Education > STUDY GUIDE > EDUC 8114 - Hemostasis Study Guide (All)
EDUC 8114 - Hemostasis Study Guide
Document Content and Description Below
Hemostasis, Sponges and Drains Hemostasis When injury to a blood vessel occurs, the reaction of plasma from vessels with connective tissue cells at the site of injury will activate clotting factor... s that leads to another series of reactions; prothrombin reacting with thromoboplastin, which is released during tissue injury. Prothrombin and thromboplastin, combine with calcium ions in the blood to form thrombin. This reaction takes place over several minutes. Finally, thrombin unites with fibrinogen to form fibrin. When this reaction occurs in small vessels, it may be sufficient to provide primary hemostasis. If blood clotting does not happen spontaneously, other methods may be used. How Hemostasis is Achieved When a blood vessel is severed or injured, constriction and some contraction occurs at the ends of the vessel. In response to this constriction and contraction, platelet formation begins to occur. Interaction with collagen fibers causes the platelets to release adenosine diphosphate (ADP), epinephrine, and serotonin from their secretory granules. ADP then causes other platelets to clump to the initial layer and to each other, forming a plug. The reaction between plasma from the vessels and connective tissue cells at the site of the injury activates clotting factors and causes a series of other reactions. Prothrombin reacts with thromboplastin; prothrombin and thromboplastin, along with calcium ions in the blood to form thrombin; thrombin unites with fibrinogen to form fibrin. When this process does not occur and there is incomplete hemostasis, control of bleeding must be achieved by alternative methods. These alternative methods can be classified as mechanical, thermal, and chemical Chemical Method Involves using chemicals such as topical powders on the wound to stop the blood flow. Thermal Method Involves the use of either high-frequency electric current provided from an electrosurgical unit to coagulate bleeding points; hypothermia; or an oscillating, high-frequency electric current generating heat to coagulate tissue. Other methods of thermal hemostasis include: vaporization, ultrasonic energy, and radio frequency energy generated by Argon gas. Mechanical Method Involves applying physical pressure on the wound to stop the blood flow. Mechanical Method Mechanical hemostasis is achieved by occluding severed vessels until platelet formation occurs. During the surgical procedure, the surgeon may use various methods to apply physical pressure including manual pressure, which incorporates the use of various types of sponges, pneumatic tourniquets, hemostatic clamps, ligating clips, Esmarch bandages, ligatures, and pledgets Pressure Manual Pressure May be implemented by hand, sponge, digit, or “packs” for pressure Hemostats Clamps for occluding vessels are used to compress blood vessels and to hold a small amount of tissue. The hemostat is the most commonly used method for achieving hemostasis. In many cases, the pressure of clamping the hemostat onto the vessel is sufficient enough to constrict and seal the vessel. In other cases a ligature may be required. Ligating Clips Ligating clips (hemoclip, weck clip) are small staple-like devices that are placed around the lumen of a vessel or structure using a special applier, and then closed to seal it off; providing hemostasis. Ligating clips may be made of titanium or stainless steel and are available in small, medium, medium-large, and large sizes. Absorbable clips that are made of a synthetic material are also available. Placed on the vessel and pinched shut to occlude the lumen of vessel. Bone Wax Bone Wax (e.g., Bone Wax) Bone wax is composed of a mixture of beeswax, isopropyl pamitate, and a softening agent. Provides a mechanical tamponade effect to stop oozing from cut bone surfaces. Used in some orthopedic and neurosurgical procedures and on the sternum during heart procedures. Caution: Bone wax should be used sparingly and is contraindicated when rapid bone regeneration is desired. Bone wax acts as a physical barrier that prevents bone union. Tourniquets Tourniquets are often indicated in surgical procedures involving extremities when a bloodless surgical site is desired. When inflated, they prevent venous oozing, but do not obstruct arterial blood supply so that circulation is preserved to the extremity. Improper application and use of a tourniquet can result in irreversible nerve and vascular damage. Because of this, careful selection, application, and monitoring of the tourniquet is imperative. The perioperative nurse should follow AORN Recommended Practices as a reference guide. The tourniquet is not a hemostatic method in the truest since. Once deflated, other measures will be needed to promote hemostasis. Caution: The use of a tourniquet is contraindicated in patients with vascular disease or poor peripheral circulation. Once applied, the tourniquet time is noted. Although there is no actual limit to the time length for tourniquets, the recommended time limits range from 1 hour for upper extremities, and 11/2 hours for lower extremities. Esmarch Bandage Used to facilitate exsanguinations of blood from the distal extremity. May be used in conjunction with a tourniquet or alone. Cautions: Do not use if the limb has suffered traumatic injury or has been in a cast because of the potential for the presence of thrombi that could be dislodged. The use of the esmarch bandage is also avoided if an infection is present or if there is a malignant tumor on the extremity. Ligature A ligature, commonly a tie, is a strand of material that is tied around a blood vessel to occlude the lumen and prevent bleeding. Large, pulsating vessels require a transfixion suture, which is a crisscross stitch placed to control bleeding from a tissue surface or small vessel when it is tied. Pledget Small squares of teflon sutured over a hole in a vessel; they exert external pressure over any small needle holes to prevent bleeding and to promote clotting; often in cardiovascular/vascular surgery. Thermal Method The thermal method of achieving hemostasis includes the application of either extreme cold or heat to body tissues. Several types of devices are available for achieving thermal hemostasis Argon Beam Coagulator (APC) The Argon beam coagulator is used to control bleeding from vascular structures, superficial bleeders, and diffuse oozing of blood. It is also used to achieve hemostasis of bone marrow. The argon beam coagulator is a device consisting of an electrode recessed inside a probe through which argon gas is passed. Hemostasis is achieved as current is delivered to tissue in a direct beam of ionized argon gas. Laser Lasers are often utilized in the same manner as electrosurgery for cutting and coagulating tissue and minimizing blood loss. Method: The laser provides a beam of light that is intense and concentrated and is able to cut and coagulate at the same time with minimal destruction to surrounding tissue. Electrosurgery The electrosurgical unit (ESU) is used to apply electrical current through the patient's tissue to cut and/or coagulate the tissue. The monopolar mode is most frequently used for coagulation (hemostasis), but may also be used to cut tissue. A dispersive pad is required when this mode is used. The bipolar mode uses a forcep like device that allows high frequency electrical current to be passed through tissue from one electrode