*NURSING > STUDY GUIDE > NURS 611 Pathophysiology Exam TWO Study Guide Contains Exam Tested Questions with Answers (Maryville (All)
NURS 611 Pathophysiology Exam TWO Study Guide Contains Exam Tested Questions with Answers (Maryville University)
Document Content and Description Below
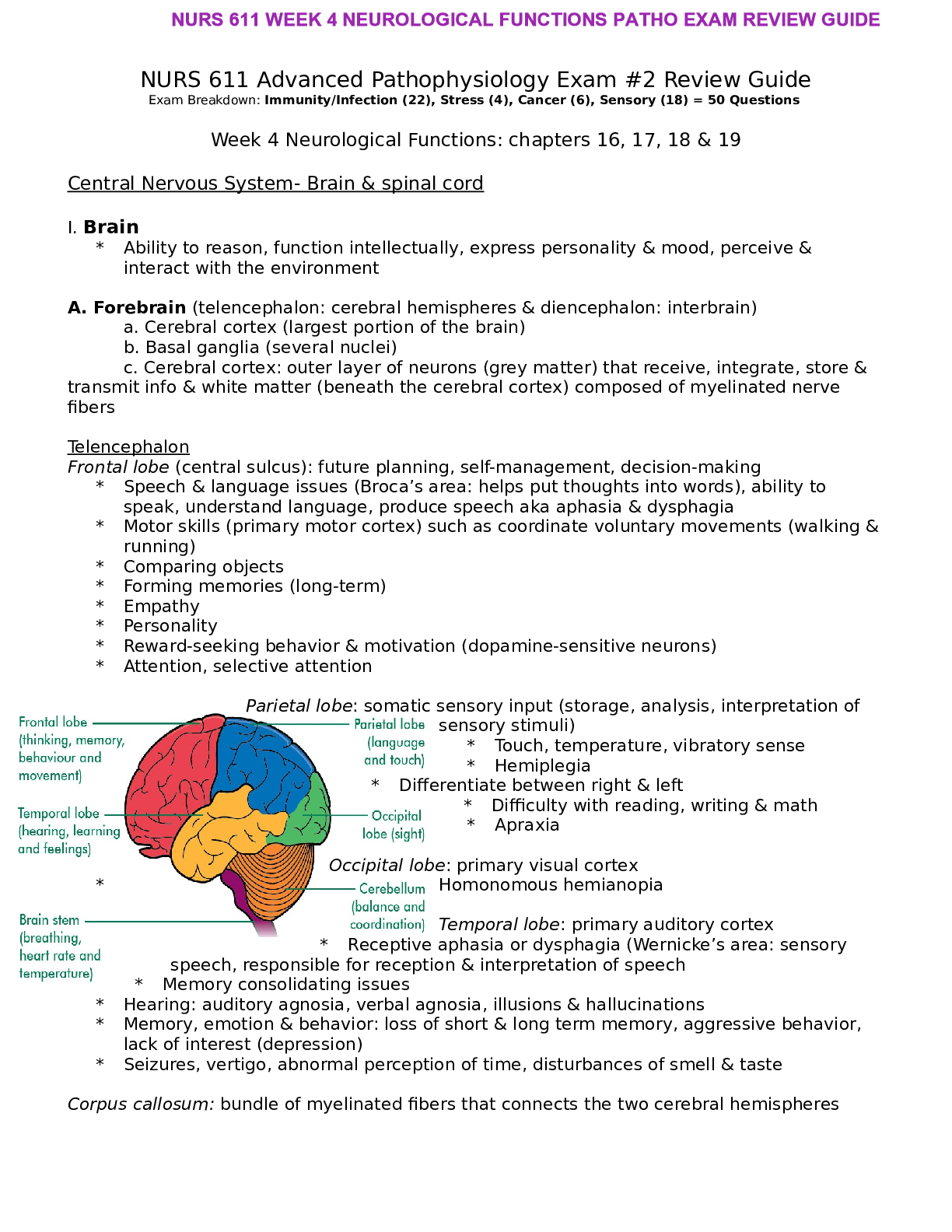
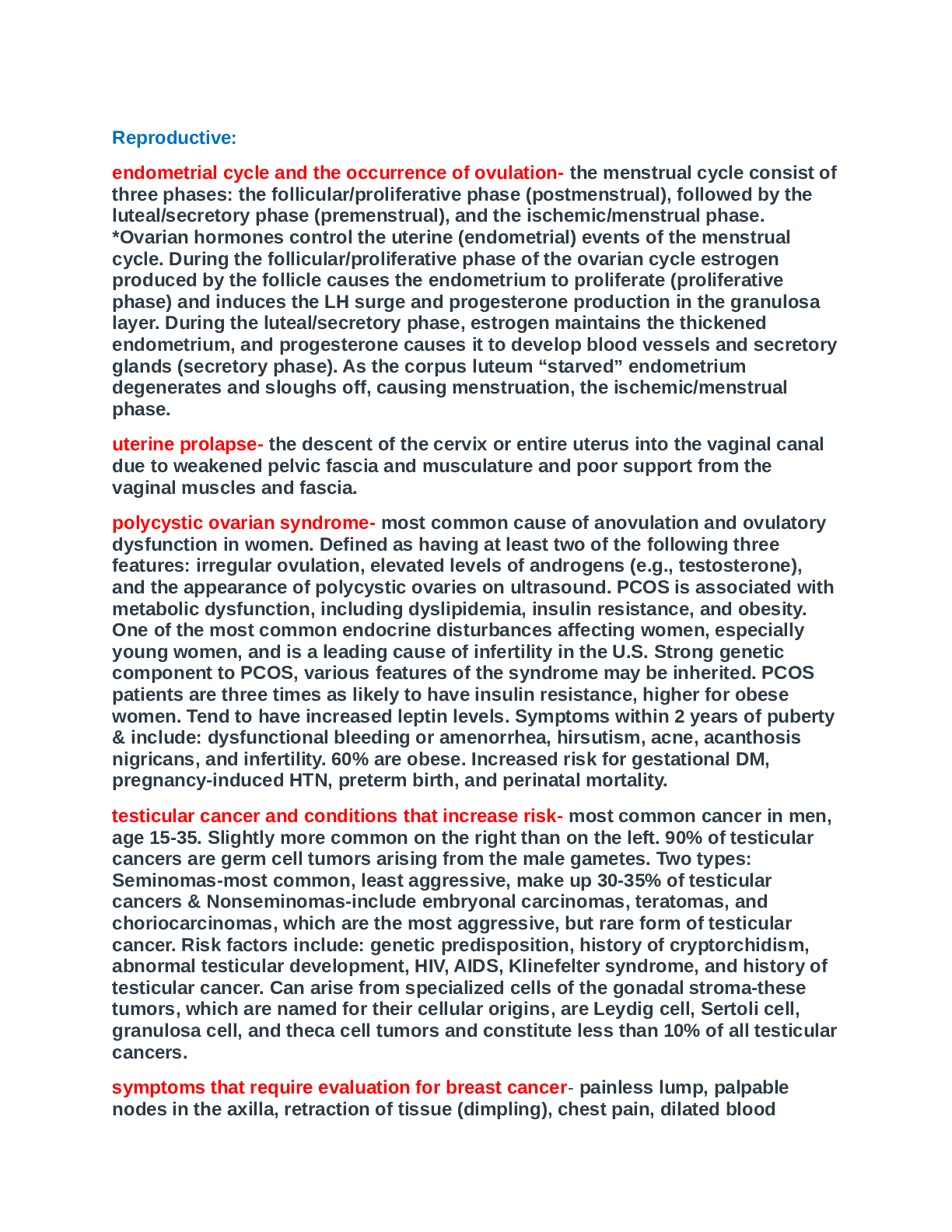
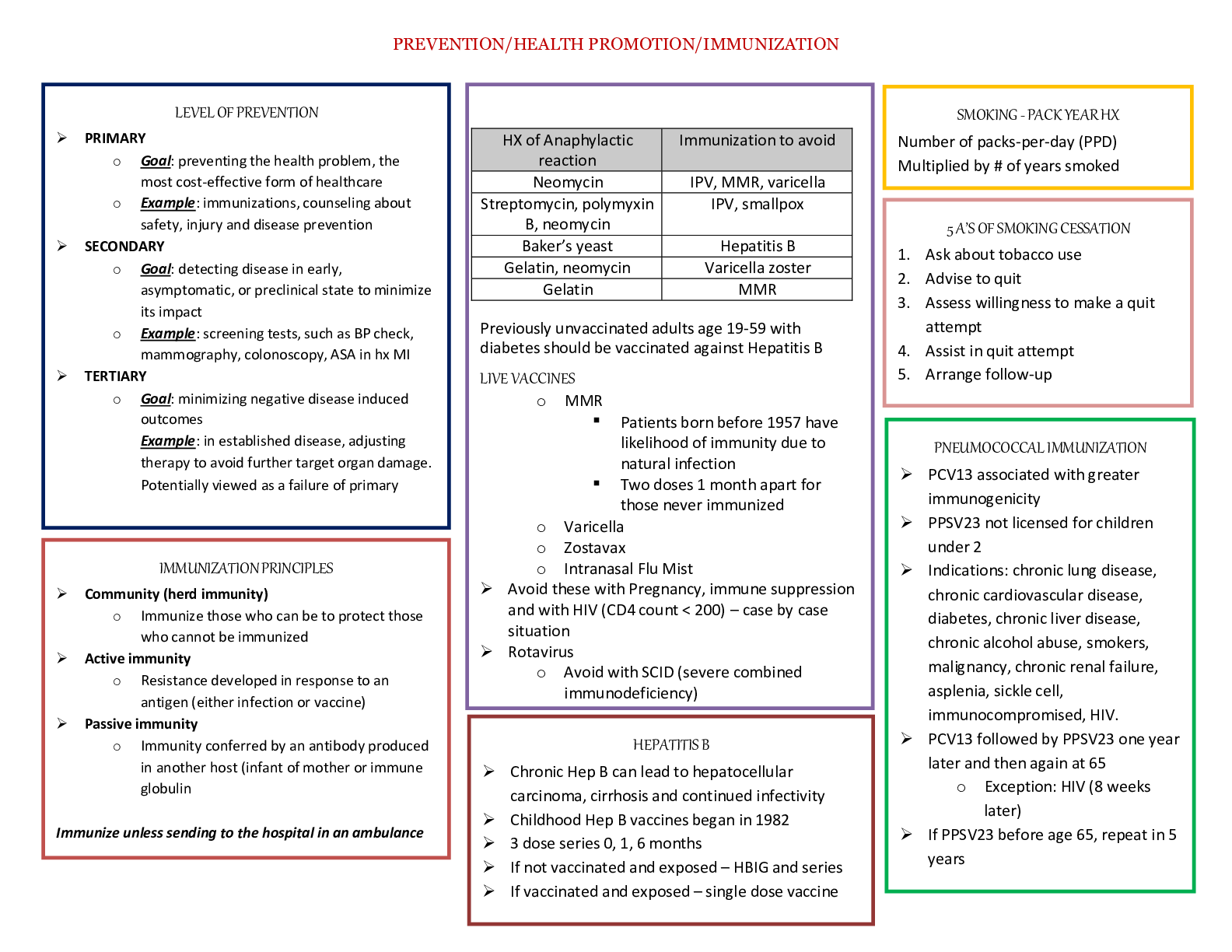
NURS 611 Advanced Pathophysiology Exam #2 Review Guide Exam Breakdown: Immunity/Infection (22), Stress (4), Cancer (6), Sensory (18) = 50 Questions Week 4 Neurological Functions: chapters 16, 17, ... 18 & 19 Central Nervous System- Brain & spinal cord I. Brain * Ability to reason, function intellectually, express personality & mood, perceive & interact with the environment A. Forebrain (telencephalon: cerebral hemispheres & diencephalon: interbrain) a. Cerebral cortex (largest portion of the brain) b. Basal ganglia (several nuclei) c. Cerebral cortex: outer layer of neurons (grey matter) that receive, integrate, store & transmit info & white matter (beneath the cerebral cortex) composed of myelinated nerve fibers Telencephalon Frontal lobe (central sulcus): future planning, self-management, decision-making * Speech & language issues (Broca’s area: helps put thoughts into words), ability to speak, understand language, produce speech aka aphasia & dysphagia * Motor skills (primary motor cortex) such as coordinate voluntary movements (walking & running) * Comparing objects * Forming memories (long-term) * Empathy * Personality * Reward-seeking behavior & motivation (dopamine-sensitive neurons) * Attention, selective attention Parietal lobe: somatic sensory input (storage, analysis, interpretation of sensory stimuli) * Touch, temperature, vibratory sense * Hemiplegia * Differentiate between right & left * Difficulty with reading, writing & math * Apraxia Occipital lobe: primary visual cortex * Homonomous hemianopia Temporal lobe: primary auditory cortex * Receptive aphasia or dysphagia (Wernicke’s area: sensory speech, responsible for reception & interpretation of speech * Memory consolidating issues * Hearing: auditory agnosia, verbal agnosia, illusions & hallucinations * Memory, emotion & behavior: loss of short & long term memory, aggressive behavior, lack of interest (depression) * Seizures, vertigo, abnormal perception of time, disturbances of smell & taste Corpus callosum: bundle of myelinated fibers that connects the two cerebral hemispheres Basal ganglia (contains substantia nigra): coordination of voluntary movements, cognitive & emotional function Extrapyramidal system: motor control system that causes involuntary reflexes, has a stabilizing effect on motor control Limbic System (group of interconnected structures located between the telencephalon & diencephalon): mediates emotion, long-term memory, behavioral responses, visceral reaction to emotion, motivation, mood, feeding behaviors, biologic rhythms, sense of smell ⟶ Amygdala ⟶ Hippocampus ⟶ Fornix ⟶ Hypothalamus Diencephalon Thalamus: major integrating system for afferent (sensory) stimuli to the cerebral cortex * Relay center for info from basal ganglia & cerebellum to the appropriate motor area * Cortical processing for interpretation Hypothalamus: maintain constant internal environment & implement behavioral patterns * Autonomic (sympathetic & parasympathetic NS) nervous system function, regulate body temperature, endocrine function- hormone synthesis, adjust emotional expression B. Midbrain Superior colliculi: voluntary & involuntary visual motor movements (eyes to track moving objects) Inferior colliculi: similar motor activities; involve movements affecting the auditory system Tegmentum (composed of the red nucleus & substantia nigra): Red nucleus- receives ascending sensory info from the cerebellum, substantia nigra- synthesizes dopamine (PD) C. Hindbrain (metencephalon & myelencephalon) Metencephalon Cerebellum: two lobes; reflexive, involuntary fine-tuning of motor control, maintaining balance & posture through extensive neural connections with the medulla * Ipsilateral (same side) control of the body (contrast to cerebral cortex) Pons: transmits info from the cerebellum to the brainstem between the two cerebellar hemispheres * Nuclei of the 5th to the 8th cranial nerves Myelencephalon (Medulla oblongata) Lowest portion of brainstem * * Reflex activities such as HR, RR, BP, coughing, sneezing, swallowing & vomiting * Nuclei of cranial nerves 9th to 12th II. Spinal cord * Transmit long motor & sensory tracts that originate in the brain and synapse with cell bodies in gray matter of the spinal cord before exiting to the body * Somatic & autonomic reflexes, motor pattern control centers, sensory & motor modulation * Divided into sections: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral & 1 coccygeal Peripheral Nervous System * Nerves outside the CNS * Somatic NS controls voluntary muscle movement (efferent nerves) and sensory info (afferent nerves) * Cranial & spinal nerves Autonomic Nervous System * Regulates involuntary function of internal organs * Part of the efferent division of the PNS * Separated by two divisions: sympathetic nervous system & parasympathetic nervous system Parasympathetic & Sympathetic NS ➢ Body organs are innervated by these two nervous systems ➢ The two divisions cause opposite responses (Ex: sympathetic stimulation of the GI tract causes peristalsis, whereas parasympathetic stimulation peristalsis) ➢ Release acetylcholine via cholinergic transmission I. Parasympathetic Nervous System: conserves/stores energy and the body’s resources ➢ Parasympathetic activity promotes rest & tranquility ➢ HR and enhanced visceral functions leading to digestion ➢ Lacks the generalized & widespread response of the sympathetic system, specific parasympathetic fibers are activated to regulate particular functions II. Sympathetic Nervous System: Promotes responses that are concerned with the protection of the individual ➢ Responds to stress by preparing the body to defend itself “fight or flight” ➢ Sympathetic stimuli blood glucose, temperature & BP * Regulation of vasomotor tone is considered the single most important function ➢ Postganglionic sympathetic fibers release norepinephrine (adrenaline) & thus are considered to function by adrenergic transmission ➢ Action of catecholamines (epinephrine, norepinephrine, dopamine) varies with the type of neuroreceptor stimulated; released by adrenal medulla (resembles sympathetic NS ➢ Dopamine is a precursor of NE and Epinephrine, synthesized by substantia nigra ➢ Mobilizes energy stores, and decreases the release of insulin ➢ Redistributes blood flow: increases to muscles (flight) and lungs, decreases to GI & integumentary Traumatic Brain Injury: can be classified as focal or diffuse - Primary brain injuries are caused by the direct impact or injury ➢ Focal: specific, involving one area of the brain. Direct impact Ex: Scalp laceration, skull fracture, contusions, hemorrhage: epidural, subdural, intracerebral, subarachnoid ➢ Diffuse: involving more than one area of the brain. Ex: Hypoxia, meningitis, encephalitis, and damage to blood vessels - Swelling, commonly seen after TBI can lead to dangerous increases in intracranial pressure (ICP) ➢ Increased ICP can cause collateral dysfunction such as diabetes insipidus (ADH not secreted thus polyuria) Autonomic hyperreflexia (Dysreflexia): Syndrome of sudden, life-threatening massive reflex sympathetic discharge associated with spinal cord injury. T5-T6 or above - Common cause is a distended bladder or rectum however any sensory stimulation can elicit dysrreflexia Characterized by: ➢ Paroxysmal HTN (up to 300 mmHg systolic) ➢ Pounding headache ➢ Blurred vision ➢ Sweating above the level of the lesion with flushing of the skin * Disturbed thermal control r/t inability for hypothalamus to regulate body heat as a result of a damaged sympathetic NS ➢ Bradycardia (HR <40 bpm) ** Stimulation of the carotid sinus to the vagus nerve to the SA node Delirium & Dementia Feature Delirium Dementia Age Usually older Usually older Onset Acute (hospitalization stay) Usually insidious; acute in stroke/trauma cases Associated conditions UTI Thyroid disorders Hypoxia Hypoglycemia Toxicity Fluid & electrolyte imbalance Renal insufficiency Trauma Multiple medications May not have any other conditions Brain trauma Course Fluctuating; remits with treatment Chronic slow decline Duration Hours-weeks Months-years Attention Impaired Intact early; often impaired late Orientation Impaired Intact early; impaired late Behavior Agitated, withdrawn/depressed Intact early Thoughts Disorganized, delusions Impoverished Perception Hallucinations/illusions Usually intact early Alzheimer Disease: dementia of Alzheimer type (DAT), senile disease complex ➢ Leading cause of dementia and one of the most common causes of severe cognitive dysfunction in older adults ➢ Greatest risks are age & family history ➢ Exact cause is unknown. No clear understanding of this complex disease process. ➢ Diagnosis is made by postmortem examination Cerebrovascular Accident (Stroke) ➢ Incidence is 2X higher in blacks than whites, runs in families ➢ No identifiable cause can be established by conventional diagnostic tests in many ischemic strokes and they are classified as “undetermined” or “cryptogenic” ➢ Outcomes: Unnoticeable --- most severe include hemiplegia, coma, and death Classified according to pathophysiology: ischemic (thrombotic or embolic), global hypoperfusion (shock), intracerebral hemorrhage Classification Cause Prevalence Risk Factors Ischemic Obstruction to an