*NURSING > STUDY GUIDE > NR 509 Final Study Guide Behavior/Mental Health Assessment and Modification for Age (Latest 2020) (All)
NR 509 Final Study Guide Behavior/Mental Health Assessment and Modification for Age (Latest 2020)
Document Content and Description Below
NR 509 Final Study Guide Behavior/Mental Health Assessment and Modification for Age 1. Assessment: a. b. Many mental health disorders are masked by other clinical conditions; 20% of primary car... e outpatients have mental disorders(50-70% go undetected and untreated) c. Physical symptoms account for approx 50% of office visits d. ⅓ of physical symptoms are unexplained; in 20-25% those symptoms become chronic e. Symptoms and Behaviors: i. Sorting symptom is a challenge; can be unexplained symptoms 1. Patients who have unexplained symptoms depression and anxiety exceeds 50% ii. Physical or “somatic” symptoms account for 50% of U.S. office visits 1. Pain, fatigue, palpitations, GI symptoms, sexual dysfunction, dizziness or loss of balance 2. Symptoms that present as clusters are called “functional syndromes” such as IBS, fibromyalgia, chronic fatigue, TMJ disorder, and multiple chemical sensitivity 3. The presence of symptom overlap is high in the common functional syndromes such as fatigue, headache, sleep disturbance, pain, GI upset iii. Patients with unexplained and somatic symptoms are often frequent users of the health care system and termed “difficult patients” iv. Patients with symptoms that last longer than 6 weeks are recognized as chronic and should be screened for depression and anxiety. a. A two tiered approach is recommended for screening. A brief screening with questions that yield high sensitivity then a more detailed investigation when indicated V. Patient who warrant a mental health screening include: 1. medically unexplained physical symptoms 2. Multiple physical or somatic symptoms 3. High severity of the presenting somatic symptom 4. Chronic pain 5. Symptoms longer than 6 weeks 6. Physician stating “a difficult encounter” 7. Recent stress 8. Low self-rating of overall health 9. Frequent use of health care services 10. Substance abuse 2. Adjustment for age: A. Elderly: a. Older adults may complain of memory problems but usually is due to benign forgetfulness. b. Older adults retrieve and process data more slowly and take longer to learn new information c. Older adults may have slower motor responses and their ability to perform complex task may diminish d. It is important to try to distinguish age-related changes from manifestations of mental disorders e. Older patients are more susceptible to delirium which could be the first sign of infection, problems with medications, or impending dementia B. Newborn: a. Assess mental status of a newborn by observing newborn activities i. Look at human faces and turn to a parents voice ii. Ability to shut out repetitive stimuli(such as a vacuum) iii. Bond with caregiver iv. self-soothe b. Assess for mental status during alert periods · Normal VS. Abnormal Findings and Interpretation 1. Attention: a. Normal: able to focus and concentrate b. Abnormal: inattentive and easily distracted 2. Memory a. Normal: able to repeat immediate repetition of material given; b. Abnormal: unable to repeat recent events 3. Orientation: a. Normal: aware of person, place, and time b. Abnormal: unaware of person, place, or time 4. Perception: a. Normal: Sensory awareness of objects in the environment b. Abnormal: hallucinations 5. Thought Process: a. Normal: logic, coherent, and relevant thoughts b. Abnormal: irrational thought 6. Thought Content: a. Normal: Has insight and judgement b. Abnormal: impaired judgement and irrational behaviors 7. Insight a. Normal: able to distinguish normal vs. abnormal b. Abnormal: Unable to distinguish normal vs. abnormal 8. Judgement a. Normal: good judgement b. Abnormal: poor or bad F· Speech Patterns 1. Note characters of speech a. Slow speech= depression b. Accelerated and Loud speech= mania c. Articulation: are the words clear and distinct; does the speech have a nasal quality i. Dysarthria(defective articulation) ii. Dysphonia-impaired volume, quality or pitch iii. Aphasia-disorder of speech d. Fluency: reflects rate, flow and melody of speech and the content and words used. Abnormalities include i. Hesitancies and gaps in flow ii. Disturbed inflections such as monotone iii. Circumlocutions, in which phrases or sentences are substituted for a word the person cannot think of ie. “what you write with” instead of “pen” iv. Paraphrasias, words are malformed(“I write with a den”), wrong (I write with a bar) or made up (I write with a dar) v. Fluency abnormalities indicate aphasia from cerebrovascular infarction. vi. Aphasia may be receptive(impaired comprehension with fluent speech) OR expressive(with preserved comprehension and slow nonfluent speech) vii. A person who can write a correct sentence does NOT have aphasia e. Testing for Aphasia i. Word Comprehension: Ask the patient to follow one-stage commands such as “Point to your nose” ii. Repetition: Ask the patient to repeat a phrase of one-syllable words “ No ifs, ands, or buts” iii. Naming: Ask the patient to name the parts of a watch iv. Reading Comprehension: Ask the patient to read a paragraph aloud v. Writing: Ask the patient to write a sentence · Mental Status Examination 1. Five components of the mental status examination a. Appearance and Behavior i. Note level of consciousness: is the patient awake and alert, does the patient understand your questions and respond appropriately 1. If the patient does not respond then speak to the patient by name in a loud voice 2. Lethargic patients are drowsy but open their eyes and look at you, respond to questions, then fall back asleep 3. Obtunded patients open their eyes and look at you but respond slowly and are somewhat confused ii. Note posture and motor behavior:does the patient sit or lie quietly or prefer to walk around; note the pace, range, and type of movement 1. Look for tense posture, restlessness, and anxious fidgeting; the crying, pacing, and hand wringing of agitated depression 2. The hopeless slumped posture and slowed movement of depression 3. The agitated and expansive movements of manic episodes iii. Note Dress, Grooming, and Personal hygiene: how is the patient dressed, clean and presentable?, how is grooming compared to those of similar age, compare one side to the other 1. May deteriorate in depression, schizophrenia, and dementia 2. Excessive fastidiousness may be seen OCD 3. One-sided negligence may result from a lesion in the opposite parietal cortex; usually the non-dominant side iv. Note facial expression: observe the face at rest and during conversation; are changes in expression appropriate 1. Note Expressions of anxiety, depression, apathy, anger, elation, or facial immobility in parkinsonism v. Manner, Affect, and Relationship to People and Things: assess the patients external expression of the inner emotional state(Affect). Is the affect appropriate to topics being discussed?, seem exaggerated at points, labile, blunted, or flat? 1. Paranoia= anger, hostility, suspiciousness, or evasiveness 2. Mania= elation and euphoria 3. Schizophrenia=flat affect with remoteness 4. Dementia and Anxiety or Depresion= apathy(dulled affect with detachment and indifference) 5. Hallucinations=schizophrenia, alcohol withdrawal, and systemic toxicity b. Speech and Language= SEE ABOVE in language patterns c. Mood: Ask patient to describe his/her mood, including usual level and fluctuations related to life events i. Moods range from sadness and melancholy, contentment, joy, euphoria, and elation; anger and rage, anxiety and worry, to detachment and indifference ii. If you suspect depression, assess its severity and any risk of suicide iii. It is your responsibility as the provider to ask directly about suicidal thoughts. This may be the only way to uncover suicidal ideation and plans that launch immediate intervention and treatment d. Thought and Perception: i. Thought Process: assess the logic, relevance, organization, and coherence of the patients thought process throughout the interview; does speech progress logically?, listen for patterns of speech that suggest disorders; Variations and Abnormalities include: 1. Circumstantiality: speech with unnecessary detail, indirection, and delay in reaching the point; Occurs in patients with obsessions 2. Derailment: “tangential” speech with shifting topics that are loosely connected or unrelated; seen in schizophrenia, manic episodes, and other psychotic disorders 3. Flight of Ideas: a continuous flow of accelerated speech with abrupt changes from one topic to the next; most frequently seen in manic episodes 4. Neologisms: Invented or distorted words, or words with new and highly idiosyncratic meanings; observed in schizophrenia, psychotic disorders, and aphasia 5. Incoherence: Speech that is incomprehensible and illogical, with lack of meaningful connections, abrupt changes in topic, or disordered grammar or word use. Flight of ideas, when severe, may produce incoherence. Seen in severe psychotic disturbances usually schizophrenia 6. Blocking: Sudden interruption of speech in mid sentence or before the idea is completed, attributed to “losing the thought.” Blocking occurs in normal people. May be striking in schizophrenia 7. Confabulation: Fabrication of facts or events in response to ques- tions, to fill in the gaps from impaired memory. Seen in Korsakoff syndrome from alcholism 8. Perseveration: Persistent repetition of words or ideas Occurs in schizophrenia and other psychotic disorders 9. Echolalia:Repetition of the words and phrases of others. Occurs in manic episodes and schizophrenia 10. Clanging: Speech with choice of words based on sound, rather than meaning, as in rhyming and punning. For example, “Look at my eyes and nose, wise eyes and rosy nose. Two to one, the ayes have it!” Seen in schizophrenia and manic episodes ii. Thought Content: to assess follow patients cues rather than asking direct questions; “Can you tell me more about that” or “What do you think about times like these?” Abnormalities in content include 1. Compulsions: Repetitive behaviors that the person feels driven to perform in response to an obsession, aimed at preventing or reducing anxiety or a dreaded event or situation; these behaviors are excessive and unrealistically connected to the provoking stimulus 2. Obsessions: Delusions 3. Recurrent persistent thoughts, images, or urges experienced as intrusive and unwanted that the person tries to ignore, suppress, or neutralize with other thoughts or actions (for example, performing a compulsive behavior) 4. Phobias :Persistent irrational fears, accompanied by a compelling desire to avoid provoking stimulus 5. Anxieties: Apprehensive anticipation of future danger or misfortune accompanied by feelings of worry, distress, and/or somatic symptoms of tension 6. Feelings of Unreality: A sense that the environment is strange, unreal, or remote 7. Feelings of Depersonalization:A sense that one’s self or identity is different, changed, unreal; lost; or detached from one’s mind or body 8. Delusions: False fixed personal beliefs that are not amenable to change in light of conflicting evidence; types of delusions include: a. ● Persecutory ● Grandiose ● Jealous ● Erotomanic—the belief than another person is in love with the individual ● Somatic—involves bodily functions or sensations ● Unspecified—includes delusions of reference without a prominent persecutory or grandiose component, or the belief that external events, objects, or people have a particular and unusual personal significance (for example, commands from the radio or television) 9. Compulsions, obsessions, phobias, and anxieties often occur in anxiety disorders. 