to another. No dispersive pad is necessary with the use of bipolar electrocautery. Cryosurgery Cryosurgical methods produce local freezing of target tissue at -20ºC to -60ºC. Liquid nitrogen is most commonly used in cryosurgery. Cryotherapy decreases the need for oxygen by the tissues thereby decreasing bleeding. Hypothermia Cooling the body's core temperature decreases cellular metabolism, thus decreasing bleeding. Hypothermia may be used in conjunction with anesthetic agents for some types of surgery. Caution: To be effective, body temperature must be lowered to 26ºC for adults and large children, and 20ºC for infants and small children. Chemical method Chemical method for achieving hemostasis involves applying collagens, sponges and topical powders on the bleeding site. Chemical methods include: Microfibrillar Collagen Microfibrillar Collagen (e.g., Avitene) Absorbable topical hemostatic agent. Available in a compacted nonwoven web form or a loose, fibrous, powdery form. Used in surgical procedures as an adjunct to hemostasis when control of bleeding by ligature or conventional methods are ineffective or impractical. Apply it directly to the bleeding source with dry, smooth forceps. Do not use in total joint surgery. Avitene reacts with methylmethacrylate. Its use is contra-indicated with prosthetic materials in orthopedic surgery. Do not use in patients with sensitivity to bovine derived collagen. Should not be used in the closure of skin incisions because it may interfere with the healing of skin edges. Do not use if methyl methacrylate is being used; may reduce the bond strength of the methylmethacrylate. Do not use in contaminated wounds; may enhance the infection. Considerations: Moistening or wetting of Microfibrillar collagen may impair its hemostatic efficacy. Oxidized Cellulose Oxidized Cellulose (e.g., NuKnit, Surgicel). Available in the form of pads or fabric (e.g., Surgicel). Supplied in gauze and cotton form and absorbs 7-8 times its weight in blood producing a clot. Blood clots rapidly in the presence of oxidized cellulose, forming a gel which aids in hemostasis as it becomes soaked with blood. Applied directly to the bleeding site and held in place until bleeding stops. Oxidized cellulose should not be left in the patient if used near the spinal cord, optic nerve, or any area with serious tissue or nerve damage. Also oxidized cellulose should never be used with thrombin, because it interferes with the action of thrombin. Should not be used for implantation in bone defects, such as fractures, as there is a chance of interference with callus formation. Collagen Sponge Collagen Sponge (e.g., Collastat, Superstat, and Helistat). Dehydrated hemostatic sponge or foam available compressed, or as a powder. Dissolves as hemostasis occurs. Must be kept dry and applied dry. It is applied directly to the bleeding surface. Absorbable collagen is contraindicated in the presence of infection or in areas where blood or other fluids have pooled. Absorbable Gelatin Sponge Absorbable Gelatin Sponge (e.g., Gelfoam). Sponge swells, forming a clot, and absorbs 40-50 times its weight within 20-40 days. Used with thrombin, saline, or dry. Always squeeze air out of sponge. Don't place in intravascular compartments due to risk of embolism. Remove excess material once hemostasis is achieved. Fibrin Sealants Fibrin Sealants (e.g., Tisseal, Crosseal, and FloSeal) Fibrin sealants are a type of surgical tissue adhesive derived from human and animal blood products. The ingredients interact during application to form a stable clot. Used to control bleeding and to speed up wound healing, to seal off hollow body organs, to cover holes made to made by sutures, and to provide slow release of application of medications to tissue that have been exposed during surgery. Fibrin Sealants are contraindicated in individuals with allergic hypersensitivity to bovine proteins. Phenol Solution (e.g., Phenol) 95% Phenol. Used for sclerotherapy of hemorrhoids. Some surgeons apply it on the tip of a cotton swab to cauterize the lumen of the appendix stump as it is cut. Contraindicated in individuals with hypersensitivity, neonates and children. Thrombin (e.g., Thrombin, Thrombostat) Extracted from dried beef blood. Available as a powder which is reconstituted with its own diluent. Used as a topical hemostatic agent. Thrombin accelerates coagulation of blood and controls capillary bleeding. In various types of surgery, solutions of thrombin are used in conjunction with an absorbable gelatin sponge for hemostasis. Thrombin should be used immediately after reconstitution. If necessary, it may be refrigerated for up to three hours after reconstitution. Contraindicated in individuals with sensitivities to any of its components including those of bovine origin. Styptics (e.g., Epinephrine, Tannic acid, and Silver Nitrate) Includes chemicals that cause blood vessels to constrict. Epinephrine 1:1000 may be added to local medications to decrease the amount of bleeding or may be used to soak small pieces of gelatin sponges prior to application. Silver nitrate when mixed with silver chloride in the form of a molded stick creates a topical hemostatic agent. Tannic acid is another hemostatic agent that is used to stop bleeding in gum tissue. Use with caution. Epinephrine can increase heart rate and blood pressure. Sponges Surgical sponges are used to apply mechanical pressure on bleeding areas or vessels to absorb excess blood, or fluid of any type, and to protect, cushion, or immobilize structures during surgical procedures. Sponges are also used for blunt dissection and "walling off " organs to provide exposure to the surgical site. Surgical sponges must contain radiopaque markers that are visible under x-ray in the event that a sponge is inadvertently left in the surgical wound. Sponges used for dressings do not contain these markers. Types of Surgical Sponges Surgical sponges are manufactured in a variety of sizes and shapes, and depending on their type of use, specific numerical increments. Surgical sponges’ serve three general purposes; absorption of blood and body fluids, blunt dissection of delicate tissue, and protection from injury. Sponges should be counted in all procedures in which there is a possibility that a sponge may be inadvertently retained. Sponges that are to be used on the sterile field must contain radiopaque markings and are to be counted before the start of the surgical procedure, and at specific intervals throughout the procedure according to the policies and procedures of the facility and to AORN Standards, Recommended Practices, and Guidelines. Two people, one of whom is the registered nurse circulator, count the sponges simultaneously and audibly as each sponge is separated. Sponges must never be cut to size for use during a surgical procedure. Identification of a retained sponge will be facilitated by the radiopaque marker in the sponge. X-ray detectable 4 x 4 X-ray detectable 4” x 4” (e.g.,Raytec) sponges are made of USP Type VII gauze with filaments that become visible under x-ray. The x-ray detectable 4”x 4” sponge absorbs fluid and is used for the other purposes as well. Cautions: These sponges should not be used for wound dressing because they may appear as a foreign body on postoperative x-rays and might invalidate a sponge count if the patient is returned to surgery with the dressing intact. Dissector sponges • Cherry dissectors are 100% cotton and are the softest dissector. • Peanut dissectors are made of USP Type III gauze