*NURSING > EXAM > NURS 351 Exam 2 Study Guide – Nevada State College | NURS351 Exam 2 Study Guide (All)
NURS 351 Exam 2 Study Guide – Nevada State College | NURS351 Exam 2 Study Guide
Document Content and Description Below
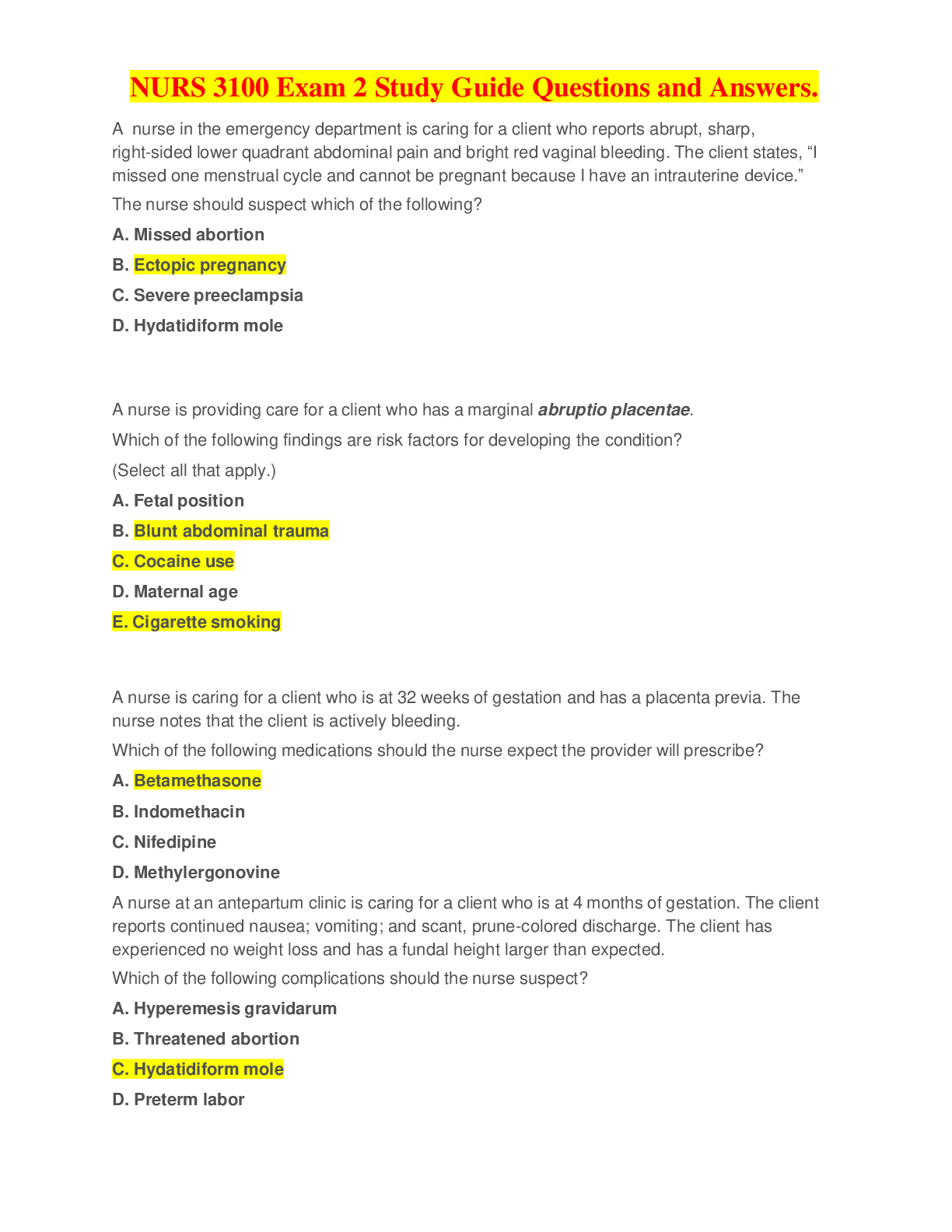
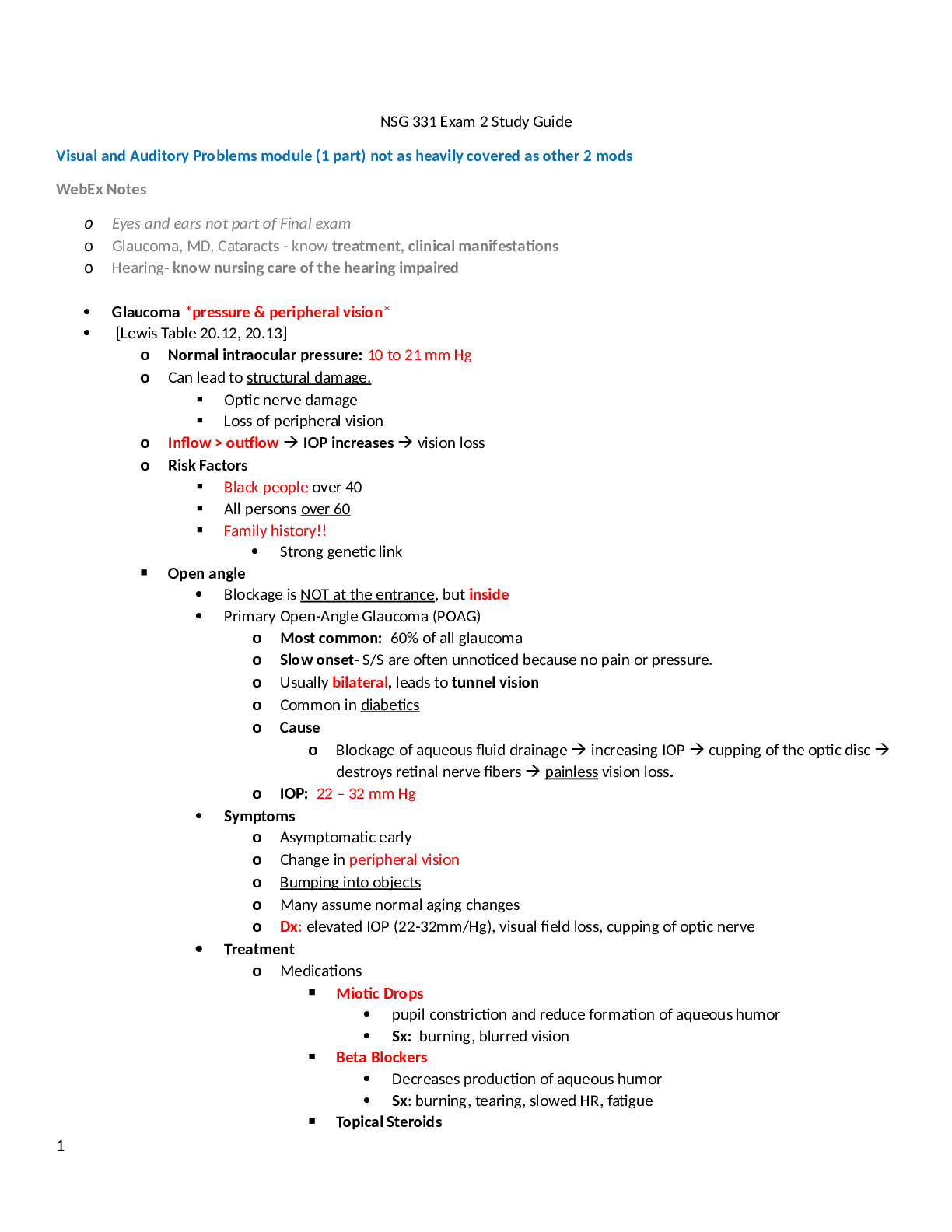
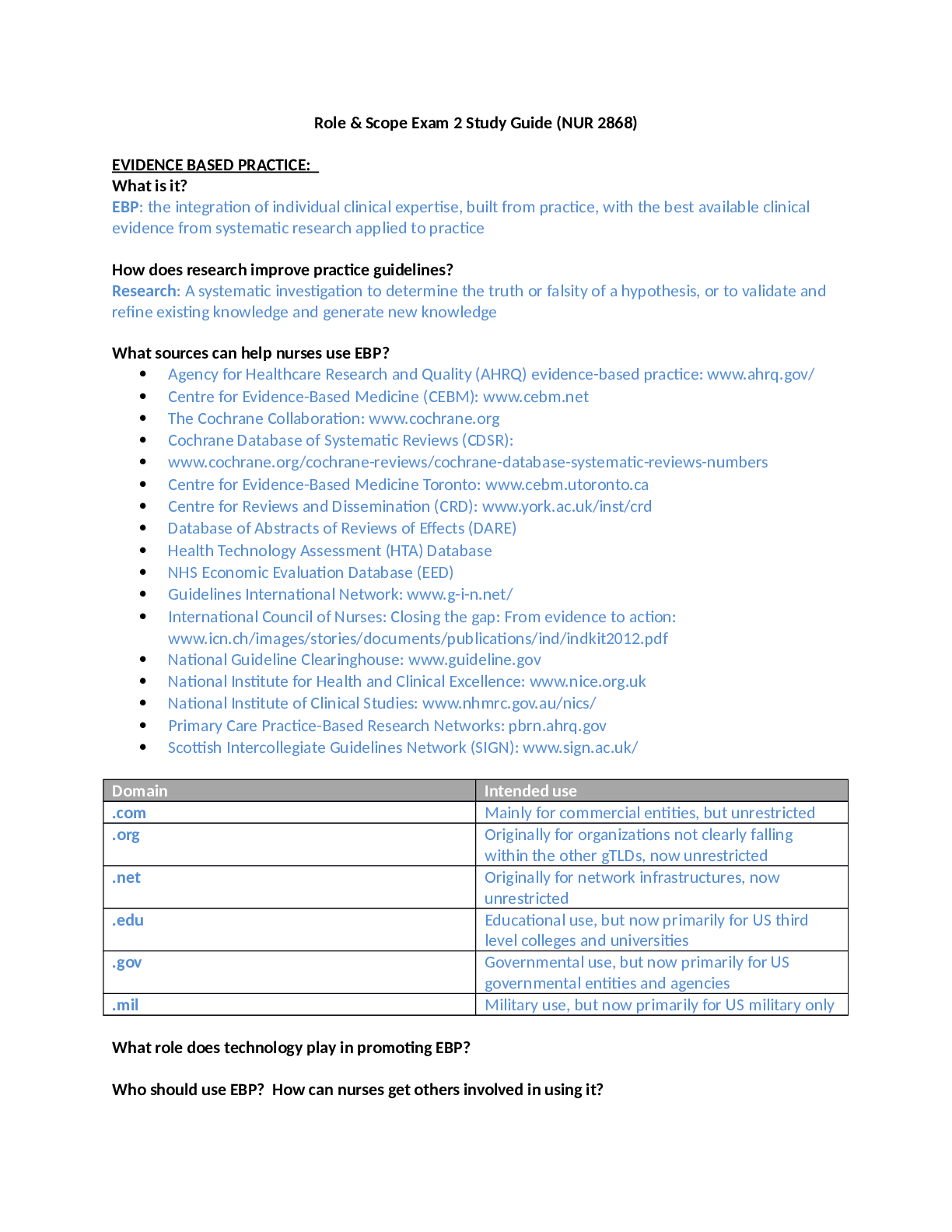
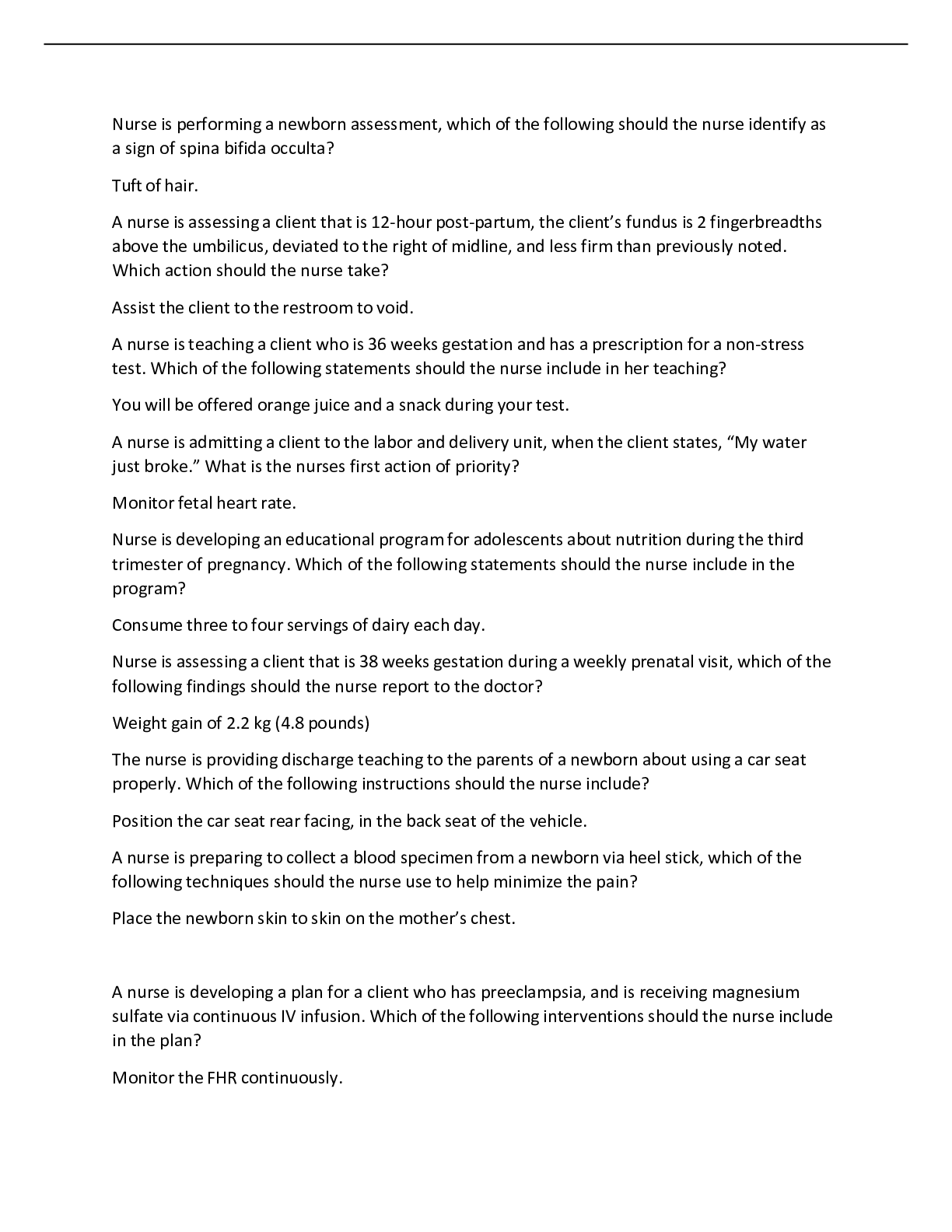
NURS 351 Exam 2 Study Guide – Nevada State College Study guide exam 2 Ch 17 Maximizing comfort • General anesthesia – rarely used for uncomplicated vaginal birth o Nitrous Oxide: laughin... g gas for labor Nitrous oxide mixed with oxygen provides analgesia during the first and second stages of labor Self-administered by laboring woman Used in any stage of labor Full effect in 30-60 seconds Effect: pain relief, euphoria, less anxiety Side effect: nausea, vomiting, poor recall of labor o Anesthesia: General anesthesia 12 (loss of consciousness) Rarely used for uncomplicated vaginal birth The woman should be premedicated with (clear) oral antacid to neutralize the acidic contents of the stomach. Because of this risk for neonatal narcosis, it is critical that the baby be delivered as soon as possible after induction of general anesthesia o Regional analgesia and anesthesia and local 13 Epidural: currently the most effective pharmacologic pain relief method for labor Combined spinal-epidural (CSE) Walking epidural – lighter version of epidural Spinal PCEA Pudendal Block • Epidural/spinal anesthesia and associated complications – everything o Regional analgesia and anesthesia: contraindications History of spinal surgery/ abnormalities Active or anticipated serious maternal hemorrhage Maternal hypotension Maternal coagulopathy Infection at the injection site Thrombocytopenia Increased intracranial pressure Maternal refusal or inability to cooperate Some types of maternal