*NURSING > EXAM > Rasmussen College :NURSING BS 3463_120 questions Exam 3 Comprehensive Exam,100% CORRECT (All)
Rasmussen College :NURSING BS 3463_120 questions Exam 3 Comprehensive Exam,100% CORRECT
Document Content and Description Below
Rasmussen College :NURSING BS 3463_120 questions Exam 3 Comprehensive Exam 120 questions A client in the emergency department is having a stroke and the provider has prescribed the tissue plasminoge... n activator (t-PA) alteplase (Activase). The client weighs 146 pounds. How much medication will this client receive? (Record your answer using a whole number.) mg 60 mg The dose of t-PA is 0.9 mg/kg with a maximum dose of 90 mg. The client weighs 66.4 kg. 0.9 mg ´ 66.4 = 59.76 mg, which rounds to 60 mg. Strips to know- V Tach, A-Fib, V-Fib, • What is A-FIB? Atrium is like jello just jiggling back and forth o How to treat ▪ Anticoagulant to prevent clots/thrombi o Monitor-SOB, Palpitations, Anxiety, Diaphoresis, Confusion o Safety at home-clear clutter, no throw rugs, fall preventions o No P waves o Narrow QRS o Irregular-Irregular o Decipher atrial and ventricle rate o Concerned with clots o If someone has cardiovascular disease it is not uncommon for them to have A-Fib o o Ventricular Tachycardia ▪ 3 or more PVC in a row or run • Pre-Ventricular Contraction o Originates below AV node o Wider QRS, bizarre o Do not include in rate o Always has an underlying rhythm ▪ Beat greater then 100 o o Ventricular Fibrillation ▪ Most common cause of hospital arrests ▪ Heart Rate 300-500 ▪ Unable to determine anything-Chaotic-no normal wave forms ▪ Needs to be shocked back into rhythm ▪ No Pulse ▪ Digoxin toxicity is a big cause • • What is a PAC o Pre-Atrial Contraction o Narrow QRS o Originates from an ectopic focus o Count in Heart Rate-it is a profusion beat o Sometimes it can be caused by caffeine o Not a concern unless client is not tolerating o How to treat o • PVC has wide QRS (With underlying rhythm) • Peaked T wave and reasons you may have a peaked T wave- • Hyperkalemia • 13 select all that apply 1. What does ectopic mean? Coming from somewhere other than normal-premature ectopic beats 2. Reasons why you would have and EKG with premature ectopic beats? Anxiety, meds, caffeine, smoking. Does not have anything to do with vagal stimulation or foods with high potassium. 3. Bells Palsey-Know what medications that may be prescribed! Medications that end in Lovir is what type of med? Acyclovir A client has been diagnosed with Bell's palsy. About what drugs should the nurse anticipate possibly teaching the client? (Select all that apply.) a. Acyclovir (Zovirax) b. Carbamazepine (Tegretol) c. Famciclovir (Famvir) d. Prednisone (Deltasone) e. Valacyclovir (Valtrex) ANS: A, C, D, E Possible pharmacologic treatment for Bell's palsy includes acyclovir, famciclovir, prednisone, and valacyclovir. Carbamazepine is an anticonvulsant and mood-stabilizing drug and is not used for Bell's palsy. 4. Whipple A nurse assesses a client who is recovering from a Whipple procedure. Which clinical manifestations alert the nurse to a complication from this procedure? (Select all that apply.) a. Clay-colored stools b. Substernal chest pain c. Shortness of breath d. Lack of bowel sounds or flatus e. Urine output of 20 mL/6 hr ANS: B, C, D, E Myocardial infarction (chest pain), pulmonary embolism (shortness of breath), adynamic ileus (lack of bowel sounds or flatus), and renal failure (urine output of 20 mL/6 hr) are just some of the complications for which the nurse must assess the client after the Whipple procedure. Clay- colored stools are associated with cholecystitis and are not a complication of a Whipple procedure. 5. Hypoparathyroidism and labs calcium na k mg (know norms), anticipated meds to give patient A nurse evaluates the following laboratory results for a client who has hypoparathyroidism: Calcium 7.2 mg/dl Sodium 144 mEq/L Magnesium 1.2 mEq/L Potassium 5.7 mEq/L Based on these results, which medications should the nurse anticipate administering? (Select all that apply.) a. Oral potassium chloride b. Intravenous calcium chloride c. 3% normal saline IV solution d. 50% magnesium sulfate e. Oral calcitriol (Rocaltrol) B, D. The client has hypocalcemia (treated with calcium chloride) and hypomagnesemia (treated with magnesium sulfate). The potassium level is high, so replacement is not needed. The client's sodium level is normal, so hypertonic IV solution is not needed. No information about a vitamin D deficiency is evident, so calcitriol is not needed. 6. PKD signs and symptoms- if your assessing someone for PKD what kind of manifestations would you assess for? Flank pain, abd girth, hematuria, nocturia-the 2 D are not on there! A nurse assesses a client who has a family history of polycystic kidney disease (PKD). For which clinical manifestations should the nurse assess? (Select all that apply.) a. Nocturia b. Flank pain c. Increased abdominal girth d. Dysuria e. Hematuria f. Diarrhea ANS: B, C, E (A according to text book) Clients with PKD experience abdominal distention that manifests as flank pain and increased abdominal girth. Bloody urine is also present with tissue damage secondary to PKD. Clients with PKD often experience constipation, but would not report nocturia or dysuria. 7. The nurse case manager jobs of admission- vitals, assessments, medication reconciliation 8. Interviewing pt and family members you should use open ended questions and appoint one person to speak? Look this up! True or False 9. Chronic ill patients how do you feel their overall quality of life are? What are some things they may not feel are good? True/False 10. Cirrhosis symptoms and labs, you would do and contributing factors A nurse assesses a client who has liver disease. Which laboratory findings should the nurse recognize as potentially causing complications of this disorder? (Select all that apply.) a. Elevated aspartate transaminase b. Elevated international normalized ratio (INR) c. Decreased serum globulin levels d. Decreased serum alkaline phosphatase e. Elevated serum ammonia f. Elevated prothrombin time (PT) ANS: B, E, F Elevated INR and PT are indications of clotting disturbances and alert the nurse to the increased possibility of hemorrhage. Elevated ammonia levels increase the client's confusion. The other values are abnormal and associated with liver disease but do not necessarily place the client at increased risk for complications. 11. Liver trauma-main thing to worry about is bleeding-low pressures, tachycardia, confusion, bruising, worry about hypovolemic-it’s a volume issue An emergency room nurse assesses a client with potential liver trauma. Which clinical manifestations should alert the nurse to internal bleeding and hypovolemic shock? (Select all that apply.) a. Hypertension b. Tachycardia c. Flushed skin d. Confusion e. Shallow respirations ANS: B, D Symptoms of hemorrhage and hypovolemic shock include hypotension, tachycardia, tachypnea, pallor, diaphoresis, cool and clammy skin, and confusion 12. What factors must be present to transmit infections-select all that apply The student nurse caring for clients understands that which factors must be present to transmit infection? (Select all that apply.) a. Colonization b. Host c. Mode of transmission d. Portal of entry e. Reservoir ANS: B, C, D, E Factors that must be present in order to transmit an infection include a host with a portal of entry, a mode of transmission, and a reservoir. Colonization is not one of these factors. 13. Standard precautions and what they entail Which statements are true regarding Standard Precautions? (Select all that apply.) a. Always wear a gown when performing hygiene on clients. b. Sneeze into your sleeve or into a tissue that you throw away. c. Remain 3 feet away from any client who has an infection. d. Use personal protective equipment as needed for client care. e. Wear gloves when touching client excretions or secretions. ANS: D, E Standard Precautions implies that contact with bodily secretions, excretions, and moist mucous membranes and tissues (excluding perspiration) is potentially infectious. Always wear gloves when coming into contact with such material. Other personal protective equipment is used based on the care being given. For example, if face splashing is expected, you should also wear a mask. Wearing a gown for hygiene is not required. Sneezing into your sleeve or tissue is part of respiratory etiquette. Remaining 3 feet away from clients is also not part of Standard Precautions. A nurse prepares to provide perineal care to a client with meningococcal meningitis. Which personal protective equipment should the nurse wear? (Select all that apply.) a. Particulate respirator b. Isolation gown c. Shoe covers d. Surgical mask e. Gloves ANS: D, E Meningeal meningitis is spread via saliva and droplets, and Droplet Precautions are necessary. Caregivers should wear a surgical mask when within 6 feet of the client and should continue to use Standard Precautions, including gloves. A particulate respirator, an isolation gown, and shoe covers are not necessary for Droplet Precautions. 14. Know what you have to do if you suspect TB as a nurse A client is being admitted with suspected tuberculosis (TB). What actions by the nurse are best? (Select all that apply.) a. Admit the client to a negative-airflow room. b. Maintain a distance of 3 feet from the client at all times. c. Order specialized masks/respirators for caregiving. d. Other than wearing gloves, no special actions are needed. e. Wash hands with chlorhexidine after providing care. ANS: A, C A client with suspected TB is admitted to Airborne Precautions, which includes a negative-airflow room and special N95 or PAPR masks to be worn when providing care. A 3-foot distance is required for Droplet Precautions. Chlorhexidine is used for clients with a high risk of infection. While triaging clients in a crowded emergency department, a nurse assesses a client who presents with symptoms of tuberculosis. Which action should the nurse take first? a. Apply oxygen via nasal cannula. b. Administer intravenous 0.9% saline solution. c. Transfer the client to a negative-pressure room. d. Obtain a sputum culture and sensitivity. ANS: C A client with signs and symptoms of tuberculosis or other airborne pathogens should be placed in a negative- pressure room to prevent contamination of staff, clients, and family members in the crowded emergency department. 15. What does your spleen do? Multiple Choice 1. Coronary Bypass how often are you doing vitals if your doing activity intolerance? 2. The dying patient-lots of pain experienced because nerve ending are shutting down 3. Advanced Directives After teaching a client about advance directives, a nurse assesses the clients understanding. Which statement indicates the client correctly understands the teaching? a. An advance directive will keep my children from selling my home when Im old. b. An advance directive will be completed as soon as Im incapacitated and cant think for myself. c. An advance directive will specify what I want done when I can no longer make decisions about health care. d. An advance directive will allow me to keep my money out of the reach of my family. ANS: C An advance directive is a written document prepared by a competent individual that specifies what, if any, extraordinary actions a person would want taken when he or she can no longer make decisions about personal health care. It does not address issues such as the clients residence or financial matters. 