracellular signaling mechanisms that control platelet activation. Calcium, not sodium, is necessary for many of the intracellular signaling mechanisms that control platelet activation. Calcium, not potassium, is necessary for many of the intracellular signaling mechanisms that control platelet activation. Calcium, not magnesium, is necessary for many of the intracellular signaling mechanisms that control platelet activation. Cognitive Level: Comprehension 491 22. Which of the following nutritional components will the nurse encourage a patient to consume as it is needed for erythropoiesis? a. Cobalamin b. Vitamin B1 c. Vitamin D d. Zinc ANS: A Cobalamin is necessary for erythropoiesis. Cobalamin or vitamin B12 is necessary for erythropoiesis, not B1. Cobalamin is necessary for erythropoiesis, not vitamin D. Cobalamin is necessary for erythropoiesis, not zinc. Cognitive Level: Comprehension 487 23. A newborn baby is diagnosed with a blood disorder in which her platelet count is low. Which of the following does the nurse suspect could be the reason? a. Increased megakaryocytes b. Increased platelet cell division c. Decreased thrombopoietin d. Decreased spleen function ANS: C Thrombopoietin (TPO), a hormone growth factor, is the main regulator of the circulating platelet mass, thus, a deficiency of TPO can lead to decreased platelets. TPO is the factor necessary for platelet production; megakaryocytes are platelet precursors, so if they are elevated, the platelets would be as well. Increased cell division would lead to increased platelets. Platelets are produced in the bone marrow, not the spleen. REF: pp. 481-482 24. A nurse is caring for a patient who cannot clot. Which end product of the clotting cascade is this patient unable to make? a. Collagen b. Fibrinogen c. Thrombin d. Fibrin ANS: D Fibrin is the end product of the coagulation cascade. Fibrin, not collagen, is the end product of the coagulation cascade. Fibrin, not fibrinogen, is the end product of the coagulation cascade. Fibrin, not thrombin, is the end product of the coagulation cascade. Cognitive Level: Comprehension 491 25. A nurse is discussing fibrinolysis. Which information should the nurse share? Fibrinolysis is mediated by: a. Heparin b. Fibrinogen c. Plasmin d. Albumin ANS: C Plasmin is an enzyme that promotes fibrinolysis by degrading fibrin and fibrinogen into fibrin degradation products. Plasmin mediates fibrinolysis, not heparin. Plasmin mediates fibrinolysis, not fibrinogen. Plasmin mediates fibrinolysis, not albumin. Cognitive Level: Comprehension 496 26. A newborn baby has a clotting disorder that results in her body being unable to produce thrombin. Which of the following phases of platelet degranulation would be impossible? a. Subendothelial exposure b. Adhesion c. Activation d. Aggregation ANS: D Without thrombin, aggregation cannot occur. Without thrombin, aggregation, not subendothelial exposure, cannot occur. Without thrombin, aggregation, not adhesion, cannot occur. Without thrombin, aggregation, not activation, cannot occur. REF: pp. 491-492 27. While checking lab results, the nurse remembers the normal leukocyte count is: a. 1,000-2,000/mm3 b. 5,000-10,000/mm3 c. 4.2-6.2 million/mm3 d. 1.2-2.2 million/mm3 ANS: B 5,000-10,000/mm3 is the normal leukocyte count. 1,000-2,000/mm3 is an abnormally low leukocyte count. 4.2-6.2 million/mm3 is the normal erythrocyte count. 1.2-2.2 million/mm3 would indicate anemia. Cognitive Level: Comprehension 479 MULTIPLE RESPONSE 1. When a staff member asks how erythrocytes can carry oxygen, which of the following properties should the nurse describe that allow erythrocytes to function as gas carriers? (Select all that apply.) a. Biconcavity b. Reversible deformability c. Undergoes mitotic division d. Presence of many mitochondria e. Presence of a nucleus ANS: A, B Erythrocytes are small disks that are biconcave in shape and have the capacity to be reversibly deformed. They cannot undergo mitotic division and do not have many mitochondria. Erythrocytes do not have a nucleus. Cognitive Level: Comprehension 480 2. A nurse is caring for an elderly patient. Which of the following are true regarding the hematological system and aging? (Select all that apply.) a. Total serum iron is decreased. b. Total iron-binding capacity is decreased. c. Intestinal iron absorption is decreased. d. Lymphocyte function is unchanged. e. Platelet aggregation is unchanged. ANS: A, B, C Total serum iron, total iron-binding capacity, and intestinal iron absorption are all decreased somewhat in elderly persons. Lymphocyte function decreases with age. Platelet adhesiveness probably increases. Chapter 23. Alterations of Hematologic Function MULTIPLE CHOICE 1. A patients anemia is described as having erythrocytes that demonstrate anisocytosis. The nurse would recognize the erythrocytes would be: a. Pale in color b. Present in various sizes c. Able to assume various shapes d. Live only a few days ANS: C Anisocytosis means the erythrocytes are able to assume various shapes. Anisocytosis means the erythrocytes are able to assume various shapes; it does not refer to color. Anisocytosis means the erythrocytes are able to assume various shapes; it does not refer to size. Anisocytosis means the erythrocytes are able to assume various shapes; it does not refer to life span. Cognitive Level: Comprehension 501 2. A newborn is diagnosed with congenital intrinsic factor deficiency. Which of the following types of anemia will the nurse see documented on the chart? a. Iron deficiency anemia b. Pernicious anemia c. Sideroblastic anemia d. Hemolytic anemia ANS: B A lack of the intrinsic factor leads to pernicious anemia. Iron deficiency anemia is not related to the intrinsic factor. Pernicious anemia is due to the lack of the intrinsic factor, sideroblastic anemia is not related to the intrinsic factor. Hemolytic anemia results from destruction of cells; pernicious is related to the lack of the intrinsic factor. Cognitive Level: Comprehension 502 3. When a nurse is reviewing lab results and notices that the erythrocytes contain an abnormally low concentration of hemoglobin, the nurse calls these erythrocytes: a. Hyperchromic b. Hypochromic c. Macrocytic d. Microcytic ANS: B Hypochromic erythrocytes have low concentrations of hemoglobin. Hyperchromic erythrocytes have high concentrations of hemoglobin. Macrocytic refers to larger cell size, not hemoglobin concentration. Microcytic refers to small cell size, not hemoglobin concentration. Cognitive Level: Comprehension 501 4. A 5-year-old male was diagnosed with normocytic-normochromic anemia. Which of the following anemias does the nurse suspect the patient has? a. Sideroblastic anemia b. Hemolytic anemia c. Pernicious anemia d. Iron deficiency anemia ANS: B Hemolytic anemia is an example of normocytic-normochromic anemia. Sideroblastic anemia is an example of microcytic hypochromic anemia. Pernicious anemia is an example of a macrocytic anemia. Iron deficiency anemia is an example of microcytic hypochromic anemia. Cognitive Level: Comprehension 501 5. After initial compensation, what hemodynamic change should the nurse monitor for in a patient who has a reduction in the number of circulating erythrocytes? a. Increased viscosity of blood b. Decreased cardiac output c. Altered coagulation d. Hyperdynamic circulatory state ANS: D After initial compensation, the blood flows faster and more turbulently than normal blood, causing a hyperdynamic circulatory state. Blood viscosity decreases rather than increases. Cardiac output increases. Alteration in coagulation does not occur. Cognitive Level: Comprehension 501 6. A 25-year-old female has a heavy menses during which she loses a profuse amount of blood. Which of the following adaptations should the nurse expect? a. Movement of fluid into the cell b. Decreased cardiac output c. Decreased oxygen release from hemoglobin d. Peripheral vasoconstriction ANS: D When the anemia is severe or acute in onset (e.g., hemorrhage), the initial compensatory mechanism is peripheral blood vessel constriction, diverting blood flow to essential vital organs. Fluid moves into the vascular space, not the cell. Blood volume increases; thus, cardiac output increases. There is an increase in hemoglobin release of oxygen. Cognitive Level: Comprehension 501 7. A 60-year-old female emphysema patient experiences a rapid and pounding heart, dizziness, and fatigue with exertion. Which of the following respiratory assessment findings indicate the respiratory system is compensating for the increased oxygen demand? a. Bronchoconstriction b. Increased rate and depth of breathing c. Dyspnea d. Activation of the renin-angiotensin response ANS: B The rate and depth of breathing increase in an effort to increase oxygen availability accompanied by an increase in the release of oxygen from hemoglobin. Bronchodilation occurs, not constriction. Dyspnea is not a compensatory mechanism but a side effect of the bodys attempt to increase oxygen. The respiratory system does not activate the renin-angiotensin response; the kidneys are involved. Cognitive Level: Comprehension 501 8. A 2-year-old malnourished child has vitamin B12 and folate deficiencies. A blood smear suggests the deficiency is macrocytic and normochromic. The nurse would expect the hemoglobin to be: a. Normal b. Sporadic c. Low d. High ANS: A The macrocytic (megaloblastic) anemias are characterized by unusually large stem cells (megaloblasts) in the marrow that mature into erythrocytes that are unusually large in size (macrocytic), thickness, and volume. The hemoglobin content is normal, thus allowing them to be classified as normochromic. The hemoglobin content is normal, not sporadic. The hemoglobin content is normal, not low. The hemoglobin content is normal, not high. Cognitive Level: Comprehension 501 9. A 45-year-old male is diagnosed with macrocytic, normochromic anemia. The nurse suspects the most likely cause of this condition is: a. Defective DNA synthesis b. Abnormal synthesis of hemoglobin c. Defective use of vitamin C d. Blocked protein synthesis ANS: A These anemias are the result of ineffective erythrocyte deoxyribonucleic acid (DNA) synthesis. These anemias are the result of ineffective erythrocyte DNA synthesis; hemoglobin is normal. These anemias are the result of ineffective erythrocyte DNA synthesis; it is not related to use of vitamin C. These anemias are the result of ineffective erythrocyte DNA synthesis; it is not due to blocked protein synthesis. Cognitive Level: Comprehension 501 10. When a patient wants to know why vitamin B12 and folate deficiencies cause anemia, how should the nurse respond? a. Red blood cells are unable to differentiate into erythrocytes. b. Red blood cells have malformed hemoglobin molecules. c. Red blood cells have decreased O2-carrying capacity. d. Red blood cells have a shorter life span. ANS: D These deficiencies lead to defective erythrocytes that die prematurely, which decreases their numbers in the circulation, causing anemia. These deficiencies lead to defective erythrocytes that die prematurely, which decreases their numbers in the circulation, causing anemia. It is not due to a lack of differentiation. These deficiencies lead to defective erythrocytes that die prematurely, which decreases their numbers in the circulation, causing anemia. It is not due to malformed hemoglobin. These deficiencies lead to defective erythrocytes that die prematurely, which decreases their numbers in the circulation, causing anemia. It is not due to decreased oxygen carrying capacity. Cognitive Level: Comprehension 506 11. A 20-year-old female undergoes lab testing for anemia. Results show high iron, bilirubin, and transferrin and low hemoglobin and hematocrit. Which of the following is the most likely diagnosis to be documented on the chart? a. Pernicious anemia b. Folate deficiency anemia c. Iron deficiency anemia d. Sideroblastic anemia ANS: D Individuals with sideroblastic anemia may show signs of iron overload (hemosiderosis), including mild to moderate enlargement of the liver (hepatomegaly) and spleen (splenomegaly). High levels of iron indicate sideroblastic anemia, not pernicious anemia. High levels of iron indicate sideroblastic anemia, not folate deficiency. High levels of iron indicate sideroblastic anemia, not iron deficiency anemia. Cognitive Level: Comprehension 505 12. A 35-year-old female is diagnosed with vitamin B12 deficiency anemia (pernicious anemia). How should the nurse respond when the patient asks what causes pernicious anemia? A decrease in is the most likely cause. a. Ferritin b. Gastric enzymes c. Intrinsic factor d. Erythropoietin ANS: C The underlying alteration in pernicious anemia (PA) is the absence of intrinsic factor (IF), an enzyme required for gastric absorption of dietary vitamin B12, a vitamin essential for nuclear maturation and DNA synthesis in red blood cells. PA is not due to a decrease in ferritin, but a lack of the intrinsic factor. PA is not due to a decrease in gastric enzymes, but a lack of the intrinsic factor. PA is not due to a decrease in erythropoietin, but a lack of intrinsic factor. Cognitive Level: Comprehension 501 13. Which of the following individuals should the nurse assess first for a vitamin B12 deficiency anemia? a. 3-year-old female who is a fussy eater b. 26-year-old female in the second trimester of her first pregnancy c. 47-year-old male who had a gastrectomy procedure (removal of the stomach) d. 64-year-old male with a history of duodenal ulcers and gastrointestinal bleeding ANS: C With removal of the stomach, the intrinsic factor is also removed, leading to an inability to absorb B12; thus, the person with removal of the stomach is at greatest risk. With removal of the stomach, the intrinsic factor is also removed, leading to an inability to absorb B12; thus, the person with removal of the stomach is at greatest risk, not the person who is a fussy eater. With removal of the stomach, the intrinsic factor is also removed, leading to an inability to absorb B12; thus, the person with removal of the stomach is at greatest risk, not the person who is pregnant. With removal of the stomach, the intrinsic factor is also removed, leading to an inability to absorb B12; thus, the person with removal of the stomach is at greatest risk, not the person with ulcers. Cognitive Level: Comprehension 503 14. A 65-year-old male experienced loss of appetite, weight loss, lemon-yellow skin, liver enlargement, and a beefy red tongue shortly before his death. Autopsy suggested pernicious anemia, and the cause of death would most likely reveal: a. Brain hypoxia b. Liver hypoxia c. Heart failure d. Kidney failure ANS: C When the hemoglobin has decreased to 7 to 8 g/dL, the individual experiences the classic symptoms of anemia: weakness, fatigue, paresthesias of feet and fingers, difficulty walking, loss of appetite, abdominal pain, weight loss, and a sore tongue that is smooth and beefy red. The skin may become lemon yellow (sallow), caused by a combination of pallor and jaundice. Hepatomegaly, indicating right-sided heart failure, may be present in the elderly. The patient died of heart failure, not brain hypoxia. The patient died of heart failure, not liver hypoxia. The patient died of heart failure, not kidney failure. Cognitive Level: Comprehension 503 15. A 40-year-old male vegetarian is diagnosed with folate deficiency anemia. He reports that he is an alcoholic. Which of the following factors put him at greatest risk for developing his disease? a. Being vegetarian b. Being alcoholic c. Age d. Gender ANS: B Folate deficiency occurs more often in alcoholics and individuals who are malnourished because of fad diets or diets low in vegetables. A diet high in vegetables would help prevent folate deficiency. Age is not a factor in folate deficiency. Being alcoholic promotes the greatest risk, since this disorder is diet related. Gender is not a factor in folate deficiency. Being alcoholic promotes the greatest risk, since this disorder is diet related. Cognitive Level: Comprehension 503 16. How should the nurse prepare a patient who is to receive a Schilling test for pernicious anemia? a. Administer radioactive cobalamin and measure its excretion in the urine. b. Measure antigen-antibody immune complexes. c. Measure serum ferritin and total iron-binding capacity. d. Administer folate and evaluate folate content in a blood serum sample. ANS: A The Schilling test is performed by administering radioactive cobalamin and then measuring its excretion in the urine. Low urinary excretion is significant for pernicious anemia (PA). The Schilling test is performed by administering radioactive cobalamin and then measuring its excretion in the urine. Low urinary excretion is significant for PA. It does not involve the measurement of antigen-antibody complexes. The Schilling test is performed by administering radioactive cobalamin and then measuring its excretion in the urine. Low urinary excretion is significant for PA. It does not involve the measurement of serum ferritin and total iron-binding capacity. The Schilling test is performed by administering radioactive cobalamin and then measuring its excretion in the urine. Low urinary excretion is significant for PA. It does not involve the administration of folate. Cognitive Level: Comprehension 503 17. A 67-year-old female has chronic gastrointestinal bleeding. A nurse recalls the primary cause of her anemia is: a. Vitamin B12 deficiency b. Iron deficiency c. Folate deficiency d. Bone marrow failure ANS: B A continuous loss of blood is one of the most common causes of iron deficiency anemia (IDA). A continuous loss of blood is one of the most common causes of IDA; gastrointestinal bleeding does not lead to vitamin B12 deficiency. A continuous loss of blood is one of the most common causes of IDA; gastrointestinal bleeding does not lead to folate deficiency. A continuous loss of blood is one of the most common causes of IDA; gastrointestinal bleeding does not lead to bone marrow failure. Cognitive Level: Comprehension 504 18. A 34-year-old male presents in the emergency room with extreme fatigue and shortness of breath. His skin and sclera appear to have a yellowish discoloration. These assessment findings are consistent with which type of anemia? a. Posthemorrhagic anemia b. Iron deficiency anemia c. Aplastic anemia d. Hemolytic anemia ANS: D A yellow appearance to the skin and sclera are consistent with hemolytic anemia. A yellow appearance to the skin and sclera are consistent with hemolytic anemia, not posthemorrhagic anemia. A yellow appearance to the skin and sclera are consistent with hemolytic anemia, not iron deficiency anemia. A yellow appearance to the skin and sclera are consistent with hemolytic anemia, not aplastic anemia. Cognitive Level: Comprehension 501 19. A 58-year-old female presents in the clinic presenting with fatigue, weight loss, and tingling in her fingers. Laboratory findings show low hemoglobin and hematocrit, a high mean corpuscular volume, and normal plasma iron. These assessment findings are consistent with which type of anemia? a. Hemolytic anemia b. Pernicious anemia c. Iron deficiency anemia d. Aplastic anemia ANS: B Pernicious anemia is manifested by tingling paresthesias of feet and fingers. Pernicious, not hemolytic, anemia is manifested by tingling paresthesias of feet and fingers. Pernicious, not iron deficiency, anemia is manifested by tingling paresthesias of feet and fingers. Pernicious, not aplastic, anemia is manifested by tingling paresthesias of feet and fingers. Cognitive Level: Comprehension 501 20. The nurse will check which of the following tests to directly measure iron stores? a. Serum ferritin b. Transferrin saturation c. Bone marrow biopsy d. Total iron-binding capacity ANS: C Iron stores are measured directly by bone marrow biopsy. Iron stores are measured directly by bone marrow biopsy, not serum ferritin. Iron stores are measured directly by bone marrow biopsy, not transferrin saturation. Iron stores are measured directly by bone marrow biopsy, not total iron-binding capacity. Cognitive Level: Comprehension 504 21. A 21-year-old female was recently diagnosed with iron deficiency anemia. In addition to fatigue and weakness, which of the following clinical signs and symptoms would she most likely exhibit? a. Hyperactivity b. Spoon-shaped nails c. Gait problems d. Petechiae ANS: B Iron deficiency anemia is manifested by fingernails that become brittle and spoon shaped or concave. Iron deficiency anemia is manifested by fingernails that become brittle and spoon shaped or concave. It does not involve hyperactivity. Iron deficiency anemia is manifested by fingernails that become brittle and spoon shaped or concave. It does not involve gait problems. Iron deficiency anemia is manifested by fingernails that become brittle and spoon shaped or concave. It does not involve petechiae. Cognitive Level: Comprehension 504 22. A 21-year-old woman was recently diagnosed with iron deficiency anemia. Her hematocrit is 32%. Which of the following treatments would the nurse expect to be prescribed for her? a. Iron replacement b. Splenectomy c. A bone marrow transplant d. No treatment is necessary ANS: A Iron replacement therapy is required and very effective. Initial doses are 150 mg to 200 mg/day and are continued until the serum ferritin level reaches 50 mg/L. Splenectomy is not indicated. Iron replacement therapy is required and very effective. Initial doses are 150 mg to 200 mg/day and are continued until the serum ferritin level reaches 50 mg/L. A bone marrow transplant is not indicated. Iron replacement therapy is required and very effective. Initial doses are 150 mg to 200 mg/day and are continued until the serum ferritin level reaches 50 mg/L. Treatment is indicated. Iron replacement therapy is required and very effective. Initial doses are 150 mg to 200 mg/day and are continued until the serum ferritin level reaches 50 mg/L. Cognitive Level: Comprehension 504 23. A 45-year-old male is diagnosed with sideroblastic anemia. When he asks what the most likely cause of this disease is, what is the nurses best response? a. Ineffective iron uptake and abnormal hemoglobin production b. Misshapen erythrocytes with low hemoglobin c. Decreased levels of tissue iron with megaloblastic erythrocytes d. Premature erythrocyte destruction and erythropoietin deficiency ANS: A Sideroblastic anemia is due to ineffective iron uptake and hemoglobin production. Erythrocytes are not misshapen in sideroblastic anemia; iron uptake is altered. Iron is increased in sideroblastic anemia. Erythrocytes are not destroyed in sideroblastic anemia; alteration in iron uptake occurs. Cognitive Level: Comprehension 505 24. A 50-year-old female was diagnosed with sideroblastic anemia. Which of the following assessment findings would most likely occur? a. Bronze colored skin b. Decreased iron c. Normochromic erythrocytes d. Aplastic bone marrow ANS: A The skin of the patient with sideroblastic anemia is bronze in color. The patient with sideroblastic anemia shows signs of iron overload. The erythrocytes of individuals with sideroblastic anemia are hypochromic. The bone marrow is not aplastic, but contains ringed sideroblasts. Cognitive Level: Comprehension 505 25. A nurse is preparing to teach the staff about aplastic anemia. Which information should the nurse include? Aplastic anemia is caused by: a. Iron deficiency b. Excess levels of erythropoietin c. Hemolysis d. Stem cell deficiency ANS: D In aplastic anemia, erythrocyte stem cells are underdeveloped, defective, or absent. In aplastic anemia, erythrocyte stem cells are underdeveloped, defective, or absent; iron is not deficient. In aplastic anemia, erythrocyte stem cells are underdeveloped, defective, or absent. There are no excess levels of erythropoietin. In aplastic anemia, erythrocyte stem cells are underdeveloped, defective, or absent. Cells do not undergo hemolysis. Cognitive Level: Comprehension 506 26. A nurse recalls posthemorrhagic anemia can result in death when a patients blood loss is in excess of: a. 20% to 29% b. 30% to 39% c. 40% to 49% d. 50% to 59% ANS: C Death can occur if blood loss exceeds 40% to 49% of plasma volume. Death can occur if blood loss exceeds 40% to 49% of plasma volume, not 20% to 29%. Death can occur if blood loss exceeds 40% to 49% of plasma volume, not 30% to 39%. Death can occur if blood loss exceeds 40% to 49% of plasma volume, not 50% to 59%. Cognitive Level: Comprehension 506 27. A 57-year-old male presents to his primary care provider for red face, hands, feet, ears, and headache and drowsiness. A blood smear reveals an increased number of erythrocytes, indicating: a. Polycythemia vera (PV) b. Leukemia c. Sideroblastic anemia d. Hemosiderosis ANS: A PV is manifested by increased numbers of erythrocytes. PV is characterized by excessive proliferation of erythrocyte precursors in the bone marrow. Leukemia is not manifested by changes in erythrocytes. PV is characterized by excessive proliferation of erythrocyte precursors in the bone marrow. Sideroblastic anemia is characterized by sideroblastic rings. PV is characterized by excessive proliferation of erythrocyte precursors in the bone marrow. Hemosiderosis is iron overload. Cognitive Level: Comprehension 506 28. A 67-year-old female is admitted to the emergency department with a diagnosis of polycythemia vera. Upon taking the history, the patient will most likely report: a. Hyperactivity b. Decreased blood pressure c. Chest pain d. A pale skin color ANS: C Coronary blood flow may be affected, precipitating angina. The patient will experience signs of interrupted blood flow due to increased blood viscosity. They will not experience hyperactivity. Blood pressure will be increased, not decreased. The skin will be red over the face hands, feet, and ears. Cognitive Level: Comprehension 507 29. A 68-year-old female is admitted to the emergency department with a diagnosis of polycythemia vera (PV). A nurse realizes the patients symptoms are mainly the result of: a. A decreased erythrocyte count b. Rapid blood flow to the major organs c. Increased blood viscosity d. Vessel injury ANS: C The symptoms of PV are due to increased blood viscosity. The symptoms of PV are due to increased blood viscosity, and the erythrocyte count is elevated. The symptoms of PV are due to increased blood viscosity, and there will be decreased blood flow to tissues and organs. The symptoms of PV are due to increased blood viscosity; vessel injury does not occur. Cognitive Level: Comprehension 507 30. A 67-year-old female is admitted to the emergency department with a diagnosis of polycythemia vera (PV). Which treatment should the nurse discuss with the patient? a. Therapeutic phlebotomy b. Restoration of blood volume by plasma expanders c. Administration of packed red blood cells d. Iron replacement therapy ANS: A Treatment of PV is phlebotomy to reduce red cell mass and blood volume. Treatment of PV is phlebotomy to reduce red cell mass and blood volume; increasing blood volume will increase symptoms. Treatment of PV is phlebotomy to reduce red cell mass and blood volume; administration of additional cells will increase the problems. Treatment of PV is phlebotomy to reduce red cell mass and blood volume; iron replacement will increase the symptoms. Cognitive Level: Comprehension 507 31. A 70-year-old male is brought to the emergency department, where he dies shortly thereafter. Autopsy reveals polycythemia vera (PV). His death was most likely the result of: a. Acute renal failure b. Cerebral thrombosis c. Sepsis d. Acute leukemia ANS: B 50% of individuals with PV die within 18 months of the onset of initial symptoms because of thrombosis or hemorrhage. 50% of individuals with PV die within 18 months of the onset of initial symptoms because of thrombosis or hemorrhage, not renal failure. 50% of individuals with PV die within 18 months of the onset of initial symptoms because of thrombosis or hemorrhage, not infection and sepsis. 50% of individuals with PV die within 18 months of the onset of initial symptoms because of thrombosis or hemorrhage, not acute leukemia. Cognitive Level: Comprehension 508 32. A 67-year-old male was diagnosed with polycythemia vera (PV) but refused treatment. His condition is at risk for converting to: a. Chronic lymphocytic leukemia b. Burkitt lymphoma c. Multiple myeloma d. Acute myeloid leukemia ANS: D A significant potential outcome of PV is the conversion to acute myeloid leukemia (AML), occurring spontaneously in 10% of individuals and generally being resistant to conventional therapy. A significant potential outcome of PV is the conversion to AML, not chronic lymphocytic leukemia. A significant potential outcome of PV is the conversion to AML, not Burkitt lymphoma. A significant potential outcome of PV is the conversion to AML, not multiple myeloma. Cognitive Level: Comprehension 508 33. A staff member asks what leukocytosis means. How should the nurse respond? Leukocytosis can be defined as: a. A normal leukocyte count b. A high leukocyte count c. A low leukocyte count d. Another term for leukopenia ANS: B Leukocytosis is present when the count is higher than normal. Leukocytosis is present when the count is higher than normal, not normal. Leukocytosis is present when the count is higher than normal, not low. Leukocytosis is present when the count is higher than normal. It is not another term for leukopenia. Cognitive Level: Comprehension 508 34. A 20-year-old female has an increase in eosinophils. When the patient wants to know the most likely cause of the eosinophilia. What is the nurses best response? a. Parasitic invasion and allergic reactions b. Viral and bacterial infections c. Stress and anxiety reactions d. Fungal infections and delayed hypersensitivity ANS: A Parasitic invasion can lead to eosinophilia. Viral infections do not lead to eosinophilia; parasitic invasions do. Stress and anxiety reactions do not lead to eosinophilia; parasitic invasions do. Fungal infections do not lead to eosinophilia; parasitic invasions do. Cognitive Level: Comprehension 509 35. A 15-year-old female presents with splenomegaly, hepatomegaly, and lymph node enlargement. She is diagnosed with infectious mononucleosis. What should the nurse tell the patient about the recovery time? a. 72 hours b. 3 to 5 days c. A few weeks d. Six months ANS: C Infectious mononucleosis (IM) is usually self-limiting, and recovery occurs in a few weeks; severe clinical complications are rare (5%). Fatigue may last for 1 to 2 months after resolution of other symptoms. Seventy-two hours is too short; the disorder may last a few weeks. Three to five days is too short; the disorder may last a few weeks. Six months is too long; the disorder may resolve in a few weeks. Cognitive Level: Comprehension 511 36. A 35-year-old male with hyperthyroidism begins treatment to decrease thyroid activity. A nurse monitors for which of the following conditions that could result secondary to the treatment? a. Eosinophilia b. Basophilia c. Monocytosis d. Lymphocytosis ANS: B Basophilia results from antithyroid therapy. Basophilia, not eosinophilia, results from antithyroid therapy. Basophilia, not monocytosis, results from antithyroid therapy. Basophilia, not lymphocytosis, results from antithyroid therapy. Cognitive Level: Comprehension 509 37. A 15-year-old male is diagnosed with infectious mononucleosis. When the patient asks how he got this disease, how should the nurse respond? The most likely cause is: a. Adenovirus b. Epstein-Barr virus (EBV) c. Cytomegalovirus (CMV) d. Toxoplasma gondii ANS: B Infectious mononucleosis (IM) is an acute infection of B lymphocytes (B cells) with EBV. IM is an acute infection of B cells with EBV, not adenovirus. IM is an acute infection of B cells with EBV, not cytomegalovirus. IM is an acute infection of B cells with EBV, not Toxoplasma gondii. Cognitive Level: Comprehension 511 38. A 15-year-old male with infectious mononucleosis is being given instructions on how to prevent the spread of this infection to others. Which statement represents a correct instruction? a. Wear a surgical mask when others are in the room. b. Do not share drinking glasses or eating utensils. c. Avoid all contact with other people. d. No precautions are necessary. ANS: B Transmission of mononucleosis is usually through saliva from close personal contact. The virus also may be secreted in other mucosal secretions of the genital, rectal, and respiratory tract, as well as blood. A surgical mask is not necessary because the disorder is not airborne. The patient does not need to avoid all contact. Precautions should be taken. Cognitive Level: Comprehension 511 39. A 10-year-old male is diagnosed with leukemia. The nurse assesses for which other condition that could be associated with his disease? a. Down syndrome b. Hemophilia c. Hyperthyroidism d. Pheochromocytoma ANS: A There is also an increased incidence of leukemia in association with other hereditary abnormalities such as Down syndrome. There is also an increased incidence of leukemia in association with other hereditary abnormalities such as Down syndrome, not hemophilia. There is also an increased incidence of leukemia in association with other hereditary abnormalities such as Down syndrome, not hyperthyroidism. There is also an increased incidence of leukemia in association with other hereditary abnormalities such as Down syndrome, not pheochromocytoma. Cognitive Level: Comprehension 513 40. A 5-year-old female is diagnosed with acute leukemia. The nurse will most likely treat this patient with: a. Bone marrow transplant b. Immunotherapy c. Chemotherapy d. Localized radiation therapy ANS: C Chemotherapy, used in various combinations, is the treatment of choice for leukemia. Bone marrow transplant may be used, but chemotherapy is the treatment of choice for leukemia. Chemotherapy, used in various combinations, is the treatment of choice for leukemia; immunotherapy is not a treatment of choice. Chemotherapy, used in various combinations, is the treatment of choice for leukemia; localized radiation therapy is not the treatment of choice. Cognitive Level: Comprehension 513 41. An oncologist is discussing multiple myeloma. Which information should the oncologist include? Multiple myeloma can be defined as a neoplasm of: a. T cells b. B cells c. Immature plasma cells d. Mature red blood cells ANS: B Multiple myeloma is a B cell cancer. Multiple myeloma is a B cell cancer, not T cells. Multiple myeloma is a B cell cancer, not immature plasma cells. Multiple myeloma is a B cell cancer, not mature red blood cells. Cognitive Level: Comprehension 518 | p. 520 42. A 65-year-old male is diagnosed with multiple myeloma. He reports severe pain. This pain can be attributed to: a. Neuropathic infiltrations b. Destruction of bone tissue c. Tissue hypoxia d. Accumulation of toxic proteins ANS: B Multiple myeloma is a B cell cancer characterized by the proliferation of malignant plasma cells that infiltrate the bone marrow and aggregate into tumor masses throughout the skeletal system; thus, the pain is related to bone destruction. Multiple myeloma is a B cell cancer characterized by the proliferation of malignant plasma cells that infiltrate the bone marrow; thus, pain is related to destruction of bone tissue, not neuropathic infiltrations. Multiple myeloma is a B cell cancer characterized by the proliferation of malignant plasma cells that infiltrate the bone marrow; thus, pain is related to destruction of bone tissue, not tissue hypoxia. Multiple myeloma is a B cell cancer characterized by the proliferation of malignant plasma cells that infiltrate the bone marrow; thus, pain is related to destruction of bone tissue, not accumulation of toxic proteins. Cognitive Level: Comprehension 520 43. A 35-year-old female is diagnosed with lymphadenopathy. Which assessment finding will help confirm this diagnosis? a. Small, hard lymph nodes b. Disordered lymph nodes c. Nonpalpable, nontender lymph nodes d. Enlarged lymph nodes ANS: D Lymphadenopathy is evidenced by enlarged lymph nodes. Lymphadenopathy is evidenced by enlarged lymph nodes, not small and hard nodes. Lymphadenopathy is evidenced by enlarged lymph nodes, not disordered nodes. Lymphadenopathy is evidenced by enlarged lymph nodes, not nonpalpable lymph nodes. Cognitive Level: Comprehension 515 44. A 35-year-old male has enlarged lymph nodes in the neck and a mediastinal mass. He was diagnosed with Hodgkin lymphoma. Which of the following abnormal cells would the nurse expect to find with this disease? a. Merkel cell b. Schwann cell c. Reed-Sternberg cell d. Kupffer cell ANS: C Hodgkin lymphoma is manifested by Reed-Sternberg cells. Hodgkin lymphoma is manifested by Reed-Sternberg cells, not Merkel cells. Hodgkin lymphoma is manifested by Reed-Sternberg cells, not Schwann cells. Hodgkin lymphoma is manifested by Reed-Sternberg cells, not Kupffer cells. Cognitive Level: Comprehension 516 45. The people from which country have the lowest risk for Hodgkin lymphoma? a. United States b. Japan c. Denmark d. Great Britain ANS: B Japan has the lowest rate of Hodgkin lymphoma. The United States has one of the highest rates. Denmark has the one of the highest rates. Great Britain is not ranked. Cognitive Level: Comprehension 517 46. A 62-year-old female tells her health care provider she has been experiencing regular night sweats that cause her to wake up drenched. She also remarks that she has been unintentionally losing weight. Physical exam reveals enlarged lymph nodes on her neck that do not appear to be painful. She should be screened for which of the following cancers? a. Epstein-Barr virus b. Hodgkin lymphoma c. Acute leukemia d. Burkitt lymphoma ANS: B The patient has symptoms of Hodgkin lymphoma. About a third of individuals will have some degree of systemic symptoms. Intermittent fever, without other symptoms of infection, drenching night sweats, itchy skin (pruritus), and fatigue are relatively common. The patient with Epstein-Barr virus does not have night sweats. The patient with acute leukemia does not have night sweats or enlarged lymph nodes. The patient with Burkitt lymphoma does not have enlarged lymph glands or night sweats. Cognitive Level: Comprehension 517 47. A 10-year-old male presents with abdominal swelling, night sweats, fever, and weight loss. He is diagnosed with Burkitt lymphoma. Upon obtaining the history, which of the following is the most likely cause? a. Cytomegalovirus (CMV) b. Adenovirus c. Human papillomavirus (HPV) d. Epstein-Barr virus (EBV) ANS: D EBV is associated with almost all cases of Burkitt lymphoma. EBV, not CMV, is associated with almost all cases of Burkitt lymphoma. EBV, not adenovirus, is associated with almost all cases of Burkitt lymphoma. EBV, not HPV, is associated with almost all cases of Burkitt lymphoma. Cognitive Level: Comprehension 519 48. For a patient experiencing hypersplenism, the nurse expects the erythrocytes to be: a. Proliferated b. Activated c. Sequestered d. Infected ANS: C Hypersplenism results in sequestering of the blood cells. Hypersplenism results in sequestering, not proliferation, of the blood cells. Hypersplenism results in sequestering, not activation, of the blood cells. Hypersplenism results in sequestering, not infection, of the blood cells. Cognitive Level: Comprehension 521 49. Thrombocytopenia may be: a. Transient or consistent b. Normal or abnormal c. Congenital or acquired d. Active or inactive ANS: C The condition may also be either congenital or acquired and may be either primary or secondary to other conditions. The condition may also be either congenital or acquired and may be either primary or secondary to other conditions. It is not referred to as transient or consistent. The condition may also be either congenital or acquired and may be either primary or secondary to other conditions. It is not normal or abnormal. The condition may also be either congenital or acquired and may be either primary or secondary to other conditions. It is not active or inactive. Cognitive Level: Comprehension 523 50. A 30-year-old female presents with hematuria, menorrhagia, and bleeding gums. She is diagnosed with immune thrombocytic purpura (ITP). A nurse realizes the most likely cause is: a. Allergy-induced platelet lysis b. An immune response to hypersplenism c. Antibody destruction of platelets d. T cell injury to megakaryocytes ANS: C The majority of cases of ITP are due to immune driven destruction of platelets. The majority of cases of ITP are due to immune driven destruction of platelets. It is not due to allergy. The majority of cases of ITP are due to immune driven destruction of platelets. It is not due to hypersplenism. The majority of cases of ITP are due to immune driven destruction of platelets. It is not due to T cell injury. Cognitive Level: Comprehension 524 51. A 50-year-old female is diagnosed with primary thrombocythemia. A nurse would expect the blood smear to reveal platelets. a. Defective b. Fragmented c. Consumed d. Overproduced ANS: D Thrombocythemia is characterized by a platelet count more than 400,000 platelets/mm3 of blood and is symptomatic when the count exceeds 1,000,000/ mm3, at which time the risk for intravascular clotting (thrombosis) is high. Thrombocythemia is characterized by a high platelet count, not a defective one. Thrombocythemia is characterized by a high platelet count, not a fragmented one. Thrombocythemia is characterized by a high platelet count, not a consumed one. Chapter 24. Alterations of Hematologic Function in Children MULTIPLE CHOICE 1. A 1-year-old female is diagnosed with anemia secondary to insufficient erythropoiesis. When the parents asked what caused this, how should the nurse respond? The most likely cause(s) is (are): a. Genetic factors b. An iron deficiency c. A hemoglobin abnormality d. An erythrocyte structural abnormality ANS: B The most common cause of insufficient erythropoiesis is iron deficiency. The most common cause of insufficient erythropoiesis is iron deficiency, not genetic factors. The most common cause of insufficient erythropoiesis is iron deficiency, not a hemoglobin abnormality. The most common cause of insufficient erythropoiesis is iron deficiency, not an erythrocyte structural abnormality. Cognitive Level: Comprehension 535 2. A 12-month-old toddler weighing 18 pounds is brought to the clinic because of weakness, slow physical growth, and developmental delays. His mother reports that the only food he will consume is cows milk. Considering this information, the nurse decides that the child probably has anemia. a. Pernicious b. Iron deficiency c. Aplastic d. Hemolytic ANS: B As many as one-third of infants with severe iron deficiency anemia have chronic intestinal blood loss induced by exposure to a heat-labile protein in cows milk. Such exposure causes an inflammatory gastrointestinal reaction that damages the mucosa and results in diffuse hemorrhage. The intake of cows milk leads to iron deficiency anemia; it does not lead to pernicious anemia. The intake of cows milk leads to iron deficiency anemia; it does not lead to aplastic anemia. The intake of cows milk leads to iron deficiency anemia; it does not lead to hemolytic anemia. Cognitive Level: Comprehension 536 3. A 16-month-old female presents with tachycardia, pallor, anorexia, and systolic murmur. The nurse is checking the lab results, and the hemoglobin determination indicates a level below g/dL. a. 5 b. 7 c. 10 d. 14 ANS: A When hemoglobin levels fall below 5 g/dL, pallor, anorexia, tachycardia, and systolic murmurs may occur. When hemoglobin levels fall below 5 g/dL, not 7, pallor, anorexia, tachycardia, and systolic murmurs may occur. When hemoglobin levels fall below 5 g/dL, not 10, pallor, anorexia, tachycardia, and systolic murmurs may occur. When hemoglobin levels fall below 5 g/dL, not 14, pallor, anorexia, tachycardia, and systolic murmurs may occur. Cognitive Level: Comprehension 536 4. Which mother is at most risk for a maternal-fetal blood incompatibility? a. Mother is Rh-positive, and fetus is Rh-negative. b. Mother is Rh-negative, and fetus is Rh-positive. c. Mother has type A blood, and fetus has type O blood. d. Mother has type AB, blood and fetus has type B blood. ANS: B Maternal-fetal incompatibility exists if mother and fetus differ in ABO blood type or if the fetus is Rh-positive and the mother is Rh-negative. Maternal-fetal incompatibility exists if mother and fetus differ in ABO blood type or if the fetus is Rh-positive and the mother is Rh-negative. Symptoms do not occur in a type O fetus. Symptoms do not occur in type AB mothers. Cognitive Level: Comprehension 536 5. A 22-year-old female gives birth at 20 weeks gestation to a stillborn fetus. Physical exam of the fetus by the nurse reveals gross edema of the entire body and anemia. This condition is referred to as: a. Hyperbilirubinemia. b. Hydrops fetalis. c. Erythroblastosis fetalis. d. Ascites. ANS: B Fetuses that do not survive anemia in utero usually are stillborn, with gross edema in the entire body, a condition called hydrops fetalis. Fetuses that do not survive anemia in utero usually are stillborn, with gross edema in the entire body, a condition called hydrops fetalis, not hyperbilirubinemia. Fetuses that do not survive anemia in utero usually are stillborn, with gross edema in the entire body, a condition called hydrops fetalis, not erythroblastosis fetalis. Fetuses that do not survive anemia in utero usually are stillborn, with gross edema in the entire body, a condition called hydrops fetalis, not ascites. Cognitive Level: Comprehension 539 6. Sickle cell disease is characterized by the presence of Hb S. A nurse is trying to differentiate between Hb S and normal Hb. Which of the following amino acids is present in Hb S and not present in normal Hb? a. Valine b. Glutamic acid c. Proline d. Histidine ANS: A Hb S is formed by a genetic mutation in which one amino acid (valine) replaces another (glutamic acid). Valine has replaced glutamic acid. Hb S is formed by a genetic mutation in the amino acid (valine), not proline. Hb S is formed by a genetic mutation in the amino acid (valine), not histidine. Cognitive Level: Comprehension 539 7. A 10-year-old male is diagnosed with sickle cell anemia. When the parents ask who is responsible for this disease, what is the nurses best response? He most likely inherited it from: a. His mother b. His father c. Noth his mother and father d. None of the above; sickle cell disease is not clearly an inherited disease. ANS: C Sickle cell is a recessive disorder inherited from both parents. Sickle cell is a recessive disorder inherited from both parents. Sickle cell is a recessive disorder inherited from both parents. Sickle cell is a recessive disorder inherited from both parents. Cognitive Level: Comprehension 540 8. In the United States, which group of people should be assessed first for sickle cell disease? a. Asians b. African-Americans c. Hispanics d. Caucasians ANS: B In the United States, sickle cell disease is most common in African-Americans. In the United States, sickle cell disease is most common in African-Americans, not Asians. In the United States, sickle cell disease is most common in African-Americans, not Hispanics. In the United States, sickle cell disease is most common in African-Americans, not Caucasians. Cognitive Level: Comprehension 540 9. A 25-year-old female has a child that is diagnosed with sickle cell anemia. She does not have the disease. Which of the following characterizes the genetic makeup of the parents with regard to this trait? a. Hb S and Hb S b. Hb S and Hb A c. Hb S and Hb C d. Hb A and Hb C ANS: B In this instance the child inherits Hb S from one parent and normal hemoglobin (Hb A), not Hb S, for both. In this instance the child inherits Hb S from one parent and normal hemoglobin (Hb A). In this instance the child inherits Hb S from one parent and normal hemoglobin (Hb A), not Hb C, and Hb S. In this instance the child inherits Hb S from one parent and normal hemoglobin (Hb A). Cognitive Level: Comprehension 540 10. When should the nurse start closely monitoring the patient with sickle cell anemia? If: a. Oxygen tension is low b. pH is increased c. Plasma osmolality is decreased d. Fever develops ANS: A Sickling occurs when oxygen tension is low. Sickling occurs when oxygen tension is low, not due to pH. Sickling occurs when oxygen tension is low, not due to a decrease in plasma osmolality. Sickling occurs when oxygen tension is low, now due to the development of fever. Cognitive Level: Comprehension 540 11. A 12-year-old male is diagnosed with sickle cell anemia. A blood smear reveals severely sickled cells. A nurse recalls the sickled cells will be removed from circulation mostly by the: a. Liver b. Pancreas c. Kidney d. Spleen ANS: D Sickled cells undergo hemolysis in the spleen or become sequestered there, causing blood pooling and infarction of splenic vessels. Sickled cells undergo hemolysis in the spleen, not the liver. Sickled cells undergo hemolysis in the spleen, not the pancreas. Sickled cells undergo hemolysis in the spleen, not the kidney. Cognitive Level: Comprehension 540 12. Which major symptom in a patient with sickle cell anemia indicates to the nurse, the patient is experiencing a vaso-occlusive crisis? a. Peripheral edema b. Pain c. Petechiae d. An enlarged spleen ANS: B Vaso-occlusive crisis is extremely painful and may last for days or even weeks, with an average duration of 4 to 6 days. Vaso-occlusive crisis is extremely painful; it does not promote peripheral edema. Vaso-occlusive crisis is extremely painful; it does not promote petechiae. Vaso-occlusive crisis is extremely painful; it does not lead to an enlarged spleen. Cognitive Level: Comprehension 541 13. For which type of sickle cell crisis should the nurse assess for in young children? a. Hyperhemolytic crisis b. Vaso-occlusive crisis c. Aplastic crisis d. Sequestration crisis ANS: D Sequestration occurs when large amounts of blood become acutely pooled in the liver and spleen. This type of crisis is seen only in a young child. Sequestration, not hyperhemolysis, occurs when large amounts of blood become acutely pooled in the liver and spleen. This type of crisis is seen only in a young child. Sequestration, not vaso-occlusive crisis, occurs when large amounts of blood become acutely pooled in the liver and spleen. This type of crisis is seen only in a young child. Sequestration, not aplastic crisis, occurs when large amounts of blood become acutely pooled in the liver and spleen. This type of crisis is seen only in a young child. Cognitive Level: Comprehension 541 14. A 6-year-old male presents with fatigue, jaundice, and irritability. A blood smear shows the presence of sickled cells. Erythropoiesis is compromised in this child; which crisis should the nurse monitor the patient for? a. Vaso-occlusive crisis b. Sequestration crisis c. Aplastic crisis d. Hyperhemolytic crisis ANS: C Aplastic anemia is caused by diminished erythropoiesis despite an increased need for new erythrocytes. Vaso-occlusive crisis is manifested by pain. Sequestered crisis is manifested by enlarged spleen. Hyperhemolytic crisis is due to infection. Cognitive Level: Comprehension 541 15. A 5-year-old female dies from sickle cell disease. The pediatrician will document the most likely cause of death is: a. Decreased hemoglobin b. Infection c. An obstructive crisis d. A hyperhemolytic crisis ANS: B Infection is the most common cause of death related to sickle cell disease. Infection, not decreased hemoglobin, is the most common cause of death related to sickle cell disease. Infection, not an obstructive crisis, is the most common cause of death related to sickle cell disease. Infection, not a hyperhemolytic crisis, is the most common cause of death related to sickle cell disease. Cognitive Level: Comprehension 541 16. A geneticist is discussing thalassemias. Which information should be included? The alpha and beta thalassemias are inherited in an fashion. a. Autosomal recessive b. Autosomal dominant c. X-linked recessive d. X-linked dominant ANS: A The alpha and beta thalassemias are inherited autosomal recessive disorders. The alpha and beta thalassemias are inherited autosomal recessive disorders, not dominant. The alpha and beta thalassemias are inherited autosomal recessive disorders, not X-linked recessive. The alpha and beta thalassemias are inherited autosomal recessive disorders, not X-linked dominant. Cognitive Level: Comprehension 542 17. A 2-year-old male presented with growth and maturation retardation and splenomegaly. He died shortly after arriving at the ER. Autopsy revealed thalassemia secondary to defective: a. Erythrocyte membranes b. Iron metabolism c. Stem cell formation d. Hemoglobin synthesis ANS: D Thalassemia would be secondary to defective hemoglobin synthesis. Thalassemia would be secondary to defective hemoglobin synthesis; it is not due to erythrocyte membrane abnormalities. Thalassemia would be secondary to defective hemoglobin synthesis. It is not due to defective iron metabolism. Thalassemia would be secondary to defective hemoglobin synthesis. It is not due to defective stem cell formation. Cognitive Level: Comprehension 535 18. A 38-year-old female gives birth to a stillborn fetus. Autopsy reveals cardiomegaly, hepatomegaly, edema, and ascites. Which of the following does the nurse suspect caused the death? a. Alpha thalassemia minor b. Alpha thalassemia major c. Hemoglobin H disease d. Alpha trait ANS: B Alpha thalassemia major causes hydrops fetalis and fulminant intrauterine congestive heart failure. In addition to edema and massive ascites, the fetus has a grossly enlarged heart and liver. The fetus has alpha thalassemia major, not minor. Major is manifested by heart failure and ascites. The stillborn fetus has symptoms of alpha thalassemia major, not hemoglobin H disease. The stillborn fetus has symptoms of alpha thalassemia major, not alpha trait, which is the mildest form of the disease. Cognitive Level: Comprehension 542 19. If an infant has hydrops fetalis, which type of thalassemia does the nurse suspect? a. Beta minor b. Beta major c. Alpha minor d. Alpha major ANS: D Hydrops fetalis is due to alpha thalassemia major. Hydrops fetalis is due to alpha thalassemia major, not beta minor. Hydrops fetalis is due to alpha thalassemia major, not beta major . Hydrops fetalis is due to alpha thalassemia major, not alpha minor which results in anemia. Cognitive Level: Comprehension 543 20. The mother of a 3-year-old child speaks to the pediatrician because the child took several hours to stop bleeding following a minor scrape. Testing reveals that the child has hemophilia A resulting from a deficiency in factor: a. IX b. XII c. XIII d. VIII ANS: D Hemophilia A is a deficiency in factor VIII. Hemophilia A is a deficiency in factor VIII, not IX. Hemophilia A is a deficiency in factor VIII, not factor XII. Hemophilia A is a deficiency of factor VIII, not factor XIII. Cognitive Level: Comprehension 544 21. A nurse wants to chart the other name for hemophilia B. Which term should the nurse write? a. Classic hemophilia b. Christmas disease c. Thalassemia d. von Willebrand disease ANS: B Hemophilia B is also known as Christmas disease. Hemophilia B is also known as