*NURSING > STUDY GUIDE > NR 507 - Week 4 Midterm Study Guide, Possible Questions & Answers Graded A+ (All)
NR 507 - Week 4 Midterm Study Guide, Possible Questions & Answers Graded A+
Document Content and Description Below
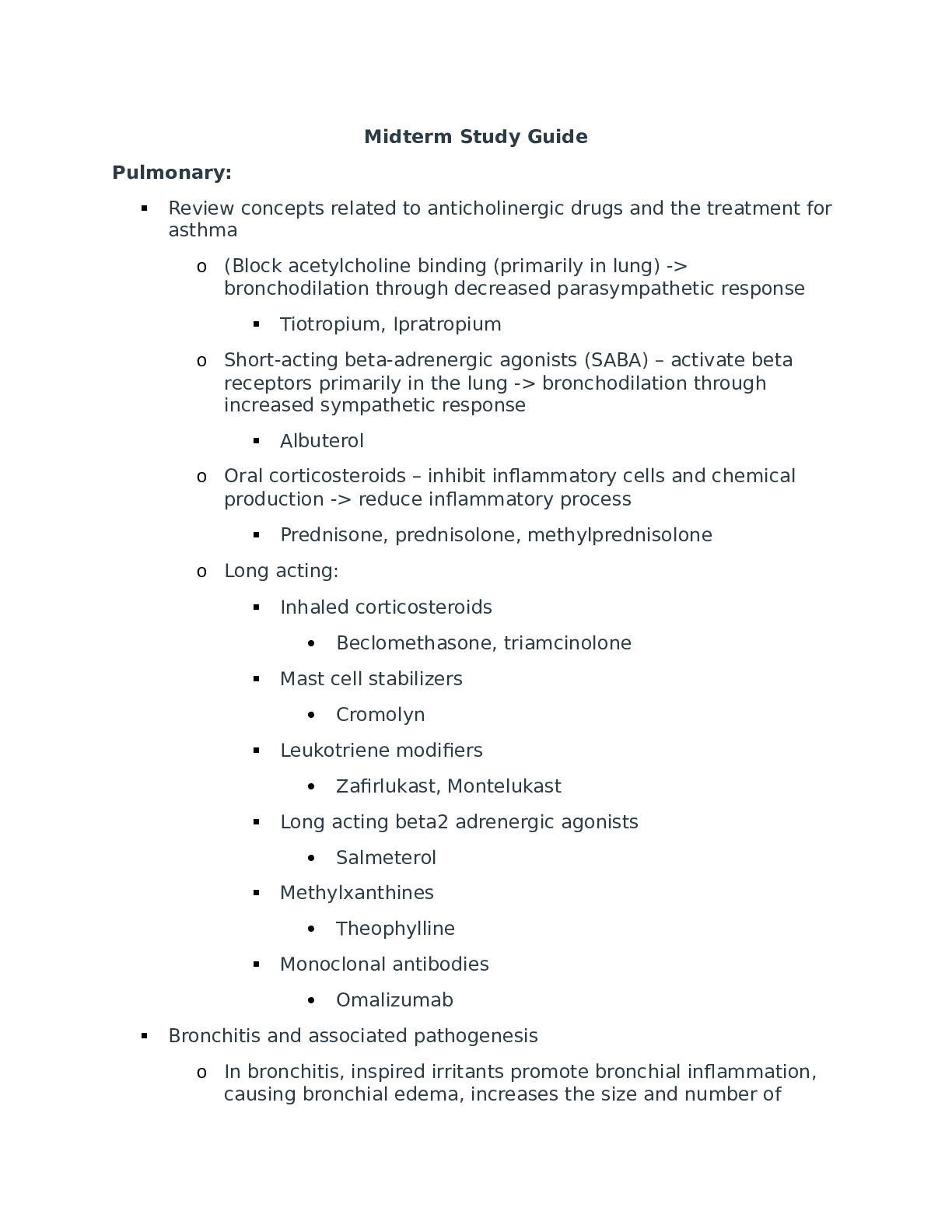
Epigenetics Defects in the encoding of histone-modifying proteins Housekeeping Genes are vital to the function and maintenance of all the body’s cells. What characteristic is … with these genes... ? They are transcriptionally active Mutations in the encoding of histone modifying proteins … shown to influence the development of what congenital condition? Heart Disease Epigenetics refers to chemical modification that are made to what? Histones and DNA Signals to change or modify epigenetic tags are … from where? Environmental factors. Hormones, Contact (all the above) What sort of molecule is responsible for transferring signals into cells to gen regulatory proteins? Kinases Epigenetics and its role on human development Research has provided support for the theory that epigenetic modification can result from deficient in utero nutrition causing? Obesity diabetes and CAD. During which stage of human development does the role of epigenetics have the greatest impact on the development of epigenetic abnormalities? In utero The difference between DNA sequence mutations and epigenetic modifications is? They are said to be pluripotent. Unlike DNA sequence mutations which cannot be altered, epigenetic modifications can be reversible. Embryonic stem cells are pluripotent, which originated as mass cells with blast cyst (not the placenta) Epigenetics is the study of heritable changes in gene expression or phenotype caused by mechanisms other than changes in DNA sequences. Epigenetic modifications can cause individuals with the same DNA sequences (such as identical twins) to have different disease profiles. There are three major types of epigenetic modifications (Figure 6-1): DNA methylation: Histone modification Micro-ribonucleic acids (miRNAs or miRs): Early in embryonic development, all cells of the embryo have the potential to become any type of cell in the fetus or adult. These embryonic stem cells are said to be pluripotent. A key event in early embryogenesis is the differential epigenetic modification (including extensive methylation) of specific DNA nucleotide sequences in these cells. This modification helps to determine the fate of each cell (i.e., the type of cell it becomes, such as a myocyte, neuron, or fibroblast) by helping to ensure that specific genes are expressed only in the cells and tissue types in which their gene products are needed (e.g., factor VIII expression primarily in hepatocytes, or dopamine receptor expression in neurons). Thus, even though nearly all cells have the same DNA sequence, the transcriptional activity of most genes varies substantially and depends on cell and tissue type. A small percentage of genes, termed housekeeping genes, are necessary for the function and maintenance of all cells. These genes escape the methylation process and remain transcriptionally active in all cells. Much remains to be learned about factors that cause epigenetic modifications. Findings so far indicate that specific environmental or nongenetic factors, such as diet and exposure to certain chemicals, can drive such modifications. For example, alcohol has been shown to affect methylation patterns in animal models,5 so the harmful effects of fetal alcohol exposure may be mediated through epigenetic mechanisms. Maternal dietary deficiency during pregnancy may cause epigenetic modifications of fetal genes, leading to an increased risk of obesity and diabetes in the offspring later in life.6 In some animal models, the insulin-like growth factor 2 gene (IGF2) is a target of these epigenetic modifications. Although the observed changes in methylation status of CpG sequences in these genes are typically small, it is possible that they affect phenotypic development. The hereditary transmission of epigenetic changes to successive generations has been termed epigenetic transgenerational inheritance. If demonstrated to occur in humans, transgenerational inheritance could have important implications for disease and disease prevention. The best evidence for epigenetic effects on disease risk comes from studies of human cancer Robust experimental observations are clarifying the roles of epigenetic states in determining cell fates and disease phenotypes. The well-documented involvement of epigenetic abnormalities in carcinogenesis and the mounting evidence for these epigenetic changes in other common diseases (discussed in other chapters) will likely elucidate possibilities for reversing the epigenetic abnormalities and preventing their establishment in