General Questions > EXAM > Questions NRP - Lessons 1-9 Answered 2022; Distinction Level Assignments for High fly learners. (All)
Questions NRP - Lessons 1-9 Answered 2022; Distinction Level Assignments for High fly learners.
Document Content and Description Below
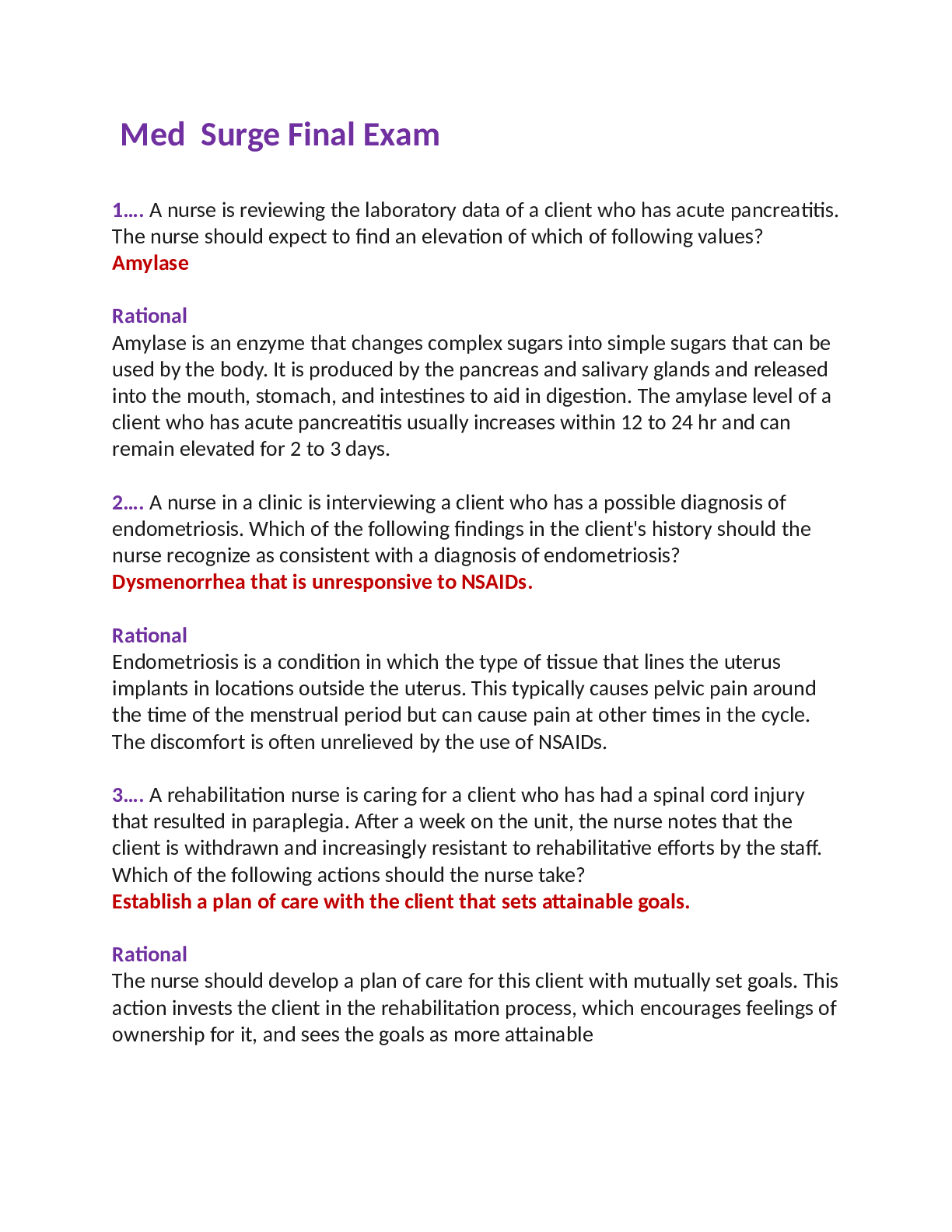
NRP Lesson Quizzes 1-9 2022 answered all correctly NRP Lesson 1 Quiz. After the initial steps in resuscitation, a newborn is apneic with a heart rate less than 100 beats per minute. What is the most i... mportant and effective action to take in the resuscitation of this baby? You are called to attend to a newborn at birth. Which 3 questions should you ask to help assess the need for resuscitation? A baby is born at 34 weeks gestation. Despite initial steps being taken, the baby is apneic and the heart rate is 70 beats per minute. What steps should be taken next? - A full term newborn is apneic after birth and fails to responds to tactile stimulation. Newborns in secondary apnea usually respond with an increase in heart rate after which intervention? Your hospital is staffed by several people skilled in neonatal resuscitation. Most of them have additional responsibilities aware from the delivery room, and you alone are called to the delivery area at this time. While extra people may be useful, when should you first start to recruit additional help? You have determined that a baby needs resuscitation at birth. What are the initial steps of resuscitation? Your hospital is planning NRP training and trying to decide who should be included. For every delivery, who should be available? A premature newborn is born depressed and requires ongoing respiratory support and chest compressions. You and 2 colleagues provide care immediately following birth. Which behavioral skills are critical to ensure successful and optimal care during resuscitation? After several hours of labor with failure to progress, a baby is born via cesarean section. The baby cries at birth and is vigorous, but appears slightly dusky at 2 to 3 minutes of age. How long may it take for this normal baby to achieve an oxygen saturation of 90% or greater? A prenatal closs is learning about labor and birth. Approximately _____% of newborns require some assistance to begin breathing at birth? A caregiver states that he can always predict which babies will need help at birth. You disagree because you know that _____ % of newborns require initial assessments to determine whether resuscitation is required. A newborn requires resuscitation, and you have begun positive-pressure ventilation and chest compressions. Which 3 signs are used to evaluate the effectiveness of your actions and the need to continue some aspect of support? Nrp lesson 2 You are at the resucitation of a newborn who is gasping and has a heart rate of 90 beats per minute. What is the most important action you can take? What is the best technique for removing secretions from the mouth and nose of a newborn who requires resuscitation? You are at a delivery of a newborn. Which of the following is an initial step in resuscitation? What is the best way to determine if a baby requires supplemental oxygen in the delivery room? What is the most effective maneuver to establish normal breathing in a baby with secondary apnea? Which statement accurately describes the role of oxygen in newborn resuscitation? – What is the appropriate technique to stimulate a baby to breathe? Which statement best describes normal transition physiology at time of birth? Which statement describes best practice when using a pulse oximeter? A baby is born with meconium stained amniotic fluid. The baby has normal muscle tone and respiratory effort and a heart rate of 120 beats per minute. What is the appropriate action? You are at a delivery of a baby born through meconium stained amniotic fluid. What is the correct indication for intubating and suctioning the trachea at birth? During the resuscitation of a newborn, you palpate the umbilical cord and count 10 beats over a 6 second period. What heart do you report to your team? NRP LESSON 3 You attend the birth of a newborn with another caretaker. The baby is born limp and apneic. Despite initial steps, you are required to provide the newborn with positive-pressure ventilation. At the same time, your team member should A baby is apneic, and has a heart rate less than 100 beats per minute. You have provided positive pressure-ventilation for 30 seconds. What are the signs that positive-pressure