Christmas disease, not classic hemophilia. Hemophilia B is also known as Christmas disease; thalassemia is not a clotting disorder. Hemophilia B is also known as Christmas disease; von Willebrand disease is a factor VIII disorder. Cognitive Level: Comprehension 544 22. A 3-year-old child presents with bruising on the legs and trunk and a petechial rash. The mother also reports frequent nosebleeds. Lab tests reveal a decreased platelet count. Which is the most likely diagnosis the nurse will see documented on the chart? a. Idiopathic thrombocytopenic purpura (ITP) b. Leukemia c. Thalassemia d. Hemophilia ANS: A A decreased platelet count is the cause of ITP. A decreased platelet count is the cause of ITP. Leukemia is not related to platelets. A decreased platelet count is the cause of ITP. Thalassemia is not related to platelets. A decreased platelet count is the cause of ITP. Hemophilia is not related to platelets. Cognitive Level: Comprehension 545 23. A 5-year-old male is diagnosed with idiopathic thrombocytic purpura (ITP). Which information should the nurse give the staff regarding the cause of this condition? a. Normal postnatal platelet lysis b. Virally induced antibody destruction of platelets c. An allergic reaction to vaccinations d. Maternal antibodies that target platelets in the neonate ANS: B In approximately 70% of cases of ITP, there is an antecedent viral disease. A viral disease leads to antibody destruction of platelets, not lysis. A viral disease leads to antibody destruction of platelets; it may be related to vaccination but is not an allergic response. A prior viral disease can lead to ITP; it is not due to maternal antibodies. Cognitive Level: Comprehension 545 24. Which of the following clusters of symptoms would lead the nurse to suspect a child has idiopathic thrombocytopenic purpura (ITP)? a. Multiple infections; bruising; abnormal bone marrow aspiration b. Lower extremity that is warm to touch, edematous, and painful c. Spontaneous nosebleeds, bruising, petechiae d. Increased platelet count; recent-onset venous thrombosis ANS: C Nosebleeds, bruising, and petechiae are signs of a lack of clotting due to low platelets and ITP. Nosebleeds, bruising, and petechiae are signs of a lack of clotting due to low platelets and ITP, not infections. Nosebleeds, bruising, and petechiae are signs of a lack of clotting due to low platelets and ITP, not warmth in extremities that are edematous and painful. Bleeding would not be related to an increased platelet count. Cognitive Level: Comprehension 545 25. A 1-year-old is diagnosed with idiopathic thrombocytopenic purpura (ITP). The nurse assesses for the most serious concern, which is development of: a. Respiratory infection b. Asymmetric bruising c. Intracranial bleeding d. Immunosuppression ANS: C Although the incidence is less than 1%, intracranial hemorrhage is the most serious complication of ITP. Intracranial hemorrhage is the most serious concern, not respiratory infection. Intracranial hemorrhage is the most serious concern, not asymmetric bleeding. Intracranial hemorrhage is the most serious concern, not immunosuppression. Cognitive Level: Comprehension 545 26. A nurse monitors for the most common childhood cancer, which is: a. Acute lymphoblastic leukemia (ALL) b. Chronic myelocytic leukemia (CML) c. Non-Hodgkin lymphoma d. Hodgkin lymphoma ANS: A Approximately 80% to 85% of leukemias in children are ALL. Approximately 80% to 85% of leukemias in children are ALL, not CML. Approximately 80% to 85% of leukemias in children are ALL, not non-Hodgkin. Approximately 80% to 85% of leukemias in children are ALL, not Hodgkin lymphoma. Cognitive Level: Comprehension 546 27. A 10-year-old male with Down syndrome undergoes chemotherapy for cancer. Following treatment, monitoring for which condition is priority? a. Acute lymphoblastic leukemia (ALL) b. Acute myelogenous leukemia (AML) c. Non-Hodgkin lymphoma (NHL) d. Hodgkin lymphoma ANS: B AML is attributable to prior chemotherapy. AML is attributable to prior chemotherapy, not ALL. AML is attributable to prior chemotherapy, not NHL. AML is attributable to prior chemotherapy, not Hodgkin lymphoma. Cognitive Level: Comprehension 546 28. A 10-year-old female is diagnosed with a malignancy in the brain and lung. DNA analysis reveals translocation at chromosome 7 and 14. The most likely medical diagnosis the primary care provider will make is: a. Lymphoblastic non-Hodgkin lymphoma (NHL) b. Nodular NHL c. Hodgkin lymphoma d. Small noncleaved cell NHL ANS: A Lymphoblastic NHL shows chromosomal translocations, particularly chromosomes 7 and 14. Lymphoblastic NHL, not nodular, shows chromosomal translocations, particularly chromosomes 7 and 14. Lymphoblastic NHL, not Hodgkin, shows chromosomal translocations, particularly chromosomes 7 and 14. Lymphoblastic NHL, not small cell non-Hodgkin, shows chromosomal translocations, particularly chromosomes 7 and 14. Cognitive Level: Comprehension 547 29. Which condition makes the patient most prone for developing non-Hodgkin lymphoma (NHL)? a. Sickle cell disease b. Sickle cell trait c. Renal failure d. AIDS ANS: D Children with AIDS have an increased risk of developing NHL. Children with AIDS, not sickle cell disease, have an increased risk of developing NHL. Children with AIDS, not sickle cell trait, have an increased risk of developing NHL. Children with AIDS, not renal failure, have an increased risk of developing NHL. Cognitive Level: Comprehension 548 30. What is a priority assessment for Hodgkin lymphoma in children? a. Painless adenopathy in cervical nodes b. Significant bruising c. Weight gain d. Petechiae ANS: A Painless adenopathy in the lower cervical chain, with or without fever, is the most common symptom in children with Hodgkin lymphoma. Painless adenopathy is the most common symptom, not bruising. Painless adenopathy is the most common symptom, not weight gain. Painless adenopathy is the most common symptom, not petechiae. Cognitive Level: Comprehension 548 31. Which laboratory test will assist the nurse in identifying infants who are prone to develop hemolytic disease of the newborn (HDN)? a. Total bilirubin b. Coombs c. Rh antibodies d. Platelets ANS: B Routine evaluation of fetuses at risk for HDN includes the Coombs test. Routine evaluation of fetuses at risk for HDN includes the Coombs test, not bilirubin. Routine evaluation of fetuses at risk for HDN includes the Coombs test, not Rh antibodies. Routine evaluation of fetuses at risk for HDN includes the Coombs test, not platelets. Cognitive Level: Comprehension 539 MULTIPLE RESPONSE 1. A nurse is planning care for a child with iron deficiency anemia. Characteristics of iron deficiency anemia include which of the following? (Select all that apply.) a. It is most common between the ages of 6 months and 2 years. b. It is related to gender and race. c. It may be related to socioeconomic factors. d. It is rare among teenagers. e. It is difficult to diagnose in early stages. ANS: A, C, E Iron deficiency anemia is the most common blood disorder of infancy and childhood, with the highest incidence occurring between 6 months and 2 years of age. Incidence is not related to gender or race, but socioeconomic factors are important because they affect nutrition. The symptoms of mild anemialistlessness and fatigueusually are not present or are undetectable in infants and young children who are unable to describe these symptoms. Therefore, parents generally do not note any change in the childs behavior or appearance until moderate anemia has developed. Cognitive Level: Comprehension 536 2. A 5-year-old male is diagnosed with leukemia. Which of the following symptoms would the nurse expect? (Select all that apply.) a. Fatigue b. Jaundice c. Pallor d. Petechiae e. Fever ANS: A, C, D Pallor, fatigue, petechiae, purpura, bleeding, and fever generally are present. Jaundice is not. Chapter 25. Structure and Function of the Cardiovascular and Lymphatic Systems MULTIPLE CHOICE 1. A 52-year-old female is admitted to the cardiac unit with a diagnosis of pericarditis. She asks the nurse to explain where the infection is. In providing an accurate description, the nurse states that the pericardium is: a. The outer muscular layer of the heart b. The innermost layer of the heart chambers c. A membranous sac that encloses the heart d. The hearts fibrous skeleton ANS: C The pericardium is the membranous sac that surrounds the heart. The outer layer of the heart is the myocardium. The innermost layer of the heart is the endocardium. The hearts fibrous skeleton is attached to the myocardium. Cognitive Level: Comprehension 552 2. A nurse is explaining the function of the heart. Which is a correct response by the nurse? A function of the pericardium is to: a. Provide a barrier against extracardial infections. b. Improve blood flow through the heart. c. Play a role in cardiac conduction. d. Assist in cardiac contraction. ANS: A A function of the pericardium is to provide a barrier against extracardial infections. The pericardium does not improve blood flow through the heart as it is on the outside. The pericardium does not have a role in cardiac conduction. The inner portions of the heart control this. The pericardium does not assist in contraction. The muscular layers assist with this. Cognitive Level: Comprehension 552 3. A 65-year-old male develops blockage in the pulmonary artery. As a result of the blockage, blood would first back up into the: a. Aorta b. Left ventricle c. Pulmonary veins d. Right ventricle ANS: D Blockage in the pulmonary artery would cause blood to back up into the right ventricle. Blockage in the pulmonary artery would cause blood to back up into the right ventricle, not the aorta. These two vessels do not communicate. Blockage in the pulmonary artery would cause blood to back up into the right ventricle, not the left ventricle. This vessel and chamber do not communicate. Blockage in the pulmonary artery would cause blood to back up into the right ventricle, not the pulmonary vein. The pulmonary vein takes blood to the left atrium. Cognitive Level: Comprehension 553 4. A nurse is teaching about the heart. Which information should the nurse include? The chamber of the heart that generates the highest pressure is the: a. Right atrium b. Left atrium c. Left ventricle d. Right ventricle ANS: C The left ventricle generates the highest pressure. The left ventricle, not the right atrium, generates the highest pressure. The left ventricle, not the left atrium, generates the highest pressure. The left ventricle, not the right ventricle, generates the highest pressure. Cognitive Level: Comprehension 553 5. A nurse recalls the chamber that receives blood from the systemic circulation is the: a. Right atrium b. Right ventricle c. Left atrium d. Left ventricle ANS: A The right atrium receives the blood from the systemic circulation. The right atrium receives the blood from the systemic circulation; the right ventricle receives blood from the right atrium. The right atrium receives the blood from the systemic circulation; the left atrium receives blood from the lungs. The right atrium receives the blood from the systemic circulation; the left ventricle receives blood from the left atrium. Cognitive Level: Comprehension 554 6. Which statement indicates the nurse understands blood flow? Oxygenated blood flows through the: a. Superior vena cava b. Pulmonary veins c. Pulmonary artery d. Cardiac veins ANS: B Oxygenated blood flows through the pulmonary veins. Oxygenated blood flows through the pulmonary veins, not the superior vena cava, which carries venous blood. Oxygenated blood flows through the pulmonary veins, not the pulmonary artery, which carries unoxygenated blood to the lungs. Oxygenated blood flows through the pulmonary veins, not the cardiac veins, which carry unoxygenated blood. Cognitive Level: Comprehension 554 7. A 20-year-old male underwent an echocardiogram to assess chest pain. Results revealed a congenital defect in papillary muscles. Which of the following would the nurse expect to occur? a. Closure of the semilunar valve b. Backward expulsion of the atrioventricular valves c. Closure of the atrioventricular valve d. Backward expulsion of the semilunar valves ANS: B The papillary muscles are extensions of the myocardium that pull the cusps together and downward at the onset of ventricular contraction, thus preventing their backward expulsion into the atria. Defects in the papillary muscles would not affect the semilunar valve closure. Defects in the papillary muscles do not affect the atrioventricular valves. The papillary muscles prevent backward expulsion into the atria. They do not affect the semilunar valves. Cognitive Level: Comprehension 554 8. A cardiologist is discussing valves with the staff. Which information should the cardiologist include? are the anchors of the atrioventricular valves. a. Chordae tendineae cordis b. Great vessels c. Coronary ostia d. Trabeculae carneae ANS: A The atrioventricular valve openings are attached to the papillary muscles by the chordae tendineae cordis. The atrioventricular valve openings are attached to the papillary muscles by the chordae tendineae cordis. The great vessels are the vessels that bring blood to and out of the heart and are not attached to the chordae tendineae. The atrioventricular valve openings are attached to the papillary muscles by the chordae tendineae cordis, not the coronary ostia, which are openings in the aorta for the coronary arteries. The atrioventricular valve openings are attached to the papillary muscles by the chordae tendineae cordis, not the trabeculae carneae, which are a portion of the myocardium. Cognitive Level: Comprehension 554 9. Which statement indicates the nurse understands coronary ostia? The coronary ostia (the openings to the coronary arteries) are found in the: a. Left ventricle b. Inferior vena cava c. Coronary sinus d. Aorta ANS: D The ostia are found on the aorta. The ostia are found on the aorta, not the ventricle. The ostia are found on the aorta, not the vena cava. The ostia are found on the aorta, not the coronary sinus. Cognitive Level: Comprehension 556 10. The nurse is planning care for a patient with heart problems. Which information should the nurse remember? The artery travels down the interventricular septum and delivers blood to portions of the left and right ventricle. a. Right coronary b. Circumflex c. Left anterior descending d. Cardiac ANS: C The left anterior descending artery delivers blood to the left and right ventricle. The left anterior descending artery, not the right coronary artery, delivers blood to the left and right ventricle. The left anterior descending artery, not the circumflex, delivers blood to the left and right ventricle. The left anterior descending artery, not the cardiac artery, delivers blood to the left and right ventricle. Cognitive Level: Comprehension 557 11. A 65-year-old male is transported to the ER for chest pain. An electrocardiogram reveals a prolonged QRS interval. What is the nurse monitoring when the nurse observes the QRS complex on the electrocardiogram? The QRS complex reflects: a. Ventricular activity b. Pulmonary artery closure c. Mitral valve opening d. Aortic valve closing ANS: A The QRS complex represents the sum of all ventricular muscle cell depolarizations. The QRS complex represents the sum of all ventricular muscle cell depolarizations, not the pulmonary artery. The QRS complex represents the sum of all ventricular muscle cell depolarizations; it does not reflect mitral opening. The QRS complex represents the sum of all ventricular muscle cell depolarizations; it does not reflect activity of the aortic valve. Cognitive Level: Comprehension 559 12. When a staff member asks where venous blood from the coronary circulation drains into, what is the best response by the nurse? The: a. Superior vena cava b. Inferior vena cava c. Right atrium d. Reft atrium ANS: C Unoxygenated blood from the coronary veins enters the right atrium through the coronary sinus. Unoxygenated blood from the coronary veins enters the right atrium through the coronary sinus. It does not flow into the superior vena cava. Unoxygenated blood from the coronary veins enters the right atrium through the coronary sinus. It does not flow into the inferior vena cava. Unoxygenated blood from the coronary veins enters the right atrium, not the left, through the coronary sinus. Cognitive Level: Comprehension 557 13. While viewing the electrocardiogram, the nurse recalls the conducts action potentials down the atrioventricular septum. a. Bachmann bundle b. Bundle of His c. Sinoatrial node d. Atrioventricular node ANS: B The bundle of His conducts action potentials down the atrioventricular septum. The bundle of His conducts action potentials down the atrioventricular septum, not the Bachmann bundle. The bundle of His conducts action potentials down the atrioventricular septum; the sinoatrial node conducts the potential along the atria. The bundle of His conducts action potentials down the atrioventricular septum; the atrioventricular node conducts impulses to the ventricles. Cognitive Level: Comprehension 557 14. A 13-year-old female took a weight loss drug that activated the sympathetic nervous system. Which of the following assessment findings would the nurse expect? a. Decreased myocardial contraction b. Decreased heart rate c. Increased cardiac conduction d. Increased intranodal conduction time ANS: C Stimulation of the SA node by the sympathetic nervous system rapidly increases cardiac conduction. Stimulation of the sympathetic nervous system would increase myocardial contraction. Stimulation of the sympathetic nervous system would increase heart rate. Stimulation of the sympathetic nervous system would not affect conduction time within the node. These are inherent rates. Cognitive Level: Comprehension 560 15. A 50-year-old female received trauma to the chest that caused severe impairment of the primary pacemaker cells of the heart. Which of the following areas received the greatest damage? a. Atrioventricular (AV) node b. Sinoatrial (SA) node c. Bundle of His d. Ventricles ANS: B The SA node is considered the pacemaker of the heart. The SA node, not the AV node, is considered the pacemaker of the heart. The SA node is considered the pacemaker of the heart; the bundle of His is not involved. The SA node is considered the pacemaker of the heart; the ventricles are not involved. Cognitive Level: Comprehension 560 16. A 54-year-old male is diagnosed with left bundle branch block. Which of the following structures would not receive an electrical impulse? a. Atrioventricular (AV) node b. Sinoatrial (SA) node c. Bundle of His d. The left ventricle ANS: D The left bundle branch conducts impulses to the left ventricle. The left bundle branch conducts impulses to the left ventricle; the AV node feeds conduction of the bundles. The left bundle branch conducts impulses to the left ventricle; the SA node initiates conduction. The left bundle branch conducts impulses to the left ventricle; the bundle of His precedes the division of the left and right bundles. Cognitive Level: Comprehension 557 17. Which information by the nurse indicates a good understanding of depolarization? Depolarization of a cardiac muscle cell occurs as the result of: a. A decrease in the permeability of the cell membrane to ions b. The rapid movement of ions across the cell membrane c. A blockade by calcium ions d. Stimuli instigated during the refractory period ANS: B Depolarization is caused by the movement of electrically charged solutes (ions) across cardiac cell membranes. Permeability must be increased for movement to occur. A blockage of calcium ions would decrease depolarization. No cardiac action potential can be initiated in the refractory period. Cognitive Level: Comprehension 558 18. A cardiologist is teaching about the period that follows depolarization of the myocardium and represents a period during which no new cardiac potential can be propagated. What is the cardiologist describing? a. Absolute refractory b. Hyperpolarization c. Resting d. Threshold ANS: A A refractory period is the time during which no new cardiac action potential can be initiated by a stimulus. It follows depolarization. A refractory period is the time, not hyperpolarization, during which no new cardiac action potential can be initiated by a stimulus. It follows depolarization. Cardiac potential does rest, but the period is termed the refractory period. Threshold is related to depolarization. Cognitive Level: Comprehension 559 19. The nurse is reviewing a normal electrocardiogram. The nurse assesses the PR interval because it represents: a. Atrial depolarization b. Ventricular depolarization c. Onset of atrial activation to onset of ventricular activity d. Electrical systole of the ventricles ANS: C The PR interval represents the onset of atrial activation to the onset of ventricular activity. The P wave represents atrial depolarization. The QRS complex represents ventricular depolarization. The QT interval represents electrical systole of the ventricles. Cognitive Level: Comprehension 559 20. The represents the sum of all ventricular muscle cell depolarization. a. PR interval b. QRS complex c. QT interval d. P wave ANS: B The QRS complex represents the sum of all ventricular muscle cell depolarizations. The PR interval represents the onset of atrial activation to the onset of ventricular activity. The QT interval represents electrical systole of the ventricles. The P wave represents atrial depolarization. Cognitive Level: Comprehension 559 21. When a student nurse asks the nurse how the cardiac electrical impulse normally begins, what is the most correct response? The cardiac electrical impulse normally begins spontaneously in the sinoatrial (SA) node because it: a. Has a superior location in the right atrium b. Is the only area of the heart capable of spontaneous depolarization c. Has rich sympathetic innervation via the vagus nerve d. Depolarizes more rapidly than other automatic cells of the heart ANS: D The electrical impulse normally begins in the SA node because its cells depolarize more rapidly than other automatic cells. Cardiac impulses occur in the SA node because its cells depolarize more rapidly than other automatic cells, not because of its superior location. Cardiac impulses occur in the SA node because its cells depolarize more rapidly than other automatic cells. The SA node is not the only area of the heart capable of spontaneous depolarization. Cardiac impulses occur in the SA node because its cells depolarize more rapidly than other automatic cells. It does have rich innervations, but by parasympathetic innervation from the vagus nerve. Cognitive Level: Comprehension 557 22. A 28-year-old female with seizure disorder has a vagus nerve stimulator implanted to help control seizure activity. Which of the following would the nurse also expect to occur? a. Increased speed of cardiac cycle b. Increased cardiac contractility c. Decreased vasodilation d. Decreased cardiac conduction ANS: D The vagus nerve releases acetylcholine. Acetylcholine causes decreased heart rate and slows conduction through the atrioventricular (AV) node. The vagus nerve releases acetylcholine. Acetylcholine causes decreased heart rate and slows conduction through the AV node, thus decreasing speed of the cardiac cycle. The vagus nerve releases acetylcholine. Acetylcholine causes decreased heart rate and slows conduction through the AV node, decreasing contractility. The vagus nerve releases acetylcholine. Acetylcholine causes decreased heart rate and slows conduction through the AV node; it does not cause vasodilation. Cognitive Level: Comprehension 560 23. A new drug is released to aid in weight loss. It stimulates the sympathetic system. The nurse monitors for an increased heart rate. The sympathetic system causes this by: a. Inhibiting the release of catecholamines b. Altering the threshold potential c. Decreasing the conduction time through the atrioventricular (AV) node d. Increasing the influx of calcium ANS: B The sympathetic system increases heart rate by altering the threshold potential. The sympathetic system increases heart rate by altering the threshold potential. It does not inhibit the release of catecholamines. The sympathetic system increases heart rate by altering the threshold potential. It does not decrease conduction through the AV node. The sympathetic system increases heart rate by altering the threshold potential. It does not increase the influx of calcium. Cognitive Level: Comprehension 560 24. A nurse assesses the heart after acetylcholine because the effect of acetylcholine on the heart is to: a. Decrease the refractory period b. Increase calcium influx c. Increase the strength of myocardial contraction d. Decrease the heart rate ANS: D Acetylcholine causes decreased heart rate and slows conduction through the atrioventricular (AV) node. Acetylcholine causes decreased heart rate and slows conduction through the AV node; it does not decrease the refractory period. It decreases calcium influx. Acetylcholine causes decreased heart rate and slows conduction through the AV node; it does not increase the strength of myocardial contraction. Cognitive Level: Comprehension 560 25. To help a nursing student differentiate cardiac muscle from skeletal muscle, which characteristic should the nurse use? One difference between cardiac muscle and skeletal muscle is that: a. Cardiac muscle cells are arranged in branching networks. b. Skeletal muscle cells have only one nucleus. c. Cardiac muscle cells appear striped. d. Skeletal muscle cells contain sarcomeres. ANS: A Cardiac cells are arranged in branching networks throughout the myocardium, whereas skeletal muscle cells tend to be arranged in parallel units throughout the length of the muscle. Cardiac muscle cells have only one nucleus, whereas skeletal muscle cells have many nuclei. Both cardiac and muscle cells appear striped. Both cardiac and muscle cells contain sarcomeres. Cognitive Level: Comprehension 560 26. A cardiologist is teaching about myocardial cells. Which information should the cardiologist include? are thickened areas of the sarcolemma of myocardial cells that enable electrical impulses to travel in a continuous cell-to-cell fashion. a. Myosins b. Intercalated disks c. Troponin Ts d. I bands ANS: B Intercalated discs allow electrical impulses to be transmitted rapidly from cardiac fiber to cardiac fiber because the network of fibers is connected at these discs. Myosins are filaments that are a part of cardiac tissue. They do not play a role in conduction. Troponin Ts are involved in contraction, but are not part of the sarcolemma. I bands are a part of the filaments bud, which do not conduct impulses in a cell-to-cell fashion. Cognitive Level: Comprehension 560 27. is the process by which an action potential in the plasma membrane of a myocardial cell triggers the events that directly cause contraction of the myocardial cells. a. Electrocontraction b. Intercalated communication c. Excitation-contraction coupling d. Myosin communication ANS: C Excitation-contraction coupling is the process by which an action potential in the plasma membrane of the muscle fiber triggers the cycle, leading to cross-bridge activity and contraction. Excitation-contraction coupling, not electrocontraction, is the process by which an action potential in the plasma membrane of the muscle fiber triggers the cycle, leading to cross-bridge activity and contraction. Excitation-contraction coupling, not intercalated communication, is the process by which an action potential in the plasma membrane of the muscle fiber triggers the cycle, leading to cross- bridge activity and contraction. Excitation-contraction coupling, not myosin communication, is the process by which an action potential in the plasma membrane of the muscle fiber triggers the cycle, leading to cross-bridge activity and contraction. Cognitive Level: Comprehension 562 28. The molecule that aids in bonding of the troponin complex to actin and tropomyosin is troponin: a. C b. I c. T d. M ANS: C Troponin T aids in the binding of the troponin complex to actin and tropomyosin. Troponin C contains binding sites for the calcium ions involved in contraction. Troponin I inhibits the ATPase of actomyosin. Troponin M is not a substance. Cognitive Level: Comprehension 563 29. A patient has searched on the internet for muscle contractions. Which information indicates a good understanding? Muscle contractions occur when there is a decreased: a. Distance between Z lines b. A band length c. Z line length d. H zone distance ANS: A Anatomically, contraction occurs when the sarcomere shortens, so adjacent Z lines move closer together. Anatomically, contraction occurs when the sarcomere shortens, so adjacent Z lines move closer together, not a decrease in A band length. Anatomically, contraction occurs when the sarcomere shortens, so adjacent Z lines move closer together, not a decrease in Z line length. Anatomically, contraction occurs when the sarcomere shortens, so adjacent Z lines move closer together, not a decrease in H zone distance. Cognitive Level: Comprehension 561 30. A nurse is discussing the pressure generated at the end of diastole. Which term is the nurse describing? a. Preload b. Afterload c. Systemic vascular resistance d. Total peripheral resistance ANS: B Preload is the volume and associated pressure generated in the ventricle at the end of diastole. B Preload, not afterload, is the volume and associated pressure generated in the ventricle at the end of diastole. Afterload is the resistance to ejection of blood from the left ventricle. Systemic vascular resistance is related to afterload. Total peripheral resistance increases afterload. Cognitive Level: Comprehension 563 31. Which principle should the nurse remember when planning nursing care for a patient with heart problems? As stated by the Frank-Starling law, there is a direct relationship between the of the blood in the heart at the end of diastole and the _ of contraction during the next systole. a. Pressure, duration b. Volume, force c. Viscosity, force d. Viscosity, duration ANS: B The Frank-Starling law of the heart describes the length-tension relationship of ventricular end- diastolic volume (VEDV) (preload) to myocardial contractility (as measured by stroke volume). The Frank-Starling law of the heart describes the length-tension relationship of VEDV (preload) to myocardial contractility (as measured by stroke volume). It does not refer to duration. The Frank-Starling law of the heart describes the length-tension relationship of VEDV (preload) to myocardial contractility (as measured by stroke volume). It does not refer to viscosity. The Frank-Starling law of the heart describes the length-tension relationship of VEDV (preload) to myocardial contractility (as measured by stroke volume). It does not refer to duration. Chapter 26. Alterations of Cardiovascular Function MULTIPLE CHOICE 1. A 60-year-old male presents to his primary care provider reporting chest pain. He is diagnosed with atherosclerosis. This disease is caused by: a. Arterial wall thinning and weakening b. Abnormally dilated arteries and veins c. Abnormal thickening and hardening of vessel walls d. Autonomic nervous system imbalances ANS: C Atherosclerosis is a form of arteriosclerosis characterized by thickening and hardening of the vessel wall. Atherosclerosis is a form of arteriosclerosis characterized by thickening and hardening of the vessel wall. Arteries are thickened, not thinning. Atherosclerosis is a form of arteriosclerosis characterized by thickening and hardening of the vessel wall. Arteries are narrowed, not dilated. Atherosclerosis is a form of arteriosclerosis characterized by thickening and hardening of the vessel wall. It is not related to autonomic nervous system imbalances, which would lead to changes in rate or rhythm. Cognitive Level: Comprehension 594 2. A patient wants to know what causes atherosclerosis. How should the nurse respond? In general, atherosclerosis is caused by: a. High serum cholesterol levels b. Endothelial injury and inflammation c. An increase in antithrombotic substances d. Congenital heart disease ANS: B Atherosclerosis begins with injury to the endothelial cells that line artery walls. High serum cholesterol levels are associated with atherosclerosis, but are not its cause. Atherosclerosis begins with injury to the endothelial cells that line artery walls. It is not due to an increase in antithrombotic substances. Atherosclerosis begins with injury to the endothelial cells that line artery walls. It is not related to congenital heart disease. Cognitive Level: Comprehension 594 3. A staff member asks a nurse what foam cells are. What is the nurses best response? Foam cells in a fatty streak are: a. Deposited adipose cells b. Injured neutrophils c. Macrophages that engulf low-density lipoprotein (LDL) d. Lipid-laden mast cells ANS: C Foam cells are lipid-laden macrophages that engulf LDL. Foam cells are lipid-laden macrophages that engulf LDL. They are deposited in vessels, not adipose cells. Foam cells are lipid-laden macrophages that engulf LDL. They are not injured neutrophils. Foam cells are lipid-laden macrophages that engulf LDL. They are not mast cells. Cognitive Level: Comprehension 595 4. A nurse takes an adult patients blood pressure and determines it to be normal. What reading did the nurse obtain? a. Systolic pressure between 140 mm Hg and 150 mm Hg b. Systolic pressure less than 120 mm Hg and diastolic pressure less than 80 mm Hg c. Systolic pressure less than 100 mm Hg regardless of diastolic pressure d. Systolic pressure greater than 140 mm Hg and a diastolic pressure of 100 mm Hg ANS: B Normal blood pressure has a systolic pressure less than 120 mm Hg and diastolic pressure less than 80 mm Hg. A systolic pressure of 140 mm Hg or more would indicate stage I hypertension. A systolic pressure of less than 100 mm Hg would indicate low blood pressure. A diastolic pressure greater than 90 mm Hg would indicate hypertension. Cognitive Level: Comprehension 587 5. Most cases of combined systolic and diastolic hypertension have no known cause and are documented on the chart as hypertension. a. Primary b. Secondary c. Congenital d. Acquired ANS: A Most cases of hypertension are diagnosed as primary hypertension. Most cases of hypertension are diagnosed as primary hypertension, not secondary, which is due to a known cause. Most cases of hypertension are diagnosed as primary hypertension, not congenital. Most cases of hypertension are diagnosed as primary hypertension, not acquired. Cognitive Level: Comprehension 587 6. A 30-year-old Caucasian female was recently diagnosed with primary hypertension. She reports that she eats fairly well, usually having red meat and potatoes daily. She also reports that her father has hypertension as well. A nurse determines which of the following risk factors is most likely associated with this diagnosis? a. Race b. Diet c. Age d. Genes ANS: D Genetic factors, such as family history of hypertension, are the number one factor in the development of hypertension. Race is a factor, but genetic factors are primary. Diet is a factor, but genetic factors are primary. Age is a factor, but not in this case; since the patient is 30, genetics are a greater factor. Cognitive Level: Comprehension 587 7. A 65-year-old male presents for a routine checkup. A blood pressure check reveals a systolic pressure of 160 mm Hg and a diastolic pressure of 70 mm Hg. Which of the following is the most likely cause of this type of pressure elevation? a. Vasospasm b. Rigidity of the aorta c. Decreased sodium intake d. Lung disease ANS: B Older adults experience stiffening of the arteries, which could lead to hypertension. A vasospasm could lead to chest pain, not hypertension. Increased sodium intake, not decreased, could lead to increased blood volume and hypertension. Lung disease would not lead to hypertension. Cognitive Level: Comprehension 587 8. A 52-year-old male is diagnosed with primary hypertension. He has no other health problems. Present treatment would cause the nurse to anticipate administering which drug to the patient? a. A beta-adrenergic agonist b. An alpha-adrenergic agonist c. A diuretic d. A calcium channel agonist ANS: C Diuretics have been shown to be the safest and most effective medications for lowering blood pressure and preventing the cardiovascular complications of hypertension. Diuretics have been shown to be the safest and most effective medications for lowering blood pressure and preventing the cardiovascular complications of hypertension. A beta-adrenergic drug would be used for patients with other concurrent health problems. Diuretics have been shown to be the safest and most effective medications for lowering blood pressure and preventing the cardiovascular complications of hypertension. An alpha-adrenergic drug would be used for patients with other concurrent health problems. Diuretics have been shown to be the safest and most effective medications for lowering blood pressure and preventing the cardiovascular complications of hypertension. A calcium channel agonist drug would be used for patients with other concurrent health problems. Cognitive Level: Comprehension 591 9. A 55-year-old female has undiagnosed hypertension. She presents to her primary care provider reporting impaired vision and chronic edema. Lab tests reveal that she also has renal insufficiency. While planning care, the nurse realizes the most likely cause for these findings is: a. Clotting and gangrene b. Free radical injury and cell toxicity c. End-organ damage d. Hypertrophy and hyperplasia ANS: C The patient is experiencing end-organ damage, as indicated by renal insufficiency. The patient is not experiencing gangrene, but end-organ damage. The patient is experiencing end-organ damage; it is not due to the formation of free radicals. Hypertrophy and hyperplasia could develop, but the cause of the patients symptoms is end-organ damage. Cognitive Level: Comprehension 590 10. A nurse monitors the patient for when rapid onset of malignant hypertension results. a. Atherosclerosis b. Encephalopathy c. Pulmonary edema d. Acute renal failure ANS: B Malignant hypertension leads to cerebral edema and cerebral dysfunction (encephalopathy) and even death. Malignant hypertension leads to cerebral edema; atherosclerosis does not. Malignant hypertension could lead to heart failure, which could lead to pulmonary edema, but encephalopathy occurs more frequently. Malignant hypertension could lead to heart failure, which could lead to renal failure, but encephalopathy occurs more frequently. Cognitive Level: Comprehension 590 11. When a nurse checks the patient for orthostatic hypotension, what did the nurse have the patient do? a. Physical exertion b. Eat c. Stand up d. Lie down ANS: C Orthostatic hypotension refers to a drop in blood pressure when standing up. Orthostatic hypotension refers to a drop in blood pressure when standing up, not a drop with exertion. Orthostatic hypotension refers to a drop in blood pressure when standing up, not a drop with eating. Orthostatic hypotension refers to a drop in blood pressure when standing up, not with lying down. Cognitive Level: Comprehension 591 12. A 50-year-old male is diagnosed with orthostatic hypotension. Which of the following symptoms would he most likely experience? a. Headache and blurred vision b. Nausea and vomiting c. Chest pain and palpitations d. Syncope and fainting ANS: D Orthostatic hypotension is often accompanied by dizziness, blurring or loss of vision, and syncope or fainting. Orthostatic hypotension is often accompanied by dizziness, blurring or loss of vision, and syncope or fainting, not by headache or blurred vision, which are symptoms of hypertension. Orthostatic hypotension is often accompanied by dizziness, blurring or loss of vision, and syncope or fainting, not nausea and vomiting. Orthostatic hypotension is often accompanied by dizziness, blurring or loss of vision, and syncope or fainting, not chest pain and palpitations, which may be symptomatic of myocardial infarction. Cognitive Level: Comprehension 591 13. A 65-year-old female presents to the emergency department reporting difficulty swallowing and shortness of breath. A CT scan would most likely reveal an aneurysm in the: a. Cerebral vessels b. Renal arteries c. Inferior vena cava d. Thoracic aorta ANS: D Thoracic aortic aneurysms can cause dysphagia (difficulty swallowing) and dyspnea (breathlessness). Aneurysms in cerebral vessels will produce a headache. Aneurysms in the renal arteries will produce flank pain. Aneurysms in the inferior vena cava may produce chest pain. Cognitive Level: Comprehension 592 14. A 60-year-old male is diagnosed with cerebral aneurysm. Where does the nurse suspect the cerebral aneurysm is located? a. Vertebral arteries b. Basilar artery c. Circle of Willis d. Carotid arteries ANS: C Cerebral aneurysms often occur in the circle of Willis. Cerebral aneurysms often occur in the circle of Willis, not the vertebral arteries. Cerebral aneurysms often occur in the circle of Willis, not the basilar artery. Cerebral aneurysms often occur in the circle of Willis, not the carotid arteries. Cognitive Level: Comprehension 592 15. What term should the nurse document for a detached blood clot? a. Thrombus b. Embolus c. Thromboembolus d. Infarction ANS: C A detached thrombus is a thromboembolus. A thrombus is a clot that remains attached to a vessel wall; a detached thrombus is a thromboembolus. An embolus is a bolus of material floating in the blood stream; a detached thrombus is a thromboembolus. An infarction is death of tissue; a detached thrombus is a thromboembolus. Cognitive Level: Comprehension 593 16. A 32-year-old female presents with lower leg pain, with swelling and redness. While obtaining the patients history, which finding could have caused her condition? a. Venous thrombus b. Heart valve damage c. Bacterial infection d. Atherosclerosis ANS: A A thrombus formation in the vein leads to inflammation that may cause pain and redness with obstruction. Increased pressure in the vein behind the clot may lead to edema of the extremity. Heart valve damage may lead to thrombus, but it is not the cause of the patients symptoms. The patient is experiencing a venous thrombus that leads to the swelling, redness, and pain. A bacterial infection would not cause these localized specific symptoms. Atherosclerosis causes narrowing, primarily of arteries, but this is a venous thrombus that is causing the patients symptoms. REF: pp. 592-593 17. A 28-year-old female presents with severe chest pain and shortness of breath. She is diagnosed with pulmonary embolism, which most likely originated from the: a. Left ventricle b. Systemic arteries c. Deep veins of the leg d. Superficial veins of the arm ANS: C The most likely origin of the embolism is from the deep veins of the legs. The most likely origin of the embolism is from the deep veins of the legs, not from the left ventricle. The most likely origin of the embolism is from the deep veins of the legs, not the systemic arteries. The most likely origin of the embolism is from the deep veins of the legs, not from the arms. Cognitive Level: Comprehension 593 18. Individuals with Raynaud disease need to be counseled to avoid which of the following conditions to prevent severe symptoms? a. Allergic reactions b. Cold exposure c. Hot water immersion d. Tissue injury ANS: B Raynaud disease consists of vasospastic attacks triggered by brief exposure to cold. Raynaud disease demonstrates symptoms when extremities are exposed to cold. It is not an allergic reaction. Raynaud disease demonstrates symptoms when extremities are exposed to cold. It is not due to hot water immersion. Raynaud disease demonstrates symptoms when extremities are exposed to cold. It is not the result of tissue injury. Cognitive Level: Comprehension 594 19. A 75-year-old obese female presents to her primary care provider reporting edema in the lower extremities. Physical exam reveals that she has varicose veins. Upon performing the history, which of the following is a possible cause for the varicose veins? a. Extreme exercise b. Long periods of standing c. Trauma to the deep veins d. Ischemia ANS: B The probable cause of the patients varicose veins is gradual venous distention caused by the action of gravity on blood in the legs due to long periods of standing. Varicose veins are most likely due to long periods of standing leading to the action of gravity promoting venous distention. Exercise would help prevent this. Trauma can occur, but usually this affects the more superficial veins. Ischemia affects arteries not veins. Cognitive Level: Comprehension 585 20. A 52-year-old male presents with pooling of blood in the veins of the lower extremities and edema. The diagnosis is chronic venous insufficiency, and an expected assessment finding of this disorder is: a. Deep vein thrombus formation b. Skin hyperpigmentation c. Gangrene d. Edema above the knee ANS: B Symptoms include edema of the lower extremities and hyperpigmentation of the skin of the feet and ankles. Edema in these areas may extend to the knees. Symptoms include edema and hyperpigmentation of the skin, but deep vein thrombi do not form. Gangrene does not occur in veins, but in arteries. Edema does not occur above the knee. Cognitive Level: Comprehension 586 21. While planning care for a patient with superior vena cava syndrome (SVCS), which principle should the nurse remember? SVCS is a progressive of the superior vena cava (SVC) that leads to venous distention of the upper extremities and head. a. Inflammation b. Occlusion c. Distention d. Sclerosis ANS: B SVCS is a progressive occlusion of the SVC that leads to venous distention in the upper extremities and head. SVCS is a progressive occlusion, not inflammation, of the SVC that leads to venous distention in the upper extremities and head. SVCS is a progressive occlusion, not distention, of the SVC that leads to venous distention in the upper extremities and head. SVCS is a progressive occlusion, not sclerosis, of the SVC that leads to venous distention in the upper extremities and head. Cognitive Level: Comprehension 586 22. A 50-year-old male with a 30-year history of smoking was diagnosed with bronchogenic cancer. He developed edema and venous distention in the upper extremities and face. Which of the following diagnosis will the nurse observe on the chart? a. Thromboembolism b. Deep vein thrombosis c. Superior vena cava syndrome (SVCS) d. Chronic venous insufficiency ANS: C SVCS is a progressive occlusion of the superior vena cava that leads to venous distention in the upper extremities and head. Thromboembolism would not lead to the generalized symptoms described in the patient. Deep vein thrombosis would not lead to upper extremity symptoms. Chronic venous insufficiency would primarily affect one extremity. Cognitive Level: Comprehension 586 23. A 52-year-old female is diagnosed with coronary artery disease. The nurse assesses for myocardial: a. Hypertrophy b. Ischemia c. Necrosis d. Inflammation ANS: B Coronary artery disease leads to myocardial ischemia. Coronary artery disease would not lead to hypertrophy, but to ischemia. Coronary artery disease can contribute to necrosis, but obstruction by a clot would more likely lead to necrosis. Coronary artery disease would lead to myocardial ischemia, not inflammation. Cognitive Level: Comprehension 587 24. A 56-year-old male is diagnosed with coronary artery disease. Which of the following modifiable risk factors would the nurse suggest the patient change? a. Eating meat b. Living arrangements c. Drinking tomato juice d. Smoking cigarettes ANS: D Cigarette smoking leads to vasoconstriction and should be the first behavior the patient changes. Eating meat alone would not lead to the development of coronary artery disease; cigarette smoking leads to vasoconstriction and should be the first behavior the patient changes. The living arrangement of the patients home would not lead to the development of coronary artery disease; cigarette smoking leads to vasoconstriction and should be the first behavior the patient changes. Drinking tomato juice would not lead to the development of coronary artery disease; cigarette smoking leads to vasoconstriction and should be the first behavior the patient changes. Cognitive Level: Comprehension 594 25. A 50-year-old obese male with hypertension and coronary artery disease visits a nutritionist for food counseling. He has an elevated level of low-density lipoprotein (LDL) and a low level of high-density lipoprotein (HDL). Which of the following should the nurse advise him to avoid? a. Monounsaturated fats b. Polyunsaturated fats c. Saturated fats d. Trans fats ANS: D Trans fats are primarily found in artificially solidified (hydrogenated) oils (e.g., margarine and vegetable shortening). By becoming more solid, they lose essential fatty acids (EFAs). They can raise LDL and lower HDL levels. Trans fats, not monounsaturated fats, are primarily found in artificially solidified (hydrogenated) oils (e.g., margarine and vegetable shortening). By becoming more solid, they lose EFAs. They can raise LDL and lower HDL levels. Trans fats, not polyunsaturated fats, are primarily found in artificially solidified (hydrogenated) oils (e.g., margarine and vegetable shortening). By becoming more solid, they lose EFAs. They can raise LDL and lower HDL levels. Trans fats, not saturated fats, are primarily found in artificially solidified (hydrogenated) oils (e.g., margarine and vegetable shortening). By becoming more solid, they lose EFAs. They can raise LDL and lower HDL levels. Cognitive Level: Comprehension 598 26. When a patient asks the nurse what is the most common cause of myocardial ischemia, which statement is the correct response? The most common cause of myocardial ischemia is: a. Idiopathic vasospasm b. Arterial emboli from heart valve c. Atherosclerosis d. Venous emboli ANS: C The most common cause of myocardial ischemia is atherosclerosis. Atherosclerosis, not vasospasm, is the major cause of myocardial ischemia. Arterial emboli may cause ischemia, but atherosclerosis is the major cause of myocardial ischemia. Venous emboli would not lead to myocardial ischemia; atherosclerosis is the major cause of myocardial ischemia. Cognitive Level: Comprehension 600 27. A 51-year-old male presents with recurrent chest pain on exertion. He is diagnosed with angina pectoris. When he asks what causes the pain, how should the nurse respond? The pain occurs when: a. Cardiac output has fallen below normal levels. b. The myocardial oxygen supply has fallen below demand. c. Myocardial stretch has exceeded the upper limits. d. The vagus nerve is stimulated. ANS: B Angina is chest pain caused by myocardial ischemia, which develops if the flow or oxygen content of coronary blood is insufficient to meet the metabolic demands of myocardial cells. A decrease in cardiac output would lead to general systemic symptoms, not just chest pain, which is due to a decrease in myocardial oxygenation. Myocardial stretch does not affect angina symptoms. When the vagus nerve is stimulated, a change in rate occurs; it does not precipitate chest pain. Cognitive Level: Comprehension 601 28. A 62-year-old male presents to his primary care provider reporting chest pain at rest and with exertion. He does not have a history of coronary artery disease and reports that the pain often occurs at night. He is most likely experiencing which type of angina? a. Unstable b. Stable c. Prinzmetal d. Silent ANS: C Chest pain that occurs at rest and at night is descriptive of Prinzmetal angina. Unstable angina is a form of acute coronary syndrome that results from reversible myocardial ischemia. Stable angina is predictable and occurs with activity. Silent angina has few, if any, symptoms. Cognitive Level: Comprehension 601 29. A 51-year-old male is at the health clinic for an annual physical exam. After walking from the car to the clinic, he developed substernal pain. He also reported discomfort in his left shoulder and his jaw, lasting 2 to 3 minutes and then subsiding with rest. He indicates that this has occurred frequently over the past few months with similar exertion. The nurse suspects he is most likely experiencing: a. Stable angina b. Unstable angina c. Prinzmetal angina d. Myocardial infarction (MI) ANS: A Stable angina is associated with activity and subsides with rest. Unstable angina is a form of acute coronary syndrome that results from reversible myocardial ischemia and occurs at rest. Chest pain that occurs at rest and at night is descriptive of Prinzmetal angina. MI pain does not subside with rest. Cognitive Level: Comprehension 601 30. A 49-year-old male presents to his primary care provider reporting chest pain. EKG reveals ST elevation. He is diagnosed with myocardial ischemia. Which of the following interventions would be most beneficial? a. Administer a diuretic to decrease volume. b. Apply oxygen to increase myocardial oxygen supply. c. Encourage exercise to increase heart rate. d. Give an antibiotic to decrease infection. ANS: B Increase myocardial oxygen supply is indicated to treat ischemia. Oxygen is indicated, not a decrease in volume. Heart rate should be decreased to decrease cardiac workload. Antibiotics are not the most beneficial; oxygen is. Cognitive Level: Comprehension 603 31. A 68-year-old male presents to the ER reporting chest pain. He has a history of stable angina that now appears to be unstable. He most likely has: a. Mild to moderate atherosclerosis b. Impending myocardial infarction (MI) c. Electrical conduction problems in the heart d. Decreased myocardial oxygen demand ANS: B Unstable angina is an indication of impending MI. Unstable angina could be caused by moderate atherosclerosis, but it is an indication of impending MI. Unstable angina could be caused by altered electrical conduction, but it is an indication of impending MI. Unstable angina is due to a decrease in myocardial oxygen, but it is an indication of impending MI. Chapter 27. Alterations of Cardiovascular Function in Children MULTIPLE CHOICE 1. An 8-week-old infant presents to his pediatrician for a well-baby checkup. Physical exam reveals a murmur and an echocardiogram confirms a ventricular septal defect. Which of the following genetic factors should the nurse assess for as it would most likely accompany this diagnosis? a. Huntington disease b. Color blindness c. Down syndrome d. Hemophilia ANS: C Down syndrome is the genetic factor that would most likely accompany the diagnosis of a congenital heart defect. Down syndrome, not Huntington disease, is the genetic factor that would most likely accompany a diagnosis of congenital heart defect. Down syndrome, not color blindness, is the genetic factor that would most likely accompany a diagnosis of congenital heart defect. Down syndrome, not hemophilia, is the genetic factor that would most likely accompany a diagnosis of congenital heart defect. Cognitive Level: Comprehension 643 2. A newborn child is diagnosed with tetralogy of Fallot. What symptoms would the nurse expect to observe in the child? a. High-pitched cry and dyspnea