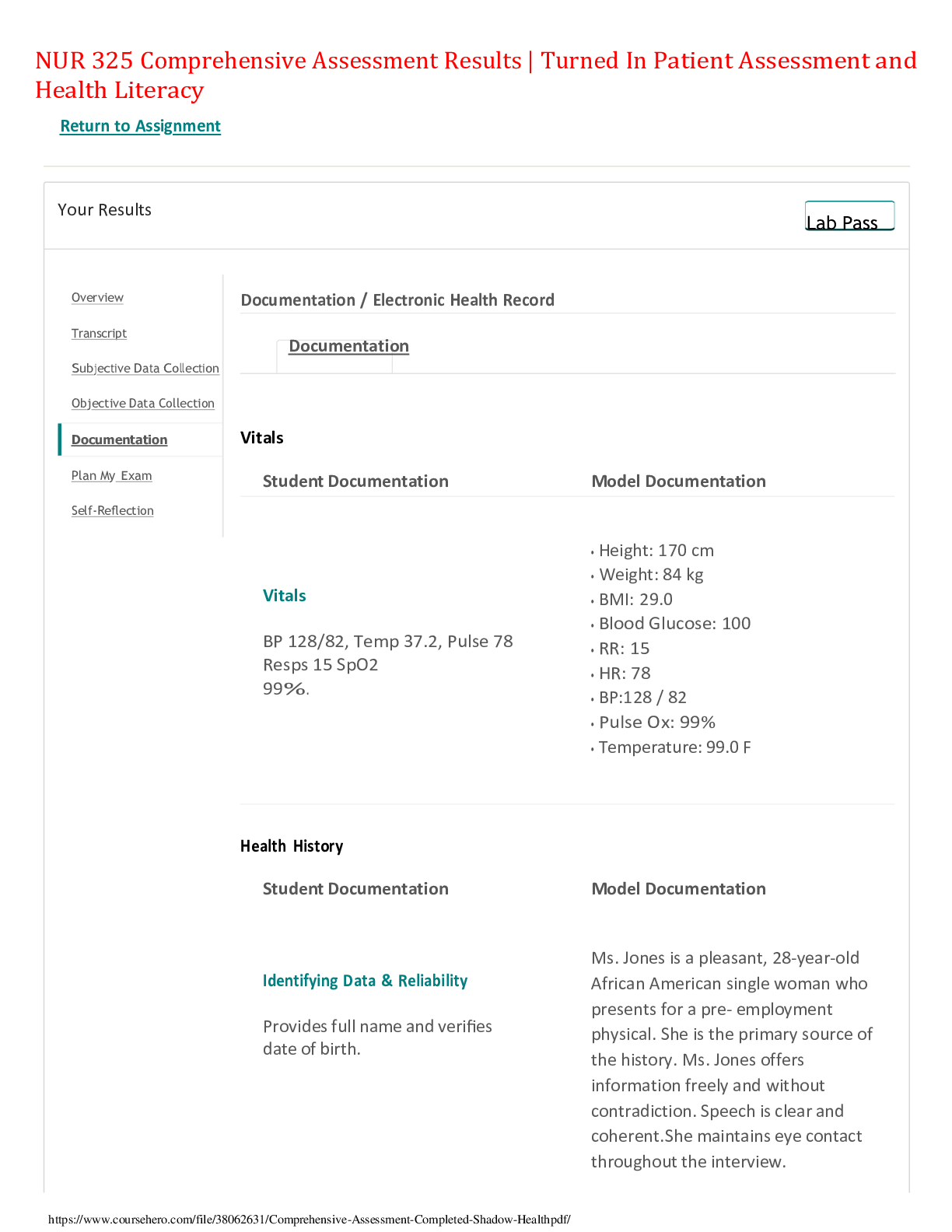
*NURSING > SHADOW HEALTH > NUR 325 Comprehensive Assessment Results | Turned In Patient Assessment and Health Literacy,100% COR (All)
NUR 325 Comprehensive Assessment Results | Turned In Patient Assessment and Health Literacy,100% CORRECT
Document Content and Description Below
NUR 325 Comprehensive Assessment Results | Turned In Patient Assessment and Health Literacy Return to Assignment Your Results Lab Pass Documentation / Electronic Health Record ... Documentation Vitals Student Documentation Model Documentation Vitals BP 128/82, Temp 37.2, Pulse 78 Resps 15 SpO2 99%. • Height: 170 cm • Weight: 84 kg • BMI: 29.0 • Blood Glucose: 100 • RR: 15 • HR: 78 • BP:128 / 82 • Pulse Ox: 99% • Temperature: 99.0 F Health History Student Documentation Model Documentation Identifying Data & Reliability Provides full name and verifies date of birth. Ms. Jones is a pleasant, 28-year-old African American single woman who presents for a pre- employment physical. She is the primary source of the history. Ms. Jones offers information freely and without contradiction. Speech is clear and coherent. She maintains eye contact throughout the interview. General Survey Ms. Jones is a pleasant, well-groomed 28 year old AFrican American female wearing glasses to correct nearsightedness, Ms. Jones is alert and oriented, seated upright on the examination table, and is in no apparent distress. She is well-nourished, well-developed, and dressed appropriately with good hygiene. Reason for Visit Ms. Jones presents to clinic today for a pre- employment physical. "I came in because I'm required to have a recent physical exam for the health insurance at my new job." This study source was downloaded by 100000802531269 from CourseHero.com on 12-03-2022 22:59:57 GMT -06:00 History of Present Illness REports no current health issues. Hx of Asthma (Albuterol); Diabetes (Metformin) and Polycystic Ovaria Syndrome (Yaz). Patient rates current health at an 8/10. Ms. Jones reports that she recently obtained employment at Smith, Stevens, Stewart, Silver & Company. She needs to obtain a pre-employment physical prior to initiating employment. Today she denies any acute concerns. Her last healthcare visit was 4 months ago, when she received her annual gynecological exam at Shadow Health General Clinic. Ms. Jones states that the gynecologist diagnosed her with polycystic ovarian syndrome and prescribed oral contraceptives at that visit, which she is tolerating well. She has type 2 diabetes, which she is controlling with diet, exercise, and metformin, which she just started 5 months ago. She has no medication side effects at this time. She states that she feels healthy, is taking better care of herself than in the past, and is looking forward to beginning the new job. Medications Metformin 850 mg PO BID; Albuterol number of mcg not available on visit; 2-3 puffs INH PRN / asthma; Yaz 1 tab PO daily. Advil OTC 200 mg PO PRN • Metformin, 850 mg PO BID (last use: this morning) • Drospirenone and ethinyl estradiol PO QD (last use: this morning) • Albuterol 90 mcg/spray MDI 1-3 puffs Q4H prn (last use: yesterday) • Acetaminophen 500-1000 mg PO prn (headaches) • Ibuprofen 600 mg PO TID prn (menstrual cramps: last taken 6 weeks ago) Allergies PCN, pediatric onset, rash / urticaria. CAts; asthma exacerbator, runny nose. • Penicillin: rash • Denies food and latex allergies • Allergic to cats and dust. When she is exposed to allergens she states that she has runny nose, itchy and swollen eyes, and increased asthma symptoms. Medical History Dx asthma as a child; triggers exertion and cats. NIDDM treated with Metformin 850 mg PO BID, FBS consistently around 90. Diagnosed with PCOS 4 months ago, Tx with Yaz; regular menses since beginning Yaz, patient reports decrease in hirsutism. Inpatient stay for infected right foot wound 6 months ago, patient denies concerns presently. DEnies surgical history. Reports No pregnancies. Asthma diagnosed at age 2 1/2. She uses her albuterol inhaler when she experiences exacerbations, such as around dust or cats. Her last asthma exacerbation was yesterday, which she resolved with her inhaler. She was last hospitalized for asthma in high school. Never intubated. Type 2 diabetes, diagnosed at age 24. She began metformin 5 months ago and initially had some gastrointestinal side effects which have since dissipated. She monitors her blood sugar once daily in the morning with average readings being around 90. She has a history of hypertension which normalized when she initiated diet and exercise. No surgeries. OB/GYN: Menarche, age 11. First sexual encounter at age 18, sex with men, identifies as heterosexual. Never pregnant. Last menstrual period 2 weeks ago. Diagnosed with PCOS four months ago. For the past four months (after initiating Yaz) cycles regular (every 4 weeks) with moderate bleeding lasting 5 days. Has new male relationship, sexual contact not initiated. She plans to use condoms with sexual activity. Tested negative for HIV/AIDS