*NURSING > SOAP NOTE > NURSING 101 UTI SOAP NOTE Demographic Information: Patient Initials: J. D. Age: 26 Sex: Male Race: (All)
NURSING 101 UTI SOAP NOTE Demographic Information: Patient Initials: J. D. Age: 26 Sex: Male Race: African American Subjective (S). CC: “I have been experiencing pain and burning sensations when urinating”
Document Content and Description Below
NURSING 101 UTI SOAP NOTE Demographic Information: Patient Initials: J. D. Age: 26 Sex: Male Race: African American Subjective (S). CC: “I have been experiencing pain and burning sensatio... ns when urinating” HPI: J. D. is a 26-year-old African American male who presented to the clinic with a one-week history of painful urination and a burning sensation. The pain is aggravated by the urge to urinate and alleviates between urgency episodes and he rates the pain at 4 on a scale of 0-10. The patient also reports having frequent urination, increased urination urge, and mild lower abdominal pains. He reports that the urine is foul-smelling, cloudy but it was not bloodstained. He denies any history of urethral discharge but he is sexually active and practices unprotected sex with multiple sexual partners. There is no history of flank pain, fever, nausea, vomiting, myalgia, or malaise. PMH: He has no known chronic illnesses but he had a herniorrhaphy when he was 5 years old for inguinal hernia. Allergies: He has no known food, drugs, or environmental allergies. Medications: 3 He is currently on oral Tylenol 1g three times a day for the pain. Social history: He denies any history of alcohol