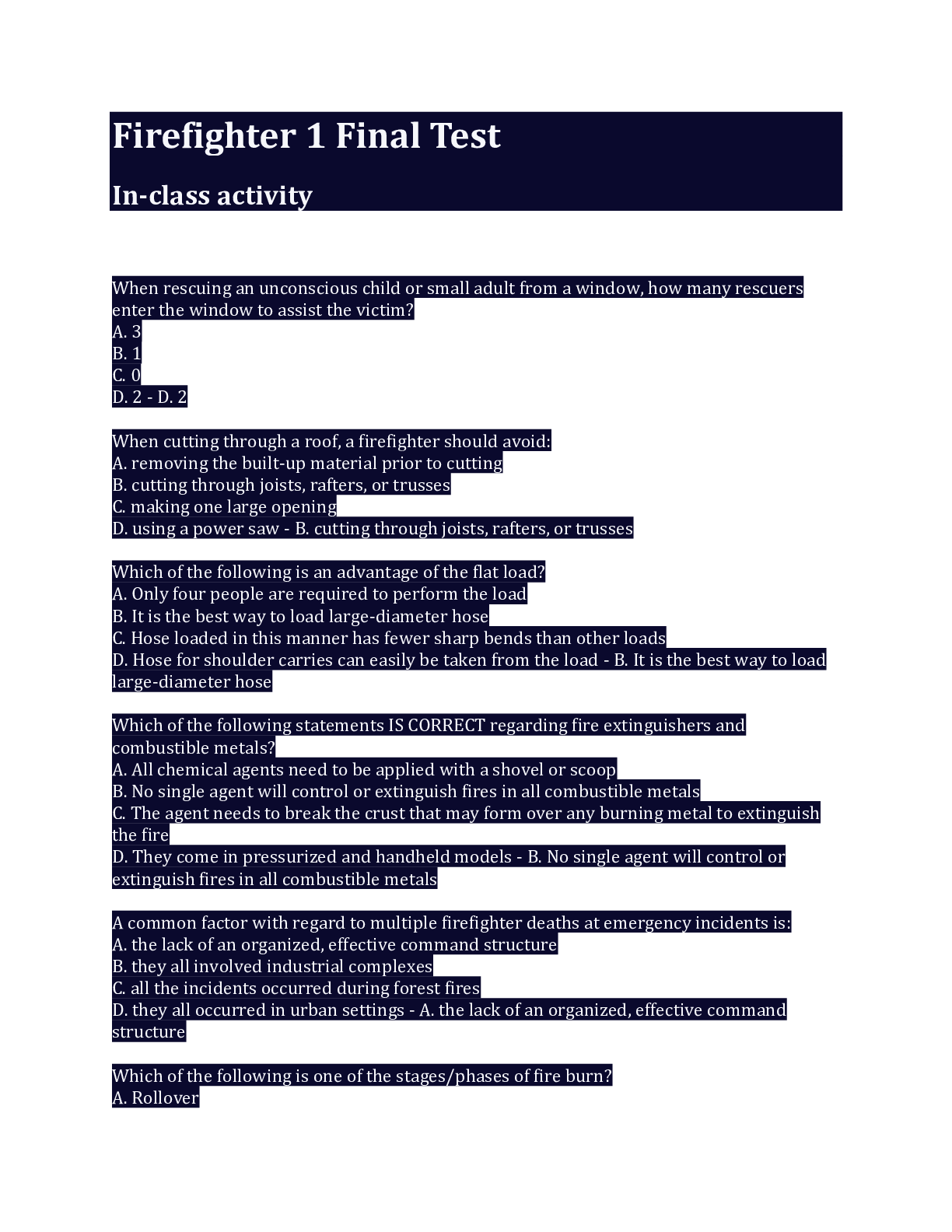
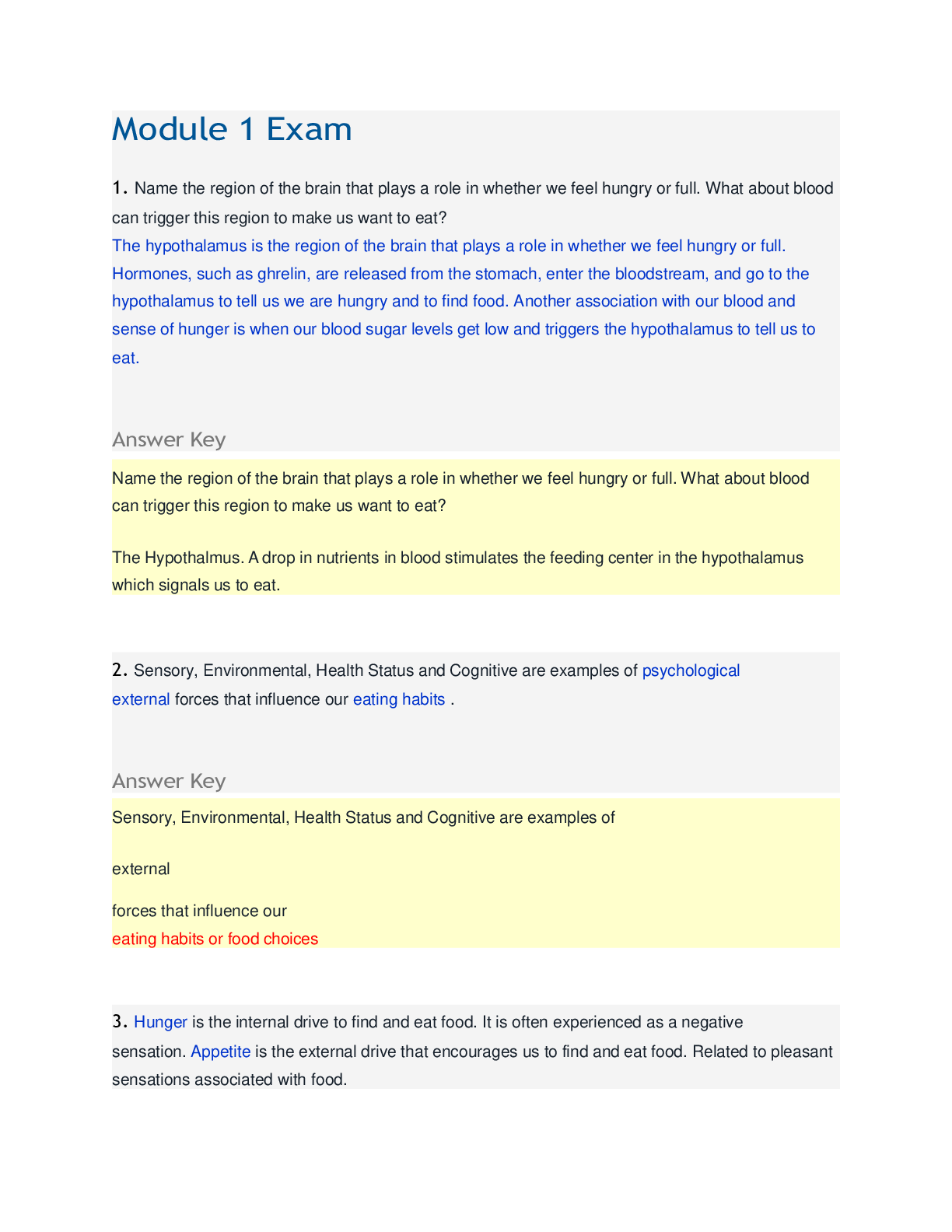
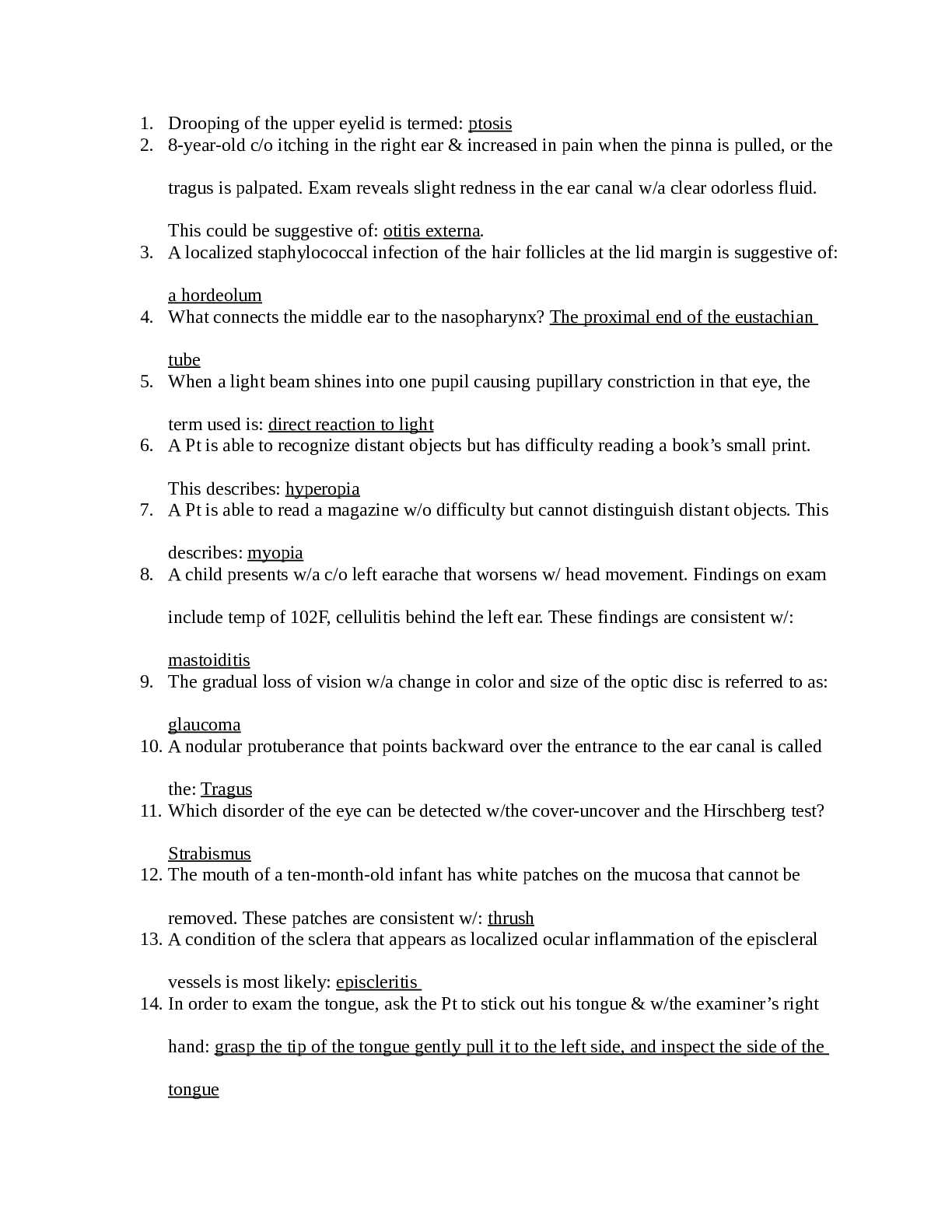
*NURSING > EXAM > NUR 3463Acute Care Exam 1 Review - Fall 2018.docx/ COMPLETE SOLUTION/RATED A (All)
NUR 3463Acute Care Exam 1 Review - Fall 2018.docx/ COMPLETE SOLUTION/RATED A
Document Content and Description Below
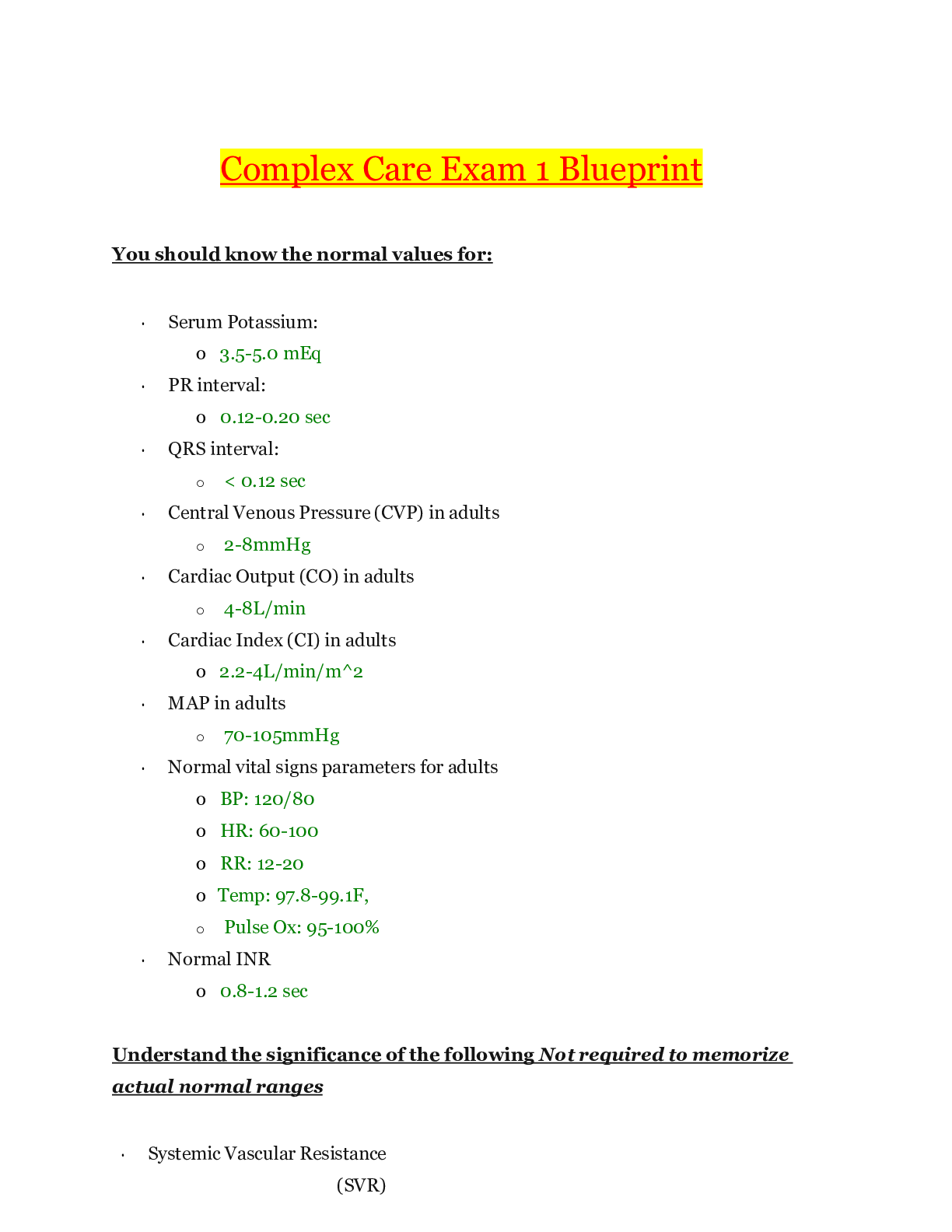
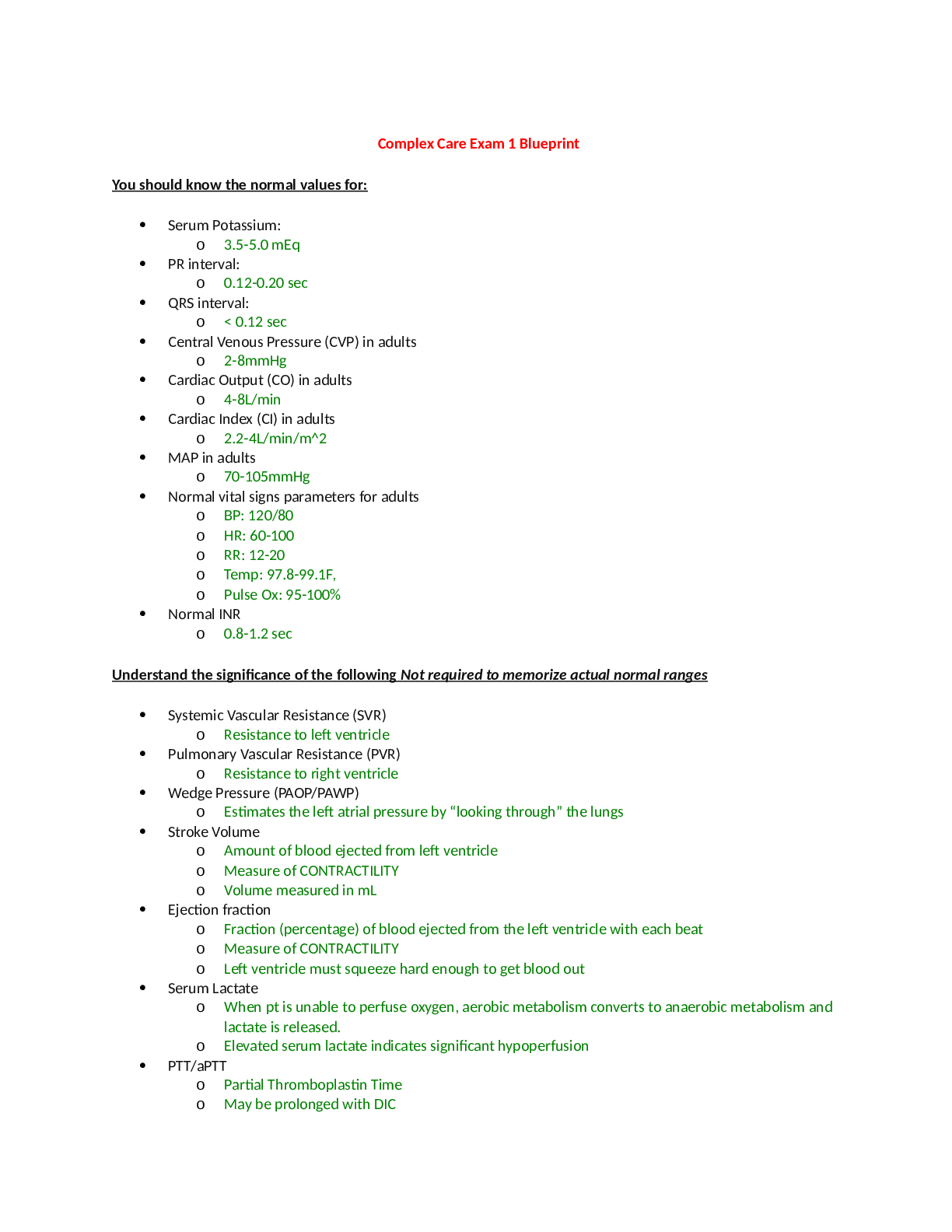
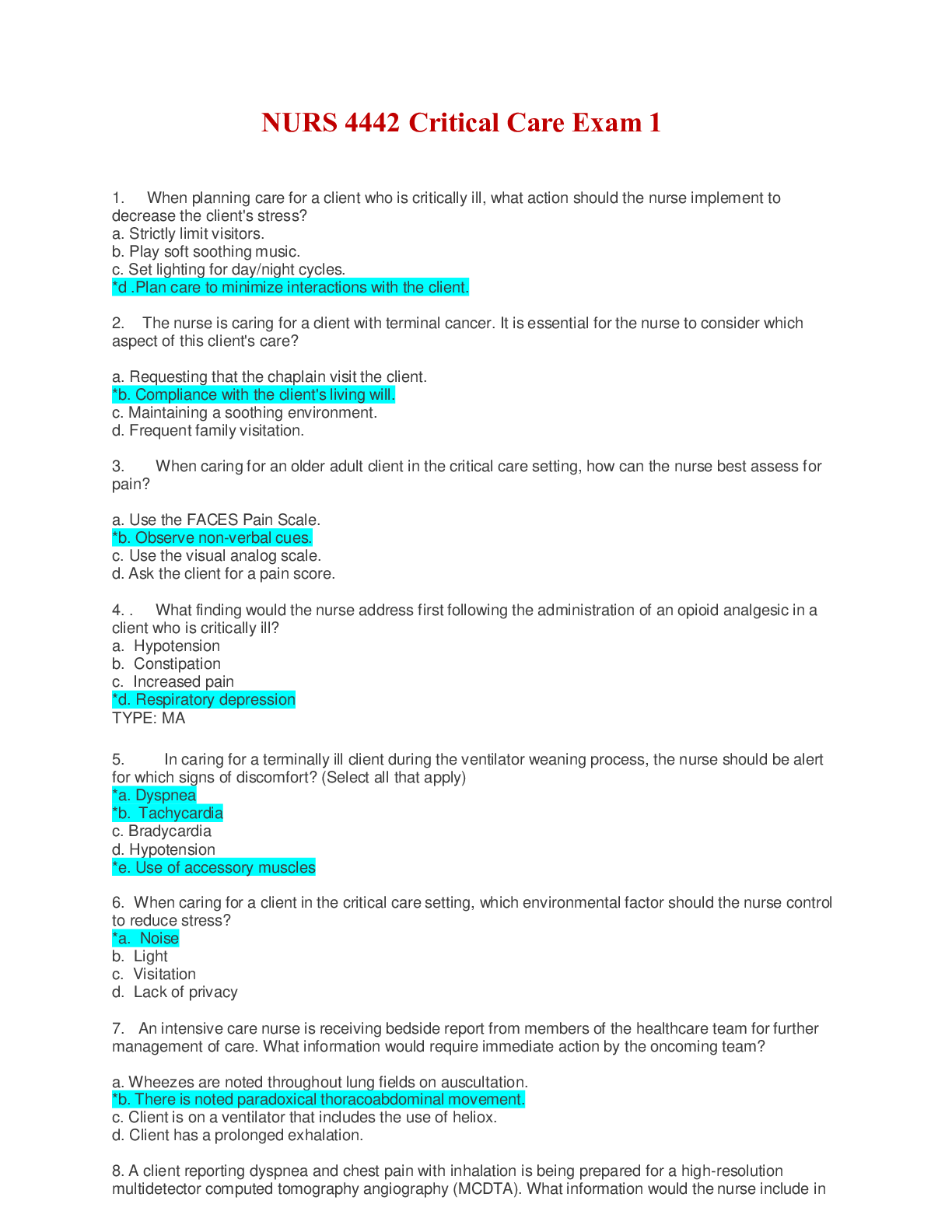
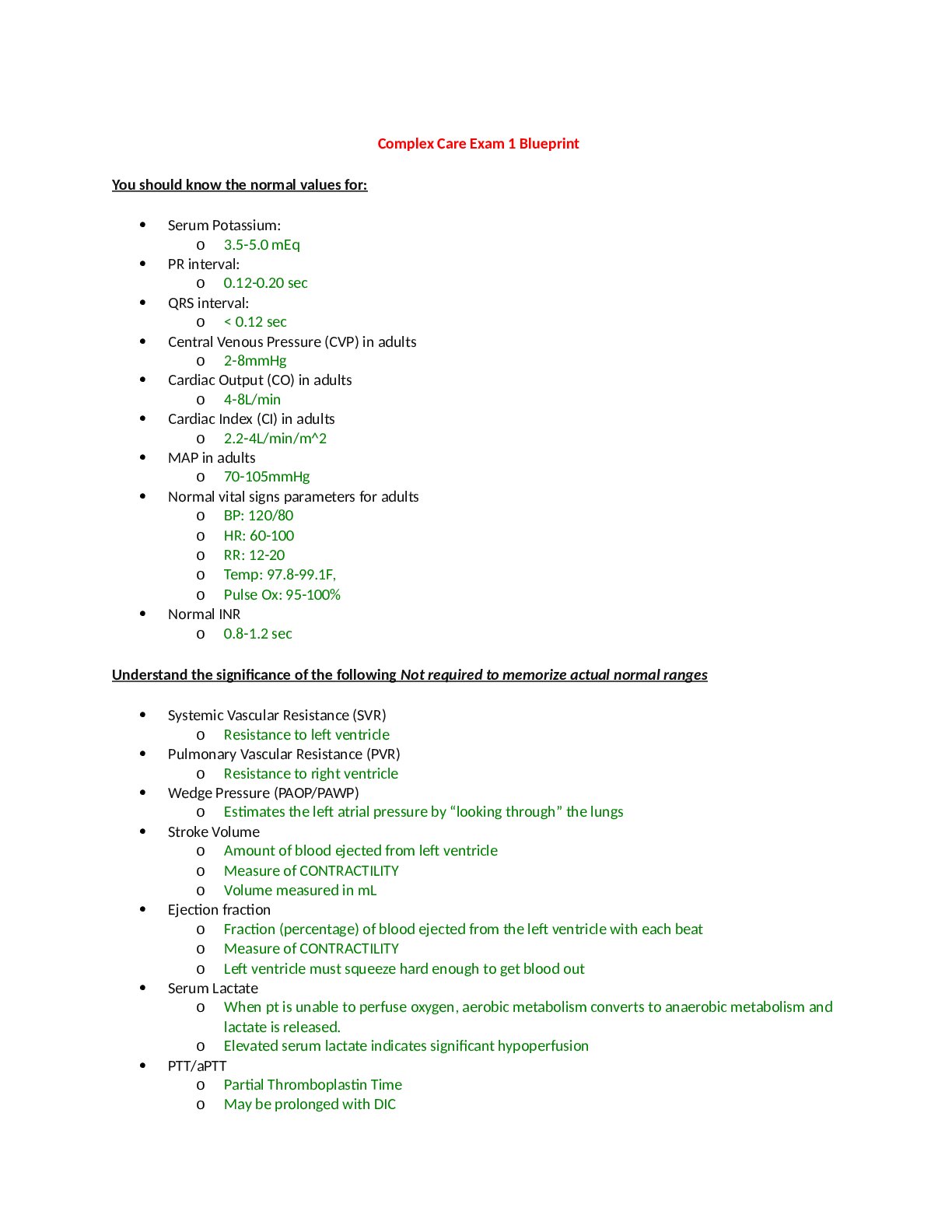
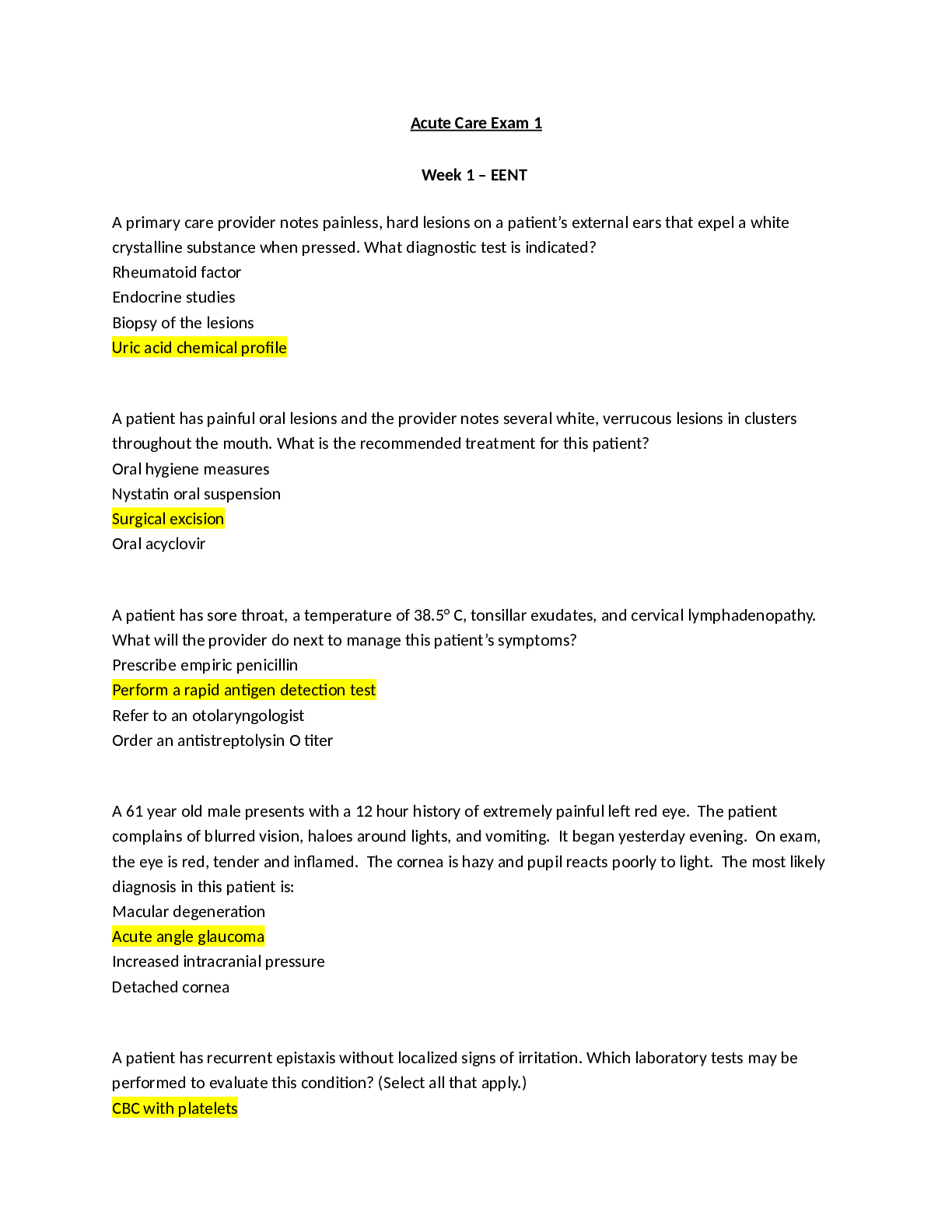
NUR 3463 Acute Care Exam 1 Review - Fall 2018.docx Chapter 1 Explain the current priority focus on patient safety and quality of care. Know the definition of safety, the scope of safety, and the att... ributes of safety. Priority: patient centered care!! And ABC, plus Pain Safety: ability to keep the patient and staff free from harm and minimize errors in care Scope of Safety: can be two types unsafe and safe Unsafe-possibly causing harm or death: errors, lack of communication Safe-prevent harm or negative outcomes Attributes of Safety: reduce rates of error and harm, need to use method of safety in order to keep working systems