utero. Totipotent cells and its ability to differentiate into any type of cell Which embryonic stem cell characteristic is referred to as a totipotent? Ability to differentiate into any type of somatic cell. Examples of two totipotent cells are? Spores and zygotes What is a Totipotent cell? One of the most important stem cell as they have the potential to develop in any cell found in the human body. Are all cells Totipotent cells? Only the morula cells are. Prader-Willi syndrome and Angelman syndrome? What characteristic of Prader-Willi syndrome is not a characteristic of Angelman syndrome? Mid-Mild-to-Moderate retardation Inherited from the father A child with Prader-Willi syndrome has been hospitalized. Which assessment findings does the nurse expect with this syndrome? Insatiable hunger – morbid obesity Prader-Willi syndrome will have short stature, hypotonia, small hands, small feet, obesity, hypogonadism, inverted V-shape upper lip The nurse is examining an 8-year-old boy with chromosomal abnormalities. Which sign, or symptom suggests the boy has Angelman syndrome? Observation shows jerky ataxic movements Angelman is SEVERE mental retardation, seizures, ataxic gait, and bouts of uncontrolled laughter Is inherited by the mother A well-known disease example of imprinting is associated with a deletion of about 4 million base pairs (Mb) of the long arm of chromosome 15. When this deletion is inherited from the father, the child manifests Prader-Willi syndrome, whose features include short stature, hypotonia, small hands and feet, obesity, mild to moderate mental retardation, and hypogonadism. The same 4-Mb deletion, when inherited from the mother, causes Angelman syndrome, which is characterized by severe mental retardation, seizures, and an ataxic gait These diseases are each seen in about 1 of every 15,000 live births, and chromosome deletions are responsible for about 70% of cases of both diseases. The deletions that cause Prader-Willi and Angelman syndromes are indistinguishable at the DNA sequence level and affect the same group of genes. For several decades, it was unclear how the same deletion could produce such disparate results in different persons. Further analysis showed that the 4-Mb deletion (the critical region) contains several genes that are normally transcribed only on the copy of chromosome 15 that is inherited from the father.17 These genes are transcriptionally inactive (imprinted) on the copy of chromosome 15 inherited from the mother. Similarly, other genes in the critical region are transcriptionally active only on the chromosome copy inherited from the mother and are inactive on the chromosome inherited from the father. Thus, several genes in this region are normally active on only one chromosome copy (Figure 6-5). If the single active copy of one of these genes is lost because of a chromosome deletion, then no gene product is produced at all, resulting in disease. Molecular analysis has revealed much about genes in this critical region of chromosome 15.17,18 The gene responsible for Angelman syndrome encodes a ligase involved in protein degradation during brain development (consistent with the mental retardation and ataxia observed in this disorder). In brain tissue, this gene is active only on the chromosome copy inherited from the mother. Consequently, a maternally transmitted deletion removes the single active copy of this gene. Several genes in the critical region are associated with Prader-Willi syndrome, and they are transcribed only on the chromosome transmitted by the father. A paternally transmitted deletion removes the only active copies of these genes, producing the features of Prader-Willi syndrome. The inheritance patterns of Prader-Willi syndrome, which can be caused by a 4-Mb deletion of chromosome 15q when inherited from the father. In contrast, Angelman syndrome can be caused by the same deletion but only when it is inherited from the mother. The reason for this difference is that different genes in this region are normally imprinted (inactivated) in the copies of 15q transmitted by the mother and the father. Cellular Proliferation 5-Azacytidine and the treatment of cancer What is 5-azacytidine? Nucleoside analog able to … incorporated into RNA & DNA Cytoxic effects 5- Azactytide has demonstrated promise in the treatment of which form of cancer? Pancreatic Cancer the role of inactive MLH1 in the development of some forms of inherited colon cancer What is the role of inactive MLH1 in the development of some forms of inherited colon cancer? DNA damage is left unrepaired A major cause of one form of inherited colon cancer (hereditary nonpolyposis colorectal cancer [HNPCC]) is the methylation of the promoter region of a gene, MLH1, whose protein product repairs damaged