NREMT Cognitive Exam updates 2022 Questions and Answers Grade A+
Document Content and Description Below
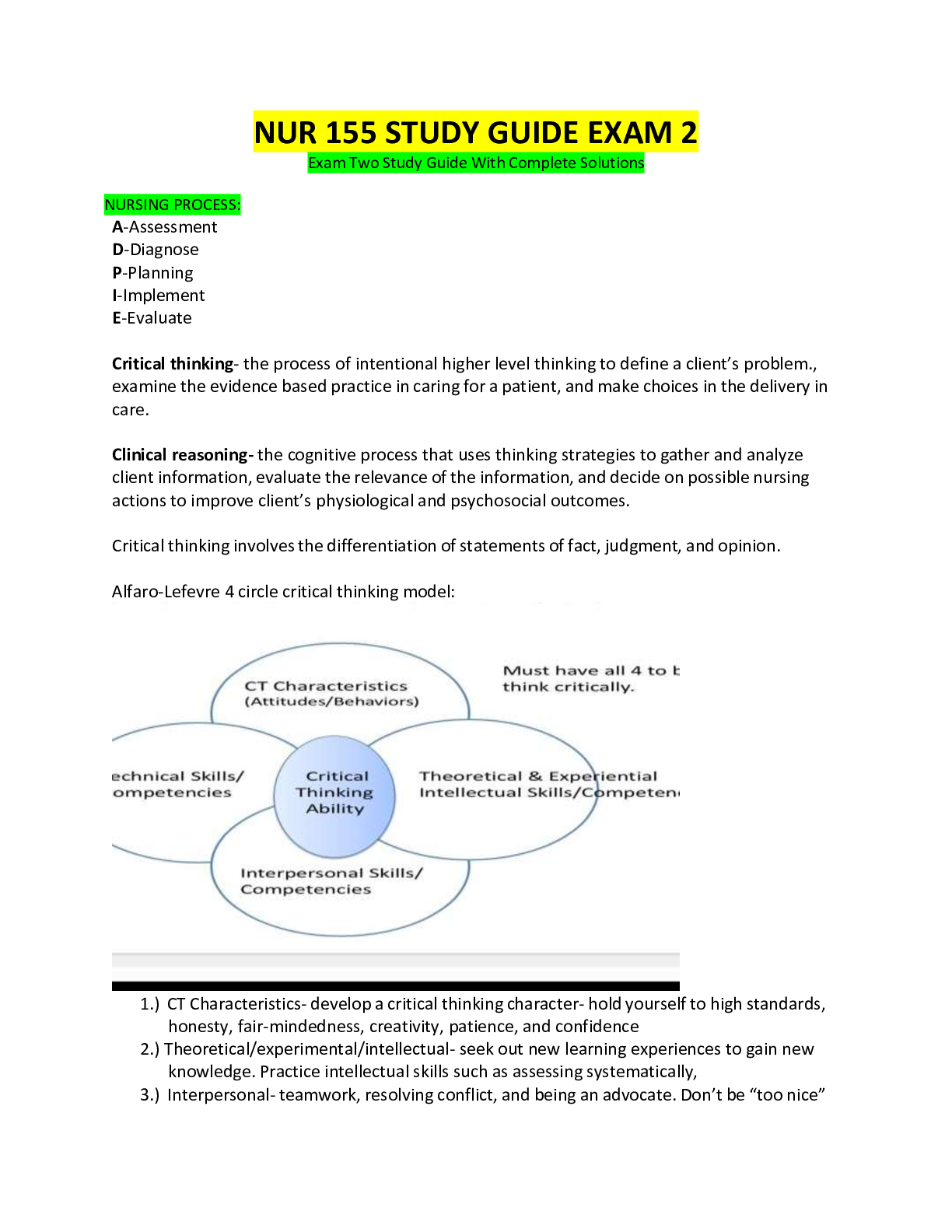
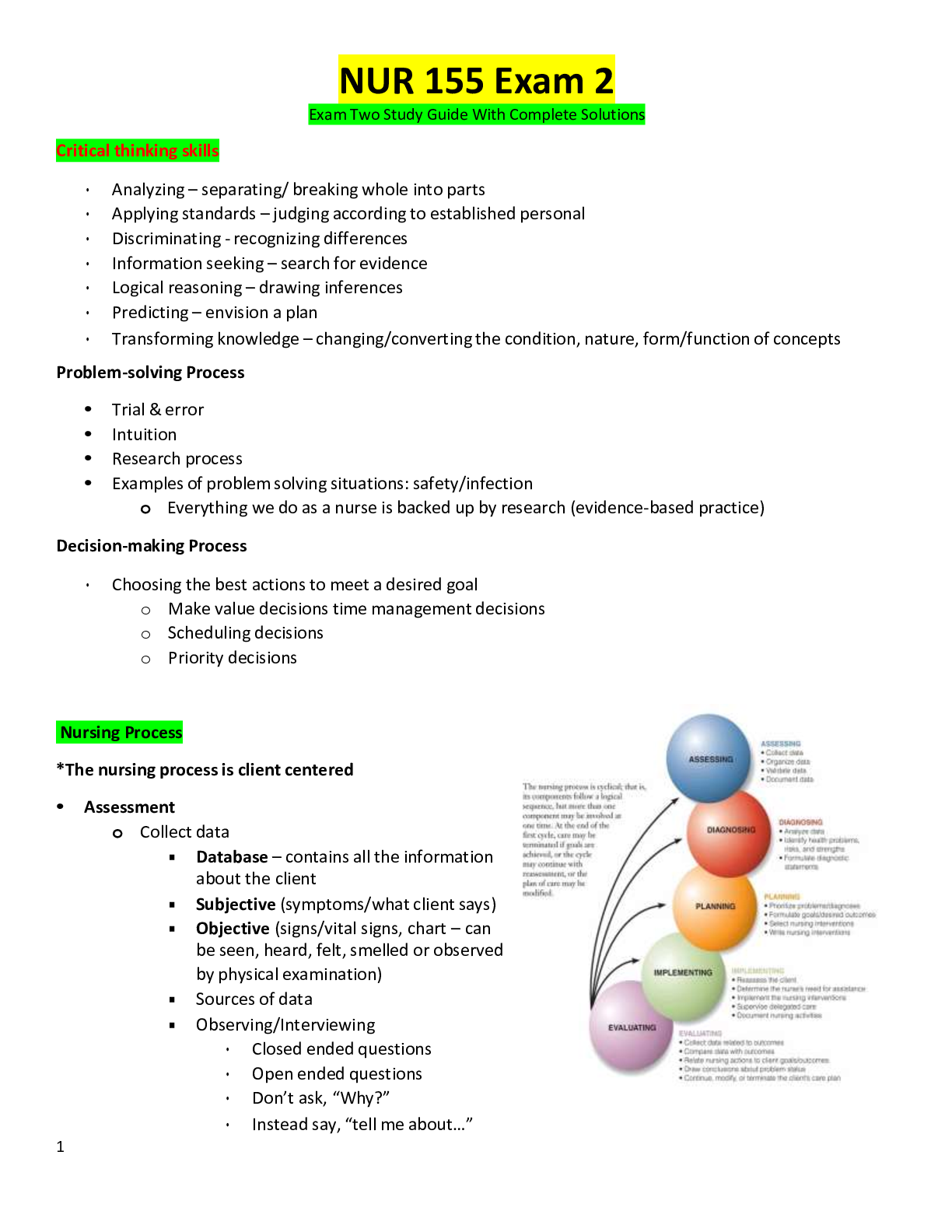
NREMT Cognitive Exam updates 2022 Questions and Answers Grade A+ Where does the modern EMS system have its origin? {{Ans- The modern EMS system has its origins in funeral homes, which often operate... d ambulances. However, funeral home operators were often serving competing business interests and patients received little trained care until the hospital. What is considered the "birth" of EMS? {{Ans- In 1966, a paper titled "Accidental Death and Disability: The Neglected Disease of Modern Society" is published by the National Academy of Sciences. This paper is widely known in the EMS profession as the White Paper. The White Paper is widely considered the birth of modern EMS. It spotlighted inadequacies of prehospital care in the United States, particularly related to trauma. Who developed the first EMT National Standard Curriculum? {{Ans- Early in the 1970s, the US Department of Transportation developed the first EMT National Standard Curriculum. What are the levels of EMS training? {{Ans- Emergency Medical Responder (EMR): provides basic, immediate care including bleeding control, CPR, AED and emergency childbirth. Emergency Medical Technician (EMT): includes all EMR skills, advanced oxygen and ventilation skills, pulse oximetry, noninvasive blood pressure monitoring, and administration of certain medications. Advanced Emergency Medical Technician (AEMT): includes all EMT skills, advanced airway devices, intravenous and intraosseous access, blood glucose monitoring, and administration of additional medications. Paramedic: includes all preceding training levels, advanced assessment and management skills, various invasive skills, and extensive pharmacology interventions. This is the highest level of prehospital care outlined in the National EMS Education Standards. What are EMT roles and responsibilities? {{Ans- Equipment preparedness Emergency vehicle operations Establish, maintain scene safety Patient assessment and treatment Lifting and moving Strong verbal and written communication skills Patient advocacy Professional development Quality improvement Illness and injury prevention Maintain certification/licensure What is the role of the medical director? {{Ans- The medical director is a physician responsible for providing medical oversight. The medical director oversees quality improvement. What are the two types of medical direction? {{Ans- Online medical direction: direct contact between the physician and EMT via or radio. Offline medical direction: written guidelines and protocols. What is an EMT's first priority? {{Ans- The EMT's first priority is always his or her own