NURS 7755 NCLEX__hurst Questions And Answers (2022/23)
Document Content and Description Below
o Calcium has an inverse relation to phosphorus When Calcium goes up, Phosphorus goes down (Hypophosphatemia) and vice versa o Sodium has an inverse relation to Potassium When sodium goes ... up, Potassium goes down and vice versa HyperParathyroidsm = HYPERCALCEMIA = HYPOPHOSPATEMIA Every time you see Hyperparathyroidism that’s the same exact thing as Hypercalcemia o Epinephrine is secreted – vasoconstrictor When Hypovolemic (blood volume deficit), ADH and aldosterone will be secreted so keep blood volume up **Weight is the best indicator for fluid status EXCEPT for Burns, Its Urine Output** Also for ventilator alarms HOLD High alarm- Obstruction due to incr. secretions, kink, pt. coughs, gag or bites Low press alarm- Disconnection or leak in ventilator or in pt. airway cuff, pt. stops spontaneous breathing To remember blood sugar: hot and dry-sugar high (hyperglycemia) cold and clammy-need some candy (hypoglycemia) Eu = Normal for example: Euthyroid is normal thyroid Increase of LDL, THINK Coronary Artery Disease Increase secretion of PTH makes serum calcium go up Decrease secretion of PTH makes serum calcium go down You dangle artery problems and you elevate vein issue problems IMPORTANT WHEN IT ASKS FOR PRIOIRTY, ASK YOURSELF YOURE GOING TO DO THAT OVER AND OVER AGAIN AND NOTHING ELSE EXAMPLE: client is hemorrhaging, do you check for vital signs or call the HCP Hypervolemia: Too much fluid in the vascular space (too much water in the hose) Will Cause: HF Weak Heart low Cardiac output Low Urine Perfusion Low Urine Output Heart Failure Renal Failure S/S: Bounding Pulse SOB; Dyspnea Crackles/ wet lung sounds (listen to the low area in the back) Distended Neck (JVD) and Peripheral Veins Peripheral Edema (sacrum area) and Third spacing Rapid Weight gain Low urine output (specific gravity of 1.010 or less) Central Venous Pressure (CVP): More volume (Hypervolemia) = More Pressure CVP normal is 2-8 Low volume (Hypovolemia) = Low Pressure Position: Semi Fowler; BED REST FOR THESE PATIENTS (hyper & Hypo) Diet: Hypertension, heart failure, CAD—low sodium, calorie-restricted, Low fat Treatment: Hydrochlorothiazide: Will make you lose Potassium Furosemide: Will make you lose Potassium Bumetanide: Will make you lose Potassium Give SPIRONOLACTONE to retain Potassium but watch for Hyperkalemia o KEEP CLIENT ON BED REST (helps reduce sodium and water) Teaching: Check Daily weights and Input and Output ***clients with History of HF and Kidney, give fluids slow and watch for Hypervolemia*** HYPOVOLEMIA: Fluid not in the vascular space SHOCK (COLD AND CLAMMY) Look for Hypovolemia in (anything that causes losing fluid): Trauma SURGERY patients NG tube Paracentesis you losing fluid Vomiting and diarrhea Ascites: fluid in the abdomen; Edema: Fluid in the wrong spot so check for Hypovolemia Polyuria: Fluid in the wrong spot so check for Hypovolemia Will Cause: Third spacing: When fluid goes somewhere else other than Other than the vascular space Ascites: fluid in the abdomen People with liver Disease will have this Edema Polyuria: When you see this, THINK Shock First ** When you go into HYPOVOLEMIC STATE (Hemorrhage, vomiting, or anything that causes you to lose water), the ALDOSTERONE hormone secretion will increase to preserve/retain sodium and water*** S/S: Increased temp Decreased skin Turgor Low mucous COLD AND CLAMMY Rapid/weak/thready pulse, High pulse (tachycardic) and Tachypnea Increased Respirations Hypotension (Orthostatic/postural mainly) Anxiety, weight loss Decreased Urine output Urine specific gravity >1.030 Low CVP pressure Vessels are vasoconstricted *Concentrated makes labs go up like hematocrit and dilute makes it go down* Position/Nursing Intervention for SHOCK: THINK DIZZINISS Bedrest with extremities elevated 20 degrees Knees straight Head slightly elevated (modified Trendelenburg) Treatment: Give Fluids Safety precautions (high risk for falls) Monitor IV fluids (weight check and I and O) TYPES OF IV FLUIDS ISOTONIC (0.9%) - *D5W - Normal Saline - Lactated Ringers - D5 ¼ NS (used for Peds) **Contraindicated: Hypertensive, Renal, and heart disease** HYPOTONIC SOLUTION (0.33%) - D2.5W - ½ NS OR 0.33 NS ***Use for: Hypertension, Heart problem, Renal Disease*** **Watch for Cellular Edema** Hypertonic Solution (TPN): - D10W, 3% NS, 5% NS - D5 LR, D1/2 NS, D5NS - **TPN (most common) - Albumin **Watch for pulmonary edema, Fluid volume excess, Hypertension** Aldosterone = Steroids aka Mineralocorticoids retains sodium and water Cushing’s Syndrome: Too much Aldosterone (steroids) Hyperaldosteronism (Conn’s Syndrome): Too much Aldosterone (steroids) S/S: HyperNa: If you are obese, you have to much sodium HypoK Hyperglycemia, Prone to infection, Muscle wasting; weakness, Edema; Obesity HTN, Hirsutism, Moon face Buffalo hump Diet: Low sodium, High potassium diet. Increase protein, Increase Calcium ***Cushing: Everything is High Except Potassium*** CLIENT NEEDS QUITE ROOM Risk for osteoporosis Protein means kidney damage Glucose and ketones are for long term use which will show in urine sample Uric acid is kidney stones ADDison disease is ABSENT of steroids. think of a bodybuilder who’s on steroids, he’s very big vs the other guy who is not taking steroids. He will be SMALL, AND WEAK AND TAN With Addison disease, they have Absent of steroids meaning LOW so everything will be LOW except 2 things LOW BP (CRITICAL) Shock LOW weight (water loss) LOW sodium (hyponatremia) LOW glucose (Hypoglycemia) LOW or slow periods (amenorrhea) LOW resistance to stress Fractures Alopecia Weight loss GI distress HIGH Potassium (hyperKalemia) HIGH pigmentation “Bronze Pigment” don’t get this confused with the Acanthosis nigricans Loss of libido and decreased axillary and pubic hair are common in Addison's disease due to lower levels of androgens. Diet: Increased sodium, low potassium diet. Addisonian Crisis: N/V Confusion Abdominal pain Extreme weakness Hypoglycemia Dehydration Decreased BP - Treatment: Meds: NEVER STOP TAKING MEDS ABRUPTLY Prednisolone: 2x a day in split days Fluicosteriods: this is Aldosterone SIADH: too much ADH potential complication of head injury Syndrome of inappropriate antidiuretic hormone (SIADH) is potential complication of head injury or Pituitary (located right through the bridge of the nose so any nose/sinus injury can also be it too) or a TRANSSPHENOIDAL HYPOPHYSCEMETY and INTERCRANIAL PRESSURE. In SIADH, the extra ADH leads to excessive water absorption by the kidneys. IF YOU HAVE ICP, ABSERVE FOR ADH PROBLEMS DO NO GIVE YOUR PATIENT FLUIDS IF THEY HAVE SIADH. KEEP THEM ON FLUID RESTRICTIONS S/S OF SIADH: Low urine output (cuz their brain is absorbing it all so no point in giving them more unless you tryna kill your patient!! HAH ROT IN JAIL) Increased urine gravity Decrease in urine osmolality (if one is increased the other one is obviously decreased Ex: high urine output so low urine osmolality) BASICALLY REMEMBER OPPOSITES ATTRACT - ALSO WILL BE HYPONATERMIA!! - Changes in LOC - Decreased deep Tendon Reflexes - Tachycardia - N/V - Side note: all these are bullshit, just know SIADH has to do with LOW URINE OUTPUT which obviously means Increase in urine gravity o The higher the urine output, the lower urine gravity o The lower the urine output, the higher urine gravity Treatment: Administer Desmopressin Diuretics Declomycin Lab work: Urine specific Gravity Sodium Hematocrit SIADH: causes include central nervous system disorders (eg, stroke, trauma, neurosurgery) and some commonly used medications (eg, desmopressin, carbamazepine Diabetes insipidus (DI): think D for dehydrated so they are Dry Inside Diabetes Insipidus R N Y S I ***WHEN YOU SEE DI, REMEMBER D FOR DIURESES*** D E High Urine Output (because they are peeing everything out, so they are dry inside) Low urine gravity which automatically means they’ll have high osmolality HyperNatremia this goes with the High Osmolality, if you have high osmolality, you’ll have high sodium and vice versa Polydipsia aka DIURESIS (since they are dry inside, they’ll be thirsty Dry mucous membranes CUZ they DRY INSIDE DUHH! HYPOTENSION REMEMBER CARDIAC, when you have a low fluid inside, you turn HYPOTENSIVE SHOCK DESMOPRESSION AKA VASOPRESSIN gets your BP up AND decreases Urine output can cause deadly headaches because it also decreases sodium ***BIGGEST COMPLICATION IS SHOCK FOR DI*** TREATMENT: Any Med with -RESSIN (desmopressin, Pitressin) Hyper Magnesium and Hyper Calcium: Think Act like Sedatives Everything goes Down!!! Magnesium: normal: 1.5-2.5 mEq/L HYPER magnesium: Excreted through Kidneys and GI - Causes of Hyper magnesium: Kidney Failure if you can’t excrete it, then it will cause this Antacids has too much magnesium S/S: (vasodilation) ----- Hyper Magnesia: will make everything go down o Depresses the CNS/ LOC o Hypotension o Facial flushing/warmth vasodilation o Muscle weakness o Absent deep tendon reflexes o Shallow/Decreased respirations o Arrhythmias o Emergency ** Sometimes Magnesium is given to Preeclampsia patients to prevent seizures because magnesium relaxes everything** Treatment: o Ventilator if O2 is >10 breathe o Dialysis: kidneys not working o Calcium Gluconate antidote o Safety precautions: HYPERCalcemia: Causes of Hypercalcemia: Too much PTH (parathyroid Hormone) Thiazides: makes you retain calcium Immobilization: If you’re immobile, calcium goes into the blood which makes PTH go up ^Intervention: client must be weight bearing and mobile S/S: (same s/s as hyper magnesium but these 2 added) o Brittle Bones o Kidney Stones Treatment: o Move o Fluids – To prevent Kidney stones o Increase Phosphorus (diet) Calcium has an inverse relation to phosphorus o Steroids: decreases calcium levels so increase in steroids o Safety precautions Meds: o Biphosphate – Adrenalin and Calcitonin Calcitonin treats osteoporosis Hypo Magnesium and Hypo Calcium: Not enough Sedatives Everything goes Down!!! HYPO magnesium: Excreted through Kidneys and GI - Causes of Hypo magnesium: Diarrhea Alcoholic – Suppresses the release of ADH so Decrease of ADH mean client will Diuresis (Urinate more) more - S/S: (not sedated so everything down) o Rigid and tight muscles o Possible seizures o Stridor/ Laryngospasm and Tetany (spasms of the hands and feet, cramps, spasm of the voice box (larynx)) o POSTIVIE CHVOSETK’S (hyper irritability) AND TROUSSEAU o Arrythmias o Increase deep tendon reflex o Mind changes (wild, see things, depression, etc) o Swallowing problems (dysphagia) - Treatment: o Give Magnesium Check kidney function before giving IV Mg Diet: High in Mg (Remember Vegetables , seeds, and peppermint) o Spinach o Greens o Squash o Broccoli o Halibut o Turnip o Pumpkin seeds o Peppermint o Cucumber o Green beans o Celery o Kale o Sunflower seeds o Sesame seeds o Flax seeds HYPOCalcemia: Causes of Hypocalcemia: Not enough Parathyroid Hormone (PTH) Hypoparathyroidism Radical Neck Thyroidectomy S/S: SAME AS HYPOMAGNESIUM o Rigid and tight muscles o Possible seizures o Stridor/ Laryngospasm and Tetany (spasms of the hands and feet, cramps, spasm of the voice box (larynx)) o POSTIVIE CHVOSETK’S (hyper irritability) AND TROUSSEAU o Arrythmias o Increase deep tendon reflex o Mind changes (wild, see things, depression, etc) o Swallowing problems (dysphagia) Treatment: o Give Calcium: Make sure client has heart monitor on when giving calcium Give IV calcium slowly b/c too fast will cause widened QRS aka Arrythmias o Vitamin D: This Utilizes the calcium for better absorption o Phosphate binders to excrete phosphate: Calcium acetate (hydrochloride) Diet: o Decrease in Phosphate foods Sodium: Think Neuro changes!!! Hypernatremia: Dehydration Causes of HyperNatremia: Think what causes Dehydration Hyperventilation: When you exhale too much, you lose water Heat stroke DI Vomiting Diarrhea S/S: o Thirsty o Dehydration o Swollen Tongue o Neuro Changes (disorientation/delusions) o Increased temp o Weakness o Hypotension o Tachycardia Treatment: Restrict Sodium IV fluids (Hypotonic Solutions) DAILY WEIGHTS AND I&O Lab work ***Clients on Tube feedings, Check Sodium levels*** HYPO Natremia: Too much water and not enough sodium Causes of HypoNatermia: Psychogenic polydipsia (drinking too much water) Too much water SIADH S/S: o Headache o Seizures o Coma