with a neck that allows the surgeon to adjust the hardness of the sponge. • The K-dissector is made of rolled chevron, 100% cotton tape, x-ray detectable and hand stitched for strength.These sponges provide blunt dissection as they absorb fluid. Neuro-patties or cottonoids Neuro-patties or cottonoids are made of highly absorbent, 100% cotton with an x-ray detectable element sewn into each sponge. Used on delicate structures such as nerves, brain tissue, and the spinal cord. Tonsil sponges Tonsil sponges are made of 100% x-ray detectable, USP Type III gauze with a cotton filling. They are available unstrung, double-strung with cotton thread for use in tight areas, or strung with a cotton tape. Used primarily during Tonsillectomies. Laparotomy sponges Laparotomy sponges are extra absorbent, 100% cotton and four-ply USP Type III prewashed gauze. They include a four-inch, x-ray detectable element and come in a variety of sizes with or without rings. These sponges help protect and pad delicate tissues and organs, as well as absorb fluids. Why Count Sponges? A sponge count is performed to accurately account for all sponges used in a surgical procedure and to ensure the safety of the patient by preventing the retention of surgical items. Sponges should be counted in all procedures in which sponges are used. Counts are performed before, during and after surgical procedures. Retained surgical items such as a sponge or other soft goods are considered a preventable occurrence. Sponges that are to be used on the sterile field must contain radiopaque markings and are to be counted before the start of the surgical procedure, and at specific intervals throughout the procedure according to the policies and procedures of the facility and to AORN Perioperative Standards and Recommended Practices. Two people, one of whom is the registered nurse circulator, should count the sponges simultaneously and audibly as each sponge is separated. Sponges must never be cut to size for use during a surgical procedure. Identification of a retained sponge will be facilitated by the radiopaque marker in the sponge. Performing a Sponge Count Facilities should establish policies and procedures that provide guidance and standardized procedures for counting. Deliberate, consistent application and adherence to standardized procedures are necessary to prevent the retention of sponges and other soft goods. A standardized count procedure assists the surgical team to achieve accuracy, efficiency, and continuity among all of the perioperative team members. Studies in human error have shown that many errors are the result of deviation from a routine practice. When to Count Sponges All sponges need to be accounted for at intervals during a surgical procedure using a standardized sponge count procedure. This assures all team members that a sponge or other soft good has not been left in the patient. Counts of sponges and other soft goods should be performed: Before the procedure to establish a baseline and identify manufacturing packaging errors - this would be the initial count. When new items are added to the field. Before closure of a cavity within a cavity (e.g., uterus). When would closure begin. At skin closure at the end of the procedure or at the end of the procedure when counted items are no longer in use - this would be the final count. At the time of permanent relief of either the scrub person or the RN circulator. Accurately accounting for sponges and other items used during a surgical procedure is the primary responsibility of the RN circulator and the perioperative team. However, the RN circulator plays a leading role in implementing measures to account for surgical items. Standardized Procedure for Counting Although there is no legally correct way to perform sponge counts, most facilities base their policies on the AORN Perioperative Recommended Practices. These recommended practices provide rationale and discussion for each of the recommendations regarding sponge counts. Health care organizations are responsible for employing standardized, transparent, verifiable, and reliable practices to account for all surgical items used during a procedure. This will lessen the potential for patient harm as a result of a retained surgical item. The following are some reliable procedures that should be implemented to account for all sponges used in surgery: • complete and accurate counting, • radiological confirmation, and • the use of adjunct technology. The key to success is the application of a consistent multidisciplinary approach for the prevention of retained sponges during all surgical invasive procedures. Establishing a system or procedure that accounts for all surgical items opened and used during a procedure constitutes a primary and proactive injury-prevention strategy. Participation in Sponge Counts All perioperative personnel involved in a surgical case are responsible for the accuracy of the sponge count. Each has a duty to remain aware of the location of the sponges in on the sterile field and in the wound. All members of the surgical team share accountability to the patient to provide a safe environment and to do no harm as a result of their intervention in the patient’s care. They must be knowledgeable in the types of sponges and their uses. They must maintain an orderly field and room to facilitate locating sponges at all times. Performing and recording initial counts establishes a baseline for subsequent counts on all procedures. Counts must be made at appropriate times according to facility policy. In addition: 1. Two people, one of whom is the registered nurse circulator, must perform the sponge count. 2. The RN circulator should facilitate the count process by initiating the count, performing count procedures in coordination with the perioperative team, documenting count reconciliation activities, and reporting any count discrepancy. 3. The scrub person should maintain awareness of the location of all soft goods (eg, radiopaque sponges, towels, textiles). 4. The scrub person and the circulating nurse should count sponges simultaneously and audibly as each sponge is separated from others in the pack before the beginning of the operation, before any closure begins, and when skin closure is begun. 5. All sponges must remain in the same OR room until the count is complete. 6. Sponges should be counted on all procedures where they are used. 7. OSHA Guidelines must be followed for handling sponges. 8. Use radiopaque sponges for dressing a wound are unacceptable. 9. Sponges with radiopaque markers must be used during any invasive procedure. Sponge Count Discrepancies If there is a sponge count discrepancy at any point, a specific policy and procedure developed by the facility is followed. This may include: The RN informs the surgeon and receives verbal acknowledgement as soon as the discrepancy is identified notified and The circulator begins a search of the area surrounding the sterile field. This includes the linen and waste containers, under bed and tables, and the rest of the room.. The scrub person assists with a visual inspection of the area surrounding the sterile field. The surgeon suspends closure of the wound and performs a methodical wound examination. The surgeon also cooperates in obtaining radiographs or other modalities as indicated to locate the missing item. The surgeon remains in the OR until the item is found or it is determined with certainty that the item is not in the patient. If the item is not found, an x-ray should be taken before final closure of the wound. An AP and Lateral views should be taken to rule out a retained sponge. An occurrence report is made if the sponge remains missing if required by facility policy. Sponge Count Documentation Correct Count Documentation of the sponge count is the responsibility of the circulating nurse. Proper documentation in case of both a correct count and an incorrect count is of prime importance. 