10. Delusions and feelings of unreality or depersonalization are often associated with psychotic disorders 11. Delusions may also occur in delirium, severe mood disorders, and dementia iii. Perceptions: Purse false perceptions, “When you heard the voice speaking to you, what did you say?” Abnormalities in perception include 1. Illusions: Misinterpretations of real external stimuli, such as mistaking rustling leaves for the sound of voices. Illuisions may occur in grief reactions, delirium, acute and posttraumatic stress disorders, and schizophrenia 2. Hallucinations: Perception-like experiences that seem real but, unlike illusions, lack actual external stimulation. The person may or may not recognize the experiences as false. Hallucinations may be auditory, visual, olfactory, gustatory, tactile, or somatic. False perceptions associated with dreaming, falling asleep, and awakening are not classified as hallucinations. Hallucinations may occur in delirium, dementia, posttraumatic stress disorder, schizophrenia, and alcoholism e. Insight:Patients with psychotic disorders often lack insight into their illness, Denial of impairment may accompany some neurologic disorders f. Judgement: may be poor in delirium, dementia, intellectual disability, and psychotic states. Anxiety, mood disorders, intelligence, education, income, and cultural values also influence judgement g. Cognitive Functions: i. Orientations: Assess person, place and time 1. Disorientation is common when memory or attention is impaired, as in delirium ii. Attention: Digit Span, Serial 7s, and Spelling Backward are used to test attention 1. Digit Span: recite a series of digits and ask patient to repeat; try increasing the series to a multiple numbers; choose digits such as street numbers and zip codes and not consecutive numbers Causes of poor performance include delirium, dementia, intellectual disability, and performance anxiety 2. Serial 7s: Tell patient to start at 100 and count back by 7s 3. Spelling Backward: Spell a 5 letter word and ask the patient to repeat it backwards iii. Remote Memory: Inquire about birthdays, anniversaries, social security #, names of schools attended, jobs held, or past historical events such as wars May be imparied in late dementia iv. Recent Memory: Ask questions with answers you can check against other sources; involve events of the day, weather, appointment time, current meds, lab test Impaired in dementia and delirium, Amnestic disorders impair memory or new learning ability and reduce social or occupational functioning, but lack the global feature of delirium or dementia. Anxiety, depression, and intellectual disability may also impair recent memory v. New Learning Ability: Give the patient 3-4 words and ask them to repeat the words. After 3-5min ask the patient to repeat the words. h. Higher Cognitive Functions i. Information and vocabulary:Ask about work, hobbies, reading, favorite television programs, or current events. Start with simple questions, then move to more difficult questions. Note the person’s grasp of information, complexity of the ideas, and choice of vocabulary. Information and vocabulary are rela- tively unaffected by psychiatric disorders except in severe cases. Testing helps distinguish adults with life-long intellectual impairment (whose infor- mation and vocabulary are limited) from those with mild or moderate dementia (whose information and vocabulary are fairly well preserved). ii. Calculating Ability: Test ability to do arithmetical calculations; start with simple addition, or pose practical functionally important questions such as if something cost 78 cents and you give the clerk $1 how much change should your receive Poor performance suggests dementia or aphasia, but should be measured against the patient’s fund of knowledge and education. iii. Abstract Thinking: ask the patient about what certain proverbs mean or explain the similarity between two things such as an apple and orange. Concrete responses are common in people with intellectual disability, delirium, or dementia, but may also reflect limited education. Patients with schizophrenia may respond concretely or with personal and bizarre interpretations iv. Constructional Ability: ability to copy figures of increasing complexity onto a piece of blank unlined paper. With intact vision and motor ability, poor constructional ability suggests dementia or parietal lobe damage. Intellectual disability can also impair performance. i. Special Techniques for the Mental Exam i. Mini-Mental State Examination: brief test used to screen for cognitive dysfunction or dementia, and follow the patients course over time j. Recording Your Findings i. Example of normal findings:The patient is alert, well-groomed, and cheerful. Speech is fluent and words are clear. Thought processes are coherent, insight is good. The patient is oriented to person, place, and time. Serial 7s accurate; recent and remote memory intact. Calculations intact. ii. Example of findings that suggest dementia: “The patient appears sad and fatigued; clothes are wrinkled. Speech is slow and words are mumbled. Thought processes are coherent, but insight into current life reverses is limited. The patient is oriented to person, place, and time. Digit span, serial 7s, and calculations accurate, but responses delayed. Clock drawing is good. · Screening for Depression: BECKY PECK Generalized Anxiety Disorder: WONGEL MARKOS Depressive Disorders: CRYSTAL SHAGENA/Ada Ejimadu Depressive Disorders ( pg 156) Ada Ejimadu Depression and anxiety disorders are a common cause of hospitalization in the United States, and mental illness is associated with increased risks for chronic medical conditions, decreased life expectancy, disability, substance abuse, and suicide. About 19million adult American or almost 7% have major depression with other co-existing anxiety disorder or substance abuse. Depression is as common in women as men, and the prevalence of postpartum depression is about 7% to 13%. Most patients with chronic medical conditions have depression. Symptoms of depression in high-risk patients may be subtle and may include; I. Low self-esteem II. Loss of pleasure in daily activities (Anhedonia) III. Sleep disorder, IV. Difficulty concentrating or making decisions. Look carefully for symptoms of depression in vulnerable patients, especially those who are young, female, single, divorced or separated, seriously or chronically ill, bereaved, or have other psychiatric disorders, including substance abuse. A personal or family history of depression also places patients at risk. Asking two simple questions about mood and anhedonia appears to be as effective as using more detailed instruments. All positive screening tests warrant full diagnostic interviews. Failure to diagnose depression can have fatal consequences—the presence of an affective disorder is associated with an 11-fold increased risk for suicide. Depression screening · Over the past 2 weeks, have you felt down, depressed, or hopeless? · Over the past 2 weeks, have you felt little interest or pleasure in doing things ·(anhedonia)? Depression tends to be long-lasting and can recur. Because of these two factors, a wait-and-see approach to treatment is not desirable and timely treatment is necessary. Suicide I. Suicide is the second leading cause of death among 15- to 24-year olds. II. Suicide rates are highest among those ages 45 to 54 years, III. followed by elderly adults ≥age 85 years. IV. Men have suicide rates nearly four times higher than women, though women are three times more likely to attempt suicide. V. Men are most likely to use firearms to commit suicide, VI. while women are most likely to use poison. VII. Overall, suicides in non-Hispanic whites account for about 90% of all suicides. VIII. American Indian/Alaska Native women ages 15 to 24 years have the highest suicide rates of any racial/ethnic group. Substance Use Disorders, Including Alcohol and Prescription Drugs. The harmful interactions between mental disorders and substance use disorders also present a major public health problem. Rates of drug-induced deaths continue to increase and are highest among whites and American Indian/Alaska Natives. The Centers for Disease Control and Prevention reports that prescription drugs have replaced illicit drugs as a leading cause of drug-induced deaths. Every patient should be asked about alcohol use, substance abuse, and misuse of prescription drugs Schizophrenia (Pg. 161, 162) Variations and abnormalities in thought process: ● See above “Thought process” section for abnormalities seen in schizophrenia Suicide Risk and Prevention KIMBERLY RAFFAELE Chapter 9 and Chapter 12 · Cardiac/Vascular Assessment and Modification for Age MADAME QT PIE Chapter 9: Cardiac/Vascular Assessment and Modifications for Age 1.) Describe the chest wall anatomy and identify the key listening areas. -The general appearance of the patient provides many clues to cardiac illness, so pay special attention to the patient’s color, respirin the right internal jugular vein, which is directly in line with the superior vena cava and right atrium. The internal jugular veins lie deep to the SCM muscles in the neck and are not directly visible. (See Figure 9-24 pg375) Pulsations in the right external jugular vein can also be used, but the route from the vena cava is more tortuous, and examination can be impaired by kinking and obstruction at the base of the neck and by obesity. Note that the jugular