4. Mass Casualty Triage A hospital responds to a local mass casualty event. Which action should the nurse supervisor take to prevent staff post-traumatic stress disorder during a mass casualty event? a. Provide water and healthy snacks for energy throughout the event. b. Schedule 16-hour shifts to allow for greater rest between shifts. c. Encourage counseling upon deactivation of the emergency response plan. d. Assign staff to different roles and units within the medical facility. a. Provide water and healthy snacks for energy throughout the event. To prevent staff post-traumatic stress disorder during a mass casualty event, the nurses should use available counseling, encourage and support co-workers, monitor each others stress level and performance, take breaks when needed, talk about feelings with staff and managers, and drink plenty of water and eat healthy snacks for energy. Nurses should also keep in touch with family, friends, and significant others, and not work for more than 12 hours per day. Encouraging counseling upon deactivation of the plan, or after the emergency response is over, does not prevent stress during the casualty event. Assigning staff to unfamiliar roles or units may increase situational stress and is not an approach to prevent post-traumatic stress disorder. A nurse is field-triaging clients after an industrial accident. Which client condition should the nurse triage with a red tag? a. Dislocated right hip and an open fracture of the right lower leg b. Large contusion to the forehead and a bloody nose c. Closed fracture of the right clavicle and arm numbness d. Multiple fractured ribs and shortness of breath d. Multiple fractured ribs and shortness of breath Clients who have an immediate threat to life are given the highest priority, are placed in the emergent or class I category, and are given a red triage tag. The client with multiple rib fractures and shortness of breath most likely has developed a pneumothorax, which may be fatal if not treated immediately. The client with the hip and leg problem and the client with the clavicle fracture would be classified as class II; these major but stable injuries can wait 30 minutes to 2 hours for definitive care. The client with facial wounds would be considered the walking wounded and classified as nonurgent. Emergency medical services (EMS) brings a large number of clients to the emergency department following a mass casualty incident. The nurse identifies the clients with which injuries with yellow tags? (Select all that apply.) a. Partial-thickness burns covering both legs b. Open fractures of both legs with absent pedal pulses c. Neck injury and numbness of both legs d. Small pieces of shrapnel embedded in both eyes e. Head injury and difficult to arouse f. Bruising and pain in the right lower abdomen A, C, D, F Clients with burns, spine injuries, eye injuries, and stable abdominal injuries should be treated within 30 minutes to 2 hours, and therefore should be identified with yellow tags. The client with the open fractures and the client with the head injury would be classified as urgent with red tags. A nurse triages clients arriving at the hospital after a mass casualty. Which clients are correctly classified? (Select all that apply.) a. A 35-year-old female with severe chest pain: red tag b. A 42-year-old male with full-thickness body burns: green tag c. A 55-year-old female with a scalp laceration: black tag d. A 60-year-old male with an open fracture with distal pulses: yellow tag e. An 88-year-old male with shortness of breath and chest bruises: green tag A, D Red-tagged clients need immediate care due to life-threatening injuries. A client with severe chest pain would receive a red tag. Yellow-tagged clients have major injuries that should be treated within 30 minutes to 2 hours. A client with an open fracture with distal pulses would receive a yellow tag. The client with fullthickness body burns would receive a black tag. The client with a scalp laceration would receive a green tag, and the client with shortness of breath would receive a red tag. 5. ER triage prioritizing-Airway and chest pain* An emergency room nurse is triaging victims of a multi-casualty event. Which client should receive care first? a. A 30-year-old distraught mother holding her crying child b. A 65-year-old conscious male with a head laceration c. A 26-year-old male who has pale, cool, clammy skin d. A 48-year-old with a simple fracture of the lower leg ANS: C The client with pale, cool, clammy skin is in shock and needs immediate medical attention. The mother does not have injuries and so would be the lowest priority. The other two people need medical attention soon, but not at the expense of a person in shock. A nurse is triaging clients in the emergency department (ED). Which client should the nurse prioritize to receive care first? a. A 22-year-old with a painful and swollen right wrist b. A 45-year-old reporting chest pain and diaphoresis c. A 60-year-old reporting difficulty swallowing and nausea d. An 81-year-old with a respiratory rate of 28 breaths/min and a temperature of 101 F ANS: B A client experiencing chest pain and diaphoresis would be classified as emergent and would be triaged immediately to a treatment room in the ED. The other clients are more stable. A nurse is triaging clients in the emergency department. Which client should be considered urgent? a. A 20-year-old female with a chest stab wound and tachycardia b. A 45-year-old homeless man with a skin rash and sore throat c. A 75-year-old female with a cough and a temperature of 102 F d. A 50-year-old male with new-onset confusion and slurred speech ANS: C A client with a cough and a temperature of 102 F is urgent. This client is at risk for deterioration and needs to be seen quickly, but is not in an immediately life-threatening situation. The client with a chest stab wound and tachycardia and the client with new-onset confusion and slurred speech should be triaged as emergent. The client with a skin rash and a sore throat is not at risk for deterioration and would be triaged as nonurgent. A nurse is triaging clients in the emergency department. Which client should the nurse classify as nonurgent? a. A 44-year-old with chest pain and diaphoresis b. A 50-year-old with chest trauma and absent breath sounds c. A 62-year-old with a simple fracture of the left arm d. A 79-year-old with a temperature of 104 F ANS: C A client in a nonurgent category can tolerate waiting several hours for health care services without a significant risk of clinical deterioration. The client with a simple arm fracture and palpable radial pulses is currently stable, is not at significant risk of clinical deterioration, and would be considered nonurgent. The client with chest pain and diaphoresis and the client with chest trauma are emergent owing to the potential for clinical deterioration and would be seen immediately. The client with a high fever may be stable now but also has a risk of deterioration. 6. Functions of trauma centers and levels-generalization (1 questions) A nurse is evaluating levels and functions of trauma centers. Which function is appropriately paired with the level of the trauma center? a. Level I Located within remote areas and provides advanced life support within resource capabilities b. Level II Located within community hospitals and provides care to most injured clients c. Level III Located in rural communities and provides only basic care to clients d. Level IV Located in large teaching hospitals and provides a full continuum of trauma care for all clients ANS: B Level I trauma centers are usually located in large teaching hospital systems and provide a full continuum of trauma care for all clients. Both Level II and Level III facilities are usually located in community hospitals. These trauma centers provide care for most clients and transport to Level I centers when client needs exceed resource capabilities. Level IV trauma centers are usually located in rural and remote areas. These centers provide basic care, stabilization, and advanced life support while transfer arrangements to higher-level trauma centers are made. 7. Know about prolonged exposure to cold-how do you warm them up in ER A client presents to the emergency department after prolonged exposure to the cold. The client is difficult to arouse and speech is incoherent. Which action should the nurse take first? a. Reposition the client into a prone position. b. Administer warmed intravenous fluids to the client. c. Wrap the clients extremities in warm blankets. d. Initiate extracorporeal rewarming via hemodialysis. b. Administer warmed intravenous fluids to the client. Moderate hypothermia manifests with muscle weakness, increased loss of coordination, acute confusion, apathy, incoherence, stupor, and impaired clotting. Moderate hypothermia should be treated by core rewarming methods, which include administration of warm IV fluids, heated oxygen, and heated peritoneal, pleural, gastric, or bladder lavage, and by positioning the client in a supine position to prevent orthostatic changes. The clients trunk should be warmed prior to the extremities to prevent peripheral vasodilation. Extracorporeal warming with cardiopulmonary bypass or hemodialysis is a treatment for severe hypothermia. 8. Lightning strike-check cardiac rhythm An emergency department nurse assesses a client admitted after a lightning strike. Which assessment should the nurse complete first? a. Electrocardiogram (ECG) b. Wound inspection c. Creatinine kinase d. Computed tomography of head a. Electrocardiogram (ECG) Clients who survive an immediate lightning strike can have serious myocardial injury, which can be manifested by ECG and myocardial perfusion abnormalities. The nurse should prioritize the ECG. Other assessments should be completed but are not the priority. 9. How do you treat a high potassium? Calcium gluconate, Albuterol, Na Bicarb, Dextrose, Insulin, Kayexalate (Candi K) The health care provider writes orders for a client who is admitted with a serum potassium level of 6.9 mEq/L. What does the nurse implement FIRST? A. Administer sodium polystyrene sulfonate (Kayexalate) orally. B. Ensure that a potassium-restricted diet is ordered. C. Place the client on a cardiac monitor. D. Teach the client about foods that are high in potassium. Answer: C Rationale: Because hyperkalemia can lead to life-threatening bradycardia, the initial action should be to place the client on a cardiac monitor. Administering a potassium-reducing medication, recommending a potassium-restricted diet, and teaching the client about diet are appropriate but will not immediately decrease the serum potassium level and do not need to be implemented as quickly as monitoring cardiac rhythm. A 77-year-old woman is brought to the emergency department by her family after she has had diarrhea for 3 days. The family tells the nurse that she has not been eating or drinking well, but that she has been taking her diuretics for congestive heart failure. Laboratory results include a potassium level of 7.0 mEq/L. Which medication does the nurse anticipate administering? A. Insulin (regular insulin) and dextrose (D20W) B. Loperamide (Imodium) C. Sodium polystyrene sulfonate (Kayexalate) D. Supplemental potassium Answer: A Rationale: If potassium levels are high, a combination of 20 units of regular insulin in 100 mL of 20% dextrose in water may be prescribed to promote movement of potassium from the blood into the intracellular fluid. Imodium is used in the treatment of diarrhea. Kayexalate is used for hyperkalemia, but not when the potassium level is this high (7.0). Additional potassium would make the client's condition more critical. 10. Know Eliza Testing A nurse is talking with a client about a negative enzyme-linked immunosorbent assay (ELISA) test for human immune deficiency virus (HIV) antibodies. The test is negative and the client states Whew! I was really worried about that result. What action by the nurse is most important? a. Assess the clients sexual activity and patterns. b. Express happiness over the test result. c. Remind the client about safer sex practices. d. Tell the client to be retested in 3 months. ANS: A The ELISA test can be falsely negative if testing occurs after the client has become infected but prior to making antibodies to HIV. This period of time is known as the window period and can last up to 36 months. The nurse needs to assess the clients sexual behavior further to determine the proper response. The other actions are not the most important, but discussing safer sex practices is always appropriate. 11. Carcinogenesis- what is it? Which statement about carcinogenesis is accurate? a. An initiated cell will always become clinical cancer. b. Cancer becomes a health problem once it is 1 cm in size. c. Normal hormones and proteins do not promote cancer growth. d. Tumor cells need to develop their own blood supply. ANS: D Tumors need to develop their own blood supply through a process called angiogenesis. An initiated cell needs a promoter to continue its malignant path. Normal hormones and proteins in the body can act as promoters. A 1-cm tumor is a detectable size, but other events have to occur for it to become a health problem. 12. Radiation and Chemo- Know dos and donts and what it is and does, what do you have to watch for? A client tells the oncology nurse about an upcoming vacation to the beach to celebrate completing radiation treatments for cancer. What response by the nurse is most appropriate? a. Avoid getting salt water on the radiation site. b. Do not expose the radiation area to direct sunlight. c. Have a wonderful time and enjoy your vacation! d. Remember you should not drink alcohol for a year. ANS: B The skin overlying the radiation site is extremely sensitive to sunlight after radiation therapy has been completed. The nurse should inform the client to avoid sun exposure to this area. This advice continues for 1 year after treatment has been completed. The other statements are not appropriate. The nurse has taught a client with cancer ways to prevent infection. What statement by the client indicates that more teaching is needed? a. I should take my temperature daily and when I dont feel well. b. I will wash my toothbrush in the dishwasher once a week. c. I wont let anyone share any of my personal items or dishes. d. Its alright for me to keep my pets and change the litter box. ANS: D Clients should wash their hands after touching their pets and should not empty or scoop the cat litter box. The other statements are appropriate for self-management. 