o Nausea o Muscle cramps o Increased ICP; Hypertension o Muscular twitching Treatment: Not water, but give Sodium (Hypertonic Solution) 3% NS or 5% NS Potassium: Excreted by kidney HyperKalemia: Excreted by Kidney Causes of HyperKalemia: Kidney Trouble Drugs such as Spironolactone S/S: Early to Late (severe) sign -Mnemonic is (FMURDER) o Muscle Weakness and twitching o Flaccid Paralysis o Urine (oliguria/anuria) o Respiratory depression o Decreased cardiac contractility o ECG changes o Reflexes Treatment: o Dialysis: Kidneys not working o Calcium Gluconate o Glucose and insulin Watch for Hypokalemia and Hypoglycemia o Sodium Polystyrene (kayexalate) used only for clients who are hyperkalemic ONLY given as enema o Push Fluids HypoKalemia: Causes of HypoKalemia They are all losing potassium NG Suction Vomiting Diuretics Not eating S/S: Early to Severe o Muscle Cramps o Muscle Weakness o Arrhythmias Treatment: o Give potassium Spironolactone o Increase K Foods Raisins Bananas Apricots Oranges Beans Potatoes Carrots Celery Safety Issues with Potassium: o Oral Potassium causes GI upsets – Give with foods o **Assess Urinary Output before/during IV Potassium** o Always put IV Potassium on a Pump o Mix well o Never give potassium PUSH o Burns during infusion? Yes, very common Acid/ Base Solution (Listen to MARK!!) From the a** (diarrhea)= metabolic acidosis From the mouth (vomitus)=metabolic alkalosis s Burns: Safety Considerations: o Electrical sockets covered o Smoke alarm o Heating elements: Only one heating element per socket o Dryers o Practice escape plan o Pot handles o Stove attached to walls o No tablecloths if toddlers present o Watch for small appliances (iron) o Water heater <120 F* Elderly with neuropathy: use Antiscald devices with devices with showerheads and faucet fixtures S/S: They can go in SHOCK HYPOTENSION: vessels are leaking o Hypotension SHOCK o Tachycardia o Hypothermia o Low hemoglobin o Low urine Output: volume deficit so low urine output o Low kidney perfusion: kidneys aren’t working properly OR needs to hold water o Epinephrine is secreted – vasoconstrictor o ADH and aldosterone are secreted: Will make blood volume go up Rule of nine o Head = 9% o Each arm = 9% o Each Leg = 18% o Stomach = 18% o Back = 18% o Genitals = 1% BURNS o 1st Degree - Red and Painful o 2nd Degree – Blisters o 3rd Degree - No Pain because of blocked and burned nerves Diet: o high protein o high caloric, o Increase in Vitamin C Treatment: o Fluid replacement: 2 large bore IVs Lactated ringers or Albumin (colloids)…. Give half of fluid for the first 8 hrs, The remaining half is given over the next 16 hrs. o Oxygen o Make sure to time what time the burn occurred Management: o Wrap client in blanket Helps with hypothermia o Cool Water: No more than 10 min – NO ICE o Remove Jewelry o Remove non-adherent clothing o Do not remove stuck Clothes o Inhalation injury Give 100% oxygen b/c low hemoglobin o Intubate if airway is compromised **Weight is the best indicator for fluid status EXCEPT for Burns, Its Urine Output** Immunizations: o Tetanus If client doesn’t know he had it, give Immunoglobulin Oncology: KNOW ALL THESE!! Risk Factors: Tobacco and alcohol Obesity Low fiber diet: you retain more carcinogens Increased red meat consumption Increased animal fat Nitrates: processed sandwich meats. Salt cured or smoke meats Preservatives and additives Aging African Americans Radiation Stress Chronic Irritations GERD History Diet: o High fiber: Increase in fruits o High Calorie o High Protein Cancer Primary Prevention: Teaching o No smoking o Exercise o Lose weight o Vaccines – Heb B, and HPV o Wear sunscreen, and avoid sun, and secondhand smoking Secondary Prevention Screening Tertiary Prevention Treatment (support group and Rehab) o The warning signs of cancer can be remembered with the acronym CAUTION: Change in bowel or bladder habits A sore that does not heal Unusual bleeding or discharge from a body orifice Thickening or a lump in the breast or elsewhere Indigestion or difficulty in swallowing Obvious change in a wart or mole Nagging cough or hoarseness Bone Marrow cancer leads to Anemia: Low RBC (hypotension) and Hypoxic; increase in pulse (Tachycardic) Leukopenia Thrombocytopenia Blood Tests: o CBC & differentials Monitor Neutrophils o Liver Enzymes AST & ALT monitor closely o Tumor markers Substance that increase in the urine, blood, or bloody tissue bio markers Treatment: o Trach When changing the string, you have to hold onto the trach If Trach falls out, You CAN reinsert the dirty trach back in o Total Laryngectomy: Removal of Epiglottis, vocal cords and Thyroid cartilage) Will have permanent Tracheostomy so suction frequently Post op care for Total Laryngectomy: o NG feedings o Monitor drains o Watch for carotid artery rupture (Hemorrhage) o Provide frequent mouth care o NO SWIMMING o Cannot whistle or drink from a straw o When client gets discharged, they will have a protective Bib to cover the trach NO PLASTIC BIB No cloth fibers No powder: it will irritate it Humidifier is good Can not whistle or drink from a straw *** CALL HCP IF PATIENT HAS HEMOORHAGE, DON’T PICK VITAL SIGNS FOR PRIORITY*** Mastectomy post op care: o Check back of draining: blood Pooling can occur into the tissues o Abdominal surgical site: if own skin has been used o Check Hemovac or Jackson pitt drains: Hemovac- Used after mastectomy, o Empty when full or q8hr, o Remove plug, empty contents, o Place on flat surface, o Cleanse opening and plug with alcohol sponge o compress evacuator completely to remove air o Release plug, o Check system for operation Nursing care for Mastectomy: o Stay away from the arm that is affected side forever o No constriction No BP cuffs No elastic No watch No pulse No nail biting No injections Wear gloves when gardening Watch for cuts No IV o CAN DO: USE WITH AFFECTED SIDES o Brush hair o Squeeze tennis balls o Wall climbing o Flexing and extending the elbow Treatment: Radiation therapy Nursing assignment should be rotated daily so same nurse isn’t getting radiation everyday One client per shift no pregnant nurse can be assigned o Hazards to others for 24-48 hrs Short visits Distance should be as far as possible Wear lead shield (shielding) o Precautions: Private room Film badge at all times Restrict visitors – limit 30 min/day per visitor and 6ft away No pregnant visitors or less than 16 yrs of age or nurses Mark the room for isotope (radiation room) Wear gloves Radiation dislodgment device: (DURING) o Keep bed rest o Low fiber diet o Prevent bladder distension – will have indwelling catheter to prevent bladder distention IF DISLODGES: Wear gloves Pick it up with forceps Place in lead lined container (YELLOW containers) Call the radiation people to grab it Post-op: o Do not share bed for 1-11 days o No public transport o Stay away from children for 3 days o No work immediately o No sharing or cooking o When flushing, close the lid and flush 2-3 times Chemotherapy precautions: This is also for body fluids excretion!! Wear coated chemotherapy gown (change if gown is contaminated) 2 pairs of chemotherapy gloves (NO LATEX) Goggles Mask if splash or inhalation can occur o TEACH FAMILY ABOUT WEARING THESE IF FLUID EXCRETIONS ARE INVOLVED!!! EXCRETIONS CAN LAST 3-7 DAYS *If chemo spills, what to do? 1. Wash Hands 2. Get the spill kit 3. Wear respirator so you don’t inhale 4. Wear chemo gown 5. 2 set of gloves 6. Wear goggles 7. Use absorbent pads to wipe up spills **Vesicant drugs should be given through PICC line so it doesn’t infiltrate (extravasation)** IF extravasation happens: S/S is PAIN Stop the infusion Get the extravasation kit Stay with the client Side effects of chemo drugs: o GI: Nausea and vomiting: antiemetics meds (Ondansetron) given for the first week to help with this or herbal stuff: ginger, acupuncture Stomatitis: diarrhea included: watch out for fluid and electrolyte imbalance and nutrient deficiency o Integumentary System: Alopecia (hair loss) Mastectomy Scar tissue o Hematopoietic system: Low RBC, WBC, and platelet: watch for infection, anemia, and bleeding Other general side effects include: Fatigue Pain: give opioids o Side effect of opioid is constipation so give stool softeners Complications: o Low neutrophils (best indicator for infection) Neutropenic clients: No live vaccines No Fresh fruits/vegetable, No milk No flowers DVT b/c prolonged bed rest DVT can delvelop into PE Thrombocytopenia: Decrease of platelets Avoid: (NSAID) o Aspirin o Clopidogrel o Heparin o warfarin o Endocrine: Thryoid gives you energy Thyroid: produces 3 hormones: T3, T4, Calcitonin Calcitonin decreases calcium levels. Calcitonin if given with med can decrease Osteoporosis You need Iodine to make all these 3 hormones Graves’ Disease: Hyperthyroidism o Attention Span Decreases o Appetite up o Weight decrease o Arrythmias o Sweating and hot o Heat tolerance and soft hair o Exophthalmos (bulging eyes) o Diarrhea and increased bowel sounds o BP and Pulse increase (Arrythmias and palpatations) o Diagnosis: o Increase in T3 and T4 o TSH will decrease o Thyroid scan: CLIENT MUST STOP ANY IODINE MED ONE WEEK BEFORE THIS TEST. Must wait 6 weeks to start any iodine med after test o Ultrasound o CT and MRI Treatment: Med o Methimazole (stops making thyroids) also used in preop to stop the thyroids from making more o Iodine Compounds (Potassium Iodine solutions, and SSKI): decreases the size and vascularity of the gland BASICALLY it will decrease them from bleeding… Give these meds in milk, juice and USE A STRAW o Beta Blockers: helps with the symptoms only like BP ALSO DECREASES ANXIETY DIABETIC AND ASTHMA PATIENTS SHOULD NOT BE TAKING THIS ** BETA BLOCKERS DECREASE HEART RATE AND BP SO YOU WILL NOT GIVE PEOPLE THIS IF THE HEART RATE IS LOW** **Euthyroid= Normal** Curative Procedure: o Radioactive iodine therapy: Destroys the thyroid cells so you will become Hypothyroid (THIS IS EXPECTED) STAY AWY FROM BABIES DON’T KISS PEOPLE FOR ONE WEEK ANYBODY WHO HAS THYROID ISSUE CAN GO TO A THYROID STORM AT ANYTIME Thyrotoxicosis (THYROID STORM) (eg, fever, chills, tachycardia), including small rises in body temperature Surgery: thyroidectomy o Post op care: HEMORRHAGE S/S: o Report any feelings of pressure on the neck o Check for bleeding or swelling behind the neck and at the incision sites for pooling Assess for Laryngeal damage by listening for an increase HOARNESS OR WEAK VOICE: can lead to vocal paralysis Keep Trach at bedside: for possibility of hypocalcemia Assess for parathyroid removal (serum calcium will go down) so look for s/s of hypocalcemia (not sedated) Support the neck by using pillows and put personal items close to them Elevate HOB to decrease Edema Thyroidectomy: Biggest thing is risk for Hypocalcemia…. facial or extremity numbness or tingling, stridor, Trousseau and Chvostek signs Thyrotoxicosis (THYROID STORM) (eg, fever, chills, tachycardia), including small rises in body temperature Position: Elevate HOB to decrease Edema Diet: Avoid spicy food for people with Hyperthyroidism MORE CALORIES b/c they are losing weight HYPO thyroidism/ Myxedema: everything is slow People with hypothyroidism usually also have CORONARY ARTERY DISEASE o S/S: No energy Dry skin and hair Slow and slurred speech Tired/sleepy Weight gain GI slow Cold intolerance Amenorrhea Diagnosis: o Decreased T3 and T4 o Increased TSH Treatment: LIFELONG MED o Levothyroxine: start from low dose b/c risk for MI HR and BP increase with this med so WATCH for Rhythm changes and chest pain TAKE IT ON AN EMPTY STOMACH!! Parathyroid: Secretes PTH so Serum calcium will go up HyperParathyroidsm = HYPERCALCEMIA = HYPOPHOSPATEMIA Every time you see Hyperparathyroidism that’s the same exact thing as Hypercalcemia o S/S: Serum Calcium is high Serum phosphorus is low Fatigue Muscle weakness Renal calculi, Back and joint pain o Treatment: Partial Parathyroidectomy o Look for S/S of HypoCalcemia Diet: o High Protein o Low Calcium HYPO Parathyroid: Every time you see HYPOparathyroidism that’s the same exact thing as HYPOcalcemia S/S: o Serum Calcium is low so think of s/s of Hypocalcium o Serum Phosphorus High Treatment: o IV calcium (Selvidmere, Calcium acetate) Pheochromocytoma: Benign tumors that secrete epi and nor epi Adrenal gland problem Avoid palpating the abdomen with Pheochromocytoma because it will cause a sudden