arterial blood flow to the brain, an embolus associated with atherosclerosis or hypoperfusion related to decreased blood volume 87% *HTN - Vasoconstriction from malignant HTN - Atherosclerosis - Inflammatory disease Thrombotic Arterial occlusions caused by thrombus formation in large or small arteries supplying the brain or intracranial vessels Embolic Fragments that break from a thrombus formed outside the brain usually in the heart, aorta, or common carotid artery * Second stroke usually follows bc the emboli continues to exist 15-25% of ischemic strokes - AF - Atrial thrombus - MI - Rheumatic valvular disease - Mechanical prosthetic valve -Thrombotic endocarditis - Patent foramen ovale - Intracardiac tumors Lacunar Perivascular edema, thickening and inflammation of the arteriolar wall in deep perforating artery that supplies small penetrating subcortical vessels 25% of ischemic strokes - HL - Smoking - HTN - DM Hemodynamic (global hypoperfusion) Shock - HF - Pulmonary embolism - Bleeding Hemorrhagic Mass of blood is formed as bleeding occurs into the brain tissue. Brain tissue is deformed, 10% * HTN - Tumors - Coagulation disorders compressed and (polycythemia & displaced producing thrombocythemia) ischemia, edema, IICP, - Trauma necrosis - Illicit drug use ➢ Risk factors: HTN, insulin resistance and DM, HL, low HDL, PVD, heart disease, AF, postmenopausal hormone therapy, high sodium intake ( > 2300mg), low potassium ( < 4700mg), smoking, physical inactivity, obesity, chronic sleep deprivation Middle Cerebral Artery: Either stem or branches of MCA Description Signs & Symptoms 1 of 3 major paired arteries that supply blood to the cerebrum - Arises from the internal carotid & continues into the lateral sulcus where it then branches & projects to many parts of the lateral cerebral cortex • Motor: contralateral hemiparesis or hemiplegia, greater in face & arm than leg • Sensation: contralateral loss in same distribution as motor loss • Speech: expressive (motor), disorder with anomia (left hemisphere) with nonfluent aphasia and some comprehension defects • Vision: contralateral homonymous hemianopsia or quadranopsia • Respirations: cheyne-stokes, contralateral hyperhidrosis, occassional mydriasis • Sensory: little or no loss. If present, contralateral following the motor distribution • Perception: transient visual & sensory neglect on the left if a right lesion Guillain-Barre Syndrome: autoimmune disease triggered by a preceding bacterial or viral infection ▪ Demyelinating disorder caused by a humoral (antibody) & cell-mediated immunological reaction directed at the peripheral nerves ▪ Occurs after a respiratory or GI infection ▪ Has been associated with surgery, immunization, & viral infections including the Zika virus Clinical manifestations: ascending flaccid paresis (starting in the legs to complete quadriplegia, respiratory insufficiency, & autonomic nervous system instability ▪ Weakness usually plateaus or improves by the 4th week in 90% of cases ▪ After weakness plateaus, strength improves over a period of days to months, individuals reaching baseline activity levels ▪ Respiratory muscle weakness leads to need for mechanical ventilation in 10-30% individuals ▪ Cranial nerve: chewing, swallowing, & coughing Diagnostic criteria include progressive weakness of more than two limbs, arereflexia and progression for no more than 4 weeks ▪ IV immunoglobulin or plasmapharesis ▪ Aggressive rehab Multiple Sclerosis: chronic inflammatory disease involving degeneration of CNS myelin, scarring or formation of plaque, and loss of axons ▪ Autoimmune response to self-antigens in genetically susceptible individuals ▪ Risk factors include smoking, vitamin D deficiency, & Epstein-Barr virus --> First demyelinating event, or “clinically isolated syndrome” (CIS), is a single episode of neurologic dysfunction lasting greater than 24 hours that can prelude to MS (optic neuritis, solitary brainstem lesions, transverse myelitis) ▪ As the disease progresses, inflammatory changes in the CNS increase, and loss of brain volume progresses more rapidly ▪ The demyelination disrupts sodium, calcium, & potassium ion channels and calcium influx is proinflammatory & neurotoxic ▪ Activated microglia & macrophages release nitric oxide and free radicals Clinical manifestations: 90% of persons present with a relapsing, remitting course. 10% present with a primary progressive course. 