*NURSING > SOAP NOTE > Herzing University NU 627 Soap Note #6 Daisy Lara November 30, 2013 Type of Site: Primary Care Offic (All)
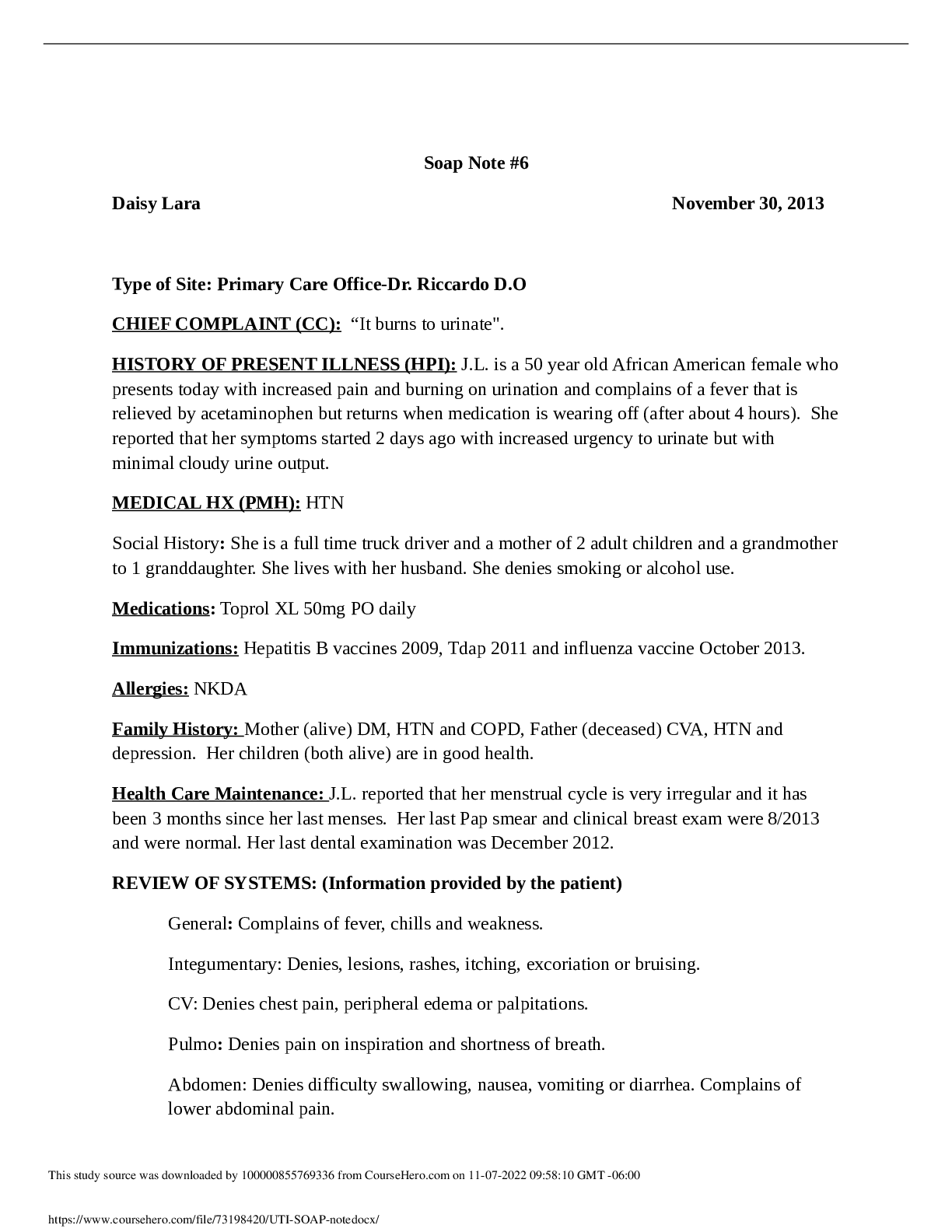
Herzing University NU 627 Soap Note #6 Daisy Lara November 30, 2013 Type of Site: Primary Care Office-Dr. Riccardo D.O CHIEF COMPLAINT (CC): “It burns to urinate".