and STIs four months ago. Health Maintenance Compliant with medication regime, reporting consistent use and consistent time of day. REcent intentional loss of 10 pounds, patient credits lifestyle changes of diet and exercise. Patient exercises 30-40 minutes / day, 4-5 x / week, eats balanced diet and snacks. Monitors blood glucose q AM, reports results typically around 90. Last Pap smear 4 months ago. Last eye exam three months ago. Last dental exam five months ago. PPD (negative) ~2 years ago. Immunizations: Tetanus booster was received within the past year, influenza is not current, and human papillomavirus has been received. She reports that she believes she is up to date on childhood vaccines and received the meningococcal vaccine for college. Safety: Has smoke detectors in the home, wears seatbelt in car, and does not ride a bike. Uses sunscreen. Guns, having belonged to her dad, are in the home, locked in parent’s room. • Mother: age 50, hypertension, elevated cholesterol Family History Father- deceased, MVA. Hx Diabetes Mother, alive, HTN. Paternal Grandfather, deceased Colon cancer, age 60s; Hx HTN, Diabetes. Maternal grandfather: Deceased MI (80 years) HTN, hyperlipidemia. Grandmother Deceased, CVA, HTN. Sister-Asthma • Father: deceased in car accident one year ago at age 58, hypertension, high cholesterol, and type 2 diabetes • Brother (Michael, 25): overweight • Sister (Britney, 14): asthma • Maternal grandmother: died at age 73 of a stroke, history of hypertension, high cholesterol • Maternal grandfather: died at age 78 of a stroke, history of hypertension, high cholesterol • Paternal grandmother: still living, age 82, hypertension • Paternal grandfather: died at age 65 of colon cancer, history of type 2 diabetes • Paternal uncle: alcoholism • Negative for mental illness, other cancers, sudden death, kidney disease, sickle cell anemia, thyroid problems Social History Denies tobacco, nicotine or recreational substance ues. Reports ETOH intake of 2-3 drinks "a couple of times per month." Currently resides with mother and sister, but is moving into her own apartment in one month. Reports new relationship, not yet sexual but patient reports that she anticipates it will become sexual. Reveiwed prevention and testing of STIs. Reports family and Baptist faith is "a big part of my life..." and reports regular attendance at church services and Bible study. Ms. Jones reports having an intimate circle of friends and family who serve in a supportive capacity. Never married, no children. Lived independently since age 19, currently lives with mother and sister in a single family home, but will move into own apartment in one month. Will begin her new position in two weeks at Smith, Stevens, Stewart, Silver, & Company. She enjoys spending time with friends, reading, attending Bible study, volunteering in her church, and dancing. Tina is active in her church and describes a strong family and social support system. She states that family and church help her cope with stress. No tobacco. Cannabis use from age 15 to age 21. Reports no use of cocaine, methamphetamines, and heroin. Uses alcohol when “out with friends, 2-3 times per month,” reports drinking no more than 3 drinks per episode. Typical breakfast is frozen fruit smoothie with unsweetened yogurt, lunch is vegetables with brown rice or sandwich on wheat bread or low-fat pita, dinner is roasted vegetables and a protein, snack is carrot sticks or an apple. Denies coffee intake, but does consume 1-2 diet sodas per day. No recent foreign travel. No pets. Participates in mild to moderate exercise four to five times per week consisting of walking, yoga, or swimming. Mental Health History DEnies ANxiety, DEpression. REports feeling "down" after unexpected deaath of her father in a MVA, but not a "true" depression. Reports healthy coping mechanisms. Reports decreased stress and improved coping abilities have improved previous sleep difficulties. Denies current feelings of depression, anxiety, or thoughts of suicide. Alert and oriented to person, place, and time. Well-groomed, easily engages in conversation and is cooperative. Mood is pleasant. No tics or facial fasciculation. Speech is fluent, words are clear. Review of Systems - General Dx Diabetes, Asthma, PCOS. Denies Pain, H/A, seizures, visual changes, hearing difficulties, reports skin intact, no CV, neurological , musculoskeletal, neuro , GI issues. DEnies concerns with GU, LMP 2 weeks ago, now regular since Dx with PCOS and Tx with Yaz. REports senses of smell, taste and touch intact. No recent or frequent illness, fatigue, fevers, chills, or night sweats. States recent 10 pound weight loss due to diet change and exercise increase. HEENT Student Documentation Model Documentation Subjective Patient reports recent visit for vision screening and received a pair of eyeglasses after evaluatuion. Reports vision is blurry without corrective lenses. DEnies problems with ears, hearing, mouth, chewing, swallowing, sinuses or neck. Denies