Differentiate the six core Quality and Safety Education for Nurses (QSEN) competencies Safety, teamwork and collaboration, quality improvement, informatics/technology, patient- centered care, evidence-based practice Describe the SBAR procedure for successful hand-off communication in health care agencies. Situation, background, assessment, recommendation/request Identify the purpose and function of the Rapid Response Team (RRT). Know the indications for when to call a rapid response in the hospital Help to make sure things do not get worse, respiratory problems, getting worse than they normally are Outline the five rights of the delegation and supervision process. Remember the “Don’t share your TEAACUP” mnemonic. Also remember the definition of supervision per the textbook. Supervision: guidance or direction, evaluation, and follow-up by the nurse to ensure that the task or activity is performed appropriately Delegation: transferring to a competent person to perform a selected nursing task or activity on a selected patient: NURSE IS ALWAYS ACCOUNTABLE TEAACUP: Teaching, Evaluating, Assessment, Advanced interventions, collaboration, unstable patients, planning Five rights: task, circumstance, person, communication, supervision Chapter 3 Explain evidence-based falls risk and prevention interventions for older adults in the hospital. Huge concern are falls!! Promote sleep and less things on floor in order to avoid things being in the way, use of transfer aids if possible, cane/wheelchair Identify the specific criteria required to meet the definition of frailty Weakness, poor balance, low gait speed, visual impairment, cognitive impairment, weight loss, low physical activity Frailty: geriatric syndrome in which older adults have unintentional weight loss, weakness, exhaustion, and slowed physical activity including walking Describe the effects of drugs on the older adult. More susceptible changes in their body, adverse effects happen more often, medication management is essential in making sure that they are not doing things that can make overall health worse Toxic effects of medications: drugs absorbed, metabolized, and distributed more slowly than in younger people-excreted more slowly by kidneys Compare characteristics of common problems of cognition: depression, delirium, and dementia Confusion, loss of memory, restless, perception