safety. Scene safety is always the top priority! The EMT's safety priorities after personal safety are for his/her partner(s), patients and bystanders. What are the types of stress? {{Ans- Acute stress: an immediate physiological and psychological reaction to a specific event. Delayed stress: a stress reaction that develops after the stressful event. It does not interfere with the EMT's ability to perform during the stressful event. PTSD is an example of delayed stress. Cumulative stress: the result of exposure to stressful situations over a prolonged period of time. What are the stages of grief? {{Ans- Denial Anger Bargaining Depression Acceptance How can you prevent the risk of infection? {{Ans- Immediately report exposures to the designated infection control officer. Handwashing is the single most important way to prevent the spread of infection. Hand sanitizers can be effective, but soap and water is preferred when available. What are the two types of PPE? {{Ans- Minimum PPE: gloves and eye protection should be used during any patient contact situation. Expanded PPE: use disposable gown and mask for significant contact with any body fluid--for example, during childbirth. Use a high-efficiency particulate air (HEPA) mask o N-95 respirator for suspected airborne disease exposure, such as tuberculosis. What are emergency moves? {{Ans- These are used when the scene is dangerous and the patient must be moved before providing patient care. Types of emergency moves include the armpit-forearm drag, shirt drag, and blanket drag. What is an urgent move? {{Ans- Used when the patient has potentially life-threatening injuries or illness and must be moved quickly for evaluation and transport. Rapid extrication: an urgent move used for patients in a motor vehicle; it requires multiple rescuers and a long backboard. The patient is rotated onto a backboard with manual cervical spine precautions and removed from the vehicle. What are non-urgent moves? {{Ans- Used when there are no hazards and no life-threatening conditions are apparent. Types of non-urgent moves include direct ground lift, extremity lift, direct carry method, and draw sheet method. What is the log roll technique? {{Ans- Commonly used to place a patient on a backboard or assess the posterior. Can be done while maintaining manual cervical spine precautions. Should have at least three trained personnel. The person controlling manual cervical spine protection should direct the log roll. What are special considerations for bariatric patients? {{Ans- Obese patients pose additional challenges and risks to providers during lifting and movement. Some EMS systems have special bariatric ambulances with specialized equipment, automated lifting systems, and wider stretchers capable of a greater weight capacity. What is