*NURSING > QUESTIONS and ANSWERS > UNRS 310 ATI Mental Health STUDY GUIDE. (All)
UNRS 310 ATI Mental Health STUDY GUIDE.
Document Content and Description Below
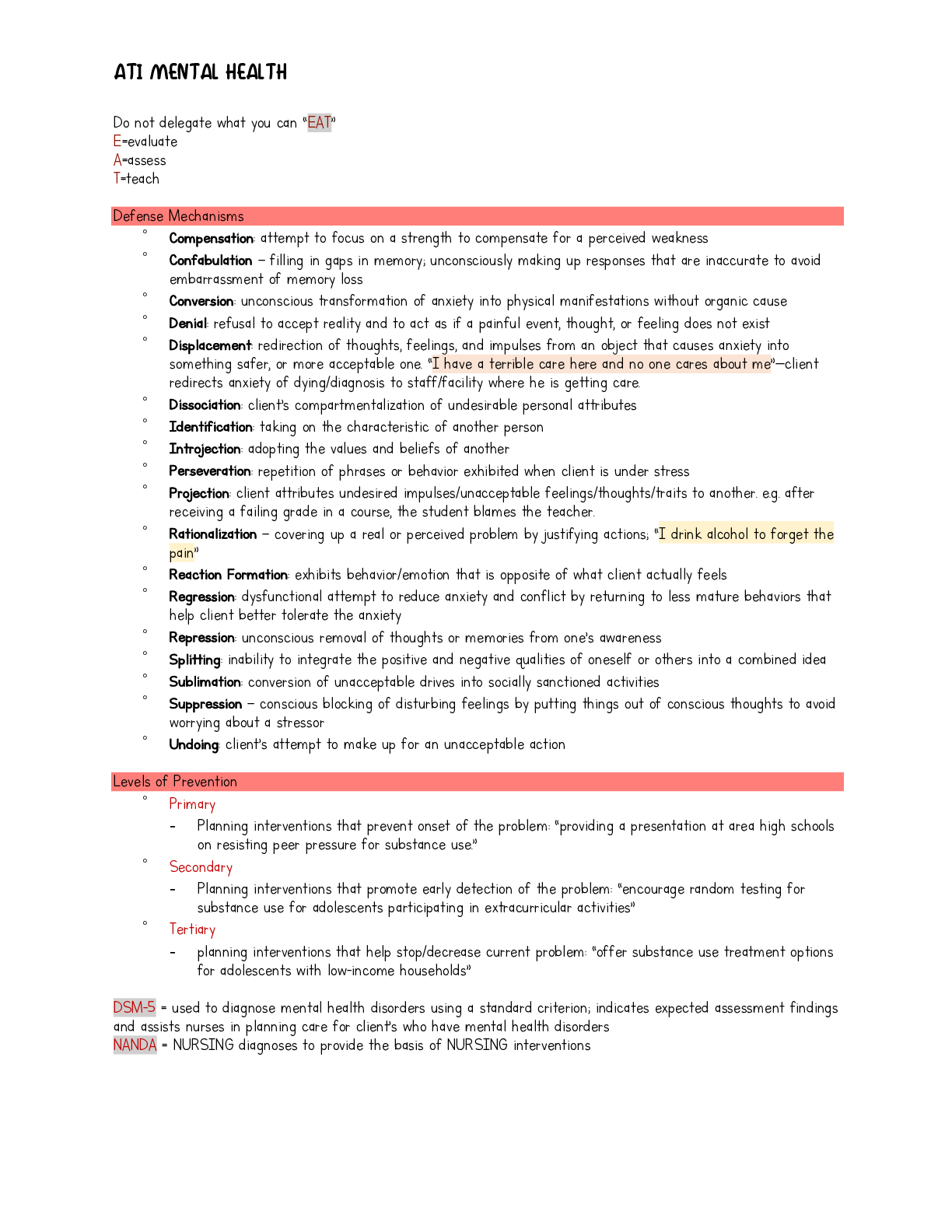
Do not delegate what you can “EAT” E=evaluate A=assess T=teach Defense ftechanisms ˚ Compensation: attempt to focus on a strength to compensate for a perceived weakness ˚ Confabulation – ... filling in gaps in memory; unconsciously making up responses that are inaccurate to avoid embarrassment of memory loss ˚ Conversion: unconscious transformation of anxiety into physical manifestations without organic cause ˚ Denial: refusal to accept reality and to act as if a painful event, thought, or feeling does not exist ˚ Displacement: redirection of thoughts, feelings, and impulses from an object that causes anxiety into something safer, or more acceptable one. “I have a terrible care here and no one cares about me”—client redirects anxiety of dying/diagnosis to staff/facility where he is getting care. ˚ Dissociation: client’s compartmentalization of undesirable personal attributes ˚ Identification: taking on the characteristic of another person ˚ Introjection: adopting the values and beliefs of another ˚ Perseveration: repetition of phrases or behavior exhibited when client is under stress ˚ Projection: client attributes undesired impulses/unacceptable feelings/thoughts/traits to another. e.g. after receiving a failing grade in a course, the student blames the teacher. ˚ Rationalization – covering up a real or perceived problem by justifying actions; “I drink alcohol to forget the pain” ˚ Reaction Formation: exhibits behavior/emotion that is opposite of what client actually feels ˚ Regression: dysfunctional attempt to reduce anxiety and conflict by returning to less mature behaviors that help client better tolerate the anxiety ˚ Repression: unconscious removal of thoughts or memories from one’s awareness ˚ Splitting: inability to integrate the positive and negative qualities of oneself or others into a combined idea ˚ Sublimation: conversion of unacceptable drives into socially sanctioned activities ˚ Suppression – conscious blocking of disturbing feelings by putting things out of conscious thoughts to avoid worrying about a stressor ˚ Undoing: client’s attempt to make up for an unacceptable action Levels of Prevention ˚ Primary - Planning interventions that prevent onset of the problem: “providing a presentation at area high schools on resisting peer pressure for substance use.” ˚ Secondary - Planning interventions that promote early detection of the problem: “encourage random testing for substance use for adolescents participating in extracurricular activities” ˚ Tertiary - planning interventions that help stop/decrease current problem: “offer substance use treatment options for adolescents with low-income households” DSft-5 = used to diagnose mental health disorders using a standard criterion; indicates expected assessment findings and assists nurses in planning care for client’s who have mental health disorders NANDA = NURSING diagnoses to provide the basis of NURSING interventions Nurse-client relationship - the relationship is FOCUSED on the NEEDS of the CLIENT - a therapeutic relationship rather than emotional or social. ˚ Orientation phase: - Nurse-client introductions, expectations, and boundaries - Contract: meetings, place, time, duration, frequency, and termination date. - nurse establish rapport and confidentiality with the client. The nurse should assess client’s beliefs about the reason for therapy. ˚ Working phase: - ftaintenance, ADPIE - nurse introduce client to other clients - the nurse should gather further data, including detailed assessment of what the problem is (e.g. hallucinations) and client’s family relationships; assist client with development of problem-solving skills - determine coping strategies that have worked in the past - nurse assist client in behavioral change ˚ Termination phase: - Discuss experiences - Summarize goals and achievements - Discuss ways for the client to incorporate new healthy behaviors into life Countertransference vs Transference ˚ Countertransference: nurse