1. Inform the surgeon of the count 2. Document the count and the results in the perioperative nursing record Incorrect Count 1. Document the counts and the results in the perioperative nursing record. 2. Document the actions taken to locate the missing sponge. 3. Document that radiographs were taken and the name of the person who read the radiograph. 4. Follow hospital policy and procedure for completion of an unusual occurrence report. Drains Drains expedite the healing process by removing blood, serosanguinous fluid, and purulent material. Drains are also used to assist with eliminating dead spaces, prevent deep wound infections and drain bile and intestinal contents. Drains function by either passive means (i.e., gravity, capillary action) or by active means (i.e., suction). Intraoperatively, drains are used prophylactically to evacuate gastric contents, intestinal fluids, or urine. Intraoperative drainage and decompression aid in the prevention of trauma to tissue. Postoperatively, drains are used to evacuate blood or fluids, air from a wound or body cavity, or when purulent, necrotic material is present. Drains are often placed adjacent to the surgical incision via a small stab wound and anchored with a fixation suture to prevent accidental dislodgement. Types of Drains and Their Uses The drainage of body fluids and purulent material can be achieved by either passive or active means. Intraoperatively, drains are used prophylactically to evacuate gastric contents, intestinal fluids, or urine. Intraoperative drainage and decompression aid in the prevention of trauma to tissue and restoration of organ function. Postoperatively, drains are used to evacuate blood and fluids, air from a wound or body cavity. They are also used to drain pus, purulent, or necrotic material from a wound. Drains are generally placed adjacent to the surgical incision via a small stab wound and anchored with a fixation suture to prevent accidental dislodgement. A variety of drainage systems exist and their selection is dependent on the nature of the surgical procedure and surgeon preference. The type, location, and patency of all drains should be covered in the hand off report to PACU or the nursing unit. The most common drains are discussed in this section. Penrose drains Sizes Generally comes in four widths (¼”, ½”, ¾”, 1”) and two lengths (12” and 18”). Purpose Multiple uses such as drainage, traction, and as a tourniquet. Drainage is pulled along the outside of the drain by capillary action and gravity (passive means) into the dressing. Procedure Insertion – Usually placed through a stab wound. Place approximately 2” from the incision. Pull drain from inside wound through skin with a clamp. Suture drain to skin using nonabsorbable material. A safety pin may be applied to the drain to prevent the drain from retracting back under the skin. Apply dressings around the drain. Drainage is pulled along the outside of the drain by capillary action and gravity into the dressing. Indications Abdominal surgery - periotoneal cavity or skin wound Nasogastric tubes Sizes Range in size from 8F for enteral feeding to 14F or larger to administer medications, gastric decompression, and for short term feeding. For neonates, 3-5F is commonly used. Purpose A nasogastric tube is used to aspirate gastric contents, or to decompress the intestinal tract postoperatively. The nasogastric tube may also be used for gastric feeding during the healing process after a surgical procedure. Procedure A plastic or rubber nasogastric tube is inserted through a nostril, past the pharynx, and into the stomach or small intestine. Confirmation of placement is verified either manually by the surgeon during open laparotomy procedures, aspiration of gastric contents, auscultation of air insufflated through the tube, or by x-ray. Indications Decompression of the stomach (Levin tube), decompression of the small intestine (Miller-Abbott tube) and nasogastric suction (Salem sump tube). T-tubes Sizes Available in a large variety of sizes. Purpose T-tubes are used to drain the common bile duct through the abdominal wall. Procedure Placed into the common duct after exploration. Suction drains Sizes 7F - 15F (i.e.; Jackson-Pratt) drains and medium or large hemovacs. Purpose To drain accumulated blood and fluid from the operative site. This drain functions by using mechanical suction to pull blood and fluid into the reservoir (active means). Procedure The perforated end of the catheter is placed somewhere inside a cavity in the body; that end is perforated. The external end of the catheter is connected to a device that when compressed and attached to the catheter, will exert gentle suction on the drainage catheter. Indications Abdominal or breast surgery (Jackson-Pratt). Orthopedic surgery (Hemovac). Chest-tubes Sizes 8F - 36F Purpose To restore an airtight pleural cavity and maintain negative pressure. chest tubes use a water seal system connected to a source of suction (active means). Procedure A tube is inserted at the base of the pleural spaces is usually inserted at the seventh costal interspace in thoracic surgery; or in the chest near the incision site following heart surgery. The tube provides a conduit for drainage of air, blood, and other fluid from the intrapleural or mediastinal space and reestablishment of negative pressure in the intrapleural space. Chest tubes are connected to a sterile water-seal or gravity drainage system. The chamber of the system collects the drainage from the intrapleural space, the second chamber provides the water seal and the third provides the suction control determined by the level of water. Indications Thoracic surgery, cardiac surgery Complications of Drains Possible complications related to the use of drains can include: Loss of drain internally if not secured properly. This may result in a second surgery. Bowel herniation if a of very large stab wound used. Sepsis due to retrograde contamination. Hemorrhage from insertion through stab wound. Accidental removal of drain or T-tube. Patient or caregiver may accidentally dislodge the drain. Dressings The final step for any surgical procedure is the application of dressings and tape. Dressings accomplish basic purposes or functions, which are all important to the outcome of the surgical intervention. These functions include: Protect the incision from contamination and/or trauma Absorb drainage and /or exudates Facilitate hemostasis by providing pressure Contain exudates Cover a wound for cosmetic reasons Ø Provide support or splinting for pain relief Selection of Dressings Most skin incisions and surgical wounds will be covered with a sterile dressing to promote physiological healing. The type of dressing used is determined by size and location of the surgical incision or wound, the surgical procedure, and surgeon preference. The perioperative nurse must have knowledge of the various types of dressings available, their method of application, and potential complications of surgical dressings. Dressings can be classified as primary or secondary. Primary dressings are used directly on the incision. Primary