DNA. When MLH1 becomes inactive, damaged DNA accumulates, eventually resulting in colon tumors Effects of ethanol on neural stem cells ability to differentiate into functional neurons- Research has demonstrated that neural stem cells have an impaired ability to differentiate into functional neurons when subjected to? Ethanol Inflammation as an etiology for cancer-note conditions in which this may occur What chronic inflammatory conditions can increase risk for cancer? Ulcerative colitis and Crohn Disease chronic inflammation also can precede and presumably initiate malignant change, as for example in inflammation-induced colon cancer. It is well documented that chronic inflammation induced by bacteria, viruses, autoimmune processes, and toxins promotes common types of cancer, including colon, liver, and lung cancer. Inflammation can be caused by numerous environmental factors, for example, inhaling tobacco smoke, asbestos fibers, or fine particles in the air from diesel engine exhaust and industrial sources. These sources are major factors in lung and other respiratory tract cancers. Cancer development in the presence of chronic inflammation involves the continuous presence of cytokines, chemokines, reactive oxygen species (ROS), oncogenes, cyclooxgenase-2 (COX-2), 5-lipoxygenase (5-LOX), and matrix metalloproteinases (MMPs) as well as the activation of essential transcription factors, such as nuclear factor κB (NF-κB). Cancer In terms of epigenetic modifications, the role of environmental stressors associated with development of cancer When considering abnormal epigenetics modifications, what factor is currently being viewed as strongly associated with the development of some cancers? Environmental stressors Cancers are caused by environmental-lifestyle behaviors and by exposures and genetic factors. Cancer is driven by genetic alterations and epigenetic abnormalities Environmental conditions, including exposure to sunlight, natural and medical radiation, workplace exposures, and involuntary or unknown exposures Cancer, initially recognized as a genetic disease, is now known to involve epigenetic abnormalities along with genetic alterations. It is becoming clear that microenvironment-mediated epigenetic perturbations play an important role in the development of neoplasia. Epigenetics refers to the study of heritable changes in gene expression that occur without a change in DNA sequence which are sufficiently powerful to regulate the dynamics of gene expression. The key processes responsible for epigenetic regulation are DNA methylation, histone modifications and post transcriptional gene regulation by noncoding RNA commonly referred as microRNAs. These mechanisms are critical components in the normal development and growth of cells and their modifications contribute to neoplastic phenotypes Defects in Mechanism of Defense Hemolytic defects in the newborn To explain hemolytic disorders in the new born to new parents, the nurse who cares for the new born population must … aware of the physiologic characteristics related to these conditions. What is the most common cause of pathologic hyperbilirubinemia? hemolytic disorders Which infant is most likely to express Rh incompatibility? Infant of an Rh-negative mother and a father who is Rh positive and homozygous for the Rh factor Rh hemolytic disease is suspected in a mother’s second baby, a son. Which factor is important in understanding how this could develop? The first child was RH + The nurse is caring for an infant with hemolytic disease. Which medication should the nurse anticipate to … prescribed to decrease the bilirubin level? Phenobarbital A newborn is found to have hemolytic disease. Which combination would … found related to the blood types of this newborn and the parents of the newborn? newborn who is type A, mother who is type O The nurse is caring for a newborn with hemolytic disease of the newborn who is receiving phototherapy. Which nursing intervention would … the most appropriate for the nurse to do? The nurse turns the newborn every 3 to 4 hours Hemolytic defects in the newborn Approximately 85% of the human population carries Rh antigen, which is also found in rhesus monkeys. If an Rhnegative pregnant woman is carrying an Rh-positive fetus, the fetus may be at risk of hemolytic disease of the newborn, in which antibodies made by the mother against the Rh antigen may cross the placenta and destroy the fetus's red blood cells. RhoGAM administered to pregnant Rh- women may prevent this disease. Hemolytic Disease of The Newborn a.k.a. HDN = HDNB = "Erythroblastosis Fetalis" The most dramatic form of acquired congenital hemolytic anemia is hemolytic disease of the newborn (HDN), also termed erythroblastosis fetalis. HDN is an alloimmune