b. Cyanosis and hypoxia c. Leg pain and twitching d. Epistaxis and anemia ANS: B The child will experience cyanosis and hypoxia. This type of shunt decreases flow through the pulmonary system, causing less than normal oxygen delivery to the tissues and resultant cyanosis. It will not cause a high-pitched cry. This type of shunt decreases flow through the pulmonary system, causing less than normal oxygen delivery to the tissues and resultant cyanosis. It will not cause leg pain; leg pain occurs in coarctation of the aorta. This type of shunt decreases flow through the pulmonary system, causing less than normal oxygen delivery to the tissues and resultant cyanosis. Epistaxis is associated with coarctation of the aorta. Cognitive Level: Comprehension 649 3. A newborn is diagnosed with congenital heart disease. Which of the following intrauterine factors should the nurse focus on during the history that could have caused this disorder? a. Diabetes b. Alcohol exposure c. Viral infection d. Dextroamphetamine ANS: C One of the identified causes of cardiac defects, such as pulmonic stenosis, is maternal conditions, such as intrauterine viral infections, especially rubella. Diabetes contributes to large babies; maternal infection contributes to cardiac abnormalities. Alcohol exposure contributes to abnormalities such as facial changes; maternal conditions, such as intrauterine viral infections, especially rubella, lead to congenital abnormalities. Medications such as dextroamphetamines lead to other abnormalities; maternal conditions, such as intrauterine viral infections, especially rubella, lead to congenital abnormalities. Cognitive Level: Comprehension 643 4. When a staff member asks what coarctation of the aorta is, how should the nurse respond? Coarctation of the aorta is the local narrowing of the aorta near the: a. Aortic valve b. Ductus arteriosus c. Diaphragm d. Bifurcation into the common iliac arteries ANS: B Coarctation of the aorta is narrowing of the aorta near the ductus arteriosus. Coarctation of the aorta is narrowing of the aorta near the ductus arteriosus, not the aortic valve. Coarctation of the aorta is narrowing of the aorta near the ductus arteriosus, not the diaphragm. Coarctation of the aorta is narrowing of the aorta near the ductus arteriosus, not the bifurcation site. Cognitive Level: Comprehension 644 5. A newborn is suspected of having coarctation of the aorta. Which of the following assessments would aid in diagnosis? a. Cyanosis b. Bounding pedal pulses c. Cool arms d. Weak or absent femoral pulses ANS: D The newborn will have weak or absent femoral pulses because blood flow is obstructed near the lower extremities. The newborn will have weak or absent femoral pulses because blood flow is obstructed near the lower extremities. Coarctation is not a cyanotic defect. The newborn will have weak or absent femoral pulses because blood flow is obstructed near the lower extremities, not bounding pedal pulses. The newborn will have weak or absent femoral pulses because blood flow is obstructed near the lower extremities. The infant will have warm arms because blood flow is present in the upper extremities. Cognitive Level: Comprehension 644 6. A 1-month-old infant visits his primary care provider for a well-baby check. Physical exam reveals decreased cardiac output, hypotension, tachycardia, and a loud murmur suggestive of aortic stenosis. Which of the following would be expected with this diagnosis? a. Atrial dilation b. Ventricular hypertrophy c. Atrial rigidity d. Decreased contractility ANS: B The infant with aortic stenosis will also be experiencing ventricular hypertrophy because of the resistance of blood flow from the left ventricle into the aorta. Ventricular hypertrophy will occur, not atrial dilation. Ventricular hypertrophy will occur, not atrial rigidity. Ventricular hypertrophy will occur, not decreased contractility. Cognitive Level: Comprehension 646 7. A newborn develops a murmur and cyanosis shortly after birth. She is diagnosed with pulmonic stenosis (PS) after an echocardiogram revealed narrowing of the pulmonary: a. Tree b. Artery c. Valve orifice d. Vein ANS: C PS is a narrowing or stricture of the pulmonary valve causing resistance to blood flow from the right ventricle to the pulmonary artery. PS is a narrowing or stricture of the pulmonary valve, not the pulmonary tree, causing resistance to blood flow from the right ventricle to the pulmonary artery. PS is a narrowing or stricture of the pulmonary valve, not the pulmonary artery, causing resistance to blood flow from the right ventricle to the pulmonary artery. PS is a narrowing or stricture of the pulmonary valve, not the vein, causing resistance to blood flow from the right ventricle to the pulmonary artery. Cognitive Level: Comprehension 647 8. When a staff member asks what the patent opening between the aorta and pulmonary artery in a fetus is called, how should the nurse reply? It is the: a. Foramen ovale b. Sinus venosus c. Ductus arteriosus d. Septal defect ANS: C In the fetal circulation, the ductus arteriosus is an opening between the aorta and the pulmonary artery. The foramen ovale allows flow of blood between the left and right atrium. The sinus venosus is a type of atrial septal defect. The septal defect is an opening in the septum. Cognitive Level: Comprehension 647 9. A 2-week-old infant presents with poor feeding, fatigue, dyspnea, and a murmur. She is diagnosed with a patent ductus arteriosus (PDA). A nurse recalls this condition results in a(n): a. Decreased pulmonary blood flow b. Right-to-left shunt c. Left-to-right shunt d. Increased systemic blood flow ANS: C PDA is failure of the fetal ductus arteriosus to close. The continued patency of this vessel allows blood to flow from the higher-pressure aorta to the lower-pressure pulmonary artery, causing a left-to-right shunt. PDA is failure of the fetal ductus arteriosus to close. The continued patency of this vessel allows blood to flow from the higher-pressure aorta to the lower-pressure pulmonary artery, causing a left-to-right shunt. It does not cause decreased pulmonary blood flow PDA is failure of the fetal ductus arteriosus to close. The continued patency of this vessel allows blood to flow from the higher-pressure aorta to the lower-pressure pulmonary artery, causing a left-to-right shunt. PDA is failure of the fetal ductus arteriosus to close. The continued patency of this vessel allows blood to flow from the higher-pressure aorta to the lower-pressure pulmonary artery, causing a left-to-right shunt. It could decrease systemic blood flow, not increase it. Cognitive Level: Comprehension 647 10. An infant undergoes an echocardiogram for a suspected heart defect. Tests reveal an opening in the middle of the atrial septum. What term would the nurse use to describe this defect? a. Ostium primum atrial septal defect (ASD) b. Ostium secundum ASD c. Sinus venosus ASD d. Eisenmenger syndrome ANS: B An opening in the middle of the atrial septum is referred to as an ostium secundum ASD. An ostium primum ASD is an opening low in the atrial septum and may be associated with abnormalities of the mitral valve. A sinus venosus ASD is an opening usually high in the atrial wall and may be associated with partial anomalous pulmonary venous connection. Eisenmenger syndrome is a condition in which shunting of blood is reversed because of high pulmonary pressure and resistance. Cognitive Level: Comprehension 648 11. Which is the most common type of congenital heart defect the nurse should assess for in infants? a. Atrial septal defect (ASD) b. Ventricular septal defect (VSD) c. Tetralogy of Fallot d. Atrioventricular canal defect ANS: B The most common type of congenital heart defect is a VSD. The most common type of congenital heart defect is a VSD, not an ASD. The most common type of congenital heart defect is a VSD, not tetralogy of Fallot. The most common type of congenital heart defect is a VSD, not atrioventricular canal defect. Cognitive Level: Comprehension 648 12. An 8-week-old infant presents to her primary care provider for a well-baby check. Physical exam reveals a murmur, and an echocardiogram shows a large ventricular septal defect. If left untreated, what condition should the nurse discuss with the parents? a. Pulmonary hypertension b. Cyanosis c. Dysrhythmias d. Valve damage ANS: A If the degree of shunting is significant and not corrected, the child is at risk for developing pulmonary hypertension. If the degree of shunting is significant and not corrected, the child is at risk for developing pulmonary hypertension. Cyanosis is not present at first if the shift is left to right. If the degree of shunting is significant and not corrected, the child is at risk for developing pulmonary hypertension. Dysrhythmias do not occur. If the degree of shunting is significant and not corrected, the child is at risk for developing pulmonary hypertension. The defect does not lead to valve damage. Cognitive Level: Comprehension 648 13. A 22-year-old pregnant woman presents to her OB/GYN for a prenatal checkup. The heartbeat sounds irregular, and a fetal echocardiogram reveals an atrioventricular canal (AVC) defect. This defect is the result of: a. Failure of the ductus arteriosus to close b. Fusion of the endocardial cushions c. A patent foramen ovale d. A right-to-left shunt ANS: B AVC defect is the result of incomplete fusion of endocardial cushions. A patent ductus is the failure of the ductus arteriosus to close. The infant will not experience a patent foramen ovale. Flow is generally left to right, not right to left. Cognitive Level: Comprehension 649 14. A newborn experiences frequent periods of cyanosis, usually occurring during crying or after feeding. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Atrioventricular canal (AVC) defect b. Ventricular septal defect (VSD) c. Tetralogy of Fallot d. Atrial septal defect (ASD) ANS: C Infants with tetralogy of Fallot experience cyanosis after crying or during feeding. Infants with AVC defect may experience cyanosis, but it is not related to feeding or crying. Infants with a VSD do not experience cyanosis. Infants with an ASD do not experience cyanosis. Cognitive Level: Comprehension 649 15. A newborn child has a murmur and cyanosis. An echocardiogram reveals that the tricuspid valve failed to develop and no blood flows between the right atrium and ventricle. What term will the nurse use to describe this condition? Tricuspid: a. Regurgitation b. Stenosis c. Atresia d. Transposition ANS: C Tricuspid atresia is failure of the tricuspid valve to develop; consequently, there is no communication from the right atrium to the right ventricle. In regurgitation, blood moves backwards, but is not obstructed. In stenosis, blood flow is narrowed, but not totally obstructed. In transposition, the two great vessels are on opposite sides. Cognitive Level: Comprehension 649 16. When the pediatrician cardiologist discusses total anomalous pulmonary venous connection, which of the following statements BEST describes this condition? a. The foramen ovale closes after birth. b. Pulmonary venous return is to the right atrium. c. Pulmonary venous return is to the left atrium. d. The foramen ovale does not close. ANS: B The pulmonary venous return is connected to the right side of the circulation, rather than to the left atrium. The pulmonary venous return is connected to the right side of the circulation, rather than to the left atrium. It does not include closure of the foramen ovale after birth. The pulmonary venous return is connected to the right side of the circulation, rather than to the left atrium. The pulmonary venous return is connected to the right side of the circulation, rather than to the left atrium. It does not involve closure of the foramen ovale. Cognitive Level: Comprehension 662 17. A newborn baby is severely cyanotic. An echocardiogram reveals transposition of the great arteries. A nurse assesses for which of the following, as it usually occurs with this defect? a. The pulmonary artery leaving the right ventricle b. The aorta leaving the right ventricle c. Ventricular septal defect (VSD) d. Atrial septal defect (ASD) ANS: B In transposition of the great arteries, the pulmonary artery leaves the left ventricle and the aorta exits from the right ventricle. The pulmonary artery normally leaves the right ventricle. A VSD is not associated with transposition of the great arteries. An ASD is not associated with transposition of the great arteries. Cognitive Level: Comprehension 651 18. A 1-month-old infant was diagnosed with truncus arteriosus (TA) with a ventricular septal defect. Which of the following would the nurse also expect? a. Hypertrophy of the aorta and major arteries b. Transposition of the aorta and the pulmonary trunk c. The aorta returning blood to the right atrium d. Blood from both ventricles mixing in a common vessel ANS: D TA is failure of normal separation and division of the embryonic outflow track into a pulmonary artery and an aorta, resulting in a single vessel that exits the heart. TA is failure of normal separation and division of the embryonic outflow track into a pulmonary artery and an aorta, resulting in a single vessel that exits the heart. It does not involve hypertrophy of the aorta. TA is failure of normal separation and division of the embryonic outflow track into a pulmonary artery and an aorta, resulting in a single vessel that exits the heart. It does not involve transposition of the aorta. TA is failure of normal separation and division of the embryonic outflow track into a pulmonary artery and an aorta, resulting in a single vessel that exits the heart. It does not involve the aorta returning blood to the right atrium. Cognitive Level: Comprehension 652 19. A 22-year-old pregnant female presents for a fetal echocardiogram. Tests reveal small left atrium and mitral valve and an absent left ventricle and aortic valve. The diagnosis is hypoplastic left heart syndrome (HLHS). The nurse will anticipate that the treatment for this defect is: a. An indication for neonatal heart transplant b. Rarely fatal c. Easily repaired d. Asymptomatic ANS: A Treatment of HLHS is heart surgery and the possibility of a heart transplant. The disorder is often fatal. Repair of the disorder requires multiple progressive surgeries. Symptoms of the disorder includes mild cyanosis, tachypnea, and low cardiac output. Cognitive Level: Comprehension 653 20. A 1-year-old female with a ventricular septal defect is experiencing left-sided heart failure. Which of the following symptoms will most likely occur? a. Failure to thrive and periorbital edema b. Edema to the hands and feet c. Weight loss and jaundice d. Flat neck veins and increased urinary output ANS: A Left heart failure in infants is manifested as poor feeding and sucking, often leading to failure to thrive and periorbital edema. Left heart failure in infants is manifested as poor feeding and sucking, often leading to failure to thrive. Peripheral edema is a sign of right-sided failure. Weight loss can occur, but not jaundice. Flat neck veins and increased urinary output are not symptomatic of failure. Cognitive Level: Comprehension 654 21. A 3-year-old male is diagnosed with Kawasaki disease. Which of the following does the nurse suspect is the most likely cause? a. A genetic defect causing left heart failure b. Autoimmune injury to the lymphatic vessels c. Infectious pericarditis d. Inflammation of the small capillaries, arteries, and veins ANS: D Kawasaki disease is related to inflammation of small capillaries. Kawasaki disease is due to inflammation, not a genetic defect. Kawasaki disease is due to inflammation, not an autoimmune disease. Kawasaki disease is due to inflammation, not infectious pericarditis. Cognitive Level: Comprehension 654 22. A 5-year-old female is found to have hypertension during three separate visits to her primary care provider. The nurse would expect tests to suggest that the hypertension is secondary to: a. Renal disease b. Brain tumor c. Hypocalcemia d. Hyponatremia ANS: A Hypertension in a 5-year-old is related to renal disease. Hypertension in a 5-year-old is related to renal disease, not a brain tumor. Hypertension in a 5-year-old is related to renal disease, not hypocalcemia. Hypertension in a 5-year-old is related to renal disease, not hyponatremia. Cognitive Level: Comprehension 655 MULTIPLE RESPONSE 1. A 40-year-old pregnant woman is concerned about the health of her unborn child. She has phenylketonuria (PKU) and recently had a viral infection. If the child is born with a congenital heart defect, which of the following is the most likely based on the mothers history? (Select all that apply.) a. Coarctation of aorta b. Pulmonic stenosis c. Ventricular septal defect d. Patent ductus arteriosus e. Tetralogy of Fallot ANS: A, D Coarctation of the aorta and patent ductus arteriosus are the disorders found in infants of mothers with PKU. Cognitive Level: Comprehension 644 2. A newborn child is diagnosed with trisomy 18. Which of the following congenital heart defects should the nurse assess for in the infant? (Select all that apply.) a. Patent ductus b. Coarctation of the aorta c. Atrioventricular canal defect d. Ventricular septal defect e. Pulmonary stenosis ANS: A, D, E The infant with trisomy 18 could present with a ventricular septal defect, a patent ductus, or pulmonary stenosis. Chapter 28. Structure and Function of the Pulmonary System MULTIPLE CHOICE 1. The nasopharynx is lined with a ciliated mucosal membrane with a highly vascular blood supply. The nurse is discussing the functions of this membrane. Which information should be included? One function of the membrane is to: a. Absorb air b. Humidify air c. Cool air d. Exchange gases ANS: B These structures are lined with a ciliated mucosa that warms and humidifies inspired air and removes foreign particles from it. Air is not absorbed, it is humidified. Air is warmed, not cooled. Gas exchange occurs in the alveoli. Cognitive Level: Comprehension 659 2. The nurse is describing the slit-shaped space between the true vocal cords. What term should the nurse use? a. Glottis b. Epiglottis c. Larynx d. Carina ANS: A The slit-shaped space between the true vocal cords forms the glottis. The slit-shaped space between the true vocal cords forms the glottis, not the epiglottis. The slit-shaped space between the true vocal cords forms the glottis, not the larynx. The slit-shaped space between the true vocal cords forms the glottis, not the carina. Cognitive Level: Comprehension 659 3. After entering a room of chemical fog, a 20-year-old male cannot stop sneezing. Which of the following structures is primarily responsible for his sneezing? a. Upper respiratory tract mucosa b. Irritant receptors in the trachea and large airways c. Irritant receptors in the nostrils d. Upper respiratory nasal hairs and turbinates ANS: C The irritant receptors in the nostrils are responsible for sneezing. The irritant receptors in the nostrils are responsible for sneezing, not the upper respiratory tract mucosa. The irritant receptors in the nostrils are responsible for sneezing, not those in the trachea. The irritant receptors in the nostrils are responsible for sneezing, not the turbinates. Cognitive Level: Comprehension 660 4. A newborn is in respiratory distress and requires ventilation. Tests reveal that he does not produce surfactant due to the absence of: a. Mucus-producing cells b. Type II alveolar cells c. Alveolar macrophages d. Goblet cells ANS: B Surfactant is produced by the type II alveolar cells. Surfactant is produced by the type II alveolar cells, not mucus-producing cells. Surfactant is produced by the type II alveolar cells, not alveolar macrophages. Surfactant is produced by the type II alveolar cells, not goblet cells. Cognitive Level: Comprehension 663 5. The nurse is describing the movement of blood into and out of the capillary beds of the lungs to the body organs and tissues. What term should the nurse use to describe this process? a. Perfusion b. Ventilation c. Diffusion d. Circulation ANS: A Perfusion is the movement of blood into and out of the capillary beds of the lungs to body organs and tissues. Ventilation is the movement of air into and out of the lungs. Diffusion is the movement of gases between air spaces in the lungs and the bloodstream. Circulation is the movement of blood throughout the blood stream. Cognitive Level: Comprehension 659 6. Which principle should the nurse remember while planning care for a patient with respiratory problems? Diffusion of respiratory gases takes place at the: a. Alveolocapillary membrane b. Visceral pleurae c. Parietal pleurae d. Respiratory center ANS: B Diffusion of respiratory gases takes place across the alveolocapillary membrane. The visceral pleurae are the linings of the lung; gas exchange does not occur here. The parietal pleurae are the linings of the lung; gas exchange does not occur here. The respiratory center is where impulses to the respiratory muscles are generated. Cognitive Level: Comprehension 672 7. Students in a histology class are assigned to identify regions of the lung. The slide shows a basement membrane, capillary lumen, and macrophages. The students are looking at the: a. Trachea b. Bronchioles c. Alveoli d. Bronchus ANS: C The alveoli contain a basement membrane, a capillary lumen, and macrophages. The trachea does not contain these substances. The bronchioles do not contain these substances. The bronchus does not contain these substances. Cognitive Level: Comprehension 662 8. A nurse recalls the pleural membranes are examples of membranes. a. Mucous b. Serous c. Synovial d. Peritoneal ANS: B The pleural membranes are serous membranes. The pleural membranes are serous membranes, not mucous membranes, which are found in the mouth. The pleural membranes are serous membranes, not synovial, which are found in joints. The pleural membranes are serous membranes, not peritoneal, which are found in the bowel. Cognitive Level: Comprehension 663 9. A nurse is teaching about the functions of the pulmonary system. Which information should the nurse include? One of the functions of the pulmonary system is the: a. Expelling of bacteria b. Exchange of gases between the environment and blood c. Movement of blood into and out of the capillaries d. Principle mechanism for cooling of the heart ANS: B The pulmonary system promotes exchange of gases between the environment and the blood. One of the functions of the pulmonary system is exchange of gases, not the expelling of bacteria. One of the functions of the pulmonary system is exchange of gases, not the movement of blood into and out of the capillaries. One of the functions of the pulmonary system is exchange of gases, not cooling the heart. Cognitive Level: Comprehension 660 10. A 42-year-old male was involved in a motor vehicle accident during which he suffered a severe head injury. He died shortly after the accident from loss of respiration. The nurse suspects the area of the brain most likely involved is the: a. Cerebral cortex b. Thalamus c. Basal ganglia d. Brainstem ANS: D The respiratory center in the brainstem controls respiration by transmitting impulses to the respiratory muscles, causing them to contract and relax. The cerebral cortex does not control respiration. The thalamus does not control respiration. The basal ganglia do not control respiration. Cognitive Level: Comprehension 665 11. The pulmonologist talks about the receptors that respond to increased pulmonary capillary pressure. What term will indicate the nurse understands? They are called: a. Irritant receptors b. Chemoreceptors c. Stretch receptors d. J receptors ANS: D J-receptors (juxtapulmonary capillary receptors) are located near the capillaries in the alveolar septa. They are sensitive to increased pulmonary capillary pressure, which stimulates them to initiate rapid, shallow breathing, hypotension, and bradycardia. The J-receptors respond to capillary changes, not the irritant receptors. The J-receptors respond to capillary changes, not the chemoreceptors. The J-receptors respond to capillary changes, not the stretch receptors. Cognitive Level: Comprehension 665 12. While reviewing the results of the pulmonary functions test, the nurse is aware that the maximum amount of gas that can be displaced (expired) from the lung is called: a. Vital capacity (VC) b. Total lung capacity c. Functional capacity d. Residual volume ANS: A VC is the amount of air that can be forcibly expired after a maximal inspiration. VC is the amount of air that can be forcibly expired after a maximal inspiration. Total lung capacity is the volume of lung capacity at full inhalation. VC is the amount of air that can be forcibly expired after a maximal inspiration. Functional capacity is not a term used to describe function tests. VC is the amount of air that can be forcibly expired after a maximal inspiration. Residual volume is the amount of air remaining after exhalation. Cognitive Level: Comprehension 669 13. The nurse is describing the receptors in the lung that decrease ventilatory rate and volume when stimulated. Which receptors is the nurse discussing? a. Carbon dioxide receptors b. Baroreceptors c. Stretch receptors d. Chemoreceptors ANS: C Stretch receptors decrease ventilatory rate and volume when stimulated. Stretch receptors, not carbon dioxide receptors, decrease ventilatory rate and volume when stimulated. Stretch receptors decrease ventilatory rate and volume when stimulated; baroreceptors regulate blood pressure. Stretch receptors decrease ventilatory rate and volume when stimulated; chemoreceptors increase the rate and depth of respiration. Cognitive Level: Comprehension 666 14. The pulmonologist is presenting a workshop over the lungs. Which information should be included? The lung receives parasympathetic innervation by the nerve. a. Vagus b. Phrenic c. Brachial d. Pectoral ANS: A Parasympathetic innervations for the lung are via the vagus nerve. Parasympathetic innervations for the lung are via the vagus nerve, not the phrenic. Parasympathetic innervations for the lung are via the vagus nerve, not the brachial. Parasympathetic innervations for the lung are via the vagus nerve, not the pectoral. Cognitive Level: Comprehension 666 15. While planning care for a patient with respiratory difficulty and retaining too much carbon dioxide, which principle should the nurse recall? would be stimulated in an attempt to maintain a normal homeostatic state. a. Irritant receptors b. Stretch receptors c. Peripheral chemoreceptors d. Central chemoreceptors ANS: D Chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of cerebrospinal fluid (CSF). The central chemoreceptors are sensitive to very small changes in the pH of CSF and can maintain a normal PaCO2. Chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of CSF. The central chemoreceptors are sensitive to very small changes in the pH of CSF and can maintain a normal PaCO2. Irritant receptors sense the need to expel unwanted substances. Chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of CSF. The central chemoreceptors are sensitive to very small changes in the pH of CSF and can maintain a normal PaCO2. Stretch receptors decrease ventilatory rate and volume when stimulated. Chemoreceptors monitor arterial blood indirectly by sensing changes in the pH of cerebrospinal fluid (CSF). The central chemoreceptors are sensitive to very small changes in the pH of CSF and can maintain a normal PaCO2. The peripheral chemoreceptors become the major stimulus to ventilation when the central chemoreceptors are reset. Cognitive Level: Comprehension 666 16. If an individual with respiratory difficulty were retaining too much carbon dioxide, which of the following compensatory responses would the nurse expect to be initiated? a. Increase in respiratory rate b. Decrease in ventilation rate c. Increase in tidal volume d. Vasodilation of the pulmonary arterioles ANS: A To rid the body of excess carbon dioxide, the rate and depth of respiration are increased. A decrease in ventilation rate would increase carbon dioxide. An increase in tidal volume would not decrease carbon dioxide. Vasodilation of the pulmonary arterioles will not rid the body of carbon dioxide. Cognitive Level: Comprehension 666 17. During inspiration, muscular contraction of the diaphragm causes air to move into the lung. The mechanisms that drive air movement during inspiration are a(n): a. Decrease in intra-alveolar pressure and shortening of the rib cage b. Decrease in the size of the thorax and alveolar expansion c. Increase in the size of the thorax and a decrease in intrapleural pressure d. Increase in atmospheric pressure and intrapleural pressure ANS: C Inspiration occurs due to an increase in the size of the thorax and a decrease in intrapleural pressure. The rib cage lengthens, not shortens. The size of the thorax increases, not decreases. Intrapleural pressure decreases, not increases. Cognitive Level: Comprehension 667 18. A nurse remembers the majority of total airway resistance occurs in the: a. Bronchi b. Nose c. Oral pharynx d. Diaphragm ANS: B One-half to two-thirds of total airway resistance occurs in the nose. One-half to two-thirds of total airway resistance occurs in the nose, not the bronchi. One-half to two-thirds of total airway resistance occurs in the nose, not the oral pharynx. One-half to two-thirds of total airway resistance occurs in the nose, not the diaphragm. Cognitive Level: Comprehension 668 19. The pressure required to inflate an alveolus is inversely related to: a. Wall thickness b. Surface tension c. Minute volume d. Alveolar radius ANS: D The radius of the alveoli is inversely related to the pressure required to inflate it. It is the radius that is related to the pressure, not the wall thickness. It is the radius that is related to the pressure, not the surface tension. It is the radius that is related to the pressure, not the minute volume. Cognitive Level: Comprehension 667 20. An aide asks a nurse how surfactant works. How should the nurse respond? Surfactant facilitates alveolar distention and ventilation by: a. Decreasing thoracic compliance b. Attracting water to the alveolar surface c. Decreasing surface tension in alveoli d. Increasing diffusion in alveoli ANS: C Surfactant decreases surface tension in alveoli, allowing the lungs to inflate. Surfactant decreases surface tension; it does not decrease thoracic compliance. Surfactant decrease surface tension; it does not attract water. Surfactant does not increase diffusion. Cognitive Level: Comprehension 667 21. Which principle should the nurse remember while planning care for a patient with a respiratory problem? Under most circumstances, increased work of breathing results in: a. Increased partial pressure of O2 in the lungs b. Increased oxygen consumption c. Decreased PaCO2 d. Alterations in alveolar perfusion ANS: B An increase in the work of breathing can result in a marked increase in oxygen consumption. An increase in the work of breathing can result in a marked increase in oxygen consumption, not in partial pressure. An increase in the work of breathing can result in a marked increase in oxygen consumption; it may not lower CO2. An increase in the work of breathing can result in a marked increase in oxygen consumption; it would not alter alveolar perfusion. Cognitive Level: Comprehension 669 22. Which of the following terms should the nurse use when there is a balance between outward recoil of the chest wall and inward recoil of lungs at rest? a. Functional residual capacity (FRC) is reached. b. Vital capacity (VC) is reached. c. Total lung capacity (TLC) is reached. d. Residual volume (RV) is reached. ANS: A Balance between the outward recoil of the chest wall and inward recoil of the lungs occurs at the resting level, the end of expiration, where the FRC is reached. VC is the amount of air that can be forcibly expired after a maximal inspiration. TLC is not reflected by outward and inward recoil. RV is the air that remains trapped in the alveoli. Cognitive Level: Comprehension 668 23. What is the partial pressure of oxygen in the lung given the following conditions? Percentage of oxygen in air: 20 Barometric pressure: 700 mm Hg a. 111 mm Hg b. 124 mm Hg c. 131 mm Hg d. 140 mm Hg ANS: D The partial pressure of oxygen is equal to the percentage of oxygen in the air, 20, times the total pressure (700 mm Hg), or 140 mm Hg (700 0.20 = 140). The partial pressure of oxygen is equal to the percentage of oxygen in the air, 20, times the total pressure (700 mm Hg), or 140 mm Hg (700 0.20 = 140). The partial pressure of oxygen is equal to the percentage of oxygen in the air, 20, times the total pressure (700 mm Hg), or 140 mm Hg (700 0.20 = 140). The partial pressure of oxygen is equal to the percentage of oxygen in the air, 20, times the total pressure (700 mm Hg), or 140 mm Hg (700 0.20 = 140). Cognitive Level: Comprehension 670 24. A pulmonologist is discussing the base of the lungs with staff. Which information should be included? At the base of the lungs: a. Alveolar gas pressure exceeds arterial perfusion pressure. b. Arterial perfusion pressure and alveolar gas pressure are less than at the apex. c. Arterial perfusion pressure exceeds alveolar gas pressure. d. Arterial perfusion and alveolar gas pressure are equal. ANS: C In the base of the lungs, both arterial and venous pressures are greater than alveolar pressure, and blood flow is not affected by alveolar pressure. In the base of the lungs, both arterial and venous pressures are greater than alveolar pressure, and blood flow is not affected by alveolar pressure. It is in the apex that alveolar pressure exceeds pulmonary arterial and venous pressures. In the base of the lungs, both arterial and venous pressures are greater than alveolar pressure, and blood flow is not affected by alveolar pressure. It is in the apex that alveolar pressure exceeds pulmonary arterial and venous pressures. In the base of the lungs, both arterial and venous pressures are greater than alveolar pressure, and blood flow is not affected by alveolar pressure. In zone II, also part of the apex, alveolar pressure is greater than venous pressure, but not arterial pressure. Cognitive Level: Comprehension 671 25. While auscultating a patients lungs, a nurse recalls the alveoli in the apexes of the lungs are than alveoli in the bases. a. Larger b. More numerous c. More compliant d. Less perfused ANS: A The alveoli in the upper portions, or apexes, of the lungs contain a greater residual volume of gas and are larger and less numerous than those in the lower portions. The alveoli in the upper portions, or apexes, of the lungs contain a greater residual volume of gas and are larger and less numerous, not more, than those in the lower portions. The alveoli in the upper portions, or apexes, of the lungs contain a greater residual volume of gas and are larger and less numerous than those in the lower portions. The apexes are less compliant. The apexes of the lungs are better perfused. Cognitive Level: Comprehension 671 26. A patient asks how oxygen is transported in the body. What is the nurses best response? Most of the oxygen (O2) is transported: a. Dissolved in the plasma b. Bound to hemoglobin c. In the form of carbon dioxide (CO2) d. As a free-floating molecule ANS: B Most O2 is transported bound to hemoglobin. Most O2 is transported bound to hemoglobin; only a small amount is dissolved in plasma. O2 is not transported in the form of CO2. O2 is transported bound to hemoglobin, not as a free-floating molecule. Cognitive Level: Comprehension 672 27. If a patients hemoglobin concentration (Hb) is 14 g/100 ml and arterial oxygen saturation (SaO2) is 98%, what would be his arterial oxygen content? Remember that 1.34 ml O2 is the maximum amount of oxygen that can be transported per gram of hemoglobin. Hint: O2 content = (1.34 Hb) SaO2 a. 13.72 ml O2 per 100 ml blood b. 15.38 ml O2 per 100 ml blood c. 18.76 ml O2 per 100 ml blood d. 19.30 ml O2 per 100 ml blood ANS: C 18.76 is the product of 14 1.34. 18.76 is the product of 14 1.34. 18.76 is the product of 14 1.34. 18.76 is the product of 14 1.34. Cognitive Level: Comprehension 672 28. In a patient with acidosis or a fever, the nurse would expect the oxyhemoglobin dissociation curve to shift: a. To the right, causing more O2 to be released to the cells b. To the left, allowing less O2 to be released to the cells c. Downward, allowing less O2 to dissolve in the plasma d. Upward, allowing more O2 to dissolve in the plasma ANS: A The oxyhemoglobin dissociation curve is shifted to the right by acidosis (low pH) and hypercapnia (increased PaCO2). The oxyhemoglobin dissociation curve is shifted to the right, not the left, by acidosis (low pH) and hypercapnia (increased PaCO2); more, not less, O2 is released to cells. The oxyhemoglobin dissociation curve is shifted to the right, not downward, by acidosis (low pH) and hypercapnia (increased PaCO2). The oxyhemoglobin dissociation curve is shifted to the right, not upward, by acidosis (low pH) and hypercapnia (increased PaCO2). Cognitive Level: Comprehension 673 29. A patient wants to know how carbon dioxide is transported in the body. How should the nurse respond? Carbon dioxide (CO2) is mainly transported in the blood: a. Attached to oxygen (O2) b. Dissolved in red blood cells c. Combined with albumin d. In the form of bicarbonate ANS: D CO2 is carried in the blood as bicarbonate. CO2 is carried in the blood as bicarbonate, not attached to O2. CO2 is carried in the blood as bicarbonate, not dissolved in red blood cells. CO2 is carried in the blood as bicarbonate, not combined with albumin. Cognitive Level: Comprehension 673 30. A consequence of alveolar hypoxia is: a. Reactive vasodilation b. Local bronchoconstriction c. Decreased respiratory rate d. Pulmonary artery vasoconstriction ANS: D Alveolar hypoxia can result in permanent pulmonary artery vasoconstriction. A consequence of alveolar hypoxia is pulmonary artery vasoconstriction, not reactive vasodilation. A consequence of alveolar hypoxia is pulmonary artery vasoconstriction, not local bronchoconstriction. A consequence of alveolar hypoxia is pulmonary artery vasoconstriction, not a decreased respiratory rate. Cognitive Level: Comprehension 675 31. An 80-year-old male presents to his primary care provider reporting difficulty breathing. Pulmonary function tests reveal that he has increased residual volume. A nurse suspects the most likely cause of this disorder is in lung compliance. a. An increase b. A decrease c. No change d. An absence ANS: A The patient is experiencing an increase in lung compliance. Increased compliance indicates that the lungs or chest wall is abnormally easy to inflate and has lost some elastic recoil. Decreased compliance is seen in acute breathing disorders. The patient will see increased compliance. The patient will see an increase in compliance. Cognitive Level: Comprehension 675 MULTIPLE RESPONSE 1. A nurse is teaching staff about the respiratory bronchi. Which information should the nurse include? may be found in the walls of the respiratory bronchi? (Select all that apply,) a. Smooth muscle b. Surfactant-producing glands c. Goblet cells d. Ciliated cells e. Epithelial lining ANS: A, C, D, E The bronchial walls have three layers: an epithelial lining, a smooth muscle layer, and a connective tissue layer. The epithelial lining of the bronchi contains single-celled exocrine glandsthe mucus-secreting goblet cellsand ciliated cells. Surfactant-producing glands are found in the alveoli. Cognitive Level: Comprehension 600 COMPLETION 1. seconds is required for oxygen (O2) concentration to equilibrate (equalize) across the alveolocapillary membrane. ANS: .25 Cognitive Level: Comprehension 672 2. % of oxygen (O2) enters the bloodstream bound to hemoglobin ANS: 97 Chapter 29. Alterations of Pulmonary Function MULTIPLE CHOICE 1. A 10-year-old female develops pneumonia. Physical exam reveals subcostal and intercostal retractions. She reports that breathing is difficult and she feels she cannot get enough air. What term should the nurse use to document this condition? a. Cyanosis b. Dyspnea c. Hyperpnea d. Orthopnea ANS: B Dyspnea is defined as a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity. Cyanosis is a bluish discoloration to the skin. Hyperpnea is an increased ventilatory rate. Orthopnea is dyspnea that occurs when an individual lies flat. Cognitive Level: Comprehension 678 2. A 20-year-old male presents to his primary care provider reporting difficulty breathing when lying down. What term should the nurse use to document this condition? a. Dyspnea b. Orthopnea c. Apnea d. Tachypnea ANS: B Orthopnea is dyspnea that occurs when an individual lies flat. Dyspnea is shortness of breath that occurs with activity. Apnea is cessation of breathing. Tachypnea is rapid breathing. Cognitive Level: Comprehension 679 3. A 50-year-old diabetic male did not take his medication and is now in metabolic acidosis. He is experiencing Kussmaul respirations. What type of breathing will the nurse observe upon assessment? a. Audible wheezing or stridor b. A slightly increased ventilatory rate, large tidal volumes, and no expiratory pause c. Rapid respirations with periods of apnea d. Very slow inhalations and rapid expirations ANS: B Kussmaul respirations are characterized by a slightly increased ventilatory rate, very large tidal volumes, and no expiratory pause. Audible wheezing is usually associated with conditions such as asthma, and stridor indicates a narrowed airway. Cheyne-Stokes respirations are characterized by alternating periods of deep and shallow breathing, with periods of apnea lasting from 15 to 60 seconds. Kussmaul respirations do not have slow inhalations; bronchiolar disorders have these characteristics. Cognitive Level: Comprehension 679 4. A 30-year-old female received a severe head injury in a motor vehicle accident. She is now experiencing respiratory abnormalities characterized by alternating periods of deep and shallow breathing with periods of apnea. What term should the nurse use when charting this condition? a. Cheyne-Stokes b. Frank-Starling c. Apnea d. Orthopnea ANS: A Cheyne-Stokes respirations are characterized by alternating periods of deep and shallow breathing, with periods of apnea lasting from 15 to 60 seconds. Frank-Starling is related to the stretch of fibers. Apnea is cessation of respirations. Orthopnea is dyspnea that occurs when an individual lies flat. Cognitive Level: Comprehension 679 5. Which patient would the nurse assess for paroxysmal nocturnal dyspnea (PND)? A patient with: a. Pulmonary fibrosis b. Asthma c. Left ventricular failure d. Hypotension ANS: C Some individuals with cardiac disease awake at night gasping for air and have to sit up or stand to relieve the dyspnea (PND). PND occurs primarily with cardiac disease, not pulmonary fibrosis. Individuals with asthma experience orthopnea, rather than PND. Individuals with left ventricular problems experience PND. It is not associated with hypotension. Cognitive Level: Comprehension 679 6. A 20-year-old male is in acute pain. An arterial blood gas reveals decreased carbon dioxide (CO2) levels. Which of the following does the nurse suspect is the most likely cause? a. Hyperventilation b. Hypoventilation c. Apnea d. Cyanosis ANS: A Individuals with hyperventilation blow off CO2. Individuals with hypoventilation retain CO2. Apnea is cessation of breathing. Cyanosis is a blue color to the skin. Cognitive Level: Comprehension 679 7. A 65-year-old female with emphysema presents to the ER for difficulty breathing. Physical exam reveals bluish skin and mucous membranes. How should the nurse chart this condition? Patient has: a. Cyanosis b. Hemoptysis c. Hematemesis d. Ischemia ANS: A Cyanosis is a blue color to the skin. Hemoptysis is the coughing up of blood or bloody secretions. Hematemesis is blood in the vomitus. Ischemia is a lack of blood supply to tissues. Cognitive Level: Comprehension 680 8. A 28-year-old male reports to his primary care provider that he has had a cold for a week and is coughing up bloody secretions. When giving report, what term should the nurse use to describe this condition? a. Hematemesis b. Cyanosis c. Rhinitis d. Hemoptysis ANS: D Hemoptysis is the coughing up of bloody secretions. Hematemesis is bloody vomiting. Cyanosis is a bluish color to the skin. Rhinitis is a runny nose. Cognitive Level: Comprehension 679 9. A nurse is reviewing the results of an ABG and finds reduced oxygenation of arterial blood. What term should the nurse use to describe this condition? a. Ischemia b. Hypoxia c. Hypoxemia d. Hypocapnia ANS: C Hypoxemia is a reduction of oxygen in arterial blood. Ischemia is a lack of blood supply to tissues. Hypoxia is reduced oxygen in tissues. Hypocapnia is decreased CO2. Cognitive Level: Comprehension 680 10. A group of mountain climbers experience confusion, tachycardia, edema, and decreased renal output after climbing Mount Rainier. A nurse recalls this condition is caused by: a. Bronchoconstriction b. Hypoventilation c. Decreased inspired oxygen d. Diffusion abnormalities ANS: C The mountain climbers are experiencing decreased inspired oxygen. Bronchoconstriction would result in wheezing. Hypoventilation would result in retained CO2. The mountain climbers are experiencing decreased inspired air, not diffusion problems. Cognitive Level: Comprehension 681 11. A nurse remembers a low ventilation-perfusion ratio results in: a. Increased dead space b. Shunting c. Alveolar collapse d. Bronchoconstriction ANS: B Hypoxemia caused by inadequate ventilation of well-perfused areas of the lung is a form of mismatching called shunting. Hypoxemia caused by inadequate ventilation of well-perfused areas of the lung is a form of mismatching called shunting, not dead space. Alveolar collapse is called atelectasis. Hypoxemia caused by inadequate ventilation of well-perfused areas of the lung is a form of mismatching called shunting, not bronchoconstriction. Cognitive Level: Comprehension 681 12. When the pulmonologist discusses the condition in which a series of alveoli in the left lower lobe receive adequate ventilation but do not have adequate perfusion, which statement indicates the nurse understands this condition? When this occurs in a patient it is called: a. A right-to-left shunt b. Alveolar dead space c. A low ventilation-perfusion ratio d. Pulmonary hypotension ANS: B When certain areas of the alveoli experience inadequate perfusion, it is referred to as dead space. When certain areas of the alveoli experience inadequate perfusion, it is referred to as dead space. It is not a right-to-left shunt. Shunting is due to a low ventilation-perfusion ratio. When certain areas of the alveoli experience inadequate perfusion, it is referred to as dead space, not pulmonary hypotension. Cognitive Level: Comprehension 681 13. A 30-year-old male is involved in a motor vehicle accident and sustains trauma to the lungs and chest wall. He experiences respiratory failure. Which of the following lab values would the nurse expect? a. Electrolyte imbalances b. Elevated PaCO2 c. Low hematocrit d. Elevated pH ANS: B In respiratory failure, inadequate gas exchange occurs such that PaO2 = 50 mm Hg or PaCO2 = 50 mm Hg with pH = 7.25. Electrolyte imbalances do not occur, but changes in blood gas values do. Hematocrit may be unaffected. pH will be decreased. Cognitive Level: Comprehension 682 14. A nurse is teaching staff about pulmonary edema. Which information should the nurse include? The most common cause of pulmonary edema is: a. Right heart failure b. Left heart failure c. Asthma d. Lung cancer ANS: B The most common cause of pulmonary edema is left-sided heart disease. The most common cause of pulmonary edema is left-sided heart disease, not right-sided. The most common cause of pulmonary edema is left-sided heart disease, not asthma. The most common cause of pulmonary edema is left-sided heart disease, not lung cancer. Cognitive Level: Comprehension 687 15. A 47-year-old male is diagnosed with pulmonary edema. Which assessment findings will the nurse observe? a. Thick mucus secretions b. Pink, frothy sputum c. Hypocapnia d. Wheezing ANS: B In severe pulmonary edema, pink frothy sputum is expectorated. In severe edema, pink frothy sputum is expectorated, not thick mucus secretions. In severe edema, pink frothy sputum is expectorated, not hypocapnia. In severe edema, pink frothy sputum is expectorated, not wheezing. Cognitive Level: Comprehension 687 16. A 65-year-old male recently had a cerebrovascular accident that resulted in dysphagia. He now has aspiration of gastric contents. The nurse assesses the patient for which complication? a. Pneumonia b. Bronchiectasis c. Pneumothorax d. Emphysema ANS: A Aspiration of stomach contents could lead to pneumonia. Aspiration could lead to pneumonia; bronchiectasis is related to dilation and is not associated with aspiration. Pneumothorax is a collapse of a portion of the lung and is not associated with aspiration. Emphysema is due to air trapping and is not associated with aspiration. Cognitive Level: Comprehension 695 17. A 26-year-old female recently underwent surgery and is now experiencing dyspnea, cough, fever, and leukocytosis. Tests reveal that she has a collapsed lung caused by removal of air from obstructed alveoli. What condition will the nurse observe on the chart? a. Compression atelectasis b. Bronchiectasis c. Absorption atelectasis d. Hypoventilation ANS: C Absorption atelectasis results from removal of air from obstructed or hypoventilated alveoli or from inhalation of concentrated oxygen or anesthetic agents. Compression atelectasis is caused by external pressure exerted by tumor, fluid, or air in pleural space or by abdominal distention pressing on a portion of lung. Bronchiectasis is dilation of the bronchi, not atelectasis. Hypoventilation is inadequate alveolar ventilation of the lungs; it is not due to removal of air. Cognitive Level: Comprehension 685 18. A 45-year-old male undergoes lung transplantation. He now suffers from airway occlusion secondary to fibrosis. Which diagnosis will the nurse see on the chart? a. Compression atelectasis b. Bronchiectasis c. Bronchiolitis d. Bronchiolitis obliterans ANS: D Bronchiolitis is a serious complication of stem cell and lung transplantation and can progress to bronchiolitis obliterans, a fibrotic process that occludes airways and causes permanent scarring of the lungs. The most likely diagnosis is bronchiolitis obliterans, not compression atelectasis. The most likely diagnosis is bronchiolitis obliterans, not bronchiectasis. Bronchiolitis is a serious complication of stem cell and lung transplantation and can progress to bronchiolitis obliterans, not just bronchiolitis. Cognitive Level: Comprehension 685 19. A 50-year-old male presents with hypotension, hypoxemia, and tracheal deviation to the left. Tests reveal that the air pressure in the pleural cavity exceeds barometric pressure in the atmosphere. Based upon these assessment findings, what does the nurse suspect the patient is experiencing? a. Pleural effusion b. Tension pneumothorax c. Open pneumothorax d. Transudative pneumothorax ANS: B Tracheal deviation suggests tension pneumothorax. Tracheal deviation suggests tension pneumothorax, not pleural effusion. Tracheal deviation suggests tension pneumothorax; with open pneumothorax, a sucking sound would be heard without tracheal deviation. Tracheal deviation suggests tension pneumothorax. Cognitive Level: Comprehension 684 20. A 60-year-old female with a history of cirrhosis presents with dyspnea, impaired ventilation, and pleural pain. A diagnosis of pleural effusion is made, and a watery fluid is drained. When giving report, the nurse will refer to this fluid as: a. Exudative b. Purulent c. Infected d. Transudative ANS: D Pleural effusions that enter the pleural space from intact blood vessels can be transudative (watery). The fluid is watery; thus, it is not exudative, which is composed of white cells. The fluid is watery; thus, it is transudative, not purulent. The fluid is watery; thus, it is transudative, not infected. Cognitive Level: Comprehension 684 21. An 80-year-old female develops pneumonia in the hospital. She becomes cyanotic, tachycardic, and develops a fever and cough. Chest x-ray reveals pus in the pleural space. Which of the following is the most likely diagnosis documented on the chart? a. Empyema b. Emphysema c. Pleurisy d. Chyle ANS: A The presence of microorganisms in the pleural space is termed empyema. The presence of microorganisms in the pleural space is termed empyema; emphysema is a total lung disorder. Pleurisy causes pain with inspiration. Chyle is milky fluid with lymph and fat. Cognitive Level: Comprehension 684 22. A 54-year-old male is diagnosed with empyema. Upon receiving and reviewing the culture result, which organism does the nurse suspect is the most likely cause? a. Virus b. Staphylococcus aureus c. Klebsiella pneumonia d. Moraxella catarrhalis ANS: B The most likely cause of empyema is Staphylococcus aureus. The most likely cause of empyema is Staphylococcus aureus; it is not due to a virus. The most likely cause of empyema is Staphylococcus aureus; it is not due to Klebsiella. The most likely cause of empyema is Staphylococcus aureus; it is not due to Moraxella catarrhalis. Cognitive Level: Comprehension 684 23. A 15-year-old female is diagnosed with restrictive lung disease caused by fibrosis. The patient had a pulmonary functions test. Which of the following findings is expected? a. Increased compliance b. Increased tidal volume c. Decreased respiratory rate d. Decreased functional residual capacity ANS: D Fibrosis progressively obliterates the alveoli, respiratory bronchioles, and interstitium (fibrosing alveolitis), which can result in chronic pulmonary insufficiency, and functional residual capacity declines. Compliance decreases in restrictive disease. In restrictive disease, tidal volume decreases. Respirations may increase with restrictive disease. Cognitive Level: Comprehension 686 24. A 57-year-old male presents with cough, sputum production, dyspnea, and decreased lung volume. He is diagnosed with pneumoconiosis. When taking the patients history, which finding is the most probable cause of his illness? a. Inhalation of silica, asbestos, mica b. Autoimmune disease c. Allergic reactions d. Flail chest ANS: A The dusts of silica, asbestos, and coal are the most common causes of pneumoconiosis. The dusts of silica, asbestos, and coal are the most common causes of pneumoconiosis; it is not an autoimmune disorder. The dusts of silica, asbestos, and coal are the most common causes of pneumoconiosis; it is not an allergic response. The dusts of silica, asbestos, and coal are the most common causes of pneumoconiosis; it is not due to flail chest. Cognitive Level: Comprehension 686 25. A 42-year-old female presents with dyspnea; rapid, shallow breathing; inspiratory crackles; decreased lung compliance; and hypoxemia. Tests reveal a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Acute respiratory distress syndrome (ARDS) b. Sarcoidosis c. Postoperative respiratory failure d. Malignant respiratory failure ANS: A The patient is experiencing ARDS. The