*NURSING > SOAP NOTE > NR 341 SOAP Note- Urinary Tract Infection SUBJECTIVE DATA Chief Complaint: “Burning and pain with (All)
NR 341 SOAP Note- Urinary Tract Infection SUBJECTIVE DATA Chief Complaint: “Burning and pain with urination”
Document Content and Description Below
University of Texas NR 341 SOAP Note- Urinary Tract Infection SUBJECTIVE DATA Chief Complaint: “Burning and pain with urination” History of present illness: 27 y/o patient presents with c/o... severe pain and burning with urination. Patient also reports unusually frequent urination, increased urge to urinate and cloudy urine with a foul smell. Patient states that the symptoms began four days ago and have worsened over the past four days. Patient noticed that she was going to the bathroom more than normal (eight to ten times daily) and is unable to produce urine sometimes. Yesterday, she started experiencing mild pain in the suprapubic area which led her into seeking medical advice. She reports that the pain gets worse when she feels the urge to urinate and it alleviates between urgency episodes. Patient rates her pain as 5/10. Patient denies nausea, chills, vomiting, fever, flank pain, back pain/myalgia, blood in urine, vaginal irritation/pruritus and vaginal discharge. Patient is sexually active, has had the same partner (husband) for the past three years. Past medical history: Childhood and adult illness: No major health problems except for minor fever and cold. No history of chronic illnesses or conditions Surgeries: None Medications: None Allergies: No known drug or food allergies Immunization: Up to date with all immunizations Family history: Father has type 2 diabetes mellitus. Mother has hypertension and history of UTIs. Elder sister has hypertension. Other siblings and patient’s children are