dizziness, H/A, seizure disorder or CVA. Reports skin discoloration to neck is improving since compliant with lifestyle changes for NIDDM. Reports no current headache and no history of head injury or acute visual changes. Reports no eye pain, itchy eyes, redness, or dry eyes. Wears corrective lenses. Last visit to optometrist 3 months ago. Reports no general ear problems, no change in hearing, ear pain, or discharge. Reports no change in sense of smell, sneezing, epistaxis, sinus pain or pressure, or rhinorrhea. Reports no general mouth problems, changes in taste, dry mouth, pain, sores, issues with gum, tongue, or jaw. No current dental concerns, last dental visit was 5 months ago. Reports no difficulty swallowing, sore throat, voice changes, or swollen nodes. Objective Alert and oriented x 3, follows directions without difficulty, speech clear, hears and responds appropriately. Head shape symmetrical, skin intact. Patent nares. Facial expression appropriate to situation. Skull intact; appropriate size, shape and contour. Hair texture appropriate for ethnicity with normal scalp distribution. Excessive facial hair growth noted to bilateral cheeks (hirsutism); pt. with Dx PCOS. Observed hyperpigmented skin to neck creases. Upper and lower sinuses palpated without pain, nares patent, no nasal flaring noted, nasal mucosa pink, intact and no polyps or drainage noted. TMJ moves freely without clicks. No ptosis, discharge or crusting noted OU, conjunctiva moist and pink, sclera white, PERRLA, cornea and lens clear. Vision 20/20 with corrective lenses worn, peripheral vision intact. Ears properly aligned, tympanic membranes intact, whispered words heard bilaterally. Lips, oral mucosa, gums and palates pink, moist and smooth. Pharynx pink and intact. Tongue pink and rough in appearance, at midline and extends symmetrically. No oral lesions or tenderness noted, gag reflex intact. Tonsils pink and without inflammation or discharge; uvula at midline, rises symmetrically. Trach at midline. Thyroid smooth and without nodules on palpation, no goiter. Neck symmetrical and without crepitus, freely moving with normal ROM. Darkened skin to base of neck. Neck strength 5/5 bilaterally. Carotid pulse 2+ bilaterally, no thrill, no bruits on auscultation. Neck lymph nodes palpated, no tenderness reported. No palpable lymph nodes in supraclavicular region. Head is normocephalic, atraumatic. Bilateral eyes with equal hair distribution on lashes and eyebrows, lids without lesions, no ptosis or edema. Conjunctiva pink, no lesions, white sclera. PERRLA bilaterally. EOMs intact bilaterally, no nystagmus. Mild retinopathic changes on right. Left fundus with sharp disc margins, no hemorrhages. Snellen: 20/20 right eye, 20/20 left eye with corrective lenses. TMs intact and pearly gray bilaterally, positive light reflex. Whispered words heard bilaterally. Frontal and maxillary sinuses nontender to palpation. Nasal mucosa moist and pink, septum midline. Oral mucosa moist without ulcerations or lesions, uvula rises midline on phonation. Gag reflex intact. Dentition without evidence of caries or infection. Tonsils 2+ bilaterally. Thyroid smooth without nodules, no goiter. No lymphadenopathy. Respiratory Student Documentation Model Documentation Subjective Pt with Dx asthma triggered by cats, exertion; well- controlled with PRN proventil inhaler. Reports using inhaler 2-3 puffs PRN, typical use 1-2 x/ week. Last needed yesterday for exposure to cats. Reports no shortness of breath, wheezing, chest pain, dyspnea, or cough. Objective Resps even and unlabored with symmetrical chest expansion and contraction, no accessory muscle use noted, nares patent, no nasal flaring. No barrell chest noted, no clubbing of finger nails noted. Lungs COA bilaterally with bronchovesicular sounds midline and vesicular sounds to periphery. DEnies cough. Palpated fremitus, resonance all fields. FVC 3.91 L, FeV1 3.15 L. Chest is symmetric with respiration, clear to auscultation bilaterally without cough or wheeze. Resonant to percussion throughout. In office spirometry: FVC 3.91 L, FEV1/FVC ratio 80.56%. Cardiovascular Student Documentation Model Documentation Subjective DEnies heart history, palpitations, circulation issues. REports previously hypertensive but "it's OK now" after MD appointment. Reports no palpitations, tachycardia, easy bruising, or edema. Objective Denies chest pain or discomfort, edema. Heart sounds as anticipated, regular rhythm, no gallups, murmurs, rubs, thrills or bruits noted. PMI nondisplaced, no heaves or lifts. Carotid, brachial, radial pulses, dorsalis pedis, popliteal, tibial and femoral pulses palpable, strong 2+ and equal bilaterally. No Sx of arterial occlusion or DVT. Cap refill <3 seconds x 4 extremities. Heart rate is regular, S1, S2, without murmurs, gallops, or rubs. Bilateral carotids equal bilaterally without bruit. PMI at the midclavicular line, 5th intercostal space, no heaves or lifts. Bilateral peripheral pulses equal bilaterally, capillary refill less than 3 seconds. No