cardiac conditions o Contraindicated for the woman who is receiving anticoagulation therapy o Side Effects/complications of regional anesthesia Hypotension Changes in FHR Nausea and Vomiting Pruritis Urinary retention, Maternal temperature Postdural puncture headache High spinal Intravascular injection Epidural hematoma • Nonpharmacological pain management o Application of heat and cold o Massage o Birthing Balls o Hydrotherapy o Acupressure and acupuncture o Frequent position change o Aromatherapy o Music o Hypnosis • All about pain; anxiety and pain Definition of pain Pain tolerance refer to the level of pain a laboring woman is willing to endure o First stage of labor (visceral pain) o Second stage (visceral +somatic pain) Somatic pain - intence, sharp, burning, and well localized o Third stage (similar to the first stage) Factors influencing pain response - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - • Fetal heart abnormal rates: tachycardia, bradycardia Tachycardia: >160 beats/min 10 minutes or more Causes: Maternal infection, chorioamnionitis Fetal anemia Fetal cardiac dysrhythmias Maternal use of cocaine/meth Maternal dehydration Fetal infection Maternal hyperthyroidism Bradycardia: <110 beats/min 10 minutes or more Causes Uteroplacental insufficiency Umbilical cord prolapse Maternal hypotension Prolong umbilical cord compression Fetal congenital heart block Anesthetic medications Viral infection Maternal hypoglycemia Fetal heart failure Maternal hypothermia • Intrauterine resuscitation: nursing interventions to address decelerations/priorities o • Baseline fetal heart rate o The baseline fetal heart rate is the average rate during a 10-minute segment that excludes periodic or episodic changes, periods of marked variability, and segments of the baseline that differ by more than 25 beats/minute. o There must be at least 2 minutes