disorder in which maternal blood and fetal blood are antigenically incompatible, causing the mother’s immune system to produce antibodies against fetal erythrocytes. Fetal erythrocytes that have been bound to maternal antibodies are recognized as foreign or defective by the fetal mononuclear phagocyte system and are removed from the circulation by phagocytosis, usually in the fetal spleen. (For a complete discussion of HDN, see p. 1059.) Other acquired hemolytic anemias— some of which begin in utero—include those caused by infections or the presence of toxins. The inherited forms of hemolytic anemia result from intrinsic defects of the child’s erythrocytes, any of which can lead to erythrocyte destruction by the mononuclear phagocyte system. Structural defects include abnormal red blood cell size and abnormalities of plasma membrane structure (spherocytosis). Intracellular defects include enzyme deficiencies, the most common of which is G6PD deficiency, and defects of hemoglobin synthesis, which manifest as sickle cell disease or thalassemia, depending on which component of hemoglobin is defective. These and other causes of childhood anemia, some more common than others Understand the meaning of infectivity No questions The ability of the pathogen to invade and multiply in the host. Colonization, Invasion, multiplication, spread Infectivity Def: The proportion of persons exposed to an infectious agent who become infected by it. Most effective treatment for HIV A patient … with acute primary HIV infection is in the clinic. What treatment should … initiated for this patient? Combination antiretroviral therapy. Defected cells of HIV A patient has human immunodeficiency virus (HIV). A nurse realizes the HIV will attack: Helper T cells The nursing instructor is discussing the development of human immunodeficiency disease (HIV) with the students. What should the instructor inform the class about helper T cells? They fight infection It infects and destroys the T-helper cell, which is necessary to provide help for the maturation of both plasma cells and T-cytotoxic cells.41 Therefore, HIV suppresses the immune response against itself and secondarily creates a generalized immune deficiency by suppressing the development of immune responses against other pathogens and opportunistic microorganisms. Signs of T-Lymphocyte deficiencyT-cell defects It infects and destroys the T-helper cell, which is necessary to provide help for the maturation of both plasma cells and T-cytotoxic cells.41 Therefore, HIV suppresses the immune response against itself and secondarily creates a generalized immune deficiency by suppressing the development of immune responses against other pathogens and opportunistic microorganisms. A patient has DiGeorge syndrome. Which assessment findings should the nurse monitor for in this patient? Low calcium level and Tetany A nurse is caring for a client who is deficient in T cells. Which result of this T cell deficiency does the nurse anticipate? Decrease in leukocytes, impaired cellular immunity. Pulmonary Alterations Pulmonary function tests Identify purposes for preforming PFT’s? Used to diagnose certain types of lung disease, such as asthma, bronchitis, and emphysema or Pulmonary Fibrosis. Finds the cause of SOB. What is the role of pulmonary function testing? Group of tests that measure how well your lungs work. How well the lungs take in and exhale air and efficiently they tx 02 into the blood. Tests that measure lung size, air flow such as spirometry and lung volume tests. What do PFT screening do? Spirometry is the most widely used screening test of lung function. can include simple screening spirometry, formal lung volume measurement, diffusing capacity for carbon monoxide, and arterial blood gases. These studies may collectively be referred to as a complete pulmonary function survey. A 15-year-old female is … with restrictive lung disease caused by fibrosis. The patient had a pulmonary functions test. Which of the following findings is expected? Decreased functional residual capacity Relationship of lung compliance and residual volume A nurse is teaching about the functions of the pulmonary system. Which information should the nurse include? One of the functions of the pulmonary system is the: Exchange of gases between the environment and blood Provides 0xygen-rich blood to tissue. The Pulmonary system (1) ventilates the alveoli, (2) diffuses gases into and out of the blood, (3) perfuses the lungs so that the organs and tissues of the body receive blood that is rich in 02 and low in C02 An 80-year-old male presents to his primary care provider reporting difficulty breathing. Pulmonary function tests reveal that he has increased residual volume. A nurse suspects the most likely cause of this