Computer Science > EXAM > CPCO 2017 CPC Final exam prep questions (100%) – American Academy of Professional Coders | CPCO201 (All)
CPCO 2017 CPC Final exam prep questions (100%) – American Academy of Professional Coders | CPCO2017 CPC Final exam prep questions (100%)
Document Content and Description Below
CPCO 2017 CPC Final exam prep questions (100%) – American Academy of Professional Coders. • Question 1 10 out of 10 points What form is provided to a patient to indicate a service may n... ot be covered by Medicare and the patient may be responsible for the charges? d. ABN d. ABN Response Feedback: Rationale: An Advanced Beneficiary Notice (ABN) is used when a Medicare beneficiary requests or agrees to receive a procedure or service that Medicare may not cover. This form notifies the patient of potential out of pocket costs for the patient. • Question 2 10 out of 10 points Which statement describes a medically necessary service? b. Using the least radical service/procedure that allows for effective treatment of the patient’s complaint or condition. b. Using the least radical service/procedure that allows for effective treatment of the patient’s complaint or condition. Response Feedback: Rationale: Medical necessity is using the least radical services/procedure that allows for effective treatment of the patient’s complaint or condition. • Question 3 10 out of 10 points What document assists provider offices with the development of Compliance Manuals? a. OIG Compliance Plan Guidance a. OIG Compliance Plan Guidance Response Feedback: Rationale: The OIG has offered compliance program guidance to form the basis of a voluntary compliance program for physician offices. Although this was released in October 2000, it is still active compliance guidance today. • Question 4 10 out of 10 points Under HIPAA, what would be a policy requirement for “minimum necessary”? a. Only individuals whose job requires it may have access to protected health information. a. Only individuals whose job requires it may have access to protected health information. Response Feedback: Rationale: It is the responsibility of a covered entity to develop and implement policies, best suited to its particular circumstances to meet HIPAA requirements. As a policy requirement, only those individuals whose job requires it may have access to protected health information. • Question 5 10 out of 10 points According to the example LCD from Novitas Solutions, measurement of vitamin D levels is indicated for patients with which condition? b. fibromyalgia b. fibromyalgia Response Feedback: Rationale: According to the LCD, measurement of vitamin D levels is indicated for patients with fibromyalgia. • Question 6 10 out of 10 points Select the TRUE statement regarding ABNs. a. ABNs may not be recognized by non-Medicare payers. a. ABNs may not be recognized by non-Medicare payers. Response Feedback: Rationale: ABNs may not be recognized by non-Medicare payers. Providers should review their contracts to determine which payers will accept an ABN for services not covered. • Question 7 10 out of 10 points Who would NOT be considered a covered entity under HIPAA? d. Patients d. Patients Response Feedback: Rationale: Covered entities in relation to HIPAA include Health Care Providers, Health Plans, and Health Care Clearinghouses. The patient is not considered a covered entity although it is the patient’s data that is protected. • Question 8 10 out of 10 points When presenting a cost estimate on an ABN for a potentially noncovered service, the cost estimate should be within what range of the actual cost? c. $100 or 25 percent c. $100 or 25 percent Response Feedback: Rationale: CMS instructions stipulate, “Notifiers must make a good faith effort to insert a reasonable estimate…the estimate should be within $100 or 25 percent of the actual costs, whichever is greater.” • Question 9 10 out of 10 points Which act was enacted as part of the American Recovery and Reinvestment Act of 2009 (ARRA) and affected privacy and security? b. HITECH b. HITECH Response Feedback: Rationale: The Health Information Technology for Economic and Clinical Health Act (HITECH) was enacted as a part of the American Recovery and Reinvestment Act of 2009 (ARRA) to promote the adoption and meaningful use of health information technology. Portions of HITECH strengthen HIPAA rules by addressing privacy and security concerns associated with the electronic transmission of health information. • Question 10 10 out of 10 points What document is referenced to when looking for potential problem areas identified by the government indicating scrutiny of the services within the coming year? c. OIG Work Plan c. OIG Work Plan Response Feedback: Rationale: Twice a year, the OIG releases a Work Plan outlining its priorities for the fiscal year ahead. Within the Work Plan, potential problem areas with claims submissions are listed and will be targeted with special scrutiny. Sunday, November 19, 2017 9:04:26 AM MST • The minimum necessary rule applies to b. Disclosures to or requests by a health care provider for treatment purposes. d. Covered entities taking reasonable steps to limit use or disclosure of PHI Response Feedback: Rationale: The Privacy Rule generally requires covered entities to take reasonable steps to limit the use or disclosure of, and requests for, protected health information to the minimum necessary to accomplish the intended purpose. The minimum necessary standard does not apply to the following: · Disclosures to or requests by a health care provider for treatment purposes. · Disclosures to the individual who is the subject of the information. · Uses or disclosures made pursuant to an individual’s authorization. · Uses or disclosures required for compliance with the Health Insurance Portability and Accountability Act (HIPAA) Administrative Simplification Rules. · Disclosures to the Department of Health & Human Services (HHS) when disclosure of information is required under the Privacy Rule for enforcement purposes. · Uses or disclosures that are required by other law. • Question 2 0 out of 4 points According to the AAPC Code of Ethics, which term is NOT listed as an ethical principle of professional conduct? d. Commitment b. Efficiency Response Feedback: Rationale: It shall be the responsibility of every AAPC member, as a condition of continued membership, to conduct themselves in all professional activities in a manner consistent with ALL of the following ethical principles of professional conduct: · · Integrity · Respect · Commitment · Competence · Fairness · Responsibility • Question 3 0 out of 4 points How many components are included in an effective compliance plan? c. 9 d. 7 Response Feedback: Rationale: The following list of components, as set forth in previous OIG Compliance Program Guidance for Individual and Small Group Physician Practices, can form the basis of a voluntary compliance program for a provider practice: • Conducting internal monitoring and auditing through the performance of periodic audits; • Implementing compliance and practice standards through the development of written standards and procedures; • Designating a compliance officer or contact(s) to monitor compliance efforts and enforce practice standards; • Conducting appropriate training and education on practice standards and procedures; • Responding appropriately to detected violations through the investigation of allegations and the disclosure of incidents to appropriate Government entities; • Developing open lines of communication, such as (1) discussions at staff meetings regarding how to avoid erroneous or fraudulent conduct, and (2) community bulletin boards, to keep practice employees updated regarding compliance activities; and • Enforcing disciplinary standards through well-publicized guidelines. These seven components provide a solid basis upon which a provider practice can create a compliance program. • Question 4 4 out of 4 points According to the OIG, internal monitoring and auditing should be performed by what means? a. Periodic audits. a. Periodic audits. Response Feedback: Rationale: A key component of an effective compliance program includes internal monitoring and auditing through the performance of periodic audits. This ongoing evaluation includes not only whether the provider practice’s standards and procedures are in fact current and accurate, but also whether the compliance program is working, (for example, whether individuals are properly carrying out their responsibilities and claims are submitted appropriately). • Question 5 4 out of 4 points When coding an operative report, what action would NOT be recommended? b. Coding from the header without reading the body of the report. b. Coding from the header without reading the body of the report. Response Feedback: Rationale: Operative report coding tips include reviewing the documentation in the detail of the procedure to further clarify or define both procedures and diagnoses. • Question 6 4 out of 4 points Which of the following choices is NOT a benefit of an active compliance plan? a. Eliminates risk of an audit. a. Eliminates risk of an audit. Response Feedback: Rationale: Although voluntary, a compliance plan may offer several benefits, among them: • Faster, more accurate payment of claims. • Fewer billing mistakes. • Diminished chances of a payer audit. • Less chance of violating self-referral and anti-kickback statutes. Additionally, the increased accuracy of provider documentation that may result from a compliance program actually may assist in enhancing patient care. • Question 7 4 out of 4 points HIPAA stands for d. Health Insurance Portability and Accountability Act d. Health Insurance Portability and Accountability Act Response Feedback: Rationale: Health Insurance Portability and Accountability Act (HIPAA) • Question 8 4 out of 4 points In what year was HITECH enacted as part of the American Recovery and Reinvestment Act? a. 2009 a. 2009 Response Feedback: Rationale: The Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, was signed into law on February 17, 2009, to promote the adoption and meaningful use of health information technology. • Question 9 4 out of 4 points The Medicare program is made up of several parts. Which part covers provider fees without the use of a private insurer? d. Part B d. Part B Response Feedback: Rationale: Medicare Part B helps to cover medically necessary provider services, outpatient care and other medical services (including some preventive services) not covered under Medicare Part A. Medicare Part B is an optional benefit for which the patient pays a monthly premium, an annual deductible, and generally has a 20% co-insurance except for preventive services covered under the healthcare law. • Question 10 4 out of 4 points Healthcare providers are responsible for developing ____ ____ and policies and procedures regarding privacy in their practices. c. Notices of Privacy Practices c. Notices of Privacy Practices Response Feedback: Rationale: Healthcare providers are responsible for developing Notices of Privacy Practices and policies and procedures regarding privacy in their practices. • Question 11 4 out of 4 points Evaluation and management services are often provided in a standard format such as SOAP notes. What does the acronym SOAP stand for? c. Subjective, Objective, Assessment, Plan c. Subjective, Objective, Assessment, Plan Response Feedback: Rationale: S-Subjective, O-Objective, A-Assessment, P-Plan • Question 12 4 out of 4 points What type of health insurance provides coverage for low-income families? b. Medicaid b. Medicaid Response Feedback: Rationale: Medicaid is a health insurance assistance program for some low-income people (especially children and pregnant women) sponsored by federal and state governments. • Question 13 0 out of 4 points The OIG recommends that provider practices enforce disciplinary actions through well publicized compliance guidelines to ensure actions that are ______. a. Frequent b. Consistent and appropriate Response Feedback: Rationale: The OIG recommends that a provider practice’s enforcement and disciplinary mechanisms ensure that violations of the practice’s compliance policies will result in consistent and appropriate sanctions, including the possibility of termination, against the offending individual. • Question 14 4 out of 4 points What is the value of a remittance advice? c. It states what will be paid and why any changes to charges were made. c. It states what will be paid and why any changes to charges were made. Response Feedback: Rationale: The determination of the payer is sent to the provider in the form of a remittance advice. The remittance advice explains the outcome of the insurance adjudication on the claim, including the payment amount, contractual adjustments and reason(s) for denial. • Question 15 4 out of 4 points HITECH provides a ____ day window during which any violation not due to willful neglect may be corrected without penalty. c. 30 c. 30 Response Feedback: Rationale: HITECH also lowers the bar for what constitutes a violation, but provides a 30-day window during which any violation not due to willful neglect may be corrected without penalty. • Question 16 4 out of 4 points AAPC credentialed coders have proven mastery of what information? d. All of the above d. All of the above Response Feedback: Rationale: AAPC credentialed coders have proven mastery of all code sets, evaluation and management principles, and documentation guidelines. • Question 17 4 out of 4 points What form is used to submit a provider’s charge to the insurance carrier? d. CMS-1500 d. CMS-1500 Response Feedback: Rationale: Once documentation is translated into codes, it is then sent on a CMS-1500 form to the insurance carrier for reimbursement. • Question 18 4 out of 4 points The minimum necessary rule is based on sound current practice that protected health information should NOT be used or disclosed when it is not necessary to satisfy a particular purpose or carry out a function. What does this mean? b. Providers should develop safeguards to prevent unauthorized access to protected health information. b. Providers should develop safeguards to prevent unauthorized access to protected health information. Response Feedback: Rationale: The minimum necessary standard requires covered entities to evaluate their practices and enhance safeguards as needed to limit unnecessary or inappropriate access to and disclosure of protected health information. Only those individuals whose job requires it may have access to PHI. Only the minimum protected information required to do the job should be shared. • Question 19 0 out of 4 points What is the purpose of National Coverage Determinations? d. To set standards for all payers on coverage items. b. To explain CMS policies on when Medicare will pay for items or services. Response Feedback: Rationale: National Coverage Determinations (NCD) explain CMS policies on when Medicare will pay for items or services. • Question 20 4 out of 4 points Twice a year the OIG releases a ____ outlining its priorities for the fiscal year ahead. b. Work Plan b. Work Plan Response Feedback: Rationale: The OIG Work Plan sets forth various projects to be addressed twice during the fiscal year by the Office of Audit Services, Office of Evaluation and Inspections, Office of Investigations, and Office of Counsel to the Inspector General. • Question 21 4 out of 4 points What will the scope of a compliance program depend on? d. The size and resources of the provider’s practice. d. The size and resources of the provider’s practice. Response Feedback: Rationale: The scope of a compliance program will depend on the size and resources of the provider practice. • Question 22 4 out of 4 points Which coding manuals do outpatient coders focus on learning? a. CPT®, HCPCS Level II and ICD-10-CM a. CPT®, HCPCS Level II and ICD-10-CM Response Feedback: Rationale: Outpatient coding focuses on provider services. Outpatient coders will focus on learning CPT®, HCPCS Level II and ICD-10-CM. • Question 23 4 out of 4 points What does CMS-HCC stand for? c. Centers for Medicare & Medicaid Services – Hierarchal Condition Category c. Centers for Medicare & Medicaid Services – Hierarchal Condition Category Response Feedback: Rationale: Centers for Medicare & Medicaid Services – Hierarchal Condition Category • Question 24 0 out of 4 points Who is responsible for enforcing the HIPAA security rule? d. HHS b. OCR Response Feedback: Rationale: The Office for Civil Rights (OCR) enforces the HIPAA Privacy Rule. • Question 25 4 out of 4 points Voluntary compliance programs also provide benefits by not only helping to prevent erroneous or ____, but also by showing that the provider practice is making additional good faith efforts to submit claims appropriately. c. Fraudulent claims c. Fraudulent claims Response Feedback: Rationale: Voluntary compliance programs also provide benefits by not only helping to prevent erroneous or fraudulent claims, but also by showing that the provider practice is making additional good faith efforts to submit claims appropriately. Sunday, November 19, 2017 9:05:23 AM MST • Question 1 10 out of 10 points Squamous cell carcinoma and basal cell carcinoma are both cancers of cell tissue of the skin, lining of the blood vessels, respiratory, intestinal, urinary tracts, and other body systems. These carcinomas are found in what type of tissue? d. Epithelial tissue d. Epithelial tissue Response Feedback: RATIONALE: Squamous cell carcinoma and basal cell carcinoma are both cancers of cells in epithelial tissue. Epithelial tissues is found in the skin, lining of the blood vessels, respiratory, intestinal, and urinary tracts, and other body systems. • Question 2 10 out of 10 points Which medical term refers to the cheek? a. Buccal a. Buccal Response Feedback: RATIONALE: Bucca means cheek. Buccal is relating to the cheek. Buccal swabs can be used for DNA testing. • Question 3 10 out of 10 points Which layer is the middle layer of the eyeball? b. Choroid b. Choroid Response Feedback: RATIONALE: The eyeball has three layers: the retina (innermost), choroid (middle), and sclera (outermost). • Question 4 10 out of 10 points Which anatomical structure in the urinary system differs in position and length between male and female, but serves the same function with regard to urine, and is often treated the same? b. Urethra b. Urethra Response Feedback: RATIONALE: The male and female urethras are quite different anatomically in position and length; however, they perform the same function with regard to urine, and are treated similarly for many surgical procedures in the coding genre. • Question 5 10 out of 10 points Which structure of the ear is considered the inner ear? b. Labyrinth b. Labyrinth Response Feedback: RATIONALE: The ear has three distinct and separate anatomical divisions: the outer ear (external ear), middle ear (tympanic cavity), and inner ear (labyrinth). • Question 6 10 out of 10 points Based on word parts, what is the definition of a tracheostomy? b. Creation of a hole in the trachea. b. Creation of a hole in the trachea. Response Feedback: RATIONALE: The root trache- means trachea. The suffix –ostomy means surgical creation of an opening. A tracheostomy is surgical creation of an opening in the trachea and is used to help a patient breathe. • Question 7 0 out of 10 points Which structure is not a true endocrine structure? c. Pituitary gland b. Carotid body Response Feedback: RATIONALE: The carotid body is not a true endocrine structure, but is made of both glandular and nonglandular tissue. • Question 8 10 out of 10 points Which layer of the epidermis is normally found on the palms of the hands and the soles of the feet? b. Stratum Lucidum b. Stratum Lucidum Response Feedback: RATIONALE: The stratum lucidum is a clear layer normally found only on the palms of the hands and the soles of the feet. • Question 9 10 out of 10 points A cystourethroscopy is examination of what structures? a. Bladder and urethra a. Bladder and urethra Response Feedback: RATIONALE: The root cyst- means urinary bladder. The root word urethr- means urethra. A cystourethroscopy is examination of the urinary bladder and urethra. • Question 10 10 out of 10 points Which leukocyte does the body use to protect against allergic reactions and parasites? d. Eosinophils d. Eosinophils Response Feedback: RATIONALE: The body uses eosinophils to protect against allergic reactions and parasites; elevated levels may indicate an allergic response. Sunday, November 19, 2017 9:05:50 AM MST • Question 1 4 out of 4 points Lacrimal glands are responsible for which of the following? c. Production of tears c. Production of tears • Question 2 4 out of 4 points Through which vessel is oxygenated blood returned to the heart from the lungs? d. Pulmonary vein d. Pulmonary vein • Question 3 4 out of 4 points Which of the following conditions results from an injury to the head? The symptoms include headache, dizziness and vomiting. b. Concussion b. Concussion • Question 4 4 out of 4 points The loop of Henle is located in which structure? b. Kidney b. Kidney • Question 5 4 out of 4 points What is a function of the alveoli in the lungs? b. Oxygen exchange b. Oxygen exchange • Question 6 4 out of 4 points Which gland is located on the superior surface of the kidney? d. Adrenal gland d. Adrenal gland • Question 7 4 out of 4 points Upon leaving the stomach, nutrients move through the small intestine in what order? a. Duodenum, jejunum, ileum. a. Duodenum, jejunum, ileum. • Question 8 4 out of 4 points How many lobes make up the right lung? b. three b. three • Question 9 0 out of 4 points Which of the following is true of the stratum germinativum? c. It is composed of about 30 layers of dead, flattened, keratinized cells. a. It lies on top of the dermis and has access to a rich supply of blood. • Question 10 4 out of 4 points Which layer is NOT considered part of the skin? b. Hypodermis b. Hypodermis • Question 11 4 out of 4 points Which of the following is significant of an abdominal aortic aneurysm? c. It is a weakness in a large artery and rupture can be deadly c. It is a weakness in a large artery and rupture can be deadly • Question 12 4 out of 4 points Which chamber of the heart is considered the one working the hardest? d. Left ventricle d. Left ventricle • Question 13 4 out of 4 points What is a myocardial infarction? b. Lack of oxygen to the heart tissue, resulting in tissue death b. Lack of oxygen to the heart tissue, resulting in tissue death • Question 14 4 out of 4 points The dome-shaped muscle under the lungs flattening during inspiration is the: c. Diaphragm c. Diaphragm • Question 15 4 out of 4 points A condition where the thyroid is overactive is called: a. Thyrotoxicosis a. Thyrotoxicosis • Question 16 4 out of 4 points The meaning of the root blephar/o is: d. Eyelid d. Eyelid • Question 17 4 out of 4 points A deficiency of cells in the blood is defined as: b. Cytopenia b. Cytopenia • Question 18 4 out of 4 points Cytopathology is the study of: d. Cells d. Cells • Question 19 4 out of 4 points The meaning of heteropsia (or anisometropia) is: b. Unequal vision in the two eyes b. Unequal vision in the two eyes • Question 20 4 out of 4 points The meaning of the root myring/o is: b. Tympanic membrane b. Tympanic membrane • Question 21 4 out of 4 points Splenorrhaphy is described as: c. Suture of a wound of the spleen c. Suture of a wound of the spleen • Question 22 4 out of 4 points A Bartholin’s gland cyst may be treated by marsupialization. This treatment is described as: d. Create an opening to the gland and suture the cut edges to form a pouch d. Create an opening to the gland and suture the cut edges to form a pouch • Question 23 4 out of 4 points Arthritis is an inflammation of what? b. Joint b. Joint • Question 24 4 out of 4 points Destruction of lesions of the vulva can be done with cryosurgery. This method uses: c. Extreme cold c. Extreme cold • Question 25 0 out of 4 points The radiology term fluoroscopy is described as: a. A scan using an X-ray beam rotating around the patient d. An X-ray procedure allowing the visualization of internal organs in motion Sunday, November 19, 2017 9:06:15 AM MST • Question 1 0 out of 10 points Which coding convention is used in the description of an ICD-10-CM code when the information in the medical record provides detail, but no specific code exists? Refer to ICD-10-CM guideline I.A.6. d. NOS c. NEC Response Feedback: Rationale: NEC "Not elsewhere classifiable" This abbreviation in the index represents "other specified." When a specific code is not available for a condition the index directs the coder to the "other specified" code in the Tabular List. When a specific code is not available for a condition the Tabular List includes an NEC entry under a code to identify the code as the "other specified" code. (see "Other" codes) • Question 2 0 out of 10 points Supplementary words enclosed in parentheses in the ICD-10-CM coding manual have what affect on the coding? Refer to ICD-10-CM guideline I.A.7. c. They identify manifestation codes that should be coded in addition to the primary code. d. They do not affect code assignment. Response Feedback: Rationale: Parentheses are used in both the ICD-10-CM Alphabetic Index and Tabular List to enclose supplementary words that may be present in the statement of a disease or procedure without affecting the code number to which it is assigned. The terms within the parentheses are referred to as nonessential modifiers. • Question 3 10 out of 10 points Applying the coding concept from ICD-10-CM guideline I.B.1., which of the following is the recommended method for using your ICD-10-CM code book? d. Always consult the Alphabetic Index first. Refer to the Tabular List to locate the selected code d. Always consult the Alphabetic Index first. Refer to the Tabular List to locate the selected code Response Feedback: Rationale: Introduction ICD-10-CM - How to Use the ICD-10-CM - Steps to Correct Coding tells us to locate the main term in the Alphabetic Index, then verify the code in the Tabular List. • Question 4 10 out of 10 points What is the ICD-10-CM code for essential hypertension? d. I10 d. I10 Response Feedback: Rationale: In the Index to Diseases and Injuries, look for Hypertension. You will see next to the main term Hypertension subterms (or nonessential modifiers) listed in parentheses, and the subterm essential is in parenthesis. Subterms that follow the main term and are enclosed in parentheses are nonessential modifiers in which they can clarify the diagnosis but are not required. Verify in the Tabular List that code I10 is for Essential Hypertension. • Question 5 0 out of 10 points What is the ICD-10-CM code for bilateral hip pain? c. M25.559 d. M25.551, M25.552 Response Feedback: Rationale: In the Index to Diseases and Injuries, look for Pain(s)/ joint/hip. You are directed to subcategory code M25.55. In the Tabular List, a sixth character is assigned to indicate laterality. Because there is no code choice for bilateral, M25.551 is reported for the right hip pain and M25.552 is reported for the left hip pain. • Question 6 10 out of 10 points Referencing ICD-10-CM guideline I.B.10., what is the time limit when assigning codes as “sequela”? c. There is no time limit on sequela. c. There is no time limit on sequela. Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section I.B.10 states there is no time limit when sequela codes can be used. • Question 7 10 out of 10 points Referencing ICD-10-CM guideline I.B.11., what is the appropriate action when a physician documents an impending condition that had not occurred by the time of discharge? a. Check the ICD-10-CM Alphabetic Index to see if there are listings under “threatened” or “impending” and if not, code the existing underlying condition(s) and not the condition described as impending. a. Check the ICD-10-CM Alphabetic Index to see if there are listings under “threatened” or “impending” and if not, code the existing underlying condition(s) and not the condition described as impending. Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section I.B.11 state to check the Index to Diseases and Injuries for listings under the main term threatened or impending. If a subterm does not exist, code the existing underlying condition(s) and not the condition described as impending. • Question 8 0 out of 10 points A patient sees the physician for chest pain, fever, and cough. The physician orders an x-ray to rule out pneumonia. Applying the coding concept from ICD-10-CM guideline IV.H., which ICD-10-CM code(s) are reported? d. R07.9, R50.9, R05, J18.9 c. R07.9, R50.9, R05 Response Feedback: Rationale: ICD-10-CM coding guidelines, Section IV.H. instructs you to code signs and symptoms when the diagnosis is uncertain. Diagnosis stated as “rule out,” “suspected,” or “probably” are not reported. The pneumonia is a “rule out” and is not coded. Instead, code the symptoms. In the Index to Diseases and Injuries, look for Pain(s)/chest (central) (R07.9), Fever (R50.9), and Cough (R05). Verify code selection in the Tabular List. • Question 9 0 out of 10 points A patient is in outpatient surgery for a laparoscopic oophorectomy for a right ovarian cyst. After admission, the anesthesiologist discovered the patient had an upper respiratory infection and the surgery was cancelled. Applying the coding concept from ICD-10-CM guideline IV.A.1., which ICD-10-CM code(s) are reported? [None Given] d. N83.201, J06.9, Z53.09 Response Feedback: Rationale: ICD-10-CM coding guidelines Section IV.A.1.states to report the reason for surgery as the first listed diagnosis even if the surgery is cancelled due to a contraindication. Look in the Index to Diseases and Injuries for Cyst/ovary, ovarian (twisted) and you are referred N83.201. In the Tabular List, 6th character 1 is reported for the right side. For the respiratory infection, look for Infection/respiratory (tract)/upper (acute) NOS and you are referred to J06.9. Then, look for Canceled procedure/because of/contraindication which refers you to Z53.09. Verify codes in the Tabular List. • Question 10 0 out of 10 points A patient is admitted for an outpatient cholecystectomy for gall stones. During recovery, the patient developed severe postoperative pain. The patient was admitted to observation to monitor the pain. Applying the coding concept from ICD-10-CM guideline IV.A.2., what ICD-10-CM code(s) are reported for the observation? c. G89.18, K80.20 a. K80.20, G89.18 Response Feedback: Rationale: According to the ICD-10-CM Guidelines, Section IV.A.2, when a patient presents for outpatient surgery and develops complications requiring admission to observation, code the reason for the surgery as the primary diagnosis, and the complications as secondary diagnosis. Look for main term Gallstone in the Index to Diseases and Injuries and you are referred to see also Calculus, gallbladder. Look for Calculus/gallbladder, which refers you to K80.20. For the postoperative pain, look for Pain(s)/postoperative NOS and you are referred to G89.18. Verify codes in the Tabular List. Sunday, November 19, 2017 9:06:56 AM MST • Question 1 4 out of 4 points What section of the ICD-10-CM guidelines contains instructions on how to code for a patient receiving diagnostic services only in an outpatient setting? d. Section IV d. Section IV Response Feedback: Rationale: Section IV Diagnostic Coding and Reporting Guidelines for Outpatient Services IV.K is specific to patients receiving diagnostic services only. • Question 2 4 out of 4 points Which of the following statements is TRUE in reference to reporting body mass index (BMI) codes? d. BMI codes should be reported as a secondary code only. d. BMI codes should be reported as a secondary code only. Response Feedback: Rationale: ICD-10-CM guideline I.B.14 indicates that BMI codes are reported as secondary diagnoses. In the Tabular List, BMI codes can be reported with any code in subcategory E66.-, not just code E66.3. • Question 3 4 out of 4 points What is an example of an eponym? a. Paget’s disease a. Paget’s disease Response Feedback: Rationale: An eponym is a word derived from someone’s name. Paget’s disease is a disorder that involves abnormal bone destruction and regrowth which results in deformity. It was described by surgeon and pathologist Sir James Paget. • Question 4 4 out of 4 points According to ICD-10-CM guideline I.B.1 use both ____ and ____ when locating and assigning a diagnosis code. b. ICD-10-CM Alphabetic Index and Tabular List b. ICD-10-CM Alphabetic Index and Tabular List Response Feedback: Rationale: According to the ICD-10-CM guideline 1.B.1 both the Alphabetical Index and Tabular List are used to locate and assign a code. Reliance on only the Alphabetic Index or the Tabular List will lead to errors and less specificity in reporting codes. • Question 5 0 out of 4 points When a patient has a condition that is both acute and chronic and there are separate entries for both, how is it reported? b. Code both sequencing the chronic first d. Code both sequencing the acute first Response Feedback: Rationale: According to the ICD-10-CM guideline 1.B.8 if the same condition is described as both acute (subacute) and chronic and separate entries exist in the ICD-10-CM Alphabetic Index at the same indentation level, code both and sequence the acute (subacute) first. • Question 6 4 out of 4 points What is the ICD-10-CM code for swine flu? b. J09.X2 b. J09.X2 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Flu/swine. You are directed to J09.X2. Verify code selection in the Tabular List. • Question 7 4 out of 4 points A 6 year-old patient is seen in the office for acute otitis media, coded as H66.90. This is an example of a ____ code. a. NOS a. NOS Response Feedback: Rationale: H66.90 is Not Otherwise Specified. ICD-10-CM guideline I.A.9.b codes titled unspecified are for use when the information in the medical record is insufficient to assign a more specific code. The inclusion terms under H66.9 include NOS in the description. • Question 8 4 out of 4 points What is the ICD-10-CM code for nausea? a. R11.0 a. R11.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Nausea. You are directed to R11.0. There is no mention of vomiting. Verify code selection in the Tabular List. • Question 9 4 out of 4 points What is the ICD-10-CM code for classical migraine? a. G43.109 a. G43.109 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Migraine/classical and you are directed to see migraine with aura. Migraine/with aura directs you to G43.109. Verify code selection in the Tabular List. • Question 10 4 out of 4 points What is the ICD-10-CM code for low back pain? b. M54.5 b. M54.5 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index Pain/low back and you are directed to M54.5. Verify code selection in the Tabular List. • Question 11 4 out of 4 points What is the sequencing order when coding a sequela (late effect)? d. The residual condition is coded first, and the code(s) for the cause of the late effect are coded as secondary. d. The residual condition is coded first, and the code(s) for the cause of the late effect are coded as secondary. Response Feedback: Rationale: Per ICD -10-CM guideline 1.B.10 coding of sequela (late effects) generally requires two codes sequenced in the following order: The condition or nature of the late effect is sequenced first and the late effect code is sequenced second. Exceptions to this guideline are those instances where the code for the late effect is followed by a manifestation code in the Tabular List and title or the late effect code has been expanded to include the manifestation. • Question 12 4 out of 4 points Which diagnosis below would be considered a combination code? a. K80.00 a. K80.00 Response Feedback: Rationale: Refer to ICD-10-CM guideline I.B.9 for the definition of a combination code. Code K80.00 reports both gallbladder calculus and acute cholecystitis. Verify code selection in the Tabular List. • Question 13 4 out of 4 points What is the ICD-10-CM code for keloid scar on the foot? d. L91.0 d. L91.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Scar/keloid L91.0. The location does not affect code selection. Verify code selection in the Tabular List. • Question 14 0 out of 4 points Which diagnosis code(s) below reports pain in the left and right ears? d. H92.01, H92.02 b. H92.03 Response Feedback: Rationale: ICD-10-CM allows for the reporting of laterality (right, left, bilateral). For bilateral sites, the final character of the code indicates laterality. ICD-10-CM guideline I.B.13 indicates if no bilateral code is provided and the condition is bilateral, assign separate codes for both the left and right side. There is a bilateral code provided for pain in the left and right ears H92.03. You would not report two separate codes. • Question 15 4 out of 4 points Refer to the ICD-10-CM Alphabetic Index. Identify the main term below that has an instructional note indicating another main term may need to be referenced providing an additional index entry to report the diagnostic code. b. Fibrosarcoma b. Fibrosarcoma Response Feedback: Rationale: Look for the main term for Fibrosarcoma in the ICD-10-CM Alphabetic Index. The main term Fibrosarcoma has a note to see also Neoplasm, connective tissue, malignant. This note instructs you to go to another main term if additional information of the diagnosis cannot be found under the first main term. • Question 16 0 out of 4 points A patient sees his primary care provider for chest pain and regurgitation. The provider’s diagnosis for the patient is gastroesophageal reflux. What diagnosis code(s) should be reported? a. R07.9, R11.10, K21.9 b. K21.9 Response Feedback: Rationale: ICD-10-CM coding guideline I.B.5 states “Signs and symptoms that are associated with routinely with a disease process should not be assigned as additional codes, unless otherwise instructed by the classification.” In the ICD-10-CM Alphabetic Index look for Reflux/gastroesophageal guiding you to code K21.9. Verify code selection in the Tabular List. • Question 17 4 out of 4 points What is the diagnosis code(s) for a patient with bronchitis and the flu? b. J11.1 b. J11.1 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Bronchitis/with/influenza, flu or grippe which states to see Influenza, with, respiratory manifestations NEC. Look for Influenza/with/respiratory manifestations NEC J11.1. Verify code selection in the Tabular List. • Question 18 4 out of 4 points A 45 year-old female with malignant Mullerian duct cancer is receiving her first treatment of chemotherapy. What diagnosis codes are reported? b. Z51.11, C57.7 b. Z51.11, C57.7 Response Feedback: Rationale: ICD-10-CM guideline I.C.2.e.2 states if a patient admission/encounter is solely for administration of chemotherapy, immunotherapy or radiation therapy assign codes Z51.0, Z51.11 or Z51.12 as the first listed or principal diagnosis. The malignancy for which the therapy is being administered should be assigned as a secondary diagnosis. In the ICD-10-CM Alphabetic Index look for Chemotherapy (session) (for)/cancer Z51.11. Next, look in the ICD-10-CM Table of Neoplasms for Mullerian duct/female and select the code from the Malignant Primary column which directs the coder to C57.7. Verify code selection in the Tabular List. • Question 19 4 out of 4 points What diagnosis codes should be reported for fragilitas ossium, osteogenesis imperfecta and osteopsathyrosis? a. Q78.0 a. Q78.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Fragilitas/ossium Q78.0. Next look for Osteogenesis imperfect Q78.0. Look for Osteopsathyrosis Q78.0. The Tabular List includes all the conditions in the code Q78.0. • Question 20 4 out of 4 points What ICD-10-CM code(s) is/are reported for enlargement of the prostate with a symptom of urinary retention? d. N40.1, R33.8 d. N40.1, R33.8 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Enlargement, enlarged/prostate/with lower urinary tract symptoms (LUTS). You are directed to N40.1. In the Tabular List under code N40.1 there is an instructional note that indicates to use additional code to identify symptoms. You report code R33.8 for urinary retention as the second code. • Question 21 4 out of 4 points A 10 month-old comes into the pediatrician’s office for a harsh, bark-like cough. She is diagnosed with croup. The mother also wants the pediatrician to look at a rash that has developed on her leg. The pediatrician prescribes over the counter medication of acetaminophen for the croup and hydrocortisone cream for the rash on the leg. She is to follow up in five days or return earlier if the conditions worsen. What ICD-10-CM code(s) should be reported for this visit? b. J05.0, R21 b. J05.0, R21 Response Feedback: Rationale: Signs and symptoms that are associated with a disease process should not be reported, refer to ICD-10-CM guideline I.B.5. For this case the ICD-10-CM code R05 should not be reported because cough is a symptom of the croup. Codes for signs and symptoms that are not routinely associated with a definitive diagnosis should be reported, according to ICD-10-CM guidelines 1.B.4 and I.B.5. For this case the rash is reported because it is not related or associated to the croup. Look for Croup in the ICD-10-CM Alphabetic Index referring you to code J05.0. Look for Rash in the Alphabetic Index referring you to code R21. Verify both codes in the Tabular List. • Question 22 0 out of 4 points What diagnosis code(s) is/are reported for behavioral disturbances in a patient with early onset Alzheimer’s? a. F02.81, G30.0 c. G30.0, F02.81 Response Feedback: Rationale: In the Alphabetic Index, look for Disease/Alzheimer’s/Early Onset/with behavioral disturbance guiding you to codes G30.0 [F02.81]. A code in brackets is reported as an additional diagnosis. There is an instructional note in the Tabular List under category code G30 that states, use additional code to identify manifestation. You see dementia with behavioral disturbance listed as an additional code. When you go to code F02.81 in the Tabular List there is an instructional note under category F02 to code first Alzheimer’s (G30.-). • Question 23 4 out of 4 points What diagnosis code(s) is/are reported for pneumonia due to SARS? a. J12.81 a. J12.81 Response Feedback: Rationale: ICD-10-CM guideline I.B.9 indicates that a combination code is a single code used to classify two diagnoses or a diagnosis with an associated secondary process (manifestation). Multiple coding should not be used when the classification provides a combination code that clearly identifies all of the elements documented in the diagnosis. In the ICD-10-CM Alphabetic Index look for Syndrome/severe acute respiratory (SARS) guiding you to code J12.81. You can also look for Pneumonia/SARS-associated coronavirus J12.81. Verify code selection in the Tabular List. • Question 24 4 out of 4 points A 32 year-old male is in a diagnostic center to have an ultrasound of his neck due to difficulty swallowing. The patient’s father had esophageal cancer. What is/are the appropriate code(s) to report for the diagnostic service? c. R13.10, Z80.0 c. R13.10, Z80.0 Response Feedback: Rationale: A patient receiving a diagnostic service (for example, ultrasound, MRI, diagnostic colonoscopy) for an encounter or visit, report the condition or problem as a primary code to indicate why the patient is having the test performed. Codes for other diagnosis, such as chronic conditions or history are reported as an additional diagnosis. In this case the family history code is reported as an additional diagnosis since it has an impact on current care or influence treatment. Refer to ICD-10-CM guideline IV.K. In the ICD-10-CM Alphabetic Index look for Difficult, difficulty (in)/swallowing which states to see Dysphagia. Look in the Alphabetic Index for Dysphagia which directs the coder to code R13.10. In the Alphabetic Index look for History/family (of)/malignant neoplasm (of)/gastrointestinal tract referring you to code Z80.0. Verify code selection in the Alphabetic Index. • Question 25 4 out of 4 points What diagnosis code(s) should be reported for primary osteoarthritis in both knees? b. M17.0 b. M17.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Osteoarthritis/primary/knee/bilateral which directs the coder to M17.0. Verify code selection in the Tabular List. Sunday, November 19, 2017 9:07:16 AM MST • Question 1 0 out of 10 points A 22-year-old female is admitted to ICU for acute renal (kidney) failure due to sepsis (causal organism unknown). Applying the coding concept from ICD-10-CM guideline I.C.1.d.1.b. what ICD-10-CM codes are reported (in the correct sequencing)? b. N17.9, R65.20, A41.9 a. A41.9, R65.20, N17.9 Response Feedback: Rationale: ICD-10-CM guideline I.C.1.d.1.b indicates: The coding of severe sepsis requires a minimum of two codes. First, a code for the underlying systemic infection, followed by a code from subcategory R65.2, Severe sepsis. If the causal organism is not documented, assign code A41.9, Sepsis, unspecified organism, for the infection. Additional codes(s) for the associated acute organ dysfunction are also required (if present). The first code to report is sepsis; look for the main term Sepsis in the ICD 10-CM Alphabetic Index referring you to code A41.9. Next, look for Sepsis/with organ dysfunction (acute) (multiple) referring you to code R65.20. For the last code, look for Failure/renal/acute referring you to code N17.9. In the Tabular List you will find an instructional note under subcategory R56.2 indicating what codes should be reported first and what codes should be reported as additional codes. • Question 2 10 out of 10 points A 45-year-old female with ovarian cancer visits her oncologist to receive an injection of Procrit®. The Procrit® has been prescribed to her for treatment of her anemia resulting from antineoplastic chemotherapy treatment. Applying the coding concept from ICD-10-CM guidelines I.C.2.c.2. What ICD-10-CM codes should be reported? a. D64.81, C56.9, T45.1X5A a. D64.81, C56.9, T45.1X5A Response Feedback: Rationale: According to ICD-10-CM guidelines 1.C.2.c.2., because the treatment is directed at the anemia associated with chemotherapy, and the treatment is only for the anemia, the anemia should be sequenced first, followed by the appropriate codes for the neoplasm and the adverse effect (T45.1X5). Look in the ICD 10-CM Alphabetic Index for Anemia/due to (in) (with)/antineoplastic chemotherapy (D64.81). According to guideline 1.C.2.c.2. the malignancy is reported secondarily followed by code T45.1X5. Look in the ICD-10-CM Table of Neoplasms for ovary and report the code from the Malignant Primary column (C56.-). In the Tabular List, C56.9 is reported because the laterality is not stated. Next, to locate T45.1X5 look in the Table of Drugs and Chemicals for Antineoplastic NEC and selecting the code from the Adverse effect column (T45.1X5). In the Tabular List, T45.1X5 requires a 7th character extender. A is selected because this is considered active treatment. • Question 3 10 out of 10 points Mrs. Fryer visits her nephrologists for an erythropoietin (EPO) injection for her anemia. She has Stage 3 chronic kidney disease, which is the cause of the anemia. Applying the coding concept from ICD-10-CM guideline I.A.13., what ICD-10-CM code(s) should be reported for the EPO injection? b. N18.3, D63.1 b. N18.3, D63.1 Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section I.A.13., states codes that fall under the category "in diseases classified elsewhere," are manifestation codes. There will be an instructional note (such as a code first note) with these manifestation codes that will indicate the proper sequencing order of the codes. Look in the ICD 10-CM Alphabetic Index for Anemia/in (due to) (with)/chronic kidney disease D63.1. See the Code first note instructing to report the CKD (N18-) code first. Look in the ICD 10-CM Alphabetic Index for Disease/kidney/chronic/stage 3 (moderate) N18.3. Verification in the Tabular List verifies correct sequencing as N18.3, D63.1. • Question 4 10 out of 10 points A 12-year-old’s diabetes mellitus is well controlled with oral antidiabetic medications. The patient has no complications. Applying the coding concept from ICD-10-CM guidelines I.C.4.a.1., I.C.4.a.2., and I.C.4.a.3, what ICD-10-CM code(s) is/are reported? a. E11.9, Z79.84 a. E11.9, Z79.84 Response Feedback: Rationale: According to ICD-10-CM Official Coding Guidelines, Section I.C.4.a.1., the age of the patient is not the determining factor in what type of diabetes is coded. In addition, Section I.C.4.a.2 says if the type of diabetes mellitus is not documented in the medical record the default type is type 2. To find the code, look in the ICD-10-CM Alphabetic Index for Diabetes, diabetic (mellitus) (sugar). The default code is E11.9. Verification in the Tabular List verifies code selection. ICD-10-CM guideline I.C.4.a.3 directs the coder to report V79.84 to indicate the patient uses oral hypoglycemic or antidiabetic drugs. Look in the Alphabetic Index for Long-term (current) (prophylactic) drug therapy (use of)/oral/antidiabetic Z79.84. • Question 5 0 out of 10 points A patient with a four-year history of eating disorders is seen in the physician's office due to significant weight loss over the past three months. She went from 82 pounds down to 53 pounds due to restricting her food intake. She is diagnosed with anorexia nervosa. Select the diagnosis code(s). c. F50.01, R63.4 d. F50.01 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Anorexia/nervosa/restricting type which directs you to code F50.01. The patient is losing weight due to restricting her intake of food; this is considered restricting type. Weight loss is integral to the diagnosis of anorexia nervosa; therefore, no additional codes are assigned. Verify code selection in the Tabular List. • Question 6 10 out of 10 points Mr. Elliot visits the surgeon for evaluation for a wedge resection of left lung cancer. During the admission, the patient reports pain in the chest due to the malignancy. Applying the coding concept from ICD-10-CM guideline I.C.6.b.5., what ICD-10-CM code(s) should be reported? b. C34.92, G89.3 b. C34.92, G89.3 Response Feedback: Rationale: According to ICD-10-CM Official Coding Guidelines, 1.C.6.b.5, when the reason for the admission/encounter is management of the neoplasm and the pain associated with the neoplasm is also documented, code G89.3 may be assigned as an additional diagnosis. In the Table of Neoplasms, look for lung and select the code from the Malignant Primary column. The Tabular List indicates a 5th character 2 for the left lung. To report the pain associated with the neoplasm, look in the ICD-10-CM Alphabetic Index for Pain/due to cancer G89.3. • Question 7 10 out of 10 points A patient is having phacoemulsification of an age-related nuclear cataract of the left eye. What ICD-10-CM code is reported? a. H25.12 a. H25.12 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Cataract/age-related and you are directed to see Cataract, senile. Cataract/senile/nuclear (sclerosis) directs you to H25.1-. A 5th character 2 is selected for the left eye. • Question 8 10 out of 10 points A patient presents with right ear pain and fever. The provider diagnoses acute otitis media. What ICD-10-CM code(s) is/are reported? d. H66.91 d. H66.91 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Otitis (acute)/media/acute, subacute H66.90. In reviewing the Tabular List, H66.90 is unspecified and there are more specific codes that indicate laterality. The 5th character 1 indicates the right ear. Right ear pain (H92.01) and fever (R50.9) are signs/symptoms for the acute otitis media and not separately reported (refer to ICD-10-CM guideline I.B.5.). • Question 9 10 out of 10 points If an ST elevation myocardial infarction coverts to a non ST elevation myocardial infarction in the course of thrombolytic therapy, how is it coded? Reference ICD-10-CM guideline I.C.9.e.1. c. Code only STEMI c. Code only STEMI Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section 1.C.9.e.1., state that if STEMI converts to NSTEMI due to thrombolytic therapy, it is still coded as STEMI. • Question 10 10 out of 10 points A patient presents for a liver transplant. The provider documents the patient has Laennec’s cirrhosis associated with long term alcohol dependent use. What is the diagnosis code for this encounter? b. K70.30, F10.20 b. K70.30, F10.20 Response Feedback: Rationale: In the ICD 10-CM Alphabetic Index, look for Cirrhosis, cirrhotic (hepatic) (liver)/Laennec’s /alcoholic K70.30. In this scenario the patient has a history of alcohol use making K70.30 the correct code. There is an instructional note under category code K70 to use additional code to identify alcohol abuse and dependence. The patient is alcohol dependent. In the Alphabetic Index look for Dependence/alcohol referring you to code F10.20. Verify code selection in the Tabular List. Sunday, November 19, 2017 9:07:46 AM MST • Question 1 10 out of 10 points A 22-year-old female is admitted to ICU for acute renal (kidney) failure due to sepsis (causal organism unknown). Applying the coding concept from ICD-10-CM guideline I.C.1.d.1.b. what ICD-10-CM codes are reported (in the correct sequencing)? a. A41.9, R65.20, N17.9 a. A41.9, R65.20, N17.9 Response Feedback: Rationale: ICD-10-CM guideline I.C.1.d.1.b indicates: The coding of severe sepsis requires a minimum of two codes. First, a code for the underlying systemic infection, followed by a code from subcategory R65.2, Severe sepsis. If the causal organism is not documented, assign code A41.9, Sepsis, unspecified organism, for the infection. Additional codes(s) for the associated acute organ dysfunction are also required (if present). The first code to report is sepsis; look for the main term Sepsis in the ICD 10-CM Alphabetic Index referring you to code A41.9. Next, look for Sepsis/with organ dysfunction (acute) (multiple) referring you to code R65.20. For the last code, look for Failure/renal/acute referring you to code N17.9. In the Tabular List you will find an instructional note under subcategory R56.2 indicating what codes should be reported first and what codes should be reported as additional codes. • Question 2 10 out of 10 points A 45-year-old female with ovarian cancer visits her oncologist to receive an injection of Procrit®. The Procrit® has been prescribed to her for treatment of her anemia resulting from antineoplastic chemotherapy treatment. Applying the coding concept from ICD-10-CM guidelines I.C.2.c.2. What ICD-10-CM codes should be reported? a. D64.81, C56.9, T45.1X5A a. D64.81, C56.9, T45.1X5A Response Feedback: Rationale: According to ICD-10-CM guidelines 1.C.2.c.2., because the treatment is directed at the anemia associated with chemotherapy, and the treatment is only for the anemia, the anemia should be sequenced first, followed by the appropriate codes for the neoplasm and the adverse effect (T45.1X5). Look in the ICD 10-CM Alphabetic Index for Anemia/due to (in) (with)/antineoplastic chemotherapy (D64.81). According to guideline 1.C.2.c.2. the malignancy is reported secondarily followed by code T45.1X5. Look in the ICD-10-CM Table of Neoplasms for ovary and report the code from the Malignant Primary column (C56.-). In the Tabular List, C56.9 is reported because the laterality is not stated. Next, to locate T45.1X5 look in the Table of Drugs and Chemicals for Antineoplastic NEC and selecting the code from the Adverse effect column (T45.1X5). In the Tabular List, T45.1X5 requires a 7th character extender. A is selected because this is considered active treatment. • Question 3 10 out of 10 points Referencing ICD-10-CM guideline I.A.13, when using a code from category D63 it is also necessary to code first: c. The chronic condition causing the anemia c. The chronic condition causing the anemia Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section I.A.13., state when using a code from a category that indicates "in diseases classified elsewhere", such as in category D63, it is necessary to code first, the chronic condition (underlying condition) causing the anemia. The codes from category D63 are manifestation codes that must be reported as the additional code following the underlying condition. • Question 4 10 out of 10 points A type 2 diabetic patient with diabetic retinopathy visits his ophthalmologist for blurred vision. After performing a visual acuity test and a dilated eye exam, the provider states the patient has macular edema. Applying the coding concept from ICD-10-CM Coding guideline I.C.4.a., what ICD-10-CM code is reported? a. E11.311 a. E11.311 Response Feedback: Rationale: According to ICD-10-CM Official Coding Guidelines, Section I.C.4.a the diabetes codes are combination codes that include the type of diabetes, the body system affected, and the complications affecting that body system. To locate the codes in the ICD-10-CM code book, look in the ICD-10-CM Alphabetic Index for Diabetes, diabetic/with/retinopathy/with macular edema E11.311. Verify code choice in the Tabular List. • Question 5 10 out of 10 points A mother brings her son into the doctor because he has been getting in trouble in school for his behavior. He is not paying attention or following the instructions. He is constantly losing his pencil and forgetting to bring in his homework. After evaluating the child, the provider diagnoses him with attention deficit disorder, predominately inattentive type, and sends the patient for a consultation with a psychiatrist to see if medication can help. Select the diagnosis code. a. F90.0 a. F90.0 Response Feedback: Rationale: The patient is diagnosed with Attention Deficit Disorder (ADD), predominately inattentive type. In the ICD 10-CM Alphabetic Index, look for Disorder (of)/attention-deficit hyperactivity (adolescent) (adult) (child)/inattentive type F90.0. Verify code selection in the Tabular List. • Question 6 0 out of 10 points Mr. Elliot visits the surgeon for evaluation for a wedge resection of left lung cancer. During the admission, the patient reports pain in the chest due to the malignancy. Applying the coding concept from ICD-10-CM guideline I.C.6.b.5., what ICD-10-CM code(s) should be reported? c. G89.3, C34.92 b. C34.92, G89.3 Response Feedback: Rationale: According to ICD-10-CM Official Coding Guidelines, 1.C.6.b.5, when the reason for the admission/encounter is management of the neoplasm and the pain associated with the neoplasm is also documented, code G89.3 may be assigned as an additional diagnosis. In the Table of Neoplasms, look for lung and select the code from the Malignant Primary column. The Tabular List indicates a 5th character 2 for the left lung. To report the pain associated with the neoplasm, look in the ICD-10-CM Alphabetic Index for Pain/due to cancer G89.3. • Question 7 10 out of 10 points A patient presents with pigmentary glaucoma bilaterally, moderate stage on the right, mild stage on the left. Reference ICD-10-CM guideline I.C.7.a.3. What ICD-10-CM code(s) is/are reported? d. H40.1312, H40.1321 d. H40.1312, H40.1321 Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section 1.C.7.a.3., state when the glaucoma codes report laterality, and each eye is in a different stage, a code is reported for each eye. Look in the ICD-10-CM Alphabetic Index for Glaucoma/pigmentary and you are directed to see Glaucoma, open angle, primary, pigmentary. This path directs you to code H40.13-. In the Tabular List, 6th character 1 indicates the right eye, 7th character 2 indicates moderate stage. For the left eye, 6th character 2 indicates the left eye and 7th character 1 indicates mild stage. The moderate stage is reported first because it is more severe. • Question 8 10 out of 10 points A patient presents with right ear pain and fever. The provider diagnoses acute otitis media. What ICD-10-CM code(s) is/are reported? d. H66.91 d. H66.91 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Otitis (acute)/media/acute, subacute H66.90. In reviewing the Tabular List, H66.90 is unspecified and there are more specific codes that indicate laterality. The 5th character 1 indicates the right ear. Right ear pain (H92.01) and fever (R50.9) are signs/symptoms for the acute otitis media and not separately reported (refer to ICD-10-CM guideline I.B.5.). • Question 9 10 out of 10 points Applying the coding concept from ICD-10-CM guideline I.C.9.a.5, how do you code hypertensive retinopathy? d. Sequencing is based on the reason for the encounter. d. Sequencing is based on the reason for the encounter. Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines, Section I.C.9.a.5, state Background retinopathy and retinal vascular changes, should be used with a code from category I10-I15 to identify the hypertension. Sequencing is based on the reason for the encounter. • Question 10 10 out of 10 points A 12-year-old child presents to the ED with an acute exacerbation of asthma. The patient is wheezing and is having difficulty breathing. She is not responding to the therapy. The physician documents as the final diagnosis asthma with status asthmaticus. What ICD-10-CM code(s) is/are reported? c. J45.902 c. J45.902 Response Feedback: Rationale: The final diagnosis is asthma with status asthmaticus. To locate the code in the ICD 10-CM Alphabetic Index, look for Asthma/with/status asthmaticus, J45.902. Verify code selection in the Tabular List. Sunday, November 19, 2017 9:08:07 AM MST • Question 1 4 out of 4 points What does the 4th character in diabetes mellitus diabetes codes indicate? c. Any complication associated with diabetes. c. Any complication associated with diabetes. Response Feedback: Rationale: The 4th character in diabetes mellitus codes indicates the complication associated with diabetes. For example, subcategory code E10.2 indicates a person that has renal (kidney) complications due to diabetes. • Question 2 4 out of 4 points If a diabetic patient uses insulin, and the type of diabetes is not documented, what type of diabetes would be coded according to ICD-10-CM guidelines? b. Type 2 b. Type 2 Response Feedback: Rationale: Some patients with type 2 diabetes mellitus are unable to control their blood sugar through diet and oral medication alone and do require insulin. If the documentation in a medical record does not indicate the type of diabetes but does indicate that the patient uses insulin, the diabetes is reported as type 2. Refer to ICD-10-CM guidelines I.C.4.a.3. • Question 3 4 out of 4 points In ICD-10-CM what condition is reported as the default code when the provider documents urosepsis? c. The provider must be queried before an ICD-10-CM code can be applied. c. The provider must be queried before an ICD-10-CM code can be applied. Response Feedback: Rationale: ICD-10-CM guideline I.C.1.d.1.a.