alive and well. No family history of cancer Social history: Patient lives with husband and son. She works as a teller at one of the local banks. Patient reports that she takes alcohol occasionally. Denies the use of tobacco and illicit drugs Review of systems: General: Patient denies generalized weakness, chills, fever, unexplained weight loss or gain and generalized weakness Eyes: Denies changes in vision, blurry vision or double vision Ears, nose & throat: No changes in hearing, hearing problems, congestion, and sore throat Respiratory: No cough, SOB, or wheezing. No history of seasonal allergies or asthma Cardiovascular: Denies chest pain, edema, palpitations, rapid heart rate, or orthopnea Gastrointestinal: c/o moderate pain in the suprapubic area. Denies N/V/D Genitourinary: c/o urgency, urinary frequency as well as dysuria for the past four days. Denies vaginal discharge or vulvar irritation. Denies a history of urinary tract infection. Patient is sexually active; married. Denies a history of STIs. Denies dyspareunia. Patient has been occasionally using spermicide-coated condoms for contraception Skin: Denies rashes, new moles, delayed healing, bruising, skin discoloration, or lesions Musculoskeletal: No back pain, myalgia, joint swelling or pain Neurologic: No changes in memory Psychiatric: No changes in mood Heme/Lymph: Denies swollen glands, increased thirst, increase hunger, cold or heat intolerance, or easy bruising OBJECTIVE DATA Physical exam Vitals: Temp- 37.9, Pulse- 74, Resp-18, O2- 98% RA, BP- 117/78, weight-120 lb., height- 63 inches, BMI-21.3 General: Well developed and nourished adult female in so acute distress. Alert and oriented X3. Well groomed Eyes: PERRLA, EOMs intact. Lymph nodes: no lymphadenopathy Skin: Skin is warm, dry, and intact. No rashes [Show More]
