*NURSING > STUDY GUIDE > NUR 2004 Exam 3 Study Guide. (All)
NUR 2004 Exam 3 Study Guide.
Document Content and Description Below
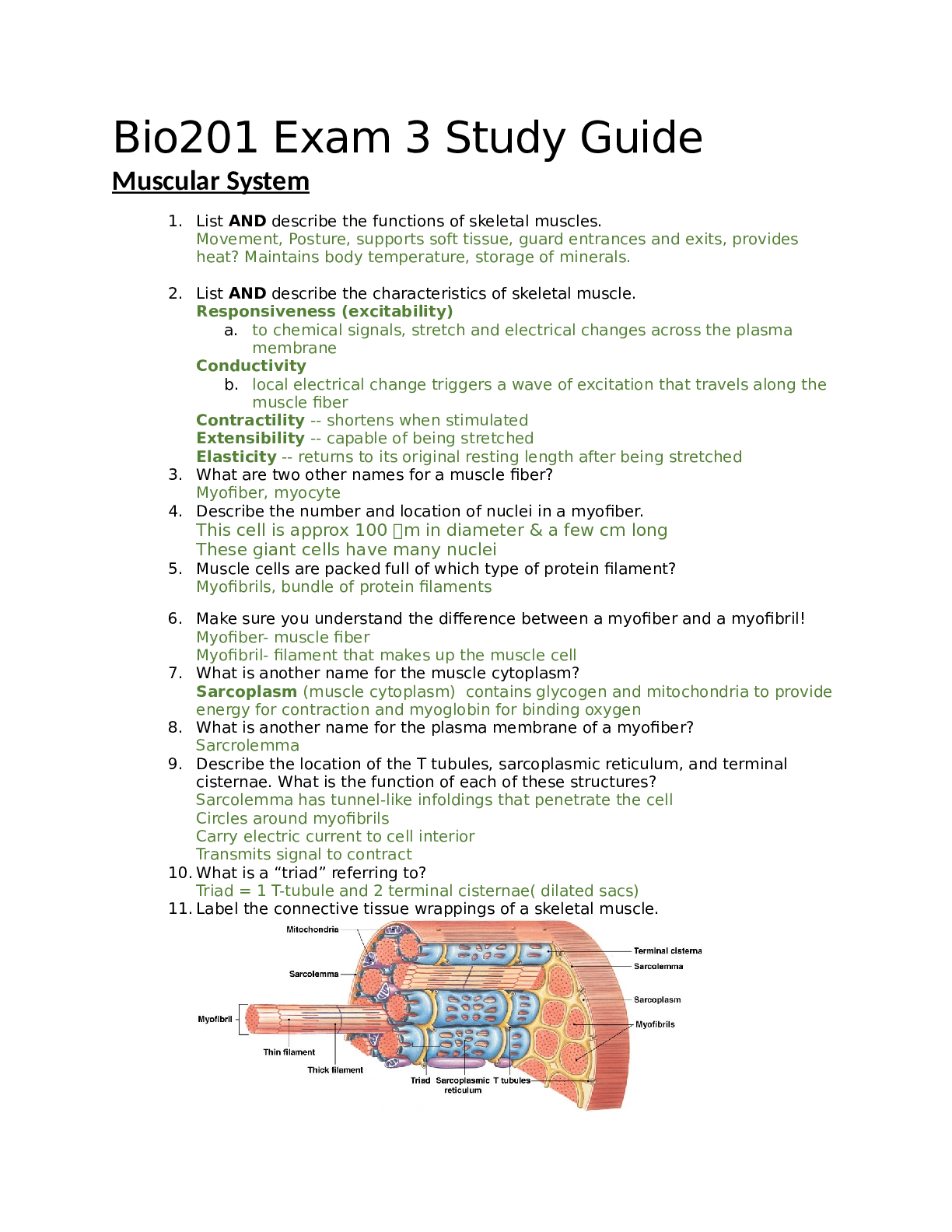
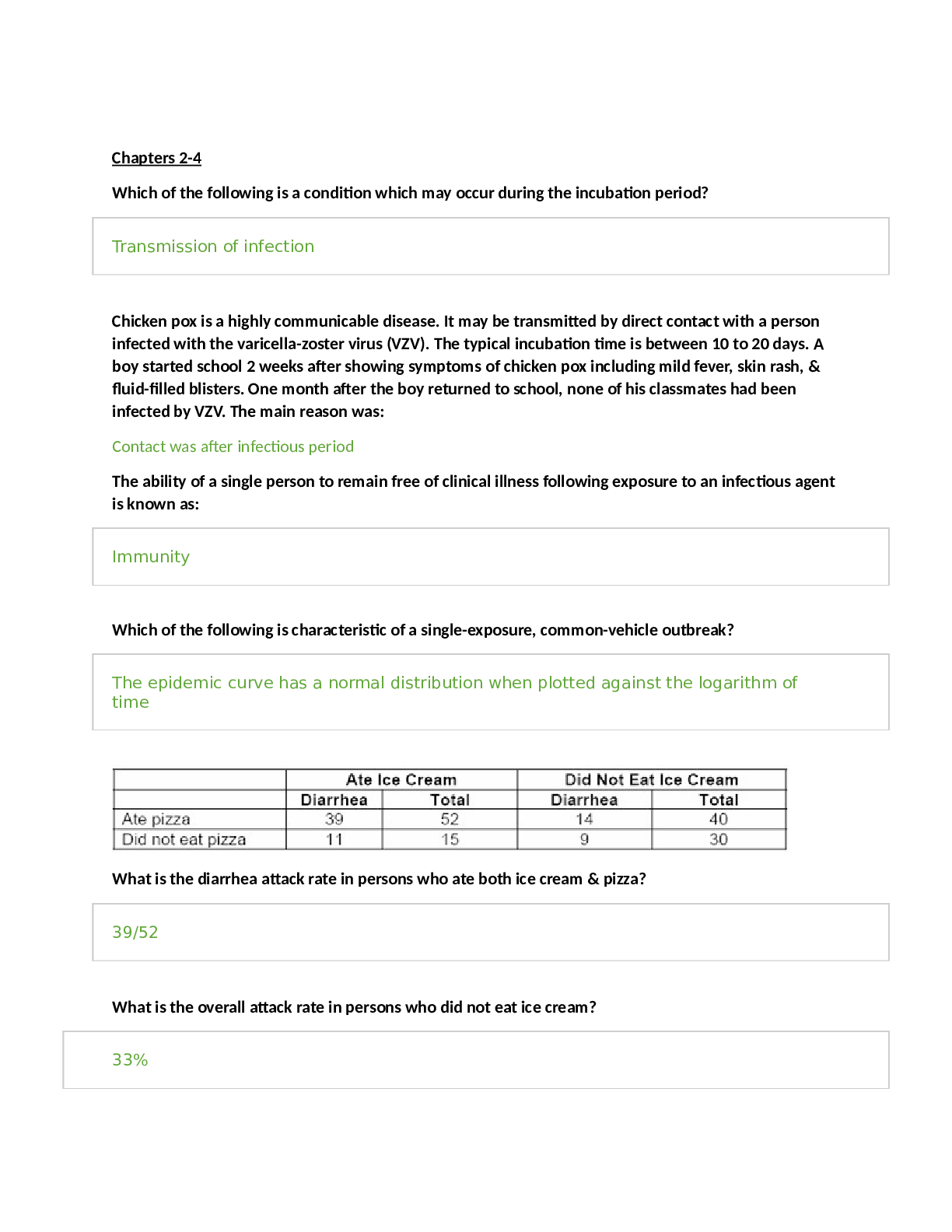
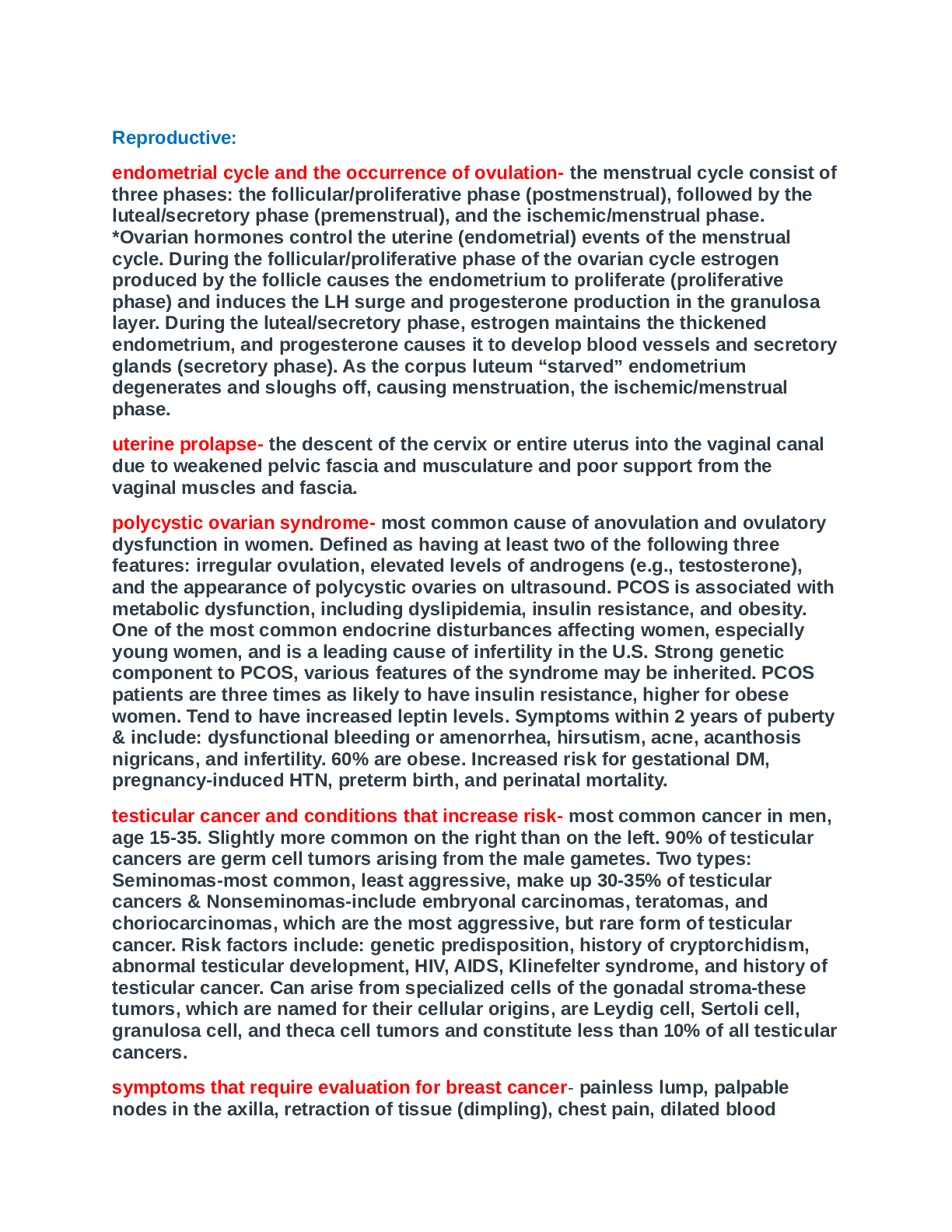
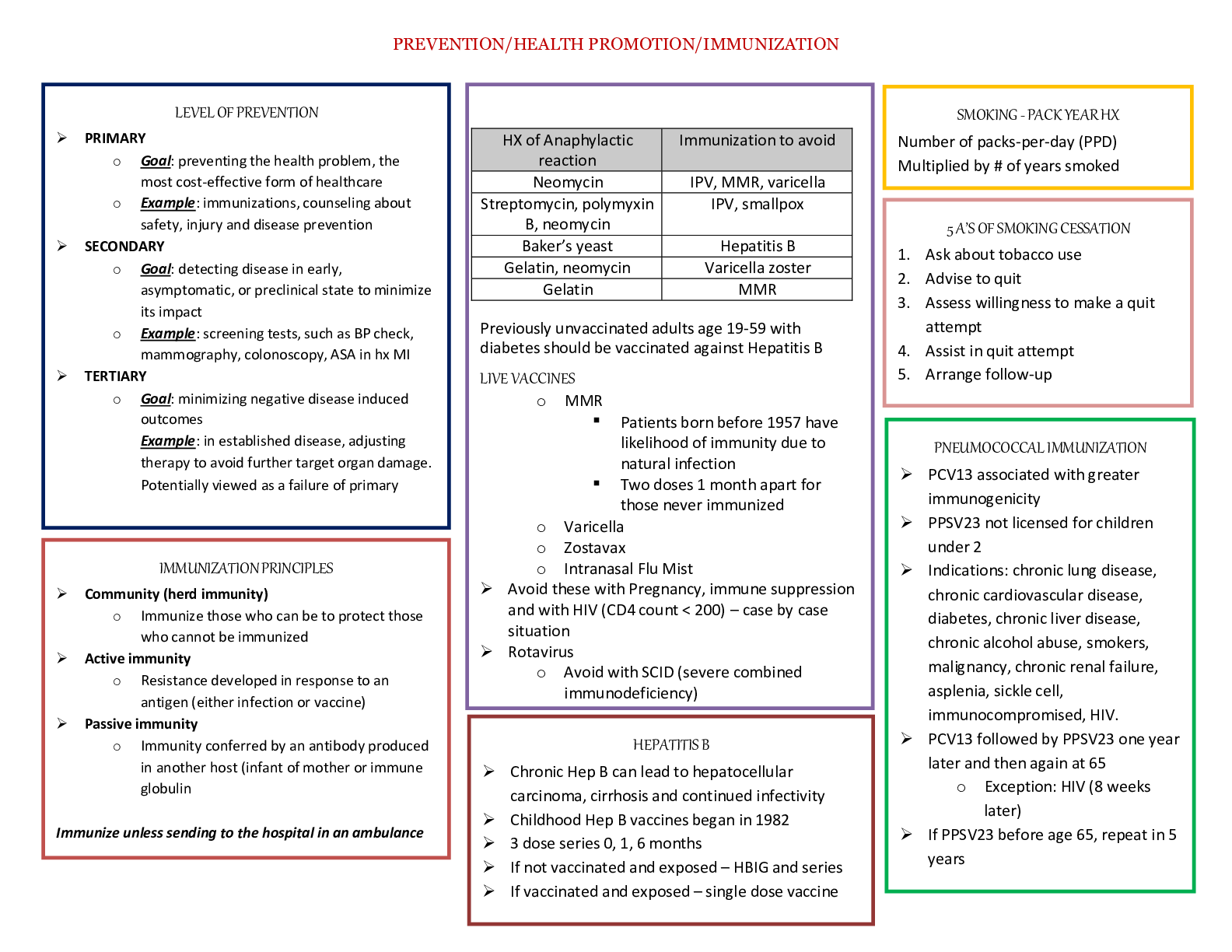
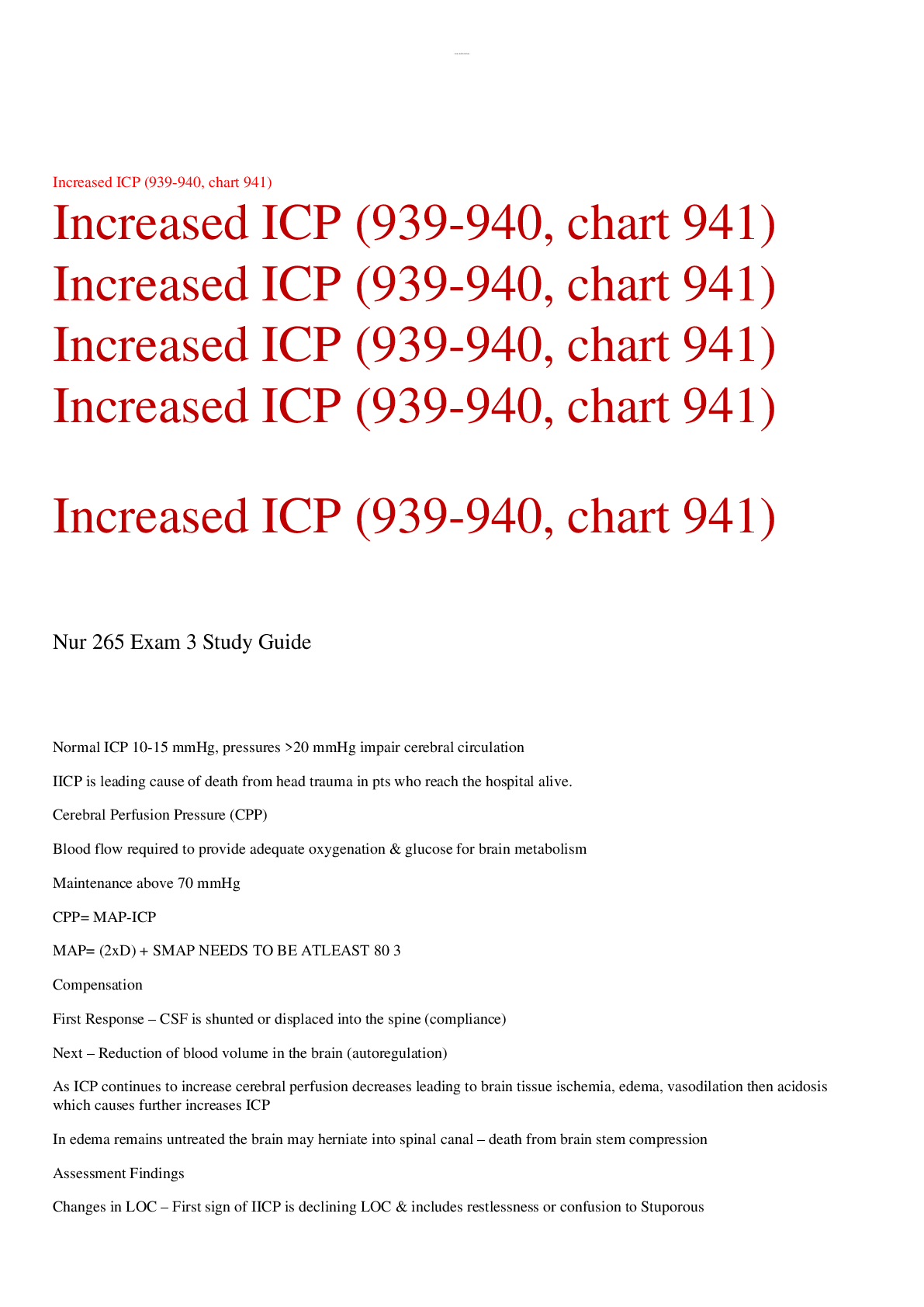
Pathophysiology Exam 3 Study Guide Hematopoiesis ~9 Questions Distinct features of erythrocytes, what they do, how they do it. • RBCs: responsible for oxygen transport. o Once mature, have no or... ganelles, no protein synthesis, do not go through mitosis. Discoid in shape, flexible structure. Life span changes, what happens as they age • Life span of 120 days, +- 20 days o Altered by conditions, decreased in certain conditions. o As RBCs age ▪ Lose flexibility ▪ Lysed or phagocytized ▪ Removed by the mononuclear phagocytic system. ▪ Erythropoiesis slows as we age. Regulation of RBC • Requires hematopoietic growth factors (HGF) o Growth factors 1. CSF- colony stimulating factors a. cytokines that act as hormones b. stimulate progenitor cells c. stimulate maturation of cells d. prevent apoptosis 2. EPO- erythropoietin a. Hormone carried form kidney through blood to marrow. b. released as response to hypoxia c. stimulate uncommitted cells to become RBC’s d. stimulate yellow marrow conversion to red marrow 3. IL-3++ (cytokine) a. Regulate the reproduction, maturation, and functional activity of blood cells. b. increased with inflammation/infection c. stimulate proliferation/maturation of immunocytes 4. Other cytokines/interleukins 5. Testosterone and Androgenic steroids- a. hormones that stimulate leukocyte production. b. Stimulate EPO, thereby increasing RBC’ c. Leads to increased erythropoiesis. What is the significance of reticulocyte count (elevated, decreased, and/or normal) in the context of anemia? • Reticulocyte count o Indicates bone marrow response to anemia. • Increased o New RBC’s produced and sent into circulation. (GOOD) • Decreased-problem o Compensatory mechanisms failed • Normal o Not normal in the anemic patient, should be increased in the anemic patient. Hemoglobin formation: heme, globins, oxygen carrying capacity. • Hemoglobin Synthesis o Hgb- the oxygen carrying protein of the RBC ▪ A single RBC contains as many as 250 billion hemoglobin molecules. o Globins- polypeptide chains ▪ Alpha chains (2) ▪ Beta chains (2) o Heme- Iron-protophoryn complexes ▪ 4 in Hgb ▪ Carry 4 O2 per each Hgb How is iron involved in hemoglobin formation? How is it brought into the body, stored, used? What are protophoryn and transferrin? • Iron o Required for RBC proliferation and Hgb synthesis o Absorbed form the duodenum and upper jejunum o Present within the plasma and extracellular fluid • Bound to transport protein, Transferrin o Helps get rid of 02 to cells. o Iron has to be properly charged, if not unusable. • Protoporphyrin o Organic compound that when complexed with ferrous iron, the molecule becomes heme. • Iron storage o Stored as ferritin ▪ Single iron chain o Hemosiderin ▪ See in bruising, gives blueish green color o Stored In ▪ Macrophages of the liver, spleen, bonemarrow. ▪ Hepatic parenchymal cells: tissue cells. What are the importance of Vitamin B12 and folic acid? Specific CNS symptoms of B12 deficiency. • B12 and Folic acid o Required to support proliferation and maturation of developing RBC o Deficiencies produce profound effects ▪ Cells are enlarged (macrocytic) ▪ Nuclei appear immature ▪ Extensive destruction of cells at the normoblast stage. o Essential for normal DNA synthesis in proliferating RBCs o B12 deficiency-myelin degeneration may occur with los of nerve fivers in spinal cord ▪ Paresthesia ▪ Gait disturbances ▪ Weakness ▪ Spasticity ▪ Reflex abnormalities. Anemias-general cause of symptoms • Hematological disorder of underlying pathology o Characterized by a decrease in Hemoglobin and/RBCs o Results when RBC loss or destruction exceeds production or ineffective RBC production. • Anemias morphologic Classification o Microcytic Hypochromic: little cell, pale color o Macrocytic Normochromic: big cell, normal color o Normocytic Normochromic: both normal • Etiology of Anemias o Blood loss o Impaired production of RBCs ▪ Diet: iron deficiency ▪ Genetic: sickle cell ▪ Bone marrow problems: leukemia o Increased RBC loss or destruction ▪ Genetic or autoimmune • Signs & Symptoms o Mild anemia in otherwise healthy individual generally asymptomatic o Symptoms become more pronounced and work capacity is reduced as severity of anemia increases. • Severity and nature of symptoms o Age and general health o General: weight loss, fever, night sweats o CNS: hypoxia ▪ Insomnia, inability to concentrate, disorientation. o G.I. ▪ Loss of appetitie ▪ Indigestion o Renal ▪ Decreased blood flow stimulates renin-angiotensin system • Sodium and water retention ▪ EPO production o Cardiovascular ▪ With baseline vascular disease, sudden onset of localized ischemic manifestations. ▪ Elderly patients should be carefully monitored for angina, heart failure, claudication, severe GI dysfunction, or marked CNS symptoms even when Hgb is 10g/dL. o Hemorrhage ▪ Reduction in number in RBCs ▪ Fluids move form interstitial into vessels and plasma volume expands o Decreased viscosity cause more turbulent flow ▪ Ventricular dysfunction ▪ Cardiac dilation ▪ Heart valve insufficiency o Decreased oxygen delivery to tissues (skin) ▪ Delayed wound healing ▪ Loss of elasticity ▪ Early graying of the hair o Skin, mucous membranes, lips, nail beds, conjunctivae, palmar creases become pale. • Iron deficiency Anemia: how does it happen, how do different stages influence symptoms. o Most common type of anemia: worldwide o Developing countries more prevalent. o Blood loss of 2-4ml/day can cause anemia. o Occurs in Stages ▪ Stage I: body’s iron stores are depleted: few symptoms. ▪ Stage II: not enough Iron for BM, iron deficiency begins once iron stores depleted fully. ▪ Stage III: small deficient cells replace normal cells in periphery. • Progressive severe symptoms can progress to nerves and muscles. • Pernicious anemia: normochromic, macrocytic o Cause: malabsorption of B12 o Defective gastric secretion of intrinsic factor ▪ Congenital deficiency ▪ Adult onset atrophy of gastic mucosa ▪ Partial/complete gastrectomy. ▪ Has autoimmune component, attack cells of the gut, thus no intrinsic factor. o Mechanism ▪ Atrophy of guy • ETOH, hot tea, smoking ▪ Inflammation ▪ IF deficiency leads to inadequate B12 absorption (AUTOIMMUNE) o More than 90% of individuals demonstrate parietal cell autoantibodies. • Hemolytic Anemia: Normochromic-normocytic: know general concept of what happens o Erythropoiesis is normal, production is increased, but can’t keep up with destruction. o Acquired or Hereditary ▪ Genetics, trauma, toxins: snake venom, radiation, autoimmune reaction. • Sickle Cell- What causes sickling, how does it lead to ischemia, how to relieve a crisis o Point mutation changes amino acid in translation. ▪ Autosomal recessive o Thus protein can unfold and cause clumping o RBC sickles becomes brittle loses flexibility and clogs up vasculature. o Persistent hypoxemia causes further reduction in PO2 in the microcirculation, RBCs sickle o How to treat crisis ▪ Giving volume, warm body temp, allows cells to regain shape and resume normal function ▪ Limit crises to prevent long term organ damage . • Thrombocytopenia o Deficient number of circulation platelets o Most common cause of hemorrhagic disorders. o Congential or acquired: more common. o Results from ▪ Decrease or defective platelet production, or increased platelet destruction. • Idiopathic Thrombocytopenic Purpura (ITP) o Immunologic platelet destruction o Acute ▪ Post-viral thrombocytopenia ▪ Usually affects child ages 2-6 o Chronic ▪ Essential thrombocytopenia ▪ Adults older than 50, especially women 20-40. • Disseminated intravascular Coagulation (DIC) o Massive Endothelial damage: lots of procoagulation factors released. o Simultaneous clotting and hemorrhage: abprutio placenta. o Increased protease activity in the blood. ▪ Unregulated release of thrombin’ ▪ Subsequent fibrin formation and accelerated fibrinolysis o Activated thrombin > antithrombins. o Widespread Thromboses ▪ Organ hypoperfusion, ischemia, and infarction o Bleeding ▪ Depletion of clotting factors ▪ Platelet destruction via Ashwell morrell receptors ▪ Very high mortality rate o Treatment ▪ Find and relieve source of bleeding o Signs and Symptoms ▪ Wide variability ▪ Bleeding from veinpuncture sites/arterial lines ▪ Purpura, petechiae, and hematomas, Cyanosis of the fingers and toes ▪ Multiple organ failure. Endocrine (~9 Questions) Lipid soluble versus water-soluble hormones 1. Receptors - Specificity- ability of receptor to bind with hormones/proteins - Affinity- strength of the bond (Hgb binding to CO2/O2 example) - Up regulation- higher amounts of something will increase number of receptors on cell - Down regulation- when certain substances are present then other things get pulled back into the cell - Permissiveness- when hormone is present it increases action of another hormone/protein (cortisol influences blood glucose) 2. Water Soluble Hormones – bind with something on cell membrane - When bound are completely inactive - Second messengers a. cAMP b. cGMP c. calcium - Examples a. peptide hormones b. catecholamines- help muscles contract; ramp things up 3. Lipid Soluble Hormones – have to get in the cell and act on nucleus - Majority bound in circulation - Receptors located in cytoplasm - Activate genes - Examples a. Steroid hormones b. Thyroid hormones Positive and negative hormone feedback loops 1. Hormone Release - Negative feedback (most common) a. Glands stimulate pituitary/hypothalamus to shut off the loop - Positive feedback a. Oxytocin – levels rise during birth Pituitary gland- hormones produced (anterior versus posterior), their actions. IV. Posterior Pituitary (Neurohypophysis) a. Hormones are synthesized in the hypothalamus and stored in the pituitary. 1. Arginine vasopressin - water regulation (a.k.a. Antidiuretic hormone, ADH) 2. Oxytocin - uterine contraction V. Anterior Pituitary (Adenohypophysis) 1. Hormone secretion is under the control of releasing hormones from the hypothalamus. 2. Hormones travel through the hypothalamic-pituitary portal system 3. Hormones - Adreno corticotrophic hormone (ACTH) - Thyroid stimulating hormone (TSH) - Follicle Stimulating Hormone (FSH) - Luteinizing Hormone (LH) - Prolactin - Growth Hormone - Melanocyte Stimulating Hormone - Lipotropin - Endorphins SIADH- pathophysiology, and clinical presentation (particularly in relation to pathophysiologic mechanism) SIADH (Syndrome of Inappropriate Antidiuretic Hormone) -Etiology - Increased AVP (ADH) -**Body holds onto too much H20; Problems= fluid overload -Causes - Tumor tissue a. Head trauma b. Medications- morphine, nicotine c. Stroke -Clinical presentation d. Free water overload e. Decreased urine output f. Increased urine specific gravity g. Hyponatremia DI- pathophysiology and clinical presentation (particularly in relation to pathophysiologic mechanism). nephrogenic versus neurogenic. Etiology - Decreased AVP (ADH) - Causes - Neurogenic (problem with synthesis/secretion) a. Tumor hypothalamus/pituitary b. Trauma c. Primary tumor d. Metastatic Cancer e. CNS infections- meningitis f. Medications - Causes - Nephrogenic (problem with receptor binding) a. Renal disease b. Renal transplant c. Heredity- receptors are fewer or less functional - Clinical presentation a. Dehydration b. Increased urine output c. Dilute urine d. Hypernatremia Physiologic axis- understand the HPA axis, primary versus secondary disease process. HYPOTHALAMUS PITUITARY THYROID ADRENAL GONADAL Hypothalamus produces neurohormones (ADH) that go down to pituitary -Hormones that kick things off Tertiary= Hypothalamus Dysfunction Secondary= Pituitary Dysfunction Primary= Gland Dysfunction (Thyroid, Adrenal, Gonadal) Thyroid hormones- T4, T3, and rT3. Also TRH and TSH. What they do, how they interact in normal and pathologic states. VI. Thyroid function 1. Cellular metabolism 2. Blood pressure maintenance 3. Some growth functions 4. Temperature maintenance HYPOTHALAMUS - TRH PITUITARY - TSH THYROID VII. Thyroid Hormones 1. Thyroxine (T4) - 90% of circulating hormone; inactive 2. Triiodothyronine (T3) - physiologically active hormone 1. Most made from conversion from T4 with iodine 3. Thyrocalcitonin - calcium regulation 4. Regulation of secretions - HPA Hyperthyroid and hypothyroid states- patho, different syndromes and causes, signs and symptoms related to patho. Patho related to Sick Euthyroid syndrome. VIII. Hyperthyroidism 1. Increased production and release of hormone 2. Increased conversion of T4 to T3 in the periphery 3. Results in increased metabolic rate and oxygen consumption (entire body) 4. Thyroid crisis a. occurs in patients with pre-existing hypersecretion b. sudden increase in catecholamine receptors from stress (surgery) 5. Causes a. Grave’s disease - autoimmune attack on thyroid gland b. Adenoma – benign tumors c. Thyroiditis d. Over treatment of hypothyroid state e. D/C of antithyroid meds f. Iodine load with preexisting hyperthyroid state (CT dyes) 6. Clinical presentation a. increased metabolic rate b. tachycardia, atrial arrhythmias c. dyspnea, palpitations d. restlessness, irritable, wakefulness e. anxiety f. heat intolerance g. weight loss h. increased GI motility, diarrhea i. exopthalmia – bulging eyes j. enlarged gland/goiter IX. Hypothyroidism 1. Inadequate circulating hormone 2. Primary = disorder at the level of the thyroid gland (95%) 3. Secondary/tertiary = disorder at the pituitary/hypothalamic level (5%) 4. Causes a. Most common cause is surgical removal/ radioiodine ablation for the treatment of hyperthyroidism b. Idiopathic c. Hashimoto’s thyroiditis –inflammation causes hyperthyroidism and then scarring ultimately leads to hypothyroidism d. Hypophysectomy, pituitary radiation e. Stress states with pre-existing hypothyroidism (surgery) 5. Clinical presentation a. bradycardia b. lethargy, decreased LOC, coma c. hypothermia d. hypoventilation e. decreased GI motility, constipation f. weight gain 6. Myxedema coma a. extreme hypothyroid state b. interstitial accumulation of a mucopolysaccharide c. lowered metabolic rate X. Sick Euthyroid Syndrome -Not a thyroid problem -SES is adaptive response to non-thyroidal illness -T4 is converted to rT3 (physiologically inactive hormone) -Seen in 70% of hospitalized patients -No long-term bad effects; good thing HORMONE CONVERSION T4 Energy RT3 T3 Normal Saving Path T2 Adrenal cortex- zones and associated hormones. Regulation of secretion of these hormones. Adrenal medulla- hormones; Adrenal insufficiency- Causes, patho