(ii) indicates urosepsis is a nonspecific term. It is not to be considered synonymous with sepsis. Urosepsis does not have a default code. If the provider documents urosepsis without additional information, the provider must be queried before an ICD-10-CM code can be applied. • Question 4 4 out of 4 points Pneumonia due to adenovirus. What ICD-10-CM code is reported? a. J12.0 a. J12.0 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Pneumonia/adenoviral and you are directed to code J12.0. Verification in the Tabular List confirms code selection. • Question 5 4 out of 4 points When the type of diabetes mellitus is not documented in the medical note, what is used as the default type? c. Type 2 c. Type 2 Response Feedback: Rationale: ICD-10-CM guideline I.C.4.a.2 indicates when the type of diabetes mellitus is not documented the default is E11.-, type 2 diabetes mellitus. • Question 6 4 out of 4 points A 21 year-old male is brought into the ED by his father who states that his son is dizzy and has anxiety. The ED provider runs a drug screen test and the test comes back positive for marijuana use. The final diagnosis is documented as marijuana abuse with anxiety disorder. What ICD-10-CM code is reported? a. F12.180 a. F12.180 Response Feedback: Rationale: The diagnosis is abuse of marijuana (cannabis). Look in the ICD-10-CM Alphabetic Index look for Abuse/drug NEC/cannabis/with/anxiety disorder which directs the coder to F12.180. Verify code selection in the Tabular List. • Question 7 0 out of 4 points A patient has a history of MRSA. She has just been diagnosed with pneumonia due to possible staphylococcus aureus. What ICD-10-CM code(s) is/are reported? d. J18.9, B95.62 a. J18.9, Z86.14 Response Feedback: Rationale: The verbiage possible staphylococcus aureus is an uncertain diagnosis and per ICD-10-CM guidelines should not be coded. The definitive diagnosis is pneumonia reported with code J18.9 which is found in the ICD-10-CM Alphabetic Index by looking for Pneumonia. The patient also has a history of MRSA. Look in the Alphabetic Index for History/personal (of)/Methicillin resistant Staphylococcus aureus (MRSA) referring you to Z86.14. Verify code selection in the Tabular List. • Question 8 4 out of 4 points A 32 year-old male was seen in the ASC for removal of two lipomas. One was located on his back and the other was located on the right forearm. Both involved subcutaneous tissue. What ICD-10-CM code(s) is/are reported? a. D17.21, D17.1 a. D17.21, D17.1 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Lipoma/site classification/arms (skin) (subcutaneous) D17.2-. In the Tabular List, a 5th character 1 is selected to indicate the right arm. Next, look for Lipoma/site classification/trunk (skin) (subcutaneous) D17.1. Verify code selection in the Tabular List. • Question 9 4 out of 4 points What ICD-10-CM code is reported for a patient who is a habitual abuser of cannabis? b. F12.10 b. F12.10 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Abuse/drug/cannabis guiding you to subcategory code F12.10. Verify in the Tabular List. • Question 10 0 out of 4 points A patient presents to the ED with weakness on the left side and aphasia. Tests are ordered and the patient is admitted with a cerebrovascular accident (CVA). What ICD-10-CM code(s) is/are reported? b. R53.1, R47.01 c. I63.9 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Accident/cerebrovascular (embolic) (ischemic) (thrombotic) guiding you to I63.9. A CVA is also known as a stroke. Verify code selection in the Tabular List. • Question 11 0 out of 4 points A 32 year-old patient with an ophthalmoplegic migraine is not responding to medication and is admitted to the observation unit. What ICD-10-CM code is reported? b. G43.B0 a. G43.B1 Response Feedback: Rationale: When a migraine does not respond to medication it is considered intractable. In the ICD-10-CM Alphabetic Index, look for Migraine/ophthalmoplegic/intractable referring you to G43.B1. Verify code selection in the Tabular List. The note under category code G43 Migraine confirms that pharmacoresistant is considered intractable. • Question 12 0 out of 4 points A 45 year-old patient is scheduled to have an INFUSAID pump installed. He has primary liver cancer and the pump is being inserted for continuous administration of 5-FU. A pocket is created just under the skin and the pump is placed in the pocket. A catheter is attached to the pump and to the subclavian vein. The pump is filled with a chemotherapy agent provided by the hospital and the patient is observed for adverse reaction and discharged to home. What ICD-10-CM codes are reported? b. C22.8, Z51.11 a. Z51.11, C22.8 Response Feedback: Rationale: ICD-10-CM Guideline I.C.2.e.2. indicates an encounter for chemotherapy code is to be reported as the primary code with a code for the cancer as secondary when the reason for the visit is solely for chemotherapy. Look in the ICD-10-CM Alphabetic Index for Chemotherapy (session) (for)/cancer Z51.11. For the malignancy, look in the ICD-10-CM Table of Neoplasms for liver/primary and use the code from the Malignant Primary column which directs the coder to C22.8. Verify code selection in the Tabular List. • Question 13 4 out of 4 points What ICD-10-CM code is used for the first episode of an acute myocardial infarction? d. I21.3 d. I21.3 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Infarct, infarction/myocardium, myocardial (acute) (with stated duration of 4 weeks or less) guiding you to I21.3. Verify code selection in the Tabular List. • Question 14 0 out of 4 points The patient has a significant visual impairment (category 2) due to astigmatism in the left eye. It is corrected with glasses. The right eye has normal vision. What ICD-10-CM code(s) is/are reported? c. H52.212 a. H52.202, H54.52 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Impaired, impairment (function)/vision NEC referring you to H54.7. In the Tabular List category H54 has a note to see the definition of visual impairment categories. Category 2 is considered low vision. Looking through the codes, low vision in the left eye is reported with H54.52. Or, you can look in the Alphabetic Index for Low/vision/one eye/left (normal vision on right) referring you to H54.52. It is important to read the instructional notes in the Tabular List that are associated with categories before selecting your code. Category H54 also has a note to code first any cause of the blindness. In this case, the low vision is due to the astigmatism. Look in the Alphabetic Index for Astigmatism referring you to H52.20-. In the Tabular List, H52.202 is reported for the left eye. • Question 15 4 out of 4 points A 35 year-old woman is experiencing dizziness with nausea and vomiting. The provider documents auditory vertigo of both ears, possible Meniere’s disease. What ICD-10-CM code(s) is/are reported? d. H81.313 d. H81.313 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Vertigo/auditory telling you to see Vertigo, aural. Vertigo/aural which guides you to code H81.31-. In the Tabular List 6th character 3 is selected because the condition is bilateral. The Meniere’s disease is a possible diagnosis and is not reported. Per ICD-10-CM guideline I.B.5 signs and symptoms that are associated routinely with a disease process should not be assigned as additional codes. Dizziness, nausea and vomiting are symptoms of the vertigo and are not reported separately. Verify code selection in the Tabular List. • Question 16 0 out of 4 points After referral from the ED, patient is seeing the ophthalmologist to examine an old injury with retained magnetic iron metal foreign body in his posterior wall within the right eye with the possibility of infection. What ICD-10-CM codes are reported? a. S05.51XA, Z18.11 b. H44.641, Z18.11 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Foreign body/intraocular/old, retained/magnetic/posterior wall guiding you to code H44.64-. In the Tabular List, 6th character 1 is assigned for the right eye. Subcategory code H44.6 has instructions to use an additional code to identify the foreign body (Z18.11). Z18.11 identifies a retained magnetic fragment. Verify code selection in the Tabular List. • Question 17 0 out of 4 points An elderly male patient presents to the ED complaining of a high fever the day prior to the encounter and of extreme lethargy. He has a history of benign hypertension which has been elevated. On arrival he was examined and admitted, with possible septic urinary tract infection and concern for his elevated blood pressure. He was noted to have hematuria. Positive UTI and pseudomonas showed in the urine culture and IV antibiotics were administered. During the course of the day, his fever decreased and his lethargy improved. He was noted to have hematuria. As the IV fluids were decreased, he resumed a benign hypertensive state. On the next hospital day, the urine was clear and he was discharged on oral antibiotics, with septicemia ruled out. What ICD-10-CM codes should be reported? c. I10, B95.6, R31.9, N39.0 d. N39.0, B96.5, I10 Response Feedback: Rationale: Per ICD-10-CM guideline IV.H Uncertain Diagnosis, we would not code diagnoses documented as probable, suspected, questionable, rule out or working diagnosis or other similar terms indicating uncertainty. During the course of the patient’s stay septicemia was ruled out and would not be coded. The reason for the visit was to treat the urinary tract infection, making that code primary. Look in the ICD-10-CM Alphabetic Index for Infection/urinary (tract) NEC directing you to code N39.0. Look in the Tabular List for code N39.0. There is an instructional note stating, “Use additional code to identify infectious agent.” This note must always be followed when the organism is known. The note states “Pseudomonas showed in the urine culture.” Look in the Alphabetic Index for Infection/Pseudomonas NEC/as cause of disease classified elsewhere which directs you to B96.5. Hematuria (R31.9) is integral to a urinary tract infection and is not reported separately. Hypertension is coded because it is a coexisting condition that was being affected by having the UTI. Look in the Alphabetic Index for Hypertension which directs you to I10. Verify code selection in the Tabular List. • Question 18 0 out of 4 points Four years post hepatic transplant, the patient is diagnosed with combined hepatocellular carcinoma and cholangiocarcinoma of the liver. What ICD-10-CM codes are reported? c. C80.2, C22.0, C22.1, Z94.4 d. T86.49, C80.2, C22.0 Response Feedback: Rationale: ICD-10-CM guideline I.C.2.r indicates this situation requires three codes (complication, neoplasm associated with transplant organ, and the malignancy) and is to be coded as a transplant complication. The guideline tells us to assign first the appropriate code from T86.-, Complications of transplanted organs, followed by code C80.2 Malignant neoplasm with transplanted organ, then to use an additional code for the specific malignancy. Hepatic means related to the liver. Look in the ICD-10-CM Alphabetic Index for Complication/transplant/liver/specified type NEC which directs you to T86.49. Next, the neoplasm associated with the transplant organ is coded. Look in the Alphabetic Index for Complication/transplant/malignant neoplasm which directs you to C80.2. In the Tabular List C80.2 has a note to code first the complication code (T86.-) and to use an additional code for the specific malignancy. Cholangiocarcinoma is bile duct carcinoma. Look in the Alphabetic Index for Carcinoma/hepatocellular/with bile duct, mixed which directs you to C22.0. You can also look for Cholangiocarcinoma/with hepatocellular carcinoma, combined which directs you to C22.0. If you look to report the status post hepatic transplant, look in the Alphabetic Index for Transplant (ed) status)/liver Z94.4. However, there is an Excludes1 note which indicates this code is not reported for post-transplant complications so Z94.4 is not reported. Verify code selection in the Tabular List. • Question 19 0 out of 4 points A young female, was brought to the clinic by her sister. She has had periods of severe depression for many years and is on Lithium. Her provider also manages her manic-depressive psychosis, hypothyroidism, and migraine headaches. Additional medications are Synthroid and Midrin. During the past week, she became manic, running all her credit cards to the limit, getting inappropriately involved in a friend’s suicide attempt, quitting her job, and trying to take over the pulpit at church. On the day of the clinic visit, she threatened to strike the telephone repairman with a lead pipe. She was admitted for Lithium adjustment. Diagnoses are: moderate manic-depressive bipolar with circular current manic state, hypothyroidism and migraine. What ICD-10-CM codes are reported? a. F31.32, E03.9, G43.909 b. F31.12, E03.9, G43.909 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Disorder/bipolar/current episode/manic/without psychotic features/moderate guiding you to code F31.12. No code assignment is necessary for depression because depression is a component of bipolar disorder. Although not psychiatric conditions, both hypothyroidism and migraine headaches are coexisting conditions under treatment and are coded. In the Alphabetic Index, look for Hypothyroidism which directs you to E03.9 and look for Migraine directing you to code G43.90- . Verify the codes in the Tabular List. When reviewing code G43.90 in the Tabular List, a 6th character of 9 is selected because there is no mention of an intractable migraine or status migrainosus. • Question 20 4 out of 4 points A 45 year-old-male patient has developed an ulcer on his upper back. He has had diabetes for several years and is on insulin. The provider determines that the ulcer is due to his diabetes. What ICD-10-CM codes are reported? d. E11.622, L98.429, Z79.4 d. E11.622, L98.429, Z79.4 Response Feedback: Rationale: ICD-10-CM guideline I.C.4.a.2 indicates if the type of diabetes is not documented in the medical record the default type is 2. ICD-10-CM guideline I.C.4.a.3 indicates the use of insulin does not mean that a patient is a type 1 diabetic. If the documentation indicates that the patient uses insulin, but does not indicate the type of diabetes you report type 2. For type 2 patients, code Z79.4 is reported to indicate long-term use of insulin. The ulcer is due to the diabetes. In the ICD-10-CM Alphabetic Index look for Diabetes, diabetic (mellitus) (sugar)/with/skin ulcer NEC which directs you to E11.622. In the Tabular List E11.622 has a note to use an additional code to identify the site of the ulcer. Look in the Alphabetic Index for Ulcer/back which directs the coder to L98.429. The severity of the ulcer is not provided. Also look for Long-term (current) (prophylactic) drug therapy (use of)/insulin which directs you to Z79.4. Verify code selections in the Tabular List. • Question 21 4 out of 4 points The patient was given thrombolytic therapy for an acute myocardial infarction (STEMI) of the anterolateral wall which converted to a NSTEMI. What ICD-10-CM code is reported? c. I21.09 c. I21.09 Response Feedback: Rationale: According to ICD-10-CM guideline I.C.9.e.1, the ICD-10-CM codes for acute myocardial infarction (AMI) identify the site, such as anterolateral wall or true posterior wall. The same section goes on to state that if STEMI converts to NSTEMI due to thrombolytic therapy, it is still coded as STEMI. Look in the ICD-10-CM Alphabetic Index for Infarct, infarction/myocardium, myocardial (acute) (with stated duration of 4 weeks or less)/ST elevation (STEMI)/anterior (anteroapical) (anterolateral) (anteroseptal) (Q wave) (wall) which directs you to I21.09. Verify code selection in the Tabular List. • Question 22 4 out of 4 points A patient is admitted after being found unresponsive at home. The patient had right-sided hemiplegia and aphasia from a previous CVA. The provider documents a current cerebral infarction due to occlusion of the right middle cerebral artery as the final diagnosis and the patient is transferred for rehabilitation. What ICD-10-CM code(s) is/are reported? a. I63.511, I69.351, I69.320 a. I63.511, I69.351, I69.320 Response Feedback: Rationale: Refer to ICD-10-CM guideline I.C.9.d.2. Look in the ICD-10-CM Alphabetic Index for Infarct, infarction/cerebral/due to/occlusion NEC/cerebral arteries directing you to code I63.5-. Report I63.511 Cerebral infarct due to unspecified occlusion or stenosis of right middle cerebral artery. This patient has a history of CVA with right-sided hemiplegia and aphasia. Look in the Alphabetic Index for Sequelae (of)/infarction/cerebral/hemiplegia which directs the coder to I69.35-. Also look for Sequelae/infarction/cerebral/aphasia I69.320. Verify in the Tabular List I69.351 Hemiplegia and hemiparesis following cerebral infarction affecting right dominant side. Per ICD-10-CM guideline I.C.9.d.1 because the right side was affected and we do not know the dominant side, the default for dominance is right. • Question 23 4 out of 4 points Friends brought a young male with type 1 diabetes to the emergency department, in a comatose state. He was admitted with ketoacidosis and was resuscitated with saline hydration via insulin drip. After regaining consciousness, the patient reported that the morning of admission he was experiencing nausea and vomiting and decided not to take his insulin because he had not eaten. He was treated with intravenous hydration and insulin drip. By the following morning, his laboratory work was within normal range and he was experiencing no symptoms. What ICD-10-CM codes are reported? d. E10.11 d. E10.11 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Diabetes, diabetic (mellitus) (sugar)/type 1/with/ketoacidosis/with coma guiding you to subcategory code E10.11. Code Z79.4 Long term use of insulin is not required for a type 1 diabetic because these patients are insulin dependent. Verify code selection in the Tabular List. • Question 24 0 out of 4 points A young male, was brought to the clinic by his mom. He has had periods of major depression for many years and is on Lithium. His provider also manages his migraine headaches and epilepsy. During the past week, he became psychotic, hearing voices to kill himself and intense feelings of worthlessness. On the day of the clinic visit, he had an epileptic seizure that could not be controlled by medication. He was admitted for Lithium adjustment. Final diagnoses are: Severe depression with psychotic behavior and epileptic seizure poorly controlled with medication. What ICD-10-CM codes should be reported? b. F33.3, G43.909, G40.909 c. F33.3, G40.919 Response Feedback: Rationale: Only two final diagnoses are documented the depression and epilepsy. The migraine headache is not coded because it was not treated or listed as a final diagnosis. In the ICD-10-CM Alphabetic Index look for Depression/major recurrent – see Disorder, depressive, recurrent. Look for Disorder/depressive/major recurrent referring you to code F33.9. The patient has severe depression and became psychotic. Look for Disorder/depressive/recurrent/current episode/severe/with psychotic symptoms referring you to code F33.3. Next, in the Alphabetic Index look for Epilepsy, epileptic, epilepsia (attack) (cerebral) (convulsion) (fit) seizure)/intractable G40.919. The mention of poorly controlled with medication makes the epilepsy intractable. • Question 25 4 out of 4 points What ICD-10-CM codes are reported for uncontrolled hypertension with stage 3 chronic kidney disease? b. I12.9, N18.3 b. I12.9, N18.3 Response Feedback: Rationale: Per ICD-10-CM guideline I.C.9.a.2 assign codes from category I12, Hypertensive chronic kidney disease, when both hypertension and a condition classified to category N18, Chronic kidney disease are present. In the ICD-10-CM Alphabetic Index look for Hypertension/kidney/with/stage 1 through stage 4 chronic kidney disease which directs you to code I12.9. In the Tabular List, there is a note to use an additional code to identify the stage of chronic kidney disease (N18.1-N18.4 or N18.9). Look in the Alphabetic Index for Disease, diseased/kidney/chronic/stage 3 (moderate) directing you to code N18.3. Verify code selection in the Tabular List. Sunday, November 19, 2017 9:08:30 AM MST • Question 1 4 out of 4 points When is it appropriate to use history of malignancy from category Z85? a. It has been excised, no evidence of any existing primary malignancy, and there is no further treatment directed to the site. a. It has been excised, no evidence of any existing primary malignancy, and there is no further treatment directed to the site. Response Feedback: Rationale: ICD-10-CM guideline 1.C.2.m indicates that when a primary malignancy has been previously excised or eradicated from its site and there is no further treatment directed to that site and there is no evidence of any existing primary malignancy, a code from category Z85 Personal history of malignant neoplasm is used to indicate the former site of the malignancy. • Question 2 4 out of 4 points According to the ICD-10-CM guidelines, how is bilateral glaucoma of the same type and stage reported? c. A bilateral code can be used to report the type of glaucoma and the stage of glaucoma. c. A bilateral code can be used to report the type of glaucoma and the stage of glaucoma. Response Feedback: Rationale: In ICD-10-CM guideline I.C.7.a.2 states when a patient has bilateral glaucoma and both eyes are documented as the same type and stage, and there is a code for bilateral glaucoma, report only the code for the type of glaucoma, bilateral, with the 7th character for the stage. • Question 3 4 out of 4 points When do you code acute respiratory failure as a secondary diagnosis? d. When it occurs after admission. d. When it occurs after admission. Response Feedback: Rationale: According to ICD-10-CM guideline I.C.10.b.2., respiratory failure may be listed as a secondary diagnosis if it occurs after admission, or if it is present on admission, but does not meet the definition of principal diagnosis. • Question 4 4 out of 4 points What does the 4th character in diabetes mellitus diabetes codes indicate? b. Any complication associated with diabetes. b. Any complication associated with diabetes. Response Feedback: Rationale: The 4th character in diabetes mellitus codes indicates the complication associated with diabetes. For example, subcategory code E10.2 indicates a person that has renal (kidney) complications due to diabetes. • Question 5 0 out of 4 points Patient with postoperative anemia due to acute blood loss during the surgery needs a blood transfusion. What ICD-10-CM code is reported? c. D50.0 a. D62 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Anemia/postoperative (postprocedural)/due to (acute) blood loss guiding you to code D62. Verify code selection in the Tabular List. • Question 6 4 out of 4 points A 32 year-old patient with hyperthyroidism has an ultrasound to determine why her neck is enlarged. The results of the ultrasound reveal a uninodular goiter. What ICD-10-CM code is reported? a. E05.10 a. E05.10 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Hyperthyroidism/with/goiter/nodular/uninodular which directs you to E05.10. The code can also be found by looking in the Alphabetic Index for Goiter/uninodular/toxic or with hyperthyroidism which guides you to code E05.10. Verify code selection in the Tabular List. • Question 7 4 out of 4 points A male patient is seen by his primary care provider for rectal bleeding and persistent intestinal cramps. After a colonoscopy with biopsy, the results come back and the provider documents that the patient has malignant neoplasm in his sigmoid colon. What ICD-10-CM code(s) is/are reported? a. C18.7 a. C18.7 Response Feedback: Rationale: According to the ICD-10-CM guideline when a definitive diagnosis is known, the related symptoms are not coded. In this case, only the malignant neoplasm of the sigmoid colon is reported. Look in the ICD-10-CM Table of Neoplasm for Colon and you are directed to see also Neoplasm, intestine, large. Look for intestine, intestinal/large/colon/sigmoid (flexure), and use the code from the Malignant Primary column C18.7. Verify code selection in the Tabular List. • Question 8 0 out of 4 points Patient is admitted to the hospital with streptococcal group B severe sepsis which has caused pneumonia. What codes are assigned? c. A40.1, J15.3 b. A40.1, J15.3, R65.20 Response Feedback: Rationale: Per ICD-10-CM guideline I.C.1.d.4 if the reason for admission is both sepsis or severe sepsis and a localized infection, such as pneumonia or cellulitis, a code for the systemic infection is assigned first, followed by the code for the localized infection. To find the codes in the ICD-10-CM Alphabetic Index, look for Sepsis/Streptococcus, streptococcal/group/ B which directs the coder to A40.1 for the Systemic infection. To locate the code for sepsis, look for Sepsis/severe which directs the coder to R65.20. Pneumonia can be found in the Alphabetic Index by looking for Pneumonia/in (due to)/Streptococcus/group B which directs the coder to J15.3. Verify all codes in the Tabular List. Pay careful attention to the instructional notes in the Tabular List to help with sequencing. • Question 9 4 out of 4 points A 35 year-old woman is experiencing dizziness with nausea and vomiting. The provider documents auditory vertigo of both ears, possible Meniere’s disease. What ICD-10-CM code(s) is/are reported? d. H81.313 d. H81.313 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Vertigo/auditory telling you to see Vertigo, aural. Vertigo/aural which guides you to code H81.31-. In the Tabular List 6th character 3 is selected because the condition is bilateral. The Meniere’s disease is a possible diagnosis and is not reported. Per ICD-10-CM guideline I.B.5 signs and symptoms that are associated routinely with a disease process should not be assigned as additional codes. Dizziness, nausea and vomiting are symptoms of the vertigo and are not reported separately. Verify code selection in the Tabular List. • Question 10 0 out of 4 points A patient returns to the provider for an injection to relieve low back pain from a car accident. What ICD-10-CM code(s) is/are reported? c. M54.5, G89.11 b. M54.5 Response Feedback: Rationale: Per ICD-10-CM guideline I.C.6.b.1, if the pain is not specified as acute or chronic, do not assign codes from category G89, except for post-thoracotomy pain, postoperative pain, neoplasm related pain or central pain syndrome. Look in the ICD-10-CM Alphabetic Index for Pain/low back which directs the coder to M54.5. Verify code selection in the Tabular List. • Question 11 4 out of 4 points A 70 year-old patient with COPD is admitted to the hospital for acute exacerbation of bronchial asthma. What diagnosis code is reported? d. J44.1 d. J44.1 Response Feedback: Rationale: COPD stands for Chronic Obstructive Pulmonary Disease. In the ICD-10-CM Alphabetic Index look for Asthma, asthmatic (bronchial)/with/chronic obstructive pulmonary disease/with/exacerbation (acute) referring you to J44.1. The code can also be located by look for Disease/lung/obstructive (chronic)/with/acute/exacerbation NEC guiding you to code J44.1. There is an includes under J44 which states chronic obstructive pulmonary disease includes asthma with chronic obstructive pulmonary disease. Verify code selection in the Tabular List. • Question 12 4 out of 4 points A 50 year-old patient has a mass removed from his chest. The surgeon sends it to pathology. The pathology report indicates the mass is a benign tumor. What ICD-10-CM code is reported? b. D36.7 b. D36.7 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, in the Table of Neoplasms, look for Chest (wall) NEC and report the code from the benign column, D36.7. Verify code selection in the Tabular List. • Question 13 4 out of 4 points A confirmed HIV positive patient who presents to the clinic for a medication refill for a condition not related to his HIV. What ICD-10-CM codes are reported? a. Z76.0, Z21 a. Z76.0, Z21 Response Feedback: Rationale: Per ICD-10-CM guideline I.C.1.a.2.d, Z21 Asymptomatic human immunodeficiency virus (HIV) infection, is to be applied when the patient without any documentation of symptoms is listed as being HIV positive, known HIV, HIV test positive, or similar terminology. In the ICD-10-CM Alphabetic Index look for HIV/positive, seropositive guiding you to code Z21. For medication refill look in the Alphabetic Index for Issue of/repeat prescription (appliance) (glasses) (medicinal substance, medicament, medicine) Z76.0. Because the main reason for the visit is for a medication refill unrelated to his HIV, the HIV code is not sequenced first. Verify code selection in the Tabular List. • Question 14 4 out of 4 points What is the time frame defining when pain becomes chronic? a. No time frame a. No time frame Response Feedback: Rationale: Per ICD-10-CM guidelines Section I.C.6.b.4, there is no time frame defining when pain becomes chronic pain. The provider’s documentation is used to guide when the pain is acute and when it is chronic. • Question 15 4 out of 4 points A 9 year-old with a history of reactive airway disease (RAD) was admitted into overnight observation with complaints of a two-day history of increased wheezing. Parents stated that nebulizer treatments were not helping. After monitoring and additional treatments given while in observation, breathing was stabilized. Documented diagnosis is RAD exacerbation. What ICD-10-CM code(s) is/are reported? c. J45.901 c. J45.901 Response Feedback: Rationale: RAD is an acronym for Reactive Airway Disease. Look in the ICD-10-CM Alphabetic Index for Disease, diseased/reactive airway and you are directed to see Asthma. Look for Asthma, asthmatic/with/exacerbation (acute) J45.901. Verify code selection in the Tabular List. According to the ICD-10-CM guidelines, when a definitive diagnosis is known, the related symptoms are not coded. • Question 16 4 out of 4 points A 33 year-old patient visits his primary care provider to discuss lap band procedure for his morbid obesity. His caloric intake is in excess of 4,000 calories per day and his BMI is currently 45. What ICD-10-CM code(s) is/are reported? d. E66.01, Z68.42 d. E66.01, Z68.42 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Obesity/morbid guiding you to code E66.01. In the Tabular List there is note under subcategory code E66 to use an additional code to identify the BMI (Z68.1-Z68.45). Look at this range in the Tabular List. The second code is Z68.42 indicating a BMI of 45.0 - 49.9 adult. This can be found in the Alphabetic Index by looking for Body, bodies/mass index (BMI)/adult/45.0-49.9 referring you to Z68.42. Verify code selection in the Tabular List. • Question 17 4 out of 4 points A patient with type 2 diabetes presents with diabetic macular edema and proliferative diabetic retinopathy in the right eye. What ICD-10-CM code(s) is/are reported? c. E11.3511 c. E11.3511 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index Diabetes, diabetic (mellitus) (sugar)/type2/with/retinopathy/proliferative/with macular edema which directs you to E11.351-. There is a checkmark next to the code in the Alphabetic Index reminding the coder to check the Tabular List for the 7th character to show laterality. From the Tabular List, assign 7th character 1 to identify the right eye. • Question 18 4 out of 4 points A young male, was brought to the clinic by his mom. He has had periods of major depression for many years and is on Lithium. His provider also manages his migraine headaches and epilepsy. During the past week, he became psychotic, hearing voices to kill himself and intense feelings of worthlessness. On the day of the clinic visit, he had an epileptic seizure that could not be controlled by medication. He was admitted for Lithium adjustment. Final diagnoses are: Severe depression with psychotic behavior and epileptic seizure poorly controlled with medication. What ICD-10-CM codes should be reported? a. F33.3, G40.919 a. F33.3, G40.919 Response Feedback: Rationale: Only two final diagnoses are documented the depression and epilepsy. The migraine headache is not coded because it was not treated or listed as a final diagnosis. In the ICD-10-CM Alphabetic Index look for Depression/major recurrent – see Disorder, depressive, recurrent. Look for Disorder/depressive/major recurrent referring you to code F33.9. The patient has severe depression and became psychotic. Look for Disorder/depressive/recurrent/current episode/severe/with psychotic symptoms referring you to code F33.3. Next, in the Alphabetic Index look for Epilepsy, epileptic, epilepsia (attack) (cerebral) (convulsion) (fit) seizure)/intractable G40.919. The mention of poorly controlled with medication makes the epilepsy intractable. • Question 19 4 out of 4 points A patient is being treated for ketoacidosis and diabetic coma due to malignant neoplasm of the pancreatic body. The patient uses insulin routinely. What ICD-10-CM codes are reported? a. C25.1, E08.11, Z79.4 a. C25.1, E08.11, Z79.4 Response Feedback: Rationale: The patient’s diabetes is due to the pancreatic cancer as an underlying condition. In the ICD-10-CM Alphabetic Index look for Diabetes, diabetic (mellitus) (sugar)/due to underlying condition/with/ketoacidosis/with coma E08.11. In the Tabular List under category code E08 an instructional note indicates to code the underlying condition first. In the Table of Neoplasms look for Neoplasm, neoplastic/pancreas/body and select the code from the Malignant Primary column which directs the coder to C25.1. There is also coding guidance under category code E08 to use additional code for patients who routinely use insulin. Report code Z79.4 which is found in the Alphabetic Index under Long-term (current) (prophylactic) drug therapy (use of)/insulin directing you to code Z79.4. Verify code selection in the Tabular List. • Question 20 4 out of 4 points A patient sees the nephrologist for a B-12 injection to treat erythropoietin resistant anemia due to stage 3 chronic kidney disease. What ICD-10-CM codes are reported? c. N18.3, D63.1 c. N18.3, D63.1 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Anemia/in (due to) (with)/chronic kidney disease or Anemia/erythropoietin resistant anemia (EPO resistant anemia) guiding you to code D63.1. In the Tabular List at D63.1 there is an instructional note stating to code first underlying chronic kidney disease. Look in the Alphabetic Index for Disease, diseased/kidney/chronic/stage 3 (moderate) guiding you to code N18.3. Verify code selection in the Tabular List. • Question 21 4 out of 4 points An elderly male patient presents to the ED complaining of a high fever the day prior to the encounter and of extreme lethargy. He has a history of benign hypertension which has been elevated. On arrival he was examined and admitted, with possible septic urinary tract infection and concern for his elevated blood pressure. He was noted to have hematuria. Positive UTI and pseudomonas showed in the urine culture and IV antibiotics were administered. During the course of the day, his fever decreased and his lethargy improved. He was noted to have hematuria. As the IV fluids were decreased, he resumed a benign hypertensive state. On the next hospital day, the urine was clear and he was discharged on oral antibiotics, with septicemia ruled out. What ICD-10-CM codes should be reported? c. N39.0, B96.5, I10 c. N39.0, B96.5, I10 Response Feedback: Rationale: Per ICD-10-CM guideline IV.H Uncertain Diagnosis, we would not code diagnoses documented as probable, suspected, questionable, rule out or working diagnosis or other similar terms indicating uncertainty. During the course of the patient’s stay septicemia was ruled out and would not be coded. The reason for the visit was to treat the urinary tract infection, making that code primary. Look in the ICD-10-CM Alphabetic Index for Infection/urinary (tract) NEC directing you to code N39.0. Look in the Tabular List for code N39.0. There is an instructional note stating, “Use additional code to identify infectious agent.” This note must always be followed when the organism is known. The note states “Pseudomonas showed in the urine culture.” Look in the Alphabetic Index for Infection/Pseudomonas NEC/as cause of disease classified elsewhere which directs you to B96.5. Hematuria (R31.9) is integral to a urinary tract infection and is not reported separately. Hypertension is coded because it is a coexisting condition that was being affected by having the UTI. Look in the Alphabetic Index for Hypertension which directs you to I10. Verify code selection in the Tabular List. • Question 22 0 out of 4 points A patient with metastatic bone cancer (primary site unknown) presents to the oncologist’s office for a chemotherapy treatment. On examination the oncologist finds the patient to be severely dehydrated and cancels the chemotherapy. The patient receives intravenous hydration in the office and reschedules the chemotherapy treatment. What ICD-10-CM codes are reported? d. C79.51, E86.0 c. E86.0, C79.51, C80.1 Response Feedback: Rationale: Per ICD-10-CM guideline I.C.2.c.3 when the admission/encounter is for management of dehydration due to the malignancy or therapy, or a combination of both, and only the dehydration is being treated (intravenous hydration); the dehydration is sequenced first, followed by the code(s) for the malignancy. The treatment is directed at the bone cancer or the metastatic site. In the ICD-10-CM Alphabetic Index look for Dehydration E86.0 In the ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/bone. Use the code from the Malignant Secondary column directing you to code C79.51. Also in the Table of Neoplasms look for unknown or unspecified site and use the code from the Malignant Primary column which directs the coder to C80.1. Verify the code selections in the Tabular List. • Question 23 4 out of 4 points The patient has a history of unstable angina, hypertension, and chronic systolic heart failure. He is seen in the ED after prolonged chest pain that was not relieved by medication. Cardiac enzymes are elevated, and EKG shows anterior infarct. A decision was made to perform a cardiac catheterization and coronary angiography. Left heart catheterization was performed in order to perform a left ventriculogram. He tolerated the procedure well and will be discharged. His final diagnosis is chronic systolic heart failure and hypertension. The two conditions are unrelated. What ICD-10-CM code(s) is/are reported? c. I50.22, I10 c. I50.22, I10 Response Feedback: Rationale: ICD-10-CM guideline I.C.9.a.1. indicates when the documentation specifically states the two conditions are unrelated between hypertension and heart disease, they are coded separately. In this case, there is no causal relationship coded. Look in the ICD-10-CM Alphabetic Index for Failure/heart/systolic (congestive)/chronic (congestive) directing you to I50.22. Then, look for Hypertension which directs you to I10. Verify code selection in the Tabular List. • Question 24 4 out of 4 points A patient with a history of hypertension controlled with medication presents to the outpatient hospital radiology department for an ultrasound due to a suspected suspicious mass. The patient’s provider performed an ACTH and a 24-hour urinary free cortisol and short suppression test confirming the diagnosis of Cushing’s disease. The radiology report indicated a 5.5 cm right adrenal mass that appeared well circumscribed and rounded. The final diagnosis indicated Cushing’s disease secondary to a right adrenal tumor. What ICD-10-CM codes are reported? a. D49.7, E24.9, I10 a. D49.7, E24.9, I10 Response Feedback: Rationale: The patient has Cushing’s disease secondary to an adrenal tumor. First code the adrenal tumor. We are told that there is a right adrenal tumor; however, we are not given more information as to whether it is benign or malignant. Look in the ICD-10-CM Table of Neoplasms for Neoplasm, neoplastic/adrenal and use the code from the Unspecified Behavior column directing you to D49.7. Next, in the ICD-10-CM Alphabetic Index find Cushing’s/syndrome or disease which directs the coder to E24.9. We are not told that the hypertension is secondary to the Cushing’s disease; therefore, look in the Alphabetic Index for Hypertension directing you to code I10. Verify all codes in the Tabular List. • Question 25 0 out of 4 points A patient is brought in by the ambulance with seizures. After examination and workup is complete, it is determined the seizures were due to alcohol abuse with intoxication. What ICD-10-CM code(s) is/are reported? b. F10.129 c. R56.9, F10.129 Response Feedback: Rationale: There is no indication this is an epileptic seizure or that there is a history of recurrent seizures or epileptic disorder, code G40.50- is not reported. This was a seizure brought on by the intake of alcohol. Look in the ICD-10-CM Alphabetic Index for Seizure(s) directing you to code R56.9. Documentation states alcohol abuse not alcoholism with intoxication. Look in the Alphabetic Index for Abuse/alcohol/with/intoxication directing you to F10.129. Verify code selection in the Tabular List. Sunday, November 19, 2017 9:08:52 AM MST • Question 1 0 out of 10 points A patient complains of a rash that is extremely itchy. It began when she started using a new laundry detergent. She is examined and the provider diagnoses her with dermatitis, due to exposure to the laundry detergent. What is the diagnosis code? c. L23.5 d. L24.0 Response Feedback: Rationale: The patient is diagnosed with dermatitis due to detergent. In the ICD-10-CM Alphabetic Index, look for Dermatitis/due to/detergents (contact) (irritant). You are referred to L24.0. Verify the code selection in the Tabular List. • Question 2 10 out of 10 points An MRI confirmed the patient has sciatica caused by a herniated disc between L5 and S1. She is scheduled for an injection in this office, after which she will be referred to a physical therapist in an effort to avoid surgery. Select the diagnosis code(s). a. M51.17 a. M51.17 Response Feedback: Rationale: L5 and S1 refer to the fifth lumbar disc and the first sacral disc in the vertebra. Look in the ICD-10-CM Alphabetic Index for Hernia, hernial/intervertebral cartilage or disc, you are referred to see Displacement, intervertebral disc. Look for Displacement, displaced/intervertebral disc NEC/ lumbosacral region/with neuritis, radiculitis, radiculopathy or sciatica M51.17. Verify code selection in the Tabular List. • Question 3 0 out of 10 points A patient returns to her gynecologist’s office to review the results of her ultrasound. She has been experiencing heavy bleeding and painful menstruation. The results of the ultrasound reveal the patient has a uterine fibroid measuring 4.0 cm. Select the diagnosis code(s). a. N94.6, N92.0, D25.9 d. D25.9 Response Feedback: Rationale: The patient is diagnosed with a uterine fibroid. The symptoms, heavy bleeding and painful menstruation, she is experiencing are integral to the definitive diagnosis and should not be coded. In the ICD-10-CM Alphabetic Index, look for main term Fibroid and then uterus. You are referred to D25.9.There is no location given of where the fibroid (leiomyoma) is located. Review of the code in the Tabular List confirms this is the correct code. • Question 4 10 out of 10 points A patient presented to the emergency department with second degree burns to both forearms, which makes up 9 percent TBSA (Total Body Surface Area). She is three months pregnant, 12 weeks. The burns are not affecting the pregnancy. Select the diagnosis codes. d. T22.212A, T22.211A, T31.0, Z33.1 d. T22.212A, T22.211A, T31.0, Z33.1 Response Feedback: Rationale: The pregnancy is incidental to the problem for which the patient is treated, so complication pregnancy code O09.90 is not reported. The first listed code is for the burns. The patient has a second degree burn to both forearms. In the ICD-10-CM Alphabetic Index, look for Burn/forearm/right/second degree T22.211 and Burn/forearm/left/second degree T22.212. The 7th character, A, completes the code to indicate initial encounter. A code from category T31 is coded to indicate the TBSA burned, as well as the percentage of the burn that is third degree. The TBSA is 9 percent and there are no third degree burns. Look for Burn/extent (percentage of body surface)/less than 10% percent T31.0. The last code is for the pregnancy. Look for State (of)/pregnant, incidental or Status (post)/pregnancy, incidental referring you to Z33.1. A code from category Z34 is not reported because that is if the patient was being seen for routine care or check-up of the pregnancy. • Question 5 10 out of 10 points Which statement is true regarding the perinatal period? b. It ends at 28 days b. It ends at 28 days Response Feedback: Rationale: According to the ICD-10-CM Guidelines for Coding and Reporting, Section I.C.16, “For coding and reporting purposes the perinatal period is defined as before birth through the 28th day following birth.” • Question 6 10 out of 10 points The hospital documentation states “normal vaginal delivery, live birth, female, with Down Syndrome.” Select the correct code(s) for the infant’s record. c. Z38.00, Q90.9 c. Z38.00, Q90.9 Response Feedback: Rationale: According to ICD-10-CM guideline I.C.17. for birth admission, the appropriate code from category Z38- Liveborn infants, according to the type of birth should be sequenced as the principal diagnosis, followed by any congenital anomaly codes Q00-Q99. To find the type of birth, look in the ICD-10-CM Alphabetic Index for Newborn/born in hospital Z38.00. Down Syndrome is reported secondarily and is found in the ICD-10-CM Alphabetic Index by looking for the main term Down Syndrome, Q90.9. Although category Q90 has a use additional note to also report associated physician condition and degree of intellectual disabilities, this is a newborn and this information is not known so it is not reported. • Question 7 0 out of 10 points Mrs. Bixby, 83, is being admitted for dehydration and anorexia. The probable cause is dementia. She was brought in by her daughter who is visiting from out of town. Her daughter will take her from our office to St. Mary's. The gerontology unit will evaluate her mental condition tomorrow after she is stabilized. How would you code the diagnoses? d. R63.0, E86.0, F02.80 b. R63.0, E86.0 Response Feedback: Rationale: ICD-10-CM guidelines tell us not to report an unsubstantiated probable or rule out diagnosis; therefore, a diagnosis of dementia is not appropriate at this time. The symptoms are dehydration and anorexia. Each of these terms requires a simple look-up in the ICD-10-CM Alphabetic Index. Although anorexia often is a short way of describing anorexia nervosa, in this case, there is no documentation of an eating disorder as a psychological disorder; look for the main term anorexia, R63.0, which is the correct diagnosis. Look for the main term Dehydration, E86.0. Verify all codes in the Tabular List. • Question 8 0 out of 10 points The provider performs an open reduction and internal fixation for left fibula and tibia fractures. Select the codes. d. S82.402B, S82.209B a. S82.402A, S82.202A Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Fracture, traumatic/ fibula (shaft) (styloid) S82.40-. Next look for Fracture, traumatic/tibia (shaft) S82.20-. Verification in the Tabular List indicates the 6th character 2 for left side. 7th character A for initial encounter is also reported. S82.402A, S82.202A. According to the ICD-10-CM guidelines, when a fracture is not specified as open or closed, the default is to code it as closed. Even though an open repair is performed, the diagnosis is not determined by the type of treatment. • Question 9 10 out of 10 points The patient was hit in the nose by the ball playing basketball on the varsity team last evening at the gym and woke up with severe epistaxis. The family physician controlled the nasal hemorrhage with cauterization and afterwards packed the nose with nasal packs. What are the correct diagnosis codes? b. R04.0, W21.05XA, Y92.39, Y93.67, Y99.8 b. R04.0, W21.05XA, Y92.39, Y93.67, Y99.8 Response Feedback: Rationale: The epistaxis is caused from an injury; it is not hereditary. This is found by looking in the ICD-10-CM Alphabetic Index for Epistaxis (multiple) and using the default code R04.0. Four external cause codes are required in this case. The first code indicates how the injury occurred (hit with a ball). Look in the External Cause of Injuries Index for Struck (accidentally) by/ball (hit) (thrown)/basketball W21.05-. Add a placeholder X for the 6th character and an A for the 7th character to indicate initial encounter, W21.05XA. The next code reports where the accident occurred. Look for Place of occurrence/Gymnasium, Y92.39. Next, code the activity he was involved in at the time. Look for Activity/basketball Y93.67. The last external cause code is a status code. Look for Status of external cause/student activity, Y99.8. • Question 10 10 out of 10 points When a patient presents for a screening test and the provider finds something abnormal, what diagnosis code should be sequenced first? Refer to ICD-10-CM guideline I.C.21.c.5. b. The Z code to identify the screening b. The Z code to identify the screening Response Feedback: Rationale: According to the ICD-10-CM guidelines I.C.21,c.5, when a screening test is performed and an abnormality is found, sequence the Z code for the screening first, followed by an additional code to report the abnormal findings. • A patient is diagnosed with pressure ulcers on each heel. Select the diagnosis code(s). d. L89.619, L89.629 d. L89.619, L89.629 Response Feedback: Rationale: Codes for pressure ulcers are determined by site, stage, and laterality. In this case, the patient has pressure ulcers on each heel. Look in the ICD-10-CM Alphabetic Index for Ulcer/pressure/heel L89.6-. In the Tabular List, a 5th character is required for laterality and 6th character is required for the stage. Report L89.619 for the right and L89.629 for the left. The stage is not documented; it is coded as unspecified stage. Unstageable can only be coded based on clinical documentation, which is not documented in this case. • Question 2 10 out of 10 points A patient with age-related osteoporosis suffers a pathologic fracture to her right hip. She is being seen for this new fracture today. Select the diagnosis code(s). c. M80.051A c. M80.051A Response Feedback: Rationale: A combination code is reported for the pathological fracture and osteoporosis. In the ICD-10-CM Alphabetic Index, look for Osteoporosis/age related/with current pathological fracture/ilium M80.05-. In the Tabular List, this section includes osteoporosis with current pathological fracture and the subcategory code is reported for age-related osteoporosis with current pathological fracture of hip. A 6th character is required. Complete the code with 6th character 1 for right femur and 7th character A for initial encounter. • Question 3 10 out of 10 points A patient diagnosed with BPH presents with urinary urgency. Select the diagnosis code(s). c. N40.1, R39.15 c. N40.1, R39.15 Response Feedback: Rationale: The patient is diagnosed with BPH (Benign Prostatic Hypertrophy) and urgency, which is a symptom of this condition. Look in the ICD-10-CM Alphabetic Index for the main term Hypertrophy then prostate, which directs you to see Enlargement, enlarged, prostate. Look for Enlargement, enlarged/prostate/with lower urinary tract symptoms (LUTS) N40.1. In the Tabular List, N40.1 has a note to "Use additional code for associated symptoms, when specified." Use R39.15 to report the urinary urgency. Because code R39.15 is listed as an additional code, it is not reported as primary code. • Question 4 0 out of 10 points A pregnant female, at 21 weeks, is diagnosed with iron-deficiency anemia and is sent to the clinic for a transfusion. Select the diagnosis code(s). a. O99.012 c. O99.012, D50.9, Z3A.21 Response Feedback: Rationale: Codes 099.012, Z3A.21 are both assigned. ICD-10-CM guideline 1.C.15.b.3. indicates, “in episodes where no delivery occurs, the principal diagnosis should correspond to the principal complication of the pregnancy which necessitated the encounter”. Look in the Alphabetic Index for Pregnancy/complicated by/anemia O99.01-.Verification in the Tabular List indicates the code is completed with a 6th character based on trimester. Choose O99.012 for second trimester. There is an instructional note under category code 099 that indicates to use an additional code to identify the specific condition. Code D50.9 is reported for iron deficiency anemia. Use additional code for number of weeks. Look for Pregnancy/weeks of gestation/21 weeks Z3A.21. • Question 5 0 out of 10 points Which statement is true regarding the perinatal period? a. It begins at six weeks b. It ends at 28 days Response Feedback: Rationale: According to the ICD-10-CM Guidelines for Coding and Reporting, Section I.C.16, “For coding and reporting purposes the perinatal period is defined as before birth through the 28th day following birth.” • Question 6 10 out of 10 points The hospital documentation states “normal vaginal delivery, live birth, female, with Down Syndrome.” Select the correct code(s) for the infant’s record. c. Z38.00, Q90.9 c. Z38.00, Q90.9 Response Feedback: Rationale: According to ICD-10-CM guideline I.C.17. for birth admission, the appropriate code from category Z38- Liveborn infants, according to the type of birth should be sequenced as the principal diagnosis, followed by any congenital anomaly codes Q00-Q99. To find the type of birth, look in the ICD-10-CM Alphabetic Index for Newborn/born in hospital Z38.00. Down Syndrome is reported secondarily and is found in the ICD-10-CM Alphabetic Index by looking for the main term Down Syndrome, Q90.9. Although category Q90 has a use additional note to also report associated physician condition and degree of intellectual disabilities, this is a newborn and this information is not known so it is not reported. • Question 7 10 out of 10 points When should a code for signs and symptoms be reported? Refer to ICD-10-CM guidelines I.C.18.a. and I.C.18.b. c. When it is not integral to the definitive diagnosis c. When it is not integral to the definitive diagnosis Response Feedback: Rationale: Signs and symptoms are reported when a definitive diagnosis has not been established. If the sign or symptom is not integral to the definitive diagnosis, the sign(s) and symptom(s) should be reported. • Question 8 10 out of 10 points A patient was sent home with a PICC line for Vancomycin treatment at home. He returns to his physician with an infection due to the PICC Line. The infection is determined to be MRSA. Select the diagnosis code(s) in the correct sequence. c. T80.218A, A49.02 c. T80.218A, A49.02 Response Feedback: Rationale: When complications are reported, a code for the complication is reported first. If the cause of the complication is known, it is reported as the additional code(s). Look in the ICD-10-CM Alphabetic Index for Infection/due to or resulting from/central venous catheter/specified NEC T80.218-. Verification in the Tabular List indicates this code needs a 7th character. 7th character extension A is reported for the initial encounter. T80.218A is correct because we do know that this is an MRSA infection, however, we do not know whether it is a local infection or bloodstream infection. Next look for MRSA (Methicillin resistant Staphylococcus aureus)/infection A49.02. Verify code in the Tabular List. • Question 9 10 out of 10 points The patient was hit in the nose by the ball playing basketball on the varsity team last evening at the gym and woke up with severe epistaxis. The family physician controlled the nasal hemorrhage with cauterization and afterwards packed the nose with nasal packs. What are the correct diagnosis codes? b. R04.0, W21.05XA, Y92.39, Y93.67, Y99.8 b. R04.0, W21.05XA, Y92.39, Y93.67, Y99.8 Response Feedback: Rationale: The epistaxis is caused from an injury; it is not hereditary. This is found by looking in the ICD-10-CM Alphabetic Index for Epistaxis (multiple) and using the default code R04.0. Four external cause codes are required in this case. The first code indicates how the injury occurred (hit with a ball). Look in the External Cause of Injuries Index for Struck (accidentally) by/ball (hit) (thrown)/basketball W21.05-. Add a placeholder X for the 6th character and an A for the 7th character to indicate initial encounter, W21.05XA. The next code reports where the accident occurred. Look for Place of occurrence/Gymnasium, Y92.39. Next, code the activity he was involved in at the time. Look for Activity/basketball Y93.67. The last external cause code is a status code. Look for Status of external cause/student activity, Y99.8. • Question 10 10 out of 10 points The provider orders serum blood tests as part of a pre-employment physical exam. What is the diagnosis? c. Z02.1 c. Z02.1 Response Feedback: Rationale: The patient has no complaints. The diagnosis codes for employment exams are found under the main term Examination in the ICD-10-CM Alphabetic Index. Look for Examination/ medical (adult) (for) (of)/ pre-employment you are referred to Z02.1. Verification in the Tabular List confirms this is the correct code. Sunday, November 19, 2017 9:09:57 AM MST • patient is diagnosed with pressure ulcers on each heel. Select the diagnosis code(s). d. L89.619, L89.629 d. L89.619, L89.629 Response Feedback: Rationale: Codes for pressure ulcers are determined by site, stage, and laterality. In this case, the patient has pressure ulcers on each heel. Look in the ICD-10-CM Alphabetic Index for Ulcer/pressure/heel L89.6-. In the Tabular List, a 5th character is required for laterality and 6th character is required for the stage. Report L89.619 for the right and L89.629 for the left. The stage is not documented; it is coded as unspecified stage. Unstageable can only be coded based on clinical documentation, which is not documented in this case. • Question 2 10 out of 10 points A provider performs an arthroscopic procedure to repair an incomplete right degenerative rotator cuff tear on a patient with primary, degenerative arthritis in the same shoulder. Select the diagnosis codes. b. M75.111, M19.011 b. M75.111, M19.011 Response Feedback: Rationale: The patient has a degenerative incomplete rotator cuff tear on the right shoulder and primary degenerative arthritis. The primary reason for the procedure is the tear, so it is reported first. In the ICD-10-CM Alphabetic Index, look for Tear, torn/rotator cuff (nontraumatic)/incomplete M75.11-. A trauma or injury needs to be indicated to report a traumatic rotator cuff tear code. In the Tabular List, complete the code for right shoulder. 6th character 1 is reported for the right shoulder. The complete code is M75.111. For the second diagnosis, look for Arthritis, arthritic/degenerative. You are referred to see Osteoarthritis. Look for Osteoarthritis/primary/shoulder M19.01-. In the Tabular List, a 6th character is required to report laterality. 6th character 1 reports the right shoulder. The complete code is M19.011. • Question 3 10 out of 10 points A 55-year-old female with right hydronephrosis presents for a cystourethroscopy with a retrograde pyelogram. What is the correct diagnosis code? c. N13.30 c. N13.30 Response Feedback: Rationale: The indication for the surgery is hydronephrosis. In the ICD-10-CM Alphabetic Index, look for the main term Hydronephrosis. There is no indication of causal organism, or that it is a congenital condition. The default code is N13.30. A review of this code in the Tabular List confirms this is the correct diagnosis. • Question 4 10 out of 10 points A pregnant female, at 21 weeks, is diagnosed with iron-deficiency anemia and is sent to the clinic for a transfusion. Select the diagnosis code(s). c. O99.012, D50.9, Z3A.21 c. O99.012, D50.9, Z3A.21 Response Feedback: Rationale: Codes 099.012, Z3A.21 are both assigned. ICD-10-CM guideline 1.C.15.b.3. indicates, “in episodes where no delivery occurs, the principal diagnosis should correspond to the principal complication of the pregnancy which necessitated the encounter”. Look in the Alphabetic Index for Pregnancy/complicated by/anemia O99.01-.Verification in the Tabular List indicates the code is completed with a 6th character based on trimester. Choose O99.012 for second trimester. There is an instructional note under category code 099 that indicates to use an additional code to identify the specific condition. Code D50.9 is reported for iron deficiency anemia. Use additional code for number of weeks. Look for Pregnancy/weeks of gestation/21 weeks Z3A.21. • Question 5 10 out of 10 points Which statement is true regarding the perinatal period? b. It ends at 28 days b. It ends at 28 days Response Feedback: Rationale: According to the ICD-10-CM Guidelines for Coding and Reporting, Section I.C.16, “For coding and reporting purposes the perinatal period is defined as before birth through the 28th day following birth.” • Question 6 10 out of 10 points A 4-year-old male is brought to the hospital by his mother. Today he is going to have surgery to repair his Cheiloschisis. Assign the correct code for his condition. c. Q36.9 c. Q36.9 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Cheiloschisis referring you to see Cleft, lip. Look for Cleft/lip, you are directed to Q36.9. Verification in the Tabular List lists Cleft lip NOS under code Q36.9. • Question 7 10 out of 10 points When should a code for signs and symptoms be reported? Refer to ICD-10-CM guidelines I.C.18.a. and I.C.18.b. c. When it is not integral to the definitive diagnosis c. When it is not integral to the definitive diagnosis Response Feedback: Rationale: Signs and symptoms are reported when a definitive diagnosis has not been established. If the sign or symptom is not integral to the definitive diagnosis, the sign(s) and symptom(s) should be reported. • Question 8 10 out of 10 points The provider performs an open reduction and internal fixation for left fibula and tibia fractures. Select the codes. a. S82.402A, S82.202A a. S82.402A, S82.202A Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Fracture, traumatic/ fibula (shaft) (styloid) S82.40-. Next look for Fracture, traumatic/tibia (shaft) S82.20-. Verification in the Tabular List indicates the 6th character 2 for left side. 7th character A for initial encounter is also reported. S82.402A, S82.202A. According to the ICD-10-CM guidelines, when a fracture is not specified as open or closed, the default is to code it as closed. Even though an open repair is performed, the diagnosis is not determined by the type of treatment. • Question 9 10 out of 10 points A male patient was a passenger in an automobile involved in a serious collision with another automobile. He sustained a closed fracture of the coronoid process of the jaw and an open left shaft fracture, Type 1, of the radius with an open Type 1 shaft fracture of the left ulna. What are the diagnosis codes? d. S52.302B, S52.202B, S02.630A, V43.62XA d. S52.302B, S52.202B, S02.630A, V43.62XA Response Feedback: Rationale: A code is reported for each fracture. The radius and ulna fracture is open, which makes it the most severe injury; therefore, it is reported first. Look in the ICD-10-CM Alphabetic Index for Fracture, traumatic/radius/shaft S52.30- Verification in Tabular List indicates for the 6th character 2 for left radius and B for the 7th character for initial encounter for open Type 1 fracture, S52.302B. Next look for Fracture, traumatic/ ulna (shaft) S52.20-. 