disorder is _____in lung compliance? An INCREASE in lung compliance (Residual volume is the amount of air left in the lungs at the end of a maximal expiration and is typically increased due to the inability to forcibly expire and remove air from the lungs). Shifts in the oxyhemoglobin dissociation In a patient with acidosis or a fever, the nurse would expect the oxyhemoglobin dissociation curve to shift: To the RIGHT, causing more 02 to be released to the cells The oxyhemoglobin dissociation curve is shifted to the right by acidosis (low pH) and hypercapnia (increased PaCO2). What factors affect oxyhemoglobin dissociation? Many factors affect O2 dissociation curve or oxygen dissociation curve. Factors include pH, PCO2, 2,3 BPG, (2,3-DPG), temperature, carbon monoxide, metabolic acidosis, metabolic alkalosis, high altitude, chronic bronchitis, hemolytic anemias like sickle cell anemia In a normal person, as PaO2 drops from 100 to 80 to 60, there is ________ in how tightly Hgb is holding onto its 02 (90-100% saturation). But when the PaO2 approaches 50, the s-curve begins to __drop sharply_, and as it does it means that _ ALMOST NO CHANGE, Hgb will be to release its 02 and more freely into tissue For a right shifted curve, for the same PaO2 there will … a lower ______ when compared to a normal curve % of 02 still bound to Hgb What causes a R shift? Exercise and Pathological conditions of body temp (wound healing or infection) In both healthy and pathological conditions, the signs of a R shift are? Increased temp/hyperthermia/febrile condition, increased PaCo2, decreased pH. What causes a L shift? Hyperventilation (high altitude) hypercapnia, hypothermia, Hgb wants to hold onto its 02 more tightly so the Pa02 must drop very low before the Hgb begins to release its 02 more freely CO2 transport in the blood Most carbon dioxide in the blood is transported? In the form of bicarbonate as carbaminohemoglobin. Dissolution directly into the blood. Binding to hemoglobin. Carried as a bicarbonate ion. If an individual with respiratory difficulty were retaining too much carbon dioxide, which of the following compensatory responses would the nurse expect to … initiated? Increased Respiratory Rate A patient wants to know how carbon dioxide is transported in the body. How should the nurse respond? Carbon dioxide (CO2) is mainly transported in the blood: In the form of bicarbonate Characteristics of alveoli Air passage between alveoli is collateral and evenly distributed because of? Pores of Kohn Changes in the alveoli that cause an increase in alveolar surface tension, alveolar collapse and decreased lung expansion are a result of? Decreased surfactant production. Students in a histology class are assigned to identify regions of the __The slide shows a basement membrane, capillary lumen, and macrophages. The students are looking at the: Alveoli While auscultating a patient’s lungs, a nurse recalls the alveoli in the apexes of the lungs are _____ than alveoli in the bases. Larger The nurse is caring for a client who is now 2 days post near-drowning. The focused assessment would involve which of the following areas of the lung involved in gas exchange? Alveoli Arterial perfusion pressure and alveolar gas pressure in the lung base A consequence of alveolar hypoxia is: Mast cells initiate a wide-spread systemic inflammation. Rationale: The common presence of an underlying inflammatory component suggests that inflammation may contribute to the pathogenesis of the systemic effects of alveolar hypoxia. The pressure … to inflate an alveolus is inversely … to: Alveolar radius The nurse is describing the movement of blood into and out of the capillary beds of the lungs to the body organs and tissues. What term should the nurse use to describe this process? Perfusion Which principle should the nurse remember while planning care for a patient with respiratory problems? Diffusion of respiratory gases takes place at the: Alveolocapillary membrane A pulmonologist is discussing the base of the lungs with staff. Which information should … included? At the base of the lungs: Arterial perfusion pressure exceeds alveolar gas pressure. When the pulmonologist discusses the condition in which a series of alveoli in the left lower lobe receive adequate ventilation but do not have adequate perfusion, which statement indicates the nurse understands this condition? When this occurs in a patient it is called: Alveolar dead space How do determine the partial pressure of oxygen given the percentage of oxygen in the air and the barometric pressure What is the partial pressure of oxygen in the lung given the following conditions? Percentage of oxygen in air: 20 Barometric pressure: 700 mm Hg : 140 mm Hg What would the partial pressure of oxygen equal if