veins and pulsations are difficult to see in children under 12 years of age, so inspection is not useful in this age group. The DOMINENT MOVEMENT of the JVP is INWARD vs the CAROTID PULSE MOVEMENT is OUTWARD! - Identify the highest point of pulsation in the right jugular vein. Extend a long rectangular object or card horizontally from this point and a centimeter ruler vertically from the sternal angle, making an exact right angle. Measure the vertical distance in centimeters above the sternal angle where the horizontal object crosses the ruler and add to this distance 5 cm, the distance from the sternal angle to the center of the right atrium. The sum is the JVP. -JVP measured at >3 cm above the sternal angle, or more than 8 cm in total distance above the right atrium, is considered elevated above normal. -Carotid Upstroke- View figure 9-27 on page 379. The first elevation, the presystolic a wave, reflects the slight rise in atrial pressure that accompanies atrial contraction. It occurs just prior to S1 and before the carotid upstroke. The normal upstroke is brisk; it is smooth, rapid, and follows S1 almost immediately. The timing of the carotid upstroke in relation to S1 and S2. Note that the normal carotid upstroke follows S1 and precedes S2. -Carotid Bruits- The carotid pulse provides valuable information about cardiac function, especially aortic valve stenosis and regurgitation. Press just inside the medial border of a relaxed SCM muscle. Never palpate both carotid arteries at the same time. This may decrease blood flow to the brain and induce syncope. Auscultate both the carotid arteries to listen for a bruit, a murmur-like sound arising from turbulent arterial blood flow. Ask the patient to stop breathing for ∼15 seconds, then listen with the diaphragm of the stethoscope, which generally detects the higher frequency sounds of arterial bruits better than the bell. 3.) Palpate and describe the apical impulse (PMI). -To assess the PMI and extra heart sounds such as S3 or S4, ask the patient to turn to the left side, termed the left lateral decubitus position—this brings the ventricular apex closer to the chest wall. To bring the left ventricular outflow tract closer to the chest wall and improve detection of aortic regurgitation, have the patient sit up, lean forward, and exhale. -Location of PMI: Left sternal Boarder 5 th intercostal space Midclavicular line -Diameter of PMI: In the supine position it usually measures 2.5cm, about the size of a quarter. In the decubitus position it may feel larger. -Amplitude of PMI: Is it Brisk and tapping, diffuse, or sustained? Normal Findings: small/brisk/ tapping 4.) Auscultate S1 and S2 in 6 positions from the base to the apex. See Figure 9-41 page 390 1.)-2 nd right interspace (Aortic) 2.)-2 nd left interspace (Pulmonic) 3.)-3 rd left interspace (Erbs Point) 4 &5) -4 th & 5 th left interspace (Tricuspid Valve can be heard) 6) -5 th left interspace midclavicular line (Mitral area) 5.) Recognize the effect of the P-R interval on the intensity of S1. -S1 is accentuated in (1) tachycardia, rhythms with a short PR interval, and high cardiac output states (e.g., exercise, anemia, hyperthyroidism) and (2) mitral stenosis. In these conditions, the mitral valve is still open wide at the onset of ventricular systole and then closes quickly. 6.) Identify physiologic and paradoxical splitting of S2. -Physiologic Splitting: Listen for physiologic splitting of S2 in the 2nd or 3rd left interspace. The pulmonic component of S2 is usually too faint to be heard at the apex or aortic area, where S2 is a single sound derived only from aortic valve closure. Normal splitting is accentuated by inspiration, which increases the interval between A2 and P2, and disappears on expiration. In some patients, especially younger ones, S2 may not become single on expiration until the patient sits up. -Paradoxical Splitting: Paradoxical or reversed splitting refers to splitting that appears on expiration and disappears on inspiration. Closure of the aortic valve is abnormally delayed so that A2 follows P2 in expiration. Normal inspiratory delay of P2 makes the split disappear. The most common cause is left bundle branch block. 7.) Auscultate and recognize abnormal sounds in early diastole, including an S3and OS of mitral stenosis. -The opening snap (OS) is a very early diastolic sound caused by abrupt deceleration during the opening of a stenotic mitral valve. It is best heard just medial to the apex and along the lower left sternal border. If loud, an OS radiates to the apex and to the pulmonic area, where it may be mistaken for the pulmonic component of a split S2. Its high pitch and snapping quality help to distinguish it from an S2, but it becomes less audible as the valve leaflets become more calcified. It is heard better with the diaphragm. -You will detect physiologic S3 frequently in children and young adults to the age of 35 or 40 years, and often during the last trimester of pregnancy. Occurring early in diastole during rapid ventricular filling, it is later than an OS, dull and low in pitch, and heard best at the apex in the left lateral decubitus position. The bell of the stethoscope should be used with very light pressure. -A pathologic S3 or ventricular gallop sounds like a physiologic S3. An S3 in adults over age 40 years is usually pathologic, arising from high left ventricular filling pressures and abrupt deceleration of inflow across the mitral valve at the end of the rapid filling phase of diastole. Causes include decreased myocardial contractility, heart failure, and ventricular volume overload from aortic or mitral regurgitation, and left-to-right shunts. The term gallop comes from the cadence of three heart sounds, especially at rapid heart rates, which sounds like “Kentucky.” 8.) Auscultate and recognize an S4 later in diastole. -An S4 (atrial sound or atrial gallop) occurs just before S1. It is dull, low in pitch, and best heard at the apex with the bell. Listen at the lower left sternal border for a right ventricular S4 (or in the subxiphoid area if obstructive lung disease). An S4 is occasionally normal, especially in trained athletes and older age groups. More commonly, it is due to ventricular hypertrophy or fibrosis causing stiffness and increased resistance (or decreased compliance) during ventricular filling following atrial contraction. -Causes of a left-sided S4 include hypertensive heart disease, aortic stenosis, and ischemic and hypertrophic cardiomyopathy. . A left-sided S4 is heard best at the apex in the left lateral decubitus position, with a cadence like “Tennessee. 9.) Distinguish systolic and diastolic murmurs, using maneuvers when needed. **See pages 408-411 the section on MURMUR and be sure and view “Maneuvers” for each Murmur . This section covers Innocent Murmurs, Physiologic Murmurs, Pathologic Murmurs: Aortic Stenosis, Hypertropic Cardiomyopathy, Pulmonic Stenosis, Mitral Regurgitation, Tricuspid Regurgitation, Ventricular Septal Defect, Aortic Regurgitation, and Mitral Stenosis. -Midsystolic ejection murmurs are the most common kind of heart murmur. They may be (1) innocent—without any detectable physiologic or structural abnormality; (2) physiologic—from physiologic changes in body metabolism; or (3) pathologic—arising from structural abnormalities in the heart or great vessels. -Pansystolic (holosystolic) murmurs are pathologic, arising from blood flow from a chamber with high pressure to one of lower pressure, through a valve or other structure that should be closed. The murmur begins immediately with S1 and continues up to S2. -Diastolic murmurs are almost always pathologic. There are two basic types in adults. Early decrescendo diastolic murmurs signify re -Smoking -Hypertension -Hyperlipidemia -Diabetes -Stroke -Coronary heart disease -Body mass index -Sedentary lifestyle -Poor Diet choices -Family history of cardiovascular disease -Approximately 13% of U.S. adults meet five or more criteria, 5% meet six or more criteria, and virtually none meet seven criteria at ideal levels. -Women have become increasingly aware that CVD is their leading cause of death. -2013 data indicate that CVD death rates remain significantly higher for black women than white women, death rates for CHD is higher for blacks than whites. Screening for cardiovascular risk factors -Step 1: Screen for global risk factors -Begin routine screening at 20 years for individual risk factors or “global” risk of CVD and for any family history of premature heart disease (age <55 years in first-degree male relatives and age <65 years in first-degree female relatives). -Risk factors to screen for at this level: family history, smoking, poor diet, physical inactivity, obesity, hypertension, dyslipidemias, diabetes, pulse -Step 2: Calculate 10-year and lifetime CVD risk using an online calculator -Use the CVD risk calculators to establish 10 yr and lifetime risk for patients ages 40-79 -Step 3: Track individual risk factors- hypertension, diabetes, dyslipidemias, metabolic syndrome, smoking, family history, and obesity -almost ⅓ of U.S. adults over the age of 20 have HTN (>140/90), representing nearly 80 million people. -While prevalence of HTN is similar between men and women, prevalence in blacks is substantially higher than in whites. Heart Disease MONICA GONZLEZ Heart Sounds S1- S1 can be best heard over the apex (bottom of heart). The first heart sound is caused by turbulence created when the mitral and tricuspid valves close. Note its intensity and any apparent splitting. Normal splitting is detectable along the lower left sternal border. (Note that S1 is louder at more rapid heart rates, and PR intervals are shorter Accentuated with pregnancy, hyperthyroidism, mitral stenosis) S2- The second heart sound (S2) is produced by the closure of the aortic and pulmonic valves. The sound produced by the closure of the aortic valve is termed A2, and the sound produced by the closure of the pulmonic valve is termed P2. May be split with inspiration. Note its intensity. Split S2- Listen for splitting of this sound in the 2nd and 3rd left interspaces. Ask the patient to breathe quietly, and then slightly more deeply than normal. Does S2 split into its two components, as it normally does? Width of split. How wide is the split? It is normally quite narrow. Timing of split. When in the respirator Such as ejection sounds or systolic clicks Note their location, timing, intensity, and pitch, and variations with respiration (The systolic click of mitral valve prolapse is the most common extra sound) Extra Sounds in Diastole- Such as S3, S4, or an opening snap Note the location, timing, intensity, and pitch, and variations with respiration. An S3 or S4 in athletes is a normal finding. S3 gallops are low pitches over apex using bell of stethoscope, accentuated in CHF, elderly pericarditis, pregnancy and a sign of heart failure S4 is heart before S1, low pitched with hypertension, heart in left lateral decubitus position with stethoscope bell over PMI Heart sounds infants (page 835) In the neonate, you should be able to detect a split S2 if you examine the infant when the infant is completely quiet or asleep. Detecting this split eliminates many, but not all, of the more serious congenital cardiac defects. Pathologic arrhythmias in children can be from structural cardiac lesions but also from other causes such as drug ingestion, metabolic abnormali- ties, endocrine disorders, serious infections, and postinfectious states, or conduction disturbances without structural heart disease. Murmurs: Murmurs are differentiated from S1 & S2 -extra sounds that are longer in duration Tips for identifying heart murmurs 1. Timing-systole or diastole? Duration? 