13. Burns (4-5 questions) An emergency room nurse assesses a client who was rescued from a home fire. The client suddenly develops a loud, brassy cough. Which action should the nurse take first? a. Apply oxygen and continuous pulse oximetry. b. Provide small quantities of ice chips and sips of water. c. Request a prescription for an antitussive medication. d. Ask the respiratory therapist to provide humidified air. ANS: A Brassy cough and wheezing are some of the signs seen with inhalation injury. The first action by the nurse is to give the client oxygen. Clients with possible inhalation injury also need continuous pulse oximetry. Ice chips and humidified room air will not help the problem, and antitussives are not warranted. A nurse prepares to administer intravenous cimetidine (Tagamet) to a client who has a new burn injury. The client asks, Why am I taking this medication? How should the nurse respond? a. Tagamet stimulates intestinal movement so you can eat more. b. It improves fluid retention, which helps prevent hypovolemic shock. c. It helps prevent stomach ulcers, which are common after burns. d. Tagamet protects the kidney from damage caused by dehydration. ANS: C Ulcerative gastrointestinal disease (Curlings ulcer) may develop within 24 hours after a severe burn as a result of increased hydrochloric acid production and a decreased mucosal barrier. This process occurs because of the sympathetic nervous system stress response. Cimetidine is a histamine2 blocker and inhibits the production and release of hydrochloric acid. Cimetidine does not affect intestinal movement and does not prevent hypovolemic shock or kidney damage. A nurse cares for a client with a burn injury who presents with drooling and difficulty swallowing. Which action should the nurse take first? a. Assess the level of consciousness and pupillary reactions. b. Ascertain the time food or liquid was last consumed. c. Auscultate breath sounds over the trachea and bronchi. d. Measure abdominal girth and auscultate bowel sounds. ANS: C Inhalation injuries are present in 7% of clients admitted to burn centers. Drooling and difficulty swallowing can mean that the client is about to lose his or her airway because of this injury. Absence of breath sounds over the trachea and bronchi indicates impending airway obstruction and demands immediate intubation. Knowing the level of consciousness is important in assessing oxygenation to the brain. Ascertaining the time of last food intake is important in case intubation is necessary (the nurse will be more alert for signs of aspiration). However, assessing for air exchange is the most important intervention at this time. Measuring abdominal girth is not relevant in this situation. A nurse receives new prescriptions for a client with severe burn injuries who is receiving fluid resuscitation per the Parkland formula. The clients urine output continues to range from 0.2 to 0.25 mL/kg/hr. Which prescription should the nurse question? a. Increase intravenous fluids by 100 mL/hr. b. Administer furosemide (Lasix) 40 mg IV push. c. Continue to monitor urine output hourly. d. Draw blood for serum electrolytes STAT. ANS: B The plan of care for a client with a burn includes fluid and electrolyte resuscitation. Furosemide would be inappropriate to administer. Postburn fluid needs are calculated initially by using a standardized formula such as the Parkland formula. However, needs vary among clients, and the final fluid volume needed is adjusted to maintain hourly urine output at 0.5 mL/kg/hr. Based on this clients inadequate urine output, fluids need to be increased, urine output needs to be monitored hourly, and electrolytes should be evaluated to ensure appropriate fluids are being infused. A nurse reviews the laboratory results for a client who was burned 24 hours ago. Which laboratory result should the nurse report to the health care provider immediately? a. Arterial pH: 7.32 b. Hematocrit: 52% c. Serum potassium: 6.5 mEq/L d. Serum sodium: 131 mEq/L ANS: C The serum potassium level is changed to the degree that serious life-threatening responses could result. With such a rapid rise in potassium level, the client is at high risk for experiencing severe cardiac dysrhythmias and death. All the other findings are abnormal but do not show the same degree of severity; they would be expected in the emergent phase after a burn injury. A nurse assesses a client who has burn injuries and notes crackles in bilateral lung bases, a respiratory rate of 40 breaths/min, and a productive cough with blood-tinged sputum. Which action should the nurse take next? a. Administer furosemide (Lasix). b. Perform chest physiotherapy. c. Document and reassess in an hour. d. Place the client in an upright position. ANS: D Pulmonary edema can result from fluid resuscitation given for burn treatment. This can occur even in a young healthy person. Placing the client in an upright position can relieve lung congestion immediately before other measures can be carried out. Although Lasix may be used to treat pulmonary edema in clients who are fluid overloaded, a client with a burn injury will lose a significant amount of fluid through the broken skin; therefore, Lasix would not be appropriate. Chest physiotherapy will not get rid of fluid. A nurse assesses bilateral wheezes in a client with burn injuries inside the mouth. Four hours later the wheezing is no longer heard. Which action should the nurse take? a. Document the findings and reassess in 1 hour. b. Loosen any constrictive dressings on the chest. c. Raise the head of the bed to a semi-Fowlers position. d. Gather appropriate equipment and prepare for an emergency airway. ANS: D Clients with severe inhalation injuries may sustain such progressive obstruction that they may lose effective movement of air. When this occurs, wheezing is no longer heard, and neither are breath sounds. These clients can lose their airways very quickly, so prompt action is needed. The client requires establishment of an emergency airway. Swelling usually precludes intubation. The other options do not address this emergency situation. A nurse uses the rule of nines to assess a client with burn injuries to the entire back region and left arm. How should the nurse document the percentage of the clients body that sustained burns? a. 9% b. 18% c. 27% d. 36% ANS: C According to the rule of nines, the posterior trunk, anterior trunk, and legs each make up 18% of the total body surface. The head, neck, and arms each make up 9% of total body surface, and the perineum makes up 1%. In this case, the client received burns to the back (18%) and one arm (9%), totaling 27% of the body. A nurse reviews the following data in the chart of a client with burn injuries: Admission Notes 36-year-old female with bilateral leg burns NKDA Wound Assessment Bilateral leg burns present with a white and leather- like appearance. No blisters or bleeding present. Client rates pain 2/10 on a scale of 0- 10. Health history of asthma and seasonal allergies Based on the data provided, how should the nurse categorize this clients injuries? a. Partial-thickness deep b. Partial-thickness superficial c. Full thickness d. Superficial ANS: C The characteristics of the clients wounds meet the criteria for a full-thickness injury: color that is black, brown, yellow, white, or red; no blisters; minimal pain; and firm and inelastic outer layer. Partial-thickness superficial burns appear pink to red and are painful. Partial-thickness deep burns are deep red to white and painful. Superficial burns are pink to red and are also painful. After assessing an older adult client with a burn wound, the nurse documents the findings as follows: Vital Signs Heart rate: 110 beats/min Blood pressure: 112/68 mm Hg Respiratory rate: 20 Oxygen saturation: 94% Pain: 3/10 Laboratory Results Red blood cell count: 5,000,000/mm3 White blood cell count: 10,000/mm3 Platelet count: 200,000/mm3 Wound Assessment Left chest burn wound, 3 cm 2.5 cm 0.5 cm, wound bed pale, surrounding tissues with edema Based on the documented data, which action should the nurse take next? a. Assess the clients skin for signs of adequate perfusion. b. Calculate intake and output ratio for the last 24 hours. c. Prepare to obtain blood and wound cultures. d. Place the client in an isolation room. ANS: C Older clients have a decreased immune response, so they may not exhibit signs that their immune system is actively fighting an infection, such as fever or an increased white blood cell count. They also are at higher risk for sepsis arising from a localized wound infection. The burn wound shows signs of local infection, so the nurse should assess for this and for systemic infection before the client manifests sepsis. Placing the client in an isolation room, calculating intake and output, and assessing the clients skin should all be implemented but these actions do not take priority over determining whether the client has an infection. An emergency room nurse implements fluid replacement for a client with severe burn injuries. The provider prescribes a liter of 0.9% normal saline to infuse over 1 hour and 30 minutes via gravity tubing with a drip factor of 30 drops/mL. At what rate should the nurse administer the infusion? (Record your answer using a whole number and rounding to the nearest drop.) drops/min 333 drops/min 1000 mL divided by 90 minutes, then multiplied by 30 drops, equals 333 drops/min. 14. What is a PE? How do they treat it? A client has been diagnosed with a very large pulmonary embolism (PE) and has a dropping blood pressure. What medication should the nurse anticipate the client will need as the priority? a. Alteplase (Activase) b. Enoxaparin (Lovenox) c. Unfractionated heparin d. Warfarin sodium (Coumadin) ANS: A a. Alteplase (Activase) Activase is a "clot-busting" agent indicated in large PEs in the setting of hemodynamic instability. The nurse knows this drug is the priority, although heparin may be started initially. Enoxaparin and warfarin are not indicated in this setting. 15. Know PTT, PT/INR levels and how to treat 4.A client is on intravenous heparin to treat a pulmonary embolism. The client's most recent partial thromboplastin time (PTT) was 25 seconds. What order should the nurse anticipate? a. Decrease the heparin rate. b. Increase the heparin rate. c. No change to the heparin rate. d. Stop heparin; start warfarin (Coumadin). ANS: B b. Increase the heparin rate. For clients on heparin, a PTT of 1.5 to 2.5 times the normal value is needed to demonstrate the heparin is working. A normal PTT is 25 to 35 seconds, so this client's PTT value is too low. The heparin rate needs to be increased. Warfarin is not indicated in this situation. 16. Know platelet count and WBC count 6.A nurse is caring for four clients on intravenous heparin therapy. Which laboratory value possibly indicates that a serious side effect has occurred? a. Hemoglobin: 14.2 g/dL b. Platelet count: 82,000/L c. Red blood cell count: 4.8/mm3 d. White blood cell count: 8.7/mm3 ANS: B b. Platelet count: 82,000/L This platelet count is low and could indicate heparin-induced thrombocytopenia. The other values are normal for either gender. 17. Zantac .A client is on mechanical ventilation and the client's spouse wonders why ranitidine (Zantac) is needed since the client "only has lung problems." What response by the nurse is best? a. "It will increase the motility of the gastrointestinal tract." b. "It will keep the gastrointestinal tract functioning normally." c. "It will prepare the gastrointestinal tract for enteral feedings." d. "It will prevent ulcers from the stress of mechanical ventilation." ANS: D d. "It will prevent ulcers from the stress of mechanical ventilation." Stress ulcers occur in many clients who are receiving mechanical ventilation, and often prophylactic medications are used to prevent them. Frequently used medications include antacids, histamine blockers, and proton pump inhibitors. Zantac is a histamine blocking agent. 