peripheral edema. Abdominal Student Documentation Model Documentation Subjective Denies abdominal pain, nausea, vomiting, constipation, diarrhea, flatulence and incontinence. Denies difficulties, pain, ferquency, nocturia and hematuria with urination, reports menstrual cycles are regular since starting on Yaz oral contraceptives to treat Dx PCOS. Gastrointestinal: Reports no nausea, vomiting, pain, constipation, diarrhea, or excessive flatulence. No food intolerances. Genitourinary: Reports no dysuria, nocturia, polyuria, hematuria, flank pain, vaginal discharge or itching. Objective Striae noted on inspection; excessive hair growth to lower abdomen. Skin intact. BS+ and WNLs x 4 quads. Percussion x 4 quads: tympanic over all quads; no dullness noted on percussion to splenic region. Liver span percussed at 7cm with liver palp 1 cm below right costal margin. Light palpation x 4 quads reveals softness, no masses over all quads. Deep palpation reveals no masses x 4 quads. Kidney and spleen nonpalpable, no tenderness Bilat CVA. Abdomen protuberant, symmetric, no visible masses, scars, or lesions, coarse hair from pubis to umbilicus. Bowel sounds are normoactive in all four quadrants. Tympanic throughout to percussion. No tenderness or guarding to palpation. No organomegaly. No CVA tenderness. Musculoskeletal Student Documentation Model Documentation Subjective Denies muscle or joint pain, denies muscle weakness or swelling. Reports no muscle pain, joint pain, muscle weakness, or swelling. Objective Neck strength bilaterally 5/5, ROM WNLs. Jaw without clicks, full ROM. Full spinal ROM on extension, flexion and rotation bilaterally. Hand, wrist, elbow and shoulder strength 5/5 bilaterally with full ROM to bilateral wrists, elbows and shoulders. Bilateral ankle, knees and hip strength 5/5 with full ROM bilaterally. Ambulates without difficulty. Bilateral upper and lower extremities without swelling, masses, or deformity and with full range of motion. No pain with movement. Neurological Student Documentation Model Documentation Subjective Denies dizziness, vision changes, numbness, tingling, loss of coordination, sensation, denies history of seizures. Reports sometimes being clumsy. Hx of a slip from a ladder 6 months ago resulting in a scrape which became septic; hospitalized for anti-infectives at Shadow General Hospital; denies issues currently. Reports no dizziness, light-headedness, tingling, loss of coordination or sensation, seizures, or sense of disequilibrium. Student Documentation Model Documentation Objective A&O x 3, hears and follows directions with ease and responds appropriately. Short and long term memory intact, good historian, speech clear. Finger to nose test accurate, rapid alternating movements smooth and intact. Correct responses bilaterally on sterognosis and graphesthesia and upper extremity and left lower extremity position sense , unsure of response to R lower extremity position sense, responding. "I think that was up" Accurately reports dull, sharp and soft sensations to Bilateral upper extremities, chest and left lower extremity. Monofilament test reveals diminished sensation to bilateral forefoot, intact at heel. Bilateral heel to shin movements WNLs. DTRs 2+ to bilateral brachioradialis, biceps, triceps, bilateral ankles and knees. Strength 5/5 bilateral upper and lower extremities. Normal graphesthesia, stereognosis, and rapid alternating movements bilaterally. Tests of cerebellar function normal. DTRs 2+ and equal bilaterally in upper and lower extremities. Decreased sensation to monofilament in bilateral plantar surfaces. Skin, Hair & Nails Student Documentation Model Documentation Subjective Reports improvement with hirsutism, acne, neck hyperpigmentation since Dx with PCOS and Tx with oral contraceptives. Denies hair loss to scalp. Denies rashes, lesions or abrasions. Denies history of sunburn. Reports improved acne due to oral contraceptives. Skin on neck has stopped darkening and facial and body hair has improved. She reports a few moles but no other hair or nail changes. Objective Skin pink, warm, dry, and intact. Hair well groomed. Denies rashes, sores. Reports dry skin and utilization of lotion regularly. Cap refill <3 seconds x 10 digits. Nails smooth, intact and without clubbing. Discoloration at neck noted. Scattered pustules on face and facial hair on upper lip, acanthosis nigricans on posterior neck. © Shadow Health® 2018 [Show More]
Last updated: 1 year ago
Preview 1 out of 17 pages
Reviews( 0 )
Recommended For You
*NURSING> SHADOW HEALTH > Musculoskeletal Results | Turned In Advanced Health Assessment -Clinical Replacement, NURS 520 ALL ANSWERS. Score 97% (All)
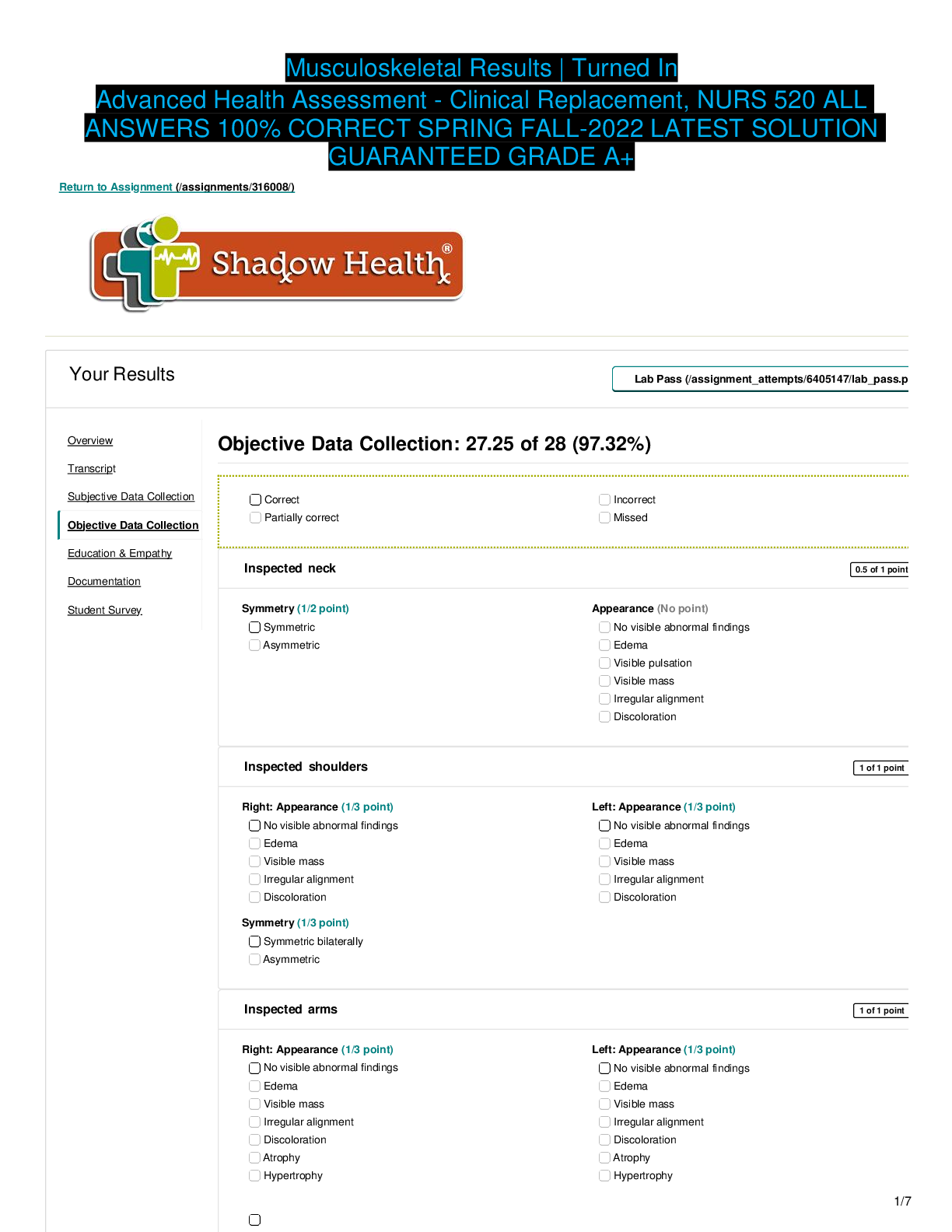
Musculoskeletal Results | Turned In Advanced Health Assessment -Clinical Replacement, NURS 520 ALL ANSWERS. Score 97%
Inspected neck 0.5 of 1 point Student Survey Symmetry (1/2 point) Symmetric Asymmetric Appearance (No point) No visible abnormal findings Edema Visible pulsation Visible mass Irregular...