6th character 2 is for the left radius and B for the 7th character for initial encounter for open Type I fracture, S52.202B. Look in the ICD-10-CM Alphabetic Index for Fracture, traumatic/jaw (bone) (lower) - see Fracture, mandible. Look for Fracture, traumatic/mandible (lower jaw (bone))/coronoid process S02.63. In the Tabular List, 6th character 0 is reported for unspecified side and an A for the 7th character for initial encounter for a closed fracture, S02.630A. The patient was a passenger in a car that collided with another car. Look in the External Cause of Injuries Index for Accident/car - see Accident/transport, car occupant. Look for Accident/transport (involving injury to) car occupant/passenger/collision (with)/car(traffic) V43.62-. Add placeholder X for the 6th character and A for the 7th character for initial encounter. There are no other circumstances known about the collision, so no other external cause codes are reported. • Question 10 10 out of 10 points When a patient presents for a screening test and the provider finds something abnormal, what diagnosis code should be sequenced first? Refer to ICD-10-CM guideline I.C.21.c.5. b. The Z code to identify the screening b. The Z code to identify the screening Response Feedback: Rationale: According to the ICD-10-CM guidelines I.C.21,c.5, when a screening test is performed and an abnormality is found, sequence the Z code for the screening first, followed by an additional code to report the abnormal findings. Sunday, November 19, 2017 9:10:11 AM MST • Question 1 4 out of 4 points Which statement is TRUE for reporting burn codes? d. The highest degree of burn is reported as the primary code. d. The highest degree of burn is reported as the primary code. Response Feedback: Rationale: ICD-10-CM guideline I.C.19.d.1 instructs you to sequence first the code that reflects the highest degree of burn when more than one burn is present. Sunburns are not classified under the traumatic burn codes (T20-T25); they have their own set of codes under category code L55. First degree burns are superficial burns through only the epidermis. • Question 2 4 out of 4 points Can Z codes be listed as a primary code? a. Yes; Z codes can be sequenced as primary and secondary codes. a. Yes; Z codes can be sequenced as primary and secondary codes. Response Feedback: Rationale: ICD-10-CM guideline I.C.21.a indicates Z codes may be used as either a first listed (principal diagnosis code in the inpatient setting) or secondary code, depending on the circumstances of the encounter. Z codes are not external cause codes. The external cause codes are listed in chapter 20 in the Tabular List and begin with alpha characters V, W, or Y, and can only be reported as secondary codes. • Question 3 0 out of 4 points What is NOT an example of active treatment for pathological fractures? b. Evaluation and treatment by a new provider a. Cast change Response Feedback: Rationale: According to ICD-10-CM guideline I.C.19.a, examples of active treatment are: surgical treatment, emergency department encounter, and evaluation and continuing treatment by the same or different provider. Cast change is considered subsequent treatment. • Question 4 4 out of 4 points What does the 7th character A indicate in Chapter 19? a. Initial encounter a. Initial encounter Response Feedback: Rationale: According to ICD-10-CM guideline I.C.19.a the 7th character A represents the initial encounter for each encounter where active treatment is received for the condition. • Question 5 4 out of 4 points The provider documents CKD stage 5 and ESRD. What ICD-10-CM code(s) is/are reported? b. N18.6 b. N18.6 Response Feedback: Rationale: According to ICD-10-CM guideline I.C.14.a.1 when both a stage of CKD and ESRD are documented, you assign only code N18.6. Verify code selection in the Tabular List. • Question 6 4 out of 4 points The patient has benign prostatic hyperplasia with urinary retention. What ICD-10-CM code(s) is/are reported? c. N40.1, R33.8 c. N40.1, R33.8 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Hyperplasia/prostate/with lower urinary tract symptoms (LUTS), guiding you to code N40.1. In the Tabular List there are instructions below code N40.1 to “Use additional code for associated symptoms, when specified.” Code R33.8 is listed for urinary retention. Verify code selection in the Tabular List. • Question 7 4 out of 4 points A patient presents for an initial encounter for swelling, tenderness and erythema at the upper extremity injection site following Hepatitis B vaccination. The patient has a local infection. What ICD-10-CM code is reported? b. T88.0XXA b. T88.0XXA Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Infection, infected, infective/due to or resulting from/immunization or vaccination. This refers you to T88.0. Cross-reference to the Tabular List shows that seven characters are needed to complete the code. A placeholder X is required for the 5th and 6th characters and the 7th character A is chosen to indicate this is the initial encounter. • Question 8 4 out of 4 points A patient was admitted three weeks following a normal vaginal delivery with a postpartum breast abscess. What ICD-10-CM code is reported? c. O91.12 c. O91.12 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Abscess/breast (acute) (chronic) (nonpuerperal)/puerperal, postpartum, gestational which guides you to see Mastitis, obstetric, purulent. Look for Mastitis (acute) (diffuse) (nonpuerperal) (subacute)/obstetric/purulent/associated with/puerperium guiding you to code O91.12. In the Tabular List, the description under O91.12 includes puerperal mammary abscess. The puerperium is the period of six weeks or 42 days following childbirth. • Question 9 4 out of 4 points What ICD-10-CM codes are reported on the maternal record for a delivery of triplets that are all liveborn at 32 weeks of pregnancy? b. O30.103, Z37.51, Z3A.32 b. O30.103, Z37.51, Z3A.32 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Pregnancy/triplet O30.10-. In the Tabular List, additional characters are required to indicate the number of placenta and the number of amniotic sacs. Because you do not have that documentation, 0 for unspecified is reported as the 5th character. The 6th character 3 is reported to indicate the 3rd trimester (trimesters are listed at the beginning of Chapter 15 in the ICD-10-CM codebook). The complete code is O30.103. Next, look in the Alphabetic Index for Outcome of Delivery/multiple births/all liveborn/triplets Z37.51. The last code indicates the weeks of gestation. Documentation indicates she delivered at her 32nd week. Look in the Alphabetic Index for Pregnancy/weeks of gestation/32 weeks Z3A.32. Verify code selection in the Tabular List. • Question 10 4 out of 4 points A patient was referred to the radiology department for chronic low back pain. The radiology report indicated there was no marrow abnormality identified and the conus medullaris was unremarkable. Additional findings include: L4–L5: There is a minor diffusely bulging annulus at L4–L5. A small focal disc bulge is seen in far lateral position on the left at L4–L5 within the neural foramen. No definite encroachment on the exiting nerve root at this site is seen. No significant spinal stenosis is identified. L5–S1: There is a diffusely bulging annulus at L5–S1, with a small focal disc bulge centrally at this level. There is minor disc desiccation and disc space narrowing at L5–S1. No significant spinal stenosis is seen at L5–S1. The final diagnosis is minor degenerative disc disease at L4–L5 and L5–S1, as described. What ICD-10-CM code(s) is/are reported? d. M51.37 d. M51.37 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Degeneration, degenerative/intervertebral disc NOS/lumbosacral region directing you to code M51.37. Verify code selection in the Tabular List. The low back pain is a symptom of the degenerative disc disease and is not reported separately. • Question 11 4 out of 4 points A 45 year-old mother of three children is going into surgery to correct an anterior vaginal wall prolapse with an incomplete uterine prolapse. What ICD-10-CM code is reported? a. N81.2 a. N81.2 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Prolapse/vagina (anterior) (wall)/with prolapse of uterus/incomplete, guiding you to code N81.2. Verify code selection in the Tabular List. • Question 12 4 out of 4 points Patient is in the facility here today for a screening colonoscopy. During the procedure, a polyp is found and removed with a hot biopsy technique. How would this be reported? a. Z12.11, K63.5 a. Z12.11, K63.5 Response Feedback: Rationale: ICD-10-CM guideline I.C.21.c.5 indicates, “A screening code may be a first listed code if the reason for the visit is specifically the screening exam…Should a condition be discovered during the screening then the code for the condition may be assigned as an additional diagnosis.” For this question, the screening code is reported first. Look in the ICD-10-CM Alphabetic Index for Screening/colonoscopy which directs you to Z12.11. Then, look for Polyp, polypus/colon which directs you to K63.5 as the secondary diagnosis. Verify both code selections in the Tabular List. • Question 13 4 out of 4 points Mr. Smith presents to the office for a screening test to detect sickle cell disorder. What ICD-10-CM code(s) is/are reported? a. Z13.0 a. Z13.0 Response Feedback: Rationale: This is considered a screening. Per ICD-10-CM guideline I.C.21.c.5, “Screening is the testing for disease or disease precursors in seemingly well individuals so that early detection and treatment can be provided for those who test positive for the disease.” In the ICD-10-CM Alphabetic Index look for Screening (for)/sickle-cell disease or trait, guiding you to code Z13.0. Verify this is the correct code in the Tabular List. The patient does not have a known sickle cell disorder so a code from D57 is not reported; results from the screening test will determine if the patient has sickle cell disorder. • Question 14 4 out of 4 points The patient has an ovarian pregnancy without intrauterine pregnancy. What ICD-10-CM codes are reported? d. O00.20, Z3A.00 d. O00.20, Z3A.00 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Pregnancy/ovarian guiding you to code O00.20. Cross-reference the code in the Tabular List to ensure code selection is correct. ICD-10-CM guideline I.C.15.b.1 states to not assign codes from category Z34 with Chapter 15 codes. At the beginning of Chapter 15 there is a note to use an additional code from Category Z3A Weeks of gestation, to identify the weeks of gestation for codes O00-O9A. In this case the weeks of gestation is not documented. In the Alphabetic Index look for Pregnancy/weeks of gestation/not specified which directs you to Z3A.00. Verify code selection in the Tabular List. • Question 15 0 out of 4 points The patient has a mass on his forehead; he says it is from a piece of sheet metal from an injury to his forehead months ago. He has an X-ray showing a foreign body is in the mass. After obtaining consent, the foreign body is removed from the subcutaneous tissue. What ICD-10-CM code(s) is/are reported? c. Z18.10, S01.82XA d. Z18.10 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Foreign Body/retained (old) (nonmagnetic) (in)/fragments and you are directed to see Retained, foreign body fragments (type of). In the Alphabetic Index, look for Retained/foreign body fragments (type of)/metal directing you to Z18.10. Verify code selection in the Tabular List. There is no mention of whether the metal is magnetic or not. The patient did not have an acute laceration with a foreign body in an open wound; therefore, code S01.82XA is not reported. • Question 16 4 out of 4 points A 63 year-old fractured her scaphoid bone in her right wrist three months ago in an accident. She now presents with a nonunion of the scaphoid bone. What ICD-10-CM code is reported? c. S62.001K c. S62.001K Response Feedback: Rationale: A nonunion fracture is when the broken bone has failed to heal or is not healing. According to ICD-10-CM guideline I.C.19.c.1 Care of complications of fractures, such as malunion and nonunion, is reported with the appropriate 7th character for subsequent care. The fracture was due to an accident and there is no mention of osteoporosis so this is a traumatic fracture. In the ICD-10-CM Alphabetic Index, look for Fracture, traumatic/scaphoid (hand) and you are directed to see also Fracture, carpal, navicular. In the Alphabetic Index, look for Fracture, traumatic/carpal bone(s)/navicular guides you to S62.00-. In the Tabular List a 6th character 1 is selected for the right wrist and 7th character K is selected for a subsequent encounter for fracture with nonunion. Verify code selection in the Tabular List. • Question 17 4 out of 4 points Patient is in the ED due to a football hitting his nose when playing tackle football in the park. X-ray shows a displaced nasal fracture. What ICD-10-CM codes are reported? d. S02.2XXA, W21.01XA, Y93.61, Y92.830 d. S02.2XXA, W21.01XA, Y93.61, Y92.830 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Fracture, traumatic/nasal (bone(s)) S02.2. In the Tabular List, seven characters are needed to complete this code. Placeholder X is used for the 5th and 6thcharacters and A is assigned as the 7th character for initial encounter for closed fracture. The dislocation code and the open fracture code are not reported. Should a fracture and dislocation occur in the same site, only the fracture code is reported. Look in the Alphabetic Index for Dislocation/with fracture and you are referred to see Fracture and a displaced fracture is a closed fracture. External cause codes are used to report the circumstances surrounding the injury. In the ICD-10-CM External Cause of Injuries Index look for Struck (accidentally) by/ball (hit) (thrown)/football W21.01. In the Tabular List seven characters are needed to complete the code. A placeholder X is used for the 6th character and A is assigned for the 7th character for the initial encounter. Next, look in the External Cause of Injuries Index for Activity/football (American)/tackle directing you to Y93.61 and Place of occurrence/park (public) directing you to Y92.830. The Y codes do not require a 7th character. Verify code selection in the Tabular List. • Question 18 4 out of 4 points A patient is coming in for follow up of a second-degree burn on the left forearm. The provider notes the burn is healing well. He is to come back in two weeks for continued care to checkup on the healing of the burn. What ICD-10-CM code is reported? b. T22.212D b. T22.212D Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Burn/forearm/left/second degree, guiding you to subcategory T22.212. Per ICD-10-CM guideline I.C.19.a indicates that the 7th character D subsequent encounter is used for encounters after the patient has received active treatment of the condition and is receiving routine care for the condition during the healing or recovery phase. Examples of subsequent care are: cast change or removal, an X-ray to check healing status of fracture, removal of external or internal fixation device, medication adjustment, other aftercare and follow up visits following treatment of the injury or condition.” Verify code selection in the Tabular List. • Question 19 0 out of 4 points A baby boy is born by cesarean section in the hospital. ABO incompatibility was documented, but the Coomb's test was negative, ruling out the ABO incompatibility, so no treatment was given. What ICD-10-CM codes are reported for the newborn’s record? c. Z38.01, P55.1 a. Z38.01, Z05.8 Response Feedback: According to ICD-10-CM guideline 1.C.15.a.2 chapter 15 codes are only used on the maternal record. Per ICD-10-CM guideline I.C.16.a.2 when coding the birth episode in a newborn record, assign a code from category Z38 Liveborn infants according to place of birth and type of delivery, as the principal diagnosis. Code Z38.01 is found in the ICD-10-CM Alphabetic Index by looking for Newborn (infant) (liveborn) (singleton)/born in hospital/by cesarean. ABO incompatibility was documented but ruled out due to the Coomb’s test being negative. Look in the Alphabetic Index for Observation/newborn (for)/ruled out/specified condition NEC referring you to Z05.8. Report only codes Z38.01 and Z05.8. • Question 20 4 out of 4 points A 24 year-old woman developed a keloid scar as a result of a third degree burn on the left upper arm. What ICD-10-CM code(s) is/are reported? d. L91.0, T22.332S d. L91.0, T22.332S Response Feedback: Rationale: A keloid is a type of scar resulting from granulation tissue at the site of healed skin injury. This would be considered a sequela (late effect) after the acute phase of the burn. Per ICD-10-CM guideline I.B.10, Coding of sequela generally requires two codes sequenced in the following order: The condition or nature of the sequela is sequenced first (keloid). The sequela code is sequenced second. In the ICD-10-CM Alphabetic Index look for Scar, scarring/keloid directing you to L91.0. To find the late effect code, look for Burn/above elbow/left/third degree which directs you to subcategory T22.332. Verify code selection in the Tabular List. For the burn code, the 7th character S is chosen to indicate sequela. • Question 21 4 out of 4 points A patient is prescribed anticonvulsant medication for her seizures. She returns to her doctor three days later with nausea and rash due to taking the anticonvulsant medication. The provider notes that this is a drug reaction to an anticonvulsant and changes the medication. What ICD-10-CM codes are reported? a. L27.0, R11.0, T42.75XA a. L27.0, R11.0, T42.75XA Response Feedback: Rationale: Per ICD-10-CM guideline I.C.19.e.5.a when the drug was correctly prescribed and properly administered, drug toxicity is considered an adverse effect. Code the nature of the adverse effect (nausea and rash in this case), followed by the appropriate code for the adverse effect of the drug (T36-T50). Look in the ICD-10-CM Alphabetic Index for Nausea (without vomiting) directing you to R11.0 and Rash (toxic)/drug (internal use) directing you to L27.0. Do not use the code for general rash, R21, because L27.0 is a more specific code. Look in the ICD-10-CM Table of Drugs and Chemicals for Anticonvulsant and select the code from the Adverse effect column which directs you to T42.75-. In the Tabular List a 6th character placeholder X is required and 7th character A is appended for the initial encounter. Verify code selection in the Tabular List. • Question 22 4 out of 4 points A male patient is here for his chemotherapy for metastatic carcinoma of the liver secondary to cancer of the right areola. What ICD-10-CM codes are reported? d. Z51.11, C78.7, C50.021 d. Z51.11, C78.7, C50.021 Response Feedback: Rationale: ICD-10-CM guideline I.C.2.e.2 states that if a patient admission/encounter is solely for the administration of chemotherapy, immunotherapy, or radiation therapy, assign code Z51.0 Encounter for antineoplastic radiation therapy, or Z51.11 Encounter for antineoplastic chemotherapy, or Z51.12 Encounter for antineoplastic immunotherapy as the first listed or principal diagnosis. In the ICD-10-CM Alphabetic Index look for Encounter (with health service) (for)/chemotherapy for neoplasm guiding you to code Z51.11. Next, look in the Alphabetic Index for Metastasis, metastatic/cancer/from specified site and you are directed to see Neoplasm, malignant, by site. In the ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/liver and select the code from the Malignant Secondary column, guiding you to code C78.7. Next look for Neoplasm, neoplastic/areola and select the code from the Malignant Primary column or Neoplasm, neoplastic/breast/areola and select the code from the Malignant Primary column, guiding you to subcategory code C50.0-. In the Tabular List, the 5th character is reported for the sex of the patient. In this case the patient is a male resulting in a 5th character of 2. The 6th character is for laterality; 1 is for right. The complete code is C50.021 for primary cancer of the right male areola. When assigning breast cancer codes make sure to select for the correct sex of the patient. The secondary cancer is listed first because the chemotherapy is directed to the secondary site per ICD-10-CM guideline I.C.2.b. Verify code selection in the Tabular List. • Question 23 4 out of 4 points A 16 year-old male is brought to the ED by his mother. He was riding his bicycle in the park when he fell off the bike. The patient’s right arm is painful to touch, discolored, and swollen. The X-ray shows a closed fracture of the ulna. What ICD-10-CM codes are reported? d. S52.201A, V18.0XXA, Y92.830 d. S52.201A, V18.0XXA, Y92.830 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Fracture, traumatic/ulna (shaft), guiding you to subcategory S52.20-. The Tabular List indicates seven characters are needed to complete the code. The 6thcharacter 1 is for the right arm, and the 7th character A is for an initial encounter for closed fracture. To find the external cause codes you will look in the ICD-10-CM External Cause of Injuries Index. Look for Accident (to)/transport/pedal cyclist/driver/noncollision accident/nontraffic which guides you to subcategory V18.0. The Tabular List indicates an appropriate 7th character is to be added to each code from category V18. You will need placeholder X for the 5th and 6th characters and the 7th character is A for the initial encounter. The second external cause code identifies the place of occurrence. In the External Cause of Injuries Index look for Place of occurrence/park (public) directing you to code Y92.830. Verify code selection in the Tabular List. • Question 24 4 out of 4 points A 3 year-old is brought to the burn unit after pulling a pot of hot soup off the stove and spilling it on herself. She sustained 18% second degree burns on her legs and 20% third degree burns on her chest and arms. Total body surface area burned is 38%. What ICD-10-CM codes are reported for the burns (do not include external cause codes for the accident)? a. T21.31XA, T22.399A, T24.299A, T31.32 a. T21.31XA, T22.399A, T24.299A, T31.32 Response Feedback: Rationale: ICD-10-CM guideline I.C.19.d.1 states to sequence first the code that reflects the highest degree of burn when more than one burn is present. In this case, the burns on her chest and arms are third degree and are reported first. In the ICD-10-CM Alphabetic Index look for Burn/chest wall/third degree, referring you to subcategory T21.31. Because the question indicates arms and legs (plural) we will code multiple sites of the upper and lower limbs. In the Alphabetic Index look for Burn/upper limb/multiple sites/third degree directing you to subcategory T22.399, and Burn/lower/limb/multiple sites/second degree directing you to subcategory T24.299. The Tabular List indicates a 7th character is needed for all three of these codes; a placeholder X is required for T21.31. The 7th character A is reported for the initial encounter. Refer to ICD-10-CM guideline I.C.19.d.6 for instructions on assigning a code from category T31 to report the extent of body surface involved. The 4th character represents the total body surface area (TBSA) (all degrees) that was burned. The 5th character represents the percentage of third degree burns to the body. In the scenario, 38% is documented as the TBSA making 3 the appropriate 4th character; 20% is third degree burns, making 2 the 5th character. In the Alphabetic Index look for Burn/extent (percentage of body surface)/30-39 percent/with 20-29 percent third degree burns directing you to code T31.32 The external cause codes would also be reported for the accident. Verify code selection in the Tabular List. • Question 25 0 out of 4 points At 39 weeks gestation, a 26 year-old woman is admitted for precipitous labor and vaginally delivers a healthy baby girl. What ICD-10-CM codes are reported on the maternal record? a. O80, 062.3, Z38.00, Z3A.39 d. O62.3, Z37.0, Z3A.39 Response Feedback: Rationale: The labor is precipitous. In the ICD-10-CM Alphabetic Index, look for Delivery (childbirth) (labor)/complicated/by/precipitate labor directing you to O62.3. ICD-10-CM guideline I.C.15.n.1 states that code O80 is reported for a full-term normal delivery of a single, healthy infant without any complications antepartum, during the delivery, or postpartum during the delivery episode. Code O80 is not to be reported with any other pregnancy complication code from chapter 15. In this case, O62.3 is reported for the complication and the normal delivery code (O80) is not reported. The outcome of delivery is also reported. Look in the Alphabetic Index for Outcome of delivery/single/liveborn directing you to Z37.0. Code Z38.00 is only to be used on the newborn’s record, not the maternal record. At the beginning of chapter 15, there is a note to use an additional code to report the weeks of gestation. The patient is 39 weeks gestation. Look in the Alphabetic Index for Pregnancy/weeks of gestation/39 weeks directing you to Z3A.39. Verify the code selection in the Tabular List. Sunday, November 19, 2017 9:10:46 AM MST • Question 1 10 out of 10 points According to the parenthetical instructions for CPT® code 33690, how should right and left pulmonary artery banding in a single ventricle be reported? b. 33620 b. 33620 Response Feedback: Rationale: The parenthetical instructions under CPT® code 33690 include: (For right and left pulmonary artery banding in a single ventricle [eg, hybrid approach stage 1], use 33620) and (Do not report modifier 63 in conjunction with 33690). • Question 2 10 out of 10 points Which one of the CPT® codes listed below would modifier 50 be appended to for a bilateral procedure? d. 37650 d. 37650 Response Feedback: Rationale: CPT® code 37650 has a parenthetic instruction below it stating to report 37650 with modifier 50 when performed bilaterally. CPT code 22510 states it is for a unilateral or bilateral procedure so modifier 50 is not appropriate. CPT code 36251 is for a unilateral procedure and CPT code 36252 is for the same procedure performed bilaterally. Because there is a code option for unilateral and another code option for bilateral, modifier 50 is not appropriate for either code. • Question 3 0 out of 10 points What are the definitions for facility and non-facility for the Physician Fee Schedule? c. Facility includes skilled nursing facilities, nursing homes, hospitals settings d. Both b and c Response Feedback: Facility practice RVU expenses include services performed in emergency rooms, hospital settings (inpatient and outpatient), skilled nursing facilities, nursing homes, or ambulatory surgical centers (ASCs). The non-facility RVUs include services performed in non-hospital owned physician practices or privately owned practices. • Question 4 10 out of 10 points What association maintains and publishes CPT® coding guidelines, codes, and descriptions? a. AMA a. AMA Response Feedback: AMA - The CPT® code set (HCPCS Level I) is copyrighted and maintained by American Medical Association (AMA). • Question 5 0 out of 10 points Which modifiers are appended to E/M codes to report payable services within the global package? d. 24, 26, 57 c. 24, 25, 57 Response Feedback: Modifiers 24 Unrelated evaluation and management service by the same physician during a postoperative period, 25 Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service, and 57 Decision for surgery are used on evaluation and management CPT® codes only. • Question 6 10 out of 10 points What services are included in the surgical global package? d. Preoperative visits, Intraoperative services, Postsurgical pain management d. Preoperative visits, Intraoperative services, Postsurgical pain management Response Feedback: The Surgical Global Package includes: Preoperative Visits, Intraoperative Services, Complications Following Surgery, Postoperative Visits, Postsurgical Pain Management, and Miscellaneous Services. • Question 7 10 out of 10 points Which set of HCPCS codes are required for use under the Medicare Outpatient Prospective Payment System? b. C codes b. C codes Response Feedback: C codes are required for use under the Medicare Outpatient Prospective Payment System (OPPS). Hospitals report new technology procedures, drugs, biologicals, and radiopharmaceuticals that do not have other HCPCS codes assigned with C codes. • Question 8 0 out of 10 points Which set of HCPCS Level II codes are used to report injected drugs? a. A codes d. J codes Response Feedback: Rationale: The J code category contains codes and descriptions specific to drugs and biologicals (J0120–J8999) as well as chemotherapy drugs (J9000–J9999). The list of drugs described in the J category can be injected by one of three means: subcutaneously, intramuscularly, or intravenously. • Question 9 0 out of 10 points What types of modifiers are listed in the Appendix A of the CPT® codebook? a. CPT®, Anesthesia Physical Status Modifiers, Surgical b. CPT®, ASC, HCPCS, Anesthesia Physical Status Modifiers Response Feedback: Appendix A lists modifiers for CPT®, Anesthesia Physical Status Modifiers, ASC, and HCPCS Level II. • Question 10 10 out of 10 points Which CPT® modifier should you append to a procedure code for a bilateral procedure? b. 50 b. 50 Response Feedback: 50 Bilateral Procedure Sunday, November 19, 2017 9:11:17 AM MST • Question 1 10 out of 10 points According to the parenthetical instructions for CPT® code 33690, how should right and left pulmonary artery banding in a single ventricle be reported? b. 33620 b. 33620 Response Feedback: Rationale: The parenthetical instructions under CPT® code 33690 include: (For right and left pulmonary artery banding in a single ventricle [eg, hybrid approach stage 1], use 33620) and (Do not report modifier 63 in conjunction with 33690). • Question 2 0 out of 10 points What is the full description for CPT® code 43622? c. Gastrectomy, total; with esophagoenterostomy with formation of intestinal pouch, any type d. Gastrectomy, total; with formation of intestinal pouch, any type Response Feedback: Rationale: The full descriptor of 43622 includes the common portion before the semi-colon of code 43620, followed by the description next to 43620 (with formation of intestinal pouch, any type). • Question 3 10 out of 10 points CPT® Category III codes are reported to indicate which type of service or procedure? a. New and emerging a. New and emerging Response Feedback: Category III codes do not indicate the service or procedure is experimental, only that they are new and emerging and are being tracked for trending purposes. This information is found in the guidelines for Category II Codes section. • Question 4 10 out of 10 points Which CPT® Appendix lists clinical examples for E/M coding? b. Appendix C b. Appendix C Response Feedback: Appendix C - Clinical Examples – Limited to E/M services, the AMA has provided clinical examples for different specialties. These clinical examples do not encompass the entire scope of medical practice, and guides professional coders to follow E/M patient encounter rules for level of service. • Question 5 10 out of 10 points What is the postoperative period included in the surgical global package for major surgery? c. 90 days c. 90 days Response Feedback: The global period of major procedures is 90 days. • Question 6 0 out of 10 points What services are included in the surgical global package? a. Preoperative Visits, Intraoperative Services, Initial consultation d. Preoperative visits, Intraoperative services, Postsurgical pain management Response Feedback: The Surgical Global Package includes: Preoperative Visits, Intraoperative Services, Complications Following Surgery, Postoperative Visits, Postsurgical Pain Management, and Miscellaneous Services. • Question 7 10 out of 10 points How often can HCPCS temporary Codes be updated? c. Quarterly c. Quarterly Response Feedback: Temporary codes can be added, changed, or deleted on a quarterly basis and once established; temporary codes are usually implemented within 90 days. • Question 8 10 out of 10 points Which set of HCPCS Level II codes are used to report injected drugs? d. J codes d. J codes Response Feedback: Rationale: The J code category contains codes and descriptions specific to drugs and biologicals (J0120–J8999) as well as chemotherapy drugs (J9000–J9999). The list of drugs described in the J category can be injected by one of three means: subcutaneously, intramuscularly, or intravenously. • Question 9 10 out of 10 points What types of modifiers are listed in the Appendix A of the CPT® codebook? b. CPT®, ASC, HCPCS, Anesthesia Physical Status Modifiers b. CPT®, ASC, HCPCS, Anesthesia Physical Status Modifiers Response Feedback: Appendix A lists modifiers for CPT®, Anesthesia Physical Status Modifiers, ASC, and HCPCS Level II. • Question 10 10 out of 10 points Which HCPCS Level II modifier should you append for a new wheelchair purchase? d. NU d. NU Response Feedback: NU - New Equipment. For example, append NU when a new walker, folding, wheeled, adjustable or fixed height is sold to a patient. Sunday, November 19, 2017 9:11:33 AM MST • Question 1 4 out of 4 points What is the correct HCPCS Level II code for parenteral nutrition solution amino acid, 3.5%? c. B4168 c. B4168 Response Feedback: Rationale: In the HCPCS Level II Index, look for Parenteral nutrition/solution. You are directed to codes B4164-B5200. When you review the B codes, B4168 is reported. • Question 2 4 out of 4 points A patient is seen in the physician’s office for a 2,400,000 U injection of Bicillin L-A. What code represents this drug and the units given? a. J0561 x 24 a. J0561 x 24 Response Feedback: Rationale: In the HCPCS Level II Table of Drugs, look up Bicillin L-A, which directs you to code J0561. One unit of J0561 represents 100,000 U, so 24 units are reported for 2,400,000 U. • Question 3 4 out of 4 points Services provided in the home by an agency are considered d. Facility services d. Facility services Response Feedback: Rationale: The Introduction in the CPT® codebook (after the Table of Contents) includes instructions under the subheading Place of Service and Facility Reporting, which indicates services provided in the home by an agency are considered facility services. • Question 4 4 out of 4 points What is the CPT® code used to report a right heart cardiac catheterization for congenital anomalies? c. 93530 c. 93530 Response Feedback: Rationale: In the CPT® Index, Catheterization/Cardiac directs you to See Cardiac Catheterization. Cardiac Catheterization/Right Heart/Congenital Cardiac Anomalies directs you to code 93530. • Question 5 4 out of 4 points How many days does it take CMS to implement HCPCS Level II Temporary Codes that have been reported as added, changed or deleted? c. 90 c. 90 Response Feedback: Rationale: Per CMS, temporary codes can be added, changed or deleted on a quarterly basis. Once established, temporary codes are usually implemented within 90 days, the time needed to prepare and issue implementation instructions and to enter the new code into CMS's and the contractors' computer systems and initiate user education. This time allows instructions, such as bulletins and newsletters, to be sent to suppliers providing them with information and assistance regarding the implementation of temporary codes. • Question 6 4 out of 4 points What is the correct code for the performance measure for moderate rheumatoid arthritis disease activity? b. 3471F b. 3471F Response Feedback: Rationale: In the CPT® Index, look for Performance Measures/Rheumatoid Arthritis/ Diagnostic/Screening Processes or Results/Rheumatoid Arthritis Disease Activity Assessment. You are directed to see codes 3470F-3472F. Upon further review, code 3471F represents the measurement of moderate disease activity in a patient with rheumatoid arthritis. • Question 7 4 out of 4 points What is the correct code for a radical maxillary sinusotomy? c. 31030 c. 31030 Response Feedback: Rationale: In the CPT® Index, look for Sinusotomy/Maxillary, which directs you to codes 31020-31032. Look in the Respiratory numeric section and review the code descriptors. Code 31030 is reported. 31032 is not correct because there is no indication of removing antrochoanal polyps. • Question 8 4 out of 4 points What is the code for partial laparoscopic colectomy with anastomosis and coloproctostomy? c. 44207 c. 44207 Response Feedback: Rationale: In the CPT® Index, look for Laparoscopy/ Colectomy/Partial. You are directed to codes 44204-44208 and 44213. In the Digestive numeric section, upon review of the codes, 44207 represents a partial colectomy with anastomosis and coloproctostomy performed laparoscopically. • Question 9 4 out of 4 points How are new additions and revisions indicated in the CPT® codebook each year? c. Green print c. Green print Response Feedback: Rationale: New additions and revisions in the CPT® codebook each year appear in green print. • Question 10 4 out of 4 points The Table of Drugs in the HCPCS Level II book indicates various medication routes of administration. What abbreviation represents the route where a drug is introduced into the subdural space of the spinal cord? d. IT d. IT Response Feedback: Rationale: In the HCPCS Level II codebook, there is an appendix that lists the abbreviations and acronyms and their meanings. IT stands for Intrathecal. IT is the route where a drug is introduced into the subdural space of the spinal cord. • Question 11 4 out of 4 points HCPCS Level II includes code ranges that consist of what type of codes? b. Permanent national codes, miscellaneous codes and temporary national codes b. Permanent national codes, miscellaneous codes and temporary national codes Response Feedback: Rationale: HCPCS Level II codes consist of permanent national codes, miscellaneous codes, and temporary national codes. • Question 12 0 out of 4 points What surgical status indicator represents the Global Surgical Package for endoscopic procedures (without an incision) where there is no postoperative period after the day of the surgery?? b. XXX a. 000 Response Feedback: Rationale: For endoscopic procedures (except procedures requiring an incision), there is no postoperative period. Surgical status indicator 000 = Endoscopic or minor procedure with related preoperative and postoperative relative values on the day of the procedure only included in the fee schedule payment amount; evaluation and management services on the day of the procedure generally not payable. • Question 13 4 out of 4 points What is the correct CPT® coding for a cystourethroscopy with brush biopsy of the renal pelvis? c. 52007 c. 52007 Response Feedback: Rationale: In the CPT® Index, look for Cystourethroscopy/Biopsy/Brush referring you to 52007. • Question 14 4 out of 4 points When procedures are “mandated” by third party payers, what modifier would you use? d. 32 d. 32 Response Feedback: Rationale: Modifier 32 reports “mandated services”. • Question 15 4 out of 4 points What code represents a secondary rhinoplasty where a small amount of work is performed on the tip of the nose? a. 30430 a. 30430 Response Feedback: Rationale: In the CPT® Index, look for Rhinoplasty/Secondary, which directs you to codes 30430-30450. Look at the codes in the Respiratory numeric section. Code 30430 represents a small amount of work for a secondary rhinoplasty when performed on the tip of the nose. • Question 16 4 out of 4 points What does “non-facility” describe when calculating Medicare Physician Fee Schedule payments? b. Non-hospital owned physician practices b. Non-hospital owned physician practices Response Feedback: Rationale: “Non-facility” location calculations are for private practices or non-hospital-owned physician practices. Reimbursement is higher for private practices because the practice incurs the full expense of providing the service. • Question 17 4 out of 4 points What is the correct CPT® code for the wedge excision of a nail fold of an ingrown toenail? d. 11765 d. 11765 Response Feedback: Rationale: In the CPT® Index, look for Excision/Nail Fold referring you to 11765. • Question 18 4 out of 4 points What is the appropriate modifier to use when two surgeons perform separate distinct portions of the same procedure? c. 62 c. 62 Response Feedback: Rationale: Modifier 62 is used when two surgeons work together as primary surgeons performing distinct part(s) of a procedure. Modifiers and their descriptions are found on the inside front cover and in Appendix A of your CPT® codebook. • Question 19 4 out of 4 points What modifier is used to report the termination of a surgery following induction of anesthesia due to extenuating circumstances or those that threaten the well-being of the patient? d. Modifier 53 d. Modifier 53 Response Feedback: Rationale: Modifier 53 is used to indicate the physician has elected to terminate a surgical or diagnostic procedure due to extenuating circumstances or those that threaten the well-being of the patient. CPT® modifiers are found on the inside front cover and in Appendix A of the CPT® codebook. • Question 20 4 out of 4 points What is the correct code for the administration of one vaccine given intramuscularly for a child under eight years of age when the physician counsels the parents? b. 90460 b. 90460 Response Feedback: Rationale: In the CPT® Index, look for Immunization Administration/One Vaccine/Toxoid/with Counseling. You are directed to use code 90460. • Question 21 4 out of 4 points What chapter in the HCPCS Level II codebook lists the code for Wheelchairs? c. Durable Medical Equipment (E0100-E8002) c. Durable Medical Equipment (E0100-E8002) Response Feedback: Rationale: A wheelchair is considered durable medical equipment. In the HCPCS index, look for the term Wheelchair. The majority of the codes listed are E codes. • Question 22 4 out of 4 points What codes are voluntarily reported to payers, provide evidence-based performance-measure data? d. CPT® Category II codes d. CPT® Category II codes Response Feedback: Rationale: Per AMA, CPT® Category II codes are a set of supplemental tracking codes used for performance measurement. • Question 23 4 out of 4 points What publications does the AMA copyright and maintain? a. CPT® codebook and CPT® Assistant a. CPT® codebook and CPT® Assistant Response Feedback: Rationale: CPT® (all three categories) and CPT® Assistant is published, copyrighted and maintained by AMA. • Question 24 4 out of 4 points What is the correct HCPCS Level II code for a removable metatarsal foot arch support that is pre-molded? c. L3050 c. L3050 Response Feedback: Rationale: In the HCPCS Level II Index, look for Support/arch. You are directed to see codes L3040-L3090. When you review the L codes, L3050 represents a removable, premolded, metatarsal foot arch support. • Question 25 4 out of 4 points How often are HCPCS Level II permanent national codes updated? a. Annually a. Annually Response Feedback: Rationale: Permanent national codes are updated once a year in January. Sunday, November 19, 2017 9:11:58 AM MST • Question 1 10 out of 10 points A provider performs a punch biopsy of two pre-cancerous lesions on the patient's back, which he has determined to be actinic keratosis (AK). List the ICD-10-CM code for the AK. d. L57.0 d. L57.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Keratosis/actinic and you are referred to L57.0. This is verified by looking in the Tabular List under L57.0. • Question 2 10 out of 10 points When coding multiple burns, which is correct? c. Sequence first the code reflecting the highest degree of burn c. Sequence first the code reflecting the highest degree of burn Response Feedback: Rationale: ICD-10-CM Official Coding Guidelines Section I.C.19.d.1. Sequencing of burn and related condition codes, “Sequence first the code that reflects the highest degree of burn when more than one burn is present.” • Question 3 10 out of 10 points A patient presents for tattooing of the nipple and areola of both breasts after undergoing breast reconstruction. The total area for the right breast is 11.5 cm2 and for the left breast of 10.5 cm2. Select the CPT® code(s) for this procedure. a. 11921, 11922 a. 11921, 11922 Response Feedback: Rationale: Code selection is based on square centimeters. The total square centimeters is 11.5 cm² plus 10.5 cm² equaling 22.0 cm². Code11921 is used to report 6.1 cm² to 20 cm²; 11922 is used to report each additional 20 cm² or part thereof. The codes are located by looking in the CPT® Index for Tattoo/Skin which refers you to 11920-11922. 11922 is an add-on code making it exempt from modifier 51. • Question 4 10 out of 10 points A patient presents to the Dermatologist with a suspicious lesion on her left arm and another one on her right arm. After examination the physician feels these lesions present as highly suspicious and obtains consent to perform punch biopsies on both sites. After prepping the area, the physician injects the sites with Lidocaine 1% and .05% Epi. A 3 mm punch biopsy of the lesion of the left arm and a 4mm punch biopsy of the lesion of the right arm is taken. The sites are closed with a simple one-layer closure and the patient is to return in 10 days for suture removal and to discuss the pathology results. The patient tolerated the procedure well. Select the CPT® code(s) for this procedure. b. 11100, 11101 b. 11100, 11101 Response Feedback: Rationale: Look in the CPT Index for Biopsy/Skin or Skin/Biopsy and you are directed to 11100, 11101. Code 11100 is reported for biopsy of the first lesion of the left arm and add-on code 11101 is reported for the biopsy of the lesion on the right arm. The simple one-layered closure (simple repair) is included in the codes and is not reported separately. • Question 5 10 out of 10 points Patient presents with a cyst on the arm. Upon examination the physician decides to incise and drain the cyst. The site is prepped and the physician takes a scalpel and cuts into the cyst. Purulent fluid is extracted from the cyst and a sample of the fluid is sent to the laboratory for evaluation. The wound is irrigated with normal saline and is covered with a bandage. The patient is to return in a week to ten days to re-examine the wound. Select the CPT® code for this procedure. a. 10060 a. 10060 Response Feedback: Rationale: Codes 10060-10061 describe the incision and drainage of abscess of a cyst; simple or complicated/multiple. There is no indication the cyst is complicated resulting in 10060. Look in the CPT® Index for Incision and Drainage/Cyst/Skin. • Question 6 10 out of 10 points A patient presents to the emergency department with multiple lacerations. After inspection and cleaning of the multiple wounds the physician proceeds to close the wounds. The documentation indicates the following: 2.7 cm complex closure to the right upper abdominal area, a 1.4 cm complex repair to the right buttock, a 7.4 cm intermediate repair to the right arm, a 3.8 cm intermediate repair to the left cheek, an 8.1 cm intermediate repair to the scalp and a 2.3 cm simple repair the right lower lip. What are the correct CPT® codes to report for this example? d. 13101, 12035-59, 12052-59, 12011-59 d. 13101, 12035-59, 12052-59, 12011-59 Response Feedback: Rationale: Repair (Closure) codes are classified as Simple, Intermediate, and Complex. Locate the code ranges by looking in the CPT Index for Repair/Skin/Wound, then selecting Complex, Intermediate, or Simple. Code selection is based on the type of repair and the anatomical location. Repairs within the same anatomical location are added together. The abdomen and buttock are both part of the trunk, so these repairs are added together. The most complex repair is coded first; CPT® code 13101 is reported for the complex repair of abdominal and buttock with total closure of 4.1 cm. The arms and scalp are in the same anatomical category , so the repair length for the arm and scalp are added together. CPT® code 12035-59 is reported for the intermediate repair of for the arm and scalp with total closure of 15.5, CPT® code 12052-59 is reported for the 3.8 cm intermediate repair of the cheek and CPT® 12011-59 is reported for the 2.3 cm simple repair of the lip. The CPT® guidelines state to use modifier 59 when more than one classification of wounds is repaired. Look in the CPT® Index for Repair/Wound and you will see the code ranges for Complex, Intermediate, and Simple. • Question 7 10 out of 10 points Operative Report: INDICATIONS FOR SURGERY: The patient has a suspicious 1.5 cm lesion of the left upper medial thigh. Clinical diagnosis of this lesion is unknown, but due to the appearance, malignancy is a realistic concern. The area is marked for elliptical excision with gross normal margins of 3-4 mm in relaxed skin tension lines of the respective area and the best guess at the resulting scars was drawn. The patient observed these marks in a mirror to understand the surgery and agreed on the location and we proceeded. PROCEDURE: The areas were infiltrated with local anesthetic. The area was prepped and draped in sterile fashion. The suspicious left upper most medial thigh lesion was excised as drawn, into the subcutaneous fat. This was sent for permanent pathology. The wound was closed in layers using 3.0 monocryl and 5.0 chromic. The repair measured 5.0 cm. Meticulous homeostasis was achieved using light pressure. The patient tolerated the procedure well. What CPT® code(s) should be reported for this example? c. 12032, 11403-51 c. 12032, 11403-51 Response Feedback: Rationale: The lesion is suspicious and not classified as malignant. A code from Excision-Benign Lesions is reported. Locate the code ranges by looking in the CPT Index for Excision/Skin/Lesion, Benign. Code selection is based on anatomic location and size in centimeters. The size is noted as 1.5 cm with margins of 3 mm on each side. 3 mm = 0.3 cm. 1.5cm + 0.3 cm + 0.3 cm = 2.1 cm. Code range 11400–11406 is used for excision of benign lesions on the trunk, arms, or legs. A size of 2.1 cm is reported with 11403. The note supports that an intermediate closure was performed. The repair measured 5.0 cm and is documented to be in layers, indicating an intermediate closure. Code range 12031–12037 is used to report intermediate repairs on the scalp, axillae, trunk and/or extremities. The repair measures 5 cm, making 12032 the correct code. • Question 8 10 out of 10 points A 32-year-old female is having excision of a mass in her left breast. The physician makes a curved incision along the inferior and medial aspect of the left areola. A breast nodule, measuring approximately 1 cm in diameter, was identified. It appeared to be benign. It was firm, gray, and discrete. It was completely excised. There was no gross evidence of malignancy. The bleeding was controlled with electrocautery. The skin edges were approximated with a continuous subcuticular 4-0 Vicryl suture. Indermil tissue adhesive was applied to the skin as well as a dry gauze dressing. What is the correct CPT® code to report for this example? a. 19120-LT a. 19120-LT Response Feedback: Rationale: The excision of a breast cyst is reported with 19120 and is found in the CPT® index by finding Breast/Excision/Lesion. Review the codes to choose the appropriate service. • Question 9 10 out of 10 points Patient presents to the dermatologist for the removal of warts on his hands. Upon evaluation it is noted the patient has nine warts on his right hand and 10 on his left hand, all of which he has indicated he would like removed today. After discussion with the patient regarding the destruction method and aftercare the patient agreed to proceed. Using cryosurgery the physician applied two squirts of liquid nitrogen on each of the warts on his right and left hand. Aftercare instructions were given to the patient's wife. The patient tolerated the procedure well. What CPT® code(s) should be reported for this example? b. 17111 b. 17111 Response Feedback: Rationale: The destruction of warts is reported with 17110 or 17111. Code selection is based on the number of warts destroyed. The patient had a total of 19 warts destroyed. 17110 describes destruction up to 14 lesions; 17111 describes the destruction of 15 or more lesions. The correct CPT® code is 17111 for removal of 19 warts. Look in the CPT® Index for Destruction/Warts/Flat. • Question 10 0 out of 10 points A patient has a squamous cell carcinoma on the tip of the nose. After prepping the patient and site, the physician removes the tumor (first stage) and divides it into seven blocks for examination. Seeing positive margins, he removes a second stage, which he divides into five blocks. The physician again identifies positive margins. He performs a third stage and divides the specimen into three blocks proving to be clear of the skin cancer. What are the correct CPT® codes to report for this example? b. 17311, 17312, 17312 a. 17311, 17312, 17312, 17315, 17315 Response Feedback: Rationale: Codes are reported by the number of stages and tissue blocks. There were a total of 3 stages performed CPT® 17311 is reported for the first stage and add-on code 17312,+17312is listed twice for each additional stage. The first stage was divided into seven tissue blocks. Code 17315 is reported for each piece of tissue beyond five for any one stage. It isn’t appropriate to add and average all blocks from all layers. CPT® +17315, +17315 for the sixth and seventh block. Look in the CPT® Index for Mohs Micrographic Surgery. Sunday, November 19, 2017 9:12:30 AM MST • Question 1 4 out of 4 points What is used for a placeholder when a code that does not have six characters to keep the 7th character extender in the 7th position? b. The letter X b. The letter X Response Feedback: Rationale: If a code that requires a 7th character does not have 6 characters; a placeholder X must be used to fill in the empty characters. • Question 2 4 out of 4 points What is commonly known as a boil of the skin? b. Furuncle b. Furuncle Response Feedback: Rationale: Carbuncles and furuncles (boils) typically are caused by a staphylococcal infection. Several furuncles together make up a carbuncle and often involve a group of hair follicles. • Question 3 4 out of 4 points What is the correct diagnosis code to report initial treatment of an infected post procedural wound of the right leg from a previous excision of a squamous cell carcinoma? c. T81.4XXA c. T81.4XXA Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Infection/post procedural referring you to T81.4-. In the Tabular List seven characters are needed to complete the code. Two X placeholders are for the 5th and 6th characters and the 7th character A is reported for initial encounter (or treatment). An instructional note indicates to use an additional code to identify the infection. We do not know what the type of infection so it is not coded. • Question 4 4 out of 4 points Which statement is TRUE regarding the Table of Neoplasms in ICD-10-CM? b. There are six columns in the Table of Neoplasms; Malignant Primary, Malignant Secondary, Ca in situ, Benign, Uncertain Behavior and Unspecified Behavior. b. There are six columns in the Table of Neoplasms; Malignant Primary, Malignant Secondary, Ca in situ, Benign, Uncertain Behavior and Unspecified Behavior. Response Feedback: Rationale: The Table of Neoplasms in ICD-10-CM is broken down into six columns: Malignant Primary, Malignant Secondary, Ca in situ, Benign, Uncertain Behavior, and Unspecified Behavior. • Question 5 4 out of 4 points What is another term for hives? b. Urticaria b. Urticaria Response Feedback: Rationale: Urticaria can also be described as hives and shows on the skin as raised, red, itchy wheals. • Question 6 0 out of 4 points Patient presents to the physician for removal of a squamous cell carcinoma of the right cheek. After the area being prepped and draped in a sterile fashion the surgeon measured the lesion, documenting the size of the lesion to be 2.3 cm in its largest diameter. Additionally, the physician took margins of 2 mm on each side of the lesion. Single layer closure was performed. The patient tolerated the procedure well. What CPT® code(s) is/are reported? a. 11643, 12013 c. 11643 Response Feedback: Rationale: Squamous cell carcinoma is a malignant neoplasm. In the CPT® Index look for Skin/Excision/Lesion/Malignant and you are directed to many codes including code range 11600-11646. Code selection is based on location and size. The lesion is on the right cheek, narrowing the range to 11640-11646. The largest diameter is 2.3 cm plus 0.4 cm (2 mm + 2 mm on each side) making the excised diameter 2.7 cm. The correct code selection is 11643. Simple one-layer repair is not reported separately. • Question 7 4 out of 4 points While whittling a piece of wood, the patient sustained an avulsion injury to a portion of his left index finger and underwent formation of a direct pedicle graft with transfer from his left middle finger. What CPT® code is reported? c. 15574 c. 15574 Response Feedback: Rationale: In the CPT® Index look for Pedicle Flap/Formation, you are directed to 15570-15576. Code selection is based on location. Category guidelines for Flaps indicate the codes refer to the recipient site not the donor site. The term pedicle indicates this is a flap not a direct graft, where skin is removed from one site and transferred to another. Instead, a flap of skin is raised, leaving it attached to its source location to maintain blood supply until it is established sufficiently in the new site. Code 15574 describes a direct pedicle graft of the hands with or without transfer. • Question 8 4 out of 4 points The patient is here to see us about some skin tags on her neck and both underarms. She has had these lesions for some time; they are irritated by her clothing, itch, and at times have a burning sensation to them. We discussed treatment options along with risks. Informed consent was obtained and we proceeded. We removed 16 skin tags from the right axilla, 16 skin tags from the left axilla, 10 from the right side of the neck and 17 from the left side of the neck. What CPT® and ICD-10-CM codes are reported? c. 11200, 11201 x 5, L91.8 c. 11200, 11201 x 5, L91.8 Response Feedback: Rationale: In the CPT® Index look for Skin/Tags/Removal and you are directed to codes 11200, 11201. Code selection is based on the number of skin tags removed. A total of 59 skin tags were removed. Code 11200 is reported for the first 15. 11201 is reported for each remaining 10 (or part thereof) removed. The words “part there of” in the code description mean you do not need to have a complete total of 10 lesions to report the add-on code. The add-on code can be reported if the additional lesions are 10 and under; so it is not necessary to append modifier 51 to this add-on code. 11200, 11201 x 5 is correct. Modifier 51 is not required for an add-on code. In the ICD-10-CM Alphabetic Index look for Tag/skin and you are directed to L91.8. Verify in the Tabular List. • Question 9 0 out of 4 points Patient is a 69 year-old woman with a biopsy-proven squamous cell carcinoma of her left forearm measuring 2.3 cm in greatest diameter. The area was marked with 4 mm gross normal margins. This area was removed as drawn, and the surgeon then incised his planned rhomboid flap, elevating the full-thickness flap into the defect and closing the sites in layers using 3-0 Monocryl, 4-0 Monocryl and 5-0 Prolene. The patient tolerated the procedure well. Final measurements were 2.7 cm x 2.1 cm. What CPT® code(s) is/are reported? b. 14020, 11603-51 c. 14020 Response Feedback: Rationale: Rhomboid flap is a flap in the shape of a rhomboid used for a rotation flap skin graft. A rotation flap is considered an adjacent tissue transfer. In the CPT® Index look for Skin Graft and Flap/Tissue Transfer and you are directed to 14000-14350. Code selection is based on location and flap size. The size of the flap is calculated in square cm and includes both the size of the primary defect and secondary defect created by the flap. CPT® guideline indicates the excision of the lesion is included in the adjacent tissue transfer. The final measurement in this case is 2.7 cm x 2.1 cm, which equals 5.67 cm2 (2.7 x 2.1 = 5.67). 