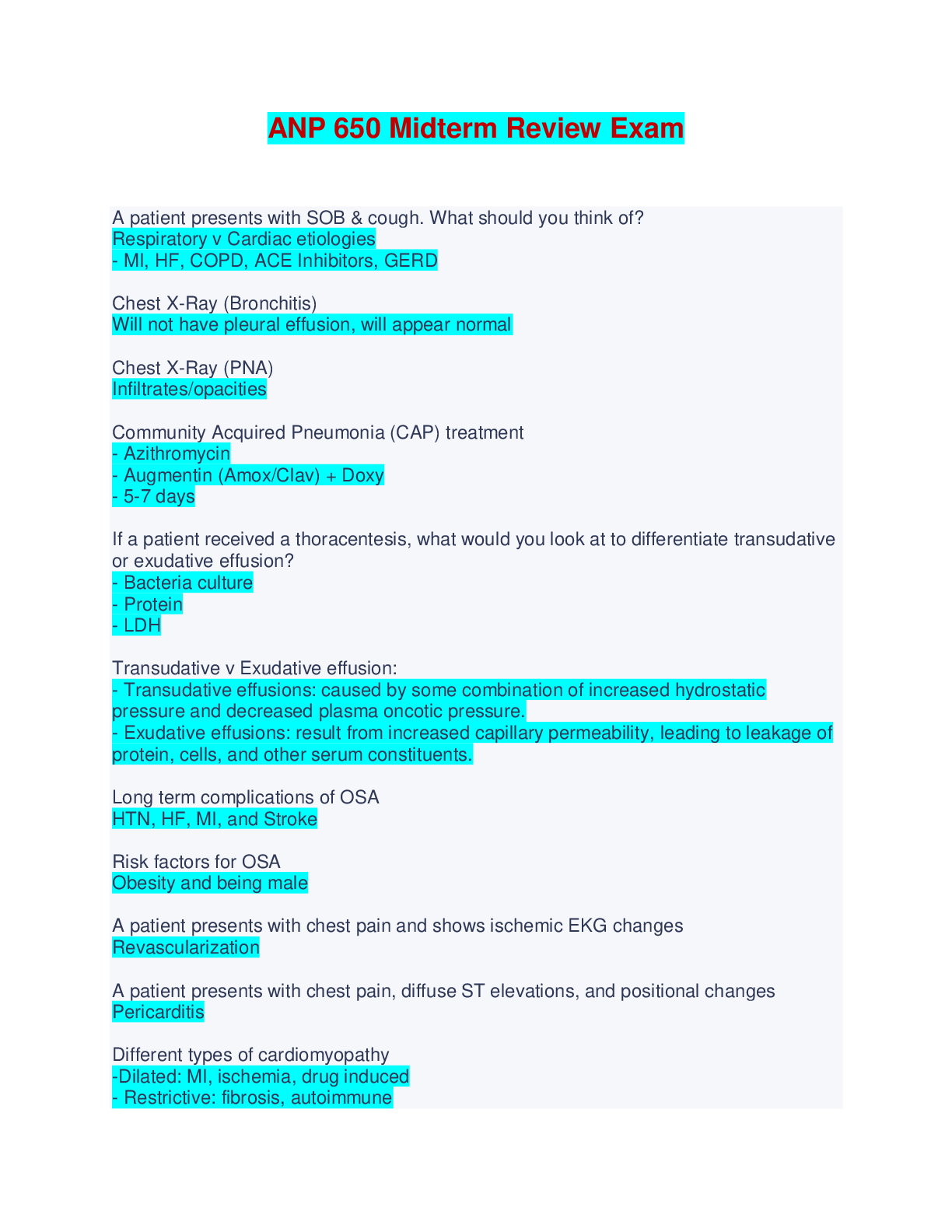
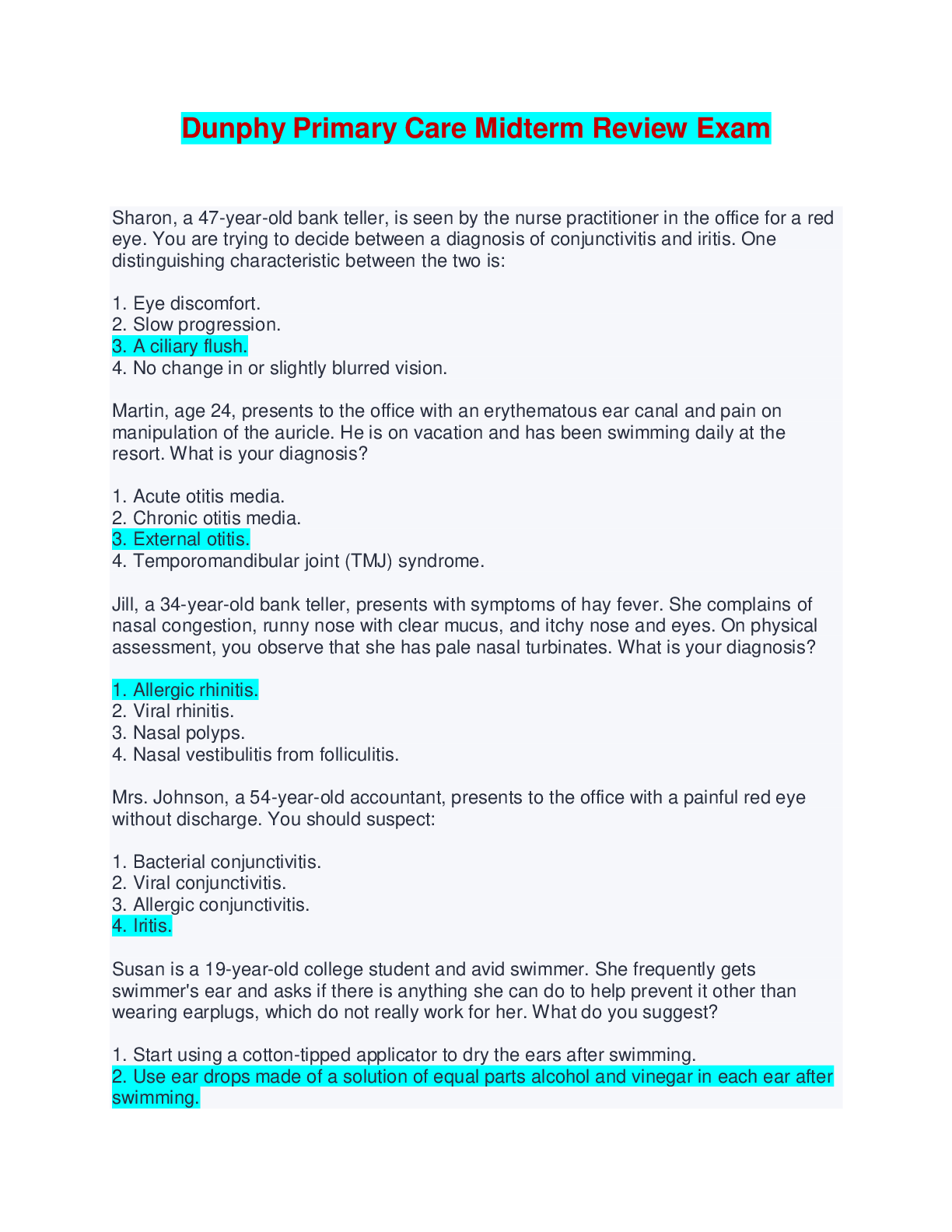
NURS 4602 Midterm review exam latest – University of Texas
Document Content and Description Below
NURS 4602 Midterm review exam latest – University of Texas 40 ACUTE INFECTIOUS DISORDERS • PHARYNGITIS o Inflammation of the throat mucosa (pharynx) is referred to as pharyngitis o Group... A streptococci account for 15% to 30% of cases, with the remainder being caused by other viruses or bacteria o Suppurative complications of group A streptococcal infection include peritonsillar or retropharyngeal abscess. ♣ Peritonsillar abscess may be noted by asymmetric swelling of the tonsils, shifting of the uvula to one side, and palatal edema. ♣ Retropharyngeal abscess may progress to the point of airway obstruction, hence requiring careful evaluation and appropriate treatment. o Additional complications include acute rheumatic fever (see Chapter 41) and acute glomerulonephritis o Viral pharyngitis is usually self-limited and does not require therapy beyond symptomatic relief. o Group A streptococcal pharyngitis requires antibiotic therapy. If either the rapid diagnostic test or throat culture (described below) is positive for group A streptococci, penicillin is generally prescribed. ♣ Appropriate alternative antibiotics include amoxicillin and, for those allergic to penicillin, macrolides, and cephalosporins. o The history may include a fever, sore throat and difficulty swallowing, headache, and abdominal pain. o Inspect the pharynx and tonsils, which may demonstrate varying degrees of inflammation. Exudate may be present but is not diagnostic of bacterial infection. Note the presence of petechiae on the palate. Inspect the tongue for a strawberry appearance. Palpate for enlargement and tenderness of the anterior cervical nodes. Inspect the skin for a fine, red, sandpaper-like rash (called scarlatiniform), particularly on the trunk or abdomen, a common finding with streptococcus A infection. o The rapid strep test is a sensitive and reliable measure, rarely resulting in false-positive readings o Comfort ♣ Saline gargles (made with 8 oz of warm water and a half teaspoon of table salt) are soothing for children old enough to cooperate. ♣ Analgesics such as acetaminophen and ibuprofen may ease fever and pain. Sucking on throat lozenges or hard candy may also ease pain. ♣ Cool mist humidity helps to keep the mucosa moist in the event of mouth breathing. ♣ Encourage the child to ingest popsicles, cool liquids, and ice chips to maintain hydration. o After 24 hours of antibiotic therapy, instruct the parents to discard the child’s toothbrush to avoid reinfection. Children may return to day care or school after they have been receiving antibiotics for 24 hours; they are considered noncontagious at that point. • Tonsillitis o Inflammation of the tonsils often occurs with pharyngitis and, thus, may also be viral or bacterial in nature. ♣ Viral infections require only symptomatic treatment. Treatment for bacterial tonsillitis is the same as for bacterial pharyngitis. o Occasionally surgical intervention is warranted. Tonsillectomy (surgical removal of the palatine tonsils) may be indicated for the child with recurrent streptococcal tonsillitis or massive tonsillar hypertrophy or for other reasons. o When hypertrophied adenoids obstruct breathing, then adenoidectomy (surgical removal of the adenoids) may be indicated. o When tonsils touch at the midline (“kissing tonsils” or 4+ in size), the airway may become obstructed. o Rapid test or culture may be positive for streptococcus A o Tonsillitis that is medically treated requires the same nursing management as pharyngitis. o Care post-tonsillectomy ♣ place the child in a side-lying or prone position to facilitate safe drainage of secretions. Once alert, the child may prefer to sit up or have the head of the bed elevated. ♣ Suctioning, if necessary, should be done carefully to avoid trauma to the surgical site ♣ Hemorrhage is unusual postoperatively but may occur any time from the immediate postoperative period to as late as 10 days after surgery • Mucus tinged with blood may be expected, but fresh blood in the secretions indicates bleeding. • Early bleeding may be identified by continuous swallowing of small amounts of blood while awake or sleeping. • Other signs of hemorrhage include tachycardia, pallor, restlessness, frequent throat clearing, and emesis of bright red blood. ♣ To avoid trauma to the surgical site, discourage the child from coughing, clearing the throat, blowing the nose, and using straws. ♣ Citrus juice and brown or red fluids should be avoided: the acid in citrus juice may irritate the throat, and red or brown fluids may be confused with blood if vomiting occurs. ♣ For the first 24 hours after surgery, the throat is very sore. Adequate pain relief is essential to establish adequate oral fluid intake. An ice collar may be prescribed, as well as analgesics with or without narcotics. • Epiglottitis o Epiglottitis (inflammation and swelling of the epiglottis) is most often caused by Haemophilus influenzae type b. o Extensive use of the Hib vaccine since the 1980s has resulted in a significant decrease in the incidence of epiglottitis o Though now rare, epiglottitis most often occurs in children between the ages of 2 and 7 years and can be life-threatening o The child may refuse to lie down and may assume the characteristic position: sitting forward with the neck extended. Drooling may be present. o Cough is usually absent. A lateral neck x-ray may be performed to determine whether epiglottitis is present. o Do not place the child in a supine position, as airway occlusion may occur. o Provide 100% oxygen in the least invasive manner that is acceptable to the child. If the child with epiglottitis experiences complete airway occlusion, an emergency tracheostomy may be necessary. o Epiglottitis is characterized by dysphagia, drooling, anxiety, irritability, and significant respiratory distress. Prepare for the event of sudden airway occlusion. • Bronchiolitis o Bronchiolitis is an acute inflammatory process of the bronchioles and small bronchi. Nearly always caused by a viral pathogen, RSV accounts for the majority of cases of bronchiolitis o The peak incidence of bronchiolitis is in the winter and spring, coinciding with RSV season. o Virtually all children will contract RSV infection within the first few years of life. RSV bronchiolitis occurs most often in infants and toddlers, with a peak incidence around 6 months of age o The severity of disease is related inversely to the age of the child. The frequency and severity of RSV infection decrease with age. o Repeated RSV infections occur throughout life but are usually localized to the upper respiratory tract after toddlerhood. o RSV infection causes necrosis of the respiratory epithelium of the small airways, peribronchiolar mononuclear infiltration, and plugging of the lumens with mucus and exudate o The small airways become variably obstructed; this allows adequate inspiratory volume but prevents full expiration. This leads to hyperinflation and atelectasis. Hypoventilation occurs secondary to markedly increased work of breathing. o Management ♣ Management of RSV focuses on supportive treatment. ♣ Supplemental oxygen, nasal and/or nasopharyngeal suctioning, oral or intravenous hydration, and inhaled bronchodilator therapy (racemic epinephrine or albuterol/levalbuterol) are used. ♣ The infant with tachypnea, significant retractions, poor oral intake, or lethargy can deteriorate quickly, to the point of requiring ventilatory support, and thus warrants hospital admission. o Exam ♣ Inspection and Observation. Observe the child’s general appearance and color (centrally and peripherally). The infant with RSV bronchiolitis might appear air-hungry, exhibiting various degrees of cyanosis and respiratory distress, including tachypnea, retractions, accessory muscle use, grunting, and periods of apnea. Cough and audible wheeze might be heard. The infant might appear listless and uninterested in feeding, surroundings, or parents. ♣ Earlier in the illness, wheezes might be heard scattered throughout the lung fields. In more serious cases, the chest might sound quiet and without wheeze. o Common laboratory and diagnostic studies ordered for the assessment of RSV bronchiolitis include: ♣ Pulse oximetry: oxygen saturation might be decreased significantly ♣ Chest x-ray: might reveal hyperinflation and patchy areas of atelectasis or infiltration ♣ Blood gases: might show carbon dioxide retention and hypoxemia ♣ Nasal-pharyngeal washings: positive identification of RSV can be made via enzyme-linked immunosorbent assay (ELISA) or immunofluorescent antibody (IFA) testing o Children with less severe disease might require only antipyretics, adequate hydration, and close observation. They can often be successfully managed at home o Airway ♣ These children often require frequent assessment and suctioning to maintain a patent airway. ♣ Use a Yankauer or tonsil-tip suction catheter to suction the mouth or pharynx of older infants or children, rinsing the catheter after each suctioning. ♣ Nasal bulb suctioning may be sufficient to clear the airway in some infants, while others will require nasopharyngeal suctioning with a suction catheter o Since RSV is easily spread through contact with droplets, isolate inpatients according to hospital policy to decrease the risk of nosocomial spread to other children o Tell parents to call the physician or nurse practitioner if the child’s breathing becomes rapid or more difficult or if the child cannot eat secondary to tachypnea. o Palivizumab (Synagis) is a monoclonal antibody that can prevent severe RSV disease in those who are most susceptible ♣ It is given as an intramuscular injection once a month throughout the RSV season. ♣ Qualifying factors for the antibody include: • Prematurity • Chronic lung disease (bronchopulmonary dysplasia) requiring medication or oxygen • Certain congenital heart diseases • Certain neuromuscular disorders • Bronchitis o Bronchitis is an inflammation of the trachea and major bronchi. It is often associated with a URI. Bronchitis is usually viral in nature o Recovery usually occurs within 5 to 10 days. Therapeutic management involves mainly supportive care. Expectorant administration and adequate hydration are important. If bacterial infection is the cause, antibiotics are indicated. o The illness might begin with a mild URI. Fever develops, followed by a dry, hacking cough that might become productive in older children. The cough might wake the child at night. Auscultation of the lungs might reveal coarse rales. Respirations remain unlabored. The chest x-ray might show diffuse alveolar hyperinflation and perihilar markings. o Teach parents that expectorants will help loosen secretions and antipyretics will help reduce the fever, making the child more comfortable. Encourage adequate hydration. Antibiotics are prescribed only in cases believed to be bacterial in nature. Discourage the use of cough suppressants: it is important for accumulated sputum to be raised. • Tuberculosis o Tuberculosis (TB) is a highly contagious disease caused by inhalation of droplets of Mycobacterium tuberculosis or Mycobacterium bovis. Children usually contract the disease from an immediate household member. o After exposure to an infected individual, the incubation period is 2 to 10 weeks. The inhaled tubercle bacilli multiply in the alveoli and alveolar ducts, forming an inflammatory exudate. The bacilli are spread by the bloodstream and lymphatic system to various parts of the body. o Though pulmonary tuberculosis is the most common, children may also have infection in other parts of the body, such as the gastrointestinal tract or central nervous system. o In the case of drug-sensitive tuberculosis, the American Academy of Pediatrics recommends a 6-month course of oral therapy. ♣ The first 2 months consist of isoniazid, rifampin, and pyrazinamide given daily. This is followed by twice-weekly isoniazid and rifampin; administration must be observed directly (usually by a public health nurse). ♣ In the case of multidrug-resistant tuberculosis, ethambutol or streptomycin is given via intramuscular injection o children considered to be at high risk for contracting tuberculosis should be screened using the Mantoux test. Children considered to be at high risk are those who: ♣ Are infected with HIV ♣ Are incarcerated or institutionalized ♣ Have a positive recent history of latent tuberculosis infection ♣ Are immigrants from or have a history of travel to endemic countries ♣ Are exposed at home to HIV-infected or homeless persons, illicit drug users, persons recently incarcerated, migrant farm workers, or nursing home residents o Children can be asymptomatic or exhibit a broad range of symptoms. Symptoms may include fever, malaise, weight loss, anorexia, pain and tightness in the chest, and rarely hemoptysis. ♣ Cough may or may not be present and usually progresses slowly over several weeks to months ♣ Dullness to percussion might be present, as well as diminished breath sounds and crackles. o Diagnosis is confirmed with a positive Mantoux test, positive gastric washings for acid-fast bacillus, interferon-gamma release assay (IGRA), and/or a chest x-ray consistent with tuberculosis. o Hospitalization of children with tuberculosis is necessary only for the most serious cases -- Supportive care includes ensuring adequate nutrition and adequate rest, providing comfort measures such as fever reduction, preventing exposure to other infectious diseases, and preventing reinfection. o latent infection - These children should be treated with isoniazid for 