ventilation has been effective and may be discontinued? A full term newborn is apneic at birth and requires positive-pressure ventilation. What concentration of oxygen should be used during resuscitation? You attend the birth of a neonate at 30 weeks' gestation who needs respiratory support. A preterm newborn has respiratory distress after birth. Her heart rate is above 100 beats per minute, but she appears dusky. A team member has placed an oximeter on the baby's right hand; it is providing a reading as you administer supplemental oxygen. What level of oxygen saturation should you try to achieve? What are the first steps you should take to correct possible problems? What is the most important indicator of successful positive-pressure ventilation? A full-term baby is born following an emergency cesarean delivery for non-reassuring fetal heart rate patterns. The baby is apneic at birth, despite tactile stimulation. What is the single most important and effective step in resuscitation of this newborn? - A baby is born in the hospital lobby as his mother waited for admission. He is apneic, despite tactile stimulation, drying, and bulb suctioning. You have brought a self-inflating bag to the birth. What should your next step be? - What features of these two devices differ, making you consider using the T-piece resuscitator instead of the flow-inflating bag? You are part of a team resuscitating a premature newborn. Shortly after birth, the baby developed apnea, followed by bradycardia. Positive-pressure ventilation with a bag-and-mask has not resulted in an improvement. You communicate to the team that you remember potential corrective steps, using the acronym MR SOPA. Despite taking the first 4 corrective steps, M-R-S-O, there is still no chest rise. You recommend that your team now consider the final 2 steps. What are the final 2 corrective steps in the acronym MR SOPA? Your hospital is deciding whether to stock self-inflating bags with oxygen reservoirs, or flow Choose the statement that is true for a flow-inflating bag and not for a self-inflating bag: NRP Lesson 4 What is the preferred technique for chest compressions? When coordinating positive-pressure ventilation with chest compressions, how many events are performed each minute? – When chest compressions are indicated, you should also consider: - Your team begins administering chest compressions to a newborn. Correct technique includes which of the following? Your team begins administering chest compressions to a newborn. Correct technique includes which of the following? – When are chest compressions indicated? – A baby has been receiving positive-pressure ventilation and chest compressions. Her heart rate is now 110 beats per minute. Your team discontinues chest compressions. She begins to breathe spontaneously. What do you do next? Which of the following is a potential danger of administering chest compressions? – What is the ideal depth of chest compressions for a newborn? Which is the appropriate position on this baby to apply chest compressions? A baby required ventilation and chest compressions. After 45 seconds of chest compressions, the oximeter indicates a heart rate of 70 beats per minute. What is your next action? A full-term baby is born by emergency cesarean delivery secondary to fetal bradycardia. The baby is limp and not breathing. The initial steps of dry, position, and stimulate have been completed. After approximately 30 seconds, you auscultate 5 heart beats in 6 seconds. What should the next step in the resuscitation process should be? NRP Lesson 5 During an intubation, you have a very clear view of the hypopharynx. Which of the following is the correct way to lift the tongue out of the way in order to expose the pharyngeal area? You are practicing the use of an algorithm to direct the sequence of interventions to correct ventilation. In which situation will the placement of a laryngeal mask airway be useful? - During an intubation, you want to be sure that you are going to enter the trachea. Which of the following is the glottis What is the approximate period within which one should ideally be able to intubate a newborn? - You are uncertain whether you have successfully intubated a newborn. Which of the following is an indication that the endotracheal tube is correctly placed in the trachea, and not in the esophagus? - A full-term newborn has a heart rate less than 60 beats per minute despite 30 seconds of bag-and-mask ventilation. Your team