90% develop a progressive course in 10-20 years after onset of the disease. ▪ Once walking problems develop, disease progression occurs quickly regardless of disease typ Myasthenia Gravis: Chronic autoimmune disease mediated by acetylcholine receptor (AChR) antibodies that act at the neuromuscular junction • Results from a defect in nerve impulse transmission • The main defect is T-cell-dependent formation of autoantibodies against nicotinic AChR, muscle-specific kinase, lipoprotein-related protein 4, or agrin in the postsynaptic membrane • Destruction of receptor sites occurs, decreasing the number of receptors on the plasma membrane and causing diminished transmission of nerve impulses Clinical Manifestations: insidious onset, variable distribution of Ach receptor sites or the # of and different isoforms of antibodies may determine when and which muscle groups are affected first ➢ Exertional fatigue & weakness that worsens with activity, improves with rest, and recurs with resumption of activity ➢ Recent history of URI ➢ Diplopia, ptosis, and ocular palsies ➢ Facial droop & expressionless face; difficulty chewing, swallowing, weight loss & drooling ➢ Episodes of aspiration & choking Parkinson’s Disease: complex motor disorder accompanied by systemic non-motor & neurologic symptoms • Pathogenesis unknown • Loss of dopaminergic pigmented neurons in the substantia Nigra (SN) & other brain areas: brainstem, thalamus & cortex • Degeneration of the basal ganglia Clinical Manifestations: onset is insidious, symptoms appear after 70-80% loss of pigmented nigral neurons and 60-70% loss of striatal dopamine ➢ Resting tremor, rigidity, bradykinesia/akinesia, postural disturbance, dysarthria, & dysphagia ➢ Wide-eyed, unblinking, staring expression ➢ Shuffling steps; arms flexed, held stiffly at the side, trunk bent forward Acute & Chronic Pain Acute Pain Chronic Pain Experience An event - Somatic pain (muscles, bone joints, skin; sharp/well localized) - Visceral (C-fibers, pain to internal organs; aching/gnawing/throbbing/cramp ing) - Referred (felt in an area removed or distant from its point of origin; supplied by same spinal segment as the actual site of pain) A situation; state of existence Source External agent or internal Unknown; if known, disease usually known treatment is prolonged or ineffective Onset Usually sudden May be sudden or develop insidiously Duration Transient (up to 6 months) Prolonged & persistent (months-years) Clinical Signs HR, BP, RR, diaphoresis, dilated pupils Response pattern varies, fewer overt signs (adaptation) Prognosis Likelihood of eventual complete relief Complete relief usually not possible Chronic Pain: ongoing or intermittent, changes in peripheral & central nervous systems that cause dysregulation of nociception & pain modulation processes are thought to be the causes Condition Description Persistent low back pain Most common Myofascial pain syndromes Second most common - Results from muscle spasm, tenderness, & stiffness Ex: myositis, fibrositis, myofibrositis, myalgia, & muscle strain (conditions that involve injury to muscle & fascia) Deafferentation pain Painful condition resulting from damage to a peripheral nerve - Common types include severe burning pain triggered by various stimuli such as cold, touch, sound, reflex sympathetic dystrophies (continuous, severe, burning pain associated with vasomotor changes & muscle wasting) Phantom pain Experienced in amputated limb after stump has completely healed; may be immediate or occur months later Headaches • Common neurologic disorder, usually benign. Can be associated with serious disease such as brain tumor, meningitis, giant cell arthritis & CVA Migraine with or without aura Cluster headache/Proximal hemicrania Tension type of headache Age of onset Childhood, adolescence, or young adulthood Young adulthood, middle age Young adulthood, middle age Gender Female Male NA Family history Yes No Yes Onset & evolution Slow to rapid Rapid Slow to rapid Time course Episodic Clusters in time Episodic, may become constant Quality Usually throbbing Steady Steady Location Variable, often unilateral Orbit, temple, cheek Variable Associated features Prodrome, vomiting Lacrimation, rhinorrhea, Harner syndrome NA Sleep deprivation: serious disturbances of the sleep-wake cycle are observed in many people under stress & in many clinical settings • Circadian disruption (rapid time-zone changes & shift workers) • Detrimental influence on respiratory & immune function • Reduced NK cell activity in healthy individuals Vision: Glaucoma • Intraocular pressures greater than 12 to 20 mmHg • Death of retinal ganglion cells & optic nerve axon degeneration with myopia & loss of peripheral vision, followed by central vision impairment & blindness. Loss of visual acuity results from pressure on the optic nerve • Leading cause of visual impairment & blindness • Open-angle glaucoma: most common The Ear: Hearing Loss • Ear is divided into 3 areas: (1) external ear, involved only with hearing, (2) middle ear, involved only with hearing and (3) inner ear, involved with hearing Conductive hearing loss: interference in air conduction ➢ Conditions: impacted cerumen, foreign bodies lodged in the ear