the barometric pressure was 600 mm Hg? 120 mm Hg Results of increased work of breathing An 80-year-old male presents to his primary care provider reporting difficulty breathing. Pulmonary function tests reveal that he has increased residual volume. A nurse suspects the most likely cause of this disorder is _____ in lung compliance. An INCREASE in lung compliance Know terms: Vital capacity (VC), While reviewing the results of the pulmonary functions test, the nurse is aware that the maximum amount of gas that can …… from the lung is called: Displaced (Expired) from the lung is called Vital capacity Vital Capacity Total lung capacity The average total lung capacity of an adult human male is about 6 liters of air. Tidal breathing is normal, resting breathing; the tidal volume is the volume of air that is inhaled or exhaled in only a single such breath. The volume of air contained in the lungs at the end of a maximal inspiration. It is the equivalent to each of the following sums: VITAL CAPACITY plus RESIDUAL VOLUME; INSPIRATORY CAPACITY plus FUNCTIONAL RESIDUAL CAPACITY; TIDAL VOLUME plus INSPIRATORY RESERVE VOLUME ... What would happen to TLC and VC of your lungs become stiff and less elasticity Can’t take in as much air because elasticity is reduced Functional capacity A functional capacity evaluation (FCE) is set of tests, practices and observations that are combined to determine the ability of the evaluated person to function in a variety of circumstances, most often employment, in an objective manner. Residual volume The volume of air remaining in the lungs after a maximal exhalation Functional residual capacity (FRC) Which of the following terms should the nurse use when there is a balance between outward recoil of the chest wall and inward recoil of the lungs at rest? Functional residual capacity (FRC) is reached A 15-year-old female is diagnosed with restrictive lung disease caused by fibrosis. The patient had a pulmonary functions test. Which of the following findings is expected? Decreased functional residual capacity Renal Alterations Types of nephrons and their functions The nephrons that determine the concentration of the urine are _____ nephrons. Juxtamedullary Which of the following renal structures is not a component of the nephron? Renal Capsule At which of the following locations in the nephron would a nurse practitioner first expect blood to … largely free of plasma proteins? Boman space Which of the following substances is most likely to … reabsorbed in the tubular segments of the nephron using passive transport mechanisms? Water What is the function of nephron? Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed and excreting the rest as urine The nephrons are the functional units of the kidney, responsible for the initial formation of urine. The nurse knows that damage to the area of the kidney where the nephrons are … will affect urine formation. Identify that area. Renal cortex (The majority of nephrons (80% to 85%) are located in the renal cortex) Overall renal physiology Substances that are actively secreted by the renal tubules Which of the following substances are actively secreted by the renal tubules? Hydrogen and potassium Which of the following comprises the kidney’s transport system? Tubules and pelvis Activation of the renin-angiotensin system Which of the following statements correctly describes a direct end-effect of the renin-angiotensin-aldosterone system? Aldosterone increases renal reabsorption of water and sodium. A major end-effect of the renin-angiotensin-aldosterone system is sodium and water reabsorption in the renal tubules through the effects of aldosterone. The result is preservation of blood volume and increased blood pressure. What does the reduced perfusion of the kidney activate that causes constriction of peripheral arterioles? Norepinephrine and epinephrine cause vasoconstriction by binding to α1-adrenoceptors, which are located mainly on the afferent arterioles. Activation of α1-adrenoceptors decreases GFR and RBF. Dehydration or strong emotional stimuli, such as fear and pain, activate sympathetic nerves and reduce GFR and RBF. Glomerular filtration rate The glomerular filtration rate (GFR) is directly related to the Perfusion pressure in the glomerular capillaries The filtration of the plasma per unit of time is known as the glomerular filtration rate(GFR), which is directly related to only the perfusion pressure in the glomerular capillaries. A nurse educator is orientating anew nurses to a renal unit of a hospital. Which of the follow teaching points should the nurse include as a part of a review of normal glomerular function? Glomerular filtrate is very similar in composition to blood plasma found elsewhere in circulation Which of the following