of interpretable baseline data in a 10-minute segment of tracing in order to determine the baseline FHR . o After 10 minutes of tracing is observed the approximate mean rate is rounded to the closest 5 beats/minute interval o The normal range at term is 110 to 160 beats/minute • All about decelerations and their management DECELERATIONS Early decelerations in response to fetal head compression Late decelerations due to uteroplacental insufficiency Variable decelerations due to umbilical cord compression Prolonged decelerations – disturbed fetal oxygen supply Variable deceleration • Variable deceleration of the FHR is defined as a visually abrupt (onset to nadir less than 30 seconds) decrease in FHR below the baseline. The decrease is at least 15 beats/minute or more below the baseline, lasts at least 15 seconds, and returns to baseline in less than 2 minutes from the time of onset . Variable decelerations are caused by compression of the umbilical cord. • Variable decelerations have a U, V, or W shape, characterized by a rapid descent and ascent to and from the nadir of the deceleration. • Some variable decelerations are preceded and followed by brief accelerations of the FHR known as shoulders, which is an appropriate compensatory response to compression of the umbilical vein. • Recurrent variable decelerations indicate repetitive disruption in the fetus’s oxygen supply. This can result in hypoxemia and metabolic acidemia. Prolonged deceleration • A prolonged deceleration is a visually apparent decrease (may be either gradual or abrupt) in FHR of at least 15 beats/minute below the baseline and lasting more than 2 minutes but less than 10 minutes. • A deceleration lasting more than 10 minutes is considered a baseline change . • Prolonged decelerations happen when the mechanisms responsible for late or variable decelerations last for an extended