14020 is the correct code. • Question 10 4 out of 4 points The patient has a suspicious lesion of the left jaw line. Clinical diagnosis of this lesion is unknown, but due to the appearance, malignancy is a realistic concern. The lesion was excised into the subcutaneous fat measuring 0.8 cm and margins of 0.1 cm on each side. Hemostasis was achieved using light pressure. The wound was closed in layers using 5.0 Monocryl and 6.0 Prolene. Pathology revealed a nevus with clear margins. What CPT® and ICD-10-CM codes are reported? b. 12051, 11441-51, D22.39 b. 12051, 11441-51, D22.39 Response Feedback: Rationale: This is excision of a benign lesion (nevus) of the face. In the CPT® Index look for Skin/Excision/Lesion/Benign and you are directed to code range 11400-11446. Code selection is based on location and size. The lesion is on the face, narrowing the code selection to 11440-11446. The lesion size is documented as 0.8 cm plus 0.2 cm for the margins (.1 cm on each side) for the complete excision to be 1.0 cm of the face making 11441 the correct code. Category guidelines for Excision-Benign Lesions state if the repair is intermediate (layers), a code from range 12031-12057 is reported in addition to the excision code. Code selection is again based on location and size. 12051 is the correct repair code. Modifier 51 is appended to indicate multiple procedures. For the diagnosis, look in the ICD-10-CM Alphabetic Index look for Nevus/skin/jaw directs you to D22.39 • Question 11 4 out of 4 points A patient presents with a recurrent seborrheic keratosis of the left cheek. The area was marked for a shave removal. The area was infiltrated with local anesthetic, prepped and draped in a sterile fashion. The lesion measuring 1.8 cm was shaved using an 11-blade. Meticulous hemostasis was achieved using light pressure. The specimen was sent for permanent pathology. The patient tolerated the procedure well. What CPT® code is reported? b. 11312 b. 11312 Response Feedback: Rationale: In the CPT® Index look for Shaving/Skin Lesion and you are referred to range 11300-11313. Code selection is based on location and size. This lesion is on the left cheek narrowing the range to 11310-11313. The size is 1.8 cm making 11312 the correct code choice. • Question 12 4 out of 4 points A patient presents to the ED physician with multiple burns. After examination the physician determines the patient has third-degree burns of the anterior and posterior portion of his left leg, starting at the knee extending above the ankle (4.5%). He also has third-degree burns of the anterior portion of the left side of his chest (12.5%). The patient also has second-degree burns on his left upper arm (7%). What ICD-10-CM codes are reported? b. T24.392A, T21.31XA, T22.232A, T31.21 b. T24.392A, T21.31XA, T22.232A, T31.21 Response Feedback: Rationale: ICD-10-CM guideline 1.C.19.d.1. indicates when more than one burn is present to sequence first the code reflecting the highest degree of burn. In the ICD-10-CM Alphabetic Index, look for Burn/lower/limb/multiple sites, except ankle and foot/left/third degree referring you to T24.392. Third-degree burns to the left leg at the knee extending above the ankle (multiple sites) are coded as T24.392; third-degree burns to the left side of the chest is found in the Alphabetic Index by looking for Burn/chest wall/third degree referring you to code T21.31 and second-degree burns to the left upper arm is found in the Alphabetic Index by looking for Burn/upper limb/above elbow — see Burn, above elbow. Look in the Alphabetic Index for Burn/above elbow/left/second degree referring you to code T22.232. The Tabular List indicates all these codes need seven characters. The 7th character A, initial encounter, is reported for all the burn codes and the X placeholder is used to keep the A in the 7th position. Last code to report is the extent or percentage of the total body surface area burned, which is 24 percent. Look in the Alphabetic Index for Burn/extent (percentage of body surface)/20-29 percent. Category T31 is used to identify the extent of the body surface involved. The 4th character identifies the total body surface area (TBSA) involved (all degree burns totaled). The 5th character identifies the percentage of body surface with third-degree burns only. Third-degree burns total 17% reporting the 5th character 1. Look in the Alphabetic Index for Burn/extent/20-29 percent/with 10-19 percent third degree burns referring you to T31.21. The TBSA codes are only five characters long and do not need a 7th character extender to complete the code. • Question 13 4 out of 4 points A 63 year-old patient arrives for skin tag removal. As previously noted in her other visit, she has 3 located on her face, 4 on her shoulder and 15 on her back. The physician removes all the skin tags with no complications. What CPT® code(s) is/are reported for this encounter? d. 11200, 11201 d. 11200, 11201 Response Feedback: Rationale: Look in the CPT® Index for Removal/Skin Tags and you are directed to 11200, 11201. Based on the documentation, the total number of skin tags removed is 22. Code 11200 is reported for the removal of up to and including 15 lesions. Notice the wording for 11201, which includes each additional 10 lesions, or part thereof. The words part thereof in the code description means you do not need to have a complete total of 10 skin tags to report the add-on code. The add-on code can be reported if the additional skin tags removed are 10 and under; so it is not necessary to append modifier 52 to this add-on code. Modifier 51 is not appended to add-on codes. Report 11200, 11201 for the removal of 22 skin tags. • Question 14 4 out of 4 points A 14 year-old boy was thrown against the window of the car on impact. The resulting injury was a star-shaped pattern cut to the top of his head. In the ED, the MD on call for plastic surgery was asked to evaluate the injury and repair it. The total length of the intermediate repair was 5+4+4+5 cm (18 cm total). The star-like shape allowed the surgeon to pull the wound edges together nicely in a natural Y-plasty in two spots. What CPT® code is reported for the repair? c. 12035 c. 12035 Response Feedback: Rationale: Category guidelines in the Adjacent Tissue Transfer or Rearrangement state that these codes are not to be used when the repair of a laceration incidentally results in a configuration such as a Y-plasty. Look in the CPT® Index for Repair/Skin/Wound/Intermediate and you are directed to code range 12031-12057. Instructions in the category guidelines for Repair state to add up all the lengths when in the same repair classification and anatomical sites grouped together into the same code descriptor. Based on the documentation, the total length is 18 cm. An intermediate repair of this length on the top of the head is reported with code 12035. • Question 15 4 out of 4 points The patient is here to follow-up for a keloid excised from his neck in November of last year. He believes it is coming back. He does have a recurrence of the keloid on the superior portion of the scar. Because the keloid is still small, options of an injection or radiation to the area were discussed. It was agreed our next course should be a Kenalog injection. Risks associated with the procedure were discussed with the patient. Informed consent was obtained. The area was infiltrated with 1.5 cc of medication. This was a mixture of 1 cc of Kenalog-10 and 0.5 cc of 1% lidocaine with epinephrine. He tolerated the procedure well. What codes are reported? b. 11900, J3301, L91.0 b. 11900, J3301, L91.0 Response Feedback: Rationale: Using the CPT® Index look for Injection/Lesion/Skin and you are referred to CPT® codes 11900, 11901. Code selection is based on the number of lesions treated, not the number of injections. In this case one lesion is treated, making 11900 the correct code. Using the HCPCS Level II codebook, look in the Table of Drugs and Biologicals for Kenalog-10 and you are referred to See Triamcinolone Acetonide. When you look up Triamcinolone Acetonide, you are referred to J3300 and J3301. Verify codes and you will see that Kenalog-10 is not listed, but Kenalog is listed under J3301. Report J3301 10 mg. Using the ICD-10-CM Alphabetic Index look for Keloid, cheloid/scar referring you to L91.0. Verify the code in the Tabular List. • Question 16 4 out of 4 points A 56 year-old pro golfer is having Mohs micrographic surgery for skin cancer on his forehead. The surgeon performs the surgery with two stages. The first stage includes 4 tissue blocks and the second stage includes 6 tissue blocks. What are the codes for both stages? b. 17311, 17312, 17315 b. 17311, 17312, 17315 Response Feedback: Rationale: Mohs codes are selected based on location and number of stages, each including up to five blocks. There is an add-on code for each additional block after the first five blocks in any stage. In the CPT® Index look for Mohs Micrographic Surgery and you are directed to 17311-17315. Code 17311 is for the first stage with four tissue blocks, and 17312 for the second stage with five tissue blocks, based on the documentation of the site forehead. The remaining 6th tissue block prepared in the 2nd stage is reported with the add-on code 17315. • Question 17 4 out of 4 points Operative Report PREOPERATIVE DIAGNOSIS: Squamous cell carcinoma, scalp. POSTOPERATIVE DIAGNOSIS: Squamous carcinoma, scalp. PROCEDURE PERFORMED: Excision of Squamous cell carcinoma, scalp with Yin-Yang flap repair ANESTHESIA: Local, using 4 cc of 1% lidocaine with epinephrine. COMPLICATIONS: None. ESTIMATED BLOOD LOSS: Less than 5 cc. SPECIMENS: Squamous cell carcinoma, scalp sutured at 12 o’clock, anterior tip INDICATIONS FOR SURGERY: The patient is a 43 year-old white man with a biopsy-proven squamous cell carcinoma of his scalp measuring 2.1 cm. I marked the area for excision with gross normal margins of 4 mm and I drew my planned Yin-Yang flap closure. The patient observed these markings in two mirrors, so he can understand the surgery and agreed on the location and we proceeded. DESCRIPTION OF PROCEDURE: The area was infiltrated with local anesthetic. The patient was placed prone, his scalp and face were prepped and draped in sterile fashion. I excised the lesion as drawn to include the galea. Hemostasis was achieved with the Bovie cautery. Pathologic analysis showed the margins to be clear. I incised the Yin-Yang flaps and elevated them with the underlying galea. Hemostasis was achieved in the donor site using Bovie cautery. The flap rotated into the defect with total measurements of 2.9 cm x 3.2 cm. The donor sites were closed and the flaps inset in layers using 4-0 Monocryl and the skin stapler. Loupe magnification was used. The patient tolerated the procedure well. What CPT® and ICD-10-CM codes are reported? a. 14020, C44.42 a. 14020, C44.42 Response Feedback: Rationale: In the CPT® codebook, Yin-Yang flap repair falls under Adjacent Tissue Transfer codes. Look in the CPT® Index for Skin Graft and Flap/Tissue Transfer which directs you to 14000-14350. Based on the measurement calculating to 9.28 sq. cm. (2.9 cm x 3.2 cm = 9.28 cm²) and the location of the scalp, the correct CPT® code is 14020. In ICD-10-CM go to the Table of Neoplasms and look for skin NOS/scalp/squamous cell carcinoma/Malignant Primary column and you are referred to C44.42. Verify in the Tabular List. • Question 18 4 out of 4 points PREOPERATIVE & POSTOPERATIVE DIAGNOSES: 1. Macromastia. 2. Back pain. 3. Neck pain. 4. Shoulder pain. 5. Shoulder grooving. 6. Intertrigo. NAME OF PROCEDURE: 1. Right breast reduction of 1950 g. 2. Right free-nipple graft. 3. Left breast reduction of 1915 g. 4. Left free-nipple graft. INDICATIONS FOR SURGERY: The patient is a 43 year-old female with macromastia and associated back pain, neck pain, shoulder pain, shoulder grooving and intertrigo. She desired a breast reduction. Because of the extreme ptotic nature of her breasts, we felt she would need a free-nipple graft technique. In the preoperative holding area, we marked her for this free-nipple graft technique of breast reduction. The patient observed these markings so she could understand the surgery and agree on the location, and we proceeded. The patient also was morbidly obese with a body mass index of 54. Because of this, we felt she met the criteria for DVT prophylaxis, which included Lovenox injection. The patient understood this would increase her risk of bleeding. She also made it known she is a Jehovah's Witness and refused blood products, but she did understand her risk of bleeding would significantly increase and we proceeded. DESCRIPTION OF PROCEDURE: The patient was given 40 mg of subcutaneous Lovenox in the preoperative holding area. She was then taken to the operating room. Bilateral thigh-high TED hose, in addition to bilateral pneumatic compression stockings were used throughout the procedure. IV Ancef 1 g was given. Anesthesia was induced. Both arms were secured on padded arm boards using Kerlix rolls. A similar body Bair Hugger was placed. The chest and abdomen were prepped and draped in sterile fashion. I began by circumscribing around each nipple-areolar complex using a 42-mm areolar marker. On each side the free-nipple grafts were harvested. They were marked to be side specific and were stored on the back table in moistened lap sponges. Meticulous hemostasis was achieved using Bovie cautery. The tail of the apex of each breast was de-epithelialized using the scalpel. I amputated the inferior portion of the breast from the right side. Again, meticulous hemostasis was achieved using the Bovie cautery. There were also large feeder vessels divided and ligated using either a medium Ligaclip or 3-0 silk tie sutures. I then moved to the left and again amputated the inferior portion of the breast. Meticulous hemostasis was achieved using the Bovie cautery. Each of these wounds were temporarily closed using the skin stapler. The patient was then sat up. I felt we had achieved a very symmetrical result. The new positions for the nipple-areolar complexes were marked with a 42-mm areolar marker and methylene blue. The patient was then placed in the supine position and the new positions for the nipple-areolar complexes were de-epithelialized using the scalpel. Meticulous hemostasis was then achieved again using the Bovie cautery. The free-nipple grafts were then retrieved from the back table. They were each defatted using scissors and were placed in an on-lay fashion on the appropriate side, and each was inset using 5-0 plain sutures. Vents were made in the skin graft to allow for the egress of fluid on each side. A vertical mattress suture was used, tied over a piece of Xeroform in critical areas of each of the nipple-areolar complexes. A Xeroform bolster wrapped over a mineral oil-moistened sponge was affixed to each of the nipple-areolar complexes using 5-0 nylon suture. The vertical and transverse incisions were closed using 3-0 Monocryl, both interrupted and running suture, and 5-0 Prolene. The patient tolerated the procedure well. Again, meticulous hemostasis was achieved using the Bovie cautery. She was given another 1 g of Ancef at the 2-hour mark by our anesthesiologist, and was taken to the recovery room in good condition. What CPT® code is reported? d. 19318-50 d. 19318-50 Response Feedback: Rationale: With breast reduction surgery, either reduction mammaplasty or reduction mammoplasty both is correct. In the CPT® Index look for Reduction/Mammaplasty and you are referred to 19318. Because this is a unilateral code per CPT®, append modifier 50. Normally, with reduction mammoplasty the patient’s nipple is repositioned with a pedicle of tissue after removal of the breast tissue and is considered part of the reduction mammoplasty. • Question 19 4 out of 4 points Patient presents with a suspicious lesion on her left arm. With the patient’s permission the physician marked the area for excision. The margins and lesion measured a total of 0.9 cm. The wound measuring 1.2 cm was closed in layers using 4-0 Monocryl and 5-0 Prolene. Pathology later reported the lesion to be a sebaceous cyst. What codes are reported? b. 12031, 11401-51, L72.3 b. 12031, 11401-51, L72.3 Response Feedback: Rationale: Understanding a sebaceous cyst is benign, look in the CPT® Index for Skin/Excision/Lesion/Benign referring you to 11400-11446. The lesion is coded based on size and location. Report 11401 for excision of the 0.9 cm arm lesion. The note also indicates the wound was closed in layers allowing for intermediate closure and is also coded based on location and size. Report 12031 for intermediate closure of 1.2 cm. Modifier 51 is appended to 11401 to show additional procedures in the same session. In the ICD-10-CM Alphabetic Index look for Cyst/sebaceous directing you to L72.3. Verify in the Tabular List. • Question 20 4 out of 4 points A malignant lesion of the forehead measuring 1.0 cm was removed. The operative report states skin margins are 1.1 cm on all sides. Layered closure of 3.5 cm was performed. How is this coded? d. 11644, 12052-51 d. 11644, 12052-51 Response Feedback: Rationale: CPT® guidelines under Excision—Malignant Lesions state closure other than simple can be coded separately. Look in the CPT® Index for Skin/Excision/Lesion/Malignant and you are referred to 11600-11646. Excision codes are based on location and size. The documented size is 1.0 cm with 1.1 cm margins on all sides making the total size with two margins 3.2 cm. Report 11644 for the excision of the forehead lesion. Because the closure is intermediate, it is also reported. Look in the CPT® Index for Repair/Skin/Wound/Intermediate and you are referred to 12031-12057. The intermediate closure is based on location and size and reported with code 12052. Modifier 51 is appended to indicate multiple procedures. • Question 21 4 out of 4 points Wire placement in the lower outer aspect of the right breast was performed by a radiologist the day prior to this procedure. During this operative session, the surgeon created an incision through the wire track and the wire track was followed down to its entrance into breast tissue. A nodule of breast tissue was noted immediately adjacent to the wire. This entire area was excised by sharp dissection, sent to pathology and returned as a benign lesion. Bleeders were cauterized, and subcutaneous tissue was closed with 3-0 Vicryl. Skin edges were approximated with 4-0 subcuticular sutures and adhesive strips were applied. The patient left the operating room in satisfactory condition. What is/are the correct code(s) for the surgeon’s service? c. 19125-RT c. 19125-RT Response Feedback: Rationale: Documentation indicates a localization wire was placed prior to the surgery by a radiologist. You are asked to select the code for the surgeon’s service; therefore, code 19285 is not reported. In the CPT® Index look for Excision/Breast/Lesion referring you to 19120, 19125, 19126. Code 19125 describes excision of breast lesion identified preoperatively with a radiology marker. Modifier RT is appended to indicate the right side. • Question 22 0 out of 4 points Operative Report PREOPERATIVE DIAGNOSIS: Diabetic foot ulceration. POSTOPERATIVE DIAGNOSIS: Diabetic foot ulceration. OPERATION PERFORMED: Debridement and split thickness autografting of left midfoot. ANESTHESIA: General endotracheal. INDICATIONS FOR PROCEDURE: This patient with multiple complications from type 2 diabetes has developed skin ulcerations which were debrided and homografted last week. The homograft is taking quite nicely; the wounds appear to be fairly clean. He is ready for autografting. DESCRIPTION OF PROCEDURE: After informed consent the patient is brought to the operating room and placed in the supine position on the operating table. Anesthetic monitoring was instituted; general anesthesia was induced. The left lower extremity is prepped and draped in a sterile fashion. Staples were removed and the homograft was debrided from the surface of the wounds. One wound appeared to have healed; the remaining two appeared to be relatively clean. We debrided this sharply with good bleeding in all areas. Hemostasis was achieved with pressure, Bovie cautery, and warm saline soaked sponges. With good hemostasis a donor site was then obtained on the left anterior thigh, measuring less than 100 cm2. The wounds were then grafted with a split-thickness autograft that was harvested with a patch of Brown dermatome set at 12,000 of an inch thick. This was meshed 1.5:1. The donor site was infiltrated with bupivacaine and dressed. The skin graft was then applied over the wound, measured approximately 60 cm2 in dimension on the left midfoot. This was secured into place with skin staples and was then dressed with Acticoat 18's, Kerlix incorporating a catheter, and gel pad. The patient tolerated the procedure well. The right foot was redressed with skin lubricant sterile gauze and Ace wrap. Anesthesia was reversed. The patient was brought back to the ICU in satisfactory condition. What CPT® and ICD-10-CM codes are reported? c. 11044-78, 15120-78, 15004-78, E11.621, L97.421 b. 15120-58, 15004-58, E11.621, L97.421 Response Feedback: Rationale: The wound was prepped with sharp debridement. Look in the CPT® Index for Creation/Recipient Site and you are referred to 15002-15005. Code selection is based on location and size resulting in 15004 as the correct code for the foot. Then a split-thickness graft was harvested. Look in the CPT® Index for Skin Graft and Flap/Split Graft referring you to codes 15100, 15101, 15120, 15121. The measurement applies to the recipient area, which is 60 cm². A split thickness autograft to the foot for the first 100 sq. cm is coded with 15120. The operative note states, “The homograft is taking quite nicely; the wounds appear to be fairly clean. He is ready for autografting,” indicating this is a staged procedure and modifier 58 is appended. In the ICD- 10-CM Alphabetic Index complications of diabetes are reported with combination codes. Diabetes is specific to the type of diabetes, and documentation supports this as type 2, with midfoot skin ulcer. Look in the Alphabetic Index for Diabetes/type 2/with/foot ulcer referring you to E11.621. The Tabular List instructs to use an additional code to identify the site of the ulcer L97.1-L97.9, L98.41-L98.49. The graft is performed on the left midfoot for the skin ulcer, L97.421. • Question 23 0 out of 4 points Patient is a 53 year-old female who yesterday underwent Mohs surgery with Dr. Smith to remove a basal cell carcinoma of her scalp. Due to the size of the defect Dr. Smith requested a Plastic Surgeon to reconstruct the site. Dr. Jones discussed with the patient his planned closure, which was a Ying-Yang type flap. The patient agreed and we proceeded. The area was prepped and draped in a sterile fashion being careful to keep betadine solution out of the open wound. Wound preparation was done by excising an additional 1 mm margin to freshen the wound and excising the wound deeper. Starting on the right, Dr. Jones incised his planned flap, elevating the flap with full-thickness and subcutaneous fat, staying superior to the galea; then Dr. Jones incised his planned flap on the left elevating the flap with full-thickness and subcutaneous fat. Both flaps were rotated together and the wound was temporarily closed using the skin stapler. Once it was determined there was minimal tension on the wound; the galea was approximated using 4.0 Monocryl. The wound was then closed in layers using 5-0 Monocryl and a 35R skin stapler. Meticulous hemostasis was achieved through-out the procedure with the Bovie cautery. Final measurements of the wound were 36.25 cm squared. What CPT® code(s) is/are reported? [None Given] b. 14301, 15004-51 Response Feedback: Rationale: A Ying Yang flap is a rotation flap coded using Adjacent Tissue Transfer codes. In the CPT® Index, look for Skin Graft and Flap/Tissue Transfer and you are directed to codes 14000-14350. When the defect size is less than 30 sq. cm, it is coded based on location and size. When it is more than 30 sq. cm, it is coded using 14301 and 14302. In this case, we have a flap 36.25 sq. cm. 14301 is reported for the first 30 sq. cm – 60.0 sq. cm. Wound preparation was also performed. In the CPT® Index look for Integumentary System/Skin Replacement Surgery and Skin Substitutes/Surgical Preparation referring you to 15002-15005. Code 15004 is reported for the scalp. Modifier 51 is used to indicate multiple procedures were performed. • Question 24 0 out of 4 points The patient is here because the cyst in her chest has come to a head and is still painful even though she has been on antibiotics for a week. I offered to drain it for her. After obtaining consent, we infiltrated the area with 1 cc of 1% lidocaine with epinephrine, prepped the area with Betadine and incised and opened the cyst in the relaxed skin tension lines of her chest, and removed the cystic material. There was no obvious purulence. We are going to have her clean this with a Q-tip. We will let it heal on its own and eventually excise it. I will have her come back a week from Tuesday to reschedule surgery. What CPT® and ICD-10-CM codes are reported? [None Given] c. 10060, L72.9 Response Feedback: Rationale: The physician performed an incision and drainage (I & D) of a cyst on the chest. To find the code, look in the CPT® Index for Incision and Incision and Drainage/Cyst/Skin and you are directed to 10040, 10060, 10061. 10040 is for acne surgery. 10060 and 10061 are for I & D of a cyst. Only one cyst was drained making 10060 the correct code. In the ICD-10-CM Alphabetic Index look for Cyst/skin and you are referred to L72.9. Verification in the Tabular List confirms code selection. • Question 25 0 out of 4 points Patient is an 81 year-old male with a biopsy-proven basal cell carcinoma of the posterior neck just near his hairline; additionally, the patient had two other areas of concern on his cheek. Informed consent was obtained and the areas were prepped and draped in the usual sterile fashion. Attention was first directed to the basal cell carcinoma of the neck. I excised the lesion measuring 2.6 cm as drawn down to the subcutaneous fat. With extensive undermining of the wound I closed it in layers using 4.0 Monocryl, 5.0 Prolene and 6.0 Prolene; the wound measured 4.5cm. Attention was then directed to the other two suspicious lesions on his cheek. After administering local anesthesia, I proceeded to take a 3mm punch biopsy of each lesion and was able to close with 5.0 Prolene. The patient tolerated the procedures well. Pathology later showed the basal cell carcinoma was completely removed and the biopsies indicated actinic keratosis. What CPT® codes should be reported? [None Given] d. 13132, 11623-51, 11100-59, 11101 Response Feedback: Rationale: Three lesions were addressed. The first lesion is a malignant neoplasm of the neck (basal cell carcinoma). Look in the CPT® Index for Skin/Excision/Lesion/Malignant. This refers you to code range 11600-11646. The range is narrowed by the location of neck, 11620-11626. The lesion size is 2.6 cm making 11623 the correct code. For this lesion, extensive undermining of the wound and the use of multiple suture materials support use of a complex closure. Complex repairs are found by looking in the CPT® Index for Repair/Skin/Wound/Complex referring you to 13100-13160. The range is narrowed again by location of neck, 13131-13133. The repair length is 4.5 cm making 13132 the correct code. After the lesion of the neck was removed the provider took two biopsies on the cheek. Look in the CPT® Index for Skin/Biopsy, which refers you to 11100, 11101. 11100 is used for the first biopsy and add-on code 11101 for the additional biopsy. Biopsies are typically included in excisions. It is necessary to use modifier 59 for the first biopsy indicating it was performed at a different location than the excision. Modifier 59 is not used on the second biopsy code because it is an add-on code. Sunday, November 19, 2017 9:12:52 AM MST • uestion 1 10 out of 10 points This type of connective tissue attaches a muscle to a bone: d. Tendon d. Tendon Response Feedback: RATIONALE: Tendons attach muscles to bone, and ligaments attach bones to other bones. • Question 2 10 out of 10 points In the CPT® book, 28400 and 28405 are used when coding a calcaneal fracture. What is the difference between these two codes? c. One includes manipulation and one does not c. One includes manipulation and one does not Response Feedback: RATIONALE: Both codes are used when coding a CLOSED treatment of a calcaneal fracture. Closed Treatment means there is not an incision made over the fracture site. Code 28400 is “without manipulation” and code 28405 is “with manipulation.” Internal fixation is not a closed treatment procedure. • Question 3 0 out of 10 points What is the correct 7th character, in ICD-10-CM, for a healing comminuted fracture of the right fibula, open, type 1? b. D d. E Response Feedback: RATIONALE: Look up Fracture/fibula/comminuted/. S82.45-. Verification in the Tabular List indicates correct 6th character is 1 for the right side. Correct 7th character is “E”, for subsequent encounter, open fracture Type 1. See list of 7th digits under category S82. Per Chapter 19 guidelines, a fracture not indicated whether displaced or not displaced should be coded to displaced. • Question 4 10 out of 10 points How would compartment syndrome of the lower extremity caused by an auto accident be listed in the ICD-10-CM Alphabetic Index? a. Syndrome/compartment (traumatic)/lower extremity a. Syndrome/compartment (traumatic)/lower extremity Response Feedback: RATIONALE: Compartment syndrome is listed under Syndrome in ICD-10-CM. The three sub-categories are non-traumatic, post-surgical, and traumatic. An auto accident would be considered a traumatic injury. • Question 5 10 out of 10 points What is the correct ICD-10-CM code for a new patient seen for a left-sided Nursemaid’s elbow? d. S53.032A d. S53.032A Response Feedback: RATIONALE: Look up Nursemaid’s elbow, S53.03-. Verification in Tabular List verifies code choice S53.032A, for left elbow, initial encounter. • Question 6 10 out of 10 points How should you code an arthroscopic abrasion chondroplasty of the medial femoral condyle? c. 29879 c. 29879 Response Feedback: RATIONALE: Look in the CPT® Index for Arthroscopy/Surgical/Knee 29871-29889. Turning to the code section, review the indentations until you arrive at abrasion arhtroplasty (Includes chondroplasty where necessary) or multiple drilling or microfracture. Note that the code is in the arthroscopy section, therefore not an open procedure. • Question 7 10 out of 10 points Mrs. Smith underwent an arthrodesis of her spine for spinal deformity, posterior approach, segments L3-L5. What procedure code is reported? d. 22800 d. 22800 Response Feedback: RATIONALE: Spinal arthrodesis is coded based on the approach; L3-L5 is considered three segments. Instrumentation is also coded, if performed. Look in the CPT® Index for Arthrodesis/Vertebra/Spinal Deformity/Posterior Approach. • Question 8 10 out of 10 points Joe was in a motorcycle accident, and fractured his right femur. The surgeon placed an intramedullary locking implant (nail) through a buttock incision. What procedure code is reported? d. 27506-RT d. 27506-RT Response Feedback: RATIONALE: The surgery is an open treatment of a closed femoral shaft fracture with internal fixation (intramedullary implant), and is reported 27506-RT. Look in the CPT® Index for Fracture/Femur/Peritrochanteric/Intramedullary Implant Shaft. Report modifier RT to indicate right femur. • Question 9 10 out of 10 points Jeff is a 13-year-old boy who fractured his left radius and ulna while snowboarding. Three weeks after the physician placed a long arm cast on Jeff, he was skateboarding and crushed the cast (without further injury to the arm). The physician replaces the cast with a short-arm fiberglass cast. What procedure code is reported for the services provided after the skateboard accident? c. 29075-58 c. 29075-58 Response Feedback: RATIONALE: The first cast or splint is included as part of the initial fracture treatment; because this was a replacement cast, it can be coded. Look in the CPT® Index for Cast/Elbow to Finger. Append modifier 58 to indicate this was a related procedure by the same physician during the postoperative period. • Question 10 10 out of 10 points Mrs. Williams has had a bunion on her right foot for many years, and is scheduled for surgery to correct this condition. The doctor plans to do a double osteotomy of the metatarsal bone. What procedure code(s) is/are reported? b. 28299-RT b. 28299-RT Response Feedback: RATIONALE: A double osteotomy can be performed on the phalanx and the metatarsal, or by making two incisions on the metatarsal bone. Look in the CPT® Index for Osteotomy/Phalanges/Toe. Sunday, November 19, 2017 9:13:15 AM MST • Question 1 4 out of 4 points A patient presents to the ED with back pain and is diagnosed with a lumbar sprain. What ICD-10-CM code is reported? b. S33.5XXA b. S33.5XXA Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Sprain/lumbar (spine) and you are directed to S33.5-. In the Tabular List this code requires a 7th character to describe the episode of care. Because the patient is presenting to the ED, this supports the definition of initial encounter. For the 5th and 6th characters use the X placeholder to maintain the 7th character position of A. Back pain is not reported because a definitive diagnosis was documented, and pain is a symptom of lumbar sprain. (See ICD-10-CM guideline I.B.6.). • Question 2 4 out of 4 points Which statement is TRUE regarding code selection for lumbago in ICD-10-CM? b. Codes exist to indicate whether sciatica is present with the low back pain. b. Codes exist to indicate whether sciatica is present with the low back pain. Response Feedback: Rationale: In ICD-10-CM, there are codes to indicate when sciatica is present with the low back pain, or low back pain is due to intervertebral disc disorder or displacement of intervertebral disc. • Question 3 4 out of 4 points In ICD-10-CM, what classification system is used to report open fracture classifications? c. Gustilo classification for open fractures c. Gustilo classification for open fractures Response Feedback: Rationale: Open fracture designations are based on the Gustilo open fracture classification. 7th characters are added to indicate the type of encounter. This classification is grouped into three major category types to indicate the mechanism of the injury, soft tissue damage and the degree of skeletal involvement. One of the main categories, Type III, is further subdivided into IIIA, IIIB, and IIIC to report levels of extensive damage. • Question 4 4 out of 4 points What is segmental instrumentation? b. A spinal fixation device attached at each end of a rod and at additional bony attachment b. A spinal fixation device attached at each end of a rod and at additional bony attachment Response Feedback: Rationale: Segmental instrumentation of the spine is a procedure used to repair a spinal defect where the fixation device is attached in at least three places: at each end of the construct (rod) and at least one additional interposed bony attachment. • Question 5 4 out of 4 points Most of the codes in ICD-10-CM Chapter 13 Diseases of the Musculoskeletal System and Connective Tissue have site and laterality designations. According to ICD-10-CM guidelines what is considered the site? c. The site may be the bone, joint or muscle involved. c. The site may be the bone, joint or muscle involved. Response Feedback: Rationale: According to ICD-10-CM guideline I.C.13.a., the site may be the bone, joint or muscle involved. • Question 6 0 out of 4 points A patient is given Xylocaine, a local anesthetic, by injection in the thigh above the site to be biopsied. A small bore needle is then introduced into the muscle, about 3 inches deep, and a muscle biopsy is taken. What CPT® code is reported for this service? c. 27324 b. 20206 Response Feedback: Rationale: In the CPT® Index, look for Biopsy/Muscle. You are referred to 20200-20206. The biopsy is taken through the skin, or percutaneously, with a needle. Although the biopsy is deep, it is performed by percutaneous technique, which is reported with 20206. • Question 7 0 out of 4 points The patient presents today for closed reduction of a nasal fracture. The depressed right nasal bone was elevated using heavy reduction forceps while the left nasal bone was pushed to the midline. This resulted in good alignment of the external nasal dorsum. What CPT® code is reported for this procedure? c. 21310 a. 21315 Response Feedback: Rationale: In the CPT® Index look for Fracture/Nasal Bone/Closed Treatment. You are referred to 21310-21320. Review codes to choose the appropriate service. 21315 is the correct code to report a displaced nasal fracture manipulated with forceps to realign the nasal bones. Code 21310 is reported when a non-displaced fracture of the nose requires no manipulation just treatment by prescribing medication and application of ice. • Question 8 4 out of 4 points A 63 year-old man presents with a neck mass to be excised. The neck mass was palpated and an incision was then made and carried down through the dermis with electrocautery. The subcutaneous tissue of the skin was opened encountering an organized mass with a benign appearance of a lipoma. Using careful blunt and sharp dissection, the mass measuring 5 cm was completely excised around its entire circumference leaving the capsule intact. The mass was removed from its posterior attachments using electrocautery. What CPT® code is reported for this procedure? d. 21552 d. 21552 Response Feedback: Rationale: In the CPT® Index, look for Neck/Tumor/Excision. You are referred to 21552-21558. Review the codes to choose the appropriate service. 21552 is the correct code to report the excision of a 5 cm mass where the surgeon incised the subcutaneous tissue to remove the mass. Codes 11426 and 11626 are reported for removal of a benign or malignant lesion, not an internal mass. • Question 9 4 out of 4 points A patient presented with a closed, displaced supracondylar fracture of the left elbow. After conscious sedation, the left upper extremity was draped and closed reduction was performed, achieving anatomical reduction of the fracture. The elbow was then prepped and with the use of fluoroscopic guidance, two K-wires were directed crossing the fracture site and piercing the medial cortex of the left distal humerus. Stable reduction was obtained, with full flexion and extension. K-wires were bent and cut at a 90-degree angle. Telfa padding and splint were applied. What CPT® code(s) is/are reported? b. 24538-LT b. 24538-LT Response Feedback: Rationale: This is a supracondylar fracture of the elbow repaired by percutaneous fixation. In the CPT® Index look for Fracture/Humerus/Supracondylar/Percutaneous Fixation and you are referred to 24538. Modifier LT is appended to indicate the procedure is performed on the left side. The application of the first cast or splint is included in the fracture codes. See the guidelines before Application of Casts and Strapping in your CPT® codebook. Fluoroscopy guidance 76000, is listed as a separate procedure; therefore, is included in the procedure. • Question 10 4 out of 4 points A 27 year-old presents with right-sided thoracic myofascial pain. A 25-gauge 1.5-inch needle on a 10 cc controlled syringe with 0.25% bupivacaine was used. After negative aspiration, 2 cc were injected into each trigger point. A total of four trigger points were injected. A total of 8 cc of bupivacaine was used on the rhomboid major, rhomboid minor, and levator scapular muscles. What CPT® code(s) is/are reported for this procedure? a. 20553 a. 20553 Response Feedback: Rationale: In the CPT® Index look for Injection/Trigger Point(s)/Three or More Muscles. You are referred to 20553. Review the code to verify accuracy. 20553 covers the three muscles (rhomboid major, rhomboid minor and scapular muscles) with a total of four (multiple) trigger point injections. Codes for trigger point injections are determined by the number of muscles injected not the number of injections administered. • Question 11 4 out of 4 points A 22 year-old female has a retained Kirschner wire in the left little finger. Using local anesthesia, the left upper extremity was thoroughly cleansed with Betadine. The end portion of the little finger was opened with a transverse incision through the subcutaneous tissue to the bone. The retained Kirschner wire was located within the distal phalanx. It was removed and the skin was closed with sutures. What CPT® code is reported? b. 20680-F4 b. 20680-F4 Response Feedback: Rationale: In the CPT® Index look for Removal/Fixation Device. You are referred to 20670-20680. Review the codes to choose the appropriate service. 20680 is the correct code because a deep incision was made all the way to the bone to locate the wire for removal. Modifier F4 is reported to indicate the left little finger. • Question 12 4 out of 4 points A 49 year-old presents with an abscess of the right thumb. The physician incises the abscess and purulent sanguineous fluid is drained. The wound is packed with iodoform packing. What CPT® code is reported? a. 26010-F5 a. 26010-F5 Response Feedback: Rationale: There are specific Incision and Drainage (I&D) procedure codes when performed on a specific anatomical area. In the CPT® Index, look for Finger/Abscess/Incision and Drainage. You are referred to 26010-26011. Review the codes to choose the appropriate service. 26010 is the correct code. Code 26011 includes extensive debridement, multiple incisions or extensive dissection. Insertion of a drain or gauze strip packing to allow continuous drainage does not constitute complicated incision and drainage. • Question 13 4 out of 4 points A 49 year-old female presented with chronic deQuervain’s disease and has been unresponsive to physical therapy, bracing or cortisone injection. She has opted for more definitive treatment. After induction of anesthesia, the patient’s left arm was prepared and draped in the normal sterile fashion. Local anesthetic was injected using a combination 2% lidocaine and 0.25% Marcaine. A transverse incision was made over the central area of the first dorsal compartment. The subcutaneous tissues were gently spread to protect the neural and venous structures. The retractors were placed. The fascial sheath of the first dorsal compartment was then incised and opened carefully. The underlying thumb abductor and extensor tendons were identified. The tissues were dissected and the extensor retinaculum of the first extensor compartment was incised. The fibrotic tissue was incised and the tendons gently released. The tendons were freely moving. Subcutaneous tissues were closed with a 3-0 Vicryl and the skin with 3-0 Prolene subcuticular closure. Steri-strips, Xeroform and dry sterile dressings were applied. What CPT® code is reported? d. 25000-LT d. 25000-LT Response Feedback: Rationale: The report states that the extensor retinaculum of the first extensor compartment was incised. Look in the CPT® Index for Incision/Wrist/Tendon Sheath 25000-25001. Code 25000 shows deQuervain’s disease in the description. Code 25001 refers to the flexor tendon sheath and this involved the extensor tendon making 25000 correct. Note this was an incision, not excision of the tendon of the extensor tendon sheath. Modifier LT is appended to indicate the procedure is performed on the left side. • Question 14 4 out of 4 points A 72 year-old female sustained a left radius fracture, resulting in volar angulation, radial shortening and loss of radioulnar inclination. A general anesthetic was administered. A standard dorsal central approach to the wrist was made. The capsule was opened in a T fashion and the malunion site was identified. A series of osteotomes was utilized to open the fracture site and the normal distal radial architecture was restored. The pie-plate was placed on the distal radius utilizing a combination of 2.0 and 1.8 screws and threaded pins for the distal segment and 2.7 screws proximally. Fragments were secured, and Norian SRS was packed into the defect and allowed to harden. With this completed, the wounds were copiously irrigated with normal saline. Soft tissue was closed over the plate and distal radius, and secured with 2-0 Vicryl. What CPT® code is reported? d. 25400-LT d. 25400-LT Response Feedback: Rationale: This is not the repair of a fracture; it is repair of a malunion. In the CPT® Index look for Repair/Radius/Malunion or Nonunion, 25400, 25405, 25415, 25420. Code 25400 reports repair of a malunion of the radius. There is no mention of an autograft; therefore, 25405 is incorrect. Norian SRS is a biocompatible bone gap filler, not a graft. Modifier LT is appended to indicate the procedure is performed on the left side. • Question 15 0 out of 4 points The patient fell and fractured his left femoral shaft in three places. The fracture is treated with an ORIF of the left femur with an intramedullary nail and interlocking screws (peritrochanterically). The orthopedist also places the leg in a plaster splint prior to leaving the OR. What CPT® code(s) is/are reported? b. 27507, 29505 a. 27506 Response Feedback: Rationale: Documentation shows the patient had a fracture of his left femoral shaft. The fracture was repaired with open reduction and internal fixation (ORIF) using an intramedullary nail and interlocking screws. Selection of codes depends on the fracture site and the method of treatment (closed, open, or percutaneous). The range of codes can be found in the CPT® Index by looking for Fracture/Femur/Peritrochanteric/Intramedullary Implant Shaft. Check the numeric section to select the correct code. Code 27245 is not correct, because this was not a peritrochanteric fracture; it is a femoral shaft fracture. The approach is from the peritrochanteric region. The application of the first cast or splint is included in 27506. See the guidelines for Application of Casts and Strapping in the CPT® codebook. • Question 16 0 out of 4 points This 56 year-old female presented with a degenerative posteromedial meniscal flap tear of the right knee. After appropriate preoperative evaluation, the patient was taken to the operating room where general anesthesia was instituted. The patient was placed supine on the operating table. The right lower extremity was sterilely prepped and draped for arthroscopic surgery. The leg was exsanguinated and the tourniquet inflated. The arthroscope was introduced first through the anterolateral portal with medial suprapatellar portal utilized. The lateral compartment looked fairly good. There were some minimal medial degenerative changes. In the medial compartment there was a full-thickness area of osteochondral degeneration with a flap of cartilage noted. It was possible to remove this with a bleeding bony bed with beveled edges of cartilage. The ligament itself was intact. The retropatellar area was normal with Grade I chondromalacia changes noted. The medial joint was inspected and there was a tear at the junction of the middle and posterior portions of the meniscus, a flap tear was based more anteriorly. This was shaved with a combination of small baskets and punches, and the meniscus debrided back to a smooth stable rim. There was additional synovitis in the medial aspect of the intercondylar notch and this was removed with the curved automated meniscal incisor. What CPT® code(s) should be reported? b. 29880, 29879-51 d. 29881 Response Feedback: Rationale: This was a surgical arthroscopy of the knee. In the CPT® Index look for Arthroscopy/Surgical/Knee, directing you to 29866-29868, 29871-29889. The medial meniscectomy and debridement are reported with 29881. In this case the synovectomy, code 29875, is a separate procedure and bundled with 29881; it is not reported separately. • Question 17 4 out of 4 points A 22 year-old female sustained a dislocation of the right elbow with a medial epicondyle fracture while on vacation. The patient was given general anesthesia and the elbow was reduced and was stable. The medial epicondyle was held in the appropriate position and was reduced in acceptable position and elevated. A long arm splint was applied. The patient is referred to an orthopedist when she returns to her home state in a few days. What CPT® code(s) are reported? b. 24565-54-RT, 24605-54-51-RT b. 24565-54-RT, 24605-54-51-RT Response Feedback: Rationale: In the CPT® Index look for Fracture/Humerus/Epicondyle/Closed Treatment. You are referred to code 24560-24565. Review the codes to choose the appropriate service. 24565 is the correct code to report the alignment of an epicondyle fracture with manipulation (reduced) without a surgical incision. In the CPT® Index, look for Dislocation/Elbow/Closed Treatment. You are referred to 24600, 24605. Review the codes to choose appropriate service. 24605 is the correct code because the patient was given general anesthesia for the procedure. Modifier 54 is appended to report the physician performed the surgical portion only. The patient is referred to an orthopedist for follow up or postoperative care. Modifier 51 is needed to report multiple procedures were performed. Append modifier RT to indicate the procedure is performed on the right side. • Question 18 0 out of 4 points A patient is seen in the hospital’s outpatient surgical area with a diagnosis of a displaced fracture of the lateral condyle, right elbow. An ORIF (open reduction) procedure was performed and included the following techniques: An incision was made in the area of the lateral epicondyle. This was carried through subcutaneous tissue, and the fracture site was easily exposed. Inspection revealed the fragment to be rotated in two places about 90 degrees. It was possible to manually reduce this quite easily, and the manipulation resulted in an almost anatomic reduction. This was fixed with two pins driven across the humerus. The pins were cut off below skin level. The wound was closed with plain catgut subcutaneously and 5-0 nylon for the skin. Dressings and a long arm cast were applied. What CPT® and ICD-10-CM codes are reported? c. 24579-RT, 29065-51-RT, S42.434B b. 24579-RT, S42.451A Response Feedback: Rationale: In the CPT® Index look for Fracture/Humerus/Condyle/Open Treatment which refers to 24579. The manipulation and internal fixation is included in 24579. The application of the first cast is always bundled with the initial surgical service and not reported separately. In the ICD-10-CM Alphabetic Index look for Fracture, traumatic/humerus/lower end/condyle/lateral (displaced) referring you to S42.45-. In the Tabular List seven characters are required to report the code. The 6thcharacter is specific to left or right. Documentation supports this as the right elbow, and the 7th character A is supported as this is the initial surgical procedure. The complete code is S42.451A. This is the open treatment of a closed fracture, so the 7th character B is not reported. • Question 19 0 out of 4 points The patient has a torn medial meniscus. An arthroscope was placed through the anterolateral portal for the diagnostic procedure. The patellofemoral joint showed grade 2 chondromalacia on the patellar side of the joint only, this was debrided with a 4.0-mm shaver. The medial compartment was also entered and a complex posterior horn tear of the medial meniscus was noted. It was probed to define its borders. A meniscectomy was carried out to a stable rim. What CPT® code(s) is/are reported? b. 29880 c. 29881 Response Feedback: Rationale: In the CPT® Index look for Arthroscopy/Surgical/Knee. You are referred to 29866-29868, 29871-29889. Review the codes to choose appropriate service. 29881 is the correct code because the tear was in the medial meniscus. A meniscectomy as well as debridement with a shaver (or chondroplasty) were performed. 29877 is not reported as this is included in 29881. 29880 is not appropriate because a meniscectomy was not performed in both the medial and lateral compartments. The surgery started out as a diagnostic procedure, but changed when the physician decided to perform surgical procedures on the knee. • Question 20 4 out of 4 points This patient presented with internal derangement of the left knee. After satisfactory anesthesia was administered for the arthroscopic procedure, the left lower extremity was prepped and draped in a sterile fashion. Routine portals were made in the knee. We first looked at the medial compartment which showed a complex small tear of the posterior horn of the medial meniscus. This was debrided using a 4.0 meniscal shaver. There was an area of grade 4 chondromalacia on the proximal medial distal femur and this was all the way down to bone. There was also evidence of chondromalacia over the patellofemoral joint of grade 4. This area was drilled with a 0.45 K-wire. Multiple drill holes were placed in an attempt to get some scar tissue to form. The notch area was normal and lateral compartment normal. Following microfracture technique, the knee was irrigated, each portal was closed with 4-0 nylon and the patient was taken to recovery. What CPT® codes are reported? c. 29879-LT, 29881-51-LT c. 29879-LT, 29881-51-LT Response Feedback: Rationale: The procedure was a surgical arthroscopy of the knee reported with codes in the range of 29871-29889. In the CPT® Index look for Arthroscopy/Surgical/Knee directing you to 29866-29868, 29871-29889. The microfracture performed in the patellofemoral joint is reported with 29879. This code is found in the same code range as indicated above. The medial meniscectomy is reported with 29881. The microfracture procedure is more complex than the meniscectomy and it is listed first. Modifier 51 is required for the meniscectomy to indicate multiple procedures. Modifier LT is appended to indicate the procedures were performed on the left side. • Question 21 4 out of 4 points A 47 year-old patient was previously treated with external fixation for a Type IIIA left lateral condyle tibial fracture. There is now nonunion of the left proximal tibia, and he is admitted for open reduction of tibia with bone grafting. Approximately 30 grams of cancellous bone was harvested from the iliac crest. The fracture site was exposed and the area of nonunion was osteotomized, cleaned and repositioned. Intrafragmentary compression was applied with three screws. The harvested bone graft was packed into the fracture site. What CPT® and ICD-10-CM codes are reported? b. 27724-LT, S82.122N b. 27724-LT, S82.122N Response Feedback: Rationale: This is the repair of a nonunion of a tibial fracture. In the CPT® Index look for Nonunion Repair/Tibia, 27720, 27722, 27724, 27725. The correct code is 27724 for the repair of nonunion or malunion of the tibia; with iliac or other autograft (includes obtaining graft). Modifier LT is appended to indicate the procedure was performed on the left side. This was nonunion of a fracture of the tibia. In the ICD-10-CM Alphabetic Index, look for Fracture, traumatic/tibia/upper end/lateral condyle (displaced) referring you to S82.12-. The notes do not indicate displacement; however, the parentheses mean that displacement may or may not be noted in the documentation. In this case a type IIIA fracture is an open fracture. In the Tabular List the code is completed with seven characters. The 6th character 2 indicates laterality (left). The 7th character for fractures is used to identify the episode of care and the healing process. Documentation indicates a nonunion of Type IIIA fracture, and the appropriate 7th character is N subsequent encounter for open fracture Type IIIA, IIIB, IIIC with nonunion. The complete code is S82.122N. • Question 22 4 out of 4 points An elderly female presented with increasing pain in her left dorsal foot. The patient was brought to the operating room and placed under general anesthesia. A curvilinear incision was centered over the lesion itself. Soft tissue dissection was carried through to the ganglion. The ganglion was clearly identified as a gelatinous material. It was excised directly off the bone and sent to pathology. There was noted to be a large bony spur at the level of the head of the 1st metatarsal. Using a double action rongeur, the spur itself was removed and sequestrectomy was performed. A rasp was utilized to smooth the bone surface. The eburnated bony surface was then covered utilizing bone wax. The wound was irrigated and closed in layers. What CPT® codes are reported? a. 28122-LT, 28090-51-LT a. 28122-LT, 28090-51-LT Response Feedback: Rationale: Look in the CPT® Index for Excision/Metatarsal/Head, and you are referred to 28110-28114, 28122, 28140, 28288. Code 28122 reports a partial excision or sequestrectomy of metatarsal bone. Next in the CPT® Index look for Lesion/Foot/Excision referring you to 28080, 28090. Code 28090 reports the excision of the ganglion of the foot. Modifier 51 is appended to indicate multiple procedures performed during the same session. Modifier LT is appended to indicate the procedure is performed on the left side. • Question 23 4 out of 4 points The patient is a 17 year-old male who was struck on the elbow by another player’s stick while playing hockey. He is found to have a fracture of the olecranon process. The patient was brought to the OR, anesthetized and intubated. The right upper extremity was prepped with Betadine scrub and draped free in the usual sterile orthopedic manner. The arm was then elevated and exsanguinated and the tourniquet inflated to 250 mm/Hg. A five-inch incision was made with the scalpel on the extensor side of the elbow, beginning distally and proceeding in an oblique fashion up the proximal forearm. Dissection was carried through subcutaneous tissue and fascia, and bleeding was controlled with electrocautery. We then subperiosteally exposed the proximal ulna and olecranon to visualize the fracture site. The fracture could be seen at the base of the olecranon process. We irrigated the site thoroughly and reduced the fracture fragments without difficulty. Extending the elbow, we inserted two smooth K-wires across the fracture site. Through a drill hole in the proximal ulnar shaft, we threaded an 18-gauge wire through it and wrapped it around the K-wires in a figure-of-eight manner to further stabilize the fixation. Wires were then twisted and placed into soft tissues. The K-wires in the olecranon were advanced slightly after being bent and cut. Sterile dressing was applied and the patient was placed in a splint. What CPT® code is reported? b. 24685-RT b. 24685-RT Response Feedback: Rationale: This is a fracture of the olecranon process which is located at the upper end of the ulna. An incision was made to expose the fracture site, making it an open treatment. Look in the CPT® Index for Fracture/Ulna/Olecranon/Open Treatment 24685. Modifier RT is appended to indicate the procedure was performed on the right side. • Question 24 4 out of 4 points A 3 year-old is brought into the ED crying. He cannot bend his left arm after his older brother twisted it. The physician performs an X-ray to diagnose the patient has a dislocated nursemaid elbow. The ED physician reduces the elbow successfully. The patient is able to move his arm again. The patient is referred to an orthopedist for follow-up care. What CPT® and ICD-10-CM codes are reported? c. 24640-54-LT, S53.032A, W50.2XXA c. 24640-54-LT, S53.032A, W50.2XXA Response Feedback: Rationale: In the CPT® Index, look for Elbow/Dislocation/Nursemaid Elbow. You are referred to 24640. Review the code for appropriate service. 24640 is the correct code to report treatment of a dislocated nursemaids elbow with manipulation. Modifier 54 is appended to report that the ED physician performed only the surgical portion of the service. The patient is referred to an orthopedist for follow-up care. Modifier LT is appended to indicate the procedure was performed on the left side. In the ICD-10-CM Alphabetic Index, look for Nursemaid’s elbow. You are referred to S53.03-. Reviewing the subcategory code in the Tabular List, the 6th character indicates the selection is based on left or right. Documentation supports this as the left arm. A 7th character is also required to indicate the episode of care. Because the patient is in the ED, this supports initial encounter and A is used. The complete code is S53.032A. In the ICD-10-CM External Cause of Injuries Index look for Twisted by person(s) (accidentally) referring you to W50.2. In the Tabular List this code requires a 7th character in which the character A is used and X will be used as a placeholder for the 5th and 6th character positions. The place of occurrence and status is not given; therefore, it is not reported. • Question 25 4 out of 4 points A 45 year-old presents to the operating room with a right index trigger finger and left shoulder bursitis. The left shoulder was injected with 1 cc of Xylocaine, 1 cc of Celestone and 1 cc of Marcaine. An approximately 1-inch incision was made over the A1 pulley in the distal transverse palmar crease. This incision was taken through skin and subcutaneous tissue. The A1 pulley was identified and released in its entirety. The wound was irrigated with antibiotic saline solution. The subcutaneous tissue was injected with Marcaine without epinephrine. The skin was closed with 4-0 Ethilon suture. Clean dressing was applied. What CPT® codes are reported? c. 26055-F6, 20610-51-LT c. 26055-F6, 20610-51-LT Response Feedback: Rationale: In the CPT® Index look for Trigger Finger Repair. You are referred to 26055. Review the code to verify accuracy. In the CPT® Index look for Injection/Joint. You are referred to 20600, 20604-20606, 20610, 20611. Review the codes to choose appropriate service. 