By Allan100 , Uploaded: Aug 03, 2022
$11
*NURSING> SHADOW HEALTH > Neurological Results | Turned In Advanced Health Assessment - Chamberlain, NR509 ALL ANSWERS. Score 99.32% (All)
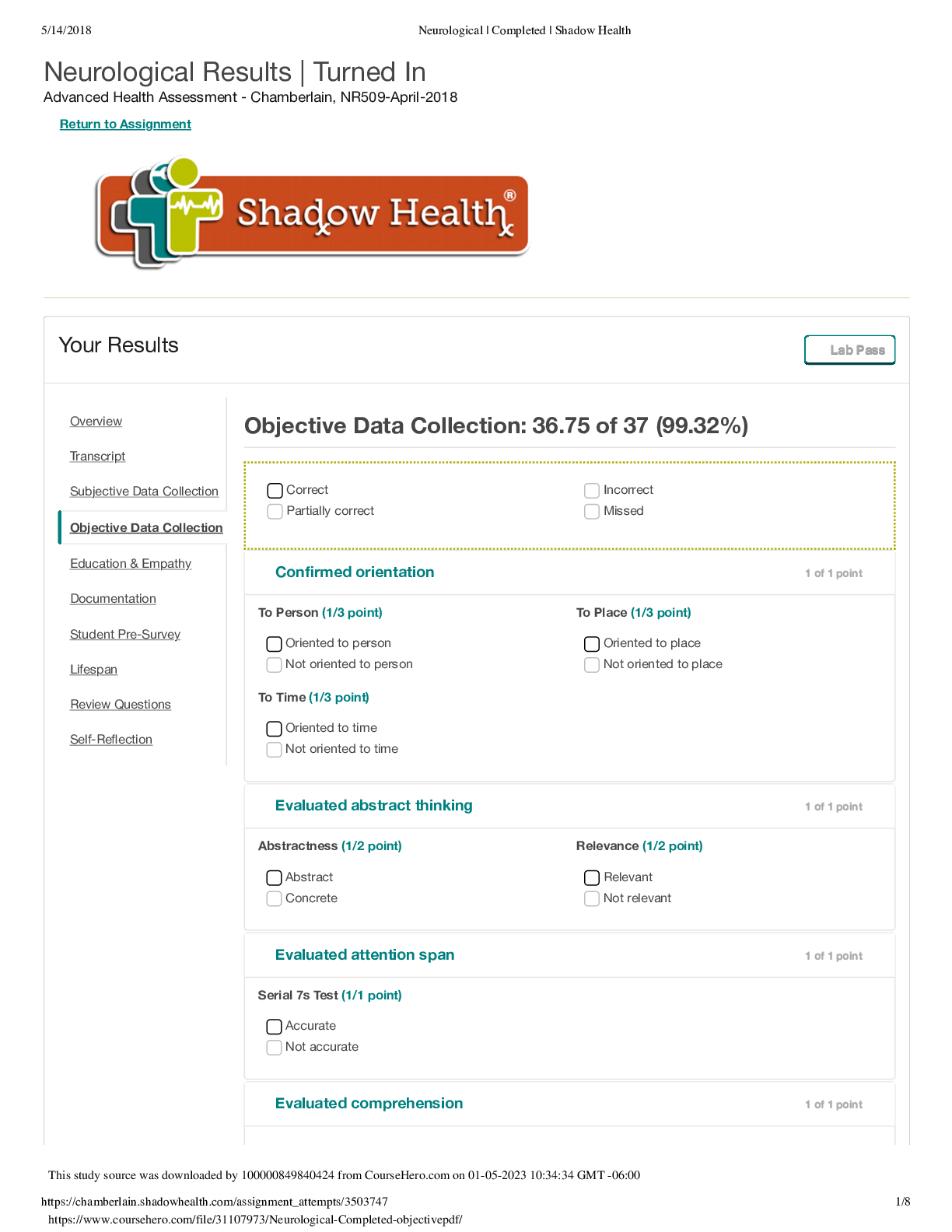
Neurological Results | Turned In Advanced Health Assessment - Chamberlain, NR509 ALL ANSWERS. Score 99.32%
Confirmed orientation 1 of 1 point To Person (1/3 point) To Place (1/3 point) Oriented to person Oriented to place Not oriented to person Not oriented to place To Time (1/3 point)...