and symptoms related to patho. IV. Adrenal Cortex 1. Hormones a. Zona Glomerulosa – mineralocorticoids (aldosterone) b. Zona Fasciculata - glucocorticoids (cortisol) c. Zona Reticularus - androgens 2. Regulation of secretions- HPA -Adrenal secretions manage: -Sugar -Energy -Fluid (RAA function/dysfunction) - aldosterone HYPOTHALAMUS - CRF PITUITARY - ACTH ADRENAL -(Glucocorticoids and androgens) V. Adrenal Medulla Hormones - Catecholamine’s -epinephrine (80%) -norepinephrine (20%) (precursor to epi) VI. Adrenal Insufficiency 1. Sudden and severe decrease in levels of hormone 2. Primary disease requires 90% loss of adrenal gland 3. Secondary at the level of pituitary (lose ACTH) 4. Causes a. Decompensation in patients with chronic adrenal insufficiency b. Destruction of the adrenal glands - hemorrhage (from HTN & TB) c. Abrupt cessation of chronic steroid therapy 5. Clinical presentation a. hypoglycemia b. hypotension – loss of aldosterone and catecholamine c. hyponatremia – Na loss from loss of aldosterone d. hyperkalemia (primary) e. hyper pigmentation (primary)- increase in POMC Renin-Angiotensin-Aldosterone System Regulation of secretions - Renin-angiotensin Low BP low renal flow renin release angiotensinogen angiotensin angiotensin II aldosterone secretion Aldosterone increases Na & H20 absorption at level of kidney in exchange for Potassium Hypercortisolism- different types (ACTH dependent and independent)- patho and differences in cause. Symptoms related to patho. Cortisol and glucose relationship. IV. Hypercortisolism 1. Cushing’s Disease/Syndrome a. Usually not acute; long-standing problem b. Iatrogenic – we give something to increase cortisol secretion c. Spontaneous 2. ACTH-dependent (pituitary) (Cushing’s Disease) a. adrenal cortical hyperfunction b. ectopic ACTH syndrome -Excess ACTH that leads to excess cortisol 3. ACTH-independent (adrenal) (Cushing’s Syndrome) -Problem with adrenal gland itself -Normal ACTH but excess Cortisol a. autonomous adrenal cortical hyperplasia b. tumorous adrenal cortical hyperfunction c. adenoma d. carcinoma 4. Clinical presentations a. hyperglycemia b. redistribution of adipose tissue (moves from legs/arms to abdomen) c. decreased protein synthesis e. osteoporosis - weakened protein matrix f. impaired humoral antibody production – drop in immune function Edema- thin skinning; shiny skin Hyperaldosteronism- primary and secondary. Patho, cause and symptoms IV. Hyperaldosteronism 1. Alteration in fluid and electrolyte balance 2. Primary - excessive production in adrenal gland from either a tumor or hyperplasia 3. Secondary - decrease in the pressure in the renal glomerulus activating the renin- angiotensin system 4. Causes a. CHF b. cirrhosis c. nephrotic syndrome d. partial occlusion of renal artery 5. Clinical presentations a. endocrine hypertension (2% of HTN – secondary) b. extracellular fluid expansion - Edema c. hypernatremia d. hypokalemia e. metabolic alkalosis – later stage; low K leads to Hydrogen exchange for Na Pheochromocytoma- major malfunction, causes, Symptoms related to patho. IV. Pheochromocytoma 1. Tumor in the medulla (90%) 2. Tumor of sympathetic ganglia 3. Excessive production of catecholamines 4. Clinical presentation a. hypertension - episodic b. headache – from HTN c. diaphoresis d. tachycardia e. weight loss f. emotionally labile Diabetes Mellitus- Patho. Classifications. Cellular level patho. IV. DIABETES MELLITUS 1. Overview a. Heterogeneous syndrome b. Glucose intolerance in common 2. Classifications a. Type 1 - lack of endogenous insulin production i. loss of beta cells in islets of Langerhans ii. immune mediated or idiopathic iii. 10% of cases, juvenile to adult onset iv. LADA v. HLA genotypes vi. Environmental exposures (viral, diet) vii. Prone to ketoacidosis b. Type 2 - insulin resistance and receptor deficit i. receptor driven? ii. genetic factors iv. environmental factors- high sugar diet, high saturated fats/transfats, obesity, lack of exercise. ‘Urban lifestyle’ v. ‘Prediabetes’ -Founder’s Effect- same people mating allowing genes to propogate c. Secondary i. surgery ii. glucocorticoids iv. pancreatic disease d. Gestational i. Type 2 like ii. 2-10% of pregnancies iii. May resolve after pregnancy- 90-95% 3. Insulin a. Anabolic hormone b. Major sites - liver, muscle, adipose tissue (red blood cells and brain cells do not require insulin) c. Cellular actions (***KNOW THESE***) i. Increases Glucose uptake ii. Increases Protein synthesis iii. Increases Carbohydrate Metabolism iv. Decreases Fat Metabolism DKA- Patho. Metabolic abnormalities, pathogenesis and symptoms related to patho. IV. Diabetic Ketoacidosis (DKA) 1. Overview a. Physical and/or emotional stress can precipitate onset b. 25-30 % no previous diagnosis of Diabetes c. Usually rapid onset 2. Metabolic Abnormalities a. Reduced glucose uptake b. Increased glucose production in the liver c. Increased metabolism of fatty acids – more ketones d. Upregulates gluconeogenesis 3. Pathogenesis a. Hyperglycemia b. Metabolic acidosis 4. Clinical Presentation a. Hyperglycemia (300-500 mg/dl) b. Polyuria and polydypsia c. Hypernatremia d. Hypokalemia d. Metabolic acidosis - Kussmaul resp. –ketone production e. Altered level of consciousness/coma ***More common in type 1*** HHNK- Patho. Symptoms related to patho and differentiation from DKA. Hyperglycemic Hyperosmolar Nonketotic Syndrome (HHNK) 1. Overview a. Precipitating factors i. physiologic stress (most common – marathon) ii. hypertonic feedings iii. hyperalimentation iv. renal dialysis (physiological stressor) b. Slow onset c. High mortality (40 - 70%) 2. Metabolic abnormalities - Reduced peripheral uptake of glucose (slowly) a. Enough to meet cell needs and therefore prevent cell starvation b. Inadequate to maintain normal serum glucose levels 3. Pathogenesis a. Hyperglycemia b. Intracellular and extracellular volume deficit -Will try to dump extra glucose by diuresing -Pulled first out of blood stream, then extracellular, then intracellular 4. Clinical Presentation a. Polyuria and polydypsia b. Hyperglycemia (1200 mg/dl +) (over periods of weeks) c. Altered level of consciousness/coma d. Mortality rate 40-70% ***Severity of hyperglycemia is a factor*** Hypoglycemia- Patho and symptoms related to patho. IV. HYPOGLYCEMIA 1. Overview a. Inadequate circulating glucose b. Defined as a blood glucose of < 50mg/dl 2. Clinical Presentation a. Adrenergic i. anxiety – impending doom ii. sweating iii. hunger iv. tachycardia b. Neuroglycopenic i. confusion ii. weakness - generalized iii. slurred speech iv. seizures Somogyi phenomenon- Patho and symptoms related to patho. Somogyi phenomenon a. Rebound hyperglycemia Glucose drops steadily until 3-4am then spikes high b. Clinical presentation i. nightmares ii. morning headaches iii. inconsistent glucose levels/elevated am glucose Food right before bed might help Cancer cell and Dysfunction (~ 11 Questions) Phases/stages of carcinogenesis and factors associated with phases -**Cancer is genetic disease that consists of different combinations of genetic alterations. It takes SEVERAL different types of alterations to contribute to malignant changes in the cell. Most cancers are sporadic and NOT hereditary.