patients symptoms demonstrate ARDS, not sarcoidosis. The patients symptoms demonstrate ARDS, not postoperative respiratory failure. The patient is experiencing ARDS, not malignant respiratory failure. Cognitive Level: Comprehension 687 26. Which of the following shows a correct cause and effect sequence in the development of acute respiratory distress syndrome (ARDS)? a. Impaired alveolar compliance causing decreased surfactant production b. Alveolocapillary membrane injury causing a massive inflammatory response c. Hyaline membrane formation and fibrosis causing pulmonary edema d. Increased alveolocapillary membrane permeability causing metabolic alkalosis ANS: B All disorders causing ARDS cause massive pulmonary inflammation that injures the alveolocapillary membrane and produces severe pulmonary edema and inflammation. All disorders causing ARDS cause massive pulmonary inflammation that injures the alveolocapillary membrane and produces severe pulmonary edema and inflammation. It does not affect surfactant. ARDS does not cause hyaline formation. Metabolic alkalosis occurs late, but inflammation occurs first. Cognitive Level: Comprehension 687 27. A 60-year-old female with emphysema is having difficulty expiring a given volume of air. When giving report, the nurse will relay that the patient is most likely experiencing pulmonary disease. a. Restrictive b. Obstructive c. Atelectatic d. Pleuritic ANS: B Emphysema is a form of obstructive pulmonary disease. Emphysema is a form of obstructive pulmonary disease, not restrictive. Emphysema is a form of obstructive pulmonary disease, not atelectatic. Emphysema is a form of obstructive pulmonary disease, not pleuritic. Cognitive Level: Comprehension 694 28. When the nurse is asked what causes asthma, how should the nurse respond? Asthma is thought to be caused by: a. An autosomal recessive trait b. Autoimmunity c. Excessive use of antibiotics as a young child d. Interactions between genetic and environmental factors ANS: D Asthma is an interaction between genetic and environmental factors. Asthma is both genetic and environmental, but is not recessive. Asthma is both genetic and environmental, but is not an autoimmune response. Asthma is not due to excessive antibiotic use in childhood. Cognitive Level: Comprehension 689 29. A nurse recalls asthma is classified by: a. Pathophysiologic differences b. Clinical severity c. Genetic traits d. Treatment outcomes ANS: B The National Asthma Education and Prevention Program offers stepwise guidelines for the diagnosis and management of chronic asthma based on clinical severity. The National Asthma Education and Prevention Program offers stepwise guidelines for the diagnosis and management of chronic asthma based on clinical severity, not pathophysiologic differences. The National Asthma Education and Prevention Program offers stepwise guidelines for the diagnosis and management of chronic asthma based on clinical severity, not genetic traits. The National Asthma Education and Prevention Program offers stepwise guidelines for the diagnosis and management of chronic asthma based on clinical severity, not treatment outcomes. Cognitive Level: Comprehension 691 30. A nurse is preparing to teach the staff about asthma. Which information should the nurse include? Airway hyper-responsiveness in asthma is related to: a. Increased sympathetic nervous system response b. The release of stress hormones c. Exposure to an allergen causing mast cell degranulation d. Hereditary decrease in IgE responsiveness ANS: C Hyper-responsiveness is due to mast cell degranulation. An increased sympathetic response would lead to bronchiolar dilation. Hyper-responsiveness is due to mast cell degranulation, not to release of stress hormones. Hyper-responsiveness is due to mast cell degranulation; heredity is associated with asthma, but the problem is the mast cells. Cognitive Level: Comprehension 689 31. A nurse is preparing to teach the staff about asthma. Which information should the nurse include? Airway obstruction contributing to increased airflow resistance and hypoventilation in asthma is caused by: a. Type II alveolar cell injury and decreased surfactant b. Alveolar fibrosis and pulmonary edema c. Mucus secretion, bronchoconstriction, and airway edema d. Collapse of the cartilaginous rings in the bronchi ANS: C The mediators of asthma cause vasodilation, increased capillary permeability, mucosal edema, bronchial smooth muscle contraction (bronchospasm), and mucus secretion from mucosal goblet cells with narrowing of the airways and obstruction to airflow. Acute respiratory distress syndrome involves type II injury. Alveolar fibrosis with pulmonary edema is not associated with asthma. Asthma is not associated with collapse of bronchiolar rings. Cognitive Level: Comprehension 689 32. A 10-year-old male is brought to the ER with prolonged bronchospasm and severe hypoxemia. The most likely diagnosis on the chart is: a. Exercise-induced asthma b. Chronic obstructive pulmonary disease (COPD) c. Status asthmaticus d. Bronchiectasis ANS: C When bronchospasm is not reversed by usual measures, the individual is considered to have severe bronchospasm or status asthmaticus. When bronchospasm is not reversed by usual measures, the individual is considered to have severe bronchospasm or status asthmaticus; exercise-induced asthma resolves. COPD is manifested by air trapping and hypercapnia, not by bronchospasm. Bronchiectasis is manifested by bronchiolar changes, not bronchospasm. Cognitive Level: Comprehension 691 33. A 22-year-old female presents with chronic bronchitis. Tests reveal closure of the airway during expiration. While planning care, a nurse recalls this condition is most likely caused by: a. Thick mucus from hypertrophied glands b. Ventilation-perfusion mismatch c. Hyperventilation d. Thinning smooth muscle in the bronchioles ANS: A Chronic bronchitis is defined by hypersecretion of thick mucus. Ventilation-perfusion mismatch may occur, but chronic bronchitis is defined as hypersecretion of mucus. Chronic bronchitis is defined as hypersecretion of mucus; dyspnea may occur, but hyperventilation is not expected. Chronic bronchitis is defined as hypersecretion of mucus; thickening of smooth muscle occurs, not thinning. Cognitive Level: Comprehension 693 34. A 25-year-old male presents with chronic bronchitis of 5 months duration. When obtaining the patients history, which of the following findings is most likely to cause this condition? a. Chronic asthma b. Air pollution c. Cigarette smoke d. Recurrent pneumonias ANS: C The most likely cause of chronic bronchitis is cigarette smoke. The most likely cause of chronic bronchitis is cigarette smoke, not chronic asthma. Air pollution may contribute, but smoking is the most common cause. Recurrent infections could contribute, but smoking is the most common cause. Cognitive Level: Comprehension 694 35. A 25-year-old male presents with chronic bronchitis of 5 months duration. Which of the following is the most significant concern for the nurse to monitor in this patient? a. Left heart failure b. Pulmonary embolus c. Immunosuppression d. Recurrent pulmonary infections ANS: D Recurrent pulmonary infections are a significant concern for this patient. Recurrent infections, not left heart failure, are a significant concern for a patient with bronchitis. Recurrent infections, not pulmonary embolus, are a significant concern for a patient with bronchitis. Recurrent infections, not immunosuppression, are a significant concern for a patient with bronchitis. Cognitive Level: Comprehension 693 36. A 53-year-old male with a 20-year history of smoking is diagnosed with emphysema. When a staff member asks why the patients airways are obstructed, how should the nurse respond? The airways are obstructed because of: a. Excessive mucus production b. Loss of elastic recoil c. Infection and inflammation d. Airway edema ANS: B The major mechanism of airflow limitation is loss of elastic recoil. The major mechanism of airflow limitation is loss of elastic recoil, not excessive mucus as with bronchitis. The major mechanism of airflow limitation is loss of elastic recoil, not infection. The major mechanism of airflow limitation is loss of elastic recoil, not airway edema. Cognitive Level: Comprehension 694 37. A 53-year-old male with a 20-year history of smoking is diagnosed with emphysema. When the nurse is asked what causes this, what is the nurses best response? Changes in his lungs are caused by: a. Viral infections b. Destruction of alveolar macrophages c. Alpha-1-antitrypsin deficiency d. Fibrotic lung disease ANS: C Changes in the lungs are associated with alpha-1-antitrypsin deficiency. Changes in the lungs are associated with alpha-1-antitrypsin deficiency; it is not due to viral infections. Changes in the lungs are associated with alpha-1-antitrypsin deficiency; it is not due to alveolar macrophage destruction. Changes in the lungs are associated with alpha-1-antitrypsin deficiency; it is not due to fibrotic lung disease. Cognitive Level: Comprehension 695 38. Individuals with a recent diagnosis of emphysema should be assessed for which most common presenting factor? a. A productive cough b. Cyanosis c. Dyspnea d. Cor pulmonale ANS: C Dyspnea is the most common presenting factor of emphysema. Dyspnea, not a productive cough, is the most common presenting factor of emphysema. Dyspnea, not cyanosis, is the most common presenting factor of emphysema. Dyspnea, not cor pulmonale, is the most common presenting factor of emphysema. Cognitive Level: Comprehension 694 39. A 60-year-old female with a 25-year history of smoking is diagnosed with emphysema. She has an increased anterior-posterior chest diameter. The nurse attributes this finding to: a. Air trapping b. Decreased inspiratory reserve volumes c. Increased flow rates d. Alveolar destruction ANS: A Air trapping expands the thorax, putting the respiratory muscles at a mechanical disadvantage. Air trapping expands the thorax, putting the respiratory muscles at a mechanical disadvantage. Air trapping, not increased flow rates, expands the thorax, putting the respiratory muscles at a mechanical disadvantage. Air trapping, not alveolar destruction, expands the thorax putting the respiratory muscles at a mechanical disadvantage. Cognitive Level: Comprehension 693 40. A patient asks what causes pneumonia. How should the nurse reply? Pneumonia is caused by: a. Use of anesthetic agents in surgery b. Atelectasis c. Chronic lung changes seen with aging d. Viral or bacterial infections ANS: D Pneumonia is caused by a viral or bacterial infection. Pneumonia is caused by a viral or bacterial infection; infections are not caused by anesthetic agents. Pneumonia is caused by a viral or bacterial infection; atelectasis does not cause pneumonia. Pneumonia is caused by a viral or bacterial infection; lung changes in aging are normal changes, not infectious. Cognitive Level: Comprehension 694 41. When the nurse observes a diagnosis of nosocomial pneumonia, the patient generally acquires this pneumonia: a. At day care centers b. On airplanes c. During hospitalization d. In the winter season ANS: C Nosocomial infections are acquired in the hospital. Nosocomial infections are acquired in the hospital, not day care centers. Nosocomial infections are acquired in the hospital, not airplanes. Nosocomial infections are acquired in the hospital; it may happen in any season. Cognitive Level: Comprehension 694 42. A 30-year-old male prison inmate contracted tuberculosis during an outbreak. When the nurse reviews the lab results, the organism that caused this condition is a: a. Bacterium b. Fungus c. Virus d. Parasite ANS: A The organism that causes tuberculosis is a bacterium. The organism that causes tuberculosis is a bacterium, not a fungus. The organism that causes tuberculosis is a bacterium, not a virus. The organism that causes tuberculosis is a bacterium, not a parasite. Chapter 30. Alterations of Pulmonary Function in Children MULTIPLE CHOICE 1. A 1-year-old female is diagnosed with croup. When the parent asks what caused this, what is the nurses best response? The most likely cause of this disease is: a. Bacteria b. Acute hyperventilation c. Allergy d. Viral infection ANS: D The cause of croup is a viral infection. The cause of croup is viral, not bacterial. Croup is due to a viral infection, not to acute hyperventilation. Croup is due to a viral infection, not to allergy. Cognitive Level: Comprehension 707 2. While planning care, a nurse recalls respiratory distress and hypoxemia in laryngotracheobronchitis are caused by: a. Infectious pulmonary edema b. Mucosal edema c. Decreased surfactant d. Nasopharyngeal obstruction ANS: B Edema leads to obstruction of the airway and respiratory distress. Pulmonary edema does not occur; it is due to edema of the mucosa. Laryngotracheobronchitis is not a problem of surfactant. The obstruction is in the airway, not the nasopharyngeal area. Cognitive Level: Comprehension 708 3. A 5-year-old male presents with high fever, inspiratory stridor, severe respiratory distress, drooling, and dysphagia. Which of the following behaviors by the student nurse would be a cause for concern? a. The student nurse tries to keep the child calm. b. The student nurse examines the throat for redness. c. The student nurse auscultates the childs respiratory rate. d. The student nurse counts the heart rate apically. ANS: B Examination of the throat should not be attempted as it may trigger laryngospasm and cause respiratory collapse. Keeping the child calm is appropriate. Auscultating the respiratory rate is appropriate. Assessing the heart rate apically is appropriate. Cognitive Level: Comprehension 709 4. A 10-year-old male was diagnosed with obstructive sleep apnea. When the parents ask what treatment comes next, how should the nurse respond? The treatment that will most likely be tried first is: a. Tonsillectomy and adenoidectomy (T&A) b. Weight loss c. Continuous positive airway pressure d. Drug therapy ANS: A Children with sleep apnea are most often referred for T&A. Children with sleep apnea are most often referred for T&A. Weight loss is secondary. Children with sleep apnea are most often referred for T&A. Continuous positive airway pressure is secondary. Children with sleep apnea are most often referred for T&A. Drug therapy is secondary. Cognitive Level: Comprehension 710 5. A newborn has respiratory distress syndrome. When obtaining the patients history, which of the following is the most important predisposing factor for this condition? a. Low birth weight b. Alcohol consumption by the mother during pregnancy c. Premature birth d. Smoking by the mother during pregnancy ANS: C Respiratory distress syndrome in the newborn is more often due to premature birth. Newborn respiratory distress occurs almost exclusively in premature infants, not low birth weight. Newborn respiratory distress occurs almost exclusively in premature infants, not from alcohol use by the mother. Newborn respiratory distress occurs almost exclusively in premature infants, not from smoking by the mother during pregnancy. Cognitive Level: Comprehension 710 6. A newborn has respiratory distress syndrome. A nurse monitors the newborn for atelectasis because of: a. A lack of surfactant b. Pulmonary edema c. Airway obstruction d. Pulmonary fibrosis ANS: A Atelectasis in newborn respiratory distress is due to lack of surfactant. Atelectasis in newborn respiratory distress is due to lack of surfactant, not pulmonary edema. Atelectasis in newborn respiratory distress is due to lack of surfactant, not airway obstruction. Atelectasis in newborn respiratory distress is due to lack of surfactant, not pulmonary fibrosis. Cognitive Level: Comprehension 711 7. A newborn has respiratory distress syndrome. A nurse recalls cardiovascular alterations seen in respiratory distress syndrome include: a. Left-to-right shunt b. Left ventricular dilation c. Pulmonary hypotension d. Opening of fetal shunt pathways ANS: D Increased pulmonary vascular resistance may even cause a partial return to fetal circulation, with right-to-left shunting of blood through the ductus arteriosus and foramen ovale. A left-to-right shunt does not occur but vice versa. A return to fetal shunting occurs, not ventricular dilation. A return to fetal shunting occurs, not pulmonary hypotension. Cognitive Level: Comprehension 711 8. A newborn has respiratory distress syndrome (RDS). The nurse reports this condition appeared: a. Within minutes of birth b. 2 to 3 hours after birth c. Within the first 12 to 24 hours after birth d. 24 to 48 hours after exposure to an infectious organism ANS: A Signs of RDS appear within minutes of birth. Signs of RDS appear within minutes of birth, not 2 to 3 hours. Signs of RDS appear within minutes of birth, not within the first 24 hours. Signs of RDS appear within minutes of birth; it is not associated with an infectious organism. Cognitive Level: Comprehension 712 9. During a respiratory assessment of an infant with respiratory distress syndrome, a sinking in the supraclavicular and intercostal areas of the thorax was noted with inspiration. This observation is documented as: a. Grunting b. Tachypnea c. Retractions d. Nasal flaring ANS: C The sinking of supraclavicular and intercostal areas is termed retractions. The symptoms describe retractions, not grunting. The symptoms describe retractions, not tachypnea. The symptoms describe retractions, not nasal flaring. Cognitive Level: Comprehension 712 10. An infant was born 10 weeks premature and put on mechanical ventilation. Two months later he presents with hypoxemia and hypercapnia. Which of the following is the most likely diagnosis the nurse will observe documented on the chart? a. Respiratory distress syndrome of the newborn b. Bronchopulmonary dysplasia (BPD) c. Bronchiolitis d. Pneumonia ANS: B Mechanical ventilation can result in a proinflammatory state that may contribute to the development of chronic lung disease, such as BPD. Mechanical ventilation can result in a proinflammatory state that may contribute to the development of chronic lung disease, such as BPD. Respiratory distress might have led to the intubation, but BPD is the diagnosis. Mechanical ventilation can result in a proinflammatory state that may contribute to the development of chronic lung disease, such as BPD, not bronchiolitis. Mechanical ventilation can result in a proinflammatory state that may contribute to the development of chronic lung disease, such as BPD, not pneumonia. Cognitive Level: Comprehension 712 11. A 6-month-old female presents with rhinorrhea, cough, poor feeding, lethargy, and fever. She is diagnosed with bronchiolitis. Which of the following will the nurse most likely observe on the culture report? a. Parainfluenza virus b. Haemophilus B influenzae c. Respiratory syncytial virus d. Group A beta-hemolytic streptococcus ANS: C The most common cause of bronchiolitis is respiratory syncytial virus. The most common cause of bronchiolitis is respiratory syncytial virus, not parainfluenza virus. The most common cause of bronchiolitis is respiratory syncytial virus, not Haemophilus B influenzae. The most common cause of bronchiolitis is respiratory syncytial virus, not strep. Cognitive Level: Comprehension 714 12. A 2-year-old male presents with fever and cough. He is diagnosed with pneumonia. While planning treatment for this patient, the nurse recognizes that which of the following is the most likely cause? a. Bacteria b. Viruses c. Mycoplasma species d. Toxic inhalations ANS: B Viral pneumonia is more common than bacterial pneumonia, and children are 2 to 3 times more likely than adults to acquire these viruses. Viral pneumonia is more common than bacterial pneumonia, and children are 2 to 3 times more likely than adults to acquire these viruses. Viral pneumonia is more common in children than Mycoplasma species. Viral pneumonia is more common in children than toxic inhalations. Cognitive Level: Comprehension 714 13. An 11-year-old female presents with a low-grade fever and cough. She is diagnosed with atypical pneumonia. What type of pneumonia does the nurse suspect the patient is experiencing? a. Pneumococcal pneumonia b. Viral pneumonia c. Mycoplasma pneumonia d. Streptococcal pneumonia ANS: C Chlamydophila pneumonia is clinically indistinguishable from and is typically grouped with Mycoplasma as atypical pneumonia. Bacterial pneumonia would not be atypical. Viral pneumonia is not an atypical pneumonia. Bacterial pneumonia is not part of atypical pneumonia. Cognitive Level: Comprehension 714 14. A 2-week-old female presents with fever, cough, respiratory distress, and empyema. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Viral pneumonia b. Pneumococcal pneumonia c. Staphylococcal pneumonia d. Mycoplasma pneumonia ANS: C Staphylococcal and group A streptococcal pneumonia can be particularly fulminant (sudden, severe) and necrotizing (causing cell death) with a high incidence of accompanying empyema, pneumatocele, and sepsis. Staphylococcal pneumonia is the more likely diagnosis than viral. Staphylococcal pneumonia is more likely to cause empyema than pneumococcal. Staphylococcal pneumonia is more likely to cause empyema than Mycoplasma. Cognitive Level: Comprehension 714 15. A 9-year-old male contracted influenza. Which of the following complications is of greatest concern to the nurse? a. Chronic bronchitis b. Bronchiolitis obliterans c. Emphysema d. Respiratory distress syndrome (RDS) ANS: B Bronchiolitis obliterans most often occurs as a sequelae of a severe viral pulmonary infection (e.g., influenza, adenovirus, pertussis [whooping cough], or measles). Bronchiolitis obliterans, not just chronic bronchitis, most often occurs as a sequelae of a severe viral pulmonary infection (e.g., influenza, adenovirus, pertussis [whooping cough], or measles). Bronchiolitis obliterans, not emphysema, most often occurs as a sequelae of a severe viral pulmonary infection (e.g., influenza, adenovirus, pertussis [whooping cough], or measles). Bronchiolitis obliterans, not RDS, most often occurs as a sequelae of a severe viral pulmonary infection (e.g., influenza, adenovirus, pertussis [whooping cough], or measles). Cognitive Level: Comprehension 715 16. While planning care for a child with asthma, which of the following is characteristic of asthma? a. Increased lung volumes b. Prolonged expirations c. Air trapping d. Dead space ANS: B On physical examination, there is expiratory wheezing that is often described as high pitched and musical, and there is prolongation of the expiratory phase of the respiratory cycle. Lung volumes are decreased. Air trapping occurs in emphysema, not asthma. Dead space occurs in emphysema, not asthma. Cognitive Level: Comprehension 716 17. A 14-year-old male is experiencing an asthma exacerbation. When reviewing the lab results, which of the following cells in the submucosa promote this inflammatory response and will be elevated? a. Neutrophils b. Eosinophils c. Macrophages d. Lymphocytes ANS: B In the late asthmatic response, there are areas of epithelial damage and shedding caused at least in part by toxicity of eosinophil products. Eosinophils, not neutrophils, promote the inflammatory response. Eosinophils, not macrophages, promote the inflammatory response. Eosinophils, not lymphocytes, promote the inflammatory response. Cognitive Level: Comprehension 716 18. A 13-year-old female is diagnosed with asthma. Which of the following should the nurse teach the patient to recognize as part of an asthmatic attack? a. Headache b. Chest pain c. Wheezing d. Low heart rate ANS: C Wheezing occurs in asthma, due to narrowing of airways. Headache is not a part of an asthma attack. Wheezing is part of an asthma attack, not chest pain. The heart rate will be increased, not decreased. Cognitive Level: Comprehension 716 19. A geneticist is discussing cystic fibrosis (CF). Which information should be included? CF is an disease. a. Autosomal recessive b. Autosomal dominant c. X-linked recessive d. X-linked dominant ANS: A CF is an autosomal recessive disease. CF is an autosomal recessive disease, not dominant. CF is not X-linked. CF is not X-linked. Cognitive Level: Comprehension 718 20. A 2-year-old female fell in a swimming pool and nearly drowned. She then developed acute respiratory distress syndrome (ARDS). Which of the following should the nurse assess the patient for? a. Decreased heart rate b. Increased lung compliance c. Increased surfactant production d. Hypoxemia ANS: D The child with ARDS will experience severe hypoxemia. The child with ARDS will have an elevated, not decreased, heart rate. The child with ARDS has decreased, not increased, lung compliance. Surfactant production is not affected in ARDS. Cognitive Level: Comprehension 718 21. While reviewing lab results, to help confirm a diagnosis of cystic fibrosis in a 1-year-old child which substance will be present in the childs sweat? a. Potassium b. Sodium chloride c. Magnesium d. Carbonic acid ANS: B The standard method of diagnosis is the sweat test, which reveals sweat chloride concentration in excess of 60 mEq/L. Sodium chloride, not potassium, is present in the sweat. Sodium chloride, not magnesium, is present in the sweat. Sodium chloride, not carbonic acid, is present in the sweat. Cognitive Level: Comprehension 719 22. A 7-month-old male presents with cystic fibrosis (CF) accompanied by failure to thrive and frequent, loose, and oily stools. Sweat testing reveals increased chloride. Which of the following should the nurse observe for that would accompany this disease? a. Autoantibodies that target the lungs and pancreas b. A thick mucus c. Enzymes that degrade surfactant in the alveoli d. A toxic amount of electrolytes from secretory glands ANS: B In CF, thick mucus is present. Thick mucus is present, not autoantibodies. Thick mucus is present; CF does not involve surfactant. Thick mucus is present, not elevated electrolytes. Cognitive Level: Comprehension 719 23. A young patient is admitted to the pediatric unit with cystic fibrosis (CF) exacerbation. The nurse monitors the patient closely because the main cause of death in a child with CF is: a. Airway rigidity b. Pulmonary edema c. Respiratory failure d. Asthma-like bronchospasms ANS: C Although CF is a multi-organ disease, its most important effects are on the lungs, and respiratory failure is almost always the cause of death. Although CF is a multi-organ disease, its most important effects are on the lungs, and respiratory failure is almost always the cause of death; airway rigidity does not occur. Mucus plugging, not pulmonary edema, occurs. Mucus plugging, not asthma-like symptoms, occurs. Cognitive Level: Comprehension 719 24. A nurse is teaching about sudden infant death syndrome (SIDS). Which information should the nurse include? SIDS peaks between and months of age. a. 1, 2 b. 3, 4 c. 6, 8 d. 10, 12 ANS: B SIDS peaks in children 3 to 4 months of age. SIDS peaks in children 3 to 4 months of age, not 1 and 2 months of age. SIDS peaks in children 3 to 4 months of age, not 6 and 8 months of age. SIDS peaks in children 3 to 4 months of age, not 10 and 12 months of age. Cognitive Level: Comprehension 720 25. A 5-month-old female is found dead in her crib. The coroner ruled sudden infant death syndrome (SIDS) as the cause of death. Which of the following risk factors is most likely associated with SIDS? a. Congenital heart disease b. Female gender c. Caucasian race d. Frequent respiratory infections ANS: D A higher rate of respiratory tract infection during those months will likely decreases sleep arousal, making it a risk factor for SIDS. Congenital anomalies play a role, but respiratory infections play a greater role. SIDS occurs in males more than females. Genetic factors may play a role, but ethnicity does not. Cognitive Level: Comprehension 720 26. To prevent sudden infant death syndrome, the nurse should instruct parents to: a. Place infants on a soft mattress for sleeping. b. Always lay infants down on their backs to sleep. c. Breast-feed their infants. d. Keep the infants room very warm. ANS: B Infants should be laid on their backs to sleep. A soft mattress is a possible contributing factor to SIDS. Feeding method does not play as great a role as positioning during sleep. Sleeping position is the most preventable risk factor. Cognitive Level: Comprehension 720 MULTIPLE RESPONSE 1. A 1-year-old female is diagnosed with croup. Which of the following symptoms is most likely to be present when the nurse performs an assessment? (Select all that apply.) a. Barking cough b. Stridor c. Hoarseness d. Drooling e. Truncal rash ANS: A, B, C Typically, the child experiences rhinorrhea, sore throat, and low-grade fever for a few days, then develops a harsh (seal-like) barking cough, inspiratory stridor, and hoarse voice. Cognitive Level: Comprehension 709 COMPLETION 1. A nurse remembers bronchiolitis mainly occurs in children under the age of . ANS: 1 one Bronchiolitis is a common, viral lower respiratory tract infection that occurs almost exclusively in infants and young toddlers. Cognitive Level: Comprehension 714 2. Asthma affects % of children between 5 and 17 years of age. ANS: 10 It is the most prevalent chronic disease in childhood, affecting 10% of U.S. children between 5 and 17 years of age. Chapter 31. Structure and Function of the Renal and Urologic Systems MULTIPLE CHOICE 1. A nurse is teaching the staff about the kidneys. Which information should the nurse include? The region of the kidneys that contains the glomeruli is the: a. Medulla b. Cortex c. Pyramids d. Columns ANS: B The outer layer of the kidney is called the cortex and it contains all of the glomeruli, most of the proximal tubules, and some segments of the distal tubule. The cortex, not the medulla, contains the glomeruli. The cortex, not the pyramids, contains the glomeruli. The cortex, not the columns, contains the glomeruli. Cognitive Level: Comprehension 724 2. When the nurse is discussing the functional unit of the kidney, what other term should the nurse use? a. Calyx b. Nephron c. Collecting duct d. Pyramid ANS: B The functional unit of the kidney is the nephron. The functional unit of the kidney is the nephron, not the calyx. The functional unit of the kidney is the nephron, not the collecting duct. The functional unit of the kidney is the nephron, not the pyramid. Cognitive Level: Comprehension 726 3. The urologist is teaching about the nephrons that determine the concentration of the urine. The urologist is discussing the nephrons. a. Juxtamedullary b. Midcortical c. Cortical d. Medullary ANS: A The juxtamedullary nephrons lie close to and extend deep into the medulla and are important for the concentration of urine. The juxtamedullary nephrons, not the midcortical nephrons, are important for the concentration of urine. The juxtamedullary nephrons, not the cortical nephrons, are important for the concentration of urine. The juxtamedullary nephrons, not the medullary nephrons, are important for the concentration of urine. Cognitive Level: Comprehension 726 4. A urologist is discussing the phagocytic cells that lie between the layers of the renal corpuscle. What is the urologist describing? a. Podocytes b. Macula densa cells c. Mesangial cells d. Filtration slits ANS: C Mesangial cells lie between and support the capillaries. Mesangial cells have phagocytic ability similar to monocytes, release inflammatory cytokines, and can contract to regulate glomerular capillary blood flow. The epithelium has specialized cells called podocytes from which pedicles (foot projections) radiate and adhere to the basement membrane. The macula densa are sodium-sensing cells. The pedicles interlock with the pedicles of adjacent podocytes, forming an elaborate network of intercellular clefts called filtration slits, or slit membranes. Cognitive Level: Comprehension 726 5. When the nurse discusses the glomerulus and Bowman capsule together, it is referred to as the renal: a. Corpuscle b. Capsule c. Medulla d. Pyramid ANS: A Together, the glomerulus and Bowman capsule are called the renal corpuscle. Together, the glomerulus and Bowman capsule are called the renal corpuscle, not capsule. Together, the glomerulus and Bowman capsule are called the renal corpuscle, not medulla. Together, the glomerulus and Bowman capsule are called the renal corpuscle, not pyramid. Cognitive Level: Comprehension 726 6. When a nurse is checking the urinalysis, plasma proteins should be absent from the urine because: a. All proteins filtered are subsequently reabsorbed. b. All of the plasma proteins are too large to fit through the filtration slits. c. All proteins filtered are subsequently degraded before elimination. d. The negative charge of the glomerular filtration membrane repels the plasma proteins. ANS: D Like other capillary membranes, the glomerulus is freely permeable to water and relatively impermeable to large colloids, such as plasma proteins. The molecules size and electrical charge affect the permeability of substances crossing the glomerulus. Proteins are not filtered because the negative charge of the glomerulus repels them. Proteins are not filtered because the negative charge of the glomerulus repels them. It is not only because of their size. Proteins are not filtered because the negative charge of the glomerulus repels them. It is not because of degradation. Cognitive Level: Comprehension 726 7. When the nurse is discussing the sodium-sensing cells of the glomerulus, what term should the nurse use? a. Podocytes b. Macula densa c. Mesangial cells d. Loop of Henle ANS: B The macula densa are sodium-sensing cells. The epithelium has specialized cells called podocytes from which pedicles (foot projections) radiate and adhere to the basement membrane. Mesangial cells lie between and support the capillaries. Mesangial cells have phagocytic ability similar to monocytes, release inflammatory cytokines, and can contract to regulate glomerular capillary blood flow. The loop of Henle is where fluid reabsorption occurs. Cognitive Level: Comprehension 726 8. When a nurse is preparing to teach about urine, which information should the nurse include? Just before entering the ureter, urine passes through the: a. Collecting duct b. Renal pelvis c. Urethra d. Major calyx ANS: B Urine is collected in the renal pelvis and then funneled into the ureters. Urine is collected in the renal pelvis, not the collecting duct, and then funneled into the ureters. Urine is collected in the renal pelvis and then funneled into the ureters. The urethra receives urine from the bladder. Urine is collected in the renal pelvis, not the major calyx, and then funneled into the ureters. Cognitive Level: Comprehension 729 9. A urologist is discussing a structure that supplies blood to the medulla. What is the urologist describing? a. Renal arteries b. Arcuate arteries c. Peritubular capillaries d. Vasa recta ANS: D The vasa recta is a network of capillaries that forms loops and closely follows the loops of Henle and is the only blood supply to the medulla. The vasa recta is the only blood supply to the medulla. The renal arteries do not meet this need. The vasa recta is the only blood supply to the medulla. The arcuate arteries do not meet this need. The vasa recta is the only blood supply to the medulla. The peritubular capillaries do not meet this need. Cognitive Level: Comprehension 734 10. A nurse is describing the trigone. Which information should be included? The trigone is defined as: a. The orifice of the ureter b. The inner area of the kidney c. A triangular area between the openings of the two ureters and the urethra d. The three divisions of the loop of Henle ANS: C The trigone is a smooth triangular area between the openings of the two ureters and the urethra. The trigone is a smooth triangular area between the openings of the two ureters and the urethra; it is not the orifice of the ureter. The trigone is a smooth triangular area between the openings of the two ureters and the urethra; it is not the inner area of the kidney. The trigone is a smooth triangular area between the openings of the two ureters and the urethra; it is not a part of the loop of Henle. Cognitive Level: Comprehension 729 11. When describing the male urinary anatomy, which information should the nurse include? The portion of the male urethra that is closest to the bladder is the portion. a. Membranous b. Prostatic c. Cavernous d. Vas deferens ANS: B In the male, the prostatic urethra is closest to the bladder. In the male, the prostatic urethra is closest to the bladder; the membranous follows after the prostatic. In the male, the prostatic urethra is closest to the bladder; the cavernous follows after the membranous. In the male, the prostatic urethra is closest to the bladder. The vas deferens is not a portion of the male urethra. Cognitive Level: Comprehension 729 12. On average the kidneys receive approximately of the cardiac output. a. 10% to 14% b. 15% to 19% c. 20% to 25% d. 26% to 35% ANS: C The kidney receives 20% to 25% of the cardiac output. The kidney receives 20% to 25%, not 10% to 14% of the cardiac output. The kidney receives 20% to 25%, not 15% to 19% of the cardiac output. The kidney receives 20% to 25%, not 26% to 35% of the cardiac output. Cognitive Level: Comprehension 729 13. While reviewing urine lab results, the nurse remembers the glomerular filtration rate (GFR) is directly related to the: a. Perfusion pressure in the glomerular capillaries b. Oncotic pressure in the glomerular capillaries c. Vascular resistance in the glomerular arterioles d. Hydrostatic pressure in the Bowman capsule ANS: A The filtration of the plasma per unit of time is known as the GFR, which is directly related to the perfusion pressure of the glomerular capillaries. The filtration of the plasma per unit of time is known as the GFR, which is directly related to the perfusion pressure, not the oncotic pressure of the glomerular capillaries. The filtration of the plasma per unit of time is known as the GFR, which is directly related to the perfusion pressure in the glomerular capillaries, not the vascular resistance in the glomerular arterioles. The filtration of the plasma per unit of time is known as the GFR, which is directly related to the perfusion pressure in the glomerular capillaries, not the hydrostatic pressure in the Bowman capsule. Cognitive Level: Comprehension 729 14. A nurse recalls the blood vessels of the kidneys are innervated by the: a. Vagus nerve b. Sympathetic nervous system c. Somatic nervous system d. Parasympathetic nervous system ANS: B The blood vessels of the kidney are innervated by the autonomic nervous system through sympathetic fibers. The blood vessels of the kidney are innervated by the autonomic nervous system through sympathetic fibers, not the vagus nerve. The somatic system regulates the musculoskeletal system. The sympathetic system, not the parasympathetic system, innervates the blood vessels of the kidneys. Cognitive Level: Comprehension 730 15. While planning care for a patient with urinary problems, the nurse recalls that the renin- angiotensin system will be activated by: a. Increased blood volume b. Elevated sodium concentrations c. Decreased blood pressure in the afferent arterioles d. Renal hypertension ANS: C The renin-angiotensin system is activated by decreased blood pressure. Decreased blood pressure, not increased volume, leads to activation of the renin-angiotensin system. Decreased blood pressure, not elevated sodium, leads to activation of the renin-angiotensin system. Decreased blood pressure, not hypertension, leads to activation of the renin-angiotensin system. Cognitive Level: Comprehension 730 16. When a patients renal system secretes rennin, what effect will that cause in the body? It causes the direct activation of: a. Angiotensin I b. Angiotensin II c. Antidiuretic hormone d. Aldosterone ANS: A Renin secretion activates angiotensin I. Renin secretion activates angiotensin I; ACE activates angiotensin II. Renin secretion activates angiotensin I; it does not activate antidiuretic hormone. Renin secretion activates angiotensin I; it does not activate aldosterone. Cognitive Level: Comprehension 730 17. A nurse is reviewing urinalysis results and notices glucose is present in the urine. A nurse realizes glucose will be excreted in the urine when: a. The maximum rate of glucose filtration is achieved b. The carrier molecules have reached their maximum c. Glucose is consumed d. The ability of the kidneys to regulate blood glucose is lost ANS: B When the carrier molecules for glucose become saturated (i.e., with the development of hyperglycemia), the excess will be excreted in the urine. There is not a maximum rate of glucose filtration. Glucose should not be found in the urine. The kidneys do not regulate blood glucose. Cognitive Level: Comprehension 733 18. When teaching about sodium reabsorption, which information should the nurse include? The majority of sodium reabsorption takes place in the: a. Proximal tubule b. Loop of Henle c. Distal tubule d. Collecting duct ANS: A The majority of sodium reabsorption takes place in the proximal tubule. The majority of sodium reabsorption takes place in the proximal tubule, not the loop of Henle. The majority of sodium reabsorption takes place in the proximal tubule, not the distal tubule. The majority of sodium reabsorption takes place in the proximal tubule, not the collecting duct. Cognitive Level: Comprehension 733 19. A kidney has a glomerular capillary hydrostatic pressure of 50 mm Hg, a Bowman capsule hydrostatic pressure of 15 mm Hg, and a glomerular capillary oncotic pressure of 12 mm Hg. The net filtration pressure is mm Hg. a. 23 b. 27 c. 35 d. 38 ANS: A /aAdd the opposing factors: a Bowman capsule hydrostatic pressure of 15 mm Hg, and a glomerular capillary oncotic pressure of 12 mm Hg equals 27 and subtract it from the promoting factor of 50 mm Hg, for a total of 23. Cognitive Level: Comprehension 732 20. A nurse is preparing to teach about the loop of Henle. Which information should be included? The descending segment of the loop of Henle primarily allows for: a. Sodium secretion b. Potassium secretion c. Hydrogen ion reabsorption d. Water reabsorption ANS: D Water reabsorption occurs in the descending segment of the loop of Henle. Water reabsorption occurs in the loop of Henle; sodium is not affected. Water reabsorption occurs in the loop of Henle; potassium is not affected. Water reabsorption occurs in the loop of Henle; hydrogen ion reabsorption does not occur. Cognitive Level: Comprehension 734 21. When a staff member asks which of the following substances are actively secreted by the renal tubules, what is the nurses best response? a. Sodium and chlorine b. Phosphate and calcium c. Hydrogen and potassium d. Bicarbonate and carbonic acid ANS: C Principal cells reabsorb sodium and secrete potassium, and intercalated cells reabsorb potassium and bicarbonate and secrete hydrogen. Hydrogen and potassium are excreted, not sodium and chlorine. Hydrogen and potassium are excreted, not phosphate and calcium. Hydrogen and potassium are excreted, not bicarbonate and carbonic acid. Cognitive Level: Comprehension 734 22. A nurse is preparing to teach about the collecting ducts. Reabsorption of water in the collecting ducts requires which of these hormones? a. Antidiuretic hormone (ADH) b. Atrial natriuretic factor (ANP) c. Renin d. Aldosterone ANS: A ADH increases water permeability and reabsorption in the last segment of the distal tubule and along the entire length of the collecting ducts. ANP inhibits secretion of renin, inhibits angiotensin-induced secretion of aldosterone, relaxes vascular smooth muscle, and inhibits sodium and water absorption by kidney tubules. Renin is secreted to raise blood pressure. Aldosterone regulates water and sodium balance. Cognitive Level: Comprehension 734 23. When a patient asks what role the kidneys play in vitamin D function, how should the nurse reply? a. Synthesizes vitamin D from cholesterol b. Activates intestinally absorbed vitamin D c. Metabolizes and breaks down vitamin D d. Excretes excess vitamin D ANS: B The kidneys play a role in activating intestinally absorbed vitamin D. The kidneys play a role in activating intestinally absorbed vitamin D. They are not involved in synthesizing vitamin D from cholesterol. The kidneys play a role in activating intestinally absorbed vitamin D. They are not involved in metabolizing vitamin D. The kidneys play a role in activating intestinally absorbed vitamin D. They do not excrete excess vitamin D. Cognitive Level: Comprehension 736 24. A 35-year-old hypertensive male begins taking a diuretic. Which of the following common side effects of this medication should the nurse monitor? a. Hypokalemia b. Hyponatremia c. Increased uric acid secretion d. Hypermagnesemia ANS: A Hypokalemia is a side effect of diuretics. Hypokalemia, not hyponatremia, is a side effect of diuretic therapy. Diuretics promote uric acid retention, not excretion. Hypokalemia is a side effect of diuretics. Hypermagnesemia is not. Cognitive Level: Comprehension 736 25. A patient has searched the Internet for hormones. The patient has a good understanding when she knows that the hormone is synthesized and secreted by the kidneys to stimulate bone marrow production of red blood cells. a. Creatinine b. Aldosterone c. Erythropoietin d. Renin ANS: C Erythropoietin stimulates the bone marrow to produce red blood cells in response to tissue hypoxia. Erythropoietin, not creatinine, stimulates the bone marrow to produce red blood cells in response to tissue hypoxia. Erythropoietin, not aldosterone, stimulates the bone marrow to produce red blood cells in response to tissue hypoxia. Erythropoietin, not renin, stimulates the bone marrow to produce red blood cells in response to tissue hypoxia. Cognitive Level: Comprehension 736 26. If a nurse wants to obtain the best estimate of renal function, which test should the nurse monitor? a. Glomerular filtration rate (GFR) b. Circulating antidiuretic hormone (ADH) levels c. Volume of urine output d. Urine-specific gravity ANS: A The GFR provides the best estimate of functioning renal tissue. The GFR provides the best estimate of functioning renal tissue. Circulating ADH levels is not the best indicator. The GFR provides the best estimate of functioning renal tissue, not urine output. The GFR provides the best estimate of functioning renal tissue. Specific gravity is not the best indicator. Cognitive Level: Comprehension 736 27. A nurse recalls the glomerular filtration rate (GFR) and plasma creatinine (Pcr) concentration are related. a. Directly b. Indirectly c. Inversely d. Not ANS: C The GFR and Pcr are inversely related. The and Pcr are inversely, not directly, related. The GFR and Pcr are inversely, not indirectly, related. The GFR and Pcr are inversely related. Cognitive Level: Comprehension 737 MULTIPLE RESPONSE 1. When a student asks what the components of the nephron are, how should the nurse respond? The components of the nephron include (select all that apply): a. Loop of Henle b. Renal corpuscle c. Proximal tubule d. Renal pelvis e. Convoluted tubule ANS: A, B, C, E The nephron is a tubular structure with subunits that include the renal corpuscle, proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct, all of which contribute to the formation of final urine. Cognitive Level: Comprehension 726 2. When a staff member asks how the urine gets from the nephrons to the calyces, what is the nurses best response? The renal structure that drains directly into the calyces is (are) the (select all that apply): a. Distal tubule b. Collecting duct c. Pyramid d. Renal pelvis e. Loop of Henle ANS: A, B The urine formed by the nephrons flows from the distal tubules and collecting ducts through the duct of Bellini and the renal papillae into the calyces. Chapter 32. Alterations of Renal and Urinary Tract Function MULTIPLE CHOICE 1. A 25-year-old female is diagnosed with urinary tract obstruction. While planning care, the nurse realizes that the patient is expected to have hydronephrosis and a decreased glomerular filtration rate caused by: a. decreased renal blood flow. b. decreased peritubular capillary pressure. c. dilation of the renal pelvis and calyces proximal to a blockage. d. stimulation of antidiuretic hormone. ANS: C Hydronephrosis occurs due to dilation of the renal pelvis and calyces proximal to a blockage. Hydronephrosis is not the result of decreased renal blood flow. Hydronephrosis is not the result of decreased peritubular capillary pressure, but due to dilation of the renal pelvis. Hydronephrosis occurs due to dilation of the renal pelvis and calyces proximal to a blockage, not to stimulation of the antidiuretic hormone. Cognitive Level: Comprehension 741 2. A 27-year-old male has a severe kidney obstruction leading to removal of the affected kidney. Which of the following would the nurse expect to occur? a. Atrophy of the remaining kidney b. Compensatory hypertrophy of the remaining kidney c. Dysplasia in the remaining kidney d. Renal failure ANS: B The remaining kidney would hypertrophy to compensate for the increased workload of the loss of the affected kidney. The remaining kidney would enlarge, not atrophy. The remaining kidney would hypertrophy, not change cell structure. The remaining kidney would hypertrophy; the patient would not go into renal failure. Cognitive Level: Comprehension 742 3. A 55-year-old male presents reporting urinary retention. Tests reveal that he has a lower urinary tract obstruction. Which of the following is of most concern to the nurse? a. Vesicoureteral reflux and pyelonephritis b. Formation of renal calculi c. Glomerulonephritis d. Increased bladder compliance ANS: B Urine stasis occurs with urinary tract obstruction and can lead to the formation of renal calculi. Reflux and pyelonephritis would not lead to calculi as much as stasis. Glomerulonephritis would not lead to calculi formation. Increased compliance would not lead to calculi. Cognitive Level: Comprehension 743 4. When a patient asks what the most common type of renal stones is composed of, how should the nurse respond? The most common type of renal stone is composed of: a. magnesium. b. struvite. c. calcium. d. phosphate. ANS: C The most common composition of a renal stone is calcium, accounting for 70% to 80%. The most common composition of a renal stone is calcium, accounting for 70% to 80%. Only a limited number of stones are composed of magnesium. The most common composition of a renal stone is calcium, accounting for 70% to 80%. Struvite accounts for less than 10% to 15%. The most common composition of a renal stone is calcium, accounting for 70% to 80%. The percentage of phosphate is very low. Cognitive Level: Comprehension 743 5. While planning care for a patient with renal calculi, the nurse remembers the most important factor in renal calculus formation is: a. urine pH. b. body temperature. c. gender. d. serum mineral concentrations. ANS: A The most important factor in renal calculus formation is urine pH. The most important factor in renal calculus formation is urine pH, not body temperature. The most important factor in renal calculus formation is urine pH, not gender, although calculi form more often in men. The most important factor in renal calculus formation is urine pH, not serum mineral concentrations. Cognitive Level: Comprehension 743 6. A 24-year-old female is diagnosed with renal calculus that is causing obstruction. Which of the following symptoms would she most likely experience? a. Anuria b. Hematuria c. Pyuria d. Flank pain ANS: D Significant flank pain is the most common manifestation. Anuria does not occur. Hematuria does occur, but it is not the most common manifestation. Flank pain is the most common symptom; pyuria does not occur. Cognitive Level: Comprehension 743 7. A 25-year-old female presents with burning urination. She was diagnosed with a urinary tract infection. When the nurse checks the culture results, which of the following organisms is most likely infecting her urinary tract? a. Streptococcus b. Candida albicans c. Chlamydia d. Escherichia coli ANS: D The most common infecting microorganisms are uropathic strains of Escherichia coli. The most common infecting microorganisms are uropathic strains of Escherichia coli. Streptococcus in not a factor. The most common infecting microorganisms are uropathic strains of Escherichia coli, not Candida albicans. The most common infecting microorganisms are uropathic strains of Escherichia coli, not Chlamydia. Cognitive Level: Comprehension 748 8. A 35-year-old male received a traumatic brain injury in a motor vehicle accident. CT scan revealed a lesion above the pontine micturition center. Which of the following would the nurse expect? a. Dyssynergia b. Detrusor hyperreflexia c. Detrusor areflexia d. Detrusor sphincter dyssynergia ANS: B Neurologic disorders that develop above the pontine micturition center result in detrusor hyperreflexia, also known as an uninhibited or reflex bladder. Lesions that develop in upper motor neurons of the brain and spinal cord result in dyssynergia. Lesions that involve the sacral micturition center (below S1; may also be termed cauda equina syndrome) or peripheral nerve lesions result in detrusor areflexia (acontractile detrusor), a lower motor neuron disorder. Neurologic lesions that occur below the pontine micturition center but above the sacral micturition center (between C2 and S1) are also upper motor neuron lesions and result in detrusor hyperreflexia with vescico-sphincter dyssynergia. Cognitive Level: Comprehension 744 9. A 75-year-old male reports to his primary care provider loss of urine with cough, sneezing, or laughing. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Urge incontinence b. Stress incontinence c. Overflow incontinence d. Functional incontinence ANS: B Reduced resistance is associated with the symptom of stress incontinence, which is incontinence with coughing or sneezing. Urge incontinence is the inability to hold the urine when the urge is felt. There is coordination between the contracting bladder and the external sphincter, but the detrusor is too weak to empty the bladder, resulting in urinary retention with overflow or stress incontinence. Functional incontinence is similar to overflow and is not associated with coughing. Cognitive Level: Comprehension 745 10. A 19-year-old female was involved in a motor vehicle accident during which she sustained a closed head injury. She is now experiencing detrusor sphincter dyssynergia. Which of the following is the most beneficial medication treatment? a. Alpha blocker b. Beta blocker c. Vasodilator d. Diuretic ANS: A Because the bladder neck consists of circular smooth muscle with adrenergic innervation, detrusor sphincter dyssynergia may be managed by alpha-adrenergic blocking (antimuscarinic) medications. Because the bladder neck consists of circular smooth muscle with adrenergic innervation, detrusor sphincter dyssynergia may be managed by alpha-adrenergic blocking (antimuscarinic) medications, not beta blockers. Because the bladder neck consists of circular smooth muscle with adrenergic innervation, detrusor sphincter dyssynergia may be managed by alpha-adrenergic blocking (antimuscarinic) medications, not a vasodilator. Because the bladder neck consists of circular smooth muscle with adrenergic innervation, detrusor sphincter dyssynergia may be managed by alpha-adrenergic blocking (antimuscarinic) medications, not a diuretic. Cognitive Level: Comprehension 746 11. A nurse assesses a patient with a complicated urinary tract infection (UTI) for: a. Several species of bacteria b. Other health problems c. Urosepsis d. Rrethral obstruction ANS: B A complicated UTI develops when there is an abnormality in the urinary system or a health problem that compromises host defenses or response to treatment. UTI may occur alone or in association with pyelonephritis, prostatitis, or kidney stones. A complicated UTI develops when there is an abnormality in the urinary system or a health problem that compromises host defenses or response to treatment. UTI may occur alone or in association with pyelonephritis, prostatitis, or kidney stones. It is not due to the involvement of several species of bacteria. A complicated UTI develops when there is an abnormality in the urinary system or a health problem that compromises host defenses or response to treatment. UTI may occur alone or in association with pyelonephritis, prostatitis, or kidney stones. It does not always cause urosepsis. A complicated UTI develops when there is an abnormality in the urinary system or a health problem that compromises host defenses or response to treatment. UTI may occur alone or in association with pyelonephritis, prostatitis, or kidney stones. It does not always result in obstruction. Cognitive Level: Comprehension 747 12. A 28-year-old female presents with fever, chills, and flank pain. She is diagnosed with pyelonephritis. A nurse recalls the patients infection is located in the: a. Bladder b. Renal pelvis c. Renal tubules d. Glomerulus ANS: B Pyelonephritis is an infection of one or both upper urinary tracts (ureter, renal pelvis, and interstitium). Pyelonephritis is an infection of one or both upper urinary tracts (ureter, renal pelvis, and interstitium). It does not affect the bladder. Pyelonephritis is an infection of one or both upper urinary tracts (ureter, renal pelvis, and interstitium). It does not affect the tubules. Pyelonephritis is an infection of one or both upper urinary tracts (ureter, renal pelvis, and interstitium). It does not involve the glomerulus. Cognitive Level: Comprehension 749 13. While planning care for a patient who has acute pyelonephritis. A nurse recalls the most common condition associated with the development of acute pyelonephritis is: a. Cystitis b. Renal cancer c. Urinary tract obstruction d. Nephrotic syndrome ANS: C Urinary obstruction and reflux of urine from the bladder are the most common underlying risk factors. Urinary obstruction and reflux of urine from the bladder are the most common underlying risk factors. Cystitis is not a common risk factor. Urinary obstruction and reflux of urine from the bladder are the most common underlying risk factors. Renal cancer is not a common risk factor. Urinary obstruction and reflux of urine from the bladder are the most common underlying risk factors. Nephrotic syndrome is not a common risk factor. Cognitive Level: Comprehension 749 14. A 29-year-old female presents with cloudy urine, flank pain, hematuria, and fever. Which of the following does the nurse suspect the patient is most likely experiencing? a. Acute cystitis b. Renal calculi c. Chronic renal failure d. Postrenal renal failure ANS: A The patient is demonstrating symptoms of acute cystitis. Although renal calculi can cause pain and hematuria, it is not manifested by fever and cloudy urine. Chronic renal failure is not manifested by cloudy urine. Postrenal renal failure is not manifested by hematuria and cloudy urine. Cognitive Level: Comprehension 747 15. A 15-year-old male was diagnosed with pharyngitis. Eight days later he developed acute glomerulonephritis. While reviewing the culture results, which of the following is the most likely cause of this disease? a. Klebsiella b. Human immunodeficiency virus (HIV) c. Genital herpes virus d. Group A -hemolytic streptococcus ANS: D Group A -hemolytic streptococcus is the primary cause of glomerulonephritis associated with a pharyngeal infection. Group A -hemolytic streptococcus is the primary cause of glomerulonephritis associated with a pharyngeal infection. Klebsiella is not associated with pharyngitis. Group A -hemolytic streptococcus is the primary cause of glomerulonephritis associated with a pharyngeal infection. HIV is not associated with pharyngitis. Group A -hemolytic streptococcus is the primary cause of glomerulonephritis associated with a pharyngeal infection. Genital herpes is not associated with pharyngitis. Cognitive Level: Comprehension 753 16. A 25-year-old male was diagnosed with Goodpasture syndrome. While planning care for this patient, which of the following mechanisms would cause tissue injury? a. Viral infection of the Bowman capsule b. Production of antibodies against the glomerular basement membrane c. Antigen-antibody complex deposition with complement activation d. Abnormal activation of clotting factors and microclotting in the glomerulus ANS: B Antiglomerular basement membrane disease (Goodpasture syndrome) is associated with antibody formation against both pulmonary capillary and glomerular basement membranes. Antiglomerular basement membrane disease (Goodpasture syndrome) is associated with antibody formation against both pulmonary capillary and glomerular basement membranes. It is not due to a viral infection. Antiglomerular basement membrane disease (Goodpasture syndrome) is associated with antibody formation against both pulmonary capillary and glomerular basement membranes. It is not an antigen-antibody complex. Antiglomerular basement membrane disease (Goodpasture syndrome) is associated with antibody formation against both pulmonary capillary and glomerular basement membranes. It is not due to abnormal clotting. Cognitive Level: Comprehension 752 17. When a nurse observes poststreptococcal glomerulonephritis as a diagnosis on a patient, which principle will the nurse remember? Acute poststreptococcal glomerulonephritis is primarily caused by: a. Swelling of mesangial cells in the Bowman space in response to the presence of bacteria b. Antigen-antibody complex deposition in the glomerular capillaries and inflammatory damage c. Inflammatory factors that stimulate cellular proliferation of epithelial cells d. Accumulation of antiglomerular basement membrane antibodies ANS: B Acute poststreptococcal glomerulonephritis is caused by an antigen-antibody complex. Acute poststreptococcal glomerulonephritis is not due to swelling of the Bowman space. Acute poststreptococcal glomerulonephritis is caused by an antigen-antibody complex. It is not an inflammatory process. Acute poststreptococcal glomerulonephritis is caused by an antigen-antibody complex. Cognitive Level: Comprehension 752 18. A 30-year-old male is demonstrating hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin being the major protein. The most probable diagnosis the nurse will see documented on the chart is: a. Cystitis b. Chronic pyelonephritis c. Acute glomerulonephritis d. Renal calculi ANS: C Two major symptoms distinctive of more severe glomerulonephritis are: (1) hematuria with red blood cell casts and (2) proteinuria exceeding 3 to 5 g/day with albumin (macroalbuminuria) as the major protein. Cystitis is not a symptom of glomerulonephritis. Chronic pyelonephritis is manifested by dysuria, not proteinuria. Proteinuria is not seen with renal calculi. Cognitive Level: Comprehension 751 19. A 45-year-old male presents with oliguria. He is diagnosed with chronic glomerulonephritis. The nurse knows oliguria is related to: a. Thickening of the glomerular membrane and decreased renal blood flow b. Increased glomerular capillary oncotic pressure and tubular obstruction c. Activation of renin-angiotensin from decreased blood volume d. Vasoconstriction of the efferent arterioles ANS: A Changes in the glomerulus are characterized by progressive thickening and fibrosis of the glomerular basement membrane. Changes in the glomerulus are characterized by progressive thickening and fibrosis of the glomerular basement membrane; there is not tubular obstruction. The renin-angiotensin system is not activated in glomerulonephritis. The efferent arterioles are not affected in glomerulonephritis. Cognitive Level: Comprehension 751 20. A 54-year-old female is diagnosed with nephrotic syndrome. Which of the following is a common symptom of this disease? a. Hematuria b. Dysuria c. Oliguria d. Proteinuria ANS: D Nephrotic syndrome is manifested by proteinuria. Nephrotic syndrome is diagnosed when the protein level in a 24-hour urine collection is greater than 3.5 g. Proteinuria is the diagnostic criteria for nephrotic syndrome. The patient with nephrotic syndrome does not experience dysuria. The patient with nephrotic syndrome does not experience oliguria. Cognitive Level: Comprehension 753 21. A 42-year-old male is involved in a motor vehicle accident during which he loses a lot of blood. The nurse realizes he is in acute renal failure caused by: a. Kidney stones b. Immune complex deposition in the glomerulus c. Inadequate renal blood flow d. Obstruction of the proximal tubule ANS: C With blood loss, renal failure is due to inadequate blood flow. Kidney stones will lead to postrenal renal failure. Intrarenal renal failure is due to glomerular nephritis. Blood loss would not cause obstruction of the proximal tubule. Cognitive Level: Comprehension 754 22. A 35-year-old female was severely burned and is hospitalized. She is now suffering from acute tubular necrosis (ATN). Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Prerenal b. Intrarenal c. Extrarenal d. Postrenal ANS: B Intrarenal acute kidney failure is associated with several systemic diseases but is commonly related to ATN. Prerenal renal failure occurs anterior to the kidney. Extrarenal renal failure occurs outside the kidney. Postrenal is due to diseases that obstruct the flow of urine from the kidneys. Cognitive Level: Comprehension 755 23. A 56-year-old male presents with flank pain and polyuria. Tests reveal that he has an enlarged prostate. Which of the following types of renal failure should the nurse monitor for as it is the most likely to occur? a. Prerenal b. Intrarenal c. Extrarenal d. Postrenal ANS: D The patient will experience postrenal renal failure due to obstruction by the prostate. The patient will experience postrenal renal failure due to obstruction by the prostate. The patient will experience postrenal renal failure due to obstruction by the prostate. The patient will experience postrenal renal failure due to obstruction by the prostate. Cognitive Level: Comprehension 755 24. A 60-year-old male is diagnosed with renal failure. While the nurse is reviewing lab results, which of the following lab values would be most consistent with this diagnosis? a. Elevated plasma creatinine level b. Decreased plasma potassium level c. Metabolic alkalosis d. Increased urea clearance ANS: A Creatinine is constantly released from muscle and excreted primarily by glomerular filtration. In chronic kidney disease (CKD), as glomerular filtration rate (GFR) declines, the plasma creatinine level increases by a reciprocal amount to maintain a constant rate of excretion. As GFR continues to decline, plasma creatinine concentration increases. Creatinine is elevated; potassium is also elevated. Metabolic acidosis develops. Decreased urea clearance occurs. Cognitive Level: Comprehension 756 25. A 45-year-old female presents with hypertension, anorexia, nausea and vomiting, and anemia. She is diagnosed with chronic renal failure. When the patient asks what caused this anemia, how should the nurse respond? Your anemia is caused by: a. Red blood cells being lost in the urine b. Inadequate production of erythropoietin c. Inadequate iron absorption in the gut d. Red blood cells being injured as they pass through the glomerulus ANS: B The kidneys are inadequate in their production of erythropoietin. The kidneys are inadequate in their production of erythropoietin; red cells may be lost in the urine, but it is the lack of erythropoietin that leads to anemia. The kidneys are inadequate in their production of erythropoietin; it is not due to inadequate iron absorption. The kidneys are inadequate in their production of erythropoietin; it is not due to red cell destruction. Cognitive Level: Comprehension 758 26. A 42-year-old female is diagnosed with chronic renal failure, and the nurse is discussing dietary treatment. Which information indicates the nurse understands dietary regimen? Treatment includes restricting: a. Fats b. Complex carbohydrates c. Proteins d. Sugars ANS: C Low-protein diets are recommended. Low-protein diets, not reduced fats, are recommended. Low-protein diets, not reduced carbohydrates, are recommended. Low-protein diets, not reduced sugars, are recommended. Cognitive Level: Comprehension 760 27. While turning a patient with chronic renal failure, which principle should the nurse recall? Bone fractures are a risk factor in chronic renal failure because: a. Calcium is lost in the urine. b. Osteoblast activity is excessive. c. The kidneys fail to activate vitamin D. d. Autoantibodies to calcium molecules develop. ANS: C Hypocalcemia is accelerated by impaired renal synthesis of 1,25-vitamin D. The combined effect of vitamin D deficiency can result in renal osteodystrophies with increased risk for fractures. Hypocalcemia is accelerated by impaired renal synthesis of 1,25-vitamin D. The combined effect of vitamin D deficiency can result in renal osteodystrophies with increased risk for fractures. Calcium is not lost in the urine. Hypocalcemia is accelerated by impaired renal synthesis of 1,25-vitamin D. The combined effect of vitamin D deficiency can result in renal osteodystrophies with increased risk for fractures. Osteoblast activity is not accelerated. Hypocalcemia is accelerated by impaired renal synthesis of 1,25-vitamin D. The combined effect of vitamin D deficiency can result in renal osteodystrophies with increased risk for fractures. Antibodies do not develop. Cognitive Level: Comprehension 760 28. Anemia accompanies chronic renal failure because of: a. Blood loss via the urine b. Renal insensitivity to vitamin D c. Inadequate production of erythropoietin d. Inadequate retention of serum iron ANS: C Chronic renal failure leads to anemia because of declining erythropoietin production. Chronic renal failure leads to anemia because of declining erythropoietin production. It is not due to blood loss. Chronic renal failure leads to anemia because of declining erythropoietin production. It is not due to insensitivity to vitamin D. Chronic renal failure leads to anemia because of declining erythropoietin production. It is not due to inadequate retention of serum iron. Cognitive Level: Comprehension 760 29. A patient with end-stage renal disease has pruritus. When the patient asks what causes this, what is the nurses best response? Pruritus, seen in patients with end-stage renal disease, is caused by high levels of: a. Potassium b. Calcium c. Sodium d. Magnesium ANS: B Pruritus is related to high levels of calcium. Pruritus is related to high levels of calcium, not potassium. Pruritus is related to high levels of calcium, not sodium. Pruritus is related to high levels of calcium, not magnesium. Cognitive Level: Comprehension 760 MULTIPLE RESPONSE 1. When a nurse is teaching about urinary pathogens in men. Which information should the nurse include? Mechanisms for defense against urinary pathogens in men include (select all that apply): a. The long length of the urethra b. Alkaline pH of urine c. Secretion of mucus that traps bacteria d. Antimicrobial secretions from the prostate e. Implantation of the ureters in the bladder ANS: A, D Both the longer urethra and prostatic secretions decrease the risk of infection in men. The urine is not more alkaline, and they do not secrete mucus that traps bacteria. The ureters in men and women are implanted in similar positions and in their normal position; it is not a factor in the development of cystitis. Chapter 33. Alterations of Renal and Urinary Tract Function in Children MULTIPLE CHOICE 1. Upon examination of a male infant, it is determined that the urethral meatus is located on the undersurface of the penis. The nurse will document this condition as: a. Hypospadias b. Epispadias c. Hydroureter d. Cryptorchidism ANS: A When the urethral meatus is located on the undersurface of the penis, it is referred to as hypospadias. Epispadias occurs when the urethral meatus is on the dorsal surface of the penis. Hydroureter is not associated with the urethra. Cryptorchidism refers to undescended testes. Cognitive Level: Comprehension 765 2. A newborn female has chronic renal failure caused by a lack of development of one of the kidneys. When a staff member asks what this condition is called, how should the nurse respond? This condition is called: a. Renal dysplasia b. Renal agenesis c. Hypoplastic kidney d. Renal aplasia ANS: D During embryologic development, the ureteric duct grows into the metanephric tissue, triggering the formation of the kidneys. If this growth does not occur, the kidney is absent, a condition called renal aplasia. Renal dysplasia usually results from abnormal differentiation of the renal tissues. Renal agenesis is the absence of one or both kidneys. Hypoplastic kidney is small with a decreased number of nephrons. Cognitive Level: Comprehension 766 3. A nurse is preparing to teach about renal agenesis. Which information should the nurse include? Infants who have bilateral renal agenesis: a. Die within 1 year of birth b. Can expect to have a normal, healthy life c. Are stillborn or die within a few hours of birth d. Have structural abnormalities that can be corrected with surgery ANS: C Bilateral renal agenesis is a rare disorder incompatible with extrauterine life. Bilateral renal agenesis is a rare disorder incompatible with extrauterine life. The infant lives only a few hours. Bilateral renal agenesis is a rare disorder incompatible with extrauterine life. Bilateral renal agenesis is a rare disorder incompatible with extrauterine life. Cognitive Level: Comprehension 766 4. An infant male experiences a constant dribbling of urine. His urethral opening is located behind the glans. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Anterior epispadias b. Posterior epispadias c. Extrophy of the bladder d. Bladder outlet obstruction ANS: A Anterior epispadias occurs when the urethral opening is small and situated behind the glans. Posterior epispadias occurs when a fissure extends the entire length of the penis and into the bladder neck. Extrophy of the bladder occurs when the bladder is exposed on the abdominal wall. Bladder outlet obstruction occurs when urinary outflow is obstructed. Cognitive Level: Comprehension 765 5. A newborn male dies shortly after birth. Physical examination reveals wide-set eyes, parrot- beak nose, low-set ears, and receding chin. The most likely diagnosis the nurse will see on the chart is: a. Unilateral renal agenesis b. Potter syndrome c. Renal aplasia d. Renal dysplasia ANS: B Potter syndrome is manifested by wide-set eyes, parrot-beak nose, low-set ears, and receding chin. Unilateral renal agenesis occurs when one kidney is nonfunctioning, but it is not associated with other congenital anomalies, such as wide-set eyes and low-set ears. Renal aplasia is the abnormal growth of one kidney, but is not associated with other anomalies. Renal dysplasia is abnormal tissue growth in a kidney, but it is not associated with other anomalies. Cognitive Level: Comprehension 766 6. A 15-year-old female presents with flank pain, irritability, malaise, and fever. Tests reveal glomerulonephritis. When the parents ask what could have caused this, how should the nurse respond? a. Poststreptococcal infection b. Nephropathy c. Nephrotic syndrome d. Potter syndrome ANS: A Glomerulonephritis is most likely related to a post-strep infection. Glomerulonephritis is most likely related to a post-strep infection. It is not related to nephropathy. Glomerulonephritis is most likely related to a post-strep infection. It is not related to nephrotic syndrome Potter syndrome is incompatible with life. Cognitive Level: Comprehension 766 7. A urologist is discussing nephritic syndrome. Which information should be included? If nephrotic syndrome is not caused initially by kidney disease, it is termed nephrotic syndrome. a. Primary b. Secondary c. Tertiary d. Idiopathic ANS: B Secondary nephrotic syndrome is not caused initially by kidney disease. Secondary, not primary, nephrotic syndrome is not caused initially by kidney disease. Secondary, not tertiary, nephrotic syndrome is not caused initially by kidney disease. Secondary, not idiopathic, nephrotic syndrome is not caused initially by kidney disease. Cognitive Level: Comprehension 767 8. A 4-year-old male is diagnosed with nephrotic syndrome. Which of the following assessment findings accompanies this condition? a. Proteinuria b. Decreased blood urea nitrogen (BUN) c. Hematuria d. Sodium loss ANS: A Proteinuria accompanies nephrotic syndrome. Proteinuria accompanies nephrotic syndrome. The BUN may be elevated. Proteinuria, not hematuria, accompanies nephrotic syndrome. Proteinuria, not sodium loss, accompanies nephrotic syndrome. Cognitive Level: Comprehension 767 9. A 7-year-old female is diagnosed with nephrotic syndrome. Which of the following should the nurse ask the parents if they or the child has noticed recently? a. Sunken fontanelles b. Vesicular skin rash c. Frothy urine d. Jaundice ANS: C In the child with nephrotic syndrome, the parents may notice diminished, frothy, or foamy urine output. Parents may notice diminished, frothy, or foamy urine output, not sunken fontanelles. Parents may notice diminished, frothy, or foamy urine output, not a vesicular skin rash. Parents may notice diminished, frothy, or foamy urine output, not jaundice. Cognitive Level: Comprehension 767 10. Which of the following clusters of symptoms would make a clinician suspect a child has developed glomerulonephritis? a. Pyuria, fever, and abdominal pain b. Proteinuria, hypotension, and ascites c. Dysuria, urinary frequency, and abdominal tenderness d. Gross hematuria, flank pain, and hypertension ANS: D The child with glomerulonephritis typically experiences gross or microscopic hematuria, proteinuria, edema, renal insufficiency, flank pain, and hypertension. The child typically has gross or microscopic hematuria, proteinuria, edema, and renal insufficiency. Pyuria and abdominal pain are typically not present. The child may experience proteinuria, but also experiences hematuria. Dysuria and frequency are symptoms of cystitis. Cognitive Level: Comprehension 767 11. A 5-year-old male was diagnosed with glomerulonephritis. History reveals that he had an infection 3 weeks before the onset of this condition. The infection was most likely located in the: a. Bone b. Gastrointestinal (GI) tract c. Respiratory tract d. Ear ANS: C The location of the infection leading to glomerulonephritis is the respiratory tract. The location of the infection leading to glomerulonephritis is the respiratory tract, not the bone. The location of the infection leading to glomerulonephritis is the respiratory tract, not the GI tract. The location of the infection leading to glomerulonephritis is the respiratory tract, not the ear. 12. When a child is admitted with acute renal failure, a clinician realizes the most common cause of acute renal failure is: a. Glomerulonephritis b. Obstruction c. Nephrotic syndrome d. Hemolytic uremic syndrome (HUS) ANS: D HUS is the most common cause of acute renal failure in children. HUS is the most common cause of acute renal failure in children. Glomerulonephritis can lead to renal failure, but it is not the most common. HUS is the most common cause of acute renal failure in children. Obstruction is not a common cause. HUS is the most common cause of acute renal failure in children. Nephrotic syndrome could contribute to renal failure, but it is not the most common cause. REF: pp. 767-768 13. A 10-year-old male is diagnosed with glomerulonephritis. Tests reveal the deposition of immunoglobulin IgA in the glomerular capillaries. The nurse will monitor for recurrent: a. Infections b. Hematuria c. Vomiting d. Enuresis ANS: B The child with immunoglobulin associated with glomerulonephritis will have recurrent hematuria. The child with immunoglobulin associated with glomerulonephritis will have recurrent hematuria; infections do not reoccur. The child with immunoglobulin associated with glomerulonephritis will have recurrent hematuria, not vomiting. The child with immunoglobulin associated with glomerulonephritis will have recurrent hematuria, not enuresis. Cognitive Level: Comprehension 767 14. When a newborn is admitted with urinary tract infections (UTIs), which type of infection will the nurse look for in the newborn? a. Blood-borne infections b. Infections caused by bacteria from the gastrointestinal (GI) tract c. Yeast infections d. Viral infections ANS: A UTIs are rare in newborns, and when they do occur, they are usually caused by bacteria from the bloodstream that have settled in the urinary tract. UTIs are rare in newborns, and when they do occur, they are usually caused by bacteria from the bloodstream that have settled in the urinary tract. Older children might have bacteria from the GI tract, but not newborns. UTIs are rare in newborns, and when they do occur, they are usually caused by bacteria from the bloodstream that have settled in the urinary tract. Older children might have UTIs associated with yeast, but not newborns. UTIs are rare in newborns, and when they do occur, they are usually caused by bacteria from the bloodstream that have settled in the urinary tract. Newborns will not have infections secondary to viral infections. Cognitive Level: Comprehension 768 15. A 3-year-old female presents with recurrent urinary tract infections (UTIs), fever, poor growth and development, and feeding problems. Tests reveal a retrograde flow of urine from the urinary bladder into the ureters. When giving report to the oncoming shift, the nurse will call this condition: a. Vesicoureteral reflux (VUR) b. Vesicourethral reflux c. Vesicoureteral influx d. Hydronephrosis ANS: A VUR is the retrograde flow of urine from the bladder into the kidney or ureters, or both. VUR is the retrograde flow of urine from the bladder into the kidney or ureters, or both. It is ureteral, not urethral. VUR is the retrograde flow of urine from the bladder into the kidney or ureters, or both. It is reflux, not influx. VUR is the retrograde flow of urine from the bladder into the kidney or ureters, or both. Reflux could lead to pyelonephritis, not hydronephrosis. Cognitive Level: Comprehension 768 16. A nurse observes on the chart that a patient is admitted with Wilms tumors. A nurse knows the tumors are found in the: a. Kidneys b. Ureters c. Bladder d. Urethra ANS: A Wilms tumor is found in the kidneys. Wilms tumor is found in the kidneys, not the ureters. Wilms tumor is found in the kidneys, not the bladder. Wilms tumor is found in the kidneys, not the urethra. Cognitive Level: Comprehension 769 17. A 6-year-old male is experiencing urine reflux from the urinary bladder into a grossly dilated ureter and calyces. He was diagnosed with vesicoureteral reflux. This condition would be graded: a. I b. II c. III d. IV ANS: D The patient has symptoms of grade IV reflux. Grade I involves a non-dilated ureter. Grade II does not involve dilation. Grade III does not involve gross dilation. Cognitive Level: Comprehension 769 18. A 2-year-old male is diagnosed with Wilms tumor. Which of the following clinical conditions is often associated with this disease? a. Cystic disease of the liver b. Aniridia c. Anemia d. Hypothyroidism ANS: B Children with Wilms tumor often have other congenital anomalies, including aniridia, a lack of an iris in the eye. Children with Wilms tumor often have other congenital anomalies, including aniridia, a lack of an iris in the eye. They could have other anomalies, but cystic liver is not one. Children with Wilms tumor often have other congenital anomalies, including aniridia. They do not experience anemia. Children with Wilms tumor often have other congenital anomalies, including aniridia. They do not experience hypothyroidism. Cognitive Level: Comprehension 770 19. A 7-year-old male presents to his primary care provider for incontinence. His mother indicates that he has never been continent. Which of the following is the most likely diagnosis the nurse will observe on the chart? a. Nocturnal enuresis b. Diurnal enuresis c. Primary enuresis d. Secondary enuresis ANS: C Primary incontinence (enuresis) means the child has never been continent. Nocturnal enuresis is nighttime incontinence. Since the child has never been continent, the child has primary enuresis. With secondary incontinence the child would have had a period of continence, which this child did not; thus, he has primary enuresis. Cognitive Level: Comprehension 770 MULTIPLE RESPONSE 1. In addition to a mass, the child with Wilms tumor may also exhibit which assessment finding? (Select all that apply.) a. Abdominal pain b. Enuresis c. Hematuria d. Weight gain e. Fever ANS: A, C, E In addition to an abdominal mass, other presenting complaints include vague abdominal pain (37%), hematuria (18%), and fever (22%). Enuresis and weight gain do not occur. Chapter 34. Structure and Function of the Reproductive Systems MULTIPLE CHOICE 1. A nurse recalls the major hormonal determinant of sexual differentiation in utero is: a. Estrogen b. Progesterone c. Growth hormone d. Testosterone ANS: D Testosterone is necessary for the genital tubercle to differentiate into male genitalia; otherwise, female genitalia develop. Testosterone, not estrogen, determines sexual differentiation in utero. Testosterone, not progesterone, determines sexual differentiation in utero. Testosterone, not growth hormone, determines sexual differentiation in utero. Cognitive Level: Comprehension 775 2. A nurse is preparing to teach about puberty. Which information should the nurse include? One substance associated with puberty in males and females is the hormone: a. Follicle-stimulating hormone (FSH) b. Luteinizing hormone (LH) c. Leptin d. Estrogen ANS: C Leptin is associated with puberty. Leptin, not FSH, is associated with puberty. Leptin, not LH, is associated with puberty. Leptin, not estrogen, is associated with puberty. Cognitive Level: Comprehension 776 3. A nurse is discussing female anatomy. Which body structure contains the openings to the vagina and urinary meatus? a. Vestibule b. Mons pubis c. Introitus d. Perineal body ANS: A The vestibule contains the vagina and the urinary meatus. The vestibule contains the vagina and urinary meatus. The mons pubis is composed of fatty layer over the pubic symphysis. The introitus is the vaginal orifice. The perineal body is the area by the anus. Cognitive Level: Comprehension 778 4. While preparing to teach the staff about female anatomy, which information should be included? During the years that a woman is more likely to be sexually active, the vagina mucosa is protected from infection by: a. Presence of autoantibodies b. An acidic pH c. Low estrogen levels d. Douching ANS: B The acidic pH protects the vaginal mucosa from infection. The acidic pH, not the presence of autoantibodies, protects the vaginal mucosa. The acidic pH, not the presence of low estrogen, protects the vaginal mucosa. The acidic pH, not douching, protects the vaginal mucosa. Cognitive Level: Comprehension 779 5. When a staff member asks the nurse what the thick middle layer of the uterine wall is called, what is the nurses best response? The: a. Epithelial layer b. Endometrium c. Myometrium d. Perimetrium ANS: C The myometrium is the thick, muscular middle layer. It is thickest at the fundus, apparently to facilitate birth. The myometrium, not the epithelial layer, is the middle layer. The endometrium, or uterine lining, is composed of a functional layer (superficial compact layer and spongy middle layer), and a basal layer. The perimetrium is the outer layer. Cognitive Level: Comprehension 780 6. A nurse recalls the is lined with columnar epithelial cells. a. Perimetrium b. Endocervical canal c. Myometrium d. Vagina ANS: B The endocervical canal does not have an endometrial layer, but is lined with columnar epithelial cells. The perimetrium is a serous membrane. The myometrium is a muscular layer. The vagina is composed of epithelium. Cognitive Level: Comprehension 780 7. A nurse is preparing to teach about female anatomy. Which information should the nurse include? The female erectile organ that secretes smegma is called the: a. Introitus b. Bartholin glands c. Clitoris d. Labia minora ANS: C The clitoris is a richly innervated erectile organ between labia minora; it is a small, cylindric structure having a visible glans and a shaft that lies beneath the skin. It secretes smegma. The clitoris, not the introitus, secretes smegma. The clitoris, not the Bartholin glands, secretes smegma. The clitoris, not the labia minora, secretes smegma. Cognitive Level: Comprehension 780 8. A nurse is teaching about the menstrual cycle. Spinnbarkeit mucus is present during which stage of the menstrual cycle? a. Follicular b. Ovulation c. Luteal d. Menstrual ANS: B Spinnbarkeit mucus is present during ovulation. Spinnbarkeit mucus is present during ovulation, not the follicular stage. Spinnbarkeit mucus is present during ovulation, not the luteal stage. Spinnbarkeit mucus is present during ovulation, not the menstrual stage. Cognitive Level: Comprehension 782 9. When the nurse describes the duct that carries the ovum from the ovary to the uterus, what is the nurse discussing? The: a. Isthmus b. Corpus c. Endocervical canal d. Fallopian tube ANS: D The duct that carries the ovum is the fallopian tube. The duct that carries the ovum is the fallopian tube, not the isthmus, which is a portion of the cervix. The duct that carries the ovum is the fallopian tube, not the corpus, which is the body of the uterus. The duct that carries the ovum is the fallopian tube, not the endocervical canal, which is the area between the internal and external os of the cervix. Cognitive Level: Comprehension 782 10. A nurse is teaching the staff about female hormones. Which hormone promotes the formation of channels in the mucus of the cervical os to facilitate sperm movement into the uterus? a. LH b. FSH c. Progesterone d. Estrogen ANS: D Increasing estrogen levels apparently contribute to the development of tiny channels in cervical mucus, providing access for sperm into the interior of the uterus. It is estrogen, not LH, that provides access for sperm movement. It is estrogen, not FSH, that provides access for sperm movement. It is estrogen, not progesterone, that provides access for sperm movement. Cognitive Level: Comprehension 787 11. When a patient who is trying to get pregnant asks where the usual site of fertilization is, how should the nurse respond? The: a. Uterus b. Fimbriae c. Ampulla of the fallopian tubes d. Os of the fallopian tubes ANS: C The ampulla, or distal third, of the fallopian tube is the usual site of fertilization. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization; implantation happens in the uterus. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization; the fimbriae move the egg forward. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization, not the os. Cognitive Level: Comprehension 791 12. A nurse is teaching about the female anatomy. Which information should the nurse include? Cells of the have receptors for gonadotropins. a. Uterus b. Breast c. Ovary d. Vagina ANS: C The ovaries contain receptors for gonadotropins. The ovaries, not the uterus, contain receptors for gonadotropins. The ovaries, not the breast, contain receptors for gonadotropins. The ovaries, not the vagina, contain receptors for gonadotropins. Cognitive Level: Comprehension 786 13. The nurse is preparing to teach the staff about female anatomy. Which information should the nurse include? The ova are contained within the ovarian: a. Corpus luteum b. Follicle c. Stroma d. Infundibulum ANS: B The ova are contained in the ovarian follicle. The ova are contained in the ovarian follicle, not the luteum. The ova are contained in the ovarian follicle, not the stroma. The ova are contained in the ovarian follicle, not the infundibulum. Cognitive Level: Comprehension 786 14. Which information indicates the nurse has a good understanding of female anatomy? Having ejected a mature ovum, the ovarian follicle then develops into: a. An atretic follicle b. A theca cell c. A corpus luteum d. Scar tissue ANS: C Having ejected a mature ovum, the follicle develops into another structure, the corpus luteum. Having ejected a mature ovum, the follicle develops into another structure, the corpus luteum, not an atretic follicle. A theca cell is a cell in the ovarian follicle. The follicle develops into the corpus luteum, not scar tissue. Cognitive Level: Comprehension 787 15. When a staff member asks the nurse what is the most potent of the following estrogens, what is the nurses best response? It is: a. Estradiol b. Testosterone c. Estrone d. Estriol ANS: A Estradiol is the most potent of the estrogens. Testosterone is not an estrogen. Estradiol is the most potent of the estrogens, not estrone. Estradiol is the most potent of the estrogens, not estriol. 16. hWich information indicates the nurse has a good understanding of progesterone? Progesterone is primarily secreted by the: a. Follicle b. Corpus luteum c. Granulose cells d. Anterior pituitary ANS: B LH from the anterior pituitary stimulates the corpus luteum to secrete progesterone. The corpus luteum secretes progesterone, not the follicle. The corpus luteum secretes progesterone, not the granulose cells. The anterior pituitary secretes LH, which stimulates the corpus luteum to secrete progesterone. Cognitive Level: Comprehension 794 17. A 56-year-old female is in menopause. She has ovarian failure. While checking the lab results, which of the following will the nurse find? a. Increased FSH b. Increased estrogen c. Decreased GnRH d. Decreased LH ANS: A Menopause is characterized by loss of ovarian function, low estrogen and progesterone levels, and high FSH and LH levels. Estrogen is decreased. GnRH is increased. LH is increased. Cognitive Level: Comprehension 794 18. Progesterone is often referred to as the hormone of pregnancy, and the patient asks what this phrase means. How should the nurse respond? Progesterone is the hormone of pregnancy because it: a. Stimulates lactation b. Increases ciliary action in the fallopian tubes c. Thins the endometrium d. Prevents smooth muscle contraction of the uterus ANS: D Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not stimulate lactation. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not increase ciliary action in the fallopian tubes. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not thin the endometrium. Cognitive Level: Comprehension 784 19. When the nurse is teaching about the menstrual cycle, which information should be included? Menstruation is followed by the phase of the menstrual cycle. a. Follicular b. Luteal c. Secretory d. Ischemic ANS: A Menstruation is followed by the follicular/proliferative phase. Menstruation is followed by the follicular phase, not luteal. Menstruation is followed by the follicular phase, not secretory. Menstruation is followed by the follicular phase, not ischemic. REF: pp. 784-785 20. Which information indicates the nurse has a good understanding of the menstrual cycle? When estrogen and progesterone levels drop, the endometrium enters the phase. a. Proliferative b. Luteal c. Menstrual d. Recovery ANS: C Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the proliferative phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the luteal phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the recovery phase. REF: pp. 785-786 21. A staff member asks the nurse when ovulation occurs. What is the nurses best response? During the menstrual cycle, ovulation occurs when: a. There is a gradual decrease in estrogen levels. b. Inhibin B sharply spikes. c. A surge in progesterone occurs. d. Activin is released. ANS: B Inhibin B is primarily secreted in the follicular phase of the cycle, but sharply spikes when ovulation occurs. Ovulation is associated with inhibin not estrogen. Ovulation is associated with inhibin B, not a surge in progesterone. Ovulation is associated with inhibin B, not the release of activin. Cognitive Level: Comprehension 786 22. A nurse remembers the LH surge transforms granulosa cells into: a. Theca cells b. Corpus luteal cells c. Ova d. Fibroblasts ANS: B The FSH and LH surge also transforms the granulosa cells of the ovulatory follicle into the corpus luteum. The granulosa cells are transformed into corpus luteal cells, not theca cells. The granulosa cells are transformed into corpus luteal cells, not the ova. The granulosa cells are transformed into corpus luteal cells, not fibroblasts. Cognitive Level: Comprehension 786 23. A nurse is teaching about female hormones. Which information should the nurse include? Endometrial thickening during the proliferative phase is stimulated by increased levels of: a. Estrogen b. Progesterone c. FSH d. Inhibin ANS: A Estrogen promotes endometrial thickening. Estrogen, not progesterone, promotes endometrial thickening. Estrogen, not FSH, promotes endometrial thickening. Estrogen, not inhibin, promotes endometrial thickening. Cognitive Level: Comprehension 784 24. A student asks the instructor which of the following hormones stimulates follicular maturation. How should the instructor respond? a. Activin b. Inhibin c. LH d. Follistatin ANS: A Activin stimulates the secretion of FSH and follicular maturation. Activin, not inhibin, stimulates the secretion of FSH and follicular maturation. Activin, not LH, stimulates the secretion of FSH and follicular maturation. Activin, not follistatin, stimulates the secretion of FSH and follicular maturation. Cognitive Level: Comprehension 786 25. Changes in the cervical mucus can be used to identify the periods in which a female is most fertile. How should the nurse describe cervical mucus during ovulation? a. Blood-tinged b. Thin and watery c. Absent d. Abundant and elastic ANS: D Cervical mucus becomes abundant and more elastic during ovulation. Cervical mucus becomes abundant and more elastic during ovulation, not blood-tinged. Cervical mucus becomes abundant and more elastic during ovulation, not thin and watery. Cervical mucus becomes abundant and more elastic during ovulation, not absent. Cognitive Level: Comprehension 787 26. A clinician is preparing to teach about spermatogenesis. Which information should the clinician include? Spermatogenesis occurs in the: a. Epididymis b. Inguinal canals c. Seminiferous tubules d. Vas deferens ANS: C Spermatogenesis takes place within the seminiferous tubules of the testes. Spermatogenesis takes place within the seminiferous tubules of the testes, not the epididymis. Spermatogenesis takes place within the seminiferous tubules of the testes, not the inguinal canals. Spermatogenesis takes place within the seminiferous tubules of the testes, not the vas deferens. Cognitive Level: Comprehension 792 27. When a nurse is describing the male anatomy, which paired glands lie posterior to the urinary bladder in the male? a. Seminal vesicles b. Prostate glands c. Cowper glands d. Parabladder glands ANS: A The seminal vesicles are glands about 4 to 6 cm long that lie behind the urinary bladder and in front of the rectum. The prostate glands surround the urethra. The Cowper glands run close to the urethra. The parabladder is not a gland. Cognitive Level: Comprehension 791 28. A patient asks the nurse what is the most sensitive area of the penis. What is the nurses best answer? The area of the penis with the most nerve endings is the: a. Foreskin b. Glans c. Corpora cavernosa d. Corpus spongiosum ANS: B Stimulation of the glans, which is endowed with copious sensitive nerve endings, provides maximum erotic sensation. The glans, not the foreskin, has the most nerve endings. The corpora cavernosa lengthens during arousal, but is not the most sensitive. The corpus spongiosum contains the urethra and is not the most sensitive. Cognitive Level: Comprehension 791 29. What term should the nurse use when discussing male sex hormones collectively? a. Gonadotropins b. Testosterones c. Catabolic steroids d. Androgens ANS: D The male sex hormones are androgens. The male sex hormones are androgens, not gonadotropins. The male sex hormones are androgens, not testosterones. The male sex hormones are androgens, not catabolic steroids. Cognitive Level: Comprehension 792 30. When discussing the difference between male and female sex hormones, which information should the nurse include? The major difference between male and female sex hormone production is that: a. LH has no apparent action in the male. b. Sex hormone production in the male is relatively constant. c. Estrogen is not produced in the male. d. In the male, GnRH does not cause the release of FSH. ANS: B In men, sex hormone production is relatively constant and does not occur in a cyclic pattern, as it does in women. In men, sex hormone production is relatively constant. LH has action in the male as it stimulates testosterone. Estrogen is present in the male in regard to the lack of breast development. In the male, GnRH causes the release of FSH. Cognitive Level: Comprehension 792 31. A nursing student asks the nurse where the glands of Montgomery are located. How should the nurse reply? The glands of Montgomery are located in the: a. Testes b. Breasts c. Uterus d. Vagina ANS: B The glands of Montgomery are located in the breasts. The glands of Montgomery are located in the breasts, not the testes. The glands of Montgomery are located in the breasts, not the uterus. The glands of Montgomery are located in the breasts, not the vagina. Cognitive Level: Comprehension 788 32. When a staff member asks which structure secretes glucose-rich fluid into the semen, how should the nurse respond? a. Seminal vesicles b. Ejaculatory duct c. Prostate gland d. Cowper gland ANS: A The ducts of the seminal vesicles join the ampulla of the vas deferens to become the ejaculatory duct, which contracts rhythmically during emission and ejaculation. The seminal vesicles, not the ejaculatory duct, secrete fluid into the semen. The seminal vesicles, not the prostate, secrete fluid into the semen. The seminal vesicles, not the Cowper gland, secrete fluid into the semen. The Cowper gland secretes the last fluid into the ejaculate. Cognitive Level: Comprehension 791 33. When a teenager asks what makes the breast grow, what is the nurses best response? The hormone that promotes breast development during puberty is: a. Progesterone b. Prolactin c. Oxytocin d. Estradiol ANS: D Estradiol promotes breast development. Estradiol promotes breast development, not progesterone. Estradiol promotes breast development, not prolactin. Estradiol promotes breast development, not oxytocin. Cognitive Level: Comprehension 776 34. When a breastfeeding mom asks what causes letdown, which information should the nurse give the patient? The hormone that plays a role in breast milk ejection (letdown) during lactation is: a. Cortisol b. Prolactin c. Oxytocin d. Progesterone ANS: C Oxytocin controls milk ejection (letdown) from acini cells. Oxytocin controls milk ejection, not cortisol. Oxytocin controls milk ejection, not prolactin. Oxytocin controls milk ejection, not progesterone. Cognitive Level: Comprehension 788 35. While speaking to a group of older males, which information should the nurse share? The following is a normal characteristic of aging and the male reproductive system: a. Changes in libido are not related to health status. b. Tissue responsiveness to testosterone is increased. c. Testicles will hypertrophy. d. Refractory time after ejaculation is prolonged. ANS: D Men can expect a prolonged refractory time after ejaculation. Changes in libido are related to health changes. Responsiveness to testosterone is decreased. The testicles undergo atrophy. Cognitive Level: Comprehension 795 MULTIPLE RESPONSE 1. The nurse is discussing information about menopause with an older woman. Which of the following characteristics are associated with declining ovarian function with age? (Select all that apply.) a. Vasomotor flush b. Decline in bone mass c. Decreased risk of coronary disease d. Atrophy of the uterus e. Dysfunctional uterine bleeding ANS: A, B, D, E Aging women can expect to experience vasomotor flashing, decline in bone mass, atrophy of the uterus, and dysfunctional uterine bleeding. Cardiovascular risk increases, not decreases. Chapter 35. Alterations of the Female Reproductive System MULTIPLE CHOICE 1. A nurse recalls the major hormonal determinant of sexual differentiation in utero is: a. Estrogen b. Progesterone c. Growth hormone d. Testosterone ANS: D Testosterone is necessary for the genital tubercle to differentiate into male genitalia; otherwise, female genitalia develop. Testosterone, not estrogen, determines sexual differentiation in utero. Testosterone, not progesterone, determines sexual differentiation in utero. Testosterone, not growth hormone, determines sexual differentiation in utero. Cognitive Level: Comprehension 775 2. A nurse is preparing to teach about puberty. Which information should the nurse include? One substance associated with puberty in males and females is the hormone: a. Follicle-stimulating hormone (FSH) b. Luteinizing hormone (LH) c. Leptin d. Estrogen ANS: C Leptin is associated with puberty. Leptin, not FSH, is associated with puberty. Leptin, not LH, is associated with puberty. Leptin, not estrogen, is associated with puberty. Cognitive Level: Comprehension 776 3. A nurse is discussing female anatomy. Which body structure contains the openings to the vagina and urinary meatus? a. Vestibule b. Mons pubis c. Introitus d. Perineal body ANS: A The vestibule contains the vagina and the urinary meatus. The vestibule contains the vagina and urinary meatus. The mons pubis is composed of fatty layer over the pubic symphysis. The introitus is the vaginal orifice. The perineal body is the area by the anus. Cognitive Level: Comprehension 778 4. While preparing to teach the staff about female anatomy, which information should be included? During the years that a woman is more likely to be sexually active, the vagina mucosa is protected from infection by: a. Presence of autoantibodies b. An acidic pH c. Low estrogen levels d. Douching ANS: B The acidic pH protects the vaginal mucosa from infection. The acidic pH, not the presence of autoantibodies, protects the vaginal mucosa. The acidic pH, not the presence of low estrogen, protects the vaginal mucosa. The acidic pH, not douching, protects the vaginal mucosa. Cognitive Level: Comprehension 779 5. When a staff member asks the nurse what the thick middle layer of the uterine wall is called, what is the nurses best response? The: a. Epithelial layer b. Endometrium c. Myometrium d. Perimetrium ANS: C The myometrium is the thick, muscular middle layer. It is thickest at the fundus, apparently to facilitate birth. The myometrium, not the epithelial layer, is the middle layer. The endometrium, or uterine lining, is composed of a functional layer (superficial compact layer and spongy middle layer), and a basal layer. The perimetrium is the outer layer. Cognitive Level: Comprehension 780 6. A nurse recalls the is lined with columnar epithelial cells. a. Perimetrium b. Endocervical canal c. Myometrium d. Vagina ANS: B The endocervical canal does not have an endometrial layer, but is lined with columnar epithelial cells. The perimetrium is a serous membrane. The myometrium is a muscular layer. The vagina is composed of epithelium. Cognitive Level: Comprehension 780 7. A nurse is preparing to teach about female anatomy. Which information should the nurse include? The female erectile organ that secretes smegma is called the: a. Introitus b. Bartholin glands c. Clitoris d. Labia minora ANS: C The clitoris is a richly innervated erectile organ between labia minora; it is a small, cylindric structure having a visible glans and a shaft that lies beneath the skin. It secretes smegma. The clitoris, not the introitus, secretes smegma. The clitoris, not the Bartholin glands, secretes smegma. The clitoris, not the labia minora, secretes smegma. Cognitive Level: Comprehension 780 8. A nurse is teaching about the menstrual cycle. Spinnbarkeit mucus is present during which stage of the menstrual cycle? a. Follicular b. Ovulation c. Luteal d. Menstrual ANS: B Spinnbarkeit mucus is present during ovulation. Spinnbarkeit mucus is present during ovulation, not the follicular stage. Spinnbarkeit mucus is present during ovulation, not the luteal stage. Spinnbarkeit mucus is present during ovulation, not the menstrual stage. Cognitive Level: Comprehension 782 9. When the nurse describes the duct that carries the ovum from the ovary to the uterus, what is the nurse discussing? The: a. Isthmus b. Corpus c. Endocervical canal d. Fallopian tube ANS: D The duct that carries the ovum is the fallopian tube. The duct that carries the ovum is the fallopian tube, not the isthmus, which is a portion of the cervix. The duct that carries the ovum is the fallopian tube, not the corpus, which is the body of the uterus. The duct that carries the ovum is the fallopian tube, not the endocervical canal, which is the area between the internal and external os of the cervix. Cognitive Level: Comprehension 782 10. A nurse is teaching the staff about female hormones. Which hormone promotes the formation of channels in the mucus of the cervical os to facilitate sperm movement into the uterus? a. LH b. FSH c. Progesterone d. Estrogen ANS: D Increasing estrogen levels apparently contribute to the development of tiny channels in cervical mucus, providing access for sperm into the interior of the uterus. It is estrogen, not LH, that provides access for sperm movement. It is estrogen, not FSH, that provides access for sperm movement. It is estrogen, not progesterone, that provides access for sperm movement. Cognitive Level: Comprehension 787 11. When a patient who is trying to get pregnant asks where the usual site of fertilization is, how should the nurse respond? The: a. Uterus b. Fimbriae c. Ampulla of the fallopian tubes d. Os of the fallopian tubes ANS: C The ampulla, or distal third, of the fallopian tube is the usual site of fertilization. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization; implantation happens in the uterus. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization; the fimbriae move the egg forward. The ampulla, or distal third, of the fallopian tube is the usual site of fertilization, not the os. Cognitive Level: Comprehension 791 12. A nurse is teaching about the female anatomy. Which information should the nurse include? Cells of the have receptors for gonadotropins. a. Uterus b. Breast c. Ovary d. Vagina ANS: C The ovaries contain receptors for gonadotropins. The ovaries, not the uterus, contain receptors for gonadotropins. The ovaries, not the breast, contain receptors for gonadotropins. The ovaries, not the vagina, contain receptors for gonadotropins. Cognitive Level: Comprehension 786 13. The nurse is preparing to teach the staff about female anatomy. Which information should the nurse include? The ova are contained within the ovarian: a. Corpus luteum b. Follicle c. Stroma d. Infundibulum ANS: B The ova are contained in the ovarian follicle. The ova are contained in the ovarian follicle, not the luteum. The ova are contained in the ovarian follicle, not the stroma. The ova are contained in the ovarian follicle, not the infundibulum. Cognitive Level: Comprehension 786 14. Which information indicates the nurse has a good understanding of female anatomy? Having ejected a mature ovum, the ovarian follicle then develops into: a. An atretic follicle b. A theca cell c. A corpus luteum d. Scar tissue ANS: C Having ejected a mature ovum, the follicle develops into another structure, the corpus luteum. Having ejected a mature ovum, the follicle develops into another structure, the corpus luteum, not an atretic follicle. A theca cell is a cell in the ovarian follicle. The follicle develops into the corpus luteum, not scar tissue. Cognitive Level: Comprehension 787 15. When a staff member asks the nurse what is the most potent of the following estrogens, what is the nurses best response? It is: a. Estradiol b. Testosterone c. Estrone d. Estriol ANS: A Estradiol is the most potent of the estrogens. Testosterone is not an estrogen. Estradiol is the most potent of the estrogens, not estrone. Estradiol is the most potent of the estrogens, not estriol. Cognitive Level: Comprehension 787 16. Which information indicates the nurse has a good understanding of progesterone? Progesterone is primarily secreted by the: a. Follicle b. Corpus luteum c. Granulose cells d. Anterior pituitary ANS: B LH from the anterior pituitary stimulates the corpus luteum to secrete progesterone. The corpus luteum secretes progesterone, not the follicle. The corpus luteum secretes progesterone, not the granulose cells. The anterior pituitary secretes LH, which stimulates the corpus luteum to secrete progesterone. Cognitive Level: Comprehension 794 17. A 56-year-old female is in menopause. She has ovarian failure. While checking the lab results, which of the following will the nurse find? a. Increased FSH b. Increased estrogen c. Decreased GnRH d. Decreased LH ANS: A Menopause is characterized by loss of ovarian function, low estrogen and progesterone levels, and high FSH and LH levels. Estrogen is decreased. GnRH is increased. LH is increased. Cognitive Level: Comprehension 794 18. Progesterone is often referred to as the hormone of pregnancy, and the patient asks what this phrase means. How should the nurse respond? Progesterone is the hormone of pregnancy because it: a. Stimulates lactation b. Increases ciliary action in the fallopian tubes c. Thins the endometrium d. Prevents smooth muscle contraction of the uterus ANS: D Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not stimulate lactation. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not increase ciliary action in the fallopian tubes. Progesterone is sometimes called the hormone of pregnancy because it relaxes smooth muscle in the myometrium, which prevents premature contractions and helps the uterus to expand. It does not thin the endometrium. Cognitive Level: Comprehension 784 19. When the nurse is teaching about the menstrual cycle, which information should be included? Menstruation is followed by the phase of the menstrual cycle. a. Follicular b. Luteal c. Secretory d. Ischemic ANS: A Menstruation is followed by the follicular/proliferative phase. Menstruation is followed by the follicular phase, not luteal. Menstruation is followed by the follicular phase, not secretory. Menstruation is followed by the follicular phase, not ischemic. REF: pp. 784-785 20. Which information indicates the nurse has a good understanding of the menstrual cycle? When estrogen and progesterone levels drop, the endometrium enters the phase. a. Proliferative b. Luteal c. Menstrual d. Recovery ANS: C Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the proliferative phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the luteal phase. Without progesterone or estrogen to maintain it, the endometrium enters the ischemic (blood- starved) phase and disintegrates, the ischemic/menstrual phase, not the recovery phase. REF: pp. 785-786 21. A staff member asks the nurse when ovulation occurs. What is the nurses best response? During the menstrual cycle, ovulation occurs when: a. There is a gradual decrease in estrogen levels. b. Inhibin B sharply spikes. c. A surge in progesterone occurs. d. Activin is released. ANS: B Inhibin B is primarily secreted in the follicular phase of the cycle, but sharply spikes when ovulation occurs. Ovulation is associated with inhibin not estrogen. Ovulation is associated with inhibin B, not a surge in progesterone. Ovulation is associated with inhibin B, not the release of activin. Cognitive Level: Comprehension 786 22. A nurse remembers the LH surge transforms granulosa cells into: a. Theca cells b. Corpus luteal cells c. Ova d. Fibroblasts ANS: B The FSH and LH surge also transforms the granulosa cells of the ovulatory follicle into the corpus luteum. The granulosa cells are transformed into corpus luteal cells, not theca cells. The granulosa cells are transformed into corpus luteal cells, not the ova. The granulosa cells are transformed into corpus luteal cells, not fibroblasts. Cognitive Level: Comprehension 786 23. A nurse is teaching about female hormones. Which information should the nurse include? Endometrial thickening during the proliferative phase is stimulated by increased levels of: a. Estrogen b. Progesterone c. FSH d. Inhibin ANS: A Estrogen promotes endometrial thickening. Estrogen, not progesterone, promotes endometrial thickening. Estrogen, not FSH, promotes endometrial thickening. Estrogen, not inhibin, promotes endometrial thickening. Cognitive Level: Comprehension 784 24. A student asks the instructor which of the following hormones stimulates follicular maturation. How should the instructor respond? a. Activin b. Inhibin c. LH d. Follistatin ANS: A Activin stimulates the secretion of FSH and follicular maturation. Activin, not inhibin, stimulates the secretion of FSH and follicular maturation. Activin, not LH, stimulates the secretion of FSH and follicular maturation. Activin, not follistatin, stimulates the secretion of FSH and follicular maturation. Cognitive Level: Comprehension 786 25. Changes in the cervical mucus can be used to identify the periods in which a female is most fertile. How should the nurse describe cervical mucus during ovulation? a. Blood-tinged b. Thin and watery c. Absent d. Abundant and elastic ANS: D Cervical mucus becomes abundant and more elastic during ovulation. Cervical mucus becomes abundant and more elastic during ovulation, not blood-tinged. Cervical mucus becomes abundant and more elastic during ovulation, not thin and watery. Cervical mucus becomes abundant and more elastic during ovulation, not absent. Chapter 36. Alterations of the Male Reproductive System MULTIPLE CHOICE 1. A clinician is preparing to teach about spermatogenesis. Which information should the clinician include? Spermatogenesis occurs in the: a. Epididymis b. Inguinal canals c. Seminiferous tubules d. Vas deferens ANS: C Spermatogenesis takes place within the seminiferous tubules of the testes. Spermatogenesis takes place within the seminiferous tubules of the testes, not the epididymis. Spermatogenesis takes place within the seminiferous tubules of the testes, not the inguinal canals. Spermatogenesis takes place within the seminiferous tubules of the testes, not the vas deferens. 2. When a nurse is describing the male anatomy, which paired glands lie posterior to the urinary bladder in the male? a. Seminal vesicles b. Prostate glands c. Cowper glands d. Parabladder glands ANS: A The seminal vesicles are glands about 4 to 6 cm long that lie behind the urinary bladder and in front of the rectum. The prostate glands surround the urethra. The Cowper glands run close to the urethra. The parabladder is not a gland. 3. A patient asks the nurse what is the most sensitive area of the penis. What is the nurses best answer? The area of the penis with the most nerve endings is the: a. Foreskin b. Glans c. Corpora cavernosa d. Corpus spongiosum ANS: B Stimulation of the glans, which is endowed with copious sensitive nerve endings, provides maximum erotic sensation. The glans, not the foreskin, has the most nerve endings. The corpora cavernosa lengthens during arousal, but is not the most sensitive. The corpus spongiosum contains the urethra and is not the most sensitive. 4. What term should the nurse use when discussing male sex hormones collectively? a. Gonadotropins b. Testosterones c. Catabolic steroids d. Androgens ANS: D The male sex hormones are androgens. The male sex hormones are androgens, not gonadotropins. The male sex hormones are androgens, not testosterones. The male sex hormones are androgens, not catabolic steroids. 5. When discussing the difference between male and female sex hormones, which information should the nurse include? The major difference between male and female sex hormone production is that: a. LH has no apparent action in the male. b. Sex hormone production in the male is relatively constant. c. Estrogen is not produced in the male. d. In the male, GnRH does not cause the release of FSH. ANS: B In men, sex hormone production is relatively constant and does not occur in a cyclic pattern, as it does in women. In men, sex hormone production is relatively constant. LH has action in the male as it stimulates testosterone. Estrogen is present in the male in regard to the lack of breast development. In the male, GnRH causes the release of FSH. 6. A nursing student asks the nurse where the glands of Montgomery are located. How should the nurse reply? The glands of Montgomery are located in the: a. Testes b. Breasts c. Uterus d. Vagina ANS: B The glands of Montgomery are located in the breasts. The glands of Montgomery are located in the breasts, not the testes. The glands of Montgomery are located in the breasts, not the uterus. The glands of Montgomery are located in the breasts, not the vagina. 7. When a staff member asks which structure secretes glucose-rich fluid into the semen, how should the nurse respond? a. Seminal vesicles b. Ejaculatory duct c. Prostate gland d. Cowper gland ANS: A The ducts of the seminal vesicles join the ampulla of the vas deferens to become the ejaculatory duct, which contracts rhythmically during emission and ejaculation. The seminal vesicles, not the ejaculatory duct, secrete fluid into the semen. The seminal vesicles, not the prostate, secrete fluid into the semen. The seminal vesicles, not the Cowper gland, secrete fluid into the semen. The Cowper gland secretes the last fluid into the ejaculate. 8. When a teenager asks what makes the breast grow, what is the nurses best response? The hormone that promotes breast development during puberty is: a. Progesterone b. Prolactin c. Oxytocin d. Estradiol ANS: D Estradiol promotes breast development. Estradiol promotes breast development, not progesterone. Estradiol promotes breast development, not prolactin. Estradiol promotes breast development, not oxytocin. 9. When a breastfeeding mom asks what causes letdown, which information should the nurse give the patient? The hormone that plays a role in breast milk ejection (letdown) during lactation is: a. Cortisol b. Prolactin c. Oxytocin d. Progesterone ANS: C Oxytocin controls milk ejection (letdown) from acini cells. Oxytocin controls milk ejection, not cortisol. Oxytocin controls milk ejection, not prolactin. Oxytocin controls milk ejection, not progesterone. 10. While speaking to a group of older males, which information should the nurse share? The following is a normal characteristic of aging and the male reproductive system: a. Changes in libido are not related to health status. b. Tissue responsiveness to testosterone is increased. c. Testicles will hypertrophy. d. Refractory time after ejaculation is prolonged. ANS: D Men can expect a prolonged refractory time after ejaculation. Changes in libido are related to health changes. Responsiveness to testosterone is decreased. The testicles undergo atrophy. 11. The nurse is instructing a client diagnosed with acute prostatitis. Which of the following instructions would be the least beneficial to the client? a. Avoid alcohol and caffeine. b. Sex should be avoided during the acute phase. c.Sit for as long as you can. d.Sitz baths may provide comfort. ANS: c The patient should be encouraged to use sitz baths for comfort but not to sit in them for long periods of time. Caffeine, alcohol, and sex should be avoided during the acute phase. 12. The nurse is documenting the health history of a client diagnosed with benign prostatic hyperplasia (BPH). In which of the following areas would the nurse take a careful history? a.Bowel patterns b.Eating patterns c.Sleeping patterns d.Urinary patterns ANS: d A careful history on urinary patterns should be taken by the nurse. The ease with which the stream of urine is started, the strength of the stream, and the perceived amount of urine eliminated with each voiding, along with the patients sense about whether the bladder is completely emptied and the presence of nocturia or dribbling, should be noted. The clients bowel, eating, and sleeping patterns are also important; however, they are not as important as the urinary patterns. 13.A client, diagnosed with benign prostatic hyperplasia (BPH), should be instructed to do which of the following? a.Do nothing since this disorder does not require any follow-up. b.Decrease water intake to avoid dribbling. c.Void every 2 to 3 hours. d.Wear scrotal support. ANS: c Clients with BPH should void every 2 to 3 hours to flush the urinary tract. Water should not be decreased because this will irritate the urinary mucosa. Scrotal support is not necessary, and BPH does require follow-up visits. 14.A client, recovering from a transurethral resection of the prostate (TURP) with a continuous bladder irrigation system to a three-way indwelling urinary catheter, tells the nurse he has to void. What nursing intervention should the nurse perform? a.Call the physician. b.Increase the flow of the irrigant. c.Irrigate the catheter. d.Tell the client to void. ANS: c After a TURP, clots that can occlude the catheter and create a sensation to void in the client are common. The nurse should irrigate the catheter to allow the urine to flow. The nurse does not need to phone the physician, increase the flow of the irrigant, or tell the client to void. 15.A client who is 12 hours postoperative after a transurethral resection of the prostate (TURP) is concerned about the blood clots in the catheter and urinary collection bag. How should the nurse respond? a.I need to call your physician. b.I will need to stop the bladder irrigation. c.Blood clots are common during this time frame and will start to decrease in a day. d.You need to stop moving and irritating the catheter. ANS: c Blood clots are common during the first 36 hours following a TURP. The irrigant should not be stopped because it is flushing the clots out of the urinary system. A large amount of bright red blood would be an indication of hemorrhage. The nurse does not need to call the physician. 16.A client is being screened for prostate cancer. What tests would be completed at this time? a.Digital rectal examination and transrectal ultrasonography b.Biopsy of the prostate and magnetic resonance imagery c.Complete blood cell count and prostate-specific antigen d.Prostate-specific antigen (PSA) and digital rectal examination ANS: d Early screening for prostate cancer includes a digital rectal examination and a PSA test. Other tests may be ordered later if either the PSA or digital rectal examination are abnormal. 17.The nurse is instructing a client about testicular self-examination (TSE). Which of the following would not be included in these instructions? a.The testis should feel smooth and egg-shaped. b.Perform TSE after a bath or shower. c.TSE should be performed monthly by every male older than age 40. d.Any lumps and changes in the testicles should be reported. ANS: c The highest risk group for testicular cancer is young men 15 to 35 years of age. TSE should be taught and performed monthly from the teenage years. The other choices are appropriate for the nurse to instruct the client. 18.A male client is diagnosed with orchitis. The nurse should assess the client for which of the following? a.Recent infection with mumps b.Recent diagnosis of prostatitis c.History of type 2 diabetes mellitus d.Diagnosis of renal insufficiency ANS: a Mumps is the most common viral cause of orchitis, with the orchitis occurring 4 to 7 days after the onset of mumps. Orchitis is not associated with prostatitis, type 2 diabetes mellitus, or renal insufficiency. 19.A client is diagnosed with a spermatocele. The nurse should instruct the client on which of the following? a.The use of heat to reduce the size of the inflamed area b.The potential need for surgery to correct the disorder c.The use of ice packs to reduce the size of the inflamed area d.The importance of using antibiotics to treat the disorder ANS: b Spermatoceles may become significantly uncomfortable and require treatment. Surgical correction may be done if infertility is associated with the spermatocele. Surgical removal of the spermatocele is performed under local anesthesia. Heat, ice, and antibiotics are not the first line treatments for the disorder. 20.A client is diagnosed with a varicocele. The nurse realizes that this client is likely to develop: a.hydrocele. b.prostate cancer. c.prostatitis. d.infertility. ANS: d Infertility or subinfertility often occurs in conjunction with varicocele because the increased blood flow in the varicocele raises the scrotal temperature about 93.2F, which is the ideal temperature for spermatogenesis. The client is not likely to develop a hydrocele, prostate cancer, or prostatitis from a varicocele. 21.A newborn male child is diagnosed with cryptorchidism. The nurse should prepare to administer which of the following to this client? a.Intravenous fluids b.Antipyretic medication c.Human chorionic gonadotropin medication d.Antibiotics ANS: c Human chorionic gonadotropin may be given intramuscularly to promote bilateral testicular descent. This medication is provided 2 to 3 times a week for up to 6 weeks. Intravenous fluids, antipyretics, or antibiotics are not indicated in the treatment of this disorder. 22.A client is experiencing priapism. Which of the following should the nurse do first to help the client? a.Apply ice packs to the perineum. b.Prepare for emergency surgery. c.Prepare for an aspiration of blood from the penis. d.Apply heat to the perineum. ANS: a The goal of treating priapism is to resolve the condition before permanent damage occurs that leaves the client unable to achieve an erection in the future. Ice packs to the perineum will resolve some cases of the disorder. This is what the nurse should do first. The client does not need emergency surgery. The client may need blood aspirated from the penis. Heat should not be applied to the perineum. 23.A client is diagnosed with testicular torsion. Which of the following might be indicated for this client? (Select all that apply.) a.Manually untwist the testicle b.Orchiopexy c.Testicle removal d.Pain management e.Application of ice and a scrotal support f. Prescribe medication ANS: a,b,c,d,e,f The goal of the treatment for testicular torsion is to untwist the spermatic cord and reestablish normal blood flow to the testicle. The testicle may be manually untwisted to promote blood flow. If this is unsuccessful, the client may need an orchiopexy or a surgical procedure to untwist the testicle. If surgical treatment occurs within 6 hours of the onset of pain, the testicle is salvaged. If treatment is delayed for 12 hours or more, the testicle will begin to necrose and will need to be removed. Pain medication is needed for this disorder. Ice and a scrotal support are used for this disorder. No medications alone will cure this disorder. 24.A client is diagnosed with epididymitis. The nurse should instruct the client on which of the following as treatment for the disorder? (Select all that apply.) a.Broad spectrum antibiotics b.NSAIDs c.Bed rest d.Elevate the scrotum e.Apply cold packs f. Apply heat ANS: a,b,c,d,e Treatment for epididymitis includes broad spectrum antibiotics, NSAIDs, bed rest, elevation of the scrotum, and application of cold packs. Heat is not recommended as treatment for this disorder. 25. Which of the following should the nurse instruct a client who is recovering from a vasectomy? (Select all that apply.) a.Use ice packs to control postoperative bleeding. b.Wear cotton jockey type briefs for scrotal support. c.Use warm sitz baths to aid in comfort. d.Recognize the signs and symptoms of postoperative infection. e.A vasectomy protects the client from sexually transmitted illnesses. f. Ejaculate will be reduced after the procedure. ANS: a,b,c,d The client recovering from a vasectomy should be instructed to use ice packs to control postoperative bleeding, wear cotton jockey type briefs for scrotal support, use warm sitz baths to aid in comfort, and recognize the signs and symptoms of postoperative infection. A vasectomy does not protect the client from sexually transmitted illnesses. Ejaculate will not be reduced after the procedure. 26. The nurse is assessing a client diagnosed with balanitis and posthitis. Which of the following will the nurse most likely assess in this client? (Select all that apply.) a.Penile discharge b.Hematuria c.Pain d.Erythema e.Flank pain f. Edema ANS: a,c,d,f, The typical manifestations for balanitis and posthitis include penile discharge, pain, erythema, and edema. Hematuria and flank pain are not associated with this disorder. 27. The nurse is assessing a client who is experiencing erectile dysfunction. For which of the following should the nurse assess the client? (Select all that apply.) a.Diagnosis of diabetes mellitus b.Thyroid disease c.Chronic renal failure d.Multiple sclerosis e.Parkinsons disease f. Gastroesophageal reflux disease ANS: a,b,c,d,e Erectile dysfunction has been associated with diabetes mellitus, thyroid disease, chronic renal failure, multiple sclerosis, and Parkinsons disease. Erectile dysfunction has not been associated with gastroesophageal reflux disease. Chapter 37. Structure and Function of the Digestive System MULTIPLE CHOICE 1. The nursing faculty is discussing digestion and indicates it begins in the mouth with salivary - amylase (ptyalin) that initiates the digestion of: a. Proteins b. Carbohydrates c. Fats d. Amino acids ANS: B Salivary amylase initiates the digestion of carbohydrates. Protein digestion occurs in the stomach and is influenced by pepsin. Fat digestion is aided by bile. Amino acids are not involved in the digestive process. Cognitive Level: Comprehension 873 2. A new drug is being tested that is known to inhibit parasympathetic nervous system activity. It is expected that the salivary glands will become: a. Hyperactive b. Hypoactive c. Atrophied d. Enlarged ANS: B Inhibition of the parasympathetic nervous system would result in decreased (hypoactive) functions of the salivary glands. The individual would experience dry mouth. The glands would be hypoactive, not hyperactive. The gland would become hypoactive, but would not atrophy. The gland would become hypoactive; it would not enlarge. Cognitive Level: Comprehension 873 3. The chemist analyzing a sample of normal saliva would expect it to reveal which immunoglobulin? a. IgG b. IgD c. IgE d. IgA ANS: D Normal saliva contains IgA. Normal saliva contains IgA, not IgG. Normal saliva contains IgA, not IgD. Normal saliva contains IgA, not IgE. Cognitive Level: Comprehension 873 4. The nursing student is teaching a class to second graders. The student would correctly identify that food moves down the esophagus via the process termed: a. Peristalsis b. Retropulsion c. Haustral segmentation d. Defecation ANS: A Swallowed food is moved from the esophagus to the stomach by peristalsis. Swallowed food is moved by peristalsis, not retropulsion. Swallowed food is moved by peristalsis; haustral segmentation occurs in the small intestine. Swallowed food is moved by peristalsis; defecation is the process of eliminating stool from the rectum. Cognitive Level: Comprehension 873 5. For the patient experiencing esophageal reflux, the nurse would expect which sphincter to be malfunctioning? a. Pyloric b. Lower esophageal c. Upper esophageal d. Gastric ANS: B The lower esophageal sphincter keeps food from refluxing into the esophagus. The pylorus is located at the connection between the stomach and the duodenum. The upper esophageal sphincter keeps air from entering the esophagus during respiration. There is no gastric sphincter. Cognitive Level: Comprehension 873 6. The patient asks how the GI system works. The nurse would identify that autonomic and hormonal control are involved in GI motility and: a. Defecation b. Swallowing c. Mastication d. Digestive enzyme secretion ANS: D Autonomic control is involved in digestive enzyme secretion. Autonomic control is involved in digestive enzyme secretion, not defecation. Autonomic control is involved in digestive enzyme secretion, not swallowing. Autonomic control is involved in digestive enzyme secretion, not mastication. Cognitive Level: Comprehension 873 7. Which cells of the gastric glands secrete hydrochloric acid? a. Chief b. Parietal c. Zymogenic d. Surface epithelial ANS: B The parietal cells secrete hydrochloric acid. The chief cells secrete pepsinogen. Zymogenic cells do not secrete acid. Epithelial cells line the GI tract and do not secrete acid. Cognitive Level: Comprehension 876 8. Mucus production to form the mucosal barrier in the stomach is stimulated by the release of: a. Somatostatin b. Gastrin c. Prostaglandins d. Histamine ANS: C Prostaglandins protect the mucosal barrier by stimulating the secretion of mucus and bicarbonate and by inhibiting secretion of acid. Somatostatin is secreted by the pancreas and is not involved in secretion of mucus. Gastrin is not involved in mucus secretion. Histamine initiates secretion of acid, not mucus. Cognitive Level: Comprehension 877 9. A young male student becomes very hungry during class. He begins thinking of a cheeseburger and fries, his favorite meal. These thoughts will trigger which phase of gastric secretion? a. Cephalic b. Caudal c. Enteral d. Intestinal ANS: A The cephalic phase is stimulated by the thought, smell, and taste of food. The gastric phase is stimulated by distention of the stomach. The enteral phase is not a phase of gastric secretion. The intestinal phase is stimulated by histamine and digested protein. Cognitive Level: Comprehension 876 10. Which sphincter prevents reflux of digested material from the colon into the small intestine? a. Haustral b. Lower esophageal c. Pyloric d. Ileocecal valve ANS: D The ileocecal valve prevents reflux of digested material from the colon into the small intestine. The haustral segments facilitate propulsion; they do not prevent reflux. Lower esophageal prevents reflux from the stomach to the esophagus. The pylorus is the opening between the stomach and the duodenum. Cognitive Level: Comprehension 878 11. The ileum and jejunum are suspended by folds of the peritoneum known as the that contains an extensive vascular and nervous network. a. Myenteric plexus b. Mesentery c. Auerbach fold d. Meissner plexus ANS: B The ileum and jejunum are suspended in loose folds from the posterior abdominal wall by a peritoneal membrane called the mesentery. Intrinsic motor innervation is mediated by the myenteric plexus (Auerbach plexus) and the submucosal plexus (Meissner plexus). Intrinsic motor innervation is mediated by the myenteric plexus (Auerbach plexus) and the submucosal plexus (Meissner plexus). Intrinsic motor innervation is mediated by the myenteric plexus (Auerbach plexus) and the submucosal plexus (Meissner plexus). Cognitive Level: Comprehension 878 12. Absorption of nutrients from the intestine occurs initially through the: a. Mesentery b. Villi c. Lamina propria d. Splenic veins ANS: B Villi are small finger-like projections that extend from the small intestinal mucosa and increase its absorptive surface area. The ileum and jejunum are suspended in loose folds from the posterior abdominal wall by a peritoneal membrane called the mesentery. The lamina propria (a connective tissue layer of the mucous membrane) lies beneath the epithelial cells of the villi and contains lymphocytes and plasma cells, which produce immunoglobulins. The splenic vein drains the stomach and is not involved in absorption. Cognitive Level: Comprehension 878 13. Digested fats are primarily absorbed into the: a. Lacteals b. Central arterioles c. Lamina propria d. Villus capillaries ANS: A Digested fats move into the lacteals and eventually reach the liver through the systemic circulation. Digested fats move into the lacteals and eventually reach the liver through the systemic circulation. They are not absorbed by central arterioles. Digested fats move into the lacteals and eventually reach the liver through the systemic circulation. They are not absorbed by the lamina propria. Digested fats move into the lacteals and eventually reach the liver through the systemic circulation. They are not absorbed by the villus capillaries. Cognitive Level: Comprehension 878 14. Which reflex inhibits gastric motility when the ileum becomes overdistended? a. Ileogastric b. Gastroduodenal c. Gastroileal d. Colonointestinal ANS: A The ileogastric reflex inhibits gastric motility when the ileum becomes distended. The ileogastric reflex, not the gastroduodenal, inhibits gastric motility when the ileum becomes distended. The ileogastric reflex, not he gastroileal, inhibits gastric motility when the ileum becomes distended. The ileogastric reflex, not the colonointestinal, inhibits gastric motility when the ileum becomes distended. Cognitive Level: Comprehension 881 15. The vermiform appendix is attached to the: a. Duodenum b. Ileum c. Cecum d. Sigmoid colon ANS: C The vermiform appendix is attached to the cecum. The vermiform appendix is attached to the cecum, not the duodenum. The vermiform appendix is attached to the cecum, not the ileum. The vermiform appendix is attached to the cecum, not the sigmoid. Cognitive Level: Comprehension 881 16. The sphincter controls the movement of chyme from the sigmoid colon into the rectum? a. Oddi b. Ileocecal c. OBeirne d. Internal anal ANS: C The OBeirne sphincter controls the movement of wastes from the sigmoid colon into the rectum. The OBeirne sphincter, not the Oddi sphincter, controls the movement of wastes from the sigmoid colon into the rectum. The OBeirne sphincter, not the ileocecal sphincter, controls the movement of wastes from the sigmoid colon into the rectum. The OBeirne sphincter, not the internal anal sphincter, controls the movement of wastes from the sigmoid colon into the rectum. Cognitive Level: Comprehension 881 17. The reflex initiates propulsion in the entire colon, usually during or immediately after eating. a. Gastrocolic b. Ileocolic c. Duodenocolic d. Cephalocolic ANS: A The gastrocolic reflex initiates propulsion in the entire colon. The gastrocolic reflex, not the ileocolic, initiates propulsion in the entire colon. The gastrocolic reflex, not the duodenocolic, initiates propulsion in the entire colon. The gastrocolic reflex, not the cephalocolic, initiates propulsion in the entire colon. Cognitive Level: Comprehension 882 18. The colon receives splanchnic blood flow from which artery(ies)? a. Celiac b. Superior and inferior mesenteric c. Hepatic and portal d. Omental ANS: B The blood supply of the large intestine and rectum is derived primarily from branches of the superior and inferior mesenteric arteries. The blood supply of the large intestine and rectum is derived primarily from branches of the superior and inferior mesenteric arteries, not the celiac. The blood supply of the large intestine and rectum is derived primarily from branches of the superior and inferior mesenteric arteries, not the hepatic or portal. The blood supply of the large intestine and rectum is derived primarily from branches of the superior and inferior mesenteric arteries, not the omental. Cognitive Level: Comprehension 882 19. The capillaries of the liver are more commonly known as hepatic: a. Canaliculi b. Ducts c. Sinusoids d. Papillae ANS: C Small capillaries, or sinusoids, are located between the plates of hepatocytes of the liver. Small capillaries, or sinusoids, not canaliculi, are located between the plates of hepatocytes of the liver. Small capillaries, or sinusoids, not ducts, are located between the plates of hepatocytes of the liver. Small capillaries, or sinusoids, not papillae are located between the plates of hepatocytes of the liver. Cognitive Level: Comprehension 884 20. Which of the following liver cells are phagocytic? a. Glisson b. Kupffer c. Meissner d. Lieberkhn W ANS: B The sinusoids are also lined with phagocytic Kupffer cells and are part of the mononuclear phagocyte system. The Glisson is the capsule that covers the liver. The Meissner is a part of the nerve plexus that innervated the liver. The Lieberkhn is a part of the livers secretory cells. Cognitive Level: Comprehension 884 21. The primary bile acids are synthesized from by hepatocytes lining the bile canaliculi. a. Lecithin b. Fatty acids c. Cholesterol d. Testosterone ANS: C Bile acids are synthesized from cholesterol. Bile acids are synthesized from cholesterol, not lecithin. Bile acids are synthesized from cholesterol, not fatty acids. Bile acids are synthesized from cholesterol, not testosterone. Cognitive Level: Comprehension 884 22. In the liver, free bilirubin moves from the plasma in the sinusoids into the hepatocytes, where it is converted into: a. Unconjugated bilirubin b. Biliverdin c. Conjugated bilirubin d. Urobilinogen ANS: C Within hepatocytes, unconjugated bilirubin joins with glucuronic acid to form conjugated bilirubin, which is water soluble and is secreted in the bile. Within hepatocytes, unconjugated bilirubin joins with glucuronic acid to form conjugated bilirubin, not unconjugated, which is water soluble and is secreted in the bile. Biliverdin is a precursor of bilirubin. When conjugated bilirubin reaches the distal ileum and colon, it is deconjugated by bacteria and converted to urobilinogen. REF: pp. 884-885 23. Which information indicates the nurse understands digestion? During the cephalic and gastric phases of digestion, gallbladder contraction is mediated by branches of the: a. Sympathetic nervous system b. Somatic nervous system c. Vagus nerve d. Glossopharyngeal nerve ANS: C Gallbladder contraction is mediated by cholinergic branches of the vagus nerve. Gallbladder contraction is mediated by cholinergic branches of the vagus nerve, not the sympathetic nervous system. Gallbladder contraction is mediated by cholinergic branches of the vagus nerve, not the somatic nerves. Gallbladder contraction is mediated by cholinergic branches of the vagus nerve, not the glossopharyngeal nerve. Cognitive Level: Comprehension 887 24. Which sphincter, when it relaxes, allows bile to flow into the duodenum? a. Pyloric sphincter b. Sphincter of Oddi c. Ampulla of Vater d. Ileocecal valve ANS: B When the Sphincter of Oddi relaxes, bile flows into the duodenum. The pyloric sphincter controls flow of fluid from the stomach to the duodenum. Secretions from the pancreas empty into the common bile duct at the ampulla of Vater. The ileocecal valve prevents reflux of digested material from the colon into the small intestine. Cognitive Level: Comprehension 887 25. The exocrine portion of the pancreas contains: a. Alpha cells b. Beta cells c. Ducts d. Islets of Langerhans ANS: C The exocrine portion of the pancreas contains ducts. The endocrine portion contains the alpha cells. The endocrine portion contains the beta cells. The endocrine portion contains the islets of Langerhans. Cognitive Level: Comprehension 888 26. The function of the acinar cells of the pancreas is to secrete: a. Bicarbonate b. Enzymes c. Mucus d. Electrolytes ANS: B The exocrine pancreas is composed of acinar cells that secrete enzymes. The exocrine pancreas is composed of acinar cells that secrete enzymes, not bicarbonate. The exocrine pancreas is composed of acinar cells that secrete enzymes, not mucus. The exocrine pancreas is composed of acinar cells that secrete enzymes, not electrolytes. Cognitive Level: Comprehension 888 27. Parasympathetic stimulation to the pancreas will cause which of the following reactions? a. Hormonal inhibition b. Enzyme secretion c. Vasoconstriction d. Decreased bicarbonate production ANS: B Pancreatic innervation arises from preganglionic parasympathetic fibers of the vagus nerve. These fibers activate postganglionic fibers, which stimulate enzymatic and hormonal secretion. Pancreatic innervations stimulate hormone secretion, not inhibit it. Sympathetic postganglionic fibers from the celiac and superior mesenteric plexuses innervate the blood vessels, cause vasoconstriction, and inhibit pancreatic secretion. Parasympathetic stimulation is not involved in bicarbonate production. Cognitive Level: Comprehension 888 28. The pancreas produces which substance to prevent the premature activation of proteolytic enzymes in the pancreas? a. Bicarbonate b. Carboxypeptidase c. Secretin d. Trypsin inhibitor ANS: D The pancreas produces trypsin inhibitor, which prevents the activation of proteolytic enzymes while they are in the pancreas. Bicarbonate is responsible for neutralizing fluid. Carboxypeptidase is a protein-digesting enzyme. Secretin is not produced by the pancreas. Cognitive Level: Comprehension 889 MULTIPLE RESPONSE 1. The patient asks the student to explain what the gastrointestinal (GI) tract actually does. The student would be correct in telling the patient the GI tract performs which of the following processes? (Select all that apply.) a. Absorption of digested food b. Chemical breakdown of food particles c. Erythropoiesis d. Mechanical breakdown of food particles e. Secretion of mucus ANS: A, B, D, E The GI tract carries out the following process: (1) ingestion of food; (2) propulsion of food and wastes from the mouth to the anus; (3) secretion of mucus, water, and enzymes; (4) mechanical digestion of food particles; (5) chemical digestion of food particles; (6) absorption of digested food; and (7) elimination of waste products by defecation. Cognitive Level: Comprehension 871 2. A 70-year-old male reports frequent GI problems. His primary care provider explains that during aging many GI processes decrease, including (select all that apply): a. Gastric juice secretion b. Gallbladder function c. Hepatic regeneration d. Efficiency of drug metabolism e. Mucosal barrier protection ANS: A, C, D, E GI processes that decrease include gastric motility, blood flow, and volume, and acid content of gastric juice may be reduced, particularly with gastric atrophy. Protective mucosal barrier decreases. Decreased hepatic regeneration occurs; size and weight decrease. Blood flow decreases, influencing efficiency of drug metabolism. No changes occur in the gallbladder and bile ducts. Chapter 38. Alterations of Digestive Function MULTIPLE CHOICE 1. A 34-year-old male was diagnosed with a bacterial GI infection. Which of the following types of diarrhea would most likely occur with his condition? a. Osmotic b. Secretory c. Hypotonic d. Motility ANS: B Infections lead to secretory diarrhea. A nonabsorbable substance in the intestine leads to osmotic diarrhea. Hypotonic diarrhea is not a form of diarrhea. Food is not mixed properly, digestion and absorption is impaired, and motility is increased, leading to motility diarrhea. Cognitive Level: Comprehension 896 2. A 20-year-old male was recently diagnosed with lactose intolerance. He eats an ice cream cone and develops diarrhea. His diarrhea can be classified as diarrhea. a. Osmotic b. Secretory c. Hypotonic d. Motility ANS: A A nonabsorbable substance in the intestine leads to osmotic diarrhea. Infections lead to secretory diarrhea. Hypotonic diarrhea is not a form of diarrhea. Food is not mixed properly, digestion and absorption is impaired, and motility is increased leading to motility diarrhea. Cognitive Level: Comprehension 896 3. A 40-year-old female presents complaining of pain near the midline in the epigastrium. Assuming the pain is caused by a stimulus acting on an abdominal organ, the pain felt is classified as: a. Visceral b. Somatic c. Parietal d. Referred ANS: A Visceral pain arises from a stimulus (distention, inflammation, ischemia) acting on an abdominal organ. Somatic is a form of parietal pain. Parietal pain, from the parietal peritoneum, is more localized and intense than visceral pain, which arises from the organs themselves. Referred pain is visceral pain felt at some distance from a diseased or affected organ. Cognitive Level: Comprehension 896 4. The most common disorder associated with upper GI bleeding is: a. Diverticulosis b. Hemorrhoids c. Esophageal varices d. Cancer ANS: C Esophageal varices is the most common disorder associated with upper GI bleeding. Diverticulosis could lead to bleeding, but it would be lower GI rather than upper. Hemorrhoids can lead to bleeding, but they would be upper GI. Duodenal ulcers could lead to upper GI bleeding, but peptic ulcers and varices are identified as more common. Cognitive Level: Comprehension 897 5. A 52-year-old presents with bleeding from the rectum. This condition is referred to as: a. Melena b. Occult bleeding c. Hematochezia d. Hematemesis ANS: C Hematochezia is bleeding from the rectum. Melena is a black or tarry stool. Occult bleeding is hidden bleeding. Hematemesis is vomiting blood. Cognitive Level: Comprehension 898 6. A 50-year-old male is experiencing reflux of chyme from the stomach. He is diagnosed with gastroesophageal reflux. This condition is caused by: a. Fibrosis of the lower third of the esophagus b. Sympathetic nerve stimulation c. Loss of muscle tone at the lower esophageal sphincter d. Reverse peristalsis of the stomach ANS: C Gastroesophageal reflux is due to loss of muscle tone at the lower esophageal sphincter. Gastroesophageal reflux is due to loss of muscle tone at the lower esophageal sphincter; it is not due to fibrosis. Gastroesophageal reflux is due to loss of muscle tone at the lower esophageal sphincter, not stimulation of sympathetic nerves. Gastroesophageal reflux is due to loss of muscle tone at the lower esophageal sphincter, not reverse peristalsis. Cognitive Level: Comprehension 898 7. Reflux esophagitis is defined as a(n): a. Immune response to gastroesophageal reflux b. Inflammatory response to gastroesophageal reflux c. Congenital anomaly d. Secretory response to hiatal hernia ANS: B When gastroesophageal reflux leads to an inflammatory response, it is termed reflux esophagitis. Esophagitis is due to an inflammatory response, not immune. Esophagitis is due to an inflammatory response, not a congenital anomaly. Esophagitis is due to an inflammatory response, not a secretory response. Cognitive Level: Comprehension 899 8. A 45-year-old male complains of heartburn after eating and difficulty swallowing. He probably has: a. Pyloric stenosis b. Gastric cancer c. Achalasia d. Hiatal hernia ANS: D Regurgitation, dysphagia, and substernal discomfort after eating are common in individuals with hiatal hernia. Pyloric stenosis is manifested by projectile vomiting. Gastric cancer is not manifested by heartburn. Achalasia is a form of functional dysphagia caused by loss of esophageal innervation. Cognitive Level: Comprehension 899 9. A serious complication of paraesophageal hiatal hernia is: a. Hemorrhage b. Strangulation c. Peritonitis d. Ascites ANS: B Strangulation of the hernia is a major complication. Strangulation of the hernia, not hemorrhage, is a major complication. Strangulation of the hernia, not peritonitis, is a major complication. Strangulation of the hernia, not ascites, is a major complication. Cognitive Level: Comprehension 899 10. A 38-year-old female complains of epigastric fullness following a meal, nausea, and epigastric pain. Tests reveal narrowing of the opening between the stomach and the duodenum. This condition is referred to as: a. Ileocecal obstruction b. Hiatal hernia c. Pyloric obstruction d. Hiatal obstruction ANS: C The pylorus is the opening between the esophagus and the duodenum; the obstruction is pyloric. Ileocecal obstruction is in the small intestine. Hiatal hernia is related to the esophagus. Hiatal obstruction is related to the esophagus. Cognitive Level: Comprehension 900 11. The cardinal sign of pyloric stenosis caused by ulceration or tumors is: a. Constipation b. Diarrhea c. Vomiting d. Heartburn ANS: C The cardinal sign of pyloric stenosis is vomiting. The cardinal sign of pyloric stenosis is vomiting, not constipation. The cardinal sign of pyloric stenosis is vomiting, not diarrhea. The cardinal sign of pyloric stenosis is vomiting, not heartburn. Cognitive Level: Comprehension 900 12. A 10-month-old is brought to the pediatrician by the mother who states the baby has been experiencing colicky pain followed by vomiting, sweating, nausea, and irritability. Testing reveals a condition in which one part of the intestine telescopes into another. From which type of intestinal obstruction is he suffering? a. Hernia b. Ileus c. Torsion d. Intussusception ANS: D Telescoping of one part of the intestine into another; this usually causes strangulation of the blood supply and is more common in infants 10 to 15 months of age than in adults. A hernia does not involve telescoping of the intestines. An ileus could lead to bowel obstruction, but it does not involve telescoping. Torsion can lead to pain and vomiting, but it does not involve telescoping. Cognitive Level: Comprehension 900 13. A 40-year-old male develops an intestinal obstruction related to protrusion of the intestine through the inguinal ring. This condition is referred to as: a. Intussusception b. A volvulus c. A hernia d. Adhesions ANS: C A hernia is a protrusion of the intestine through a weakness in the abdominal muscles or through the inguinal ring. Intussusception is telescoping of one part of the intestine into another; this usually causes strangulation of the blood supply and is more common in infants 10 to15 months of age than in adults. A volvulus is a twisting of the intestine on its mesenteric pedicle, with occlusion of the blood supply, often associated with fibrous adhesions. It occurs most often in middle-aged and elderly men. Adhesions are irritation from surgery or trauma that leads to formation of fibrin and adhesions that attach to intestine, omentum, or peritoneum and can cause obstruction; they are most common in small intestine. Cognitive Level: Comprehension 900 14. Chronic gastritis is classified according to the: a. Severity b. Location of lesions c. Patients age d. Signs and symptoms ANS: B Chronic gastritis is classified as type A (fundal) or type B (antral), depending on the pathogenesis and location of the lesions. Gastritis is not classified by severity but by location. Gastritis is not classified by age, but by location. Gastritis is not classified by symptoms, but by location. Cognitive Level: Comprehension 903 15. A 42-year-old female presents with abdominal discomfort, epigastric tenderness, and bleeding. Gastroscopy reveals degeneration of the gastric mucosa in the body and fundus of the stomach. Which of the following would most likely follow? a. Pernicious anemia b. Osmotic diarrhea c. Increased acid secretion d. Decreased gastrin secretion ANS: A Pernicious anemia can develop because the damage to the mucosa makes the intrinsic factor less available to facilitate vitamin B12 absorption in the ileum. Osmotic diarrhea would not occur as a portion of the damage to the mucosa, but pernicious anemia could. Increased acid secretion would not occur as a portion of the damage to the mucosa, but pernicious anemia could. Decreased gastrin secretion would not occur as a portion of the damage to the mucosa, but pernicious anemia could. Cognitive Level: Comprehension 903 16. A 54-year-old male is diagnosed with peptic ulcer disease. This condition is most likely caused by: a. Hereditary hormonal imbalances with high gastrin levels b. Breaks in the mucosa and presence of corrosive secretions c. Decreased vagal activity and vascular engorgement d. Gastric erosions related to high ammonia levels and bile reflux ANS: B Peptic ulcer disease is caused by breaks in the mucosa and the presence of corrosive substances. High gastrin occurs, but the disease is due to breaks in the mucosa. Vagal activity increases. Gastric erosions occur, but they are not due to high ammonia. Cognitive Level: Comprehension 903 17. A 60-year-old male presents with GI bleeding and abdominal pain. He reports that he takes NSAIDs daily to prevent heart attack. Tests reveal that he has a peptic ulcer. The most likely cause of this disease is: a. Increasing subepithelial bicarbonate production b. Accelerating the H+ (proton) pump in parietal cells c. Inhibiting mucosal prostaglandin synthesis d. Stimulating a shunt of mucosal blood flow ANS: C Use of NSAIDs inhibit prostaglandins and maintenance of the mucosal barrier and decrease bicarbonate secretion. NSAIDs decrease bicarbonate production. H. pcryelaori in ses hydrogen secretion. NSAIDs do not affect mucosal blood flow. Cognitive Level: Comprehension 904 18. A 39-year-old female with chronic intermittent pain in the epigastric area 2 to 3 hours after eating is diagnosed with a duodenal ulcer. Which of the following behaviors may have contributed to the development of the ulcer? a. Cigarette smoking b. Drinking caffeinated beverages c. Consuming limited fiber d. Antacid consumption ANS: A Acid production is stimulated by cigarette smoking. Caffeinated beverages do not contribute to ulcer formation. Fiber is important, but consuming limited fiber will not contribute to ulcer formation. Antacids may relieve pain, but they do not contribute to ulcer formation. Cognitive Level: Comprehension 904 19. A 22-year-old male underwent brain surgery to remove a tumor. Following surgery, he experienced a peptic ulcer. His ulcer is referred to as a(n) ulcer. a. Infectious b. Cushing c. Ischemic d. Curling ANS: B A Cushing ulcer is a stress ulcer associated with severe head trauma or brain surgery that results from decreased mucosal blood flow and hypersecretion of acid caused by overstimulation of the vagal nerve. The stress ulcer is termed Cushing, not infectious. The stress ulcer is termed Cushing, not ischemic. Curling ulcers develop secondary to burns. Cognitive Level: Comprehension 907 20. A 24-year-old male who sustained a head injury and fractured femur develops a stress ulcer. A common clinical manifestation of this ulcer is: a. Bowel obstruction b. Bleeding c. Pulmonary embolism d. Hepatomegaly ANS: B The most common clinical manifestation is bleeding. The most common clinical manifestation is bleeding; bowel obstruction would occur much later and would not be expected. The most common clinical manifestation is bleeding, not pulmonary embolism. The most common clinical manifestation is bleeding; hepatomegaly is not associated with stress ulcers. Cognitive Level: Comprehension 907 21. A 3-month-old female develops colicky pain, abdominal distention, and diarrhea after drinking cows milk. The best explanation for her symptoms is: a. Deficiency of bile that stimulates digestive secretions and bowel motility b. Excess of amylase, which increases the breakdown of starch and causes an osmotic diarrhea c. Overgrowth of bacteria from undigested fat molecules, which leads to gas formation and decreased bowel motility d. Excess of undigested lactose in her digestive tract, resulting in increased fluid movement into the digestive lumen and increased bowel motility ANS: D Undigested lactose increases the osmotic gradient in the intestine, causing irritation and osmotic diarrhea. The child is experiencing lactose intolerance, not bile deficiency. This child is experiencing lactose intolerance, not an excess of amylase. The child is experiencing lactose intolerance, not in infectious process. Cognitive Level: Comprehension 908 22. Clinical manifestations of bile salt deficiencies are related to poor absorption of: a. Fats and fat-soluble vitamins b. Water-soluble vitamins c. Proteins d. Minerals ANS: A Clinical manifestations of bile salt deficiency are related to poor intestinal absorption of fat and fat-soluble vitamins (A, D, E, K). Water-soluble vitamins do not require bile salts for absorption; thus, they are not affected. Protein breakdown is facilitated by bile, but its absorption is not dependent upon it; thus, the correct answer is the fat soluble vitamins. Absorption of minerals do not require bile salts for absorption; thus, they are not affected. Cognitive Level: Comprehension 908 23. A 30-year-old obese female underwent gastric resection in an attempt to lose weight. Which of the following complications could the surgery cause? a. Constipation b. Acid reflux gastritis c. Anemia d. Hiccups ANS: C One of the complications is anemia due to iron malabsorption, which may result from decreased acid secretion. Diarrhea, not constipation, occurs. The reflux would be alkaline, not acidic. Hiccups are not associated with gastrectomy. Cognitive Level: Comprehension 907 24. A 50-year-old male complains of frequently recurring abdominal pain, diarrhea, and bloody stools. A possible diagnosis would be: a. Ulcerative colitis b. Hiatal hernia c. Pyloric obstruction d. Achalasia ANS: A Ulcerative colitis is manifested by fever, elevated pulse rate, frequent diarrhea (10 to 20 stools/day), urgency, obviously bloody stools, and continuous lesions present in the colon. Hiatal hernia is most often asymptomatic and would not be manifested by abdominal pain. Pyloric obstruction would be manifested by forceful or projectile vomiting. Achalasia would be manifested by difficulty or uncomfortable swallowing. Cognitive Level: Comprehension 908 25. Which of the following symptoms would help a health care provider distinguish between ulcerative colitis and Crohn disease? a. Abdominal pain b. Pattern of remission/exacerbations c. Diarrhea d. Malabsorption ANS: D Malabsorption is common in Crohn disease and is rare in ulcerative colitis. Both disorders can lead to abdominal pain. Both disorders have a clinical course of remissions and exacerbations. Both disorders lead to diarrhea. REF: pp. 908-909 26. A 16-year-old female presents with abdominal pain in the right lower quadrant. Physical