dressings are used to absorb drainage and wick it away. They should have a non-adhesive layer to prevent debridement of tissue when removed. Secondary dressings are placed over the primary dressing. They are used mainly for absorption of drainage, to apply pressure for hemostasis and to protect the wound. The basic types of dressings used are: Occlusive dressings Gauze dressings Hydrogel dressings Pressure dressings Biological dressings Rigid support dressings Primary Dressings Occlusive Dressings (semipermeable films) Indications : Used to prevent drying of the surgical wound and to increase the proliferation of epithelial cells. These dressings also reduces pain, tenderness and scarring of the skin. Used for pressure, dermal ulcers, donor sites, burns, and abrasions. Material: Impermeable materials made of polyurethane or fine mesh gauze that is impregnated with petroleum, xeroform, iodophor, or an antibiotic ointment. Brand Names: Bioclusive, Dermicel, DuoDerm Hydrocolloids, Opsite, Tegaderm Properties: Adheres to both dry and moist skin. Waterproof barrier for exogenous microorganisms. May leave an odor. Method: Leave in place for up to 7 days; difficult to remove if changed too early. Caution: Take care while removing, to protect the newly formed skin. Occlusive Dressings (Hydrogels) Indications Hydrates and soothes tissue. Material Transparent polyethylene membranes, wafers, pastes and rings Brand Names: Tegagel, Nu-gel, Vigilon, Karaya, colloplast Properties: Absorb fluid and blood and protect wound from drying out. Also has cooling effect. Method Apply on wound and leave. Secondary Dressings Pressure Dressing Indications On the wound in the immediate postoperative period to minimize the accumulation of intercellular fluid, eliminate dead space, distribute pressure evenly, absorb extensive drainage, facilitate wound healing, minimize scarring, immobilize an area, and to provide patient comfort. Material Fluffed gauze; non-radiopaque, and gauze-covered absorbent pads, covered by heavy, elastic tape. Biological Dressing Indications Biological dressings are used to help control infection by covering denuded area, preventing loss of serum, decreasing pain, stimulating the formation of epithelium in the dermis directly underneath it, and promoting formation of granulation tissue. Material May be allografts of human skin from a living or cadaver donor, placental or amniotic membranes, or a xenograft of porcine skin. Antimicrobial or chemotherapeutic ointments such as silver sulfadiazine, mafenide acetate, or silver nitrate may be used as part of biological dressings. Brand Names: Silvadene, Scarlet Red. Method Apply to the wound. Rigid Support Dressing Indications To immobilize a body area or support soft tissue. For example after fracture fixation. Material Soft padding stockinette, cotton bandage, cotton roll (depending on location), and cast material. Cast - Plaster of Paris (gypsona), fiberglass. Brand Names: Cast, Splint Method Apply the protective cast to the wound Considerations for Selection of Dressings When selecting surgical dressings, consideration must be given to patient allergies, surgeon preference, and properties of the dressings. Allergies Allergies can occur due to tape or adhesive material used in the dressing. Allergic reaction to adhesive materials. Skin Reactions There can be conditions where the skin is frail and tears easily. Skin sensitivity to dressing materials. Surgeon’s Preference The surgeon is the ultimate determinant of the selection and use of dressing material. Postop Suture Care Leave sutures in longer if incision is in an extremity or under pressure. Remove sutures if suture tract is infected. Only minimal stress should be exerted on wounds for 6- 8 weeks. Adhesive Skin Tape Care Keep dry without ointment. The patient may shower first week. Cover with sealed dressing first 3-5 days. Liquid Skin Adhesive Keep the wound dry without ointment. Do not soak or scrub the wound. A film remains in place for 5-10 days and then falls off the skin. Staples Remove after an average of 7-14 days, depending on location and tension. You may cover with a topical antibiotic. Avoid prolonged exposure to moisture. The patient may shower the next day. Contaminated Wound Skin and subcutaneous tissues are left open and loosely packed with fine mesh gauze or saline- soaked gauze. Packing should be removed in 2-3 days postoperatively. If there is no infection, the incision may be closed. If infected, for second intention healing, repack the wound twice daily with moist-to-dry dressings. Module Summary Hemostasis: Hemostasis is the process of arresting or slowing the flow of blood. Hemostasis can be achieved by mechanical, thermal, or chemical methods. Mechanical Hemostasis includes the use of manual pressure, ligating clips, and tourniquets. The thermal method of hemostasis includes the use of electrocautery in the form of an electrosurgical unit, cryosurgery, and argon beam coagulator. Absorbable gelatin, absorbable collagen, tannic acid, and silver nitrate are types of chemical hemostasis. Sponges: Sponges may have multiple indications for use. Sponge counts are performed before the surgical procedure begins, at specific intervals during the procedure, at the beginning of wound closure, and the beginning of skin closure to ensure the prevention of retained sponge. Facility procedure must be followed in the event of an incorrect sponge count. t is important that the registered nurse circulator maintain accurate documentation of the surgical sponge count. Drains: Drains expedite the healing process by removing blood, serosanguinous fluid, and purulent material. Drains are categorized based on the functions they perform; either passive or active. Examples of passive include: Penrose drains, T-Tubes, and Gastrostomy tubes. Active drains are low-pressure suction devices that continuously remove fluids against gravity via a closed chamber. Jackson-Pratt and Hemovac drains are common active drains. Drains are required in case of an abscess, an insecure closure of GI tract, an anticipated leakage, trauma, or in decompression of GI tract. Drains are categorized based on the functions they perform, such as Penrose drains, Nasogastric drains, T-tubes, Suction drains and Chest tubes. Complications of drainage can include hemorrhage, sepsis, bowel herniation, and accidental loss of drains. Dressings: Dressings are applied to assist in hemostasis and to maintain an optimal healing environment. Dressings protect the wound from further injury, absorb excess fluids, apply pressure on the wound and support the wound. Occlusive dressings prolong moisture to increase the proliferation of epithelial cells. Gauzes help in protecting the wound and absorbing the fluids. Hydrogels hydrate and soothe tissue. Other types of dressings include biological and rigid support. [Show More]
Last updated: 1 year ago
Preview 1 out of 18 pages
Reviews( 0 )
Recommended For You
*NURSING> STUDY GUIDE > ATI Med-Surg Proctored Exam already Graded A. (All)
ATI Med-Surg Proctored Exam already Graded A.
A nurse is reinforcing teaching with a client who has HIV and is being discharged to home. Which of the following instructions should the nurse include in the teaching? 1) Take temperature once a da...
By Academia1434 , Uploaded: Jan 15, 2021
$13
*NURSING> STUDY GUIDE > NUR 254 Exam 2 Study Guide (100% Accurate ). (All)
NUR 254 Exam 2 Study Guide (100% Accurate ).
NUR 254 (NUR254 EXAM2 STUDY GUIDE)/NUR 254 - Exam 2 Study Guide (100% Accurate ).
