*NURSING > STUDY GUIDE > NURS 611 Exam #4 study guide/ Download To Score An A (All)
NURS 611 Exam #4 study guide/ Download To Score An A
Document Content and Description Below
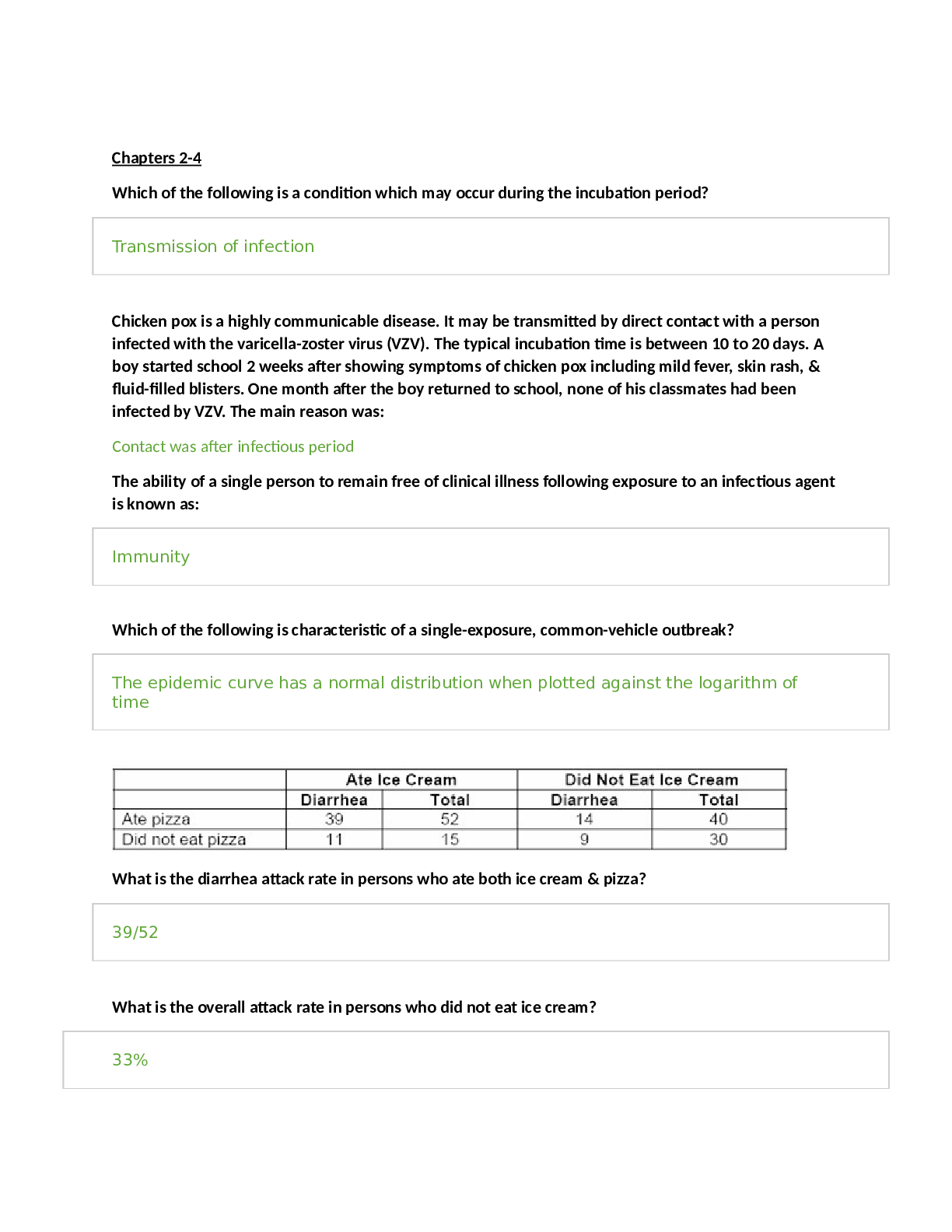
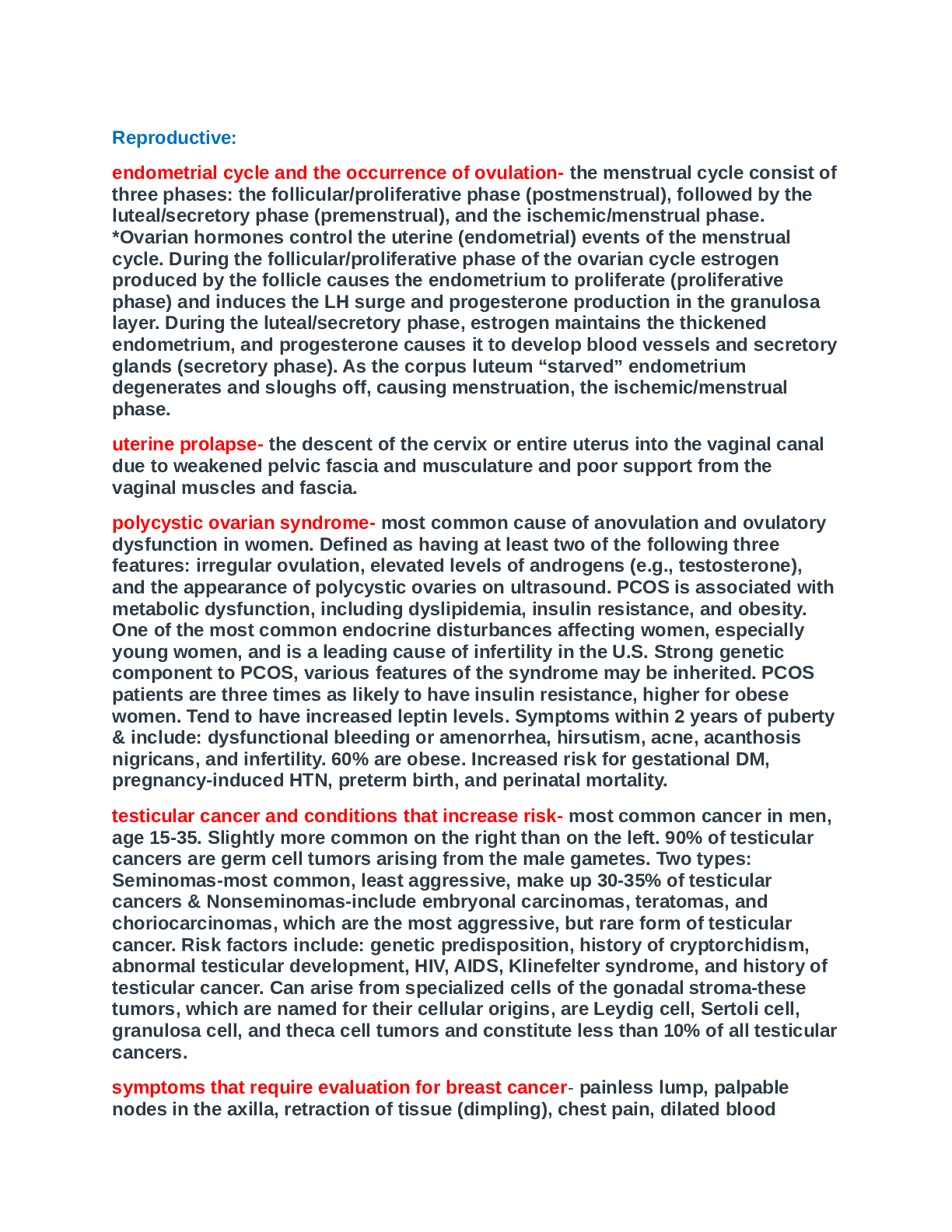
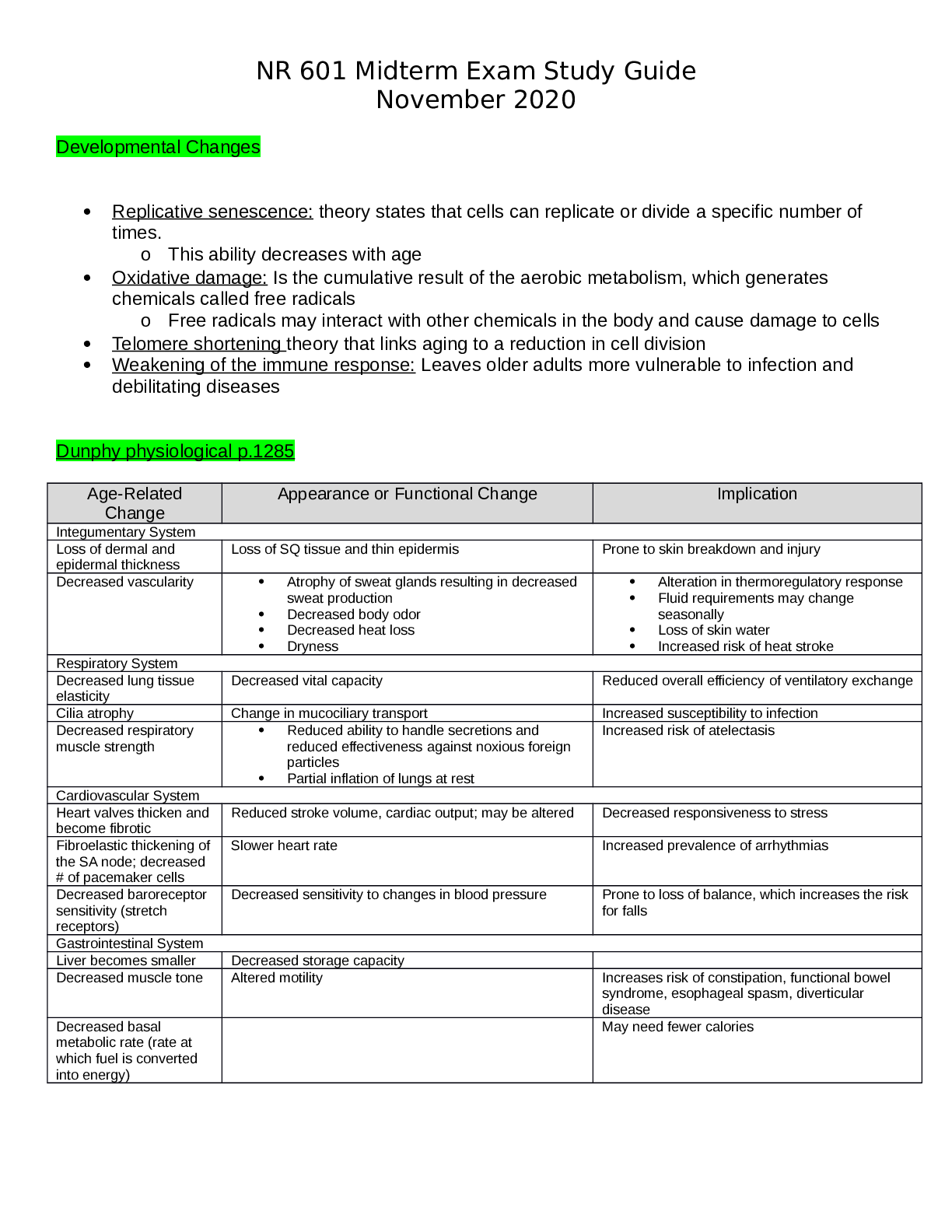
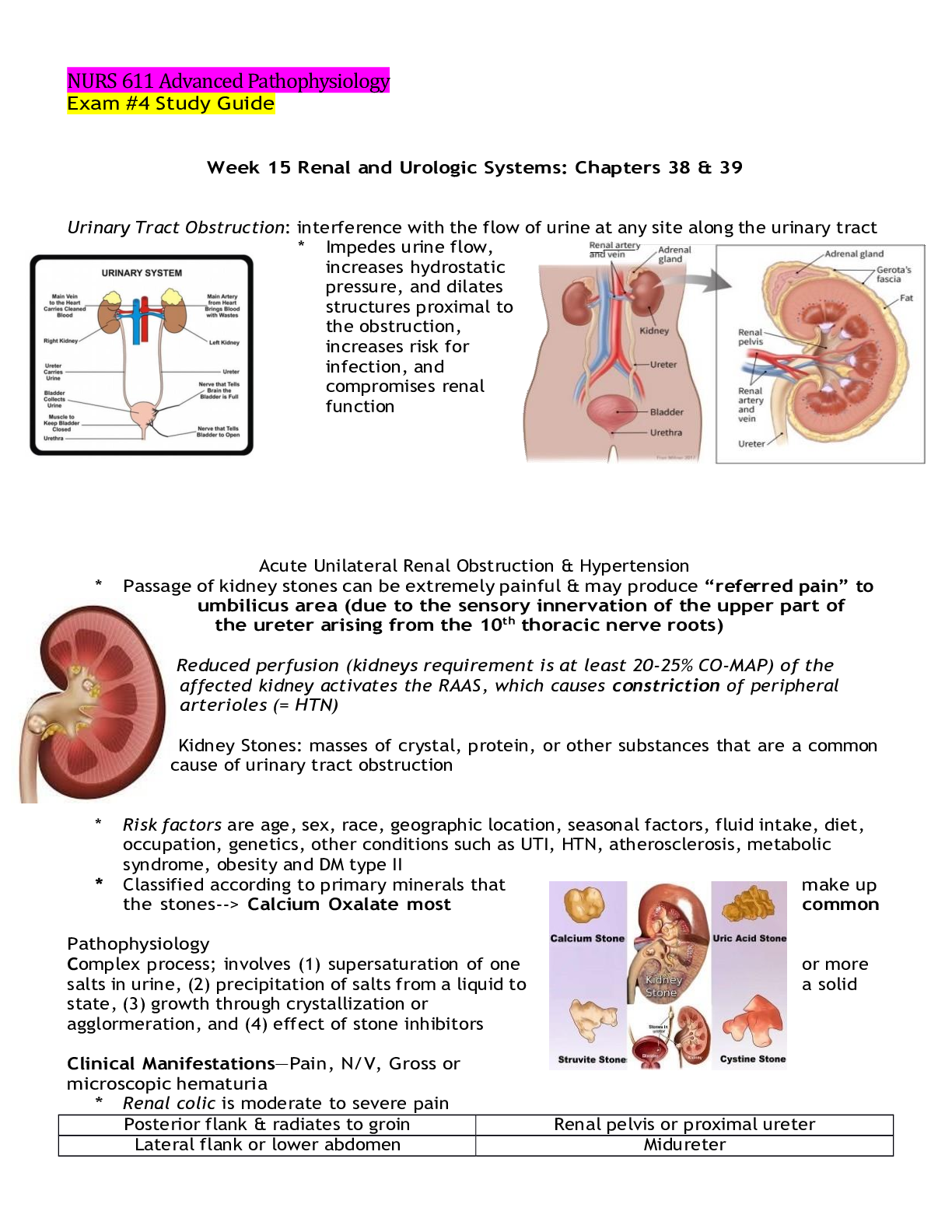
NURS 611 Advanced Pathophysiology Exam #4 Study Guide Week 15 Renal and Urologic Systems: Chapters 38 & 39 Urinary Tract Obstruction: interference with the flow of urine at any site along the ur... inary tract * Impedes urine flow, increases hydrostatic pressure, and dilates structures proximal to the obstruction, increases risk for infection, and compromises renal function Acute Unilateral Renal Obstruction & Hypertension * Passage of kidney stones can be extremely painful & may produce “referred pain” to umbilicus area (due to the sensory innervation of the upper part of the ureter arising from the 10th thoracic nerve roots) Reduced perfusion (kidneys requirement is at least 20-25% CO-MAP) of the affected kidney activates the RAAS, which causes constriction of peripheral arterioles (= HTN) Kidney Stones: masses of crystal, protein, or other substances that are a common cause of urinary tract obstruction * Risk factors are age, sex, race, geographic location, seasonal factors, fluid intake, diet, occupation, genetics, other conditions such as UTI, HTN, atherosclerosis, metabolic syndrome, obesity and DM type II * Classified according to primary minerals that make up the stones--> Calcium Oxalate most common Pathophysiology Complex process; involves (1) supersaturation of one or more salts in urine, (2) precipitation of salts from a liquid to a solid state, (3) growth through crystallization or agglormeration, and (4) effect of stone inhibitors Clinical Manifestations—Pain, N/V, Gross or microscopic hematuria * Renal colic is moderate to severe pain Posterior flank & radiates to groin Renal pelvis or proximal ureter Lateral flank or lower abdomen Midureter Bothersome UTI symptoms (urgency, frequent voiding, urge incontinence) Lower ureter or uterovesical junction Urinary Tract Infections (UTI) * Inflammation of the urinary epithelium usually caused by bacteria from gut flora, occurs anywhere along the urinary tract (urethra, bladder, ureter, or kidney) Who is at risk? Premature newborns; prepubertal children; sexually active and pregnant women; women treated with antibiotics that disrupt vaginal flora; spermicide users; estrogen-deficient postmenopausal women; individuals with indwelling catheters; persons with DM, neurogenic bladder, or urinary tract obstruction Clinical manifestations of a UTI in an older adult are confusion and poorly localized abdominal discomfort, very difficult diagnose due to vague symptoms Types I. Cystitis * Inflammation of the bladder & the most common site of UTI Pathophysiology—most common infecting microbe is E.coli (80-85%), second is Staphylococcus saprophyticus (10%). Bacterial contamination of the sterile urine usually occurs by retrograde movement of uropathic gram-negative bacilli from the gut into the urethra and bladder and then to the ureter and kidney Clinical Manifestations: related to the host inflammatory response & usually include frequency, urgency, dysuria (painful urination), & suprapubic and low back pain › Inflammatory edema in the bladder wall stimulates discharge of stretch receptors, initiating symptoms of bladder fullness with small volumes of urine & producing urgency and frequency Hematuria, flank pain, cloudy & foul-smelling urine are most serious symptoms Treatment--> urosepsis & septic shock are medical emergencies, demand parenteral, broad-spectrum antibx tx and may require hospitalization II. Pyelonephritis * Infection of one or both upper urinary tracts (ureter, renal pelvis, kidney interstitium) Urinary obstruction & reflux of urine from the bladder (vasicoureter reflux) are the most common underlying risk factors ⟶ Common causes are kidney stones, vesicoureteral reflux, pregnancy, neurogenic bladder, instrumentation, and female sexual trauma Pathophysiology— Microbes associated include E.coli, Proteus, & Pseudomonas. Latter two are associated with infections after surgery. These specific microbes split urea in to ammonia, making alkaline urine that increases the risk of stone formation. In severe infections, localized abscesses may form in the medulla and extend to the cortex. Clinical Manifestations: acute, with fever, chills, and flank or groin pain. Older adults may experience low-grade fever and malaise. ** Differentiating symptoms of cystitis from those of pyelonephritis by clinical assessment alone is difficult. The specific diagnosis is established by urine culture, UA, and clinical signs & symptoms. WBC casts indicate pylenephritis** Painful Bladder Syndrome/Interstitial Cystitis (PBS/IC): unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder associated with lower urinary tract symptoms of more than 6 weeks’ duration in the absence of infection or other identifiable causes * Includes nonbacterial infectious cystitis (viral, mycobacterial, chlamydial, fungal) and noninfectious cystitis (radiation, chemical, autoimmune, hypersensitivity) * Cause is UNKNOWN, but an autoimmune reaction may be responsible for the inflammatory response ⟶ Characteristic symptoms of IC include bladder fullness, frequency (nocturia), small urine volume, and chronic pelvic pain with symptoms lasting more than 6 months Glomerular Disorders Diseases affect kidney function by attacking the glomeruli (tiny units within the kidney where blood is cleaned), significant cause of CKD and ESRD These diseases