outburst of epi and nor epi o S/S: Persistent HTN Increased HR and have palpations Flushed and headaches (comes and goes) Hyperglycemia Diaphoresis Tremor Pounding Headaches Diagnosis: o Catecholamine test o VMA test: Vanilla will alter this test o 24 hr urine test: throw away the first one and the keep the last Client teaching before the test Avoid stress Treatment: Frequent bathing and rest breaks Avoid cold and stimulating foods Surgery to remove tumor Adrenal Cortex are steroids Steroids puts a patient on high risk for infection 4 major actions of steroids o Changes mood – can cause depression, and insomnia o Lowers/ Suppress the immune system and inflammatory response o Makes glucose higher o Breaks down fat **NEVER STOP STERIODS ABRUPTLY** With steroid medications, you increase if you have stress!! Mineral corticosteroids makes you retain Aldosterone (sodium and water) Also helps you lose Potassium Given to Addison Patients Diabetes Mellites: body starts breaking down fat and protein, When you break down fat, you get ketones Diabetes Lab values that are effected are fat and protein in the urine Type 1: Think MAC Kussmauls (Metabolic acidosis kusmaals respirations DKA = Hydrate them first no matter what IF YOU SEE DKA, PICK DEHYDRATION first thing you do is give normal saline Patients who go DKA, will be Hyperkalemic (potassium goes up) so make sure to give them potassium even if their potassium levels are stable because you don’t want it going down after giving them Insulin Monitor: Hourly outputs ECG: because of the hypokalemia Watch for HypoKalemia and hypoglycemia when giving them insulin Type 2 Diabetes Mellitis: is usually Found by accident Diagnose: o wound that won’t heal o Repeated vaginal infections o Acanthosis nigricans is a skin condition that occurs with diabetes Treatment: Meds oral or subQ o Metformin: Discontinue if undergoing surgery or any radiologic procedure (contrast (with dye) xray o Can resume after 48 hrs. if kidney function is good and creatinine is good **Clients should eat when insulin is at its peak** Hypoglycemia: o S/S: Cold & Clammy Confusion Shaky Headache Nervous Nausea Increased pulse and low BP Hunger ** When treating Hypoglycemia, DO NOT pick a food that’s high on fat, Pick simple carbs like coke or juice** Then Eat complex carbs after recovering NPH Peak (cloudy): 4-12 hrs Duration: 16-24 hrs Long Acting: Peak: no peak Duration: 24 hrs Detemir is a long-acting (basal) insulin Client Teaching o Clients should have an A1C drawn every 3-6 months o Increase insulin dose when sick Illness= DKA o Rotate sites o Wear well fitting shoes o Inspect feet everyday o No harsh chemicals o Infusion pumps are only used for Rapid acting insulin Gestational Diabetes o Scan on 1st prenatal visit, then retest 24-28 weeks o All moms ate 24-28 weeks Complications to baby if mom has GD: Increased birth weight Hypoglycemia Cardiac Left ventricle = Cardiac Output Meds that affect (increase) HR and BP Beta blockers Calcium channel blockers Digoxin Meds that affect (increase) BP only: Furosemide Nitrates (nitroglycerin) Inotropes (dopamine, Ace inhibitors (enalprines) ARBS (losartan) Atropine is AN agent used to increase heart rate in clients with symptomatic bradycardic - ATROPINE (ANTI CHEOLNERGIC MEDS CAN TREAT COPD AND OVERACIVE BLADDERS) Anything 50 and below give atropine!!! Coronary Artery Disease: Decrease blood flow to the heart ..Angina or CAD or any heart disease is also linked with ISCHEMIA meaning no oxygen so when YOU THINK HEART, also think ISCHEMIA CAN HAPPEN which can bring on temp pain and pressure to the chest o Treatment: Nitroglycerin Causes Venous and Arterial dilation (which is good) Have to take it every 5 min x (up to) 3 doses DO NOT SWALLOW NITRO KEEP IN DARK GLASS BOTTLE DO NOT MIX AND DO NOT OPEN FREQUENTLY KEEP IT DRY May burn or fizz in client’s mouth (normal and expected) Headache is normal and expected so don’t report Replace every 6 months and 2 years if it’s a spray Nitroglycerin is used for chest pain BUT can worsen hypotension and should be held. Other pain medications (eg, morphine) may be given for chest pain if blood pressure is low. (CONTRAINDICATED FOR PEOPLE WITH HYPOTENSTION) Beta blockers – prevents angina NOT for angina attacks Drops BP, AND Pulse Calcium channel blockers- Prevention of angina Digoxin: used in long-term treatment of heart failure. When you are getting a cardiac test done, DO NOT take your cardiac meds such as: Nitrates (nitroglycerine or isosorbide) Dipyridamole Beta blockers And DO NOT TAKE THEOPHYLINE: used for asthma or COPD Over the counter meds increase BP not Decrease so if a client is having hypertensive and is feeling dizziness, PLEASE DON’T ASKM if hes taking any OTC meds CUZ AGAIN those things INCREEASE BP o Patient education: Rest frequently and reduce stress Avoid overeating; LOSE weight Low fat and high fiber diet Avoid excess caffeine Wait 2 hours after eating to exercise Avoid extreme temperatures Stop smoking Lose weight AVOID ISOMETRIC EXERCISE (weight lifting) o Diet: Low fat and high fiber diet low- sodium, calorie-restricted Avoid excess caffeine o Procedure to Diagnose: Cardiac Catherization dye excretes from kidney Pre- procedure: Ask if allergic to iodine or shellfish Check kidney function if poor renal function DON’T give Give Acetylcysteine (mucomyst): protects the kidneys Will receive “hot shot” (dye) but called hot shot b/c they will feel warm and flushed this is for any dyebased things PALPATATIONS are NORMAL Do baseline assessment Post procedure: Hold Glucophage meds for 48 hours Monitor vital signs Watch for hematoma or bleeding Assess extremity DISTAL to the puncture site Assess for 5 P’s: Pulselessness Pallor Pain Paralysis Paresthesia: Abnormal sensation of the skin (tingling) Check circulation Bed rest, flat, 4-6 hrs Worry about HEMMORRHAGE/ BLEEDING o Position: flat o Complication: bleeding and Hemorrhage Acute Coronary Syndrome: Ischemia and Necrosis can occur this isn’t cause by client’s action, they can be asleep and still have an MI REST OR NITRO WILL NOT relieve this pain o S/S: Crushing pain OR “elephant sitting on me” Discomfort in left jaw Women present with GI pains Indigestion Feeling of fullness in the abdomen Chronic fatigue Inability to catch ones breathe #1 sign in the elderly patients Cold and clammy BP is dropping ECG changes and PVC Vomiting o Complications for Acute coronary syndrome Sudden death Arrythmias Pulseless v- tach V-fib…… REMEMBER for V-fib, you Defib Asystole V-fib, you Defib also do CPR till you get a heartbeat (CPR between Defib) If client remains in V-fib after doing Defib, give Epinephrine, and if that doesn’t work, give Amiodarone (Cardarone) Amiodarone or Lidocaine is used to prevent a second V-fib Lidocaine: toxicity Watch for neuro change o Amiodarone: Watch for Hypotension b/c it can lead to Asystole o Treatment for Acute Coronary Syndrome: Follow the order o Oxygen if O2 is <90 o Aspirin (chewable works faster than tablets) o Nitro o Morphine (if pain is not relieved by morphine) o Position for Acute Coronary sydrome: Head up (Semi fowler) Thrombolytic therapy eg, alteplase, tissue plasminogen activator [tPA]) is used to dissolve blood clots and restore perfusion to brain tissue in clients with an ischemic stroke unless contraindicated (eg, active bleeding, uncontrolled hypertension, aneurysm). ***Anything with the suffix -Place (mostly -place) or - Kinase will be a thrombolytic*** o Complication for Thrombolytic is BLEEDING so ask for any recent surgeries, or bleeding histories Bleeding precautions when using: o Acetameiphine o Liver problems o Contraindication for thrombolytic: If given, will cause Hemorrhage Intercranial neoplasm or bleed Suspected aortic dissection Internal bleeding ***Do NOT draw ABGs on thrombolytic patients*** Heart patients: Teaching No Isometric No straining Client will be on docusate You can have sex, if you walk a flight of stairs or 1 week to 10 days o Safest time for sex is morning Walking best exercise for MI client Teach them about S/S: Weight gain Ankle edema SOB Confusion ***ANYTIME an elderly client has mood/behavioral changes, its not normal, she can be having a UTI *** Assume the worst Heart failure: o Causes: Cardiomyopathy Valvular heart disease Endocarditis Acute MI Hypertension (leading cause) Left sided heart failure: blood is not moving forward from the Aorta to the body, rather it’s moving back to the lungs o Left = Lungs That’s why your S/S are all pulmonary o S/S: LEFT D- DSYPNEA O- ORTHOPNEA C- COUGH and CRACKLES H- HEMOPTYSIS (coughing up blood aka lung bleeding) A-ADVENTIOUS SOUNDS P- PULMONARY EDEMA/CONGESTION Right Sided Heart Failure: Blood is not moving forward so it will go back into the venous system o Right = Venous system o S/S: RIGHT A - Anorexia W- weight gain H- hepatomegaly E- edema pitting A-Acities D- distended veins Pulmonary Embolism is right Sided heart failure!! Hypoxic will always be right sided heart failure!! NSAIDS ARE CONTRAINDICATED WITH HEART FAILURE!!! Diagnosis: Clients with heart failure are expected to have elevated brain natriuretic peptide (BNP) levels best indicator Turn off Nesiritide 2 hrs before you draw a BNP b/c it will give a false positive o BNP o Enlarged heart (xray) o ECG When you are getting a cardiac test done, DO NOT take your cardiac meds such as: Nitrates (nitroglycerine or isosorbide) Dipyridamole Beta blockers And DO NOT TAKE THEOPHYLINE: used for asthma or COPD o Treatment for HF: ACE inhibitors o Drug of choice for HF o Blocks Aldosterone (you will lose water and sodium BUT retain Potassium) so monitor for HyperKalemia o Increases stroke volume (which is good) o Side effect: Nagging Dry cough (normal) ARBS: Beta blockers: also drug of choice Digoxin: Used in long-term treatment of heart failure, sinus rhythm or A-fib o Slows heart rate down; hold if below 50 o Monitor for Toxicity anything over 2, you are toxic o Monitor electrolytes Especially Potasassium (hyperkalemia) Early signs for Digoxin toxicity Nausea/vomiting Anorexia Late signs for Digoxin toxicity Arrythmias Vision changes (halos) Diuresis: Lasix o Give in the morning o Nursing consideration for HF patients: o Do NOT give whole blood unless if going into surgery o Always diuresis HF clients o Digitalizing dose (loading dose) first few doses will be a larger dose o Check APICAL pulse before giving Digioxin 5 th intercostal space and left mid clavicular line Fluid retention think HF first o Diet: Low fat and high fiber diet low- sodium, calorie-restricted Avoid excess caffeine Pacemakers: sends out impulses to make the heart o Post procedure: Monitor the incision Electrode displacement aka the wires are pulled out (common complication) Immobilize the arm You can do some range of motion to Prevent frozen shoulder NEVER EVER raise higher than shoulder wires can get pulled out Monitor ECG for pacemaker malfunction o S/S: Loss of capture Contraction does not follow the stimulus Any sign of decrease Cardiac output or pulse o Client Education: Check pulse daily Carry ID card or bracelet Avoid magnet fields like cellphones sould be used in the opposite ears Stay away from MRI They CAN use a microwave Pulmonary Edema: can’t move the volume forward o Causes: Usually occurs at night Anybody getting fluids fast Young or very old Anyone with heart or kidney disease o S/S: Sudden onset Breathless: hard to breathe when lungs are filling up with fluid Restless, and anxious Severe hypoxia Pink frothy sputum ***Anytime you see restless and anxious, think of severe HYPOXIA*** frothy, pink-tinged sputum or blood tinged is always going to be pulmonary edema crackles (left sided HF) o Treatment: Administer high flow oxygen and keep above 90% Lasix give slowly over 1-2 min to prevent hypotension and ototoxicity Bumetanide: to provide rapid fluid removal Nitroglycerine: it decreases afterload Morphine IV push: vasodilator Nesiritide: vasodilator and has a diuretic effect o Position: Upright; legs down o Prevention: Check lung sounds Avoid fluid volume excess -------- Cardiac Tamponade: When you have blood, fluid or exucdates that has leaked into the pericardial sac RESULTING into compression of the heart muscle When assessing clients with pericarditis, it is critical for the nurse to observe for signs of cardiac tamponade (eg, muffled or distant heart tones, hypotension, jugular