period (more than 2 minutes). • Examples of conditions that can cause an interruption in the fetal oxygen supply long enough to produce a prolonged deceleration include maternal hypotension, uterine tachysystole or rupture, extreme placental insufficiency, and prolonged cord compression or prolapse. Early deceleration • Early deceleration of the FHR is a visually apparent gradual (onset to lowest point ≥30 seconds) decrease in and return to baseline FHR associated with UCs. • It is thought to be caused by transient fetal head compression and is considered a normal and benign finding. • Generally the onset, nadir (lowest point), and recovery of the deceleration correspond to the beginning, peak, and end of the contraction. • For this reason, an early deceleration is sometimes called the “mirror image” of a contraction. Late deceleration • Late deceleration of the FHR is a visually apparent gradual decrease in and return to baseline FHR associated with UCs. • The deceleration begins after the contraction has started, and the nadir of the deceleration occurs after the peak of the contraction. • The deceleration usually does not return to baseline until after the contraction is over. How to remember: early/late - - - - - - - -- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Ch. 32 Labor and Birth complications • Preterm labor, PROM, PPROM o Preterm labor Preterm labor is defined as uterine contractions and cervical changes that occur between 20 and 37 weeks of gest. Risk Factors infections of the urinary tract, vagina, or chorioamnionitis (infection of the amniotic sac), previous preterm birth, multifetal pregnancy, short cervix, hydramnios (excessive amniotic fluid), age below 17 or above 35, low socioeconomic status, smoking, substance use, domestic violence, history of multiple miscarriages or abortions, diabetes mellitus or hypertension, lack