20610 is the correct code for the shoulder injection. Modifier F6 is used to report the right index finger that was repaired. Modifier LT is used to indicate the left shoulder joint. Modifier 51 is used to indicate multiple procedures were performed. Sunday, November 19, 2017 9:13:35 AM MST • Question 1 10 out of 10 points Where does the exchange of oxygen and carbon dioxide take place within the lungs? c. Alveoli c. Alveoli Response Feedback: Rationale: The alveoli or air sacs are where the exchange of oxygen from the lungs and carbon dioxide from the capillaries of the circulatory system take place. High partial pressure of oxygen in the alveoli diffuses into the low partial pressure of oxygen in the capillaries and high partial pressure of carbon dioxide in the capillaries diffuses to the low partial pressure of carbon dioxide in the alveoli. • Question 2 10 out of 10 points What is also referred to as the “Windpipe?” c. Trachea c. Trachea Response Feedback: Rationale: The trachea carries air from the mouth and throat down to the lungs and is often referred to as the windpipe. • Question 3 10 out of 10 points What is the ICD-10-CM code for acquired lymphedema? b. I89.0 b. I89.0 Response Feedback: Rationale: Acquired lymphedema typically occurs after major surgery or cancer treatment such as radiation therapy. It is more common than con-genital lymphedema. Look in the ICD-10-CM Alphabetic Index for Lymphedema (acquired) (see also Elephantiasis) Locate Elephantiasis (nonfilarial) referring you to I89.0. • Question 4 10 out of 10 points What is the ICD-10-CM code for primary malignant thymoma? a. C37 a. C37 Response Feedback: Rationale: Primary malignancy of the thymus is coded with C37. Look in the ICD-10-CM Alphabetic Index for Thymoma/malignant. • Question 5 10 out of 10 points What is the ICD-10-CM code for a child with an acute exacerbation of hay fever asthma? b. J45.901 b. J45.901 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Asthma/with/Hay Fever which points to see Asthma, allergic extrinsic. Locate Asthma/allergic extrinsic/with/exacerbation (acute) referring you to J45.901. In ICD-10-CM asthma codes are specific to severity - mild, moderate, severe as well as intermittent or persistent. In this case the indexing leads to an unspecified code. • Question 6 0 out of 10 points Which CPT® code(s) describes VATS therapeutic wedge resection of the left upper lobe followed by left upper lobectomy? c. 32663, 32666 d. 32663 Response Feedback: Rationale: CPT® subsection guidelines for Lungs and Pleura indicate therapeutic wedge resection is bundled into the lobectomy when it is the same lobe. The wedge resection can only be coded separately if it was performed on a different lobe or contralateral lung. • Question 7 10 out of 10 points An indirect endoscopic procedure of the larynx means the larynx is viewed: b. With mirrors b. With mirrors Response Feedback: Rationale: Indirect endoscope of the larynx is performed by viewing the larynx with the use of mirrors. A direct laryngoscopy is the use of an endoscope to look directly at the larynx. • Question 8 0 out of 10 points Can bronchoscopy codes be coded together by a physician, and if yes, how? Are multiple procedures reported with modifier 51? d. Yes: Report multiple bronchoscopy codes together because no modifier is required b. Yes: Report multiple procedures with modifier 51 (if required by the payer) Response Feedback: Rationale: Yes, bronchoscopy codes are billed as multiple procedures with a modifier 51. List the highest RVU valued code first and then all other codes with a modifier 51. • Question 9 10 out of 10 points A patient has a mass in her left axilla that is a suspected recurrence of lymphoma. She has a left axillary node excisional biopsy. The lymph node biopsied is under the pectoralis minor. What CPT® code is reported? d. 38525 d. 38525 Response Feedback: Rationale: The patient has an excisional biopsy of the left axillary node. Because the lymph node biopsied is under the pectoralis minor muscle, it is considered a deep lymph node. Look in the CPT® Index for Biopsy/Lymph Nodes/Open and you are directed to 38500, 38510-38530. 38525 is for biopsy of the deep axillary nodes. • Question 10 10 out of 10 points Can a diagnostic thoracoscopy be billed with a surgical thoracoscopy (VATS) under certain circumstances? a. No: A diagnostic thoracoscopy is always included in the surgical VATS. a. No: A diagnostic thoracoscopy is always included in the surgical VATS. Response Feedback: Rationale: Diagnostic thoracoscopy is bundled into surgical VATS and cannot be billed separately during the same surgical session, per CPT® instruction. In contrast, if the results of a diagnostic thoracoscopy prompts an open procedure to excise tissue, the diagnostic VATS may be billed, and the appropriate open surgical code may be reported with modifier 58 Staged Procedure; some payers may require a modifier 59 in this situation; check with your payers for appropriate modifier usage. Sunday, November 19, 2017 9:14:09 AM MST • Question 1 4 out of 4 points What ICD-10-CM code is reported for spontaneous pneumothorax? c. J93.83 c. J93.83 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Pneumothorax/spontaneous NOS which directs you to code J93.83. Verify code selection in the Tabular List. • Question 2 4 out of 4 points What CPT® code is reported for open decortication and parietal pleurectomy? b. 32320 b. 32320 Response Feedback: Rationale: In the CPT® Index look for Decortication/Lung/with Parietal Pleurectomy. This directs you to code 32320. • Question 3 4 out of 4 points What is the largest single mass of lymphatic tissue? a. Spleen a. Spleen Response Feedback: Rationale: The spleen is the largest single mass of lymphatic tissue. • Question 4 4 out of 4 points What ICD-10-CM code is reported for a patient that has RSV (respiratory syncytial virus) pneumonia? d. J12.1 d. J12.1 Response Feedback: Rationale: RSV stands for respiratory syncytial virus. In the ICD-10-CM Alphabetic Index look for Pneumonia/respiratory syncytial virus which directs you to code J12.1. Verify code selection in the Tabular List. • Question 5 4 out of 4 points What is the name of the structure made of bone and cartilage separating the nostrils? a. Nasal septum a. Nasal septum Response Feedback: Rationale: A septum is a partition. The nasal septum separates the nostrils. • Question 6 4 out of 4 points Where in the respiratory system is the carina located? c. Tracheal bifurcation c. Tracheal bifurcation Response Feedback: Rationale: The carina is located at the tracheal bifurcation. The tracheal bifurcation is the opening of the bronchi as it splits into left and right sides. • Question 7 4 out of 4 points A patient presents with wheezing and shortness of breath. After evaluating the patient, the provider determines the patient is suffering from an exacerbation of his asthma. The provider orders nebulizer treatments to be administered in his office. According to the ICD-10-CM guidelines for coding signs and symptoms, what is/are the correct ICD-10-CM code(s)? a. J45.901 a. J45.901 Response Feedback: Rationale: Because the type of asthma is not indicated, the correct code is J45.901. In the ICD-10-CM Alphabetic Index look for Asthma, asthmatic/with/exacerbation (acute) directing you to J45.901. The Tabular List verifies this code choice. Wheezing and shortness of breath are signs and symptoms of an exacerbation of asthma and not reported separately. According to the Official ICD-10-CM guideline I.B.4, do not report signs and symptoms when a definitive diagnosis has been established. • Question 8 0 out of 4 points A 43 year-old female is seen in the emergency room with severe epistaxis. She said this is a common occurrence for her during the cold dry months of winter and this is why she is here for the third time this week. Extensive bilateral posterior cautery and packing is again required to control the hemorrhage. What CPT® code is reported for the procedure? (Note: Do not code the E/M) b. 30905-50 d. 30906-50 Response Feedback: Rationale: Epistaxis is the term for nasal hemorrhage. In the CPT® Index look for Packing/ Nasal Hemorrhage and you are directed to code range 30901-30906. Code selection is determined by whether the procedure is posterior or anterior. This is posterior and is subsequent making the correct code 30906. Modifier 50 indicates this was done bilaterally. • Question 9 4 out of 4 points A 20 year-old patient is seen for 5 transbronchial lung biopsies of 2 separate lobes. One biopsy is taken in one lobe and 4 biopsies in another lobe. What CPT® code(s) is/are reported? d. 31628, 31632 d. 31628, 31632 Response Feedback: Rationale: Transbronchial biopsies are performed via a bronchoscopy. In the CPT® Index look for Bronchoscopy/Biopsy and we are directed to codes 31625-31629, 31632, 31633. Code 31628 represents a transbronchial biopsy of one lobe. A parenthetical statement under this code indicates to use code 31632 for any additional transbronchial biopsies on additional lobes. Code 31632 is reported once even when multiple biopsies are taken in a lobe. • Question 10 4 out of 4 points A surgeon performed a transthoracic median sternotomy for exploration of the space around the lung sacs and for drainage of fluid, caused by pneumonia. What is/are the appropriate code(s) for this scenario? b. 39010 b. 39010 Response Feedback: Rationale: In the CPT® Index look for Mediastinum/Exploration which directs us to codes 39000-39010, 60505. Code selection is made based on the approach used. In this case, it is a transthoracic approach making 39010 the correct code. Drainage of fluid is already included in the code and is not separately reportable. • Question 11 0 out of 4 points Most nasal passages have how many turbinates present on the lateral wall of each nasal cavity? c. 2 d. 3 Response Feedback: Rationale: There are three turbinates on each side of the nose: superior, middle and inferior. These turbinates may become swollen and require surgery to restore airflow. • Question 12 4 out of 4 points A patient is seen in the endoscopy suite for a diagnostic maxillary sinusotomy. During the sinusotomy, the provider observes some diseased tissue which needs to be removed. The provider decides to perform a maxillary antrostomy with tissue removal. Bleeding is controlled. The patient tolerated the procedure well. What CPT® code(s) is/are reported? d. 31267 d. 31267 Response Feedback: Rationale: According to the CPT® guidelines for coding of endoscopies, a surgical sinus endoscopy includes a sinusotomy and diagnostic endoscopy. In the CPT® Index look for Sinus/Sinuses/ Maxillary/Antrostomy and you are directed to code range 31256-31267. We see code 31267 represents a surgical maxillary antrostomy with maxillary tissue removal. • Question 13 4 out of 4 points A patient with AML (Acute Myelogenous Leukemia) has just learned his sister is an HLA (Human Leukocyte Antigen) match for him. Stem cells taken from the donor (the patient’s sister) will be transplanted into the patient to help with his treatment. What CPT® code is used to report the harvesting of the stem cells from the donor (his sister)? c. 38205 c. 38205 Response Feedback: Rationale: In the CPT® Index look for Stem Cell/Harvesting. This directs you to code range 38205, 38206. Code selection is based on whether it is allogenic (from a donor) or autologous (from the patient). This is allogenic making 38205 the correct code choice. • Question 14 0 out of 4 points A 55 year-old patient has history of lung cancer of the right lower lobe. He is complaining of difficulty breathing and mild chest pain. Patient is scheduled for a diagnostic VATS (Video-assisted thoracoscopic surgery). Under general anesthesia he was placed in left lateral decubitus position and a thoracoscope was inserted through a port site. The VATS exploration immediately revealed a mass of the left upper lobe. A biopsy was performed and sent to pathology. Results from pathology revealed small cell carcinoma. Decision was made to remove the upper lobe of his left lung by performing an open procedure. The thoracoscope is withdrawn and the surgeon opens the chest cavity and rib spreaders are inserted to separate the ribs to gain access to the lung. The upper lobe of the left lung is identified, isolated and removed. The instruments are removed and the chest incision is closed in layers. What CPT® codes are reported? c. 32663 d. 32480-58, 32608-51 Response Feedback: Rationale: The patient presented for a diagnostic VATS and a biopsy was performed. Look in the CPT® Index for Thoracoscopy/Diagnostic/with Biopsy 32604, 32606, 32607-32609. Code 32608 reports thoracoscopy with diagnostic biopsy of a lung mass. The biopsy was positive for cancer which prompted the surgeon to perform a thoracotomy to remove the upper lobe of the left lung. Look in the CPT® Index for Lung/Excision/Lobe 32480-32482. Code 32480 describes the removal of a single lobe. Report modifier 58 with 32480 to show the lobectomy was performed by a thoracotomy as a staged procedure. Some payers may require modifier 59 on 32480. Check with your payer. • Question 15 4 out of 4 points An 18 month-old patient is seen in the ED unable to breathe due to a toy he swallowed which had lodged in his throat. Soon brain death will occur if an airway is not established immediately. The ED provider performs an emergency transtracheal tracheostomy. What CPT® and ICD-10-CM codes are reported? c. 31603, T17.290A c. 31603, T17.290A Response Feedback: Rationale: In the CPT® Index look for Tracheostomy/Emergency and you are directed to code range 31603-31605. Code selection is based on the approach. In this case, the approach is transtracheal making 31603 the correct code choice. Because the toy is a foreign body that was lodged in his throat, in the ICD-10-CM Alphabetic Index look for Foreign Body/pharynx/causing/asphyxiation/specified type NEC and you are directed to T17.290. The foreign body was causing an obstruction or suffocation in the respiratory tract. Verification in the Tabular List indicates that the code requires seven characters. 7th character A, initial encounter, is the correct choice because this is an emergency department encounter. • Question 16 4 out of 4 points A 3 year-old girl is playing with a marble and sticks it in her nose. Her mother is unable to dislodge the marble so she takes her to the provider’s office. The provider removes the marble with hemostats. What CPT® and ICD-10-CM codes are reported? b. 30300, T17.1XXA b. 30300, T17.1XXA Response Feedback: Rationale: Since the marble is a foreign body look in the CPT® Index for Removal/Foreign Body/Nose. Here you are directed to use code 30300. For the ICD-10-CM code look in the ICD-10-CM Alphabetic Index for Foreign Body/entering through orifice/nose (passage) or nostril. This directs us to code T17.1. Verification in the Tabular List indicates the code requires seven characters. The 5th and 6th characters would require a placeholder X and the 7th character A for initial encounter. • Question 17 4 out of 4 points A patient with laryngeal spasms undergoes therapeutic injection of the vocal cords. Topical anesthesia is administered to the oral cavity, pharynx and larynx. Using an operating microscope, a direct laryngoscope is inserted into the patient’s mouth. The interior larynx is examined and the surgeon injects the vocal cords at two sites with glycerin. What CPT® and ICD-10-CM codes are reported? b. 31571, J38.5 b. 31571, J38.5 Response Feedback: Rationale: In the CPT® Index look for Laryngoscopy/Direct directing you to 31515-31571. 31571 is appropriate for the injection into the vocal cords using an operating microscope. There is a parenthetical instruction note that states, “Do not report code 69990 in addition to code 31571”. In the ICD-10-CM Alphabetic Index look for Spasm(s), spastic, spasticity/larynx, laryngeal which directs you to code J38.5. Verify code selection in the Tabular List. • Question 18 0 out of 4 points A 55 year-old female smoker presents with cough, hemoptysis, slurred speech and weight loss. Chest X-ray done today demonstrates a large, unresectable right upper lobe mass, and brain scan is suspicious for metastasis. Under fluoroscopic guidance in an outpatient facility, a percutaneous needle biopsy of the right lung lesion is performed for histopathology and tumor markers. A diagnosis of small cell carcinoma is made and chemoradiotherapy is planned. What CPT® and ICD-10-CM codes are reported? d. 32400-RT, 77002-26, C34.90 a. 32405-RT, 77002-26, C34.11 Response Feedback: Rationale: In the CPT® Index look for Biopsy/Lung/Needle. This directs you to code 32405. Code 77002 is the appropriate code for the fluoroscopic guidance as indicated by the parenthetical statement under code 32405 and by reviewing the code descriptor for 77002. Modifier 26 is appended to report the professional component. RT modifier is to indicate the right lung was where the biopsy was performed. We have a diagnosis of small cell carcinoma of the right lung which is code C34.11. In the ICD-10-CM Alphabetic Index look for Carcinoma which states see also Neoplasm, malignant, by site. Look in the Table of Neoplasms for Neoplasm, neoplastic/lung/upper lobe and select from the Malignant Primary column directing you to C34.1-. Verification in the Tabular List requires a 5th character to indicate laterality. Report C34.11 to indicate the right lung. The signs and symptoms are not coded because we do have a definitive diagnosis (ICD-10-CM guideline I.B.4). Brain metastasis is suspected but not confirmed so it would not be reported. The chemotherapy is planned but not performed so it would not be reported either. • Question 19 4 out of 4 points A 14 year-old boy presents at the Emergency Department experiencing an uncontrolled epistaxis. Through the nares, the ED provider packs his entire nose via an anterior approach with extensive packing of medicated gauze. In approximately 15 minutes the nosebleed stops. What CPT® and ICD-10-CM codes are reported? c. 30903-50, R04.0 c. 30903-50, R04.0 Response Feedback: Rationale: Epistaxis is the term for nasal hemorrhage. In the CPT® Index look for Packing/Nasal Hemorrhage which directs you to code range 30901-30906. 30903 represents anterior packing for an uncontrolled or extensive nasal hemorrhage. Modifier 50 indicates this was done in both nares (bilaterally). In the ICD-10-CM Alphabetic Index look for Epistaxis referring you to code R04.0. Verification in the Tabular List confirms code selection. • Question 20 4 out of 4 points A patient underwent bilateral nasal/sinus diagnostic endoscopy. Finding the airway obstructed the provider fractures the middle turbinates to perform the surgical endoscopy with total bilateral ethmoidectomy and nasal septoplasty. What CPT® codes are reported? d. 30520, 31255-50-51 d. 30520, 31255-50-51 Response Feedback: Rationale: According to the CPT® guidelines for coding of endoscopies, a surgical sinus endoscopy includes a sinusotomy and diagnostic endoscopy. In the CPT® Index look for Ethmoidectomy/Endoscopic directing you to 31254, 31255. Code 31255 represents a total ethmoidectomy. In the CPT® Index look for Septoplasty which directs you to code 30520. The fracturing of the turbinates is inclusive to the procedures and not reported separately because the provider is fracturing the turbinates to perform the endoscopy. Modifier 50 indicates the ethmoidectomy was performed bilaterally and modifier 51 is reported with code 31255 to indicate multiple procedures performed at same session, for maximum reimbursement. • Question 21 4 out of 4 points A patient presents to the emergency department (ED) with a sucking chest wound. The ED provider on duty performs an immediate tube thoracostomy in order to restore normal breathing to the patient before rushing him to surgery for another provider to address other injuries. What CPT® code is reported by the ED provider? a. 32551 a. 32551 Response Feedback: Rationale: In the CPT® Index look for Thoracostomy/Tube which directs you code 32551. The ED provider would not be performing the surgery for other injuries so we would not bundle the tube insertion into any of those procedures. • Question 22 4 out of 4 points A returning 2 year-old child is seen in the pediatrician’s office with stridor and a bark like cough. The pediatrician examines the child quickly and determines the child has stridulous croup. The child is given a nebulizer breathing treatment in the office to improve PO2 levels. Medication used is breathable Epinephrine. What CPT® and ICD-10-CM codes are reported? c. 94640, J38.5 c. 94640, J38.5 Response Feedback: Rationale: To code the nebulizer treatment look in the CPT® index for Inhalation Treatment/for Airway Obstruction Pressurized or Nonpressurized directing you to code 94640. This code accurately represents a nebulizer treatment. A definitive diagnosis of stridulous croup is given and the signs and symptoms the child presented with is not coded (ICD-10-CM guideline I.B.4). In the ICD-10-CM Alphabetic Index look for Croup/stridulous directing you to J38.5. Verification in the Tabular List confirms code selection. • Question 23 4 out of 4 points A 20 year-old female who returned from spring break in Mexico six days ago, presents to the ED with a high fever for three days, a sore throat, general aches and a miserable cough. The ED provider suspects flu and orders a rapid flu test. What ICD-10-CM code(s) is reported? d. R50.9, J02.9, R52, R05 d. R50.9, J02.9, R52, R05 Response Feedback: Rationale: According to the ICD-10-CM guideline I.B.4, signs and symptoms are reported when a related definitive diagnosis has not been established. The flu was suspected but not established therefore we code the patient's presenting symptoms. In the ICD-1-CM Alphabetic Index look for Fever directing you to R50.9. She also has a sore throat, look for Pharyngitis directing you to code J02.9. For the general aches look for Pain(s) directing you to R52. Look for Cough directing you to R05. Verify code selection in the Tabular List. • Question 24 0 out of 4 points A 55 year-old patient has history of lung cancer of the right lower lobe. He is complaining of difficulty breathing and mild chest pain. Patient is scheduled for a diagnostic VATS (Video-assisted thoracoscopic surgery). Under general anesthesia he was placed in left lateral decubitus position and a thoracoscope was inserted through a port site. The VATS exploration immediately revealed a mass of the left upper lobe. A biopsy was performed and sent to pathology. Results from pathology revealed small cell carcinoma. Decision was made to remove the upper lobe of his left lung by performing an open procedure. The thoracoscope is withdrawn and the surgeon opens the chest cavity and rib spreaders are inserted to separate the ribs to gain access to the lung. The upper lobe of the left lung is identified, isolated and removed. The instruments are removed and the chest incision is closed in layers. What CPT® codes are reported? d. 32663 a. 32480-58, 32608-51 Response Feedback: Rationale: The patient presented for a diagnostic VATS and a biopsy was performed. Look in the CPT® Index for Thoracoscopy/Diagnostic/with Biopsy 32604, 32606, 32607-32609. Code 32608 reports thoracoscopy with diagnostic biopsy of a lung mass. The biopsy was positive for cancer which prompted the surgeon to perform a thoracotomy to remove the upper lobe of the left lung. Look in the CPT® Index for Lung/Excision/Lobe 32480-32482. Code 32480 describes the removal of a single lobe. Report modifier 58 with 32480 to show the lobectomy was performed by a thoracotomy as a staged procedure. Some payers may require modifier 59 on 32480. Check with your payer. • Question 25 0 out of 4 points How are multiple moderate lacerations of the spleen, initial encounter coded in ICD-10-CM? d. S36.031A b. S36.032A Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Laceration/spleen/moderate which directs the coder to S36.031. In the Tabular List code S36.032 has an inclusion for multiple moderate lacerations of spleen. This code requires a 7th character of A, D, or S. Sunday, November 19, 2017 9:14:28 AM MST • Question 1 10 out of 10 points Which valves are the semilunar valves? d. Pulmonary and Aortic d. Pulmonary and Aortic Response Feedback: RATIONALE: The tricuspid and mitral valves are the atrioventricular valves. The pulmonary and aortic valves are the semilunar valves because of their shape. • Question 2 0 out of 10 points What type of circulation refers to the movement of blood through tissues of the heart? b. Systemic d. Coronary Response Feedback: RATIONALE: Coronary circulation refers to the movement of blood through the tissues of the heart. • Question 3 10 out of 10 points A patient is diagnosed with acute on chronic diastolic congestive heart failure (CHF). What is/are the ICD-10-CM code(s) reported? a. I50.33 a. I50.33 Response Feedback: RATIONALE: There is a combination code for acute on chronic diastolic congestive heart failure. Look in the Index to Diseases and Injuries for Failure/heart/diastolic (congestive)/acute/and (on) chronic (congestive. You are referred to I50.33. Always verify your codes in the Tabular List. • Question 4 0 out of 10 points Patient is diagnosed as having renal failure with hypertension. He is end stage receiving dialysis. What ICD-10-CM codes are reported? d. I13.0, N18.6, Z99.2 c. I12.0, N18.6, Z99.2 Response Feedback: RATIONALE: According to the ICD-10-CM guidelines, a relationship is assumed between hypertension and chronic kidney disease. Look for Hyper-tension, hypertensive/ kidney/with/stage 5 chronic kidney disease (CKD) or end stage renal disease (ESRD). You are referred to I12.0. Verify in the Tabular List. An instructional note indicates to use additional code to identify the stage of chronic kidney disease (N18.5, N18.6). Code N18.6 is reported for the end stage renal failure. There is an instructional note to use additional code to identify dialysis status (Z99.2). • Question 5 10 out of 10 points Patient presents for removal and replacement of her permanent dual chamber transvenous pacemaker system (generator and leads). What CPT® codes are reported? c. 33235, 33208-51, 33233-51 c. 33235, 33208-51, 33233-51 Response Feedback: RATIONALE: Multiple codes are needed to show the entire procedure. 33235 is for removing the electrodes, 33208 is for putting in the new system, and 33233 is for removing the pacemaker pulse generator. These codes are all found under Pacemaker, Heart/Insertion 33206-33208, Pacemaker, Heart/Removal/Pulse Generator Only, and Pacemaker, Heart /Removal/Transvenous Electrodes 33234-33235. Modifier 51 reports multiple procedures performed during the same session. • Question 6 10 out of 10 points Patient had mitral valve prolapse, and a mitral valve ring was inserted with cardiopulmonary bypass. What CPT® code is reported? a. 33426 a. 33426 Response Feedback: RATIONALE: The mitral valve was repaired, not replaced. Look in the CPT® Index for Repair/Heart/Mitral Valve 0345T, 33418-33420, 33422, 33425-33427 Code 33426 Valvuloplasty, mitral valve, with cardiopulmonary bypass; with prosthetic ring, is correct. Cardiopulmonary bypass is included in the code description and not coded separately. • Question 7 10 out of 10 points A catheter was advanced into the left and right renal artery, and the SMA (superior mesenteric artery), and imaging was performed in all vessels. What CPT® codes are reported? c. 36252, 36245-59, 75726-26 c. 36252, 36245-59, 75726-26 Response Feedback: RATIONALE: Look in the CPT® Index for Angiography/Renal Artery, you are directed to 36251–36254. Code 36252 includes selective catheter placement (first-order) of the main renal artery and any accessory arteries, including arterial puncture, catheter placement(s), fluoroscopy, con-trast injection(s), image postprocessing, permanent recording of images, and radiological supervision and interpretation, including pressure gradient measurements when performed, and flush aortogram when performed, bilaterally. The selective catheterization code for the SMA is found in the CPT® Index under Artery/Abdomen/Catheterization 36245–36248. The SMA is considered a visceral artery. Look in Appendix L and you will see the SMA is a first order vessel. The radiology code is found in the CPT® Index under Angiography/Abdomen. You are referred to 74174, 74175, 74185, 75635, and 75726. The correct code is 75726. Modifier 26 denotes the professional service. • Question 8 10 out of 10 points A 5 French pigtail catheter was placed in the abdominal aorta and a run-off was performed following injection of 80cc of contrast. Oblique DSA images of the iliac circulation were performed following 2 injections, each 15cc. The catheter was not moved to another position within the aorta for the additional injections. What CPT® codes are reported? a. 36200, 75630-26 a. 36200, 75630-26 Response Feedback: RATIONALE: Nonselective catheter placement in the aorta is reported with 36200, which is found in the CPT® Index under Aorta/Catheterization/Catheter. Contrast was injected from one catheter placement site, and there is a report for the aorta and the extremities, making this an abdominal aortogram with bilateral iliofemoral lower extremity angiography, 75630. This is found in the CPT® Index under Aortography/with Iliofemoral Artery 75630. Modifier 26 is required for the professional service. • Question 9 10 out of 10 points A complete transthoracic echocardiography (TTE) was performed with spectral Doppler and color flow. Report the global service. What CPT® code(s) is/are reported? b. 93306 b. 93306 Response Feedback: RATIONALE: A combination code exists to bundle the Doppler and color flow. Look in the CPT® Index for Echocardiography/Transthoracic 93306–93308, 93350–93352. Code 93306 is correct. • Question 10 10 out of 10 points Left and right heart catheterization, selective coronary angiogram, left ventriculogram, ascending aortogram to access the aortic root, descending aortogram, right iliac angiogram, Perclose closure. Access is from the right femoral artery and right femoral vein. c. 93460-26, 93567 c. 93460-26, 93567 Response Feedback: RATIONALE: Cardiac catheterization code 93460 reports right and left heart catheterization, selective coronary angiography with imaging interpretation and reporting, as well as left ventriculography. The cardiac catheterization code includes injection procedures and radiologic S &I (Supervision & Interpretation). The ascending aortography to review the aortic root is reported with add-on code 93567. Aortography is always included in cardiac catheterizations unless it is performed for a specific purpose, such as to study an aortic aneurysm or occlusive disease. The right iliac angiogram is not reported. It was performed to assess the femoral artery for the Perclose device. The Perclose closure is not reported; it is bundled with the cardiac catheterization procedure. Modifier 26 is required to indicate the professional services only for 93460. The add-on code for the injection service is a professional service; a modifier is not required. In the index, look up Cardiac Catheterization/Combined Left and Right Heart and with Left Ventriculography directing you to the correct codes. Sunday, November 19, 2017 9:15:04 AM MST • Question 1 4 out of 4 points How many layers of tissue does an artery have? c. Three c. Three Response Feedback: Rationale: An artery has three layers: an outer layer of tissue, a muscular middle and an inner layer of epithelial cells. • Question 2 4 out of 4 points ____ is a term standing for enlargement of the heart. c. Cardiomegaly c. Cardiomegaly Response Feedback: Rationale: Cardio = heart, megaly = enlargement • Question 3 4 out of 4 points The conduction system contains pacemaker cells, nodes, the ____ and the ____. c. Purkinje fibers and bundle of His c. Purkinje fibers and bundle of His Response Feedback: Rationale: The conduction system contains pacemaker cells, nodes, the bundle of His and the Purkinje fibers. • Question 4 4 out of 4 points A patient suffering from an abdominal aortic aneurysm involving a renal artery undergoes endovascular repair deploying a fenestrated visceral autograft using two visceral artery endoprostheses. Radiological supervision and interpretation was performed. Select the CPT® code for this procedure. b. 34842 b. 34842 Response Feedback: Rationale: Look in the CPT® Index for Repair/Aorta/Visceral/Endovascular directing you to code 34841-34848. Code 34842 is correct to report because two visceral artery endoprostheses were used. • Question 5 0 out of 4 points Patient presents to her physician 10 weeks following a true posterior wall myocardial infarction. The patient is still symptomatic. What is (are) the correct ICD-10-CM code(s) for this condition? c. I22.8 d. Z51.89, I25.9 Response Feedback: Rationale: Because it is past four weeks since the myocardial infarction and the patient is still symptomatic, ICD-10-CM guideline, I.C.9.e.1, indicates that the appropriate aftercare code is assigned rather than a code from category I21. Look in the ICD-10-CM Alphabetic Index for Aftercare which directs the coder to Z51.89. Verify code selection in the Tabular List. The notes under category Z51 instruct to code also condition requiring care. This patient still has symptoms. Look in the Alphabetic Index for Disease/heart/ischemic (chronic or with a stated duration of over 4 weeks) directing you to I25.9. Verify in the Tabular List. • Question 6 4 out of 4 points A patient in the ED was found to have a ruptured abdominal aortic aneurysm. He was taken to emergency surgery; a physician performed a direct repair. The physician documented that the aneurysm involved the common iliac. Select the proper CPT® code for this procedure. d. 35103 d. 35103 Response Feedback: Rationale: You must read the question carefully because this is a ruptured aortic aneurysm involving the common iliac not a ruptured aneurysm of the common iliac. Look in the CPT® Index for Aneurysm Repair/Abdominal Aorta which directs you to multiple codes. On review of the code ranges, code 35103 is correct. Code 35102 is a repair of an aneurysm not ruptured. • Question 7 0 out of 4 points Aortography and bilateral extremity angiography were performed. The physician placed the catheter in the aorta at the level of the renal arteries and injected contrast for the aortography and repositioned the catheter just above the bifurcation for angiography of the lower extremities. Which CPT® codes are reported? d. 36200, 75716-26 a. 36200, 75625-26, 75716-26 Response Feedback: Rationale: Because the catheter was repositioned, and separate studies were performed, both the aortography and the extremity angiography are reported. Look in the CPT® Index for Catheterization/Aorta which directs you to 36160-36200. In the CPT® Index see Aorta/Aortography and you are referred to 75600-75630. To locate angiography of the lower extremities, look for Angiography/Leg Artery referring you to 73706, 75635, 75710-75716. Modifier 26 reports the professional service. • Question 8 4 out of 4 points A patient presents to the outpatient surgery department for revision to his autogenous radiocephalic fistula so he can continue his hemodialysis. What is the correct CPT® code? d. 36832 d. 36832 Response Feedback: Rationale: The patient is undergoing revision of the arteriovenous (radiocephalic) fistula. Look in the CPT® Index for Arteriovenous Fistula/Revision/without Thrombectomy referring you to code 36832. • Question 9 4 out of 4 points Physician changes the old battery to a new one on a patient’s dual chamber permanent pacemaker. What CPT® code(s) is/are reported? a. 33228 a. 33228 Response Feedback: Rationale: CPT® guidelines state “When the battery of a pacemaker is changed, it is actually the pulse generator that is changed.” It is reported with one code. In the CPT® Index look for Pacemaker, Heart/Replacement/Pulse Generator and you are referred to 33227-33229. Code 33228 is reported for dual chamber (dual lead system). • Question 10 4 out of 4 points Select the ICD-10-CM diagnosis codes used for pseudoaneurysm, cardiac tamponade and left ventricular failure. d. I72.9, I31.4, I50.1 d. I72.9, I31.4, I50.1 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Pseudoaneurysm which directs the user to see Aneurysm. Look for Aneurysm and the subterm pseudoaneurysm is not listed; therefore, the unspecified code I72.9 is correct. In the Alphabetic Index look for Tamponade, heart referring you to I31.4. Next, in the Alphabetic Index look for Failure/ventricular/left which directs you to I50.1. Verify code selection in the Tabular List. • Question 11 0 out of 4 points In the cath lab, from a right femoral artery access, the following procedures are performed: Catheter placed in the left renal, accessory renal superior to the left renal and one main right renal artery. Radiologic supervision and imaging is performed in all locations. What CPT® code(s) is/are reported? b. 36252, 36251 c. 36252 Response Feedback: Rationale: Look in the CPT® Index for Angiography/Renal Artery and you are directed to 36251-36254. This is a bilateral procedure, with an accessory left renal artery. Code 36252 includes bilateral and accessory renal angiography, and radiologic supervision and imaging. • Question 12 0 out of 4 points A patient presents for epicardial lead placement via median sternotomy to the right atrium and right ventricle. A dual pacemaker generator is then inserted subcutaneously. The patient has bundle branch block and sinoatrial node dysfunction. What CPT® and ICD-10-CM codes are reported? d. 33208, 33213-51, I45.4, I49.5 a. 33202, 33213-51, I45.4, I49.5 Response Feedback: Rationale: Because leads were placed on the right atrium and right ventricle, it is a dual chamber system. Two codes are necessary to report placement of an epicardial system. The parenthetical note under 33203 directs the coder to report codes 33202 and 33203 with 33212, 33213, 33221, 33230, 33231, and 33240. Look in the CPT® Index for Pacemaker, Heart/Insertion/Pulse Generator Only. You are referred to 33212, 33213, and 33221. For the placement of the epicardial electrodes look in the CPT® Index for Pacemaker, Heart/Insertion/Electrode, and you are referred to 33202-33203. In the ICD-10-CM Alphabetic Index look for Block, blocked/bundle-branch referring you to code I45.4. Look in the Alphabetic Index for Dysfunction/sinoatrial node referring you to code I49.5. Verify code selection in the Tabular List. • Question 13 4 out of 4 points A patient presents to the hospital for a cardiovascular SPECT study. A single study is performed under stress, but without quantification, with a wall motion study, and ejection fraction. Select the CPT® code(s) for this procedure. a. 78451 a. 78451 Response Feedback: Rationale: Code 78451 indicates a perfusion study either qualitative or quantitative. There is no mention of cardiac blood pooling imaging which eliminates choices a and b. Code 78453 reports a planar study, and this was a SPECT study, thus eliminating c. Look in the CPT® Index for Nuclear Medicine/Diagnostic/Heart/Myocardial Perfusion Imaging which directs you to 78451-78454 or SPECT/Heart/Single which directs you to 78451, 78453. • Question 14 0 out of 4 points A physician states he performed a comprehensive EP study with induction of arrhythmia in the hospital. The report shows bundle of His recording, pacing and recording of the right atrium, and induction of arrhythmia by electrical pacing. What CPT® code(s) is/are reported? a. 93620-26 b. 93600-26, 93602-26, 93610-26, 93618-26 Response Feedback: Rationale: Although the physician stated a comprehensive EP study was performed, the right ventricular pacing and recording, and left atrial pacing and recording from the coronary sinus or left atrium were not done. The components must be billed separately. Look in the CPT® Index for Electrophysiology Procedure directing you to 93600-93660. The procedure was performed in the hospital; therefore, modifier 26 is appended to all the codes to report the professional service. • Question 15 4 out of 4 points What information is required to accurately code PVD with diabetes in ICD-10-CM? c. Whether the patient has gangrene. c. Whether the patient has gangrene. Response Feedback: Rationale: PVD is the abbreviation for Peripheral Vascular Disease. ICD-10-CM indexes PVD with diabetes with one code. For proper code selection the provider must document if the patient has gangrene or not. Look in the ICD-10-CM Alphabetic Index for Diabetes, diabetic/with/peripheral angiopathy which directs the coder to E11.51. • Question 16 4 out of 4 points In the hospital setting a patient undergoes transcatheter placement of an extracranial vertebral artery stent in the right vertebral artery. Which CPT® code is reported by the physician providing only the radiologic supervision and interpretation? a. 0075T-26 a. 0075T-26 Response Feedback: Rationale: This is a Category III code. Look in the CPT® Index for Stent/Placement/Transcatheter/Intravascular/Extracranial and you are referred to 0075T-0076T. When you check these codes you see supervision and interpretation is included; therefore, modifier 26 reports the professional service. • Question 17 4 out of 4 points A 35 year-old patient presented to the outpatient hospital for PTA of an obstructed hemodialysis AV graft in the venous anastomosis and the immediate venous outflow. The procedure was performed under moderate sedation administered by the physician performing the PTA. The physician performed all aspects of the procedure, including radiological supervision and interpretation. Code for all services performed. c. 36902 c. 36902 Response Feedback: Rationale: PTA is the abbreviation for percutaneous transluminal angioplasty. This procedure involves the peripheral dialysis segment, which in the upper extremity extends through the axillary vein or the entire cephalic vein in the case of cephalic venous outflow. The correct code is 36902, which includes angioplasty and all radiological supervision and interpretation. Moderate sedation is not included in this code; however, 99152 is not reported, because the documentation does not indicate who monitored the patient, the medication, the dosage, or the time of the moderate sedation. • Question 18 4 out of 4 points During an inpatient hospitalization, a patient who suffered myocardial infarction had a combined right and left heart catheterization. Access was achieved through the right femoral artery and the right femoral vein. Selective catheterization of the coronary arteries and selective catheterization of the left ventricle were followed by injections of contrast and angiography. During right heart catheterization, angiography of the right atrium was performed. Imaging supervision, interpretation and report for all angiography was performed during the cardiac catheterization. Select the CPT® code(s) for this procedure by the cardiologist. c. 93460-26, 93566 c. 93460-26, 93566 Response Feedback: Rationale: There are three parts to cardiac catheterization: selective catheter placement, injection of contrast, and radiologic supervision and interpretation and report which are included in most of the cardiac catheterization codes. In the CPT® Index look for Cardiac Catheterization/Combined Left and Right Heart/with Left Ventriculography which directs you to 93453, 93460-93461. Code 93460 includes right and left heart catheterization, coronary angiography, and left ventriculography. None of the combined right and left heart catheterizations include right atrial angiography; therefore, the add-on code 93566 is reported. Modifier 26 is required to report the professional service. The add-on code 93566 for the injection procedure is a professional service, and modifier 51 is not required. • Question 19 0 out of 4 points The skin over the left groin was prepped and draped in a sterile fashion and anesthetized with 1% Xylocaine. Through a right femoral artery access, a 5 French pigtail catheter was placed in the abdominal aorta and a run-off was performed following injection of 80cc of contrast. Oblique DSA images of the iliac circulation were performed following two injections, each 15cc. Findings: Abdominal aorta: no signs of renal artery stenosis. There is mild atheromatous change involving the lower abdominal aorta. There are two eccentric plaques arising from the distal aorta just above the iliac bifurcation. There are high-grade stenoses involving both proximal iliacs, the right far more pronounced than the left. The right superficial femoral, profunda femoral, popliteal arteries are normal. The trifurcation vessels are unremarkable. On the left, there is an eccentric plaque in the common femoral artery just below the catheter entrance site. This creates approximately 40-50% stenosis at this site. The remainder of the proximal femoral artery is normal. The trifurcation vessels and popliteal artery are normal. b. 36200, 75625-26 d. 36200, 75630-26 Response Feedback: Rationale: The nonselective catheter placement in the aorta is reported with 36200. Look in the CPT® Index for Aorta/Catheterization/Catheter. Contrast was injected from one catheter placement site, and there is a report for the aorta and the extremities, making this an abdominal aortogram with bilateral iliofemoral lower extremity angiography which directs you to 75630. Modifier 26 is required for the professional service. Look in the CPT® Index for Aortography/Aorta Imaging and you are referred to 75600, 75630, 93567. • Question 20 0 out of 4 points CLINICAL SUMMARY: The patient is a 55 year-old female with known coronary disease and previous left anterior descending and diagonal artery intervention, with recent recurrent chest pain. Cardiac catheterization demonstrated continued patency of the stented segment, but diffuse borderline changes in the ostial/proximal portion of the right coronary artery. PROCEDURE: With informed consent obtained, the patient was prepped and draped in the usual sterile fashion. With the right groin area infiltrated with 2percent Xylocaine and the patient given 2 mg of Versed and 50 mcg of fentanyl intravenously for conscious sedation and pain control, the 6 French catheter sheath from the diagnostic study was exchanged for a 6 French sheath and a 6 French JR4 catheter with side holes utilized. The patient initially received 3000 units of IV heparin, and then IVUS interrogation was carried out using an Atlantis Boston Scientific probe. After it had been determined that there was significant stenosis in the ostial/proximal segment of the right coronary artery, the patient received an additional 3000 units of IV heparin, as well as Integrilin per double bolus injection. A 3.0 16-mm-long Taxus stent was then deployed in the ostium and proximal segment of the right coronary artery in a primary stenting procedure with inflation pressure up to 12 atmospheres applied. Final angiographic documentation was carried out, and then the guiding catheter pulled, the sheath upgraded to a 7 French system, because of some diffuse oozing around the 6 French sized sheath, and the patient is now being transferred to telemetry for post-coronary intervention observation and care. RESULTS: The initial guiding picture of the right coronary artery demonstrates the right coronary artery to be dominant in distribution, with luminal irregularities in its proximal and mid-third with up to 50 percent stenosis in the ostial/proximal segment per angiographic criteria although some additional increased radiolucency observed in that segment. IVUS interrogation confirms severe, concentric plaque formation in this ostial/proximal portion of the right coronary artery with over 80 percent area stenosis demonstrated. The mid, distal lesions are not significant, with less than 40 percent stenosis per IVUS evaluation. Following the coronary intervention with stent placement, there is marked increase in the ostial/proximal right coronary artery size, with no evidence for intimal disruption, no intraluminal filling defect, and TIMI III flow preserved. CONCLUSION: Successful coronary intervention with drug eluting Taxus stent placement to the ostial/proximal right coronary artery. b. 92924-RC, 92925-RC, 92978-51 a. 92928-RC, 92978 Response Feedback: Rationale: IVUS is the abbreviation for Intravascular Ultrasound. Stent placement (92928) and IVUS (92978) are reportable. To find the stent placement code look in the CPT® Index for Coronary Artery/Angioplasty/with Stent Placement which directs you to 92928-92929. Modifier 51 is not appended to IVUS as it is an add-on code. IVUS is reported for each vessel when performed in multiple vessels. Modifier RC is appended to 92928 to indicate the right coronary artery. The coronary artery modifiers are only used for coronary artery interventions. To locate IVUS look in the CPT® Index for Vascular Procedures/Intravascular Ultrasound/Coronary Vessels which directs you to 92978-92979. Do not append modifier RC to the IVUS code. • Question 21 0 out of 4 points In the cardiac suite, an electrophysiologist performs an EP study. With programmed electrical stimulation, the heart is stimulated to induce arrhythmia. Observed is right atrial and ventricular pacing, recording of the bundle of His, right atrial and ventricular recording and left atrial and ventricular pacing and recording from the left atrium. d. 93620, 93618, 93621 c. 93620, 93621, 93622 Response Feedback: Rationale: The studies performed make up a comprehensive study (93620) which includes: evaluation with right atrial pacing and recording, right ventricular pacing and recording, and His bundle recording with induction of or attempted induction of arrhythmia. Left atrial pacing and recording (93621) and left ventricular pacing and recording (93622) are add-on codes. Look in the CPT® Index for Electrophysiology Procedure which directs you to 93600-93660. • Question 22 4 out of 4 points The cardiologist advances a 6 French catheter into the left renal artery via a right common femoral puncture. It is selectively catheterized and angiographic films are taken. The catheter was then removed and a diagnostic guiding type, RDC catheter was used and the left renal artery was selectively engaged. A 0.014 Supracore wire was used and the lesion was crossed. A 6.0 X 18 mm balloon expandable Racer stent was introduced. This was expanded around 8 atmospheres of pressure which is nominal. Angiography revealed excellent results with no residual stenosis. c. 36245-LT, 37236 c. 36245-LT, 37236 Response Feedback: Rationale: The left renal artery is a first order vessel as noted in Appendix L of the CPT® codebook (36245-LT). To locate the selective catheterization, look in the CPT® Index for Artery/Abdomen/Catheterization 36245-36248. Angiography of the left renal vessel was performed; however, there is no mention in the report of the results of the angiography. This is not a diagnostic angiography, rather it is angiography for mapping (checking out known stenosis). The stent was deployed (37236) in the left renal artery; this code also includes the radiologic supervision and interpretation. In the CPT® Index look for Stent/Placement/Transcatheter/Intravascular which directs the coder to 37215-37218, 37236-37239. Follow-up renal angiography is bundled with the stent procedure. • Question 23 0 out of 4 points Catheter advanced from the right femoral vein into the left and right pulmonary artery. The catheter was further negotiated into the right lung lower lobe. Pulmonary angiography performed in all locations including radiologic supervision and interpretation. a. 36014-50, 75741, 75774-26 d. 36015-RT, 36014-59-LT, 75743-26, 75774-26 Response Feedback: Rationale: Look in the CPT® Index for Pulmonary Artery/Catheterization and you are referred to 36013-36015. 36015-RT reports the second order selective catheterization of the right pulmonary artery; 36014-59-LT reports the first order selective catheterization in a different family of the left pulmonary artery. Look in the CPT® Index for Angiography/Pulmonary and you are directed to 75741-75746, 93568. Code 75743-26 reports bilateral pulmonary angiography, and 75774 reports the additional angiography after the basic study of the right and left pulmonary arteries. Look in the CPT® Index for Angiography/Other Artery which directs you to 75774. • Question 24 4 out of 4 points MAZE procedure is performed on a patient with atrial fibrillation. The physician isolates and ablates the electric paths of the pulmonary veins in the left atrium, the right atrium and the atrioventricular annulus while on cardiopulmonary bypass. b. 33256 b. 33256 Response Feedback: Rationale: The procedure described above is extensive according to CPT® definition. Look in the CPT® Index for Maze Procedure/Open and you are referred to 33254-33256. The patient was on bypass; therefore, the correct code is 33256. • Question 25 4 out of 4 points PREOPERATIVE DIAGNOSIS: Heart Block POSTOPERATIVE DIAGNOSIS: Heart Block ANESTHESIA: Local anesthesia NAME OF PROCEDURE: Reimplantation of dual chamber pacemaker DESCRIPTION: The chest was prepped with Betadine and draped in the usual sterile fashion. Local anesthesia was obtained by infiltration of 1% Xylocaine. A subfascial incision was made about 2.5 cm below the clavicle, and the old pulse generator was removed. Using the Seldinger technique, the subclavian vein was cannulated and through this, the old atrial lead was removed, and a new atrial lead (serial # 6662458) was placed in the right atrium and to the atrial septum. Thresholds were obtained as follows: The P-wave was 1.4 millivolts, atrial threshold was 1.6 millivolts with a resultant current of 3.5 mA and resistance of 467 ohms. Using a second subclavian stick in the Seldinger technique, the old ventricular lead was removed and a new ventricular lead (serial # 52236984) was inserted and placed into the right ventricular apex. The thresholds were obtained and were as follows: R-wave was 23.5 millivolts. The patient was pacing at 100% at 0.5 volts, with resultant current of 0.8 mA and resistance of 480 ohms. When we were satisfied with the thresholds, the leads were connected to the pacemaker generator (serial # 22561587), which was inserted into the previously created pocket. The wound was thoroughly irrigated with antibiotic solution and hemostasis was obtained. The incision was closed in layered fashion with 2-0 Dexon. A compressive dressing was applied, and the patient tolerated the procedure very well. He was taken to the recovery room in satisfactory condition. c. 33235, 33208-51, 33233-51 c. 33235, 33208-51, 33233-51 Response Feedback: Rationale: Code 33235 reports removal of the electrodes of a dual pacemaker lead system. Code 33208 reports replacement of permanent pacemaker generator with transvenous electrodes to the right atrium and right ventricle, and 33233 reports the removal of a pacemaker generator. Modifier 51 reports multiple procedures performed during the same session. Look in the CPT® Index for Pacemaker, Heart/Insertion which direct you to 33206-33208. Next look for Pacemaker, Heart/Removal/Pulse Generator Only which directs you to 33233. Look for Pacemaker, Heart /Removal/Transvenous Electrodes which directs the coder to 33234-33235. Sunday, November 19, 2017 9:15:25 AM MST • Question 1 10 out of 10 points Name the three sections of the small intestine. d. Duodenum, jejunum, ileum d. Duodenum, jejunum, ileum Response Feedback: Rationale: The three sections of the small intestine are the duodenum, jejunum, and the ileum. The ilium (note spelling) is one of the bones located in the pelvis. The sigmoid, rectum, and cecum are parts of the large intestine. • Question 2 10 out of 10 points What is the function of the gall bladder? b. It conveys and stores bile. b. It conveys and stores bile. Response Feedback: Rationale: The gall bladder is a sac-shaped organ located under the liver. It stores bile that is produced by the liver. • Question 3 10 out of 10 points Approximately how long is the large intestine in normal anatomy? d. 5ft. long d. 5ft. long Response Feedback: Rationale: The large intestine is about five feet long. • Question 4 10 out of 10 points A 28-year-old female has constant abdominal pain and diarrhea. The provider runs blood tests and takes a stool sample. A colonoscopy with biopsy is performed to rule out ulcerative colitis. The provider determines the patient has IBS. What is/are the correct diagnosis code(s)? d. K58.0 d. K58.0 Response Feedback: Rationale: IBS is an acronym for irritable bowel syndrome, and can cause the intestinal tract to contract stronger and longer than normal. This may cause symptoms such as abdominal pain, constipation or diarrhea, and/or flatulence. To find IBS in the ICD-10-CM, look in the ICD-10-CM Alphabetic Index for Syndrome/irritable/bowel/with diarrhea leading you to code K58.0. Abdominal pain and diarrhea are symptoms of IBS, and not coded separately. Ulcerative colitis is a rule-out diagnosis and is not coded. • Question 5 10 out of 10 points A patient with a large prolapsed hemorrhoid arrives at the Emergency Department. After multiple attempts, the provider is unable to reduce it. The physician applies granulated sugar to the hemorrhoid and is able to reduce the hemorrhoid. What is the correct diagnosis code? c. K64.8 c. K64.8 Response Feedback: Rationale: Hemorrhoids are dilated or enlarged varicose veins which occur in and around the anus and rectum. The condition can be complicated by thrombosis, strangulation, prolapse, and ulceration. To find hemorrhoids in the ICD-10-CM Alphabetic Index, locate Hemorrhoids/Prolapsed directing you to K64.8. Verify code selection in the Tabular List. • Question 6 10 out of 10 points A 42-year-old patient visits his doctor for chest pain and a dry cough lasting for two months. After evaluating the patient, the physician states the patient has GERD. What is/are the correct diagnosis code(s)? b. K21.9 b. K21.9 Response Feedback: Rationale: GERD is the definitive diagnosis. Chest pain and a dry cough are both symptoms of GERD and are not reported separately. GERD is an acronym for gastroesophageal reflux disease. In the ICD-10-CM Alphabetic Index, look for Disease/gastroesophageal reflux (GERD) or look for GERD, and you are guided to K21.9. There is no indication the patient has esophagitis. • Question 7 10 out of 10 points Code intraoral incision and drainage of hematoma of tongue, submandibular space. What CPT® code is reported? a. 41008 a. 41008 Response Feedback: Rationale: CPT® code 41008 is specifically for Intraoral incision and drainage of abscess, cyst, or hematoma of tongue or floor of mouth; submandibular space. Look in the CPT® Index for Drainage/Hematoma/Mouth/Submandibular Space. The code selection is made because it is intraoral, not extraoral. • Question 8 10 out of 10 points A 55-year-old patient underwent a repair of an initial left inguinal hernia. An incision was made at the groin. A hernia sac was readily identified and cleared from the surrounding tissue, inverted into the preperitoneal space, and plugged. Mesh was tacked to the surrounding muscle layers and then placed over the entire floor. What CPT® code(s) is/are reported? b. 49505-LT b. 49505-LT Response Feedback: RATIONALE: In the CPT® Index, look for Hernia Repair/Inguinal/Initial, Child 5 Years or Older. You are referred to 49505 and 49507. Review the codes to choose the appropriate service. 49505 is the correct code. The repair was through an incision (not by laparoscopy) on an initial inguinal hernia on a patient over five years of age and the hernia was not incarcerated or strangulated. According to CPT® guidelines, “With the exception of the incisional hernia repairs (49560–49566), the use of mesh or other prosthesis is not separately reported.” It is inappropriate to code the mesh in this scenario. Modifier LT is appended to indicate the hernia is on the left side. • Question 9 0 out of 10 points Code peritoneoscopy with laparoscopic partial colectomy and anastomosis. What CPT® code(s) is/are reported? c. 49320, 44140 b. 44204 Response Feedback: Rationale: A peritoneoscopy is a separate procedure and is not separately reportable when it is performed with a more extensive procedure. It is incidental to the laparoscopic partial collection and anastomosis. Look in the CPT® Index for Colectomy/Partial/with Anastomosis/Laparoscopic. The code is selected based on whether additional procedures, such as a coloproctostomy, is performed. There are no additional procedures in this case making 44204 the correct code choice. • Question 10 10 out of 10 points Code proximal subtotal pancreatectomy, with total duodenectomy, partial gastrectomy, choledochoenterostomy, and gastrojejunostomy, with pancreatojejunostomy. What CPT® code is reported? a. 48150 a. 48150 Response Feedback: Rationale: The CPT® code 48150 is specifically for pancreatectomy, proximal subtotal with total duodenectomy, partial gastrectomy, choledochoenterostomy, and gastrojejunostomy (Whipple-type procedure); with pancreatojejunostomy. Look in the CPT® Index for Pancreas/Excision/Partial. Sunday, November 19, 2017 9:15:59 AM MST • Question 1 4 out of 4 points A patient is seen to have an esophageal motility procedure with acid perfusion study performed. What CPT® code(s) is/are reported? c. 91010, 91013 c. 91010, 91013 Response Feedback: Rationale: This is a diagnostic gastrointestinal procedure. Look in the CPT® Index for Gastroenterology, Diagnostic/Esophagus Tests/Motility Study which directs you to codes 91010, 91013. 