9 months to prevent progression to active disease. o Thus, hospitalized children with tuberculosis must be isolated according to hospital policy to prevent nosocomial spread of tuberculosis infection o Administration of bacille Calmette–Guérin (BCG) vaccine can provide incomplete protection against tuberculosis, and it is not widely used in the United States ACUTE NONINFECTIOUS DISORDERS • Asthma o Asthma is a chronic inflammatory airway disorder characterized by airway hyperresponsiveness, airway edema, and mucus production o The incidence and severity of asthma are increasing; this might be attributed to increased urbanization, increased air pollution, and more accurate diagnosis. o o A significant long-term complication, chronic airway remodeling, may result from recurrent asthma exacerbation and inflammation. Children with asthma are more susceptible to serious bacterial and viral respiratory infections (John & Brady, 2013a). Acute complications also include status asthmaticus and respiratory failure. o Autonomic neural control of airway tone is affected, airway mucus secretion is increased, mucociliary function changes, and airway smooth muscle responsiveness increases. As a result, acute bronchoconstriction, airway edema, and mucus plugging occur o . Following the acute response to a trigger, continued allergen response results in a chronic phase. During this phase, the epithelial cells are denuded and the influx of inflammatory cells into the airway continues. This results in structural changes of the airway that are irreversible, and further loss of pulmonary function might occur. – airway remodling o Management ♣ Current goals of medical therapy are avoidance of asthma triggers and reduction or control of inflammatory episodes ♣ Short-acting bronchodilators may be used in the acute treatment of bronchoconstriction and long-acting forms may be used to prevent bronchospasm. ♣ Most children may avoid exercise-induced bronchospasm by using a longer warm-up period prior to vigorous exercise and, if necessary, inhaling a short-acting bronchodilator just prior to exercise. Long-term prevention usually involves inhaled steroids. ♣ Leukotriene modifiers may be used as an alternative but are not preferred for mild persistent asthma o Common signs and symptoms reported during the health history might include: ♣ Cough, particularly at night: hacking cough that is initially nonproductive, becoming productive of frothy sputum ♣ Difficulty breathing: shortness of breath, chest tightness or pain, dyspnea with exercise ♣ Wheezing o o Some children present with mild retractions, while others demonstrate significant accessory muscle use and eventually head bobbing if not treated effectively. The child may appear anxious and fearful or may be lethargic and irritable. An audible wheeze might be present. o Wheezing is the hallmark of airway obstruction and might vary throughout the lung fields. A quiet chest in an asthmatic child can be an ominous sign With severe airway obstruction, air movement can be so poor that wheezes might not be heard upon auscultation. Percussion may yield hyperresonance. o Laboratory and diagnostic studies commonly ordered for the assessment of asthma include: ♣ Pulse oximetry: oxygen saturation may be decreased significantly or normal during a mild exacerbation ♣ Chest x-ray: usually reveals hyperinflation ♣ Blood gases: might show carbon dioxide retention and hypoxemia ♣ Pulmonary function tests (PFTs): can be very useful in determining the degree of disease but are not useful during an acute attack. Children as young as 5 or 6 years might be able to comply with spirometry. ♣ Peak expiratory flow rate (PEFR): is decreased during an exacerbation ♣ Allergy testing: skin test or RAST can determine allergic triggers for the asthmatic child o Stress the concept of maintenance medications for the prevention of future serious disease in addition to controlling or preventing current symptoms. o In children who have more severe asthma, the NAEPP (2007) recommends the use of the PEFR to determine daily control. ♣ The child’s “personal best” is determined collaboratively with the physician or nurse practitioner during a symptom-free period. o The fatigue and fear associated with chronic asthma may reduce the child’s confidence and sense of control over his or her body and life. o To live in fear of an exacerbation or to be unable to participate in activities affects the child’s self-esteem • Cystic Fibrosis o Cystic fibrosis is an autosomal recessive disorder that affects 30,000 children and adults in the United States (Cystic Fibrosis Foundation [CFF], n. d.). o DNA testing can be used prenatally and in newborns to identify the presence of the mutation o Complications include hemoptysis, pneumothorax, bacterial colonization, cor pulmonale, volvulus, intussusception, intestinal obstruction, rectal prolapse, gastroesophageal reflux disease, diabetes, portal hypertension, liver failure, gallstones, and decreased fertility. o The epithelial cells fail to conduct chloride, and water transport abnormalities occur. This results in thickened, tenacious secretions in the sweat glands, gastrointestinal tract, pancreas, respiratory tract, and other exocrine tissues. ♣ The pancreas, intrahepatic bile ducts, intestinal glands, gallbladder, and submaxillary glands become obstructed by viscous mucus and eosinophilic material. ♣ Pancreatic enzyme activity is lost and malabsorption of fats, proteins, and carbohydrates occurs, resulting in poor growth and large, malodorous stools. ♣ Abnormally thick mucus plugs the small airways, and then bronchiolitis and further plugging of the airways occur. ♣ Boys have tenacious seminal fluid and experience blocking of the vas deferens, often making them infertile (Hazle, 2010). In girls, thick cervical secretions might limit penetration of sperm o Management ♣ Therapeutic management of cystic fibrosis is aimed toward minimizing pulmonary complications, maximizing lung function, preventing infection, and facilitating growth. ♣ All children with cystic fibrosis who have pulmonary involvement require chest physiotherapy with postural drainage several times daily to mobilize secretions from the lungs. ♣ Recombinant human DNase (Pulmozyme) is given daily using a nebulizer to decrease sputum viscosity and help clear secretions ♣ Inhaled bronchodilators and anti-inflammatory agents are prescribed for some children. Aerosolized antibiotics are often prescribed and may be given at home as well as in the hospital ♣ Pancreatic enzymes and supplemental fat-soluble vitamins are prescribed to promote adequate digestion and absorption of nutrients and optimize nutritional status. ♣ Some children require total parenteral nutrition to maintain or gain weight. o Common signs and symptoms reported during the health history in the undiagnosed child might include: ♣ A salty taste to the child’s skin (resulting from excess chloride loss via perspiration) ♣ Meconium ileus or late, difficult passage of meconium stool in the newborn period ♣ Abdominal pain or difficulty passing stool (infants or toddlers might present with intestinal obstruction or intussusception at the time of diagnosis) ♣ Bulky, greasy stools ♣ Poor weight gain and growth despite good appetite ♣ Chronic or recurrent cough and/or upper or lower respiratory infections o assessment ♣ The child with cystic fibrosis often has a barrel chest. The child might have a protuberant abdomen and thin extremities, with decreased amounts of subcutaneous fat. Observe for the presence of edema (sign of cardiac or liver failure). Note distended neck veins or the presence of a heave (signs of cor pulmonale) ♣ Fine or coarse crackles and scattered or localized wheezing might be present. With progressive obstructive pulmonary involvement, breath sounds might be diminished. Tachycardia might be present. Note the presence of a gallop (might occur with cor pulmonale). ♣ Percussion over the lung fields usually yields hyperresonance due to air trapping. Diaphragmatic excursion might be decreased. Percussion of the abdomen might reveal dullness over an enlarged liver or mass related to intestinal obstruction. ♣ Palpation might yield a finding of asymmetric chest excursion if atelectasis is present o Common laboratory and diagnostic studies ordered for the diagnosis and assessment of cystic fibrosis include: ♣ Sweat chloride test: considered suspicious if the level of chloride in collected sweat is above 50 mEq/L and diagnostic if the level is above 60 mEq/L ♣ Pulse oximetry: oxygen saturation might be decreased, particularly during a pulmonary exacerbation ♣ Chest x-ray: may reveal hyperinflation, bronchial wall thickening, atelectasis, or infiltration ♣ Pulmonary function tests: might reveal a decrease in forced vital capacity and forced expiratory volume, with increases in residual volume o Chest physiotherapy is often used as an adjunct therapy in respiratory illnesses, but for children with cystic fibrosis it is a critical intervention. Chest physiotherapy involves percussion, vibration, and postural drainage, and either it or another bronchial hygiene therapy must be performed several times a day to assist with mobilization of secretions. o For older children and adolescents, the flutter-valve device, positive expiratory pressure therapy, or a high-frequency chest compression vest may also be used. ♣ The flutter valve device provides high-frequency oscillation to the airway as the child exhales into a mouthpiece that contains a steel ball. ♣ Positive expiratory pressure therapy involves exhaling through a flow resistor, which creates positive expiratory pressure. The cycles of exhalation are repeated until coughing yields expectoration of secretions ♣ The vest airway clearance system provides high-frequency chest wall oscillation to increase airflow velocity to create repetitive cough-like shear forces and to decrease the viscosity of secretions ♣ Encourage physical exercise, as it helps to promote mucus secretion as well as provides cardiopulmonary conditioning. ♣ Ensure that Pulmozyme is administered, as well as inhaled bronchodilators and anti-inflammatory agents if prescribed. o Pancreatic enzyme supplements (pancrelipase) must be administered with all meals and snacks to promote adequate digestion and absorption of nutrients. ♣ The number of capsules required depends on the extent of pancreatic insufficiency and the amount of food being ingested. ♣ The dosage can be adjusted until an adequate growth pattern is established and the number of stools is consistent at one or two per day. ♣ Children will need additional enzyme capsules when high-fat foods are being eaten. ♣ In the infant or young child, the enzyme capsule can be opened and sprinkled on cereal or applesauce. o In infants, breastfeeding should be continued with enzyme administration. Some infants will require fortification of breast milk or supplementation with high-calorie formulas. ♣ Supplementation with vitamins A, D, E, and K is necessary. o Providing daily intense care can be tiring, and noncompliance on the part of the family or child might occur as a result of this fatigue. Overvigilance may also occur as parents attempt to control the difficult situation and protect the child. 33 Infants and Toddlers • For many children, entering the hospital is like entering a foreign world. The result is anxiety and fear. Anxiety often stems from the rapid onset of the illness or injury, particularly when the child has limited experiences with disease or injury. • Normal fears of childhood include the fear of separation from their parents and family or guardians, loss of control, and bodily injury, mutilation, or harm. • Children’s fears are similar to adult fears of the unknown, including fear of unfamiliar environments and losing control. • Timing of separation anxiety varies among children. It typically begins once a child has developed object permanence (an understanding that things exist even when they are out of sight) which is usually around 4 to 9 months • James Robertson and John Bowlby described three stages that the infant and child goes through during separation anxiety—protest, despair, and detachment o he first phase, protest, occurs when the child is separated from the parents or primary caretaker. ♣ This phase may last from a few hours to several days. ♣ The child reacts aggressively to this separation and exhibits great distress by crying, expressing agitation, and rejecting others who attempt to offer comfort. ♣ The child may also display anger and inconsolable grief. o If the parents do not return within a short time, the child exhibits the second phase, despair. The child displays hopelessness by withdrawing from others, becoming quiet without crying, and exhibiting apathy, depression, lack of interest in play and food, and overall feelings of sadness. o Detachment (also known as denial) is the third and final phase of separation anxiety. During this phase the child forms coping mechanisms to protect against further emotional pain. This occurs more often in long-term separations. ♣ During this stage, the child shows interest in the environment, starts to play again, and forms superficial relationships with the nurses and other children. If the parents return, the child ignores them. ♣ A child in this phase of separation anxiety exhibits resignation, not contentment. It is more difficult to reverse this stage, and developmental delays may occur. • Hospitalization also affects the child’s control over decisions related to his or her own body. Many of the procedures and treatments that occur in the hospital are invasive or are at least disturbing to children, and much of the time they do not have the option