examination reveals rebound tenderness and a low-grade fever. A possible diagnosis would be: a. Colon cancer b. Pancreatitis c. Appendicitis d. Hepatitis ANS: C Appendicitis is manifested by right lower quadrant pain with rebound tenderness. Colon cancer may be asymptomatic, followed by bleeding. Pancreatitis is manifested by vomiting. Hepatitis would be manifested by upper abdominal pain, not lower. Cognitive Level: Comprehension 910 27. The most common cause of chronic vascular insufficiency among the elderly is: a. Anemia b. Aneurysm c. Lack of nutrition in gut lumen d. Atherosclerosis ANS: D The most common cause of chronic vascular insufficiency is atherosclerosis, especially in the elderly. Anemia does not lead to vascular insufficiency. An aneurysm would lead to acute vascular insufficiency. Lack of nutrition does not lead to vascular insufficiency; it is due to atherosclerosis. Cognitive Level: Comprehension 911 28. Which of the following characteristics is associated with an acute occlusion of mesenteric blood flow to the small intestine? a. Often precipitated by an embolism b. Commonly associated with disease such as pancreatitis and gallstones c. Caused by chronic malnutrition and mucosal atrophy d. Often a complication of hypovolemic shock ANS: A Occlusion of blood flow is often precipitated by embolism. Occlusion of blood flow is often precipitated by embolism; it is not associated with pancreatitis. Occlusion of blood flow is often precipitated by embolism, even if chronic malnutrition is present. Occlusion of blood flow is often precipitated by embolism; it is not a complication of hypovolemic shock. Cognitive Level: Comprehension 911 29. The risk of hypovolemic shock is high with acute mesenteric arterial insufficiency because: a. The resulting liver failure causes a deficit of plasma proteins and a loss of oncotic pressure. b. Ischemia alters mucosal membrane permeability, and fluid is shifted to the bowel wall and peritoneum. c. Massive bleeding occurs in the GI tract. d. Overstimulation of the parasympathetic nervous system results in ischemic injury to the intestinal wall. ANS: B Fluid shifts lead to hypovolemia. Arterial insufficiency is not related to liver failure. Bleeding may occur, but hypovolemia is related to fluid shifts. Fluid shifts lead to hypovolemia; it is not due to overstimulation of the parasympathetic nerves. Cognitive Level: Comprehension 911 30. Which of the following conditions is thought to contribute to the development of obesity? a. Insulin excess b. Leptin resistance c. Adipocyte failure d. Malabsorption ANS: B Leptin resistance disrupts hypothalamic satiety signaling and promotes overeating and excessive weight gain and is a factor in the development of obesity. Insulin becomes resistant, not present in excess. Leptin resistance, not adipocyte failure, leads to obesity. Malabsorption does not lead to obesity, but primarily to weight loss. Cognitive Level: Comprehension 912 31. A 13-year-old female confides to her mother that she binge eats and induces vomiting to prevent weight gain. This disease is referred to as: a. Anorexia nervosa b. Bulimia nervosa c. Long-term starvation d. Laxative abuse ANS: B Binge eating and vomiting is characteristic of bulimia nervosa. Anorexia nervosa is starvation eating. Binge eating and vomiting is characteristic of bulimia nervosa, not long-term starvation. Binge eating and vomiting is characteristic of bulimia nervosa, not laxative abuse. Cognitive Level: Comprehension 914 32. A 54-year-old male complains that he has been vomiting blood. Tests reveal portal hypertension. Which of the following is the most likely cause of his condition? a. Thrombosis in the spleen b. Cirrhosis of the liver c. Left ventricular failure d. Renal stenosis ANS: B Portal hypertension occurs secondarily to cirrhosis of the liver. Portal hypertension occurs secondarily to cirrhosis of the liver, not thrombosis of the spleen. Portal hypertension occurs secondarily to cirrhosis of the liver, not left ventricular failure. Portal hypertension occurs secondarily to cirrhosis of the liver, not renal stenosis. Cognitive Level: Comprehension 915 33. The most common clinical manifestation of portal hypertension is bleeding. a. Rectal b. Duodenal c. Esophageal d. Intestinal ANS: C Vomiting of blood from bleeding esophageal varices is the most common clinical manifestation of portal hypertension. Esophageal bleeding, not rectal bleeding, is the most common clinical manifestation of portal hypertension. Esophageal bleeding, not duodenal bleeding, is the most common clinical manifestation of portal hypertension. Esophageal bleeding, not intestinal bleeding, is the most common clinical manifestation of portal hypertension. Cognitive Level: Comprehension 915 34. A 60-year-old female with a history of alcoholism complains of recent weight gain and right flank pain. Physical examination reveals severe ascites. This condition is caused by decreased: a. Albumin and lack of cellular integrity b. Capillary filtration pressure c. Capillary permeability d. Antidiuretic hormone secretion ANS: A Ascites is due to decreased albumin and lack of cellular integrity. Ascites is due to decreased albumin and lack of cellular integrity, not capillary filtration pressure. Ascites is due to decreased albumin and lack of cellular integrity, not decreased capillary permeability. Ascites is due to decreased albumin and lack of cellular integrity, not antidiuretic hormone secretion. Cognitive Level: Comprehension 916 35. Manifestations associated with hepatic encephalopathy from chronic liver disease are the result of: a. Hyperbilirubinemia and jaundice b. Fluid and electrolyte imbalances c. Impaired ammonia metabolism d. Decreased cerebral blood flow ANS: C Impaired ammonia metabolism leads to the symptoms of hepatic encephalopathy. Impaired ammonia metabolism leads to the symptoms of hepatic encephalopathy. Symptoms are primarily neurologic, not jaundice oriented. Impaired ammonia metabolism leads to the symptoms of hepatic encephalopathy. Fluid and electrolyte changes that occur would not lead to the manifestations seen in hepatic encephalopathy. Impaired ammonia metabolism leads to the symptoms of hepatic encephalopathy. Cerebral blood flow is not affected. Cognitive Level: Comprehension 917 36. An increase in the rate of red blood cell breakdown causes which form of jaundice? a. Obstructive b. Hemolytic c. Hepatocellular d. Metabolic ANS: B Excessive hemolysis (breakdown) of red blood cells can cause hemolytic jaundice (prehepatic jaundice). Excessive hemolysis (breakdown) of red blood cells can cause hemolytic jaundice (prehepatic jaundice). It is not due to obstruction. Excessive hemolysis (breakdown) of red blood cells can cause hemolytic jaundice (prehepatic jaundice). It is not hepatocellular. Excessive hemolysis (breakdown) of red blood cells can cause hemolytic jaundice (prehepatic jaundice). It is not metabolic. Cognitive Level: Comprehension 918 37. Complete obstruction of bile flow to the liver would be manifested by: a. Elevated hemoglobin and hematocrit b. Lower-leg edema c. Clay-colored stools d. Hypotension ANS: C Complete obstruction of bile flow leads to clay-colored stools. Complete obstruction of bile flow leads to clay-colored stools, not elevated hemoglobin and hematocrit. Complete obstruction of bile flow leads to clay-colored stools, not lower-leg edema. Complete obstruction of bile flow leads to clay-colored stools, not hypotension. Cognitive Level: Comprehension 920 38. The icteric phase of hepatitis is characterized by which of the following clinical manifestations? a. Fatigue, malaise, vomiting b. Jaundice, dark urine, enlarged liver c. Resolution of jaundice, liver function returns to normal d. Fulminant liver failure, hepatorenal syndrome ANS: B The icteric phase is manifested by jaundice, dark urine, and clay-colored stools. The liver is enlarged, smooth, and tender, and percussion causes pain; this is the actual phase of illness. Fatigue and vomiting occur during the prodromal stage. Resolution occurs in the recovery phase. Fulminant liver failure does not involve icterus. Cognitive Level: Comprehension 920 39. A 55-year-old male died in a motor vehicle accident. Autopsy revealed an enlarged liver caused by fatty infiltration, testicular atrophy, and mild jaundice secondary to cirrhosis. The most likely cause of his condition is: a. Bacterial infection b. Viral infection c. Alcoholism d. Drug overdose ANS: C The most common cause of cirrhosis is alcoholism. The most common cause of cirrhosis is alcoholism, not a bacterial infection. The most common cause of cirrhosis is alcoholism, not a viral infection. The most common cause of cirrhosis is alcoholism, not drug overdose. Cognitive Level: Comprehension 921 40. In alcoholic cirrhosis, hepatocellular damage is caused by: a. Acetaldehyde accumulation b. Bile toxicity c. Acidosis d. Fatty infiltrations ANS: A Alcoholic cirrhosis is caused by the toxic effects of alcohol metabolism on the liver. Alcohol is transformed to acetaldehyde, and excessive amounts significantly alter hepatocyte function and activate hepatic stellate cells, a primary cell involved in liver fibrosis. Bile toxicity does not cause alcoholic cirrhosis. Acidosis does not cause alcoholic cirrhosis. Fatty infiltrations do not cause alcoholic cirrhosis. Chapter 39. Alterations of Digestive Function in Children MULTIPLE CHOICE 1. The family learns that a 3D ultrasound of a 9-week fetus shows incomplete fusion of the nasomedial or intermaxillary process. The family will be told that the child will be born with: a. Cleft lip b. Nasal passage atresia c. Esophageal atresia d. Lack of dentition ANS: A Cleft lip is caused by the incomplete fusion of the nasomedial or intermaxillary process beginning the fourth week of embryonic development, a period of rapid development. Cleft lip, not nasal passage atresia, occurs when there is lack of or incomplete fusion of the nasomedial or intermaxillary process. In esophageal atresia, the esophagus ends in a blind pouch. It is not associated with nasomedial processes. Lack of dentition is not due to incomplete fusion of the processes. Cognitive Level: Comprehension 938 2. Examination of a newborn female revealed that the esophagus ends in a blind pouch. This condition is referred to on the chart as: a. Esophageal atresia b. Tracheoesophageal stenosis c. Esophagitis d. Pyloric stenosis ANS: A . When the esophagus ends in a blind pouch, the condition is referred to as esophageal atresia. When the esophagus ends in a blind pouch, the condition is referred to as esophageal atresia; the trachea is not involved. Esophagitis is inflammation of the esophagus. Pyloric stenosis is a narrowing of the connection between the stomach and the duodenum. Cognitive Level: Comprehension 939 3. Which condition should the nurse assess for in mothers carrying fetuses affected by esophageal malformations? a. Enlarged placentas b. Excessive amniotic fluid c. Short umbilical cords d. Foul smelling vaginal discharge ANS: B Polyhydramnios (excessive amniotic fluid) is reported to occur in 14% to 90% of mothers of affected infants because of alterations in fetal swallowing. Excessive amniotic fluid, not an enlarged placenta, is a possible manifestation of fetuses with esophageal malformations. Excessive amniotic fluid, not a short umbilical cord, is a possible manifestation of fetuses with esophageal malformations. Excessive amniotic fluid, not foul smelling vaginal discharge, is a possible manifestation of fetuses with esophageal malformations. Cognitive Level: Comprehension 939 4. A mother brings her 2-week-old infant to the pediatrician because he vomits forcefully for no apparent reason and food sometimes is regurgitated as though undigested. The infant is most likely suffering from: a. Pyloric stenosis b. Meconium ileus c. Esophageal atresia d. Galactosemia ANS: A Pyloric stenosis is manifested by forceful vomiting. Pyloric stenosis is manifested by forceful vomiting, not meconium ileus. Pyloric stenosis is manifested by forceful vomiting, not esophageal atresia. Pyloric stenosis is manifested by forceful vomiting, not galactosemia. Cognitive Level: Comprehension 940 5. A sign that a newborn infant may have pyloric stenosis is: a. Diarrhea b. Bile regurgitation c. Olive-sized mass in the upper abdomen d. Ascites with a fluid wave visible across the abdomen ANS: C A firm, small, movable mass, approximately the size of an olive, is felt in the right upper quadrant in 70% to 90% of infants with pyloric stenosis. Diarrhea is not a sign of pyloric stenosis. Bile regurgitation is not a sign of pyloric stenosis. Ascites is not a sign of pyloric stenosis. Cognitive Level: Comprehension 940 6. A 2-month-old female is brought to the emergency room (ER) for persistent bile-stained vomiting after feeding. Physical examination reveals dehydration, and x-ray reveals that the colon is located in the upper right quadrant. What is the most likely cause of this condition? a. Malrotation b. Ileocecal displacement c. Pyloric stenosis d. Meconium ileus ANS: A In infants, malrotation obstruction causes intermittent or persistent bile-stained vomiting after feedings. In infants, malrotation obstruction, not ileocecal displacement, causes intermittent or persistent bile-stained vomiting after feedings. Pyloric stenosis is manifested by vomiting, but it is not bile stained and the colon is not displaced. In meconium ileus, there is an intestinal obstruction caused by meconium formed in utero. Cognitive Level: Comprehension 941 7. Meconium ileus is associated with which of the following disorders? a. Pyloric stenosis b. Esophageal atresia c. Cystic fibrosis d. Esophagitis ANS: C Meconium ileus is associated with cystic fibrosis. Meconium ileus is associated with cystic fibrosis, not pyloric stenosis. Meconium ileus is associated with cystic fibrosis, not esophageal atresias. Meconium ileus is associated with cystic fibrosis, not esophagitis. Cognitive Level: Comprehension 941 8. Intussusception is treated initially by: a. Bowel resection b. An air enema c. Laxative d. Doubling fluid intake ANS: B Reduction is an emergency procedure using an air enema. Bowel resection is not indicated unless the enema is ineffective. Laxatives are not indicated in the treatment of intussusception. Doubling fluid intake would not help treat intussusception. Cognitive Level: Comprehension 944 9. A 2-month-old female with Down syndrome is diagnosed with Hirschsprung disease following family complaints of chronic constipation. The most likely cause of these symptoms is: a. Absence of ganglia along the length of the colon b. The use of cows milk instead of formula c. Excessive use of glycerin suppositories to promote bowel elimination d. Additional ganglia throughout the length of the colon ANS: A Congenital aganglionic megacolon is caused by the absence of the enteric ganglia (Meissner and Auerbach plexuses) along a variable length of the colon, resulting in inadequate motility. Megacolon is a functional anatomic disorder not related to formula. Megacolon is a functional anatomic disorder not related to use of suppositories. Megacolon is not due to additional ganglia, but an absence of ganglia. Cognitive Level: Comprehension 942 10. The primary complication of enterocolitis associated with Hirschsprung disease is related to which finding? a. Fecal impaction b. Pancreatic insufficiency c. Hyperactive peristalsis d. Ileal atresia ANS: A The most serious complication in the neonatal period is enterocolitis related to fecal impaction. The most serious complication in the neonatal period is enterocolitis related to fecal impaction. It does not result in pancreatic insufficiency. The most serious complication in the neonatal period is enterocolitis related to fecal impaction. It does not result in hyperactive peristalsis, but slowed peristalsis. The most serious complication in the neonatal period is enterocolitis related to fecal impaction, not ileal atresia. Cognitive Level: Comprehension 942 11. A 6-month-old male infant is brought to the ER after the sudden development of abdominal pain, irritability, and vomiting followed by passing of currant jelly stool. Ultrasound reveals intestinal obstruction in which the ileum collapsed through the ileocecal valve and invaginated into the large intestine. This type of obstruction is referred to as: a. Prolapse b. Pyloric stenosis c. Intussusception d. Imperforation ANS: C These are symptoms of intussusception. These are symptoms of intussusception, not prolapse. These are symptoms of intussusception, not stenosis, which would be vomiting. These are symptoms of intussusception, not imperforation, which would be a closed anal opening. Cognitive Level: Comprehension 942 12. An 8-week-old female is diagnosed with a congenital heart disease and Down syndrome. Her parents report that she has difficulty defecating. X-ray reveals anorectal malformation that causes complete obstruction often referred to as: a. Intussusception b. Imperforate anus c. Meckel diverticulum d. Megacolon ANS: B Deformities that cause complete obstruction are known collectively as imperforate anus. Intussusception is manifested by red jelly-like stools. Meckel diverticulum is a congenital malformation of the gastrointestinal (GI) tract involving all layers of the small intestinal wall usually in the ileum. Megacolon is due to lack of nerve innervations. Cognitive Level: Comprehension 942 13. Occurrence of gastroesophageal reflux is highest in which pediatric population? a. Premature infants b. Infants with Down syndrome c. Children with cystic fibrosis d. Children with esophageal atresia ANS: A The frequency of reflux is highest in premature infants and decreases during the first 6 to 12 months of life. The frequency of reflux is highest in premature infants, not infants with Down syndrome. The frequency of reflux is highest in premature infants, not children with cystic fibrosis. The frequency of reflux is highest in premature infants, not infants with esophageal atresia. Cognitive Level: Comprehension 944 14. An 8-week-old male was recently diagnosed with cystic fibrosis. Which of the following digestive alterations would be expected? a. Insufficient bile production b. Gastric atrophy c. Hypersecretion of stomach acid d. Malabsorption ANS: D Cystic fibrosis results in malabsorption. Infants with cystic fibrosis have normal bile production; they experience pancreatic enzyme deficiency. Infants with cystic fibrosis experience malabsorption, not gastric atrophy. Infants with cystic fibrosis experience malabsorption; they do not have hypersecretion of stomach acid. Cognitive Level: Comprehension 944 15. A 13-month-old infant presents with vomiting; abdominal pain; and pale, bulky, greasy, and foul-smelling stools. A possible diagnosis the clinician would document on the chart might be: a. Failure to thrive b. Gluten-sensitive enteropathy c. Gastroesophageal reflux d. Meconium ileus ANS: B Infants with gluten-sensitive enteropathy experience greasy stools. Infants with failure to thrive experience weight loss, but not abnormal stools. Infants with gastroesophageal reflux do not experience bulky, greasy stools. Infants with meconium ileus do not experience bulky, greasy stools. Cognitive Level: Comprehension 945 16. Celiac disease, or sprue, is caused by alterations of the intestinal: a. Glands b. Villi c. Smooth muscle wall d. Sphincters ANS: B Gluten-sensitive enteropathy, formerly called celiac sprue or celiac disease, is an autoimmune disease that damages small intestinal villous epithelium. Celiac disease affects the villi, not the glands. Celiac disease affects the villi, not the smooth muscle wall. Celiac disease affects the villi, not the sphincters. Cognitive Level: Comprehension 946 17. Kwashiorkor is a severe dietary deficiency of: a. Fat-soluble vitamins b. Carbohydrates c. Protein d. Calcium and magnesium ANS: C Kwashiorkor is a severe dietary deficiency of protein. Kwashiorkor is a severe dietary deficiency of protein, not fat-soluble vitamins. Kwashiorkor is a severe dietary deficiency of protein, not carbohydrates. Kwashiorkor is a severe dietary deficiency of protein, not minerals such as calcium and magnesium. Cognitive Level: Comprehension 946 18. Marasmus is most common in children of which age group? a. Younger than one b. 1 to 2 years c. 5 to 6 years d. 12 to 15 years ANS: A Marasmus is most common in children younger than one. Marasmus is most common in children younger than one, not 1 to 2 years. Marasmus is most common in children younger than one, not 5 to 6 years. Marasmus is most common in children younger than one, not 12 to 15 years. Cognitive Level: Comprehension 946 19. A 1-week-old female is brought to her pediatrician for abdominal distention and unstable temperature. Physical examination reveals bradycardia and apnea. Tests reveal hypoxic injury to the bowel resulting in bacterial invasion and perforation. This condition is referred to as: a. Infective enteropathy b. Necrotizing enterocolitis (NEC) c. Mucoviscidosis d. Ileus ANS: B NEC is an ischemic, inflammatory condition of the bowel that causes necrosis, perforation, and death, if untreated. NEC is an ischemic, inflammatory condition of the bowel that causes necrosis, perforation, and death, if untreated. Infective enteropathy may be related to infection, but it is not necrotic. Mucoviscidosis is related to cystic fibrosis. Ileus is manifested by decreased bowel sounds, but not ischemia. Cognitive Level: Comprehension 947 20. Prolonged diarrhea is more serious in children than adults because: a. Children have lower adipose reserves. b. Fluid reserves are lower in children. c. Children have a lower metabolic rate. d. Children are more resistant to antimicrobial therapy. ANS: B Prolonged diarrhea is more dangerous in children because they have much smaller fluid reserves than adults. Prolonged diarrhea is more dangerous in children because they have much smaller fluid reserves than adults, not due to lower adipose reserves. Prolonged diarrhea is more dangerous in children because they have much smaller fluid reserves than adults. Children have higher metabolic rates. Prolonged diarrhea is more dangerous in children because they have much smaller fluid reserves than adults. It is not due to microbial resistance. Cognitive Level: Comprehension 948 21. When an infant has increased bilirubin production and impaired hepatic excretion of bilirubin, what does the nurse suspect is occurring in the patient? a. Biliary hypertrophy b. Physiologic jaundice c. Hepatitis A d. Infantile cirrhosis ANS: B Impaired excretion of bilirubin can lead to physiologic jaundice. Impaired excretion of bilirubin can lead to physiologic jaundice, not biliary hypertrophy. Impaired excretion of bilirubin can lead to physiologic jaundice, not hepatitis A. Impaired excretion of bilirubin can lead to physiologic jaundice, not cirrhosis. Cognitive Level: Comprehension 948 22. A 7-month-old female presents with jaundice, clay-colored stool, and failure to gain weight. Testing reveals the absence of intrahepatic bile ducts. This condition is referred to as atresia. a. Hepatic b. Portal c. Sinusoidal d. Biliary ANS: D Jaundice is the primary clinical manifestation of biliary atresia, along with hepatomegaly and acholic (clay-colored) stools. Jaundice is the primary clinical manifestation of biliary atresia, not hepatic atresia, along with hepatomegaly and acholic (clay-colored) stools. Jaundice is the primary clinical manifestation of biliary atresia, not portal atresia, along with hepatomegaly and acholic (clay-colored) stools. Jaundice is the primary clinical manifestation of biliary atresia, not sinusoidal atresia, along with hepatomegaly and acholic (clay-colored) stools. Cognitive Level: Comprehension 949 23. A 7-month-old female presents with jaundice, clay-colored stool, and failure to gain weight. She is diagnosed with biliary atresia. The nurse realizes the treatment for this disorder will most likely be: a. Immunoglobulins b. Liver transplant c. Bone marrow transplant d. Dietary modifications ANS: B The treatment for biliary atresia is liver transplant. The treatment for biliary atresia is liver transplant, not immunoglobulins. The treatment for biliary atresia is liver transplant, not bone marrow transplant. The treatment for biliary atresia is liver transplant, not dietary modifications. Cognitive Level: Comprehension 949 24. The nurse assessing the patient with biliary atresia would expect to find which primary clinical manifestation? a. Anemia b. Jaundice c. Hypobilirubinemia d. Ascites ANS: B The primary clinical manifestation is jaundice. The primary clinical manifestation is jaundice, not anemia. The primary clinical manifestation is jaundice, not hypobilirubinemia; it would be hyperbilirubinemia. The primary clinical manifestation is jaundice; ascites occurs with other liver disorders, but not atresia. Cognitive Level: Comprehension 949 25. Outbreaks of hepatitis often occur in young children attending day care centers and can be attributed to poor hand washing. a. A b. B c. C d. D ANS: A Outbreaks of hepatitis A occur in condition where poor hand washing occurs. Hepatitis B is blood borne and not related to hand washing. Hepatitis C is blood borne and not related to hand washing. Hepatitis D is blood borne and depends on an active HIV infection. Cognitive Level: Comprehension 949 26. Where does the nurse expect the obstruction to be in a patient with extrahepatic portal hypertension? a. Sinusoids b. Bile ducts c. Hepatic portal vein d. Hepatic artery ANS: C Extrahepatic (prehepatic) portal venous obstruction causes 50% to 70% of extrahepatic portal hypertension in children. Sinusoids can be inflamed, but would not lead to hypertension. Obstruction of the bile ducts would lead to interruption in the flow of bile to the duodenum; it would not cause hypertension. The obstruction is in the vein, not the artery. Cognitive Level: Comprehension 949 27. Early identification and treatment for metabolic disorders is important because: a. Permanent damage to vital organs can be prevented. b. Surgery is usually necessary. c. Cure rates are higher with early detection. d. Death usually occurs within the first month. ANS: A The earliest possible identification of metabolic disorders is essential because early treatment may prevent permanent damage to vital organs, such as the liver or brain. Surgery is not the treatment in most of the metabolic disorders; they are controlled by dietary modifications. A cure is not possible in most disorders. Death does not occur in the first month; dietary control is effective. Cognitive Level: Comprehension 951 28. A 3-month-old female presents with intention tremors, dystonia, greenish-yellow rings in the cornea, and hepatomegaly. eTaelsatsdrefvect on chromosome 13. Which of the following is the most likely diagnosis? a. Galactosemia b. Fructosemia c. Wilson disease d. Cirrhosis ANS: C Wilson disease is manifested by dystonia and greenish-yellow rings in the cornea. Galactosemia is manifested by high levels of blood galactose and vomiting. Fructosemia is manifested by high levels of blood fructose and hepatomegaly, but not dystonia and rings in the cornea. Cirrhosis is manifested by hepatomegaly, but not dystonia and greenish-yellow rings in the cornea. Cognitive Level: Comprehension 951 29. A 27-year-old male presents with fever, GI bleeding, hepatomegaly, and transient joint pain. He reports that as a child he received blood transfusions following a motor vehicle accident. He also indicates he was vaccinated against hepatitis B. Which of the following types of hepatitis does the clinician think he most likely has? a. A b. B c. C d. D ANS: C Hepatitis C virus is transmitted with blood transfusions. Hepatitis A is transmitted in situations where there are unsanitary conditions or poor hand washing. Hepatitis B is transmitted by blood transfusions, but the individual has been vaccinated to this type of hepatitis. Hepatitis D is dependent upon the presence of hepatitis B infection. Cognitive Level: Comprehension 949 30. The nurse would correctly identify the most common symptom of Meckel diverticulum as: a. Constipation b. Vomiting c. Rectal bleeding d. Ascites ANS: C Although most Meckel diverticuli are asymptomatic, the most common symptom is painless rectal bleeding. The most common symptom of Meckel diverticuli is rectal bleeding, not constipation. The most common symptom of Meckel diverticuli is rectal bleeding, not vomiting. The most common symptom of Meckel diverticuli is rectal bleeding, not ascites. Cognitive Level: Comprehension 942 MULTIPLE RESPONSE 1. A newborn male is diagnosed with cleft palate. The pediatrician counsels the parents that complications of cleft palate include (select all that apply): a. Tonsil hypertrophy b. Recurrent paranasal infections c. Difficulty breathing d. Excessive dental decay e. Hearing loss ANS: A, B, D, E Children with cleft palate tend to have tonsil hypertrophy, tend to have repeated infections of the paranasal sinuses, do not experience difficulty breathing, experience excessive dental decay, and experience hearing loss. Cognitive Level: Comprehension 939 2. Which of the following are complications of gastroesophageal reflux? (Select all that apply.) a. Aspiration pneumonia b. Anemia c. Weight loss d. Delayed growth e. Hepatomegaly ANS: A, B, C, D Aspiration pneumonia develops in one-third of infants with gastroesophageal reflux. In cases that persist into childhood, chronic cough, wheezing, and recurrent pneumonia are common. Inadequate retention of nutrients can adversely impact growth and weight gain. Esophagitis resulting from exposure of the esophageal mucosa to acidic gastric contents is manifested by pain, bleeding, and eventually stricture formation and abnormal motility. Approximately 25% have iron deficiency anemia caused by frank or occult blood loss. Hepatomegaly is not a complication of gastroesophageal reflux. Chapter 40. Structure and Function of the Musculoskeletal System MULTIPLE CHOICE 1. A clinician is preparing to teach about bone matrix. Which information should be included? The component of the bone matrix that gives bone tensile strength is: a. Calcium b. Phosphate c. Collagen d. Magnesium ANS: C Collagen is the component of bone matrix that gives bone tensile strength. Calcium plays a role on bone formation, but collagen is the component of bone matrix that gives bone tensile strength. Phosphate plays a role in bone formation, but collagen is the component of bone matrix that gives bone tensile strength. Magnesium plays a role in bone formation, but collagen is the component of bone matrix that gives bone tensile strength. Cognitive Level: Comprehension 954 2. Which information indicates the nurse has a good understanding of osteoblasts? Once their initial function is complete, osteoblasts become: a. Osteoclasts b. Osteocytes c. Chondroblasts d. Osteoids ANS: B Osteoblasts are the bone-forming cells. Their primary function is to lay down new bone. Once this function is complete, osteoblasts become osteocytes. Osteoclasts reabsorb bone. Chondroblasts are a part of mature bone. Osteoids are part of non-mineralized bone matrix that the osteoblasts work on. Cognitive Level: Comprehension 955 3. Which information indicates the nurse understands osteocalcin? Osteocalcin is a: a. Glycoprotein b. Hormone c. Mineral d. Vitamin ANS: A Osteocalcin is a glycoprotein. Osteocalcin is a glycoprotein, not a hormone. Osteocalcin is a glycoprotein, not a mineral. Osteocalcin is a glycoprotein, not a vitamin. Cognitive Level: Comprehension 958 4. A clinician is preparing to discuss hydroxyapatite. Which information should be included? Hydroxyapatite in the bone matrix contains which of the following molecules in its crystalline structure? a. Calcium and magnesium b. Calcium and phosphate c. Phosphate and magnesium d. Magnesium and hydrogen ANS: B Calcium and phosphate form amorphous (fluid) calcium phosphate compounds that are converted, in stages, to solid hexagonal crystals of hydroxyapatite. Hydroxyapatite contains calcium and phosphate, not calcium and magnesium. Hydroxyapatite contains calcium and phosphate, not phosphate and magnesium. Hydroxyapatite contains calcium and phosphate, not magnesium and hydrogen. Cognitive Level: Comprehension 958 5. Which information indicates the nursing student has a good understanding between compact bone and spongy bone? The major difference between compact bone and spongy bone is the: a. Organization of the structural elements b. Location within the body c. Activating chemicals in each d. Types of minerals in the bone matrix ANS: A The major difference between the two types of tissue is the organization of the elements. The major difference between the two types of tissue is the organization of the elements, not the location in the body. The major difference between the two types of tissue is the organization of the elements, not the activating chemicals in each. The major difference between the two types of tissue is the organization of the elements, not the type of minerals. Cognitive Level: Comprehension 960 6. A staff member asks a nurse how blood gets to the bone. How should the nurse reply? Blood vessels penetrate to the inner structures of the bone via: a. Volkmann canals b. Canaliculi c. Sharpey fibers d. Lamellae ANS: A The outer layer of the periosteum contains blood vessels and nerves, some of which penetrate to the inner structures of the bone through channels called Volkmann canals. Canaliculi are small channels or canals. Sharpey fibers also help hold or attach tendons and ligaments to the periosteum of bones. Concentric layers of bone matrix are called lamellae. Cognitive Level: Comprehension 960 7. A nurse is preparing to teach the staff about bones. Which information should the nurse include? After puberty, the epiphyseal plate calcifies, and the epiphysis and merge. a. Epiphyseal line b. Diaphyseal plate c. Metaphysis d. Articular cartilage ANS: C After puberty, the epiphyseal plate calcifies, and the epiphysis and metaphysis merge. After puberty, the epiphyseal plate calcifies, and the epiphysis and metaphysis, not the epiphyseal line, merge. After puberty, the epiphyseal plate calcifies, and the epiphysis and metaphysis, not the diaphyseal plate, merge. After puberty, the epiphyseal plate calcifies, and the epiphysis and metaphysic, not the articular cartilage, merge. Cognitive Level: Comprehension 960 8. When a staff member asks how remodeling of bone occurs, what is the nurses best response? Remodeling is done by clusters of bone cells called: a. Precursor stimulating cells b. Osteoclastic cutting cones c. Basic multicellular units d. Haversian system cells ANS: C Remodeling is carried out by clusters of bone cells termed basic multicellular units. Precursor cells differentiate into osteoclasts and osteoblasts. The osteoclasts form a cutting cone, which gradually resorbs bone, not remodels it. Haversian canals are part of compact bone. Cognitive Level: Comprehension 961 9. A nurse is discussing the different phases of bone remodeling. Which information should be included? Phase 2 of the bone remodeling cycle involves bone: a. Formation b. Activation c. Resorption d. Fracturing ANS: C Phase 2 is resorption. Phase 2 is resorption, not formation. Phase 2 is resorption, not activation. Phase 2 is resorption, not fracturing. Cognitive Level: Comprehension 962 10. When the physical therapist is describing a freely movable joint, which term should be used? a. Synarthrosis b. Amphiarthrosis c. Fibrous d. Diarthrosis ANS: D A diarthrotic joint is freely moveable. A synarthrotic joint is immovable. An amphiarthrotic joint is slightly movable. A fibrous joint has little, if any, movement. Cognitive Level: Comprehension 963 11. A nurse recalls fibrous joints generally are: a. Rotating b. Slightly movable c. Freely movable d. Calcified ANS: B A fibrous joint has little, if any, movement. A fibrous joint has little, if any, movement; it is not rotating. A fibrous joint has little, if any, movement; it is not freely moveable. A fibrous joint has little, if any, movement; it is not calcified. Cognitive Level: Comprehension 963 12. Which of the following should the nurse include when discussing the different types of cartilaginous joints? a. Sutures and gomphosis b. Syndesmosis and gomphosis c. Symphysis and synchondrosis d. Gomphosis and synchondrosis ANS: C There are two types of cartilaginous joints: symphyses and synchondroses. There are two types of cartilaginous joints: symphyses and synchondroses. It is not sutures and gomphosis. There are two types of cartilaginous joints: symphyses and synchondroses. It is not syndesmosis and gomphosis. There are two types of cartilaginous joints: symphyses and synchondroses. It is not gomphosis and synchondrosis. Cognitive Level: Comprehension 964 13. Which statement indicates the nurse has a good understanding of joints? The joints between the teeth and the maxilla or mandible are examples of a: a. Symphysis b. Diarthrosis c. Gomphosis d. Syndesmosis ANS: C The teeth held in the maxilla or mandible are gomphosis joints. The teeth held in the maxilla or mandible are gomphosis joints, not symphysis. The teeth held in the maxilla or mandible are gomphosis joints, not diarthrosis. The teeth held in the maxilla or mandible are gomphosis joints, not syndesmosis. Cognitive Level: Comprehension 964 14. A nurse recalls the elbow joint is an example of a(n): a. Amphiarthrosis b. Diarthrosis c. Synarthrosis d. Symphysis ANS: B The elbow joint is an example of a diarthrosis joint. The elbow joint is freely moveable and is an example of a diarthrosis joint; amphiarthrosis joints are only slightly moveable. The elbow joint is freely moveable and is an example of a diarthrosis joint; synarthrosis joints are immoveable. The elbow joint is freely moveable and is an example of a diarthrosis joint; a symphysis is a cartilaginous joint in which bones are united by a pad or disk of fibrocartilage. Cognitive Level: Comprehension 965 15. When a staff member asks where costal cartilage is located, how should the nurse respond? Between the: a. Vertebrae b. Ribs and sternum c. Sutures of the skull d. Facial bones ANS: B Costal cartilage is located between the ribs and the sternum. Costal cartilage is not found between the vertebrae. Costal cartilage is not found between the sutures of the skull. Costal cartilage is not found between the facial bones. Cognitive Level: Comprehension 964 16. The epimysium, perimysium, and endomysium are made of: a. Bone b. Epithelium c. Fascia d. Cartilage ANS: C Each skeletal muscle is a separate organ, encased in a three-part connective tissue framework called fascia. Each skeletal muscle is a separate organ, encased in a three-part connective tissue framework called fascia. It is not bone. Each skeletal muscle is a separate organ, encased in a three-part connective tissue framework called fascia. It is not epithelium. Each skeletal muscle is a separate organ, encased in a three-part connective tissue framework called fascia. It is not cartilage. Cognitive Level: Comprehension 965 17. Which layer forms the fascicles in skeletal muscle? a. Tendon sheath b. Endomysium c. Epimysium d. Perimysium ANS: D The perimysium further subdivides the muscle fibers into bundles of connective tissue called fascicles. The perimysium further subdivides the muscle fibers into bundles of connective tissue called fascicles. It is not the tendon sheath. The endomysium is the smallest unit of muscle. The outermost layer, the epimysium, is located on the surface of the muscle and tapers at each end to form the tendon. Cognitive Level: Comprehension 967 18. When a staff member asks the nurse about the contractile unit of a muscle, how should the nurse reply? The contractile unit of a muscle cell is called the: a. Motor unit b. Basement membrane c. Myofibril d. Ribosome ANS: C The muscle fiber contains bundles of myofibrils, the fibers functional subunits. The muscle fiber contains bundles of myofibrils, not the motor unit; it is the fibers functional subunits. The muscle fiber contains bundles of myofibrils, the fibers functional subunits. It is not the basement membrane. The muscle fiber contains bundles of myofibrils, the fibers functional subunits. It is not the ribosome. Cognitive Level: Comprehension 968 19. An isolated muscle is believed to be a type 1 fiber. Which of the following should be observed by the nurse when the muscle is stimulated? a. The muscle resists fatigue. b. The muscle tires easily. c. The muscle will not contract. d. The muscle has no fascia. ANS: A Type I fibers can resist fatigue for longer periods because of their capacity for oxidative metabolism. Type I fibers resist fatigue; it would not tire easily. Type I fibers resist fatigue; not contracting does not describe a type I fiber. Type I fibers resist fatigue; it would not be that the muscle has no fascia. Cognitive Level: Comprehension 968 20. An isolated muscle is believed to be a type II fiber. Which of the following should be observed by the nurse when the muscle is stimulated? a. The muscle has slow contraction speed. b. The muscle is fatigued easily. c. The muscle has a profuse capillary supply. d. The muscle has no fascia. ANS: B Type II fibers rely on anaerobic glycolytic metabolism and fatigue readily. Type II fibers rely on anaerobic glycolytic metabolism and fatigue readily. They may not have slow contraction speed. Type II fibers rely on anaerobic glycolytic metabolism and fatigue readily. The do not have additional capillary supply. Type II fibers rely on anaerobic glycolytic metabolism and fatigue readily. They do have fascia around the muscle. Cognitive Level: Comprehension 969 | p. 972 21. When the nurse is using the term sarcopenia, what is the nurse describing? It is the: a. Absence of muscle cells b. Fatigue of muscle cells c. Age-related loss in skeletal muscle d. Muscles that are unable to contract ANS: C Age-related loss in skeletal muscle is referred to as sarcopenia and is a direct cause of the age- related decrease in muscle strength. Age-related loss in skeletal muscle is referred to as sarcopenia and is a direct cause of the age- related decrease in muscle strength. It is not the absence of muscle cells. Age-related loss in skeletal muscle is referred to as sarcopenia and is a direct cause of the age- related decrease in muscle strength. It is not muscle fatigue. Age-related loss in skeletal muscle is referred to as sarcopenia and is a direct cause of the age- related decrease in muscle strength. It is not muscles that cannot contract. Cognitive Level: Comprehension 974 22. A nurse is preparing to teach about myofibrils. Which information should the nurse include? The structure of the contractile subunit of the myofibril is called the: a. Sarcoplasmic reticulum b. Actin c. Motor endplate d. Sarcomere ANS: D The sarcomere is the contractile portion of the myofibril. The sarcoplasmic reticulum is made like the endoplasmic reticulum in other cells. Actin is a protein of the sarcomere. It is at the motor nerve endplate where the nerve impulse is transmitted. Cognitive Level: Comprehension 968 23. While planning care for a patient with muscle problems, which information should the nurse remember? ions directly control the contraction of muscles. a. Sodium b. Potassium c. Calcium d. Magnesium ANS: C Contraction begins as the calcium ions combine with troponin, a reaction that overcomes the inhibitory function of the troponin-tropomyosin system. Calcium, not sodium, controls the contraction of muscles. Calcium, not potassium, controls the contraction of muscles. Calcium, not magnesium, controls the contraction of muscles. Cognitive Level: Comprehension 972 24. A patient has researched muscles on the internet. Which information indicates the patient has a good understanding? The molecule that prevents a muscle contraction from occurring when the muscle is at rest is: a. Calcium b. Troponin-tropomyosin c. Actin d. Myosin ANS: B Contraction begins as the calcium ions combine with troponin, a reaction that overcomes the inhibitory function of the troponin-tropomyosin system. Calcium does not prevent contraction; it could facilitate it. Actin does not prevent contraction; it facilitates it. Myosin facilitates contraction. Cognitive Level: Comprehension 972 25. A nursing student wants to know during which stage actin binds to myosin. What is the nurses best response? During: a. Coupling b. Relaxation c. Discharging d. Excitation ANS: A During coupling, depolarization of the transverse tubules occurs. This triggers the release of calcium ions from the sarcoplasmic reticulum, exposing binding sites on the actin molecule. Relaxation is the last step. It begins as calcium ions are actively transported back into the sarcoplasmic reticulum, removing ions from interaction with troponin. Discharging is not a step in the process. Excitation is the first step of muscle contraction and it begins with the spread of an action potential from the nerve terminal to the neuromuscular junction. Cognitive Level: Comprehension 972 26. When a patient asks what the fuel for skeletal muscle contraction is, how should the nurse respond? The main energy source or fuel for skeletal muscle contraction is: a. Calcium b. Lactic acid c. Adenosine triphosphate (ATP) d. Actin ANS: C The main energy source for muscle contraction is ATP. The main energy source for muscle contraction is ATP, not calcium. The main energy source for muscle contraction is ATP, not lactic acid. The main energy source for muscle contraction is ATP, not actin. Cognitive Level: Comprehension 972 27. The nurse observed the patients muscle contracted, but the limb did not move. How should the nurse chart this muscle contraction? a. Isotonic contraction b. Isometric contraction c. Eccentric contraction d. Concentric contraction ANS: B During isometric contraction, the muscle contracts, but the limb does not move. During isotonic contraction, the muscle maintains a constant tension as it moves. Eccentric contraction is a form of isotonic contraction. Concentric contraction is a form of isotonic contraction. Cognitive Level: Comprehension 973 28. A nurse recalls that when a muscle acts as the prime mover, it is called the: a. Flexor b. Recruiter c. Antagonist d. Agonist ANS: D When a muscle contracts and acts as a prime mover, it is called an agonist. When a muscle contracts and acts as a prime mover, it is called an agonist, not a flexor. When a muscle contracts and acts as a prime mover, it is called an agonist, not a recruiter. When a muscle contracts and acts as a prime mover, it is called an agonist; its reciprocal muscle, or antagonist, relaxes. Cognitive Level: Comprehension 973 MULTIPLE RESPONSE 1. The nurse has a good understanding of bone matrix when he comments that the following molecules are part of the bone matrix? (Select all that apply.) a. Collagen fibers b. Elastin fibers c. Proteoglycans d. Glycoproteins e. Epithelial cells ANS: A, B, D Bone matrix is composed of collagen fibers, proteoglycans, and glycoproteins. Cognitive Level: Comprehension 955 2. The nursing student has a good understanding of glycoproteins when he states that the following glycoproteins are present in the bone? (Select all that apply.) a. Osteocalcin b. Sialoprotein c. Bone albumin d. Alpha-glycoprotein e. Collagen ANS: A, B, C, D Four glycoproteins are present in bone: sialoprotein, which binds easily with calcium; osteocalcin, which binds preferentially to crystallized calcium; bone albumin, which is identical to serum albumin and possibly transports essential nutrients to and from bone cells and maintains the osmotic pressure of bone fluid; and alpha-glycoprotein (-glycoprotein). Collagen is not a glycoprotein. Cognitive Level: Comprehension 958 3. A patient has researched compact bones on the Internet. Which information indicates the patient has a good understanding of compact bone? The structures present in compact bone include the (select all that apply): a. Haversian canals b. Trabeculae c. Canaliculi d. Lamellae e. Lacunae ANS: A, C, D, E Compact bone is highly organized, solid, and extremely strong. The basic structural unit in compact bone is the haversian system. Each haversian system is made up of haversian canals, lamellae, and canaliculi. Trabeculae are found in spongy bone. Cognitive Level: Comprehension 960 4. Which information indicates the staff member has a good understanding of bone classifications? The shapes that represent bone classifications include (select all that apply): a. Long b. Flat c. Short d. Irregular e. Round ANS: A, B, C, D Bones can be classified by shape as long, flat, short (cuboidal), or irregular. Chapter 41. Alterations of Musculoskeletal Function MULTIPLE CHOICE 1. The incidence of fractures of the pelvis is highest in: a. Preadolescent boys b. Adolescent boys c. Adolescent girls d. Older adults ANS: D The incidence of fractures of the upper femur, upper humerus, vertebrae, and pelvis is highest in older adults and is often associated with osteoporosis. Fractures of healthy bones, particularly the tibia, clavicle, and lower humerus, tend to occur in young persons. Fracture of the pelvis is highest in older adults. Fractures of healthy bones, particularly the tibia, clavicle, and lower humerus, tend to occur in young persons. Fracture of the pelvis is highest in older adults. Fractures of healthy bones, particularly the tibia, clavicle, and lower humerus, tend to occur in young persons. Fracture of the pelvis is highest in older adults. Cognitive Level: Comprehension 978 2. A 65-year-old Hispanic female is admitted to the hospital with a pathologic, compound, transverse fracture of the femur. Which of the following statements best describes this type of fracture? a. The fracture line is parallel to the bone. b. The fracture line is straight across the bone. c. The fracture line is perpendicular to the bone. d. The fracture line is vertical to the shaft of the bone. ANS: B A transverse fracture occurs straight across the bone. A linear fracture runs parallel to the long axis of the bone. A transverse fracture runs straight across the bone, not perpendicular. A transverse fracture runs straight across the bone, not vertically. Cognitive Level: Comprehension 979 3. A 70-year-old female with osteoporosis fractures her leg at a location of preexisting abnormality. She reports that the fracture occurred following a minor fall. Which of the following best describes the fracture? a. Fatigue fracture b. Stress fracture c. Pathologic fracture d. Greenstick fracture ANS: C A pathologic fracture is a break at the site of a preexisting abnormality, usually by force that would not fracture a normal bone. A fatigue fracture is caused by abnormal stress or torque applied to a bone with normal ability to deform and recover. Stress fractures occur in normal or abnormal bone that is subjected to repeated stress, such as occurs during athletics. A greenstick fracture perforates one cortex and splinters the spongy bone. Cognitive Level: Comprehension 979 4. A 32-year-old obese male begins a jogging routine. A week after beginning, he fractures his leg. This is referred to as a what type of fracture? a. Comminuted b. Greenstick c. Fatigue d. Compound ANS: C A fatigue fracture is caused by abnormal stress or torque applied to a bone that usually occurs in individuals who engage in a new activity that is both strenuous and repetitive. A comminuted fracture is one in which a bone breaks into two or more fragments. A greenstick fracture perforates one cortex and splinters the spongy bone. An open fracture is a complete and incomplete fracture that breaks through the skin. Cognitive Level: Comprehension 980 5. Transchondral fractures are most prevalent in: a. Adolescents b. Older adults c. Infants d. Premenopausal females ANS: A Transchondral fractures are most prevalent in adolescents. Transchondral fractures are most prevalent in adolescent, not older adults. Transchondral fractures are most prevalent in adolescents, not infants. Transchondral fractures are most prevalent in adolescents, not premenopausal females. Cognitive Level: Comprehension 980 6. A 35-year-old female suffers a broken clavicle following a motor vehicle accident. X-ray reveals that the bone surfaces in the joint partially lost contact with each other. This condition is called: a. Dislocation b. Subluxation c. Distortion d. Nonunion ANS: B Subluxation occurs when contact between the opposing joint surfaces of a fracture are partially lost. Dislocation is the displacement of one or more bones in a joint in which the opposing joint surfaces lose contact entirely. Distortion is not a term applicable to fracture healing. Nonunion is failure of the bone ends to grow together. Cognitive Level: Comprehension 981 7. A 12-year-old female hurts her ankle while playing basketball. Tests reveal that she tore a ligament. This condition is known as a: a. Sprain b. Strain c. Disunion d. Subluxation ANS: A A torn ligament is also called a sprain. Tearing or stretching of a muscle or tendon is commonly known as a strain. Disunion occurs when fracture ends fail to heal. Subluxation occurs when contact between the opposing joint surfaces of a fracture are partially lost. Cognitive Level: Comprehension 982 8. A 36-year-old male complains of pain and weakness in the elbow. He reports that he is a warehouse worker and lifts boxes daily. MRI reveals inflammation of the tendon where it attaches to bone. This condition is called: a. Periostitis b. Muscle strain c. Bursitis d. Epicondylopathy ANS: D When force is sufficient to cause microscopic tears (microtears) in tissue, the result is known epicondylopathy. When force is sufficient to cause microscopic tears (microtears) in tissue, the result is known epicondylopathy, not periostitis. Muscle strain is local muscle damage that occurs when the muscle is stretched beyond capacity. Bursitis is inflammation of the bursae. Cognitive Level: Comprehension 982 9. An important and useful clinical measure in the diagnosis of rhabdomyolysis is measurement of which laboratory value? a. White blood cell count b. Antinuclear antibodies c. Aspartate aminotransferase d. Creatine kinase (CK) ANS: D The most important and clinically useful measurement in rhabdomyolysis is serum CK. A level five times the upper limit of normal (about 1000 units/liter) is used to identify rhabdomyolysis. White blood cell count may be measured, but it is not more important than the CK. Antinuclear antibodies may be measured, but it is not more important than the CK. Aspartate aminotransferase may be measured, but it is not more important than the CK. Cognitive Level: Comprehension 985 10. Which of the following clinical findings would be expected in the patient with rhabdomyolysis? a. Sweating b. Dark urine c. Yellow color to the skin d. Lower extremity swelling ANS: B A classic triad of muscle pain, weakness, and dark urine is considered typical of rhabdomyolysis. Dark urine, not sweating, is a classic sign of rhabdomyolysis. Dark urine, not yellow skin, is a classic sign of rhabdomyolysis. Dark urine, not lower extremity swelling, is a classic sign of rhabdomyolysis. Cognitive Level: Comprehension 984 11. A 70-year-old female presents with a hip fracture