*NURSING > EXAM > NSG 6005 Chapter 1 test (role of the nurse practitioner) with verified answers – South University (All)
NSG 6005 Chapter 1 test (role of the nurse practitioner) with verified answers – South University (A grade)
Document Content and Description Below
NSG 6005 Chapter 1 test (role of the nurse practitioner) with verified answers – South University (A grade) Chapter 1. The Role of the Nurse Practitioner Multiple Choice Identify the choice t... hat best completes the statement or answers the question. ____ 1. Nurse practitioner prescriptive authority is regulated by: 1. The National Council of State Boards of Nursing 2. The U.S. Drug Enforcement Administration 3. The State Board of Nursing for each state 4. The State Board of Pharmacy ____ 2. The benefits to the patient of having an Advanced Practice Registered Nurse (APRN) prescriber include: 1. Nurses know more about Pharmacology than other prescribers because they take it both in their basic nursing program and in their APRN program. 2. Nurses care for the patient from a holistic approach and include the patient in decision making regarding their care. 3. APRNs are less likely to prescribe narcotics and other controlled substances. 4. APRNs are able to prescribe independently in all states, whereas a physician’s assistant needs to have a physician supervising their practice. ____ 3. Clinical judgment in prescribing includes: 1. Factoring in the cost to the patient of the medication prescribed 2. Always prescribing the newest medication available for the disease process 3. Handing out drug samples to poor patients 4. Prescribing all generic medications to cut costs ____ 4. Criteria for choosing an effective drug for a disorder include: 1. Asking the patient what drug they think would work best for them 2. Consulting nationally recognized guidelines for disease management 3. Prescribing medications that are available as samples before writing a prescription 4. Following U.S. Drug Enforcement Administration guidelines for prescribing ____ 5. Nurse practitioner practice may thrive under health-care reform because of: 1. The demonstrated ability of nurse practitioners to control costs and improve patient outcomes 2. The fact that nurse practitioners will be able to practice independently 3. The fact that nurse practitioners will have full reimbursement under health-care reform 4. The ability to shift accountability for Medicaid to the state level Chapter 2. Review of Basic Principles of Pharmacology Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A patient’s nutritional intake and laboratory results reflect hypoalbuminemia. This is critical to prescribing because: 1. Distribution of drugs to target tissue may be affected. 2. The solubility of the drug will not match the site of absorption. 3. There will be less free drug available to generate an effect. 4. Drugs bound to albumin are readily excreted by the kidneys. ____ 2. Drugs that have a significant first-pass effect: 1. Must be given by the enteral (oral) route only 2. Bypass the hepatic circulation 3. Are rapidly metabolized by the liver and may have little if any desired action 4. Are converted by the liver to more active and fat-soluble forms ____ 3. The route of excretion of a volatile drug will likely be the: 1. Kidneys 2. Lungs 3. Bile and feces 4. Skin ____ 4. Medroxyprogesterone (Depo Provera) is prescribed intramuscularly (IM) to create a storage reservoir of the drug. Storage reservoirs: 1. Assure that the drug will reach its intended target tissue 2. Are the reason for giving loading doses 3. Increase the length of time a drug is available and active 4. Are most common in collagen tissues ____ 5. The NP chooses to give cephalexin every 8 hours based on knowledge of the drug’s: 1. Propensity to go to the target receptor 2. Biological half-life 3. Pharmacodynamics 4. Safety and side effects ____ 6. Azithromycin dosing requires that the first day’s dosage be twice those of the other 4 days of the prescription. This is considered a loading dose. A loading dose: 1. Rapidly achieves drug levels in the therapeutic range 2. Requires four- to five-half-lives to attain 3. Is influenced by renal function 4. Is directly related to the drug circulating to the target tissues ____ 7. The point in time on the drug concentration curve that indicates the first sign of a therapeutic effect is the: 1. Minimum adverse effect level 2. Peak of action 3. Onset of action 4. Therapeutic range ____ 8. Phenytoin requires that a trough level be drawn. Peak and trough levels are done: 1. When the drug has a wide therapeutic range 2. When the drug will be administered for a short time only 3. When there is a high correlation between the dose and saturation of receptor sites 4. To determine if a drug is in the therapeutic range ____ 9. A laboratory result indicates that the peak level for a drug is above the minimum toxic concentration. This means that the: 1. Concentration will produce therapeutic effects 2. Concentration will produce an adverse response 3. Time between doses must be shortened 4. Duration of action of the drug is too long ____ 10. Drugs that are receptor agonists may demonstrate what property? 1. Irreversible binding to the drug receptor site 2. Upregulation with chronic use 3. Desensitization or downregulation with continuous use 4. Inverse relationship between drug concentration and drug action ____ 11. Drugs that are receptor antagonists, such as beta blockers, may cause: 1. Downregulation of the drug receptor 2. An exaggerated response if abruptly discontinued 3. Partial blockade of the effects of agonist drugs 4. An exaggerated response to competitive drug agonists ____ 12. Factors that affect gastric drug absorption include: 1. Liver enzyme activity 2. Protein-binding properties of the drug molecule 3. Lipid solubility of the drug 4. Ability to chew and swallow ____ 13. Drugs administered via IV: 1. Need to be lipid soluble in order to be easily absorbed 2. Begin distribution into the body immediately 3. Are easily absorbed if they are nonionized 4. May use pinocytosis to be absorbed ____ 14. When a medication is added to a regimen for a synergistic effect, the combined effect of the drugs is: 1. The sum of the effects of each drug individually 2. Greater than the sum of the effects of each drug individually 3. Less than the effect of each drug individually 4. Not predictable, as it varies with each individual ____ 15. Which of the following statements about bioavailability is true? 1. Bioavailability issues are especially important for drugs with narrow therapeutic ranges or sustained-release mechanisms. 2. All brands of a drug have the same bioavailability. 3. Drugs that are administered more than once a day have greater bioavailability than drugs given once daily. 4. Combining an active drug with an inert substance does not affect bioavailability. ____ 16. Which of the following statements about the major distribution barriers (blood-brain or fetal-placental) is true? 1. Water soluble and ionized drugs cross these barriers rapidly. 2. The blood-brain barrier slows the entry of many drugs into and from brain cells. 3. The fetal-placental barrier protects the fetus from drugs taken by the mother. 4. Lipid-soluble drugs do not pass these barriers and are safe for pregnant women. ____ 17. Drugs are metabolized mainly by the liver via phase I or phase II reactions. The purpose of both of these types of reactions is to: 1. Inactivate prodrugs before they can be activated by target tissues 2. Change the drugs so they can cross plasma membranes 3. Change drug molecules to a form that an excretory organ can excrete 4. Make these drugs more ionized and polar to facilitate excretion ____ 18. Once they have been metabolized by the liver, the metabolites may be: 1. More active than the parent drug 2. Less active than the parent drug 3. Totally “deactivated” so they are excreted without any effect 4. All of the above ____ 19. All drugs continue to act in the body until they are changed or excreted. The ability of the body to excrete drugs via the renal system would be increased by: 1. Reduced circulation and perfusion of the kidney 2. Chronic renal disease 3. Competition for a transport site by another drug 4. Unbinding a nonvolatile drug from plasma proteins ____ 20. Steady state is: 1. The point on the drug concentration curve when absorption exceeds excretion 2. When the amount of drug in the body remains constant 3. When the amount of drug in the body stays below the minimum toxic concentration 4. All of the above ____ 21. Two different pain medications are given together for pain relief. The drug—drug interaction is: 1. Synergistic 2. Antagonistic 3. Potentiative 4. Additive ____ 22. Actions taken to reduce drug—drug interaction problems include all of the following EXCEPT: 1. Reducing the dosage of one of the drugs 2. Scheduling their administration at different times 3. Prescribing a third drug to counteract the adverse reaction of the combination 4. Reducing the dosage of both drugs ____ 23. Phase I oxidative-reductive processes of drug metabolism require certain nutritional elements. Which of the following would reduce or inhibit this process? 1. Protein malnutrition 2. Iron-deficiency anemia 3. Both 1 and 2 4. Neither 1 nor 2 ____ 24. The time required for the amount of drug in the body to decrease by 50% is called: 1. Steady state 2. Half-life 3. Phase II metabolism 4. Reduced bioavailability time ____ 25. An agonist activates a receptor and stimulates a response. When given frequently over time, the body may: 1. Upregulate the total number of receptors 2. Block the receptor with a partial agonist 3. Alter the drug’s metabolism 4. Downregulate the numbers of that specific receptor ____ 26. Drug antagonism is best defined as an effect of a drug that: 1. Leads to major physiological and psychological dependence 2. Is modified by the concurrent administration of another drug 3. Cannot be metabolized before another dose is administered 4. Leads to a decreased physiological response when combined with another drug ____ 27. Instructions to a client regarding self-administration of oral enteric-coated tablets should include which of the following statements? 1. “Avoid any other oral medicines while taking this drug.” 2. “If swallowing this tablet is difficult, dissolve it in 3 ounces of orange juice.” 3. “The tablet may be crushed if you have any difficulty taking it.” 4. “To achieve best effect, take the tablet with at least 8 ounces of fluid.” ____ 28. The major reason for not crushing a sustained-release capsule is that, if crushed, the coated beads of the drugs could possibly result in: 1. Disintegration 2. Toxicity 3. Malabsorption 4. Deterioration ____ 29. Which of the following substances is the most likely to be absorbed in the intestines rather than in the stomach? 1. Sodium bicarbonate 2. Ascorbic acid 3. Salicylic acid 4. Glucose ____ 30. Which of the following variables is a factor in drug absorption? 1. The smaller the surface area for absorption, the more rapidly the drug is absorbed. 2. A rich blood supply to the area of absorption leads to better absorption. 3. The less soluble the drug, the more easily it is absorbed. 4. Ionized drugs are easily absorbed across the cell membrane. ____ 31. An advantage of prescribing a sublingual medication is that the medication is: 1. Absorbed rapidly 2. Excreted rapidly 3. Metabolized minimally 4. Distributed equally ____ 32. Drugs that use CYP 3A4 isoenzymes for metabolism may: 1. Induce the metabolism of another drug 2. Inhibit the metabolism of another drug 3. Both 1 and 2 4. Neither 1 nor 2 ____ 33. Therapeutic drug levels are drawn when a drug reaches steady state. Drugs reach steady state: 1. After the second dose 2. After four to five half-lives 3. When the patient feels the full effect of the drug 4. One hour after IV administration ____ 34. Upregulation or hypersensitization may lead to: 1. Increased response to a drug 2. Decreased response to a drug 3. An exaggerated response if the drug is withdrawn 4. Refractoriness or complete lack of response Chapter 5. Adverse Drug Reactions Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Which of the following patients would be at higher risk of experiencing adverse drug reactions (ADRs): 1. A 32-year-old male 2. A 22-year-old female 3. A 3-month-old female 4. A 48-year-old male ____ 2. Infants and young children are at higher risk of ADRs due to: 1. Immature renal function in school-age children 2. Lack of safety and efficacy studies in the pediatric population 3. Children’s skin being thicker than adults, requiring higher dosages of topical medication 4. Infant boys having a higher proportion of muscle mass, leading to a higher volume of distribution ____ 3. The elderly are at high risk of ADRs due to: 1. Having greater muscle mass than younger adults, leading to higher volume of distribution 2. The extensive studies that have been conducted on drug safety in this age group 3. The blood-brain barrier being less permeable, requiring higher doses to achieve therapeutic effect 4. Age-related decrease in renal function ____ 4. The type of adverse drug reaction that is idiosyncratic when a drug given in the usual therapeutic doses is type: 1. A 2. B 3. C 4. D ____ 5. Digoxin may cause a type A adverse drug reaction due to: 1. Idiosyncratic effects 2. Its narrow therapeutic index 3. Being a teratogen 4. Being a carcinogen ____ 6. Sarah developed a rash after using a topical medication. This is a type __ allergic drug reaction. 1. I 2. II 3. III 4. IV ____ 7. A patient may develop neutropenia from using topical Silvadene for burns. Neutropenia is a(n): 1. Cytotoxic hypersensitivity reaction 2. Immune complex hypersensitivity 3. Immediate hypersensitivity reaction 4. Delayed hypersensitivity reaction ____ 8. Anaphylactic shock is a: 1. Type I reaction, called immediate hypersensitivity reaction 2. Type II reaction, called cytotoxic hypersensitivity reaction 3. Type III allergic reaction, called immune complex hypersensitivity 4. Type IV allergic reaction, called delayed hypersensitivity reaction ____ 9. James has hypothalamic-pituitary-adrenal axis suppression from chronic prednisone (a corticosteroid) use. He is at risk for what type of adverse drug reaction? 1. Type B 2. Type C 3. Type E 4. Type F ____ 10. Immunomodulators such as azathioprine may cause a delayed adverse drug reaction known as a type D reaction because they are known: 1. Teratogens 2. Carcinogens 3. To cause hypersensitivity reactions 4. Hypothalamus-pituitary-adrenal axis suppressants ____ 11. A 24-year-old male received multiple fractures in a motor vehicle accident that required significant amounts of opioid medication to treat his pain. He is at risk for a _____ adverse drug reaction when he no longer requires the opioids. 1. Rapid 2. First-dose 3. Late 4. Delayed ____ 12. An example of a first-dose reaction that may occur includes: 1. Orthostatic hypotension that does not occur with repeated doses 2. Purple glove syndrome with phenytoin use 3. Hemolytic anemia from ceftriaxone use 4. Contact dermatitis from neomycin use ____ 13. Drugs that are prone to cause adverse drug effects include: 1. Diuretics 2. Inhaled anticholinergics 3. Insulins 4. Stimulants ____ 14. The U.S. Food and Drug Administration MedWatch system is activated when: 1. There is an adverse event to a vaccine. 2. The patient has a severe reaction that is noted in the “Severe Reaction” section in the medication label. 3. A lactating woman takes a medication that is potentially toxic to the breastfeeding infant. 4. An adverse event or serious problem occurs with a medication that is not already identified on the label. ____ 15. The Vaccine Adverse Events Reporting System is: 1. A mandatory reporting system for all health-care providers when they encounter an adverse vaccine event 2. A voluntary reporting system that health-care providers or consumers may use to report vaccine adverse events 3. Utilized to send out safety alerts regarding emerging vaccine safety issues 4. Activated when a vaccine has been proven to cause significant adverse effects Chapter 6. Factors That Foster Positive Outcome Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A comprehensive assessment of a patient should be holistic when trying to determine competence in drug administration. Which of the following factors would the NP omit from this type of assessment? 1. Financial status 2. Mobility 3. Social support 4. Sexual practices ____ 2. Elena Vasquez’s primary language is Spanish, and she speaks very limited English. Which technique would be appropriate to use in teaching her about a new drug you have just prescribed? 