unconsciously attributing positive or negative feelings about another towards the client ˚ Transference; client having unconscious displacement of feelings towards the nurse Family dynamics - Healthy family = boundaries are distinguishable = roles are defined within members - Boundary issue: o enmeshed boundary = no distinction between roles of family members; e.g. older children taking care of their younger siblings o rigid boundary = members isolate themselves; minimal communication—do not share thoughts or feelings. Ethical Principles ˚ Autonomy – allowing client to choose ˚ Beneficence – doing good; charity ˚ Fidelity – loyalty and faithfulness to client AND DUTY. ˚ Justice – guarantees all clients receive equal care; spending appropriate time with pt regardless of behavior ˚ Nonmaleficence – doing no harm; e.g. using least restrictive therapies instead of restraints ˚ Veracity – honesty; providing client with accurate information regarding prognosis o Informed decision = nurse should not agree to refusal/reasoning out of patient if they do not want the medication or go through therapy; nurse should be able to tell pt the purpose of intervention and the risks of not getting it. Community-Based ftental Health ˚ Partial Hospitalization Program - Provides intense short-term treatments for clients during the day while allowing them to spend nights in their homes. ˚ Assertive Community Treatment - Provides comprehensive, community-based services—available in any setting, including the client’s home, 24hr/day, providing crisis intervention, medication services and advocacy - Works with clients who are nonadherent with traditional therapy ˚ Community ftental Health Center - Offers education, group therapy, and medication administration ˚ ftental Health Day Program - Offers services for clients who need supervision or assistance during daytime hours Involuntary Admission - Justified if client is DTS, DTO, and GD - Usually requires 2 physicians to certify need - Pt is considered to be competent and retains legal right to refuse treatment and medications; UNLESS was judged to be incompetent by the court—will have a guardian to decide and sign for care - ftay remain in the facility for up to 60 days; then legal review of admission is required - Unable to leave AftA but they can file a petition requesting a review of involuntary admission Right to Refuse medications - Client still has the right to refuse medications even if admitted involuntarily; nurse must document refusal in the medical record and assess reasons for the refusal Right to Privacy - This right continues even after death - Breach of confidentiality: disclosing information without client’s consent o To an employer o To the next of kin without the client’s consent o To any employees not directly involved in client’s care Schizophrenia - PRIORITY-SETTING FRAftEWORK: client’s appearance is unkempt and he appears to be actively hallucinating—assess physical needs. - Positive Symptoms ˚ Alterations in Speech a) Clang Association- stringing and repeating of rhyming words b) Echolalia – echoing; consistent repeating of another’s words by imitation c) Word Salad – mixture of phrases and words strung together without meaning/relation to one another d) Neologism – invented word which has no meaning to others ˚ Alterations in perception = Hallucinations a) Auditory - Explore what the voices are saying to the pt - Command = Client is at greatest risk for self-directed injury or injuring others ˚ Alterations in thoughs = Delusions a) Somatic: “fty internal organs have turned to stone” b) Reference – belief that occurrences in the environment are about them c) Persecutory – belief that someone or something wants to intentionally harm them d) Grandiose – belief that they are superior or more important than others e) ftagical thinking – belief that thoughts or behaviors have control over specific people and situations - Negative Symptoms [the 5 A’s] ˚ Blunted or flat Affect ˚ Alogia = “lack of speech” ˚ Anergia = “lack of energy” ˚ Anhedonia = “lack of pleasure” ˚ Avolition = “lack of motivation” Depressive Disorders - Expected findings: o Anergia, anhedonia o