venous distension) o Risks: MI Car accident Right ventricle biopsy Hemorrhage post CABG (open heart transplant) Remember High BP = High CVP and EXCEPT FOR CARDIC TAMP Low BP = Low CVP EXCEPT FOR CARDIC TAMP Hallmark sign for cardiac Tamponade: Low BP and High CVP o S/S: BIGGEST sign is Low BP and High Muffled/distant heart sounds: because you’re listening through blood, fluid or excaudate Neck vein distended BUT client will have clear lung sounds Shock: due to decreased BP Narrowed pulse pressure Tachycardic Tachypnea; dyspnea o Treatment: Pericardiocentesis: To remove the blood around the heart Surgery so monitor fluid output ------------- Atherosclerosis: if you have it in one place, you have it everywhere Emergency only if you have an ACUTE arterial occlusion Remember Arterial blood is oxygenated blood**** and veins= deoxygenated blood IF you see Artery think OXYGEN Artery can include: o Carotid: feeds brain o Femoral: feeds legs o Radial Artery: hands C is correct o S/S: Numbness and pain Extremeity will be cold No palpable pulses Decreased peripheral pulse: Priority nursing assessment Decreased muscle tone: lack of oxygen to muscles Bruit: Anytime you see bruit, think turbulent blood flow Symptomatic Lower extremities Intermittent claudication AKA Pain is the biggest sign You ONLY have intermittent claudication with Artery problems NOT vein problems You dangle artery problems and you elevate vein issue problems o Position: Dangle legs o Treatment: Angioplasty Angina or CAD or any heart disease is also linked with ISCHEMIA meaning no oxygen so when YOU THINK HEART, also think ISCHEMIA CAN HAPPEN Distended jugular veins and lung crackles indicate volume overload. The main risk with ectopic pregnancy is hypovolemic (hemorrhagic) shock. Jugular veins would be flat in hypovolemic shock. Atropine is AN agent used to increase heart rate in clients with symptomatic bradycardic - ATROPINE (ANTI CHEOLNERGIC MEDS CAN TREAT COPD AND OVERACIVE BLADDERS) Anything 50 and below give atropine!!! Spironolactone makes potassium high so avoid high potassium foods Hypokalemia results in muscle weakness/paralysis and soft, flabby muscles. Paralytic ileus (abdominal distension, decreased bowel sounds) is also common with hypokalemia. However, the most serious complication is cardiac arrhythmias. frothy, pink-tinged sputum or blood tinged is always going to be pulmonary edema crackles (left sided HF) cardiac is mostly with water and fluid overload for the lungs If you see cardioversion or cardioverter, PICK SOMETHING WITH SYNC Right sided VS Left Sided HF: Atorvastatinis a lipid-lowering medication Dipine: calcium channel Verapamil: same as metoprolol Lisinopril may cause hyperkalemia and hypotension, and should be administered only to clients with normokalemia and normotension Metoprolol lowers blood pressure and heart rate Docusate sodium is a stool softener that reduces straining during bowel movements When giving Furosimide, Assess for BP, BUN, creatinine, and Potasissum Partial thrmobinplastin time (PTT) checks of overose of heparin Normal Value of PTT is 100 seconds or less Cardiac Tamponade s/s: Hypotension with narrowed pulse pressure (Option 1) Muffled or distant heart tones (Option 4) Jugular venous distension (Option 5) Pulsus paradoxus Dyspnea, tachypnea Tachycardia A coronary arteriogram(angiogram) is an invasive diagnostic study of the coronary arteries, PACEMAKER IS WITH HEART RATE SO IF YOU SEE PACEMAKER, GO WITH HEART RATE ***Pace maker CANNN use microwave Nitroglycerin is used for chest pain BUT can worsen hypotension and should be held. Other pain medications (eg, morphine) may be given for chest pain if blood pressure is low. (CONTRAINDICATED FOR PEOPLE WITH HYPOTENSTION) When MAP is asked use formula: Systolic + (diastolic x2) / 3 A normal MAP is 70-105 mm Hg Dry, shiny, hairless skin are common clinical manifestations of chronic peripheral arterial disease Positioning the client on the left side is appropriate if a central line is inadvertently pulled out Hypotension has to do with dehydration which means fluid volume deficiency VITAMIN K is a reversal agent for WARFARIN therapeutic aPTT level between 46-70 seconds Antidote for Heparin is Protamine sulfate About 1 question so know these KNOW BOTH LEFT AND RIGHT HEAT FAILUTE!!! Know what’s below Left: D- DSYPNEA O- ORTHOPNEA C- COUGH H- HEMOPTYSIS (coughing up blood aka lung bleeding) A-ADVENTIOUS SOUNDS P- PULMONARY EDEMA/CONGESTION Right: A - Anorexia W- weight gain H- hepatomegaly E- edema A-Acities D- distended veins CVP is a measurement of right ventricular preload (volume within the ventricle at the end of diastole) and reflects fluid volume problems. The normal CVP is 2-8 mm Hg. An elevated CVP can indicate right ventricular failure or fluid volume overload. Clinical signs of fluid volume overload include the following: Peripheral edema Increased urine output that is dilute Acute, rapid weight gain Jugular venous distension S3heart sound in adults Tachypnea, dyspnea, crackles in lungs Bounding peripheral pulses Dry mucous membranes and hypotension are signs of deficient fluid volume or dehydration. Ventricular tachcardia^ Anticoagulation with heparin is indicated if the client's pain is determined to be due to acute coronary syndrome you give heparin if patient has acute CORONARY SYNDROME The client should avoid lifting the arm above the shoulder on the side of the pacemaker until approved by the HCP as this can cause dislodgement of the pacemaker lead wires. Elevating the legs promotes venous return but does not promote arterial circulation SO DO NOT PUT LEGS UP WHEN A PATIENT HAS PAD (PERIPHERAL ATERIAL DISEASE) (PERIPHERAL ATERIAL DISEASE): Heating pads should not be used in clients with altered perfusion or sensation due to the increased risk for burns. When assessing clients with pericarditis, it is critical for the nurse to observe for signs of cardiac tamponade (eg, muffled or distant heart tones, hypotension, jugular venous distension) Rescue breaths every 5-6 seconds (10-12 breaths/min) are given to clients who have a pulse but are not breathing normally. For clients with no pulse, the nurse should deliver cycles of 30 compressions followed by 2 rescue breaths. CHEST TUBE OUTPUT IS THE SAME THING AS CHEST DRAINAGE They just wanna trick you to see if you know what they both are SO 100< or less is good 100> or more REPORT TO THE DAMN DOCTOR When you think of vomiting, what do you think of??? DEHYDRATION (forget this and you can sit your ass back to nursing school and kiss business goodbye) Over the counter meds increase BP not Decrease so if a client is having hypertensive and is feeling dizziness, PLEASE DON’T ASKM if hes taking any OTC meds CUZ AGAIN those things INCREEASE BP A normal platelet count is 150,000-400,000/mm3 BUT 80,000 is expected for liver cirhossis A normal prothrombin time is 11-16 seconds for WARFARIN Digoxin: used in long-term treatment of heart failure. When you are getting a cardiac test done, DO NOT take your cardiac meds such as: Nitrates (nitroglycerine or isosorbide) Dipyridamole Beta blockers And DO NOT TAKE THEOPHYLINE: used for asthma or COPD Clients with heart failure are expected to have elevated brain natriuretic peptide (BNP) levels. Stridor is consistent with a laryngospasm or edema, of the upper airway, and epiglottitis. Bronchial breath sounds are normally heard over the trachea When you see the word TRANSPLANT, always remember client is at risk for INFECTION IF central venous catheter (CVC) gets dislodged, you are at risk of developing AIR EMBOLISM you want to put them on their left side TRENDELONBURG POSITION, so all the blood comes rushing to the heart. --- DO NOT PICK FOWLERS, CUZ THAT’S NOT GOING TO DO ANYTHING BUT CAUSE THEM HARM. BY MAKING THEIR RESPRITORY DISTRESS EVEN WORSE Diuretic medications cause clients to urinate more. Morning is the appropriate time to take this type of medication. Evening administration would cause nocturia and interrupted sleep. NSAIDS ARE CONTRAINDICATED WITH HEART FAILURE ANY ENDOVASCULAR repairs are not invasive so NO INCISIONS think of Endo as Easy; E for Easy……… Make sure to palpate or monitor peripheral body and monitor urine output Patients with HF, their BNP will go up VENOUS INSUFFUCIENCY are varicose vein Know your damn TRENDELUNBURG AND REVERSE TRENEDELONBRUG Bounding pulse has to do with fluid overload aka hypertension You check INR only for clients who are taking WARFRIN CARDIAC TAMPONADE: life threatening BP is becoming slow so they dying remember BLM (Black lives matter) for signs and symptoms B: Big jugular vein distention (JVD) L: Low BP M: Muffled heart sounds or distant heart sounds aka YOU CAN’T HEAR THE DAMN HEART SOUNDS AKA when you see distant heart sounds/tone PICK IT!!! Cardioverters have the same restrictions as a pace maker so meaning you cant put your hands above your heart Septic shock can lead to HYPOTENSION so give fluids Psychiatric….REVIEW SECTION 3!!!! Anhedonia: loss of pleasure For suicide, use closed ended statements You never give naloxone PO and YES, they do need hosputalizaion after emergency treatment of Naloxone… AND must be administered every few hours till opiod levels are non toxic Treamtment for Opoid is Methoadone: Long acting opoid Can later on be titrated to ease withdrawal symptoms Alcohol: seizure precautions You can give them Anxiolytic drugs ----------------- Renal: Kidneys and heart coincide so if you have heart problem you’ll have kidney problem -Glomerulo = Filtering -Nephr = Kidney Glomerulonephritis: Inflammation of the filtering portion of the kidneys so DECREASED filtering will occur o It can start with sore throat or skin disease o Causes: o Strep – Group A Beta heart and kidney can be infected if not treated o Skin infection – impetigo, hepatitis o S/S: Flank pain aka Costovertebral angle tenderness or CVA tenderness Decreased urinary output Urine gravity is increased Hematuria – Blood in the urine Proteinuria – protein in the urine Periorbital Edema Raised BP – fluid volume excess Raised BUN and Creatinine Malaise (discomfort) and headache o Treatment: o Cure the Strep o Monitor I &O and daily weights o Diuretics o Monitor BP o Restrict fluids – To determine how much fluid to give= 24hr fluid loss + 500 mL o Balanced activity with rest o Diet: everything low except carbs Increased carbs Protein restricted Restrict/low sodium Fluid restricted Potassium restricted Phosphorus restricted o Client education: Client will dieurese within 1-3 weeks after onset Blood and protein may stay in the urine for months Teach S/S of Renal failure: o Malaise (discomfort) o Headache o Anorexia o N/V o Decreased Output o Weight gain Notify doctor if you see these symptoms ---------------------------- Nephrotic Syndrome: inflamed kidneys (glomeurlous) where big holes starts forming and protein leaks out Protein = Albumin So they will be hypoalbuminemia (low albumin) KNOW ABOUT ALBUMINS (HYPERALBUMINIEMIA AND HYPOALBUMENIA When Albumins are low (HYPO), pitting edema and Ascites can occur proteins (albumin) in the blood that pulls water into the circulatory system. Albumin (normal: 3.5-5.0 g/dL [35-50 g/L]) When Albumin is low, Aldosterone kicks which makes you retain sodium and water Anasarca is extreme edema When you Lose protein, you can develop: Blood clots (thrombosis) High Cholesterol and triglycerides o Causes: Infection NSAIDS Cancer Lupus and diabetes o S/S: Massive Proteinuria Hypoalbuminemia Edema (anasarca) Hyperlipidemia o Treatment: Diuretics (Thiazides or diuretics prescribed) Ace inhibitors to block aldosterone secretions Prednisone for inflammation Cyclophosphamide: chemotherapy agent that decreases body’s immune response So, it will shrink holes and inflammation But they will be immunosuppressed So, INFECTION is major complication o Diet: Small frequent meals sodium-restricted high calorie high protein: only kidney problem where you increase protein potassium- restricted give lipid lowering drugs – anything with statins dialysis Anticoagulants therapy for up to 6 months o Nursing considerations: Monitor Daily weights and I&Os Measure abdominal girth and extremity size Good skin care with edema Acute Kidney Injury (AKI): o Causes: Pre-Renal Failure: Hypotensive Decreased Heart rate: means Decreased cardiac output which will decrease the amount of blood coming