1. Use correct medical terminology because Spanish has a Latin base. 2. Use a family member who speaks more English to act as an interpreter. 3. Use a professional interpreter or a reliable staff member who can act as an interpreter. 4. Use careful, detailed explanations. ____ 3. Rod, age 68, has hearing difficulty. Which of the following would NOT be helpful in assuring that he understands teaching about his drug? 1. Stand facing him and speak slowly and clearly. 2. Speak in low tones or find a provider who has a lower voice. 3. Write down the instructions as well as speaking them. 4. If he reads lips, exaggerate lips movements when pronouncing the vowel sounds. ____ 4. Which of the following factors may adversely affect a patient’s adherence to a therapeutic drug regimen? 1. Complexity of the drug regimen 2. Patient perception of the potential adverse effects of the drugs 3. Both 1 and 2 4. Neither 1 nor 2 ____ 5. The health-care delivery system itself can create barriers to adherence to a treatment regimen. Which of the following system variables creates such a barrier? 1. Increasing copayments for care 2. Unrestricted formularies for drugs, including brand names 3. Increasing the number of people who have access to care 4. Treating a wider range of disorders ____ 6. Ralph’s blood pressure remains elevated despite increased doses of his drug. The NP is concerned that he might not be adhering to his treatment regimen. Which of the following events would suggest that he might not be adherent? 1. Ralph states that he always takes the drug “when I feel my pressure is going up.” 2. Ralph contacts his NP to discuss the need to increase the dosage. 3. Ralph consistently keeps his follow-up appointments to check his blood pressure. 4. All of the above show that he is adherent to the drug regimen. ____ 7. Nonadherence is especially common in drugs that treat asymptomatic conditions, such as hypertension. One way to reduce the likelihood of nonadherence to these drugs is to prescribe a drug that: 1. Has a short half-life so that missing one dose has limited effect 2. Requires several dosage titrations so that missed doses can be replaced with lower doses to keep costs down 3. Has a tolerability profile with fewer of the adverse effects that are considered “irritating,” such as nausea and dizziness 4. Must be taken no more than twice a day ____ 8. Factors in chronic conditions that contribute to nonadherence include: 1. The complexity of the treatment regimen 2. The length of time over which it must be taken 3. Breaks in the usual daily routine, such as vacations and weekends 4. All of the above ____ 9. While patient education about their drugs is important, information alone does not necessarily lead to adherence to a drug regimen. Patients report greater adherence when: 1. The provider spent a lot of time discussing the drugs with them 2. Their concerns and specific area of knowledge deficit were addressed 3. They were given written material, such as pamphlets, about the drugs 4. The provider used appropriate medical and pharmacological terms ____ 10. Patients with psychiatric illnesses have adherence rates to their drug regimen between 35% and 60%. To improve adherence in this population, prescribe drugs: 1. With a longer half-life so that missed doses produce a longer taper on the drug curve 2. In oral formulations that are more easily taken 3. That do not require frequent monitoring 4. Combined with patient education about the need to adhere even when symptoms are absent ____ 11. Many disorders require multiple drugs to treat them. The more complex the drug regimen, the less likely the patient will adhere to it. Which of the following interventions will NOT improve adherence? 1. Have the patient purchase a pill container with compartments for daily or multiple times-per-day dosing. 2. Match the clinic appointment to the next time the drug is to be refilled. 3. Write prescriptions for new drugs with shorter times between refills. 4. Give the patient a clear drug schedule that the provider devises to fit the characteristic of the drug. ____ 12. Pharmacologic interventions are costly. Patients for whom the cost/benefit variable is especially important include: 1. Older adults and those on fixed incomes 2. Patients with chronic illnesses 3. Patients with copayments for drugs on their insurance 4. Patients on public assistance ____ 13. Providers have a responsibility for determining the best plan of care, but patients also have responsibilities. Patients the provider can be assured will carry through on these responsibilities include those who: 1. Are well-educated and affluent 2. Have chronic conditions 3. Self-monitor drug effects on their symptoms 4. None of the above guarantee adherence ____ 14. Monitoring adherence can take several forms, including: 1. Patient reports from data in a drug diary 2. Pill counts 3. Laboratory reports and other diagnostic markers 4. All of the above ____ 15. Factors that explain and predict medication adherence include: 1. Social 2. Financial 3. Health system 4. All of the above Chapter 7. Cultural and Ethnic Influences in Pharmacotherapeutics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Cultural factors that must be taken into account when prescribing include(s): 1. Who the decision maker is in the family regarding health-care decisions 2. The patient’s view of health and illness 3. Attitudes regarding the use of drugs to treat illness 4. All of the above ____ 2. Ethnic differences have been found in drug: 1. Absorption 2. Hepatic metabolism 3. Filtration at the glomerulus 4. Passive tubular reabsorption ____ 3. The National Standards of Culturally and Linguistically Appropriate Services are required to be implemented in all: 1. Hospitals 2. Clinics that serve the poor 3. Organizations that receive federal funds 4. Clinics that serve ethnic minorities ____ 4. According to the National Standards of Culturally and Linguistically Appropriate Services, an interpreter for health care: 1. May be a bilingual family member 2. May be a bilingual nurse or other health-care provider 3. Must be a professionally trained medical interpreter 4. Must be an employee of the organization ____ 5. According to the U.S. Office of Minority Health, poor health outcomes among African Americans are attributed to: 1. The belief among African Americans that prayer is more powerful than drugs 2. Poor compliance on the part of the African American patient 3. The genetic predisposition for illness found among African Americans 4. Discrimination, cultural barriers, and lack of access to health care ____ 6. The racial difference in drug pharmacokinetics seen in American Indian or Alaskan Natives are: 1. Increased CYP 2D6 activity, leading to rapid metabolism of some drugs 2. Largely unknown due to lack of studies of this population 3. Rapid metabolism of alcohol, leading to increased tolerance 4. Decreased elimination of opioids, leading to increased risk for addiction ____ 7. Pharmacokinetics among Asians are universal to all the Asian ethnic groups. 1. True 2. False ____ 8. Alterations in drug metabolism among Asians may lead to: 1. Slower metabolism of antidepressants, requiring lower doses 2. Faster metabolism of neuroleptics, requiring higher doses 3. Altered metabolism of omeprazole, requiring higher doses 4. Slower metabolism of alcohol, requiring higher doses ____ 9. Asians from Eastern Asia are known to be fast acetylators. Fast acetylators: 1. Require acetylization in order to metabolize drugs 2. Are unable to tolerate higher doses of some drugs that require acetylization 3. May have a toxic reaction to drugs that require acetylization 4. Require higher doses of drugs metabolized by acetylization to achieve efficacy ____ 10. Hispanic native healers (curanderas): 1. Are not heavily utilized by Hispanics who immigrate to the United States 2. Use herbs and teas in their treatment of illness 3. Provide unsafe advice to Hispanics and should not be trusted 4. Need to be licensed in their home country in order to practice in the United States Chapter 10. Herbal Therapy and Nutritional Supplements Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. A good history of herb and supplement use is critical before prescribing because approximately ____ % of patients in the United States are using herbal products. 1. 10 2. 5 3. 38 4. 70 ____ 2. A potential harmful effect on patients who take some herbal medication is: 1. Constipation 2. Lead poisoning 3. Diarrhea 4. Life-threatening rash ____ 3. A thorough understanding of herbs is critical to patient safety. An example is the use of cinnamon to treat type II diabetes. It is important the patient uses Ceylon cinnamon, as the commercially available cassia cinnamon contains: 1. Coumadin, which may lead to bleeding problems 2. Coumarin, which can cause liver and kidney damage 3. Cinnamic aldehyde, which is toxic to the kidney 4. Cinnamate eugenol, which is toxic to the liver ____ 4. Traditional Chinese medicine utilizes yin (cooling) versus yang (warming) in assessing and treating disease. Menopause is considered a time of imbalance, therefore the Chinese herbalist would prescribe: 1. Herbs which are yang in nature 2. Herbs that are yin in nature 3. Ginger 4. Golden seal ____ 5. According to traditional Chinese medicine, if a person who has a fever is given a herb that is yang in nature, such as golden seal, the patient’s illness will: 1. Get worse 2. Get better 3. Not be adequately treated 4. Need additional herbs to treat the yang ____ 6. In Ayurvedic medicine, treatment is based on the patient’s dominant dosha, which is referred to as the person’s: 1. Vata 2. Pitta 3. Kapha 4. Prakriti ____ 7. Herbs and supplements are regulated by the U.S. Food and Drug Administration. 1. True 2. False ____ 8. When melatonin is used to induce sleep, the recommendation is that the patient: 1. Take 10 mg 30 minutes before bed nightly 2. Take 1 to 5 mg 30 minutes before bed nightly 3. Not take melatonin more than three nights a week 4. Combine melatonin with zolpidem (Ambien) for the greatest impact on sleep ____ 9. Valerian tea causes relaxation and can be used to help a patient fall asleep. Overdosage of valerian (more than 2.5 gm/dose) may lead to: 1. Cardiac disturbances 2. Central nervous system depression 3. Respiratory depression 4. Skin rashes ____ 10. The standard dosage of St John’s wort for the treatment of mild depression is: 1. 300 mg daily 2. 100 mg three times a day 3. 300 mg three times a day 4. 600 mg three times a day ____ 11. Patients need to be instructed regarding the drug interactions with St John’s wort, including: 1. MAO inhibitors 2. Serotonin reuptake inhibitors 3. Over-the-counter cough and cold medications 4. All of the above ____ 12. Ginseng, which is taken to assist with memory, may potentiate: 1. Aricept 2. Insulin 3. Digoxin 4. Propranolol ____ 13. Licorice root is a common treatment for dyspepsia. Drug interactions with licorice include: 1. Antihypertensives, diuretics, and digoxin 2. Antidiarrheals, antihistamines, and omeprazole 3. Penicillin antibiotic class and benzodiazepines 4. None of the above ____ 14. Patients should be warned about the overuse of topical wintergreen oil to treat muscle strains, as overapplication can lead to: 1. Respiratory depression 2. Cardiac disturbance 3. Salicylates poisoning 4. Life-threatening rashes ____ 15. The role of the NP in the use of herbal medication is to: 1. Maintain competence in the prescribing of common herbal remedies 2. Recommend common over-the-counter herbs to patients 3. Educate patients and guide them to appropriate sources of care 4. Encourage patients to not use herbal therapy due to the documented dangers Chapter 12. Pharmacoeconomics Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Pharmacoeconomics is: 1. The study of the part of the U.S. economy devoted to drug use 2. The study of the impact of prescription drug costs on the overall economy 3. The analysis of the costs and consequences of any health-care-related treatment or service 4. The analysis of the clinical efficacy of the drug ____ 2. The direct costs of drug therapy include: 1. The actual cost of acquiring the medication 2. The loss of income due to illness 3. Pain and suffering due to inadequate drug therapy 4. The cost of a funeral associated with premature death ____ 3. Indirect costs associated with drug therapy include: 1. The cost of diagnostic tests to monitor therapeutic levels 2. Health-care provider time to prescribe and educate the patient 3. Child-care expenses incurred while receiving therapy 4. Loss of wages while undergoing drug therapy ____ 4. The intangible costs of drug therapy include: 1. Loss of wages while undergoing therapy 2. Inconvenience, pain, and suffering incurred with therapy 3. Cost of medical equipment in the laboratory used to monitor therapeutic drug levels 4. Cost of prescription drug coverage, such as Medicare Part D ____ 5. When a pharmacoeconomic analysis looks at two or more treatment alternatives that are considered equal in efficacy and compares the costs of each it is referred to as: 1. Cost-minimization analysis 2. Cost-of-illness analysis 3. Cost-effectiveness analysis 4. Cost-benefit analysis ____ 6. Cost-effectiveness analysis compares two or more treatments or programs that are: 1. Not necessarily therapeutically equivalent 2. Considered equal in efficacy 3. Compared with the dollar value of the benefit received 4. Expressed in terms of patient preference or quality-adjusted life years ____ 7. When the costs of a specific treatment or intervention are calculated and then compared with the dollar value of the benefit received it is referred to as: 1. Cost-minimization analysis 2. Cost-of-illness analysis 3. Cost-effectiveness analysis 4. Cost-benefit analysis ____ 8. Mary has a two-tiered prescription benefit plan, which means: 1. She can receive differing levels of care based on whether she chooses an “in-plan” provider or not. 2. She is eligible for the new Medicare Part D “donut hole” reduction of costs program. 3. She pays a higher copay for brand-name drugs than for generic drugs. 4. She must always choose to be treated with generic drugs first. ____ 9. Prescribing less-expensive generic drugs or drugs off the $4 retail pharmacy lists: 1. Increases the complexity of the pharmacoeconomics of prescribing for the individual patient 2. Increases compliance by reducing the financial burden of drug costs to the patient 3. Is not sound prescribing practice due to the inferiority of the generic products 4. Will increase the overall cost of drugs to the system due to the ease of overprescribing less-expensive drugs ____ 10. James tells you that he is confused by his Medicare Part D coverage plan. An appropriate intervention would be: 1. Order cognitive testing to determine the source of his confusion. 2. Sit down with him and explain the whole Medicare Part D process. 3. Refer him to the Medicare specialist in his insurance plan to explain the benefit to him. 4. Request his son come to the next appointment so you can explain the benefit to him. ____ 11. The “donut hole” in Medicare Part D: 1. Will be totally eliminated with the federal health-care reform enacted in 2010 2. Refers to the period of time when annual individual drug costs are between $250 and $2,250 per year and drug costs are covered 75% 3. Refers to the period between when the annual individual drug costs are $2,970 and $4,750 and the patient pays 52.5% of the costs of brand name drugs (2013) 4. Has no effect on whether patients continue to fill their prescriptions during the coverage gap ____ 12. Research has shown that when patients who are covered by Medicare Part D reach the “donut hole” in coverage they: 1. Ask for extra refills of medication to get them through the months of no coverage 2. Fill their prescriptions less frequently, including critical medications such as warfarin or a statin 3. Fill their critical medications, but hold off on filling less-critical medications 4. Demonstrate no change in their prescription filling pattern Chapter 13. Over-the-Counter Medications Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Michael asks you about why some drugs are over-the-counter and some are prescription. You explain that in order for a drug to be approved for over-the-counter use the drug must: 1. Be safe and labeled for appropriate use 2. Have a low potential for abuse or misuse 3. Be taken for a condition the patient can reliably self-diagnose 4. All of the above ____ 2. In the United States, over-the-counter drugs are regulated by: 1. No one. There is no oversight for over-the-counter medications. 