** Stages of Carcinogenesis 1) Initiation a. Carcinogen interacts with/damages DNA b. Repair can occur after this point and can be REVERSED c. Initiating event is genetic mutation oncogene 2) Promotion a. Reproduction or proliferation of damaged cells, forming a mass of cells or benign tumor b. At beginning removal of promoting agent can stop the expansion of tumor mass c. Reversible in early stages 3) Progression a. Irreversible b. Involves a number of sequential mutations in genes including oncogenes and tumor suppressor genes c. End result is tumor malignancy **6 Hallmarks of Cancer** 1) Evasion of Apoptosis – produce IGF survival factors -**One of most important factors for survival of cancer (live longer, grow faster) -**P53 Gene – commonly mutated tumor suppressing genes –responsible for evasion of apoptosis 2) Self-Sufficiency in growth signals – activate H-RAS oncogene -Modulation of extracellular growth signals -Alteration of trans-cellular signal transducers (surface receptors) -Deregulation of intracellular signaling pathways (such as RAS) 3) Insensitivity to growth inhibition signals – Lose Rb suppressor -Most/All anti-proliferative signals are funneled through retinoblastoma (Rb) -TGFB suppresses cell growth -Downregulation of Smad 4 4) Limitless replicative potential – turn on telomerase -**Cancer cells lengthen telomeres – allowing to keep replicating -Limit for most cells is 60-70 divisions 5) Sustained angiogenesis – produce VEGF -Acquire/inherit their own blood supply -**VEGF stimulates angiogenesis initiation 6) Tissue invasion/metastasis – inactivate E-cadherin -Cell-cell adhesion molecules (CAMs) and integrins** -Adaptation required through shifts in the spectrum of integrin alpha and beta s ubunits -**Metastasis account for 90% of cancer deaths** Proto-oncogenes- stimulate cell to grow, divide, and move through cell checkpoints -Mutation leads to oncogenes that do not go through checkpoints -Oncogenes= bad (HER-2, EGFR, RAS) Genes implicated in Cancer Prime Suspects= -Oncogenes -Tumor Suppressor Genes (P53) -DNA Repair Genes (BRCA 1 & 2) Characteristics of malignancies, metastasis, benign tumors -**Benign tumors grow locally only and do not metastasize** -Metastasis Patterns- related to: -Circulatory flow – colon cancer seeds to liver via portal vein -Lymphatic system – sentinel node= primary node to where they travel; take out sentinel node and almost sure the rest of the nodes are negative -Seeding of surface of body cavities -Protease- Plasmin – allows the destruction of protective extracellular matrix allowing for metastasis **Most malignant tumors are epithelial in origin Cancer classification system and prognosis TNM Stage T- tumor size or original and whether is has invaded nearby tissue Tx: cannot be evaluated Tis: carcinoma in situ T0: no signs of tumor T1-4: size of tumor N- nodes; describes nearby lymph node involvement Nx: cannot be evaluated N0: absent from regional lymph nodes N1-3: degree of spreading M- metastasis; describes distant metastasis M0: no distant metastasis M1: metastasis to distant organs G- degree of differentiation G1: well differentiated G2: moderately differentiated G3: poorly differentiated G4: undifferentiated Theories related to Cancer: Double Hit theory, Seed and Soil Hypothesis Seed & Soil Hypothesis -Tumor Cells (Seed); Distant Tissue (Soil) -Hypothesis that suggests certain cancers metastasize to certain tissues where they like to grow. For example, lung cancer will metastasize to brain, but not breasts. Breast cancers will metastasize to lung. -Grow where they are happy -TSG and Oncogenes do not play role in development of metastasis Double Hit Theory 1st Event - Initiation -Carcinogen = Initiatior 2nd Event – Promotion -Agent = Promoter -Lag period- time between exposure (first hit) and development of clinically apparent cancer Viruses and cancer- relationship 7 Different Viruses Related to Cancer -Epstein-Barr b cell lymphoma, nasopharyngeal cancer -Hepatitis B & C liver cancer, non hodgkins; from recurrent infections -Human Papillomavirus cervical, anal, oropharyngeal cancer -Human T-cell lymphotropic -Kaposi’s Sarcoma Herpesvirus -Merkel Cell Polyomavirus Bacteria: H. pyloria stomach cancer -Chronic Inflammation- can damage DNA, proteins, cell surfaces -Interaction with Cellular DNA- activates genes that promote growth of tumors or inactivates genes that prevent tumor growth -Immunosuppression- decreases efficiency in recognizing cancer cells Discuss progression of cancer- angiogenesis -Every tumor has to learn/acquire angiogenesis or they will not survive* -Angiogenesis- induction of blood vessel growth -Anti-Angiogenesis: -Inhibit endothelial cells that line the blood vessels -Endostatin, Combretasatin A4, Thalidomide -Inhibit angiogenesis signaling cascade -Bevacizumab, Interferon Alpha -Block endothelial cells from breaking down extracellular matrix -Marimistat, Neovastat Latency period Can be up to 20 years or more -From initiation up until malignancy Tumor suppressor genes Act to stop cell growth – prevent cancer -**P53- transcription factor that regulates cell division/death -Rb- alters activity of transcription factors (controls division) -APC- controls availability of transcription factors Characteristics of tumor cells -Senescene- limits the total number of times cells can reproduce themselves -Identifiable at 1 gram in size and 30 population doublings; slows down by detection Gompertzian Equation- most tumors originate 2 years prior to detection -30 doublings= clinically detectable; 7th & 10th doubling = metastatic potential Change in bowel/bladder habits A sore that does not heal Unusual bleeding or discharge Thickening or lump in the breast, testicles, or any part of the body Indigestion or difficulty swallowing Obvious change in a wart, mole, or skin condition Nagging cough or hoarseness Cancer prevention- proto-oncogenes Proto-oncogenes- stimulate cell to grow, divide, and move through cell checkpoints -Mutation leads to oncogenes that do not go through checkpoints -Oncogenes= bad (HER-2, EGFR, RAS) Cancer treatment: targeted therapy, stem cells, all those discussed Local- surgery, radiation Systemic- chemo, targeted therapies, immunotherapy Surgery- 90% have some; 75% presumed curative Radiation- Ejects electron charged – unstable – damages tissue -Deeper= loses charge -Radiosensitive cells- rapidly diving cells -Tissue tolerance – different delivery systems -Gray is the radiation absorbed Chemo- blunt tool, can damage both cancer and normal cells SE- n/v, nerve damage, bone marrow suppression -Predicted cell death: alkylating agents, anti-metabolies, anti-tumor antibiotics, plan alkyloids -Fractional cell kill in logarithmic fashion for best cure -Resistance is common – combination therapy works best Goldie Coldman Model= 10k1mil divisions = resistance -Smaller tumors are less likely to be resistant Immunotherapy: Vaccines- trigger immune system, produce anti-tumor response Monoclonal Antibodies- illicit immune response- marks cancer cells Angiogenesis Inhibitors (Avastin) Checkpoint Inhibitors- “releases the brakes” Cytokines- inerleukin-2 and interferon –a Targeted Therapies: Target oncogenes (epidermal growth factor receptor and HER-2) Target oncogenes (signal transduction molecules) Target adhesion molecules/matrix proteins Tumor cell markers -Substances produced by cancers -Hormones, enzymes, antigens, antibodies -Used: diagnosis, tracking, screening -Examples: Alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), human chorionic gonadotropin (HCG), lactate