include many conditions with a variety of genetic and environmental causes, but they fall into two main categories: glomerulonephritis & glomerulosclerosis ⟶ Reduced GFR during glomerular disease is evidenced by elevated plasma urea, creatinine concentration, or reduced renal creatinine clearance Acute Glomerulonephritis: inflammation of the glomerulus caused by immune mechanisms that damage the glomerular capillary filtration membrane including the endothelium, basement membrane, and epithelium (podocytes) * Secondary glomerular injury is a consequence of systemic diseases, including DM, SLE, and, less commonly, CHF and HIV-related kidney disease Pathophysiology—Immune mechanisms ⟶ Deposition of circulating antigen-antibody immune complexes (type III), (2) reaction of antibodies in situ against planted antigens within the glomerulus (type II), (3) action of antibodies directed against the glomerular capillary wall (least common but most severe, type II); and (4) cell-mediated immune injury (type IV) Clinical Manifestations: hematuria—RBC casts, proteinuria (milder than nephrotic syndrome), and in more severe cases, these symptoms are also accompanied by edema, HTN and impaired renal function Nephrotic Syndrome: excretion of 3.5g or more of protein in the urine per day, hypoalbuminemia (less than 3.0 g/dL), and peripheral edema ? Nephrotic syndrome is characteristic of glomerular injury, and occurs when filtration of protein exceeds tubular reabsorption ? Primary causes include minimal change disease (lipid nephrosis), membranous glomerulonephritis, and focal segmental glomerulosclerosis ? Secondary forms of nephrotic syndrome occur in systemic diseases including DM, SLE, and amyloidosis ? Also seen with certain drugs, infections, malignancies, and vascular disorders Pathophysiology—disturbances in the glomerular basement membrane (GBM) and podocyte injury lead to loss of electrical negative charge and increased permeability ⟶ Loss of plasma proteins, particularly albumin & some immunoglobulins, occurs across the injured glomerular filtration membrane ⟶ Loss of plasma proteins decreases plasma oncotic pressure, resulting in edema. Predominant cause is minimal-change nephropathy Clinical Manifestations: related to loss of serum proteins and associated retention of Na. S/S: Edema, HTN, HL, lipiduria, vitamin D deficiency, hypothyroidis ? Vitamin D deficiency is related to loss of serum transport proteins and decreased vitamin D activation by the kidney Acute Kidney Injury (AKI) May be acute and rapidly progressive, may be reversible. Kidney failure also can be chronic, progressing to ESRD over a period of months or years ? Renal insufficiency refers to a decline in renal function to about 25% of normal or a GFR of 25 to 30 ml/minute * Levels of serum creatinine and urea are mildly elevated. However, changes in serum creatinine level occur only if more than 50% of flomerular filtration is lost and are often delayed by more than 24 hours * Diagnostic delays make the implementation of early therapy very difficult, contributing to disease progression and mortality Prone to HYPERKALEMIA & METABOLIC ACIDOSIS RENAL PHOSPHATE EXCRETION IS causing hyperphosphatemia Pathophysiology—results from extracellular volume depletion, decreased renal blood flow, or toxic/inflammatory injury to kidney cells that result in alterations in renal function that may be minimal or severe. Etiologies of AKI can be described considering 3 categories of injury * Renal hypoperfusion (pre-renal AKI), disorders involving the renal parenchymal or interstitial tissue, and disorders associated with acute urinary tract obstruction (post- renal AKI) I. Initiation phase: reduced perfusion or toxicity in which renal injury evolving, usually lasting 24-36 hours II. Extension phase: infiltration of inflammatory cells, mostly neutrophils; release of cytokines; inflammation; and cell injury contributing to tubular obstruction and back leak III. Maintenance phase: established renal injury and dysfunction after the initiating event has been resolved, may last weeks to months * Urine output is lowest at this phase, serum creatinine lowest, BUN and serum K+, increase, metabolic acidosis develops, Salt and H2O overload IV. Recovery phase: interval when renal injury is repaired and normal renal function is reestablished * Oliguria, anuria (output < 50mL/day), nonoliguric RF (represents less severe injury & is associated with toxin exposure or drug toxicity), urine output >2L/day, but BUN and plasma creatinine concentrations increase * Symptoms of CHF develop with cardiac disease: N/V, fatigue, uremia, electrolyte imbalances Clinical Manifestations: fluid retention may cause edema, CHF symptoms in people with CV disease, N/V, fatigue accompany uremia & electrolyte imbalances ? Wound healing is delayed, risk of infection (PNA) is greater ? ** As renal function improves during the recovery phase, urine volume (diuresis) is progressive. Na and K lost in urine, risk for hypokalemia. Volume depletion may ensue,fluid losses of 3-4 L/day Fluid and electrolyte balance must be monitored and excessive urinary losses replaced. Return to normal status may take 3-12 months. AKI is a risk factor for progression to ESRD, CV events, and CVA** Week 14 Digestive System: chapters 41 & 42 The Digestive System GI tract & accessory organs of digestion: liver, gallbladder, exocrine pancreas ▪ Breaks down ingested food, prepares it for uptake by the body’s cells, provides body water, and eliminated wastes ▪ Except for chewing, swallowing, and defecation of solid wastes, the activities of the digestive system are controlled by hormones and the autonomic