2. The U.S. Food and Drug Administration Center for Drug Evaluation and Research 3. The U.S. Drug Enforcement Administration 4. MedWatch ____ 3. As drugs near the end of their patent, pharmaceutical companies may apply for the drug to change to over-the-counter status in order to: 1. Get a new patent for the over-the-counter form of the drug 2. Lower the costs because most prescription benefit plans do not cover generics 3. Market the drug to a whole new population, as they are able to market to patients instead of just providers 4. Continue to make large profits from their blockbuster brand-name drug ____ 4. New over-the-counter drug ingredients must undergo the U.S. Food and Drug Administration New Drug Application process, just as prescription drugs do. 1. True 2. False ____ 5. The ailment that generates the greatest over-the-counter annual drug sales is: 1. Constipation 2. Cough and colds 3. Heartburn 4. Acute and chronic pain ____ 6. Common over-the-counter pain relievers such as acetaminophen or ibuprofen: 1. Are always safer for the patient than prescription pain medication 2. Are harmful if taken in higher than recommended amounts 3. Have minimal interaction with prescription medications 4. Should never be given to children unless recommended by their provider ____ 7. When obtaining a drug history from Harold, he gives you a complete list of his prescription medications. He denies taking any other drugs, but you find that he occasionally takes aspirin for his arthritis flare ups. This is an example of: 1. His appropriately only telling you about his regularly prescribed medications 2. His hiding information regarding his inappropriate use of aspirin from you 3. A common misconception that intermittently taken over-the counter medications are not an important part of his drug history 4. A common misuse of over-the-counter aspirin ____ 8. The Combat Methamphetamine Epidemic Act, which is part of the 2006 U.S. Patriot Act: 1. Requires all providers to screen their patients for methamphetamine use 2. Restricts the prescribing of amphetamines to U.S. citizens 3. Requires a prescription be written for all methamphetamine precursors in all states 4. Restricts the sales of drugs that contain methamphetamine precursors, including a daily and 30-day limit on sales ____ 9. When prescribing a tetracycline or quinolone antibiotic it is critical to instruct the patient: 1. Not to take their regularly prescribed medications while on these antibiotics 2. Regarding the need for lots of acidic foods and juices, such as orange juice, to enhance absorption 3. Not to take antacids while on these medications, as the antacid decreases absorption 4. That there are no drug interactions with these antibiotics Chapter 15. Drugs Affecting the Central Nervous System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Sarah, a 42-year-old female, requests a prescription for an anorexiant to treat her obesity. A trial of phentermine is prescribed. Prescribing precautions include: 1. Understanding that obesity is a contraindication to prescribing phentermine 2. Anorexiants may cause tolerance and should only be prescribed for 6 months 3. Patients should be monitored for postural hypotension 4. Renal function should be monitored closely while on anorexiants ____ 2. Before prescribing phentermine to Sarah, a thorough drug history should be taken including assessing for the use of serotonergic agents such as selective serotonin reuptake inhibitors (SSRIs) and St John’s wort due to: 1. Additive respiratory depression risk 2. Additive effects affecting liver function 3. The risk of serotonin syndrome 4. The risk of altered cognitive functioning ____ 3. Antonia is a 3-year-old child who has a history of status epilepticus. Along with her routine antiseizure medication, she should also have a home prescription for_________ to be used for an episode of status epilepticus. 1. IV phenobarbital 2. Rectal diazepam (Diastat) 3. IV phenytoin (Dilantin) 4. Oral carbamazepine (Tegretol) ____ 4. Rabi is being prescribed phenytoin for seizures. Monitoring includes assessing: 1. For phenytoin hypersensitivity syndrome 3 to 8 weeks after starting treatment 2. For pedal edema throughout therapy 3. Heart rate at each visit and consider altering therapy if heart rate is less than 60 bpm 4. For vision changes, such as red-green blindness, at least annually ____ 5. Dwayne has recently started on carbamazepine to treat seizures. He comes to see you and you note that while his carbamazepine levels had been in the therapeutic range, they are now low. The possible cause for the low carbamazepine levels include: 1. Dwayne hasn’t been taking his carbamazepine because it causes insomnia. 2. Carbamazepine auto-induces metabolism, leading to lower levels in spite of good compliance. 3. Dwayne was not originally prescribed the correct amount of carbamazepine. 4. Carbamazepine is probably not the right antiseizure medication for Dwayne. ____ 6. Carbamazepine has a Black Box Warning due to life-threatening: 1. Renal toxicity, leading to renal failure 2. Hepatotoxicity, leading to liver failure 3. Dermatologic reaction, including Steven’s Johnson and toxic epidermal necrolysis 4. Cardiac effects, including supraventricular tachycardia ____ 7. Long-term monitoring of patients who are taking carbamazepine includes: 1. Routine troponin levels to assess for cardiac damage 2. Annual eye examinations to assess for cataract development 3. Monthly pregnancy tests for all women of childbearing age 4. Complete blood count every 3 to 4 months ____ 8. Six-year-old Lucy has recently been started on ethosuximide (Zarontin) for seizures. She should be monitored for: 1. Increased seizure activity, as this drug may auto-induce seizures 2. Altered renal function, including renal failure 3. Blood dyscrasias, which are uncommon but possible 4. Central nervous system excitement, leading to insomnia ____ 9. Sook has been prescribed gabapentin to treat neuropathic pain and is complaining of feeling depressed and having “strange” thoughts. The appropriate initial action would be: 1. Increase her dose 2. Assess for suicidal ideation 3. Discontinue the medication immediately 4. Decrease her dose to half then slowly titrate up the dose ____ 10. Selma, who is overweight, recently started taking topiramate for seizures and at her follow-up visit you note she has lost 3 kg. The appropriate action would be: 1. Tell her to increase her caloric intake to counter the effects of the topiramate. 2. Consult with a neurologist, as this is not a common adverse effect of topiramate. 3. Decrease her dose of topiramate. 4. Reassure her that this is a normal side effect of topiramate and continue to monitor her weight. ____ 11. Monitoring of a patient on gabapentin to treat seizures includes: 1. Routine therapeutic drug levels every 3 to 4 months 2. Assessing for dermatologic reactions, including Steven’s Johnson 3. Routine serum electrolytes, especially in hot weather 4. Recording seizure frequency, duration, and severity ____ 12. Scott’s seizures are well controlled on topiramate and he wants to start playing baseball. Education for Scott regarding his topiramate includes: 1. He should not play sports due to the risk of increased seizures 2. He should monitor his temperature and ability to sweat in the heat while playing 3. Reminding him that he may need higher dosages of topiramate when exercising 4. Encouraging him to use sunscreen due to photosensitivity from topiramate ____ 13. Cara is taking levetiracetam (Keppra) to treat seizures. Routine education for levetiracetam includes reminding her: 1. To not abruptly discontinue levetiracetam due to risk for withdrawal seizures 2. To wear sunscreen due to photosensitivity from levetiracetam 3. To get an annual eye exam while on levetiracetam 4. To report weight loss if it occurs ____ 14. Levetiracetam has known drug interactions with: 1. Combined oral contraceptives 2. Carbamazepine 3. Warfarin 4. Few, if any, drugs ____ 15. Zainab is taking lamotrigine (Lamictal) and presents to the clinic with fever and lymphadenopathy. Initial evaluation and treatment includes: 1. Reassuring her she has a viral infection and to call if she isn’t better in 4 or 5 days 2. Ruling out a hypersensitivity reaction that may lead to multi-organ failure 3. Rapid strep test and symptomatic care if strep test is negative 4. Observation only, with further assessment if she worsens ____ 16. Samantha is taking lamotrigine (Lamictal) for her seizures and requests a prescription for combined oral contraceptives (COCs), which interact with lamotrigine and may cause: 1. Contraceptive failure 2. Excessive weight gain 3. Reduced lamotrigine levels, requiring doubling the dose of lamotrigine 4. Induction of estrogen metabolism, requiring higher estrogen content OCs be prescribed ____ 17. The tricyclic antidepressants should be prescribed cautiously in patients with: 1. Eczema 2. Asthma 3. Diabetes 4. Heart disease ____ 18. A 66-year-old male was prescribed phenelzine (Nardil) while in an acute psychiatric unit for recalcitrant depression. The NP managing his primary health care needs to understand the following regarding phenelzine and other monoamine oxidase inhibitors (MAOIs): 1. He should not be prescribed any serotonergic drug such as sumatriptan (Imitrex) 2. MAOIs interact with many common foods, including yogurt, sour cream, and soy sauce 3. Symptoms of hypertensive crisis (headache, tachycardia, sweating) require immediate treatment 4. All of the above ____ 19. Taylor is a 10-year-old child diagnosed with major depression. The appropriate first-line antidepressant for children is: 1. Fluoxetine 2. Fluvoxamine 3. Sertraline 4. Escitalopram ____ 20. Suzanne is started on paroxetine (Paxil), a selective serotonin reuptake inhibitor (SSRI), for depression. Education regarding her antidepressant includes: 1. SSRIs may take 2 to 6 weeks before she will have maximum drug effects. 2. Red-green color blindness may occur and should be reported. 3. If she experiences dry mouth or heart rates greater than 80, she should stop taking the drug immediately. 4. She should eat lots of food high in fiber to prevent constipation. ____ 21. Cecilia presents with depression associated with complaints of fatigue, sleeping all the time, and lack of motivation. An appropriate initial antidepressant for her would be: 1. Fluoxetine (Prozac) 2. Paroxetine (Paxil) 3. Amitriptyline (Elavil) 4. Duloxetine (Cymbalta) ____ 22. Jake, a 45-year-old patient with schizophrenia, was recently hospitalized for acute psychosis due to medication noncompliance. He was treated with IM long-acting haloperidol. Besides monitoring his schizophrenia symptoms, the patient should be assessed by his primary care provider: 1. For excessive weight loss 2. With the Abnormal Involuntary Movement Scale (AIMS) for extrapyramidal symptoms (EPS) 3. Monthly for tolerance to the haloperidol 4. Only by the mental health provider, as most NPs in primary care do not care for mentally ill patients ____ 23. Anticholinergic agents, such as benztropine (Cogentin), may be given with a phenothiazine to: 1. Reduce the chance of tardive dyskinesia 2. Potentiate the effects of the drug 3. Reduce the tolerance that tends to occur 4. Increase central nervous system (CNS) depression ____ 24. Patients who are prescribed olanzapine (Zyprexa) should be monitored for: 1. Insomnia 2. Weight gain 3. Hypertension 4. Galactorrhea ____ 25. A 19-year-old male was started on risperidone. Monitoring for risperidone includes observing for common side effects, including: 1. Bradykinesia, akathisia, and agitation 2. Excessive weight gain 3. Hypertension 4. Potentially fatal agranulocytosis ____ 26. In choosing a benzodiazepam to treat anxiety the prescriber needs to be aware of the possibility of dependence. The benzodiazepam with the greatest likelihood of rapidly developing dependence is: 1. Chlordiazepoxide (Librium) 2. Clonazepam (Klonopin) 3. Alprazolam (Xanax) 4. Oxazepam (Serax) ____ 27. A patient with anxiety and depression may respond to: 1. Duloxetine (Cymbalta) 2. Fluoxetine (Prozac) 3. Oxazepam (Serax) 4. Buspirone (Buspar) and an SSRI combined ____ 28. When prescribing temazepam (Restoril) for insomnia, patient education includes: 1. Take temazepam nightly approximately 15 minutes before bedtime. 2. Temazepam should not be used more than three times a week for less than 3 months. 3. Drinking 1 ounce of alcohol will cause additive effects and the patient will sleep better. 4. Exercise for at least 30 minutes within 2 hours of bedtime to enhance the effects of temazepam. ____ 29. Patients should be instructed regarding the rapid onset of zolpidem (Ambien) because: 1. Zolpidem should be taken just before going to bed. 2. Zolpidem may cause dry mouth and constipation. 3. Patients may need to double the dose for effectiveness. 4. They should stop drinking alcohol at least 30 minutes before taking zolpidem. ____ 30. One major drug used to treat bipolar disease is lithium. Because lithium has a narrow therapeutic range, it is important to recognize symptoms of toxicity, such as: 1. Orthostatic hypotension 2. Agitation and irritability 3. Drowsiness and nausea 4. Painful urination and abdominal distention ____ 31. Tom is taking lithium for bipolar disorder. He should be taught to: 1. Take his lithium with food 2. Eat a diet with consistent levels of salt (sodium) 3. Drink at least 2 quarts of water if he is in a hot environment 4. Monitor blood glucose levels ____ 32. Cynthia is taking valproate (Depakote) for seizures and would like to get pregnant. What advice would you give her? 1. Valproate is safe during all trimesters of pregnancy. 2. She can get pregnant while taking valproate, but she should take adequate folic acid. 3. Valproate is not safe at any time during pregnancy. 4. Valproate is a known teratogen, but may be taken after the first trimester if necessary. ____ 33. When prescribing an opioid analgesic such as acetaminophen and codeine (Tylenol #3), instructions to the patient should include: 1. The medication may cause sedation and they should not drive. 2. Constipation is a common side effect and they should increase fluids and fiber. 3. Patients should not take any other acetaminophen-containing medications at the same time. 4. All of the above ____ 34. Kirk sprained his ankle and is asking for pain medication for his mild-to-moderate pain. The appropriate first-line medication would be: 1. Ibuprofen (Advil) 2. Acetaminophen with hydrocodone (Vicodin) 3. Oxycodone (Oxycontin) 4. Oral morphine (Roxanol) ____ 35. Kasey fractured his ankle in two places and is asking for medication for his pain. The appropriate first-line medication would be: 1. Ibuprofen (Advil) 2. Acetaminophen with hydrocodone (Vicodin) 3. Oxycodone (Oxycontin) 4. Oral morphine (Roxanol) ____ 36. Jack, age 8, has attention deficit disorder (ADD) and is prescribed methylphenidate (Ritalin). He and his parents should be educated about the side effects of methylphenidate, which are: 1. Slurred speech and insomnia 2. Bradycardia and confusion 3. Dizziness and orthostatic hypotension 4. Insomnia and decreased appetite ____ 37. Monitoring for a child on methylphenidate for attention deficit hyperactivity disorder (ADHD) includes: 1. ADHD symptoms 2. Routine height and weight checks 3. Amount of methylphenidate being used 4. All of the above ____ 38. When prescribing Adderall (amphetamine and dextroamphetamine) to adults with ADHD the nurse practitioner will need to monitor: 1. Blood pressure 2. Blood glucose levels 3. Urine ketone levels 4. Liver function Chapter 16. Drugs Affecting the Cardiovascular and Renal Systems Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Ray has been diagnosed with hypertension and an angiotensin-converting enzyme inhibitor is determined to be needed. Prior to prescribing this drug, the NP should assess for: 1. Hypokalemia 2. Impotence 3. Decreased renal function 4. Inability to concentrate ____ 2. Angiotensin-converting enzyme inhibitors are the drug of choice in treating hypertension in diabetic patients because they: 1. Improve insulin sensitivity 2. Improve renal hemodynamics 3. Reduce the production of angiotensin II 4. All of the above ____ 3. A potentially life-threatening adverse response to angiotensin-converting enzyme inhibitors is angioedema. Which of the following statements is true about this adverse response? 1. Swelling of the tongue or hoarseness are the most common symptoms. 2. It appears to be related to the decrease in aldosterone production. 3. Presence of a dry, hacky cough indicates a high risk for this adverse response. 4. Because it takes time to build up a blood level, it occurs after being on the drug for about 1 week. ____ 4. Angiotensin-converting enzyme inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use? 1. Stable angina because it decreases the thickening of vascular walls due to decreased modified release. 