By Allan100 , Uploaded: Aug 03, 2022
$13
*NURSING> SHADOW HEALTH > Shadow Health Comprehensive Assessment Transcript Tina Jones. Comprehensive Assessment Results. NR 509 Charmberlain University. (All)
Shadow Health Comprehensive Assessment Transcript Tina Jones. Comprehensive Assessment Results. NR 509 Charmberlain University.
Shadow Health Comprehensive Assessment Transcript Tina Jones. Comprehensive Assessment Results. NR 509 Charmberlain University.
By Expert1 , Uploaded: Aug 02, 2020
$11.5
*NURSING> SHADOW HEALTH > Focused Exam: Hypertension and Type 2 Diabetes Results | Turned In Differential Diagnosis & Primary Care Practicum (All)
Focused Exam: Hypertension and Type 2 Diabetes Results | Turned In Differential Diagnosis & Primary Care Practicum
Focused Exam: Hypertension and Type 2 Diabetes Results | Turned In Differential Diagnosis & Primary Care Practicum - May 2020, NR511-April-2020 Return to Assignment (/assignments/328814/) Yo...
By Stuvia , Uploaded: Aug 02, 2022
$14
*NURSING> SHADOW HEALTH > Comprehensive Assessment Results | Turned InNursing 562/562L Advanced Health Assessment - Spring 2021, N5622 (All)
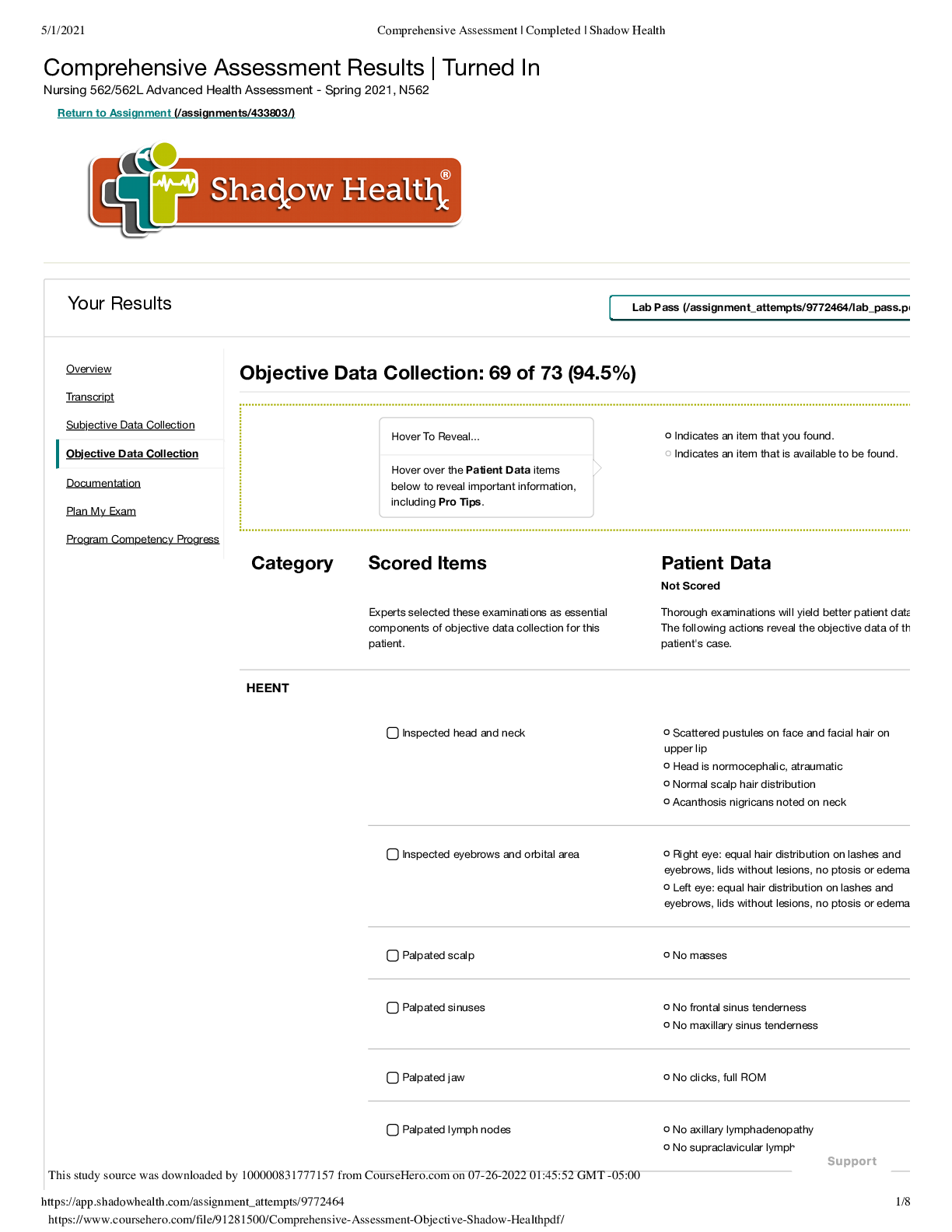
Comprehensive Assessment Results | Turned InNursing 562/562L Advanced Health Assessment - Spring 2021, N5622