NS GI tract: mouth, esophagus, stomach, small intestine, large intestine, rectum, and anus Carries out the following digestive processes: 1) ingestion of food, 2) propulsion of food and wastes from the mouth to the anus, 3) secretion of mucus, water, and enzymes, 4) mechanical digestion of food particles, 5) chemical digestion, 6) absorption of digested food, 7) elimination of waste products by defecation, 8) immune and microbial protection against infection Obesity defined as a BMI > 30 kg/m2 ▪ Visceral obesity distribution of body fat is localized around the abdomen and upper body, resulting in an apple shape. Visceral obesity is associated with accelerated lipolysis and has an increased risk for inflammation, metabolic syndrome (hypertriglyceridemia, reduced HDL, increased LDL, HTN, and insulin resistance), type 2 DM, CV complications, and cancer ▪ Peripheral obesity distribution of body fat is extra peritoneal and distributed around the thighs and buttocks and through the muscle, resulting in pear shape; it is more common in women. Risk factors are still present for the complications of obesity but they are less severe than for visceral obesity. Gastroesophageal Reflux Disease (GERD) Reflux of acid & pepsin from the stomach to the esophagus that causes esophagitis ▪ Risk factors include obesity, hiatal hernia, and drugs or chemicals that relax the lower esophageal sphincter (LES) such as anticholinergic, nitrates, calcium channel blockers, nicotine ▪ GERD may be a trigger for asthma, sinusitis, or chronic cough Pathophysiology—abnormalities in lower esophageal sphincter function, esophageal motility, and gastric motility or emptying are the causes ⟶ Vomiting, coughing, lifting, bending, obesity, or pregnancy increases abdominal pressure, contributing to the development of reflux esophagitis ⟶ Delayed gastric emptying contributes to reflux esophagitis by (1) lengthening the period during which reflux is possible, (2) increasing the acid content of chyme ⟶ Disorders that delay emptying include gatroparesis, gastric or duodenal ulcers, which can cause pyloric edema; and strictures that narrow the pylorus Clinical Manifestations: related to mucosal injury heartburn from acid regurgitation, chronic cough, asthma attacks, and laryngitis ▪ Upper abdominal pain usually occurs within 1 hour of eating and can be relapsing and remitting ▪ Symptoms can worsen if the individual lies down or if intra-abdominal pressure increases Heartburn also may be experienced as CP, which requires r/o cardiac ischemia Bowel Obstructions Most common occurring small intestinal obstruction is related to adhesions account for 50-70% of SBOs ▪ Presents early with abdominal distention ▪ If obstruction is at the pylorus or high in the small intestine, metabolic alkalosis develops initially as a result of excessive loss of hydrogen ions that normally would be reabsorbed from the gastric juice ▪ In prolonged intestinal obstruction the lack of circulation produces lactic acid (decreased tissue perfusion) thus metabolic acidosis Pathophysiology—post-op paralytic ileus results from inhibitory neural reflexes associated with inflammation mediators, and the influence of exogenous (meperidine or morphine) and endogenous opioids (endorphins) that affect the entire GI tract, including the stomach ⟶ SBO caused by post-op adhesions, tumors, CD, hernias, and intussusception ⟶ Large bowel obstruction is less common & often related to carcinoma Clinical Manifestations: SBO include colicky pains caused by distention, N/V, pain intensifies with peristaltic wave of muscle contraction, sweating, tachycardia occur as sympathetic NS response to hypotension, fever, severe leukocytosis, abdominal distention, and rebound tenderness develop as ischemia progresses to necrosis, perforation, and peritonitis ▪ Obstruction at pylorus causes early, profuse vomiting of clear gastric fluid Peptic Ulcer Disease Break, or ulceration, in the protective mucosal lining of the lower esophagus, stomach, or duodenum Risk factors include genetics, H.pylori, and habitual use of ASA and NSAIDs ▪ Additional factors include ETOH, smoking, acute pancreatitis, COPD, obesity, cirrhosis, age > 65, socioeconomic status/ psychological stress ▪ Chronic use of NSAIDs suppresses mucosal prostaglandin synthesis, resulting in decreased HCO3 secretion and mucin (a component of gut barrier) production and increased secretion of HCl Postgastrectomy Syndromes-- Dumping Syndrome Rapid emptying of hypertonic chyme from the surgically created, residual stomach (stomach component remaining after surgical resection following gastric or bariatric surgery) into the small intestine 10-20 minutes after eating ▪ Rapid gastric emptying and creation of a high osmotic gradient within the small intestine cause a sudden shift of fluid from the vascular compartment to the intestinal lumen ▪ Rapid distention of the intestine produces a feeling of epigastric fullness, cramping, nausea, vomiting, and diarrhea. Clinical Manifestations: increased pulse, hypotension, weakness, pallor, sweating, & dizziness following a partial gastrectomy or pyloroplasty ▪ Occurs 20 minutes after eating ** Usually managed very well with dietary management: frequent small meals; no fluid during meals; high protein, low carbs** Inflammatory Bowel Diseases: Crohn Disease compared to Ulcerative Colitis (UC) Feature Ulcerative Colitis Crohn Disease Age of onset Any age; 10-40 years most common Any age; 10-30 years most common Family History Less common More common Sex (prevalence) Equal in women & men Equal in women & men Cancer risk Increased Increased Pathophysiology Location of lesions Colon and rectum, no “skip” lesions All of GI tract: mouth to anus, “skip” lesions common Inflammation & ulceration Mucosal layer involved Entire intestinal wall involved Fistulae & Abscesses Rare Common Strictures & possible obstruction Rare Common Granulomas Rare Common Friable mucosa Common Less common Clinical Manifestations Abdominal pain Occasional Common Diarrhea Common Common Bloody stools Common Less common Abdominal mass Rare Common Small intestinal malabsoprtion Rare Common Steatorrhea Rare Common ▪ Chronic, relapsing idiopathic inflammatory bowel diseases (IBDs) The Liver – One of the main functions of the liver is the synthesis of amino acids. Protein synthesis requires the presence of all the essential amino acids (obtained only from food), as well as nonessential amino acids. ▪ Within hepatocytes, amino acids are converted to carbohydrates by the removal of ammonia (NH3), a process known as deamination ▪ The ammonia is converted to urea by the liver and passes into the blood to be excreted by the kidneys ▪ The plasma proteins, including albumins and α- and β- globulins (not gamma globulin, which is formed in lymph nodes and lymphoid tissue), are synthesized by the liver. The liver also synthesizes several nonessential amino acids and serum enzymes that become elevated with liver injury Any condition that disrupts the normal functioning of the liver, thus hepatocyte dysfunction, can cause hypoalbuminemia Cirrhosis Irreversible inflammatory, fibrotic liver disease ▪ 12th leading cause of death in the U.S. ▪ ETOH abuse & viral hepatitis (HCV) are the most common causes ▪ Chaotic fibrosis alters or obstructs biliary channels & blow flow, producing jaundice and portal HTN New vascular channels form shunts, and blood from the portal vein bypasses the liver, contributing to portal hypertension, metabolic alterations, and toxin accumulation. Portal Hypertension (elevation of hepatic venous pressure > 5 mmHg): abnormally high BP in the portal venous system caused by resistance to portal blood flow, usually by disorders that obstruct or impede blood flow ▪ Esophageal varices is the most common clinical manifestation ▪ Thrombocytopenia is the most common manifestation of congestive splenomegaly and can contribute to an increased bleeding risk Clinical Manifestations: vomiting of blood r/t varices, anemia, melena ▪ Acute rupture of varices causes hemorrhage & voluminous vomiting of dark blood ▪ Rupture is caused by a combination of erosion by gastric acid & elevated venous pressure Hepatic Encephalopathy: results from a combination of biochemical alterations that affect neurotransmission ▪ Liver dysfunction and collateral vessels that shunt blood around the liver to the systemic circulation permit neurotoxins and other harmful substances absorbed from the gastrointestinal tract to accumulate and circulate freely to the brain ▪ The most hazardous substances are end-products of intestinal protein digestion, particularly ammonia, which cannot be converted to urea by the diseased liver Risk factors in the presence of advanced liver disease include GI bleeding, increased dietary protein, electrolyte imbalance, and hypoxia Acute Pancreatitis: mild disease & resolves spontaneously, develops due to obstruction to the outflow of pancreatic digestive enzymes caused by bile duct or pancreatic duct obstruction (gallstones) ▪ Can also result from direct cellular injury from drugs or viral infection Pathophysiology—in obstructive disease, the backup of pancreatic secretions or duodenal contents or both, triggers activation & release of enzymes (activated trypsin activates chymotrypsin, lipase, and elastase) within the pancreatic acinar cells Clinical Manifestations: epigastric or midabdominal constant ▪ The pain may radiate to the back because of the retroperitoneal location of the pancreas ▪ Fever and leukocytosis accompany the inflammatory response ▪ Electrolyte imbalances – hypocalcemia ▪ Hypotension and shock occur with hypovolemia and SIRS ▪ Tachypnea and hypoxemia are indicative of complications (SEPSIS and ARDS) In severe cases, hypovolemia decreases renal blood flow sufficiently to impair renal function. Transient hyperglycemia also can occur if glucagon is released from damaged A cells in the pancreatic islets. SIRS and multiple organ failure account for most deaths with severe pancreatitis Week 12 Reproductive System: Chapters 24, 25, 26 & 27 Primary Dysmenorrhea • Painful menstruation associated with the release of prostaglandins in ovulatory cycles, but not with pelvic disease • Elevated levels of prostaglandins cause uterine hypercontractility, decreased blood flow to the uterus, and increased nerve hypersensitivity, thus resulting in pain Pathophysiology: attributed to excessive endometrial prostaglandin production, primarily released during the first 48 hours of menstruation, when the symptoms are most intense. Women with painful periods produce 10 times as much prostaglandin F, a potent myometrial stimulant and vasoconstrictor, as asymptomatic women Secondary dysmenorrhea is related to pelvic pathologic disorders that manifests in later reproductive years & may occur any time in the menstrual cycle • Most common cause endometriosis • Other causes include: endomeritis (infection), pelvic inflammatory disease, obstructive uterine or vaginal anomalies, uterine fibroids, polyps, tumors, ovarian cysts, pelvic congestion syndrome, or nonhormonal intrauterine devices (IUDs) Clinical Manifestations—pelvic pain associated with the onset of menses, pain often radiates into the groin & may be accompanied by backache, anorexia, vomiting, diarrhea, syncope, insomnia & headache Polycystic Ovarian Syndrome (PCOS): most common cause of anovulation & ovulatory dysfunction. Defined as having at least 2 of the following 3 features: irregular ovulation, elevated levels of androgens (testosterone), and the appearance of polycystic ovaries on ultrasound • No single factor fully accounts for the abnormalities of PCOS • Hyperandrogenic state is a cardinal feature in the pathogenesis of PCOS. Glucose intolerance/insulin resistance (IR) & hyperinsulinemia often run parallel & markedly aggravate the hyperandrogenic state, thus contributing to the severity of S/S ⟶ Obesity adds to & worsens IR. Excessive androgens affect follicular growth, and insulin affects follicular decline by suppressing apoptosis & enabling follicles, which would normally disintegrate, to survive Benign Ovarian Cysts Produced when a follicle or a # of follicles are stimulated but no dominant follicle develops & completes maturity process • Fluid-filled sac forms in the ovary, vary in size & may occur at different sites in the ovary • Most common type develops when an egg-producing follicle does not rupture & release an egg but instead fills with fluid and forms a follicular cyst ⟶ Often disappear on their own without treatment Human Papillomavirus (HPV) Most common symptomatic viral STI, easily transmissible through direct contact with lesions or infected secretions; vertical transmission in utero & during vaginal birth is also possible • HPV vaccine recommended for females 11-26 y/o and for nonimmunocompromised males ages 11-21 Pathophysiology—non-enveloped, circular, double-stranded DNA virus, transmitted via close physical contact with infected skin, mucosa, or fluids ⟶ Initial infection follows trauma to the epithelium that allows the virus to reach & infect the basal cells of the epithelium, which appear to be supportive or viral propagation ⟶ Enters the nuclear DNA & changes the expression of cell proteins, leading to either increased but noncancerous cell growth (genital warts) OR unchecked cell growth (cancer) - HPV infection may occur months to years before symptoms appear Clinical Manifestations: Genital warts (condylomata acuminata) may cause dyspareunia (painful intercourse) & may be friable and bleed • Laryngeal papillomas can occur in infants & children whose mothers had genital warts at the time of delivery; stridor, hoarseness, abnormal cry, cough, & respiratory distress • Precancerous changes often do NOT have any visible manifestations & are not painful— hampering early detection • Cervical & anal cancer may not cause symptoms until late in the disease, routine screening for cervical cancer was begun to increase early detectio ** Previous efforts at early screening resulted in many young women receiving TXs on their cervix. These TXs destroyed or removed cervical cells & in many cases altered the structural integrity of the cervix, resulting in an INCREASE in preterm births in women treated w/o substantially decreasing the later rates of cervical cancer. It is UNKNOWN why some women are able to clear HPV & others cannot. Smoking has been shown to increase the risks of persistent infection & later development of cervical cancer. Infection with “high-risk” (oncogenic) types of HPV is a necessary precursor to development of the precancerous dysplasia of the cervix that leads to invasive cancer** Sexually Transmitted Infection (STI) Have been called the “hidden epidemic” by the CDC due to high prevalence rate, yet rarely discussed • Many infected individuals don’t seek TX due to lack of symptoms or minor or transient symptoms or b/c health services are inaccessible, unaffordable, or culturally insensitive • Urogenital infections caused by Chlamydia closely parallel those caused by gonorrhea ⟶ Zika virus is a single-stranded RNA virus from the Flaviviridae family, genus Flavivirus The virus is predominantly transmitted through bites from infected mosquitos. However, vertical transmission easily occurs in infected women, and sexual transmission also has been confirmed At this time, the exact mechanism of sexual transmission is not known, although shedding of the virus in semen is suspected. The CDC is investigating the issue and advises safer sex precautions for all sexual contact (including vagina, anal, and oral sex) between an infected person and his or her partners **Infection with zika virus during pregnancy has been associated with severe fetal infection and associated CNS abnormalities** Pelvic organ prolapse (POP) The descent of one or more of the following into the vaginal space: the vaginal wall, the uterus, or the apex of the vagina (after hysterectomy) • Multifactorial, several factors contribute to the weakening of the pelvic fascia that support the female reproduction tract (trauma is the #1 risk factor including childbirth) The Cele’s Cystocele: descent of a portion of the posterior bladder wall & trigone into the vaginal canal and usually is caused by the trauma of childbirth ⟶ In severe cases, the bladder & anterior vaginal wall bulge outside the introitus ⟶ Occasionally, can cause significant residual urine & an increased rate of bladder infections Rectocele: bulging of the rectum & posterior vaginal wall into the vaginal canal; lifelong chronic constipation & straining may produce aggravate it ⟶ Larger ones can cause vaginal pressure, rectal fullness, & incomplete bowel evacuation ⟶ If severe, defecation is difficult & can be facilitated by manual pressure to the posterior vaginal wall ** During childbirth women may sustain damage that can lead to a rectocele** Spermatocele (epididymal cysts):benign cystic collecti ons of fluid of the epididymis located between the head of the epididymis and the