factors affect glomerular filtration rate? A) constriction or dilatation of afferent and efferent arterioles B) plasma osmotic pressure C) hydrostatic pressure D) ALL THE ABOVE Mesangial cells A urologist is discussing the phagocytic cells that lie between the layers of the renal corpuscle Mesangial cells Lying between the layers of the renal corpuscle is a population of phagocytic cells called? Mesangial cells Renal system anatomy When the renal system secretes rennin, it causes the direct activation of? Angiotensin I Why plasma proteins should … absent from the urine The fluid formed in the capillary cluster of the nephron is the same as blood plasma except for the absence of? Larger molecules of plasma protein Which of the following substances does not normally get filtered in the kidneys? Plasma proteins Effects of urinary tract obstruction- hydronephrosis and a decreased glomerular filtration rate A 25-year-old female is … with urinary tract obstruction. while planning care, the nurse realizes that the patient is expected to have hydronephrosis and a decreased glomerular filtration rate caused by? Dilation of the renal pelvis and calyces proximal to a blockage Which of the following changes will result in a decreased glomerular filtration rate? Increased hydrostatic pressure in Bowman's capsule Effect of urinary retention A 55-year-old male presents reporting urinary retention. Tests reveal that he has a lower urinary tract obstruction. Which of the following is of most concern to the nurse? Formation of renal calculi A group of students are reviewing information about disorders of the bladder and urethra. The students demonstrate understanding of the material when they identify which of the following as a voiding dysfunction? Urinary retention A client presents at the clinic with complaints of urinary retention. What question should the nurse ask to obtain additional information about the client’s complaint? When did you last urinate? The nurse is teaching a group of nursing students about acute glomerulonephritis genitourinary conditions. A student asks the about a condition that occurs when there is a decreased volume of urine output. The condition the student is referring to is which of the following? Oliguria (Oliguria is a subnormal volume of urine) Most common type of renal stone When a patient asks what the most common type of renal stones is …. of, how should the nurse respond? The most common type of renal stone is … of Calcium The nurse recognizes that a referral for genetic counseling is inappropriate for the client with: Renal calculi (Explanation: Wilms’ tumor, polycystic disease, and Alport are Because a client’s renal stone was found to ….. of uric acid, a low-purine, alkaline-ash diet was ordered. Incorporation of which of the following food items into the home diet would indicate that the client understands the necessary diet modifications? Foods that may be eaten as desired in a low-purine diet include milk, all fruits, tomatoes, cereals, and corn. RATIONALE: Because a high-purine diet contributes to the formation of uric acid, a low-purine diet is advocated. An alkaline-ash diet is also advocated because uric acid crystals are more likely to develop in acid urine. Foods allowed on an alkaline-ash diet include milk, fruits (except cranberries, plums, and prunes), and vegetables (especially legumes and green vegetables). Gravy, chicken, and liver are high in purine. Epispadias The optimal time for surgical repair of the Hypospadias and epispadias is In the EARLY pre-school period What gender has predominance for exstrophy-epispadias complex? Males (by factor of 2.5) What 4 considerations must … addressed when performing the epispadias repair? 1) Correction of dorsal chordee 2) Urethra recon 3) Glanular recon 4) Penile skin closure What are 2 anomalies noted with epispadias? Along with bladder and cloacal exstrophy, you can have: 1) VUR 2) inguinal hernias List 3 goals of surgical treatment of epispadias 1) Urinary continence 2) Upper tract preservation 3) Cosmetic penis What is the most important indicator of successful continence with epispadias repair? Good bladder capacity What are the 3 types of female epispadias? 