plans to intubate. Which of the following is a true statement regarding the procedure? You have successfully intubated a newborn with an estimated 35-week gestational age newborn and an estimated birth weight of 2 kg. What is the correct tip-to-lip depth of tube insertion for correct placement in the mid-trachea? You are part of a team resuscitating a baby who has meconium-stained fluid. A person experienced in endotracheal intubation should be Which of the following is an indication for intubation? - What size (internal diameter) endotracheal tube should be used to intubate a newborn with an estimated gestational age of 26 weeks (estimated birth weight of 800 g)? What size laryngoscope blade should be used to intubate a newborn with an estimated gestational age of 38 weeks and an estimated birth weight of 3200 grams? What size laryngoscope blade should be used to intubate a newborn with an estimated gestational age of 30 weeks (estimated birth weight of 1,200 g)? NRP lesson 6 A 34-week gestational age baby is delivered following prolonged premature rupture of membranes and cord prolapse. The newborn has not responded to the initial steps of resuscitation, 30 seconds of positive-pressure ventilation with chest movement, or 45 to 60 seconds of cardiac compressions coordinated with positive-pressure ventilation in a 3:1 ratio. An emergency umbilical venous catheter is placed. The catheter should be inserted You are called to an emergency cesarean delivery of a 28-week gestational age baby because of prolonged rupture of membranes, chorioamnionitis, and non-reassuring fetal heart rate tracing. You called for additional help, which arrived prior to delivery. At birth the baby is non-vigorous with apnea, very poor tone, and a gray color. The baby appears to be about 1 kg. You place the newborn in plastic wrap, cover the head, and lay the baby in warm blankets under the radiant warmer. You position the newborn, dry and stimulate, but the baby remains apneic with a heart rate of 30 beats per minute. You initiate ventilation but have no improvement in heart rate or chest movement despite checking your mask seal and position, suctioning, opening the mouth, and trying increased pressure (MR SOPA). You quickly intubate, confirm appropriate endotracheal tube placement, and secure the tube. The heart rate continues to be 30 beats per minute. You provide 45 to 60 seconds of coordinated compressions and ventilations with no improvement in heart rate. You decide to administer epinephrine and a team member places an umbilical venous catheter. What dose of 1:10,000 concentration epinephrine will best result in return of spontaneous circulation? You are called to an emergency cesarean delivery of a term baby due to a Category 3 fetal heart rate monitoring strip. At your request, additional help has arrived. At delivery the baby is apneic with very poor tone and color. The baby appears to be about 3 kg. Despite repositioning, drying and stimulation, the newborn remains apneic with a heart rate of 30 beats per minute. You initiate ventilation and achieve chest rise, but the heart rate does not improve. You intubate, confirm appropriate endotracheal tube placement, and secure the tube. The heart rate is now 30 beats per minute, and a team member begins chest compressions. Together you provide 45 to 60 seconds of coordinated compressions and ventilations, but the heart rate is now undetectable. You decide to administer epinephrine via the endotracheal tube while another team member obtains IV access. What is the appropriate dose of 1:10,000 concentration of epinephrine for endotracheal delivery to a 3 kg baby A 32-week gestational age baby is delivered following 50% abruption and has not responded to the initial steps of resuscitation, 30 seconds of positive-pressure ventilation with chest movement, or 45 to 60 seconds of cardiac compressions coordinated with positive-pressure ventilation in a 3:1 ratio. A dose of epinephrine is administered. The epinephrine should be administered over the following timeframe - Rapid push as quickly as possible If a newborn's heart rate remains less than 60 beats per minute after positive-pressure ventilation and chest compressions, you should do all of the following except - A 34-week gestational age baby is delivered following prolonged premature rupture of membranes and cord prolapse. The newborn has not responded to initial resuscitation attempts, to 30 seconds of positive-pressure ventilation with chest