91010 best describes the motility study with add-on code 91013 used to identify the acid profusion study. Parenthetical note under add-on code 91013 indicates it is reported with code 91010. • Question 2 4 out of 4 points What ICD-10-CM code(s) is reported for ulcerative colitis with rectal bleeding? b. K51.911 b. K51.911 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Colitis/ulcerative (chronic)/with complication/rectal bleeding which directs you to K51.911. Verify the code in the Tabular List. This is a combination code that covers both ulcerative colitis and rectal bleeding. An additional code for rectal bleeding would not be reported. • Question 3 4 out of 4 points What are the CPT® and ICD-10-CM codes for a hemicolectomy performed on a patient with colon cancer? a. 44140, C18.9 a. 44140, C18.9 Response Feedback: Rationale: For the CPT® code, hemi- means half or partial and colectomy is the removal of the colon. Look in the CPT® Index for Colectomy/Partial which directs you to code 44140. Next, look in the ICD-10-CM Alphabetic Index for Carcinoma, which directs you to see also, Neoplasm, by site, malignant. Go to the Table of Neoplasms and look for Neoplasm, neoplastic/colon which directs you to see also Neoplasm/intestine/large and report code C18.9 under the Malignant Primary column. Since there is no documentation the cancer is secondary or had metastasized from another site, it is considered primary. Verify the code in the Tabular List. • Question 4 4 out of 4 points What parts make up the large intestine? d. Cecum with vermiform appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum and anus d. Cecum with vermiform appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum and anus Response Feedback: Rationale: The large intestine consists of the cecum with vermiform appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum and anus. • Question 5 0 out of 4 points A patient is seen in the ED for nausea and vomiting that has persisted for 4 days. The ED physician treats the patient for dehydration which is documented in the patient’s record as the final diagnosis. What ICD-10-CM code(s) is/are reported for this encounter? a. R11.2, E86.0 b. E86.0 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Dehydration which directs you to E86.0. Because there is a definitive diagnosis, it is reported instead of the symptoms. • Question 6 4 out of 4 points Bile empties into the duodenum through what structure? b. Common bile duct b. Common bile duct Response Feedback: Rationale: The liver produces bile which passes from the bile duct of the liver and finds its way into the small intestine by way of common bile duct. • Question 7 4 out of 4 points What is the correct CPT® coding for a partial distal gastrectomy with Roux-en-Y reconstruction with vagotomy? d. 43633, 43635 d. 43633, 43635 Response Feedback: Rationale: In CPT® Index, look for Gastrectomy/Partial, which directs us to several codes including 43631-43635. When reviewing these codes in the main section of CPT®, code 43633 code descriptor represents a partial gastrectomy with Roux-en-Y reconstruction. Next, look for Vagotomy/with Partial Distal Gastrectomy in the CPT Index. Code 43635 represents the vagotomy. Modifier 51 is not used as code 43635 is an add-on code and is modifier 51 exempt. • Question 8 4 out of 4 points What ICD-10-CM code is reported for non-erosive duodenitis? a. K29.80 a. K29.80 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Duodenitis (nonspecific) (peptic) K29.80. An additional code is listed including the description of bleeding K29.81. There is no mention of bleeding so verification of both codes in the Tabular List confirms code selection is K29.80. • Question 9 0 out of 4 points A patient presents with a 2 cm benign lip lesion. The provider decides to remove the lesion along with a portion of the lip by performing a wedge excision. Single-layer suture repair is performed. What CPT® code(s) is/are reported for this service? d. 11442, 40510 b. 40510 Response Feedback: Rationale: Because the physician is not only removing the lesion, but also removing part of lip, code 11422 is not reported. The lesion and a portion of the lip are removed by a transverse wedge technique. Look in the CPT® Index for Wedge Excision/Lip referring you to code 40510. The code description for code 40510 includes primary closure (suture repair) indicating an integumentary system repair code (12011) is not reported separately. • Question 10 4 out of 4 points What CPT® and ICD-10-CM codes are reported for a gastric restriction by placing a gastric band via laparoscopic surgery for an adult patient diagnosed as morbidly obese having a BMI of 43, type 2 uncontrolled diabetes and elevated blood sugar readings daily? a. 43770, E66.01, Z68.41, E11.9 a. 43770, E66.01, Z68.41, E11.9 Response Feedback: Rationale: In the CPT® Index, look for Laparoscopy/Stomach/Gastric Restrictive Procedures which refers to 43770-43775, 43848, 43886-43888 or Laparoscopy/Gastric Restrictive Procedures and you are directed to 43644, 43645, 43770-43775. In reviewing the code descriptions, 43770 is correct code for placement of adjustable gastric bands laparoscopically. Look in the ICD-10-CM Alphabetic Index for Obesity/morbid. You are directed to code E66.01. An instructional note beneath E66 states, “Use additional code to identify body mass index (BMI), if known (Z68.-)”. Turning to Z68 in the Tabular List, you find a list of subcategories specific to adult and pediatric BMI ranges. The patient has a BMI of 43 falling into the range of ICD-10 code Z68.41. Next, look for Diabetes/type 2, directing you to subcategory code E11.9 Verification of the codes in the Tabular List confirms code selections. • Question 11 4 out of 4 points A 12 year-old patient had an adenoidectomy in 2013 and a second adenoidectomy this year. What CPT® code(s) is/are reported for the second adenoidectomy performed this year? a. 42836 a. 42836 Response Feedback: Rationale: Sometimes adenoid tissue, even after it has been removed, will grow back when a few cells are left behind. For the removal of the secondary adenoid tissue, report code 42836 which represents the secondary adenoidectomy. Look in the CPT® Index for Adenoids/Excision with a code range of 42830-42836. In this case, the patient is over 12 years of age upon presentation for the secondary adenoidectomy, further supporting the criteria for 42836. • Question 12 4 out of 4 points What is the correct ICD-10-CM code for a patient with IBS? b. K58.9 b. K58.9 Response Feedback: Rationale: IBS stands for Irritable Bowel Syndrome. Look in the ICD-10-CM Alphabetic Index for Syndrome/irritable/bowel which directs you to code K58.9. Verify the code in the Tabular List. • Question 13 4 out of 4 points A 7 year-old female presents to the same day surgery unit for a tonsillectomy. During the surgery the physician notices the adenoids are very inflamed and must be taken out as well. The adenoids, although not planned for removal, are removed following the tonsillectomy. What CPT® code(s) is/are reported for the procedure? b. 42820 b. 42820 Response Feedback: Rationale: In the CPT® Index look for Tonsils/Excision/with Adenoids directing you to 42820-42821. Code 42820 represents the removal of both the tonsils and adenoids. These are age specific codes and 42820 represents anyone younger than age 12. • Question 14 4 out of 4 points What CPT® code(s) is/are reported for an endoscopic direct placement of a percutaneous gastrostomy tube for a patient who previously underwent a partial esophagectomy? c. 43246 c. 43246 Response Feedback: Rationale: Code 43246 represents the direct percutaneous placement of a gastrostomy tube. We do not code for the partial esophagectomy (43116) because it was not performed at this time but was done prior to the tube placement. The code is indexed in CPT® under Endoscopy/Gastrointestinal/Upper/Tube Placement which refers you to code 43246. There are a couple of other ways to find this in the Index. It helps to remember anatomy and that each surgical section in CPT has a diagram for you to review. The esophagus is part of the upper GI tract. • Question 15 4 out of 4 points A 45 year-old woman underwent a cholecystectomy performed laparoscopically. The procedure was performed for recurrent bouts of acute cholecystitis. What CPT® and ICD-10-CM codes are reported? b. 47562, K81.0 b. 47562, K81.0 Response Feedback: Rationale: In the CPT® Index, look for Cholecystectomy/Laparoscopic which directs you to 47562-47564. 47600 and 47605 are open cholecystectomy codes. By turning to the numeric section of CPT and reviewing the code descriptions, you can verify that 47562 is the appropriate code for a laparoscopic cholecystectomy with no additional procedures performed. Acute cholecystitis is indexed in ICD-10-CM Alphabetic Index under Cholecystitis/acute for code K81.0. • Question 16 4 out of 4 points A patient was taken to the emergency room for severe abdominal pain, nausea and vomiting. A WBC (white blood cell count) was taken and the results showed an elevated WBC count. The general surgeon suspected appendicitis and performed an emergent appendectomy. The patient had extensive adhesions secondary to two previous Cesarean deliveries. Dissection of this altered the anatomical field and required the surgeon to spend 40 additional intraoperative minutes. The surgeon discovered the appendix was not ruptured nor was it hot. Extra time was documented in order to thoroughly irrigate the peritoneum. What CPT® and ICD-10-CM codes are reported? c. 44950-22, R10.9, R11.2, D72.829 c. 44950-22, R10.9, R11.2, D72.829 Response Feedback: Rationale: Code 44950 represents the appendectomy performed. In the CPT® Index, look for Appendectomy/Appendix Excision. Modifier 22 is appended due to the extensive adhesions that required 40 additional minutes be spent in order to perform the procedure safely and correctly. The signs and symptoms are reported because the surgeon suspected appendicitis. In the ICD-10-CM Alphabetic Index, look for Pain(s)/abdominal, which directs you to R10.9. Next, in the Alphabetic Index look for Nausea/with vomiting and you are directed to R11.2. Then, look for Leukocytosis, abnormally large number of leukocytes, which directs you to D72.829. Verification in the Tabular List confirms code selections. • Question 17 4 out of 4 points An 11 year-old patient is seen in the OR for a secondary palatoplasty for complete unilateral cleft palate. Shortly after general anesthesia is administered, the patient begins to seize. The surgeon quickly terminates the surgery in order to stabilize the patient. What CPT® and ICD-10-CM codes are reported for the surgeon? b. 42220-53, Q35.9, R56.9 b. 42220-53, Q35.9, R56.9 Response Feedback: Rationale: In the CPT® Index, look for Palatoplasty 42145, 42200-42225. An alternate path is Cleft Palate/Repair, 42200-42225. Review of the code descriptions in the main section confirms code 42220 represents a secondary repair to a cleft palate. Modifier 53 is appended because the procedure was terminated after anesthesia due to extenuating circumstances. The diagnosis of a complete unilateral cleft palate is indexed in the ICD-10-CM Alphabetic Index under Cleft/palate referring you to code Q35.9. The unspecified code is the appropriate code because the surgeon did not provide specific information for the location of the cleft. Next, return to the Alphabetic Index and look for Seizure(s) (see also Convulsions) R56.9. Both listings direct the coder to R56.9 Unspecified convulsions in the Tabular List. Code R56.9 is reported because the patient began to seize after administering the general anesthesia. • Question 18 4 out of 4 points Surgical laparoscopy with a cholecystectomy and exploration of the common bile duct for cholelithiasis. What CPT® and ICD-10-CM codes are reported? a. 47564, K80.20 a. 47564, K80.20 Response Feedback: Rationale: Look in the CPT® Index for Cholecystectomy/Laparoscopic 47562-47564. Code 47564 is accurate for laparoscopic cholecystectomy when the exploration of the common bile duct is also performed There is a diagnosis of cholelithiasis but no mention of obstruction and not with cholecystitis. The correct ICD-10-CM code is K80.20. In the ICD-10-CM Alphabetic Index, look for Cholelithiasis (cystic duct) (gallbladder) (impacted) (multiple) which instructs you to see Calculus, gallbladder. Look for Calculus/gallbladder you are directed to K80.20. • Question 19 0 out of 4 points A patient suffering from cirrhosis of the liver from alcohol abuse presents with a history of coffee ground emesis (bleeding). The surgeon diagnoses the patient with esophageal gastric varices. Two days later, in the hospital GI lab, the surgeon ligates the varices with bands via an UGI endoscopy. What CPT® and ICD-10-CM codes are reported? c. 43205, K74.60, I85.01, F10.20 b. 43244, K70.30, I85.11, F10.10 Response Feedback: Rationale: Ligation of esophageal gastric varices endoscopically is coded with CPT® code 43244. This is indexed in CPT® under Ligation/Esophageal Varices. In the ICD-10-CM Alphabetic Index, look for Varices – see Varix. Look for Varix/esophagus/in (due to)/cirrhosis of liver/bleeding. You are directed to I85.11. In the Tabular List there are two instructional notes. The first one is under subcategory code I85.1-. It instructs you to code first underlying disease, which in this case, is the cirrhosis of the liver from the alcohol. Look for Cirrhosis/liver/alcoholic and you are directed to K70.30. The other instructional note is under category code I85 which says to use an additional code to report alcohol abuse and dependence. Alcohol abuse is reported with code F10.10. • Question 20 4 out of 4 points A 57 year-old patient with chronic pancreatitis presents to the operating room for a pancreatic duct-jejunum anastomosis by the Puestow-type operation. What are the correct CPT® and ICD-10-CM codes for the encounter? a. 48548, K86.1 a. 48548, K86.1 Response Feedback: Rationale: In the CPT® Index, look for Puestow Procedure. Code 48548 represents a Puestow-type procedure for the anastomosis of the pancreatic duct to the jejunum. Code K86.1 represents the chronic pancreatitis. Look in the ICD-10-CM Alphabetic Index for Pancreatitis/chronic (infectious). • Question 21 4 out of 4 points How do you report a screening colonoscopy performed on a 65 year-old Medicare patient with a family history of colon cancer? The patient’s 72 year-old brother was just diagnosed with colon cancer. The physician was able to pass the scope to the cecum. What CPT® and ICD-10-CM codes are reported? d. G0105, Z12.11, Z80.0 d. G0105, Z12.11, Z80.0 Response Feedback: Rationale: For a Medicare patient the preferred code to report a screening colonoscopy is HCPCS code G0105 Colonoscopy/Screening/Individual at high risk. In the ICD-10-CM Alphabetic Index, look for Screening/colonoscopy which directs you to Z12.11. An instructional note under Z12 instructs the coder, “Use additional code to identify any family history of malignant neoplasm (Z80.-)”. Since the patient is high risk due to a family history of colon cancer, look for Z80 in the Tabular List. The patient’s brother has colon cancer so the appropriate code is Z80.0, Family history of primary malignancy neoplasm of digestive organs. To find the code, look in the Alphabetic Index for History/family (of)/malignant neoplasm/gastrointestinal tract. • Question 22 0 out of 4 points A patient with hypertension is scheduled for same day surgery for removal of her gallbladder due to chronic gallstones. She is examined preoperatively by her cardiologist to be cleared for surgery. What ICD-10-CM codes are reported by the cardiologist? d. I10, Z01.818, K80.20 c. Z01.810, K80.20, I10 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Examination/preoperative – see Examination, pre-procedural. Look for Examination/pre-procedural/cardiovascular referring you to Z01.810. Next, look for Calculus/gallbladder K80.20 and Hypertension which refers you to I10. Correct codes and sequencing are Z01.810, K80.20 and I10. Sequencing of preoperative clearance first, then the reason for the surgery, and last, any other findings or diagnoses. (Sequencing rule from Official Coding Guidelines of ICD-10-CM Section IV.M.) • Question 23 4 out of 4 points A 4 year-old patient, who accidentally ingests valium found in his mother’s purse, is found unconscious and rushed to the ED. The child is treated by the ED physician, who inserts a tube orally into the stomach and performing a gastric lavage and removing the stomach contents. What CPT® and ICD-10-CM codes are reported? b. 43753, T42.4X1A, R40.20 b. 43753, T42.4X1A, R40.20 Response Feedback: Rationale: Code 43753 is the correct CPT® code for gastric lavage performed for the treatment of ingested poison and is found in the CPT® Index under Gastric Lavage, Therapeutic/Intubation. The ICD-10-CM code for the poisoning is found in the Table of Drugs and Chemicals by looking for Valium/Poisoning, Accidental (unintentional) column. You are referred to code T42.4X1-. In the Tabular List a 7thcharacter is needed to complete the code. A is reported as the 7th character because this was the patient’s initial encounter. The next code is the manifestation of ingesting the Valium – unconsciousness. Unconsciousness is found in the ICD-10-CM Alphabetic Index and directs you to see Coma R40.20. The Tabular List confirms this code is reported for unconsciousness. • Question 24 4 out of 4 points A 56 year-old patient complains of occasional rectal bleeding. His physician decides to perform a rigid proctosigmoidoscopy. During the procedure, two polyps are found in the rectum. The polyps are removed by a snare. What CPT® and ICD-10-CM codes are reported? d. 45315, K62.1 d. 45315, K62.1 Response Feedback: Rationale: In the CPT® Index, look for Proctosigmoidoscopy/Removal/Polyp which directs you to 45308-45315. During the proctosigmoidoscopy, polyps were removed by snare technique. 45315 is the correct code for the removal of more than one polyp by snare technique. The correct ICD-10-CM code is K62.1 because the polyps are located in the rectum. In the ICD-10-CM Alphabetic Index, look for Polyp, polypus/rectum. You are directed to K62.1. The other code, K63.5, is for polyps that are located in the large intestine and would be inappropriate in this case. • Question 25 4 out of 4 points A 20 year-old patient presented to the hospital with a history of bloody stools for three weeks’ duration. The patient was prepped for a sigmoidoscopy. The sigmoidoscope was passed without difficulty to about 40 cm. The entire mucosal lining was erythematosus. There was no friability of the overlying mucosa and no bleeding noted. No pseudo polyps were identified. Biopsies were taken at about 30 cm; these were thought to be representative of the mucosa in general. The scope was retracted; no other abnormalities were seen. What CPT® and ICD-10-CM codes are reported? a. 45331, K92.1 a. 45331, K92.1 Response Feedback: Rationale: CPT® code for a sigmoidoscopy with single or multiple biopsies is reported 45331. This is indexed in CPT® under Sigmoidoscopy/Biopsy. Diagnostic sigmoidoscopy is always bundled with a surgical sigmoidoscopy when both are performed in the same operative session. The ICD-10-CM code for bloody stools is found in the ICD-10-CM Alphabetic Index under Blood/in/feces or Hematochezia (see also Melena) and is coded K92.1. When a patient comes in with a GI symptom (bloody stool, abdominal pain, etc.) and no definitive diagnosis is documented, the symptom(s) should be reported. Sunday, November 19, 2017 9:16:14 AM MST • Question 1 10 out of 10 points Which gland in the male reproductive system is partly muscular and partly glandular? a. Prostate a. Prostate Response Feedback: Rationale: The prostate gland is the gland that is partly muscular and glandular. • Question 2 10 out of 10 points Urine is expelled from the body through the: c. Urethra c. Urethra Response Feedback: Rationale: The urine travels from the kidneys to the ureters, to the bladder, where it is stored until it is expelled through the urethra. • Question 3 10 out of 10 points Mr. Jones is an 85-year-old male who has gross hematuria, likely from a prostatic source. He has had a TURP in the past. What is the ICD-10-CM code for gross hematuria? c. R31.0 c. R31.0 Response Feedback: RATIONALE: Although there is documentation that the patient previously had a TURP, there is no documentation of continuing BPH (a condition for which a TURP routinely is performed). Because documentation states gross hematuria, microscopic or unspecified hematuria would be inappropriate codes. Gross hematuria R31.0 is the correct answer. In the ICD-10-CM Alphabetic Index look for Hematuria/gross directing you to R31.0. Verify code selection in the Tabular List. • Question 4 10 out of 10 points A 13-year-old male presents with complaints of urinary hesitancy, frequency and dysuria. A microscopic urinalysis confirmed the presence of white blood cells (WBC) and diagnosis of UTI is confirmed. What is the ICD-10-CM code? d. N39.0 d. N39.0 Response Feedback: RATIONALE: Urinary hesitancy (R39.11), urinary frequency (R35.0) and dysuria (R30.0) are all symptoms of a urinary tract infection. Because a diagnosis of UTI was confirmed by microscopic analysis, the symptoms would not be coded. Look in the ICD-10-CM Alphabetic Index for Infection, infected, infective/urinary (tract) N39.0. Verify code selection in the Tabular List. • Question 5 10 out of 10 points The urologist is asked by the general surgeon to place ureteral catheters for visualization of ureters during a complicated bowel surgery. Cystoscopy is performed and ureteral catheters are inserted. The general surgeon removes the catheters at the end of the case. Code the procedure. b. 52005 b. 52005 Response Feedback: RATIONALE: Placement of the ureteral catheters was performed via cystoscopy; CPT® 50605 would not be appropriate as this code is for an open insertion of indwelling stent into the ureter. CPT® 52332 describes the insertion of an indwelling ureteral stent and is not reported for temporary catheter insertion. CPT® 52310 describes the removal of a ureteral stent, but does not cover the insertion of the catheters. CPT® 52005 Cystourethroscopy, with ureteral catheterization, with or without irrigation, instillation or ureteropyelography, exclusive of radiologic services is correct. There would be no additional code reported for removal of these catheters. Look in the CPT® Index for Catheterization/Cystourethroscopy/Ureteral. No modifier is used, because this code includes both ureters. • Question 6 10 out of 10 points Patient presents with recurrent bladder outlet obstruction secondary to prostate enlargement and requires transurethral resection of the prostate (TURP). Patient previously had a TURP 10 years ago. Code the TURP: b. 52630 b. 52630 Response Feedback: RATIONALE: As a previous TURP was performed, CPT® 52601 is not appropriate because this code is used for the initial TURP and any subsequent transurethral resection procedures of the prostate would not be reported using this code. CPT® 52648 is described as laser vaporization of the prostate which is not the case. CPT® 52500 is described as transurethral resection of bladder neck. Because the prostate was resected, not the bladder neck, this is inappropriate. CPT® 52630 describes TURP of residual or regrowth of obstructive prostate tissue, which is the appropriate code. Look in the CPT® Index for TURP - See Prostatectomy, Transuretheral 52601, 52630. Verify in the numeric section. • Question 7 0 out of 10 points A circumcision was performed on a newborn using a dorsal penile nerve block for anesthesia. The provider used a Plastibell for this circumcision. What CPT® code is reported? b. 54160 a. 54150 Response Feedback: Rationale: In the CPT® Index, look for Circumcision/Surgical Excision/Neonate 54150, 54160. A Plastibell is a type of device used in circumcision. Code 54150 is correct. Modifier 52 is not required; because a dorsal penile nerve block was used. • Question 8 10 out of 10 points A right side epididymectomy and spermatocelectomy are performed on a 15-year-old male. What code is reported for this procedure? c. 54840 c. 54840 Response Feedback: RATIONALE: Code 54840 describes the excision of spermatocele, with or without epididymectomy and is the correct code. The epididymectomy codes (58460-58461) are not reported as the procedure is included in 54840. A lesion was not removed from the epididymis, making 54830 incorrect. Look in the CPT® Index for Spermatocele/Excision 54840. • Question 9 0 out of 10 points What modifier is appended to report the technical component of a procedure? b. 26 a. TC Response Feedback: RATIONALE: Some CPT® codes have a technical component and a professional component. Modifier 26 is appended when the professional component is provided and modifier TC is appended when the technical component is provided. Professional services are those in which the physician performs supervision and an interpretation and report. Technical services includes ownership of the equipment, space, and employment of the technicians or nurses who performed the study. • Question 10 10 out of 10 points What modifier is appended to report a bilateral procedure? d. B or C d. B or C Response Feedback: RATIONALE: Depending upon the insurer, either modifier 50 or RT and LT is appended to the surgical procedure. Sunday, November 19, 2017 9:16:42 AM MST • Question 1 4 out of 4 points Left ureteral stent placement and Extracorporeal Shock Wave Therapy or Lithotripsy (ESWL) of the left kidney are performed. What CPT® code(s) is/are reported for this service? d. 50590-LT, 52332-51-LT d. 50590-LT, 52332-51-LT Response Feedback: Rationale: Two procedures are performed. CPT® 52353 describes laser lithotripsy and does not include ESWL. CPT® 52332 describes the stent placement, but does not include the ESWL. CPT® 50590 describes the ESWL but not the placement of the stent. CPT® 50590 and 52332 describe both procedures performed. Modifier LT is appended to 50590 to indicate the lithotripsy was performed on the left kidney. Modifiers 51 and LT are appended to code 52332 to indicate more than one procedure was performed on the left side. Look in the CPT® Index for Lithotripsy/Kidney and Insertion/Stent/Ureteral. • Question 2 4 out of 4 points Preoperative diagnosis: Hematuria. Postoperative diagnosis: Right renal calculi and bladder calculus. What ICD-10-CM code(s) is/are reported for this service? c. N20.0, N21.0 c. N20.0, N21.0 Response Feedback: Rationale: The preoperative diagnosis indicates the reason why the patient is having surgery. The postoperative diagnosis indicates what was found during the surgery. Hematuria is a symptom of renal calculi and bladder calculus, and not coded separately. Refer to ICD-10-CM guideline 1.B. 4. Look in the ICD-10-CM Alphabetic Index for Calculus, calculi, calculous/kidney which directs you to code N20.0 and Calculus, calculi, calculous /bladder which directs you to code N21.0. Verify code selection in the Tabular List. • Question 3 4 out of 4 points What ICD-10 -CM code is reported for carcinoma of the bladder dome? d. C67.1 d. C67.1 Response Feedback: Rationale: Neoplasm codes of the bladder, as well as other organs, are specific to site. In the ICD-10-CM Table of the Neoplasms look for Neoplasm, neoplastic/bladder (urinary)/dome and select the code from the Malignant Primary column which directs you to code C67.1. If the provider documentation does not report the exact location of the tumor, this information may be obtained in the body of the operative report. In this case, it is specifically stated as carcinoma of the bladder dome if no location information is available, using the unspecified diagnosis of C67.9 would be acceptable. Verify code selection in the Tabular List. • Question 4 4 out of 4 points Transurethral resection of a medium-size (3.0 cm) bladder tumor was performed in an outpatient setting. What CPT® code is reported for this service? c. 52235 c. 52235 Response Feedback: Rationale: Transurethral resection of bladder tumors are coded by the size of the tumor; less than 0.5 cm (52224), 0.5 cm- up to 2.0 cm (52234), 2.0 cm up to 5.0 cm (52235), 5.0 cm or larger (52240). In the CPT® Index see Resection/Tumor/Bladder or Tumor/Bladder. • Question 5 4 out of 4 points What are the filtering units of the kidney called? a. Nephrons a. Nephrons Response Feedback: Rationale: The glomerulus and tubules are components of the nephrons. The calyx is an extension of the renal pelvis that encloses the papilla of a renal pyramid; urine from the papillary duct is emptied into it. • Question 6 4 out of 4 points Closure of exstrophy of the bladder is performed with epispadias repair. What CPT® code is reported for this service? b. 54390 b. 54390 Response Feedback: Rationale: In the CPT® Index look for Repair/Epispadias with code range 54380-54890. Code 54390 Plastic operation on penis for epispadias distal to external sphincter; with exstrophy of bladder. Code 51940 is repair of the exstrophy only; code 51860 is a cystorrhaphy, suture of bladder wound or injury; code 51880 is the closure of a cystostomy. • Question 7 4 out of 4 points The urologist performs a cystourethroscopy with ureteroscopy to fulgurate a ureteral lesion. What is/are the CPT® code(s) for the procedure? c. 52354 c. 52354 Response Feedback: Rationale: In the CPT® Index look for Cystourethroscopy/with Fulguration/Lesion. Code choices are 52224, 52354. Code 52354 describes Cystourethroscopy, with ureteroscopy and pyeloscopy; with biopsy and fulguration of ureteral or renal pelvic lesion. • Question 8 4 out of 4 points When a cystectomy is performed, there are various means of diverting the urine. One method is to create a neobladder which allows the patient to void through his or her urethra. Which code describes this procedure? c. 51596 c. 51596 Response Feedback: Rationale: Creation of a neobladder allows the patient the ability to void and is reported with 51596. In CPT® code 51580 an -ostomy is created and urine is emptied into an appliance bag. In CPT® 51590 a catheter is placed and used to remove urine from the body. Look in the CPT® Index for Neobladder/Construction. • Question 9 4 out of 4 points Patient is admitted for acute bilateral pyelonephritis. What is the appropriate ICD-10-CM code? a. N10 a. N10 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Pyelonephritis/acute which directs you to N10. Verify code selection in the Tabular List. • Question 10 4 out of 4 points Which statement is TRUE regarding reporting calculi in both the kidney and ureter? d. One code reports both the calculi in the kidney and the ureter. d. One code reports both the calculi in the kidney and the ureter. Response Feedback: Rationale: ICD-10-CM has a combination code to report when there are stones (calculi) in the kidney and ureter. Look in the ICD-10-CM Alphabetic Index for Calculus, calculi, calculous/kidney/with calculus, ureter which directs you to N20.2. Verify code selection in the Tabular List. • Question 11 4 out of 4 points The patient is a 53 year-old male with a benign prostatic hypertrophy causing urinary obstruction and requires the placement of a temporary urethral stent. What CPT® code is reported for this service? c. 53855 c. 53855 Response Feedback: Rationale: Urethral stents are inserted to maintain patency of the urethra. In the CPT® Index look for Stent/Indwelling/Insertion/Ureter and you are given code choices 50605, 52282, 52356 and 53855. CPT® 50605 is used for an ureterotomy and CPT® 52282 is for the insertion of a permanent stent. Code 52332 is used for a cystourethroscopy. CPT® 53855 describes placement of a temporary prostatic urethral stent. • Question 12 0 out of 4 points Transurethral resection of bladder neck and nodular prostatic regrowth. What CPT® code is reported for this service? b. 52500 d. 52630 Response Feedback: Rationale: CPT® 52630 is reported for a transurethral resection of residual or regrowth of the prostatic tissue. In the CPT® Index look for Transurethral Procedure/Prostate/Resection. CPT® 52500 is a separate procedure and considered an integral part of the prostate resection. CPT® 52640 is used for the transurethral resection of a postoperative bladder neck contracture. • Question 13 0 out of 4 points A partial cystectomy is performed due to the prior administration of radiation. It is complicated due to extensive adhesions and required and additional 2 hours beyond the usual cystectomy procedure. What CPT® code is reported for this service? a. 51555-22 b. 51555 Response Feedback: Rationale: In the CPT® Index look for Cystectomy/Partial/Complicated. The description of code 51555 is Cystectomy, partial; complicated (for example, postradiation, previous surgery, difficult location). Modifier 22 is not appended to the code as it already includes the additional work involved in the procedure. • Question 14 4 out of 4 points Patient presents to the emergency room with complaints of an erection lasting longer than two hours. Saline solution is used to irrigate the corpora cavernosa. What CPT® code is reported for this service? d. 54220 d. 54220 Response Feedback: Rationale: Priapism is a condition marked by a prolonged erection. This condition must be treated or permanent damage may result. Usually the penis is irrigated to reduce the erection; however, in some cases, surgical intervention may be necessary. In the CPT® Index look for Irrigation/Penis/for Priapism or Repair/Penis/Priapism. • Question 15 4 out of 4 points A 63 year-old gentleman comes into the ED complaining of the urge to urinate but has been unable to empty his bladder. The provider decides to place a Foley catheter to relieve the urine retention due to prostate hypertrophy. What is the code selection for the procedure and diagnosis codes? a. 51702, N40.1, R33.8 a. 51702, N40.1, R33.8 Response Feedback: Rationale: In the CPT® Index look for Catheter/Bladder referring you to codes 51701-51703. CPT® code 51702 is correct to report for this scenario since an indwelling catheter (for example a Foley catheter) is left in the bladder and urine is drained. Code 51701 is used when a non-indwelling catheter is inserted to determine post void residual urine; this is sometimes called a straight cath. The patient is diagnosed with urine retention and prostate hypertrophy. In the ICD-10-CM Alphabetic Index look for Enlargement, enlarged/prostate/with lower urinary retention guiding you to code N40.1. In the Tabular List locate N40.1 and you are directed to use additional code for associated symptoms. Code R33.8 is used to describe urinary retention. Verify code selection in the Tabular List. • Question 16 0 out of 4 points Preoperative diagnosis: Cytologic atypia and gross hematuria Postoperative diagnosis: Cytologic atypia and gross hematuria Procedure performed: Cystoscopy and random bladder biopsies and GreenLight laser ablation of the prostate. Description: Bladder biopsies were taken of the dome, posterior bladder wall and lateral side walls. Bugbee was used to fulgurate the biopsy sites to diminish bleeding. Cystoscope was replaced with the cystoscope designed for the GreenLight laser. We introduced this into the patient's urethra and performed GreenLight laser ablation of the prostate down to the level of verumontanum on, the prostatic crest near the wall of the urethra. There were some calcifications at the left apex of the prostate, causing damage to the laser but adequate vaporization was achieved. What CPT® code(s) is/are reported for this service? c. 52648, 52204 d. 52648, 52224-59 Response Feedback: Rationale: Laser vaporization is coded using CPT® 52648. In the CPT® Index look for Prostate/Vaporization/Laser directing you to 52648. A biopsy is usually not reported at the same time of the laser procedure. In this case, the operative report clearly states that this procedure is a distinct procedure; it is a different procedure from the GreenLight laser ablation and is reported separately using modifier 59. CPT® 52224 describes cystourethroscopy, with fulguration, with or without biopsy. In the CPT® Index look for Cystourethroscopy/Biopsy. • Question 17 4 out of 4 points Patient is a 67 year-old male with chronic orchialgia following a right inguinal hernia repair. He is admitted for scrotal exploration and simple orchiectomy. The patient is brought to the operating room and placed supine on the operating table in. After adequate anesthesia was accomplished, he was prepped and draped in the usual sterile fashion; 0.25% Marcaine plain was infused in the skin along his median rhaphe and a 4cm median rhaphe incision was made. We dissected into his right hemiscrotum and identified his right testis which was small and atrophic. The spermatic cord was identified and separated into 2 sections each section was double tied with #1 silk suture. The testis was then transected from the spermatic cord, distal to the sutures and no bleeding was noted from the stump of the spermatic cord. Scrotal skin was closed in two layers, the first layer with a running stitch of 3-0 Monocryl and the second was a 3-0 chromic in the horizontal mattress. Dermabond was applied over the incision. He was extubated and taken to the recovery room in good condition. What CPT® code(s) is/are reported for this service? a. 54520 a. 54520 Response Feedback: Rationale: The procedure is a simple orchiectomy with only the removal of the testis. The closure of a surgical incision in included in the procedure code and usually not reported separately. In the CPT® Index look for Orchiectomy/Simple. CPT® 54530 describes a radical orchiectomy which is the removal of the testis and all associated structures. CPT® 54522 describes the partial excision of one or both testis. • Question 18 0 out of 4 points The patient has significant morbid obesity and her pannus has been retracted to help with dissection. The planned procedure is to place a catheter/tube to drain the bladder. It is apparent she has quite a bit of scarring from her previous surgeries and also appears to have an old sinus tract just above the symphysis. A midline incision is made following her old scar from just above the symphysis for a length of about 4-6cm. The sinus tract was excised, as this was also in the midline, and carefully dissected down to the level of the fascia. It does not appear to be an actual hernia, as there are no ventral contents within it. Again, there is quite a bit of distortion from previous scarring because of the obesity, but staying in the midline, the fascia is incised just above the symphysis of a length of about 2cm. The fat and scar is incised above the fascia more superiorly and with palpation, mesh from a previous hernia repair is felt. This was not palpable prior to the incision because of her body habitus. The mesh was not exposed or entered, it comes down quite close to the symphysis and certainly is too close to place a suprapubic (SP) tube. There is concern the mesh may become infected with an SP tube tract right there. Therefore, decision to abort the procedure is made. What CPT® code and modifier are reported for this service? c. 51102-53 b. 51040-53 Response Feedback: Rationale: The intended procedure is cystostomy. In the CPT® Index look for Cystostomy/with Drainage. Modifier 53 is appended when the procedure is terminated due to the well-being of the patient and is appended to the initial procedure intended. CPT® 51102 describes insertion of a suprapubic catheter by aspiration of the bladder; this is not the correct code to report. • Question 19 4 out of 4 points Cystoscopy, left ureteroscopy, holmium laser lithotripsy, stone manipulation, stent removal and replacement are performed. The holmium laser was used to break up a cluster of stones at the ureteropelvic (UP) junction which were removed with a basket and a Gibbons stent was exchanged. Previous CT scan showed stones in the lower right pole. It was decided to proceed with ureteroscopy. Ureteroscope was inserted in the right ureter, confirming multiple stones within the proximal ureter. These were basketed and removed. What CPT® codes are reported for this service? c. 52356-LT, 52352-59-RT c. 52356-LT, 52352-59-RT Response Feedback: Rationale: When a stent is removed and replaced, the removal of the initial stent is included in the stent replacement and is not reported. One code is reported for performing the lithotripsy and replacement of the stent in the left ureter. In the CPT® Index look for Lithotripsy/with indwelling Ureteral Stent Insertion directing you to 52356. Usually the basketing of the stones is included with the laser lithotripsy; however, because basketing of stones is performed on a different ureter (RT) than the laser lithotripsy (LT), it is appropriate to add modifier 59 to CPT® 52352. In the CPT® Index, look for Cystourethroscopy/Removal/Calculus directing you to 52352. • Question 20 4 out of 4 points Benign prostatic hypertrophy with outlet obstruction and hematuria. Operation: TURP Anesthesia: Spinal Description of procedure: The patient was placed on the operating room table in sitting position and spinal anesthesia induced. He was placed in the lithotomy position, prepped and draped appropriately. Resection was begun at the posterior bladder neck and extended to the verumontanum (a crest near the wall of the urethra). Posterior tissue was resected first from the left lateral lobe, then right lateral lobe, then anterior. Depth of resection was carried to the level of the circular fibers. Bleeding vessels were electrocauterized as encountered. Care was taken to not resect distal to the verumontanum, thus protecting the external sphincter. At the end of the procedure, prostatic chips were evacuated from the bladder. Final inspection showed good hemostasis and intact verumontanum. The instruments were removed, Foley catheter inserted and the patient returned to the recovery area in satisfactory condition. What CPT® code is reported for this service? c. 52601 c. 52601 Response Feedback: Rationale: TURP is a Transurethral Resection of the Prostate and reported with 52601. In the CPT® Index TURP directs you to See Prostatectomy, Transurethral. Prostatectomy/Transurethral directs you to 52601, 52630. A TURP is not a bilateral procedure and is not reported with modifier 50. Code 52630 is reported when it is done for residual or regrowth of the obstructive prostate tissue. Code 52640 describes postoperative procedures on the bladder neck. • Question 21 4 out of 4 points Removal of a malfunctioning AMS 700 inflatable penile prosthesis and all components and implantation of an inflatable multi-component AMS Tambocor 14 mm diameter 15 mm length with 2 cm rear tip extender bilaterally in the same surgery session. What CPT® code is reported for this service? a. 54410 a. 54410 Response Feedback: Rationale: In the CPT® Index look for Prosthesis/Penis/Replacement for the code range. The penile prosthesis insertion, repair, removal and replacement codes are very specific. By reading the descriptions carefully you can determine the correct code to report. A repair of the prosthesis was not performed eliminating CPT® 54408. CPT® 54406 describes only the removal of the prosthesis. CPT ® code 54411 is the removal and replacement through an infected field which is not indicated in the question. CPT® 54410 describes the removal and replacement of all components of a multi-component, inflatable penile prosthesis. This is not an appropriate code for a bilateral procedure and modifier 50 is not appended. • Question 22 4 out of 4 points A 67 year-old gentleman with localized prostate cancer will be receiving brachytherapy treatment. Following calculation of the planned transrectal ultrasound, guidance was provided for percutaneous perineal placement of 1-125 seeds into the prostate tissue. What CPT® code is reported for needle placement to insert the radioactive seeds into the prostate? a. 55875 a. 55875 Response Feedback: Rationale: Brachytherapy is a form of radiation in which radioactive seeds or pellets are implanted directly into the tissue being treated to deliver their dose of radiation in a direct fashion and longer period of time. The placement of the seeds is performed percutaneously. The code is indexed in CPT® under Prostate/Insertion/Needle guiding you to code 55875. • Question 23 4 out of 4 points What ICD-10-CM code is reported for Phimosis? a. N47.1 a. N47.1 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Phimosis which directs you to N47.1. Verify code selection in the Tabular List. • Question 24 4 out of 4 points The patient is a pleasant 51 year-old male with morbid obesity, weighing approximately 560 pounds and BMI being 85.1. He has uncontrolled diabetes and was evaluated due to testicular pain. He was found to have erythema, edema and possible areas of eschar on the scrotum. He was transferred to the hospital, evaluated and found to be stable with cellulitis and suspect early Fournier's gangrene. What are the appropriate ICD-10-CM codes reported? b. N49.2, E11.9, E66.01, Z68.45 b. N49.2, E11.9, E66.01, Z68.45 Response Feedback: Rationale: There is incomplete information to determine if the scrotal cellulitis is a complication of the diabetes, therefore, you choose diabetes mellitus without mention of complication. Though Fournier's gangrene is suspected, you do not code a suspected condition. Cellulitis is confirmed. The scrotal cellulitis and diabetes are the appropriate diagnosis codes. In the ICD-10-CM Alphabetic Index look for Cellulitis/scrotum directing you to N49.2. Look for Diabetes/type 2 directing you to E11.9. Look for Obesity/morbid directing you to E66.01. Look for Body, bodies/mass index (BMI)/adult/70 and over Z68.45. • Question 25 4 out of 4 points Patient comes in today to the provider’s office for routine monthly Foley catheter change. A two way Foley catheter is replaced in the usual sterile fashion. An abdominal urinary drainage bag and bedside bag are given to the patient. What is/are the correct code(s)? d. 51702, A4338, A4357, A4358 d. 51702, A4338, A4357, A4358 Response Feedback: Rationale: Routine catheter changes are coded using the insertion of temporary indwelling catheter code 51702. In the CPT® Index look for Catheter/Bladder for the code range 51701-51703. Code 51701 is used for a non-indwelling catheter. Code 51100 and 51102 describe the aspiration of the bladder by needle or catheter. In addition to reporting the catheter insertion, you report the dispensed supplies from the HCPCS Level II book. Sunday, November 19, 2017 9:17:06 AM MST • Question 1 10 out of 10 points A 52-year-old patient is scheduled for surgery for a right ovarian mass. Through an open incision, the surgeon finds a healthy left ovary. A right ovarian mass is visualized and the decision is made to remove the mass and the right ovary. What CPT® code is reported? a. 58940 a. 58940 Response Feedback: RATIONALE: The right ovary was removed which is an oophorectomy. Code 58925 reports removal of an ovarian cyst. Code 58920 reports removal of a wedge (triangular piece) of an ovary or of both ovaries. Code 58720 reports the removal of tube and ovary, unilateral or bilateral. Look in the CPT® Index for Ovary/Excision/Total 58940-58943. Code 58940 is reported for the removal of an ovary. Verify in the numeric section. • Question 2 10 out of 10 points A 63-year-old patient has severe intramural fibroids. The surgeon performs an open total abdominal hysterectomy with removal of the fallopian tubes and ovaries. What CPT® code is reported? b. 58150 b. 58150 Response Feedback: RATIONALE: This is an open total abdominal hysterectomy, not a vaginal hysterectomy 58262. The procedure was not performed laparoscopically 58548. It does not mention that a partial vaginectomy with para-aortic and pelvic lymph node sampling was performed 58200. Look in the CPT® Index for Hysterectomy/Abdominal/Total 58150, 58200, 58956. The correct code is 58150. Verify in the numeric section. • Question 3 10 out of 10 points Physician performs an incision and drainage of an abscess located on the labia majora. What CPT® code is reported? b. 56405 b. 56405 Response Feedback: RATIONALE: The vulva consists of the external female genitalia, which includes the labia minora and majora, clitoris and vestibule. Code 56405 re-ports the I &D of the abscess of the vulva or perineal abscess. Because there is a specific code for an ID of an abscess of the vulva, do not code 10060. Look in the CPT® Index for Incision and Drainage/Abscess/Vulva 56405 Verify in the numeric section. • Question 4 10 out of 10 points Patient comes in with uterine bleeding. Physician performs a diagnostic dilation and curettage by scraping all sides of the uterus. What CPT® code is reported? d. 58120 d. 58120 Response Feedback: RATIONALE: The D &C is performed in the uterus. Look in the CPT® Index for Dilation and Curettage/Corpus Uteri 58120. There is no mention that the patient is postpartum, so you do not report 59160. Verify in the numeric section. • Question 5 0 out of 10 points A patient delivers twins at 32 weeks' gestation for her first pregnancy. The first baby is delivered vaginally, but during the delivery, the second baby turns into a breech position. The physician decides to perform a cesarean delivery for the second baby. How would the deliveries be reported? d. 59618, 59612-51 c. 59510, 59409-51 Response Feedback: RATIONALE: Only one baby is delivered vaginally making 59400, 59409-51 is incorrect. Only one baby was delivered by cesarean section making 59510 incorrect. Because this is the patient’s first pregnancy, do not report codes 59618, 59612. Look in the CPT® Index for Cesarean Delivery/Routine Care 59510 and Vaginal Delivery/Delivery Only 59409. Modifier 51 is appended to indicate additional procedures during the same session. The code with the highest value is sequenced first. Verify codes in the numeric section. • Question 6 10 out of 10 points A pregnant patient presents to the ED with cramping and bleeding. On examination, the cervix is dilated and there are no retained products of conception. The physician documents an abortion at 10 weeks. What is the type of abortion? b. Spontaneous abortion b. Spontaneous abortion Response Feedback: Rationale: ICD-10-CM and CPT® recognize three types of abortions, spontaneous (also called a miscarriage), induced or therapeutic (TAB) caused by a deliberate procedure, or missed. A missed abortion occurs when the fetus dies but the products of conception are retained. • Question 7 10 out of 10 points A 68-year-old female presents with vaginal bleeding. It has been 5 years since her last period. Choose the code to describe her bleeding. d. N95.0 d. N95.0 Response Feedback: RATIONALE: This bleeding is after the end of the woman’s menses and is described as postmenopausal. Look in the ICD-10-CM Alphabetic Index for Bleeding/postmenopausal N95.0. Verify in the Tabular List. • Question 8 0 out of 10 points A woman with a long history of essential hypertension is managed throughout her pregnancy and delivers today. The hypertension has not resolved after the delivery. How is this coded? d. O10.03, I10 c. O10.03 Response Feedback: RATIONALE: It is important to assess if a condition existed prior to pregnancy, developed during, or due to the pregnancy in order to assign the correct code. In this case, the hypertension is pre-existing. Look in the ICD-10-CM Alphabetic Index for Hypertension/complicating/puerperium, pre-existing/pre-existing/essential O10.03. Puerperium is the time period immediately after the birth of the baby and up to six weeks following childbirth. • Question 9 10 out of 10 points The uterine adnexa refers to which two structures of the female reproductive system? d. Fallopian tubes and ovaries d. Fallopian tubes and ovaries Response Feedback: RATIONALE: The word adnexa means appendages. Uterine appendages are the tubes and ovaries. • Question 10 10 out of 10 points The two structures that make up the uterus are b. The cervix and uterine fundus b. The cervix and uterine fundus Response Feedback: RATIONALE: The uterine tubes, vulva and vagina are not part of the uterus. The uterus is made up of the cervix (cervix uteri) and the fundus (corpus uteri). Sunday, November 19, 2017 9:17:24 AM MST • Question 1 4 out of 4 points Patient with genital warts has cryotherapy of an extensive number of lesions on her mons pubis, labia and perineum. How is this procedure coded? b. 56515 b. 56515 Response Feedback: Rationale: The mons pubis and labia are part of the vulva. In the CPT® Index look for Destruction/Lesion/Vulva/Extensive and you are referred to 56515. The extensive code is reported due to the extensive number of lesions. Verify the code in the numeric section. • Question 2 4 out of 4 points A patient presents in her 15th week of pregnancy with cramping, cervix dilated to 2 cm and bulging amniotic sac. The physician confirms a threatened abortion and decides to manage the patient expectantly with monitoring. What is the ICD-10-CM code? a. O20.0, Z3A.15 a. O20.0, Z3A.15 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Abortion/threatened (spontaneous) O20.0. Chapter notes indicate to code the weeks of gestation. In the Alphabetic Index look for Pregnancy/weeks of gestation/15 weeks referring you to Z3A.15. Verify codes in the Tabular List. • Question 3 0 out of 4 points The patient presents with a recurrent infection of the Bartholin’s gland which has previously been treated with antibiotics and I&D. At this visit her gynecologist incises the cyst, draining the material from it and tacks the edges of the cyst open creating an open pouch to prevent recurrence. How is this procedure coded? d. 56420 a. 56440 Response Feedback: Rationale: Marsupialization is a procedure where a scalpel is used to cut an opening in the top of the abscess pocket. The leaflets created by this procedure are pulled away from the pocket and attached to the surrounding skin with stitches or glue. This creates an open pouch to help prevent recurrence of the abscess. Look in the CPT® Index look for Bartholin’s Gland/Cyst/Marsupialization or Marsupialization/Cyst/Bartholin’s Gland directing you to code 56440. Marsupialization of Bartholin’s gland cyst is reported with CPT® code 56440. • Question 4 4 out of 4 points What is a root word for vagina? a. Colp/o a. Colp/o Response Feedback: Rationale: Colp/o refers to the vagina. • Question 5 4 out of 4 points What does the abbreviation VBAC mean? d. Vaginal birth after cesarean d. Vaginal birth after cesarean Response Feedback: Rationale: In the CPT® codebook guidelines under the heading Delivery after Previous Cesarean Delivery, for codes 59610-59622, you will find the abbreviation VBAC. VBAC is the abbreviation for vaginal birth after cesarean although CPT® notes this as vaginal delivery after cesarean delivery. • Question 6 4 out of 4 points If a non-Medicare patient has an age and gender appropriate preventive medicine exam (i.e., a breast and pelvic exam) this is coded with the age appropriate Preventive Medicine codes from the E/M chapter of CPT®. If a Medicare patient has a breast and pelvic exam, how is this coded? b. G0101 b. G0101 Response Feedback: Rationales: Medicare Part B requires that for pelvic examination (including clinical breast examination), use HCPCS Level II code G0101 when ordered by a physician. This information can be found on the CMS website at this link: http://www.cms.gov/manuals/downloads/Pub06_PART_50.pdf, under the CHAPTER II - COVERAGE ISSUES APPENDIX, 50-20.1. In your HCPCS Level II Index look for Screening/cancer/cervical or vaginal and you are directed to code G0101. • Question 7 4 out of 4 points A pregnant patient presents to the hospital in active labor. The obstetrician providing her prenatal care is contacted to perform the delivery. The provider delivers twins vaginally. The obstetrician will also provide the postnatal care. What CPT® code(s) describe this procedure? d. 59400, 59409-51 d. 59400, 59409-51 Response Feedback: Rationale: The delivery is vaginal. Look in the CPT® Index for Vaginal Delivery directing you to codes 59400, 59610-59614. As the physician has provided the prenatal care and will provide the postpartum care, the vaginal delivery for twin A is the global service described by 59400. The delivery of twin B is coded with 59409 with modifier 51 appended indicating this is a multiple procedure. Prenatal and postpartum care applies to the total care of the patient and not to both deliveries. • Question 8 4 out of 4 points What does the abbreviation IVF mean? d. In vitro fertilization d. In vitro fertilization Response Feedback: Rationale: In the CPT® Index, look for IVF and you are directed to See Artificial Insemination; In Vitro Fertilization. IVF stands for in vitro fertilization. • Question 9 4 out of 4 points What ICD-10-CM category is used to report the weeks of gestation of pregnancy? d. Z3A d. Z3A Response Feedback: Rationale: When a code from Chapter 15 is reported, an additional code is reported to identify the specific week of the pregnancy. This is reported from category Z3A Weeks of gestation. • Question 10 4 out of 4 points Ultrasound indicates a 20-week fetus has a distended bladder and the decision is made to perform vesicocentesis. The procedure is successful and the bladder is emptied. What CPT® is code reported for this procedure? b. 59074 b. 59074 Response Feedback: Rationale: In the CPT® Index look for Fetal Procedure/Fluid Drainage directing you to 59074. Verify in the numeric section. • Question 11 0 out of 4 points What modifier is appropriate for a separately billable antenatal service during the global OB package period? b. 57 c. No modifier is needed Response Feedback: Rationale: An antenatal service is performed before the baby is delivered. According to the notes in the Maternity Care and Delivery subsection in the CPT® codebook “Antepartum care includes the initial prenatal history and physical examinations; recording of weight, blood pressures, fetal heart tones, routine chemical urinalysis, and monthly visits up to 28 weeks gestation; biweekly visits to 36 weeks gestation; and weekly visits until delivery.” • Question 12 4 out of 4 points If a physician obtains a Pap smear specimen from a non-Medicare patient and incurs the cost for it to be transferred to an outside laboratory. How is this coded? c. 99000 c. 99000 Response Feedback: Rationale: Look to the CPT® Index for Specimen Handling and you are directed to 99000, 99001. CPT® code 99000 is reported when the physician incurs cost for collection, handling and/or conveyance of a specimen for transfer from the office to a laboratory. This is a non-Medicare patient, the HCPCS Level II code Q0091 is only reported for a Medicare patient. • Question 13 4 out of 4 points A pregnant patient presents to the ED with bleeding, cramping, and concerns of loss of tissue and material per vagina. On examination, the physician discovers an open cervical os with no products of conception seen. He tells the patient she has had an abortion. What type of abortion has she had? c. Spontaneous c. Spontaneous Response Feedback: Rationale: There is no indication this was an induced abortion. A missed abortion does not occur with passage of material and tissue; it is silent, meaning that the body does not recognize the pregnancy loss or expel the pregnancy tissue. This case is considered a spontaneous abortion or miscarriage. • Question 14 0 out of 4 points What CPT® code is used to report 50% removal of the vulva and deep subcutaneous tissues? c. 56620 d. 56630 Response Feedback: Rationale: In the CPT® Index look for Vulvectomy/Radical, directing you to codes 56630, 56631, 56633-56640. Removal of 50% of the tissue is a partial vulvectomy and removal of deep subcutaneous tissue is radical. Read the definitions in CPT® codebook at the beginning of the section: Vulva, Perineum, and Introitus. • Question 15 4 out of 4 points Patient presents with no menses and positive pregnancy test but ultrasound finds no uterine contents. Embryo has implanted on left ovary and this is treated with laparoscopic oophorectomy. What are the CPT® and ICD-10-CM codes reported for this procedure? Do not code the ultrasound. c. 59151, O00.20 c. 59151, O00.20 Response Feedback: Rationale: When an embryo implants on the ovary, it is an ectopic (ovarian) pregnancy. In the CPT® Index look for Ectopic Pregnancy/Laparoscopy with Salpingectomy and/or Oophorectomy and you are referred to 59151. For the diagnosis, look in the ICD-10-CM Alphabetic Index for Pregnancy/ovarian and you are directed to O00.20. • Question 16 4 out of 4 points An 88 year-old widow with uterine prolapse and multiple comorbid conditions has been unsuccessful in the use of a pessary for treatment elects to receive colpocleisis (LeFort type) to prevent further prolapse and avoid more significant surgery like hysterectomy. The treatment is successful. What are the CPT® and ICD-10-CM codes reported for this procedure? d. 57120, N81.4 d. 57120, N81.4 Response Feedback: Rationale: This surgical procedure of a colpocleisis is performed to prevent uterine prolapse. In this procedure, the walls of the vagina are sewn together. This obliterates the vagina and prevents uterine prolapse. It is only performed in patients not sexually active. In the CPT® Index, look for Colpocleisis or LeFort Procedure/Vagina referring you to code 57120. The reason for the operation is uterine prolapse. In the ICD-10-CM Alphabetic Index look for Prolapse, prolapsed/uterus (with prolapse of vagina) referring you to code N81.4. Verify in the Tabular List. • Question 17 0 out of 4 points A 27 year-old woman’s regular obstetrician delivers her twins. The first is delivered vaginally but the second is delivered by cesarean delivery. Both are delivered without complications. Patient will return in two weeks for a postpartum visit. What is/are the CPT® code(s) reported for this service? c. 59400, 59514-51 b. 59510, 59409-51 Response Feedback: Rationale: Rationale: Two codes are reported for this twin delivery to indicate one delivery is cesarean and the other delivery is vaginal. First code the global package with the cesarean delivery to capture the highest reimbursement. It is listed in this order even though the vaginal delivery was performed first, followed by the cesarean delivery. Look in the CPT® Index for Cesarean Delivery/Routine care referring you to 59510. The caesarean delivery is coded first because the global package includes the appropriate postsurgical follow up reimbursement. Look in the CPT® Index for Vaginal Delivery/Delivery Only referring you to 59409. Appending modifier 51 to this procedure indicates multiple procedures performed in the same session. The global obstetrical package is reported when a physician from a solo practice or the same physician group practice provides the global routine obstetric care, which includes the antepartum care, delivery, and postpartum care. This scenario informs us the delivery is being performed by her obstetrician, meaning the she has been going to her obstetrician for check-ups during her pregnancy before delivery and will be returning for postpartum care. The Maternity Care and Delivery guidelines list the services included in the global service. • Question 18 4 out of 4 points A 56 year-old woman with biopsy-proven carcinoma of the vulva with metastasis to the lymph nodes has complete removal of the skin and deep subcutaneous tissues of the vulva in addition to removal of her inguinofemoral, iliac and pelvic lymph nodes bilaterally. The diagnosis of carcinoma of the vulva with 7 of the nodes also positive for carcinoma is confirmed on pathologic review. What are the CPT® and ICD-10-CM codes reported for this procedure? a. 56640-50, C51.9, C77.4, C77.5 a. 56640-50, C51.9, C77.4, C77.5 Response Feedback: Rationale: The patient has her vulva removed to treat malignancy (vulvectomy, radical complete). She also has removal of inguinofemoral, iliac and pelvic lymph nodes. In the CPT® Index, look for Vulvectomy/Radical/Complete/with Inguinofemoral, Iliac, and Pelvic Lymphadenectomy referring you code 56640. All areas removed are listed in the code description for code 56440. There is a parenthetical note under this code to report 56640 with modifier 50 for a bilateral procedure. This scenario needs two ICD-10-CM codes. The first one is to show the carcinoma of the vulva. Look in the ICD-10-CM Alphabetic Index for Carcinoma – see also Neoplasm, malignant by site. Go to the ICD-10-CM Table of Neoplasms and look for Neoplasm, neoplastic/vulva/Malignant Primary column referring you to C51.9. The second diagnosis code is for the metastasis of the cancer to the lymph nodes. Look in the Table of Neoplasms for Neoplasm, neoplastic/lymph, lymphatic channel NEC/gland (secondary)/inguina, inguinal/Malignant Secondary column, guiding you to code C77.4. Also look under gland (secondary) in the Malignant Secondary column for iliac C77.5 and pelvic C77.5. Verify all codes in the Tabular List. • Question 19 4 out of 4 points A woman with abdominal pain and bleeding has a diagnosis of multiple fibroid tumors and undergoes laparoscopic resection without hysterectomy. After the abdomen is entered and inspected it is found she has 5 separate intramural fibroid tumors to be removed. The fibroid tumors are successfully removed, with a total weight of 300 grams. Pathology confirms leiomyoma (myomas or fibroids). What are the CPT® and ICD-10-CM codes reported for this service? a. 58546, D25.1 a. 58546, D25.1 Response Feedback: Rationale: Surgical laparoscopy is performed to remove the five fibroid tumors weighing over 250 grams. Look in the CPT® Index for Laparoscopy/Removal/Leiomyomata referring you to 58545, 58546. 