to the kidneys Any type of shock Intra-Renal Failure o Damage inside the kidney – Glomuronephritis, nephrotic syndrome o Malignant hypertension: aka uncontrolled hypertension o Diabetes o Hypotension o Sepsis o Drugs that causes kidney injury – mycin and NSaids drugs o Dyes can damage kidneys too Post-kindey: urine cant leave the kidney o Enlarged prosate o Kidney stones o Ureter obstructions o Tumors o Edematous stoma 4 phases of Acute kidney injury: o Initiation Phase Injury occurs o Oliguric phase Output is less <100ml/24hr o Diuretic phase Kidneys are recovering o Recovery phase 3-12 months o S/S: BUN and Creatinine levels increase Serum Calcium levels Decrease: Clients with kidney injuries retain phosphorus clients will be hypocalceamic o To compensate, the body will pull calcium from the bones so now they have Osteoporosis too now Anemia can occur: Anytime kidney is damaged, they can’t produce a good amount of erythropoietin (blood) Hyperkalemia: we get rid of Potassium from our kidneys so If kidneys are damaged, the body cant excrete potassium Metabolic Acidosis: Client cant filter acids produced by the body Specific gravity will increase BUT Severe Kidney injury, you’ll get a fixed specific gravity Hypertension and HF: b/c they are retaining fluids Anorexia: they are retaining toxins Can’t fliter Hydrogen and Bicarb Itching frost (Uremic Frost) Maintain good skin care: too much urea and it will come out from your skin Phosphorus is linked with calcemia o Nursing Consideratons: Monitor hourly outputs Checking CVP Looking for S/S of urinary infection so if they have an indwelling catheter, GET RID OF IT Assess BP and treat Hypotension QUICKLY o Give them fluids o Bed rest o Elevate the leg Prevent infections Use aseptic technique Prevent pressure ulcers Mouth care No catheter Protect from infection disease Renal replacement therapy may be needed: they replace kidney functions aka dialysis Client and family support o Treatment: Bedrest to decrease Metabolism Turn, cough, and deep breathe Monitor intake and output Daily weights Monitor vital signs closely Meds: o Loop and osmotic Diuretics o IV glucose and insulin: for hyperkalemia IV and insulin moves the potassium out of the blood and back to the cells o Make sure to check drugs o IV calcium Gluconate: for dysrhythmias o K-acelate: to decrease Potassium o Phosphate bindings drugs: to prevent Hypocalcemia Give IV meds in small volumes so you don’t overload with fluids o Diet: Increase calories, carbs and fat Low protein Avoid phosphate food Low sodium Low potassium: coffee Renal Replacement Therapy Hemodialysis: o Before Dialysis begins, assess fluid status weight, BP, peripheral edema, lungs and heart sounds, and temp o Electrolyte and BP are monitored constantly o Vital signs 30-60 min during dialysis o Some can’t tolerate hemodialysis: some go to shock every single time o Client is given Heparin during dialysis so watch for bleeding precautions, and avoid invasive procedure o Depression suicide by eating too many bananas Vascular access: During Dialysis, 2 needles are inserted into the vascular access One will allow the blood to go to the dialysis machine and the other from the dialysis machine To the dialysis machine = Arterial From the dialysis machine = Low pressure venous o Care of Access: Do not use as IV access No BP No needle Stick No constriction – no watches, no carrying purses o Assessment of access: to ensure patency Palpate for thrill Auscultate for bruit Continuous renal replacement therapy is used for Acute kidney injury Peritoneal Dialysis: o Warm the dialysis o Drainage should look clear or straw colored …. Cloudy = infection o If all fluid doesn’t come out, turn client side to side o Increase protein and fiber when doing dialysis Kidney stones: Fancy words Nephrolithiasis, Urolithiasis, or Ureterolithiasis Sharp flank pain N/V due to extreme flank pain Increased WBC in the urine Hematuria*** blood in the urine Anytime you suspect kidney stone, get a urine specimen and checked for RBC (hematuria) If kidney stone is present, the client will get pain medication immediately o Treatment: Ondansetron NSAIDS or opioid narcotics Alpha adrenergic blockers (relax smooth muscles of ureter) Increase fluids FOREVER Maybe surgery to remove stone Lithotripsy to crush stone Strain urine – to keep and send stones for analysis o Diet: Increased fluid intake Calcium-controlled Low oxalate Total means Always and it will never be always GI: Pancreatitis: o Cause: Gallbladder Disease: #1 cause for acute or chronic Alcohol: #2 leading cause o S/S: Pain increases Abdominal distention: can lead to ascites Abdominal mass: that’s your swollen pancreas Rigid board-like abdomen: this means they’re bleeding inside, and it can lead to peritonitis Peritonitis Bruising: They can have bruising around the umbilical area AKA Cullen’s sign Bruising in the Flank pain: called Gray Turner’s sign Fever and inflammation N/V Jaundice: means liver is involved Hypotensive: b/c they might be bleeding or cuz of ascites o Diagnosis: everything will go up Lipase and Amylase serum going to increase o Lipase is the most specific enzyme for pancreatitis WBC increase Blood sugar will increase you can be diabetic forever ALT and AST will increase: These are your liver enzymes…….*Hint liver enzymes will always go up or be normal but NEVER down** PT and aPTT will be longer: which means it takes longer for your blood to clot If it was shorter, you would be at risk for too many clots Serum bilirubin will increase: Liver HgB and HcT can go up or down: If you are bleeding it will go down If you are dehydrated, it will go up o Treatment: KEEP THEM NPO and daily weights Fix pain o Meds: Morphine is contraindicated in Pancreatitis. It causes spasm of the Sphincter of Oddi. Therefore, Demerol should be given Demerol Anticholinergic drugs: they keep the stomach dry PPI Antacids TPN (total parenteral nutrition) Insulin: because pancreas is sick so no adequate insulin o Diet: low-fat, regular, small frequent feedings; tube feeding or total parenteral nutrition. ---------- Liver: o 4 main functions: Detoxifying your body Helps your blood to clot: so with liver problems, bleeding is the biggest complication Breaks down drugs: NEVER GIVE ACTEMINOPHEN OR TYLONOL to patients with liver problems Synthetizes albumin Antidote for Tylenol: Acetylcysteine or Mucomyst Should be mixed with carbonated drink cuz it smells like rotten eggs Cirrhosis: Liver cells are destroyed so it alters the circulation within the liver o BP goes up in the liver known as Portal Hypertension which can lead to hepatic coma o S/S: Firm nodular liver: it becomes HUGE Jaundice Abdominal pain Chronic dyspepsia (GI upset) Change in bowel habits Ascites Splenomegaly Peripheral Edema Fatigue Anemia Hepatic encephalopathy: anytime you have liver problems, look for the ammonia levels Rye syndrome o Diagnosis: Decreased serum Albumin: Main reason why people have ascites is because their albumin is messed up. Albumin is in charge to keep water in the vascular o Liver makes ALBUMIN Increased ALT and AST Confirmed with Liver biopsy: concerned about bleeding so do o Clotting studies: PT, aPTT, INR o Vital signs: b/c of hemorrhage o Position: Pre-Procedure: Supine with right arm behind head Then exhale and hold breathe: to move the diaphragm Post procedure: Lie on right side o Treatment: Antacids, vitamins, diuretics No more alcohol Monitor I&O and daily weights Rest Prevent bleeding: no aspirin, or no IM injection Measure abdominal girth: cuz of ascites Paracentesis o Have client void before o High fowler position; NO SUPPINE or semi fowl o Get baseline vitals and check it later Monitor Jaundice Skin care Avoid Narcotics o Diet: Low protein: if they eat high protein, it will make their ammonia levels go up which will make their LOC decrease Low sodium Low Fluids COOL Side info: When you eat protein, it transforms into ammonia, then your liver turns it into Urea. Urea gets excreted through the kidneys Hepatic Coma: when your body can’t transform ammonia into urea o S/S: LOC down Asterixis: hand tremors Handwriting changes: First sign of ammonia changes Reflexes decreases EEG will be slow Breathe smells like ammonia GI bleeders o Treatment: Lactulose: decreases Ammonia Enemas: need to take too much blood out from body cuz blood increases ammonia levels When giving this, place client on left side Decreased protein Monitor Ammonia levels everyday --------- Bleeding Esophageal Varices: You have High BP in your liver, and that pressure, excretes back to the esophageal o No one realizes they have this, till it pops o Once it ruptures, most commonly you start vomiting large bright red blood o Treatment: Replace blood Check vital signs Check CVP Anemic = oxygen Enema: to get rid of blood Lactulose Saline lavage: to get blood out of the stomach Sengstaken- Blakemore tube AKA balloon tamponade: o It holds pressure on the bleeding varices so hemorrhage doesn’t occur o Mark the tube o These clients are usually hypoxic b/c they were bleeding so much and alcoholic, so they are confused o Doctor might order restraints b/c clients will want to remove it o IF THE PATIENT CAN’T BREATHE, CUT IT!! ** In the NCLEX, stay away from restraints, they don’t lke nurses to use restraints*** --------- Peptic Ulcer: H. pylori o Common cause of GI bleeding o S/S: Erosion is present Can lead to burning pain or knowing sensation all the way to the back Heart burn or dyspepsia o Diagnosis: Gastroscopy (EGD) These things can be applied to any tube going to the mouth o NPO pre procedure o Sedated o NPO till gag reflex returns o Watch for perforation: S/S: pain, bleeding or trouble swallowing monitor for these when they come back Upper GI serious: Looks at stomach and esophagus with dye o NPO past midnight o No gum, no mints o REMOVE nicotine patch this applies to anyone whos NPO too o No smoking either: it will increase stomach secretions o Treatment: Antacids: liquid only to coat stomach o Empty and at bedtime (only med where you take at bedtime) Usually after meals you would take Antacids Proton pump inhibitors Any drug with suffix -prazole H2 Antagonist: like Pepcid Antibiotics for H. Pylori Sucralfate o Client Teaching: Decrease stress No smoking Eat what you can handle (Avoid spicy food) Avoid caffeine Follow up b/c it takes long for it to heal Hiatal Hernia: The hole in the diaphragm is too large, so the stomach moves up into the thoracic cavity o S/S: Large abdomen: b/c something is pushing it up Heartburn Fullness after eating Regurgitation: This is when they tie their shoes, and all the food and water comes up Reflux Dysphagia: difficulty swallowing o Treatment: Small frequent meals Sit up for 1 hr after eating Elevate HOB upright postion Dumping Syndrome: When stomach empties too quickly after eating o Gastric bypass or Gastrectomy and gallbladder disease can cause this o S/S: Fullness, weakness, palpitations Cramping, faintness, diarrhea o Treatment: No fluids with meals Small and frequent Avoid foods high in carbs and electrolyte o Position: Semi recumbent: that’s to lie back a little while eating Lie left flat after meals Lie flat on left to keep food in Lie flat on right side helps empty the food Ulcerative Colitis and Crohn’s Disease are classified as IBD: o Ulcerative Colitis: just in the Large Intestine o Crohn’s disease: also called Regional Enteritis, but inflammation in the ileum (small intestine) but it can be found either in small or large o S/S: Bloody Diarrhea Rectal bleeding Vomiting Anemia Weight loss Anorexia Cramping Dehydration Blood in stool Rebound tenderness means peritoneal inflammation Fever Pain o Diagnose: Colonoscopy o Need to be Clear liquid diet for 12-24 hrs o NPO for 6-8 hrs o Avoid NSAIDS prior to the procedure: because of bleeding o Laxatives and enemas till clear Watch client so they don’t get too weak o Drink polyethylene glycol: Get it icy cold: the colder it is, the more they can tolerate it Don’t drink it with a straw o Will be sedated for this procedure o Watch for Perforation: S/S pain and unusual discomfort, and abdominal distention Barium enema: AKA lower GI series o Diet: Low residue diet aka Low fiber diet Avoid cold foods and smoking o Treatment: Illiosotomy: care is for any ostomy o Post op care: Going to drain liquid, they don’t get clogged up so we don’t have irrigate it