1) Patulous urethra 2) Dorsally split along most of urethra 3) Complete urethral cleft with incontinence PIC: A=normal, B=clitoris altered, C and D=varying degree of urethral defect What are other aspects of female epispadias? Urinary incontinence, abnormal anatomical features such as: bilateral labia minora, bifid clitoris (split in two) and patulous (spread widely apart) urethra, and a low bladder leak pressure on cystometrography. Glomerulonephritis A 15-year-old male was … with pharyngitis. Eight days later he developed acute glomerulonephritis. While reviewing the culture results, which of the following is the most likely cause of this disease? Group A ßhemolytic streptococcus When a nurse observes post-streptococcal glomerulonephritis as a diagnosis on a patient, which principle will the nurse remember? Acute post-streptococcal glomerulonephritis is primarily caused by? Antigen-antibody complex deposition in the glomerular capillaries and inflammatory damage A 30-year-old male is demonstrating hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin being the major protein. The most probable diagnosis the nurse will see documented on the chart is? Acute glomerulonephritis A 15-year-old female presents with flank pain, irritability, malaise, and fever. Tests reveal glomerulonephritis. When the parents ask what could have caused this, how should the nurse respond? Poststreptococcal infectin Which of the following clusters of symptoms would make a clinician suspect a child has developed glomerulonephritis? Gross hematuria, flank pain, and hypertension A 5-year-old male was … with glomerulonephritis. History reveals that he had an infection 3 weeks before the onset of this condition. The infection was most likely … in the Respiratory tract A 30-year-old male is demonstrating hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day, with albumin being the major protein. The most probable diagnosis the nurse will see documented on the chart is? Acute glomerulonephritis A 45-year-old male presents with oliguria. He is … with chronic glomerulonephritis. The nurse knows oliguria is … to? Thickening of the glomerular membrane and decreased renal blood flow Which assessment finding is most important in determining nursing care for a client with acute glomerulonephritis? Blurred vision. Visual disturbances can be indicative of rising blood pressure in a client with acute glomerulonephritis. The nurse is assessing a child with acute poststreptococcal glomerulonephritis. Which of the following would the nurse expect to assess? Hematuria, proteinuria, edema, and renal insufficiency. Tea-colored urine is an indication of hematuria. A child with acute poststreptococcal glomerulonephritis (APSGN) is admitted to the pediatric ICU for overnight observation. Which of the following physical assessment findings should the nurse expect? Pallor Reports of anorexia Lethargy Nephrotic syndrome A urologist is discussing nephritic syndrome. Which information should … included? If nephrotic syndrome is not caused initially by kidney disease, it is termed ____ nephrotic syndrome? Secondary Response Feedback: Secondary nephrotic syndrome is not caused initially by kidney disease. A 4-year-old male is … with nephrotic syndrome. Which of the following assessment findings accompanies this condition? Proteinuria Response Feedback: Proteinuria accompanies nephrotic syndrome. A 7-year-old female is … with nephrotic syndrome. Which of the following should the nurse ask the parents if they or the child has noticed recently? Frothy urine Response Feedback: In the child with nephrotic syndrome, the parents may notice diminished, frothy, or foamy urine output. Nephrotic syndrome occurs when there is loss of _____ in the urine. Protein Secondary forms of nephrotic syndrome are … with all of the following conditions except: Hyperthyroidism. ARE ASSOCIATED: Diabetes, Renal disease, Systemic lupus erythematosus, Which of the following diseases is a glomerular disorder? Glomerular diseases are associated with many solid and hematologicmalignancies Minimal Change Disease (MCD) is the most common primary glomerular disease in children, accounting for 70% to 90% of cases of nephrotic syndrome glomerular disease causes problems at the cellular level Which assessment finding is common in children …. with nephrotic syndrome? Generalized edema Rationale: Nephrotic syndrome is defined as massive proteinuria, hypoalbuminemia, hyperlipemia, and edema. Other manifestations include weight gain; periorbital and facial edema that is most prominent in the morning; leg, ankle, labial, or scrotal edema; decreased urine output and urine that is dark and frothy; abdominal swelling; and blood pressure that is normal or slightly decreased. A child is getting a diagnostic work-up for nephrotic syndrome. Which of the following lab results would the nurse expect to see? Proteinuria, hypoalbuminemia, and hypercholesterolemia are diagnostic of a child with nephritic syndrome. Rationale: The child will also present symptomatically with a sudden onset of edema. Hematuria is typically seen with glomerulonephritis. [Show More]
Last updated: 1 year ago
Preview 1 out of 14 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 13, 2021
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Aug 13, 2021
Downloads
0
Views
45



.png)

.png)