to refuse to undergo them. • Infants o They gain a sense of trust in the world through rhythmic and reciprocal patterns of contact and feeding, resulting in bonding to the primary caregiver. o during illness and hospitalization, these critical patterns of feeding, contact, comfort, sleeping, elimination, and stimulation are disrupted, resulting in fear, separation anxiety, and loss of control. o By 5 to 6 months of age, infants have developed an awareness of self as separate from mother. o The constraints of hospitalization result in loss of control over the environment, leading to additional anxiety in the infant. o Assess the development or lack of development that is occurring in the infant, and assess the baby’s attachment to the parents or primary caregivers. o The infant’s facial expression is the most consistent indicator of pain or bodily injury. To decrease fear and minimize separation anxiety, avoid separation from the primary caregiver if possible; this will also promote healthy attachment. o Maintaining the infant’s home routine related to sleep and feeding helps decrease feelings of loss of control. Weigh the infant daily, at the same time, on the same scale. o Be alert to signs of discomfort other than crying, such as a furrowed brow or tense body posture. • Toddler o Toddlers are more aware of self and can communicate their desires. Because their autonomy is developing, toddlers need to master accomplishments to minimize the development of shame and doubt. o Toddlers also need opportunities to explore, and they need consistent routines o Toddlers are often fearful of strangers and can recall traumatic events. Simply walking toward the treatment room where a traumatic procedure previously occurred may upset the toddler. o When the toddler is separated from his or her parents or caregivers in an unfamiliar environment, separation anxiety is compounded. ♣ In response to this anxiety, toddlers may demonstrate behaviors such as pleading for the parents to stay, physically trying to go after the parents, throwing temper tantrums, and refusing to comply with usual routines. o Key nursing concerns when caring for toddlers are separation anxiety, growth and development, and autonomy. Establishing a trusting relationship with the toddler through nonthreatening play may decrease the amount of fear the toddler feels. Be alert to subtle, nonverbal indicators of grief or discontent. o Encourage the parent or primary caregiver to stay with the toddler in the hospital to decrease separation anxiety. Maintaining the home routine related to meals and sleep or a nap provides structure and may help decrease the toddler’s feelings of loss of control. If indicated, weigh the toddler daily. Closely monitor intake and output. 45 Impetigo Contagiosa • Bacterial infections of the skin include bullous and nonbullous impetigo, folliculitis, cellulitis, and staphylococcal scalded skin syndrome. • Impetigo, folliculitis, and cellulitis are usually self-limited disorders that rarely become severe. • Impetigo is a readily recognizable skin rash (Fig. 45.2). • Nonbullous impetigo generally follows some type of skin trauma or may arise as a secondary bacterial infection of another skin disorder, such as atopic dermatitis. • Bullous impetigo demonstrates a sporadic occurrence pattern and develops on intact skin, resulting from toxin production by S. aureus. • Obtain the history as noted in the nursing process overview section. Note history of skin disruption such as a cut, scrape, or insect or spider bite (nonbullous impetigo and cellulitis). • Note body piercing in the adolescent, which can lead to impetigo or cellulitis. Measure the child’s temperature. Fever may occur with bullous impetigo or cellulitis and is common with scalded skin syndrome. • Palpate for regional lymphadenopathy, which may be present with impetigo or cellulitis. • Teach the family about antibiotic administration and care of the lesions or rash. Soak impetiginous lesions with cool compresses or Burow solution to remove crusts before applying topical antibiotics. • Though impetigo is considered a contagious disorder among vulnerable populations, removal from school or day care is not necessary unless the condition is widespread or actively weeping. • • Burn impetigo is characterized by multifocal small superficial abscesses. Burn impetigo causes marked destruction of skin-grafted areas. Atopic Dermatitis • Atopic dermatitis (eczema) is one of the disorders in the atopy family (along with asthma and allergic rhinitis). • The chronic itching associated with atopic dermatitis causes a great deal of psychological distress. The child’s self-image may be affected, particularly if the rash is extensive. Difficulty sleeping may occur because of the itching. The child is irritable and has difficulty concentrating, and family life is disrupted. • Therapeutic management includes good skin hydration, application of topical corticosteroids or immune modulators, oral antihistamines for sedative effects, and antibiotics if secondary infection occurs. • Patho o Atopic dermatitis is a chronic disorder characterized by extreme itching and inflamed, reddened, and swollen skin. o It has a relapsing and remitting nature. o The skin reaction occurs in response to specific allergens, usually food (especially eggs, wheat, milk, and peanuts) or environmental triggers (e.g., molds, dust mites, and cat dander). ♣ Other factors, such as high or low ambient temperatures, perspiring, scratching, skin irritants, or stress, may contribute to flare-ups. o When the child encounters a triggering antigen, antigen-presenting cells stimulate interleukins to begin the inflammatory process. o The skin begins to feel pruritic and the child starts to scratch. o The sensation of itchiness comes first, and then the rash becomes apparent. The scratching causes the rash to appear. Sweating causes atopic dermatitis to worsen, as does excessively humid or dry environments. • Common signs and symptoms reported during the health history might include: o Wiggling or scratching o Dry skin o Scratch marks noticed by the parents o Disrupted sleep o Irritability • Assessement o Document dry, scaly, or flaky skin, as well as hypertrophy and lichenification (Fig. 45.11). If lesions are present they may be dry lesions or weepy papules or vesicles (fluid-filled lesions). o In children younger than 2 years old, the rash is most likely to occur on the face, scalp, wrists, and extensor surfaces of the arms or legs. o In older children it may occur anywhere on the skin, but is found more commonly on the flexor areas. o Note erythema or warmth, which may indicate associated secondary bacterial infection. o Auscultate the lungs for wheezing (commonly found in the associated condition of asthma). o Serum immunoglobulin E (IgE) levels may be elevated in the child with atopic dermatitis. Skin prick allergy testing may determine the food or environmental allergen to which the child is sensitive. • Maintain hydration o First and foremost, avoid hot water and any skin or hair product containing perfumes, dyes, or fragrance. Bathe the child twice daily in warm (not hot) water. o Use a mild soap to clean only the dirty areas. Recommended mild soaps or cleansing agents include: ♣ Unscented Dove or Dove for sensitive skin ♣ Tone ♣ Caress ♣ Oil of Olay ♣ Cetaphil ♣ Aquanil o Slightly pat the child dry after the bath, but do not rub the skin with the towel. Leave the child moist. Apply prescribed topical ointments or creams to the affected area. Apply fragrance-free moisturizer over the prescribed topical medication and all over the child’s body. Recommended moisturizers include: ♣ Eucerin, Moisturel, Curel (cream or lotion) ♣ Aquaphor ♣ Vaseline ♣ Crisco o Taking evening primrose oil and other essential fatty acids as an oral supplement may result in a reduction in redness and scaling o Cut the child’s fingernails short and keep them clean. Avoid tight clothing and heat. Use 100% cotton bed sheets and pajamas. o Scratching causes the rash to appear and further scratching may lead to secondary infection. Antihistamines given at bedtime may sedate the child enough to allow him or her to sleep without awakening because of itching. o A handheld clicker or counter may help to identify the scratching episode for the child, thus raising awareness. The use of diversion, imagination, and play may help to distract the child from scratching Diaper Dermatitis • Dermatitis refers to an inflammatory reaction of the skin. Diaper dermatitis refers to an inflammatory reaction of the skin in the area covered by a diaper. • Prolonged exposure to urine and feces may lead to skin breakdown (Fig. 45.10). Diaper wearing increases the skin’s pH, activating fecal enzymes that further contribute to skin maceration. • Ordinary diaper dermatitis does not usually result in a bumpy rash, but starts as a flat red rash in the convex skin creases. • It may appear red and shiny and may or may not also have papules. Untreated, it may become more widespread or severe. Some cases of diaper dermatitis are caused by overgrowth of C. albicans • Prevention is the best management of diaper dermatitis. Topical products such as ointments or creams containing vitamins A, D, and E; zinc oxide; or petrolatum are helpful to provide a barrier to the skin • Blow-dry the diaper area/rash area with the dryer set on the warm (not hot) setting for 3 to 5 minutes. • Discourage parents from using any type of baby powder to avoid the risk of aspiration; inhalation of talcum-containing powders may result in pneumonitis Fungal infection – tinea pedis • Tinea is a fungal disease of the skin occurring on any part of the body. • Examples of tinea infections occurring on various parts of the body include: o Tinea pedis: fungal infection on the feet o Tinea corporis: fungal infection on the arms or legs o Tinea versicolor: fungal infection on the trunk and extremities o Tinea capitis: fungal infection on the scalp, eyebrows, or eyelashes o Tinea cruris: fungal infection on the groin • The three organisms most often responsible for tinea are Epidermophyton, Microsporum, and Trichophyton, though Malassezia furfur causes tinea versicolor. • Therapeutic management of fungal infections involves appropriate hygiene and administration of an antifungal agent. • Note contact with damp areas such as locker rooms and swimming pools, use of nylon socks or nonbreathable shoes, or minor trauma to the feet (tinea pedis). • Maintain appropriate hygiene and administer antifungal agents as prescribed o Instruct the child with tinea pedis to keep the feet clean and dry. o Rinse feet with water or a water/vinegar mixture and dry them well, especially between the toes. o Encourage the child to wear cotton socks and shoes that allow the feet to breathe. o Going barefoot at home is allowed, but flip-flops should be worn around swimming pools and in locker rooms. Pediculosis 46 • Hemoglobin - Three types of normal hemoglobin (Hgb) are present at any given time in the blood: Hgb A, Hgb F or fetal, and Hgb A2. After 6 months of age, Hgb A is the predominant type. In the neonatal period, the largest difference is with the RBCs. Fetal hemoglobin, which has a much shorter cell life, is present in higher quantities, putting the infant at risk for anemia and leading to problems with the oxygen-carrying capacity of the blood. • Iron - In the term infant, a period of physiologic anemia occurs between the age of 2 and 6 months. This is due to the fact that the infant demonstrates rapid growth and an increase in blood volume over the first several months of life, and maternally derived iron stores are depleted by 4 to 6 months of age. Cancer • Pediatric cancers most often arise from primitive embryonal (mesodermal) and neuroectodermal tissues, resulting in leukemias, lymphomas, sarcomas, or central nervous system (CNS) tumors • This is in direct contrast to adult cancers, which mostly arise from epithelial cells, resulting in carcinomas. The most common childhood cancers, in order of frequency, are leukemia, CNS tumors, lymphoma, neuroblastoma, rhabdomyosarcoma, Wilms tumor, bone tumors, and retinoblastoma • Changes in blood cell production may result in fatigue, pallor, frequent or severe infection, or easy bruising. COMMON MEDICAL TREATMENTS • A clinical trial is a carefully designed research study that assesses the effectiveness of a treatment as well as its acute and long-term effects on the child. o A clinical trial may include existing medications or treatments in combination with new drugs or may involve a different approach to sequencing or dosing of medications and treatment • In the child with cancer, particularly advanced disease, the decision to provide treatment (“let’s do everything we can”) or to withhold treatment in the event of an extremely poor prognosis is extraordinarily challenging in an ethical sense. • Hospice or palliative care may be needed for the child with cancer. Children facing the end of life experience the same symptoms that adults do, including pain, fatigue, nausea, and dyspnea. • Children’s Hospice International (CHI) has demonstration models in several U.S. states that focus on enhancing the quality of life of children with life-threatening conditions. o Formerly, only children with a life expectancy of less than 6 months had access to hospice care, and they were required to forego curative care to enroll in hospice. o CHI’s goal is to provide a comprehensive, interdisciplinary continuum of care to the child and family from the time of diagnosis with a life-threatening condition through the time of death, if cure is not achieved • Commonly, chemotherapy and radiation therapy are used to treat childhood cancers. In