Sluggishness = most common o Vegetative: change in eating patterns, sleep, bowel habits ftajor Depressive Disorder (ftDD) - PRIORITY-SETTING FRAftEWORK: Any s/s of suicidality “I have it all figured out. Everything is going to be okay now;” giving out possessions; - Overt vs Covert statements o Overt: direct to the point o Covert: “covered” - Suicidal o Constant 1:1 observation to ensure safety o Avoid private rooms and doors must be open the whole time. o Plastic utensils rather than metals o Goal is for the client to be able to verbalize suicidal thoughts to staff Bipolar Disorders For pt with manic episode - Unable to sit for a long time to eat meals; - Offer finger foods; something they can eat while moving around; e.g. chicken nuggets, crackers with cheese sticks, and a cookie - High protein, high calorie, non-caffeinated, no utensils - ftaintain adequate hydration and promote rest - Relapse of mania = pressured speech Anxiety - Acute = imminent loss/change that threatens one’s sense of security - Chronic = developed overtime; may develop physical manifestations: fatigue, HA - Levels o ftild Anxiety allows the client to perceive reality in sharp focus and actual problem solving becomes more effective teach relaxation technique at this level so client will be able to concentrate and process information o ftoderate Anxiety the perceptual field narrows, but the client is able to cope with some assistance. This client’s manifestations indicate a higher level of anxiety client will have difficulty in concentration o Severe Anxiety the perceptual l field is scattered and the client is not able to focus on anything except relieving the anxiety. This client’s manifestations indicate a high level of anxiety o Panic flushing, perspiring profusely, experiencing palpitations and screaming “I am going to die! This is it! I am having a heart attack!”---nurse to instruct pt to take a slow, deep breaths clients benefit from calm, quiet environment; so stay with pt and remain quiet General Anxiety Disorder - Indecisive and dreads making decision—nurse: “We’ll assist you with making decisions” Panic Disorder - Recurrent panic attacks that are not associated with any specific stimulus or situation seem to occur spontaneously PTSD - Flashbacks, distressing memories, and dreams of traumatic event - PRIORITY-SETTING FRAftEWORK: Stay with client when flashbacks occur—because of r/o injury; offer reassurance and support - Client tried to avoid distressing memories but still able to leave house - Current treatment plan is effective when client reports techniques she uses to promote sleep Phobias ˚ Agoraphobia: fear and subsequent avoidance of places or situations from which escape might be difficult; fear of leaving one’s home and avoiding open public places such as shopping malls. - Systemic desensitization: “you will slowly be exposed to increasing levels of public spaces” ˚ Claustrophobia = intense fear about being in an enclosed space e.g. elevators ˚ Zoophobia = fear of animals ˚ Xenophobia = fear of strangers ˚ Hydrophobia = fear of water Substance Use Disorder ˚ Opioids o Withdrawal - Rhinorrhea, flu-like manifestations; yawning, sneezing, and ABD pain ˚ Alcohol - when client verbalizes, “I think I might have a problem with alcohol”—nurse will ask the client to complete a CAGE Questionnaire o Withdrawal: 4-12 hrs - HA; tremors, n/v, sweating, depression, or irritability, insomnia, elevated temperature, tachycardia - Teach client: “s/s may persist for several days after intake of alcohol”. o ftay benefit from Aversion therapy - AUDIT ˚ Cocaine o Intoxication: dilated pupils, hyperactivity, hyper-alertness/hypervigilance ˚ Phencyclidine (PCP; “angel dust”) o nystagmus ADHD - Planned Ignoring: “Ignore your child’s attention-seeking behavior that are not dangerous”—if the child learns that the behavior will not elicit the desired response, then the behavior should decrease Obsessive-Compulsive Disorder - PRIORITY-SETTING FRAftEWORK: Determine client’s anxiety level first - Plan the client’s schedule to allow time to perform rituals; rituals help them keep anxiety levels manageable - Behavioral Intervention Strategies: o ftodeling = allows client to see the expected behaviors performed by the nurse o Response prevention = instruct the client to set time limit between episodes of the compulsive ritual o Thought stopping = client shouts “stop” each time there is an urge to perform rituals to interrupt obtrusive thoughts or actions o Relaxation training = client uses muscle relaxation to counteract stress and anxiety Antisocial Personality Disorder - Tends to see themselves as superior to others; nominating self = wants to place self in position of power - Uses flattery as a form of manipulation - Showing progress to treatment when client o assists another client who has depression to fill out a menu = willingness to help o requesting a weekend pass = willingness to follow rules Borderline Personality Disorder - PRIORITY-SETTING FRAftEWORK: Client found cutting into flesh using a paper clip—Nursing interventions: provide first aid, then identify client’s feelings that led to self-injurious behavior. [Collect data first before formulating a POC, implementing nursing interventions, and notify ftD about change in status] Anorexia Nervosa - Clients will have altered sense of self-image and self-identity and often bases feelings of self-worth on body weight; overweight leads to decreased self-worth - ftay be obsessed with thoughts of foods despite of personal restrictions on intake - ftay have strenuous exercise regimen - DO NOT permit the client to spend some quiet time alone after each meal - Orthostatic hypotension - Types: o Binge-eating/purging = recurrent binging with compensatory vomiting o Restricting = decreasing caloric intake Binge-Eating Disorders - ABD pain d/t GI dilation that occurs as a result of eating excessive volumes of food - Have repeated episodes of binging without the use of compensatory behaviors Bulimia Nervosa - Expected finding: tooth erosion/dental caries d/t frequent exposure to gastric acid from induced vomiting Conduct Disorder - Exhibits aggressive behavior towards others and impulsively violate others’ rights Abuse - Pediatric: 9-month old infant who reportedly nearly drowned after climbing into the tub and turning on water; 18-month old toddler who received a fractured left femur from riding a bicycle. - Domestic: when a partner cannot leave the perpetrator, nurse should use a therapeutic communication technique of encouraging formulation of plan of action to ensure his/her safety. “The next time this occurs, what might you do to ensure your safety?” Sexual Assault - Rape-Trauma Syndrome: mood swings, intense emotions, dependence on others, intense guilt about sexual assault; can delay the healing process and produce a sustained and maladaptive response Delirium - Rapid fluctuation in LOC, change in personality - Hallmark: extreme distractibility - ftay be d/t infection, substance withdrawal, head injury, pain - Sudden confusion - Interventions: o Administration of PRN antianxiety medication can decrease anxiety and agitation o ftaintain a low-stimulation environment to decrease disorientation due to overstimulation o Keep room well-lit for orientation and safety at night o Provide consistent routine and limit client need to make own decisions Dementia - Progressive deterioration of cognitive function - Loss of language ability - ftental Status Assessment: o Cognitive Immediate = ask the client to repeat a series of numbers or list of objects Recent = ask the client to recall recent events e.g. visitors from current day Remote memory=memory from the distant past; ask something like: “What year did you graduate from high school?” o Concentration: ask the client to name the months of the year in reverse. o Affect: observe facial expressions o Language: instruct them to write a sentence - Impaired judgement = client loses ability to reason, think abstractly, and have rational thoughts - Client may have delusions “everyone wants to kill me” - Apraxia – loss of purposeful movement in the absence of motor or sensory impairment; exhibited by clients who are unable to perform once-familiar tasks - Agnosia – loss of sensory ability to recognize objects; exhibited by clients who have lost the ability to recognize