18. Coumadin/Warfarin-Know dietary restrictions A client is being discharged soon on warfarin (Coumadin). What menu selection for dinner indicates the client needs more education regarding this medication? a. Hamburger and French fries b. Large chef's salad and muffin c. No selection; spouse brings pizza d. Tuna salad sandwich and chips ANS: B b. Large chef's salad and muffin Warfarin works by inhibiting the synthesis of vitamin K-dependent clotting factors. Foods high in vitamin K thus interfere with its action and need to be eaten in moderate, consistent amounts. The chef's salad most likely has too many leafy green vegetables, which contain high amounts of vitamin K. The other selections, while not particularly healthy, will not interfere with the medication's mechanism of action. A nurse is teaching a client about warfarin (Coumadin). What assessment finding by the nurse indicates a possible barrier to self-management? a. Poor visual acuity b. Strict vegetarian c. Refusal to stop smoking d. Wants weight loss surgery ANS: B b. Strict vegetarian Warfarin works by inhibiting the synthesis of vitamin K-dependent clotting factors. Foods high in vitamin K thus interfere with its action and need to be eaten in moderate, consistent amounts. A vegetarian may have trouble maintaining this diet. The nurse should explore this possibility with the client. The other options are not related. 19. Risk factors for cardiovascular disease 20. S/S of stroke? First thing you would address! 21. EKG know what the P(Atrium) and QRS represent 22. Amiodarone-What does it do and treat and interventions you would expect 23. Right sided heart failure A client is diagnosed with right-sided heart failure. Which assessment findings will the nurse expect the client to have? (Select all that apply.) a. Peripheral edema b. Crackles in both lungs c. Increased abdominal girth d. Ascites e. Tachypnea ANS: A, C, D, E Peripheral edema, increased abdominal girth, ascites, and tachypnea are all symptoms associated with right-sided heart failure due to the back up into the peripheral system. Crackles in the lungs are associated with left-sided heart failure. 24. Digoxin-food/diet An 84-year-old client with heart failure presents to the emergency department with confusion, blurry vision, and an upset stomach. Which assessment data is most concerning to the nurse? a. Digoxin (Lanoxin) therapy daily. b. Daily metoprolol (Lopressor). c. Furosemide (Lasix) twice daily. d. Currently taking an antacid for upset stomach ANS: A Confusion, blurry vision, and upset stomach are symptoms of Digoxin toxicity, which is common in older adults and requires immediate treatment. The other answers are important assessment data but do not indicate immediate connection to the client's presentation. 25. Cholesterol levels The nurse is reviewing the lipid panel of a male client who has atherosclerosis. Which finding is most concerning? a. Cholesterol: 126 mg/dL b. High-density lipoprotein cholesterol (HDL-C): 48 mg/dL c. Low-density lipoprotein cholesterol (LDL-C): 122 mg/dL d. Triglycerides: 198 mg/dL Triglycerides: 198 mg/dL 26. Furosemide/Lasix The nurse is caring for four hypertensive clients. Which drug-laboratory value combination should the nurse report immediately to the health care provider? a. Furosemide (Lasix)/potassium: 2.1 mEq/L b. Hydrochlorothiazide (Hydrodiuril)/potassium: 4.2 mEq/L c. Spironolactone (Aldactone)/potassium: 5.1 mEq/L d. Torsemide (Demadex)/sodium: 142 mEq/L Furosemide ( Lasix )/ potassium: 2.1 mEq/L Lasix is a loop diuretic and can cause hypokalemia. A potassium level of 2.1 mEq/L is quite low and should be reported immediately. Spironolactone is a potassium-sparing diuretic that can cause hyperkalemia. A potassium level of 5.1 mEq/L is on the high side, but it is not as critical as the low potassium with furosemide. The other two laboratory values are normal. 27. HCTZ 28. Spironolactone The nurse is providing discharge instructions to a client on spironolactone (Aldactone) therapy. Which comment by the client indicates a need for further teaching? A. "I must call the provider if I am more tired than usual." B. "I need to increase my salt intake." C. "I should eat a banana every day." D. "This drug will not control my heart rate." C. Spironolactone increases potassium levels, so potassium supplements and foods rich in potassium, such as bananas, should be avoided to prevent hyperkalemia. While taking spironolactone, symptoms of hyponatremia such as drowsiness and lethargy must be reported; the client may need increased dietary sodium. Spironolactone will not have an effect on the client's heart rate. 29. Torsemide 30. PVD 31. Several delegations question A nurse collaborates with an unlicensed assistive personnel (UAP) to provide care for a client who is in the healing phase of acute pancreatitis. Which statements focused on nutritional requirements should the nurse include when delegating care for this client? (Select all that apply.) a. "Do not allow the client to eat between meals." b. "Make sure the client receives a protein shake." c. "Do not allow caffeine-containing beverages." d. "Make sure the foods are bland with little spice." e. "Do not allow high-carbohydrate food items." ANS: B, C, D During the healing phase of pancreatitis, the client should be provided small, frequent, moderate- to high-carbohydrate, high-protein, low-fat meals. Protein shakes can be provided to supplement the diet. Foods and beverages should not contain caffeine and should be bland. A client with iatrogenic Cushing's syndrome is a resident in a long-term care facility. Which nursing action included in the client's care would be best to delegate to unlicensed assistive personnel (UAP)? A. Assist with personal hygiene and skin care. B. Develop a plan of care to minimize risk for infection. C. Instruct the client on the reasons to avoid overeating. D. Monitor for signs and symptoms of fluid retention. A. Assisting a client with bathing and skin care is included in UAP scope of practice. It is not within their scope of practice to develop a plan of care, although they will play a very important role in following the plan of care. Client teaching requires a broad education and should not be delegated to UAP. Monitoring for signs and symptoms of fluid retention is part of client assessment, which requires a higher level of education and clinical judgment. A client is referred to a home health agency after a transsphenoidal hypophysectomy. Which action does the RN case manager delegate to the home health aide who will see the client daily? A. Document symptoms of incisional infection or meningitis. B. Give over-the-counter laxatives if the client is constipated. C. Set up medications as prescribed for the day. D. Test any nasal drainage for the presence of glucose. D. Cerebrospinal fluid (CSF) will test positive using a glucose "dipstick." Nasal drainage that is positive for glucose after a transsphenoidal hypophysectomy would indicate a CSF leak that would require immediate notification of the health care provider. Home health aides can be taught the correct technique to perform this procedure. Assessing for symptoms of infection and documenting them in the record, medication administration, and setting up medication are not within the scope of practice of the home health aide. A client with a possible adrenal gland tumor is admitted for testing and treatment. Which nursing action is most appropriate for the charge nurse to delegate to the nursing assistant? A. Assess skin turgor and mucous membranes for hydration status. B. Discuss the dietary restrictions needed for 24-hour urine testing. C. Plan ways to control the environment that will avoid stimulating the client. D. Remind the client to avoid drinking coffee and changing position suddenly. D. Drinking caffeinated beverages and changing position suddenly are not safe for a client with a potential adrenal gland tumor because of the effects of catecholamines. Reminding the client about previous instructions is an appropriate role for a nursing assistant who may observe the client doing potentially risky activities. Client assessment, client teaching, and environment planning are higher-level skills that require the experience and responsibility of the RN, and are not within the scope of practice of the nursing assistant. A client is on a ventilator and is sedated. What care may the nurse delegate to the unlicensed assistive personnel (UAP)? a. Assess the client for sedation needs. b. Get family permission for restraints. c. Provide frequent oral care per protocol. d. Use nonverbal pain assessment tools. ANS: C c. Provide frequent oral care per protocol. The client on mechanical ventilation needs frequent oral care, which can be delegated to the UAP. The other actions fall within the scope of practice of the nurse. 32. Levophed 33. D/C teaching for MI/Bypass graph- are they understanding what your teaching? 34. TPA A client with a stroke is being evaluated for fibrinolytic therapy. What information from the client or family is most important for the nurse to obtain? a. Loss of bladder control b. Other medical conditions c. Progression of symptoms d. Time of symptom onset ANS: D The time limit for initiating fibrinolytic therapy for a stroke is 3 to 4.5 hours, so the exact time of symptom onset is the most important information for this client. The other information is not as critical. A nurse is caring for four clients in the neurologic/neurosurgical intensive care unit. Which client should the nurse assess first? a. Client who has been diagnosed with meningitis with a fever of 101° F (38.3° C) b. Client who had a transient ischemic attack and is waiting for teaching on clopidogrel (Plavix) c. Client receiving tissue plasminogen activator (t-PA) who has a change in respiratory pattern and rate d. Client who is waiting for subarachnoid bolt insertion with the consent form already signed ANS: C The client receiving t-PA has a change in neurologic status while receiving this fibrinolytic therapy. The nurse assesses this client first as he or she may have an intracerebral bleed. The client with meningitis has expected manifestations. The client waiting for discharge teaching is a lower priority. The client waiting for surgery can be assessed quickly after the nurse sees the client who is receiving t-PA, or the nurse could delegate checking on this client to another nurse. 35. CABG A client has just returned from coronary artery bypass graft surgery. For which finding does the nurse contact the surgeon? a. Temperature 98.2° F b. Chest tube drainage 175 mL last hour c. Serum potassium 3.9 mEq/L d. Incisional pain 6 on a scale of 0 to 10 b. Chest tube drainage 175 mL last hour Some bleeding is expected after surgery; however, the nurse should report chest drainage over 150 mL/hr to the surgeon. Although hypothermia is a common problem after surgery, a temperature of 98.2° F is a normal finding. Serum potassium of 3.9 mEq/L is a normal finding. Incisional pain of 6 on a scale of 0 to 10 is expected immediately after major surgery; the nurse should administer prescribed analgesics. 36. What is a Romberg sign? 37. Know something about seizures-types of seizures-tonic clonic seizure, what do they look like A nurse assesses a client with a history of epilepsy who experiences stiffening of the muscles of the arms and legs, followed by an immediate loss of consciousness and jerking of all extremities. How should the nurse document this activity? a. Atonic seizure b. Tonic-clonic seizure c. Myoclonic seizure d. Absence seizure ANS: B Seizure activity that begins with stiffening of the arms and legs, followed by loss of consciousness and jerking of all extremities, is characteristic of a tonic-clonic seizure. An atonic seizure presents as a sudden loss of muscle tone followed by postictal confusion. A myoclonic seizure presents with a brief jerking or stiffening of extremities that may occur singly or in groups. Absence seizures present with automatisms, and the client is unaware of his or her environment. 38. Dilantin After teaching a client who is diagnosed with new-onset status epilepticus and prescribed phenytoin (Dilantin), the nurse assesses the client's understanding. Which statement by the client indicates a correct understanding of the teaching? a. "To prevent complications, I will drink at least 2 liters of water daily." b. "This medication will stop me from getting an aura before a seizure." c. "I will not drive a motor vehicle while taking this medication." d. "Even when my seizures stop, I will continue to take this drug." ANS: D Discontinuing antiepileptic drugs can lead to the recurrence of seizures or status epilepticus. The client does not need to drink more water and can drive while taking this medication. The medication will not stop an aura before a seizure. A client has a brain abscess and is receiving phenytoin (Dilantin). The spouse questions the use of the drug, saying the client does not have a seizure disorder. What response by the nurse is best? a. "Increased pressure from the abscess can cause seizures." b. "Preventing febrile seizures with an abscess is important." c. "Seizures always occur in clients with brain abscesses." d. "This drug is used to sedate the client with an abscess." ANS: A Brain abscesses can lead to seizures as a complication. The nurse should explain this to the spouse. Phenytoin is not used to prevent febrile seizures. Seizures are possible but do not always occur in clients with brain abscesses. This drug is not used for sedation. 