2. Where is the murmur heard the loudest? Base, Sternal Boarder, Apex, Does it radiate? 3. Have the patient exhale and lean forward turn to left side 4. Shape-crescendo or decrescendo or holosystolic? 5. Grade the intensity from 1-6-listen for pitch and quality 6. Associated features-are S1 & S2 normal? Extra sounds (S3 S4)? Timing Systolic- Comes between S1 & S2-with carotid upstroke-valvular disease or physiologic flow murmurs with normal heart valves. Systolic murmurs can be midsystolic (functional murmurs that decrease in intensity with positions that decrease left ventricular volume ex standing, sitting up or straining during valsalva maneuver). 1. Innocent-heard in healthy patients, common. 2. Physiologic-from physiologic changes in metabolism or 3. Pathologic-structural abnormalities in the heart or great vessels. Pansystolic-starts with S1 and stops at S2 no gap-regurgitation across the AV valves Late systolic murmur-starts mid or late systole-Mitral valve prolapse (systolic click) Diastolic-comes between S2 & S1-usually represent valvular heart disease Early diastolic-regurgitation with incompetent semilunar valves Middiastolic-turbulent flow across Crescendo-grows louder (mitral stenosis) Decrescendo-grows softer (aortic regurgitation) Crescendo-decrescendo-rises then falls (aortic stenosis and innocent flow murmurs) Plateau-constant intensity throughout (mitral regurgitation) Location of Maximal Intensity Determined by the site the murmur originates from-ex murmur heard in 2 nd right intercostal space usually originates from the aortic valve Radiation or transmission from PMI Reflects the site of origin, intensity of murmur, direction of blood flow and bone conduction. Ex-murmurs associated with aortic stenosis radiate to the neck in the direction of atrial flow- mitral regurgitation murmur radiates to axilla. Intensity Graded on a 6 point scale-Grade 1-very faint, listener must be “tuned in”, not heard in all positions. Grade 2-quiet but heard immediately after placing stethoscope on chest. Grade 3- Moderately loud. Grade 4- Loud with palpable thrill. Grade 5- Very loud, with thrill. May be heard when stethoscope is partly off chest. Grade 6- very loud with thrill. May be heard with stethoscope completely off chest. *Identical murmurs may be louder in a thin person than a muscular or obese person. Emphysema may diminish intensity of murmurs. Pitch High, medium or low Quality Blowing, harsh, rumbling, musical *Right sides murmurs usually increase with inspiration and left sided murmurs increase with expiration* Special techniques to identify murmurs and heart failure Standing and sitting-standing decreases venous return to the heart and peripheral vascular resistance. Atrial blood pressure, stroke volume and blood volume in the left ventricle decline. Squatting has the opposite effect on vascular and volume changes. These maneuvers help identify 1. Mitral valve prolapse and 2. Distinguish hypertrophic cardiomyopathy from aortic stenosis. Squatting-increase intensity of murmur in aortic stenosis; decrease intensity of murmur in hypertrophic cardiomyopathy. Standing-increase intensity of murmur hypertrophic cardiomyopathy and decrease intensity of murmur if aortic stenosis Valsalva-hypertrophic cardiomyopathy murmur will increase during the “strain phase” due to increased outflow tract obstruction (patient in supine position). This maneuver can also determine severe heart failure-blood pressure remains elevated and there are Korotkoff sounds during the phase 2 strain phase but not during the phase 4 release-this is highly correlated with volume overload and elevated left ventricular end-diastolic pressure and pulmonary capillary wedge pressure (possibly better than BNP at predicting) Isometric Handgrip-increases systolic murmurs (mitral regurgitation, pulmonic stenosis, ventricular septal defect) and diastolic murmurs (aortic regurgitation and mitral stenosis) Transient Arterial Occlusion-compression of b/l arms via blood pressure cuff inflated 20 mm hg greater than peak systolic blood pressure increases certain murmurs (mitral regurgitation, aortic regurgitation and ventricular septal defect). Innocent-heard left 2 nd -4 th interspaces between the left sternal boarder and the apex- minimal radiation-intensity 1-3, pitch-soft to medium-quality- variable, maneuvers- decreases or disappears with sitting Physiologic-similar to innocent-turbulence due to temporary increase in blood flow (anemia, pregnancy, fever, hyperthyroidism) Pathologic- Aortic stenosis-right 2 nd & 3 rd interspaces, radiates to carotids, down the left sternal boarder. Usually loud with a thrill Grade4/6 and above, medium harsh pitch, crescendo-decrescendo, harsh quality, heard best sitting and leaning forward. Most common cause is valve calcification in older adults Hypertrophic cardiomyopathy-Left 3 rd and 4 th interspaces, radiates down left sternal border (NOT to NECK), variable intensity, quality harsh, intensity decreases with squatting and Valsalva release, increases with standing and strain. Usually benign but can progress to syncope, ischemia a fib. And heart failure Pulmonic Stenosis-left 2 nd & 3 rd interspaces. Radiates toward left shoulder and neck, soft to loud intensity, medium pitch, harsh. Congenital disorder valvular stenosis Mitral regurgitation-location apex radiates- left axilla and left sternal boarder, soft to loud (apical thrill), pitch medium to high, harsh quality. Intensity does not change with inspiration. Increases left ventricular preload leading to left ventricular dilation (structural, mitral valve prolapse, endocarditis, rheumatic heart disease, ventricular dilatation). Tricuspid regurgitation-Left 3 rd , 4 th and 5 th , wide radiation, often loud with thrill, pitch high (smaller defects have higher pitch), harsh quality. Congenital abnormality-blood flows from high pressure left ventricle to low pressure right ventricle. Aortic regurgitation-left 2 nd -4 th interspaces radiates to apex if loud, Grade 1-3, High pitch, blowing decrescendo, best heard when sitting leaning forward holding breath. Leads to left ventricular overload. Causes-leaflet abnormalities, aortic pathology (Marfan syndrome), subaortic stenosis, atrial septal defect Mitral stenosis-Apex, no radiation, Grade 1-4, decrescendo low-pitched rumble. Use the bell on the apical impulse with patient left lateral, heard better in exhalation. Most common cause rheumatic fever (causes fibrosis, calcification and thickening of leaflets) · Congestive Heart Failure TIFFANY RAMSEY Peripheral Artery Disease PAD refers to stenotic, occlusive, and aneurysmal disease of the abdominal aorta, its mesenteric and renal branches, and the arteries of the lower extremities, exclusive of the coronary arteries Peripheral artery disease (PAD) is generally defined as atherosclerotic disease distal to the aortic bifurcation, although some guidelines also include the abdominal aorta. Prevalence increases with age, rising from 7% of adults aged 60 to 69 years to 23% of adults 80 years of age and older.4 Detection is doubly important because PAD is both a marker for cardiovascular morbidity and mortality. Risk of death from myocardial infarction and stroke triples in adults with PAD. ● Ask about abdominal, flank, or back pain, especially in older smokers. Is there unusual constipation or distention? An expanding hematoma from an abdominal aortic aneurysm (AAA) may cause symptoms by compressing the bowel, aortic branch arteries, or the ureters ● If there is persisting abdominal pain, ask about any related “food fear,” weight loss, or dark stool.symptoms suggest mesenteric ischemia from arterial embolism, arterial or venous thrombosis, bowel volvulus or strangulation, or hypoperfusion. ● Ask about any pain or cramping in the legs during exertion that is relieved by rest within 10 minutes, called intermittent claudication. The positive likelihood ratio (LR) of spinal stenosis is >6 if the pain is relieved by sitting and bending forward, or if there is bilateral buttock or leg pain ● Ask also about coldness, numbness, or pallor in the legs or feet or loss of hair over the anterior tibial surfaces. Hair loss over the anterior tibiae points to decreased arterial perfusion. “Dry” or brown–black ulcers from gangrene may ensue. Peripheral Artery Disease Warning Signs: 1. Fatigue, aching, numbness, or pain that limits walking or exertion in the legs; if present, identify the location. Ask also about erectile dysfunction. 