intake, smoking, or use of recreational drugs. He lives with a friend and he is an accountant in a local bank. Family history: He is the last born in a family of three, all his siblings are alive but the firstborn is hypertensive. Both parents are alive but the dad is both hypertensive and diabetic while the mother is asthmatic and she is a breast cancer survivor. Health Maintenance/Promotion: He reported that he visits the hospital annually for a checkup and the last visit was 7 months ago. His immunization history is up to date and received pneumococcal and influenza vaccination 2 months ago. He reports that he takes junk foods most of the time but he reports to be taking early morning joggings every day and visits the gym once a week. ROS: General: He denies loss of appetite, general body weakness, fever, chills, excessive sweating, recent weight loss or gain, dizziness, or changes in sleep patterns. HEENT: Head: Denies recent head trauma, headache, dizziness, or loss of appetite. Eye: He denies eye pain or secretions, loss of vision, changes in vision, blurry vision, or double vision. Ear: Denies 4 ear discharge, hearing difficulties, or tinnitus. Nose: Denies nasal congestion, nasal obstruction, sinus pain, postnasal discharge, loss of sense of smell, or nose bleeding. Throat: Denies pain during swallowing, difficulty in swallowing, hoarseness of voice, or a sore throat. [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
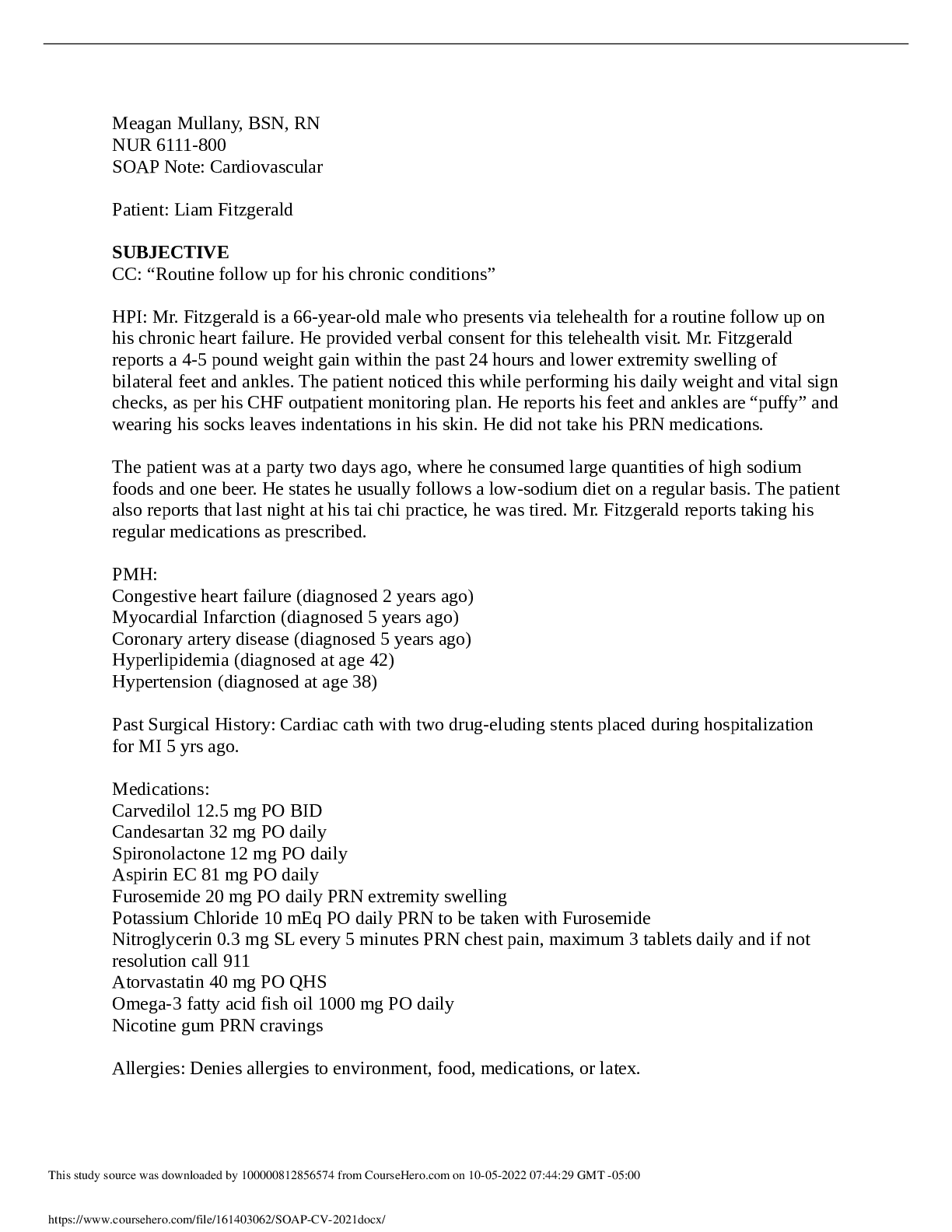
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Health Care> SOAP NOTE > Caroline Casey SOAP (All)