39. Spinal cord injury- big things- bowl and bladder issues A nurse assesses a client with a spinal cord injury at level T5. The client's blood pressure is 184/95 mm Hg, and the client presents with a flushed face and blurred vision. Which action should the nurse take first? a. Initiate oxygen via a nasal cannula. b. Place the client in a supine position. c. Palpate the bladder for distention. d. Administer a prescribed beta blocker ANS: C The client is manifesting symptoms of autonomic dysreflexia. Common causes include bladder distention, tight clothing, increased room temperature, and fecal impaction. If persistent, the client could experience neurologic injury. Precipitating conditions should be eliminated and the physician notified. The other actions would not be appropriate. 40. Guillen Bar syndrome-what would be the priority (Airway) A client is admitted with Guillain-Barré syndrome (GBS). What assessment takes priority? a. Bladder control b. Cognitive perception c. Respiratory system d. Sensory functions ANS: C Clients with GBS have muscle weakness, possibly to the point of paralysis. If respiratory muscles are paralyzed, the client may need mechanical ventilation, so the respiratory system is the priority. The nurse will complete urinary, cognitive, and sensory assessments as part of a thorough evaluation. A client with Guillain-Barré syndrome is admitted to the hospital. The nurse plans caregiving priority to interventions that address which priority client problem? a. Anxiety b. Low fluid volume c. Inadequate airway d. Potential for skin breakdown ANS: C Airway takes priority. Anxiety is probably present, but a physical diagnosis takes priority over a psychosocial one. The client has no reason to have low fluid volume unless he or she has been unable to drink for some time. If present, airway problems take priority over a circulation problem. An actual problem takes precedence over a risk for a problem. 41. If a person is going to a procedure what do you need to make sure is there? Consent! A client is being prepared for a mechanical embolectomy. What action by the nurse takes priority? a. Assess for contraindications to fibrinolytics. b. Ensure that informed consent is on the chart. c. Perform a full neurologic assessment. d. Review the client's medication lists. ANS: B For this invasive procedure, the client needs to give informed consent. The nurse ensures that this is on the chart prior to the procedure beginning. Fibrinolytics are not used. A neurologic assessment and medication review are important, but the consent is the priority. 42. TBI? What is it-when would you call rapid response? Some kind of acute change A client has a traumatic brain injury. The nurse assesses the following: pulse change from 82 to 60 beats/min, pulse pressure increase from 26 to 40 mm Hg, and respiratory irregularities. What action by the nurse takes priority? a. Call the provider or Rapid Response Team. b. Increase the rate of the IV fluid administration. c. Notify respiratory therapy for a breathing treatment. d. Prepare to give IV pain medication. ANS: A These manifestations indicate Cushing's syndrome, a potentially life-threatening increase in intracranial pressure (ICP), which is an emergency. Immediate medical attention is necessary, so the nurse notifies the provider or the Rapid Response Team. Increasing fluids would increase the ICP. The client does not need a breathing treatment or pain medication. 43. Cirrhosis-Diet 44. Hepatic portal system Encelopathy-know diet 45. Hepatits A B and C 46. PCA pump-training you would use A nurse cares for a client who is prescribed patient-controlled analgesia (PCA) after a cholecystectomy. The client states, "When I wake up I am in pain." Which action should the nurse take? a. Administer intravenous morphine while the client sleeps. b. Encourage the client to use the PCA pump upon awakening. c. Contact the provider and request a different analgesic. d. Ask a family member to initiate the PCA pump for the client ANS: B The nurse should encourage the client to use the PCA pump prior to napping and upon awakening. Administering additional intravenous morphine while the client sleeps places the client at risk for respiratory depression. The nurse should also evaluate dosages received compared with dosages requested and contact the provider if the dose or frequency is not adequate. Only the client should push the pain button on a PCA pump. 47. Chronic pancreatitis-Whipple A nurse assesses a client who is recovering from an open Whipple procedure. Which action should the nurse perform first? a. Assess the client's endotracheal tube with 40% FiO2. b. Insert an indwelling Foley catheter to gravity drainage. c. Place the client's nasogastric tube to low intermittent suction. d. Start lactated Ringer's solution through an intravenous catheter. ANS: A Using the ABCs, airway and oxygenation status should always be assessed first, so checking the endotracheal tube is the first action. Next, the nurse should start the IV line (circulation). After that, the Foley catheter can be inserted and the nasogastric tube can be set. A nurse assesses a client who is recovering from a Whipple procedure. Which assessment finding alerts the nurse to urgently contact the health care provider? a. Drainage from a fistula b. Absent bowel sounds c. Pain at the incision site d. Nasogastric (NG) tube drainage ANS: A Complications of a Whipple procedure include secretions that drain from a fistula and peritonitis. Absent bowel sounds, pain at the incision site, and NG tube drainage are normal postoperative findings. A nurse cares for a client who is recovering from an open Whipple procedure. Which action should the nurse take? a. Clamp the nasogastric tube. b. Place the client in semi-Fowler's position. c. Assess vital signs once every shift. d. Provide oral rehydration. Postoperative care for a client recovering from an open Whipple procedure should include placing the client in a semi-Fowler's position to reduce tension on the suture line and anastomosis sites, setting the nasogastric tube to low suction to remove free air buildup and pressure, assessing vital signs frequently to assess fluid and electrolyte complications, and providing intravenous fluids. 48. What does the nurse do for nucal rigidity 49. Cushings A client with Cushing's disease says that she has lost 1 pound. What does the nurse do next? A. Auscultates the lungs for crackles B. Checks urine for specific gravity C. Forces fluids D. Weighs the client D. Fluid retention with weight gain is more of a problem than weight loss in clients with Cushing's disease. Weighing the client with Cushing's disease is part of the nurse's assessment. Crackles in the lungs indicate possible fluid retention, which would cause weight gain, not weight loss. Urine specific gravity will help assess hydration status, but this would not be the next step in the client's assessment. Forcing fluids is not appropriate because usually excess water and sodium reabsorption cause fluid retention in the client with Cushing's disease. A client with Cushing's disease begins to laugh loudly and inappropriately, causing the family in the room to be uncomfortable. What is the nurse's best response? A. "Don't mind this. The disease is causing this." B. "I need to check the client's cortisol level." C. "The disease can sometimes affect emotional responses." D. "Medication is available to help with this." C. The client may have neurotic or psychotic behavior as a result of high blood cortisol levels. Being honest with the family helps them to understand what is happening. Telling the family not to mind the laughter and that the disease is causing it is vague and minimizes the family's concern. This is the perfect opportunity for the nurse to educate the family about the disease. Cushing's disease is the hypersecretion of cortisol, which is abnormally elevated in this disease and, because the diagnosis has already been made, blood levels do not need to be redrawn. Telling the family that medication is available to help with inappropriate laughing does not assist them in understanding the cause of or the reason for the client's behavior. 50. What is adrenal hyperfunction? What might manifest in your patient (going crazy) 51. Hypothyroidism 52. Hyperthyroidism 53. Hashimotos A nurse cares for a client who has hypothyroidism as a result of Hashimoto's thyroiditis. The client asks, "How long will I need to take this thyroid medication?" How should the nurse respond? a. "You will need to take the thyroid medication until the goiter is completely gone." b. "Thyroiditis is cured with antibiotics. Then you won't need thyroid medication." c. "You'll need thyroid pills for life because your thyroid won't start working again." d. "When blood tests indicate normal thyroid function, you can stop the medication." c. Hashimoto's thyroiditis results in a permanent loss of thyroid function. The client will need lifelong thyroid replacement therapy. The client will not be able to stop taking the medication. 54. Parathyroidectomy-calcium is big lab! A nurse cares for a client who is recovering from a parathyroidectomy. When taking the client's blood pressure, the nurse notes that the client's hand has gone into flexion contractions. Which laboratory result does the nurse correlate with this condition? a. Serum potassium: 2.9 mEq/L b. Serum magnesium: 1.7 mEq/L c. Serum sodium: 122 mEq/L d. Serum calcium: 6.9 mg/dL D. Hypocalcemia destabilizes excitable membranes and can lead to muscle twitches, spasms, and tetany. This effect of hypocalcemia is enhanced in the presence of tissue hypoxia. The flexion contractions (Trousseau's sign) that occur during blood pressure measurement are indicative of hypocalcemia, not the other electrolyte imbalances, which include hypokalemia, hyponatremia, and hypomagnesemia. 55. Comfort measures for graves disease A nurse cares for a client newly diagnosed with Graves' disease. The client's mother asks, "I have diabetes mellitus. Am I responsible for my daughter's disease?" How should the nurse respond? a. "The fact that you have diabetes did not cause your daughter to have Graves' disease. No connection is known between Graves' disease and diabetes." b. "An association has been noted between Graves' disease and diabetes, but the fact that you have diabetes did not cause your daughter to have Graves' disease." c. "Graves' disease is associated with autoimmune diseases such as rheumatoid arthritis, but not with a disease such as diabetes mellitus." d. "Unfortunately, Graves' disease is associated with diabetes, and your diabetes could have led to your daughter having Graves' disease." B. An association between autoimmune diseases such as rheumatoid arthritis and diabetes mellitus has been noted. The predisposition is probably polygenic, and the mother's diabetes did not cause her daughter's Graves' disease. The other statements are inaccurate. While assessing a client with Graves' disease, the nurse notes that the client's temperature has risen 1° F. Which action should the nurse take first? a. Turn the lights down and shut the client's door. b. Call for an immediate electrocardiogram (ECG). c. Calculate the client's apical-radial pulse deficit. d. Administer a dose of acetaminophen (Tylenol). A. A temperature increase of 1° F may indicate the development of thyroid storm, and the provider needs to be notified. But before notifying the provider, the nurse should take measures to reduce environmental stimuli that increase the risk of cardiac complications. The nurse can then call for an ECG. The apical-radial pulse deficit would not be necessary, and Tylenol is not needed because the temperature increase is due to thyroid activity. 