some instances, hematopoietic stem cell transplantation is used. • Review chart 46.1 on PAGE 1779 • CHEMOTHERAPY o The cell cycle consists of five phases: ♣ G0 phase: the resting phase; lasts from a few hours to a few years; cells have not started to divide ♣ G1 phase: cell makes more protein in preparation for dividing; lasts 18 to 30 hours ♣ S phase: chromosomes are copied so that newly formed cells have the appropriate DNA; lasts 18 to 20 hours ♣ G2 phase: just before the cell splits into two cells; lasts 2 to 10 hours ♣ M phase: mitosis, the actual splitting of the cell into two new cells; lasts 30 minutes to 1 hour o Chemotherapy drugs work in two different ways in relation to the cell cycle. Cell cycle–specific agents exert their actions during a specific phase of the cell cycle. o Cell cycle–nonspecific drugs exert their effect on the cells regardless of which phase the cell is in. o Chemotherapy protocols often call for a combination of drugs that act on different phases of the cell cycle, thus maximizing the destruction of cancer cells o The cells most likely to be affected by chemotherapy are those in the bone marrow, the digestive tract (especially the mouth), the reproductive system, and hair follicles. o Adverse effects common to chemotherapeutic drugs include immunosuppression, infection, myelosuppression, nausea, vomiting, constipation, oral mucositis, alopecia, and pain. ♣ Long-term complications include microdontia and missing teeth as a result of damage to developing permanent teeth; hearing and vision changes; • hematopoietic, immunologic, or gonadal dysfunction; endocrine dysfunction, including altered growth and precocious or delayed puberty; various alterations of the cardiorespiratory, gastrointestinal, and genitourinary systems; and development of a second cancer as an adolescent or adult • RADIATION THERAPY o Radiation therapy uses high-energy radiation to damage or kill cancer cells o It may be used as a curative, adjuvant, or palliative treatment, either alone or in combination with chemotherapy. Radiation therapy is also used to shrink a tumor prior to surgical resection. o Adverse effects of radiation therapy include fatigue, nausea, vomiting, oral mucositis, myelosuppression, and alterations in skin integrity at the site of irradiation. ♣ Long-term complications are related to the area of the body that was irradiated and include alterations in growth; hormone dysfunction; hearing and vision alterations; learning problems; cardiac dysfunction; pulmonary fibrosis; hepatic, sexual, or renal dysfunction; osteoporosis; and development of secondary cancer • HEMATOPOEITIC STEM CELL TRANSPLANT o Hematopoietic stem cell transplantation (HSCT), also called bone marrow transplantation, is a procedure in which hematopoietic stem cells are infused intravenously into the child.\ o The use of high-dose chemotherapy and total body irradiation kills the tumor cells but also destroys the child’s bone marrow. The transplanted cells migrate to the empty spaces in the child’s bone marrow and reestablish normal hematopoiesis in the child. o Autologous HSCT is achieved through harvest and treatment of the child’s own bone marrow, followed by infusion of the treated stem cells. Risk for relapse of the original disease is highest in autologous HSCT. Allogenic HSCT refers to transplantation using stem cells from another individual that are harvested from the bone marrow, peripheral blood, or umbilical cord blood. o the lesser the degree of HLA matching in the donor, the higher the risk for graft rejection and GVHD. GVHD occurs to at least some extent in 11% to 85% of all allogenic HSCT recipients o In addition to graft rejection and GVHD, additional initial complications of HSCT are infection, electrolyte imbalance, bleeding, and organ, skin, and mucous membrane toxicities. ♣ Long-term complications include impaired growth and fertility related to endocrine dysfunction, developmental delay, cataracts, pulmonary and cardiac disease, avascular necrosis of the bone, and development of secondary cancers. ANEMIA • Anemia is a condition in which levels of RBCs and Hgb are lower than normal. • he loss of production can be related to lack of dietary intake of the nutrients needed to produce the cells, alterations in the cell structure, or malfunctioning tissues (e.g., bone marrow). • Anemia related to nutritional deficiency includes iron deficiency, folic acid deficiency, and pernicious anemia. • Anemia caused by the alteration or destruction of the RBCs is termed hemolytic anemia. There are several types of hemolytic anemia, such as sickle cell disease and thalassemia Iron-Deficiency Anemia • Iron-deficiency anemia occurs when the body does not have enough iron to produce Hgb. In the United States, iron-deficiency anemia has a peak prevalence in children between the ages of 6 and 24 months, and again at the age of puberty • The heme portion of Hgb consists of iron surrounded by protoporphyrin. When not enough iron is available to the bone marrow, Hgb production is reduced. Adequate dietary intake of iron is required for the body to make enough Hgb. • As Hgb levels decrease, the oxygen-carrying capacity of the blood is decreased, resulting in weakness and fatigue. In addition to delayed growth, iron-deficiency anemia has been associated with cognitive delays and behavioral changes. • Management o Iron supplements are usually provided in the form of ferrous sulfate or ferrous fumarate and are available over the counter. The recommended dose is 3 mg of elemental iron once or twice daily o In more severe cases, blood transfusions may be indicated. Transfusion of PRBCs is reserved for the most severe cases • Elicit a description of the current illness and chief complaint. Common signs and symptoms reported during the health history may include irritability, headache, dizziness, weakness, shortness of breath, pallor, and fatigue. o Other symptoms may be subtle and difficult for the clinician to identify; these include difficulty feeding, pica, muscle weakness, or unsteady gait. • Assessement o Observe the child for fatigue and lethargy. Inspect the skin, conjunctivae, oral mucosa, palms, and soles for pallor. Note spooning of the nails (concave shape) (Fig. 46.6). Obtain a pulse oximeter reading. Evaluate the heart rate for tachycardia. Auscultate the heart for a flow murmur. Palpate the abdomen for splenomegaly. o Laboratory evaluation will reveal decreased Hgb and Hct, decreased reticulocyte count, microcytosis, hypochromia, decreased serum iron and ferritin levels, and an increased free erythrocyte protoporphyrin (FEP) level. • The child with anemia is at risk for changes in neurologic functioning related to the decreased oxygen supply to the brain. This can lead to fatigue and inability to eat enough. Neurologic effects may be manifested when the child’s ability to sit, stand, or walk is impaired. • Ensure that iron-deficient infants are fed only formulas fortified with iron. Interventions for breast-fed infants include beginning iron supplementation around the age of 4 or 5 months. • For children over 1 year of age, limit cow’s milk intake to 24 oz per day. • Limit fast-food consumption and encourage intake of iron-rich foods such as o red meats (iron from red meat is the easiest for the body to absorb), tuna, salmon, eggs, tofu, enriched grains, dried beans and peas, dried fruits, leafy green vegetables, and iron-fortified breakfast cereals. • Teach parents to precisely measure the amount of iron to be administered. Parents should place the liquid behind the teeth, as iron in liquid form can stain the teeth. Iron supplementation can also cause constipation LEAD POISONING ANEMIA • Lead exerts toxic effects on the bone marrow, erythroid cells, nervous system, and kidneys. The presence of lead in the bloodstream interferes with the enzymatic processes of the biosynthesis of heme. The process results in hypochromic, microcytic anemia, and children may exhibit classic signs of anemia • Risk factors for lead poisoning are related to lead exposure in the home, school, or local environment. Sources of lead include: o Paint in homes built before 1978, at which time lead was banned as an additive to paint used in houses o Soil where cars that used leaded gas have been in the past (lead was removed from all gasoline in the United States as of 1996) o Glazed pottery o Stained glass products o Lead pipes supplying water to the home o On the clothing of parents who work in certain manufacturing jobs (battery makers, cable makers) o Certain folk remedies, such as greta or arzacon o Old painted toys or furniture • Complications of lead poisoning include behavioral problems and learning difficulties and, with higher lead levels, encephalopathy, seizures, and brain damage. • Therapeutic management for high blood levels of lead involves chelation therapy (removal of heavy metals from the body via chelating agents), either orally or intravenously • Blood levels of lead greater than 10 μg/dL require conscientious follow-up. • If the child is undergoing chelation therapy, ensure adequate fluid intake and monitor intake and output closely. Refer children with elevated lead levels and developmental or cognitive deficits to developmental centers. APLASTIC ANEMIA • The inherited types present as congenital bone marrow failure; the best known is Fanconi anemia, an autosomal recessive disorder. Acquired aplastic anemia is thought to be an immune-mediated response. o Most cases are idiopathic, meaning the trigger remains unidentified. Other causes include exposure to environmental toxins, viruses, myelosuppressive drugs, or radiation. • Aplastic anemia may be classified as severe or nonsevere. o In the severe form, the granulocyte count is less than 500, the platelet count is less than 20,000, and the reticulocyte count is less than 1%. o In nonsevere aplastic anemia, the granulocyte count is about 500, the platelet count is over 20,000, and the reticulocyte count is over 1% (Ambruso et al., 2014). • Complications of aplastic anemia include severe overwhelming infection, hemorrhage, and death. • Therapeutic management of aplastic anemia in children involves hematopoietic stem cell transplantation from a human leukocyte antigen (HLA)–matched sibling donor; if one is not available, immunosuppressive therapy or high-dose cyclophosphamide can be given. • Note history of epistaxis, gingival oozing, or increased bleeding with menstruation. Anemia may lead to headache and fatigue. On physical examination, note ecchymoses, petechiae or purpura, oral ulcerations, tachycardia, or tachypnea. • Safety is of the utmost concern in children with aplastic anemia. It is important to prevent injury in order to avoid hemorrhage. Stool softeners may be used to prevent anal fissures associated with constipation. Administer only irradiated and leukocyte-depleted PRBCs or platelet transfusions as necessary. Sickle Cell Disease • Sickle cell disease is a group of inherited hemoglobinopathies in which the RBCs do not carry the normal adult hemoglobin, but instead carry a less effective type • Sickle cell anemia is a severe chronic blood disorder that occurs once in every 2,000 newborns in the United States each year (Chandrakason & Kamat, 2013). It is most common in individuals of African, Mediterranean, Middle Eastern, and Indian decent. • Persons with heterozygous representation (Hgb AS) are said to have sickle cell trait and are carriers for the disorder; about 8% of African Americans have sickle cell trait (Ambruso et al., 2014). Generally, persons with sickle cell trait have only minimal health problems. • Hgb A refers to normal adult hemoglobin and Hgb S refers to sickle hemoglobin. These recessive genes for sickle cell may be passed on to the child. The risk for developing Hgb SS is one in four, or 25%, in each child from this union. • Infants with sickle cell anemia are usually asymptomatic until 3 to 4 months of age because Hgb F protects against sickling. • Complications of sickle cell anemia include recurrent vaso-occlusive pain crises, stroke, sepsis, acute chest syndrome, splenic sequestration, reduced visual acuity related to decreased retinal blood flow, chronic leg ulcers, cholestasis and gallstones, delayed growth and development, delayed puberty, and priapism (the sickled cells prevent blood from flowing out of an erect penis). o Children with sickle cell anemia have an increased incidence of enuresis because the kidneys cannot concentrate urine effectively • As the cells sickle, the blood becomes more viscous because the sickled cells clump together and prevent normal blood flow to the tissues of that area. o The sickle-shaped RBCs cannot pass through the smaller capillaries and venules of the circulatory system (Fig. 46.9). o This vaso-occlusive process leads to local tissue hypoxia followed by ischemia and may result in infarction. Pain crisis results as circulation is decreased to the area. Pain can occur in any part of the body but is most common in the joints. o Pain causes increased metabolic need by resulting in tachycardia and sometimes tachypnea, which leads to further sickling. o Clumping of cells in the lungs (acute chest syndrome [ACS]) results in decreased gas exchange, producing hypoxia, which leads to further sickling. ACS is the most common cause of death in children with sickle cell disease o The increased activity of the spleen related to RBC hemolysis leads to splenomegaly, then fibrosis and atrophy. • Prevention of infection is critical because the child with sickle cell anemia is at increased risk for serious infection related to alterations in splenic function. • Functional asplenia (decrease in the ability of the spleen to function