supine hypotensive syndrome? {{Ans- Patients in the later stages of pregnancy should not be placed supine due to the risk of supine hypotensive syndrome. Place the pregnant patient on her left side. If patient has potential cervical spine trauma, tilt backboard to the left about 20 degrees. When can patients be restrained? {{Ans- In general, patients may be forcibly restrained if they pose a significant, immediate threat to you, your partner, or others. Restraining a patient against his will is a last resort. Anticipate and plan. Request law enforcement assistance. Contact medical direction when possible. Guidelines for restraining a patient: -Get additional help whenever possible; at least 4 people is recommended. -Use the minimum amount of force necessary to protect yourself, the patient and others. -Secure patient supine, with backboard if available. DO NOT secure the patient in a prone position. -Use soft, padded restraints. -Monitor the patient's level of consciousness, airway, and distal circulation continuously. -Thoroughly document the reason for restraining the patient, the method of restraint, the duration of restraint, and frequent reassessment of the patient while restrained. What is the use of force doctrine? {{Ans- The EMT must act reasonably to prevent harm to a patient being forcibly restrained. The use of force must be protective, not punitive. What is scope of practice? {{Ans- Scope of practice outlines the actions a provider is legally allowed to perform based on his or her license or certification level. Scope of practice is tied to the licensure or certification, not the individual's knowledge or experience. Each state determines the scope of practice for its EMS providers. What is standard of care? {{Ans- Standard of care is the degree of care a reasonable person with similar training would provide in a similar situation. Standard of care requires EMTs to competently perform the indicated assessment and treatment within their scope of practice. What are sources that help establish standard of care? {{Ans- National EMS Education Standards State protocols and guidelines Medical direction EMS agency's policies and procedures Reputable textbooks Care considered acceptable by similarly trained providers in the same community. What is informed consent? {{Ans- Informed consent is required from all patients who are alert and competent. -Patient must be informed of your carer plan and associated risks of accepting or refusing care and transport. -Patient must be informed of, and understand, all information that would impact a reasonable person's decision to accept or refuse care and transport. What is expressed consent? {{Ans- Expressed consent also requires that the patient be alert and competent to give expressed consent. Expressed consent can