56. How would you explain to somebody why you have to worry about their blood glucose in diabetes? A nurse is teaching a client with diabetes mellitus who asks, "Why is it necessary to maintain my blood glucose levels no lower than about 60 mg/dL?" How should the nurse respond? a. "Glucose is the only fuel used by the body to produce the energy that it needs." b. "Your brain needs a constant supply of glucose because it cannot store it." c. "Without a minimum level of glucose, your body does not make red blood cells." d. "Glucose in the blood prevents the formation of lactic acid and prevents acidosis." ANS: B Because the brain cannot synthesize or store significant amounts of glucose, a continuous supply from the body's circulation is needed to meet the fuel demands of the central nervous system. The nurse would want to educate the client to prevent hypoglycemia. The body can use other sources of fuel, including fat and protein, and glucose is not involved in the production of red blood cells. Glucose in the blood will encourage glucose metabolism but is not directly responsible for lactic acid formation. 57. Assessment for diabetes A nurse assesses a client who has a 15-year history of diabetes and notes decreased tactile sensation in both feet. Which action should the nurse take first? a. Document the finding in the client's chart. b. Assess tactile sensation in the client's hands. c. Examine the client's feet for signs of injury. d. Notify the health care provider. ANS: C Diabetic neuropathy is common when the disease is of long duration. The client is at great risk for injury in any area with decreased sensation because he or she is less able to feel injurious events. Feet are common locations for neuropathy and injury, so the nurse should inspect them for any signs of injury. After assessment, the nurse should document findings in the client's chart. Testing sensory perception in the hands may or may not be needed. The health care provider can be notified after assessment and documentation have been completed. A nurse assesses clients who are at risk for diabetes mellitus. Which client is at greatest risk? a. A 29-year-old Caucasian b. A 32-year-old African-American c. A 44-year-old Asian d. A 48-year-old American Indian Diabetes is a particular problem among African Americans, Hispanics, and American Indians. The incidence of diabetes increases in all races and ethnic groups with age. Being both an American Indian and middle-aged places this client at highest risk. A nurse assesses a client with diabetes mellitus and notes the client only responds to a sternal rub by moaning, has capillary blood glucose of 33 g/dL, and has an intravenous line that is infiltrated with 0.45% normal saline. Which action should the nurse take first? a. Administer 1 mg of intramuscular glucagon. b. Encourage the client to drink orange juice. c. Insert a new intravenous access line. d. Administer 25 mL dextrose 50% (D50) IV push. ANS: A The client's blood glucose level is dangerously low. The nurse needs to administer glucagon IM immediately to increase the client's blood glucose level. The nurse should insert a new IV after administering the glucagon and can use the new IV site for future doses of D50 if the client's blood glucose level does not rise. Once the client is awake, orange juice may be administered orally along with a form of protein such as a peanut butter. A nurse assesses a client who has diabetes mellitus and notes the client is awake and alert, but shaky, diaphoretic, and weak. Five minutes after administering a half-cup of orange juice, the client's clinical manifestations have not changed. Which action should the nurse take next? a. Administer another half-cup of orange juice. b. Administer a half-ampule of dextrose 50% intravenously. c. Administer 10 units of regular insulin subcutaneously. d. Administer 1 mg of glucagon intramuscularly. ANS: A This client is experiencing mild hypoglycemia. For mild hypoglycemic manifestations, the nurse should administer oral glucose in the form of orange juice. If the symptoms do not resolve immediately, the treatment should be repeated. The client does not need intravenous dextrose, insulin, or glucagon. A nurse assesses a client with diabetes mellitus who self-administers subcutaneous insulin. The nurse notes a spongy, swelling area at the site the client uses most frequently for insulin injection. Which action should the nurse take? a. Apply ice to the site to reduce inflammation. b. Consult the provider for a new administration route. c. Assess the client for other signs of cellulitis. d. Instruct the client to rotate sites for insulin injection. ANS: D The client's tissue has been damaged from continuous use of the same site. The client should be educated to rotate sites. The damaged tissue is not caused by cellulitis or any type infection, and applying ice may cause more damage to the tissue. Insulin can only be administered subcutaneously and intravenously. It would not be appropriate or practical to change the administration route. After teaching a client who is newly diagnosed with type 2 diabetes mellitus, the nurse assesses the client's understanding. Which statement made by the client indicates a need for additional teaching? a. "I should increase my intake of vegetables with higher amounts of dietary fiber." b. "My intake of saturated fats should be no more than 10% of my total calorie intake." c. "I should decrease my intake of protein and eliminate carbohydrates from my diet." d. "My intake of water is not restricted by my treatment plan or medication regimen." ANS: C The client should not completely eliminate carbohydrates from the diet, and should reduce protein if microalbuminuria is present. The client should increase dietary intake of complex carbohydrates, including vegetables, and decrease intake of fat. Water does not need to be restricted unless kidney failure is present. 58. Know difference between DM 1+2 59. 20 questions on DM 1+2 After teaching a young adult client who is newly diagnosed with type 1 diabetes mellitus, the nurse assesses the client's understanding. Which statement made by the client indicates a correct understanding of the need for eye examinations? a. "At my age, I should continue seeing the ophthalmologist as I usually do." b. "I will see the eye doctor when I have a vision problem and yearly after age 40." c. "My vision will change quickly. I should see the ophthalmologist twice a year." d. "Diabetes can cause blindness, so I should see the ophthalmologist yearly." ANS: D Diabetic retinopathy is a leading cause of blindness in North America. All clients with diabetes, regardless of age, should be examined by an ophthalmologist (rather than an optometrist or optician) at diagnosis and at least yearly thereafter. A nurse cares for a client who has a family history of diabetes mellitus. The client states, "My father has type 1 diabetes mellitus. Will I develop this disease as well?" How should the nurse respond? a. "Your risk of diabetes is higher than the general population, but it may not occur." b. "No genetic risk is associated with the development of type 1 diabetes mellitus." c. "The risk for becoming a diabetic is 50% because of how it is inherited." d. "Female children do not inherit diabetes mellitus, but male children will." ANS: A Risk for type 1 diabetes is determined by inheritance of genes coding for HLA-DR and HLA-DQ tissue types. Clients who have one parent with type 1 diabetes are at increased risk for its development. Diabetes (type 1) seems to require interaction between inherited risk and environmental factors, so not everyone with these genes develops diabetes. The other statements are not accurate. A nurse teaches a client who is diagnosed with diabetes mellitus. Which statement should the nurse include in this client's plan of care to delay the onset of microvascular and macrovascular complications? a. "Maintain tight glycemic control and prevent hyperglycemia." b. "Restrict your fluid intake to no more than 2 liters a day." c. "Prevent hypoglycemia by eating a bedtime snack." d. "Limit your intake of protein to prevent ketoacidosis." ANS: A Hyperglycemia is a critical factor in the pathogenesis of long-term diabetic complications. Maintaining tight glycemic control will help delay the onset of complications. Restricting fluid intake is not part of the treatment plan for clients with diabetes. Preventing hypoglycemia and ketosis, although important, are not as important as maintaining daily glycemic control. A nurse teaches a client about self-monitoring of blood glucose levels. Which statement should the nurse include in this client's teaching to prevent bloodborne infections? a. "Wash your hands after completing each test." b. "Do not share your monitoring equipment." c. "Blot excess blood from the strip with a cotton ball." d. "Use gloves when monitoring your blood glucose." ANS: B Small particles of blood can adhere to the monitoring device, and infection can be transported from one user to another. Hepatitis B in particular can survive in a dried state for about a week. The client should be taught to avoid sharing any equipment, including the lancet holder. The client should be taught to wash his or her hands before testing. The client would not need to blot excess blood away from the strip or wear gloves. After teaching a client who has diabetes mellitus and proliferative retinopathy, nephropathy, and peripheral neuropathy, the nurse assesses the client's understanding. Which statement made by the client indicates a correct understanding of the teaching? a. "I have so many complications; exercising is not recommended." b. "I will exercise more frequently because I have so many complications." c. "I used to run for exercise; I will start training for a marathon." d. "I should look into swimming or water aerobics to get my exercise." ANS: D Exercise is not contraindicated for this client, although modifications based on existing pathology are necessary to prevent further injury. Swimming or water aerobics will give the client exercise without the worry of having the correct shoes or developing a foot injury. The client should not exercise too vigorously. A nurse cares for a client who has type 1 diabetes mellitus. The client asks, "Is it okay for me to have an occasional glass of wine?" How should the nurse respond? a. "Drinking any wine or alcohol will increase your insulin requirements." b. "Because of poor kidney function, people with diabetes should avoid alcohol." c. "You should not drink alcohol because it will make you hungry and overeat." d. "One glass of wine is okay with a meal and is counted as two fat exchanges." ANS: D Under normal circumstances, blood glucose levels will not be affected by moderate use of alcohol when diabetes is well controlled. Because alcohol can induce hypoglycemia, it should be ingested with or shortly after a meal. One alcoholic beverage is substituted for two fat exchanges when caloric intake is calculated. Kidney function is not impacted by alcohol intake. Alcohol is not associated with increased hunger or overeating. A nurse teaches a client with type 1 diabetes mellitus. Which statement should the nurse include in this client's teaching to decrease the client's insulin needs? a. "Limit your fluid intake to 2 liters a day." b. "Animal organ meat is high in insulin." c. "Limit your carbohydrate intake to 80 grams a day." d. "Walk at a moderate pace for 1 mile daily." ANS: D Moderate exercise such as walking helps regulate blood glucose levels on a daily basis and results in lowered insulin requirements for clients with type 1 diabetes mellitus. Restricting fluids and eating organ meats will not reduce insulin needs. People with diabetes need at least 130 grams of carbohydrates each day. A nurse assesses a client with diabetes mellitus. Which clinical manifestation should alert the nurse to decreased kidney function in this client? a. Urine specific gravity of 1.033 b. Presence of protein in the urine c. Elevated capillary blood glucose level d. Presence of ketone bodies in the urine ANS: B Renal dysfunction often occurs in the client with diabetes. Proteinuria is a result of renal dysfunction. Specific gravity is elevated with dehydration. Elevated capillary blood glucose levels and ketones in the urine are consistent with diabetes mellitus but are not specific to renal function. A nurse reviews the laboratory results of a client who is receiving intravenous insulin. Which should alert the nurse to intervene immediately? a. Serum chloride level of 98 mmol/L b. Serum calcium level of 8.8 mg/dL c. Serum sodium level of 132 mmol/L d. Serum potassium level of 2.5 mmol/L ANS: D Insulin activates the sodium-potassium ATPase pump, increasing the movement of potassium from the extracellular fluid into the intracellular fluid, resulting in hypokalemia. In hyperglycemia, hypokalemia can also result from excessive urine loss of potassium. The chloride level is normal. The calcium and sodium levels are slightly low, but this would not be related to hyperglycemia and insulin administration. A nurse assesses a client who is being treated for hyperglycemic-hyperosmolar state (HHS). Which clinical manifestation indicates