By Solution101 , Uploaded: Mar 11, 2021
$12
*NURSING> STUDY GUIDE > NR 533 Financial Management In Healthcare Organizations, Week 5 Assignment Break-Even Analysis (All)
NR 533 Financial Management In Healthcare Organizations, Week 5 Assignment Break-Even Analysis
NR 533 Financial Management In Healthcare Organizations, NR 533 Week 5 Assignment Break-Even Analysis
By TopScholar , Uploaded: Mar 15, 2021
$8
*NURSING> STUDY GUIDE > NR 511Midterm Exam Study Guide Chamberlain College of Nursing - (All)
NR 511Midterm Exam Study Guide Chamberlain College of Nursing -
NR511 Midterm Exam Study Guide Week 1 1. Define diagnostic reasoning: type of critical thinking Critical thinking involves the process of questioning one’s thinking to determine if all possible...
By Muchiri , Uploaded: Mar 12, 2021
$11
Finance> STUDY GUIDE > FINANCE 238 Oxford College of Commerce, Lahore - rev test. (All)
FINANCE 238 Oxford College of Commerce, Lahore - rev test.
I recently visited Kennedy's Orbiter Processing Facility to find out how a highly skilled team of shuttle technicians spent the past few months preparing Endeavour for STS-126. (upbeat music) I'm...
By Muchiri , Uploaded: Mar 17, 2021
$7
*NURSING> STUDY GUIDE > NR 222 / NR222 Health and Wellness Exam 1 Review Study Guide Chamberlain College (All)
NR 222 / NR222 Health and Wellness Exam 1 Review Study Guide Chamberlain College
1. Nursing - the protection, promotion, and optimization of health and abilities; - prevention of illness and injury; - alleviation of suffering through the diagnosis and treatment of human resp...
By nurse_steph , Uploaded: Nov 14, 2020
$13
*NURSING> STUDY GUIDE > NUR 2488 - Exam 3 Key Concept Guide (All)
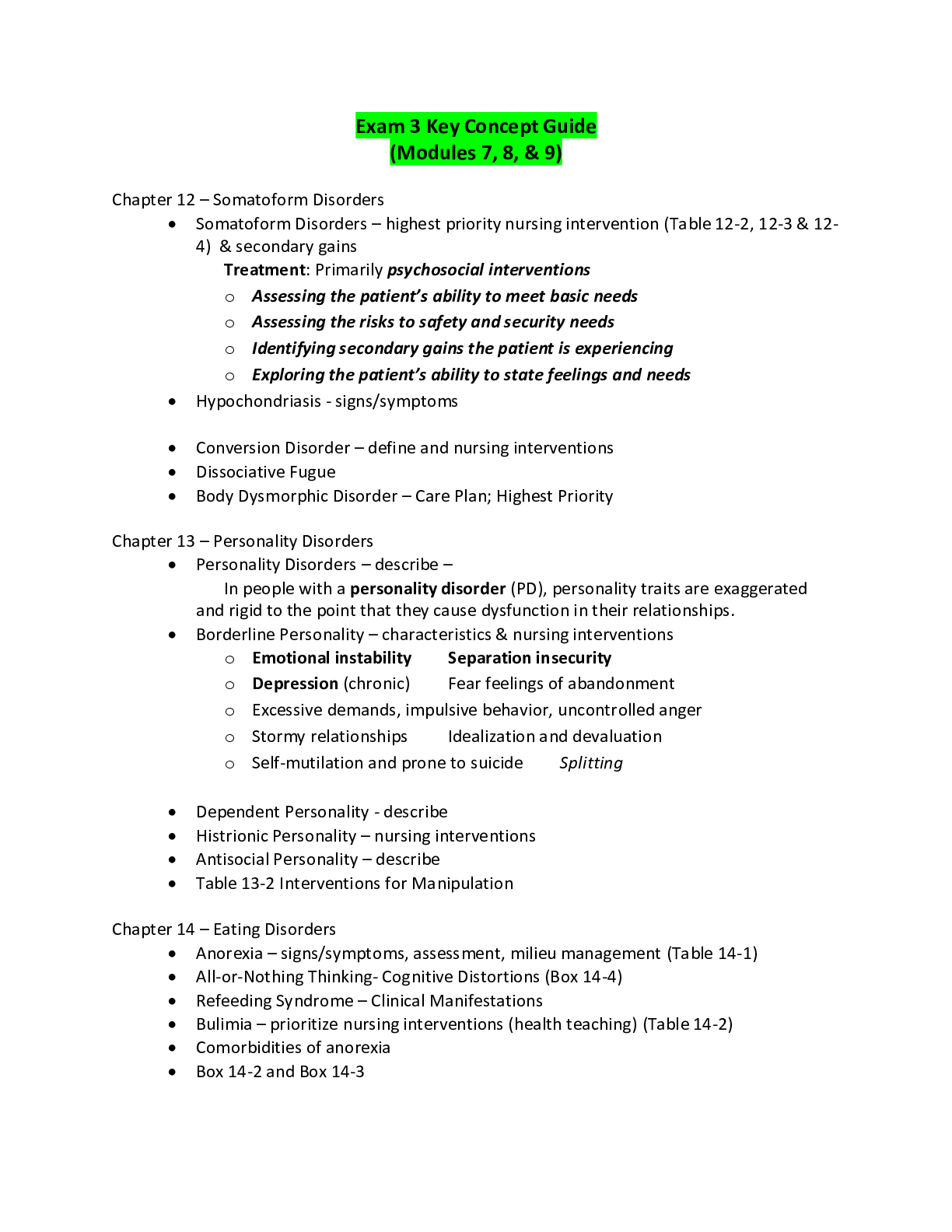
NUR 2488 - Exam 3 Key Concept Guide
Exam 3 Key Concept Guide (Modules 7, 8, & 9) Chapter 12 – Somatoform Disorders • Somatoform Disorders – highest priority nursing intervention (Table 12-2, 12-3 & 12-4) & secondary gains Treatme...