testis the testis ⟶ Filled with milky fluid that contain sperm ⟶ Differentiated from hydrocele in that aspiration of the hydrocele recovers a clear, yellow fluid, and unlike a hydrocele, a spermatocele doesn’t cover the entire anterior surface of Prostatitis Inflammation of the prostate; inflammation is usually limited to a few of the gland’s excretory ducts Classified by the NIH as... I. Acute bacterial prostatitis • An ascending infection of the prostate • Manifested by systemic signs of infection and a positive UA II. Chronic bacterial prostatitis • Chronic bacterial infection in which bacteria are recovered in significant numbers from a purulent prostatic fluid, these bacteria are thought to be the most common cause of recurrent UTIs in men III. Chronic pelvic pain syndrome (CPPS) • Diagnosed when no pathogenic bacteria can be localized to the prostate • Further divided into IIIa (inflammatory CPPS in which a significant # of WBCs are localized to the prostate) and IIIb (noninflammatory) IV. Asymptomatic inflammatory prostatitis • Bacteria or WBCs are localized to th e prostate, individuals are asymptomatic Clinical Manifestations: sudden onset of malaise, low back & perineal pain, high fever (up to 104° F), chills, dysuria, inability to empty the bladder, nocturia, and painful ejaculation • Rhythmic and effortless, ventilatory rate is 8 to 16 bpm • Tidal volume ranges from 400 to 800 ml • A short expiratory pause occurs with each breath, and the individual takes an occasional deeper breath or sigh Sigh breaths, which help maintain normal lung function, are usually 1.5 to 2 times the normal tidal volume and occur approximately 10 to 12 times per hour Kussmaul respirations (hyperpnea) • Kussmaul respirations are characterized by a slightly increased ventilatory rate, very large tidal volume, and no expiratory pause. Cheyne-Stokes respirations • Characterized by alternating periods of deep and shallow breathing • Apnea lasting 15 to 60 seconds is followed by ventilations that increase in volume until a peak is reached, after which ventilation (tidal volume) decreases again to apnea • Cheyne-Stokes respirations result from any condition that slows the blood flow to the brainstem, which in turn slows impulses sending information to the respiratory centers of the brainstem Hypoventilation • Inadequate alveolar ventilation in relation to metabolic demands • It is caused by alterations in pulmonary mechanics or in the neurologic control of breathing such that minute volume (tidal volume × respiratory rate) is reduced • When alveolar ventilation is normal, carbon dioxide (CO2) is removed from the lungs at the same rate at which it is produced by cellular metabolism. This maintains arterial CO2 pressure (PaCO2) at normal levels (40 mmHg) • With hypoventilation, CO2 removal does not keep up with CO2 production and PaCO2 increases, causing hypercapnia (PaCO2 greater than 44 mmHg). This results in an increase in hydrogen ion in the blood, termed respiratory acidosis, which can affect the function of many tissues throughout the body. Hyperventilation • Response to hypoxemia, anxiety, pain • Removal of CO2 at a faster rate than it is produced by cellular metabolism, resulting in decreased PaCO2 or hypocapnia (PaCO2 less than 36 mmHg) • Hypocapnia results in a respiratory alkalosis that also can interfere with tissue function Tuberculosis (TB): infection caused by Mycobacterium tuberculosis, an acid-fast bacillus that usually affects the lungs, but may invade other body systems Pathophysiology: highly contagious & is transmitted from person-to-person by inhalation of airborne droplets After inhalation of M. tuberculosis, the bacilli lodge in the lung periphery, are phagocytized by resident macrophages, and cause nonspecific pneumonitis ➢ Inflammation causes neutrophils & macrophages to migrate to the area ➢ Phagocytes engulf the bacilli and begin the process by which the body’s defense mechanisms isolate the bacilli, preventing their spread * However, the bacterium can survive within macrophages, resist lyosomal killing, multiply within the cell, and transmit into a stage of dormancy rendering itself extremely resistant to host defense & drug treatment ➢ Once bacilli are isolated in tubercles & immunity develops, TB may remain dormant for life Clinical Manifestations: Latent TB is asymptomatic with no radiologic evidence of disease. • Fatigue, weight loss, lethargy, anorexia, a low-grade fever that usually occurs in the afternoon & night sweats • Cough with purulent sputum • Dyspnea, CP & hemopytsis **Diagnosed by a positive tuberculin skin test (TST; purified protein derivative (PPD)), sputum culture, immunoassays, and chest radiographs** ➢ A positive TB skin test indicates the need for yearly detect active disease ➢ Skin test does not differentiate between past, latent, or active forms of the disease ➢ Individuals who have received the TB vaccine with bacille Calmette-Guerin (BCG) will have a positive TST even if they have never had TB Aging & The Pulmonary System • Loss of elastic recoil, stiffening of the chest wall, changes in gas exchange and increases in flow resistance • Changes are gradual & usually without adverse consequences in healthy individuals • Changes are influenced by environmental & sociocultural factors, nutritional status, respiratory disease, body size, gender & race Asthma: chronic inflammatory disorder of the bronchial mucosa that causes bronchial hyperresponsiveness, constriction of the airways & variable airflow obstruction that is reversible Pathophysiology: airway epithelial exposure to antigen initiates both an innate & an adaptive immune response in sensitized