2. Heart failure because it reduces remodeling of injured myocardial tissues. 3. Both 1 and 2 are true and the reasons are correct. 4. Both 1 and 2 are true but the reasons are wrong. 5. Neither 1 nor 2 are true. ____ 5. Despite good blood pressure control, an NP might change a patient’s drug from an angiotensin-converting enzyme (ACE) inhibitor to an angiotensin II receptor blocker (ARB) because the ARB: 1. Is stronger than the ACE inhibitor 2. Does not produce a dry, hacky cough 3. Has no effect on the renal system 4. Reduces sodium and water retention ____ 6. While taking an angiotensin II receptor blocker (ARB), patients need to avoid certain over-the-counter drugs without first consulting the provider because: 1. Cimetidine is metabolized by the CYP 3A4 isoenzymes 2. Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels 3. Both 1 and 2 4. Neither 1 nor 2 ____ 7. Laboratory monitoring for patients on angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers should include: 1. White blood cell counts with the drug dosage increased for elevations above 10,000 feet 2. Liver function tests with the drug dosage stopped for alanine aminotransferase values twice that of normal 3. Serum creatinine levels with the drug dosage reduced for values greater than 2.5 mg/dL 4. Serum glucose levels with the drug dosage increased for levels greater than 120 mg/dL ____ 8. Jacob has hypertension, for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it: 1. Decreases the amount of calcium inside the cell 2. Reduces stroke volume 3. Increases the activity of the Na+/K+/ATPase pump indirectly 4. Decreases heart rate ____ 9. Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker? 1. Bradycardia 2. Hepatic impairment 3. Increased contractility 4. Edema of the hands and feet ____ 10. Patient teaching related to amlodipine includes: 1. Increase calcium intake to prevent osteoporosis from a calcium blockade. 2. Do not crush the tablet; it must be given in liquid form if the patient has trouble swallowing it. 3. Avoid grapefruit juice as it affects the metabolism of this drug. 4. Rise slowly from a supine position to reduce orthostatic hypotension. ____ 11. Vera, age 70, has isolated systolic hypertension. Calcium channel blocker dosages for her should be: 1. Started at about half the usual dosage 2. Not increased over the usual dosage for an adult 3. Given once daily because of memory issues in the older adult 4. Withheld if she experiences gastroesophageal reflux ____ 12. Larry has heart failure, which is being treated with digoxin because it exhibits: 1. Negative inotropism 2. Positive chronotropism 3. Both 1 and 2 4. Neither 1 nor 2 ____ 13. Furosemide is added to a treatment regimen for heart failure that includes digoxin. Monitoring for this combination includes: 1. Hemoglobin 2. Serum potassium 3. Blood urea nitrogen 4. Serum glucose ____ 14. Which of the following create a higher risk for digoxin toxicity? Both the cause and the reason for it must be correct. 1. Older adults because of reduced renal function 2. Administration of aldosterone antagonist diuretics because of decreased potassium levels 3. Taking an antacid for gastroesophageal reflux disease because it increases the absorption of digoxin 4. Doses between 0.25 and 0.5 mg/day ____ 15. Serum digoxin levels are monitored for potential toxicity. Monitoring should occur: 1. Within 6 hours of the last dose 2. Because a reference point is needed in adjusting a dose 3. After three half-lives from the starting of the drug 4. When a patient has stable renal function ____ 16. Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: 1. Widening of the area of infarction 2. Onset of congestive heart failure 3. An electrolyte imbalance involving potassium 4. Renal dysfunction ____ 17. Which of the following is true about procainamide and its dosing schedule? 1. It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. 2. Gastrointestinal adverse effects are common so the drug should be taken with food. 3. Adherence can be improved by using a sustained release formulation that can be given once daily. 4. Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. ____ 18. Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT: 1. Notify your health-care provider immediately if you have visual change. 2. Monitor your own blood pressure and pulse daily. 3. Take a hot shower or bath if you feel dizzy. 4. Use a sunscreen on exposed body surfaces. ____ 19. The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response? 1. Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism. 2. Amiodarone damages the thyroid gland and can result in inflammation of that gland, causing hyperthyroidism. 3. Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given. 4. Amiodarone can cause corneal deposits in up to 25% of patients. ____ 20. Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 a.m. and 2 p.m. because: 1. It is a long-acting drug with potential for toxicity. 2. Nitrate tolerance can develop. 3. Orthostatic hypotension is a common adverse effect. 4. It must be taken with milk or food. ____ 21. Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: 1. This is a parasympathetic response to the vasodilating effects of the drug. 2. Headaches are common side effects with these drugs. How severe are they? 3. This is associated with your smoking. Let’s work on having you stop smoking. 4. This is not related to your medication. Are you under a lot of stress? ____ 22. In teaching about the use of sublingual nitroglycerine, the patient should be instructed: 1. To swallow the tablet with a full glass of water 2. To place one tablet under the tongue if chest pain occurs and allow it to dissolve 3. To take one tablet every 5 minutes until the chest pain goes away 4. That it should “burn” when placed under the tongue or it is no longer effective ____ 23. Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: 1. Become a vegetarian because this disorder is associated with eating red meat. 2. Stop taking the drug if abdominal cramps and diarrhea develop. 3. Report muscle weakness or tenderness and dark urine to his provider immediately. 4. Expect “hot flash” sensations during the first 2 weeks of therapy. ____ 24. Which of the following diagnostic studies would NOT indicate a problem related to a reductase inhibitor? 1. Elevated serum transaminase 2. Increased serum creatinine 3. Elevated creatinine kinase 4. Increased white blood cell counts ____ 25. Because of the pattern of cholesterol synthesis, reductase inhibitors are given: 1. In the evening in a single daily dose 2. Twice daily in the morning and the evening 3. With each meal and at bedtime 4. In the morning before eating ____ 26. Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following laboratory results should be monitored? 1. Serum alanine aminotransferase 2. Serum amylase 3. Serum creatinine 4. Phenylketonuria ____ 27. Niaspan is less likely to cause which side effect that is common to niacin? 1. Gastrointestinal irritation 2. Cutaneous flushing 3. Dehydration 4. Headaches ____ 28. Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? 1. Reactive airway disease/asthma 2. Inflammatory bowel disease 3. Allergy to aspirin 4. Gallbladder disease ____ 29. Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct. 1. Reductase inhibitors, due to an increased risk for rhabdomyolysis 2. Bile-acid sequestering resins, due to interference with folic acid absorption 3. Grapefruit juice, due to interference with metabolism 4. Niacin, due to decreased gemfibrozil activity ____ 30. Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug: 1. Blocks synthesis of cholesterol in the liver 2. Exchanges chloride ions for negatively charged acids in the bowel 3. Increases HDL levels the most among the classes 4. Blocks the lipoprotein lipase pathway ____ 31. Because of their site of action, bile acid sequestering resins: 1. Should be administered separately from other drugs by at least 4 hours 2. May increase the risk for bleeding 3. Both 1 and 2 4. Neither 1 nor 2 ____ 32. Colestipol comes in a powdered form. The patient is taught to: 1. Take the powder dry and follow it with at least 8 ounces of water 2. Take it with a meal to enhance its action on fatty food 3. Mix the powder with 4 to 6 ounces of milk or fruit juice 4. Take after the evening meal to coincide with cholesterol synthesis ____ 33. The choice of diuretic to use in treating hypertension is based on: 1. Presence of diabetes with loop diuretics being used for these patients 2. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40mL/min range 3. Ethnicity with aldosterone antagonists best for African Americans and older adults 4. Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL ____ 34. Direct renin inhibitors have the following properties. They: 1. Are primarily generic drugs 2. Are a renin-angiotensin-aldosterone system (RAAS) medication that is safe during pregnancy 3. Can be used with an angiotensin-converting enzyme and angiotensin II receptor blocker medications for stronger impact 4. “Shut down” the entire RAAS cycle ____ 35. When comparing angiotensin-converting enzyme (ACE) and angiotensin II receptor blocker (ARB) medications, which of the following holds true? 1. Both have major issues with a dry, irritating cough 2. Both contribute to some retention of potassium 3. ARBs have a stronger impact on hypertension control than ACE medications 4. ARBs have stronger diabetes mellitus renal protection properties than ACE medications ____ 36. What does the provider understand about the issue of “Diabetic Renal Protection” with angiotensin-converting enzyme (ACE) medications? Diabetes mellitus patients: 1. Have a reduced rate of renal progression, but still need to be discontinued when advanced renal issues present 2. Who start these medications never progress to renal nephropathy 3. With early renal dysfunction will see it reverse when on ACE medications 4. Without renal issues are the only ones who benefit from ACE protection ____ 37. What dermatological issue is linked to Amiodarone use? 1. Increased risk of basal cell carcinoma 2. Flare up of any prior psoriasis problems 3. Development of plantar warts 4. Progressive change of skin tone toward a blue spectrum ____ 38. Commercials on TV for erectile dysfunction (ED) medications warn about mixing them with nitrates. Why? 1. Increased risk of priapism 2. Profound hypotension 3. Development of blue discoloration to the visual field 4. Inactivation of the ED medication effect Chapter 17. Drugs Affecting the Respiratory System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Digoxin levels need to be monitored closely when the following medication is started: 1. Loratadine 2. Diphenhydramine 3. Ipratropium 4. Albuterol ____ 2. Patients with pheochromocytoma should avoid which of the following classes of drugs because of the possibility of developing hypertensive crisis? 1. Expectorants 2. Beta-2-agonists 3. Antitussives 4. Antihistamines ____ 3. Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? 1. Betamethasone, an inhaled corticosteroid 2. Salmeterol, an inhaled long-acting beta-agonist 3. Albuterol, a short-acting beta-agonist 4. Montelukast, a leukotriene modifier ____ 4. Long-acting beta-agonists (LTBAs) received a Black Box Warning from the U.S. Food and Drug Administration due to the: 1. Risk of life-threatening dermatological reactions 2. Increased incidence of cardiac events when LTBAs are used 3. Increased risk of asthma-related deaths when LTBAs are used 4. Risk for life-threatening alterations in electrolytes ____ 5. The bronchodilator of choice for patients taking propranolol is: 1. Albuterol 2. Pirbuterol 3. Formoterol 4. Ipratropium ____ 6. James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin’s diet for weight loss. The appropriate response would be: 1. Congratulate him on making a positive change in his life. 2. Recommend he try stopping smoking instead of the Atkin’s diet. 3. Schedule him for regular testing of serum theophylline levels during his diet due to increased excretion of theophylline. 4. Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels. ____ 7. Li takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: 1. Reassure him this is probably a viral infection and should be better soon 2. Have him seen the same day for an assessment and theophylline level 3. Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better 4. Order a theophylline level at the laboratory for him ____ 8. Tiotropium bromide (Spiriva) is an inhaled anticholinergic: 1. Used for the treatment of chronic obstructive pulmonary disease (COPD) 2. Used in the treatment of asthma 3. Combined with albuterol for treatment of asthma exacerbations 4. Combined with fluticasone for the treatment of persistent asthma ____ 9. Christy has exercise-induced and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes: 1. Use one to two puffs of albuterol per day to prevent an attack with no more than eight puffs per day 2. Beclomethasone needs to be used every day to treat her asthma 3. Report any systemic side effects she is experiencing, such as weight gain 4. Use the albuterol metered-dose inhaler (MDI) immediately after her corticosteroid MDI to facilitate bronchodilation ____ 10. When prescribing montelukast (Singulair) for asthma, patients or parents of patients should be instructed: 1. Montelukast twice a day is started when there is an asthma exacerbation. 2. Patients may experience weight gain on montelukast. 3. Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast. 4. Lethargy and hypersomnia may occur when taking montelukast. ____ 11. Montelukast (Singulair) may be prescribed for: 1. A 6-year-old child with exercise-induced asthma 2. A 2-year-old child with moderate persistent asthma 3. An 18-month-old child with seasonal allergic rhinitis 4. None of the above; montelukast is not approved for use in children ____ 12. The known drug interactions with the inhaled corticosteroid beclomethasone (QVAR) include: 1. Albuterol 2. MMR vaccine 3. Insulin 4. None of the above ____ 13. When educating patients who are starting on inhaled corticosteroids, the provider should tell them that: 1. They need to get any live vaccines before starting the medication. 2. Inhaled corticosteroids need to be used daily during asthma exacerbations to be effective. 3. Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush. 4. They can triple the dose number of inhalations of medication during colds to prevent needing systemic steroids. ____ 14. Patients with allergic rhinitis may benefit from a prescription of: 1. Fluticasone (Flonase) 2. Cetirizine (Zyrtec) 3. OTC cromolyn nasal spray (Nasalcrom) 4. Any of the above ____ 15. Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: 1. Urinary retention 2. Cardiac output 3. Peripheral edema 4. Skin rash ____ 16. First-generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they are: 1. More effective than first-generation antihistamines 2. Less sedating than the first-generation antihistamines 3. Prescription products, therefore are covered by insurance 4. Able to be taken with central nervous system (CNS) sedatives, such as alcohol ____ 17. When recommending dimenhydrinate (Dramamine) to treat motion sickness, patients should be instructed to: 1. Take the dimenhydrinate after they get nauseated 2. Drink lots of water while taking the dimenhydrinate 3. Take the dimenhydrinate 15 minutes before it is needed 4. Double the dose if one tablet is not effective ____ 18. Decongestants such as pseudoephedrine (Sudafed): 1. Are Schedule III drugs in all states 2. Should not be prescribed or recommended for children under 4 years of age 3. Are effective in treating the congestion children experience with the common cold 4. May cause drowsiness in patients of all ages ____ 19. Cough and cold medications that contain a sympathomimetic decongestant such as phenylephrine should be used cautiously in what population: 1. Older adults 2. Hypertensive patients 3. Infants 4. All of the above ____ 20. Martin is a 60-year-old patient with hypertension. The first-line decongestant to prescribe would be: 1. Oral pseudoephedrine 2. Oral phenylephrine 3. Nasal oxymetazoline 4. Nasal azelastine ____ 21. The first-line treatment for cough related to an upper respiratory tract infection (URI) in a 5-year-old child is: 1. Fluids and symptomatic care 2. Dextromethorphan and guaifenesin syrup (Robitussin DM for Kids) 3. Guaifenesin and codeine syrup (Tussin AC) 4. Chlorpheniramine and dextromethorphan syrup (Nyquil for Kids) Chapter 18. Drugs Affecting the Hematopoietic System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Kenneth is taking warfarin and is asking about what he can take for minor aches and pains. The best recommendation is: 1. Ibuprofen 400 mg three times a day 2. Acetaminophen, not to exceed 4 grams per day 3. Prescribe acetaminophen with codeine 4. Aspirin 640 mg three times a day ____ 2. Juanita had a deep vein thrombosis (DVT) and was on heparin in the hospital and was discharged on warfarin. She asks her primary care provider NP why she was getting both medications while in the hospital. The best response is to: 1. Contact the hospitalist as this is not the normal guideline for prescribing these two medications and she may have had a more complicated case. 2. Explain that warfarin is often started while a patient is still on heparin because warfarin takes a few days to reach effectiveness. 