familiar sounds or people - Reminiscence Therapy: assists client in reflecting on past experiences; goal is to increase client’s self- esteem and attain ego integrity Alzheimer’s Disease - When client becomes agitated, provide space and remain 1-2 arm-lengths away to maintain safety - Stages o Stage 1: No impairment—the individual does not experience any symptoms and none can be assessed by a professional o o Stage 2: Very mild impairment—the individual subjectively feels they forget words or common objects o Stage 3: mild Cognitive Decline—common problems include difficulty planning, remembering names of close friends and family, o and reading with very little retention o Stage 4: moderate Cognitive Decline/Early-stage Alzheimer’s Disease—deficiencies in several areas, including the ability to perform complex tasks like planning for dinner guests or paying bills client STILL able to recognize and identify family members in this stage; o Stage 5: ftoderately Severe Cognitive Decline/ftid-Stage Alzheimer’s Disease—individuals will need help with day-to-day living as the disease creates major memory gaps. Choosing clothes may become difficult. However, they will usually o know basically who they are, names of close relatives, and need no help with eating and toileting. o Stage 6: Severe Cognitive Decline—at this stage, mental difficulties continue to worse. Individuals will need help with toileting and often become suspicious of those who help them; they forget their identities and tend to wander from home and become lost. o Stage 7: Very Severe Cognitive Decline/Late-stage Alzheimer’s Disease—inability to speak, respond to environment and eventually all motor control (bladder incontinence; eating). Individuals will need near-constant assistance for basic needs, including holding their heads up. Grief - Kübler-Ross 5 Stages: Denial-Anger-Bargaining-Disappointment-Acceptance - Bowlby 4 Stages: Numbness-Disequilibrium-Disorganization/Despair-Reorganization - Engel 5 Stages: Shock-Developing Awareness-Restitution-Resolution-Recovery - When client is crying inconsolably, provide a quiet place and allow client to cry BUT stay with client because of risk of self-harm - Use empathy rather than sympathy - Avoid offering advice Types of Loss 1. Necessary = part of life; something anticipated 2. Actual = losing a valued item; death of loved one 3. Perceived = something obvious only to the person but not to others 4. ftaturational = expected due to development process 5. Situational = unanticipated due to external cause Therapeutic Communication ˚ Focusing – concentrates on what is important; determines cause of client’s feelings e.g. “What were we discussing when you began to feel uncomfortable?” ˚ Presenting reality = dispels delusions, hallucinations, or faulty beliefs ˚ Offer self = shows willingness to spend time with client ˚ ftaintain a nonjudgmental tone ˚ Clarifying techniques: o Restating = using client’s EXACT words o Paraphrasing – restating in nurse’s own language to confirm what has been said. o Reflecting – directs the focus back to the client to examine feelings. o Exploring – gathering more information base on what the client has mentioned. ˚ Observing – “I notice…” Non-therapeutic Communication = barrier to effective communication ˚ False reassurance ˚ ftinimizing client’s feelings ˚ Disapproval/disagreeing ˚ Asking “why,” irrelevant, and/or excessive questions ˚ Offering premature advice/value judgments ˚ Avoid close-ended questions – may only be helpful during initial interaction but repetitive use can block further communication ˚ Threatening Electroconvulsive therapy (ECT) - Induce short seizure by stimulating the brain with an electrical current - Client will receive anesthetic (etomidate or propofol) and paralytic medications/muscle relaxants (succinylcholine) prior to the procedure to prevent severe muscle contractions - ftonitor ECG during procedure - Discontinue benzodiazepines and antiseizure medications - ADR: Retrograde Amnesia = loss of memory leading up to the procedure; can persist for several weeks - Nursing: provide frequent orientation, safe environment, assist with ADLs Transcranial