is different Delirium: acute confusion that has sudden onset with fluctuating course Dementia: chronic confusion Depression: most common and most underdiagnosed/undertreated mental health/behavioral health disorder among older adults Identify key interventions to prevent tissue integrity changes in older adults. Identify specific risk factors for skin tears in older adults. Nutritional support, avoidance of skin injury from friction and shearing forces, repositioning and support surfaces, a plan to increase mobility and activity level when appropriate, and skin cleaning and use of moisture barriers Risk factor for those on steroid therapy and old-old adult group Chapter 11 – Fluid and Electrolytes Describe the significance of the Renin-Angiotensin II Pathway. What conditions trigger it? How is this pathway used in the management of HTN (e.g. specific drugs, etc) helps to maintain adequate tissue perfusion: renin secretes from kidneys when they sense things are not normal Triggered by: low blood pressure, low blood volume, low blood sodium, low blood oxygen ACE inhibitors are used to manage blood pressure or diuretics help to manage HTN: less vasoconstriction, less peripheral resistance: in turn disrupt RAS pathways What is postural hypotension and how do we assess for it? A decrease in blood pressure (20 mm Hg systolic, 10 mmHg diastolic) that occurs during the first few seconds to minutes after changing from sitting or lying position to standing position Assess by first measuring when they are laying down then sitting then when they are standing: causes light headedness and dizziness General types of food to avoid on a low sodium diet (e.g. processed, etc.) Processed or preserved foods: smoked, pickled foods, snack foods, condiments If your patient is receiving IV potassium, what action do you take if they report pain at the IV site? Report pain-stop and assess Need to give very slowly, prefer oral if possible What does aldosterone do and what electrolyte imbalance are we most at risk for if secretion is inhibited Aldosterone: secreted by adrenal cortex whenever sodium levels in ECF are low, prevents both water and sodium loss, acts of kidney nephrons triggering them to reabsorb sodium and water from urine back into blood (increase blood osmolarity and volume). Also promotes kidney potassium excretion POTASSIUM