Comprehensive Assessment Results | Turned InNursing 562/562L Advanced Health Assessment - Spring 2021, N56
By markstudys , Uploaded: Jul 26, 2022
$11
Health Care> SHADOW HEALTH > Week 4 - Health History Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP - February 2020, nurs6512-usw1.504.202050 (All)
Week 4 - Health History Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP - February 2020, nurs6512-usw1.504.202050
Week 4 - Health History Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP - February 2020, nurs6512-usw1.504.202050
By markstudys , Uploaded: Jul 26, 2022
$12
*NURSING> SHADOW HEALTH > Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP (Section N-12) - February 2021, nurs6512-usw1.31747.202150 (All)
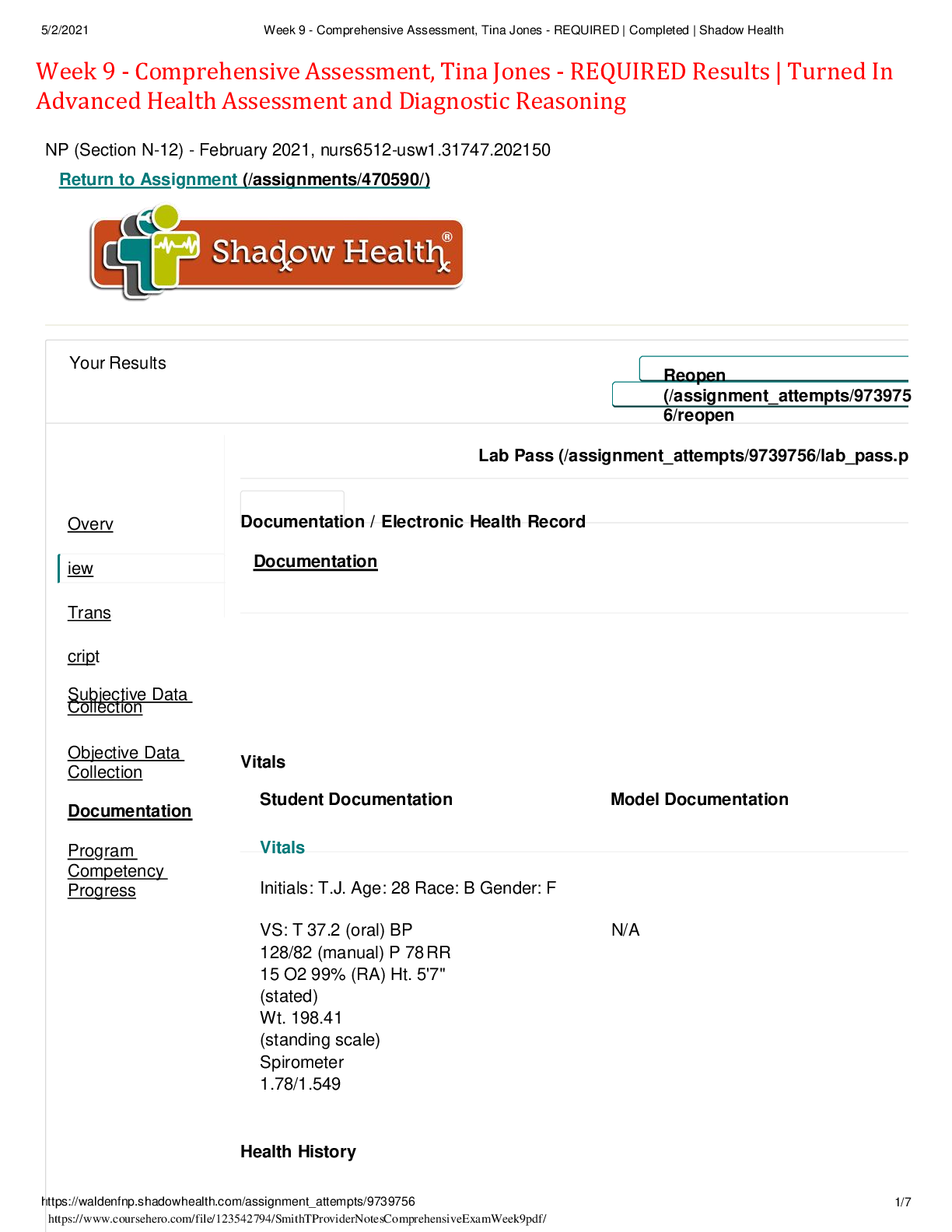
Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP (Section N-12) - February 2021, nurs6512-usw1.31747.202150
Week 9 - Comprehensive Assessment, Tina Jones - REQUIRED Results | Turned InAdvanced Health Assessment and Diagnostic Reasoning - NP (Section N-12) - February 2021, nurs6512-usw1.31747.202150
By markstudys , Uploaded: Jul 26, 2022
$11
*NURSING> SHADOW HEALTH > Focused Exam: Abdominal Pain Results | Turned In Health Assessment Simulations - Spring 2020 (All)