to the nurse that the therapy needs to be adjusted? a. Serum potassium level has increased. b. Blood osmolarity has decreased. c. Glasgow Coma Scale score is unchanged. d. Urine remains negative for ketone bodies. ANS: C A slow but steady improvement in central nervous system functioning is the best indicator of therapy effectiveness for HHS. Lack of improvement in the level of consciousness may indicate inadequate rates of fluid replacement. The Glasgow Coma Scale assesses the client's state of consciousness against criteria of a scale including best eye, verbal, and motor responses. An increase in serum potassium, decreased blood osmolality, and urine negative for ketone bodies do not indicate adequacy of treatment. After teaching a client with type 2 diabetes mellitus, the nurse assesses the client's understanding. Which statement made by the client indicates a need for additional teaching? a. "I need to have an annual appointment even if my glucose levels are in good control." b. "Since my diabetes is controlled with diet and exercise, I must be seen only if I am sick." c. "I can still develop complications even though I do not have to take insulin at this time." d. "If I have surgery or get very ill, I may have to receive insulin injections for a short time." ANS: B Clients with diabetes need to be seen at least annually to monitor for long-term complications, including visual changes, microalbuminuria, and lipid analysis. The client may develop complications and may need insulin in the future. When teaching a client recently diagnosed with type 1 diabetes mellitus, the client states, "I will never be able to stick myself with a needle." How should the nurse respond? a. "I can give your injections to you while you are here in the hospital." b. "Everyone gets used to giving themselves injections. It really does not hurt." c. "Your disease will not be managed properly if you refuse to administer the shots." d. "Tell me what it is about the injections that are concerning you."` ANS: D Devote as much teaching time as possible to insulin injection and blood glucose monitoring. Clients with newly diagnosed diabetes are often fearful of giving themselves injections. If the client is worried about giving the injections, it is best to try to find out what specifically is causing the concern, so it can be addressed. Giving the injections for the client does not promote self-care ability. Telling the client that others give themselves injections may cause the client to feel bad. Stating that you don't know another way to manage the disease is dismissive of the client's concerns. 60. When you should medicate them A nurse reviews laboratory results for a client with diabetes mellitus who presents with polyuria, lethargy, and a blood glucose of 560 mg/dL. Which laboratory result should the nurse correlate with the client's polyuria? a. Serum sodium: 163 mEq/L b. Serum creatinine: 1.6 mg/dL c. Presence of urine ketone bodies d. Serum osmolarity: 375 mOsm/kg ANS: D Hyperglycemia causes hyperosmolarity of extracellular fluid. This leads to polyuria from an osmotic diuresis. The client's serum osmolarity is high. The client's sodium would be expected to be high owing to dehydration. Serum creatinine and urine ketone bodies are not related to the polyuria. A nurse teaches a client with type 2 diabetes mellitus who is prescribed glipizide (Glucotrol). Which statement should the nurse include in this client's teaching? a. "Change positions slowly when you get out of bed." b. "Avoid taking nonsteroidal anti-inflammatory drugs (NSAIDs)." c. "If you miss a dose of this drug, you can double the next dose." d. "Discontinue the medication if you develop a urinary infection." ANS: B NSAIDs potentiate the hypoglycemic effects of sulfonylurea agents. Glipizide is a sulfonylurea. The other statements are not applicable to glipizide. A nurse cares for a client who is prescribed pioglitazone (Actos). After 6 months of therapy, the client reports that his urine has become darker since starting the medication. Which action should the nurse take? a. Assess for pain or burning with urination. b. Review the client's liver function study results. c. Instruct the client to increase water intake. d. Test a sample of urine for occult blood. ANS: B Thiazolidinediones (including pioglitazone) can affect liver function; liver function should be assessed at the start of therapy and at regular intervals while the client continues to take these drugs. Dark urine is one indicator of liver impairment because bilirubin is increased in the blood and is excreted in the urine. The nurse should check the client's most recent liver function studies. The nurse does not need to assess for pain or burning with urination and does not need to check the urine for occult blood. The client does not need to be told to increase water intake. A nurse cares for a client with diabetes mellitus who is visually impaired. The client asks, "Can I ask my niece to prefill my syringes and then store them for later use when I need them?" How should the nurse respond? a. "Yes. Prefilled syringes can be stored for 3 weeks in the refrigerator in a vertical position with the needle pointing up." b. "Yes. Syringes can be filled with insulin and stored for a month in a location that is protected from light." c. "Insulin reacts with plastic, so prefilled syringes are okay, but you will need to use glass syringes." d. "No. Insulin syringes cannot be prefilled and stored for any length of time outside of the container." ANS: A Insulin is relatively stable when stored in a cool, dry place away from light. When refrigerated, prefilled plastic syringes are stable for up to 3 weeks. They should be stored in the refrigerator in the vertical position with the needle pointing up to prevent suspended insulin particles from clogging the needle. 61. Ketoacidosis-kussmauls breathing-deep shallow rapid An emergency department nurse assesses a client with ketoacidosis. Which clinical manifestation should the nurse correlate with this condition? a. Increased rate and depth of respiration b. Extremity tremors followed by seizure activity c. Oral temperature of 102° F (38.9° C) d. Severe orthostatic hypotension ANS: A Ketoacidosis decreases the pH of the blood, stimulating the respiratory control areas of the brain to buffer the effects of increasing acidosis. The rate and depth of respiration are increased (Kussmaul respirations) in an attempt to excrete more acids by exhalation. Tremors, elevated temperature, and orthostatic hypotension are not associated with ketoacidosis. A nurse cares for a client experiencing diabetic ketoacidosis who presents with Kussmaul respirations. Which action should the nurse take? a. Administration of oxygen via face mask b. Intravenous administration of 10% glucose c. Implementation of seizure precautions d. Administration of intravenous insulin ANS: D The rapid, deep respiratory efforts of Kussmaul respirations are the body's attempt to reduce the acids produced by using fat rather than glucose for fuel. Only the administration of insulin will reduce this type of respiration by assisting glucose to move into cells and to be used for fuel instead of fat. The client who is in ketoacidosis may not experience any respiratory impairment and therefore does not need additional oxygen. Giving the client glucose would be contraindicated. The client does not require seizure precautions. 62. ABG what to expect for DKA-Respiratory alkalosis A nurse assesses a client who has diabetes mellitus. Which arterial blood gas values should the nurse identify as potential ketoacidosis in this client? a. pH 7.38, HCO3- 22 mEq/L, PCO2 38 mm Hg, PO2 98 mm Hg b. pH 7.28, HCO3- 18 mEq/L, PCO2 28 mm Hg, PO2 98 mm Hg c. pH 7.48, HCO3- 28 mEq/L, PCO2 38 mm Hg, PO2 98 mm Hg d. pH 7.32, HCO3- 22 mEq/L, PCO2 58 mm Hg, PO2 88 mm Hg ANS: B When the lungs can no longer offset acidosis, the pH decreases to below normal. A client who has diabetic ketoacidosis would present with arterial blood gas values that show primary metabolic acidosis with decreased bicarbonate levels and a compensatory respiratory alkalosis with decreased carbon dioxide levels. 63. Cymbalta and DM A nurse reviews the medication list of a client with a 20-year history of diabetes mellitus. The client holds up the bottle of prescribed duloxetine (Cymbalta) and states, "My cousin has depression and is taking this drug. Do you think I'm depressed?" How should the nurse respond? a. "Many people with long-term diabetes become depressed after a while." b. "It's for peripheral neuropathy. Do you have burning pain in your feet or hands?" c. "This antidepressant also has anti-inflammatory properties for diabetic pain." d. "No. Many medications can be used for several different disorders." ANS: B Damage along nerves causes peripheral neuropathy and leads to burning pain along the nerves. Many drugs, including duloxetine (Cymbalta), can be used to treat peripheral neuropathy. The nurse should assess the client for this condition and then should provide an explanation of why this drug is being used. This medication, although it is used for depression, is not being used for that reason in this case. Duloxetine does not have anti-inflammatory properties. Telling the client that many medications are used for different disorders does not provide the client with enough information to be useful. 64. Regular and NPH onsets A nurse cares for a client who has diabetes mellitus. The nurse administers 6 units of regular insulin and 10 units of NPH insulin at 0700. At which time should the nurse assess the client for potential problems related to the NPH insulin? a. 0800 b. 1600 c. 2000 d. 2300 ANS: B Neutral protamine Hagedorn (NPH) is an intermediate-acting insulin with an onset of 1.5 hours, peak of 4 to 12 hours, and duration of action of 22 hours. Checking the client at 0800 would be too soon. Checking the client at 2000 and 2300 would be too late. The nurse should check the client at 1600. A nurse prepares to administer insulin to a client at 1800. The client's medication administration record contains the following information: • Insulin glargine: 12 units daily at 1800 • Regular insulin: 6 units QID at 0600, 1200, 1800, 2400 Based on the client's medication administration record, which action should the nurse take? a. Draw up and inject the insulin glargine first, and then draw up and inject the regular insulin. b. Draw up and inject the insulin glargine first, wait 20 minutes, and then draw up and inject the regular insulin. c. First draw up the dose of regular insulin, then draw up the dose of insulin glargine in the same syringe, mix, and inject the two insulins together. d. First draw up the dose of insulin glargine, then draw up the dose of regular insulin in the same syringe, mix, and inject the two insulins together. ANS: A Insulin glargine must not be diluted or mixed with any other insulin or solution. Mixing results in an unpredictable alteration in the onset of action and time to peak action. The correct instruction is to draw up and inject first the glargine and then the regular insulin right afterward. A nurse prepares to administer prescribed regular and NPH insulin. Place the nurse's actions in the correct order to administer these medications. 1. Inspect bottles for expiration dates. 2. Gently roll the bottle of NPH between the hands. 3. Wash your hands. 4. Inject air into the regular insulin. 5. Withdraw the NPH insulin. 6. Withdraw the regular insulin. 7. Inject air into the NPH bottle. 8. Clean rubber stoppers with an alcohol swab. ANS: 3, 1, 2, 8, 7, 4, 6, 5 After washing hands, it is important to inspect the bottles and then to roll the NPH to mix the insulin. Rubber stoppers should be cleaned with alcohol after rolling the NPH and before sticking a needle into either bottle. It is important to inject air into the NPH bottle before placing the needle in a regular insulin bottle to avoid mixing of regular and NPH insulin. The shorter-acting insulin is always drawn up first. 65. Know how metformin reacts with CT scans and IV contrast-Kidney function-hold for 48 hours A nurse reviews the medication list of a client recovering from a computed tomography (CT) scan with IV contrast to rule out small bowel obstruction. Which medication should alert the nurse to contact the provider and withhold the prescribed dose? a. Pioglitazone (Actos) b. Glimepiride (Amaryl) c. Glipizide (Glucotrol) d. Metformin (Glucophage) ANS: D Glucophage should not be administered when the kidneys are attempting to excrete IV contrast from the body. This combination would place the client at high risk for kidney failure. The nurse should hold the metformin dose and contact the provider. The other medications are safe to administer after receiving IV contrast. 