By Ajay25 , Uploaded: Jan 25, 2021
$10
*NURSING> STUDY GUIDE > NR 533 Financial Management In Healthcare Organizations Week 4 Staffing Budgets FTEs Variance Analysis Assignment Guidelines with Scoring Rubric2 (All)
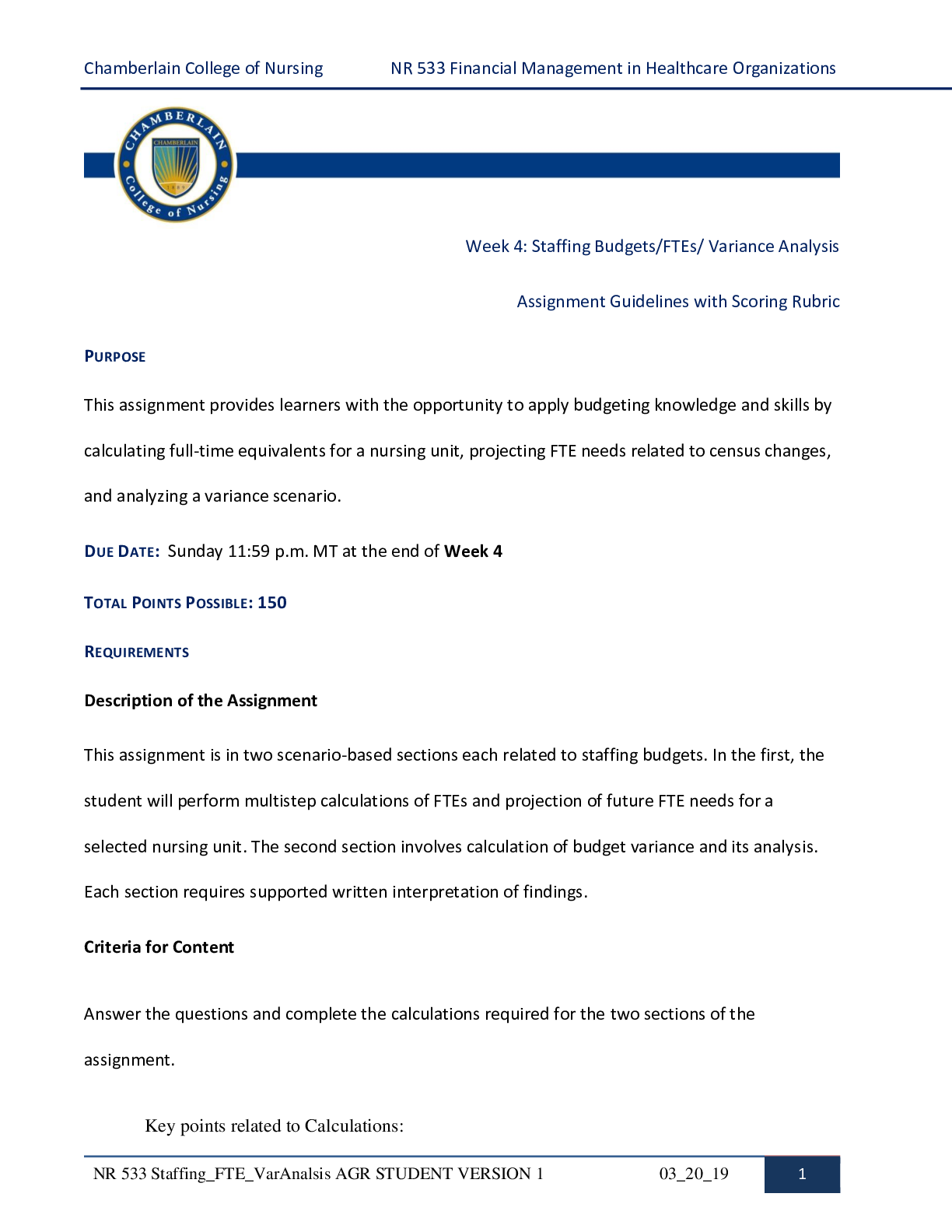
NR 533 Financial Management In Healthcare Organizations Week 4 Staffing Budgets FTEs Variance Analysis Assignment Guidelines with Scoring Rubric2
NR 533 Financial Management In Healthcare Organizations Week 4 Staffing Budgets FTEs Variance Analysis Assignment Guidelines with Scoring Rubric2
By TopScholar , Uploaded: Mar 15, 2021
$11
*NURSING> STUDY GUIDE > NSG 5002 Week 1 Quiz / NSG5002 Week 1 Quiz (All)
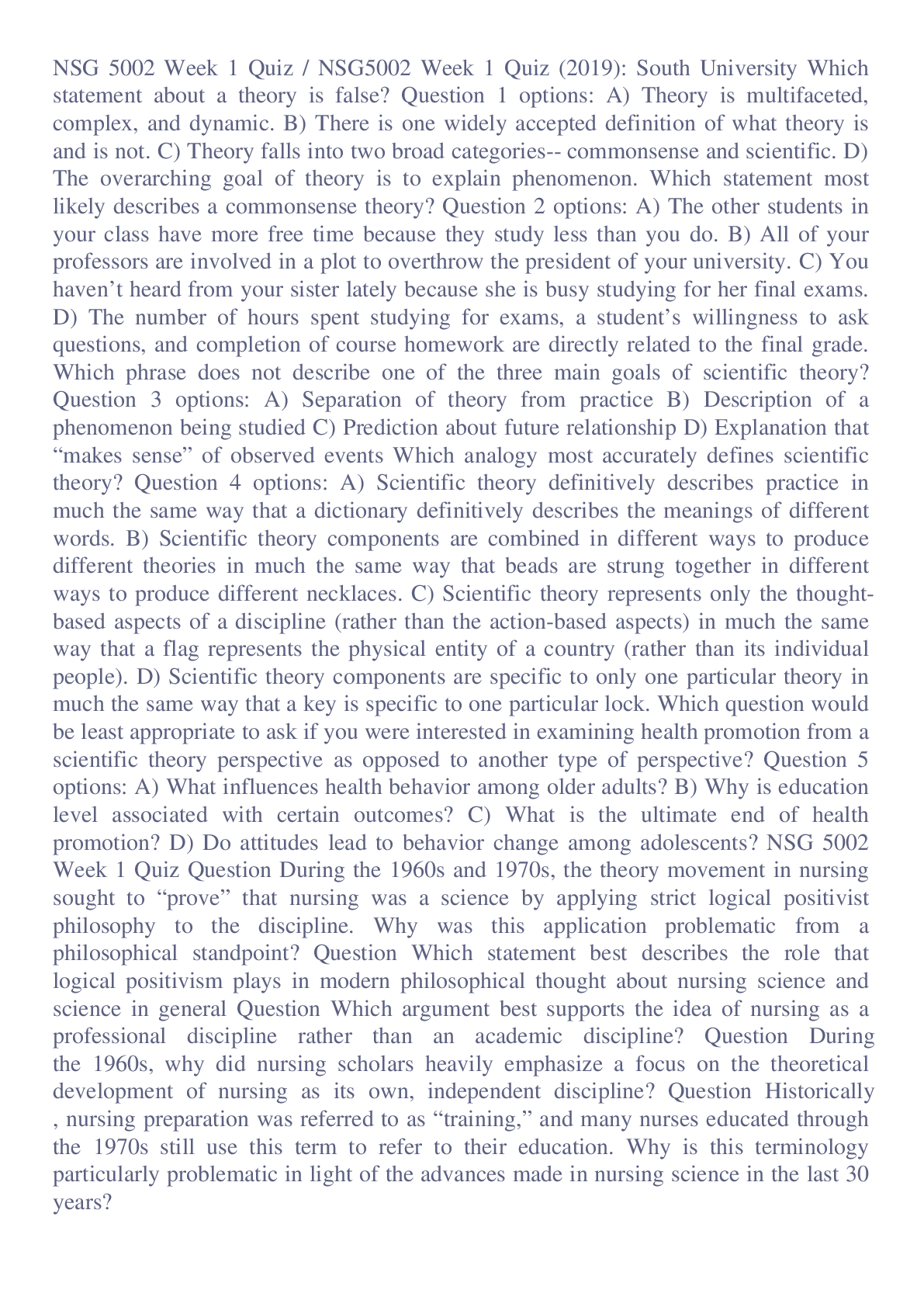
NSG 5002 Week 1 Quiz / NSG5002 Week 1 Quiz