appropriately) places the child at significant risk for serious infection • Oxygen administration is necessary during episodes of crisis to prevent additional cell sickling. Adequate hydration with intravenous fluids is critical. • Assessment o Note blood pressure, which may be decreased with severe anemia or increased with sickle cell nephropathy. Determine baseline mental status. Perform a neurologic assessment frequently, as about 11% of children with sickle cell anemia will experience an overt stroke o Auscultate heart sounds for a murmur. The heart rate is often elevated with pain, hyperthermia, or dehydration. Adventitious breath sounds may be present if a respiratory infection has triggered the sickle cell crisis or in the case of ACS. About half of the cases of ACS occur in the child already hospitalized for a pain crisis. o If the screening test result indicates the possibility of sickle cell anemia or sickle cell trait, Hgb electrophoresis is performed promptly to confirm the diagnosis. Hgb electrophoresis is the only accurate test for sickle cell disease. Hgb electrophoresis will demonstrate the presence of Hgb S and Hgb F only in the young infant; in the older infant or child, the result will be Hgb SS. • Common laboratory and diagnostic studies ordered for the assessment of sickle cell anemia include: o Hemoglobin: baseline is usually 7 to 10 mg/dL; will be significantly lower with splenic sequestration, acute chest syndrome, or aplastic crisis o Reticulocyte count: greatly elevated o Peripheral blood smear: presence of sickle-shaped cells and target cells o Platelet count: increased o Erythrocyte sedimentation rate: elevated o Abnormal liver function tests with elevated bilirubin • Teach families how to administer prophylactic penicillin. Encourage families to seek medical evaluation urgently for any febrile illness. Educate families about how to prevent and recognize vaso-occlusive events • Discuss complications such as delayed growth and development, delayed puberty, stroke, cholelithiasis, retinopathy, avascular necrosis, priapism, and leg ulcers. • To bring the pain under control, initially administer analgesics routinely rather than on an “as needed” (PRN) basis. Once the pain is better managed, medications may be moved to PRN status. o Nonsteroidal anti-inflammatory medications and acetaminophen are often used for less severe pain. Adequate pain management helps to decrease the child’s stress level; elevated stress may contribute to further sickling and additional pain • Increasing fluid intake will dilute the blood and decrease its viscosity. To promote hemodilution, provide 150 mL/kg of fluids per day or as much as double maintenance, either orally or intravenously. Maintain appropriate electrolyte and pH balance. • Administer supplemental oxygen if the pulse oximetry reading is 92% or less to promote adequate oxygenation • By 2 months of age, begin administration of oral penicillin V potassium as prophylaxis against pneumococcal infection. In the penicillin-allergic child, erythromycin may be used. Continue prophylaxis until at least age 5 years. • To prevent overwhelming sepsis or meningitis as a result of infection with S. pneumoniae, the child should receive not only the 7-valent pneumococcal vaccine series in infancy but also the 23-valent pneumococcal conjugate vaccine annually after age 2 years. Thalassemia • The genetics of thalassemia are similar to those of sickle cell disease in that it is inherited via an autosomal recessive process. Children with thalassemia have reduced production of normal hemoglobin. • There are two basic types of thalassemia, α and β. In α-thalassemia, synthesis of the α chain of the hemoglobin protein is affected. Problems with the β chain occur more often, and the condition β-thalassemia can be divided into three subcategories based on severity: o Thalassemia minor (also called β-thalassemia trait): leads to mild microcytic anemia; often no treatment is required. o Thalassemia intermedia: child requires blood transfusions to maintain adequate quality of life. o Thalassemia major: to survive the child requires ongoing medical attention, blood transfusions, and iron removal (chelation therapy). ♣ β-thalassemia major (Cooley anemia). ♣ A large number of unstable globulin chains accumulate, causing the RBCs to be rigid and hemolyzed easily. The result is severe hemolytic anemia and chronic hypoxia. ♣ The result is severe hemolytic anemia and chronic hypoxia. In response to the increased rate of RBC destruction, erythroid activity is increased. ♣ Hemosiderosis (excessive supply of iron) is an additional complication of significant concern. • It occurs as a result of rapid hemolysis of RBCs, the decrease in hemoglobin production, and the increased absorption of dietary iron in response to the severely anemic state. • The excess iron is deposited in the body’s tissues, causing bronze pigmentation of the skin, bony changes, and altered organ function, particularly in the cardiac system. • Additional complications include splenomegaly, endocrine abnormalities, osteoporosis, liver and gallbladder disease, and leg ulcers o Iron overload related to thalassemia leads to bony changes such as frontal bossing and maxillary prominence. o Laboratory testing may reveal the following: ♣ Hemoglobin and hematocrit are significantly decreased. ♣ Peripheral blood smear shows prominence of target cells, hypochromia, microcytosis, and extensive anisocytosis and poikilocytosis (variation in the size and shape of the RBCs, respectively). ♣ Bilirubin levels are elevated. ♣ Hgb electrophoresis shows the presence of Hgb F and Hgb A2 only. ♣ Iron level is elevated • Excess iron (hemosiderosis) is removed by chelation therapy. Administer the chelating agent deferoxamine with the transfusion. Deferoxamine binds to the iron and allows it to be removed through the stool or urine. Oral deferasirox may also be prescribed and is generally well tolerated, with minimal gastrointestinal side effects. • Chelation therapy must be maintained at home to continuously decrease the iron levels in the body. Teach family members to administer deferoxamine subcutaneously with a small battery-powered infusion pump over a several-hour period each night o If oral deferasirox is prescribed, instruct the family to dissolve the tablet in juice or water and administer it once daily. G6PD deficiency • Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme that is responsible for maintaining the integrity of RBCs by protecting them from oxidative substances. G6PD deficiency is an X-linked recessive disorder that occurs when the RBCs have insufficient G6PD, or the enzyme is abnormal and does not function properly. • Complications include prolonged neonatal jaundice and life-threatening acute episodes of hemolysis. Therapeutic management is primarily aimed at avoiding triggers that cause oxidative stress. • Note health history, including fatigue. Determine the parents’ understanding of the disorder and the medications and foods to avoid. Inspect the skin for pallor or jaundice. Evaluate neurologic status, which may also be affected. Measure heart rate and respiratory rate, noting elevations. Determine oxygen saturation via pulse oximeter or blood gas analysis. Note tea-colored urine. Palpate the abdomen for splenomegaly. Laboratory studies will reveal anemia. LEUKEMIA • It is a primary disorder of the bone marrow in which the normal elements are replaced with abnormal WBCs • Leukemia may be classified as acute or chronic, lymphocytic or myelogenous. Acute leukemias are rapidly progressive diseases affecting the undifferentiated or immature cells; the result is cells without normal function. • Chronic leukemias progress more slowly, permitting maturation and differentiation of cells so that they retain some of their normal function. • Complications of leukemia include metastasis (spread of cancer to other sites) to the blood, bone, CNS, spleen, liver, or other organs and alterations in growth. Late effects include problems with neurocognitive function and ocular, cardiovascular, or thyroid dysfunction. Acute Lymphoblastic Leukemia • Acute lymphoblastic leukemia is the most common form of cancer in children. Eighty-five percent of cases of ALL occur in children between 2 and 10 years of age • Generally, the higher the WBC count at diagnosis, the worse the prognosis. Children between 1 and 9 years of age and with a WBC count less than 50,000 at diagnosis have the best prognosis. When a child experiences a relapse, the prognosis becomes poorer. Complications include infection, hemorrhage, poor growth, and CNS, bone, or testicular involvement. • The lymphoblasts are fragile and immature, lacking the infection-fighting capabilities of the normal WBC. The growth of lymphoblasts is excessive and the abnormal cells replace the normal cells in the bone marrow • The bone marrow becomes unable to maintain normal levels of RBCs, WBCs, and platelets, so anemia, neutropenia, and thrombocytopenia result • Therapeutic management of the child with ALL focuses on giving chemotherapy to eradicate the leukemic cells and restore normal bone marrow function. • • Common signs and symptoms reported during the health history might include: o Fever (may be persistent or recurrent, with unknown cause) o Recurrent infection o Fatigue, malaise, or listlessness o Pallor o Unusual bleeding or bruising o Abdominal pain o Nausea or vomiting o Bone pain o Headache • Common laboratory and diagnostic studies ordered for the assessment of ALL include: o Complete blood counts: abnormal findings include low hemoglobin and hematocrit, decreased RBC count, decreased platelet count, and elevated, normal, or decreased WBC count o Peripheral blood smear may reveal blasts. o Bone marrow aspiration: stained smear from bone marrow aspiration will show greater than 25% lymphoblasts. Bone marrow aspirate is also examined for immunophenotyping (lymphoid vs. myeloid, and level of cancer cell maturity) and cytogenetic analysis (determines abnormalities in chromosome number and structure). Immunophenotyping and cytogenetic analysis are used in the classification of the leukemia, which helps guide treatment. o Lumbar puncture will reveal whether leukemic cells have infiltrated the CNS. o Liver function tests and blood urea nitrogen (BUN) and creatinine levels determine liver and renal function, which, if abnormal, may preclude treatment with certain chemotherapeutic agents. o Chest radiography may reveal pneumonia or a mediastinal mass. • Nursing care of children with ALL focuses on managing disease complications such as infection, pain, anemia, bleeding, and hyperuricemia and the many adverse effects related to treatment. Many children require blood product transfusion for the treatment of severe anemia or low platelet levels with active bleeding • Chemotherapy drugs commonly used in leukemia may cause peripheral neuropathy and headache. Lumbar puncture and bone marrow aspiration, which are periodically performed throughout the course of treatment, also cause pain. The most common areas of pain are the head and neck, legs, and abdomen (probably from protracted vomiting with chemotherapy). • Administer mild analgesics such as acetaminophen for acute episodes of pain. Using EMLA cream prior to venipuncture, port access, lumbar puncture, and bone marrow aspiration may decrease procedure-related pain events. Acute Myelogenous Leukemia • AML affects the myeloid cell progenitors or precursors in the bone marrow, resulting in malignant (invasive and fast-growing) cells. • Complications include treatment resistance, infection, hemorrhage, and metastasis. The induction phase of AML requires intense bone marrow suppression and prolonged hospitalization because AML is less responsive to treatment than ALL. Toxicity from treatment is more common in AML and is likely to be more serious than with ALL. Empiric broad-spectrum antibiotics and prophylactic platelet transfusions may be prescribed. • Explore the health history for common signs and symptoms, including recurrent infections, fever, or fatigue. Explore the medical history for risk factors, such as Hispanic race, previous chemotherapy, and genetic abnormalities such as Down syndrome, Fanconi anemia, neurofibromatosis type I, Shwachman syndrome, Bloom syndrome, and familial monosomy 7. • Perform a thorough physical examination. Note skin pallor and salmon-colored or blue-gray papular lesions. Palpate the skin for subcutaneous rubbery nodules. Palpate for lymphadenopathy. Note headache, visual disturbance, or signs of increased intracranial pressure, such as vomiting, which may indicate CNS involvement. Upon diagnosis of AML, the child’s WBC count is typically extremely elevated. Bone marrow aspiration will reveal greater than 20% blast cells NEUROBLASTOMA • Neuroblastoma, a tumor that arises from embryonic neural crest cells, is the most common extracranial solid tumor in children • It most frequently occurs in the abdomen, mainly in the adrenal gland, but it may occur anywhere along the paravertebral sympathetic chain in the chest or retroperitoneum • Staging of the tumor at diagn Prognosis depends on the tumor stage, age at diagnosis, location of tumor, and location of metastasis. Infants younger than 12 months of age and children with stage I disease have the best survival rates osis determines the course of treatment and prognosis • Metastasis to the bone is a worse prognostic factor than metastasis to the skin, liver, or bone marrow. • • Presenting signs and symptoms of neuroblastoma depend on the location of the primary tumor and the extent of metastasis. Often parents are the first to notice a swollen or asymmetric abdomen. Elicit the health