movement, or to 45 to 60 seconds of cardiac compressions coordinated with positive-pressure ventilation in a 3:1 ratio. A dose of epinephrine is administered. What is the most important effect of epinephrine? Which of the following medications may be used during the first several minutes of neonatal resuscitation? You are called to an emergency cesarean delivery of a term baby because of chorioamnionitis, meconium-stained amniotic fluid, and late decelerations that are not recovering. You call for additional help. At delivery the newborn is apneic, with very poor tone, meconium staining, and a gray color. You quickly intubate and suction for meconium; none is obtained below the cords. You then reposition the baby, dry, and stimulate, but the newborn remains apneic with a heart rate of 40 beats per minute. What is the most appropriate next step of resuscitation? During resuscitation, one of your team members suggests that the baby might benefit from a bolus of fluid. Which of the following is an indication for volume expansion during resuscitation? - Which fluid is not a reasonable choice for volume expansion? - How soon after delivery of epinephrine should you recheck the baby's heart rate? A 34-week gestational age baby is delivered following prolonged premature rupture of membranes and cord prolapse. The newborn has not responded to the initial steps of resuscitation, 30 seconds of positive-pressure ventilation with chest rise, or 45 to 60 seconds of cardiac compressions coordinated with positive pressure ventilation in a 3:1 ratio. You decide to administer intravenous epinephrine. Which vessel in the drawing should be used? NRP Lesson 7: Special Considerations Which of the following is true about pneumothoraces in the newborn? Which of the following statements is true about the use of therapeutic hypothermia in a baby with hypoxic-ischemic encephalopathy? A baby does not appear to be improving after intubation. Which of the following is a common cause of asymmetric breath sounds in an intubated baby? Your team is resuscitating a preterm newborn. Positive-pressure ventilation with bag and mask has resulted in good bilateral air entry, normal heart rate, and normal oxygen saturations. However; the baby fails to breathe effectively on her own. Which of the following is the most likely cause of ineffective respirations in this newborn? A 10-day-old, mechanically ventilated newborn suddenly develops bradycardia and low oxygen saturation, despite the oxygen concentration being increased to 100%. What is the first and the most important step in the resuscitation of this newborn? – Remembering the MR SOPA acronym helps your team correct problems with ventilation. Which of the following steps are included in MR SOPA? Which of the following are special steps necessary in the resuscitation of a newborn with suspected congenital diaphragmatic hernia? During positive-pressure ventilation of a newborn, the breath sounds suddenly become inaudible on one side of the chest. Which of the following statements is true? A baby is unable to breath adequately after birth. Which of the following statements is true? A baby under your care has severe respiratory distress after birth, but can be easily ventilated with positive-pressure ventilation by mask. How can you test for choanal atresia? You have established a team to help care for a newborn with a known congenital heart defect. Which of the following statements is true for babies with major congenital heart disease? – While resuscitating a term newborn, you observe that the baby has severe respiratory distress and an unusually flat abdomen, with no air entry on the left side. Which of the following is the most likely diagnosis? – NRP Lesson 8 You are in the delivery room caring for a preterm newborn at 27 weeks' gestation. The baby's mother had a fever and chorioamnionitis. Resuscitation has been completed and the baby is ready to be transported to the neonatal intensive care unit. Which of the following is a true statement about the baby's subsequent care? What action is appropriate with this equipment during and immediately following resuscitation of babies born preterm? Which of the following is an appropriate action? Which of the following is a true statement about the complications that may occur in this extremely premature baby compared to a term newborn? What resources are needed to prepare for a preterm birth? You are in the delivery room caring for a preterm newborn at 28 