of prenatal care, recurrent premature dilation of the cervix, placenta previa or abruptio placentae, preterm premature rupture of membranes, short interval between pregnancies, uterine abnormalities Signs and symptoms of preterm labor Uterine activity • UC, more frequent than every 10 minutes persisting for 1 hour or more • UC may be painful or painless Discomfort • Lower abdominal cramping; may be accompanied by diarrhea • Dull, intermittent low back pain (below the waist) • Pelvic pressure or heaviness; feeling that “baby is pushing down” • Urinary frequency Vaginal discharge • Change in character or amount of usual discharge: thicker or thinner, bloody, brown or colorless, increased amount, odor • Rupture of amniotic membranes Laboratory and diagnostic procedures Fetal fibronectin – fFN • (fFN) - diagnostic test for preterm labor. • is a glycoprotein “glue” found in between the fetal membranes and decidua • normally appears in cervical and vaginal secretions early in pregnancy and then again in late pregnancy. • the presence of fFN during the late second and early third trimesters may be related to placental inflammation (one cause of spontaneous preterm labor) • preterm labor is very unlikely to occur • in women with a negative result Cervical cultures, CBC, Urinalysis Biophysical profile (BPP) Medications Uterine relaxants (Tocolytics) Indomethacin (NSAID) Nifedipine (CA chanel blocker) Magnesium Sulfate Terbutaline (adrenergic agonist) Promotion of fetal lung maturity: preterm labor Antenatal glucocorticoids have been shown to significantly reduce the incidence of respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and death in neonates o Premature Rupture of Membrane (PROM) spontaneous rupture of the amniotic membranes 1 hour or more prior to the onset of true labor. o Preterm premature rupture of membranes (PPOM) premature