be given verbally or nonverbally. -Expressed consent is similar to informed consent, but not usually as in-depth as informed consent. -Expressed consent is often used to obtain consent for more basic assessments or procedures. What is implied consent? {{Ans- Implied consent allows assumption of consent for emergency care from an unresponsive or incompetent patient. -Patients might be incompetent for many reasons, such as alcohol, drugs, head injury, hypoxia, hypoglycemia, or mental incompetency. -Implied consent can be used to treat a patient who initially refused care but later loses consciousness or becomes otherwise incapacitated. What is minor consent? {{Ans- Minors are not competent to accept or refuse care. -Consent is required from a parent or legal guardian. Implied consent can be used when unable to reach a parent or guardian and treatment is needed. -Minor consent is not required for emancipated minors. Criteria for emancipation varies but usually includes minors who are married or pregnant, already a parent, a member of the armed forces, financially independent, or emancipated by the courts. What is involuntary consent? {{Ans- Involuntary consent is used for mentally incompetent adults or those in custody of law enforcement. Consent must be obtained from the entity with the appropriate legal authority. What are advance directives? {{Ans- Advance directives are written instructions, signed by the patient, specifying the patient's wishes regarding treatment and resuscitative efforts. There are several types of advance directives. -Do Not Resuscitate (DNR): DNRs are specific to resuscitation efforts and do not affect treatment prior to the patient entering cardiac arrest. -Living will: Living wills are broader than DNRs. They address health care wishes prior to entering cardiac arrest. This may include use of advanced airways, ventilators, feeding tubes, etc. How do Good Samaritan Laws affect EMTs? {{Ans- Good Samaritan laws are designed to protect someone who renders care as long as he or she is not being compensated and gross negligence is not committed. -Each state has some form of Good Samaritan laws. Some protect health care providers, but some do not. -Some states extend their Good Samaritan law to publicly employed EMS providers but not to those in the private sector. What is assault? {{Ans- A person can be guilty of assault even if another person only perceived that they intended to inflict harm. Physical contact is not required to be guilty of assault. [Show More]
Last updated: 1 year ago
Preview 1 out of 67 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 24, 2022
Number of pages
67
Written in
Additional information
This document has been written for:
Uploaded
Jun 24, 2022
Downloads
0
Views
125

 RN HESI EXIT EXAM VERSIONS TEST BANK.png)