66. Lots of insulin and ketoacidosis questions After teaching a client with type 2 diabetes mellitus who is prescribed nateglinide (Starlix), the nurse assesses the client's understanding. Which statement made by the client indicates a correct understanding of the prescribed therapy? a. "I'll take this medicine during each of my meals." b. "I must take this medicine in the morning when I wake." c. "I will take this medicine before I go to bed." d. "I will take this medicine immediately before I eat." ANS: D Nateglinide is an insulin secretagogue that is designed to increase meal-related insulin secretion. It should be taken immediately before each meal. The medication should not be taken without eating as it will decrease the client's blood glucose levels. The medication should be taken before meals instead of during meals. A nurse cares for a client with diabetes mellitus who asks, "Why do I need to administer more than one injection of insulin each day?" How should the nurse respond? a. "You need to start with multiple injections until you become more proficient at self-injection." b. "A single dose of insulin each day would not match your blood insulin levels and your food intake patterns." c. "A regimen of a single dose of insulin injected each day would require that you eat fewer carbohydrates." d. "A single dose of insulin would be too large to be absorbed, predictably putting you at risk for insulin shock." ANS: B Even when a single injection of insulin contains a combined dose of different-acting insulin types, the timing of the actions and the timing of food intake may not match well enough to prevent wide variations in blood glucose levels. One dose of insulin would not be appropriate even if the client decreased carbohydrate intake. Additional injections are not required to allow the client practice with injections, nor will one dose increase the client's risk of insulin shock. After teaching a client with diabetes mellitus to inject insulin, the nurse assesses the client's understanding. Which statement made by the client indicates a need for additional teaching? a. "The lower abdomen is the best location because it is closest to the pancreas." b. "I can reach my thigh the best, so I will use the different areas of my thighs." c. "By rotating the sites in one area, my chance of having a reaction is decreased." d. "Changing injection sites from the thigh to the arm will change absorption rates." ANS: A The abdominal site has the fastest rate of absorption because of blood vessels in the area, not because of its proximity to the pancreas. The other statements are accurate assessments of insulin administration. A nurse teaches a client who is prescribed an insulin pump. Which statement should the nurse include in this client's discharge education? a. "Test your urine daily for ketones." b. "Use only buffered insulin in your pump." c. "Store the insulin in the freezer until you need it." d. "Change the needle every 3 days." ANS: D Having the same needle remain in place through the skin for longer than 3 days drastically increases the risk for infection in or through the delivery system. Having an insulin pump does not require the client to test for ketones in the urine. Insulin should not be frozen. Insulin is not buffered. A nurse assesses a client with diabetes mellitus 3 hours after a surgical procedure and notes the client's breath has a "fruity" odor. Which action should the nurse take? a. Encourage the client to use an incentive spirometer. b. Increase the client's intravenous fluid flow rate. c. Consult the provider to test for ketoacidosis. d. Perform meticulous pulmonary hygiene care. ANS: C The stress of surgery increases the action of counterregulatory hormones and suppresses the action of insulin, predisposing the client to ketoacidosis and metabolic acidosis. One manifestation of ketoacidosis is a "fruity" odor to the breath. Documentation should occur after all assessments have been completed. Using an incentive spirometer, increasing IV fluids, and performing pulmonary hygiene will not address this client's problem. A nurse reviews laboratory results for a client with diabetes mellitus who is prescribed an intensified insulin regimen: • Fasting blood glucose: 75 mg/dL • Postprandial blood glucose: 200 mg/dL • Hemoglobin A1c level: 5.5% How should the nurse interpret these laboratory findings? a. Increased risk for developing ketoacidosis b. Good control of blood glucose c. Increased risk for developing hyperglycemia d. Signs of insulin resistance ANS: B The client is maintaining blood glucose levels within the defined ranges for goals in an intensified regimen. Because the client's glycemic control is good, he or she is not at higher risk for ketoacidosis or hyperglycemia and is not showing signs of insulin resistance. 67. Nephrostomy tube-abdominal assessment- looking for bleeding on inside-where your going to do first assessment? Always add vitals to end A nurse cares for a client who is recovering after a nephrostomy tube was placed 6 hours ago. The nurse notes drainage in the tube has decreased from 40 mL/hr to 12 mL over the last hour. Which action should the nurse take? a. Document the finding in the client's record. b. Evaluate the tube as working in the hand-off report. c. Clamp the tube in preparation for removing it. d. Assess the client's abdomen and vital signs. ANS: D The nephrostomy tube should continue to have a consistent amount of drainage. If the drainage slows or stops, it may be obstructed. The nurse must notify the provider, but first should carefully assess the client's abdomen for pain and distention and check vital signs so that this information can be reported as well. The other interventions are not appropriate. 68. Refresh on pyelonephritis A nurse cares for a middle-aged female client with diabetes mellitus who is being treated for the third episode of acute pyelonephritis in the past year. The client asks, "What can I do to help prevent these infections?" How should the nurse respond? a. "Test your urine daily for the presence of ketone bodies and proteins." b. "Use tampons rather than sanitary napkins during your menstrual period." c. "Drink more water and empty your bladder more frequently during the day." d. "Keep your hemoglobin A1c under 9% by keeping your blood sugar controlled." ANS: C Clients with long-standing diabetes mellitus are at risk for pyelonephritis for many reasons. Chronically elevated blood glucose levels spill glucose into the urine, changing the pH and providing a favorable climate for bacterial growth. The neuropathy associated with diabetes reduces bladder tone and reduces the client's sensation of bladder fullness. Thus, even with large amounts of urine, the client voids less frequently, allowing stasis and overgrowth of microorganisms. Increasing fluid intake (specifically water) and voiding frequently prevent stasis and bacterial overgrowth. Testing urine and using tampons will not help prevent pyelonephritis. A hemoglobin A1c of 9% is too high. A nurse cares for a client who has pyelonephritis. The client states, "I am embarrassed to talk about my symptoms." How should the nurse respond? a. "I am a professional. Your symptoms will be kept in confidence." b. "I understand. Elimination is a private topic and shouldn't be discussed." c. "Take your time. It is okay to use words that are familiar to you." d. "You seem anxious. Would you like a nurse of the same gender to care for you?" ANS: C Clients may be uncomfortable discussing issues related to elimination and the genitourinary area. The nurse should encourage the client to use language that is familiar to the client. The nurse should not make promises that cannot be kept, like keeping the client's symptoms confidential. The nurse must assess the client and cannot take the time to stop the discussion or find another nurse to complete the assessment. 69. What do you see in a patient who has been doing exercise out in sun- elevated HR and temp, if they’re walking and talking to me what would I do- slowly drink water A marathon runner comes into the clinic and states "I have not urinated very much in the last few days." The nurse notes a heart rate of 110 beats/min and a blood pressure of 86/58 mm Hg. Which action by the nurse is the priority? a. Give the client a bottle of water immediately. b. Start an intravenous line for fluids. c. Teach the client to drink 2 to 3 liters of water daily. d. Perform an electrocardiogram. ANS: A This athlete is mildly dehydrated as evidenced by the higher heart rate and lower blood pressure. The nurse can start hydrating the client with a bottle of water first, followed by teaching the client to drink 2 to 3 liters of water each day. An intravenous line may be ordered later, after the client's degree of dehydration is assessed. An electrocardiogram is not necessary at this time. 70. BUN/Creat know parameters and what its significant of A male client comes into the emergency department with a serum creatinine of 2.2 mg/dL and a blood urea nitrogen (BUN) of 24 mL/dL. What question should the nurse ask first when taking this client's history? a. "Have you been taking any aspirin, ibuprofen, or naproxen recently?" b. "Do you have anyone in your family with renal failure?" c. "Have you had a diet that is low in protein recently?" d. "Has a relative had a kidney transplant lately?" ANS: A There are some medications that are nephrotoxic, such as the nonsteroidal anti- inflammatory drugs ibuprofen, aspirin, and naproxen. This would be a good question to initially ask the client since both the serum creatinine and BUN are elevated, indicating some renal problems. A family history of renal failure and kidney transplantation would not be part of the questioning and could cause anxiety in the client. A diet high in protein could be a factor in an increased BUN. 71. Acute kidney injury-what are the main concerns A client is admitted with acute kidney injury (AKI) and a urine output of 2000 mL/day. What is the major concern of the nurse regarding this client's care? a. Edema and pain b. Electrolyte and fluid imbalance c. Cardiac and respiratory status d. Mental health status ANS: B This client may have an inflammatory cause of AKI with proteins entering the glomerulus and holding the fluid in the filtrate, causing polyuria. Electrolyte loss and fluid balance is essential. Edema and pain are not usually a problem with fluid loss. There could be changes in the client's cardiac, respiratory, and mental health status if the electrolyte imbalance is not treated. 72. What kind of access and how do you care for them for dialysis-heparin A client has just had a central line catheter placed that is specific for hemodialysis. What is the most appropriate action by the nurse? a. Use the catheter for the next laboratory blood draw. b. Monitor the central venous pressure through this line. c. Access the line for the next intravenous medication. d. Place a heparin or heparin/saline dwell after hemodialysis. ANS: D The central line should have a heparin or heparin/saline dwell after hemodialysis treatment. The central line catheter used for dialysis should not be used for blood sampling, monitoring central venous pressures, or giving drugs or fluids. 73. CKD-goals of treatment A client is diagnosed with chronic kidney disease (CKD). What is an ideal goal of treatment set by the nurse in the care plan to reduce the risk of pulmonary edema? a. Maintaining oxygen saturation of 89% b. Minimal crackles and wheezes in lung sounds c. Maintaining a balanced intake and output d. Limited shortness of breath upon exertion ANS: C With an optimal fluid balance, the client will be more able to eject blood from the left ventricle without increased pressure in the left ventricle and pulmonary vessels. Other ideal goals are oxygen saturations greater than 92%, no auscultated crackles or wheezes, and no demonstrated shortness of breath 74. Why do we need case management? Main function-resources keep them in the community and keeps them out of the hospital, and drives down costs Chapters since exam 2-31, 32 42-45, 61-64 • CBC Values o WBC= 4,500-10,000 o RBC= 4.5-5.5 o Hematocrit= 36-50 o Hemoglobin= 12-16 o Platelet= 100,000-450,000 o Neutrophils= 54-62 • BMP Values o Sodium=135-145 o Potassium=3.5-5.0 o BUN=8-21 o Creat=0.8-1.3 • Lactic Levels o 0.5-2.2 shows sepsis • Troponin Level o <0.04=normal o >0.4=probable for MI • Coag Time o PT= 11-12.5 o INR= 0.8-1.1 o PTT= 20-30 [Show More]
Last updated: 1 year ago
Preview 1 out of 84 pages
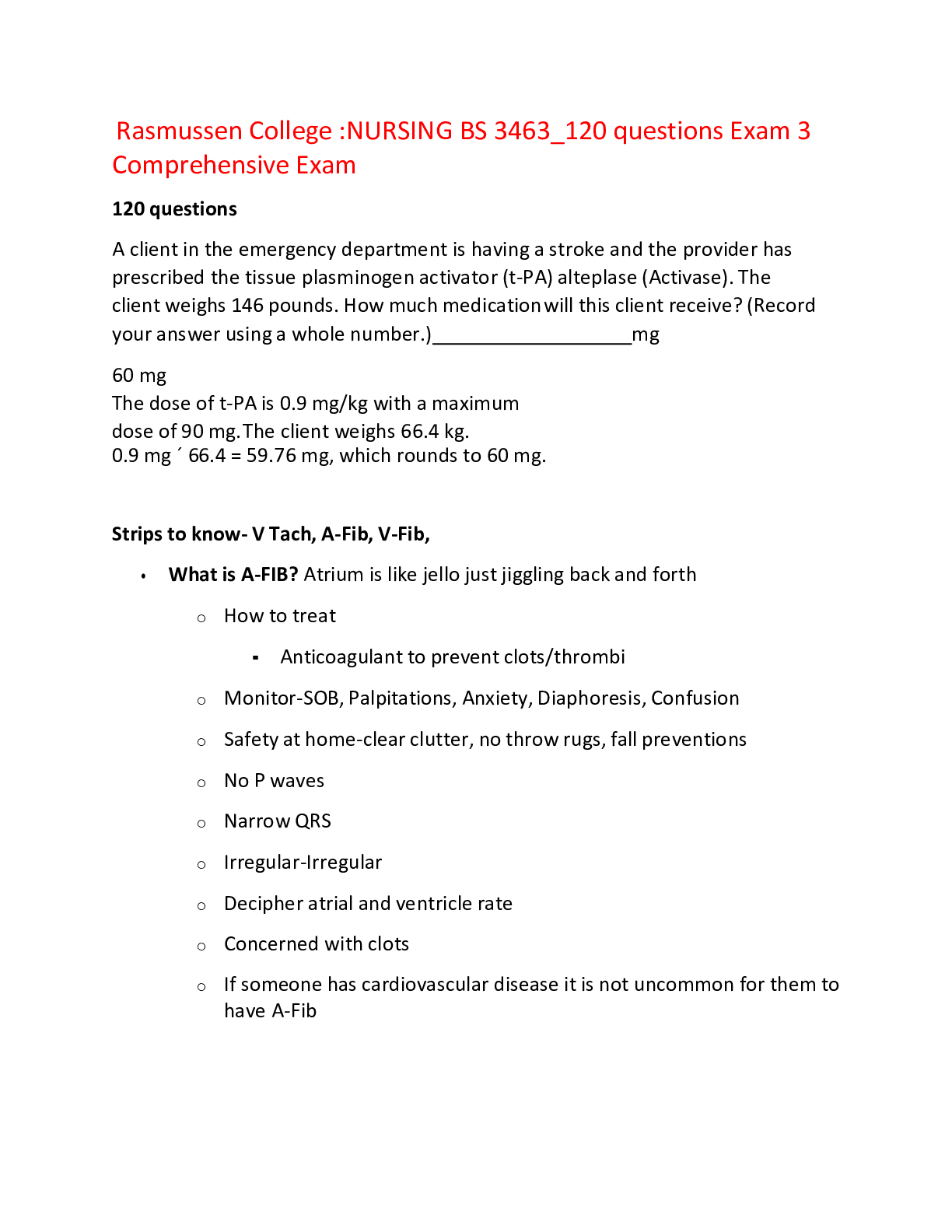
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 22, 2022
Number of pages
84
Written in
Additional information
This document has been written for:
Uploaded
Jul 22, 2022
Downloads
0
Views
40


.png)