spontaneous rupture of membranes after 20 weeks of gestation and prior to 37 weeks of gestation. Risk factors Infection is the major risk of PROM and PPROM for both the client and the fetus. Increased risk: if there is a lag period over the 24-hr period from when the membranes rupture to delivery • Augmentation/induction of labor, everything Induction of labor: deliberate initiation of uterine contractions to stimulate labor before spontaneous onset Bishop score: used to determine maternal readiness for labor by evaluating whether the cervix is favorable by rating the following: Cervical dilation Cervical effacement Cervical consistency (firm, medium, or soft) Cervical position (posterior, midposition, or anterior) Station of presenting part Methods Mechanical (indwelling catheter, Laminaria tents) or chemical approach (Cytotec, Cervidil, Prepidil) Administration of IV oxytocin (Pitocin) Surgical methods (Stripping of membranes, amniotomy) Nipple stimulation to trigger the release of endogenous oxytocin Augmentation of labor Augmentation of labor involves stimulation of hypotonic contractions once labor has spontaneously begun, but progress is inadequate Certain providers favor active management of labor to establish effective labor with the aggressive use of oxytocin (Pitocin) or rupture of membranes. Contraindications • Prolapsed umbilical cord emergency; complications; management [Show More]
Last updated: 1 year ago
Preview 1 out of 18 pages
Also available in bundle (1)
NURS 351 Exam 1 & 2 Study Guide – Nevada State College
NURS 351 Exam 1 Study Guide – Nevada State College NURS 351 Exam 2 Study Guide – Nevada State College
By Martin Freeman 3 years ago
$18.5
2
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 22, 2020
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Dec 22, 2020
Downloads
0
Views
78


 – CHAMBERLAIN COLLEGE OF NURSING.png)