Which statement about a theory is false? Question 1 options: A) Theory is multifaceted, complex, and dynamic. B) There is one widely accepted definition of what theory is and is not. C) Theory falls i...
By Academia1434 , Uploaded: May 30, 2020
$9
*NURSING> STUDY GUIDE > NR 511 Completed Midterm study guide Worksheet. Chamberlain College of Nursing. (All)
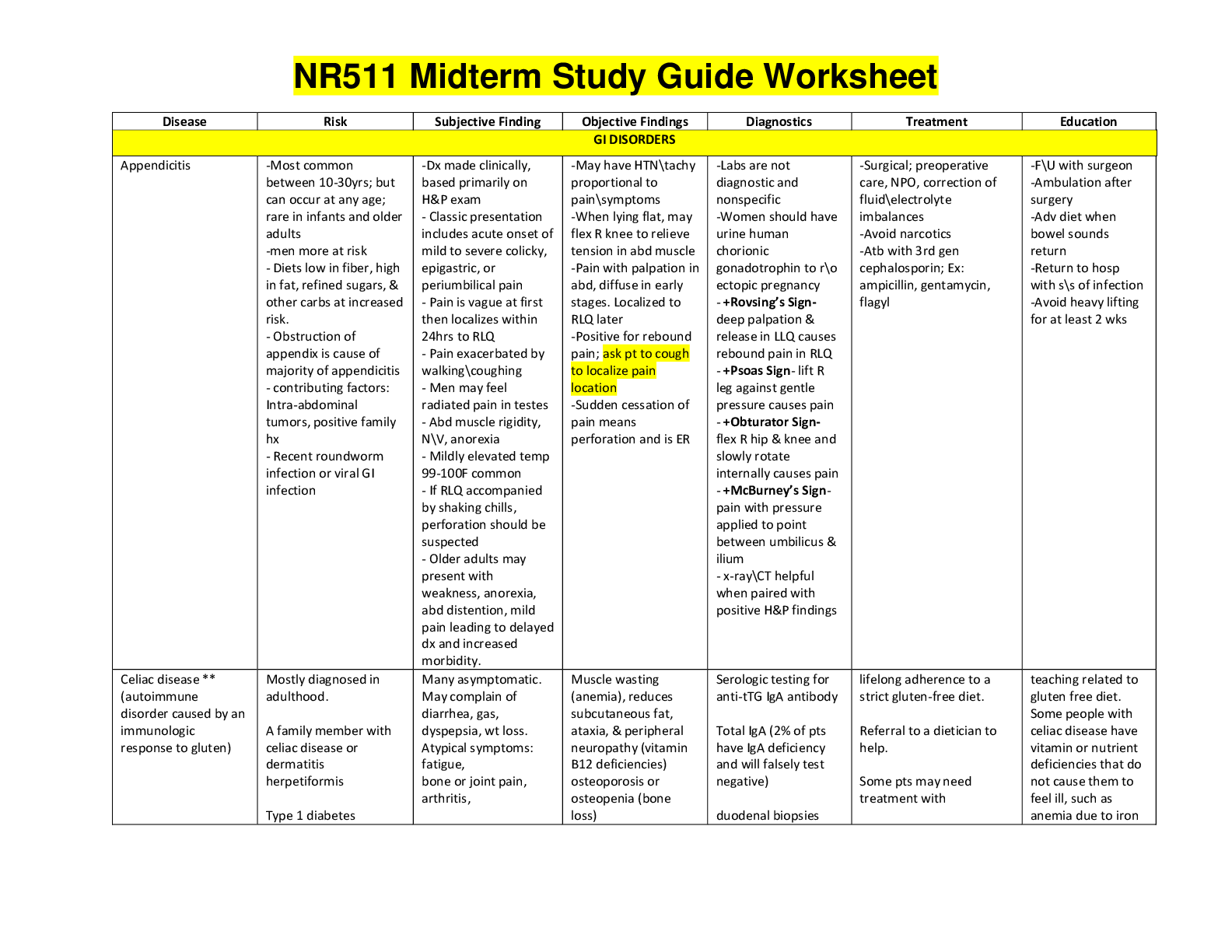
NR 511 Completed Midterm study guide Worksheet. Chamberlain College of Nursing.
NR 511 Completed Midterm study guide | NR511 Midterm Study Guide Worksheet(2020) Complete A+ Guide;Chamberlain College of Nursing. Disease Risk Subjective Finding Objective Findings Diagnostics Treat...
By Expert1 , Uploaded: May 31, 2020
$13
Document information
Connected school, study & course
About the document
Uploaded On
Dec 16, 2020
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Dec 16, 2020
Downloads
0
Views
111