EXCRETION AND SODIUM ABSORPTION What conditions can trigger the release of ADH Released from posterior pituitary gland in response to changes in blood osmolarity Blood osmolarity increased, or plasma sodium increased, then ADH released Makes blood more dilute by nephrons being more permeable to water Assessment finding for dehydrated patients Turgor/tenting (forehead or sternum), output, electrolyte imbalance, weight loss or gain Monitor cardiac and pulmonary status at least every hour when patients with dehydration are receiving IV fluid replacement therapy Common causes of dehydration Electrolyte imbalance, not enough liquids taken in (intake), medications (diuretics) Sodium (hypo/hyper) – Common causes, assessment findings, and interventions Normal: 136-145 mEq/L Hyponatremia: lower than 136 mEq/L - inhibit secretion of ADH and NP and trigger aldosterone secretion – diuretics, heart failure, NPO, kidney disease, low salt diet, hyperglycemia - behavioral changes, muscle weakness, increased motility of intestines, CO changes (low HR low BP) – treat with drug therapy (excrete water not sodium), 3% saline infusion, nutrition therapy (oral sodium intake) Hypernatremia: higher than 145 mEq/L - inhibit aldosterone secretion and stimulate ADH and NP secretion – dehydration, hyperventilation, corticosteroids, kidney failure – attention span and cognitive function muscle twitching or irregular contractions, decreased contractibility of cardiac muscle (HR increased) – drug therapy (isotonic saline and dextrose in sodium chloride), increase water intake and sodium restriction Potassium (hypo/hyper) – Common causes, assessment findings (including what we see on ECG), and interventions Normal: 3.5-5.0 mEq/L Hypokalemia: lower than 3.5 mEq/L – every part of body system is affected! – alkalosis, use of drugs, D/V, kidney disease, NPO, increase aldosterone – older adult (age), drugs (diuretics), diseases/surgeries, respiratory changes b/c muscle weakness (shallow resp.), muscle weakness, thready/weak pulse, irregular heartbeat, altered mental status (irritability, anxiety, lethargy), decreased peristalsis (hypoactive bowel sounds, N/V, constipation) – ST segment depression, flat or inverted T waves, and increased U waves – increase potassium intake, make sure gas exchange is actually happening!, fall prevention, avoid diuretics Hyperkalemia: higher than 5.0 mEq/L – really affects the heart – increases cell excitability – salt substitute, repid infusion or potassium, kidney failure, ACE inhibitors, acidosis, tissue damage – bradycardia, hypotension, tall and peaked T waves, prolonged PR intervals, flat or absent P waves, wide QRS complexes, ectopic beats may appear, twitchy muscles then numbness, diarrhea/hyperactive bowl sounds – drug therapy is key! Stop potassium infusion if needed, patiromer drug to stop potassium absorption, increase potassium secretion (diuretics), cardiac monitoring, teaching about diets, drugs, and indicators Calcium (hypo/hyper) – Common causes, assessment findings (including what we see on ECG), and interventions Normal: 9.0-10.5 mg/dL Hypocalcemia: below 9.0 mg/dL – lactose intolerance, celiac, crohns, end-stage kidney disease, diarrhea – muscle spasms, recent surgery, overstimulation of nerves, paresthesia (numbness/tingling) (Trousseau sign), hypotension, prolonged ST interval and prolonged QT [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 12, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Jul 12, 2021
Downloads
0
Views
32


 (1).png)
 (1).png)
 (1).png)


.png)