3. Encourage the patient to contact the Customer Service department at the hospital as this was most likely a medication error during her admission. 4. Draw anticoagulation studies to make sure she does not have dangerously high bleeding times. ____ 3. The safest drug to use to treat pregnant women who require anticoagulant therapy is: 1. Low-molecular-weight heparin 2. Warfarin 3. Aspirin 4. Heparin ____ 4. The average starting dose of warfarin is 5 mg daily. Higher doses of 7.5 mg daily should be considered in which patients? 1. Pregnant women 2. Elderly men 3. Overweight or obese patients 4. Patients with multiple comorbidities ____ 5. Cecil and his wife are traveling to Southeast Asia on vacation and he has come into the clinic to review his medications. He is healthy with only mild hypertension that is well controlled. He asks about getting “a shot” to prevent blood clots like his friend Ralph did before international travel. The correct respond would be: 1. Administer one dose of low-molecular weight heparin 24 hours before travel. 2. Prescribe one dose of warfarin to be taken the day of travel. 3. Consult with a hematologist regarding a treatment plan for Cecil. 4. Explain that Cecil is not at high risk of a blood clot and provide education about how to prevent blood clots while traveling. ____ 6. Robert, age 51 years, has been told by his primary care provider (PCP) to take an aspirin a day. Why would this be recommended? 1. He has arthritis and this will help with the inflammation and pain. 2. Aspirin has anti-platelet activity and prevents clots that cause heart attacks. 3. Aspirin acidifies the urine and he needs this for prostrate health. 4. He has a history of GI bleed, and one aspirin a day is a safe dosage. ____ 7. Sally has been prescribed aspirin 320 mg per day for her atrial fibrillation. She also takes aspirin four or more times a day for arthritis pain. What are the symptoms of aspirin toxicity for which she would need to be evaluated? 1. Tinnitus 2. Diarrhea 3. Hearing loss 4. Photosensitivity ____ 8. Patient education when prescribing clopidogrel includes: 1. Do not take any herbal products without discussing it with the provider. 2. Monitor urine output closely and contact the provider if it decreases. 3. Clopidogrel can be constipating, use a stool softener if needed. 4. The patient will need regular anticoagulant studies while on clopidogrel. ____ 9. For patients taking warfarin, INRs are best drawn: 1. Monthly throughout therapy 2. Three times a week throughout therapy 3. Two hours after the last dose of warfarin to get an accurate peak level 4. In the morning if the patient takes their warfarin at night ____ 10. Patients receiving heparin therapy require monitoring of: 1. Platelets every 2 to 3 days for thrombocytopenia that may occur on day 4 of therapy 2. Electrolytes for elevated potassium levels in the first 24 hours of therapy 3. INR throughout therapy to stay within the range of 2.0 4. Blood pressure for hypertension that may occur in the first 2 days of treatment ____ 11. The routine monitoring recommended for low molecular weight heparin is: 1. INR every 2 days until stable, then weekly 2. aPTT every week while on therapy 3. Factor Xa levels if the patient is pregnant 4. White blood cell count every 2 weeks ____ 12. When writing a prescription for warfarin it is common to write _________ on the prescription. 1. OK to substitute for generic 2. The brand name of warfarin and Do Not Substitute 3. PRN refills 4. Refills for 1 year ____ 13. Education of patients who are taking warfarin includes discussing their diet. Instructions include: 1. Avoiding all vitamin K-containing foods 2. Avoiding high-vitamin K-containing foods 3. Increasing intake of iron-containing foods 4. Making sure they eat 35 grams of fiber daily ____ 14. Patients who are being treated with epoetin alfa need to be monitored for the development of: 1. Thrombocytopenia 2. Neutropenia 3. Hypertension 4. Gout ____ 15. The FDA issued a safety announcement regarding the use of erythropoiesis-stimulating agents (ESAs) in 2010 with the recommendation that: 1. ESAs no longer be prescribed to patients with chronic renal failure 2. The risk of tumor development be explained to cancer patients on ESA therapy 3. Patients should no longer receive ESA therapy to prepare for allogenic transfusions 4. ESAs be prescribed only to patients younger than age 60 years ____ 16. When patients are started on darbepoetin alfa (Aranesp) they need monitoring of their blood counts to determine a dosage adjustment in: 1. 6 weeks if they are a cancer patient 2. 1 week if they have chronic renal failure 3. 2 weeks if they are taking it for allogenic transfusion 4. Each week throughout therapy ____ 17. Jim is having a hip replacement surgery and would like to self-donate blood for the surgery. In addition to being prescribed epogen alpha he should also be prescribed: 1. Folic acid to prevent megaloblastic anemia 2. Iron, to start when the epogen starts 3. An antihypertensive to counter the adverse effects of epogen 4. Vitamin B12 to prevent pernicious anemia ____ 18. Monitoring for a patient being prescribed iron for iron deficiency anemia includes: 1. Reticulocyte count 1 week after therapy is started 2. Complete blood count every 2 weeks throughout therapy 3. Hemoglobin level at 1 week of therapy 4. INR weekly throughout therapy ____ 19. Patient education regarding taking iron replacements includes: 1. Doubling the dose if they miss a dose to maintain therapeutic levels 2. Taking the iron with milk or crackers if it upsets their stomach 3. Iron is best taken on an empty stomach with juice 4. Antacids such as Tums may help the upset stomach caused by iron therapy ____ 20. Patients with pernicious anemia require treatment with: 1. Iron 2. Folic acid 3. Epogen alpha 4. Vitamin B12 ____ 21. The first laboratory value indication that vitamin B12 therapy is adequately treating pernicious anemia is: 1. Hematocrit levels start to rise 2. Hemoglobin levels return to normal 3. Reticulocyte count begins to rise 4. Vitamin B12 levels return to normal ____ 22. Patients who are beginning therapy with vitamin B12 need to be monitored for: 1. Hypertensive crisis that may occur in the first 36 hours 2. Hypokalemia that occurs in the first 48 hours 3. Leukopenia that occurs at 1 to 3 weeks of therapy 4. Thrombocytopenia that may occur at any time in therapy Chapter 20. Drugs Affecting the Gastrointestinal System Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing it with their provider or a pharmacist first? 1. Patients with kidney stones 2. Pregnant patients 3. Patients with heartburn 4. Postmenopausal women ____ 2. Patients taking antacids should be educated regarding these drugs, including letting them know that: 1. They may cause constipation or diarrhea 2. Many are high in sodium 3. They should separate antacids from other medications by 1 hour 4. All of the above ____ 3. Kelly has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide: 1. Can be given to patients of all ages, including infants and children, for viral gastroenteritis 2. Slows gastric motility and reduces fluid and electrolyte loss from diarrhea 3. Is the treatment of choice for the diarrhea associated with E. coli 0157 4. May be used in pregnancy and by lactating women ____ 4. Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate: 1. May lead to toxicity if taken with aspirin 2. Is contraindicated in children with flu-like illness 3. Has antimicrobial effects against bacterial and viral enteropathogens 4. All of the above ____ 5. Hannah will be traveling to Mexico with her church group over spring break to build houses. She is concerned she may develop traveler’s diarrhea. Advice includes following normal food and water precautions as well as taking: 1. Loperamide four times a day throughout the trip 2. Bismuth subsalicylate with each meal and at bedtime 3. A prescription for diphenoxylate with atropine to use if she gets diarrhea 4. None of the above ____ 6. Josie is a 5-year-old patient who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie? 1. Prochlorperazine (Compazine) 2. Meclizine (Antivert) 3. Promethazine (Phenergan) 4. Ondansetron (Zofran) ____ 7. Jim presents with complaints of “heartburn” that is minimally relieved with Tums (calcium carbonate) and is diagnosed with gastroesophageal reflux disease (GERD). An appropriate first-step therapy would be: 1. Omeprazole (Prilosec) twice a day 2. Ranitidine (Zantac) twice a day 3. Famotidine (Pepcid) once a day 4. Metoclopramide (Reglan) four times a day ____ 8. Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for: 1. Iron deficiency anemia, vitamin B12 and calcium deficiency 2. Folate and magnesium deficiency 3. Elevated uric acid levels leading to gout 4. Hypokalemia and hypocalcemia ____ 9. Sadie is a 72-year-old patient who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: 1. Megaloblastic anemia 2. Osteoporosis 3. Hypertension 4. Strokes ____ 10. Patrick is a 10-year-old patient who presents with uncomfortable constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10-year-old child would be: 1. PEG 3350 (Miralax) 2. Bisacodyl (Dulcolax) suppository 3. Docusate (Colace) suppository 4. Polyethylene glycol electrolyte solution ____ 11. Methylnaltrexone is used to treat constipation in: 1. Patients with functional constipation 2. Patients with irritable bowel syndrome-associated constipation 3. Children with encopresis 4. Opioid-associated constipation ____ 12. An elderly person has been prescribed lactulose for treatment of chronic constipation. Monitoring with long-term treatment would include: 1. Electrolytes, including potassium and chloride 2. Bone mineral density for osteoporosis 3. Magnesium level 4. Liver function Chapter 24. Drugs Used in Treating Infectious Diseases Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Factors that place a patient at risk of developing an antimicrobial-resistant organism include: 1. Age over 50 years 2. School attendance 3. Travel within the U.S. 4. Inappropriate use of antimicrobials ____ 2. Infants and young children are at higher risk of developing antibiotic-resistant infections due to: 1. Developmental differences in pharmacokinetics of the antibiotics in children 2. The fact that children this age are more likely to be in daycare and exposed to pathogens from other children 3. Parents of young children insisting on preventive antibiotics so they don’t miss work when their child is sick 4. Immunosuppression from the multiple vaccines they receive in the first 2 years of life ____ 3. Providers should use an antibiogram when prescribing. An antibiogram is: 1. The other name for the Centers for Disease Control guidelines for prescribing antibiotics 2. An algorithm used for prescribing antibiotics for certain infections 3. The reference also known as the Pink Book, published by the Centers for Disease Control 4. A chart of the local resistance patterns to antibiotics developed by laboratories ____ 4. There is often cross-sensitivity and cross-resistance between penicillins and cephalosporins because: 1. Renal excretion is similar in both classes of drugs. 2. When these drug classes are metabolized in the liver they both produce resistant enzymes. 3. Both drug classes contain a beta-lactam ring that is vulnerable to beta-lactamase-producing organisms. 4. There is not an issue with cross-resistance between the penicillins and cephalosporins. ____ 5. Jonathan has been diagnosed with strep throat and needs a prescription for an antibiotic. He says the last time he had penicillin he developed a red, blotchy rash. An appropriate antibiotic to prescribe would be: 1. Penicillin VK, because his rash does not sound like a serious rash 2. Amoxicillin 3. Cefadroxil (Duricef) 4. Azithromycin ____ 6. Sarah is a 25-year-old female who is 8 weeks pregnant and has a urinary tract infection. What would be the appropriate antibiotic to prescribe for her? 1. Ciprofloxacin (Cipro) 2. Amoxicillin (Trimox) 3. Doxycycline 4. Trimethoprim-sulfamethoxazole (Septra) ____ 7. Pong-tai is a 12-month-old child who is being treated with amoxicillin for acute otitis media. His parents call the clinic and say he has developed diarrhea. The appropriate action would be to: 1. Advise the parents that some diarrhea is normal with amoxicillin and recommend probiotics daily. 2. Change the antibiotic to one that is less of a gastrointestinal irritant. 3. Order stool cultures for suspected viral pathogens not treated by the amoxicillin. 4. Recommend increased fluids and fiber in his diet. ____ 8. Lauren is a 13-year-old child who comes to clinic with a 4-day history of cough, low-grade fever, and rhinorrhea. When she blows her nose or coughs the mucous is greenish-yellow. The appropriate antibiotic to prescribe would be: 1. Amoxicillin 2. Amoxicillin/clavulanate 3. TMP/SMZ (Septra) 4. None ____ 9. Joanna had a small ventricle septal defect (VSD) repaired when she was 3 years old and has no residual cardiac problems. She is now 28 and is requesting prophylactic antibiotics for an upcoming dental visit. The appropriate antibiotic to prescribe according to current American College of Cardiology and American Heart Association guidelines is: 1. None, no antibiotic is required for dental procedures 2. Amoxicillin 2 grams 1 hour before the procedure 3. Ampicillin 2 grams IM or IV 30 minutes before the procedure 4. Azithromycin 1 gram 1 hour before the procedure ____ 10. To prevent further development of antibacterial resistance it is recommended that fluoroquinolones be reserved for treatment of: 1. Urinary tract infections in young women 2. Upper respiratory infections in adults 3. Skin and soft tissue infections in adults 4. Community-acquired pneumonia in patients with comorbidities ____ 11. Fluoroquinolones have a Black Box Warning regarding ________ even months after treatment. 1. Renal dysfunction 2. Hepatic toxicity 3. Tendon rupture 4. Development of glaucoma ____ 12. Janet was recently treated with clindamycin for an infection. She calls the advice nurse because she is having frequent diarrhea that she thinks may have blood in it. What would be the appropriate care for her? 1. Encourage increased fluids and fiber. 2. Assess her for pseudomembranous colitis. 3. Advise her to eat yogurt daily to help restore her gut bacteria. 4. Start her on an antidiarrheal medication. ____ 13. Keng has chronic hepatitis that has led to mildly impaired liver function. He has an infection that would be best treated by a macrolide. Which would be the best choice for a patient with liver dysfunction? 1. Azithromycin (Zithromax) 2. Clarithromycin (Biaxin) 3. Erythromycin (E-mycin) 4. None of the above ____ 14. Jamie has glucose-6-phosphate dehydrogenase deficiency (G6PD) and requires an antibiotic. Which class of antibiotics should be avoided in this patient? 1. Penicillins 2. Macrolides 3. Cephalosporins 4. Sulfonamides ____ 15. If a patient is allergic to sulfonamide antibiotics, he or she will most likely have cross-sensitivity to: 1. Loop diuretics 2. Sulfonylureas 3. Thiazide diuretics 4. All of the above ____ 16. Tetracyclines such as minocycline are safe to use in: 1. Pregnant women 2. Adolescents 3. Patients with renal dysfunction 4. Patients with hepatic dysfunction ____ 17. Tetracyclines should not be prescribed to children younger than 8 years due to: 1. Risk of developing cartilage problems 2. Development of significant diarrhea 3. Risk of kernicterus 4. Adverse effects on bone growth ____ 18. Nicole is a 16-year-old female who is taking minocycline for acne. She comes to the clinic complaining of a headache. What would be the plan of care? 1. Advise acetaminophen or ibuprofen as needed for headaches. 2. Prescribe sumatriptan (Imitrex) to be taken at the onset of the headache. 3. Evaluate her for pseudotremor cerebri. 