canal, benign tumors of the middle ear ➢ S/S: diminished hearing, soft Open-Angle Glaucoma Narrow-Angle Glaucoma Obstruction of outflow of Blocked drainage of aqueous humor at aqueous, anterior trabecular meshwork or chamber angle very Schlemm canal; myopia narrow therefore may be a risk factor reducing fluid outflow speaking voice (r/t individual hearing his or her voice, conducted by bone, as loud) ➢ Hears better in a noisy environment than in a quiet one Sensorineural hearing loss: caused by impairment of the organ of corti ➢ Conditions: noise exposure, aging, Meniere disease, ototoxicity, and systemic disease (syphillis, Paget disease, collagen diseases, DM) Presbycusis: age-related hearing loss usually in the high frequencies ➢ Most common form of sensorineural hearing loss and is especially common in older adults Week 5 Alterations in Immunity, Infection and Stress: Chapters 7, 8 & 9 o Humans has 2 types of defense mechanisms: first is innate (natural barriers; skin and mucous membranes) & second is adaptive (acquired) Inflammatory Response: body’s 2nd line of defense o Nonspecific, Rapidly initiated, NO memory cells o Vascular response—vasodilation, capillary permeability & WBC adherence to inner vessel walls o Systemic effects of inflammation are fever, leukocytosis and increase in circulating plasma proteins Benefits of inflammation include: A) Prevention of infection & further damage by contaminating microbes o Via influx of fluid to dilute toxins o Influx & activation of plasma protein synthesis (help destroy & contain bacteria- complement system and clotting system) o Influx of cells (neutrophils and macrophages) that eat & destroy cellular debris B) Limitation & Control o Influx of plasma protein systems, plasma enzymes, and cells that prevent the inflammatory response from spreading to areas of healthy tissue C) Interaction with components of the adaptive immune system to elicit a more specific response to pathogens through macrophages & lymphocytes D) Preparation of the area of injury for healing via removal of bacterial products & dead cells o Channels through epithelium or drainage by lymphatic vessels o Initiation of mechanisms of healing & repair Plasma Protein Systems: biochemical barrier against invading pathogens in the circulation o Complement pathways, results in opsoinization, activation of anaphylatoxins, cell lysis, leukocyte chemotaxis o Clotting cascade prevents spread of microbes: platelets interact with the coagulation cascade to stop bleeding & release a number of mediators that promote & control inflammation o Kinin system: promote vasodilation & capillary permeability and induce pain Principal Mediators of Inflammation o Eosinohpils- control mast cell vascular mediators & defend against parasite infections o Cytokines- regulate inflammatory response (interleukins, interferons, tumor necrosis factor) o Tumor necrosis factor- produced by macrophages and promotes inflammation with local & systemic effects First Defense: Skin & Mucous membranes Second Defense- The Inflammatory Process: occurs when the first line of defense (physical, mechanical & biochemical barriers) is breached Inflammatory response: 1. Occurs in tissues with a blood supply 2. Activated rapidly after damage occurs 3. Depends on the activity of both the cellular & chemical components 4. Nonspecific; takes place in the same way regardless of the type of stimulus or whether exposure to the same stimulus has occurred in the past Four Cardinal Signs o Edema: arterioles near the site of infection or injury constrict briefly. Vasodilation increases local blood flow to the injured site causing swelling (edema) in the surrounding tissue o Warmth & Redness: Increased blow flow & increasing concentration of RBCs at the site of inflammation cause locally increased warmth and redness ➢ Leukocytes adhere to vessel walls. Chemotactic factor helps them find their way o Pain: Biochemical mediators (histamine, bradykinins, leukotrienes, prostaglandins) Phagocytosis: destruction of microbes and cellular debris o Two most important phagocytes: neutrophils and macrophages * Both cells must leave blood circulation and migrate to the site of inflammation before process can begin The 4 step process (1) Opsonization-recognition of the target and adherence of the phagocyte to it (2) Engulfment- ingestion or endocytosis, and formation of phagosome (3) Fusion with lysosomal granules within the phagocyte (phagolysosome) (4) Destruction of the target Systemic Inflammation: three systemic changes associated with the acute inflammatory response are fever, leukocytosis, and plasma protein synthesis I. Fever o Induced by specific cytokines aka endogenous pyrogens o Pyrogens act on hypothalamus, released after phagocytosis, after exposure to bacterial endotoxins, or after exposure to