history, documenting bowel or bladder dysfunction, especially watery diarrhea, neurologic symptoms (brain metastasis), bone pain (bone metastasis), anorexia, vomiting, or weight loss. • Note neck or facial swelling, bruising above the eyes, or edema around the eyes (metastasis to skull bones). Inspect the skin for pallor or bruising (bone marrow metastasis) and document cough or difficulty breathing. Auscultate the lungs for wheezing. Palpate for lymphadenopathy, especially cervical. Palpate the abdomen, noting a firm, nontender mass. Palpate for and note hepatomegaly or splenomegaly if present. • Laboratory and diagnostic testing may reveal the following: o CT scan or MRI to determine site of tumor and evidence of metastasis o Chest x-ray, bone scan, and skeletal survey to identify metastasis o Bone marrow aspiration and biopsy to determine metastasis to the bone marrow o 24-hour urine collection for homovanillic acid (HVA) and vanillylmandelic acid (VMA); levels will be elevated. BONE AND SOFT TISSUE TUMORS • Bone tumors are most often diagnosed in adolescence, whereas soft tissue tumors tend to occur in younger children • The most common bone tumors in children are osteosarcoma and Ewing sarcoma • Rhabdomyosarcoma is the most common soft tissue tumor in childhood Osteosarcoma • Osteosarcoma is the most common malignant bone cancer in children, occurring most frequently in adolescents at the peak of the growth spurt • It presumably arises from the embryonic mesenchymal tissue that forms the bones. The most common sites are in the long bones, particularly the proximal humerus, proximal tibia, and distal femur. • Complications include metastasis, particularly to the lungs and other bones, and recurrence of disease within 3 years, primarily affecting the lungs. • The type of surgery performed depends on the tumor size, extent of disease outside of the bone, distant metastasis, and skeletal maturity. Radical amputation may be performed, but often teens undergo a limb salvage procedure. Radical amputation may include the entire extremity or the entire affected bone. • Limb-sparing surgery entails removing only the affected portion of the bone, replacing it with either an endoprosthesis or cadaver bone • Inspect the affected limb for erythema and swelling. Palpate the affected area for warmth and tenderness and to determine the size of the soft tissue mass, if also present. As with other pediatric cancers, a thorough physical examination is warranted to detect other abnormalities that may indicate metastasis. o Laboratory and diagnostic testing may include: ♣ CT scan or MRI to determine the extent of the lesion and to identify metastasis ♣ Bone scan to determine the extent of malignancy • Educate the adolescent and parents on the care of the stump, if amputation is necessary, and ensure that the teen becomes competent in crutch walking. A prosthesis may be ordered. • Peer support groups are often helpful, as teens value their peers’ opinions and enjoy being part of a group. Ewing Sarcoma • Ewing sarcoma is a highly malignant bone tumor. It is rarer than osteosarcoma, accounting for only about 10% of childhood bone tumors (Graham et al., 2014). It occurs most frequently in the pelvis, chest wall, vertebrae, and long bone diaphyses (midshaft). • Radiation, chemotherapy, and surgical excision are usually used in combination. Treatment varies depending on the site of the primary tumor and the extent of metastasis at diagnosis. Myeloablative chemotherapy (which destroys the child’s marrow) may be used for metastatic disease, followed by a stem cell rescue transplant. • Before treatment begins, discourage active play or weight bearing on the affected extremity to avoid pathologic fracture at the tumor site • Depending on the age of the child, fantasy play, art or pet therapy, drama, writing, humor, and/or music may help the child to work through the psychological impact of this disease. Rhabdomyosarcoma • Rhabdomyosarcoma is a soft tissue tumor that usually arises from the embryonic mesenchymal cells that would ordinarily form striated muscle. The most common locations for the tumor are the head and neck, genitourinary tract, and extremities • The tumor is highly malignant and spreads via local extension or through the venous or lymphatic system, with the lung being the most common site for metastasis. • Prognosis is generally favorable for stage I disease, but 3-year survival occurs in only 39% of children with metastatic disease • Complications of rhabdomyosarcoma include metastasis to lung, bone, or bone marrow and direct extension into the CNS, resulting in brain stem compromise or cranial nerve palsy. • Laboratory and diagnostic testing may include: o CT scan or MRI of primary lesion and the chest for metastasis o Open biopsy of the primary tumor for definitive diagnosis o Bone marrow aspiration and biopsy, bone scan, and skeletal survey to determine metastasis o WILMS TUMOR • Wilms tumor is the most common renal tumor and the fourth most common solid tumor in children (Hendershot, 2010). Peak incidence occurs between the ages of 2 and 3 years • It usually affects only one kidney • Wilms tumor demonstrates rapid growth and is usually large at diagnosis. Metastasis occurs via direct extension or through the bloodstream. Wilms tumor most commonly metastasizes to the perirenal tissues, liver, diaphragm, lungs, abdominal muscles, and lymph nodes • Complications include metastasis or complications from radiation therapy such as liver or renal damage, female sterility, bowel obstruction, pneumonia, or scoliosis. • Surgical removal of the tumor and affected kidney (nephrectomy) is the treatment of choice and also allows for accurate staging and assessment of tumor spread. Radiation or chemotherapy may be administered either before or after surgery. • History o Note abdominal pain, which may be related to rapid tumor growth. Document history of constipation, vomiting, anorexia, weight loss, or difficulty breathing. Determine risk factors such as hemihypertrophy of the spine, Beckwith–Wiedemann syndrome, genitourinary anomalies, absence of the iris, or family history of cancer. • Assess o Measure blood pressure; hypertension occurs in 25% of children with Wilms tumor . Inspect the abdomen for asymmetry or a visible mass. Observe for associated anomalies as noted above. Auscultate the lungs for adventitious breath sounds associated with tumor metastasis. Palpate for lymphadenopathy. • Laboratory and diagnostic testing may include: o Renal or abdominal ultrasound to assess the tumor and the contralateral kidney o CT scan or MRI of the abdomen and chest to determine local spread to lymph nodes or adjacent organs, as well as any distant metastasis o Complete blood count, BUN, and creatinine: usually within normal limits o Urinalysis: may reveal hematuria or leukocytes o 24-hour urine collection for HVA and VMA to distinguish the tumor from neuroblastoma (levels will not be elevated with Wilms tumor) 41 CONGENITAL HEART DISEASE • Many chromosome defects are associated with CHD, including Down syndrome, velocardiofacial syndrome, Turner syndrome, trisomy 13, trisomy 18, Williams syndrome, Prader–Willi syndrome, and cri-du-chat • Complications of CHD include heart failure, hypoxemia, growth retardation, developmental delay, and pulmonary vascular disease. Children with severe anomalies frequently experience failure to thrive. • Hypothermia, cardiopulmonary bypass required during cardiac surgery for CHD, and episodes of hypoxemia may have a long-term impact on the child’s cognitive ability and academic function • Pathophysiology o The exact cause of CHD is unknown. However, the belief is that it results from interplay of several factors, including genetics (e.g., chromosomal alterations) and maternal exposure to environmental factors (e.g., toxins, infections, chronic illnesses, and alcohol). o Congenital heart defects result from some interference in the development of the heart structure during fetal life. Subsequently, the septal walls or valves may fail to develop completely, or vessels or valves may be stenotic, narrowed, or transposed. o If the ductus arteriosus fails to close, blood will move from the aorta to the pulmonary artery, ultimately increasing right atrial pressure. With this shunting of blood, highly oxygenated blood can mix with less oxygenated blood, interfering with the amount available to the tissues via the systemic circulation • Congenital heart defects are categorized based on hemodynamic characteristics (blood flow patterns in the heart): o Disorders with decreased pulmonary blood flow: tetralogy of Fallot and tricuspid atresia o Disorders with increased pulmonary blood flow: PDA, atrial septal defect (ASD), and ventricular septal defect (VSD) o Obstructive disorders: coarctation of the aorta, aortic stenosis, and pulmonary stenosis o Mixed disorders: transposition of the great vessels (TGV), total anomalous pulmonary venous return (TAPVR), truncus arteriosus, and hypoplastic left heart syndrome (HLHS) • In newborns and very young infants with severe cyanosis (tricuspid atresia, TGV), a prostaglandin infusion will maintain patency of the ductus arteriosus, improving pulmonary blood flow Disorders with Decreased Pulmonary Blood Flow • As a result of the obstruction, pressure in the right side of the heart increases and becomes greater than that of the left side of the heart. o Blood from the higher-pressure right side of the heart then shunts to the lower-pressure left side through a structural defect. o Subsequently, deoxygenated blood mixes with oxygenated blood on the left side of the heart. o This mixed blood, which is low in oxygen, is pumped via the systemic circulation to the body tissues. • child exhibits oxygen saturation levels ranging from 50% to 90% o To compensate for low blood oxygen levels, the kidneys produce the hormone erythropoietin to stimulate the bone marrow to produce more red blood cells (RBCs). This increase in RBCs is called polycythemia. • Tetralogy of Fallot o Tetralogy of Fallot is a congenital heart defect composed of four heart defects: ♣ pulmonary stenosis (a narrowing of the pulmonary valve and outflow tract, creating an obstruction of blood flow from the right ventricle to the pulmonary artery), ♣ VSD, ♣ overriding aorta (enlargement of the aortic valve to the extent that it appears to arise from the right and left ventricles rather than the anatomically correct left ventricle), and ♣ right ventricular hypertrophy (the muscle walls of the right ventricle increase in size due to continued overuse as the right ventricle attempts to overcome a high-pressure gradient) o The obstructed flow (pulmonary stenosis) also increases the pressure in the right ventricle. ♣ This blood, which is poorly oxygenated, is then shunted across the VSD into the left atrium. ♣ Poorly oxygenated blood also travels through the overriding aorta (if it extends to both ventricles). ♣ In some cases when the VSD is large, the pressure in the right ventricle may be equal to that of the left ventricle. ♣ In this case, the path of blood shunting depends on which circulation is exerting the higher pressure, pulmonary or systemic. ♣ The oxygen saturation of the blood in the systemic circulation is reduced, leading to cyanosis. The degree of cyanosis depends on the extent of the pulmonary stenosis, the size of the VSD, and the vascular resistance of the pulmonary and systemic circulations. o Tetralogy of Fallot is usually diagnosed during the first weeks of life due to the presence of a murmur and/or cyanosis. Some newborns may be acutely cyanotic, while others may exhibit only mild cyanosis that gradually becomes more severe, particularly during times of stress as the child grows older o o Hypercyanosis develops suddenly and is manifested as increased cyanosis, hypoxemia, dyspnea, and agitation. If the infant’s oxygen demand is greater than the supply, such as with crying or during feeding, then the spell progresses to anoxia. ♣ The walking infant or toddler may squat periodically. These positions improve pulmonary blood flow by increasing systemic vascular resistance o Note increased hematocrit, hemoglobin, and RBC count associated with polycythemia. Additional testing may include: ♣ Echocardiography (ultrasound study of structure and motion of heart), possibly revealing right ventricular hypertrophy, decreased pulmonary blood flow, and reduced size of the pulmonary artery ♣ Electrocardiogram (ECG), indicating right ventricular hypertrophy ♣ Cardiac catheterization and angiography, which reveal the extent of the structural defects • Tricuspid Atresia o Tricuspid atresia is a congenital heart defect in which the valve between the right atrium and right ventricle fails to develop. As a result, there is no opening to allow blood to flow from the right atrium to the right ventricle and subsequently through the pulmonary artery into the lungs o n tricuspid atresia, blood returning from the systemic circulation to the right atrium cannot directly enter the right ventricle due to agenesis of the tricuspid valve. Subsequently, deoxygenated blood may pass through an opening in the atrial septum (patent foramen ovale) into the left atrium, never entering the pulmonary vasculature. Thus, deoxygenated blood mixes with oxygenated blood in the left atrium. The blood then travels to the lungs through a PDA. Most cases of tricuspid atresia are associated with a VSD and the newborn receives inadequately oxygenated blood o o Note history of rapid respirations and difficulty with feeding. Inspect the skin for cyanosis or a pale gray color. Observe the apical impulse, noting overactivity. Evaluate the baby’s sucking strength (will usually have a weak