Client will a lot of fluid and electrolyts, so they will be dehydrated so they will need Gatorade or water at risk for kidney stones Decrease motility so low fiber foods Colostomy care: Post op o Irrigate in the descending colon irrigate same time and Irrigate after a meal too o If client starts cramping, stop the fluid and lower the bag or/and check the temp of the bag this is also for enema For colostomy bags Eliminate foods that cause gas and odor (broccoli, cauliflower, dried beans, brussels sprouts) AND EMPTY THE BAG OUT WHEN ITS ONE THIRD FULL….. Also give low fiber foods in the beginning Appendicitis: inflammation of the appendix o Position client in semi fowler right side o Causes: McBurney’s point: meaning pain in RLQ Rebound tenderness N/V With suspected Appendicitis, NEVER give Enemas or Laxative, b/c it will cause it to burst o Treatment: Surgery o After Abdominal surgery, place in fowler position --------- Total Parenteral Nutrient or parenteral nutrition: o Keep it refrigerated o Warm it up before giving (meaning keep it on the counter) o Central line only not peripheral unless it’s a picc line o Filter needed o Nothing can be mixed with this, this is specifically for the TPN o We discontinue gradually to Avoid hypoglycemia never go into the room and discontinue it abruptly o Do daily weights client should not be losing weight!! o Clients may have to take insulin accu checks every 6 hrs o Check Urine: for glucose and ketones…. if you got glucose in your, they need insulin and if you have ketones in your urine, it means TPN isn’t doing its job b/c your body breaking down its fat…it means they need fat o Mixture adjusted according to their electrolytes so monitor electrolytes o TPN can be hung only for 24 hours and tubing needs to change with each new bag o TPN is covered with dark bag: to prevent chemical breakdowns o Needs to be on a pump o Handwash Is important infection is most common complication o Placement will be confirmed via chest Xray and to see if pneumothorax has occurred o Position will be Trendelenburg when putting in a TPN in the central line o If air gets into the line, left side Trendelenburg o To avoid Air into the tubes: Clamp it off Valsalva: take a deep breathe, hold or Hummmm Side note: protein will not leak from the kidneys (glomerulus to be more specific) unless there is kidney damage so if you want to click proteinuria, ask yourself, is there kidney damage? ---------- Respiratory Hemothorax: blood in the pleural space Pneumothorax: air in the pleural space o S/S: Short of breath Tachycardic Diminished breathe sounds on the effected side Chest pain and cough Air or blood will show up on Xray Off track side note: never pull out a penetrating object!! o Treatment: Thoracentesis/chest tubes: GO DOWN to find out more info about these Daily chest Xray Tension Pneumothorax: pressure has built up and has collapsed the lungs so pressure pushes everything to the opposite side called mediastinal shift Basically, if your trachea is on one side of your neck, it aint good sis!! You’d rather have a normal pneumothorax Medical Emergency!!! o Causes: Trauma Too much PEEP (positive end expiratory pressure) set on the ventilator Clamping a chest tube Insertion of central venous lines Taping a pneumothorax on all 4 sides without an air valve So, TAPE only 3 sides!!! o S/S: Subcutaneous emphysema Decreases cardiac output Absence of breath sounds Asymmetry of thorax: trachea will be off centered Respiratory distress JVD Cyanosis o Treatment: Large bore needle placed in the second intercostal space for air to escape Find the cause Chest tubes will be inserted Open Pneumothorax: when an opening is in the chest, which is large enough that it allows air into the pleural space “sucking chest wound” o Treatment: Valsalva: inhale and hold Then place Petroleum gauze over the area and tape ONLY 3 SIDES!! LEAVE THE 4TH SIDE OPEN Sit up to assist with lung expansion Valsalva maneuver is contraindicated in clients with glaucoma and recent eye surgery, stroke and abdominal surgery, and liver cirrhosis. o Thoracentesis: Chest procedure to remove excess fluid or air o Pre-Procedure: Check for signed consent Stop any anticoagulant meds Obtain baseline vitals: O2 and pain level so we can compare Make sure chest Xray has been performed Either client will be upright, if they can’t then head of the bed elevated (45 degrees) and lie on unaffected side (good lung is down) o During procedure: As the fluid is being removed in this stage, the lungs should re-expand Client must be still (no coughing or deep breathing) Check vital signs O2 and pain levels When you are removing large volumes, BP goes down and Pulse goes up o Post procedure: Another chest Xray will be done Monitor vital signs and listen to lungs Check puncture sites for bleeding Monitor for tension pneumothorax, emphysema, infection We want them to turn, cough and deep breathe o Chest tube: The lung has collapsed so that’s why we need a chest tube Ex: Chest drainage tube o If the chest tube is placed in the upper lungs (second intercostal space), that’s for removal of air o If the chest tube is placed laterally in the lower chest (8th or 9th intercostal space), that’s for drainage o Client can have both **Air rises and drain goes down*** o The steps are the same thing as the thoracentesis with the petroleum gauze and shit o Chest Drainage tube/Unit is to normalize the pressure o Nursing Management: Palpate chest tube insertion: can indicate poor tube placement Record chest drainage every hour for 24 hours then every 8 hrs Report if bright red Use incentive spirometer Watch for elevated WBC or fever Promote gravity drainage o Maintaining chest tube: Straight and free from all kinks Tape all connections It must be a closed system Seeing tidaling and fluctuation is good Bubbling becomes a problem if its continuous in the water seal chamber can indicate an air leak NEVER CLAMP A CHEST TUBE WITHOUT A PRESCRIPTION o PROBLEMS: If it dislodges reconnect it EVEN if its dirty because the lung will collapse If Chamber falls over Reestablish the water seal, deep breathe and cough in case any air went inside the pleural space If the tube dislodges directly from the chest DO NOT PUT IT BACK INTO THE BODY, surgeon can only do that. Use sterile occlusion and TAPE IT ON 3 SIDES When Doctor takes the chest tube out, you tell the patient to take a deep breath and hold aka VALSALVA CPAP: delivered continuously Used for obstructive sleep apnea and infants who can’t breathe BiPAP: Used for nonobstructive sleep apnea, and its more tolerated You NEVER GIVE TOO MUCH OXYGEN FOR A COPD PATIENT UNLESS THEY ARE COATING (THEY ARE NOT BREATHING AT ALL) Pulmonary/air embolism: this is usually a blot clot in your lungs, but can also be fat, if there’s a clot, then gas exchange isn’t taking place o Causes: This can be for DVT, PE, VTE (meaning both) Dehydrated Prolonged immobility Birth control pills Heart Arrythmias like Afib Clotting disorders o S/S: Hypoxemia: #1 sign PO2 will go down Cough Cor pulmonae: Means Right sided heart failure Chest pain Increased resp rate/ tachpnea Tachycardic Petechia over the chest Short of breath Restless Cyanosis Atelectasis Hemoptysis (Coughing up blood) Cor Pulmonae is right sided heart failure caused by left ventricular failure (so pick edema, jvd, if it is a choice. o Diagnosed: D-dimer: this will tell you if theres a clot anywhere in the body CT scan: if dye is used, be sure to check renal function because that’s contraindicated Angiography: invasive o Prevention: Early mobilization: change position every 2 hours Flex and extend knees and hips Compression hose: be sure it’s on correctly Pneumatic compression is not used if they suspect a DVT Hydrate o Treatment: Elevate legs Administer anticoagulants: Warfarin, heparin, factor X YES, they can take Heparin and warfarin together Limit Green leafy vegtables when on warfarin o Use soft brush o Electric razor o Avoid rough activities tPA can DISSOLVE blood clots and is used for strokes Thrombolytic therapy eg, alteplase, tissue plasminogen activator [tPA]) is used to dissolve blood clots and restore perfusion to brain tissue in clients with an ischemic stroke unless contraindicated (eg, active bleeding, uncontrolled hypertension, aneurysm). o Position: Turn patient to the left side and Lower HOB Orthopedic: Fat embolus is a big complication for fractures Fat emobolism likes to go to the lungs o You can find fat embolus in: long bones pelvic fractures, and crushing injuries S/S: Petechia on chest Conjunctival hemorrhages SNOW STORM on chest xray: white fluffy stuff Fat embolism syndrome: is a rare, but life-threatening complication that occurs in clients with long bone and pelvis fractures S/S: Dyspnea Confusion Petechia (rash): PE (PULMOARY EMBOLISM doesn’t have this type Of rash Fever -------- Compartment syndrome: Fluid accumulates in the tissue and impairs tissue perfusion common areas are forearms and quadriceps Carpal tunnel is a type of compartment syndrome Carpel Tunnel Syndrome: paresthesia and pain of the wrist; to RELIEVE it wear wrist immobilization splints……. EXCERCISES MAKE IT WORSE That’s why we elevate when you have fractures Compartment Syndrome: 6 Ps (pain, Paranesthesia, pallor, paralysis, poikilothermic, pulseless) Volkmann contracture: inability to extend the fingers; is a sign of compartment syndrome IF PAIN DOES NOT HEAL AFTER GIVING MEDS, THAT IS A SIGN OF COMPARTMENT SYDROME!!!!! o Treatment: If you have a cast, loosen it to restore circulation if you see an answer that says “remove the cast” that shouldn’t be your first choice unless if that’s the only right answer Fasciotomy: Doctor cuts into the tissure to remove pressure and restore circulation o Cast care: Use palm to handle plaster cast no fingertips cuz of indentation Keep uncovered for plaster cast Always ask if they are diabetic Don’t rest cast on hard surface or sharp edge but you can rest it on SOFT PILLOWs BUT NOT PLASTIC If they bleed, circle the area and mark date and time Neurovascular checks especially if the client is in pain NEVER INSERT ANYTHING INSIDE A CAST, I DON’T CARE HOW SOFT IT IS just use a hair dryer o Traction: This has to be continuous SO NEVER RELEASE CONTRACTION Buck’s Traction—elevate foot of bed for counter-traction. Exercise mobile joints Ropes should move freely Weight should hang freely Monitor pin sites for any inflammation every 8 hrs Pin sites, use sterile technique Purpose of pins are to immobilize the leg so if pins fall out, immobilize the leg o Total hip replacement: Pre-op: Buck’s traction is used Post op: Neurovascular checks Monitor drains if they have drain Firm mattress Over bed trapeze We want to limit flexion and neutral position We want abduction: feet apart, like an abduction pillow They can do isometric exercises in bed Trochanter roll: to prevent external rotation... Document this too No weight bearing No bending over, or no crossing legs Don’t sleep on the operative side Hydration is important: pneumonia can occur if they are immobile No pain meds in the operative hip o Complication: Dislocation: you may see shortening of the leg and pain Infection: remove foley catheter ASAP Avascular necrosis DVT/VTE o Client education/rehab: Walking Swimming Rocking in the wheelchair Avoid flexion: So avoid low chairs Traveling long distances Sitting more than 30 min Lifting heavy objects Excessive bending Stair climbing residual limb refers to the part of the body that remains after an amputation has been performed o Amputation: Post op: o Limb should lie completely flat o Put client on prone position o Phantom pain: pain that isn’t there, but don’t be judgy so do some diversional activity and then some pain med avoid meds in the nclex as much as you can o Massages are okay o Proper way of walking with a crutch: Should fit properly: 1-2 in below the axilla (armpit) you’ll get brachial nerve damage if not fitted properly Rest body weight on hands Walking up and down the Stairs: up with the good and down with the bad o Proper way of walking with a cane: Use strong side with the cane Neuro: Glasgow Coma Scale (E)ye opening (Maximum = 4) 4 - Spontaneous (open with blinking at baseline) 3 - To speech 2 - To pain only 1 - None (C - Not assessable [eg, trauma, edema]) (V)erbal response (Maximum = 5) 5 - Oriented 4 - Confused (converses but