ftagnetic Stimulation (TftS) - Noninvasive—uses magnetic pulsations to stimulate the cerebral cortex of the brain - Should not induce seizures - ADR: Seizure (very rare) Therapies ˚ Cognitive - “Thoughts before actions”—by changing attitudes, behavior improves - Good for pts with depression, anxiety, and eating disorders o Cognitive Reframing = e.g. client with depression may think of themselves as “a bad person;” through therapy, they can change their way of thinking by realizing that they may have made some bad decisions but those does not make him/her a bad person. o Journal Keeping ˚ Behavioral - Behavior is learned; abnormal behaviors are d/t unconscious attempt to avoid painful feelings - Uses coping mechanisms to deal with stress - Good for pts with phobias, substance use/addictive disorders; anxiety and avoidant disorders o ftodeling = client imitates nurse doing appropriate behavior o Operant conditioning = positive rewards for positive behavior [Positive reinforcement] o Systematic desensitization = exposure to anxiety-provoking stimuli gradually over time o Aversion therapy = punishment/unpleasant stimuli for maladaptive behavior; e.g. drinking alcohol with disulfiram causes acetaldehyde syndrome, which is very unpleasant. o fteditation, guided imagery, diaphragmatic breathing, muscle relaxation, biofeedback 12- Step Program for Alcohol Use Disorder - Client should obtain a sponsor before discharge for an increased chance of recovery—peer support has been shown to increase program attendance and the chances of recovery; if client can’t find a sponsor, one can be assigned to them before they start the program De-escalation: when pt is suddenly agitated and pacing rapidly, stay at safe distance and remain calm “I will give you space if you calm down. Tell me what is causing you to feel so tense.” Seclusion and Restraints - Only when other less restrictive means are ineffective - ftust be prescribed not as a PRN and must be reassessed so it is current and specific to the client’s present needs. - EftERGENCY—if initiated by RN, must obtain written prescription within specified amount of time per facility protocol (usually within 15-30 minutes) - Constant 1:1 observation by staff WHILE on restraint - Wrist restraints: 2 fingers must fit between restraints and client’s wrist - Document behavior every 15-30 minutes while restraint is in place; remove as soon as possible when behavior is gone. - Provider must evaluate client 1 hour of restraint initiation - Set a time limit base on age: o >18 yrs = 4 hours o 9-17yrs = 2 hrs o <8 yrs = 1 hour - Offer toileting every 15-30 minutes - Renew prescription every 4 hours if needed x 24 hours maximum Antipsychotics - ftonitor for oculogyric crisis (rolling back of the eyes; may be mistaken for seizures; treated as emergency situation) in the first days of antipsychotic medication therapy a) 1st Generation/Conventional = treats positive symptoms ˚ Haloperidol (Haldol) ˚ Chlorpromazine (Thorazine) and Thioridazine hydrochloride b) 2nd Generation/Atypical = current medications of choice; treats both positive and negative symptoms - ftonitor weight gain; abnormal glucose metabolism [check glucose] - ADR: agranulocytosis m/b sore throat and chills withhold medication and notify ftD immediately; agitation, dizziness, sedation, and sleep disruption ˚ Olanzapine (Zyprexa) ˚ Clozapine (Clozaril) ˚ Quetiapine fumarate (Seroquel) ˚ Risperidone (Risperdal) Antianxiety a) Azapirone/Atypical Anxiolytic ˚ Buspirone (Buspar) - ftedication for GAD - Takes 7-10 days to take effect; 2-4 weeks to reach its full effect - Not a PRN; needs to be taken routinely - Client understanding: “I should expect to feel full effect of my medication in 2-4 weeks” - Side effects; dizziness, myalgia, blurry vision, tachycardia - ADR: XEROSTOftIA = dry mouth b) Benzodiazepines - Short-term medication for GAD and panic disorders - habit-forming (physical dependence) - take with food to decrease GI disturbances - Acute Toxicity—gastric lavage + activated charcoal, antidote: flumazenil, ABC! o Oral: drowsiness, lethargy, confusion o IV: respiratory depression, severe hypotension, cardiac arrest - Side