4. Assess her caffeine intake and sleep patterns. ____ 19. Patricia has been prescribed doxycycline for a chlamydia infection. She is healthy and her only medication is an oral combined contraceptive. Patricia’s education would include: 1. Use a back-up method of birth control (condom) until her next menses. 2. Doxycycline may cause tendonitis and she should report any joint pain. 3. Her partner will need treatment if her infection doesn’t clear with the doxycycline. 4. Doxycycline is used for one-dose treatment of STIs; take the whole prescription at once. ____ 20. To prevent the development of peripheral neuropathy in patients taking isoniazid for tuberculosis the patient is also prescribed: 1. Niacin (vitamin B3) 2. Pyridoxine (vitamin B6) 3. Riboflavin (vitamin B2) 4. Thiamine (vitamin B1) ____ 21. Sadie is an 82-year-old patient who has herpes zoster (shingles) and would benefit from an antiviral such as valacyclovir. Prior to prescribing valacyclovir she will need an assessment of: 1. Complete blood count to rule out anemia 2. Liver function 3. Renal function 4. Immunocompetence ____ 22. When prescribing acyclovir, patients should be educated regarding the: 1. High risk of developing diarrhea 2. Need to drink lots of fluids during treatment 3. Risk for life-threatening rash such as Stevens-Johnson 4. Eccentric dosing schedule ____ 23. Nicholas has been diagnosed with type A influenza. Appropriate prescribing of oseltamivir (Tamiflu) would include: 1. Starting oseltamivir within the first 48 hours of influenza symptoms 2. Advising the patient he can stop the oseltamivir when his symptoms resolve 3. Educating the patient that oseltamivir will cure influenza 4. Prophylactic treatment of all family members ____ 24. Monitoring for patients who are on long-term antifungal therapy with ketoconazole includes: 1. Platelet count 2. BUN and creatinine 3. White blood cell count 4. AST, ALT, alkaline phosphatase, and bilirubin ____ 25. When prescribing metronidazole (Flagyl) to treat bacterial vaginosis, patient education would include: 1. Metronidazole is safe in the first trimester of pregnancy. 2. Consuming alcohol in any form may cause a severe reaction. 3. Sexual partners need concurrent therapy. 4. Headaches are a sign of a serious adverse reaction and need immediate evaluation. ____ 26. Every antibiotic drug class has resistant organisms that influence prescribing decisions. 1. True 2. False Chapter 26. Drugs Used in Treating Eye and Ear Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The Centers for Disease Control recommends all newborn infants receive prophylactic administration of __________ within 1 hour of birth. 1. Gentamicin ophthalmic ointment 2. Ciprofloxacin ophthalmic drops 3. Erythromycin oral suspension 4. Erythromycin ophthalmic ointment ____ 2. Conjunctivitis in a child that is accompanied by acute otitis media is treated with: 1. Sulfacetamide 10% ophthalmic solution (Bleph-10) 2. Bacitracin/polymyxin B (Polysporin) ophthalmic drops 3. Ciprofloxacin (Ciloxan) ophthalmic drops 4. High-dose oral amoxicillin ____ 3. Twenty-year-old Annie comes to the clinic complaining of copious yellow-green eye discharge. Gram stain indicates she most likely has gonococcal conjunctivitis. While awaiting the culture results, the plan of care should be: 1. None, wait for the culture results to determine the course of treatment 2. Ciprofloxacin (Ciloxan) ophthalmic drops 3. IM ceftriaxone 4. High-dose oral amoxicillin ____ 4. Education of women who are being treated with ophthalmic antibiotics for conjunctivitis includes: 1. Throwing away eye makeup and purchasing new 2. Redness and intense burning is normal with ophthalmic antibiotics 3. When applying eye ointment, set the tip of the tube on the lower lid and squeeze in inch 4. Use a cotton swab to apply ointment, spreading the ointment all over the lid and in the conjunctival sac ____ 5. Sadie was prescribed betaxolol ophthalmic drops by her ophthalmologist to treat her glaucoma. Oral beta blockers should be avoided in patients who use ophthalmic beta blockers because: 1. There may be an antagonistic reaction between the two. 2. The additive effects may include bradycardia. 3. They may potentiate each other and cause respiratory depression. 4. The additive effects may cause metabolic acidosis. ____ 6. David presents to the clinic with symptoms of allergic conjunctivitis. He is prescribed cromolyn sodium (Opticrom) eye drops. The education regarding using cromolyn eye drops includes: 1. He should not wear his soft contacts while using the cromolyn eye drops. 2. Cromolyn drops are instilled once a day to prevent allergy symptoms. 3. Long-term use may cause glaucoma. 4. He may experience bradycardia as an adverse effect. ____ 7. Ciprofloxacin otic drops are contraindicated in: 1. Children 2. Patients with acute otitis externa 3. Patients with a perforated tympanic membrane 4. Swimmer’s ear ____ 8. __________ is / are prescribed to prevent swimmer’s ear. 1. Ciprofloxacin otic drops (Ciloxan) 2. Isopropyl ear drops (EarSol) 3. Colistin (Coly-Mycin S Otic) 4. Gentamicin otic drops ____ 9. Patient education regarding the use of ciprofloxacin-hydrocortisone (Cipro HC otic) ear drops includes: 1. Fill the canal with the drops with each dose. 2. Some redness and itching around the ear canal is normal. 3. Warm the bottle of ear drops in his or her hand before administering. 4. Cipro HC otic may cause ototoxicity. ____ 10. Janie presents to the clinic with hard ear wax in both ear canals. Instructions regarding home removal of hard cerumen include: 1. Moisten a cotton swab (Q-tip) and swab the ear canal twice daily. 2. Instill tap water in both ears while bathing. 3. Squirt hydrogen peroxide into ears with each bath. 4. Instill carbamide peroxide (Debrox) twice daily until canals are clear. Chapter 27. Anemia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Pernicious anemia is treated with: 1. Folic acid supplements 2. Thiamine supplements 3. Vitamin B12 4. Iron ____ 2. Premature infants require iron supplementation with: 1. 10 mg/day of iron 2. 2 mg/kg per day until age 12 months 3. 7 mg/day in their diet 4. 1 mg/kg per day until they are receiving adequate intake of iron from foods ____ 3. Breastfed infants should receive iron supplementation of: 1. 3 mg/kg per day 2. 6 mg/kg per day 3. 1 mg/kg per day 4. Breastfed babies do not need iron supplementation ____ 4. Valerie presents to the clinic with menorrhagia. Her hemoglobin is 10.2 and her ferritin is 15 ng/mL. Initial treatment for her anemia would be: 1. 18 mg/day of iron supplementation 2. 6 mg/kg per day of iron supplementation 3. 325 mg ferrous sulfate per day 4. 325 mg ferrous sulfate tid ____ 5. Chee is a 15-month-old male whose screening hemoglobin is 10.4 g/dL. Treatment for his anemia would be: 1. 18 mg/day of iron supplementation 2. 6 mg/kg per day of elemental iron 3. 325 mg ferrous sulfate per day 4. 325 mg ferrous sulfate tid ____ 6. Monitoring for a patient taking iron to treat iron deficiency anemia is: 1. Hemoglobin, hematocrit, and ferritin 4 weeks after treatment is started 2. Complete blood count every 4 weeks throughout treatment 3. Annual complete blood count 4. Reticulocyte count in 4 weeks ____ 7. Valerie has been prescribed iron to treat her anemia. Education of patients prescribed iron would include: 1. Take the iron with milk if it upsets her stomach. 2. Antacids may help with the nausea and GI upset caused by iron. 3. Increase fluids and fiber to treat constipation. 4. Iron is best tolerated if it is taken at the same time as her other medications. ____ 8. Allie has just had her pregnancy confirmed and is asking about how to ensure a healthy baby. What is the folic acid requirement during pregnancy? 1. 40 mcg/day 2. 200 mcg/day 3. 800 mcg/day 4. 2 gm/day ____ 9. Kyle has Crohn’s disease and has a documented folate deficiency. Drug therapy for folate deficiency anemia is: 1. Oral folic acid 1 to 2 mg per day 2. Oral folic acid 1 gram per day 3. IM folate weekly for at least 6 months 4. Oral folic acid 400 mcg daily ____ 10. Patients who are being treated for folate deficiency require monitoring of: 1. Complete blood count every 4 weeks 2. Hematocrit and hemoglobin at 1 week and then at 8 weeks 3. Reticulocyte count at 1 week 4. Folate levels every 4 weeks until hemoglobin stabilizes ____ 11. The treatment of vitamin B12 deficiency is: 1. 1,000 mcg daily of oral cobalamin 2. 2 gm per day of oral cobalamin 3. Vitamin B12 100 mcg/day IM 4. 500 mcg/dose nasal cyanocobalamin 2 sprays once a week ____ 12. The dosage of Vitamin B12 to initially treat pernicious anemia is: 1. Nasal cyanocobalamin 1 gram spray in each nostril daily x 1 week then weekly x 1 month 2. Vitamin B12 IM monthly 3. Vitamin B12 1,000 mcg IM daily x 1 week then 1,000 mg IM weekly for a month 4. Oral cobalamin 1,000 mcg daily ____ 13. Before beginning IM vitamin B12 therapy, which laboratory values should be obtained? 1. Reticulocyte count, hemoglobin, and hematocrit 2. Iron 3. Vitamin B12 4. All of the above ____ 14. ________ should be monitored when vitamin B12 therapy is started. 1. Serum calcium 2. Serum potassium 3. Ferritin 4. C-reactive protein ____ 15. Anemia due to chronic renal failure is treated with: 1. Epoetin alfa (Epogen) 2. Ferrous sulfate 3. Vitamin B12 4. Hydroxyurea Chapter 28. Chronic Stable Angina and Low-Risk Unstable Angina Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Angina is produced by an imbalance between myocardial oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS? 1. Calcium channel blockers 2. Beta blockers 3. Angiotensin-converting-enzyme (ACE) inhibitors 4. Aspirin ____ 2. Not all chest pain is caused by myocardial ischemia. Noncardiac causes of chest pain include: 1. Pulmonary embolism 2. Pneumonia 3. Gastroesophageal reflux 4. All of the above ____ 3. The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is class: 1. I 2. II 3. III 4. IV ____ 4. Patients at high risk for developing significant coronary heart disease are those with: 1. LDL values between 100 and 130 2. Systolic blood pressure between 120 and 130 3. Class III angina 4. Obesity ____ 5. To reduce mortality, all patients with angina, regardless of class, should be on: 1. Aspirin 81 to 325 mg/d 2. Nitroglycerin sublingually for chest pain 3. ACE inhibitors or angiotensin receptor blockers 4. Digoxin ____ 6. Patients who have angina, regardless of class, who are also diabetic, should be on: 1. Nitrates 2. Beta blockers 3. ACE inhibitors 4. Calcium channel blockers ____ 7. Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct. 1. Lose at least 10 pounds of body weight. Excessive weight increases cardiac workload. 2. Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload. 3. Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of potassium to improve contractility and oxygen supply. 4. Intake a moderate amount of alcohol. Moderate intake has been shown by research to improve cardiac function. ____ 8. Nitrates are especially helpful for patients with angina who also have: 1. Heart failure 2. Hypertension 3. Both 1 and 2 4. Neither 1 nor 2 ____ 9. Beta blockers are especially helpful for patients with exertional angina who also have: 1. Arrhythmias 2. Hypothyroidism 3. Hyperlipidemia 4. Atherosclerosis ____ 10. Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use? 1. These drugs are useful for immediate symptom relief when the patient is certain it is angina. 2. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away. 3. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than two doses. If chest pain is still not relieved, call 911. 4. All of the above ____ 11. Isosorbide dinitrate is a long-acting nitrate given twice daily. The schedule for administration is 7 a.m. and 2 p.m. because: 1. Long-acting forms have a higher risk for toxicity. 2. Orthostatic hypotension is a common adverse effect. 3. It must be taken with milk or food. 4. Nitrate tolerance can develop. ____ 12. Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because: 1. Nitrates increase MOS and beta blockers increase MOD. 2. Their additive effects permit lower doses of both drugs and their adverse reactions cancel each other out. 3. They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease. 4. All of the above ____ 13. Drug choices to treat angina in older adults differ from those of younger adults only in: 1. Consideration of risk factors for diseases associated with and increased in aging 2. The placement of drug therapy as a treatment choice before lifestyle changes are tried 3. The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult 4. Those with higher risk for silent myocardial infarction ____ 14. Which of the following drugs has been associated with increased risk for myocardial infarction in women? 1. Aspirin 2. Beta blockers 3. Estrogen replacement 4. Lipid-lowering agents ____ 15. Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT: 1. Patients often require multiple drugs 2. A large number of angina patients are older adults on fixed incomes 3. Generic formulations may be cheaper but are rarely bioequivalent 4. Lack of drug selectivity may result in increased adverse reactions ____ 16. Situations that suggest referral to a specialist is appropriate include: 1. When chronic stable angina becomes unpredictable in its characteristics and precipitating factors 2. When a post-myocardial infarction patient develops new-onset angina 3. When standard therapy is not successful in improving exercise tolerance or reducing the incidence of angina 4. All of the above ____ 17. The rationale for prescribing calcium blockers for angina can be based on the need for: 1. Increased inotropic effect in the heart 2. Increasing peripheral perfusion 3. Keeping heart rates high enough to ensure perfusion of coronary arteries 4. Help with rate control ____ 18. Medications are typically started for angina patients when: 1. The first permanent EKG changes occur 2. The start of class I or II symptoms 3. The events trigger a trip to the emergency department 4. When troponin levels become altered ____ 19. The most common cause of angina is: 1. Vasospasm of the coronary arteries 2. Atherosclerosis 3. Platelet aggregation 4. Low systemic oxygen ____ 20. Ranolazine is used in angina patients to: 1. Dilate plaque-filled arteries 2. Inhibit platelet aggregation 3. Restrict late sodium flow in the myocytes 4. Induce vasoconstriction in the periphery to open coronary vessels ____ 21. When is aspirin (ASA) used in angina patients? 1. All angina patients should be taking ASA unless it is contraindicated for allergy or other medical reasons. 2. ASA should only be used in men. 3. ASA has no role in angina, but is useful in MI prevention. 4. The impact of ASA is best at the time of an angina attack. Chapter 30. Asthma and Chronic Obstructive Pulmonary Disease Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur: 1. Daily 2. Daily and limit physical activity 3. Less than twice a week 4. More than twice a week and less than once a day ____ 2. In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur: 1. At nighttime one to two times a month 2. At nighttime three to four times a month 3. Less than twice a week 4. Daily ____ 3. One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is: 1. Ability to use albuterol daily to control symptoms 2. Minimize exacerbations to once a month 3. Keep nighttime symptoms at a maximum of twice a week 4. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms ____ 4. A stepwise approach to the pharmacologic management of asthma: 1. Begins with determining the severity of asthma and assessing asthma control 2. Is used when asthma is severe and requires daily steroids 3. Allows for each provider to determine their personal approach to the care of asthmatic patients 4. Provides a framework for the management of severe asthmatics, but is not as helpful when patients have intermittent asthma ____ 5. Treatment for mild intermittent asthma is: 1. Daily inhaled medium-dose corticosteroids 2. Short-acting beta-2-agonists (albuterol) as needed 3. Long-acting beta-2-agonists every morning as a preventative 4. Montelukast (Singulair) daily ____ 6. The first-line therapy for mild-persistent asthma is: 1. High-dose montelukast 2. Theophylline 3. Low-dose inhaled corticosteroids 4. Long-acting beta-2-agonists ____ 7. Monitoring a patient with persistent asthma includes: 1. Monitoring how frequently the patient has an upper respiratory infection (URI) during treatment 2. Monthly in-office spirometry testing 3. Determining if the patient has increased use of his or her long-acting beta-2-agonist due to exacerbations 4. Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy ____ 8. Asthma exacerbations at home are managed by the patient by: 1. Increasing frequency of beta-2-agonists and contacting their provider 2. Doubling inhaled corticosteroid doses 3. Increasing frequency of beta-2-agonists 4. Starting montelukast (Singulair) ____ 9. Patients who are at risk of a fatal asthma attack include patients: 1. With moderate persistent asthma 2. With a history of requiring intubation or ICU admission for asthma 3. Who are on daily inhaled corticosteroid therapy 4. Who are pregnant ____ 10. Pregnant patients with asthma may safely use ________ throughout their pregnancy. 1. Oral terbutaline 2. Prednisone 3. Inhaled corticosteroids (budesonide) 4. Montelukast (Singulair) ____ 11. One goal of asthma management in children is: 1. They independently manage their asthma 2. Participation in school and sports activities 3. No exacerbations 4. Minimal use of inhaled corticosteroids ____ 12. Medications used in the management of patients with chronic obstructive pulmonary disease (COPD) include: 1. Inhaled beta-2-agonists 2. Inhaled anticholinergics (ipratropium) 3. Inhaled corticosteroids 4. All of the above ____ 13. Patients with a COPD exacerbation may require: 1. Doubling of inhaled corticosteroid dose 2. Systemic corticosteroid burst 3. Continuous inhaled beta-2-agonists 4. Leukotriene therapy ____ 14. Patients with COPD require monitoring of: 1. Beta-2-agonist use 2. Serum electrolytes 3. Blood pressure 4. Neuropsychiatric effects of montelukast ____ 15. Education of patients with COPD who use inhaled corticosteroids includes: 1. Doubling the dose at the first sign of a URI 2. Using their inhaled corticosteroid first and then their bronchodilator 3. Rinsing their mouth after use 4. Abstaining from smoking for at least 30 minutes after using ____ 16. Education for patients who use an inhaled beta-agonist and an inhaled corticosteroid includes: 1. Use the inhaled corticosteroid first, followed by the inhaled beta-agonists. 2. Use the inhaled beta-agonist first, followed by the inhaled corticosteroid. 3. Increase fluid intake to 3 liters per day. 4. Avoid use of aspirin or ibuprofen while using inhaled medications. Chapter 34. Gastroesophageal Reflux and Peptic Ulcer Disease Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Gastroesophageal reflux disease may be aggravated by the following medication that affects lower esophageal sphincter (LES) tone: 1. Calcium carbonate 2. Estrogen 3. Furosemide 4. Metoclopramide ____ 2. Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Food or drink that may aggravate GERD include: 1. Eggs 2. Caffeine 3. Chocolate 4. Soda pop ____ 3. Metoclopramide improves gastroesophageal reflux disease symptoms by: 1. Reducing acid secretion 2. Increasing gastric pH 3. Increasing lower esophageal tone 4. Decreasing lower esophageal tone ____ 4. Antacids treat gastroesophageal reflux disease by: 1. Increasing lower esophageal tone 2. Increasing gastric pH 3. Inhibiting gastric acid secretion 4. Increasing serum calcium level ____ 5. When treating patients using the “Step-Down” approach the patient with gastroesophageal reflux disease is started on _______ first. 1. Antacids 2. Histamine2 receptor antagonists 3. Prokinetics 4. Proton pump inhibitors ____ 6. If a patient with symptoms of gastroesophageal reflux disease states that he has been self-treating at home with OTC ranitidine daily, the appropriate treatment would be: 1. Prokinetic (metoclopramide) for 4 to 8 weeks 2. Proton pump inhibitor (omeprazole) for 12 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 2 weeks ____ 7. If a patient with gastroesophageal reflux disease who is taking a proton pump inhibitor daily is not improving, the plan of care would be: 1. Prokinetic (metoclopramide) for 8 to 12 weeks 2. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks 3. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks 4. Cytoprotective drug (misoprostol) for 4 to 8 weeks ____ 8. The next step in treatment when a patient has been on proton pump inhibitors twice daily for 12 weeks and not improving is: 1. Add a prokinetic (metoclopramide) 2. Referral for endoscopy 3. Switch to another proton pump inhibitor 4. Add a cytoprotective drug ____ 9. Infants with reflux are initially treated with: 1. Histamine2 receptor antagonist (ranitidine) 2. Proton pump inhibitor (omeprazole) 3. Anti-reflux maneuvers (elevate head of bed) 4. Prokinetic (metoclopramide) ____ 10. Long-term use of proton pump inhibitors may lead to: 1. Hip fractures in at-risk persons 2. Vitamin B6 deficiency 3. Liver cancer 4. All of the above ____ 11. An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is: 1. Histamine2 receptor antagonists for 4 to 8 weeks 2. Proton pump inhibitor bid for 12 weeks until healing is complete 3. Proton pump inhibitor bid plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor bid and levofloxacin for 14 days ____ 12. Treatment failure in patients with peptic ulcer disease associated with H. pylori may be because of: 1. Antimicrobial resistance 2. An ineffective antacid 3. Overuse of proton pump inhibitors 4. All of the above ____ 13. If a patient with H. pylori-positive peptic ulcer disease fails first-line therapy, the second-line treatment is: 1. Proton pump inhibitor bid plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days 2. Test H. pylori for resistance to common treatment regimens 3. Proton pump inhibitor plus clarithromycin plus amoxicillin for 14 days 4. Proton pump inhibitor and levofloxacin for 14 days ____ 14. After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is: 1. Testing for H. pylori eradication with a serum ELISA test 2. Endoscopy by a specialist 3. A proton pump inhibitor for 8 to 12 weeks until healing is complete 4. All of the above Chapter 36. Heart Failure Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Angiotensin-converting-enzyme (ACE) inhibitors are a central part of the treatment of heart failure because they have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors? 1. Changes in the structure of the left ventricle so that it dilates, hypertrophies, and uses energy less efficiently. 2. Reduced formation of cross-bridges so that contractile force decreases. 3. Activation of the sympathetic nervous system that increases heart rate and preload. 4. Decreased renal blood flow that decreases oxygen supply to the kidneys. ____ 2. One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include: 1. Myocardial ischemia and injury secondary to myocardial infarction 2. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction 3. Increased demands of the heart beyond its ability to adapt secondary to anemia 4. Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension ____ 3. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as stage: 1. A 2. B 3. C 4. D ____ 4. Diagnosis of heart failure cannot be made by symptoms alone because many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is: 1. Chest x-rays that show cephalization and measure heart size 2. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction 3. Complete blood count, blood urea nitrogen, and serum electrolytes that facilitate staging for end-organ damage 4. Measurement of brain natriuretic peptide to distinguish between systolic and diastolic dysfunction ____ 5. Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with: 1. Drugs for hypertension and hyperlipidemia, if they exist 2. Lifestyle management including diet, exercise, and smoking cessation only 3. Angiotensin-converting enzyme (ACE) inhibitors to directly affect the heart failure only 4. No drugs are used in this early stage ____ 6. Class I recommendations for stage A heart failure include: 1. Aerobic exercise within tolerance levels to prevent the development of heart failure 2. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention 3. Beta blockers for all patients regardless of cardiac history 4. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias ____ 7. Stage B patients should have beta blockers added to their heart failure treatment regimen when: 1. They have an ejection fraction less than 40% 2. They have had a recent MI 3. Both 1 and 2 4. Neither 1 nor 2 ____ 8. Increased life expectancy for patients with heart failure has been associated with the use of: 1. ACE inhibitors, especially when started early in the disease process 2. All beta blockers regardless of selectivity 3. Thiazide and loop diuretics 4. Cardiac glycosides ____ 9. Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true? 1. Diuretics reduce preload associated with fluid retention. 2. Diuretics can be used earlier than stage C when the goal is control of hypertension. 3. Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism. 4. Diuretics from the potassium-sparing class should be used when using an angiotensin receptor blocker (ARB). ____ 10. Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with: 1. Ejection fractions above 40% 2. An audible S3 3. Mitral stenosis as a primary cause for heart failure 4. Renal insufficiency ____ 11. Which of the following classes of drugs is contraindicated in heart failure? 1. Nitrates 2. Long-acting dihydropyridines 3. Calcium channel blockers 4. Alpha-beta blockers ____ 12. Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is: 1. Aldosterone antagonists 2. Eplerenone 3. ACE inhibitors 4. ARBs ____ 13. ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes is considered to be safe, at least in the later parts of pregnancy? 1. Diuretics 2. ARBs 3. Beta blockers 4. Nitrates ____ 14. Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: 1. Symptoms markedly worsen or the patient becomes hypotensive and has syncope 2. There is evidence of progressive renal insufficiency or failure 3. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic 4. Any of the above ____ 15. ACE inhibitors are a foundational medication in HF. Which group of patients cannot take them safely? 1. Elderly patients with reduced renal clearance 2. Pregnant women 3. Women under age 30 4. 1 and 2 ____ 16. What assessment that can be done at home is the most reliable for making decisions to change HF medications? 1. Weight 2. BP 3. Heart rate 4. Serum Glucose ____ 17. Evidence is strong that the timing of HF interventions are best initiated when: 1. The person enters stage C 2. The person has functional disabilities 3. At the earliest indication 4. When stage IV is determined ____ 18. HF patients frequently take more than one drug. When are anticoagulants typically used? 1. When the patient enters stage III 2. Only in cases of diastolic failure 3. When there is concurrent A Fib 4. In all cases ____ 19. What can chest x-rays contribute to the diagnosis and management of HF? 1. They have no role. 2. They can give very precise pictures of pulmonary fluid status. 3. They provide an idea of general cardiac size and pulmonary great vessel distribution. 4. They can confirm the diagnosis. Chapter 37. Human Immunodeficiency Virus Disease and Acquired Immunodeficiency Syndrome Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The goals of treatment when prescribing antiretroviral medication to patients with HIV include: 1. Prevent vertical HIV transmission 2. Improve quality of life 3. Prolong survival 4. All of the above ____ 2. A challenge faced with antiretroviral therapy (ART) is: 1. Patients abusing ART 2. Drug-resistant mutations of HIV 3. Reduction of transmissibility of HIV 4. Lack of efficacy data ____ 3. Predictors for successful treatment with antiretroviral therapy (ART) in HIV-positive patients include: 1. They respond to a low-potency treatment regimen 2. They have demonstrated resistance in the past and should respond to newer ART drugs 3. The patient is strictly adherent to the ART treatment regimen 4. Lower baseline CD4 T-cell count at baseline ____ 4. The goal of antiretroviral therapy in HIV-positive patients is: 1. Maximum suppression of HIV replication 2. Eradication of HIV virus from the body 3. Determining a treatment regimen that is free of adverse effects 4. Suppression of CD4 T-cell count ____ 5. Pregnant women who are HIV positive: 1. Are treated with AZT alone to prevent birth defects 2. Are treated with a combination antiretroviral therapy (ART) regimen 3. Should not be treated with ART due to teratogenicity of the drugs 4. Are at high risk of developing resistance to ART drugs ____ 6. Antiretroviral therapy is recommended for HIV-positive patients with: 1. A history of AIDS-defining illness 2. Pregnant women 3. Hepatitis B co-infection 4. All of the above ____ 7. If considering starting a patient on the nucleoside reverse transcriptase inhibitor abacavir, the following testing is recommended prior to prescribing: 1. Renal function 2. HLA B*5701 testing 3. Pancreatic enzyme levels 4. CYP 450 enzyme activity ____ 8. Suzanne is pregnant and has tested HIV positive. Which antiretroviral drug should be avoided in women who are pregnant? 1. Lopinavir/r 2. Zidovudine 3. Ritonavir 4. Lopinavir/ritonavir ____ 9. The cost of HIV treatment can be prohibitive for any patient. Patients can receive assistance from the: 1. Best Pharmaceuticals for HIV/AIDS Patient Act 2. Ryan White HIV/AIDS Treatment Modernization Act 3. National Institute of Health HIV/AIDS Assistance Fund 4. Centers for Disease Control HIV/AIDS Treatment Fund ____ 10. Resistance to antiretroviral therapy (ART) is measured by: 1. Measuring the DNA viral load in the serum 2. Determining plasma viral RNA on two successive measurements 3. Phenotype assays of the combination of ART the patient is on 4. Elevation of T4 counts ____ 11. Phenotype assays are used to measure _______ of antiretroviral therapy. 1. Effectiveness 2. Genotype 3. Sensitivity 4. Hypersensitivity susceptibility ____ 12. Patient factors that contribute to antiretroviral therapy (ART) failure include: 1. Being a male who has sex with males 2. HIV diagnosis in pregnancy 3. Good compliance with the ART treatment regimen 4. ART adverse effects ____ 13. Patients who are taking antiretroviral therapy need to have the following monitored: 1. Lipid levels 2. Sexual functioning 3. Platelet count 4. All of the above ____ 14. Successful antiretroviral therapy (ART) in an HIV-positive patient is determined by: 1. Being able to stop ART therapy due to HIV virus eradication 2. Lowering HIV viral load to unmeasurable amounts 3. Individual measures of success based on their personal situation 4. Normal blood hematologic factors Chapter 39. Hyperlipidemia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The overall goal of treating hyperlipidemia is: 1. Maintain an LDL level of less than 160 mg/dL 2. To reduce atherogenesis 3. Lowering apo B, one of the apoliproteins 4. All of the above ____ 2. When considering which cholesterol-lowering drug to prescribe, which factor determines the type and intensity of treatment? 1. Total LDL 2. Fasting HDL 3. Coronary artery disease risk level 4. Fasting total cholesterol ____ 3. First-line therapy for hyperlipidemia is: 1. Statins 2. Niacin 3. Lifestyle changes 4. Bile acid-binding resins ____ 4. James is a 45-year-old patient with an LDL level of 120 and normal triglycerides. Appropriate first-line therapy for James may include diet counseling, increased physical activity, and: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative ____ 5. Joanne is a 60-year-old patient with an LDL of 132 and a family history of coronary artery disease. She has already tried diet changes (increased fiber and plant sterols) to lower her LDL and after 6 months her LDL is slightly higher. The next step in her treatment would be: 1. A statin 2. Niacin 3. Sterols 4. A fibric acid derivative ____ 6. Sharlene is a 65-year-old patient who has been on a lipid-lowering diet and using plant sterol margarine daily for the past 3 months. Her LDL is 135 mg/dL. An appropriate treatment for her would be: 1. A statin 2. Niacin 3. A fibric acid derivative 4. Determined by her risk factors Mike is a 47 year old who has been on standard dose atorvastatin for 3 months and his repeat LDL is 124 mg/dL. He is a smoker and has a strong family history of cardiovascular disease. His treatment plan would include reinforcing diet, exercise, plant sterol intake, and: A Increasing his dose of atorvastatin B Changing to another statin C Adding niacin to the treatment regimen D Adding a bile acid-binding resin ____ 7. Phil is a 54-year-old male with multiple risk factors who has been on a high-dose statin for 3 months to treat his high LDL level. His LDL is 135 mg/dL and his triglycerides are elevated. A reasonable change in therapy would be to: 1. Discontinue the statin and change to a fibric acid derivative. 2. Discontinue the statin and change to ezetimibe. 3. Continue the statin and add in ezetimibe. 