confused, disoriented) 3 - Inappropriate (inappropriate words) 2 - Incomprehensible (sounds, no words) 1 - None (T - Not assessable [intubated]) (M)otor response (Maximum = 6) 6 - Obeys commands for movement 5 - Localizes to pain 4 - Withdraws from pain 3 - Flexion in response to pain (decorticate posturing) 2 - Extension in response to pain (decerebrate posturing) 1 - None Use best response for each category (range = 3-15). Coma: Does not open eyes, does not follow commands, and does not utter understandable words; Glasgow Coma Score (GCS) 3-8. Head injury classification: Mild, GCS 13-15; moderate, GCS 9-12; severe, GCS ≤8. ---------- Normal pupils are 2-6 mm in diameter from hurst and Uworld is 3-5 mm Positive Babinski: when toes fan out when you stroke it normal for infants up to 1 yr if they do, it means theres a nervous system problem Know this thing above^^^^^^^^^^^^^^^ Lumbar puncture: The site will be at the lumbar subarachnoid space o Purpose is to attain spinal fluid to analyze for infecetion, tumor Reduce CSF Measure Pressure readings o Position: Fetal postion o Nursing Consideration: Be sure to inspect the puncture site so its clean Spinal fluid should look clear like water Post procedure: they should lie flat or prone 4-8hrs Increase fluids o Complication: Common one is headache: bed rest, fluids, pain meds and BLOOD PATCH Increases when they are sitting up Decreases when they are lying down Brain herniation: if you even think, they are having ICP, tell the doctor because when the needle is inserted, the brain will pull down and it will cut supply to the brain Ischemia Infected lesions on the puncture site can cause meningitis Lumbar puncture is contraindicated if you have ICP Increased intercranial pressure: o S/S: Early signs: o Change in LOC o Change in attention span or even coma o Slurred speech o Delay in response in verbal commands o Increase in drowsiness o Restlessness o Confusion Late signs: o Change in LOC o Progressing tto stupor o Coma o Vital sign changes o Cushing triad immediate intervention Systolic hypertension with a WIDENING PULSE SLOW, AND BOUNDING PULSE IRREGULAR RESPIRATIONS Cheyne-stokes o Decerebrate and decorticate they are burning calories a lot Remembering DeCORticate: is towards the core of your body Remembering Decerebrate: away from you body this one is more dangerous Cushing's triad is related to increased intracranial pressure (ICP). Early signs include change in level of consciousness. Late signs include bradycardia, increased systolic blood pressure with a widening pulse pressure(difference between systolic and diastolic), and slowed irregular (Cheyne-Stokes) respirations. o ANYTIME A PERSON HAS A HEADACHE, THINK ICP IS GOING UP Same thing with PROJECTILEE VOMITITNG Anytime you have a fast or acute bleeding in your head, ICP will go up, whether be stroke, head injury, cerebral anyreusm o MISCELENOUS SIGNS: Changes in pupils Projectile vomiting o Complications for ICP: Brain herniation Obstructs blood flow DI and SIADH o Treatment: reduce cerebral edema by maintaining maintain cerebral perfusion Short term drugs o Avoid hypotension/bradycardia o Give oxygen o Isotonic saline o Norepinephrine o Dobutamine: (short term drug) Long term Keep temp below <100.4 Elevate head of bed (high fowlers) Watch ICP while turning but its supposed to come down within 15 min Avoid o restraints o Avoid bowel and bladder distention o Hip o Valsalva o No nose o Limit suctioning and coughing o No isometric Use osmotic diuretics mannitol decreases ICP FLUID RESTRICTION ICP medication: Mannitol (osmotic diuretic)-crystallizes at room temp so ALWAYS use filter needle Meningitis: inflammation of the brain Caused by viral or bacterial It can also be caused by a lumbar puncture Make sure client is on Droplet precautions!! o S/S: Chills and high fever Severe headache Disorientation that can become into a coma Nuchal rigidity (stiff neck) N/V Photophobia Seizures Positive Kernig (Severe stiffness of hamstring) and Brudzinski (sever neck stiffness causes hips and knees to flex neck is flexed) o Treatment: Corticosteroids Antibiotic: if its bacterial Analgesics Anticonvulsants: if seizures are present -------- Contusions: o Seen with acceleration and deceleration o Brain is bruised and damaged Hematomas: A small hematoma that develops rapidly is more fatal than a large hematoma that develops slowly ICP will go up Epidural Hematoma: Rupture or laceration of the middle EMERGENCY o Treatment: Burr holes: to remove, clot stop the bleeding and control the ICP Subdural Hematoma: Collection of blood between the dura and brain o Classifications: o Acute: means fast o Sub-acute: means medium o Chronic: means slow tricky one b/c it imitates other conditions. Sometimes we think he’s drunk!! Things can happen after a month Here, they bleed inside but it compensates till the body can’t handle o Treatment: Immediate Craniotomy: to remove clot and control ICP --- Concussion: Temp loss of neuro function with complete recovery key here is no obvious damage o Client Education: Teach client to come back to the hospital if these occur: Difficulty Awakening*** Speaking Confusion Severe headache Vomiting Pulse changes Unequal pupils One sided weakness ^^^^^^All of these are signs of ICP going UP meaning its not just a concussion anymore!!!!!!!!! -------- Autonomic dysreflexia/Hyper-reflexia: life threatening emergency that occurs above the level of T6 EMERGENCY - If not treated, hypertensive Stroke can occur o S/S: sudden onset Severe hypertension Headache Bradycardia Nasal stuffiness Flushing and sweating Especially on the forehead Blurred vison Nausea Anxiety o Causes: Distended bladder****** Constipation or impaction Stimuli to the skin place client in sitting position (elevate HOB) first before any other implementation. o Treatment: place client in sitting position (elevate HOB) first before any other implementation. Sit up to lower BP Semi fowlers Insert catheter Remove impaction Alleviate skin pressure even a cold breeze Antihypertensive: if the BP remains high after stimuli has been removed Teach preventive measures Management of Care: LISTEN TO MARK FOR THIS!! - 5 rights of delegation/Assignment: Right task: Right Circumstances Right person Right direction or communication Right supervision and evaluation & feedback o UAP: Right task can perform tasks on Stable clients Routine, simple and Repetitive: feeding, hygiene, I &O, routine vital signs and ambulation’s CANNOT let UAP take vital signs for a client who’s receiving blood, IV dopamine, or IV nitro UAP cannot get a urine specimen from a catheter: that is a sterile procedure UAP can do some enemas BUT NOT medicated enemas o LPN: Think what a nursing student can do!! Can ONLY do stable clients LPN’s cannot do tasks that involve assessments or evaluation LPN cannot do any sort of evaluation CANNOT develop a plan of care Can do data collection Updates client data Can NOT do IV PAIN MEDS They can monitor blood transfusion BUT CANNOT ADMINISTER Can implement task: treatments, administer meds, and fingerstick, and suction They can monitor and reinforce, AND calculate o Unstable clients include: Low Blood sugar Sudden changes of nuero checks No admission Client who is returning from a procedure ANYTIME you see acid-base imbalance, they are always unstable COPD client is stable Acute is unstable Critical Thinking: Clients with AIDS/HIV have to be in different rooms Try thinking like the next nurse isn’t as bright aka dumb so would you really give a partial thickness burn patient (open wound) to a dumb nurse who is taking care of an HIV (contagious) person. What if the dumb nurse doesn’t wash his/her’s hand? Management Care: LPNs don’t do Triage (Assessment) Nonmaleficence is best illustrated with the nurse’s action, as the goal is to do no harm to the client. With timely reporting of an error, further complications may be prevented. Beneficence : refers to doing good. This may include compassion and kindness. Justice : refers to equitable distribution of resources. Triage in the ED is one action that illustrates justice. Fidelity : refers to truth-telling. If the client were to ask if a medication error was made, the nurse would answer yes to the question as a way of demonstrating fidelity NO BROCHURE = when family expresses fear for something don’t encourage/promote it. Even if it’s good, it’s not the right time. FLUIDS near bedside = juices, LPN do NOT mess with IV Do NOT delegate infections that are contagious and Newly admitted patients with crazy syndromes to a Floating nurse. POST CARDIAC CATH is fine to delegate when no S:S ( OB to MED ) Pancreatitis: Back pain , Fever, TACHY, Bruising on the umbilical. Morphine no good- give Demerol. AAA- S/S Do NOT include SOB & Hoarseness. Watch out for pulsation, Abdominal Bruit Thoracic aneurysm : Hoarseness, back pain and SOB are present. CARE for ICP and hemorrhage: clients with increased intracranial pressure need the head placed midline to facilitate cerebral drainage. Placing the client on the right side would not be performed while the drain remains in place. POST-OP- IF patients health is declining, high chances of CALL HCP Guillain-Barre’ Syndrome- is an acute, rapidly progressing, and potentially fatal form of polyneuritis. It is characterized by ascending, symmetric paralysis affecting the cranial and peripheral nerves. Signs and symptoms include paresthesia, hypotonia, areflexia, muscle aches, cramps, orthostatic hypotension, hypertension, bradycardia, facial flushing, facial weakness, dysphagia, and respiratory distress. Myasthenia Gravis: worsens with exercise and improves with rest These are three of the primary symptoms of myasthenia gravis. The muscles of the head and neck are weak and have difficulty holding the head up. Facial paralysis occurs and drooping of the eyelids develops as the client’s muscles get tired. The main symptom is weakness in the voluntary skeletal muscles, which are muscles under your control Huntington’s disease: Writhing, twisting movements of the face, limbs, and body is known as chorea Buerger’s diseas: Tingling, numbness and cool feet are expected findings. These signs/symptoms are typical of this disorder. The disease is characterized by inflammation in the arteries that results in a vaso-occlusion type phenomenon. The claudication, with symptoms described here, can quickly progress to a critical degree of limb ischemia. As it progresses, revascularization may not be possible, and amputation may be the only viable option. This is seen almost exclusively in heavy smokers or those who use other forms of tobacco. Medications are not generally helpful, so stopping tobacco use is basically the only way to stop the progression of this disease. Changes associated with menopause, with its dramatic decline in estrogen, include loss of muscle mass, increased fat tissue leading to thicker waist, dryness of the skin and vagina, hot flashes, sleep abnormalities, and mood changes. [Show More]
Last updated: 1 year ago
Preview 1 out of 106 pages
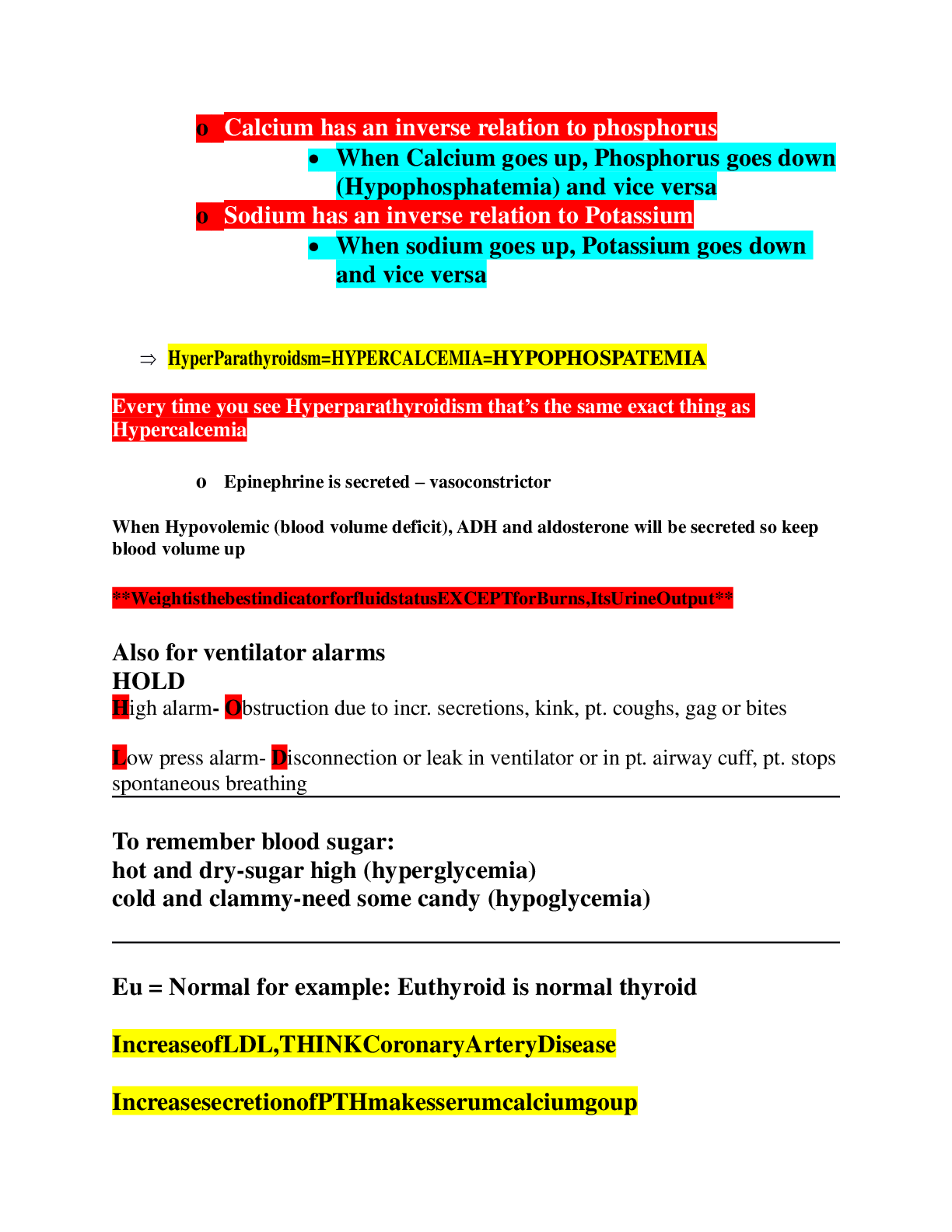
Also available in bundle (1)
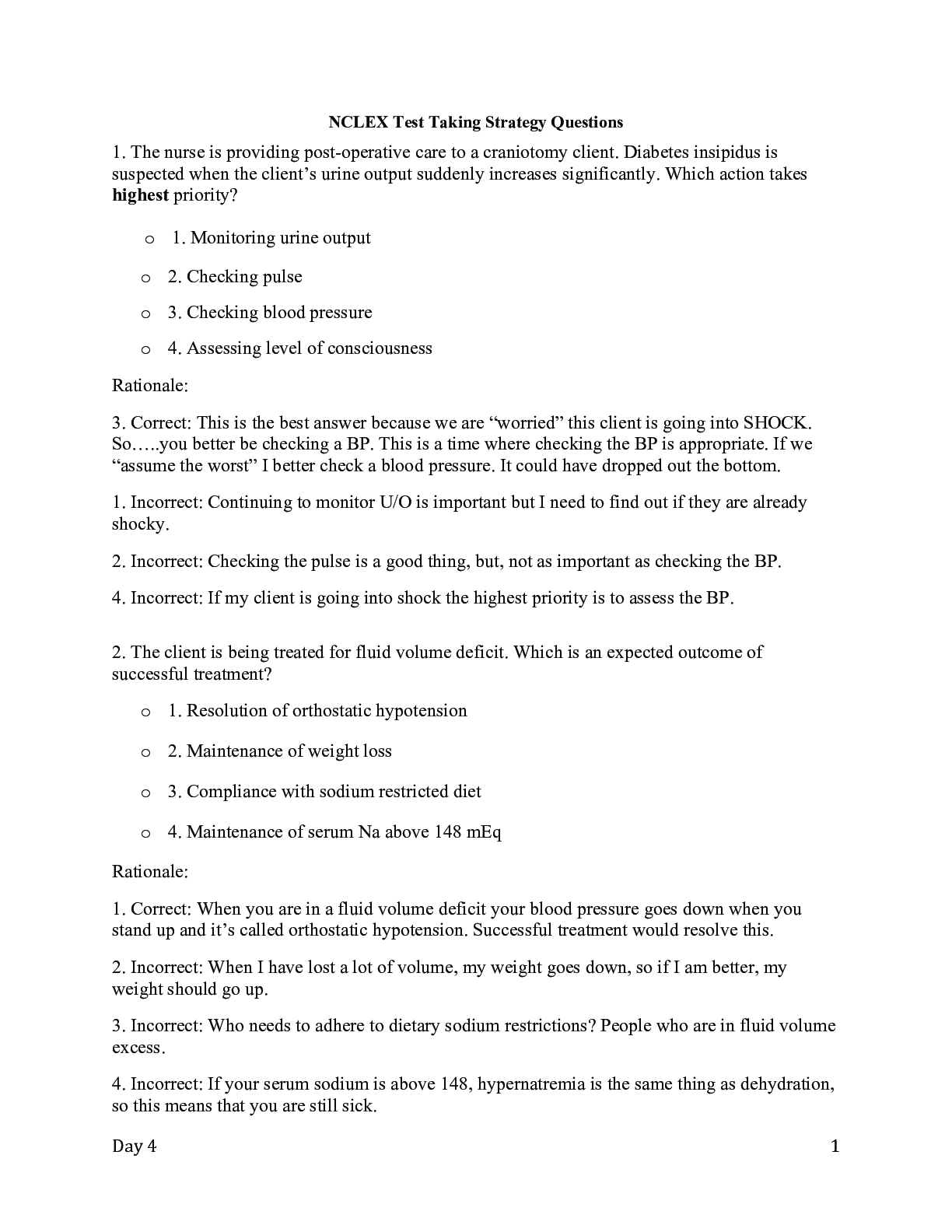
Hurst Review NCLEX RN Exam Files With Rationale And a PDF BOOK
Hurst review Nckex RN Files
By Good grade 1 year ago
$28.5
5
Reviews( 0 )
Recommended For You
*NURSING> EXAM > ENPC Test Questions & Answers (All)
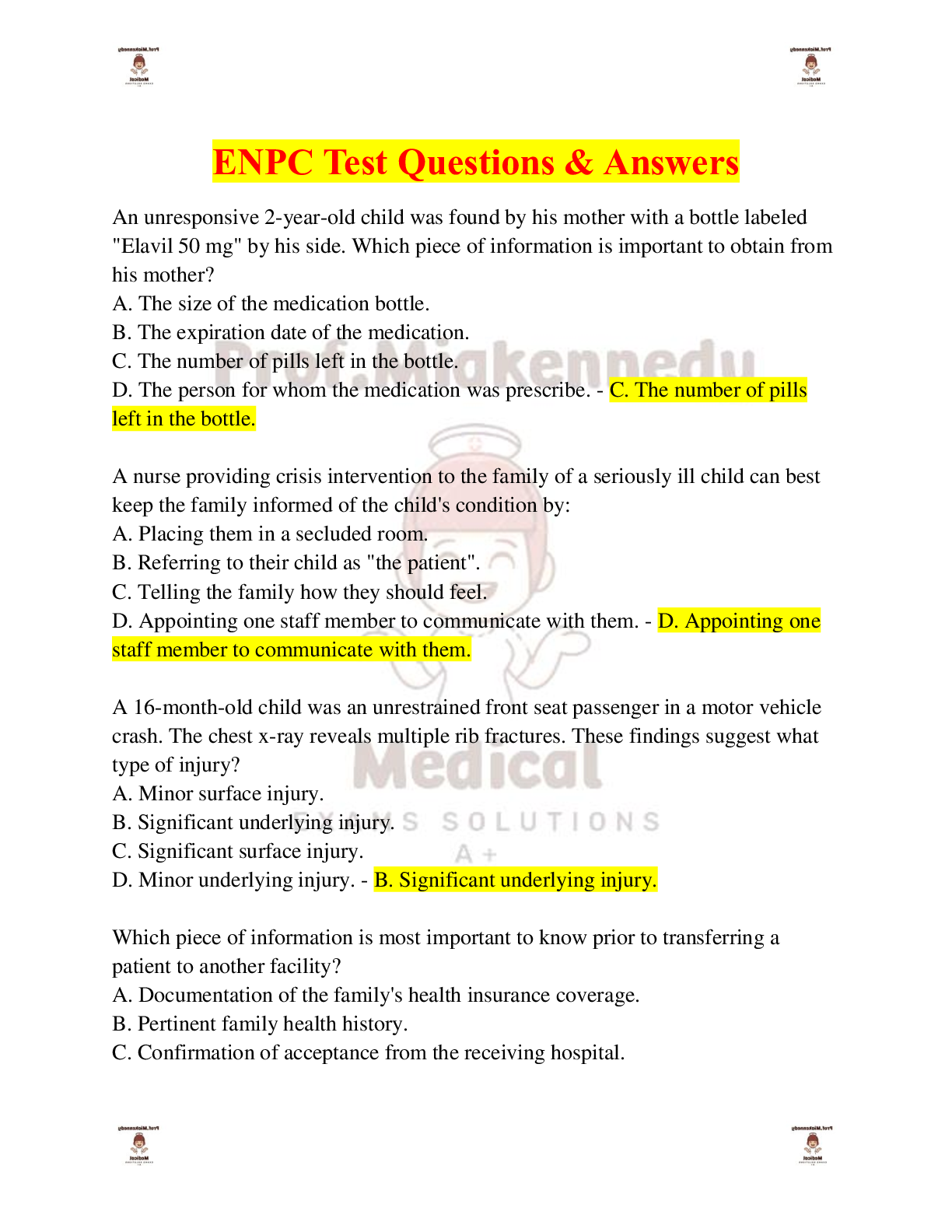
ENPC Test Questions & Answers
ENPC Test Questions & Answers-An unresponsive 2-year-old child was found by his mother with a bottle labeled "Elavil 50 mg" by his side. Which piece of information is important to obtain from his moth...
By PROF , Uploaded: Apr 25, 2024
$9.5
Religious Studies> EXAM > CWV TOPIC 2 QUIZ. QUESTIONS AND ANSWERS LATEST UPDATED. (Score 100%) (All)
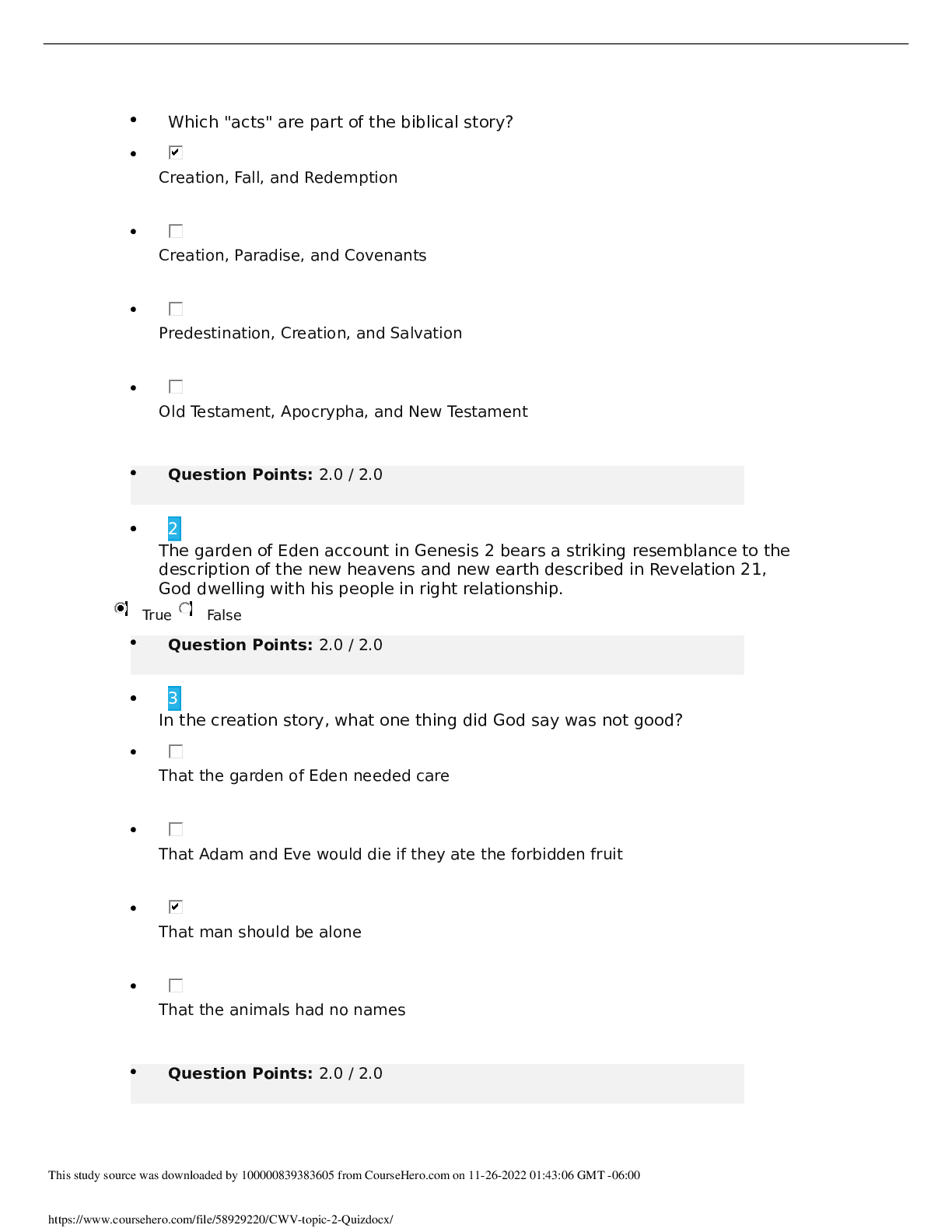
CWV TOPIC 2 QUIZ. QUESTIONS AND ANSWERS LATEST UPDATED. (Score 100%)
CWV TOPIC 2 QUIZ QUESTIONS AND ANSWERS LATEST UPDATED
By ELIANA , Uploaded: Aug 01, 2022
$9
ATI MED SURG PROCTORED> EXAM > Med Surg ATI Proctored Exam Test Bank 2023/2024 With NGN (All)
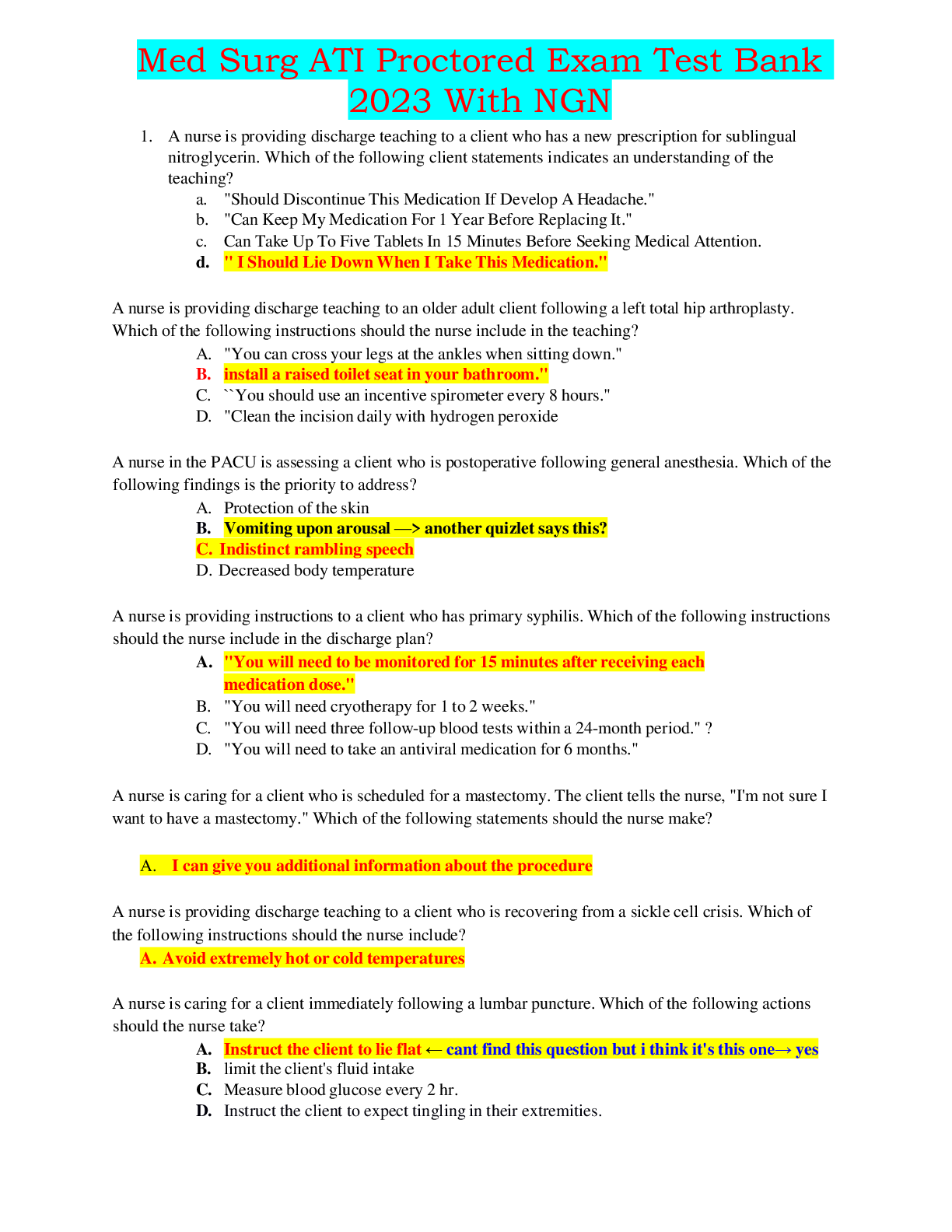
Med Surg ATI Proctored Exam Test Bank 2023/2024 With NGN
Med Surg ATI Proctored Exam Test Bank 2023/2024 With NGN Med Surg ATI Proctored Exam Test Bank 2023/2024 With NGN Med Surg ATI Proctored Exam Test Bank 2023/2024 With NGN Med Surg ATI Proctored E...