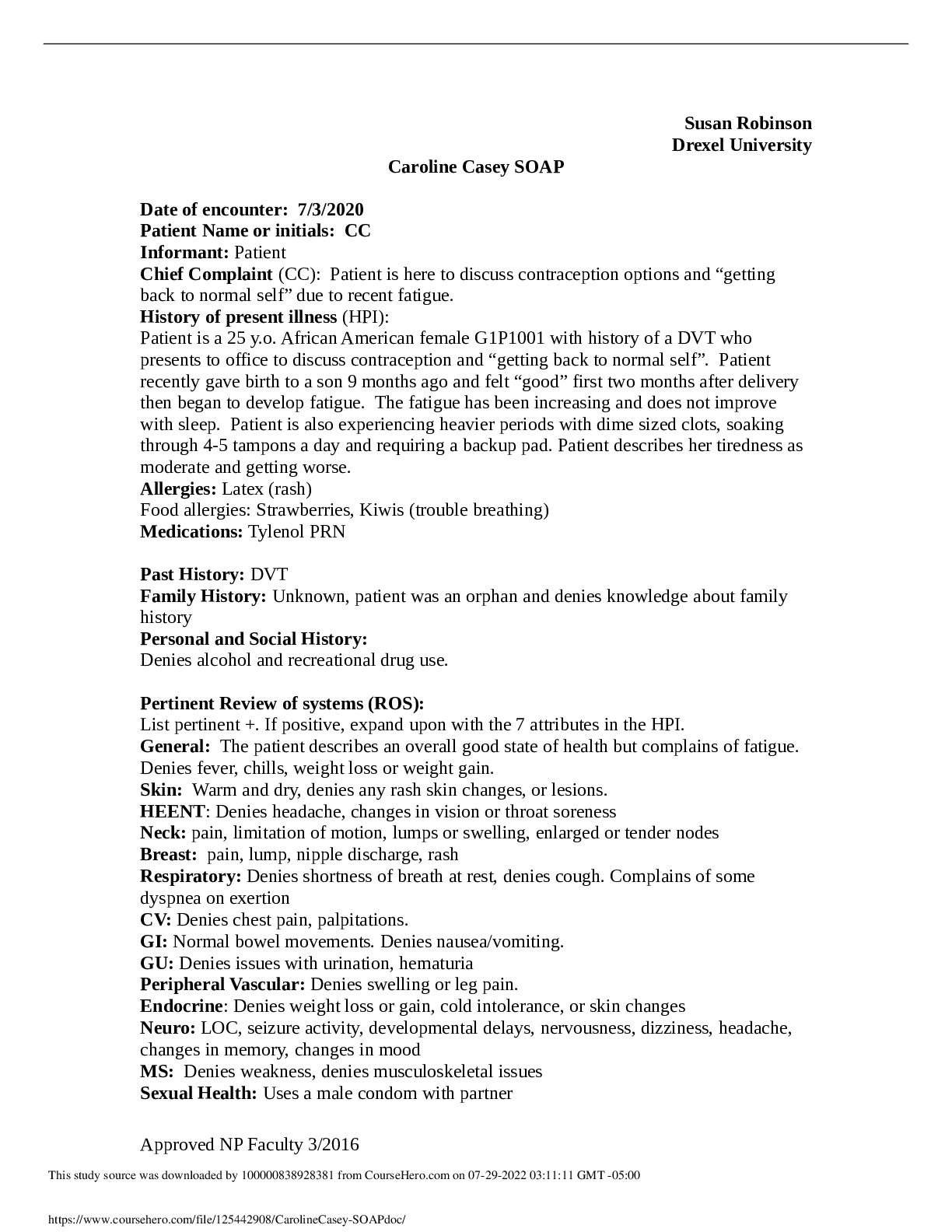
Caroline Casey SOAP
Caroline Casey SOAP
By Ellen Ronald , Uploaded: Jul 29, 2022
$8
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Nancylect , Uploaded: Jul 20, 2022
$9
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By MARKALLAN , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Prof.Pierro , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > ADULT 620 Week 4 make up SOAP note clinical patient (All)
ADULT 620 Week 4 make up SOAP note clinical patient
ADULT 620 Week 4 make up SOAP note clinical patient Chief Complaint The patient presents in the clinic today with complaints of loss of voice 6 days ago, has rhinitis and congestion. Says has just...
By Topmentor , Uploaded: Jul 12, 2022
$10
*NURSING> SOAP NOTE > BACTERIAL VAGINOSIS SOAP NOTE (All)
.png)
BACTERIAL VAGINOSIS SOAP NOTE
BACTERIAL VAGINOSIS SOAP NOTE KL is a 25-year old female of a Caucasian decent
By Topmentor , Uploaded: Jul 12, 2022
$10
*NURSING> SOAP NOTE > Week 6 SOAP note Patient Initials P.R. A 94 year old female (All)
Week 6 SOAP note Patient Initials P.R. A 94 year old female
Week 6 SOAP note Patient Initials P.R. A 94 year old female Chief Complaint Follow-up from last week on peri-area rash. Patient states was in the hospital with a catheter, then in rehab was given ‘...
By Topmentor , Uploaded: Jul 12, 2022
$10
Document information
Connected school, study & course
About the document
Uploaded On
Nov 07, 2022
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Nov 07, 2022
Downloads
0
Views
36