4. Refer him to a specialist in managing patients with recalcitrant hyperlipidemia. Scott is presenting for follow up on his lipid panel. He had elevated total cholesterol, triglycerides, and an LDL of 122 mg/dL. He has already implemented diet changes and increased physical activity. He has mildly elevated liver studies. An appropriate next step for therapy would be: A Atorvastatin (Lipitor) B Niacin (Niaspan) C Simvastatin and ezetimibe (Vytorin) D Gemfibrozil (Lopid) ____ 8. Jamie is a 34-year-old pregnant woman with familial hyperlipidemia and elevated LDL levels. What is the appropriate treatment for a pregnant woman? 1. A statin 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resins ____ 9. Han is a 48-year-old diabetic with hyperlipidemia and high triglycerides. His LDL is 112 mg/dL and he has not tolerated statins. He warrants a trial of a: 1. Sterol 2. Niacin 3. Fibric acid derivative 4. Bile acid-binding resin ____ 10. Jose is a 12-year-old overweight child with a total cholesterol of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____________ with a reevaluation in 6 months. 1. Statins 2. Niacin 3. Sterols 4. Bile acid-binding resins ____ 11. Monitoring of a patient who is on a lipid-lowering drug includes: 1. Fasting total cholesterol every 6 months 2. Lipid profile with attention to serum LDL 6 to 8 weeks after starting therapy, then again in 6 weeks 3. Complete blood count, C-reactive protein, and erythrocyte sedimentation rate after 6 weeks of therapy 4. All of the above ____ 12. Before starting therapy with a statin, the following baseline laboratory values should be evaluated: 1. Complete blood count 2. Liver function (ALT/AST) and creatine kinase 3. C-reactive protein 4. All of the above ____ 13. When starting a patient on a statin, education would include: 1. If they stop the medication their lipid levels will return to pretreatment levels. 2. Medication is a supplement to diet therapy and exercise. 3. If they have any muscle aches or pain, they should contact their provider. 4. All of the above ____ 14. Omega 3 fatty acids are best used to help treat: 1. High HDL 2. Low LDL 3. High triglycerides 4. Any high lipid value ____ 15. When are statins traditionally ordered to be taken? 1. At bedtime 2. At noon 3. At breakfast 4. With the evening meal ____ 16. Which the following persons should not have a statin medication ordered? 1. Someone with 3 first- or second-degree family members with history of muscle issues when started on statins 2. Someone with high lipids, but low BMI 3. Premenopausal woman with recent history of hysterectomy 4. Prediabetic male with known metabolic syndrome ____ 17. Fiber supplements are great options for elderly patients who have the concurrent problem of: 1. End-stage renal failure on fluid restriction 2. Recurrent episodes of diarrhea several times a day 3. Long-term issues of constipation 4. Needing to take multiple medications around the clock every 2 hours ____ 18. What is considered the order of statin strength from lowest effect to highest? 1. Lovastatin, Simvastatin, Rosuvastatin 2. Rosuvastatin, Lovastatin, Atorvastatin 3. Atorvastatin, Rosuvastatin, Simvastatin 4. Simvastatin, Atorvastatin, Lovastatin Chapter 40. Hypertension Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Because primary hypertension has no identifiable cause, treatment is based on interfering with the physiological mechanisms that regulate blood pressure. Thiazide diuretics treat hypertension because they: 1. Increase renin secretion 2. Decrease the production of aldosterone 3. Deplete body sodium and reduce fluid volume 4. Decrease blood viscosity ____ 2. Because of its action on various body systems, the patient taking a thiazide or loop diuretic may also need to receive the following supplement: 1. Potassium 2. Calcium 3. Magnesium 4. Phosphates ____ 3. All patients with hypertension benefit from diuretic therapy, but those who benefit the most are: 1. Those with orthostatic hypertension 2. African Americans 3. Those with stable angina 4. Diabetics ____ 4. Beta blockers treat hypertension because they: 1. Reduce peripheral resistance 2. Vasoconstrict coronary arteries 3. Reduce norepinephrine 4. Reduce angiotensin II production ____ 5. Which of the following disease processes could be made worse by taking a nonselective beta blocker? 1. Asthma 2. Diabetes 3. Both might worsen 4. Beta blockade does not affect these disorders ____ 6. Disease states in addition to hypertension in which beta blockade is a compelling indication for the use of beta blockers include: 1. Heart failure 2. Angina 3. Myocardial infarction 4. Dyslipidemia ____ 7. Angiotensin-converting enzyme (ACE) inhibitors treat hypertension because they: 1. Reduce sodium and water retention 2. Decrease vasoconstriction 3. Increase vasodilation 4. All of the above ____ 8. Compelling indications for an ACE inhibitor as treatment for hypertension based on clinical trials includes: 1. Pregnancy 2. Renal parenchymal disease 3. Stable angina 4. Dyslipidemia ____ 9. An ACE inhibitor and what other class of drug may reduce proteinuria in patients with diabetes better than either drug alone? 1. Beta blockers 2. Diuretics 3. Nondihydropyridine calcium channel blockers 4. Angiotensin II receptor blockers ____ 10. If not chosen as the first drug in hypertension treatment, which drug class should be added as a second step because it will enhance the effects of most other agents? 1. ACE inhibitors 2. Beta blockers 3. Calcium channel blockers 4. Diuretics ____ 11. Treatment costs are important for patients with hypertension. Which of the following statements about cost is NOT true? 1. Hypertension is a chronic disease where patients may be taking drugs for a long time. 2. Most patients will require more than one drug to treat the hypertension. 3. The cost includes the price of any routine or special laboratory tests that a specific drug may require. 4. Few antihypertensive drugs come in generic formulations. ____ 12. Caffeine, exercise, and smoking should be avoided for at least how many minutes before blood pressure measurement? 1. 15 2. 30 3. 60 4. 90 ____ 13. Blood pressure checks in children: 1. Should occur with their annual physical examinations after 6 years of age 2. Require a blood pressure cuff that is one-third the diameter of the child’s arm 3. Should be done during every health-care visit after 3 years of age 4. Require additional laboratory tests such as serum creatinine ____ 14. Lack of adherence to blood pressure management is very common. Reasons for this lack of adherence include: 1. Lifestyle changes are difficult to achieve and maintain. 2. Adverse drug reactions are common and often fall into the categories more associated with nonadherence. 3. Costs of drugs and monitoring with laboratory tests can be expensive. 4. All of the above ____ 15. Lifestyle modifications for patients with prehypertension or hypertension include: 1. Diet and increase exercise to achieve a BMI greater than 25. 2. Drink 4 ounces of red wine at least once per week. 3. Adopt the dietary approaches to stop hypertension (DASH) diet. 4. Increase potassium intake. ____ 16. Which diuretic agents typically do not need potassium supplementation? 1. The loop diuretics 2. The thiazide diuretics 3. The aldosterone inhibitors 4. They all need supplementation ____ 17. Aldactone family medications are frequently used when the hypertensive patient also has: 1. Hyperkalemia 2. Advancing liver dysfunction 3. The need for birth control 4. Rheumatoid arthritis ____ 18. Hypertensive African Americans are typically listed as not being as responsive to which drug groups? 1. ACE inhibitors 2. Calcium channel blockers 3. Diuretics 4. Bidil (hydralazine family of medications) ____ 19. What educational points concerning fluid intake must be covered with diuretic prescriptions? 1. Fluid should be restricted when on them. 2. Fluids should contain at least one salty item daily. 3. Fluid intake should remain near normal for optimal performance. 4. Avoidance of potassium-rich fluids is encouraged. ____ 20. What is a common side effect concern with hypertensive medications and all individuals, but especially the elderly? 1. Risk of falls 2. Triggering of a hypertensive crisis 3. Erectile priapism 4. Risk for bladder cancer development Chapter 42. Pneumonia Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The most common bacterial pathogen in community-acquired pneumonia is: 1. Haemophilus influenzae 2. Staphylococcus aureus 3. Mycoplasma pneumoniae 4. Streptococcus pneumoniae ____ 2. The first-line drug choice for a previously healthy adult patient diagnosed with community-acquired pneumonia would be: 1. Ciprofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline ____ 3. The first-line antibiotic choice for a patient with comorbidities or who is immunosuppressed who has pneumonia and can be treated as an outpatient would be: 1. Levofloxacin 2. Amoxicillin 3. Ciprofloxacin 4. Cephalexin ____ 4. If an adult patient with comorbidities cannot reliably take oral antibiotics to treat pneumonia, an appropriate initial treatment option would be: 1. IV or IM gentamicin 2. IV or IM ceftriaxone 3. IV amoxicillin 4. IV ciprofloxacin ____ 5. Samantha is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe? 1. Levofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline ____ 6. Adults with pneumonia who are responding to antimicrobial therapy should show improvement in their clinical status in: 1. 12 to 24 hours 2. 24 to 36 hours 3. 48 to 72 hours 4. 4 or 5 days ____ 7. Along with prescribing antibiotics, adults with pneumonia should be instructed on lifestyle modifications to improve outcomes, including: 1. Adequate fluid intake 2. Increased fiber intake 3. Bedrest for the first 24 hours 4. All of the above ____ 8. John is a 4-week-old infant who has been diagnosed with chlamydial pneumonia. An appropriate treatment for his pneumonia would be: 1. Levofloxacin 2. Amoxicillin 3. Erythromycin 4. Cephalexin ____ 9. Wing-Sing is a 4-year-old patient who has suspected bacterial pneumonia. He has a temperature of 102°F, oxygen saturation level of 95%, and is taking fluids adequately. What would be appropriate initial treatment for his pneumonia? 1. Ceftriaxone 2. Azithromycin 3. Cephalexin 4. Levofloxacin ____ 10. Giselle is a 14-year-old patient who presents to the clinic with symptoms consistent with mycoplasma pneumonia. What is the treatment for suspected mycoplasma pneumonia in an adolescent? 1. Ceftriaxone 2. Azithromycin 3. Ciprofloxacin 4. Levofloxacin Chapter 45. Tuberculosis Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Drug resistant tuberculosis (TB) is defined as TB that is resistant to: 1. Fluoroquinolones 2. Rifampin and isoniazid 3. Amoxicillin 4. Ceftriaxone ____ 2. Goals when treating tuberculosis include: 1. Completion of recommended therapy 2. Negative purified protein derivative at the end of therapy 3. Completely normal chest x-ray 4. All of the above ____ 3. The principles of drug therapy for the treatment of tuberculosis include: 1. Patients are treated with a drug to which M. tuberculosis is sensitive. 2. Drugs need to be taken on a regular basis for a sufficient amount of time. 3. Treatment continues until the patient’s purified protein derivative is negative. 4. All of the above ____ 4. Isabella has confirmed tuberculosis and is placed on a 6-month treatment regimen. The 6-month regimen consists of: 1. Two months of four-drug therapy (INH, rifampin, pyrazinamide, and ethambutol) followed by Four months of INH and rifampin 2. Six months of INH with daily pyridoxine throughout therapy 3. Six months of INH, rifampin, pyrazinamide, and ethambutol 4. Any of the above ____ 5. Kaleb has extensively resistant tuberculosis (TB). Treatment for extensively resistant TB would include: 1. INH, rifampin, pyrazinamide, and ethambutol for at least 12 months 2. INH, ethambutol, kanamycin, and rifampin 3. Treatment with at least two drugs to which the TB is susceptible 4. Levofloxacin ____ 6. Lila is 24 weeks pregnant and has been diagnosed with tuberculosis (TB). Treatment regimens for a pregnant patient with TB would include: 1. Streptomycin 2. Levofloxacin 3. Kanamycin 4. Pyridoxine ____ 7. Bilal is a 5-year-old patient who has been diagnosed with tuberculosis. His treatment would include: 1. Pyridoxine 2. Ethambutol 3. Levofloxacin 4. Rifabutin ____ 8. Ezekiel is a 9-year-old patient who lives in a household with a family member newly diagnosed with tuberculosis (TB). To prevent Ezekiel from developing TB he should be treated with: 1. 6 months of Isoniazid (INH) and rifampin 2. 2 months of INH, rifampin, pyrazinamide, and ethambutol, followed by 4 months of INH 3. 9 months of INH 4. 12 months of INH ____ 9. Leonard is completing a 6-month regimen to treat tuberculosis (TB). Monitoring of a patient on TB therapy includes: 1. Monthly sputum cultures 2. Monthly chest x-ray 3. Bronchoscopy every 3 months 4. All of the above ____ 10. Compliance with directly observed therapy can be increased by: 1. Convenient clinic times 2. Incentives such as food, clothing, and transportation costs 3. Offering gifts for compliance 4. All of the above Chapter 46. Upper Respiratory Infections, Otitis Media, and Otitis Externa Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. Caleb is an adult with an upper respiratory infection (URI). Treatment for his URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Phenylpropanolamine 4. Topical oxymetazoline ____ 2. Rose is a 3-year-old patient with an upper respiratory infection (URI). Treatment for her URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Pseudoephedrine 4. Nasal saline spray ____ 3. Patients who should be cautious about using decongestants for an upper respiratory infection (URI) include: 1. School-age children 2. Patients with asthma 3. Patients with cardiac disease 4. Patients with allergies ____ 4. Jaheem is a 10-year-old low-risk patient with sinusitis. Treatment for a child with sinusitis is: 1. Amoxicillin 2. Azithromycin 3. Cephalexin 4. Levofloxacin ____ 5. Jacob has been diagnosed with sinusitis. He is the parent of a child in daycare. Treatment for sinusitis in an adult who has a child in daycare is: 1. Azithromycin 500 mg q day for 5 days 2. Amoxicillin-clavulanate 500 mg bid for 7 days 3. Ciprofloxacin 500 mg bid for 5 days 4. Cephalexin 500 mg qid for 5 days ____ 6. The length of treatment for sinusitis in a low-risk patient should be: 1. 5–7 days 2. 7–10 days 3. 14–21 days 4. 7 days beyond when symptoms cease ____ 7. Patient education for a patient who is prescribed antibiotics for sinusitis includes: 1. Use of nasal saline washes 2. Use of inhaled corticosteroids 3. Avoiding the use of ibuprofen while ill 4. Use of laxatives to treat constipation ____ 8. Myles is a 2-year-old patient who has been diagnosed with acute otitis media. He is afebrile and has not been treated with antibiotics recently. First-line treatment for his otitis media would include: 1. Azithromycin 2. Amoxicillin 3. Ceftriaxone 4. Trimethoprim/sulfamethoxazole ____ 9. Alyssa is a 15-month-old patient who has been on amoxicillin for 2 days for acute otitis media. She is still febrile and there is no change in her tympanic membrane examination. What would be the plan of care for her? 1. Continue the amoxicillin for the full 10 days. 2. Change the antibiotic to azithromycin. 3. Change the antibiotic to amoxicillin/clavulanate. 4. Change the antibiotic to trimethoprim/sulfamethoxazole. ____ 10. A child that may warrant “watchful waiting” instead of prescribing an antibiotic for acute otitis media includes patients who: 1. Are low risk with temperature of less than 39oC or 102.2oF 2. Have reliable parents with transportation 3. Are older than age 2 years 4. All of the above ____ 11. Whether prescribing an antibiotic for a child with acute otitis media or not, the parents should be educated about: 1. Using decongestants to provide faster symptom relief 2. Providing adequate pain relief for at least the first 24 hours 3. Using complementary treatments for acute otitis media, such as garlic oil 4. Administering an antihistamine/decongestant combination (Dimetapp) so the child can sleep better ____ 12. First-line therapy for a patient with acute otitis externa (swimmer’s ear) and an intact tympanic membrane includes: 1. Swim-Ear drops 2. Ciprofloxacin and hydrocortisone drops 3. Amoxicillin 4. Gentamicin ophthalmic drops [Show More]
Last updated: 1 year ago
Preview 1 out of pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 14, 2020
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
May 14, 2020
Downloads
0
Views
66

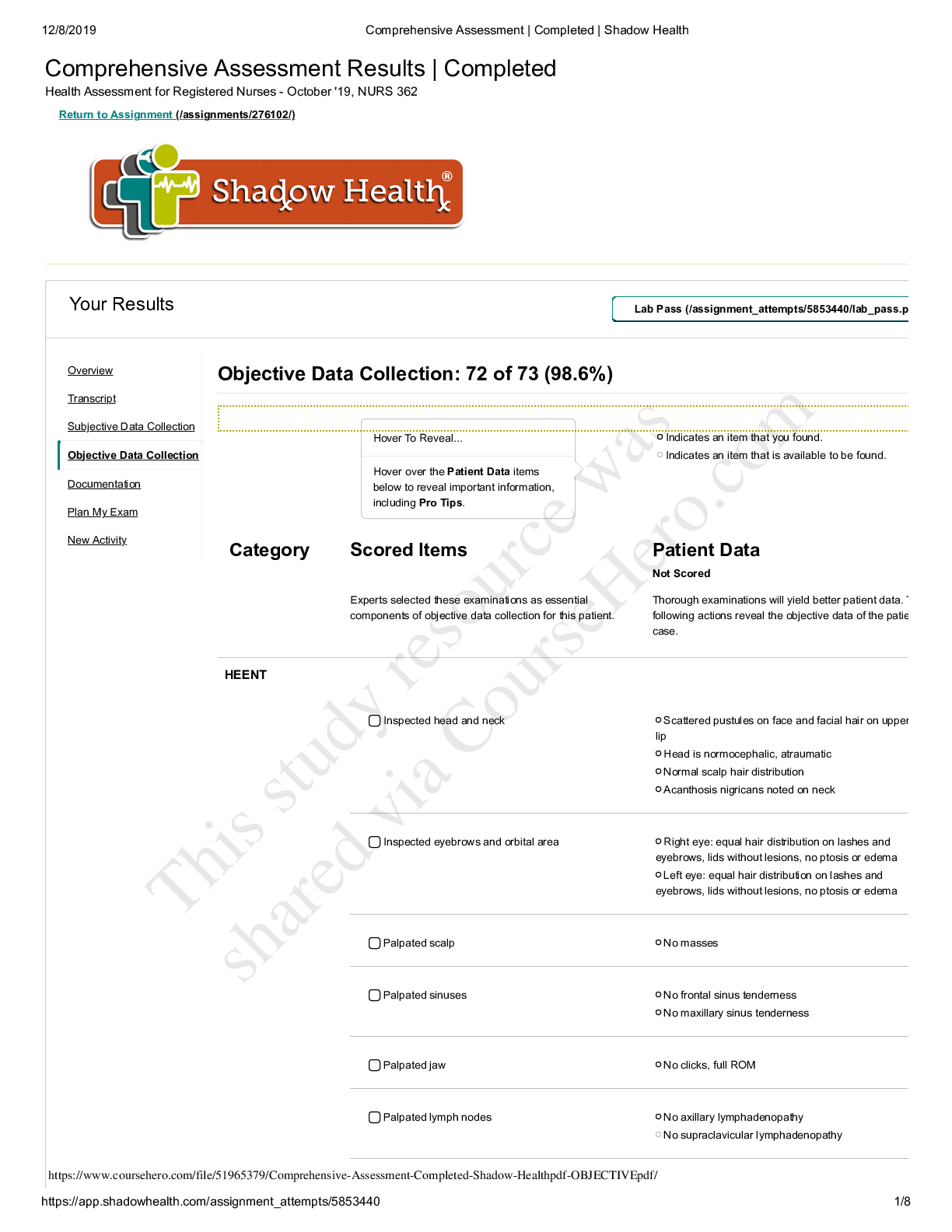
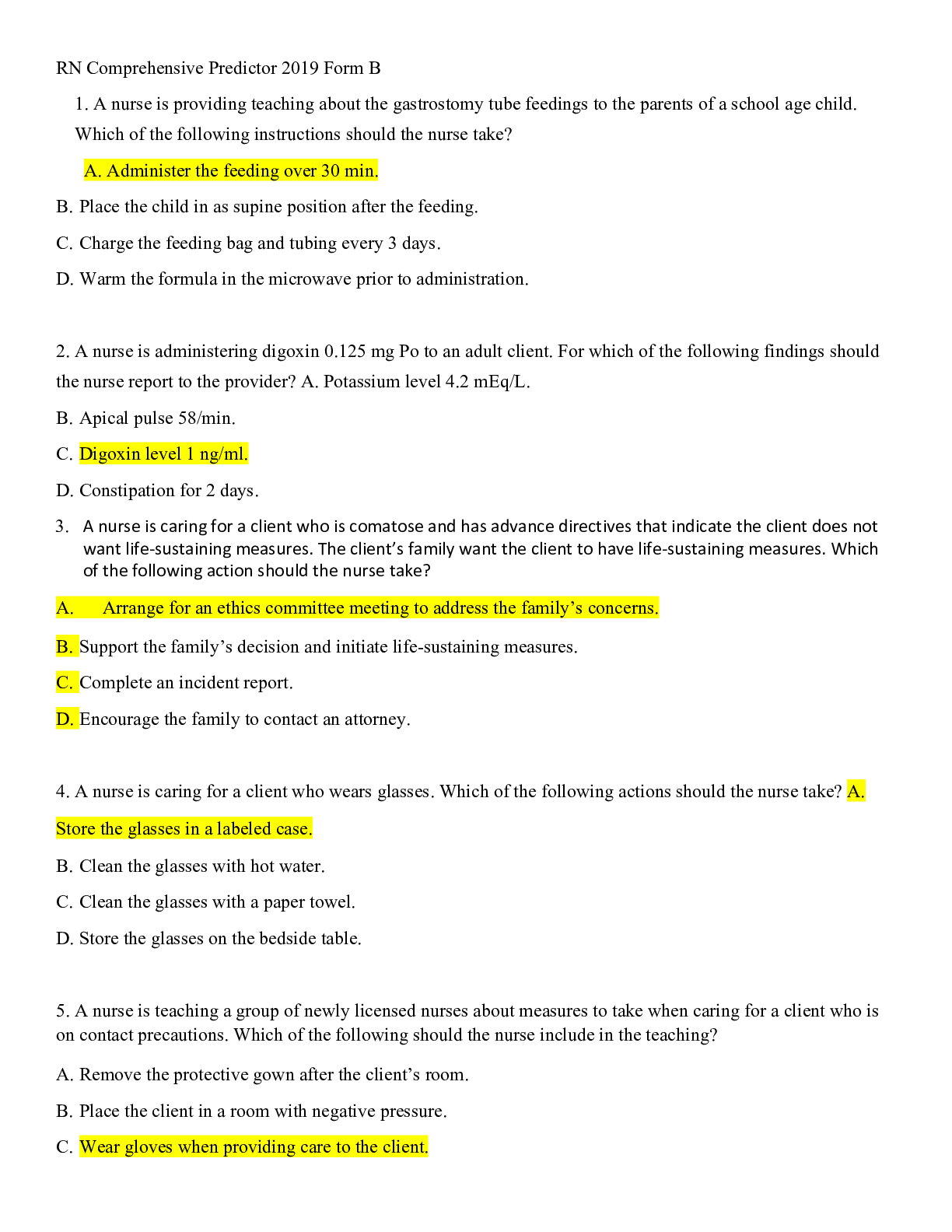

 – CHAMBERLAIN COLLEGE OF NURSING.png)