Last updated: 1 year ago
Preview 1 out of 7 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
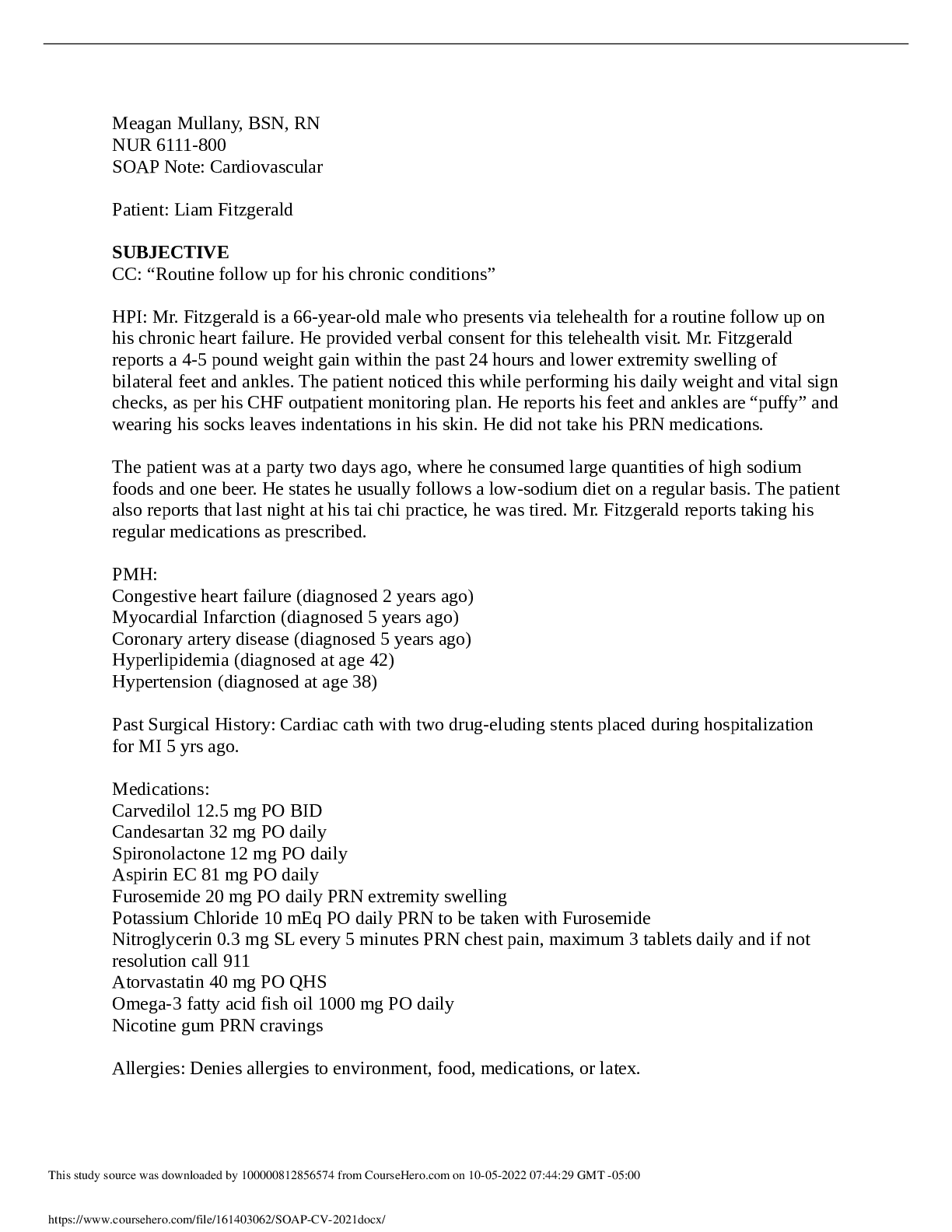
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Health Care> SOAP NOTE > Caroline Casey SOAP (All)
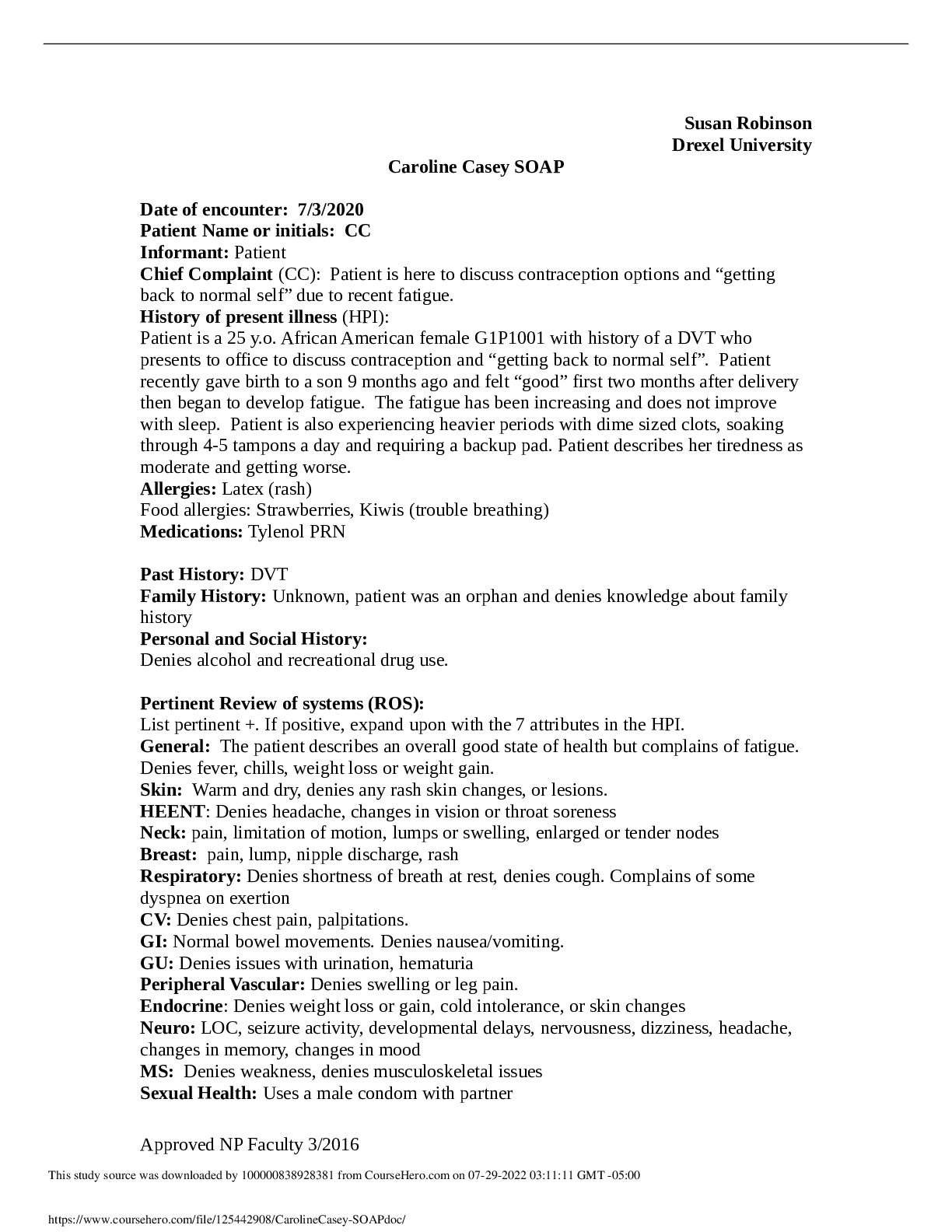
Caroline Casey SOAP
Caroline Casey SOAP
By Ellen Ronald , Uploaded: Jul 29, 2022
$8
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Nancylect , Uploaded: Jul 20, 2022
$9
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By MARKALLAN , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Prof.Pierro , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > ADULT 620 Week 4 make up SOAP note clinical patient (All)
ADULT 620 Week 4 make up SOAP note clinical patient
ADULT 620 Week 4 make up SOAP note clinical patient Chief Complaint The patient presents in the clinic today with complaints of loss of voice 6 days ago, has rhinitis and congestion. Says has just...
By Topmentor , Uploaded: Jul 12, 2022
$10
*NURSING> SOAP NOTE > BACTERIAL VAGINOSIS SOAP NOTE (All)
.png)
BACTERIAL VAGINOSIS SOAP NOTE
BACTERIAL VAGINOSIS SOAP NOTE KL is a 25-year old female of a Caucasian decent
By Topmentor , Uploaded: Jul 12, 2022
$10
*NURSING> SOAP NOTE > Week 6 SOAP note Patient Initials P.R. A 94 year old female (All)
Week 6 SOAP note Patient Initials P.R. A 94 year old female
Week 6 SOAP note Patient Initials P.R. A 94 year old female Chief Complaint Follow-up from last week on peri-area rash. Patient states was in the hospital with a catheter, then in rehab was given ‘...
By Topmentor , Uploaded: Jul 12, 2022
$10
Document information
Connected school, study & course
About the document
Uploaded On
Nov 07, 2022
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
Nov 07, 2022
Downloads
0
Views
59