antigen-antibody complexes o Febrile response can be beneficial b/c the microbes that cause this condition (syphilis, gonococcal urethritis) are highly sensitive to small increases in body temperature II. Leukocytosis o Increase in the # of circulating WBCs (> 11,000/mL3) o Can be associated with a left shift in the ratio of immature to mature neutrophils. Production of immature leukocytes increases primarily from proliferation and release of granulocyte and monocyte precursors in the bone marrow, which is stimulated by several products of inflammation, including complement C3a and G-CSF III. Plasma Protein Synthesis o Increased during inflammation, occurs in the liver o These proteins can be pro-inflammatory or anti- inflammatory are referred to as acute-phase reactants o Common lab tests- fibrinogen (r/t increased adhesion among erythrocytes), sedimentation rate (alteration in plasma proteins leads to an enhanced erythrocyte rouleaux formation) Adaptive (Acquired) Immunity: 3rd line of defense Distinguished by being inducible, specific, long-lived, and having memory o Lymphocytes and Serum proteins called antibodies o Can be through active or passive immunity, depends on whether the antibodies or T cells are produced by the person or are administered directly A. Humoral Immunity: antibody circulates in the blood & binds to antigens on infectious agents B. Cellular Immunity: T-cells undergo differentiation during an immune response & develop into several subpopulations of cells that react directly with antigen on the surface of infectious agents o Some develop into T cells that stimulate activities of other leukocytes via cell-to-cell contact or through the secretion of cytokines o Others develop into T-cytotoxic cells (Tc cells) that attack & kill targets directly o Targets for Tc cells include cells infected by a variety of viruses, as well as cells that have become cancerous Active vs. Passive Immunity o Active acquired immunity (active immunity): produced by an individual either after a) antigen or b) immunization o Passive acquired immunity (passive immunity): does not involve the host’s immune system. Occurs when preformed antibodies or T lymphocytes are transferred from a donor to a recipient (breast milk). This can occur naturally or artificially (clinic using immunotherapy for a specific disease such as Hep A or rabies) Classes of Immunoglobulins (Antibodies) o Serum glycoprotein produced by plasma cells in response to a challenge by an immunogen o Term immunoglobulin is used as a generic description of a general group of antibodies o Term antibodies commonly denotes one particular set of immunoglobulins known to have specificity for a specific antigen IgG - Most abundant class - Constitute 80% to 85% of those circulating in the body - Account for most of the protective activity against infections - Maternal IgG transported across the placenta during pregnancy & protects the newborn during the first 6 months of life IgA - Found in bodily secretions are dimers anchored together through a J chain “secretory piece” - This secretory piece is attached to the IgAs inside mucosal epithelial cells - Two subclasses: IgA1 (blood) and IgA2 (body secretions) IgM - Largest one - First antibody produced during the initial, or primary, response to antigen - IgM usually synthesized early in neonatal life, may be as a reponse to infection in utero IgE -Least concentrated in circulation - Mediator of many common allergic responses & in defense against parasitic infections Hypersensitivity Reactions Type I Hypersensitivity Reaction: mediated by antigen-specific IgE & products of tissue mast cells o Most common allergies (pollen, nuts) are type I reactions o Healthcare workers tend to use the term allergy to indicate only IgE-mediated reactions o Most potent mediator is histamine Type II Hypersensitivity Reaction: characterized by a specific cell or tissue being the target of an immune response o Antibody-dependent cell-mediated cytotoxicity (ADCC) is a mechanism that involves a subpopulation of cytotoxic cells that are not antigen specific (natural kill (NK) cells) o Antibody binds to the antigen on the cell surface o For ex: hyperthyroidism of Grave’s disease, autoantibody binds to & activates receptors for thyroid-stimulating hormone (TSH), a pituitary hormone that controls the production of the hormone thyroxine by the thyroid Type III Hypersensitivity Reaction: caused by antigen-antibody (immune) complexes that are formed in circulation & deposited later in vessel walls or extravascular tissue o Antibody binds to soluble antigen that was released into the blood or body fluids, complex is then deposited in the tissues o For ex: Raynaud phenomenon, condition caused by the temperature-dependent deposition of immune complexes in the capillary beds at the