individuals. Dendritic cells, T helper 2, lymphocytes, B-lymphocytes, mast cells, neutrophils, eosinophils, and basophils involved. An immediate & a late response Early asthmatic response: first 30 minutes, resolves within 1-3 hours. Antigen exposure to the bronchial mucosa activates the above mediators causing vasodilation, capillary permeability, mucosal edema, bronchial smooth muscle contraction (bronchospasm), and tenacious mucus secretion from mucosal goblet cells with narrowing of & obstruction to airway Late asthmatic response: begins 4-8 hours after the early response. Hypoxemia further hyperventilation, causing PaCO2 to and pH to (respiratory alkalosis). Progressive obstruction of expiratory airflow puts the respiratory muscles at a mechanical disadvantage. This leads to a fall in tidal volume with increasing CO2 retention & respiratory acidosis (indicates respiratory failure) Clinical Manifestations: asymptomatic between attacks & PFTS are normal. During partial remission PFTs are abnormal. Beginning of the attack-- chest constriction, expiratory wheezing, dyspnea, nonproductive coughing, prolonged expiration, tachycardia, tachypnea • Severe attacks involve accessory muscles of respiration & wheezing is heard during inspiration & expiration • Pulse paradoxus: decrease in SBP of 10 mmHg during inspiration • ABG should be measured if SpO2 falls below 90% (usual findings are hypoxemia with resp. alkalosis) Status Asthmaticus--> occurs when bronchospasm is not reversed. Hypoxemia worsens, expiratory flow rates decrease further, and effective ventilation decreases. Acidosis begins when arterial PaCO2 rises. • Silent chest & PaCO2 greater than 70 mmHg are signs of impending death Evaluation & Treatment: history of allergies, recurrent episodes of wheezing, dyspnea, cough or exercise intolerance. • Spirometry which documents reversible decreases in FEV1during an attack • Rapid assessment of ABG & expiratory flow rates and search for underlying triggers Chronic Obstructive Pulmonary Disease (COPD) Common, preventable disease characterized by airflow limitation that is not fully reversible & is usually progressive. Includes two primary phenotypes that overlap each other- Chronic Bronchitis and Emphysema Risk Factors—tobacco smoke, occupational dusts & chemicals, indoor air pollution from biomass fuel used for cooking and heating & outdoor air pollution Chronic Bronchitis Emphysema Hypersecretion of mucus & chronic productive cough that continues for at least 3 months of the year (usually winter) for at least 2 consecutive years Abnormal permanent enlargement of gas- exchange airways (acini) accompanied by destruction of alveolar walls without obvious fibrosis Continual inflammation causes bronchial edema & increases the size and # of mucous glands and goblet cells in the airway epithelium - Thick, tenacious mucus is produced & cannot be cleared b/c of impaired ciliary function Destruction of alveoli through the breakdown of elastin within the septa Hypercapnia (PaCO2 ) r/t chronic hypoventilation is common Expiration becomes difficult b/c loss of elastic recoil reduces the volume of air that can be expired passively and air is trapped in the lungs Lung’s defense mechanisms compromised: vaccines for pneumococcal PNA & yearly Haemophilus influenza (flu shot) is SO important in the management Air trapping causes hyperexpansion of the chest (barrel chest), putting the muscles of respiration at a mechanical disadvantage 50/50 Gases: pH 7.28, PaCO2 60, PaO2 58 Inherited mutation in the α1-antitrypsin gene Both are associated with an enhanced chronic inflammatory response in the airways to noxious particles or gases Chronic irritant exposure recruits neutrophils, macrophages & lymphocytes to the lung, resulting in progressive damage from inflammation, oxidative stress, extracellular matrix proteolysis, and apoptic and autophagic cell death Clinical Manifestation Chronic Bronchitis Emphysema Productive cough Classic sign Late in course with infection Dyspnea Late in course Common Hx of smoking Common Common α1-antitrypsin gene deficiency is suggested in nonsmokers & individuals who develop emphysema before the age of 40 Barrel chest Occasionally Classic Prolonged expiration Always present Always present Cyanosis Common Uncommon Chronic hypoventilation Common Late in course Polycythemia Common Late in course Cor pulmonale: S&S: PND and orthopnea; hepatic congestion, peripheral edema, JVD often may be detected Common Late in course Pneumoconiosis: represents ANY change in the lung caused by inhalation of inorganic dust particles, usually occurring in the workplace o Dusts of silica, asbestos, and coal (black lung) are the most common causes o Often occurs after years of exposure to the offending dust with progressive fibrosis of lung tissue & an increased risk of lung cancer ⟶ Deposition of these materials causes the release of proinflammatory cytokines thus leading to chronic inflammation with scarring of the alveolocapillary membrane, resulting in pulmonary fibrosis and progressive pulmonary deterioration Lung Cancer Tumors that arise from the epithelium of the respiratory tract, 2nd most common cancer in the world Non-small Cell Lung Cancer (NSCLC): squamous cell carcinoma (SCC) accounts for 30% of bronchogenic carcinomas & is associated with smoking and COPD o Tumors are located centrally near the hila and proj ect into bronchi ; symptoms such as nonproductive cough or hemoptysis are common o PNA and atelectasis are associated with SCC * CP is a LATE symptom associated with large tumors. These tumors can remain fairly well localized and tend not to metastasize until late in the