Document Content and Description Below
Herzing University NU 627 Soap Note #6 Daisy Lara November 30, 2013 Type of Site: Primary Care Office-Dr. Riccardo D.O CHIEF COMPLAINT (CC): “It burns to urinate". HISTORY OF PRESENT ILLNESS... (HPI): J.L. is a 50 year old African American female who presents today with increased pain and burning on urination and complains of a fever that is relieved by acetaminophen but returns when medication is wearing off (after about 4 hours). She reported that her symptoms started 2 days ago with increased urgency to urinate but with minimal cloudy urine output. MEDICAL HX (PMH): HTN Social History: She is a full time truck driver and a mother of 2 adult children and a grandmother to 1 granddaughter. She lives with her husband. She denies smoking or alcohol use. Medications: Toprol XL 50mg PO daily Immunizations: Hepatitis B vaccines 2009, Tdap 2011 and influenza vaccine October 2013. Allergies: NKDA Family History: Mother (alive) DM, HTN and COPD, Father (deceased) CVA, HTN and depression. Her children (both alive) are in good health. Health Care Maintenance: J.L. reported that her menstrual cycle is very irregular and it has been 3 months since her last menses. Her last Pap smear and clinical breast exam were 8/2013 and were normal. Her last dental examination was December 2012. REVIEW OF SYSTEMS: (Information provided by the patient) General: Complains of fever, chills and weakness. Integumentary: Denies, lesions, rashes, itching, excoriation or bruising. CV: Denies chest pain, peripheral edema or palpitations. Pulmo: Denies pain on inspiration and shortness of breath. Abdomen: Denies difficulty swallowing, nausea, vomiting or diarrhea. Complains of lower abdominal pain. GU: Denies vaginal discharge, hematuria, polyuria or incontinence. Complains of foul smelling urine, pain and burning on urination, urinary hesitancy, urgency and dysuria. Musculoskeletal: Denies flank pain, joint pain, muscle pain and decrease in range of motion. Neuro- Denies dizziness or headaches. Psych- Denies feeling depressed or anxious. PHYSICAL EXAM: BP: 125/87, HR: 92, Temp: 100.2 F, Pulse Oximetry: 99% on room air, respirations: 22 per minute, Height: 5 feet and 4 inches, Weight: 167 pounds, BMI: 28.7 kg/m2 (overweight) APPEARANCE: J.L looks younger than her stated age. She is sitting upright on the examination table. She is over dressed for the weather. She is alert and oriented to person, place and time. Her affect is appropriate and speaks in a low tone. She has good insight, is attentive, answers and asks questions appropriately. HEENT: Head: Normocephalic and atraumatic with normal strength and tone of facial muscles. She does not have lesions, rashes, deformities or dandruff to scalp. Eyes: Her conjunctiva are pink and sclera is white bilaterally. Eyes are without discharge or redness. No papilledema or lesions bilaterally. PERRLA bilaterally. She follows all 6 cardinal movements of gaze without nyastagmus bilaterally. The cover and uncover eye test is negative for strabismus bilaterally. Ears: Symmetrical bilaterally. Normal pinnae without rashes, scars or masses bilaterally. Her TMs are gray, non-bulging and freely mobile bilaterally. Hearing is normal. Nose: Normal shape and appearance. The nares are patent without inflammation of the turbinates. The nasal mucosa is moist and pink in bilateral nares. Throat: Mouth has good dentition, without foul breath and with pink and moist oral mucosa. The posterior oropharynx has no erythema, exudate, lesions or cobblestoning. Her tongue is midline. NECK: Her neck is supple with trachea at midline; no difficulty swallowing and the thyroid is non-tender on palpation. No lymphadenopathy noted. CV: Her skin is consistent with a black female without paleness, or mottling of the face or hands. No carotid bruits. Capillary refill to her nail beds are quick and less than 3 seconds. Chest is symmetrical. S1 and S2 were auscultated. No thrills, murmurs or gallops heard. PMI heard at the apex at the mid-clavicular line 5th intercostal space. Positive and strong radial, ulnar, brachial, femoral, popliteal, dorsalis pedis and posterior tibial pulses. No edema to the peripheral extremities. Pulmo: Lungs sounds are clear in bilateral lung fields. No use of accessory muscles and no signs of respiratory distress. No nasal flaring or cyanosis. The nail beds are at 180 degrees without clubbing or deformities. Abdomen: Abdomen is symmetric, round and old striae are present throughout the abdomen. No visible peristalsis, abnormal pulsations or hernias. Normal bowel sounds in all four quadrants. Tenderness on palpation of the lower abdomen. Percussion revealed tympany over the abdomen and dullness over the liver and the spleen. Pelvic/GU/Rectal: No tenderness to the costovertebral angle with blunt percussion. Tenderness on palpation in the suprapubic area. Pelvic and Rectal assessment deferred. Musculoskeletal: No tenderness on palpation of lower back and flank area. No tenderness to her bilateral upper and lower extremities. Normal range of motion and a steady gait. [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > Walden University - NURS 6512_SOAP Week4. Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest and Annual physical and my psoriasis. All Parts Complete (All)

Walden University - NURS 6512_SOAP Week4. Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest and Annual physical and my psoriasis. All Parts Complete
SLIDE 2: Patient Initials: __MP_____ Age: ___68____ Gender: _M SUBJECTIVE DATA: Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest History of Present Ill...
By QuizMaster , Uploaded: Jul 29, 2020
$8
*NURSING> SOAP NOTE > Walden University - NURS 6512: SOAP Week4: Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest and Annual physical and my psoriasis. All Parts Complete (All)
Walden University - NURS 6512: SOAP Week4: Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest and Annual physical and my psoriasis. All Parts Complete
Walden University - NURS 6512: SOAP Week4: Chief Complaint (CC): Annual physical and multiple hard red bumps on my chest and Annual physical and my psoriasis. All Parts Complete Walden University - N...
By VERIFIED A+ , Uploaded: Jun 26, 2021
$14
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Health Care> SOAP NOTE > Caroline Casey SOAP (All)
Caroline Casey SOAP
Caroline Casey SOAP
By Ellen Ronald , Uploaded: Jul 29, 2022
$8
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By MARKALLAN , Uploaded: Jul 20, 2022
$9
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Nancylect , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Prof.Pierro , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > BACTERIAL VAGINOSIS SOAP NOTE (All)
.png)
BACTERIAL VAGINOSIS SOAP NOTE
BACTERIAL VAGINOSIS SOAP NOTE KL is a 25-year old female of a Caucasian decent
By Topmentor , Uploaded: Jul 12, 2022
$10
Document information
Connected school, study & course
About the document
Uploaded On
Nov 07, 2022
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Nov 07, 2022
Downloads
0
Views
44