By EXAMHUB SOLUTIONS , Uploaded: Apr 15, 2024
$30.5
NURSING.> EXAM > ATI RN CUSTOM; MENTAL HEALTH NEXT GEN (All)
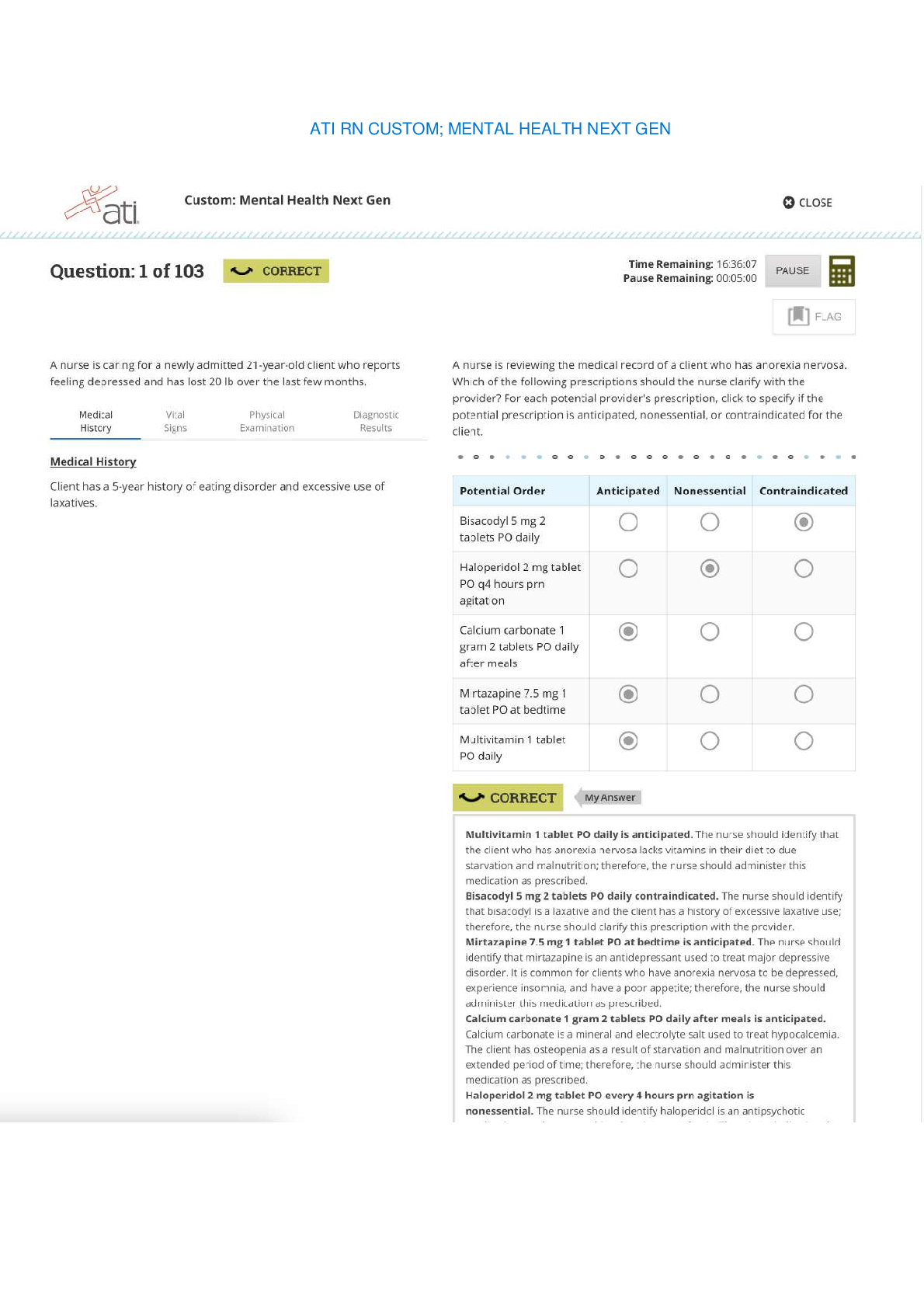
ATI RN CUSTOM; MENTAL HEALTH NEXT GEN
ATI RN CUSTOM; MENTAL HEALTH NEXT GEN ATI RN CUSTOM; MENTAL HEALTH NEXT GEN ATI RN CUSTOM; MENTAL HEALTH NEXT GEN ATI RN CUSTOM; MENTAL HEALTH NEXT GEN ATI RN CUSTOM; MENTAL HEALTH NEXT GE...
By EXAMHUB SOLUTIONS , Uploaded: Apr 05, 2024
$45.5
ATI Med Surg> EXAM > RN ATI MED SURG ALTERATIONS IN KIDNEY FUNCTION AND ELIMINATION ASSESSMENT. (All)
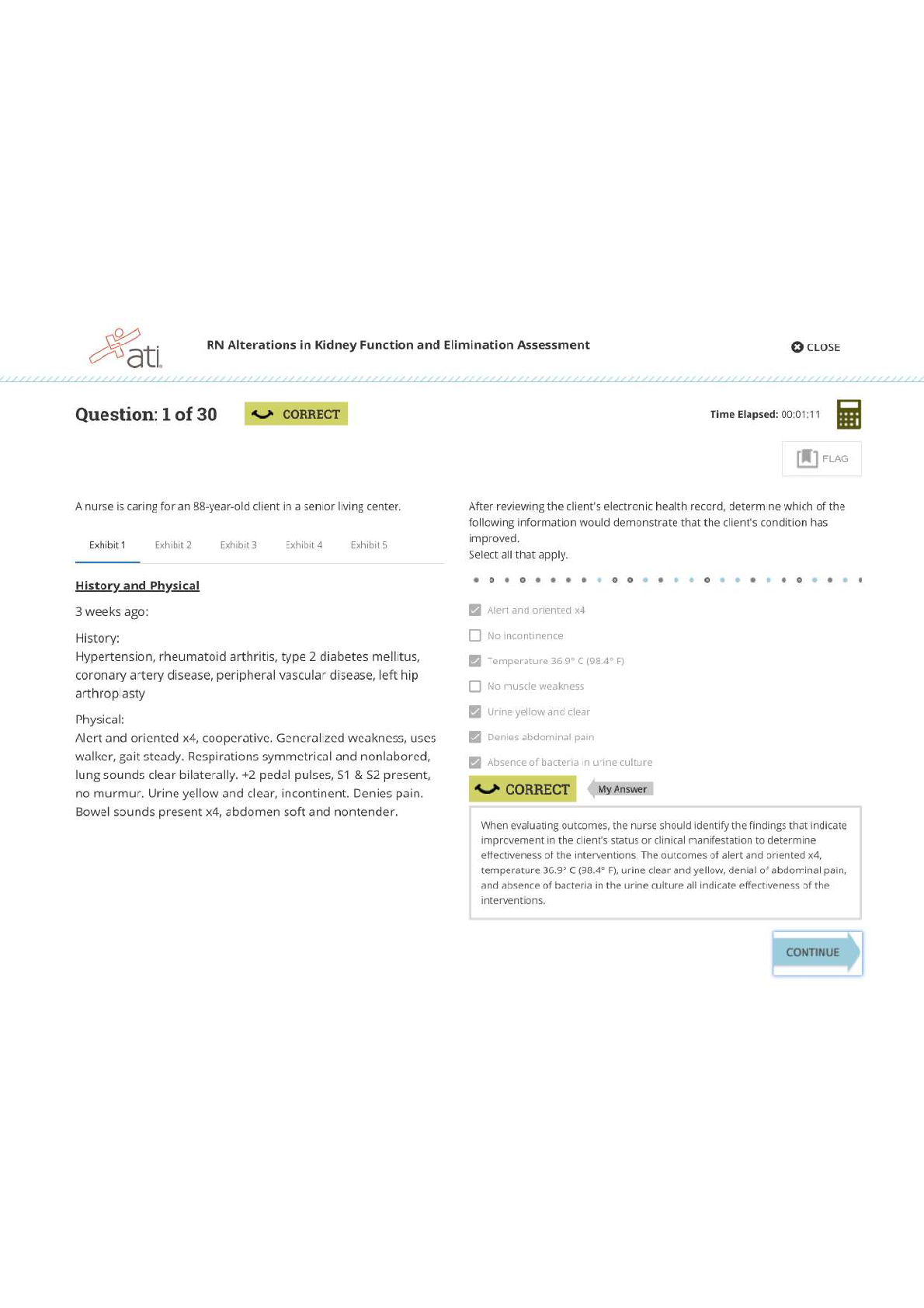
RN ATI MED SURG ALTERATIONS IN KIDNEY FUNCTION AND ELIMINATION ASSESSMENT.
RN ATI MED SURG ALTERATIONS IN KIDNEY FUNCTION AND ELIMINATION ASSESSMENT. RN ATI MED SURG ALTERATIONS IN KIDNEY FUNCTION AND ELIMINATION ASSESSMENT. RN ATI MED SURG ALTERATIONS IN KIDNEY FUNCTI...
By EXAMHUB SOLUTIONS , Uploaded: Apr 10, 2024
$28.5
Nutrition> EXAM > Nutrition Through the Life Cycle EXAM 2. 50 Questions & Answers. (Score 100%) (All)
Nutrition Through the Life Cycle EXAM 2. 50 Questions & Answers. (Score 100%)
Nutrition Through the Life Cycle EXAM 2 Latest
By Academic mines , Uploaded: Apr 27, 2023
$10
*NURSING> EXAM > NGR 6172 Pharm Midterm Exam- Questions and Answers. Score 98% (All)
NGR 6172 Pharm Midterm Exam- Questions and Answers. Score 98%
NGR 6172 Pharm Midterm Exam- Questions and Answers GRADED A-1). A patient who takes daily doses of aspirin is scheduled for surgery next week. The nurse should advise the patient to: a. continue to...
By PROF , Uploaded: Feb 01, 2022
$11
Philosophy> EXAM > PHL 200 Intro to Ethics Unit 3 - Score 100% (All)
PHL 200 Intro to Ethics Unit 3 - Score 100%
PHL 200 Intro to Ethics Unit 3 For a utilitarian, which consideration is most important? Why is utilitarianism an objectivist or relativist theory? Which of the following considerations is important f...
By Ajay25 , Uploaded: Jan 04, 2022
$8
Philosophy> EXAM > PHL 200 Intro to Ethics Unit 2 -Score 100% (All)
PHL 200 Intro to Ethics Unit 2 -Score 100%
PHL 200 Intro to Ethics Unit 2 Which of the following statements about divine command theory is true? Norman learns from his pastor that God commands people to love one another. Thus according to divi...
By Ajay25 , Uploaded: Jan 04, 2022
$8
Philosophy> EXAM > PHL 200 Intro to Ethics Unit Final. Score 100% (All)
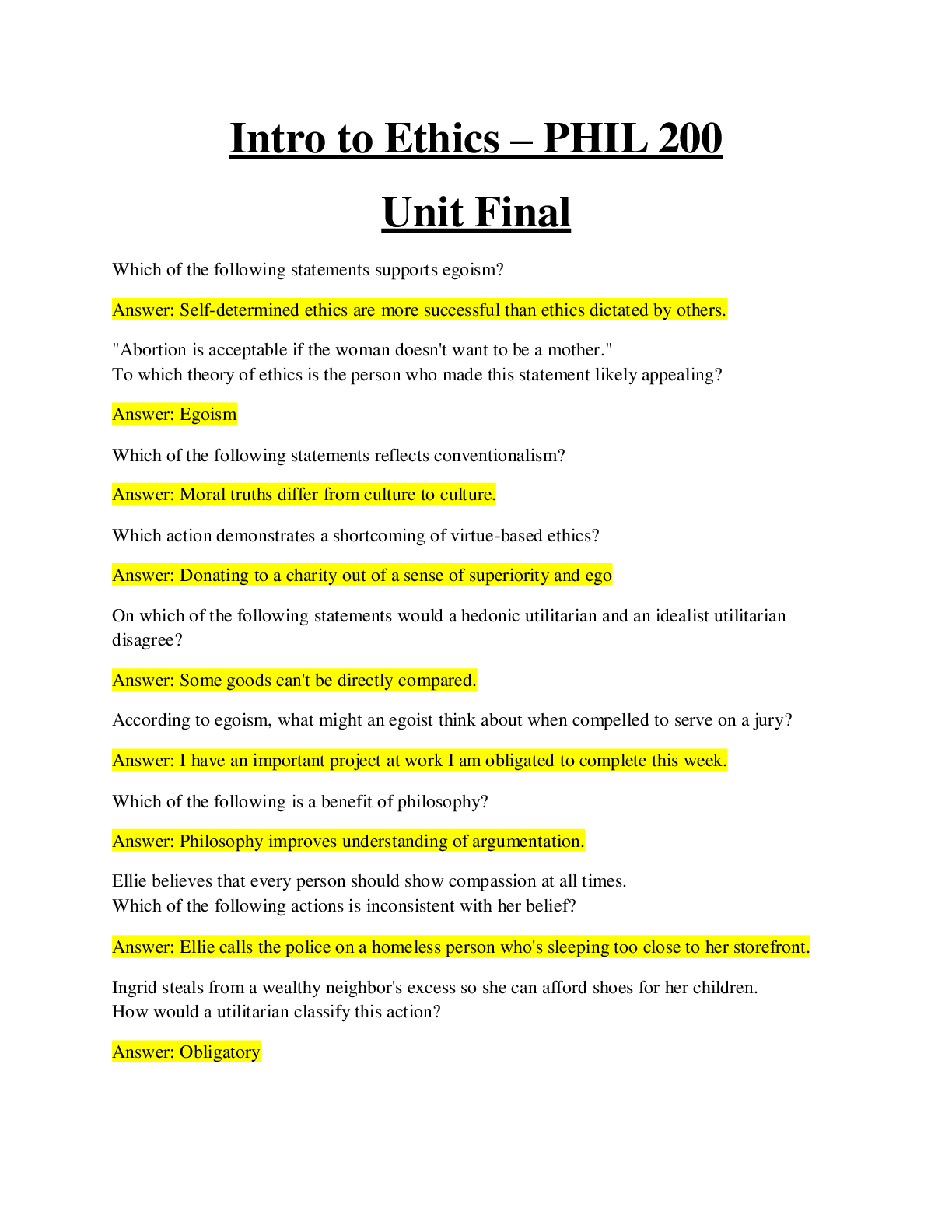
PHL 200 Intro to Ethics Unit Final. Score 100%
PHL 200 Intro to Ethics Unit Final Which of the following statements supports egoism? "Abortion is acceptable if the woman doesn't want to be a mother." To which theory of ethics is the person who mad...
By Ajay25 , Uploaded: Jan 04, 2022
$8
Document information
Connected school, study & course
About the document
Uploaded On
Jul 06, 2022
Number of pages
106
Written in
Additional information
This document has been written for:
Uploaded
Jul 06, 2022
Downloads
0
Views
83