or poor suck). Count the respiratory rate, noting tachypnea. Note increased work of breathing. Auscultate the lungs, noting crackles or wheezes if heart failure is beginning to develop. Auscultate the heart, noting a murmur. o Lab tests – same as tetraology of fallot Disorders with Increased Pulmonary Flow • Excessive blood flow to the lungs can produce a compensatory response such as tachypnea or tachycardia. • Tachypnea increases caloric expenditure; poor cellular nutrition from decreased peripheral blood flow leads to feeding problems. • Increased pulmonary blood flow also places the child at higher risk for pulmonary infections. As the child grows, the continuous increased pulmonary blood flow will cause vasoconstriction of the pulmonary vessels, actually decreasing the pulmonary blood flow • For children with congenital defects with increased pulmonary blood flow, oxygen supplementation is not helpful. Oxygen acts as a pulmonary vasodilator. If pulmonary dilation occurs, pulmonary blood flow is even greater, causing tachypnea, increasing lung fluid retention, and eventually causing a much greater problem with oxygenation • Atrial Septal Defect o An ASD is a passageway or hole in the wall (septum) that divides the right atrium from the left atrium (Fig. 41.4). Three types of ASDs are identified based on the location of the opening: ♣ Ostium primum (ASD1): the opening is at the lower portion of the septum. ♣ Ostium secundum (ASD2): the opening is near the center of the septum. ♣ Sinus venosus defect: the opening is near the junction of the superior vena cava and the right atrium. o When the ASD is small, as many as 80% of infants may have a spontaneous closure within the first 18 months of life. If it does not spontaneously close by age 3, the child will most likely need corrective surgery o With ASD, blood flows through the opening from the left atrium to the right atrium due to pressure differences. The shunting increases the blood volume entering the right atrium. This, in turn, leads to increased blood flow into the lungs. If untreated, the defect can cause problems such as pulmonary hypertension, heart failure, atrial arrhythmias, or stroke o o Auscultate the heart, noting a fixed split second heart sound and a systolic ejection murmur, best heard in the pulmonic valve area o Echocardiography is done to confirm the diagnosis. An electrocardiogram (ECG) (graphic recording of the heart’s electrical activity) may show normal sinus rhythm or prolonged PR intervals. The chest x-ray may show enlargement of the heart and increased vascularity of the lungs. • Ventricular Septal Defect o A VSD is an opening between the right and left ventricular chambers of the heart o Spontaneous closure of small VSDs occurs in about half of children by age 2 years. Long-term outcomes for surgically repaired VSDs are good. Repair of larger defects by 2 years of age is recommended to prevent the development of pulmonary disease o o When the pulmonary vascular resistance exceeds the systemic vascular resistance, right-to-left shunting of blood across the VSD occurs, resulting in Eisenmenger syndrome (pulmonary hypertension and cyanosis). Heart failure commonly occurs in children with moderate to severe unrepaired VSDs. Children with VSDs are also at risk for the development of aortic valve regurgitation as well as infective endocarditis o Determine the health history, which commonly reveals signs of heart failure around 4 to 8 weeks of age. o Ask the parent about color change or diaphoresis with nipple feeding in the infant. o Auscultate the heart, noting a characteristic holosystolic harsh murmur along the left sternal border o Magnetic resonance imaging (MRI) or echocardiogram with color flow Doppler may reveal the opening as well as the extent of left-to-right shunting. These studies also may identify right ventricular hypertrophy and dilation of the pulmonary artery resulting from the increased blood flow. Cardiac catheterization may be used to evaluate the extent of blood flow being pumped to the pulmonary circulation and to evaluate hemodynamic pressures. • Atrioventricular Canal Defect o Atrioventricular canal defect (atrioventricular septal defect [AVSD], AV canal, or endocardial cushion defect) accounts for 3.5% of CHD. Forty-five percent of children with Down syndrome and CHD have this defect o AV canal defect occurs as a result of failure of the endocardial cushions to fuse (Fig. 41.6). These cushions are needed to separate the central parts of the heart near the tricuspid and mitral (AV) valves. The complete AV canal defect involves ASDs and VSDs as well as a common AV orifice and a common AV valve o o The complete AV canal defect permits oxygenated blood from the lungs to enter the left atrium and ventricle, crossing over the atrial or ventricular septum and returning to the lungs via the pulmonary artery. o Therefore, this specific type of cardiac defect causes a large left-to-right shunt; an increased workload of the left ventricle; and high pulmonary arterial pressure, resulting in an increased amount of blood in the lungs and causing pulmonary edema o Inspect the skin, fingernails, and lips for cyanosis. Observe for retractions, tachypnea, and nasal flaring. Auscultate the lungs and heart, noting rales and a loud murmur. The murmur is commonly noted within the first 2 weeks of life. Infants with partial or transitional AV canal defects may display more subtle signs. o Echocardiography will reveal the extent of the defect and shunting as well as right ventricular hypertrophy. ECG may indicate right ventricular hypertrophy and possible first-degree heart block due to impulse blocking before reaching the AV node. • Patent Ductus Arteriosus o PDA is failure of the ductus arteriosus, a fetal circulatory structure, to close within the first weeks of life (Fig. 41.7). As a result, there is a connection between the aorta and pulmonary artery o o This altered blood flow pattern increases the workload of the left side of the heart. Pulmonary vascular congestion occurs, causing an increase in pressure. Right ventricular pressure increases in an attempt to overcome this increase in pulmonary pressure. Eventually, right ventricular hypertrophy occurs o If it is small, the infant may be asymptomatic. Some infants demonstrate signs and symptoms of heart failure. o Echocardiogram reveals the extent of the defective opening and confirms the diagnosis. ECG may be normal or it may indicate ventricular hypertrophy, especially if the defect is large. Chest radiography demonstrates cardiomegaly. Obstructive Disorders o These disorders involve some type of narrowing of a major vessel, interfering with the ability of the blood to flow freely through the vessel. As a result, peripheral circulation or blood flow to the lungs is affected. Coarctation of the Aorta o Coarctation of the aorta is narrowing of the aorta, the major blood vessel carrying highly oxygenated blood from the left ventricle of the heart to the rest of the body o Coarctation of the aorta occurs most often in the area near the ductus arteriosus. The narrowing can be preductal (between the subclavian artery and ductus arteriosus) or postductal (after the ductus arteriosus) ♣ As a result of the narrowing, blood flow is impeded, causing pressure to increase in the area proximal to the defect and to decrease in the area distal to it. ♣ Thus, BP is increased in the heart and upper portions of the body and decreased in the lower portions of the body. Left ventricular afterload is increased, and in some children this may lead to heart failure. ♣ Collateral circulation also may develop as the body attempts to ensure adequate blood flow to the descending aorta. Due to the elevation in BP, the child is also at risk for aortic rupture, aortic aneurysm, and CVA o Assess ♣ Determine BP in all four extremities. BP in the upper extremities may be 20 mm Hg or higher than that in the lower extremities. Inspect the school-age child’s chest, noting notching of the ribs. Auscultate the heart for a soft or moderately loud systolic murmur, most often heard at the base of the heart (on the back or in the left axilla) o TESTS ♣ In addition, an echocardiogram may disclose the extent of narrowing and evidence of collateral circulation. Chest radiography may reveal left-sided cardiac enlargement and rib notching indicative of collateral arterial enlargement. Other tests, such as ECG, computed tomography, or MRI, may be done to provide additional evidence about the extent of the coarctation and subsequent effects. o Aortic Stenosis o Aortic stenosis is a condition causing obstruction of the blood flow between the left ventricle and the aorta. o Aortic stenosis can be caused by a muscle obstruction below the aortic valve, an obstruction at the valve itself, or an aortic narrowing just above the valve o Aortic stenosis occurs when the aortic valve narrows, causing an obstruction between the left ventricle and the aorta. As a result, cardiac output decreases o When the aortic valve does not function properly, the left ventricle must work harder to pump blood into the aorta. Because of the increased workload, the left ventricular muscle hypertrophies o . If this continues, left ventricular failure can occur, leading to a backup of pressure in the pulmonary circulation and pulmonary edema. o Obtain the child’s health history, noting easy fatigability or complaints of chest pain similar to anginal pain when active. Dizziness with prolonged standing also may be reported. In the infant, note difficulty with feeding. Palpate the child’s pulse; if aortic stenosis is severe, the pulses may be faint. Palpate the child’s chest, noting a thrill at the base of the heart. Auscultate the heart, noting a systolic murmur best heard along the left sternal border with radiation to the right upper sternal border. o The echocardiogram is the most important noninvasive test to identify aortic stenosis. An ECG may be normal in children with mild to moderate forms of aortic stenosis. For children with severe aortic stenosis, left ventricular hypertrophy may be determined from the ECG. For children experiencing easy fatigability and chest pain, an exercise stress test may be done to evaluate the degree of cardiac compromise. o Pulmonary Stenosis o Pulmonary stenosis is a condition that causes an obstruction in blood flow between the right ventricle and the pulmonary arteries. o Children may be asymptomatic, although some children with severe stenosis may exhibit dyspnea and fatigue with exertion (demonstrating hypercyanotic spells similar to those in children with tetralogy of Fallot) o Pulmonary stenosis may occur as a muscular obstruction below the pulmonary valve, an obstruction at the valve, or a narrowing of the pulmonary artery above the valve o The most common problem causing pulmonary stenosis is that the pulmonary valve leaflets are thickened and fused together along their separation lines, causing the obstruction to blood flow. o When the pulmonary valve is severely obstructed, the right ventricle cannot eject sufficient blood into the pulmonary artery. As a result, pressure in the right atrium increases, which could lead to a reopening of the foramen ovale. o o Elicit the health history, noting mild dyspnea or cyanosis with exertion. Document the child’s growth history, which is typically normal. Carefully palpate the sternal border for a thrill (not always present). Auscultate the heart, noting a high-pitched click following the second heart sound and a systolic ejection murmur loudest at the upper left sternal border. o An echocardiogram reveals the extent of obstruction present at the valve, as well as right ventricular hypertrophy. An ECG also helps to detect right ventricular hypertrophy. Heart Failure o Heart failure occurs most often in children with CHD and is the most common reason for admission to the hospital for children with CHD. Most cases of heart failure in children with CHD occur by 6 months of age o Heart failure refers to a set of clinical signs and symptoms that reflect the heart’s inability to pump effectively to provide adequate blood, oxygen, and nutrients to the body organs and tissues o When the ventricular contraction is impaired (systolic dysfunction), reduced ejection of blood occurs, and therefore cardiac output is reduced – RAAS activated – distension occurs – CO diminishes further. o Management of heart failure is supportive. Promotion of oxygenation and ventilation is of utmost importance. Digitalis, diuretics, inotropic agents, vasodilators, antiarrhythmics, and antithrombotics have been widely used in children for palliation of symptoms. o o Common complaints reported during the health history might include: o Failure to gain weight or rapid weight gain o Failure to thrive o Difficulty feeding o Fatigue o Dizziness, irritability o Exercise intolerance o Shortness of breath o Sucking and then tiring quickly o Syncope o Decreased number of wet diapers o Also be alert for statements such as “The baby drinks a small amount of breast milk (or formula) and stops, but then wants to eat again very soon afterwards”; “The baby seems to perspire a lot during feedings”; or “The baby seems to be more comfortable when he’s sitting up or on my shoulder than when he’s lying flat.” o Assess o Weigh the child and note recent rapid weight gain or lack of weight gain. Obtain the child’s vital signs, noting tachycardia or tachypnea. o Note decreased BP, which may be due to impaired cardiac muscle function. Inspect the skin color, noting pallor or cyanosis. Also observe for diaphoresis (profuse sweating). Inspect the face, hands, and lower extremities for edema. Observe for increased work of breathing, such as nasal