2. Any poorly healing or non-healing wounds of the legs or feet 3. Any pain present when at rest in the lower leg or foot and changes when standing or supine 4. Abdominal pain after meals and associated “food fear” and weight loss (see Chapter 11) 5. Any first-degree relatives with an AAA Symptom location suggests the site of arterial ischemia: ● buttock, hip: aortoiliac ● erectile dysfunction: iliac–pudendal ● thigh: common femoral or aortoiliac ● upper calf: superficial femoral ● lower calf: popliteal ● foot: tibial or peroneal · Valve Stenosis ELLIE NGUYEN · Arterial/Venous Insufficiency REBECCA BROWN Chapter 10 Breast/Axillae Assessment The Breast A thorough examination of the breasts includes careful inspection for skin changes, symmetry, contours, and retraction in four views. Inspect: Arms at side: note the appearance of the skin, color, thickening of the skin, pores. Inspect size and symmetry of the breasts. Some differences in the size of the breasts and areolae are common and usually normal.Contour of the breasts. Look for changes such as masses, dimpling, or flattening. Compare one side with the other.The characteristics of the nipples, including size and shape, direction in which they point, any rashes or ulceration, or any discharge. Arms Over Head: Hands Pressed Against Hips; Leaning Forward. To bring out dimpling or retraction that may otherwise be invisible, ask the patient to raise her arms over her head, then press her hands against her hips to contract the pectoral muscles. Inspect the breast contours care- fully in each position. If the breasts are large or pendulous, it may be useful to have the patient stand and lean forward, ), supported by the back of the chair or the examiner’s hands. Palpate: Palpation is best performed when the breast tissue is flattened. The patient should be supine. Palpate the rectangular area extending from the clavicle to the inframammary fold or bra line, and from the midsternal line to the posterior axillary line and well into the axilla to ensure that you examine the tail of the breast. A thorough examination takes at least 3 minutes for each breast. Palpate in small, concentric circles applying light, medium, and deep pressure at each examining point. Press more firmly to reach the deeper tissues of a large breast. Examine the entire breast, including the periphery, tail, and axilla. Examining the lateral portion of the breast. To examine the lateral portion of the breast, ask the patient to roll onto the opposite hip, placing her hand on her forehead but keeping the shoulders pressed against the bed or examining table. This flattens the lateral breast tissue. Begin palpation in the axilla, moving in a straight line down to the bra line, then move the fingers medially and palpate in a vertical strip up the chest to the clavicle. Continue in verti- cal overlapping strips until you reach the nipple, then reposition the patient to flatten the medial portion of the breast. Examining the medial portion of the breast. To examine the medial portion of the breast, ask the patient to lie with her shoulders flat against the bed or examining table, placing her hand at her neck and lifting up her elbow until it is even with her shoulder (Fig. 10-13). Palpate in a straight line down from the nipple to the bra line, then back to the clavicle, continuing in vertical over- lapping strips to the mid-sternum. Examine the breast tissue carefully for: Consistency of the tissues. Normal consistency varies widely, depending on the proportions of firmer glandular tissue and soft fat. Physiologic nodularity may be present, increasing before menses. Note the firm inframammary ridge, which is the transverse ridge of compressed tissue along the lower margin of the breast, especially in large breasts. This ridge is sometimes mistaken for a tumor. Tenderness that may occur prior to menses. Nodules. Palpate carefully for any lump or mass that is qualitatively different from or larger than the rest of the breast tissue. This is sometimes called a dominant mass that may be pathologic when evaluated by mammogram, aspiration, or biopsy. Assess and describe the characteristics of any nodule Location—by quadrant or clock, with centimeters from the nipple Size—in centimeters Shape—round or cystic, disc-like, or irregular in contour Consistency—soft, firm, or hard Delimitation—well circumscribed or not Tenderness Mobility—in relation to the skin, pectoral fascia, and chest wall. Gently move the breast near the mass and watch for dimpling. The Axillae Although the axillae may be examined with the patient lying down, a sitting position is preferable. Inspect: Inspect-skin, rash, infection, unusual pigment. Palpate: Palpate- To examine the axilla, ask the patient to relax with the arm down and warn the patient that the examination may be uncomfortable. Support the patient’s wrist or hand with your hand. Cup together the fingers of your hand and reach as high as you can toward the apex of the axilla. Place your fingers directly behind the pectoral muscles, pointing toward the midclavicle. Now press your fingers in toward the chest wall and slide them downward, trying to palpate the central nodes against the chest wall. Of the axillary nodes, the central nodes are most likely to be palpable. If the central nodes feel large, hard, or tender, or if there is a suspicious lesion in the drainage areas for the axillary nodes, palpate for the other groups of axillary lymph nodes: ■ Pectoral nodes—grasp the anterior axillary fold between your thumb and fingers, and with your fingers, palpate inside the border of the pectoral muscle. ■ Lateral nodes—from high in the axilla, feel along the upper humerus. ■ Subscapular nodes—step behind the patient and, with your fingers, feel inside the muscle of the posterior axillary fold. ■ Infraclavicular and supraclavicular nodes—Also re-examine the infraclavicular and supraclavicular nodes · Normal VS. Abnormal Findings and Interpretation NICOLE JOHNSOn Breast Cancer Self-Breast Examination ● The BSE is best timed 5 to 7 days after menses, when hormonal stimulation of breast tissue is low. ● Masses, nodularity, and change in color or inflammation, especially in the incision line (mastectomy), suggest recurrence of breast cancer. Patient Instructions for the Breast Self-Examination— American Cancer Society Lying supine- ● Lie down with a pillow under your right shoulder. Place your right arm behind your head. ● Use the finger pads of the three middle fingers on your left hand to feel for lumps in the right breast. The finger pads are the top third of each finger. Make overlapping, dime-sized circular motions to feel the breast tissue. ● Apply three levels of pressure in each spot: light, medium, and firm, using firmer pressure for tissue closest to the chest and ribs. A firm ridge in the lower curve of each breast is normal. Standing- ● While standing in front of a mirror with your hands pressing firmly down on your hips, look at your breasts for any changes of size, shape, contour, or dimpling, or redness or scaliness of the nipple or breast skin. (Then pressing down on the hips position contracts the chest wall muscles and enhances any breast changes.) ● Examine the breast in an up-and-down or “strip” pat- tern. Start at an imaginary straight line under the arm, moving up and down across the entire breast, from the ribs to the collarbone, until you reach the middle of the chest bone (the sternum). Remember how your breast feels from month to month. ● Repeat the examination on your left breast, using the finger pads of the right hand. ● If you find any masses, lumps, or skin changes, see your clinician right away. ● Examine each underarm while sitting up or standing and with your arm only slightly raised so you can easily feel in this area. Raising your arm straight up tightens the tissue in this area and makes it harder. Chapter 11 and Chapter 15 · Abdominal/Peritoneal/Rectal Assessment and Modification for Age STACEY WARD · Normal VS. Abnormal Findings and Interpretation JANNINA DIAZ · Pancreatitis JENN RISNER · Peptic Ulcer Disease CATHY LEE Peptic Ulcer Disease - Cathy Lee ● Health history ○ Ask about any vomitus - ask specifically if the vomitus contains aby blood, and quanify the amount ○ Brownish or blackish vomitus with a “coffee grounds” appearance suggests blood altered by gastric acid ○ Coffee ground emesis or red blood (hematemesis) → hematemesis may accompany PUD ● · GERD PAYAL PATEL Appendicitis CH 11 pg 454 For descriptive purposes, the abdomen is often divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants (Fig. 11-2). Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric or suprapubic Examine the abdomen, moving in a clockwise rotation; several organs are often palpable. Exceptions are the stomach and much of the liver and spleen which lie high in the abdominal cavity close to the diaphragm, where they are protected by the thoracic ribs beyond the reach of the palpating hand. The dome of the diaphragm lies at about the fifth anterior intercostal space. Right upper quadrant Liver, gallbladder, pylorus, duodenum, hepatic flexure of colon, and head of pancreas Left upper quadrant Spleen, splenic flexure of colon, stomach, body and tail of pancreas, and transverse colon Left lower quadrant Sigmoid colon, descending colon, left ovary Right lower quadrant Cecum, appendix, ascending colon, right ovary Visceral pain occurs when hollow abdominal organs such as the intestine or biliary tree contract unusually forcefully or are distended or stretched (Fig. 11-7). Solid organs such as the liver can also become painful when their capsules are stretched. Visceral pain may be difficult to localize. It is typically palpable near the midline at levels that vary according to the structure involved, as illustrated on the next page. Ischemia also stimulates visceral pain fibers. Visceral periumbilical pain suggests early acute appendicitis from distention of an inflamed appendix. It gradually changes to parietal pain in the RLQ from inflammation of the adjacent parietal peritoneum. For pain disproportionate to physical findings, suspect intestinal mesenteric ischemia In emergency rooms, 40% to 45% of patients have nonspecific pain, but 15% to 30% need surgery, usually for appendicitis, intestinal obstruction, or cholecystitis.6 RLQ pain or pain that migrates from the periumbilical region, combined with abdominal wall rigidity on palpation, is suspicious for appendicitis. In women, consider pelvic inflammatory disease, ruptured ovarian follicle, and ectopic pregnancy. Combining signs with laboratory inflammatory markers and CT scans markedly reduces misdiagnosis and unnecessary surgery. Parietal pain originates from inflammation of the parietal peritoneum, called peritonitis. It is a steady, aching pain that is usually more severe than visceral pain and more precisely localized over the involved structure. It is typically aggravated by movement or coughing. Patients with parietal pain usually prefer to lie still · Diverticulitis MORGAN ROGERS · Hepatitis LYNN DUKES Viral Hepatitis: Risk Factors, Screening, and Vaccination. The best strategy for preventing infection and transmission of hepatitis A and B is vaccination. Also, educate patients about how the hepatitis viruses spread and behavioral strategies to reduce the risk of infection. Screen high-risk groups for hepatitis B. Hepatitis A. Transmission of hepatitis A virus (HAV) is through a fecal– oral route. Fecal shedding followed by poor hand washing contaminates water and foods, leading to infection of household and sexual contacts. Infected children are often asymptomatic, contributing to spread of infection. To reduce transmission, advise