dehydrogenase (LDH), prostate specific antigen (PSA), and neuron Discuss proteomics Changing levels of active proteins inside tumor cells – could help determine diagnosis and treatment effectiveness Rationale for why cancer occurs more frequently in different age groups Cancer trajectory and risk factors from first contact to clinical evidence of malignancy Hormone release from cancer cells Genetic factors and cancer development Manifestations of Cancer Exam 3- Part 2: Abnormal Cardiovascular content Abnormal adult (~12 Questions) Hypertension Determinants of BP Primary –v- secondary –v- isolated systolic hypertension Mechanism of primary hypertension Causes of secondary hypertension Emerging risk factors for secondary hypertension Complications of prolonged, uncontrolled hypertension. HTN- sustained elevation of systemic arterial blood pressure Associated with: -Endothelial dysfunction -Vascular smooth muscle constriction or remodeling -Increased impedence to LV ejection -Propensity for atherosclerosis -…often but not always manifested by an elevated blood pressure Normal BP= <120/ <80 Pre-HTN= 120-139/80-89 Stage 1 HTN= 140-159/90-99 Stage 2 HTN= ≥160 / ≥100 Diagnosis: -Average 2 or more BPs made on 2 more consecutive clinical visits -Seated at rest for 5 minutes on chair, feet on floor -Arm at heart level -No smoking/exercise/eating prior 30 minutes -Take 3 measurements and record average of last 2 Manifestations: -Early stages- none -Difficult to achieve tx compliance due to no symptoms, but SE of medications -Undetected- promotes accelerated atherosclerosis and CVD beginning at age 30 -Results in end organ damage Results: -Each increment 20/10mmHg doubles risk of CVD starting at 115/75 -Pre-HTN signals need for increased education to reduce BP -Lowering BP lowers stroke, MI, HF in that order Classifications (HTN): -Primary- -No known cause (90-95% of all cases) -Most combined systolic/diastolic HTN -SBP rises throughout life -DBP rises until 50, plateaus, then falls -DBP HTN more potent predictor until age 50, SBP more important at >50 -SBP more difficult to control -Pts with HTN tend to secrete less salt in urine, holding onto volume Etiology: -Complicated interaction between genetics and environment -Increases vascular tone and blood volume sustained increase in BP -Increased osmolality – increased ADH = concentrated urine = increased free water absorption -SNS: Overactivity of catecholamines increase PVR -RAAS: -Ang 2= remodeling, endothelial dysfunction, platelet aggregation, myocardial hypertrophy -Aldosterone= Na retention, toxic to CV system -Insulin Resistance: -Leads to hyperinsulinemia endothelial dysfunction -Activates Norepi and Ang II (heart toxins) -Increases dyslipidemia, BP -Contributes to target organ damage -Inflammation/Endothelium Dysfunction: -Endothelial injury/tissue ischemia cytokine release -Vascular remodeling, smooth muscle contraction, decreased vasodilators (NO), increased vasoconstrictors (endothelin) -Decreased renal perfusion tubular ischemia & preglomular arteriopathy -Decreased Na filtration -Increaed Na retention -Natriuretic peptides: -Modulate renal Na excretion – ANP, BNP, Urodilanton -Dysfunction: increased vascular tone, shift in pressure natriuretesis curve -Obesity: -Lepin, Adiponectin= vasoconstriction, Na/H20 retention, renal dysfunction -Sodium Intake: - >100meq/day (2.3g) Genetics: -Monogenic (rare)- increased renal Na reabsorption -Polygenic- inherited defects associated with renal Na excretion, insulin sensitivity, activation of SNS/RAAS, and cell membrane Na or Ca transport Blacks= variations of apolipoprotein L1 gene -Family Hx, Age, Gender, Black race, High dietary Na intake (small role), glucose intolerance, cigarette smoking, obesity, ETOH consumption, low dietary intake of K, Ca, Mg -Isolated Systolic HTN -Increased SBP with normal DBP (<90) -Occurs in Elderly -Rigidity of aorta due to atherosclerosis and/or aging of aortic valve -Important risk factor for CVD (treat aggressively) -Secondary- -Systemic disease process producing increased CO and/or SVR -Causes: -Renal disease -Oral contraceptives -Pheochromocytoma -Primary aldosteronism -Cushing’s Syndrome -Sleep apnea -Coarctation of the Aorta -Hypothyroidism -Primary Hyperparathyroidism -Malignant- -DBP >120 -Retinal hemorrhages, exudates, or papilledema -HTN encephalopathy- preeclampsia, acute glomerulonephritis -Urgently reduce BP -Hypertensive Urgency- -DBP >120 in asymptomatic patients -No benefit from rapid reduction Atherosclerosis Definition Lesion development- pathological events- How does a lesion grow? Modifiable –v- nonmodifiable risk factors Atherosclerosis- thickening or hardening of vessel wall -initiated by injury/inflammation leading to endothelial dysfunction and accumulation of lipid-laden macrophages within arterial wall lesion (plaque) Risk Factors: -Aging, smoking, diabetes, HTN, dyslipidemia, estrogen withdrawal, homocysteine, infection, inflammation, sedentary lifestyle -Role of oxidative stress in reduced endothelium-derived nitric oxide bioactivity and mechanisms of atherogenesis -Cytokines from inflammation prothrombotic state -Insulin resistance hyperinsulinemia -Increased norepinephrine and angiotensin 2; increased BP, dyslipidemia -Norepi, Ang 2, aldosterone myocardial toxicity, hyperinsulinemia -Endothelial Dysfunction -Impaired functions of vasodilation, antithrombosis, anti-inflammation -Inflammation no antithrombotic/vasodilating cytokines -Numerous inflammatory cytokines -Growth factors released which stimulate smooth muscle cell proliferation in affected vessel -Macrophages adhere to injured endothelium -Macrophages release enzyme and toxic O2 radicals that produce further injury and promote oxidation of LDL-C -LDL Oxidation 1) LDL enters intima through intact endothelium 2) Intimal LDL is oxidized into proinflammatory lipids 3) Oxidized LDL causes adhesion and entry of monocytes and T lymphocytes across endothelium 4) Monocytes differentiate into macrophages and then consume large amounts of LDL, transforming into foam cells 5) Foam cells release growth factors (cytokines) that encourage atherosclerosis (lead to fatty streaks) Do not obstruct blood flow Clinical Manifestations: -May have 50-70% occlusion before symptoms -Partial obstruction may results in transient ischemic events, often associated with stress or exercise -May lead to s/s of ischemic heard disease Lifestyle Modifcations: -Smoking cessation, exercise, weight reduction, control of HTN & DM, decrease fat& cholesterol intake 250-300mg/d -Meds= ASA, beta blockers, statins, ACE-I -Interventional= PTCA/Stents, CABG MI- basic problem When is ischemia not reversible at the cellular level? Classes of angina- define and be able to differentiate. Overall goal of MI treatment. Signs and symptoms of MI- know physical signs/symptoms, EKG changes and enzymes. What enzymes peak at what times? Ischemia (angina)- local state in which myocardial O2 supply is diminished to the extent that myocardial cellular metabolism is impaired -Stable -same amount of work everytime develops symptoms- usually does not rupture plaque -Variant (Prinzmetal’s)(vasospasm) -caused by a spasm -Silent Ischemia -Innervation problems (diabetes) -Unstable (ACS) -In process of rupturing -Infarction- -Endpoint of ACS, myocyte necrosis -Subendocardial= endo & myocardium (most common) -Transmurual= all 3 muscle layers -Subepicardial= endo & epicardium -STEMI and NSTEMI -Systolic dysfunction- reduced ability to squeeze -wall motion abnormality, decreased CO -increased end-diastolic volume -Diastolic dysfunction- reduced ability to relax -increased preload leading to increased wall tension -increased O2 consumption, incomplete emptying Sustained Ischemia: Stunned= acute Hibernation- reperfusion scan 24hrs later shows uptake of isotope (will survive) Cell Death Mechanisms: -Cell anoxic – 20 minutes -Anaerobic metabolism acidosis -Electrolyte disturbance -Catecholamine released -Angiotensin II release ACS Symptoms: -Precipitating factors -Pain: substernal chest pain, ache, squeeze, jaw pain -SOB -N/V, diarrhea -Weakness, dizziness -Palpitations -Cold perspiration -Sense of impending doom ECG Changes: -ST depression, T wave inversion, ST elevation Cardiac Enzyme Patterns: Death from MI= V-fib, cardiogenic shock, pulmonary edema STEMI: restoration of flow with early reperfusion of infarct-related artery limit infarct size, plaque stabilization, pain relief, optimize O2 supply/demand Unstable Angina/NSTEMI: early conservative vs. early invasive strategy Heart Failure/Cardiomyopathies- general concepts. What is/are the big problem/dysfunction, causes, symptoms, long term/outcome profile, etc… involved in left heart failure versus right heart failure, systolic versus diastolic, etc… influence of cardiac function concepts- preload, afterload and contractility. What are the compensatory mechanisms, and how does that influence symptoms or pathology? What are the different types of cardiomyopathies- restrictive-vs-dilated-vs-hypertrophic. Mechanisms, risk factors of MI, Hypertension, atherosclerosis, cardiac myopathies. Symptoms/laboratory tests for different pathologies Interactions between hypertension, atherosclerosis and cardiac pathologies. FOR EXAMPLE: How does atherosclerosis influence hypertension? How does hypertension influence cardiac pathologies? Compensatory Neurohormonal Response: -Increased SNS increased contractility, increased HR, arterial vasoconstriction -Short-Term Effects- increases HR and ejection -Long-Term Effects- increases energy expenditure -Increased RAAS venous vasoconstriction, increased circulating volume, increased preload -Short-Term Effects- Augments Preload -Long-Term Effects- Pulmonary Congestion, Anasarca (edema) -Vasoconstriction -Short-Term Effects- maintains BP for perfusion of vital organs -Long-Term Effects- exacerbates pump dysfunction (excessive afterload), increases cardiac energy expenditure Decreased systemic BP secretion vasopressin SE Catecholamines: -Toxic -Induce myocite apoptosis -Myocardial remodeling -Down regulation of adrenergic receptors -Facilitate arrhythmia -Potentiation of autoimmune effects LV Dysfunction Decreased CO, BP Starling Mechanism, Remodeling, Neurohormonal activation increased CO, BP increased cardiac workload etc. HEART FAILURE LV Failure= Systolic HF -Impaired contractility -Increased, preload, afterload, ventricular remodeling Symptoms -Dyspnea on exertion, fatigue = 2 most common symptoms -Also get fluid retention pulmonary congestion, peripheral edema -Paroxysmal nocturnal dyspnea, tachycardia, cough, hemoptysis Physical Signs -Basilar rales, pulmonary edema, S3 gallop, pleural effusion, cheyne-stokes resps RV Dysfunction: Causes -Left HF, diffuse pulmonary hypoxemia (COPD, CF, ARDS, pulm HTN) Manifestations -Jugular vein distention, hepatic congestion, peripheral edema Diastolic Heart Failure: -Pulmonary congestion despite normal SV and CO -Occurs singly or with Systolic HF -Cause of 40-50% of cases of LHF, more common in women -Decreased compliance & abnormal diastolic relaxation Causes -HTN, myocardial hypertrophy, MI, DM, CM, Disease of heart valves Symptoms -Dyspnea on exertion, fatigue, pulmonary edema, pleural effusions High Output Failure: -Inability of heart to adequately supply body despite adequate blood volume and normal or elevated myocardial contractility CARDIOMYOPATHY Dilated: Etiology- idiopathic, alcohol, myocarditis, IHD, VHD, postpartum, radiation, chemo, genetic, cocaine, connective tissue/neuromuscular disease, sarcoidosis, hemochromatosis, pheochromocytoma Patho- injured myocytes replaced by connective tissue, myocardial fibers lengthen and ventricles dilate, CO falls and LVP rises HF -Dilation of one or both ventricles -Primary consequence SYSTOLIC dysfunction Symptoms- dyspnea, fatigue, palpitations, emboli, chest pain, heart murmurs, normal/low sbp, tachycardia, JVD, cool/pale skin Hypertrophic: Etiology- genetic disease of cardiac sarcomere – Autosomal dominant Patho- hallmark HYPERCONTRACTILITY, CO normal, EF supranormal -DIASTOLIC DYSFUNCTION Symptoms- VT, FV, Angina, syncope, palpitations, LV failure, MI Restrictive: Etiology- familial, amyloidosis, hemochromatosis, sarcoidosis, radiation Patho- DIASTOLIC dysfunction, rigid ventricle walls impedes ventricular filling, impaired contractility Symptoms- exercise intolerance, weakness, dyspnea, edema, dysrhythmias, heart failure Pediatric CV ~5 Questions: Understand normal patterns of blood flow before birth o Start to see 4 chambers at 4 weeks. o Foramen ovale supposed to be there before birth. o If doesn’t close after birth causes A.S.D. o 6 weeks fully developed heart. o Therefore some congential defects are formed usually before the pregnancy is recognized. o Fetal Ciruculation o Anatomically and physiology differ from postnatal circulation o Oxygenation occurs in the placenta and not in the lungs. o Fetal lungs are fluid filled and with low arterial 02 tension produces pulmonary vasoconstriction. ▪ Not involved with Oxygenation yet, mom provides via placenta. ▪ Because of the pulmonary constriction only 8% of the fetal cardiac output is received by the pulmonary circulation. o Fetal SVR is low ▪ Nearly half of the descending aortic blood flow enters the placenta which provides low resistance to flow. ▪ Low SVR: aka easy to pump ▪ 02 sat only 40-60% ▪ But has high C.O. HR 140-150 avg. 400-500 ml/kg o O2Pulmonary VeinliverIVCforamen ovaleLARVPDAAorta o Normal Circulatory Changes After Birth o With the first few breaths the lungs are filled with air and becomes a more efficient oxygenator. ▪ With this increase in O2 and decrease in CO2 the pulmonary vasculature resistance starts to drop. ▪ As PVR stars to decrease RA and RV pressure decreases. o SVR increases due to elimination of the placenta thus increasing LA and LV pressures. ▪ *This change in pressure gradient functionally closes the foramen ovale. ▪ Anatomic closure, due to fibrin deposits is completed within the first few months of life. o The change in O2 and CO2 levels causes constriction of the ductus arterious ▪ Another factor in constriction of ductus arterious is the sudden drop in PGE1 • Sometimes give prostaglandin if need to keep open longer. o The ductus is usually functionally closed by 15 to 18 hours after birth with anatomical closure within 10-21 days of life. ▪ If a defect is present the duct can stay open or be reopened with medications. o Due to the vasoconstriction of the umbilical arteries and vein blood flow through the ductus venosus is eliminated and by 7 days post-natal there is no flow through the duct. ▪ Becomes the ligamentum venosum o Pulmonary Resistance in Neonate o Marked changes occur after birth ▪ Is variable and related to neonate’s condition o Problems with increased PVR that