flaring or retractions. Note the presence of a cough, which may be productive with bloody sputum. Auscultate the apical pulse, noting its location and character. Listen for a murmur, Note the temperature and color of the extremities; they may be cool, clammy, and pale. o These include: o Chest x-ray, revealing an enlarged heart and/or pulmonary edema o Electrocardiogram, indicating ventricular hypertrophy o Echocardiogram, revealing the underlying cause of heart failure, such as a congenital heart defect o Arterial blood gas results may demonstrate respiratory alkalosis in mild heart failure or metabolic acidosis. Tissue hypoxia may be evidenced by increased lactic acid and decreased bicarbonate levels. o Promoting Oxygenation o Position the infant or child in a semi-upright position to decrease work of breathing and lessen pulmonary congestion. o Suction as needed. o Chest physiotherapy and postural drainage may also be beneficial. Administer supplemental oxygen as ordered and monitor oxygen saturation via pulse oximetry. o Supporting Cardiac Function o Administer digitalis, angiotensin-converting enzyme (ACE) inhibitors, and diuretics as prescribed. o Digoxin therapy begins with a digitalizing dose divided into several doses (oral or intravenous [IV]) over a 24-hour period to reach maximum cardiac effect. ♣ During digitalization, monitor the ECG for a prolonged PR interval and decreased ventricular rate. ♣ Doses are then administered every 12 hours. ♣ Monitor the child for signs of digoxin toxicity. o Measure BP before and after administration of ACE inhibitors, holding the dose and notifying the physician if the BP falls more than 15 mm Hg. o Observe for signs of hypotension such as lightheadedness, dizziness, or fainting. o Weigh the child daily to determine fluid loss. o Maintain accurate records of intake and output, restricting fluid intake if ordered. o Carefully monitor potassium levels, administering potassium supplements if prescribed. Sodium intake is not usually restricted in the child with heart failure o Providing Adequate Nutrition o Due to the increased metabolic rate associated with heart failure, the infant may require as much as 150 calories/kg/day. o During the acute phase of heart failure, many infants in particular will require continuous or intermittent gavage feeding to maintain or gain weight. Concentrate infant formula to 24 to 28 calories/ounce as instructed by the nutritionist. ACUTE RHEUMATIC FEVER o Acute rheumatic fever (ARF) is a delayed sequela of group A streptococcal pharyngeal infection. o It usually develops 2 to 4 weeks after the initial streptococcal infection. o The antibodies then cross-react with antigens in cardiac muscle and neuronal and synovial tissues, causing carditis, arthritis, and chorea (involuntary random, jerking movements). ARF affects the joints, central nervous system, skin, and subcutaneous tissue and causes chronic, progressive damage to the heart and valves. o Most attacks of ARF last 6 to 12 weeks and then are resolved, o Therapeutic management is directed toward managing inflammation and fever, eradicating the bacteria, preventing permanent heart damage, and preventing recurrences. A full 10-day course of penicillin therapy (or equivalent) is used along with corticosteroids and nonsteroidal anti-inflammatory drugs o Children without valvular disease will receive continued prophylaxis with monthly intramuscular injections of penicillin G benzathine or daily oral doses of penicillin or erythromycin following the initial illness in order to prevent a new streptococcal infection and recurrent ARF. Prophylaxis is continued until adulthood o o Assessement o Elicit a description of the present illness and chief complaint, noting fever and joint pain. o Explore the child’s recent medical history for risk factors such as documented streptococcal infection or sore throat within the past 2 to 3 weeks, or for past history of ARF. o Observe the child for Sydenham chorea, a movement disorder of the face and upper extremities. o Inspect the skin for evidence of the classic rash, erythema marginatum, a maculopapular red rash with central clearing and elevated edges. o Auscultate the heart, noting a murmur. o Palpate the surfaces of the wrist, elbows, and knees for firm, painless, subcutaneous nodules. o Note prolonged PR interval on the ECG. o Throat culture will provide definitive diagnosis of current streptococcal infection, while streptococcal antibody tests may yield evidence of recent infection. Echocardiogram is required to determine if carditis is present. o Nursing management of the child with ARF focuses on ensuring compliance with the acute course of antibiotics as well as prophylaxis following initial recovery from ARF. o Some children may require a neuroleptic agent such as haloperidol (Haldol) for management of chorea. Administer corticosteroids or nonsteroidal anti-inflammatory agents for control of joint pain and swelling. KAWASAKI DISEASE o Kawasaki disease is an acute systemic vasculitis occurring mostly in children 6 months to 5 years of age o Although Kawasaki disease affects all ethnic groups, it occurs more frequently in those of Asian or Pacific descent. It is a self-limited syndrome but can cause cardiovascular complications such as coronary artery aneurysm and cardiomyopathy, among others o Therapeutic management of acute Kawasaki disease focuses on reducing inflammation in the walls of the coronary arteries and preventing coronary thrombosis. o Chronic management of children developing aneurysms during the initial phase is directed toward preventing myocardial ischemia. o In the acute phase, high-dose aspirin in four divided doses daily and a single infusion of intravenous immunoglobulin (IVIG) are used. o It appears that the best response occurs if IVIG is given within the first 7 to 10 days of the illness o Kawasaki disease appears to be an autoimmune response mediated by cytokine-induced endothelial cell surface antigens that leads to vasculitis. o Generalized systemic vasculitis occurs in the blood vessels throughout the body due to the inflammation and edema and can lead to coronary dilatation or aneurysm. o Elicit the health history, noting any of the following: o Fever o Chills o Headache o Malaise o Extreme irritability o Vomiting o Diarrhea o Abdominal pain o Joint pain o Of particular note is a history of high fever (39.9°C) of at least 5 days’ duration that is unresponsive to antibiotics. o Observe for significant bilateral conjunctivitis without exudate. Inspect the mouth and throat for dry, fissured lips; strawberry (cracked and reddened) tongue; and pharyngeal and oral mucosa erythema. Note hyperdynamic precordium. Evaluate the skin for: o Diffuse, erythematous, polymorphous rash o Edema of the hands and feet o Erythema and painful induration of the palms and soles o Desquamation (peeling) of the perineal region, fingers, and toes, extending to the palms and soles o Possible jaundice o The CBC count may reveal mild to moderate anemia, an elevated white blood cell count during the acute phase, and significant thrombocytosis (elevated platelet count [500,000 to 1 million]) in the later phase. The erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) level are elevated. Echocardiogram is performed as soon as possible after the diagnosis is confirmed to provide a baseline of a healthy heart or to evaluate for coronary artery involvement. Nursing Management o Administer intravenous and oral fluids as ordered, evaluating intake and output carefully. Prepare the child for the echocardiogram. Assess frequently for signs of developing heart failure such as tachycardia, gallop, decreased urine output, or respiratory distress. o Provide acetaminophen for fever management and apply cool cloths as tolerated. Keep the environment quiet and cluster nursing care activities to decrease stimulation and hence irritability. Teach parents that irritability is a prominent feature of Kawasaki disease, and support their efforts to console the child. Apply petrolatum jelly or another lubricating ointment to the lips. o Teach parents to continue to monitor the child’s temperature after discharge until the child has been afebrile for several days. Children with prolonged or recurrent fever may require a second dose of IVIG o Report any toxic effects of aspirin therapy, such as headache, confusion, dizziness, or tinnitus to the physician or nurse practitioner. It is important to avoid nonsteroidal anti-inflammatory agents while aspirin therapy is ongoing. CARDIAC CATHETERIZATION o Indications for cardiac catheterization include: o Cardiovascular disease causing cyanosis in infants: these infants need to be catheterized as soon as they are in a reasonably stable condition o Severe heart failure or progressive problems such as pulmonary edema o Questionable anatomic or physiologic abnormalities o Planned cardiac surgery o Progressive monitoring related to pulmonary hypertension o Periodic assessment after repair of a cardiac defect o Therapeutic interventions such as septostomy or balloon valvotomy o Diagnostic cardiac catheterization typically is used to identify structural defects. o Interventional cardiac catheterization is used as a treatment measure to dilate occluded or stenotic structures or vessels or close some defects. o Electrophysiologic cardiac catheterization involves the use of electrodes to identify abnormal rhythms and destroy sites of abnormal electrical conduction. o In cardiac catheterization, a radiopaque catheter is inserted into a blood vessel and is then guided through the vessel to the heart with the aid of fluoroscopy. For a right-sided catheterization, the catheter is threaded to the right atrium via a major vein such as the femoral vein. With a left-sided catheterization, the catheter is threaded to the aorta and heart via an artery. Once the tip of the catheter is in the heart, contrast material is injected via the catheter and radiographic images are taken. o With the injection of contrast material, information is revealed about the heart anatomy, ventricular wall motion and ejection fraction, intracardiac pressures and hemodynamic parameters, cardiac valve function, and structural abnormalities. o The movement of the contrast material is filmed so that the details of the cardiac procedure are recorded. Samples of heart tissue to evaluate for infection, muscular dysfunction, or rejection after a transplant may also be obtained o Before the Procedure o Note fever or other signs and symptoms of infection, which may necessitate rescheduling the procedure. o Obtain the child’s height and weight to aid in determining medication dosages. Assess the child for any allergies, especially to iodine and shellfish, because some contrast materials contain iodine as a base. o Review the child’s medications: medications such as anticoagulants are typically withheld for several days or longer prior to the procedure to reduce the child’s risk for bleeding. o Use an indelible pen to mark the location of the child’s pedal pulses so they can be easily assessed after the procedure. o xplain the use of intravenous fluid therapy, sedation, and, if ordered, anesthesia to the child and parents. Tell the child that he or she may feel a sensation of the heart racing when the catheter is inserted. Also warn the older child that he or she may experience a feeling of warmth or stinging when the contrast material is injected o Typically, food and fluid are withheld for 4 to 6 hours before the procedure. Prescribed medications may be taken with a sip of water. On the day of the procedure, check to ensure that a signed informed consent form o Inform the parents of the possible complications that might occur, such as bleeding, low-grade fever, loss of pulse in the extremity used for the catheterization, and development of arrhythmia (abnormal heart rhythm). o Explain to the child that he or she will have a dressing over the catheter site and that he or she will need to keep the leg straight for several hours after the procedure. o After the Procedure. o Throughout the postprocedure period, closely monitor the child for complications of bleeding, arrhythmia, hematoma, and thrombus formation and infection. o After the procedure, evaluate the child’s vital signs, the neurovascular status of the lower extremities, and the pressure dressing over the catheterization site every 15 minutes for the first hour and then every 30 minutes for 1 hour. o Hypotension may signify hemorrhage due to perforation of the heart muscle or bleeding from the insertion site. Expect to monitor cardiac rhythm and oxygen saturation levels o assess the color and temperature of the extremity; pallor or blanching would indicate an obstruction in blood flow. o Ensure that the child maintains the extremity in a straight position for approximately 4 to 8 hours o If bleeding occurs after a cardiac catheterization, apply pressure 1 in above the site to create pressure over the vessel, thereby reducing the blood flow to the area. o The contrast material has a diuretic effect, so assess the child for signs and symptoms of dehydration and hypovolemia. [Show More]
Last updated: 1 year ago
Preview 1 out of 73 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 20, 2020
Number of pages
73
Written in
Additional information
This document has been written for:
Uploaded
May 20, 2020
Downloads
0
Views
44

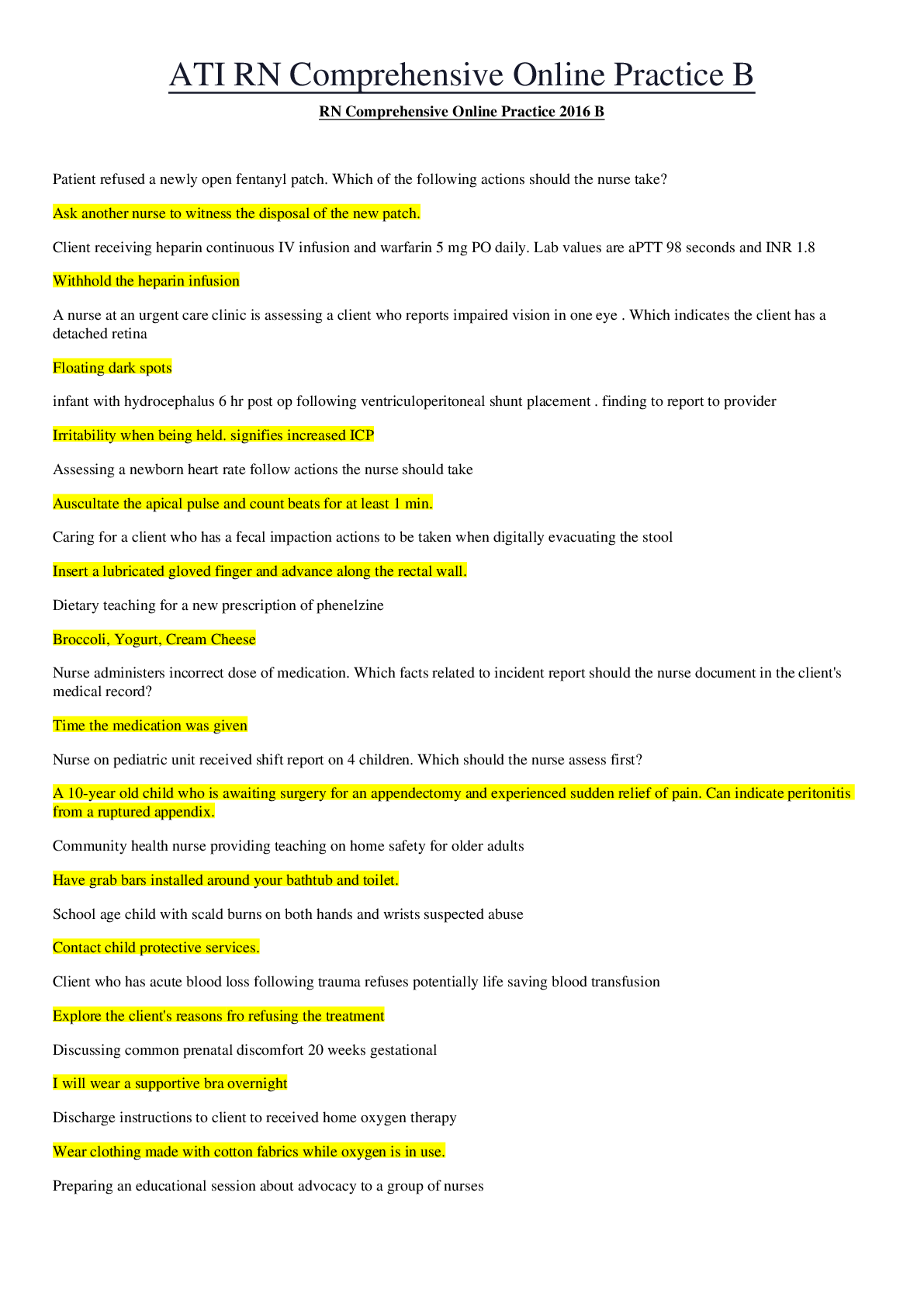
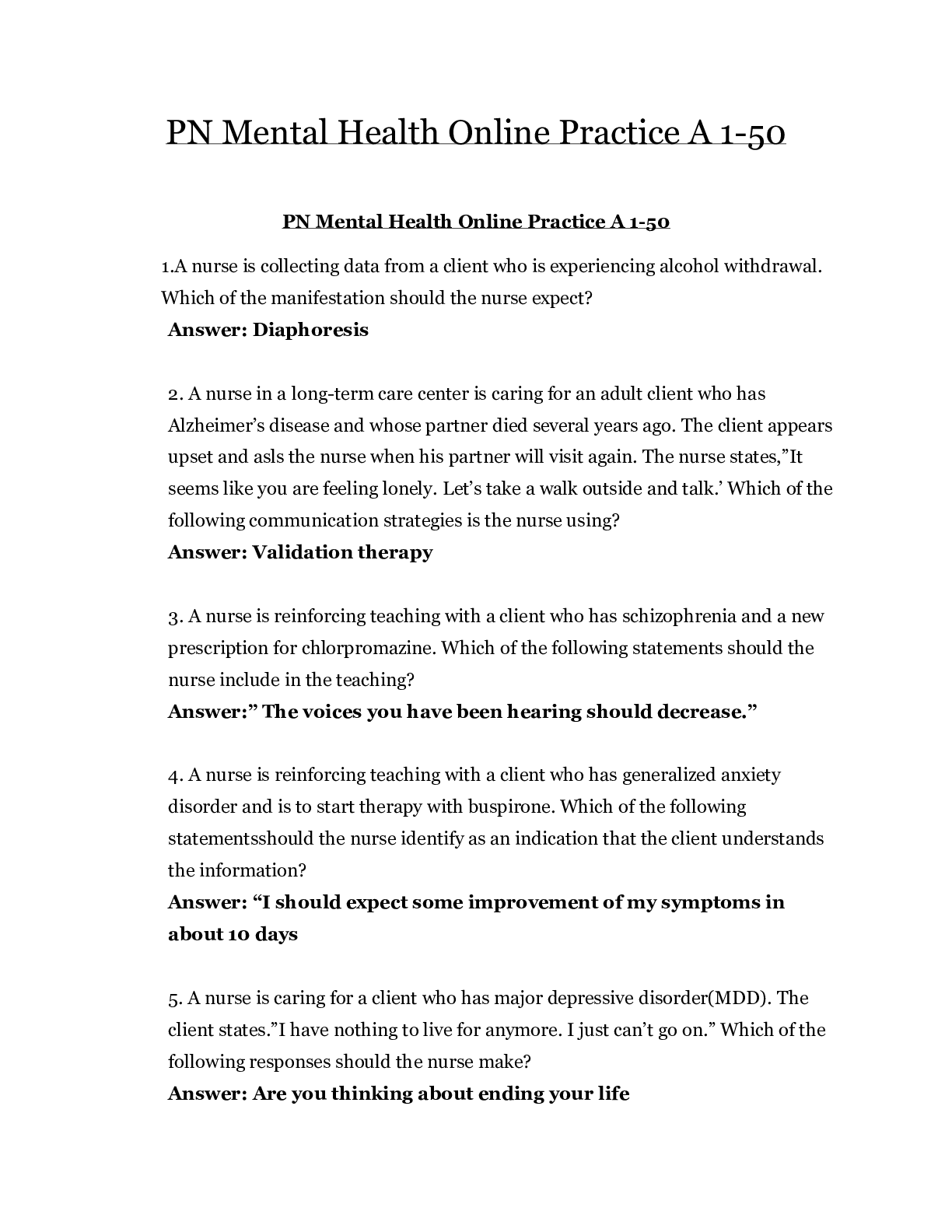
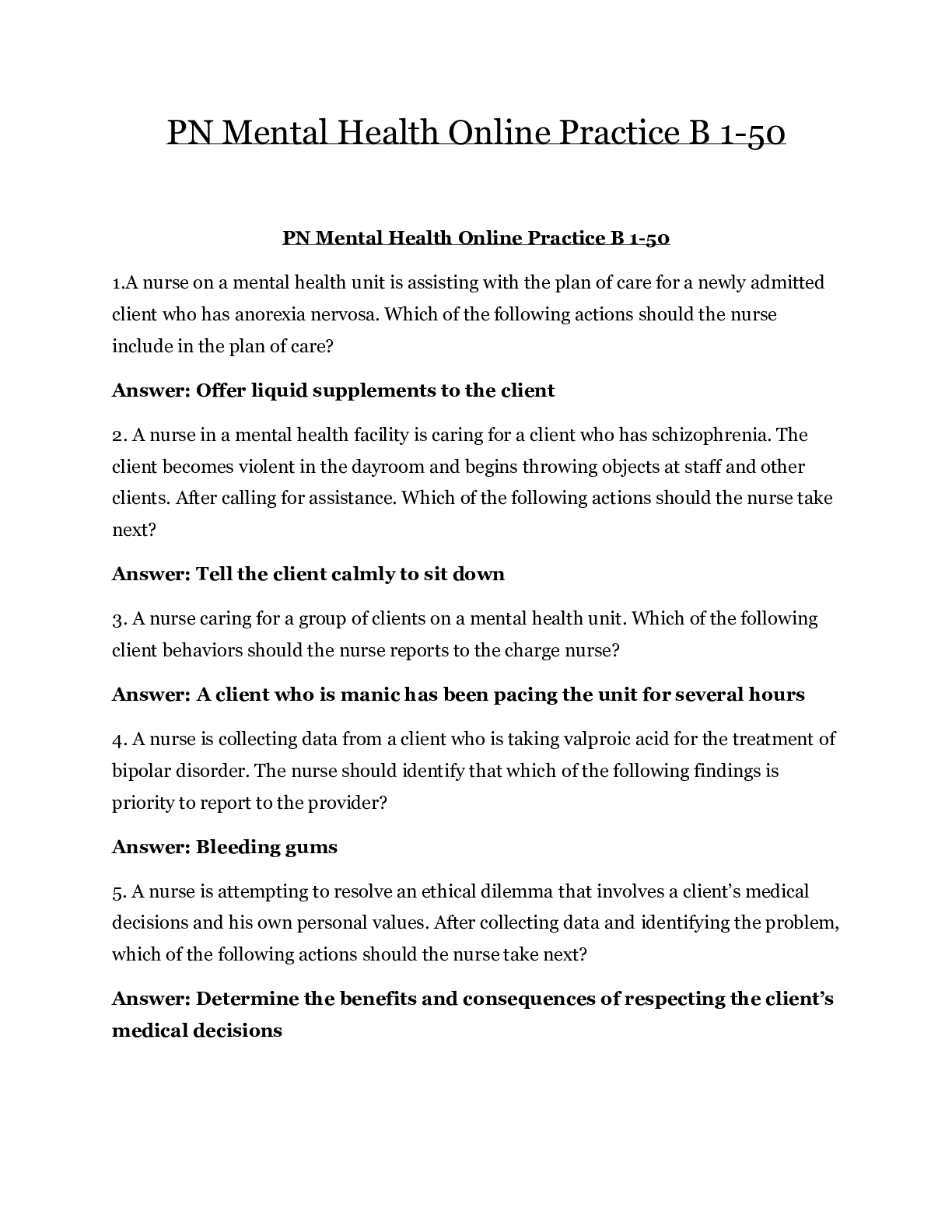
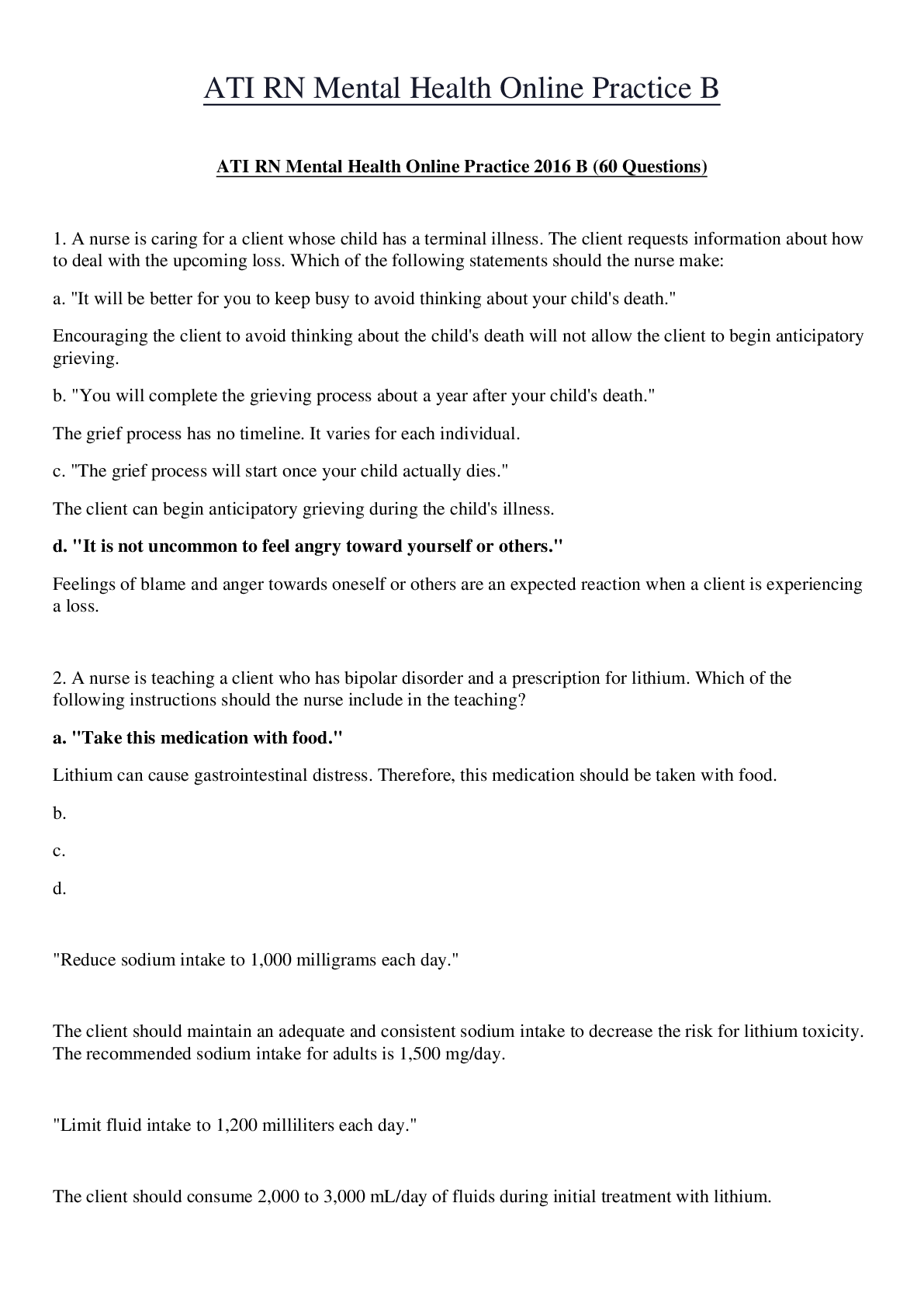
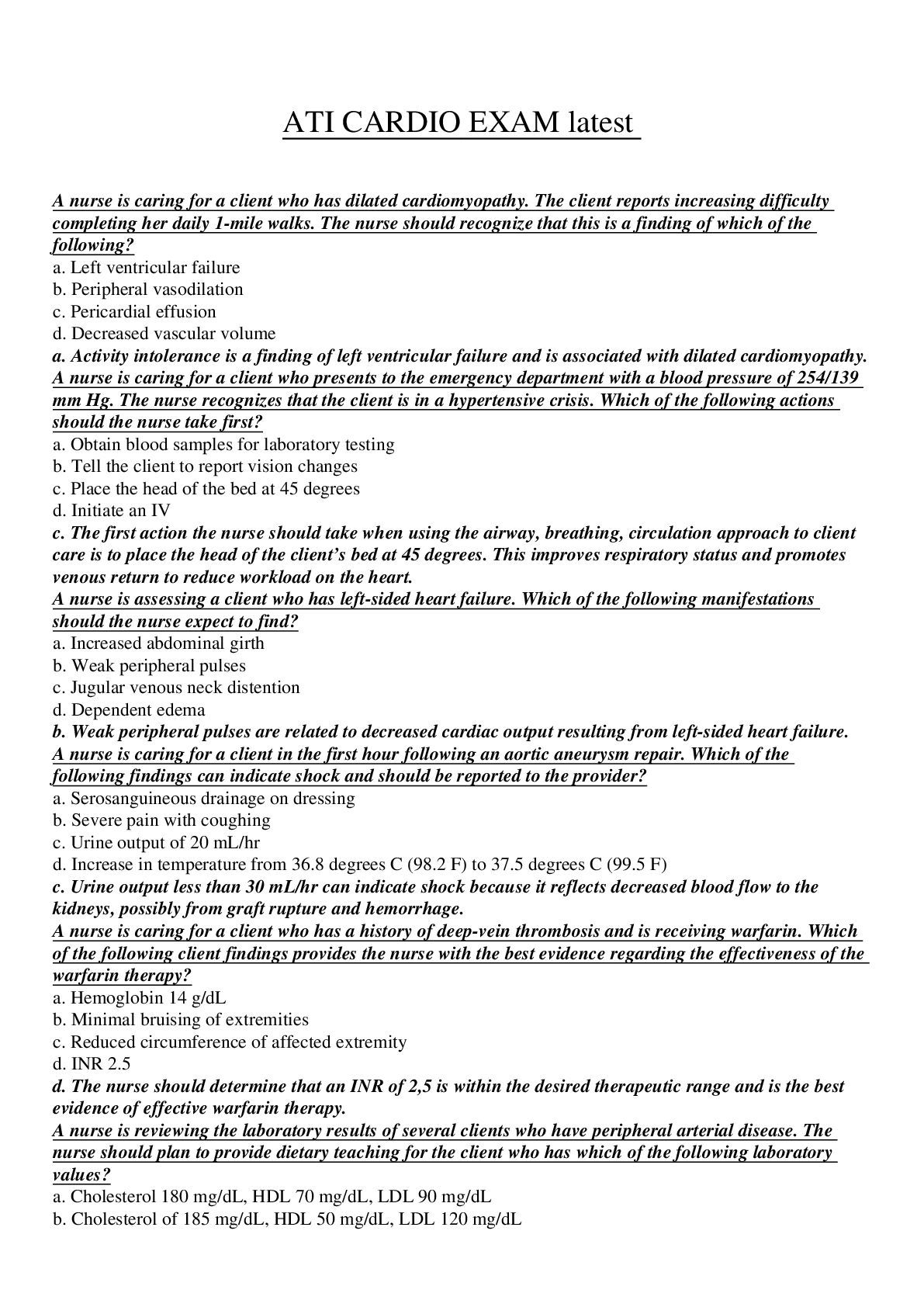
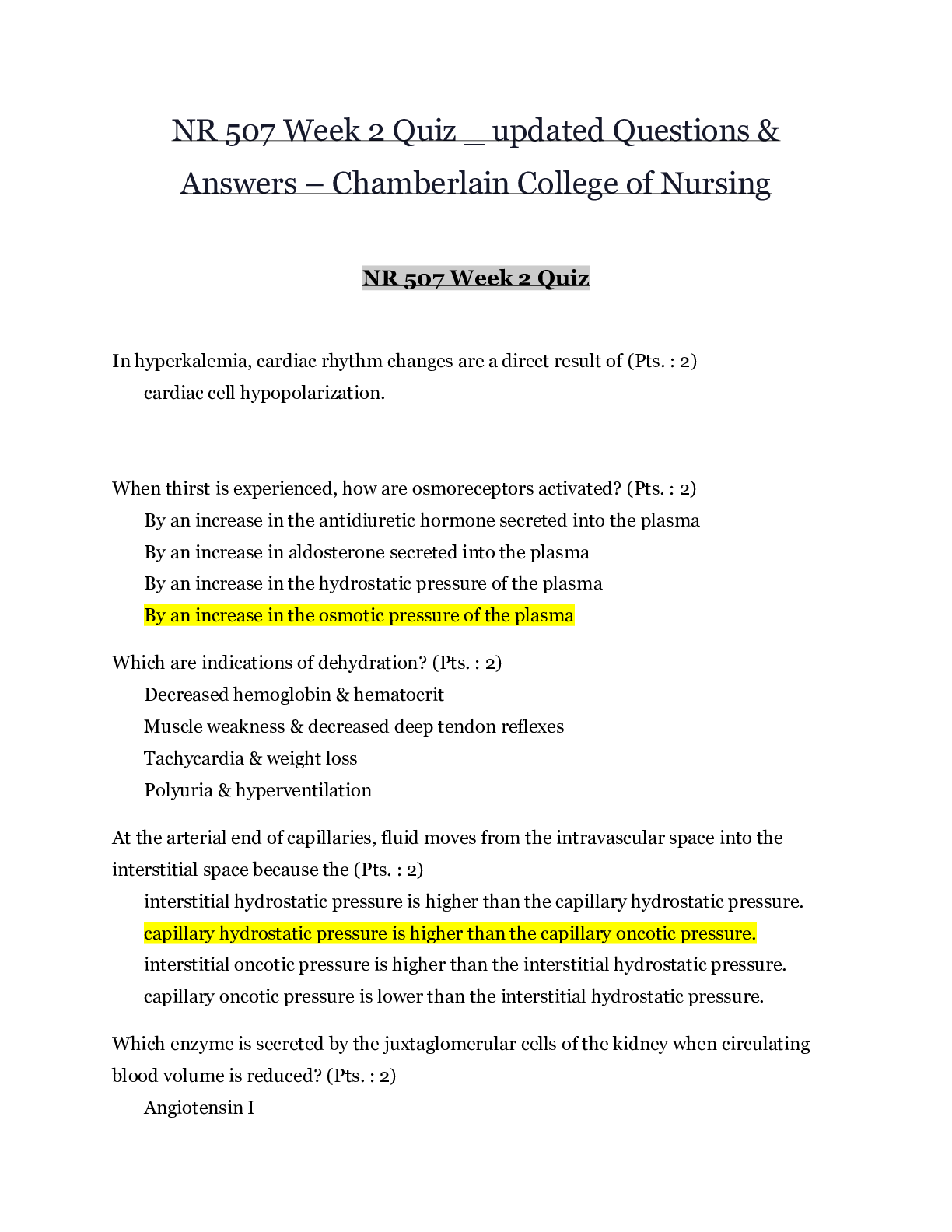
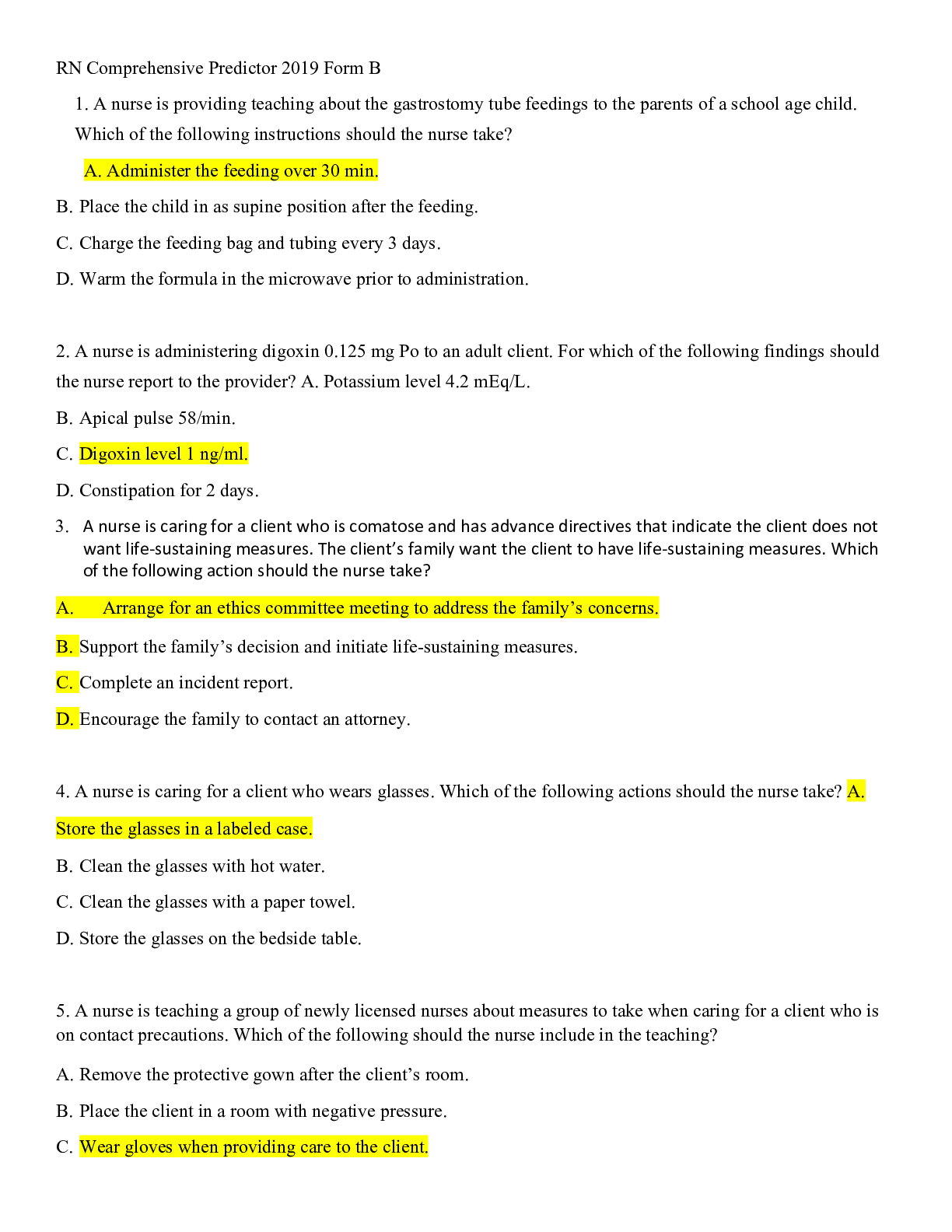

 – CHAMBERLAIN COLLEGE OF NURSING.png)