hand washing with soap and water after bathroom use or changing diapers, and before preparing or eating food. Diluted bleach can be used to clean environmental surfaces. HAV infection is rarely fatal—fewer than 100 deaths occur each year—and usually only in people with other liver diseases; it does not cause chronic hepatitis. CDC Recommendations for Hepatitis A Vaccination ● All children at age 1 year ● Individuals with chronic liver disease ● Groups at increased risk of acquiring HAV: travelers to areas with high endemic rates of infection, men who have sex with men, injection and illicit drug users, individuals working with nonhuman primates, and persons who have clotting factor disorders. The vaccine alone may be administered at any time before traveling to endemic areas. Postexposure Prophylaxis.Healthy unvaccinated individuals should receive either a hepatitis A vaccine or a single dose of immune globulin (preferred for those ≥age 40 years) within 2 weeks of being exposed to HAV. These recommendations apply to close personal contacts of persons with confirmed HAV, coworkers of infected food handlers, and staff and attendees (and their household members) of child care centers where HAV has been diagnosed in children, staff, or households of attendees. Hepatitis B. Hepatitis B virus (HBV) infection is a more serious threat than infection with hepatitis A. The fatality rate for acute infection can be up to 1% and HBV infection can become chronic. Approximately 95% of infections in healthy adults are self-limited, with elimination of the virus and development of immunity. Risk of chronic HBV infection is highest when the immune system is immature—chronic infection occurs in 90% of infected infants and 30% of children infected before age 5 years. About 15% to 25% of those with chronic HBV infection die from cirrhosis or liver cancer, accounting for nearly 3,000 deaths each year in the United States. Most persons with chronic infection are asymptomatic until the onset of advanced liver disease. Screening. The USPSTF recommends screening for HBV in persons at high risk for infection (grade B), including those born in countries with a high endemic prevalence of HBV infection, persons with HIV, injection drug users, men who have sex with men, and household contacts or sexual partners of HBV-infected persons. The CDC recommends screening all pregnant women, ideally in the first trimester, and universal vaccination for all infants beginning at birth. For adults, vaccine recommendations also target high-risk groups, including those in high-risk settings (see below). CDC Recommendations for Hepatitis B Vaccination: High-Risk Groups and Settings ● Sexual contacts, including sex partners of hepatitis B surface antigen-positive persons, people with more than one sex partner in the prior 6 months, people seeking evaluation and treatment for sexually transmitted infections, and men who have sex with men ● People with percutaneous or mucosal exposure to blood, including injection drug users, household contacts of antigen-positive persons, residents and staff of facilities for developmentally disabled, health care workers, and people on dialysis ● Others, including travelers to endemic areas, people with chronic liver disease and HIV infection, and people seeking protection from hepatitis B infection ● All adults in high-risk settings, such as sexually transmitted disease (STD) clinics. HIV testing and treatment programs, drug-abuse treatment programs and programs for injection drug users, correctional facilities, programs for men having sex with men, chronic hemodialysis facilities and end-stage renal disease programs, and facilities for people with developmental disabilities. Hepatitis C. There is no vaccination for hepatitis C, so prevention targets counseling to avoid risk factors. Screening should be recommended for high-risk groups. Hepatitis C virus (HCV), transmitted mainly by percutaneous exposures, is the most prevalent chronic bloodborne pathogen in the United States. Anti-HCV antibody is detectable in just under 2% of the population, though prevalence is markedly increased in high-risk groups, particularly injection drug users.45 Additional risk factors for HCV infection include blood transfusion or organ transplantation before 1992, transfusion with clotting factors before 1987, hemodialysis, health care workers with needle stick injury or mucosal exposure to HCV-positive blood, HIV infection, and birth from an HCV-positive mother. Sexual transmission is rare. Hepatitis C becomes a chronic illness in over 75% of those infected and is a major risk factor for subsequent cirrhosis, hepatocellular carcinoma, and need for liver transplant for end-stage liver disease.45–47 However, the majority of persons with chronic HCV are unaware of being infected. Response to antiviral therapy (undetectable HCV RNA 24 weeks after completing treatment) ranges from 40% to over 90% depending on the viral genotype and the combination of drugs used for treatment. Consequently, the USPSTF has concluded that screening for hepatitis C infection is of moderate benefit for per- sons at high risk for infection as well as those born between 1945 and 1965 (grade B). · IBS JACKELINE CONDE · Incontinence HOLLY MCCORD INCONTINENCE Females: Due to weakness of the pelvic floor muscle. Risk factors: advanced age, prior pelvic surgery or trauma, childbirth. Clinical conditions like obesity, diabetes, MS and Parkinson’s disease. Chronically increased intra-abdominal pressure r/t COPD, constipation or obesity. Medication Risk Factors: anticholinergics, a-adrenergic blockers. Pelvic organs are supported by muscle, ligaments and endo pelvic fascia (pelvic floor) which all aide in continence. Loss of urethral support = stress incontinence. Childbirth predisposes to rectoceles and enteroceles. RCT in 2012: USPSTF found that estrogen plus progestin and estrogen alone increased risk for urinary incontinence. Stress incontinence = muscle weakness due to aging, vaginal deliveries, neuro conditions. Assess pelvic floor muscle for strength during pelvic exam: fingers are spread against the vaginal walls-ask patient to squeeze. Snug compression of fingers 3 seconds or greater = full strength. Ask patient to cough or bear down to assess for urinary leakage. Increased intraurethral pressure helps prevent incontinence. Voluntary control of bladder depends on higher centers in the brain and motor/sensory pathways connecting the brain and reflex arcs of sacral spinal cord. Ask if the patient is leaking small amounts of urine due to increased intra-abdominal pressure from coughing, sneezing, laughing or lifting or following urge to void is there and involuntary loss of large amounts of urine. Urge incontinence-urgency followed by involuntary leakage due to uncontrolled detrusor contractions that overcome urethral resistance. Overflow incontinence- neurologic disorders or anatomic obstruction from pelvic organs or prostate, decreased bladder emptying until bladder becomes over distended Functional incontinence- arises from impaired cognition, musculoskeletal problems or immobility Mixed incontinence= stress & urge incontinence combined. Colon/ Anorectal cancer: Grant Freiberg Ch11, pg. 468 Screening for colorectal cancer Epidemiology: 3rd most frequently diagnosed cancer in MEN AND WOMEN and the 3rd leading cause of cancer deaths each year in the US. The lifetime risk of diagnosis is about 5%, while the lifetime risk for dying of colorectal cancer is about 2% Incidence rates steadily decreasing due to changes in risk factors, such as decreased tobacco use and increased screenings. Risk factors: The strongest risk factors include increased age, hx of colorectal cancer, family history of colorectal neoplasms, long-standing inflammatory bowel disease, and adenomatous polyps. Weaker risk factors include male sex, African Americans, tobacco use, excessive alcohol use, red meat consumption, and obesity **All are risk factors, but the STRONGEST LINK WILL ALWAYS BE GENETIC IN NATURE** 90% of new cases and 94% of deaths occur in population over 50 years of age Prevention: The MOST EFFECTIVE prevention strategy is to screen for and remove pre-cancerous adenomatous polyps. Physical activity, ASA and NSAIDs, and postmenopausal combined hormone replacement therapy are associated with decreased risk of colorectal cancer. ** -The USPSTF recommends against ASA and NSAIDS for prevention in average-risk populations because of potential GI issues, hemorrhagic CVA, and renal impairment. - Also, increased hormonal replacement therapy is associated with an increased risk of developing breast cancer, CV events (like MI), and thromboembolism. ** there has been NO CONVINCING EVIDENCE that dietary changes or supplements can prevent colorectal cancer** Screening tests: - Stool tests that detect occult fecal blood- test include immunochemical tests, high-sensitivity guaiac-based tests, and tests that detect abnormal DNA - Endoscopic tests are also usedsigmoidoscopy warrants further evaluation via colonoscopy** Guidelines: (page 469) Screening recommendations include: Ages 50-75 years High sensitivity fecal occult blood test (FBOT) annually Sigmoidoscopy every 5 years Screening colonoscopy every 10 years Ages 76-85 years Do not screen routinely Benefits small when compared to risks associated with colonoscopy Use individual decision making if initial screening Ages 85 or older DO NOT SCREEN! **Higher-risk persons, based on personal history of colorectal neoplasia or long-standing inflammatory bowel disease, or a family history of colorectal neoplasia, should begin screening at a younger age, usually with colonoscopy, and get more frequent testing than average-risk adults** Chapter 13 · Male Genitalia Assessment and Modification for Age KYNA HERNANDEZ · Normal VS. Abnormal Findings and Interpretation CHRISTI DIPAOLO · Prostate Issues and Cancer TIFFANY SCHWARTZ Prostate Issues and Cancer Prostate Cancer: 2nd leading cause of cancer of cancer in the US. Risk Factors:<40, African American men, genetics, (potentially exposure to agent orange, diets high in animal fats, smoking, obesity. Prevention: PSA TESTING (normal levels are >4.0). False positives are caused by BPH, prostate infections, and ejaculation. Digital Rectal Exam: finds palpable nodules in the posterior and lateral areas of the prostate gland. It is unable to detect cancer in the anterior and central areas of the gland. The exam is performed by having the pt bear down and note any irregularities or nodules. Sweep your finger carefully over the prostate gland, identifying it’s lateral lobes and the groove