peripheral circulation. The precipitates block the circulation & cause localized pallor and numbness, followed by cyanosis & eventually gangrene if circulation is not restored Type IV Hypersensitivity Reaction: mediated by T lymphocytes and do not involve antibodies o Graft rejection o Allergic reactions resulting from contact (Poison ivy & metals) o T-cells rejection to type II collagen (protein in joint tissues) contribute to the destruction of joints in Rheumatoid Arthritis o T-cells against a thyroid cell surface antigen contribute to the destruction of the thyroid in Autoimmune Throiditis (Hashimoto disease) Autoimmune & Alloimmune Disease Autoimmunity: originate from the coincidence of an irritating event in genetically predisposed individual leading to an autoimmune mechanism that affects specific target cells or tissues ◆ Can be familial & attributed to the presence of a very small # of susceptible genes ◆ Breakdown of peripheral tolerance ◆ Examples: Graves disease (autoimmune, maternal antibody against the receptor for TSH causes neonatal hyperthyroidism), Myasthenia Graves (maternal antibody binds with receptors for neural transmitters on muscle cells (acetycholine receptors), causing neonatal muscular weakness --> Systemic Lupus Erythematosus (SLE), a chronic, multisystem, inflammatory disease and is one of the most common, complex, and serious of the autoimmune disorders ◆ Deposition of immune complexes containing antibodies AGAINST DNA produce tissue damage- deposited in renal tubules, heart, spleen etc. Clinical Manifestations: ◆ Facial rash confined to the cheeks (Malar rash) ◆ Photosensitivity (skin rash developed by exposure to sunlight) ◆ Renal disorder (proteinuria of 0.5 g/day or cellular casts) ◆ Neurologic disorders (seizures or psychosis) ◆ Hematologic disorders (hemolytic anemia, leukopenia, lymphopenia, or thrombocytopenia) Alloimmunity: occurs when individual’s immune system reacts against antigens on the tissues of other members of the same species ◆ Several transient neonatal diseases (maternal immune system becomes sensitized against antigens expressed by the fetus) ◆ Transplant rejection & transfusion reactions (immune system of a recipient of an organ transplant or blood transfusions reacts against antigens on the donor cells) ◆ Examples: Alloimmune neutropenia (disease in which maternal antibody against neutrophils destroys neutrophils in neonate), Rh and ABO alloimmunization (maternal antibody against erythrocyte antigens induces anemia in the child) Alloimmune reaction to ABO-mismatched transfused blood cells ◆ Individuals with type O blood lack both types of antigens they are considered universal donors, anyone can accept their RBCs ◆ Type AB individuals are considered universal recipients b/c they have both anti-A and anti-B antibodies & can be transfused with any ABO blood type ◆ Aggulination and lysis cause harmful transfusion Immunodeficiency Disorders Primary immune deficiencies- Very rare (30-50 cases/year), three most commonly diagnosed deficiencies are common variable immune deficiency (34%), selective IgA deficiency (24%), and IgG subclass deficiency (17%) Secondary or acquired immune and inflammatory deficiencies- complications of other physiologic or pathophysiologic conditions ⟶ Metabolic diseases or genetic syndromes Examples: Alcoholic cirrhosis, sickle cell disease, SLE ⟶ Environmental Agents Examples: UV light, ionizing radiation, chronic hypoxia ⟶ Medical Treatments Examples: Anesthesia, splenectomy Week 6 Infection Stress and Disease: Chapters 10 & 11 Infection Invasion and Evasion » Invasion results in direct confrontation with the individual’s primary defense mechanisms against bacteria, which include the complement system, antibodies, and phagocytes, such as neutrophils and macrophages » Evasion of the body’s defense mechanism results in the microbes transported in the blood to organs (Septicemia) » Exotoxins are proteins released during bacterial growth—usually enzymes & can damage cell membranes, activate second messengers, and inhibit protein synthesis » Exotoxins are immunogenic and elicit the production of antibodies (known as antitoxins). Vaccines are available for many of the exotoxins (tetanus, diphtheria, pertussis) » Endotoxin can lead to fatal endotoxic shock (Septic shock), leading cause of death in ICUs » Usual cause is proliferation of gram-negative bacteria » Once in the blood, endotoxins cause the release of vasoactive peptides & cytokines- cause decrease oxygen delivery, and produces subsequent cardiovascular shock » Endotoxin can activate the coagulation cascade, leading to the syndrome of disseminated (or diffuse) intravascular coagulation » Endotoxin induces the release of TNF-α (cachectin) by macrophages Acquired Immunodeficiency Syndrome (AIDS) » Most notable form of