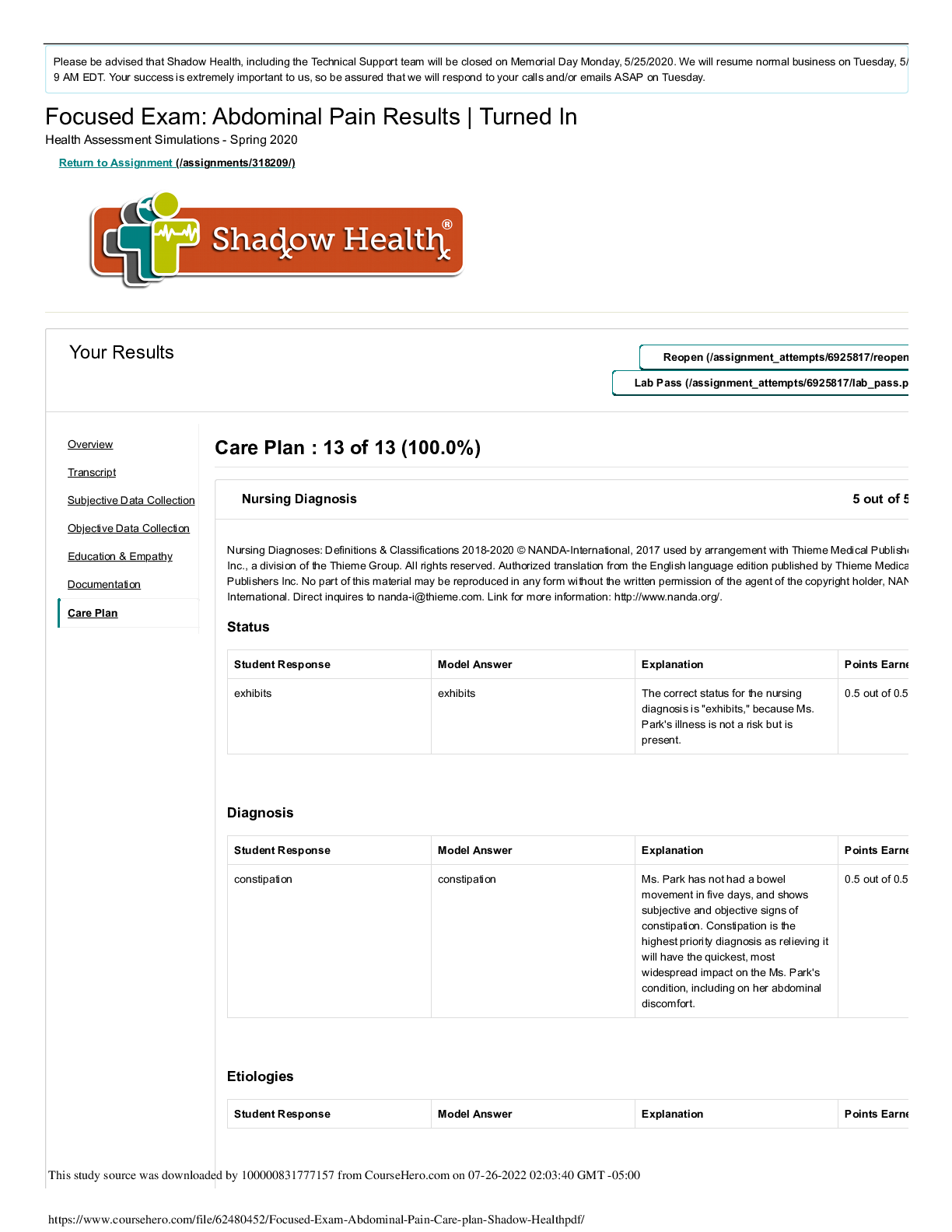
Focused Exam: Abdominal Pain Results | Turned In Health Assessment Simulations - Spring 2020
Focused Exam: Abdominal Pain Results | Turned In Health Assessment Simulations - Spring 2020
By markstudys , Uploaded: Jul 26, 2022
$11
*NURSING> SHADOW HEALTH > Comprehensive Assessment Results | Turned InAdvanced Health Assessment - Chamberlain, NR509-April-2018 (All)
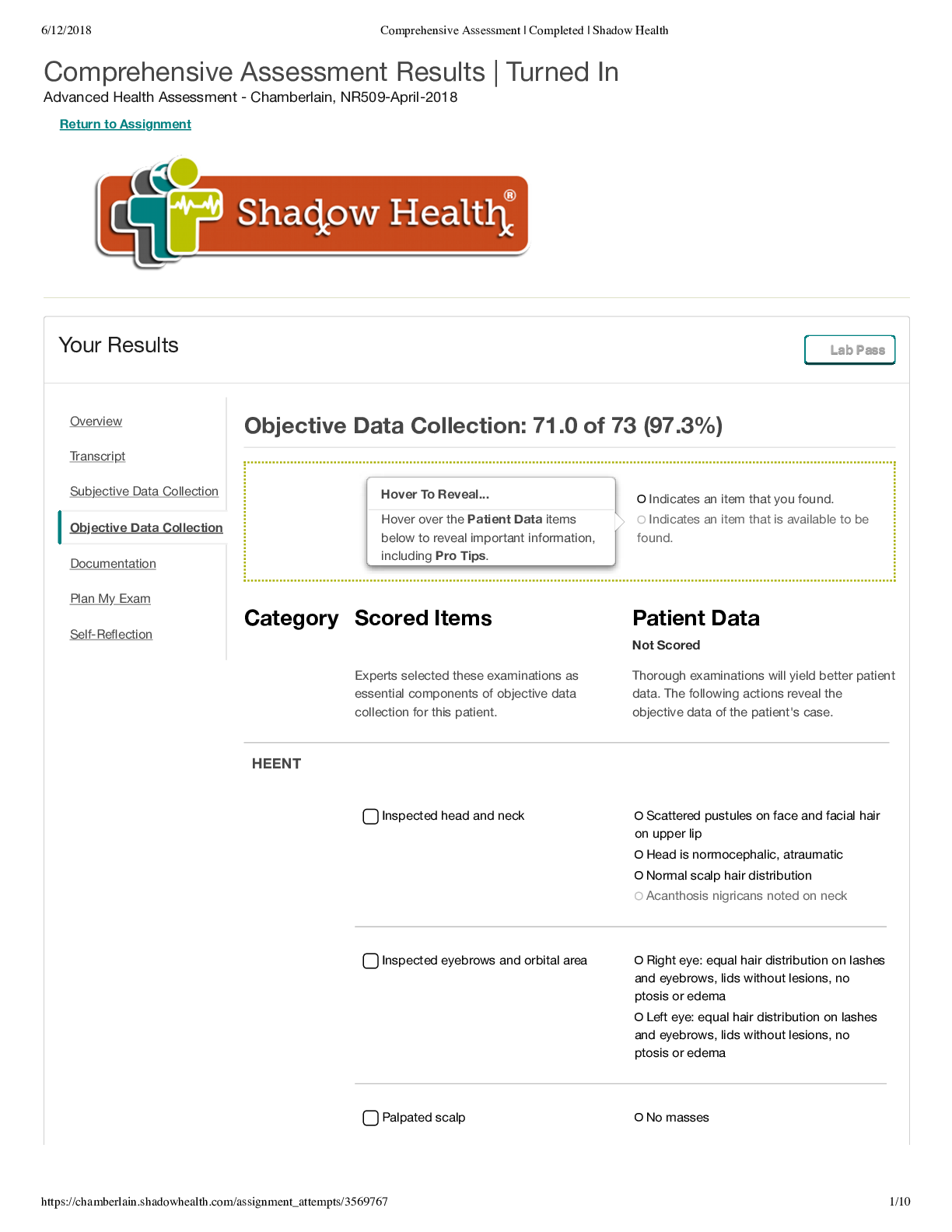
Comprehensive Assessment Results | Turned InAdvanced Health Assessment - Chamberlain, NR509-April-2018
Comprehensive Assessment Results | Turned InAdvanced Health Assessment - Chamberlain, NR509-April-2018
By markstudys , Uploaded: Jul 26, 2022
$11
*NURSING> SHADOW HEALTH > Shadow health Focused Exam: Chest Pain Results | Turned In Advanced Health Assessment (All)

Shadow health Focused Exam: Chest Pain Results | Turned In Advanced Health Assessment
Shadow health Focused Exam: Chest Pain Results | Turned In Advanced Health Assessment
By Nightingale , Uploaded: Jul 08, 2022
$6
Document information
Connected school, study & course
About the document
Uploaded On
Dec 04, 2022
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Dec 04, 2022
Downloads
0
Views
39