occur are related to factors that cause constriction of the pulmonary bed. ▪ This can result in pulmonary hypertension ▪ Something occurred in utero to cause pressure to stay high o Fetal stress in utero: release meconium: ▪ Thick tar stool o Child born with meconium 2/100 live births ▪ Takes breathmeconium aspiration ▪ If see meconium in amio fluid • Becomes high risk • Aggressive suctioning o Cyanotic vs Acyanotic o Cyanotic: usually have an obstruction to pulmonary blood flow. ▪ Pressure higher on Right, causes RL shunt ▪ **Blood shunts right to left decreasing blood flow to pulmonary circulation ▪ Causes mixing of oxygenated and deoxygenated blood • Sats 85% area, will look blue. o Acyanotic: overstress pulmonary system ▪ **Usually left to right shunt. ▪ Blood moves from high pressure to low pressure ▪ Usually this causes over circulation of pulmonary blood flow. o Obstructive ▪ Stenotic area with restrictive blood flow ▪ Hypertension proximally to obstruction ▪ Hypoperfusion distally form obstruction o Selected Congential Cardiac Defects o Patent Ductus Arteriosus (PDA) ▪ Failure of ductus arteriosus to close. ▪ Blood shunts left to right • Acyanotic defect o Atrial Septal Defect (ASD) ▪ **Failure of foramen ovale to close ▪ Improper formation of septal wall ▪ LR shunt ▪ Acyanotic o Ventricular Septal Defect (VSD): most common ▪ LR shunt, Acyanotic defect ▪ Defect in ventricular septal wall ▪ Usually asymptomatic until fall in PVR • 2-4 weeks of age • Then get lots of shunting • Increased blood volume to lungs o Tetralogy of Fallot (TET) ▪ Most common cyanotic defect ▪ Four defects in one • VSD • Pulmonary stenosis • Right ventricular hypertrophy (RVH) • Overidding Aorta ▪ TET spells: crying, turn blue. • Drop to a squat • To increase SVR to help dec. shunt o Coarctation of the Aorta (Coarc) ▪ Severe narrowing of the arch of the aorta ▪ Take BP in all extremities inc in U.E. ▪ Dec in L.E. o Transposition of the Great Arteries (TGA) ▪ Aorta and pulmonary artery are switched ▪ Mixing defect. Usually can see on U.S. before birth ▪ Put on Prostaglandin to re open ovale to get some shunting. o Kawasaki Disease ▪ Also known as mucocutanesou lymph node syndrome ▪ Acute self-limiting vasculitis that may result in cardiac complications ▪ Patho occurs in stages ▪ Acute • Strawberry tongue: red flag • Increased platelet count • Dec. sed rate means child recovered. o Eisenmenger’s syndrome ▪ ASD or VSD now turns into cyanotic defect. ▪ Overcirculation causes irritation to pulmpulm vasconstricitonpulm HTN. ▪ Usually go into VTACH or V fib. ▪ Need heart/lung transplant or fix heart then transplant. ▪ Reproductive – 8 Questions Overview (general concepts) of normal male and female anatomy and physiology, including general concepts of hormonal control (but not the menstrual cycle slide in any detail.) Female General Concepts o The uterus has two major parts: corpus (body) and cervix. o Corpus: o Fundus o Isthmus o Uterus and upper vagina are innervated by autonomic nervous system. o The Uterus o Perimetrium: serous membranous o Myometrium: muscular middle layer; facilitates birthing o Endometrium: uterine lining; responsive to hormones o Cervix: barrier; pH inhospitable to bacteria o Fallopian Tubes o Conduct ovum from ovaries to the uterus o Fimbrae: create a current to promote ovum moving into the infundibulum o Ovaries o Secrete female sex hormones o Estrogen, Progesterone o From: ovarian follicle, granulosa cells, theca cells, and cells of corpus luteum o Release Ova: 200,000 – 400,000 at birth o Interestingly – uninterrupted ovulation (meaning monthly ovulation from menarche to menopause – not interrupted by pregnancy, breast feeding, contraceptives – is associated with a higher risk of ovarian cancer. o Hypothalamic Hormones o Gonadotropin Releasing Hormone (GnRH) o GnRH stimulates synthesis and secretion of the gonadotropins in the pituitary: ▪ FSH: Follicle Stimulating Hormone ▪ LH: Luteinizing Hormone o GnRH secretion differs between females and males. ▪ Males: GnRH secreted in constant frequency pulses. ▪ Females: variable frequency pulses; large surge before ovulation o GnRH necessary for reproductive function ▪ Females: follicular growth, ovulation & corpus luteum development ▪ Males: spermatogenesis o Pituitary Hormones o FSH/LH ▪ Gonads ovaries/testes primary targets of LH/FSH o LH: Stimulates theca cells of the ovaries to produce androstenedione. o FSH stimulates the granulosa cells of ovarian follicles to convert androstenedione into estradiol in granulosa cells o Ovarian Hormones o All female sex hormones are steroids o Estrogens – a generic term for three similar hormones: ▪ Estradiol –most abundant. 95% is produced by ovarian follicles and corpus luteum; 5% produced in the adrenal cortex. ▪ Estrone – Androgens are converted to estrone in ovarian and peripheral adipose tissue. ▪ Estriol – The peripheral metabolite of estrone and estradiol; formed in the placenta during pregnancy. o Role of Estrogens ▪ Proliferation of squamous epithelium in the vaginal mucosa. ▪ Production of secretions that enhance sperm survival and motility. ▪ Promotes motility and ciliary action in the fallopian tubes. ▪ Body effects: • Especially bone health. • Reduces bone resorption and increases bone formation. o Progesterone ▪ Small amounts secreted steadily by the adrenal cortex and ovaries. ▪ LH stimulates release of larger amounts from corpus luteum during the luteal phase ▪ “The hormone of pregnancy o Role of Progesterone ▪ Relaxation of myometrium ▪ Thickening of myometrium ▪ Promotes development of breast tissue o During human pregnancy, progesterone is produced in increasingly high amounts by the ovaries and placenta. At first, the source is the corpus luteum that has been "rescued" by the presence of human chorionic gonadotropin (hCG) from the conceptus. However, after the 8th week, production of progesterone shifts to the placenta. o Adrenal Hormones o Androgens released from the adrenal cortex o Precursors for estrogen and progesterone ▪ DHEA – Dehydroepiandrosterone: a steroid hormone produced in the adrenal cortex from cholesterol. It is the primary precursor of natural estrogens. o Higher levels in males o Contribute to skeletal growth during pregnancy o Development of pubic and axillary hair. Menopause o Menopause o Due to cessation of ovarian function o Gradual decrease in size of ovaries o Usually occurs between ages 4552 o Variability in frequency and flow 10 years prior o Mechanism o Atresia of oocytes o Dec. in Estrogen, Progesterone from ovaries o Inc. in FSH and LH o Estrogen still produced in ▪ adrenal cortex ▪ Adipose tissue (conversion of androstenedione) ▪ insufficient to maintain secondary sexual characteristics. o Manifestations o Decrease in density of Breast tissue o Reduction in Body hair o Decreased subcutaneous fat o Decreased Bone mass o Uterus and ovaries decrease in size o Vaginal lining becomes thin and dry o Hot flashes and night sweats –estrogen withdrawal o Hormone replacement therapy o Who should take? ▪ <45y/o ▪ Severe hot flashes ▪ Lowest effective dose for shortest period of time. Amenorrhea o Amenorrhea: absence or suppression of menstruation. o Normal/expected: ▪ prior to menarch, after menopause, during pregnancy, during lactation. o Primary Amenorrhea o failure of menarche (no onset of menses) by ▪ Age 14 without development of secondary sex characteristic. ▪ Age 16 regardless of development of secondary sex char. o Pathophysiology: think gonadal axis. All aspects of the axis must be working properly. o Compartment IV: Amenorrhea caused by disorders of the CNS: o Hypothalamus unable to synthesize GnRH. ▪ No stimulation of LH/FSH production by pituitary. ▪ Ovary does not receive signals that initiate ovarian and endometrial changes of the menstrual cycle. ▪ No ovulation. No menstruation. ▪ No ovarian hormones; secondary sex characteristics don’t develop o Compartment III: disorders of the anterior pituitary o Anatomic defects or tumors within CNS or pituitary o Interferes/interrupts secretion of FSH or LH (or GnRH) o Depending on timing some skeletal growth and secondary sex characteristics may develop o Compartment II: disorders involving the ovaries o Gonadal dysgenesis (e.g. Turner’s syndrome) Absence of gametes o Without gametes and follicles, estrogen secretion cannot occur – even in presence of high FSH and LH o Androgen insensitivity syndrome o Male genetically; female morphologically o Compartment I: anatomic defects affecting menstrual outflow o Congenital absence of vagina/uterus o Uterine hypoplasia o Usually have normal ovarian function ▪ Normal skeletal growth ▪ Normal secondary sexual characteristics ▪ No menstruation Secondary Amenorrhea o Secondary o The absence of menstruation for 3 or more cycles or 6 months in women who have previously menstruated o Normal during early adolescence, perimenopausal period, pregnancy, and lactation. o Wide range of causes: again think of HPO axis. ▪ Diseases (more to follow) ▪ Dramatic weight loss ▪ Malnutrition ▪ Excessive exercise o Patho o Normal ovarian hormone secretion: ▪ Pregnancy ▪ Uterine dysfunction (hysterectomy; adhesions) o Increased ovarian hormone secretion r/t ▪ Feminizing tumors; masculinizing tumors; polycystic ovary syndrome o Decreased Ovarian Hormone Secretion o With high gonadotropin levels: o Menopause o Acquired ovarian failure ▪ Autoimmune disease ▪ Chemotherapy ▪ Resistance to gonadotropins ▪ Environmental Toxins o Low gonadotropin levels ▪ Hyperprolactinemia (overproduction by hypothal.) ▪ Tumor or trauma to hypothal or pituitary ▪ Disorders extrinsic to HP tract: • Starvation, stress/psychogenic disorder; endocrine disease) Polycystic ovary syndrome (PCOS) o Diagnosed by presence of at least 2 of the following conditions o Oligo or an ovulation o Elevated androgen levels o Polycystic ovaries o Clinical signs of hyperandrogenism and polycystic ovaries o (!!presence of polyscystic ovaries is neither NECESSARY nor SUFFICIENT to diagnose PCOS!!) o Manifestatsions o Obesity (38% of women with PCOS) o Dysmennorhea/Amenorhhea/Oligomenorrhea o Infertility o Hormonal abnormalities o Late Sequelae ▪ Dyslipidemia ▪ Diabetes Mellitus ▪ Cardiovascular disease & hypertension ▪ Endometrial Carcinoma o Treatment o Insulin sensitizers (to prevent diabetes and heart disease and restore fertility) o Progesterone to oppose estrogen’s effects on endometrium and to initiate monthly menstruation) o Oral contraceptives to suppress androgen production and hirsutism. o 40% of women with PCOS can become pregnant with medical management. Pelvic relaxation disorders o Endopelvic fascia and perineal muscles stretch and lose tone/strength o Unable to maintain organs in proper position. o Precipitating factors: o Anything that increases intraabdominal pressure o Estrogen helps maintain elasticity of tissue. o Uterine prolapse: Descent of cervix or entire uterus into the vaginal canal. o Goal is to prevent with muscular exercise (Kegel exercises) o Estrogen can be useful in postmenopause o Surgery as a last resort. o Cystocele: Descent of the bladder into the vaginal canal. o Causes feelings of pressure, difficulty in completely emptying the bladder; o Can increase risk for bladder infections. o Treated with Kegel exercises to strengthen the pelvic floor muscles or use of a vaginal pessary. o Rectocele o Usually caused by trauma to the fascia during childbirth o Chronic constipation contributes to development. o Rectocele also causes constipation, feelings of rectal fullness, and difficult defecation. Pelvic Inflammatory Disease o Inflammation of the uterus, fallopian tubes, and/or ovaries cause by infection. Can progress to the entire peritoneal cavity. o Consequences associated with scarring. Ectopic pregnancy, pelvic pain, pain on intercourse, pelvic adhesions, abscesses o Etiology: mediated by failure of normal defense mechanisms. o Chlamydia and Gonorrhea; but infections usually mixed. o Infection may change columnar epithelium facilitating invasion by other micro organisms o Inflammation: Scar tissue formation with adhesions to nearby tissues and organs. o Can lead to necrosis and abscess formation. o Manifestations o Asymptomatic o Abd. Pain, Fever o Symptoms after menstruation or intercourse o Septic shock 89% fatality o Bowel obstruction o Infertility Endometriosis: Presence of functioning endometrial tissue outside the uterus. This tissue also responds to hormonal fluctuations in the menstrual cycle o Etiology o Retrograde flow –common in MOST women. o Decreased immune response to endometrial cells outside uterus. May be related to depressed cytotoxic Tcell response. Allows implantation. o Genetic predisposition o Bleeding Inflammation o Pain, fibrosis, scarring adhesions o Manifestations: ▪ Dysmenorrhea ▪ Abnormal bleeding ▪ Pain with intercourse ▪ Constipation ▪ Infertility HPV: o 2 general types of HPV : o Lowrisk types associated with genital warts and mild Pap test abnormalities o Highrisk types associated with mild to severe Pap test abnormalities and cervical cancer o *Most genital HPV infections are transient, asymptomatic, and have no clinical consequences. o Persistent infection o Risks for women ▪ Smoking in a cofactor o But, most women with persistent HPV infection do not develop cervical cancer precursors or cervical cancer Cervical Cancer o Classifications o ASC–US—atypical squamous cells of undetermined significance. Sometimes the changes are related to HPV infection. ASC–US changes are usually mild abnormalities. In the absence of HPV infection, this is considered “Normal”. o 1012 years between preinvasion lesions and cancer. o Staging o Stage 0 Carcinoma in situ; CIN 3. The abnormal cells have not invaded deeper tissues. This stage is not cancer. Precancerous. Endometrial Cancer: o Risk factors: o Both estrogen (when unopposed by progesterone) and insulin exert proliferative effects on the endometrium. o Manifestations o Only sign may be postmenopausal bleeding!!! Any postmenopausal woman with vaginal bleeding should have an endometrial biopsy! Ovarian Cancer o Epithelial – 8590% of all ovarian cancers“Ovarian carcinomas” o NEW EVIDENCE THAT THESE TUMORS MAY ORIGINATE IN THE FALLOPIAN TUBES o Symptoms o Urinary frequency, urgency o GI upset (indigestion; constant feeling of fullness) o Pelvic &/or abdominal pain or discomfort o Pelvic &/or abdominal bloating or swelling Prostate Cancer o Death rate has decreased 4%/year since 1994! o Mortality is 2x higher in A.A.! o Screening Controversies: PSA o ***Not currently recommended as general screening. [Show More]
Last updated: 1 year ago
Preview 1 out of 40 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2021
Number of pages
40
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2021
Downloads
0
Views
57



.png)