secondary or acquired immune deficiency is caused by Human Immunodeficiency virus (HIV) Currently accepted definition relies on both lab tests and clinical symptoms » If the individual is seropositive, the diagnosis is made in association with various clinical symptoms » Most commonly, new cases of AIDS are diagnosed initially by decreased CD4+T-cell numbers at or below 200 cells/μL Symptoms include: » Atypical or opportunistic infections and cancers as well as indications of debilitating chronic disease (wasting syndrome, recurrent fevers) Human Immunodeficiency Virus » Retrovirus that infects & depletes a portion of the immune system (CD4+Th cells) » Infected persons are more susceptible to life-threatening infections & malignancies ** As with all blood-borne infections, healthcare providers are at increased risk of contracting the infection from an individual’s blood. The infectivity of HIV is relatively low compared to other major blood-borne contaminants; from a single needle stick of contaminated blood the probability of acquiring HIV infection is 0.3%, compared to 3% hepatitis C and 30% for hepatitis B** Stress and Disease General Adaptation Syndrome: Three-stage process developed by Hans Selye, describes the physiological changes the body goes through under stress Stage Name Description 1 Alarm stage or reaction CNS is aroused and the body’s defenses are mobilized (fight or flight) - Initially one becomes alarmed by a stressor that activates the hypothalamus and sympathetic nervous system 2 Stage of resistance or adaptation Individual perceives that he/she has a choice of either “fighting” or “flighting” -The resistance or adaptation phase begins with the actions of the hormones cortisol, norepinephrine, and epinephrine 3 Stage of exhaustion Continuous stress causes the progressive breakdown of compensatory mechanisms (acquired adaptations) and homeostasis - Exhaustion marks the onset of certain diseases (diseases of adaptation) The role of Cortisol & Stress * Secretion during stress exerts beneficial effects by inhibiting inflammatory effects (for ex: vasodilation & increased capillary permeability) * Acts to suppress the activity of helper T cells (Th1) cells, which leads to a decrease in innate immunity and to pro-inflammatory response * Promotes resolution and repair ** Whether cortisol-induced effects are adaptive or destructive may depend on the intensity, type, and duration of the stressor; the tissue involved; and the subsequent concentration and length of cortisol exposure Week 7 Cancer: Chapters 12 & 13 Cancer: diseases in which abnormal cells divide without control and are able to invade other tissues • Benign tumors named according to the tissues in which they arise with the suffix “- oma” • Cancers arising in epithelial tissue are called carcinomas, and if they arise from or form ductal or glandular structures are named adenocarcinomas, cancers that arise from meshencymal tissue (connective tissue, muscle, and bone) usually have the suffix sarcoma & cancers of lymphatic tissue are called lymphomas Benign versus Malignant Characteristic Benign Malignant Appearance of cells Well differentiated Poorly differentiated Usual rate of growth Slow Rapid Mitotic Index Low High Presence of capsule Yes No Vascularization Slight Neovascularization through angiogenesis Mode of growth Expansile Invasive Ability to metastasize No Yes Staging System of Cancer • Involves the size of the tumor, degree to which it has locally invaded, the extent to which it has spread. Important d/t treatment choice (aggressiveness) Four-stage system is used • Stage 1 confined to the organ of origin • Stage 2 locally invasive • Stage 3 spread to regional structures • Stage 4 spread to distant sites (liver ca spreading to lung) TNM System: Tumor spread, Node involvement, distant Metastasis • Prognosis is worse with increasing size of the tumor, lymph node involvement, and metastasis. Ex) T3N2M2 Tumor Markers: “blood test for cancer” • Hormones, enzymes, genes, antigens & antibodies. Produced by benign and malignant cells Used to: A. Screen and identify individuals who are at a high risk for cancer B. Diagnose the specific type of tumor in individuals with clinical manifestations relating to their tumor C. Follow the clinical course of tumor (post therapy) Paraneoplastic syndrome: s/s that is the consequence of cancer, unlike mass effect, it is not due to the local presence of cancer cells • Mediated by humoral factors -hormones or cytokines • Ex) Benign tumors of the adrenal medulla (pheochromocytoma) can produce catecholamines (adrenaline) in vast excess, leading to rapid pulse rate and high BP [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2021
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2021
Downloads
0
Views
70



.png)
 Rasmussen College.png)