effects: CNS depression—“this medication can affect your ability to drive or handle mechanical equipment” - Anterograde amnesia = memory recall after dose—withhold dose and notify provider - Rapid withdrawal has been associated with anxiety, insomnia, diaphoresis, tremors, lightheadedness, delirium and development of seizures; Discontinue by gradually tapering it off over time. ˚ Alprazolam (Xanax) ˚ Lorazepam (Ativan) ˚ Diazepam (Valium) ˚ Chlordiazepoxide (Librium) ˚ Clonazepam (Klonopin) Antidepressants [https://www.youtube.com/watch?v=l8pObJTzRzY] - 2-3 weeks delay to feel full therapeutic effects - Anticipate greatest risk of attempting suicide as affect and energy improve a) SSRIs = +se - First line of treatment for depression, panic disorders, and trauma/stress-related disorders - Long half-life; 4 weeks to produce therapeutic effect - ADR: sexual dysfunction (impotence, delayed/absence orgasm/ejaculation, decreased sexual interest), wt gain, HA, GI bleed with anticoagulants, hyponatremia with diuretics, serotonin syndrome with other medications that affects serotonin reuptake in the brain, bruxism - Withdrawals = nausea, sensory disturbances, anxiety, tremors, malaise, uneasiness ˚ Paroxetine (Paxil) - Rapidly absorbed; increased for withdrawal - CNS stimulation causing insomnia - Pregnancy risk category D ˚ Sertraline (Zoloft) - Safer for pregnant and breast-feeding ˚ Fluoxetine (Prozac) - Longest half-life; less withdrawal, more toxicity = serotonin syndrome! b) SNRIs = +se, +ne - Used for ftDD, panic disorders and GAD - ADR: ALftOST THE SAftE AS SSRIs; wt loss in anorexia; HA, nausea, agitation, anxiety, dry mouth, sleep disturbances, HTN, sexual dysfunction; hyponatremia with diuretics; GI bleed with anticoagulants ˚ Venlafaxine (Effexor) ˚ Duloxetine (Cymbalta) - Contra with Alcohol Use Disorder or hepatic disease ˚ ftirtazapine (Remeron) - Increases appetite c) Tricyclic Antidepressants (TCA) = +se, +ne, -ach, -his, -na, -ca - For depressive disorders - Can take 10-14 days to work; 4-8 weeks for full effects - Common side effects: anticholinergic effects, drowsiness/sedation, orthostatic hypotension - Contraindication for pts with seizure disorder d/t effect on decreasing sz threshold - ftay increase suicide risk - Overdose = widened QRS - PRIORITY-SETTING FRAftEWORK: Urinary retention can lead to bladder infection and loss of bladder tone, notify ftD immediately! ˚ Imipramine (Tofranil) - Used for bedwetting in children ˚ Amitriptyline (Elavil) ˚ Doxepine - Antidote: bicarbonate d) ftonoamine Oxidase Inhibitor (ftAOI) = +se, +da, +ne - CNS stimulation = anxiety, agitation, hypomania, mania - Contraindicated with sympathomimetics, SSRIs, TCAs, - HTN Crisis if taken with products containing tyramine (e.g. aged cheese, pepperoni, salami, avocados, figs, bananas, smoked fish, beer, red wine) and ephedrine (e.g. Pseudoephedrine, phenylephrine) ˚ Phenelzine ˚ Tranylcypromine ˚ Selegiline = transdermal patch; affects only the dopamine - Good for Parkinson’s Disease e) Atypical ˚ Bupropion (Wellbutrin) = dopamine + NE - Lower sz threshold; contra with head injury and eating disorders ˚ Trazodone (Desyrel) = +se, -se - Used for sleep; - ADR: Priapism “trazobone” Antimanic/ftood Stabilizers ˚ Lithium carbonate (Lithobid) - Therapeutic: 0.5-1.5mEq/L (for acute mania); 0.6-1.2mEq/L (for long term control) o Side effects: polyuria, fine hand tremors will subside with continued use - Lithium toxicity = 2.0 – 2.5 mEq/L o ftonitor for ADR: ataxia, oliguria, blurred vision - Drink 6-8 glasses of water a day to maintain a normal state of hydration - ftonitor renal function, thyroid function and make sure pt is not pregnant - Take medication with meals - Consume adequate amount of sodium to prevent lithium toxicity - Safe to administer with anticonvulsants--valproic acid, carbamazepine, and lamotrigine to treat Bipolar Disorder - Interacts with o NSAIDs = lithium toxicity o Haloperidol = EPS, TD o Diuretics = promote sodium loss Anticonvulsants - Used for mood stabilizer—used to treat/prevent relapse of manic and depressive episodes in Bipolar disorders ˚ Carbamazepine (Tegretol) - Therapeutic level = 4-12 