course* Small Cell Lung Carcinomas (SCLC): most common of the neuroendocrine lung tumors & contribute about 15% of lung cancers but cause 25% of lung cancer deaths--- rapid rate of growth & tend to metastasize early and widely, WORST PROGNOSIS of all lung cancers o Most tumors arise from the central part of the lung o Cell sizes range from 6-8 μm o This cell type has the STRONGEST correlation with tobacco smoking Pneumonia Infection of the lower respiratory tract caused by bacteria, viruses, fungi, protozoa, or parasites o Categorized as community-acquired (CAP) or healthcare- associated (HCAP), including hospital-acquired (HAP), or ventilator-assisted (VAP) Pathophysiology— I. Aspiration of oropharyngeal secretions is the most common route of lower respiratory tract infection; thus the nasopharynx and oropharynx constitute the first line of defense for most infectious agents II. Inhalation of microbes that have been released in the air when an individual coughs, sneezes, or talks; this route is most important in viral & mycobacterial PNAs and in Legionella outbreaks Clinical Manifestations: preceded by an URI (viral), onset of cough, dyspnea, fever, chills, malaise, pleuritic chest pain o Physical exam reveals signs of pulmonary consolidation (inspiratory crackles), increased tactile fremitus (palpable chest vibrations), egophony (a voice sound heard on auscultation as a prolonged “a” over consolidated lung tissue, when a person says “e”) and whispered pectoriloquy (sound of whispering heard on auscultation over consolidated lung tissue) o Individuals also may demonstrate S/S of underlying systemic disease or sepsis Evaluation/Treatment—history, physical exam, WBC, C-reactive protein level (used to help differentiate bacterial from viral PNA), CXR o Sputum culture o Blood culture Pulmonary Emboli (PE) Occlusion or partial occlusion of the pulmonary artery or its branches by an embolus, PE commonly results from embolization of a clot from DVT Pathophysiology—effect of the embolus depends on the extent of pulmonary blood flow obstruction, the size of the affected vessels, the nature of the embolus, and the secondary effects PE can result in any of the following: 1. Embolus with infarction: an embolus that causes infarction (death) of a portion of lung tissue 2. Embolus w/o infarction (perfusion of the affected lung segment is maintained by the bronchial circulation) circulation 3. Massive occlusion: embolus that occludes a major portion of the pulmonary circulation 4. Multiple pulmonary emboli (may be chronic or recurrent) As a result of the thrombus lodging in the pulmonary ⟶ Release of both neurohumoral substances such as serotonin, histamine, catecholamines, and angiotensin II ⟶ Inflammatory mediators such as endothelin, leukotrienes, thromboxanes, and toxic oxygen free radicals = Causes widespread VASOCONSTRICTION that further impedes blood flow to the lung o Hemodynamically, this results in pulmonary artery pressures (pulm. HTN) and can lead to RIGHT ventricular dilation, and afterload o Absent blood flow to a lung segment causes a ventilation-perfusion mismatch (dead space), and a in surfactant production The resulting atelectasis of the affected lung segments further contributes to HYPOXEMIA Clinical Manifestations: nonspecific; evaluation of risk factors & predisposing factors is important! - Sudden onset of pleuritic CP, cough, dyspnea, tachypnea, tachycardia, & unexplained anxiety; syncope & hemoptysis (sometimes) o Larger PE: pleural friction rub, pleural effusion, fever and leukocytosis o Massive occlusion causes severe pulmonary HTN and shock » Small emboli may not be detected until progressive incapacitation, precordial pain, anxiety, dyspnea, and right ventricular enlargement » In suspected PE, assessment of DVT (calf pain, tenderness, calf asymmetry) may indicate the source Evaluation/Treatment: based on the use of Clinical Decision Rules (such as Well’s score) o CXR are nonspecific in PE & can often be normal for the first 24 hours until atelectasis occurs o Serum D-dimer measures a product of thromub degradation by the fibrinolytic system, and if normal, makes the presence of a PE highly unlikely o Single or multidetector spiral CT arteriography, highly sensitive & specific test has replaced the radionucleotide V/P scan in many hospitals Acute Respiratory Distress Syndrome (ARDS) Spectrum of acute lung inflammation & injury to the alveolocapillary membrane producing massive pulmonary inflammation, capillary permeability, severe pulmonary edema as a result of bronchioles filling with fluid, shunting, mismatch, and hypoxemia Defined as (1) acute onset of BLE infiltrates on CXR not explained by cardiac failure or fluid overload and (2) a low ratio of the partial pressure of arterial O2 to the fraction of inhaled O2 Pathophysiology—can occur directly (aspiration of highly acidic gastric contents, inhalation of toxic gases, development of PNA) or indirectly (from circulating proinflammatory mediators released in response to systemic disorders, such as sepsis, trauma, & multiple transfusions) Clinical Manifestations: Progressive as follows Dyspnea and hypoxemia with poor response to oxygen supplementation Hyperventilation and respiratory ALKALOSIS Decreased tissue perfusion, metabolic ACIDOSIS, and organ dysfunction Increased work of breathing, decreased tidal volume, and hypoventilation Hypercapnia, respiratory ACIDOSIS, and worsening hypoxemia Decreased CO, hypotension, and death [Show More]
Last updated: 1 year ago
Preview 1 out of 31 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2021
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2021
Downloads
0
Views
40