of the median sulcus. Note shape, mobility, and consistency of the prostate. Screening: Patients with average risk should begin screening between 50-55 years of age. PSA screening should continue every 1-2 years. High risk screening: should start at 40-45 years of age · STI ANNE KAMAU To assess for STIs, ask about any discharge from the penis, dripping or staining of the underwear. If the discharge is present, clarify the amount, color and any fever, chills rash or associated symptoms. Gonorrhea- yellow penile discharge Chlamydia- white discharge. Genital warts-single or multiple papules or plaques of variable shapes. May be raised, flat or cauliflower like caused by HPV and can take weeks to months for incubation and the infected contact may not have visible warts. Can rise on penis, scrotum, groin, thighs, and anus, usually asymptomatic, occasionally cause itching and pain and may disappear without treatment. Genital herpes simplex- small scattered or grouped vesicles, 1 to 3mm in size on glans or shaft of penis. Appears as erosions if vesicular membrane breaks. It is usually caused by herpes simplex virus and incubation takes 2 to 7 days. Primary episode may be asymptomatic, recurrence is usually less painful of shorter duration. It is associated with fever, malaise, headache, arthralgia, local pain and edema, and lymphadenopathy. Primary syphilis- small red papule that becomes a chancre, a painless erosion up to 2cm in diameter. Base of chancre is clean, smooth and glistening; borders are raised and indurated. Chancre heals between 3 to 8 weeks. Incubation: 9-90 days and is caused by Treponema pallidium. May develop inguinal lymphadenopathy within 7 days; lymph nodes are rubbery, nontender and mobile. 20-30% of patients may develop secondary syphilis while chancre still present suggesting coinfection with HIV. Chancroid- red papule or pustule initially, then forms a painful deep ulcer with raged nonindurated margins; contains necrotic exudate, has a friable base. It is caused by haemophilus ducreyi with incubation of 3-7 days after exposure. Painful inguinal adenopathy with suppurative buboes in 25% of the patients · Testicular Disorders and Cancer JAMIE KERN · Erectile Dysfunction JEANETTE CARPENTER ● Erectile dysfunction, or the inability to maintain an erection, affects approximately 50% of older men. Vascular causes are the most common, from both atherosclerotic arterial occlusive disease and corpora cavernosa venous leak. Chronic diseases such as diabetes, hypertension, dyslipidemia, and smoking, as well as medication side effects, all contribute to the prevalence of erectile dysfunction ● Men with screen-detected cancers who undergo aggressive treatment with surgery or radiation frequently leads to complications such as erectile d · Menstruation JAMIE CHAMBERLIN · Cervical Disorders and Cancer SHEILA RAMAS Abnormalities of the cervix: p.599-600 As estrogen stimulation increases during adolescence, all or part of this columnar epithelium is transformed into squamous epithelium by a process termed metaplasia. This change may block the secretions of columnar epithelium and cause retention cysts, also called nabothian cysts. This appear as translucent nodules on the cervical surface and have no pathologic significance. A cervical polyp usually arises from the endocervical canal, becoming visible when it protrudes through the cervical os. It is bright red, soft, and rather fragile. When only the tip is seen, it cannot be differentiated clinically from a polyp originating in the endometrium. Polyps are benign but may bleed Mucopurulent cervicitis - produces purulent yellow drainage from the cervical os, usually from the Chlamydia trachomatis, Neisseria gonorrhoeae, or herpes infection. These infections are sexually transmitted and may occur without signs and symptoms Carcinoma of the cervix - begins in an area of metaplasia. In its earliest stages, it cannot be distinguished from a normal cervix. In later stages, an extensive, irregular, cauliflower-like growth may develop. Early frequent intercourse, multiple partners, smoking, and infection with HPV increase the risk for cervical cancer Fetal exposure to diethylstilbestrol (DES) - daughters of women who took DES during pregnancy are greatly increased risk for several abnormalities, including 1.) columnar epithelium that covers most or all of the cervix, 2.) vaginal adenosis, i.e. extension of the epithelium to the vaginal wall, and 3.) a circular collar or ridge of tissue, of varying shapes, between the cervix and vagina. Much less common is an otherwise rare carcinoma of the upper vagina Chapter 18 · Newborn/Infant/Pediatric Assessment and Modification for Age VIOLET FLOWER · Normal VS. Abnormal Findings and Interpretation TRACY RUTZ · Newborn Skin Disorders CLARIS AYUK · Birthmarks CELESTE MARIE Childhood Vaccinations Childhood immunizations are part of health promotion. Heralded as the most significant clinical achievement in public health worldwide. Check for yearly updates with CDC and AAP. Vaccine-preventable diseases: Cervical Cancer Approximately 90%-95% of recipients of a single dose of certain live vaccines administered by injection at the recommended age (i.e., measles, rubella, and yellow fever vaccines) develop protective antibodies, generally within 14 days of the dose. For varicella and mumps vaccines, 80%-85% of vaccines are protected after a single dose. However, because a limited proportion (5%-20%) of measles, mumps, and rubella (MMR) or varicella vaccines fail to respond to 1 dose, a second dose is recommended to provide another opportunity to develop immunity. Of those who do not respond to the first dose of the measles component of MMR or varicella vaccine, 97%-99% respond to a second dose -immunocompromised patients sot prerequisites for vaccinating persons who appear to be healthy. The provider should ask the parent or guardian if the child is ill. If the child has a moderate or severe illness, the vaccination should be postponed. * CDC -a personal or family history of seizures is a precaution for MMRV vaccine. Recommended for all children, unless patient can not safely receive the vaccine. Recommended for children with certain health or lifestyle conditions that put them at greater risk for serious disease. Vaccine should be given if a child is catching up on missed vaccines Children not at an increased risk may get the vaccine after speaking with provider. · Developmental Milestones JENNIFER WASHINGTON · Tanner Staging MEGHAN HENRY Tanner Staging- also known as Sexual Maturity Rating (SMR), is an objective classification system that providers use to document and track the development and sequence of secondary sex characteristics of children during puberty. Sexual Maturity Ratings in Girls: Breasts Generally, over a four year period, the breasts progress through five stages, called Tanner stages or Tanner sex maturity rating stages. The stages are described below: Chapter 19 · Pregnancy and Assessment SARAH CLARK CHAPTER 19 - Pregnancy and Assessment Physiologic Hormonal Changes: · Estrogen - promotes endometrial growth that supports the early embryo - stimulates enlargement of pituitary gland increases prolactin output from anterior lobe = readies breast tissue for lactation - contributes to hypercoagulable state increased risk for venous thrombosis (4-5 times greater in pregnancy) · Progesterone - levels increase throughout pregnancy - increases tidal volume and alveolar minute ventilation (respiratory rate remains constant) = results in respiratory alkalosis and subjective SOB - Relaxes tone in ureters and bladder = causes hydronephrosis and increased risk of bacteriuria. - Increased levels of progesterone and estradiol lower esophageal sphincter tone = results in gastroesophageal reflux · Human chorionic gonadotropin (HCG) - 5 variant subtypes: o 2 types produced in placenta – support progesterone synthesis in the corpus luteum, stabilizes endometrium to prevent loss of pregnancy o Other 3 types are produced by certain cancers and the pituitary gland · Placental growth hormone - Influences placental growth, development of preeclampsia - May contribute to insulin resistance and gestational diabetes · Thyroid function changes -increase in thyroid-binding globulin due to rising estrogen levels and stimulation of TSH receptors by HCG = slight increase in serum free T3 ,T4 and decrease in TSH levels (transient hyperthyroidism – considered physiologic) · Relaxin - secreted by corpus luteum and placenta - involved in remodeling of reproductive tract connective tissue to facilitate delivery - increases renal hemodynamics - increases serum osmolality - does not affect peripheral joint laxity during pregnancy *Weight gain and shifts in center of gravity contribute to lumbar lordosis and musculoskeletal strain. · Erythropoietin - Levels increase during pregnancy - Raises erythrocyte mass - Plasma volume increases which causes hemodilution and physiologic anemia – protects against blood loss during birth - Cardiac output increases, systemic vascular resistance decreases = results in net fall in BP (more prominent in 2nd trimester, returns to normal in 3rd trimester) · Basal metabolic rate - Increased 15-20% during pregnancy - Daily energy demand is increased, requiring additional kcal/day o 1st trimester = additional 85 kcal/day o 2nd trimester = additional 285 kcal/day o 3rd trimester = additional 475 kcal/day Anatomic Changes: · Breasts - Moderately enlarged due to hormonal changes – increased vascularity and glandular hyperplasia, more tender during exam - 3rd month of gestation – breasts become more nodular - Nipples become larger and more - Growth related to muscle cell hypertrophy, increase in fibrous and elastic tissue, and development of blood vessels and lymphatic vessels - Externally palpable by 12-14 weeks - In 2nd trimester, size of fetus pushes uterus into anteverted position – puts pressure on bladder causes frequent voiding - Round ligament pain (felt in lower quadrants) - caused by uterus stretching its own supporting ligaments · Vagina - Increased vascularity causes vagina to look bluish – known as Chadwick sign - Normal secretions may become thick, white and more profuse – known as leukorrhea of pregnancy - Increased glycogen stores causes proliferation of lactobacillus acidophilus = lowers vaginal pH – contributes to higher rates of yeast infections (vaginal candidiasis) · Cervix - Softens ~ 1 month after conception – turns bluish in color. - Hegar sign = palpable softening of the cervical isthmus (portion of uterus that narrows into the cervix) - Mucous plug forms from cervical secretions – protects uterine environment from outside pathogens, expelled as “bloody show” at delivery. · Adnexae - Small nodule/mass on ovary that may be seen on ultrasound – usually benign, disappears by midpregnancy. · External abdomen - Skin stretches – striae gravidarum (stretch marks) and a linea nigra (brownish black vertical stripe along abdomen) may appear. - Rectus abdominis muscles may separate – known as diastasis recti *Common Concerns During Pregnancy and Their Explanations – page 931 The Health History: Prenatal care – focuses on optimizing health and minimizing risk for both mother and fetus. · Goals of initial prenatal visit: o Define health status of mother and fetus o Confirm pregnancy and estimate gestational age o Develop plan for continuing care o Counsel mother about her expectations/concerns · Subsequent visits: o Assess any interim changes in health status of mother and fetus o Review specific physical exam findings r/t pregnancy o Provide counseling and timely preventive screenings Initial Prenatal History: · Confirmation of pregnancy – Ask: o Has patient taken a urine pregnancy test? When? o Last menstrual period (LMP) ? o Has she had an ultrasound to establish dates? *Explain to patient that serum pregnancy tests are rarely required to confirm pregnancy. · Symptoms of pregnancy – Ask: o Has patient missed period? o Breast tenderness? o Nausea or vomiting? o Fatigue? o Urinary frequency? · Concerns and Attitudes Toward Pregnancy – Ask? o How patient feels about the pregnancy? Excited? Concerned? Scared? o Pregnancy planned and desired? o Does patient plan to complete pregnancy to term, terminate, or consider adoption? o Is partner the father? Support from family? *Use open-ended questions and be nonjudgmental; respect diverse families, support patient’s choices. · Current Health and Past Clinical History - Ask patient about current or past medical history - Conditions that may affect pregnancy include: o Abdominal surgeries o Hypertension o Diabetes o Cardiac disorders (including childhood surgeries for congenital heart disease) o Asthma o Hypercoagul - Term deliveries? - Preterm deliveries? - Spontaneous and terminated pregnancies? - How many live births? - Any complications from diabetes, hypertension, preeclampsia, intrauterine growth restriction (IUGR), preterm labor? - Delivery complications? i.e. fetal macrosomia (large baby), fetal distress, emergency interventions - Vaginal delivery, assisted delivery (forceps, vacuum) or C-section? · Risk Factors for Maternal and Fetal Health – Ask: - Tobacco, alcohol or illicit drug use? - Medications, OTC drugs, herbal preparations? - Any toxic exposures at work, home or other settings? - Adequate nutrition? Obese? - Good social support? Adequate income? - Unusual sources of stress at home or work? - History of physical abuse or domestic violence? · Family History – Ask: - Genetic and family history of patient and father of baby (FOB)? - Ethic background of patient and FOB? - Family hx of genetic diseases? (i.e. sickle cell, cystic fibrosis, muscular dystrophy, etc.) - Previous children born with congenital problems? · Plans for Breastfeeding - Educate patient about benefits of breastfeeding o Protects baby from infectious/noninfectious conditions o Protects mother against breast cancer and other conditions *Encouragement from provider and education during pregnancy increases rate and duration of breastfeeding. · Plans for Postpartum Contraception - Initiate discussion early - Postpartum contraception reduces risk of unintended pregnancy and shortened interpregnancy intervals – linked to increased adverse pregnancy outcomes - Plan for contraception depends on: o Patient preference o Clinical history o Decision about breastfeeding Determining Gestational Age and Expected Date of Delivery (EDD): · Accurate dating is best done early: - Helps manage pregnancy appropriately - Establishes time frame for normal progress - Establishes paternity - Timing of screening tests - Track fetal growth - Triaging preterm and postdated (late gestation) labor · To establish gestational age: - Count # of weeks and days from the first day of the LMP - Average length of pregnancy = 40 weeks - If actual date of con - Online calculators (more reliable) · Limitations on pregnancy dating - Patient recall highly variable - LMP affected by hormonal contraceptives, menstrual irregularities, variations in ovulation/atypical cycle lengths *LMP dating should be checked against physical exam markers (i.e. fundal height) -Discrepancies should be clarified by ultrasound. *At end of initial visit: review findings, discuss any tests or screenings that are needed, and reinforce need for regular prenatal care/timing of future visits. Prenatal Visit Schedule: ❖ Monthly appts. until 28 weeks gestation ❖ Biweekly until 36 weeks ❖ Weekly until delivery Physical exam findings at every visit: ❖ Vital signs (especially BP and weight) ❖ Fundal height ❖ Verification of fetal heart rate (FHR) ❖ Determination of fetal position and activity ❖ Urinalysis to assess for infection and proteinuria Health Promotion and Counseling: Nutrition · Take a diet history (assess types of food, frequency, nausea that limits eating) · Review BMI and lab findings (Hct screened for anemia – may reflect nutritional deficiencies, underlying clinical issues, or expected hemodilution as a result of pregnancy) - Recommend prenatal multivitamin: o Folic acid 400 mcg o Vitamin D 600 IU o Iron 27mg o Calcium 1,000mg o Iodine 150-290mcg *Advise patients that excess amounts of fat-soluble vitamins (A, D, E, K) can cause toxicity. · Caution patients on foods to avoid in order to prevent listeriosis: - Unpasteurized milk and foods made with unpasteurized milk - Raw and undercooked seafood, eggs and meat - Refrigerated paté, meat spreads, smoked salmon - Hot dogs, lunch meats, cold cults unless served steaming hot · Fish and shellfish are rich in DHEA – enhances fetal brain development - Recommend two servings per week - Avoid high-mercury fish (shark, swordfish, king mackerel) Weight gain (p. 937) o Meningococcal o Hep B - Vaccines NOT safe during pregnancy: o MMR o Polio o Varicella *All pregnant women should have rubella titers drawn during pregnancy. If nonimmune, they should be immunized after birth. *Check Rh (D) and antibody typing at first prenatal visit, at 28 weeks and at delivery. -Anti-D immunoglobulin should be given to all Rh-negative women at 28 weeks gestation and again w/in 3 days of delivery to prevent sensitization if infant is Rh-D positive. · Exercise during pregnancy – recommend 30 min. of moderate exercise each day. - Psychological benefits - Reduces risk of: o Excessive gestational weight gain o Gestational diabetes o Preeclampsia o Preterm birth o Varicose veins o DVT - May reduce length of labor and complications during delivery - Excessive activity during pregnancy may cause low birth weight. - After 1st trimester, avoid exercise in supine position (causes compression of inferior vena cava, dizziness and decreased placental blood flow) - 3rabor. - Increased risk of spontaneous abortion, fetal death, and fetal digit anomalies - Cessation is goal but any decrease in use is favorable. · Alcohol: - Causes fetal alcohol syndrome – leading cause of preventable mental retardation in the US - No safe dose established - ACOG strongly recommends women abstain throughout pregnancy · Illicit drugs: - Cause significant detrimental effects on fetal development - Pregnant women with addiction should be referred for treatment immediately and screened for HIV, Hep C. · Prescription drug abuse: - Ask patient about use of narcotics, stimulates, benzos, and other prescription drugs · Herbal and unregulated supplements - Poor studies, limited data - May contain toxins that could harm fetus Intimate Partner Violence: - Increased risk during pregnancy -Pre-existing patterns of abuse may intensify -1 in 5 women experience some form of abuse during pregnancy -Associated with delayed prenatal care, low infant birth weight, or even murder of mother and fetus *Watch for nonverbal clues of abuse: -frequent last-minute appt. changes - unusual behavior during visits - partners who refuse to leave the patient during the visit - bruises/other injuries *If patient acknowledges abuse, ask how you can help. -Accept her decision about how to handle the situation safely. Prenatal Lab Screenings · Standard prenatal screening: - Blood type and Rh - Antibody screen - CBC - Rubella titer - Syphilis test - Hep B surface antigen - HIV test - STI screen for gonorrhea and chlamydia - UA w/ culture · Scheduled screenings: · Vaccinations and Laboratory Testing Recommended vaccine is TDAP at 27 to 36 weeks of gestation, regardless of prior vaccine history. Caretakers in direct contact with the infant should also receive Tdap. Inactivated influenza vaccination is indicated in any trimester of pregnancy. Safe Vaccines during pregnancy: Pneumococcal, meningococcal, hep B, Hep A, meningococcal polysaccharide and conjugate, and pneumococcal polysaccharide NOT SAFE during pregnancy: Measle/mumps/rubella, polio, and varicella All pregnant women should have rubella titers drawn during pregnancy and be immunized after birth if found to be nonimmune Check Rh (D) and antibody typing at the first prenatal visit, at 28 weeks, and at delivery. Anti-D immunoglobulin should be given to all Rh-negative women at 28 weeks gestation and again within 3 days of delivery to prevent sensitization if the infant is Rh-d positive. Chapter 20 · Geriatric Assessment LINDAY LOU · Normal VS. Abnormal Findings and Interpretation ERICA LUDWIG · Elder Abuse MERIDETH YARBROUGH · Functional Assessments RACHEL COX · Adult Vaccinations RAASHIADA PORTIER [Show More]
Last updated: 11 months ago
Preview 1 out of 62 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 23, 2020
Number of pages
62
Written in
Additional information
This document has been written for:
Uploaded
Aug 23, 2020
Downloads
1
Views
99

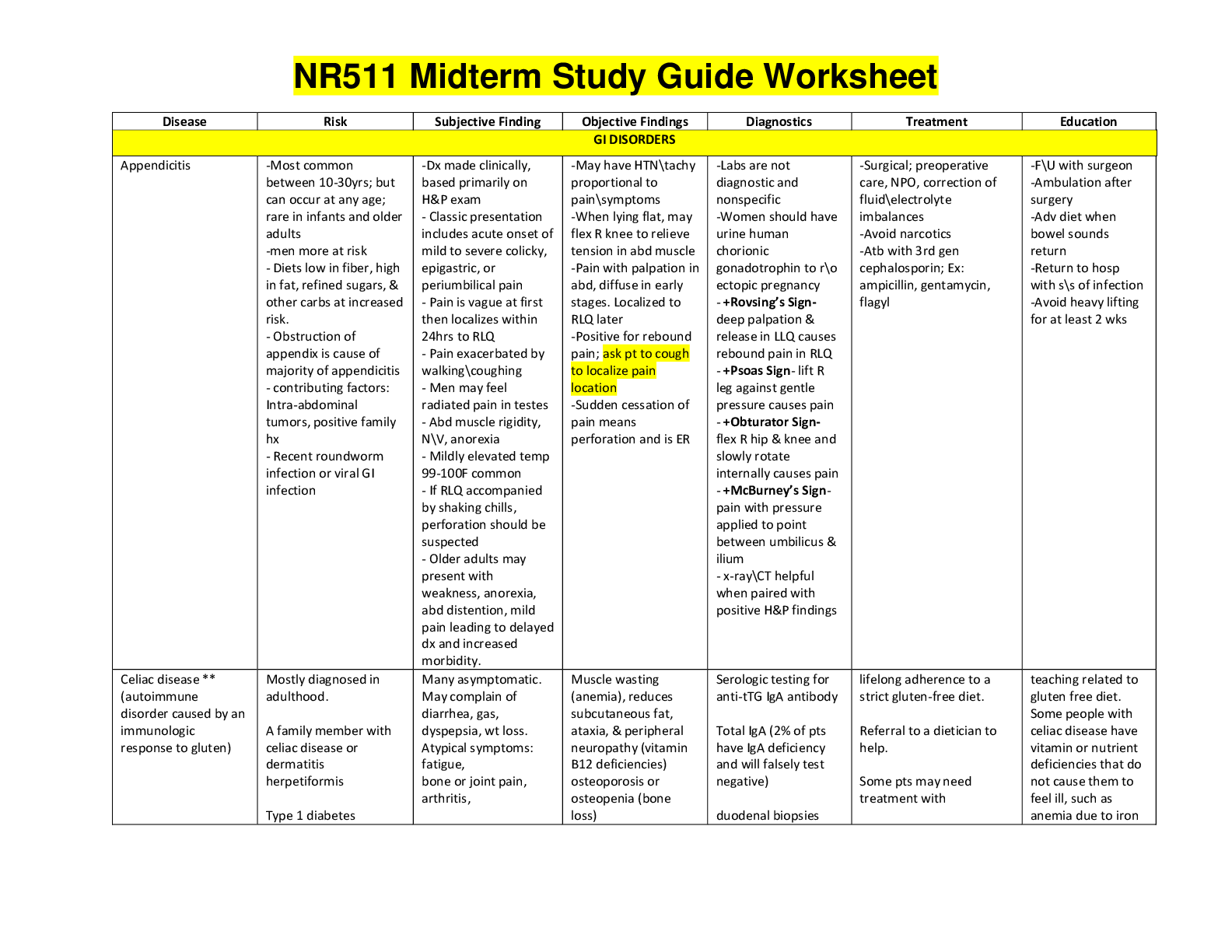
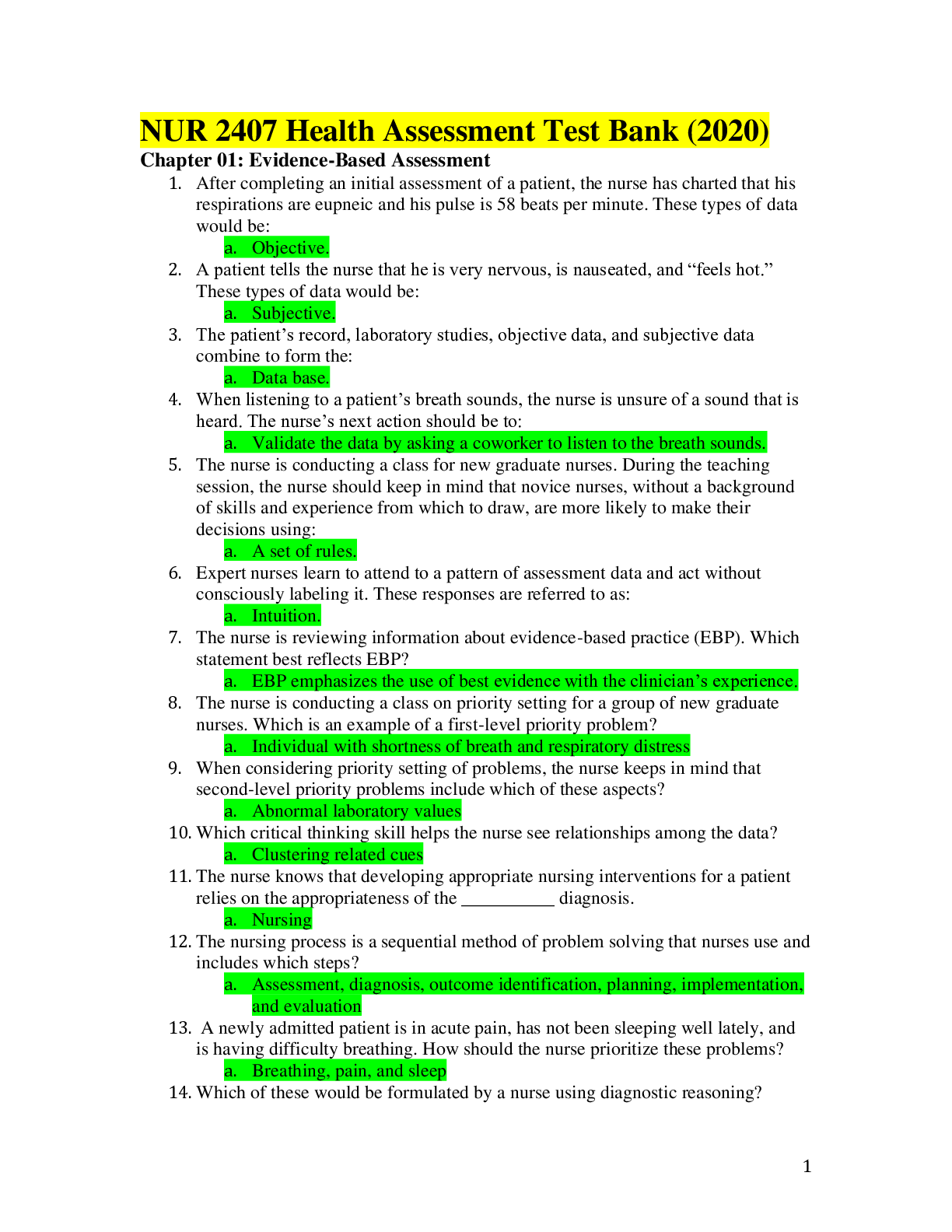
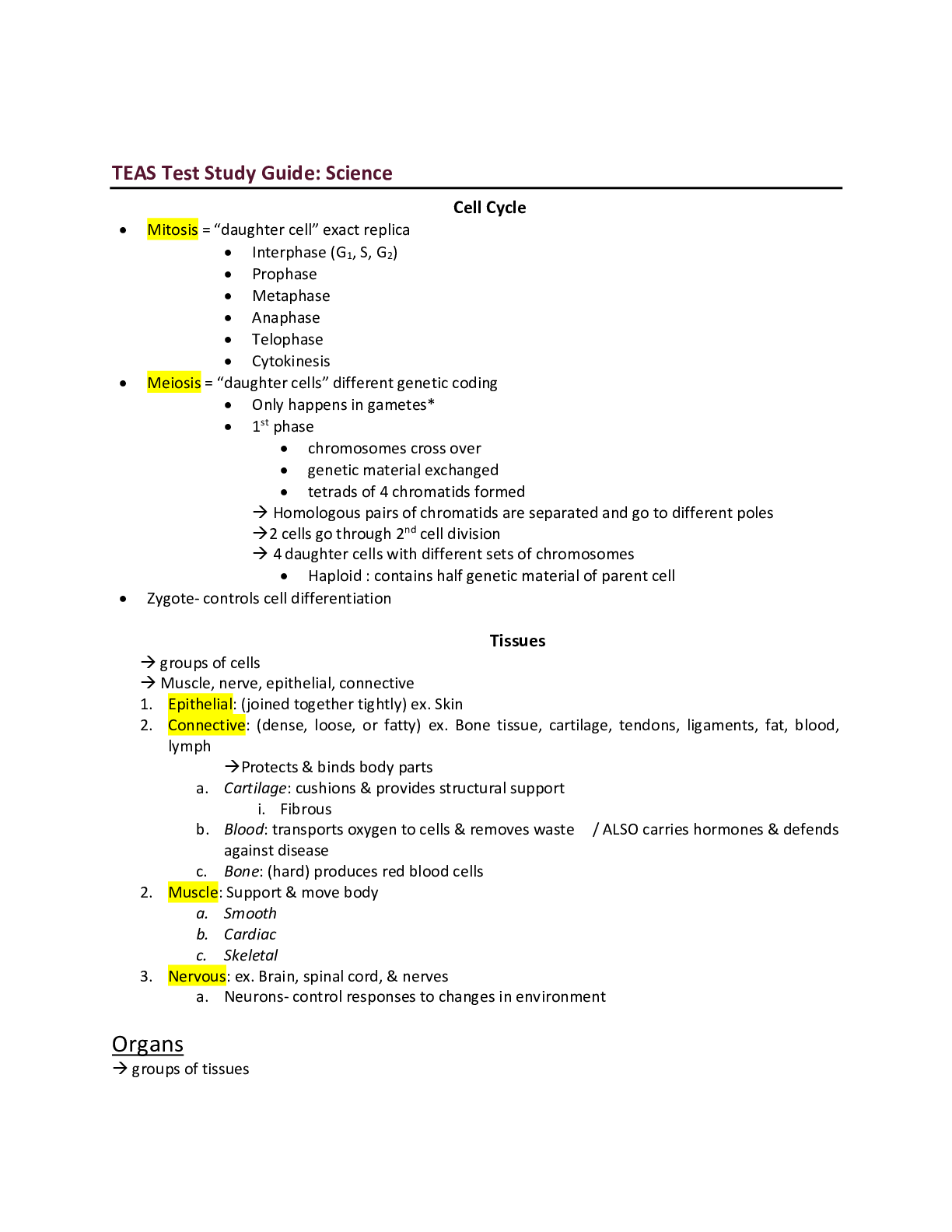
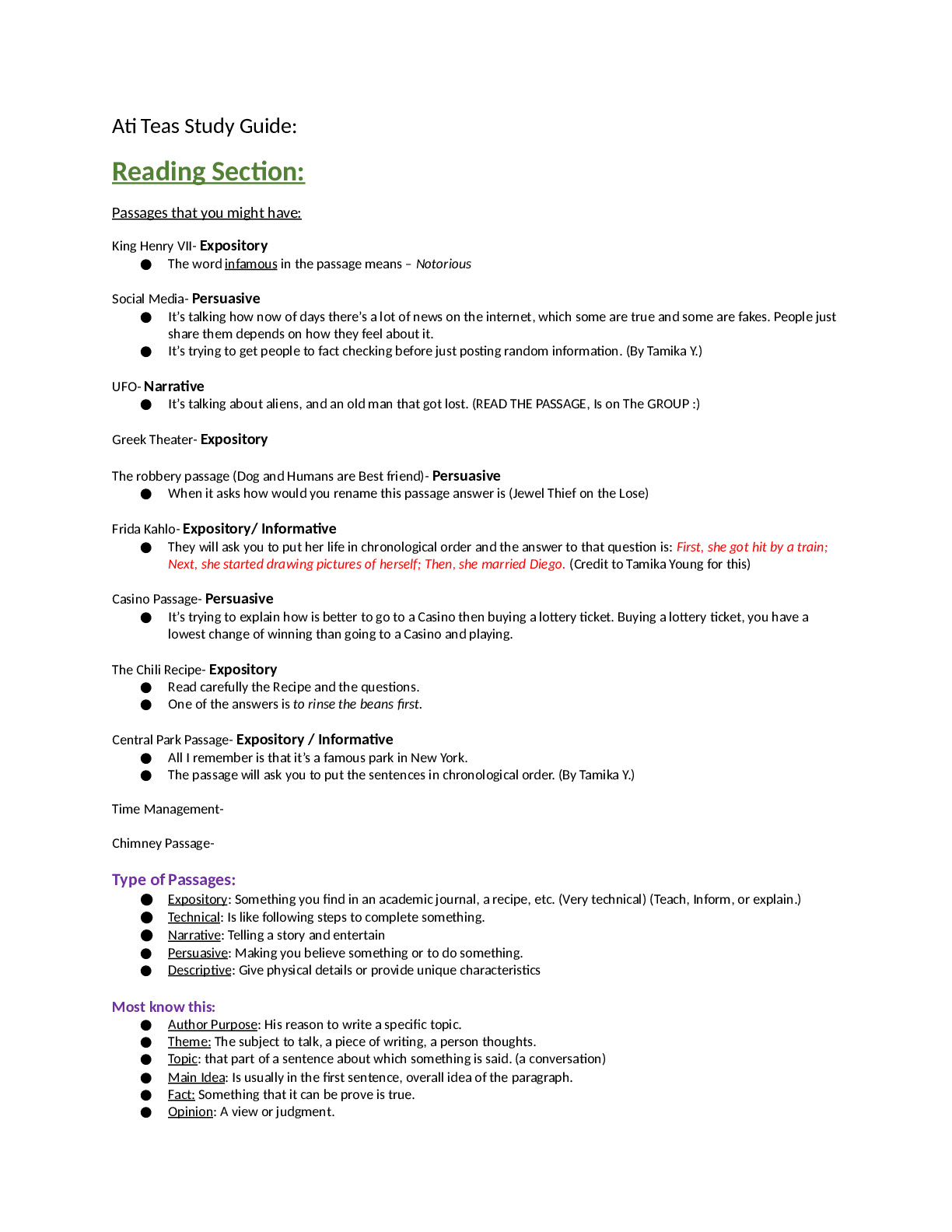

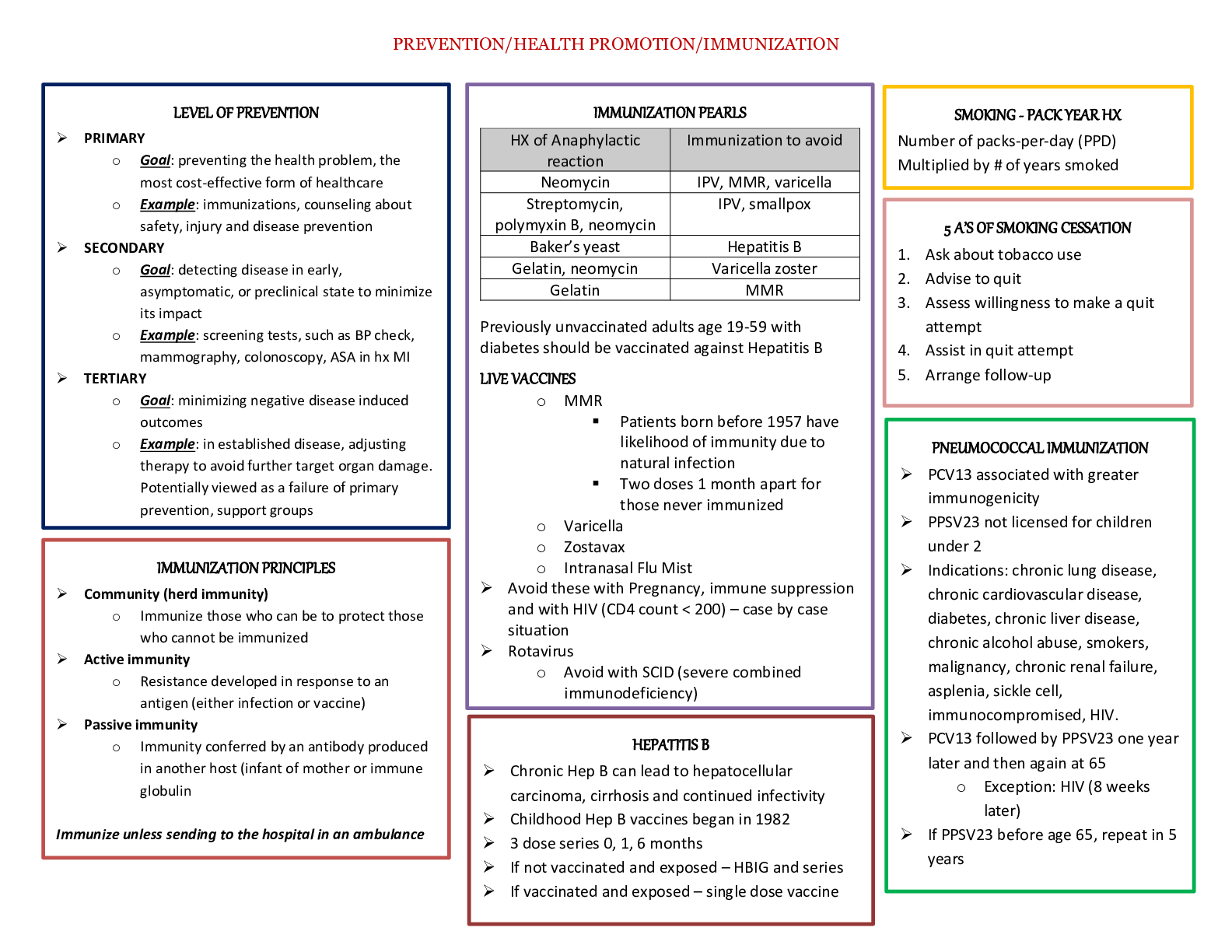
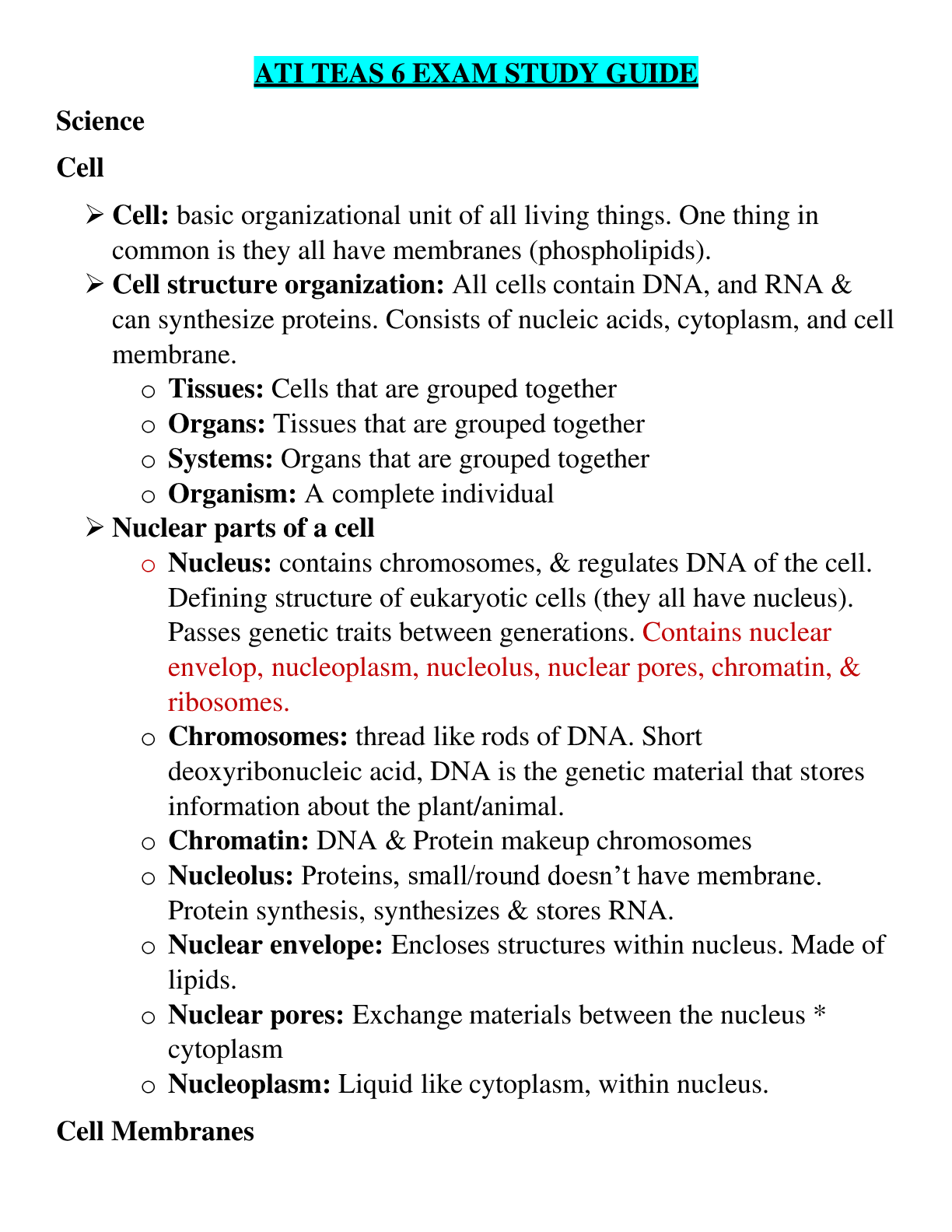
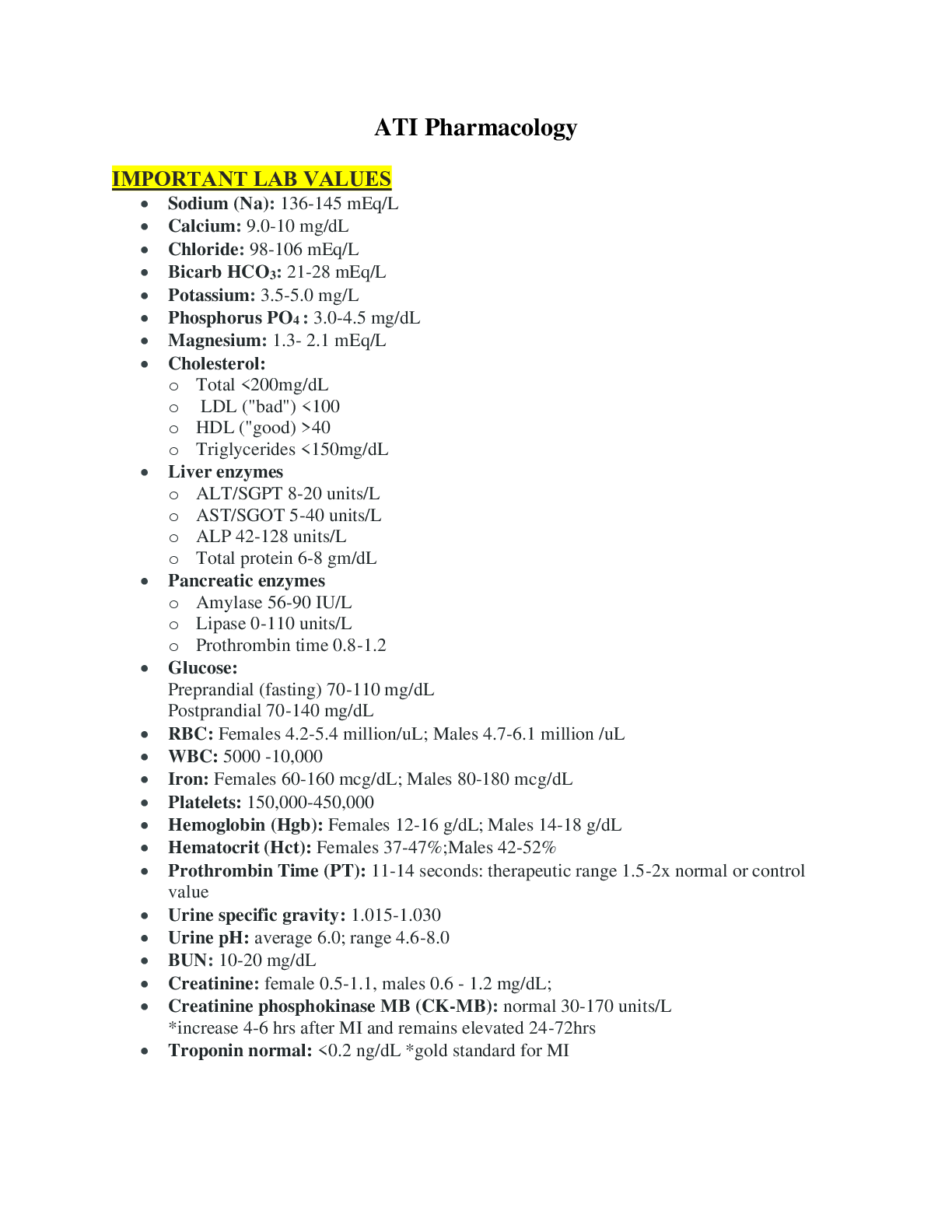

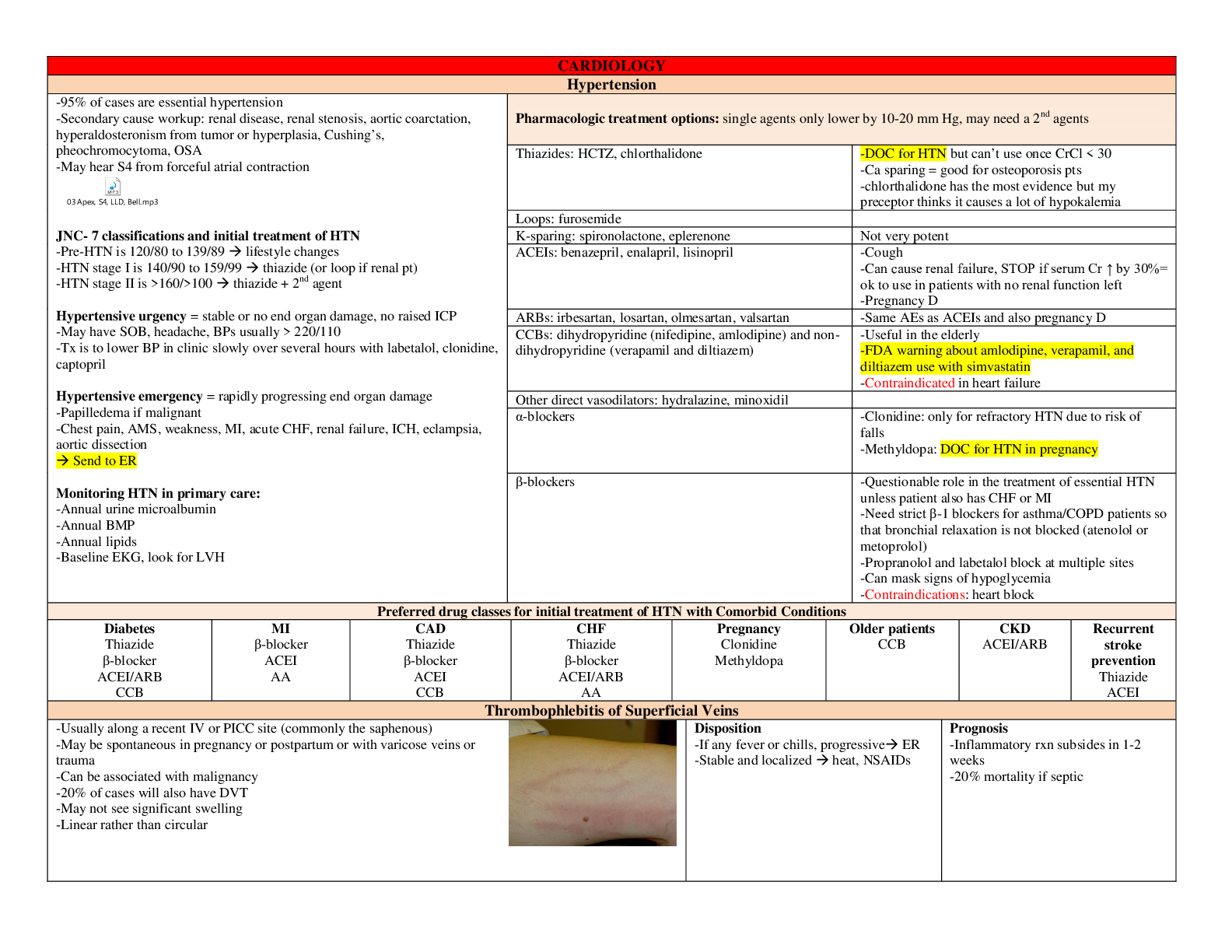
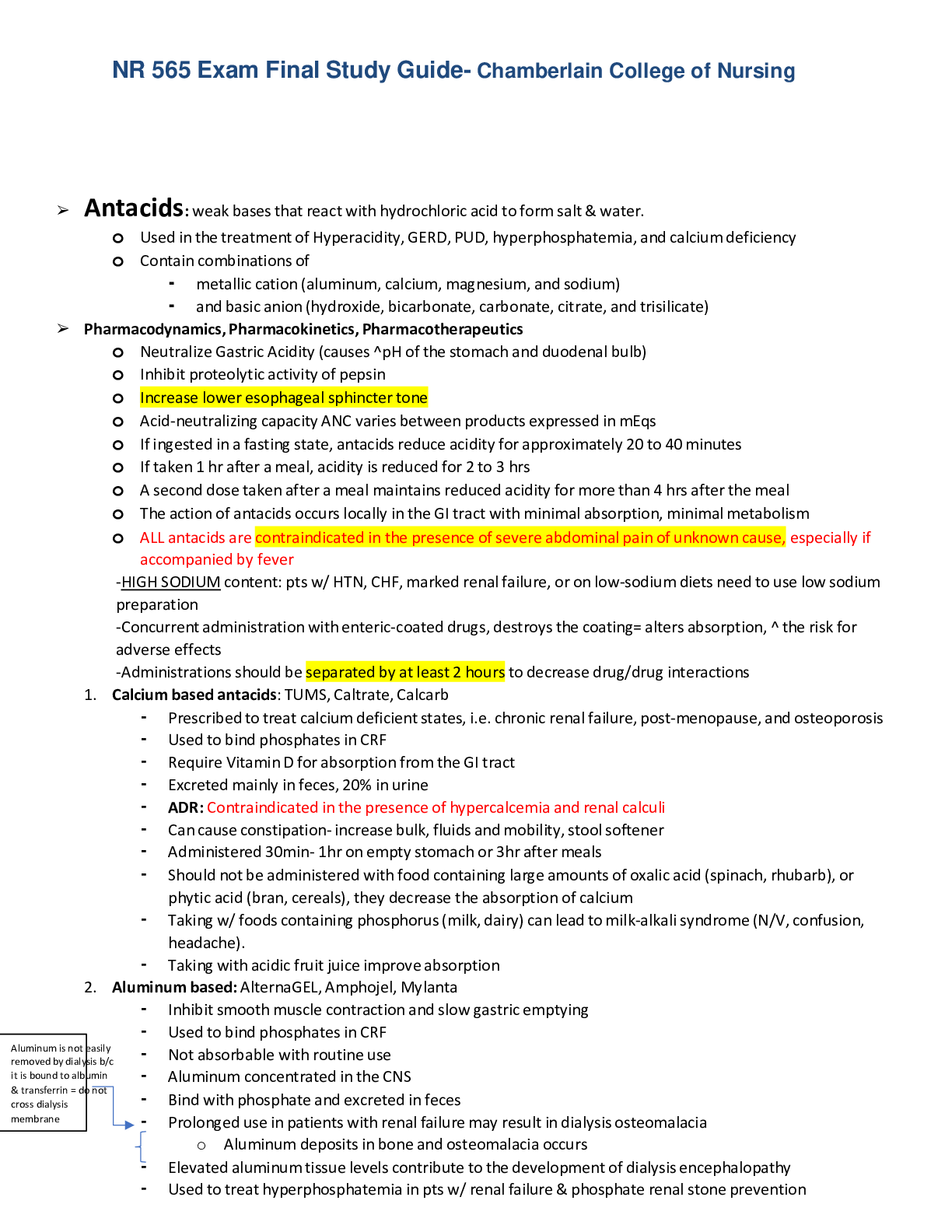
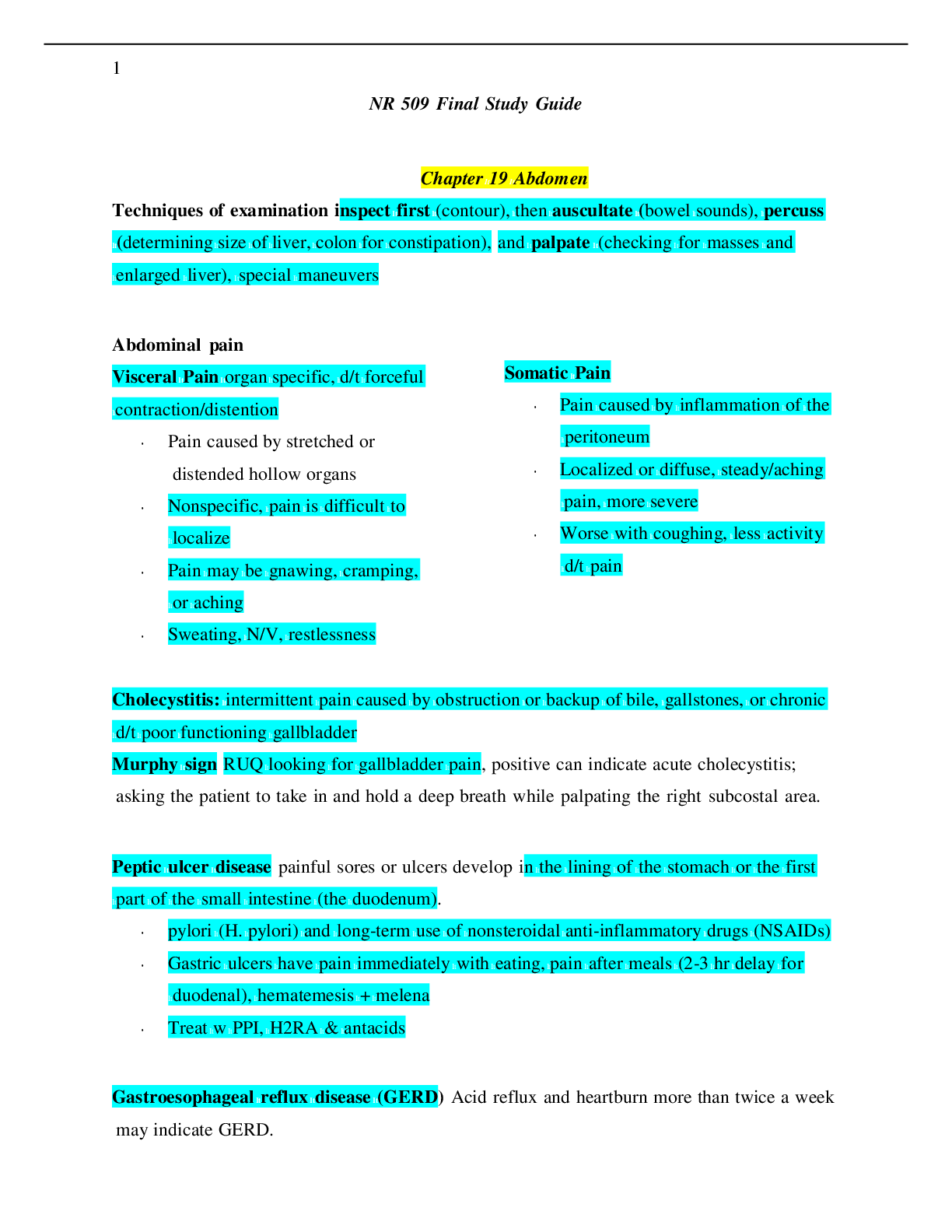

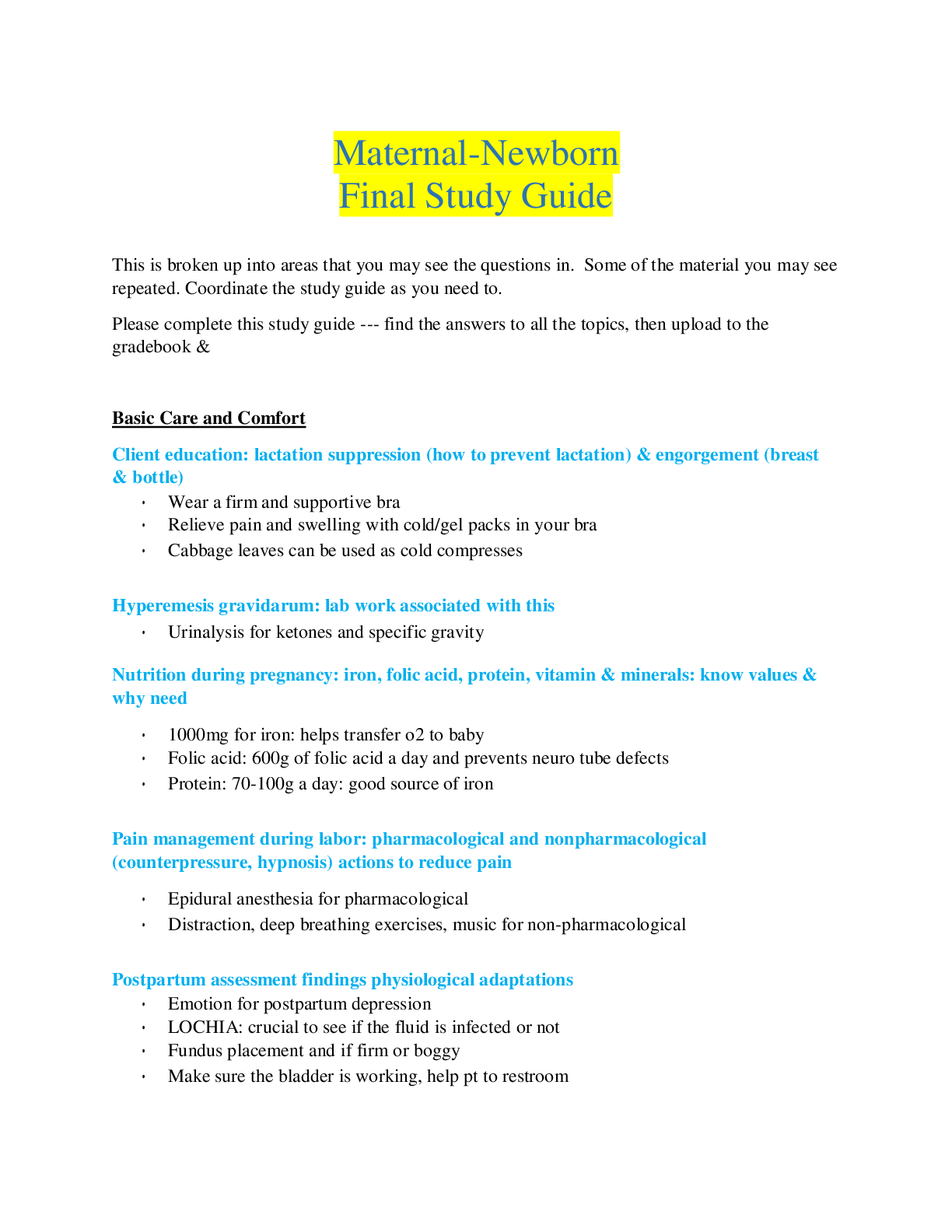
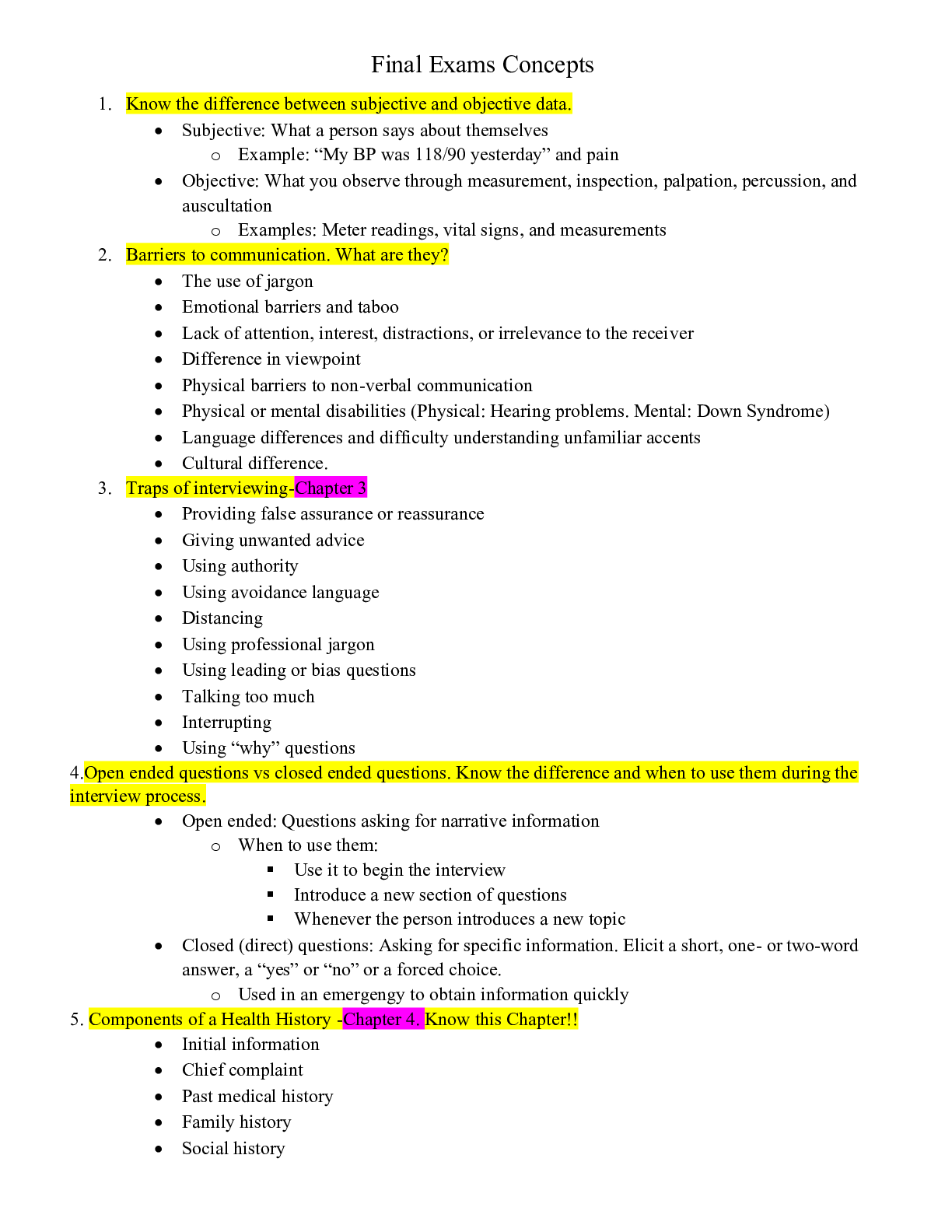
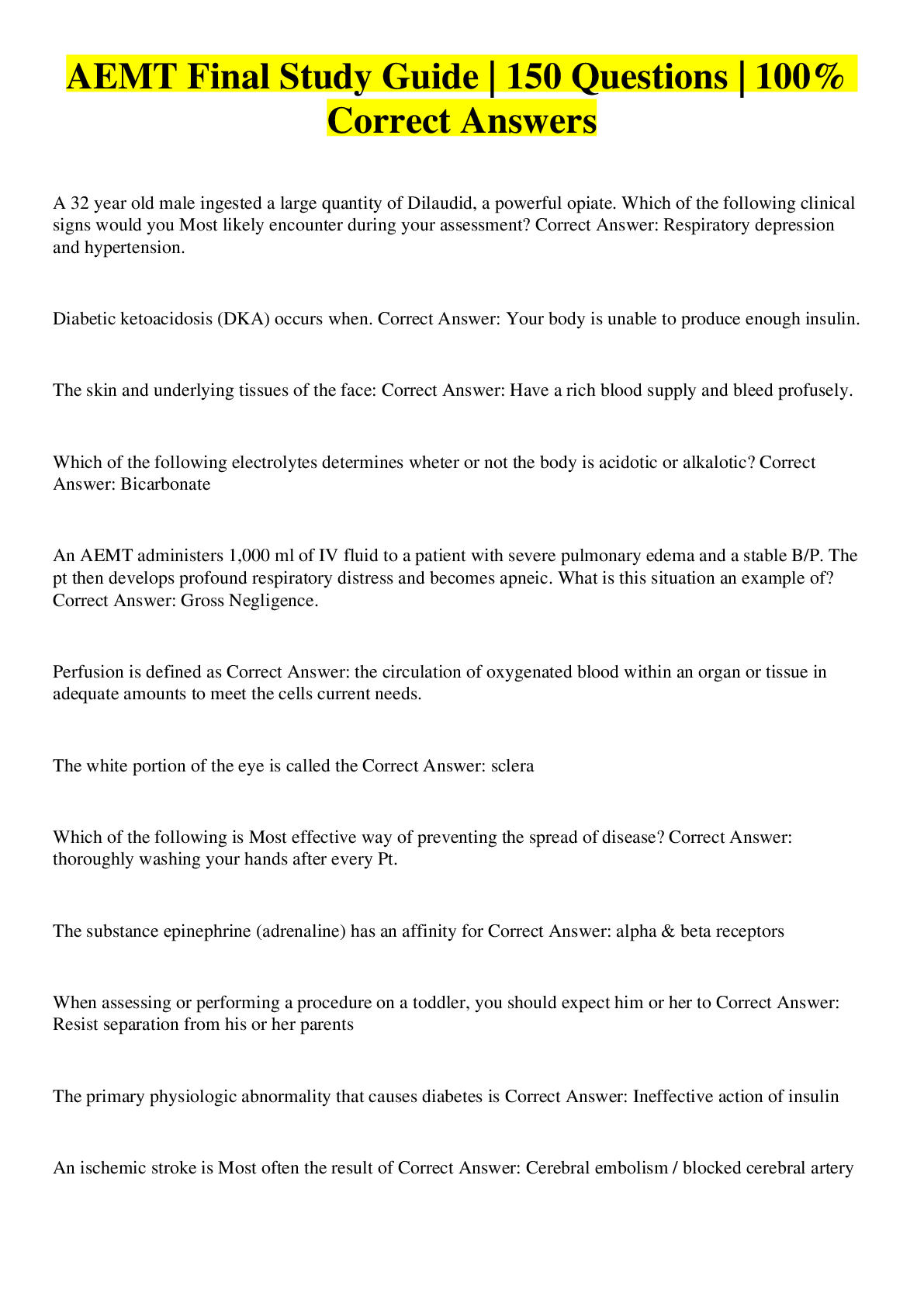

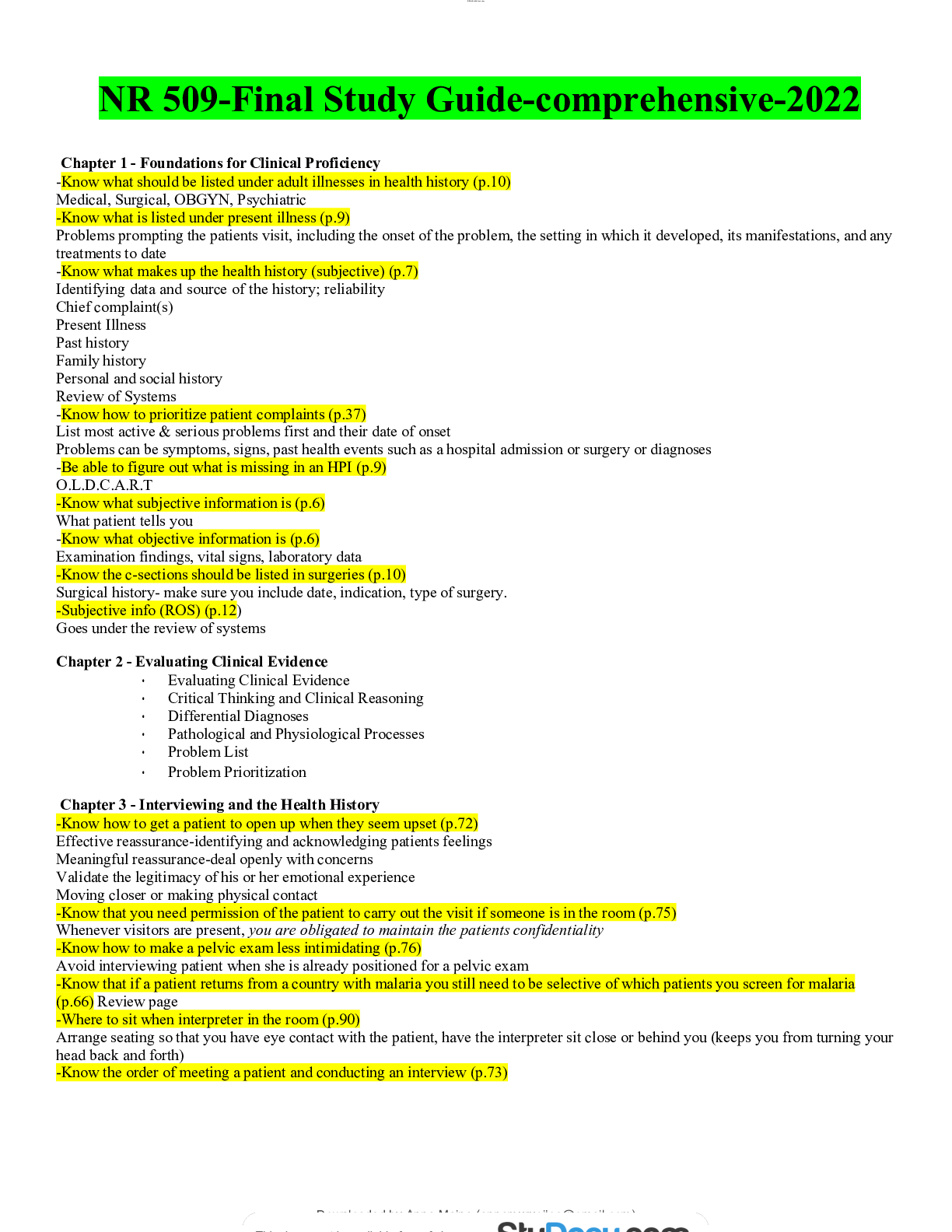
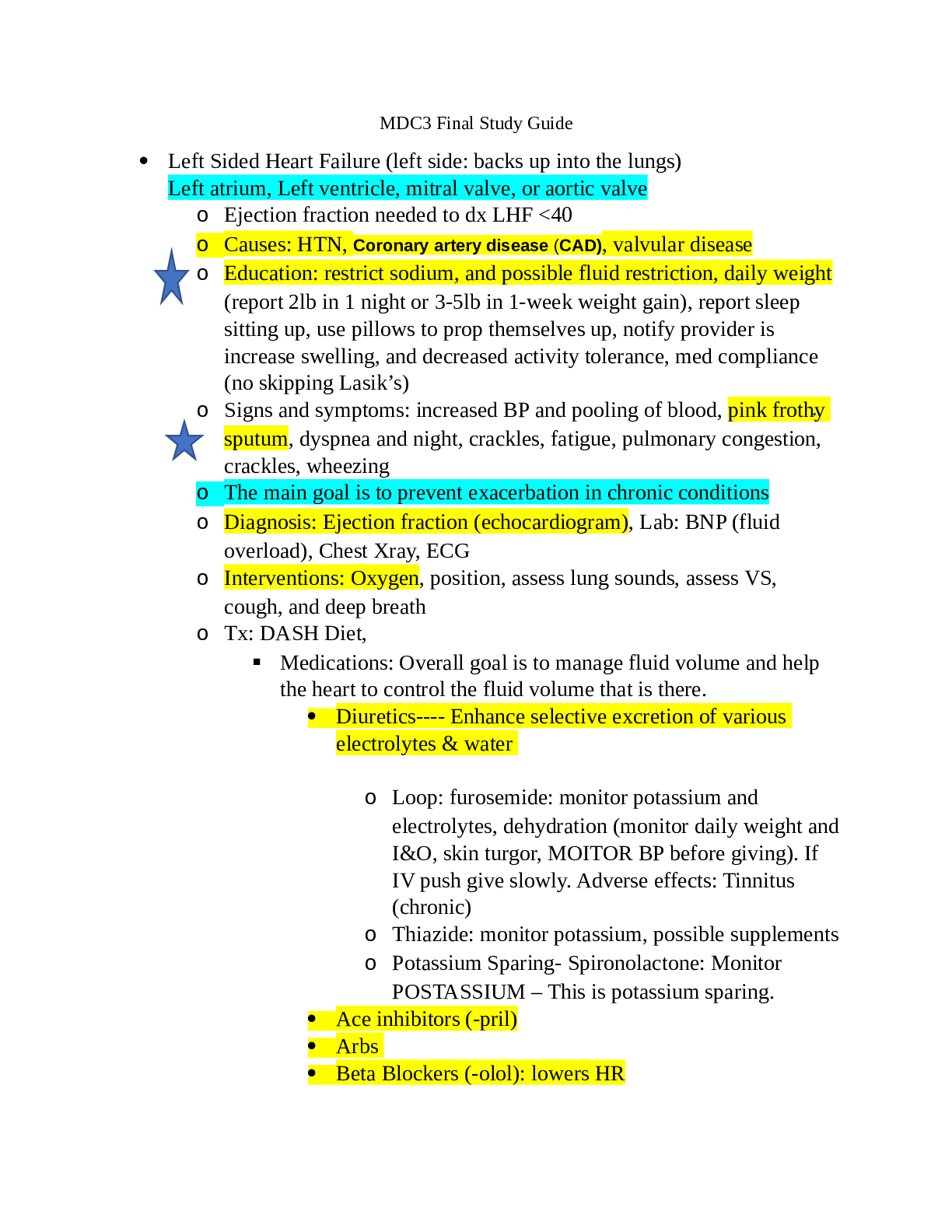
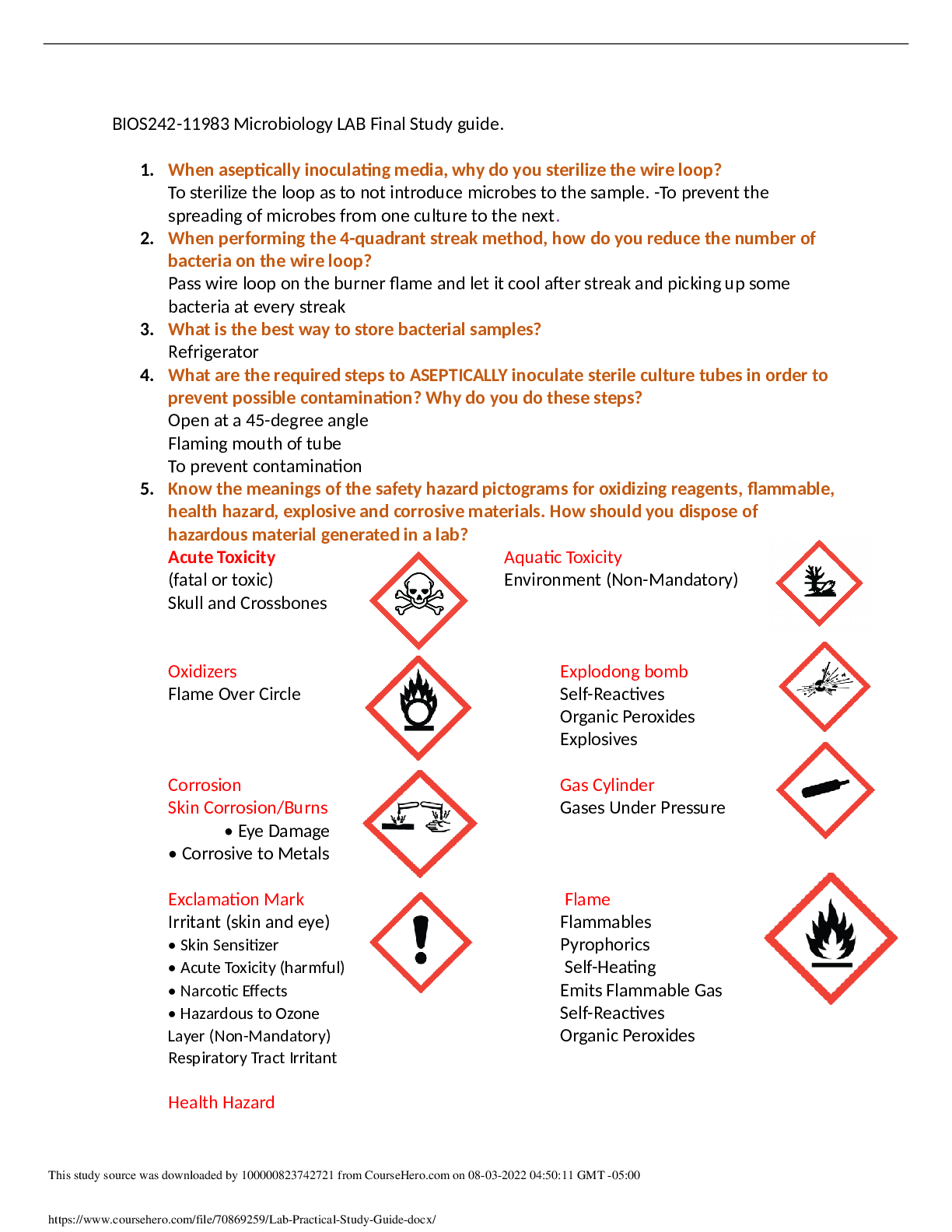

.png)