weeks' gestation. The baby was intubated for poor respiratory effort, and you are providing positive-pressure ventilation. You initially started with 30% oxygen (0.30 FiO2). The newborn has a pulse oximeter on the right wrist; after 10 minutes, oxygen saturation is 80% and not rising. Which of the following is an appropriate action? Which of the following is a true statement about the preparation and resources needed for this preterm birth? - A compressed air source, oxygen blender, and pulse oximeter should be in the room and available for immediate use. NRP Lesson 9 Ethics and Care at the End of Life Which statement best describes the ethical principles that guide the resuscitation of a newborn? - The approach to decisions in the newborn should be guided by the same principles used for adults and older children You are called to counsel the parents of a fetus who is believed to be at the lower limits of viability whose birth is imminent. What should you tell the parents when they ask you how decisions about resuscitation are made? - The decision agreed before birth may need to be modified based on the condition of the baby after birth and the postnatal gestational age assessment. A woman is admitted at 24 weeks gestation with rupture of membranes, maternal fever, and premature labor. The baby is likely to be born in the next few hours with an estimated weight of 750 g. The care team offers the parents counseling. What is likely to be helpful in the process? - It is worth obtaining up-to-date outcome data for your institution or region, or use the NRP website and National Institute of Child Health and Human Development estimator for national data. When a fetus has a borderline chance of survival, and there is a high rate of complications, what should be included in your discussion with the parents concerning options for resuscitation? - The option of only providing comfort care can be considered. You are part of a team called to an emergency cesarean delivery done for apparent acute placental abruption at 41 weeks gestation. The newborn emerged without respirations or heart rate and has had no detectable heart rate (by palpation or by oximetry monitoring) from the time the baby was first assessed. You and the team are convinced that resuscitation has been adequate (good chest movement with PPV, timely and correct placement of umbilical catheter and administration of medications, fluids, and performance of chest compressions.) After what duration might it be appropriate to discontinue resuscitative efforts? - After 10 minutes of asystole You are called to the birth of a newborn weighing 385g and gestional age of just under 23 weeks, a birth weight that is associated with almost certain early death and nearly universal rate of severe morbidity among rare survivors. Which action is appropriate? - Attempts at resuscitation are not indicated under these circumstances, care should focus on comfort alone. In the course of planning care for a newborn with a known genetic disorder, one of your team members suggests that no resuscitation be offered. The parents agree. Other team members think this decision might jeopardize them personally. Which of the following statements is true? - Withdrawal or non-initiation of support may be acceptable if there is agreement between parents and the treating team that this support will be futile. Good decisions are based on good data. Which statement about obstetric dating and assessment is correct? - Techniques for obstetric dating are accurate to within 3-5 days, when assessed during the first trimester. You are counseling a set of 17 year old parents, whose baby is about to be born at 23 weeks gestation. You have explained that survival is unlikely and that in the event of survival, the likelihood of severe long term morbidity is high. The parents firmly request that everything be done, starting with resuscitation at birth. How might you answer them? - You assure them that as the parents, they are the appropriate voice for their baby and you will support their wishes. In most cases, who is (are) the usual and appropriate surrogate decision maker(s) for a newborn - The parents. What is the age and weight for non-initiation of resuscitation? - Gestational age of 23 weeks Birth weight of 400 g [Show More]
Last updated: 1 year ago
Preview 1 out of 25 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 22, 2022
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Jun 22, 2022
Downloads
0
Views
87

.png)