58546 is correct for 5 or more fibroid tumors. In the ICD-10-CM Alphabetic Index, look for Leiomyoma/uterus/intramural referring you to code D25.1. Verify this code in the Tabular List. • Question 20 4 out of 4 points A patient with a previous low transverse incision cesarean delivery is attempting VBAC (vaginal birth after cesarean), also known as TOLAC (trial of labor after cesarean) with her second child. During labor her uterus ruptured. She had an emergency cesarean section followed immediately by hysterectomy to remove her ruptured uterus. Mother and baby survived. The same obstetrician provided her antepartum and postpartum care. What are the CPT® and ICD-10-CM codes reported for this service? b. 59618, 59525, O71.1, O34.211, Z3A.00, Z37.0 b. 59618, 59525, O71.1, O34.211, Z3A.00, Z37.0 Response Feedback: Rationale: This patient has a previous history of caesarean delivery and is attempting to deliver her second child vaginally (VBAC). Due to her uterus rupturing, the planned vaginal delivery was changed to a caesarean delivery. Look in the CPT® Index for Cesarean Delivery/Previous Cesarean/Unsuccessful Attempted Vaginal Delivery/Routine Care referring you to code 59618. After the delivery a hysterectomy was performed. The procedure is located in the CPT® Index by looking for Cesarean Delivery/with hysterectomy referring you to 59525. Modifier 51 is not appended to this code, because it is an add-on code. The first-listed diagnosis will reflect the rupture of the uterus during labor which is the reason for the cesarean. Look in the ICD-10-CM Alphabetic Index for Rupture/uterus/during or after labor O71.1. Next look for Delivery/cesarean (for)/previous/cesarean delivery/classical (vertical) scar, O34.212. Notes at the beginning of Chapter 15 states to use an additional code from category Z3A to identify the weeks of gestation. The weeks of gestation are not provided. In the ICD-10-CM Alphabetic Index look for Pregnancy/weeks of gestation/not specified and you are referred to Z3A.00. The last code to report is the outcome of the delivery. In the Alphabetic Index look for Outcome of delivery/single NEC/live born, referring you to Z37.0. Verify the codes in the Tabular List. • Question 21 4 out of 4 points What is the code for ultrasound evaluation of a fetus and mother, usually performed early in pregnancy (first trimester), to confirm fetal age, set an anticipated delivery date, for qualitative assessment of amniotic fluid volume/gestational sac shape and examination of the maternal uterus and adnexa? a. 76801 a. 76801 Response Feedback: Rationale: The service performed in this question is an ultrasound to evaluate the fetus and mother in the first trimester. In the CPT® Index look for Ultrasound/Obstetrical/Pregnant Uterus referring you to 76801, 76802, 76805, 76810-76817. Code 76801 is correct to report the evaluation of both the fetus and the mother in her first trimester. This scenario does not qualify for a non-stress test; there is no monitoring of the fetal heart. • Question 22 4 out of 4 points A patient with severe adenomyosis has a vaginal hysterectomy with bilateral salpingo-oophorectomy. After the uterus is removed it is weighed at 300 grams. What is the CPT® code reported for this procedure? a. 58291 a. 58291 Response Feedback: Rationale: A vaginal hysterectomy code can be selected based on the weight of the uterus and additional procedures included with the hysterectomy. In the CPT® Index look for Hysterectomy/Vaginal/Removal Tubes/Ovaries directing you to codes 58262, 58263, 58291, 58292, 58552, 58554. A vaginal hysterectomy for a uterus greater than 250 grams is reported from code range 58290-58294. Further selection of removal of tubes and ovaries defines code 58291. • Question 23 0 out of 4 points A patient with a long history of endometriosis has an exploratory laparotomy for an enlarged right ovary seen on ultrasound with other possible masses on the uterus and in the peritoneum. Exploration reveals these masses to be endometriosis including a chocolate cyst (endometrioma) of the right ovary, right fallopian tube and peritoneum. The endometriomas are all small, less than 5 cm, and laser is used to ablate them, except the ovarian cyst, which is excised. During the procedure the patient also has a tubal ligation. What are the CPT® and ICD-10-CM codes reported for this service? a. 58662, 58600-51, N80.1, N80.2, N80.3, Z30.2 c. 49203, 58611, N80.1, N80.2, N80.3, Z30.2 Response Feedback: Rationale: The exploratory laparotomy is not a separately billable service because it is no longer just examination of the intraabdominal organs; it became a surgical procedure in which the endometriomas were destroyed by laser. Remember a surgical laparotomy always includes a diagnostic (exploratory) laparotomy. Look in the CPT® Index for Endometrioma/Abdomen/Destruction/Excision referring you to 49203-49205. 49203 is correct for destruction for 1 or more tumors with the largest less than 5 cm in diameter. The second procedure is a tubal ligation (female sterilization in which the fallopian tubes are sealed or severed). Look in the CPT® Index for Fallopian tube/Ligation referring you to 58600, 58611. Add-on code 58611 is correct to report because the tubal ligation was performed at the same time as another intra-abdominal surgery. Modifier 51 is not appended because 58611 is an add-on code. The endometriosis included the ovary and the right fallopian tube. Look in the ICD-10-CM Alphabetic Index for Endometriosis/ovary guiding you to code N80.1. Next look in the Alphabetic Index for Endometriosis/fallopian tube referring you to code N80.2. Then look for Endometriosis/peritoneal directing you to code N80.3. Reporting a diagnosis for the tubal ligation is found by looking in the Alphabetic Index for Encounter (with health service) (for)/sterilization guiding you to code Z30.2. Verify all codes in the Tabular List. • Question 24 4 out of 4 points A woman presents for hysterectomy after ECC (endocervical curettage) and EMB (endometrial biopsy) indicates endometrial cancer. Transabdominal approach (incision) is chosen for exposure of all structures possibly affected. The abdomen is thoroughly inspected with no gross disease outside the enlarged uterus but several lymph nodes are enlarged and the decision is made to perform a hysterectomy with bilateral removal of tubes and ovaries and bilateral pelvic lymphadenectomy with periaortic lymph node sampling. Specimens sent to pathology confirm endometrial cancer but find normal tissue in the lymph nodes. What are the CPT® and ICD-10-CM codes reported for this service? d. 58210, C54.1 d. 58210, C54.1 Response Feedback: Rationale: An open approach is performed to remove the uterus, cervix, tubes, ovaries and bilateral pelvic lymph nodes along with sampling (biopsy) the peri-aortic lymph nodes. In the CPT® Index look for Hysterectomy/Abdominal/Radical referring you to 58210. The key to choosing this code from the other choices is the removal of the pelvic lymph nodes and a biopsy of the peri-aortic lymph nodes (radical procedure) which is located in the description for code 58210. Because the lymph nodes were benign, the endometrial cancer is the only diagnosis to report. Look in the ICD-10-CM Table of Neoplasms for Neoplasm, neoplastic/endometrium/Malignant Primary column referring you to C54.1. Verify in the Tabular List. • Question 25 0 out of 4 points A pregnant patient presents to labor and delivery with the baby in a breech presentation. During the delivery the doctor attempts to turn the baby (version of the breech presentation) while it is still in the uterus. The baby turns but then immediately resumes his previous breech position. Can this service (the version of the breech) be billed? If so, what is the code? c. No, this procedure is included in the obstetrical global package a. Yes, because the doctor did the work, even though the outcome was unsuccessful. Report this procedure with code 59412 Response Feedback: Rationale: The physician can bill for this service separately. Look in the CPT® Index Version, Cephalic — see Cephalic Version. Look in the CPT® Index for Cephalic Version/of Fetus/External and you are referred to 459412. Verify in the numeric section. Sunday, November 19, 2017 9:17:49 AM MST • Question 1 0 out of 10 points What part of the brain is affected when one has a stroke and is unable to speak or write? b. Cerebellum d. Parietal lobe Response Feedback: Rationale: The parietal lobes are at the top of the brain. The right lobe processes visuo-spatial information, while the left lobe processes spoken and written information. • Question 2 10 out of 10 points What does it mean when a patient has a thymectomy performed by a sternal split approach? c. Excision of the thymus by cutting into the chest c. Excision of the thymus by cutting into the chest Response Feedback: Rationale: Thymectomy (partial or total) describes excision of the thymus. This may be achieved by a number of surgical approaches, including transcervical (via the neck), transthoracic or sternal split (via chest) • Question 3 10 out of 10 points Select the code for a patient diagnosed with thyrotoxicosis crisis with an overactive nodular goiter. c. E05.21 c. E05.21 Response Feedback: Rationale: The diagnosis is indexed under Thyrotoxicosis/with/goiter/nodular/with thyroid storm guiding you to code E05.21. Verification in tabular indicates E05.21 is correct code (thyroid crisis/storm). Verify code selection in the Tabular List. • Question 4 10 out of 10 points A 65-year-old patient with type 1 diabetes may need left lower leg amputation due to diabetic gangrene. Select the ICD-10-CM code(s) to report. a. E10.52 a. E10.52 Response Feedback: Rationale: Type 1 diabetes with diabetic gangrene is found in the ICD-10-CM Alphabetic Index under Diabetes, diabetic/Type 1/with gangrene, directing you to E10.52. There is no documentation that the patient has secondary diabetes so it would be inappropriate to code that type of diabetes for this scenario. Code E10.52 is a combination code so a separate code for the gangrene is not reported. Verify code selection in the Tabular List. • Question 5 10 out of 10 points A 35-year-old male has a left chronic subdural hematoma. He will undergo a left burr hole evacuation of the hematoma. What CPT® code is reported for this surgery? b. 61154 b. 61154 Response Feedback: Rationale: The keywords in this scenario are burr hole, evacuation, hematoma and subdural. All of those words are found in the code description of procedure code 61154. Look in the CPT Index for Burr Hole/for Drainage/Hematoma guiding you to codes 61154–61156. Look in the Nervous System section to select the correct code. • Question 6 10 out of 10 points A college student goes to the ER with symptoms of headache and high fever for the past two days. A Lumbar Puncture is performed and spinal fluid is sent to the lab to check for meningitis. What CPT® code is reported for this surgery? c. 62270 c. 62270 Response Feedback: Rationale: The patient is not having an injection or an aspiration of contents found in the nucleus pulposus, intervertebral disc, or paravertebral tissue. The procedure is a spinal puncture in the lumbar area to determine if the patient has meningitis. Look in the CPT Index for Spinal Tap/Lumbar guiding you to code 62270. Verify the code in the Nervous System section. • Question 7 10 out of 10 points A 59-year-old female with failed back syndrome has undergone a recent test dose of intrathecal narcotics with good pain response. She is brought to the operating room for preparation and insertion of Medtronic programmable pain pump and intrathecal catheter. What CPT® codes are reported for this surgery? d. 62362, 62350-51 d. 62362, 62350-51 Response Feedback: Rationale: The patient is having an insertion of a programmable pump and an intrathecal catheter implanted to infuse pain meds for pain management. An infusion of pain medications is not performed. Look in the CPT Index for Infusion Pump/Spinal Cord guiding you to codes 62361–62362. Look in the CPT Index for Catheterization/Spinal Cord guiding you to codes 62350–62351 for the second code. Look in the Nervous System section to select the correct code. • Question 8 10 out of 10 points A 6-week-old baby had a cerebrospinal fluid shunt placed two days ago. The shunt is not draining the excess CSF and the baby is returning to the OR for shunt removal and replacement by the same surgeon who placed the original shunt. What CPT® code is reported for this surgery? c. 62258-78 c. 62258-78 Response Feedback: Rationale: A complete removal of the cerebrospinal fluid shunt system with a replacement is performed. Look in the CPT® Index for Shunt/Brain/Removal guiding you to codes 62256–62258. Modifier 78 is the appropriate modifier to append for two reasons: (1) the patient returned to the operating room following the initial procedure during the postoperative period; (2) The same surgeon performed the initial procedure and the removal and replacement of the shunt. • Question 9 10 out of 10 points A neurosurgeon was called to the ER to examine a young child hit by a car. The neurosurgeon examines the patient with a diagnosis of a subdural hematoma and takes the child to the OR. Which modifier is appended to the Evaluation and Management service? c. 57 c. 57 Response Feedback: Rationale: Modifier 57 is the appropriate modifier to append to the Evaluation and Management Service since the evaluation and examination of the child’s condition led the surgeon to make a decision for surgery. This surgical procedure is a major procedure with a 90-day global period. Modifier 25 is only appended to minor procedures which have a 0–10-day global period. Modifiers 22 and 54 are only appended to procedure codes, not Evaluation and Management services. • Question 10 10 out of 10 points A 45-year-old female has carpal tunnel syndrome. A neuroplasty is performed on her left wrist. During the surgery the patient’s blood pressure starts dropping and the surgeon decides to stop the operation. How should the procedure be reported? b. 64721-53 b. 64721-53 Response Feedback: Rationale: Modifier 53 is the appropriate modifier to append when the surgeon elects to terminate a surgical procedure due to the patient’s blood pressure dropping which threatens the well-being of the patient. Sunday, November 19, 2017 9:18:11 AM MST • Question 1 4 out of 4 points What ICD-10-CM code is reported for Addisonian crisis? a. E27.2 a. E27.2 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Crisis/Addisonian which directs you to E27.2. Verify code selection in the Tabular List. • Question 2 4 out of 4 points What is a laminotomy? c. Partial excision of one or more lamina. c. Partial excision of one or more lamina. Response Feedback: Rationale: A laminotomy is partial excision of a vertebral lamina (placing a hole in the lamina). A laminectomy is complete excision of a lamina. • Question 3 4 out of 4 points What is a parathyroidectomy? a. Removal of glands on the posterior surface of the thyroid. a. Removal of glands on the posterior surface of the thyroid. Response Feedback: Rationale: The parathyroid glands are four glands embedded on the posterior surface of the thyroid. A parathyroidectomy is the removal of a parathyroid gland or glands. • Question 4 4 out of 4 points Migraines are reported from what category in ICD-10-CM? d. G43 d. G43 Response Feedback: Rationale: Migraines are reported with codes from category G43. These codes report if the migraine is with or without aura, intractable or not intractable, with or without status migrainosus. • Question 5 4 out of 4 points Looking in the CPT® manual the Nervous System is divided into what subheadings? c. Skull, Meninges, and Brain; Spine and Spinal Cord; Extracranial Nerves, Peripheral Nerves, and Autonomic Nervous System. c. Skull, Meninges, and Brain; Spine and Spinal Cord; Extracranial Nerves, Peripheral Nerves, and Autonomic Nervous System. Response Feedback: Rationale: CPT® divides the nervous system into three primary subheadings: 1. Skull, Meninges, and Brain (61000–62258) 2. Spine and Spinal Cord (62263–63746) 3. Extracranial Nerves, Peripheral Nerves, and Autonomic Nervous System (64400–64999) • Question 6 4 out of 4 points What CPT® code is reported for a subtotal thyroidectomy for malignancy, with removal of only a few selected lymph nodes? d. 60252 d. 60252 Response Feedback: Rationale: The removal of all of the lymph nodes of the neck during a thyroidectomy is considered a radical neck dissection. When limited removal of all of the lymph nodes of the neck is performed, it is reported with 60252. The thyroidectomy is performed due to the patient having a malignancy. In the CPT® Index look for Thyroidectomy/Total/for Malignancy/Limited Neck Dissection. • Question 7 4 out of 4 points How is Streptococcal A Meningitis reported in ICD-10-CM? c. Streptococcal meningitis is reported first; Streptococcal, group A, as the cause of diseases classified elsewhere is reported second. c. Streptococcal meningitis is reported first; Streptococcal, group A, as the cause of diseases classified elsewhere is reported second. Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Meningitis/streptococcal (acute) which directs the coder to G00.2. In the Tabular List, G00.2 has a note to use an additional code to further identify the organism. The organism is Streptococcus A. In the Alphabetic Index, look for Streptococcus, streptococcal/group/A, as cause of disease classified elsewhere which directs the coder to B95.0. • Question 8 4 out of 4 points A patient has a right thyroid lobectomy for a thyroid follicular lesion. An incision is made 2 cm above the sternal notch and carried through the platysma. The right thyroid was dissected free from the surrounding tissues. The isthmus was divided from the left thyroid lobe. The left thyroid lobe was explored revealing a single nodule. The right thyroid lobe was completely removed from the trachea and surrounding tissues. It was marked and sent off the table as a specimen. What CPT® code is reported? b. 60220 b. 60220 Response Feedback: Rationale: The patient had a unilateral thyroidectomy. Because only the right side is removed, it is a total unilateral (partial) thyroidectomy. In the CPT® Index look for Thyroidectomy/Partial and you are directed to code range 60210-60225. 60220 reports a unilateral total thyroid lobectomy with or without isthmusectomy. • Question 9 4 out of 4 points A patient with chronic lumbago is seen by the provider to have an epidural injection at the sacral level. What CPT® code is reported for this procedure? d. 62322 d. 62322 Response Feedback: Rationale: Documentation shows a single injection was given at the sacral level. Neither a catheter nor a device is documented as being used. In the CPT® Index look for Epidural/Injection or you can find the code in the CPT® Index by looking up Epidural/Administration/Drug. Single injection codes are selected based on the level of the spine injected. The lumbar sacral area is 62322. • Question 10 4 out of 4 points A patient has a programmable pump implanted for chemotherapy administration. She has a neoplasm of the spinal meninges. What CPT® and ICD-10-CM codes are reported? c. 62362, C70.1 c. 62362, C70.1 Response Feedback: Rationale: In the CPT® Index look for Insertion/Infusion Pump/Spinal Cord and you are directed to code range 62361-62362. This is a programmable pump making 62362 the correct code selection. In ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/spine, spinal (column)/meninges and select from the Malignant Primary column which directs you to C70.1. Verification in the Tabular List confirms code selection. • Question 11 4 out of 4 points A patient has a total thyroidectomy to remove thyroid cancer. Removal of all the lymph nodes along with the spinal accessory nerve, jugular vein and sternocleidomastoid muscles are performed to remove a malignant lymphatic chain. What CPT® and ICD-10-CM codes are reported? d. 60254, C73 d. 60254, C73 Response Feedback: Rationale: In the CPT® Index look for Thyroidectomy/Total/for Malignancy/Radical Neck Dissection and you are directed to 60254. A radical neck dissection includes removal of all lymph nodes. In the ICD-10-CM Alphabetic Index go to the Table of Neoplasms and look for Neoplasm, neoplastic/thyroid (gland) and selection from the Malignant Primary column directing you to C73. Verification in the Tabular List confirms code selection. • Question 12 0 out of 4 points A 50 year-old male is diagnosed with a tumor of the skull base just below the occipital tonsils. The neurosurgeon performs a transpetrosal approach to the posterior cranial fossa. He then performs an intradural removal of the tumor of the posterior cranial fossa at the base of the skull. Dural repair is done and the area is closed with Neurolon. What CPT® code(s) is/are reported? a. 61597, 61616-51 c. 61598, 61616-51 Response Feedback: Rationale: You are coding for both the approach and definitive procedures for the skull base surgery. In the CPT® Index look for Skull Base Surgery/Posterior Cranial Fossa/Transpetrosal Approach which directs you to 61598 and Skull Base Surgery/Posterior Cranial Fossa/Intradural which directs you to code 61616 which includes the repair. Modifier 51 is added to indicate the same surgeon performed more than one procedure. • Question 13 0 out of 4 points A patient with a status post (after or following) lumbar puncture headache receives an epidural blood patch. The patient’s venous blood is injected into the lumbar epidural space; this blood forms a clot sealing the leak of CSF from the lumbar puncture. What CPT® and ICD-10-CM codes are reported? b. 62282, G97.1 c. 62273, G97.1 Response Feedback: Rationale: In the CPT® Index look for Spinal Cord/Injection/Blood and you are directed to 62273. In ICD-10-CM Alphabetic Index, look for Headache/lumbar puncture and you are directed to G97.1. Verification in the Tabular List confirms code selection. • Question 14 4 out of 4 points A patient is receiving pain management treatment for chronic cervical pain caused by a motor vehicle accident. What ICD-10-CM code(s) and sequencing is/are reported? c. G89.21, M54.2 c. G89.21, M54.2 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Pain(s)/chronic/due to trauma and you are directed to G89.21. Cervical pain is found by looking in the Alphabetic Index for Pain(s)/neck NEC which directs you to M54.2. According to the ICD-10-CM guideline I.C.6.b.(b).(ii) when the treatment is for pain management, the chronic pain is listed first. • Question 15 4 out of 4 points What ICD-10-CM code is reported for Ataxia telangiectasia? b. G11.3 b. G11.3 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index, look for Ataxia/telangiectasia which directs you to code G11.3. Verification in the Tabular List confirms code selection. • Question 16 4 out of 4 points A 15 year-old has been taken to surgery for crushing his index and middle fingers and injuring his digital nerves. The provider located the damaged nerves in both fingers and sutures them to restore sensory function. What CPT® codes are reported? d. 64831, 64832 d. 64831, 64832 Response Feedback: Rationale: Look in the CPT® Index for Suture/Nerve or Repair/Nerve/Suture. 64831 is the correct code to report the digital nerve was repaired. 64832 is the correct secondary code because there was an additional digital nerve that needed repair. Modifier 51 is not appended to the secondary code because this code is an add-on code and add-on codes are modifier 51 exempt. • Question 17 4 out of 4 points A 36 year-old male suffered back pain after heavy lifting and was found to have bilateral disc herniation. The patient was placed prone and general anesthesia given. Incision was then made with a 10-blade knife and dissection was carried downward through the thick adipose tissue to the fascia in a subperiosteal plane. The paraspinous muscles were reflected off L5 and S1. A laminotomy was drilled with the Midas Tex AMB on the inferior end of L5. The thecal sac was retracted medially. The microscope was brought in, direct with microdissection there was a massive disk herniation on the right side underneath the nerve root as well as the left. The disc was incised with an 11-blade knife and was cleaned out with a series of straight and angled curettes and rongeurs. The disc was intertwined with the posterior longitudinal ligament. The space was cleaned out, the foramina were checked and no further compression was found on any of the neural elements. What CPT® codes are reported for this procedure? c. 63030-50, 69990 c. 63030-50, 69990 Response Feedback: Rationale: A laminotomy is also known as a hemilaminectomy. In the CPT® index look for Hemilaminectomy, and you are directed to code range 63020-63044. Code selection is based on the number of interspaces and the section of spine. This is the lumbar spine and only one interspace is treated making 63030 the correct code. The parenthetical instructions state to use modifier 50 for a bilateral procedure. This occurred on the left and right side so modifier 50 is appended. According to CPT®, 69990 is not inclusive to 63030 and is reported separately. According to the National Correct Coding Initiatives (NCCI), 69990 is inclusive and cannot be reported separately. For this note, we are following CPT® guidelines. We have included it on all choices to avoid confusion. • Question 18 4 out of 4 points Operative Report PROCEDURE: Left L3-L4 peri-articular paravertebral facet joint injection. PATIENT HISTORY: The patient is a 67 year-old woman referred by Dr. X for repeat diagnostic/therapeutic spinal injection procedure. She is about 1 1/2 years status post lumbar decompression for stenosis. Two weeks ago she underwent an interarticular left L4-L5 paravertebral facet joint injection. She had no relief of symptoms from that injection. TECHNIQUE: The patient was positioned prone and the skin was prepped and draped in the usual sterile fashion. The skin and underlying soft tissues were anesthetized with 3 cc of 1% lidocaine. Due to the advanced degenerative changes, the left L3-L4 paravertebral facet joint could not be distinctly visualized fluoroscopically, despite trying numerous angles. This was explained to the patient who wished to proceed with the injection. A 22-gauge 6-inch spinal needle was advanced toward the region of the left L3-L4 paravertebral facet joint under fluoroscopic guidance. Injection of 0.5 cc of Isovue 200 contrast showed the needle was not in an intravascular location. Intra-articular placement could not be confirmed and the injection was presumed to be peri-articular. 2 cc containing equal parts preservative free 2% Lidocaine plus Depo-Medrol (80 mg per ml) was injected. The patient reported injection of medication produced discomfort in the region of her usual left low back pain. Immediately following the procedure, upon standing up from the procedure table, she reported her pain was a little bit better. What CPT® code(s) is/are reported for this procedure? b. 64493 b. 64493 Response Feedback: Rationale: Nerve block injections are selected based on location. Code 64493 is described as a paravertebral facet joint of lumbar spine, single level. This code descriptor includes imaging guidance, and it is not reported separately. In the CPT® Index look for Injection/Paravertebral Facet Joint/Nerve/with image guidance. • Question 19 4 out of 4 points A patient recently experienced muscle atrophy and noticed she did not have pain when she cut herself on a piece of glass. The provider decides to obtain a needle biopsy of the spinal cord under ultrasound guidance in the outpatient setting. The biopsy results come back as syringomyelia. What CPT® and ICD-10-CM codes are reported for the biopsy procedure? c. 62269, 76942-26, G95.0 c. 62269, 76942-26, G95.0 Response Feedback: Rationale: In the CPT® Index look for Biopsy/Spinal Cord/Percutaneous and you are directed to code 62269. Instructional note under code 62269 indicates for radiological supervision and interpretation, see 76942, 77002, and 77012. Ultrasound guidance for needle placement, 76942, can be separately billed. Modifier 26 is appended for the professional services. In the ICD-10-CM Alphabetic Index look for Syringomyelia which directs you to code G95.0. Verification in the Tabular List confirms code selection. • Question 20 4 out of 4 points A 47 year-old male presents with chronic back pain and lower left leg radiculitis. A laminectomy is performed on the inferior end of L5. The microscope is used to perform microdissection. There was a large extradural cystic structure on the right side underneath the nerve root as well as the left. The entire intraspinal lesion was evacuated. What CPT® code(s) is/are reported for this procedure? a. 63267, 69990 a. 63267, 69990 Response Feedback: Rationale: In the CPT® Index look for Laminectomy/for Excision/Intraspinal Lesion/Other than Neoplasm and you are directed to code range 63265-63268 and 63270-63273. The code range is divided based on whether the lesion is extradural or intradural. In this case, it is extradural narrowing the range to 63265-63268 and 63270-63273. The range is further divided based on the section of the spine the lesion is located. Laminectomy with evacuation of an intraspinal lesion in the lumbar spine is described by code 63267. The use of a microscope is documented to perform microdissection. In the CPT® Index look for Operating Microscope which directs you to 69990. • Question 21 4 out of 4 points A 41 year-old female has carpal tunnel syndrome in her left hand. The patient underwent release of the carpal ligament with internal neurolysis. An incision was made directly over the carpal ligament through the skin to the carpal ligament. Under direct vision the carpal ligament was divided then internal neurolysis of the median nerve was performed using a magnifying loupes. What CPT® code is reported? b. 64721 b. 64721 Response Feedback: Rationale: In the CPT® Index look for Carpal Tunnel Syndrome/Decompression. 64721 is the correct code because it is the median nerve being stretched (neurolysis) to relieve the pain in the wrist for a person with carpal tunnel syndrome. • Question 22 4 out of 4 points PROCEDURES PERFORMED: 1. Bilateral facet joint injections, L4-L5 2. Bilateral facet joint injections, L5-S1. 3. Fluoroscopy. TECHNIQUE: The AP view was aligned with the proper tilt so that the end plates for the desired levels were perpendicular. The AP image showed the sacrum and the L5 spinous process. Manual palpation located the sacral hiatus. The 6 inch, 20 gauge needle with a slight volar bend was inserted using fluoroscopic into each facet joint under AP image. The bilateral L4-L5, and L5-S1 facet joints were injected in a systematic fashion from caudal to cranial. A sterile dressing was applied. The patient tolerated the procedure well with no complications and was transferred to recovery in good condition. b. 64493-50, 64494-50 b. 64493-50, 64494-50 Response Feedback: Rationale: The initial and one additional separate level lumbar facet joint injections were performed bilaterally, at two levels, so use modifier 50 on facet injection codes 64493, and 64494. Modifier 51 is not reported on add-on code 64494 because add-on codes are exempt from modifier 51. Fluoroscopy was utilized for all services and is bundled in codes 64490-64495 and not reported separately. • Question 23 4 out of 4 points A patient with McCune-Albright syndrome has a fibrous tissue neoplasm of the frontal bone (skull of cranium) extending into the orbit on the left. The surgeon excises the fibrous tissue neoplasm off the bone and down through the dura mater. Prophylactic decompression of the optic nerve was also performed. What CPT® and ICD-10-CM codes are reported? a. 61564, Q78.1 a. 61564, Q78.1 Response Feedback: Rationale: The frontal bone is part of the cranium. In the CPT® Index look for Excision/Cranial Bone/Tumor and you are directed to code range 61563-61564. Because decompression of the optic nerve was also performed, 61564 is the correct code. In the ICD-10-CM Alphabetic Index, look for McCune-Albright syndrome which directs you to Q78.1. Verification in the Tabular List confirms code selection. • Question 24 4 out of 4 points A patient who has a malignant neoplasm of the spinal meninges is receiving a programmable pump implantation for chemotherapy. The patient is placed in the prone position where the provider made a midline incision overlying the area of the spinal cord. The reservoir was placed in the subcutaneous tissues and attached to the previously placed catheter. Layered sutures were used to close the incision. The patient tolerated the procedure well and was released in good condition. What CPT® and ICD-10-CM codes are reported for this procedure? a. 62362, C70.1 a. 62362, C70.1 Response Feedback: Rationale: The procedure performed is implanting a programmable pump which allows the infusion of a medication (e.g., chemotherapy) for treatment. For insertion or implantation of the pump, in the CPT® Index look for Infusion Pump/Spinal Cord guiding you to codes 62361-62362. This is a programmable pump making 62362 the correct code selection. In ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/spine, spinal (column)/meninges and select from the Malignant Primary column which directs you to C70.1. Verification in the Tabular List confirms code selection. • Question 25 4 out of 4 points A 55 year-old man presents with uncontrolled tremors that have become quite severe and are now disabling. A trial of a deep brain stimulator electrode is recommended. The patient is placed in the head holder adapter for the frame. The scalp is incised exposing the skull using a perforator to make a single burr hole 2.5 cm from the midline at the level of the coronal suture exposing the dura and is punctured for access. Microelectrode recording (MER) and stimulation is done to target and reposition the electrodes to determine the best placement for the neurostimulator electrode. The neurostimulator electrode array is placed in the thalamus and fastened into position with radiographic image monitoring placement. The lead is coiled in a pocket under the galea, which is sutured closed, followed by skin closure. What CPT® code is reported? d. 61867 d. 61867 Response Feedback: Rationale: In the CPT® Index look for Neurostimulators/Implantation/Electrode Array/by Craniectomy directing you to 61863-61864, 61867-61868. Code 61867 is the correct code to report the neurostimulator electrode placed in the subcortical site (thalamus) by going through a burr hole using microelectrode recording. Sunday, November 19, 2017 9:18:32 AM MST • Question 1 10 out of 10 points What is a blepharoplasty? c. Surgical repair of the eyelid. c. Surgical repair of the eyelid. Response Feedback: RATIONALE: Blephar/o is a root word identifying the eyelid, and plasty indicates a surgical repair. • Question 2 10 out of 10 points Based on what you have learned so far, which of the following statements is true? d. All of the above. d. All of the above. Response Feedback: RATIONALE: All of the above are correct. The eye and ear both occur bilaterally, and their individual components occur bilaterally as well. Even within ophthalmology, you will find specialists in one area. For example, retinal specialists work with diseases/conditions of the retina, and an ophthalmologist may specialize in cataract surgery. The same is true for otorhinolaryngolgy: within the specialty, you will find subspecialists for hearing and vestibular disturbances. Because they are organs of communication, the eye and ear are considered to be the most important sense organs in the body. Physicians work very hard to safeguard and optimize their patients' sight and hearing. • Question 3 10 out of 10 points Topical antibiotics were prescribed today for Jack Jones, who presented with pink eye in both eyes. His four children are all being treated for the same condition by their pediatrician. What is the correct diagnosis code? b. H10.023 b. H10.023 Response Feedback: RATIONALE: Pink eye is a highly infectious form of mucopurulent conjunctivitis. This infection typically is accompanied by very bloodshot eyes and a heavy discharge. In the ICD-10-CM Alphabetic Index, look for Pink/eye - see Conjunctivitis, acute, mucopurulent. Look for Conjunctivitis/acute/mucopurulent H10.02-. In the Tabular List, the codes contain laterality and documentation indicates both eyes (bilateral) are affected. • Question 4 10 out of 10 points While dressing for work, the patient caught her earring in her shirt, and the force of her arm’s motion ripped the earring free, tearing her earlobe. She is seen in the emergency department to have the left earlobe repaired and to receive a tetanus shot. What diagnosis codes are assigned? d. S01.312A, Z23 d. S01.312A, Z23 Response Feedback: RATIONALE: This is an open wound of the earlobe. In the ICD-10-CM Alphabetic Index look for Laceration/ear (canal) (external), which directs you to S01.31-. In the Tabular List, the code selection indicates a 6th character for laterality and 7th character to indicate the episode of care is required. Complete code S01.312A is for laceration of the left ear, initial encounter. The patient received a vaccination for tetanus, which is reported with Z23. Look in the Alphabetic Index for Vaccination/encounter for directs you to Z23. • Question 5 10 out of 10 points Mable reports her hearing is not what it used to be. Indeed, everything that was discussed today during her visit has been repeated loudly, and within very close range. The physician scheduled a hearing testing with Acme Audiology. What is the diagnosis code? d. H91.90 d. H91.90 Response Feedback: RATIONALE: Without more specific information for the type of hearing loss, a nonspecific diagnosis is reported. In the ICD-10-CM Alphabetic Index, look for Loss/hearing (see also Deafness). Look for Deafness directing you to H91.9-. In the Tabular List, select code H91.90 Unspecified hearing loss, unspecified ear. No scientific study of the hearing loss was made, making R94.120 incorrect. • Question 6 0 out of 10 points What CPT® code is used to report surgery to remove an aqueous shunt from the patient’s eye? d. 67121 c. 67120 Response Feedback: RATIONALE: An aqueous shunt is implanted material in the extraocular posterior segment of the eye. In the CPT® Index, look for Eye/Removal/Implant/Posterior Segment referring you to 67120-67121. It can also be found by looking for Removal/Implant/Eye. • Question 7 10 out of 10 points A patient has an oversized and embedded dacryolith in the lacrimal sac, and a dacryocystoectomy is performed. What CPT® code(s) is/are reported for this procedure? c. 68520 c. 68520 Response Feedback: RATIONALE: In the CPT® Index, look for Dacryocystectomy referring you to 68520. The stone was embedded in the sac, which was removed. Only one code is used for removal of the stone and removal of the sac. The lacrimal gland is located near the eyebrow; the lacrimal sac is the upper dilated end of the lacrimal duct, aligned with the nostril. • Question 8 10 out of 10 points The patient is complaining of severe corneal pain and believes a wood chip entered his eye. He was working in his woodworking shop without goggles this morning. After placing two drops of proparacaine 0.5% in the right eye, I administered fluorescein and examined the cornea under ultraviolet light using a slit lamp. Seidel sign negative for penetrating injury. A small piece of wood was identified under a flap of lamellar cornea, and I was able to dislodge the wood and flush it from the eye. A single suture was placed to secure the flap. What CPT® code is appropriate for this procedure? b. 65275 b. 65275 Response Feedback: RATIONALE: The presence of the foreign body has no bearing on code selection. In the CPT® Index , see Cornea/Repair/Wound/Nonperforating 65275. Note the code reads with or without removal of foreign body. The key to code choice is the site of the injury, which is the cornea and it was a nonperforating injury (lamellar means partial thickness of the cornea). The topical anesthetic is bundled into the procedure, although the physician could bill separately for any IV sedation used or if a therapeutic contact lens was applied. • Question 9 10 out of 10 points A patient underwent mastoidotomy for ossicular chain reconstruction with tympanic membrane repair, atticotomy, and partial ossicular replacement prosthesis. What CPT® code is reported for this procedure? d. 69637 d. 69637 Response Feedback: RATIONALE: In the CPT® Index, look for Mastoidotomy. Code 69637 represents a mastoidotomy (including atticotomy and tympanic membrane repair) with ossicular chain reconstruction and partial ossicular replacement prosthesis. • Question 10 0 out of 10 points A patient with severe mixed hearing loss from chronic otitis media undergoes a round window implant with floating mass transducer. What CPT® code is reported for this procedure? d. 69710 a. 69799 Response Feedback: RATIONALE: In the CPT® Index, look for Ear/Unlisted Services and Procedures. The correct answer is A, for an unlisted procedure. Round window implants are a new technology not yet assigned CPT® a code. The word transducer should alert you to the hearing aid component of this procedure. There isn’t a new technology Category III code for this type of procedure so an unlisted code is the best choice. The round window is the barrier between the middle and inner ear, but it is still considered middle ear. Sunday, November 19, 2017 9:18:59 AM MST • Question 1 10 out of 10 points The incus bone is between the malleus and the stapes. In which part of the ear is the incus located? b. The middle ear b. The middle ear Response Feedback: RATIONALE: The three ossicles (malleus, incus and stapes) are found in the middle ear. When sound travels by air into the external auditory canal, it causes the tympanic membrane to vibrate. The sound is then transferred from the membrane to the tiny ossicles. From the stapes, the vibration is transferred to the oval window, which causes the round window to move and vibrate the endolymph of the cochlea duct. This causes the fine hairs in the organ of Corti to transmit impulses to the auditory nerve to the brain. From there, the signal is transmitted through the cochlear nerve. • Question 2 10 out of 10 points What is a blepharoplasty? c. Surgical repair of the eyelid. c. Surgical repair of the eyelid. Response Feedback: RATIONALE: Blephar/o is a root word identifying the eyelid, and plasty indicates a surgical repair. • Question 3 10 out of 10 points The pathology report comes back and the tumor is a malignant acoustic schwannoma. What is the correct diagnosis code? c. C72.40 c. C72.40 Response Feedback: RATIONALE: In the ICD-10-CM Alphabetic Index look for Neuroma/acoustic (nerve) D33.3. Although an acoustic neuroma is indexed to D33.3, the question indicates malignant which changes the way the diagnosis is reported. A note at the beginning of the Table of Neoplasms discusses classifications in the columns of the table, and advises, “the guidance in the index can be overridden if one of the descriptors is present.” Because the pathologist stated this particular acoustic neuroma is malignant, the word malignant overrides the index entry. Look in the Table of Neoplasms for Neoplasm, neoplastic/acoustic nerve/Malignant Primary which directs you to C72.4-. Verify in the Tabular List and code C72.40 is reported because the laterality is not addressed. It’s very important to study and understand the information provided in the guidelines and notes within the codebook. Be willing to look beyond the codes for the answers because the answers may be in the instructional notes and guidelines. • Question 4 0 out of 10 points The patient has been compliant with his Xalatan eye drops and his intraocular pressure (IOP) is now within normal limits at 20 mm Hg. The glaucoma seems to be in good control. He will continue the current regime and return for a follow-up exam in six months. What diagnosis code is reported? c. Z86.69 a. H40.9 Response Feedback: RATIONALE: There is not a lot of information to work with and H40.9 Unspecified glaucoma is the appropriate choice. In the ICD-10-CM Alphabetic Index, look for Glaucoma and the default code is H40.9. In a medical office, you would have access to the entire patient record and to the physician to find out more about the type of glaucoma. The important thing to remember is the patient still has glaucoma, despite the normal (WNL is within normal limits) IOP (intraocular pressure). Code Z86.69 is inappropriate because it reports a history of a resolved condition. • Question 5 10 out of 10 points The patient underwent an enucleation for retinal cancer and is here today with right orbital cellulitis, a foreign body response to the temporary implant placed following the surgery. The implant was removed, and the patient was admitted for observation and IV antibiotics. Select the correct diagnosis codes. a. T85.79XA, H05.011, Z85.840 a. T85.79XA, H05.011, Z85.840 Response Feedback: RATIONALE: In the ICD-10-CM Alphabetic Index, look for Complication/eye/implant (prosthetic)/infection and inflammation directing you to T85.79-. In the Tabular List, code T85.79- requires a 7th character. Based on active treatment for the condition this would support A, initial encounter. Because T85.79 is a five character code the place holder X is needed to maintain the 7th character position. Subcategory code T85.7 states to "Use additional code to identify specified infections". There is no documentation of the infective agent. Orbital cellulitis is indexed under Cellulitis/orbit, orbital H05.01-. In the Tabular List, the 6th character 1 is for the right side. The implant is the result of the patient’s previous cancer indicated with Z85.840. This is found under History/personal (of)/malignant neoplasm (of)/eye Z85.840. This is not a family history of cancer of the eye, Z80.8. • Question 6 10 out of 10 points The ophthalmologist performs a review of history, external exam, ophthalmoscopy, biomicroscopy and tonometry on an established patient with a new cataract. What CPT® code is reported for this procedure? c. 92012 c. 92012 Response Feedback: RATIONALE: In the CPT® Index, look for Ophthalmology, Diagnostic/Eye Exam/Established Patient referring you to 92012-92014. A comprehensive exam includes a biomicroscopy and tonometery. Code 92002 is reported for a new patient and 92012 for an existing patient. This service is for an existing patient, making 92012 the correct code. Documentation does not support E/M service 99212. • Question 7 10 out of 10 points Today we excised bilateral recurrent pterygiums under topical anesthetic. The conjunctival incisions were repaired simply. What CPT® code is reported for this procedure? a. 65420-50 a. 65420-50 Response Feedback: RATIONALE: In the CPT® Index, see Pterygium/Excision 65420. A pterygium is an overgrowth of conjunctiva forming in the nasal aspect of the eye and growing outward toward the cornea. Excision of a pterygium is reported separately from other conjunctival disorders, with codes 65420 and 65426. Because this was a simple repair without a graft, 65420 is the correct code. Modifier 50 indicates a bilateral procedure was performed. • Question 8 10 out of 10 points A patient has an oversized and embedded dacryolith in the lacrimal sac, and a dacryocystoectomy is performed. What CPT® code(s) is/are reported for this procedure? c. 68520 c. 68520 Response Feedback: RATIONALE: In the CPT® Index, look for Dacryocystectomy referring you to 68520. The stone was embedded in the sac, which was removed. Only one code is used for removal of the stone and removal of the sac. The lacrimal gland is located near the eyebrow; the lacrimal sac is the upper dilated end of the lacrimal duct, aligned with the nostril. • Question 9 10 out of 10 points A patient underwent mastoidotomy for ossicular chain reconstruction with tympanic membrane repair, atticotomy, and partial ossicular replacement prosthesis. What CPT® code is reported for this procedure? d. 69637 d. 69637 Response Feedback: RATIONALE: In the CPT® Index, look for Mastoidotomy. Code 69637 represents a mastoidotomy (including atticotomy and tympanic membrane repair) with ossicular chain reconstruction and partial ossicular replacement prosthesis. • Question 10 10 out of 10 points The patient is complaining of severe corneal pain and believes a wood chip entered his eye. He was working in his woodworking shop without goggles this morning. After placing two drops of proparacaine 0.5% in the right eye, I administered fluorescein and examined the cornea under ultraviolet light using a slit lamp. Seidel sign negative for penetrating injury. A small piece of wood was identified under a flap of lamellar cornea, and I was able to dislodge the wood and flush it from the eye. A single suture was placed to secure the flap. What CPT® code is appropriate for this procedure? b. 65275 b. 65275 Response Feedback: RATIONALE: The presence of the foreign body has no bearing on code selection. In the CPT® Index , see Cornea/Repair/Wound/Nonperforating 65275. Note the code reads with or without removal of foreign body. The key to code choice is the site of the injury, which is the cornea and it was a nonperforating injury (lamellar means partial thickness of the cornea). The topical anesthetic is bundled into the procedure, although the physician could bill separately for any IV sedation used or if a therapeutic contact lens was applied. Sunday, November 19, 2017 9:19:09 AM MST • Question 1 4 out of 4 points What does IOL stand for? c. Intraocular lens c. Intraocular lens Response Feedback: Rationale: IOL stands for intraocular lens. • Question 2 4 out of 4 points What is the abbreviation for EACH EYE? b. O.U. b. O.U. Response Feedback: Rationale: O. U. stands for each eye or both eyes. O.D. stands for the right eye. O.S. stands for the left eye. • Question 3 4 out of 4 points What ICD-10-CM code is reported for mild nonproliferative diabetic retinopathy with macular edema? b. E11.3219 b. E11.3219 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Diabetes/type 2/with/retinopathy/nonproliferative/mild/with macular edema and you are directed to E11.321-. The Category E11.- indicates the type of diabetes. Since the type is not indicated, the default is type 2 per ICD-10-CM guideline I.C.4.a.1. Verify code selection in the Tabular List. The code requires a 7th character to identify the eye involved. Because the laterality of the eye is not indicated in the question, use the 7th character 9 for unspecified eye. • Question 4 4 out of 4 points A surgeon performed a cataract extraction with an intraocular lens implant on the right eye of a Medicare patient. What modifier(s) would be reported? c. RT c. RT Response Feedback: Rationale: Modifiers RT and LT are used to identify procedures performed on paired organs such eyes, ears, breasts (excluding skin) or on sides of the body. • Question 5 4 out of 4 points Which option best describes what is being done during strabismus surgery? a. Corrects the muscle misalignment. a. Corrects the muscle misalignment. Response Feedback: Rationale: Strabismus surgery is surgery on the extraocular muscles to correct the misalignment of the eyes. • Question 6 4 out of 4 points A patient has heavy skin and muscle (myogenic) that is drooping down and blocking his vision due to ptosis of upper muscular eyelid disorder. The provider performed a bilateral upper blepharoplasty. What ICD-10-CM code(s) is (are) reported? c. H02.423 c. H02.423 Response Feedback: Rationale: Drooping (ptosis) of the upper eyelid is due to a muscle disorder (myogenic). In the ICD-10-CM Alphabetical Index look for Ptosis/eyelid which states see Blepharoptosis. Look for Blepharoptosis/myogenic and you are directed to H02.42-. Tabular List indicates 6th character is needed to indicate laterality. 6th character of 3 is for bilateral. Only one code is reported for both eyelids, not two separate codes. • Question 7 4 out of 4 points A 12 year-old male patient has an abscess located at the external auditory meatus. The ENT incises the abscess and packs it to absorb the drainage. What CPT® code is reported? d. 69020 d. 69020 Response Feedback: Rationale: The external auditory meatus is also referred to as the external auditory canal which starts from the opening of the ear to the eardrum. If you look in the CPT® Index under Ear Canal it refers you to See Auditory Canal. Look up Auditory Canal/External/Abscess/Incision and Drainage which guides you to codes 69000, 69005 and 69020. Verify the correct code in the numeric section. 69020 is the correct code for an abscess of the auditory canal. The other codes refer only to the external ear. • Question 8 4 out of 4 points A patient with right and left prominent ears presents for an otoplasty. What CPT® and ICD-10-CM codes are reported? a. 69300-50, Q17.5 a. 69300-50, Q17.5 Response Feedback: Rationale: In the CPT® Index look for Otoplasty and you are directed to 69300. The parenthetical instruction below 69300 states to use modifier 50 to report a bilateral procedure. In the ICD-10-CM Alphabetical Index look for Prominence, prominent/auricle (congenital) (ear) and you are directed to Q17.5. • Question 9 4 out of 4 points Patient had an abscess in the external auditory canal which was incised and drained in the office. What CPT® code is reported? c. 69020 c. 69020 Response Feedback: Rationale: In the CPT® Index, look for Abscess/Tissue/Auditory Canal, External/Incision and Drainage which directs you to 69020. Verify in the numeric section that code 69020 is the appropriate code for drainage of an abscess located in the external auditory canal of the ear. For this procedure, the provider makes an incision in the skin and drains the external auditory canal abscess. • Question 10 4 out of 4 points A patient with a cyst like mass on his left external auditory canal was visualized under the microscope and a microcup forceps was used to obtain a biopsy of tissue along the posterior superior canal wall. What CPT® code is reported? b. 69105-LT b. 69105-LT Response Feedback: Rationale: In the CPT® Index look for Auditory Canal/External/Biopsy. Verify in the CPT® numeric section. Code 69105 with modifier LT is correct since the biopsy was taken from the left ear in the auditory canal. • Question 11 4 out of 4 points The provider makes an incision in the patient's left tympanic membrane in order to inflate eustachian tubes and aspirate fluid in a patient with acute eustachian salpingitis. The procedure is completed without anesthesia. What CPT® and ICD-10-CM codes are reported? c. 69420, H68.012 c. 69420, H68.012 Response Feedback: Rationale: In the CPT® Index look for Myringotomy and you are directed to 69420-69421. Verify the code in the numeric section. In the ICD-10-CM Alphabetical Index, look for Salpingitis/eustachian (tube)/acute and you are directed to H68.01-. Verification in the Tabular List indicates a 5th character is needed for laterality. 