secondary to osteoporosis. This condition is caused by an increase in bone: a. Density b. Formation c. Resorption d. Mineralization ANS: C Osteoporosis is due to an increase in bone resorption. Osteoporosis is due to an increase in bone resorption; density would be decreased, not increased. Osteoporosis is due to an increase in bone resorption, not formation. Osteoporosis is due to an increase in bone resorption, not mineralization. Cognitive Level: Comprehension 988 12. A 70-year-old female presents with a hip fracture. She is diagnosed with osteoporosis. One factor that most likely contributed to her condition is: a. Increased androgen levels b. Decreased estrogen levels c. Strenuous exercise d. Excessive dietary calcium ANS: B Osteoporosis can be attributed to decreased estrogen levels. Osteoporosis can be attributed to decreased estrogen levels, not increased androgen levels. Osteoporosis can be attributed to decreased estrogen levels, not strenuous exercise. Osteoporosis can be attributed to decreased estrogen levels, not excessive dietary calcium. Cognitive Level: Comprehension 989 13. A 76-year-old female was diagnosed with osteoporosis by radiologic exam. She is at high risk for: a. Bone infections b. Joint injuries c. Pathologic bone fractures d. Ssteomalacia ANS: C The patient will be at risk for pathologic bone fractures due to bone fragility. The patient will not be at increased risk for infection. The patient could be at risk for joint injury, but will be at greatest risk for fracture. The patient is not at risk for osteomalacia. Cognitive Level: Comprehension 989 14. An 80-year-old male presents with skeletal pain and tenderness, especially in the hips. He is diagnosed with osteomalacia caused by: a. Collagen breakdown in the bone matrix b. Excessive bone resorption c. Crowding of bone marrow by excessive bone growth d. Inadequate bone mineralization ANS: D Osteomalacia is a metabolic disease characterized by inadequate and delayed mineralization of osteoid in mature compact and spongy bone. Idiopathic osteoarthritis leads to collagen breakdown. Giant cell tumors promote excessive bone resorption. Abnormal remodeling causes crowding of bone marrow. Cognitive Level: Comprehension 993 15. A 56-year-old male was admitted to the hospital with a diagnosis of osteomalacia. History reveals that he takes anticonvulsants, underwent small bowel resection 3 years earlier, and suffers from chronic pancreatitis. What is the common link between these three factors and the development of osteomalacia? a. Impaired phosphate absorption b. Increased calcium excretion c. Vitamin D deficiency d. Impaired vitamin C metabolism ANS: C Disorders of the small bowel, hepatobiliary system, and pancreas are causes of vitamin D deficiency in the United States. Vitamin D deficiency is the most important factor in osteomalacia. Vitamin D deficiency, not impaired phosphate absorption, is the common cause of osteomalacia. Vitamin D deficiency, not increased calcium excretion, is the common cause of osteomalacia. Vitamin D deficiency, not impaired vitamin C metabolism, is the common cause of osteomalacia. Cognitive Level: Comprehension 993 16. A disorder similar to osteomalacia that occurs in growing bones of children is termed: a. Paget disease b. Rickets c. Osteomyelitis d. Osteosarcoma ANS: B Abnormal bone growth in children is termed rickets. Paget disease is a state of increased metabolic activity in bone characterized by abnormal and excessive bone remodeling, both resorption and formation. Osteomyelitis is a bone infection. Osteosarcoma is a form of bone cancer. Cognitive Level: Comprehension 993 17. The cause of Paget disease is: a. Fluoride deficiency b. Unknown at present c. Excess vitamin A d. Osteogenic sarcoma ANS: B The cause of Paget disease is unknown. The cause of Paget disease is unknown; it is not due to fluoride deficiency. The cause of Paget disease is unknown; it is not due to excess vitamin A. The cause of Paget disease is unknown; it is not due to osteosarcoma. Cognitive Level: Comprehension 994 18. A 70-year-old male presents with back pain, fever, and weight loss. He reports that he had a recent respiratory infection from which he thought he recovered. Tests revealed increased white blood cell count, and a diagnosis of endogenous osteomyelitis was made. The primary organism causing this condition is: a. Staphylococcus aureus b. Salmonella c. Mycobacterium d. Haemophilus influenza ANS: A Staphylococcus aureus remains the primary microorganism responsible for osteomyelitis. Staphylococcus aureus, not Salmonella, remains the primary microorganism responsible for osteomyelitis. Staphylococcus aureus, not Mycobacterium, remains the primary microorganism responsible for osteomyelitis. Staphylococcus aureus, not Haemophilus influenza, remains the primary microorganism responsible for osteomyelitis. Cognitive Level: Comprehension 995 19. A 54-year-old female was recently diagnosed with degenerative joint disease. This condition is characterized by loss of: a. The epiphyses b. Articular cartilage c. Synovial fluid d. The joint capsule ANS: B Degenerative joint disease is caused by loss of the articular cartilage. Degenerative joint disease is caused by loss of the articular cartilage, not the epiphyses. Degenerative joint disease is caused by loss of the articular cartilage, not the synovial fluid. Degenerative joint disease is caused by loss of the articular cartilage, not the joint capsule. Cognitive Level: Comprehension 996 20. A 54-year-old male was recently diagnosed with rheumatoid arthritis (RA). Which of the following is the expected treatment of choice? a. Nonsteroidal anti-inflammatory drugs (NSAIDs) b. Gold salts c. Methotrexate d. Hydroxychloroquine ANS: C Methotrexate remains the first line of treatment for RA. Methotrexate, not NSAIDs, remains the first line of treatment for RA. Methotrexate, not gold salts, remains the first line of treatment for RA. Methotrexate, not hydroxychloroquine, remains the first line of treatment for RA. Cognitive Level: Comprehension 1002 21. Researchers now believe that RA is: a. Curable with antiviral agents b. An autoimmune disease c. A complication of rheumatic fever d. Related superficial joint injury ANS: B RA is now thought to be an autoimmune disease. RA is an incurable disease. RA is not a complication of rheumatic fever. RA is not due to joint injury. Cognitive Level: Comprehension 999 22. A 34-year-old female was recently diagnosed with RA. Physical examination revealed that inflammation started in the: a. Synovial membrane b. Articular cartilage c. Subchondral bone d. Surrounding ligaments ANS: A Inflammation of RA starts in the synovial membrane. Inflammation of RA starts in the synovial membrane, not the articular cartilage. Inflammation of RA starts in the synovial membrane, not the subchondral bone. Inflammation of RA starts in the synovial membrane, not the surrounding ligaments. Cognitive Level: Comprehension 999 23. A 21-year-old female presents with low back pain and stiffness that is alleviated by physical activity. She was diagnosed with ankylosing spondylitis (AS). The first joint to be affected would be the: a. Sacroiliac b. Carpal c. Shoulder d. Knee ANS: A The sacroiliac joint is affected first, usually before any damage can be radiographically detected. The sacroiliac joint, not the carpal joint, is affected first, usually before any damage can be radiographically detected. The sacroiliac joint, not the shoulder, is affected first, usually before any damage can be radiographically detected. The sacroiliac joint, not the knee, is affected first, usually before any damage can be radiographically detected. Cognitive Level: Comprehension 1002 24. Which of the following people is at highest risk for the development of gout? a. Men aged 40 to 50 years b. Premenopausal women c. Male adolescents d. Female children ANS: A People at highest risk for gout are men aged 40 to 50 years of age. People at highest risk for gout are men aged 40 to 50 years of age, not premenopausal women. People at highest risk for gout are men aged 40 to 50 years of age, not male adolescents. People at highest risk for gout are men aged 40 to 50 years of age, not female children. Cognitive Level: Comprehension 1005 25. A 46-year-old male presents with severe pain, redness, and tenderness in the right big toe. He was diagnosed with gouty arthritis. The symptoms he experienced are caused by the crystallization of within the synovial fluid. a. Purines b. Pyrimidines c. Uric acid d. Acetic acid ANS: C Gout is caused by an increase in uric acid. Gout is caused by an increase of uric acid. Uric acid is a result of purine metabolism, but purine is not present in the joint. Gout is caused by an increase in uric acid, not pyrimidines. Gout is caused by an increase in uric acid, not acetic acid. Cognitive Level: Comprehension 1005 26. A 46-year-old male presents with severe pain, redness, and tenderness in the right big toe. He was diagnosed with gouty arthritis. He is at risk for developing: a. Cholelithiasis b. Myocarditis c. Renal stones d. Liver failure ANS: C Renal stones are 1000 times more prevalent in individuals with primary gout than in the general population. Renal stones, not cholelithiasis, are a risk factor in gout. Renal stones, not myocarditis, are a risk factor in gout. Renal stones, not liver failure, are a risk factor in gout. Cognitive Level: Comprehension 1005 27. A 51-year-old male experienced severe acute gouty arthritis. Which of the following is the most common trigger for the symptoms? a. Trauma b. Anemia c. High-fat foods d. Lack of exercise ANS: A Trauma is the most common trigger for gout symptoms. Trauma is the most common trigger for gout symptoms. Gout is not manifested by anemia. Trauma is the most common trigger for gout symptoms. Gout is not caused by high-fat foods, but high purine. Trauma, not lack of exercise, is the most common trigger for gout symptoms. Cognitive Level: Comprehension 1005 28. The final stage of gout, characterized by crystalline deposits in cartilage, synovial membranes, and soft tissue, is called: a. Monarticular arthritis b. Tophaceous gout c. Asymptomatic hyperuricemia d. Complicated gout ANS: B Tophaceous gout is a progressive inability to excrete uric acid, which expands the urate pool. Until urate crystal deposits (tophi) appear in cartilage, synovial membranes, tendons, and soft tissue. Tophaceous gout, not monarticular arthritis gout, is characterized by crystalline deposits. Asymptomatic hyperuricemia would not lead to crystalline deposits. Tophaceous gout, not complicated gout, is characterized by crystalline deposits. Cognitive Level: Comprehension 1007 29. A 32-year-old male was injured in a motor vehicle accident and confined to bed for 3 weeks. During this time, the size and strength of muscle fibers decreased, a condition referred to as: a. Myodysplasia b. Ischemic atrophy c. Disuse atrophy d. Deconditioning hypoplasia ANS: C The term disuse atrophy describes the pathologic reduction in normal size of muscle fibers after prolonged inactivity from bed rest. The patient is experiencing disuse atrophy, not myodysplasia. The patient is experiencing disuse atrophy, not ischemic, which would be due to decreased blood flow. The patient is experiencing disuse atrophy, not hypoplasia. Cognitive Level: Comprehension 1008 30. Fibromyalgia is a chronic musculoskeletal disorder characterized by: a. Pain resulting from joint and muscle inflammation b. Muscle pain in the back and gastrointestinal symptoms c. Neurologic pain in the skeletal muscles d. Diffuse pain, fatigue, and tender points ANS: D Fibromyalgia is characterized by diffuse pain, fatigue, and point tenderness. Fibromyalgia is not related to joint and muscle inflammation. Fibromyalgia is not related to specific back pain and is not manifested by gastrointestinal upset. Fibromyalgia is not related to neurologic pain in muscles. Cognitive Level: Comprehension 1008 31. Myotonia is characterized by: a. Prolonged depolarization of muscle cell membranes b. Absence of adenosine triphosphate (ATP) for muscle contraction c. Delayed muscle contraction d. Hyperactive reflexes ANS: A Myotonia is a delayed relaxation after voluntary muscle contraction caused by the prolonged depolarization of the muscle membrane. Myotonia is a delayed relaxation after voluntary muscle contraction caused by the prolonged depolarization of the muscle membrane, not due to absence of ATP for muscle contraction. Myotonia is a delayed relaxation after voluntary muscle contraction caused by the prolonged depolarization of the muscle membrane, not delayed muscle contraction. Myotonia is a delayed relaxation after voluntary muscle contraction caused by the prolonged depolarization of the muscle membrane, not hyperactive reflexes. Cognitive Level: Comprehension 1010 32. A 13-year-old female is admitted to the hospital for evaluation and treatment of an osteosarcoma in her left distal femur. Which statement best describes osteosarcoma? a. Myelogenic, develops in red bone marrow only b. Benign, develops in spongy bone tissue c. Collagenic, originates in the periosteum d. Osteogenic, most often develops in the bone marrow ANS: D Osteosarcomas are osteogenic tumors. Osteosarcomas are osteogenic tumors, not myelogenic. Osteosarcomas are osteogenic tumors, not benign. Osteosarcomas are osteogenic tumors, not collagenic. Cognitive Level: Comprehension 1015 33. A 60-year-old male presents with swelling and pain in the knee. CT reveals a tumor of spongy bone. His diagnosis would be: a. Chondrosarcoma b. Rhabdomyoma c. Rhabdomyosarcoma d. Fibrosarcoma ANS: A A chondrosarcoma is an ill-defined malignant tumor that infiltrates trabeculae in spongy bone. Rhabdomyoma is an extremely rare benign tumor of muscle that generally occurs in the tongue. The malignant tumor of striated muscle is called rhabdomyosarcoma. A fibrosarcoma is a solitary tumor that most often affects the metaphyseal region of the femur or tibia. Cognitive Level: Comprehension 1016 34. The most common cause of toxic myopathy is: a. Infection b. A tumor c. Alcoholism d. Osteoporosis ANS: C Alcohol remains the most common cause of toxic myopathy. Alcohol, not infection, remains the most common cause of toxic myopathy. Alcohol, not a tumor, remains the most common cause of toxic myopathy. Alcohol, not osteoporosis, remains the most common cause of myopathy. Cognitive Level: Comprehension 1012 35. A malignant tumor of striated muscle tissue origin is called: a. Myelogenic tumor b. Giant cell tumor c. Rhabdomyosarcoma d. Rhabdomyoma ANS: C The malignant tumor of striated muscle is called rhabdomyosarcoma. Myelogenic tumors originate from various bone marrow cells. Giant cell tumor is the sixth most common of the primary bone tumors. A rhabdomyoma is an extremely rare benign tumor of muscle that generally occurs in the tongue. Cognitive Level: Comprehension 1013 MULTIPLE RESPONSE 1. A 35-year-old female presents with impaired motor function and visual disturbances. The diagnosis is Paget disease. What additional symptoms would be expected? (Select all that apply.) a. Skull thickness b. Dementia c. Deafness d. Headache e. Hypertension ANS: A, B, C, D In Paget disease, the skull thickens and assumes an asymmetric shape. Thickened segments of the skull may compress areas of the brain, producing altered mentality and dementia. Impingement of new bone on cranial nerves causes deafness. Headache is commonly noted. Hypertension does not occur. Cognitive Level: Comprehension 994 2. Signs and symptoms of subluxation include (select all that apply): a. Pain b. Swelling c. Hemorrhage d. Limitation of movement e. Joint deformity ANS: A, B, D, E Signs and symptoms of dislocations or subluxations include pain, swelling, limitation of motion, and joint deformity. Cognitive Level: Comprehension 982 3. A 29-year-old male was recently diagnosed with AS. He is interested in obtaining more information about his disease. Patient teaching would include which of the following? (Select all that apply.) a. A diagnosis is made from history, physical examination, x-rays, and genetic analysis. b. Inflammation of the fibrocartilage in cartilaginous joints results in the erosion of bone structure, scar tissue formation, and joint fusion. c. The more common signs and symptoms of early disease include restricted joint movement and increased pain after physical activity. d. The usual treatment includes anti-inflammatory and analgesic medications, exercises, and physical therapy. e. The spine becomes bent forward as the normal convex curve of the lower spine diminishes. ANS: A, B, D, E The most common signs and symptoms of early AS are low back pain and stiffness. Typically, the individual with primary disease develops low back pain during the early 20s. The pain is at first insidious but progressively becomes persistent. It is often worse after prolonged rest and is alleviated by physical activity. The normal convex curve of the lower spine (lumbar lordosis) diminishes and concavity of the upper spine (kyphosis) increases. NSAIDs will often provide temporary symptom relief within 48 hours. Analgesic medications are prescribed to suppress some of the pain and stiffness and to facilitate exercise. Cognitive Level: Comprehension 1004 4. The pattern of bone destruction indicative of an aggressive malignant tumor is known as J pattern. (Select all that apply.) a. Moth-eaten b. Permeative c. Geographic d. Radial e. Selective ANS: A, B, C Three patterns of bone destruction by bone tumors have been identified: (1) the geographic pattern, (2) the moth-eaten pattern, and (3) the permeative pattern. Radial and selective are not considered patterns of malignancy. Cognitive Level: Comprehension 1014 COMPLETION 1. To make a diagnosis of fibromyalgia, tenderness must be present in of the 18 points necessary for diagnosis. ANS: 11 Chapter 42. Alterations of Musculoskeletal Function in Children MULTIPLE CHOICE 1. While performing an assessment of a 2-month-old, the nurse notes a positive Ortolani click. The nurse would suspect the child has: a. A hip fracture b. Hip dysplasia c. Osteogenesis imperfecta d. Osteomyelitis ANS: B Ortolani click is symptomatic of developmental dysplasia of the hip. A hip fracture would be evident by shortening of the leg and external rotation. Osteogenesis imperfecta is diagnosed by fractures. Osteomyelitis is diagnosed by fever and infection. Cognitive Level: Comprehension 1024 2. A 9-month-old male was diagnosed with osteogenesis imperfecta (OI) following recurrent fractures and findings of osteopenia. This disease is caused by: a. Uterine teratogens b. A genetic defect c. Malnutrition d. Trauma ANS: B OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, the main component of bone and blood vessels. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, the main component of bone and blood vessels. It is not due to teratogens. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, the main component of bone and blood vessels. It is not due to malnutrition. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, the main component of bone and blood vessels. It is not due to trauma, although trauma does result in fracture. Cognitive Level: Comprehension 1025 3. A 9-month-old male was diagnosed with OI following recurrent fractures and findings of osteopenia. This disease is caused by errors in the synthesis of: a. Elastin b. Glycoproteins c. Collagen d. Calcium salts ANS: C OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, not elastin. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, not glycoproteins. OI (brittle bone disease) is a spectrum of disease caused by genetic mutation in the gene that encodes for type I collagen, not calcium salts. Cognitive Level: Comprehension 1025 4. Children with OI suffer from frequent: a. Bone fractures b. Dislocations c. Bone infections d. Joint injuries ANS: A Children with OI suffer from bone fractures. Children with OI suffer from bone fractures, not dislocations. Children with OI suffer from bone fractures, not bone infections. Children with OI suffer from bone fractures, not joint injuries. Cognitive Level: Comprehension 1025 5. A 1-year-old female was diagnosed with OI. Which of the following is a complication in this patient? a. Congestive heart failure b. Liver failure c. Aortic aneurysm d. Pulmonary emboli ANS: C Because type I collagen also is the main component of blood vessels, vascular deformity, such as aortic aneurysm, can occur. Aortic aneurysm, not congestive heart failure, could occur in this child. Aortic aneurysm, not liver failure, could occur in this child. Aortic aneurysm, not pulmonary emboli, could occur in this child. Cognitive Level: Comprehension 1025 6. A 5-year-old female was diagnosed with seropositive juvenile rheumatoid arthritis (RA). The treatment option for this disease is termed: a. Supportive b. Curative c. Antibacterial d. Experimental ANS: A Treatment is supportive, not curative. Nonsteroidal anti-inflammatory drugs (NSAIDs) are a mainstay, and methotrexate is also being used with success. The aims are to minimize inflammation and deformity. Treatment is supportive, not curative. Juvenile RA is not infectious, so treatment is not antibacterial. Treatment may include experimental options, but the treatment remains supportive. Cognitive Level: Comprehension 1027 7. LCP disease affects which of the following joints? a. Vertebral b. Shoulder c. Hip d. Knee ANS: C LCP affects the hip. LCP affects the hip, not the vertebrae. LCP affects the hip, not the shoulder. LCP affects the hip, not the knee. Cognitive Level: Comprehension 1029 8. Osgood-Schlatter disease causes inflammation of the: a. Shoulder joint b. Patellar tendon c. Elbow ligaments d. Hip cartilage ANS: B Osgood-Schlatter disease affects the patella. Osgood-Schlatter affects the patella, not the shoulder. Osgood-Schlatter affects the patella, not the elbow. Osgood-Schlatter affects the patella, not the hip. Cognitive Level: Comprehension 1029 9. Which of the following types of scoliosis accounts for the majority of the cases of scoliosis? a. Idiopathic b. Infectious c. Iatrogenic d. Secondary ANS: A Eighty percent of all scoliosis is idiopathic. Eighty percent of all scoliosis is idiopathic, not infectious. Eighty percent of all scoliosis is idiopathic, not iatrogenic. Eighty percent of all scoliosis is idiopathic, not secondary. Cognitive Level: Comprehension 1029 10. A 3-year-old male presents with developmental delay. Testing reveals that the child has muscular dystrophy. Treatment will include: a. Aspirin b. Antivirals c. Steroids d. Chemotherapy ANS: C Treatment with steroids can prolong the ability to walk by several years and improves life expectancy. Treatment with steroids, not aspirin, can prolong the ability to walk by several years and improves life expectancy. Treatment with steroids, not antivirals, can prolong the ability to walk by several years and improves life expectancy. Treatment with steroids, not chemotherapy, can prolong the ability to walk by several years and improves life expectancy. Cognitive Level: Comprehension 1031 11. The treatment of Osgood-Schlatter disease includes: a. Steroids b. Restriction from physical activity c. High doses of aspirin d. Knee replacement ANS: B The primary treatment of Osgood-Schlatter disease includes restriction from physical activity. The primary treatment of Osgood-Schlatter disease includes restriction from physical activity, not steroids. The primary treatment of Osgood-Schlatter disease includes restriction from physical activity, not high doses of aspirin. The primary treatment of Osgood-Schlatter disease includes restriction from physical activity, not knee replacement. Cognitive Level: Comprehension 1029 12. Duchenne muscular dystrophy (DMD) has a(n) inheritance pattern. a. Autosomal recessive b. X-linked recessive c. Y-linked dominant d. Autosomal dominant ANS: B DMD is X-linked, occurring only in boys. DMD is X-linked, not autosomal recessive. DMD is X-linked, not Y-linked. DMD is X-linked, not autosomal dominant. Cognitive Level: Comprehension 1030 13. The onset of DMD most often occurs at: a. 3 to 6 months of age b. Preschool years c. School age d. The onset of puberty ANS: C Boys with DMD will present in the preschool years with muscle weakness, difficulty walking, and large calves. Boys with DMD will present in the preschool years, not as early as 3 to 6 months. Boys with DMD will present in the preschool years, not as late as school age. Boys with DMD will present in the preschool years with muscle weakness, not at puberty. Cognitive Level: Comprehension 1030 14. A 22-year-old female has a brother with DMD and wants to know if her children will inherit it. A fairly accurate test to identify female carriers of the disease is measurement of serum levels of: a. Dystrophin b. Myoglobin c. Creatine kinase (CK) d. Troponin 1 ANS: C Diagnosis is confirmed by measuring the blood CK level, which is sometimes 100 times the normal level, with confirmation by genetic testing for mutations in the dystrophin gene. Diagnosis is confirmed by measuring the blood CK level, which is sometimes 100 times the normal level, with confirmation by genetic testing for mutations in the dystrophin gene. Diagnosis is confirmed by measuring the blood CK level, which is sometimes 100 times the normal level, with confirmation by genetic testing for mutations in the dystrophin gene. Diagnosis is confirmed by measuring the blood CK level, which is sometimes 100 times the normal level, with confirmation by genetic testing for mutations in the dystrophin gene. Cognitive Level: Comprehension 1031 15. A 13-year-old female presents with pain at night, cough, and dyspnea. Testing reveals a metastasizing malignant bone tumor. The most likely type of tumor is: a. Nonossifying fibroma b. Chondrosarcoma c. Ewing sarcoma d. Osteosarcoma ANS: D With osteosarcoma, the most common presenting complaint is pain. Night pain, awakening a child from sleep, is a particularly foreboding sign. There may be swelling, warmth, and redness caused by the vascularity of the tumor. Symptoms also may include cough, dyspnea, and chest pain if lung metastasis is present. a With osteosarcoma, not nonossifying fibroma, the most common presenting complaint is pain. Night pain, awakening a child from sleep, is a particularly foreboding sign. There may be swelling, warmth, and redness caused by the vascularity of the tumor. Symptoms also may include cough, dyspnea, and chest pain if lung metastasis is present. With osteosarcoma, not chondrosarcoma, the most common presenting complaint is pain. Night pain, awakening a child from sleep, is a particularly foreboding sign. There may be swelling, warmth, and redness caused by the vascularity of the tumor. Symptoms also may include cough, dyspnea, and chest pain if lung metastasis is present. With osteosarcoma, not Ewing sarcoma, the most common presenting complaint is pain. Night pain, awakening a child from sleep, is a particularly foreboding sign. There may be swelling, warmth, and redness caused by the vascularity of the tumor. Symptoms also may include cough, dyspnea, and chest pain if lung metastasis is present. Cognitive Level: Comprehension 1033 16. In reviewing the history of the patient with osteosarcoma, the nurse might also expect the patient to have: a. Rhabdomyosarcoma b. Ewing sarcoma c. Fibroma d. Retinoblastoma ANS: D In children with osteosarcoma, there has been a link to individuals with retinoblastoma (a hereditary eye tumor). In children with osteosarcoma, there has been a link to individuals with retinoblastoma (a hereditary eye tumor), not rhabdomyosarcoma. In children with osteosarcoma, there has been a link to individuals with retinoblastoma (a hereditary eye tumor), not Ewing sarcoma. In children with osteosarcoma, there has been a link to individuals with retinoblastoma (a hereditary eye tumor), not fibromas. Cognitive Level: Comprehension 1033 17. A 16-year-old male was recently diagnosed with osteosarcoma. The tumor is most likely present in the of long bones. a. Epiphyses b. Metaphyses c. Marrow d. Osteocytes ANS: B Osteosarcoma is most likely present in the metaphyses of long bones. Osteosarcoma occurs mainly in the metaphyses of long bones near sites of active physical growth, not in the epiphyses. Osteosarcoma occurs mainly in the metaphyses of long bones near sites of active physical growth, not in the marrow. Osteosarcoma occurs mainly in the metaphyses of long bones near sites of active physical growth, not in osteocytes. Cognitive Level: Comprehension 1033 18. Ewing sarcoma originates from: a. Osteoblasts b. Epithelial cells c. The spleen d. The bone marrow ANS: D Ewing sarcoma originates from the bone marrow. Ewing sarcoma originates from the bone marrow, not osteoblasts. Ewing sarcoma originates from the bone marrow, not epithelial cells. Ewing sarcoma originates from the bone marrow, not the spleen. Cognitive Level: Comprehension 1034 19. A major predictor of poor prognosis for Ewing sarcoma is: a. Age of onset b. Size of tumor c. Presence of metastasis d. Gender of child ANS: C Metastasis at diagnosis is another poor prognostic indicator, with 5-year survival rate dropping to under 40%. Metastasis is the major indicator of poor prognosis, not age of onset. Metastasis is the major indicator of poor prognosis, not size of tumor. Metastasis is the major indicator of poor prognosis, not gender. Cognitive Level: Comprehension 1034 MULTIPLE RESPONSE 1. A 6-year-old male presents with fever, pain, swelling, and warmth. Tests reveal osteomyelitis In addition to the clinical symptoms, the nurse would expect elevations in which lab tests? (Select all that apply.) a. C-reactive protein b. White blood cell count c. Red cell count d. Erythrocyte sedimentation rate (ESR) e. Liver enzymes ANS: A, B, D Children often will present with fever, elevated white blood cell count (50% to 70%), elevated C-reactive protein (98%), and elevated ESR (90%). Cognitive Level: Comprehension 1026 COMPLETION 1. Polyarthritis is a type of juvenile arthritis in which more than joints are affected ANS: three 3 Cognitive Level: Comprehension 1027 2. Incidence of Legg-Calv-Perthes (LCP) disease peaks at age . ANS: 6 six LCP disease is a common osteochondrosis usually occurring in children between the ages of 3 and 10 years, with a peak incidence at 6 years. Chapter 43. Structure, Function, and Disorders of the Integument MULTIPLE CHOICE 1. A 12-year-old female notices her hair and skin feel more oily than normal. Her primary care provider explains that during puberty her sebaceous glands enlarge and are stimulated by: a. Androgens b. Estrogen c. Vitamin D d. Progesterone ANS: A Sebaceous glands secrete sebum, composed primarily of lipids, which oils the skin and hair and prevents drying. Androgens stimulate the growth of sebaceous glands, and their enlargement is an early sign of puberty. Androgens, not estrogen, are responsible for enlargement of the sebaceous glands. Androgens, not vitamin D, are responsible for enlargement of the sebaceous glands. Androgens, not progesterone, are responsible for enlargement of the sebaceous glands. Cognitive Level: Comprehension 1040 2. Of the sweat glands, the glands are most abundant in the axillae and genital areas. a. Eccrine b. Apocrine c. Sebaceous d. Subcutaneous ANS: B The apocrine sweat glands are located in the axillae, scalp, face, abdomen, and genital areas. The eccrine sweat glands are distributed over the body, with the greatest numbers in the palms of the hands, soles of the feet, and forehead. Apocrine sweat glands, not the sebaceous glands, are located in the axillae and genital areas. Apocrine sweat glands, not the subcutaneous glands, are located in the axillae and genital areas. Cognitive Level: Comprehension 1040 3. If a patient has carbuncles, the infection will be located in the: a. Hair follicles b. Papillary layer of the dermis c. Reticular layer of the dermis d. Subcutaneous tissue ANS: A Carbuncles are a collection of infected hair follicles and usually occur on the back of the neck, the upper back, and the lateral thighs. Carbuncles are a collection of infected hair follicles, not the papillary layer of the dermis. Carbuncles are a collection of infected hair follicles, not the reticular layer of the dermis. Carbuncles are a collection of infected hair follicles, not the subcutaneous tissue. Cognitive Level: Comprehension 1053 4. Which cells are involved in initiating immune responses in the skin? a. Langerhans cells b. Merkel cells c. Keratinocytes d. Melanocytes ANS: A The Langerhans cells process the antigen and carry it to T cells. T cells then become sensitized to the antigen, inducing the release of inflammatory cytokines and the symptoms of dermatitis. Langerhans cells initiate the immune response. Merkel cells are associated with nerve cells. Keratinocytes are part of the epidermal layer of the skin and are not involved in immune responses. Melanocytes synthesize the skins pigment. Cognitive Level: Comprehension 1048 5. Fat cells are located in the: a. Epidermis b. Dermis c. Hypodermis d. Fascia beneath the skin ANS: C The hypodermis is an underlying layer of connective tissue that contains macrophages, fibroblasts, and fat cells. Fat cells are not found in the epidermis but in the hypodermis. Fat cells are not found in the dermis but in the hypodermis. Fat cells are not found in the fascia but in the hypodermis. Cognitive Level: Comprehension 1038 6. A 25-year-old paralyzed male develops a dermal pressure ulcer. When assessing the patients skin, which finding is the first indication of this ulcer? a. Redness b. Whiteness c. Indurations d. Ulceration ANS: A The initial sign of a pressure ulcer is redness. The initial sign of a pressure ulcer is redness, not whiteness. The initial sign of a pressure ulcer is redness, not an area of induration. The initial sign of a pressure ulcer is redness, not ulceration. Cognitive Level: Comprehension 1049 7. To promote efficient wound healing, which dressing should be applied to a superficial ulcer? a. Thick and dry b. Flat and moist c. Bulky and dry d. None ANS: B Superficial ulcers should be covered with flat, moisture-retaining dressings. Superficial ulcers should be covered with flat and moist dressings, not dry and thick. Superficial ulcers should be covered with flat, not bulky, dressings. Superficial ulcers should be covered with flat, moisture-retaining dressings. Dressings should not be avoided. Cognitive Level: Comprehension 1047 8. Individuals of descent are more prone to developing keloids? a. African-American b. Northern European c. Asian d. Native American ANS: A African Americans are at greater risk for the development of keloids. African Americans, not Northern Europeans, are at greater risk for the development of keloids. African Americans, not Asians, are at greater risk for the development of keloids. African Americans, not Native Americans, are at greater risk for the development of keloids. Cognitive Level: Comprehension 1047 9. A 23-year-old male received a knife wound in a fight. His scar was sharply elevated, irregularly shaped, and progressively enlarging. This condition is caused by excessive amounts of in the corneum during connective tissue repair. a. Elastin b. Collagen c. Keratin d. Calcification ANS: B Irregular scar formation is due to excessive fibroblast activity and collagen formation. Irregular scar formation is due to excessive fibroblast activity and collagen, not elastin, formation. Irregular scar formation is due to excessive fibroblast activity and collagen, not keratin, formation. Irregular scar formation is due to excessive fibroblast activity and collagen, not calcification, formation. Cognitive Level: Comprehension 1047 10. A 23-year-old male reports a rash and pruritus. An increase in is associated with pruritus? a. Substance P b. Norepinephrine c. Dopamine d. Acetylcholine ANS: D Acetylcholine is one of the itch mediators. Acetylcholine, not substance P, is one of the itch mediators. Acetylcholine, not norepinephrine, is one of the itch mediators. Acetylcholine, not dopamine, is one of the itch mediators. Cognitive Level: Comprehension 1047 11. A 19-year-old female developed a circular, demarcated, and salmon-pink lesion. Two weeks later she developed more lesions over the trunk and upper part of the extremities. The diagnosis is pityriasis rosea, and the nurse knows the disorder is caused by a: a. Parasite b. Virus c. Bacteria d. Fungus ANS: B Pityriasis rosea is caused by a virus. Pityriasis rosea is caused by a virus, not a parasite. Pityriasis rosea is caused by a virus, not bacteria. Pityriasis rosea is caused by a virus, not a fungus. Cognitive Level: Comprehension 1050 12. A 12-year-old female visits her primary care provider to obtain acne medication for recurrent acne vulgaris. This condition is an inflammatory disorder of the: a. Apocrine glands b. Pilosebaceous follicle c. Dermal layer d. Eccrine gland ANS: B Acne vulgaris is an inflammatory disorder of the pilosebaceous follicle. Acne vulgaris is an inflammatory disorder of the pilosebaceous follicle, not the apocrine glands. Acne vulgaris is an inflammatory disorder of the pilosebaceous follicle, not the dermal layer. Acne vulgaris is an inflammatory disorder of the pilosebaceous follicle, not the eccrine gland. Cognitive Level: Comprehension 1051 13. A 42-year-old female presents with raised red lesions with a brownish scale. She was diagnosed with discoid lupus erythematosus. A clinician recalls this disorder is related to: a. Infection b. Trauma c. Autoimmunity d. Cancer ANS: C Discoid lupus is related to autoimmunity. Discoid lupus is related to autoimmunity, not infection. Discoid lupus is related to autoimmunity, not trauma. Discoid lupus is related to autoimmunity, not cancer. Cognitive Level: Comprehension 1051 14. In discoid lupus erythematosus, skin lesions may be accompanied by Raynaud phenomenon, which is manifested by: a. Bone deformities b. Vasospasm in the extremities c. Arterial aneurysms d. Venous thrombus ANS: B Raynaud phenomenon is manifested by vasospasm in the extremities. Raynaud phenomenon is manifested by vasospasm, not bone deformities, in the extremities. Raynaud phenomenon is manifested by vasospasm, not arterial aneurysms, in the extremities. Raynaud phenomenon is manifested by vasospasm, not venous thrombus, in the extremities. Cognitive Level: Comprehension 1056 15. A 45-year-old male presents with a chronic blister-forming disease of the skin and oral mucous membranes. The nurse would recognize this condition as: a. Lupus erythematosus b. Pemphigus c. Psoriasis d. Eczema ANS: B Pemphigus is manifested by chronic blister formation. Lupus erythematosus is manifested by rash and arthritis, not blisters. Psoriasis is manifested by gray-white skin plaques, not blisters. Eczema is not manifested by blisters. REF: pp. 1051-1052 16. A 9-year-old male presents with severe erythematous bullous lesions that are believed to be an adverse response to a medication. Which of the following is the most likely diagnosis? a. Pemphigus b. Acne vulgaris c. Lupus erythematosus d. Stevens-Johnson syndrome ANS: D The most common form of erythema multiforme in children and young adults is Stevens- Johnson syndrome. Pemphigus is not manifested by erythema. Acne is not manifested by erythema. Lupus erythematosus is not manifested by bullae. Cognitive Level: Comprehension 1052 17. A 50-year-old male recently underwent a liver transplant and is taking immunosuppressive drugs. He now has painful vesicular eruptions on the face and trunk. He reports that he had chickenpox as a child. Which of the following is the most likely diagnosis based on his chicken pox history? a. Erysipelas b. Poliomyelitis c. Warts d. Herpes zoster ANS: D Herpes zoster causes shingles, a disorder similar to chicken pox. Erysipelas is caused by strep. Poliomyelitis is not manifested by painful vesicles. Warts are not painful. Cognitive Level: Comprehension 1054 18. Tinea corporis (ringworm) is a infection of the skin. a. Nematode b. Fungal c. Viral d. Bacterial ANS: B Tinea corporis is caused by a fungus. Tinea corporis is caused by a fungus, not a nematode. Tinea corporis is caused by a fungus, not a virus. Tinea corporis is caused by a fungus, not bacteria. Cognitive Level: Comprehension 1055 19. A 20-year-old female presents with vaginal itch and thin-walled pustular lesions. She is diagnosed with candidiasis. This condition is caused by a: a. Yeast b. Virus c. Bacterium d. Fungus ANS: A Candidiasis is a yeast. Candidiasis is a yeast, not a virus. Candidiasis is a yeast, not a bacterium. Candidiasis is a yeast, not a fungus. Cognitive Level: Comprehension 1055 20. For a patient with candidiasis, which factor will exacerbate the condition? a. Poor hygiene b. Older age c. Systemic antibiotics d. Anemia ANS: C Candidiasis is exacerbated by the use of systemic antibiotics because the antibiotics eliminate normal flora. Candidiasis is exacerbated by the use of systemic antibiotics because the antibiotics eliminate normal flora. It is not due to poor hygiene. Candidiasis is exacerbated by the use of systemic antibiotics because the antibiotics eliminate normal flora. Older age is not a factor. Candidiasis is exacerbated by the use of systemic antibiotics because the antibiotics eliminate normal flora. Anemia is not a factor. Cognitive Level: Comprehension 1055 21. A 10-year-old male is given penicillin for an infection. He has an allergic reaction, during which he develops urticarial lesions. These lesions are mediated by the release of: a. Beta-adrenergic agonists b. Histamine c. Calcium d. Cortisol ANS: B Urticarial lesions are mediated by the histamine response. Urticarial lesions are mediated by the histamine response, not beta responses. Urticarial lesions are mediated by the histamine response, not calcium. Urticarial lesions are mediated by the histamine response, not cortisol. Cognitive Level: Comprehension 1056 22. When assessing a patient with scleroderma, which changes in the skin will be observed? a. Thinning b. Hyperpigmented c. Necrosis d. Hardening ANS: D Scleroderma is manifested by hardening of the skin. Scleroderma is manifested by hardening, not thinning, of the skin. Scleroderma is manifested by hardening, and the skin becomes hypopigmented. Scleroderma is manifested by hardening, not necrosis, of the skin. Cognitive Level: Comprehension 1056 23. A 52-year-old female is diagnosed with scleroderma. Which complication leads to ulcer formation? a. Cutaneous vasculitis b. Raynaud phenomenon c. Cellulitis d. Infection ANS: B Ulcer formation is due to Raynaud phenomenon. Ulcer formation is due to Raynaud phenomenon, not vasculitis. Ulcer formation is due to Raynaud phenomenon, not cellulitis. Ulcer formation is due to Raynaud phenomenon, not infection. Cognitive Level: Comprehension 1056 24. What of the following behavior in the patient with scleroderma would cause the nurse concern? a. Wears mittens on cold days b. Smokes a few cigarettes a day c. Applies lotion daily d. Seeks warmer environments ANS: B Smoking should be avoided as it promotes vasoconstriction that may worsen Raynaud phenomenon. Mittens are appropriate. Lotion may not help, but could help skin remain supple. Warm environments are better than cold. Cognitive Level: Comprehension 1056 25. A 13-year-old female is concerned about several pigmented skin lesions on her body. Her primary care provider tells her that these lesions must be monitored because of their ability to transform into malignant melanoma. These lesions are referred to as: a. Macules b. Nevi c. Plaques d. Keloids ANS: B Nevi may undergo transition to malignant melanoma. Nevi, not macules, may undergo transition to malignant melanoma. Nevi, not plaques, may undergo transition to malignant melanoma. Nevi, not keloids, may undergo transition to malignant melanoma. Cognitive Level: Comprehension 1057 26. A patient wants to know which malignant skin lesion is the most serious. The correct response is: a. Basal cell carcinoma b. Squamous cell carcinoma c. Kaposi sarcoma (KS) d. Malignant melanoma ANS: D Malignant melanoma is the most serious skin cancer. Malignant melanoma, not basal cell carcinoma, is the most serious skin cancer. Malignant melanoma, not squamous cell carcinoma, is the most serious skin cancer. Malignant melanoma, not KS, is the most serious skin cancer. Cognitive Level: Comprehension 1058 27. A 40-year-old female is diagnosed with skin cancer. Her primary care provider explains that the most important risk factor for skin cancer is: a. Amount of direct sun exposure at a young age b. Amount of sun exposure over age 50 c. Lifetime amount of sun exposure d. Living in equatorial regions where the sun is most intense ANS: A Protection from the sun, particularly during the childhood years of life, significantly reduces the risk of skin cancer in later years. Protection from the sun at a young age, not after 50, is the most important way to decrease cancer risk. Protection from the sun, particularly during the childhood years of life, significantly reduces the risk of skin cancer in later years. Protection from the sun, particularly during the childhood years of life, not avoiding equatorial regions, significantly reduces the risk of skin cancer in later years. Cognitive Level: Comprehension 1058 28. A 27-year-old male lung transplant patient developed KS. He tells the nurse he thought only people with AIDS developed this type of cancer. The nurse knows that the cause of this patients KS is most likely related to the fact that the patient: a. Is malnourished b. Was exposed to hepatitis B c. Is immunosuppressed d. Is diabetic ANS: C KS is a vascular malignancy associated with immunodeficiency states and occurs among transplant recipients taking immunosuppressive drugs. KS is not related to malnourishment. KS is not related to exposure to hepatitis B. KS is not related to the presence of diabetes. Chapter 44. Alterations of the Integument in Children MULTIPLE CHOICE 1. A 4-month-old male is brought to his primary care provider for severe itching and skin lesions. He is diagnosed with atopic dermatitis. Which of the following would be elevated in this patient? a. Immunoglobulin D (IgD) b. Immunoglobulin M (IgM) c. Immunoglobulin E (IgE) d. Immunoglobulin G (IgG) ANS: C Most individuals affected with atopic dermatitis show an increased serum IgE level. Most individuals affected with atopic dermatitis show an increased serum IgE level, not IgD. Most individuals affected with atopic dermatitis show an increased serum IgE level, not IgM. Most individuals affected with atopic dermatitis show an increased serum IgE level, not IgG. Cognitive Level: Comprehension 1071 2. A 4-month-old female is diagnosed with atopic dermatitis (AD). Which of the following assessment findings by the nurse will most likely support this diagnosis? a. Blistering b. Moist reddened skin c. Dry, itchy skin d. White patches ANS: C AD has a constellation of clinical features that include dry, sensitive, itchy, and easily irritated skin because the barrier function of the skin is impaired. Dry skin, not blistering, occurs in AD. Dry skin, not moist skin, occurs in AD. White patches are characteristic of other disorders, such as measles. Cognitive Level: Comprehension 1071 3. A 2-month-old female develops diaper dermatitis. A nurse will monitor this patient for which secondary infection that frequently accompanies diaper dermatitis? a. Streptococcus b. Proteus c. Candida albicans d. Staphylococcus aureus ANS: C Diaper dermatitis is secondarily infected with Candida albicans. Diaper dermatitis is secondarily infected with Candida albicans, not Streptococcus. Diaper dermatitis is secondarily infected with Candida albicans, not Proteus. Diaper dermatitis is secondarily infected with Candida albicans, not Staphylococcus aureus. Cognitive Level: Comprehension 1072 4. Acne vulgaris involves inflammation of the: a. Hair follicles b. Sebaceous follicles c. Eccrine glands d. Apocrine glands ANS: B Acne is a disorder of the pilosebaceous units, known as sebaceous follicles. Acne is a disorder of the pilosebaceous units, known as sebaceous follicles, not hair follicles. Acne is a disorder of the pilosebaceous units, known as sebaceous follicles, not eccrine glands. Acne is a disorder of the pilosebaceous units, known as sebaceous follicles, not apocrine glands. Cognitive Level: Comprehension 1070 5. A 14-year-old female presents with severe acne. Which of the following promotes acne development? a. Androgens b. Estrogens c. Gonadotropins d. Glucocorticoids ANS: A Androgens increase the size and productivity of the sebaceous glands and promote P. acnes. Androgens, not estrogens, increase the size and productivity of the sebaceous glands and promote P. acnes. Androgens, not gonadotropins, increase the size and productivity of the sebaceous glands and promote P. acnes. Androgens, not glucocorticoids, increase the size and productivity of the sebaceous glands and promote P. acnes. Cognitive Level: Comprehension 1071 6. Bullous impetigo is caused by a strain of: a. Staphylococcus aureus b. Molluscum contagiosum c. Escherichia coli d. Candida albicans ANS: A S. aureus is currently the most common overall cause of impetigo. S. aureus, not molluscum contagiosum, is currently the most common overall cause of impetigo. S. aureus, not E. coli, is currently the most common overall cause of impetigo. S. aureus, not Candida albicans, is currently the most common overall cause of impetigo. Cognitive Level: Comprehension 1072 7. A 10-year-old female from east Africa presents with vesicles consistent with vesicular impetigo. Which of the following is the most likely cause of her condition? a. Herpes virus b. Candida albicans c. Streptococcus pyogenes d. Human papillomavirus (HPV) ANS: C Vesicular impetigo is caused by Streptococcus pyogenes. Vesicular impetigo is caused by Streptococcus pyogenes, not herpes. Vesicular impetigo is caused by Streptococcus pyogenes, not Candida albicans. Vesicular impetigo is caused by Streptococcus pyogenes, not HPV. Cognitive Level: Comprehension 1073 8. A 3-year-old male develops tinea capitis after playing with the family dog. This infection is caused by a: a. Fungus b. Bacterium c. Virus d. Parasite ANS: A Tinea capitis is caused by a fungus. Tinea capitis is caused by a fungus, not bacteria. Tinea capitis is caused by a fungus, not a virus. Tinea capitis is caused by a fungus, not a parasite. Cognitive Level: Comprehension 1074 9. A 5-year-old male is diagnosed with tinea corporis following development of lesions on the non-hairy parts of his face, trunk, and limbs. A common source of this condition is a: a. Kitten b. Pet bird c. Hamster d. Horse ANS: A Tinea corporis is usually attributed to contact with young dogs and cats. Tinea corporis is usually attributed to contact with young dogs and cats, not birds. Tinea corporis is usually attributed to contact with young dogs and cats, not hamsters. Tinea corporis is usually attributed to contact with young dogs and cats, not horses. Cognitive Level: Comprehension 1074 10. The nurse would correctly identify the medical term for ringworm as: a. Impetigo b. Tinea corporis c. Thrush d. Psoriasis ANS: B Ringworm is also known as tinea corporis. Ringworm is not impetigo. Ringworm is not thrush. Ringworm is not psoriasis. Cognitive Level: Comprehension 1074 11. A 4-month-old female develops white spots and shallow ulcers in her mouth. Her pediatrician diagnoses her with thrush. This condition is caused by: a. Escherichia coli b. Streptococcal bacteria c. Candida albicans d. Staphylococcal bacteria ANS: C Thrush is caused by Candida albicans. Thrush is caused by Candida albicans, not E coli. Thrush is caused by Candida albicans, not strep. Thrush is caused by Candida albicans, not staph. Cognitive Level: Comprehension 1074 12. A 6-year-old male presents with slightly umbilicated, dome-shaped lesions on the skin of the trunk, face, and extremities. He is diagnosed with molluscum contagiosum caused by a highly contagious: a. Bacterium b. Virus c. Fungus d. Parasite ANS: B Molluscum contagiosum is caused by a virus. Molluscum contagiosum is caused by a virus, not bacteria. Molluscum contagiosum is caused by a virus, not a fungus. Molluscum contagiosum is caused by a virus, not a parasite. Cognitive Level: Comprehension 1074 13. Molluscum contagiosum affects the skin and: a. Nails b. Tongue c. Conjunctiva d. Hair follicles ANS: C Molluscum contagiosum affects the skin and conjunctiva. Molluscum contagiosum affects the skin and conjunctiva, not the nails. Molluscum contagiosum affects the skin and conjunctiva, not the tongue. Molluscum contagiosum affects the skin and conjunctiva, not the hair. Cognitive Level: Comprehension 1074 14. The nurse would be correct in identifying the duration of rubella as: a. 12 hours b. 1 to 3 days c. 7 days d. 12 to 15 days ANS: B Rubella has a duration of 1 to 3 days. Rubella has a duration of 1 to 3 days, not 12 hours. Rubella has a duration of 1 to 3 days, not 7 days. Rubella has a duration of 1 to 3 days, not 12 to 15 days. Cognitive Level: Comprehension 1075 15. Rubella, rubeola, and roseola are common communicable diseases caused by infection. a. Viral b. Bacterial c. Yeast d. Fungal ANS: A Rubella, rubeola, and roseola are all caused by a virus. Rubella, rubeola, and roseola are all caused by a virus, not bacteria. Rubella, rubeola, and roseola are all caused by a virus, not yeast. Rubella, rubeola, and roseola are all caused by a virus, not a fungus. REF: pp. 1075-1076 16. A 5-year-old female develops chickenpox after exposure at her day care center. This disease is caused by: a. A pox virus b. A herpes virus c. An adenovirus d. HPV ANS: B Chickenpox is caused by a herpes virus. Chickenpox is caused by a herpes virus, not a pox virus. Chickenpox is caused by a herpes virus, not adenovirus. Chickenpox is caused by a herpes virus, not HPV. Cognitive Level: Comprehension 1076 17. The pathophysiology student would correctly identify the etiologic agent of smallpox as: a. A bacteria b. A virus c. Insects d. Mites ANS: B The etiologic agent of smallpox is the pox virus. The etiologic agent of smallpox is a virus, not bacteria. The etiologic agent of small pox is a virus, not insects. The etiologic agent of small pox is a virus, not mites. Cognitive Level: Comprehension 1077 18. The nurse would expect the occurrence of scabies to occur more commonly among children who: a. Attend day care b. Live in crowded, unsanitary conditions c. Reside in rural areas d. Play outside ANS: B Scabies is often epidemic in areas of overcrowded housing and poor sanitation. Scabies does occur in day care centers, but it occurs more commonly in unsanitary conditions. Scabies occurs more commonly in areas of poor sanitation, not in rural areas. Scabies can occur in children who play outside, but more commonly in areas of poor sanitation. [Show More]
Last updated: 1 year ago
Preview 1 out of pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 03, 2021
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
Sep 03, 2021
Downloads
0
Views
26

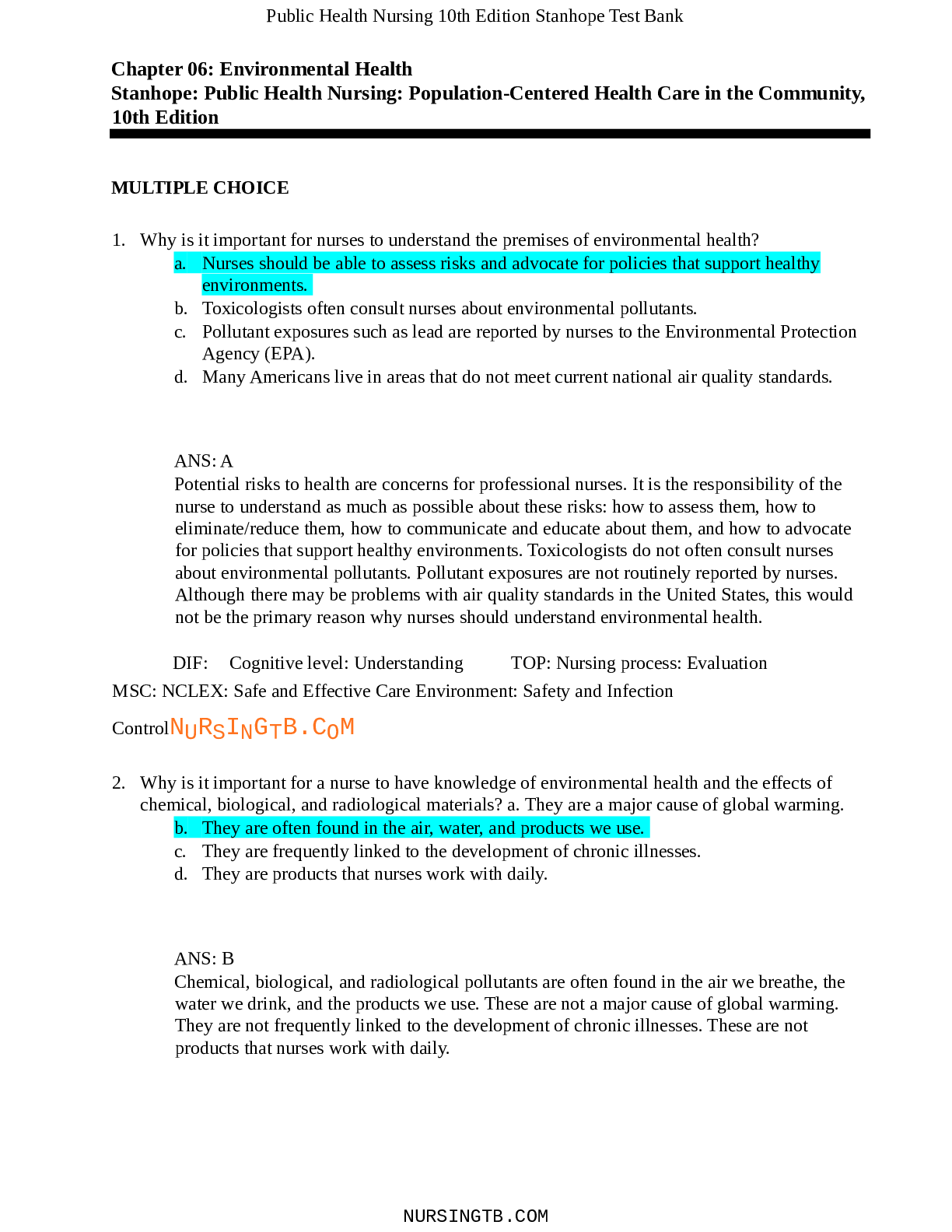
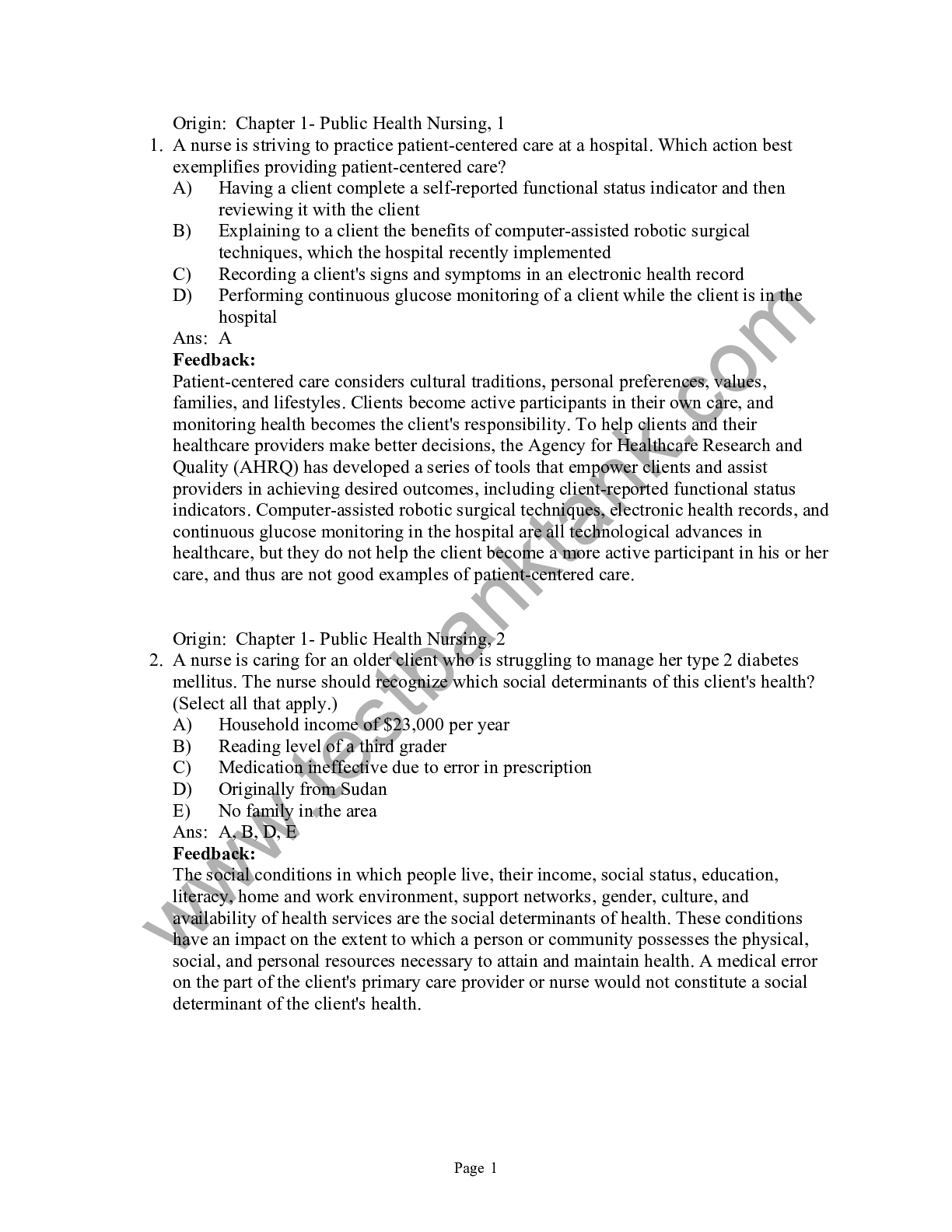
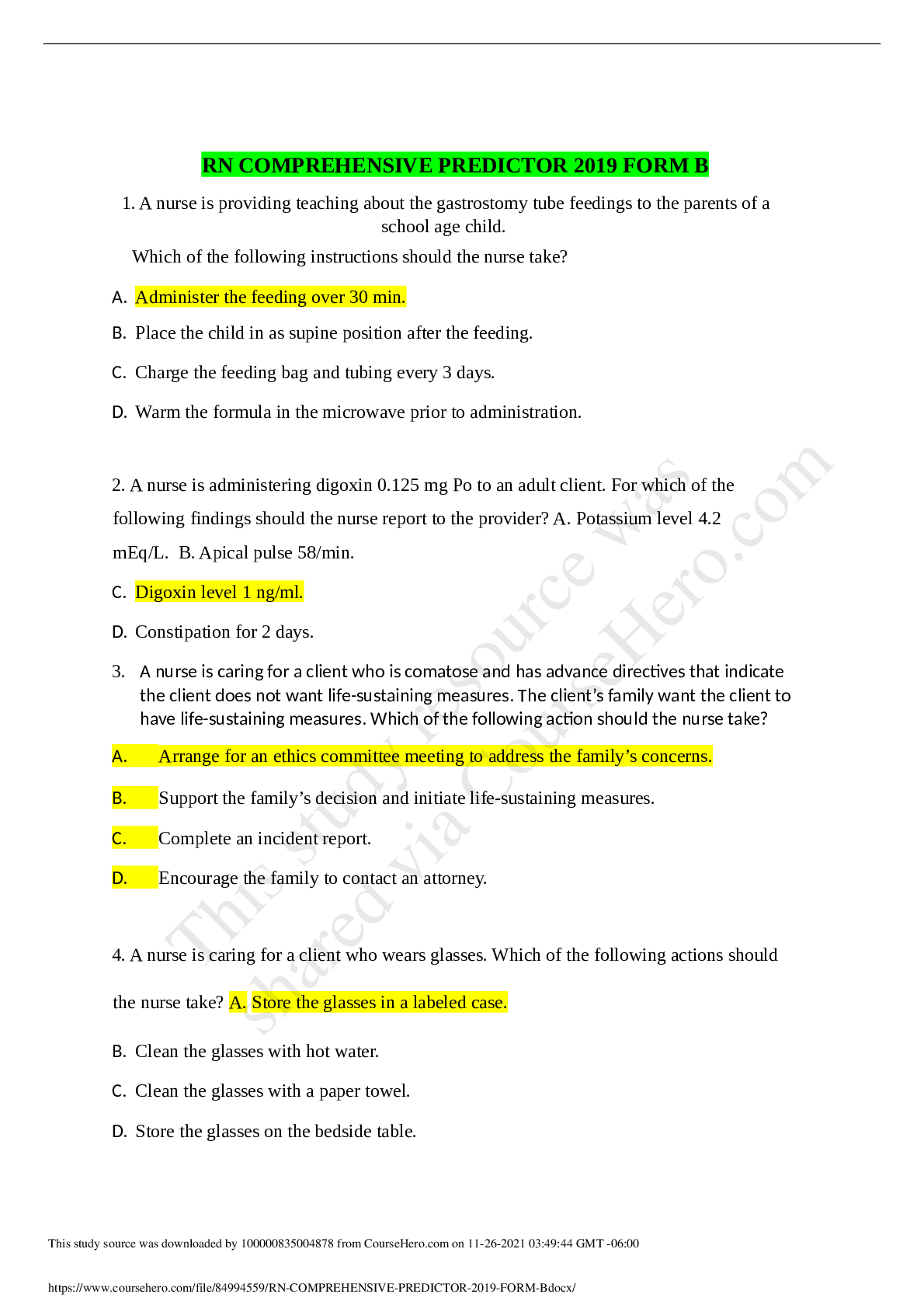
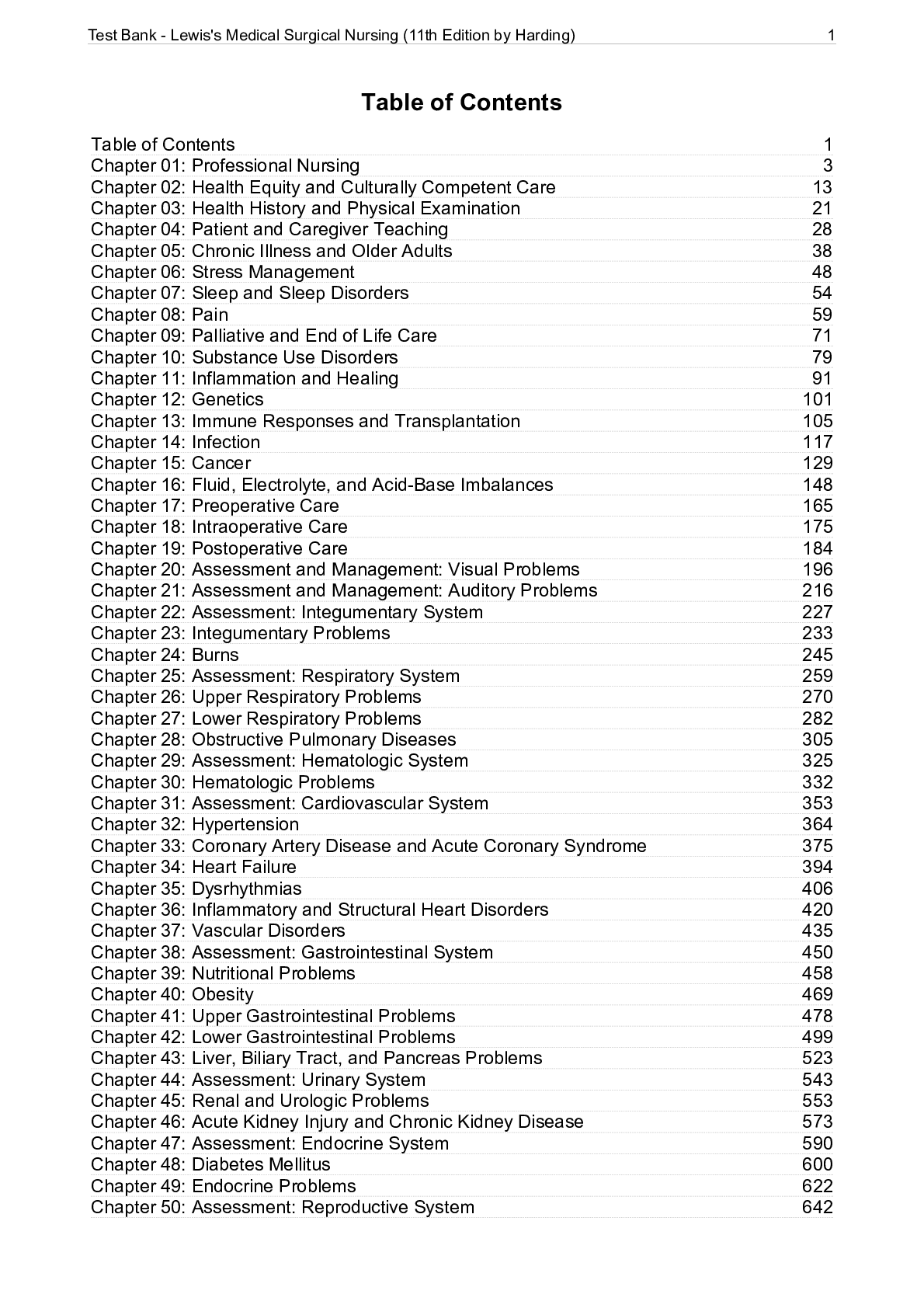




.png)
 (1).png)