mcg/mL - Teratogenic ˚ Valproic Acid, or Divalproex Sodium (Depakote), or Valproate Sodium - Treats acute mania - Therapeutic level = 50-120 mcg/mL - Teratogenic - “you should have your LFT monitored regularly” due to risk of hepatotoxicity. - Take baseline level and then repeat every 2 months during the first 6 months of therapy ˚ Lamotrigine (Lamictal) - ftaintenance therapy for bipolar mania - Needs to be slowly titrated to reduce r/o ADR - ftonitor for s/s SJS ftedications for ADHD a) CNS Stimulants - ADR: CNS stimulation—insomnia and restlessness, appetite and growth suppression, CV effects— dysrhythmias, CP, HBP; hallucinations and paranoia - Withdrawal: HA, n/v, muscle weakness, depression—do not D/C abruptly! - Toxicity = dizziness, palpitations, HTN, hallucinations, sz ˚ ftethylphenidate (Ritalin, Concerta) ˚ ftethylphenidate patch (Daytrana) - Alternate hips daily - Keep for no longer than 9 hours - Flush in the toilet - can be worn in the shower; notify ftD for skin reaction - reaction to patch = reaction to PO—may need to change medication ˚ Amphetamine (Adderall) b) Non-stimulants ˚ Atomoxetine (Strattera) and Bupropion (Wellbutrin) - SNRIs = suicidal ideations - Atomoxetine is contraindicated with pts who have angle-closure glaucoma and pheochromocytoma - Bupropion is contraindicated with purging-type eating disorders ˚ Guanfacine (Tenex) - Alpha2-adrenergic agonist ftedications for Substance Use Disorders 1. Alcohol - Withdrawal ˚ Benzodiazepines: chlordiazepoxide, diazepam, lorazepam - Administer ATC - Abstinence – following withdrawal ˚ Disulfiram (Antabuse) - Alcohol + disulfiram = acetaldehyde syndrome [hyperventilation, dizziness, vomiting, hypotension] - Avoid alcohol or alcohol-containing substances e.g. pure vanilla extract ˚ Naltrexone PO (ReVia), Ift (Vivitrol) ˚ Acamprosate (Campral) - Diarrhea is common - Detoxification ˚ Benzodiazepines: diazepam and chlordiazepoxide - Long-acting CNS depressant to minimize manifestations of alcohol withdrawal 2. Nicotine ˚ Bupropion (Wellbutrin) - Decreases cravings and manifestations of withdrawals ˚ Nicotine gum, patch, spray, or lozenges - Replaces cigarettes and tobacco - Gum: chew slowly and intermittently for over 30 min; do not eat or drink 15 minutes before and while chewing the gum; do not use for >6 months - Patch: discontinue if local skin reaction occurs; wear 16hrs during the day—remove HS to reduce r/o nightmares and sleep disturbances - Spray: one spray in each nostril = 1 cigarette - Lozenges: allow to dissolve 20-30 minutes, limit use to 5-6h period or max 20 lozenges/day ˚ Varenicline (Chantix) - Reduces cravings and manifestations of withdrawals - ftonitor T2Dft for loss of glycemic control - Can cause neuropsychiatric episodes—behavior/mood changes, and suicidal thoughts 3. Opiate ˚ Antidotes: Naloxone (Narcan) and Flumazenil - Naloxone can be given Ift, SQ, IV, and inhalation - Flumazenil can be given IV - Flumazenil = benzodiazepine antagonist - Reverse toxicity and sedative effects such as respiratory depression and coma ˚ ftethadone - substitute to prevent cravings and severe manifestations of withdrawals - must be administered from an approved treatment center; cannot be prescribed and dispensed ˚ Buprenorphine (Belbuca) - Used for both withdrawal and maintenance ftedications for Alzheimer’s Disease a) Cholinesterase Inhibitor - Slows cognitive deterioration of AD in mild-moderate stages - Contraindicated with asthma=increased acetylcholine can cause bronchoconstriction ˚ Donepezil (Aricept) - “can improve cognitive functioning during the earlier stages of the disease” - Administer at HS to reduce risk for injury d/t bradycardia and syncope ˚ Rivastigmine (Exelon) - Available in PO and patch—administered once daily ˚ Galantamine (Razadyne) b) NftDA receptor agonist - Blocks entry of calcium into nerve cells = slows brain-cell death ˚ ftemantine (Namenda) - For moderate-severe stages of AD [Show More]
Last updated: 1 year ago
Preview 1 out of 15 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 08, 2021
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Jun 08, 2021
Downloads
0
Views
22




.png)



 - Copy (2).png)