5th character of 2 for the left ear. • Question 12 4 out of 4 points What CPT® code(s) is/are reported for the placement of two adjustable sutures during strabismus surgery involving the horizontal muscles? d. 67312, 67335 d. 67312, 67335 Response Feedback: Rationale: Code 67312 represents strabismus surgery on two (2) horizontal muscles. In the CPT® Index look for Strabismus/Repair/Two Horizontal Muscles. In the numeric section below code 67316, there is a parenthetical note with instructions to use code 67335 in addition to codes 67311-67334 when adjustable sutures are used for primary procedure reflecting number of muscles operated on. Code 67335 is an add-on code and exempt from multiple procedures modifier 51. This is located in the CPT® Index by looking for Strabismus/Repair/Adjustable Sutures. • Question 13 4 out of 4 points A patient had another recession strabismus procedure of the lateral rectus muscle. This muscle had previously been recessed during an operative session six months ago which resulted in scarring of the extraocular muscle. What CPT® code(s) is/are reported? c. 67311, 67332 c. 67311, 67332 Response Feedback: Rationale: In the CPT® Index look for Strabismus/Repair/One Horizontal Muscle (the lateral rectus muscle is a horizontal muscle). You are directed to 67311. Strabismus surgery add-on code 67332 is used to indicate the procedure is performed on a patient with scarring of the extraocular muscles. The parenthetical note for this code states to use 67332 in conjunction with 67311-67318. • Question 14 4 out of 4 points A patient is diagnosed with nuclear sclerotic cataract, right eye. She is taken to the operating room and a phacoemulsification with intraocular lens, right eye is performed. What code(s) is/are reported? a. 66984-RT a. 66984-RT Response Feedback: Rationale: In the CPT® Index look for Phacoemulsification/Removal/Extracapsular Cataract and you are directed to 66982 and 66984. Verify these codes in the numeric section. Code 66982 is for a complex procedure. There is nothing in the note indicating this is a complex procedure. The correct code is 66984 which includes the insertion of the intraocular lens. Modifier RT is used to indicate it is performed on the right eye. • Question 15 4 out of 4 points A patient with aphakia and anisometropia in the right eye undergoes surgery to implant a lens. An incision is made in the corneal-scleral juncture and a scleral tunnel is made. A partial vitrectomy is performed and the provider guides the intraocular implant into the eye pulling it into position by Prolene sutures. What CPT® code is reported? b. 66985-RT b. 66985-RT Response Feedback: Rationale: Code 66985 is the correct code since the insertion of lens is for aphakia (not associated with cataract). In the CPT® Index look for Intraocular Lens/Insertion/Not Associated with Concurrent Cataract Removal. • Question 16 0 out of 4 points A 26 year-old female with a one-year history of a left tympanic membrane perforation has consented to have it repaired. A postauricular incision was made under general anesthesia. Dissection was carried down to the temporalis fascia and a 3 x 3 cm segment of fascia was harvested and satisfactorily desiccated. The tympanic membrane was excised. Using a high speed drill a canaloplasty was performed until the entire annulus could be seen. The ossicular chain was examined, it was found to be freely mobile. The previously harvested skin was trimmed and placed in the anterior canal angle with a slight overlapping over the temporalis fascia. Packing is placed in the ear canal, external incisions are closed, and dressings are applied. What CPT® code is reported? a. 69641-LT c. 69631-LT Response Feedback: Rationale: In the CPT® Index look for Tympanoplasty/without Mastoidectomy. You are referred to 69631. Review the code in the numeric section to verify accuracy. This is the correct code with LT modifier because the repair of the left ear is performed (tympanoplasty) with a canaloplasty, without an ossicular chain replacement or mastoidectomy (removal of a portion of the mastoid of the posterior temporal bone). • Question 17 4 out of 4 points A provider uses cryotherapy for removal trichiasis of the right upper eyelid. What CPT® and ICD-10-CM codes are reported? c. 67825, H02.051 c. 67825, H02.051 Response Feedback: Rationale: In the CPT® Index, look for Trichiasis/Repair/Epilation, by Other than Forceps. Verify this code in the numeric section. Code 67825 describes the correction of trichiasis by other than forceps, for example cryotherapy. In the ICD-10-CM Alphabetic Index look for Trichiasis (eyelid)/right/upper directs you to code H02.051 and is verified in the Tabular List as Trichiasis without mention of entropion. • Question 18 4 out of 4 points A 60 year-old female with uncontrolled intraocular pressure and early cataracts is coming in for laser trabeculoplasty. This is her first treatment application. She will be examined over the next three months to ensure the normal inflammations subside. What CPT® code is reported? d. 65855 d. 65855 Response Feedback: Rationale: In the CPT® Index look for Trabeculoplasty/by Laser Surgery directing you to 65855. Verify this in the numeric section. Code 65855 is the correct code since trabeculoplasty by laser surgery was performed on the patient. • Question 19 4 out of 4 points A 65 year-old male with a history of chronic glaucoma has progressive optic nerve damage and elevated intraocular pressure. A clear corneal incision is made and viscoelastic material is injected into the anterior chamber over the lens to increase and maintain anterior chamber depth. The endoscope is inserted through the temporal incision to view the nasal ciliary processes, which is coagulated with the endpoint of shrinkage and whitening. The endoscope is moved in an arc, allowing treatment of the processes over an arc of 180° and a second corneal incision is made 90° away and 180° of ciliary processes are destroyed with laser therapy. The surgeon has completed coagulation of 270° of angle. The eye is reformed with balanced salt solution. Wounds are checked for leakage and sutures are placed to seal the wound. What CPT® code is reported? d. 66711 d. 66711 Response Feedback: Rationale: In the CPT® Index look for Ciliary Body/Destruction/Cyclophotocoagulation 66710, 66711. Code 66711 is the correct code because using an endoscopic approach, ciliary processes were coagulated and were destroyed by laser therapy. • Question 20 4 out of 4 points A 53 year-old woman with scarring of the right cornea has significant corneal thinning with a high risk of perforation and underwent reconstruction of the ocular surface. The eye is incised and an operating microscope is used with sponges and forceps to debride necrotic corneal epithelium. Preserved human amniotic membrane is first removed from the storage medium and transplanted by trimming the membrane to fit the thinning area of the cornea then sutured. This process was repeated three times until the area of thinning is flush with surrounding normal thickness cornea. All of the knots are buried and a bandage contact lens is placed with topical antibiotic steroid ointment. What CPT® code is reported? a. 65780 a. 65780 Response Feedback: Rationale: In the CPT® Index look up Transplantation/Eye/Amniotic Membrane. You are referred to 65778-65780. Verify in the numeric section. Code 65780 is the correct code because the amniotic membrane transplantation is for an ocular surface reconstruction for corneal defects of scarring and perforation. • Question 21 0 out of 4 points The ENT surgeon performs an anterior skull base LeFort I osteotomy approach for the intradural removal of a meningioma by a neurosurgeon. What CPT® code is reported by the ENT surgeon? c. 61586-62 b. 61586 Response Feedback: Rationale: In the CPT® Index look for Skull Base Surgery/Anterior Cranial Fossa/LeFort I Osteotomy Approach directing you to 61586. The only portion of the surgery that the ENT provided was the anterior skull base approach. The next to last paragraph in the guidelines for surgery of the skull base instructs that each surgeon reports the code for only his portion. Since each procedure is separate, modifier 62 Two Surgeons is not needed. Modifier 62, as explained in the CPT® appendix A, is to be used when two surgeons are working together to perform a single procedure. Skull base surgery has been divided so that each part of the procedure is reported with its own code. • Question 22 4 out of 4 points A patient presents to the emergency room with a severely damaged eye. The injury was sustained when the patient was a passenger in a multi-car accident on the public highway. The patient sustained a large open lacerated wound to the left eye. The posterior chamber was ruptured and significant vitreous and some intraocular tissue was lost. The eyeball was not repairable and was removed, en masse. A permanent implant was inserted but not attached to the extraocular muscles. The patient was released with an occlusive eye patch. What CPT® and ICD-10-CM codes are reported? c. 65103-LT, S05.22XA, V49.59XA, Y92.411 c. 65103-LT, S05.22XA, V49.59XA, Y92.411 Response Feedback: Rationale: Enucleation is the removal of the eye. At the time of surgery, an implant was inserted and extraocular muscles were not attached to it. In the CPT® Index look for Enucleation/Eye which gives codes 65101, 65103, 65105. Code 65103 best describes this procedure. The LT modifier is appended to indicate that this was the left eye. In the ICD-10-CM Alphabetical Index look for Laceration/eye (ball)/with prolapse or loss of intraocular tissue directing you to S05.2-. Tabular List indicates that seven characters are reported to complete the code. The 5th character 2 is reported to indicate left eye. X is used as placeholder for the 6th character position. The 7th character is A to report initial encounter for the patient receiving active treatment in the ED. Documentation does not provide sufficient details of the multi-car accident to specify whether the other cars were in motion and if a collision occurred with other objects/persons. Look in the ICD-10-CM External Cause of Injuries Index for Accident/transport/car occupant/passenger/collision (with)/motor vehicle NOS (traffic)/specified type NEC (traffic) V49.59-. The 6th character X is used as a placeholder and 7th character A for initial encounter in the ED. Look for Place of occurrence/highway (interstate) directing you to Y92.411. • Question 23 4 out of 4 points A patient with mixed conductive and sensorineural hearing loss in the right ear has tried multiple medical therapies without recovery of her hearing. Patient has consented to have an electromagnetic bone conduction hearing device implanted. What CPT® and ICD-10-CM codes are reported? b. 69710-RT, H90.71 b. 69710-RT, H90.71 Response Feedback: Rationale: In the CPT® Index look for Hearing Aid/Implants/Bone Conduction/Implantation. You are referred to 69710. Review the code to verify accuracy. In the ICD-10-CM Alphabetical Index look for Loss (of)/hearing which states see also Deafness. Look for Deafness/mixed conductive and sensorineural/unilateral. You are referred to H90.7-. Review the code in the Tabular List to verify accuracy and 5th character 1 is for right ear. • Question 24 0 out of 4 points Operative Report PREOPERATIVE DIAGNOSIS: Prolapsed vitreous in anterior chamber with corneal edema POSTOPERATIVE DIAGNOSIS Same OPERATION PERFORMED Anterior vitrectomy The patient is a 72 year-old woman who approximately 10 months ago underwent cataract surgery with a YAG laser capsulotomy, developed corneal edema and required a corneal transplant. The patient has done well. Over the last few weeks, she developed posterior vitreous detachment with vitreous prolapse to the opening in the posterior capsule with vitreous into the anterior chamber with corneal touch and adhesion to the graft host junction and early corneal edema. The patient is admitted for anterior vitrectomy. PROCEDURE: The patient was prepped, and draped in the usual manner after first undergoing retrobulbar anesthetic. A lid speculum was inserted. An incision was made at approximately the 10 o’clock meridian 3 mm in length, 2 mm posterior to the limbus, and grooved forward into clear cornea with a 3.2 mm anterior chamber. An anterior vitrectomy was carried out, placing a visco-elastic substance in the anterior chamber to maintain it. A Sinskey hook was used to sweep vitreous away from the corneal wound and this was removed with the disposable vitrectomy instrument. The patient’s pupil is noted to be round. There was no vitreous to the wound. The wound self-sealed without aqueous leak. Cautery was used to close the conjunctiva. Subconjunctival Decadron and Gentamicin was given. The patient tolerated the procedure well and was discharged to the recovery room in good condition. What CPT® code(s) is/are reported? a. 67005 c. 67010 Response Feedback: Rationale: In the CPT® Index look for Vitrectomy/Anterior Approach/Subtotal. This was a subtotal removal using a mechanical tool to sweep the vitreous away. Subtotal using a mechanical tool is reported with 67010. • Question 25 4 out of 4 points The surgeon performed an insertion of an intraocular lens prosthesis. Treatment plan was established and discussed with the patient six weeks earlier when the cataract was removed (by the same surgeon). What CPT® code is reported? b. 66985-58 b. 66985-58 Response Feedback: Rationale: In the CPT® Index look for Insertion/Intraocular Lens/Manual or Mechanical Technique/Not Associated with Concurrent Cataract Removal and directs you to code 66985. The procedure was planned because it was decided to perform this procedure with the patient before the cataract removal was performed six weeks earlier. This planned procedure indicates the need for modifier 58 Staged or related procedure or service by the same physician during the postoperative period. Sunday, November 19, 2017 9:20:28 AM MST • Question 1 10 out of 10 points Using your CPT® Index, look for anesthesia for a diagnostic shoulder arthroscopy. Which of the following is the correct anesthesia code? a. 01622 a. 01622 Response Feedback: RATIONALE: There is not a listing for Anesthesia/Diagnostic Arthroscopy in CPT® Index. Look for Anesthesia/Arthroscopic Procedures/Shoulder or Anesthesia/Shoulder. Both provide a range of code choices. Code 01622 identifies anesthesia for a diagnostic arthroscopic procedure of the shoulder joint. • Question 2 10 out of 10 points Using the CPT® Index, look for anesthesia for a diagnostic thoracoscopy. Which of the following is the correct anesthesia code? a. 00528 a. 00528 Response Feedback: RATIONALE: Look in the CPT® Index for Anesthesia/Thoracoscopy. All of these codes are related to thoracoscopy. Code 00528 describes a diagnostic procedure not using 1 lung ventilation utilization. • Question 3 10 out of 10 points A patient is scheduled for monitored anesthesia care (MAC) to remove an eyelid cyst. Normally the surgeon provides moderate sedation for the removal; however, this patient has a history of failed moderate sedation. Select the correct diagnosis code(s). c. H02.829, Z92.83 c. H02.829, Z92.83 Response Feedback: RATIONALE: The reason for the anesthesiologist’s involvement for the monitored anesthesia care (MAC) in the surgery is the patient’s history of failed moderate sedation. The eye cyst is first-listed as it is the medical necessity for the surgery and Z92.83 is an additional diagnosis to explain the need for anesthesia care. In the ICD-10-CM Alphabetic Index, look for Cyst/eyelid (sebaceous) directing you to H02.829. Next, look in the Alphabetic Index for History/personal (of)/failed conscious sedation directing you to Z92.83. Verify code selection in the Tabular List. • Question 4 0 out of 10 points Using your ICD-10-CM Alphabetic Index, look for the diagnosis code for a patient with a preoperative diagnosis of abdominal pain, right lower quadrant and a postoperative diagnosis of uterine fibroids. Which of the following is the correct diagnosis code? c. D26.9 d. D25.9 Response Feedback: RATIONALE: The preoperative diagnosis is disregarded because a more definitive diagnosis is determined following surgery. Look in the ICD-10-CM Alphabetic Index for Fibroid/uterus D25.9. Verify code selection in the Tabular List. • Question 5 10 out of 10 points Which of the following physical status modifiers best describes a normal health patient who is undergoing anesthesia? d. P1 d. P1 Response Feedback: RATIONALE: A normal healthy patient is reported with physical status modifier P1. No additional value is recognized. • Question 6 10 out of 10 points Which of the following codes is used to report placement of a flow directed Swan-Ganz catheter? b. 93503 b. 93503 Response Feedback: RATIONALE: Look in the CPT® Index for Swan-Ganz Catheter/Insertion. You're directed to 93503 which is the Insertion and placement of flow directed catheter (eg, Swan-Ganz) for monitoring purposes. • Question 7 10 out of 10 points Which of the following is not included in the base unit value of anesthesia services? c. Arterial line placement c. Arterial line placement Response Feedback: RATIONALE: The placement of an arterial line for intraoperative monitoring is not included in the base value services listed in the Anesthesia Guidelines. • Question 8 10 out of 10 points A 78 year old patient is undergoing lens surgery for cataracts. An anesthesiologist personally performed monitored anesthesia care (MAC). Which modifier(s) appropriately report(s) the anesthesiologist's service? c. 00142-AA-QS c. 00142-AA-QS Response Feedback: RATIONALE: An anesthesiologist who is performing personally administration of anesthesia reports the service with an AA modifier. Because the service was performed using MAC, a QS modifier is also reported. • Question 9 10 out of 10 points An anesthesiologist is medically supervising five cases at the same time. Which modifier(s) report(s) the anesthesiologist and CRNA services? d. AD and QX d. AD and QX Response Feedback: RATIONALE: An anesthesiologist who is medically supervising reports the service separately from the CRNA. Supervision of more than four concurrent anesthesia procedures is reported with modifier AD. The CRNA reports with modifier QK. • Question 10 10 out of 10 points A 22-year-old patient delivered a healthy baby boy by cesarean delivery with general anesthesia. The anesthesiologist performed all required steps for medical direction and was medically directing two other cases concurrently. Which modifier(s) report(s) the anesthesiologist and CRNA services? b. 01961-QK and 01961-QX b. 01961-QK and 01961-QX Response Feedback: RATIONALE: An anesthesiologist who is medically directing reports the service separately from the CRNA, depending on the number of concurrent cases. Because there was more than one concurrent (QY) case and fewer than five concurrent (AD) cases, the appropriate modifiers to report are QK for the physician claim and QX for the CRNA claim. A QZ modifier is reported when indicating a case is performed by a CRNA without medical direction by a physician. Sunday, November 19, 2017 9:20:55 AM MST • Question 1 4 out of 4 points A 22 year-old patient who has severe medical problems is placed under general anesthesia by an anesthetist for a service not usually requiring anesthesia. What modifier would be appended to the service? c. 23 c. 23 Response Feedback: Rationale: In the CPT® codebook go to Appendix A – Modifiers. Review the modifiers to determine that modifier 23 is reported to indicate a procedure not usually requiring anesthesia (either none or local) but due to unusual circumstances general anesthesia is necessary. • Question 2 4 out of 4 points What is the anesthesia code for a shoulder arthroscopy which became an open procedure on the shoulder joint? c. 01630 c. 01630 Response Feedback: Rationale: In the CPT® Index, look for Anesthesia/Arthroscopic Procedures/Shoulder which directs you to code range 01622-01638. Review the codes in the numeric section to determine 01630 is the appropriate code selection because the description of the code includes open or surgical arthroscopic procedures. • Question 3 4 out of 4 points What intraperitoneal organs are found in the lower abdomen? c. Appendix, cecum, ileum, sigmoid colon c. Appendix, cecum, ileum, sigmoid colon Response Feedback: Rationale: Intraperitoneal organs in the lower abdomen include the appendix, cecum, ileum and sigmoid colon. • Question 4 4 out of 4 points Report the appropriate anesthesia code for an obstetric patient who had a planned general anesthesia for cesarean hysterectomy. b. 01963 b. 01963 Response Feedback: Rationale: Use the CPT® Index look for Anesthesia/Hysterectomy/Cesarean which directs you to 01963, 01969. Review the codes in the numeric section to determine that code 01963 is the appropriate code. Note: Code 01969 is an add-on code and cannot be coded without a primary procedure code. • Question 5 4 out of 4 points What is the anesthesia code for a mediastinoscopy utilizing OLV (one lung ventilation)? b. 00529 b. 00529 Response Feedback: Rationale: In the CPT® Index look for Anesthesia/Mediastinoscopy directing you to codes 00528, 00529. These codes represent mediastinoscopy and diagnostic thoracoscopy. Review the codes in the numeric section to determine that 00529 describes the procedure utilizing one lung ventilation (OLV). • Question 6 4 out of 4 points What time is used to report the start of anesthesia time? b. When the anesthesiologist begins to prepare the patient for anesthesia b. When the anesthesiologist begins to prepare the patient for anesthesia Response Feedback: Rationale: Per Anesthesia Guidelines in the CPT® codebook under the subheading Time Reporting: Anesthesia time begins when the anesthesiologist begins to prepare the patient for anesthesia in the operating room (or an equivalent area). Pre-anesthesia assessment time is not part of reportable anesthesia time, as it is considered in the base values assigned. • Question 7 4 out of 4 points What ICD-10-CM code is reported for an uncomplicated incomplete abortion? b. O03.4 b. O03.4 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Abortion/incomplete (spontaneous) which directs you to code O03.4. Verify code selection in the Tabular List. Note that spontaneous is a nonessential modifier to Abortion. • Question 8 4 out of 4 points What anesthesia code(s) should be assigned for an obstetric patient who had neuraxial labor analgesia provided by the anesthesiologist when the delivery was expected to be a normal vaginal delivery but the obstetrician performed a cesarean delivery when the fetal heart rate dropped? d. 01967, 01968 d. 01967, 01968 Response Feedback: Rationale: In the CPT® Index under Anesthesia/Neuraxial/Labor which directs you to code range 01967-01969. Review the codes in the numeric section to determine that codes 01967, 01968 are the correct codes. Code 01967 describes the initial service without the cesarean delivery. Code 01968 is an add-on code which adds the cesarean delivery. Add-on codes must be coded in conjunction with the primary code and cannot be coded alone. The correct codes are 01967, 01968. • Question 9 0 out of 4 points A 42 year-old patient was undergoing anesthesia in an ASC and began having complications prior to the administration of anesthesia. The surgeon immediately discontinued the planned surgery. If the insurance company requires a reported modifier, what modifier best describes the extenuating circumstances? c. 53 a. 73 Response Feedback: Rationale: In the CPT® codebook go to Appendix A and look for the subheading, Modifiers Approved for Ambulatory Surgery Center (ASC) Hospital Outpatient Use. Review the modifiers to determine that modifier 73 best describes an anesthesia service discontinued prior to administration of anesthesia in an ASC. • Question 10 4 out of 4 points What is the anesthesia code for an insertion of a penile prosthesis performed via a perineal approach? c. 00938 c. 00938 Response Feedback: Rationale: In the CPT® Index look for Anesthesia/Penis which directs you to code range 00932-00938. Review the code range in the numeric section to determine 00938 is the appropriate code selection. • Question 11 4 out of 4 points What is the appropriate code for a patient who had regional block anesthesia provided for carpal tunnel surgery? a. 01810 a. 01810 Response Feedback: Rationale: In this example it is important to understand the type of anesthesia provided will not determine the anesthesia code. In the CPT® Index look for Anesthesia/Arm/Lower which directs you to code ranges 00400, 01810-01820, 01830-01860. Review the codes in the numeric section to determine code 01810 is correct. The coder must know that carpal tunnel surgery refers to the median nerve in the wrist. Hint –Try looking up the surgical code for clues to the anatomical area when necessary for assistance. • Question 12 4 out of 4 points The patient is receiving a cast change for a compound left trimalleolar fracture (ankle). What ICD-10-CM code is reported? c. S82.852D c. S82.852D Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Fracture, traumatic/ankle/trimalleolar (displaced) which directs you to code S82.85-. In the Tabular List it indicates the code requires a 6th character for the laterality and a 7th character for the episode of care. The 6th character 2 is for the left ankle and the 7th character D is for subsequent care with routine healing. The correct code is S82.852D. According to ICD-10-CM guideline, I.C.19.c., a fracture not indicated whether displaced or not displaced should be coded to displaced. According to ICD-10-CM guideline, I.C.19.a., an example of subsequent care is a cast change. • Question 13 4 out of 4 points The patient had surgery to remove and replace an existing Hickman catheter. The anesthesiologist reported a postoperative diagnosis of a catheter related bloodstream infection (CRBSI). What ICD-10-CM code(s) is/are reported? c. T80.211A c. T80.211A Response Feedback: Rationale: A catheter related bloodstream infection (CRBSI) is a complication. In ICD-10-CM Alphabetic Index look for Infection/due to or resulting from/Hickman catheter/bloodstream which directs you to code T80.211-. In the Tabular List a 7th character is required to complete the code. Character A is selected for initial encounter. • Question 14 4 out of 4 points Using your ICD-10-CM codebook look for the diagnosis code for a patient with a preoperative diagnosis of abdominal pain, right lower quadrant and a postoperative diagnosis of acute appendicitis with peritoneal abscess. What ICD-10-CM code is reported? d. K35.3 d. K35.3 Response Feedback: Rationale: The preoperative diagnosis of abdominal pain in the right lower quadrant is not reported because there is definitive diagnosis listed post-operatively. The postoperative diagnosis specifies acute appendicitis with peritoneal abscess. Look in the ICD-10-CM Alphabetic Index for Appendicitis/with/peritoneal abscess which directs you to K35.3. Verify code selection in the Tabular List. • Question 15 4 out of 4 points Following labor and delivery, the mother developed acute kidney failure. What ICD-10-CM code is reported? d. O90.4 d. O90.4 Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Failure/renal/following labor and delivery (acute) which directs you to code O90.4. Verify code selection in the Tabular List. Note: when the failure occurred the patient had already given birth so it should not be coded as a complication during pregnancy. • Question 16 0 out of 4 points Code 00940 Anesthesia for vaginal procedures (including biopsy of labia, vagina, cervix or endometrium); not otherwise specified has a base value of three (3) units. The patient was admitted under emergency circumstances, qualifying circumstance code 99140, which allows two (2) extra base units. A preanesthesia assessment was performed and signed at 2:00 a.m. Anesthesia start time is reported as 2:21 am, and the surgery began at 2:28 am. The surgery finished at 3:25 am and the patient was turned over to PACU at 3:36 am, which was reported as the ending anesthesia time. Using fifteen-minute time increments and a conversion factor of $100, what is the correct anesthesia charge? c. $800.00 a. $1,000.00 Response Feedback: Rationale: Determining the base value is the first step in calculating anesthesia charges and payment expected. Time reporting is the second step. Per Anesthesia Guidelines in the CPT® codebook under the subheading Time Reporting: Anesthesia time begins when the anesthesiologist begins to prepare the patient for anesthesia in the operating room (or an equivalent area) and ends when the anesthesiologist is no longer in personal attendance, that is, when the patient may be safely placed under postoperative supervision. In the scenario above, base units equal three (3) plus two (2) emergency qualifying circumstances units (Base 3 + QC 2 = 5 units). Five (5) time units, in fifteen minute increments, is calculated by taking the anesthesia start time (2:21) and the anesthesia end time (3:36) and determining one hour 15 minutes (75/15 = 5) of total anesthesia time. Ten units (5 + 5 = 10) are then multiplied by the $100 conversion factor (10 X $100 = $1,000.00). Note: Base Unit Values are not separately listed in the CPT®. The American Society of Anesthesiologists (ASA) determines the base units’ values for anesthesia codes. • Question 17 4 out of 4 points An 11 month-old patient presented for emergency surgery to repair a severely broken arm after falling from a third story window. What qualifying circumstance code(s) may be reported in addition to the anesthesia code? d. 99100, 99140 d. 99100, 99140 Response Feedback: Rationale: In the CPT® Anesthesia Guidelines under the subheading Qualifying Circumstances each of the qualifying circumstances codes identifies a different circumstance, and more than one may be appended when applicable, unless the reported anesthesia code already contains the risk factor. In this case, 99100 is assigned for extreme age of one year or younger and 99140 is assigned for emergency conditions. Note: Qualifying Circumstances codes may also be found in CPT® Medicine Subsection Miscellaneous Services/Qualifying Circumstances for Anesthesia. • Question 18 4 out of 4 points A 94 year-old patient is having surgery to remove his parotid gland with dissection and preservation of the facial nerve. The surgeon has requested the anesthesia department place an arterial line. What CPT® code(s) is/are reported for anesthesia? c. 00100, 36620, 99100 c. 00100, 36620, 99100 Response Feedback: Rationale: In the CPT® Index look for Anesthesia/Salivary Glands which directs you to code 00100. Reference the code in the numeric section to confirm that 00100 is the correct code. Hint - Coders may need to use the Surgery Section to determine that the parotid gland is included in the salivary glands. The arterial line placement is NOT included in the base value and may be reported separately with code 36200. In the CPT® Index look for Catheterization/Arterial System/Percutaneous. Due to patient’s advanced age of 94, qualifying circumstance add-on code 99100 is also reported. Furthermore, the patient’s age implies he is on Medicare, therefore we do not use Physical Status Modifiers as they are not accepted. • Question 19 4 out of 4 points A 5 year-old patient is experiencing atrial fibrillation with rapid ventricular rate. The anesthesia department is called to insert a nontunneled central venous (CV) catheter. What CPT® code is reported? b. 36556 b. 36556 Response Feedback: Rationale: The coder should note that this is NOT a general anesthesia service so a code from the Anesthesia Section of CPT® would not be appropriate. In the CPT® Index look for Catheterization/Central Venous which states see Central Venous Catheter Placement. Look for Central Venous Catheter Placement/Insertion/Central/Non-tunneled which directs you to codes 36555, 36556. Review the numeric section to determine the correct code is 36556 for the 5 year-old patient. Note: The coder should note the type of insertion and the age of the patient to make the correct choice of codes. • Question 20 4 out of 4 points Mr. Johnson, age 82, having been in poor health with diabetes and associated peripheral neuropathy, is having a fem-pop bypass. The anesthesiologist documents he has severe systemic disease. What code(s) is/are correct for anesthesia? a. 01270-P3, 99100 a. 01270-P3, 99100 Response Feedback: Rationale: Fem-pop bypass is an abbreviation for femoral-popliteal bypass of arteries in the upper leg. Look in the CPT® Index for Anesthesia/Bypass Graft/Leg, Upper which directs you to code 01270. Review the code in numeric section to determine the correct code is 01270. The qualifying circumstance code 99100 is added to indicate the extreme age of the patient. Physical status modifier P3 indicates the patient has severe systemic disease. • Question 21 4 out of 4 points A patient presents to the OR for a craniotomy with evacuation of a hematoma. What CPT® code is reported for the anesthesiologist’s services? a. 00211 a. 00211 Response Feedback: Rationale: Look in the CPT® Index for Anesthesia/Head which directs you to codes 00210-00222, 00300 or Anesthesia/craniotomy which directs you to code 00211. Review the numeric section to determine that the correct code is 00211 as it includes verbiage for the evacuation of a hematoma. • Question 22 4 out of 4 points A 74 year-old patient is undergoing surgery under monitored anesthesia care (MAC). The surgeon has determined the procedure will be markedly invasive. What modifier(s) is/are appropriate for Medicare? a. G8 a. G8 Response Feedback: Rationale: In the HCPCS Level II codebook locate where the HCPCS Level II Modifiers are listed. A patient who is undergoing monitored anesthesia care (MAC) for a deep complex, complicated or markedly invasive surgical procedure may be reported with modifier G8. The additional modifier QS is not necessary because the description for G8 includes monitored anesthesia care. • Question 23 4 out of 4 points A 72 year-old patient is undergoing a corneal transplant. An anesthesiologist is personally performing monitored anesthesia care. What CPT® code and modifier(s) are reported for anesthesia? a. 00144-AA-QS, 99100 a. 00144-AA-QS, 99100 Response Feedback: Rationale: In the HCPCS Level II codebook locate where the HCPCS Level II Modifiers are listed. An anesthesiologist who is personally performing services reports the service with a modifier AA and when the service performed is Monitored Anesthesia Care (MAC) modifier QS is also reported. The modifiers are sequenced first by the anesthesia provider then the MAC modifier which are attached to the appropriate anesthesia code. The Qualifying Circumstances add-on code 99100 is assigned for extreme age of the patient being older than 70 years of age. • Question 24 4 out of 4 points A 30 year-old patient had anesthesia for an extensive spinal procedure with instrumentation under general anesthesia. The anesthesiologist performed all required steps for medical direction while directing one CRNA. What modifier(s) and CPT® code(s) is/are reported for the anesthesiologist and CRNA services? b. 00670-QY and 00670-QX b. 00670-QY and 00670-QX Response Feedback: Rationale: In the CPT® Index look for Anesthesia/Spinal Instrumentation which directs you to code 00670. Review code in the numeric section. An anesthesiologist who is medically directing care reports their service separately from the CRNA, depending on the number of concurrent cases and the appropriate modifiers for distinction. Because there was only one case, the appropriate modifiers to report are QY for the physician and QX for the CRNA. A QZ modifier would indicate the case was performed by a non-medically directed CRNA. Refer to your HCPCS Level II codebook to verify these anesthesia modifiers. • Question 25 4 out of 4 points What ICD-10-CM code is reported for a reaction to anesthesia, initial encounter? c. T88.59XA c. T88.59XA Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Anesthesia, anesthetic/complication or reaction NEC (see also Complications, anesthesia) which directs you to code T88.59-. The Tabular List indicates that code T88.59- requires a 7thcharacter with no 6th character listing. Insert the placeholder X as the 6th character. Select the 7th character A for initial encounter. Sunday, November 19, 2017 9:21:09 AM MST • Question 1 10 out of 10 points What X-Ray projection enters the front of the body and exits through the back of the body with the patient lying down on the back? a. AP a. AP Response Feedback: RATIONALE: AP is the abbreviation for anteroposterior where the projection enters the front of the body and exits through the back of the body. Because the patient is lying on their back, it cannot be oblique. • Question 2 10 out of 10 points What position is the body placed in when it is in an oblique position? c. At an angle, neither frontal nor lateral c. At an angle, neither frontal nor lateral Response Feedback: RATIONALE: An oblique position is a slanted position where the patient is lying at an angle which is neither prone nor supine. • Question 3 10 out of 10 points A young boy presents to the emergency department with pain in his lower left leg after being kicked in a soccer game. The X-ray report reveals a fractured tibia and fibula. What diagnosis code(s) should the radiologist report for reading the X-ray? Do not report the external cause code. d. S82.202A, S82.402A d. S82.202A, S82.402A Response Feedback: RATIONALE: The final diagnosis is available at the time of reporting and is used instead of the sign or symptom. The final diagnosis of a fracture of the tibia and fibula is reported as the diagnosis. In the ICD-10-CM Alphabetic Index, look for Fracture, traumatic/tibia (shaft) S82.20-. In the Tabular List, a 6th character 2, is reported for the left side and the 7th character A, is reported for the initial encounter. Final code choice: S82.202A. Verify code selection in the Tabular List. Next, look in the ICD-10-CM Alphabetic Index for Fracture, traumatic/fibula (shaft) (styloid) S82.40-. In the Tabular List, 6th character 2, is reported for the left side and the 7th character A is reported for the initial encounter. Final code choice is S82.402A. Verify code selection in the Tabular List. • Question 4 10 out of 10 points Mary visited her family physician for a lump in her breast. The physician ordered a mammogram to rule out breast cancer. The radiologist did not find any abnormal findings. What diagnosis is reported for the professional portion of the mammography? b. N63 b. N63 Response Feedback: RATIONALE: When a test is ordered for a sign or symptom, and the outcome of the test is a normal result with no confirmed diagnosis, the coder reports the sign or symptom that prompted the physician to order the test. Because the test was ordered for a lump in the breast, but the outcome is normal, the lump in the breast, N63 is reported as the diagnosis. In the ICD-10-CM Alphabetic Index, look for Lump which directs you to see Mass. Look in the Alphabetic Index for Mass/breast N63. Verify code selection in the Tabular List. • Question 5 10 out of 10 points A parent brings a child to the Emergency Department after realizing the child swallowed a metal jack. A radiological exam from the nose to the rectum is performed. What is/are the CPT® code(s) for this service? b. 76010-26 b. 76010-26 Response Feedback: RATIONALE: Look in the CPT® Index for X-ray/Nose to Rectum/Foreign Body 76010. Turning to 76010 in the numeric section, this code is applicable to a child for a single view. • Question 6 10 out of 10 points A contrast radiograph of the salivary glands and ducts is performed, resulting in a diagnosis of salivary fistula. What are the CPT® and ICD-10-CM codes for the supervision and interpretation of this procedure? d. 70390-26, K11.4 d. 70390-26, K11.4 Response Feedback: RATIONALE: Contrast radiography of the salivary gland and ducts is considered sialography. Code 70390 describes sialography supervision and interpretation. Look in the CPT® Index for Salivary Glands/X-ray/with contrast. The patient is diagnosed with a salivary fistula, which is found in the ICD-10-CM Alphabetic Index under Fistula/salivary duct or gland K11.4. Verify code selection in the Tabular List. • Question 7 0 out of 10 points A complete B-scan ultrasound without duplex Doppler of the kidney is performed in the physician's office on a patient following a kidney transplant. What is the CPT® code for the ultrasound? c. 76776 b. 76775 Response Feedback: RATIONALE: Look in the CPT® Index for Ultrasound/Kidney, 76770–76776. CPT® code 76776 is an ultrasound for a transplanted kidney, including real-time and duplex Doppler with image documentation. A duplex Doppler of the kidney is not performed. The parenthetical instruction under CPT® 76776 indicates to report 76775 for an ultrasound of transplanted kidney without duplex Doppler. The correct code is 76775. • Question 8 10 out of 10 points A patient with left breast pain and a lump in the breast visits her physician. After examination, the physician orders a mammogram of the left breast. The mammography is performed using computer-aided detection software. What CPT® code is reported for the mammography? c. 77065 c. 77065 Response Feedback: RATIONALE: The physician ordered a unilateral diagnostic mammogram with computer-aided detection (CAD). Code 77065 describes a diagnostic mammography, including computer-aided detection (CAD) when performed; unilateral. • Question 9 10 out of 10 points A patient with osteoporosis reports to her physician's office for a DXA bone density study of her spine to monitor the severity of her condition. What is the correct CPT® code for the DXA scan? a. 77080 a. 77080 Response Feedback: RATIONALE: DXA is dual-energy X-ray absorption. The site is of the spine, which is part of the axial skeleton. For DXA-See Dual X-ray Absorptiometry (DXA); Dual X-ray Absorptiometry (DXA)/Axial Skeleton. In this case one site (spine) is involved in the study. The correct code is 77080. • Question 10 0 out of 10 points A patient receives complex radiation oncology treatments two times a day, for three days. Which radiology code(s) is/are appropriate for this series of clinical management fractions? d. 77427, 77431 b. 77427 Response Feedback: RATIONALE: Radiation therapy management is based on the number of fractions. Each time the patient receives the radiation is considered a fraction. If the patient receives radiation two times in one day, it is considered two fractions. This patient had a total of 6 fractions of radiation. Code 77427 indicates five fractions. According to the radiation treatment management guidelines, when a patient has one or two fractions left at the end of a course of treatment, it is not separately billable. Code 77431 is used when the entire course of treatment consist of only 1 or 2 fractions. The correct code to report for the management is 77427. Look in the CPT® Index for Radiation Therapy/Treatment Management/Weekly. Sunday, November 19, 2017 9:21:34 AM MST • Question 1 4 out of 4 points An axillary view might be included in an X-ray of what part of the skeleton? a. Shoulder a. Shoulder Response Feedback: Rationale: The axillary view is an X-ray view taken of the shoulder. • Question 2 4 out of 4 points What ICD-10-CM code is reported for a routine chest X-ray? c. Z00.00 c. Z00.00 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Encounter/X-ray of chest (as part of general medical examination) Z00.00. There is no mention of abnormal findings making Z00.00 the correct code choice. Verify code selection in the Tabular List. • Question 3 4 out of 4 points The patient presents for a screening CT colonography. What CPT® code(s) is/are reported? c. 74263 c. 74263 Response Feedback: Rationale: The patient presents for a colonography. In the CPT® Index look for Colonography/CT Scan/Screening. You are referred to 74263. Refer to the code descriptions to confirm selection of the correct code. The purpose of the test is for a screening. 74263 is the correct code. • Question 4 4 out of 4 points A patient arrives at the urgent care facility with a swollen ankle. Anteroposterior and lateral view X-rays of the ankle are taken to determine whether the patient has a fractured ankle. What CPT® code(s) is/are reported? d. 73600 d. 73600 Response Feedback: Rationale: In the CPT® Index look for X-ray/Ankle and you are guided to range 73600-73610. There were two views taken (anteroposterior and lateral views), so CPT® code 73600 is correct. • Question 5 4 out of 4 points Which anatomic position has the patient lying at an angle instead of lying flat or directly on their side? c. Oblique c. Oblique Response Feedback: Rationale: The oblique position is a slanted position where the patient is lying at an angle that is neither prone nor supine. • Question 6 4 out of 4 points A 32 year-old patient is coming into an outpatient facility to have a catheterization performed of the uterus with saline infusion sonohysterography due to dysfunctional uterine bleeding. A previous scan showed suspected endometrial polyps. What CPT® and ICD-10-CM codes are reported? d. 58340, 76831-26, N93.8 d. 58340, 76831-26, N93.8 Response Feedback: Rationale: The uterus is being catheterized not the bladder. Look in the CPT® Index for Sonohysterography/Saline Infusion/Injection Procedure directing you to 58340. The catheterization is included in the code description for 58340. A parenthetical note under this code states “For radiological supervision and interpretation of saline infusion, use 76831.” Modifier 26 is reported for the professional service. The diagnosis to report is the dysfunctional uterine bleeding, which is found in the ICD-10-CM Alphabetic Index by looking for Bleeding/uterus, uterine NEC/dysfunctional of functional which guides you to code N93.8. According to ICD-10-CM guideline IV.H you do not code for a condition documented as suspected such as the endometrial polyps in the outpatient setting. • Question 7 4 out of 4 points In ICD-10-CM when a patient is seen for a routine examination, what additional information is needed in order to accurately code the routine examination? d. Whether or not abnormal findings were identified. d. Whether or not abnormal findings were identified. Response Feedback: Rationale: In ICD-10-CM the codes for radiologic exam have been expanded to specify when abnormal findings are found on the radiology exam. Look in the ICD-10-CM Alphabetic Index for Examination/radiological. There is a subentry for with abnormal findings. These entries default to the codes for a general adult medical examination. Z00.00 Encounter for general adult medical examination without abnormal findings. Z00.01 Encounter for general adult medical examination with abnormal findings. • Question 8 4 out of 4 points A patient with hydronephrosis has a left nephrostomy and he has agreed to a pyelography (IVP) to rule out a right renal obstruction. The patient was placed prone on the X-ray table one hour after IV infusion of contrast. Contrast flowed from the left and right renal pelvis, down the ureters into the bladder where a Foley catheter was positioned. The IVP showed no obstruction or abnormalities in the urinary tract aside from the left hydronephrosis of the pelvis. The right kidney and ureter showed no obstruction. Bladder appeared within normal limits. What CPT® code is reported for the radiological services? d. 74400-26 d. 74400-26 Response Feedback: Rationale: A radiographic exam of the urinary tract is performed with IV injection of contrast medium and radiographs are taken. This is performed to assess the anatomy and function of the kidneys, bladder, and ureters. In the CPT® Index look for X-ray/with Contrast/Urinary Tract directing you to 74400-74425 or Urography/Intravenous 74400-74415. Reviewing the codes in the numeric section leads you to report 74400 for an intravenous pyelography. Modifier 26 is appended to indicate the professional service. • Question 9 4 out of 4 points Tomographic axial images (CT or CAT scan) through the abdomen were obtained without administration of intravenous contrast. This showed a 3 cm diameter mass in the upper pole of the right kidney abutting the liver. Cryoablation of the lesion was performed utilizing two freezing cycles with good cosmetic results. What CPT® codes are reported? d. 50250, 77013-26 d. 50250, 77013-26 Response Feedback: Rationale: A kidney (renal) mass, not tumor, is being destroyed (ablation) by freezing (cryoablation) the lesion to remove it. This procedure was performed under CT (computed tomography) guidance to ablate parenchymal (vital organ-example: kidney) tissue. Look in the CPT® Index for Ablation/Cryosurgical/Renal Mass directing you to 50250. Cryosurgery/Lesion/Kidney also leads to 50250. 50250 includes ultrasound guidance if performed. The CT guidance was performed to locate the mass and not to accomplish the ablation. CT guidance is found in the CPT® Index by looking for Ablation/CT Scan Guidance directing you to code 77013. Modifier 26 denotes the professional service. • Question 10 4 out of 4 points A 66 year-old male with a history of anemia presents for a liver core biopsy to evaluate for possible cirrhosis. The patient was brought to the CAT scan suite in which limited CT images of the upper abdomen were performed for biopsy needle placement. The appropriate site for the liver core biopsy was chosen. The patient's skin was then marked with the computer coordinates. An 18-gauge needle was advanced into the appropriate site and a sample was obtained. What CPT® codes are reported? a. 47000, 77012-26 a. 47000, 77012-26 Response Feedback: Rationale: Biopsy of the liver is taken by a needle (percutaneous) under computed tomography guidance (CT). In the CPT® Index look for Biopsy/Liver 47000, 47001, 47100, 47700. Code 47000 describes a percutaneous needle biopsy of the liver. Below CPT code 47000 you are given codes for imaging guidance. Code 77012 describes the CT guidance for needle placement. Modifier 26 is appended to indicate the professional service. • Question 11 4 out of 4 points A 56 year-old patient who has been admitted requires a tunneled CV catheter insertion. The physician uses ultrasound guidance to perform the insertion. The physician documented vessel patency and that permanent recordings are in the patient’s record. What CPT® codes are reported for the physician’s services? b. 36558, 76937-26 b. 36558, 76937-26 Response Feedback: Rationale: The physician inserts a tunneled CV catheter (central venous). The patient is 56 years-old and there is no indication that a port or pump is involved. In the CPT® Index look for Central Venous Catheter Placement/Insertion/Central/Tunneled without Port or Pump 36557-36558, 36565. The correct code is 36558. The physician uses ultrasound guidance, which is reported with 76937. In the coding guidelines for Central Venous Access Procedures, it states that imaging can be reported separately. The codes you are referred to are 76937 and 77001. Because the imaging used is ultrasound, report with 76937. Note that 76937 is an add-on code and it can only be reported if the physician documents selected vessel patency and permanent ultrasound recordings are in the patient records. Modifier 26 is appended to report the professional component. • Question 12 4 out of 4 points A patient 14 weeks pregnant is coming back to her obstetrician’s office for a repeat transabdominal ultrasound to measure fetal size and to confirm abnormalities seen in a previous scan. The obstetrician documented the ultrasound results in the medical record. What CPT® code is reported by the obstetrician? b. 76816 b. 76816 Response Feedback: Rationale: The patient is coming back for a follow-up (repeat) ultrasound to re-evaluate conditions affecting the fetus seen on the last ultrasound scan. In the CPT® Index look for Ultrasound/Obstetrical/Pregnant Uterus to find the code range 76801, 76802, 76805, 76810-76817. The correct code for a follow-up ultrasound is 76816. No modifier 26 is needed because the ultrasound and the interpretation of the results were performed in the obstetrician’s office. • Question 13 4 out of 4 points A patient is seen in the clinic with sharp abdominal pain, vomiting and nausea and a history of cholelithiasis. An ultrasound of the gallbladder is performed revealing she has stones in the gallbladder. What CPT® code is reported? c. 76705 c. 76705 Response Feedback: Rationale: The patient has a limited ultrasound performed because only a single organ (gallbladder) was examined. A complete ultrasound of the abdomen is defined in the subsection guidelines under the heading of Abdomen and Retroperitoneum. This is found in the CPT® Index by looking for Ultrasound/Abdomen directing you to 76700-76705. Pay close attention to the guidelines throughout the ultrasound codes to determine what must be examined and documented to be considered a complete exam. • Question 14 4 out of 4 points A 65 year-old female has a 2.5 cm x 2.0 cm non-small cell lung cancer in her right upper lobe. The tumor is inoperable due to severe respiratory conditions. She will be receiving stereotactic body radiation therapy under image guidance. Beams arranged in 8 fields will deliver 25 Grays per fraction for 4 fractions. What CPT® and ICD-10-CM codes are reported? b. 77373, Z51.0, C34.11 b. 77373, Z51.0, C34.11 Response Feedback: Rationale: Patient is having stereotactic radiation therapy technique delivered, not managed, in a large radiation dose to tumor sites in the upper right lobe of the lung. In the CPT® Index look for Radiation Therapy/Stereotactic Body which directs you to 77373. Codes 77371-77373 do not need modifier TC or 26, because they are facility only codes. 77373 is correct with stereotactic body radiation not exceeding 5 fractions. According to ICD-10-CM guideline I.C.2.a. “If a patient admission/encounter is solely for the administration of chemotherapy, immunotherapy or radiation therapy, assign the appropriate Z51.-code as the first-listed or principal diagnosis, and the diagnosis or problem for which the service is being performed as a secondary diagnosis.” In the ICD-10-CM Alphabetic Index look for Encounter/radiation therapy (antineoplastic) which directs you to Z51.0. In the ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/lung/upper lobe and select from the Malignant Primary column referring you to C34.1-. Verification in the Tabular List indicates a 4th character is needed, report 1 for the right lung. • Question 15 4 out of 4 points A 38 year-old male seen in the Emergency Department sustained an injury several hours ago to his left hand when he fell and a team member stepped on it when playing tackle football. X-ray was taken in lateral, external oblique and PA positions. The interpretation of the X-rays revealed a fracture of the shaft of the third metacarpal. What CPT® and ICD-10-CM codes are reported for the radiological services? a. 73130-26, S62.323A, W50.0XXA, Y93.61 a. 73130-26, S62.323A, W50.0XXA, Y93.61 Response Feedback: Rationale: A total of three views were taken of the hand. Lateral (side), oblique (diagonal) and PA (posterior-anterior) views. Look in the CPT® Index for X-ray/Hand which directs you to 73120-73130. Code 73130 describes a radiologic examination of the hand with a minimum of 3 views. Modifier 26 denotes the professional service. The diagnosis is found in the ICD-10-CM Alphabetic Index by looking for Fracture traumatic/ metacarpal/third/shaft (displaced) guiding you to code S62.32-. Tabular List indicates a 6th character is required to indicated laterality and a 7th character is required for the episode of care. A for initial encounter is selected as the 7th character for initial encounter. A review of the ICD-10-CM guideline, I.C.19.c., states “A fracture not indicated as closed or open should be classified as closed. A fracture not indicated whether displaced or not displaced should be coded to displaced.” The next two codes are found in the ICD-10-CM External Cause of Injuries Index. The first external cause code is found by looking for Stepped on/by/person guiding you to code W50.0-. Tabular List indicates seven characters are needed to complete the code. The 5th and 6th characters will have X as placeholders and the 7th character will report A for the initial encounter Only one code is reported for the patient falling down while playing sport activity and then getting stepped on. The second external cause code is found by looking for Activity/football (American) NOS/tackle guiding you to code Y93.61. • Question 16 4 out of 4 points Magnetic resonance imaging of the chest is first done without contrast medium enhancement and then is performed with an injection of contrast. What CPT® code(s) is/are reported for the radiological services? c. 71552 c. 71552 Response Feedback: Rationale: The patient is having magnetic resonance imaging in which the images were performed first without contrast and again following the injection of contrast. In the CPT® Index look for Magnetic Resonance Imaging (MRI)/Diagnostic/Chest directing you to 71550-71552. • Question 17 4 out of 4 points A patient is taken to the inpatient cardiac cath lab and 1% Lidocaine is infused into the skin of the right groin. The artery is punctured with a needle and a guidewire with a catheter is advanced into the abdominal aorta. The guidewire is removed. Contrast medium is injected through the catheter and abdominal aortography is performed. What CPT® code(s) is/are reported for the physician’s services? d. 36200, 75625-26 d. 36200, 75625-26 Response Feedback: Rationale: The physician gains access to the aorta through the right groin (femoral artery). The procedure is reported with 36200. In the CPT® Index look for Catheterization/Aorta 36106, 36200. In the CPT® Index look for Aorta/Aortography or see Aortography/Aorta Imaging. Abdominal aortography is performed which is reported with 75625. There is no documentation that both iliofemoral arteries of the lower extremities were also performed, code 75630 is not reported. The services were provided by the physician in the inpatient setting. Append modifier 26 to indicate the professional component. • Question 18 0 out of 4 points A CT study of the lumbar spine (L2–L4) was performed with IV contrast in the hospital outpatient radiology department and the interpretation of the images is performed by the radiologist. What CPT® code(s) should be reported by the radiologist who is not an employee of the hospital? a. 72132-26, 72132-TC d. 72132-26 Response Feedback: Rationale: Look in the CPT® Index for CT Scan/with Contrast/Spine/Lumbar which directs you to 72132. Modifier 26 is appended to the radiological service for the professional service. The hospital would also bill the radiological service for the technical component as the hospital owns the equipment used for the service. • Question 19 4 out of 4 points The patient is a 63 year-old gentleman diagnosed with rectal cancer, who had a resection of the cancer performed. He now presents to have a Port-A-Cath (a central venous access device) inserted for postoperative adjuvant therapy. An 18-gauge introducer needle was inserted into the left subclavian vein through which a soft tipped guide wire was inserted into the superior vena cava under fluoroscopy. A subcutaneous pouch in the anterior part of the chest was created for the port. The catheter was then tunneled and measured to length. The dilator and introducer sheath were passed over the wire into the superior vena cava under fluoroscopic guidance. The catheter was passed through the sheath and the port was applied with good venous return. What CPT® codes are reported? a. 36561, 77001-26 a. 36561, 77001-26 Response Feedback: Rationale: The insertion of a tunneled Port-A-Cath via the subclavian vein (which is a central venous access device with a subcutaneous port) was performed on a 63 year-old. It is important to note, it is tunneled. The procedure was performed under fluoroscopic guidance for placement of a central venous access device. The Port-A-Cath procedure is found in the CPT® Index by looking for Central Venous Catheter Placement/Insertion/Central/Tunneled with Port directs you to 36560, 36561, 36566. Code 36561 is the correct code. The guidelines for central venous access procedures instruct you to use 77001 for fluoroscopic guidance. This can be found in the CPT® Index by looking for Fluoroscopy/Venous Access Device or Venous Access Device/Fluoroscopic Guidance directing you to add-on code 77001. If the procedure was performed going through the basilic or cephalic vein in the arm you would report code 36571. 36563 would be reported if a pump was placed. • Question 20 4 out of 4 points A patient in her 2nd trimester with a triplet pregnancy is seen in the obstetrician’s office for an obstetrical ultrasound only for obtaining fetal heartbeats and position of the fetuses. What CPT® code(s) is/are reported for the ultrasound? a. 76815 a. 76815 Response Feedback: Rationale: This is a limited ultrasound performed on three fetuses. CPT® code 76815 has in its code description the ultrasound is for 1 or more fetuses. There is also a parenthetical note stating “Use 76815 only once per exam and not per element.” This is found in the CPT® Index under Ultrasound/Obstetrical/Pregnant Uterus guiding you to 76801, 76802, 76805, 76810-76817. • Question 21 4 out of 4 points A patient was admitted to observation status after losing control and crashing his motorcycle into the guardrail on the highway. A CT scan of the brain without contrast and the chest is performed. It revealed a fracture of the skull base with no hemorrhage in the brain. There was no puncture of the lungs. Three views of the right and left sides of the ribcage reveal fractures of the left third and fifth rib. What CPT® and ICD-10-CM codes are reported? a. 70450-26, 71250-26, 71110-26, S02.109A, S22.42XA, V27.4XXA, Y92.411 a. 70450-26, 71250-26, 71110-26, S02.109A, S22.42XA, V27.4XXA, Y92.411 Response Feedback: Rationale: The first radiological code is 70450 because a CT scan without contrast of the brain was performed. Code 71250 is correct because thorax is a synonym for chest, and the CT was performed without contrast. Code 71275 is a CTA (computed tomographic angiography) which is used for imaging vessels to find a blood clot, aneurysm and other vascular irregularities in the chest making it an inappropriate code to report for this scenario. Code 71110 is correct to report the X-ray of the ribs taken bilaterally (left and right side). These codes are found in the CPT® Index by looking for CT Scan/without contrast/Brain which directs you to 70450, and CT Scan/without contrast/Thorax which directs you to 71250. Radiology for the ribs is found in the CPT® Index under X-ray/Ribs 71100-71111. Confirmation in the numeric section shows 71110 is correct for the three views of the ribs. Modifier 26 denotes the professional service performed in a facility setting. The first diagnosis is found in the ICD-10-CM Alphabetic Index by looking for Fracture, traumatic/skull/base directing you to code S02.10-. Verification in the Tabular List indicates the codes needs seven characters to be complete. Report 9 for the 6th character and then A for 7th character to indicate initial encounter. Two left ribs were fractured. Look in the Alphabetic Index for Fracture, traumatic/rib/multiple guiding you to S22.4-. Verification in the Tabular List indicates the need for seven characters to complete the code. Report 2 for as the 5th character for the left side. Report placeholder X for the 6th character and then an A for initial encounter as the 7th character. The next two codes are found in the External Cause of Injuries Index. Look for Accident/transport/motorcyclist/driver/collision with/stationary object (traffic) guiding you to V27.4-. In the Tabular List seven characters are required to complete the code. An X placeholder is used for the 5th and 6thcharacters and a 7th character of A indicates this is for initial encounter or active treatment. The last external cause code is found by looking for Place of occurrence/highway which directs you to code Y92.411. • Question 22 4 out of 4 points An oncology patient is having weekly radiation treatments with a total of seven conventional fractionated treatments. Two fractionated treatments daily for Monday, Tuesday and Wednesday and one treatment on Thursday. What radiology code(s) is/are appropriate for the clinical management of the radiation treatment? b. 77427 b. 77427 Response Feedback: Rationale: There are seven fractions given in this patient’s weekly treatment. According to CPT® guidelines, radiation treatment management is reported in units of five fractions or treatment sessions, regardless of the actual time-period in which the services are furnished. Code 77427 is also reported if there are three or four fractions beyond a multiple of five at the end of a course of treatment, one or two fractions beyond a multiple of five at the end of a course of treatment are not reported separately.” This instruction is found in CPT® under the heading Radiation Treatment Management in the Radiology/Radiation Oncology Section of the Radiology Chapter. In the CPT® Index look for Radiation Therapy/Treatment Management/Weekly directing you to 77427. • Question 23 0 out of 4 points A patient with thickening of the synovial membrane undergoes a fluoroscopic guided radiopharmaceutical therapy joint injection on his right knee without ultrasound. What CPT® code(s) is/are reported by the physician if performed in an ASC setting? d. 79440, 20610 a. 79440-26, 20610, 77002-26 Response Feedback: Rationale: Arthrocentesis is aspiration or injection with a needle involving a joint. According to CPT® coding guidelines, when radiopharmaceutical therapy is performed, you should select a code for the injection as well as the radiological guidance. Because the injection is intra-articular, the radiopharmaceutical therapy is reported with 79440. Fluoroscopic image guidance for a joint injection is reported with 77002. Modifier 26 is appended to both radiology codes to report the professional services performed by the physician in the ASC setting. The joint injection was performed on the knee, which is considered a large joint reported with 20610. The notes in the numeric section for Radiology/Nuclear Medicine under the Therapeutic heading indicates to also use the appropriate injection and/or procedure codes as well as imaging guidance. When multiple procedures are performed, they are listed in RVU order. Look in the CPT ® Index for Nuclear Medicine/Therapeutic/Radiopharmaceutical, Administration/Intra-articular directing you to 79440. Next in the CPT® Index look for Arthrocentesis/Large Joint directing you to 20610, 20611. Then look in the CPT® Index look for Needle Localization/Fluoroscopic Guidance directing you to 77002. • Question 24 4 out of 4 points A young child is taken to the OR to reduce a meconium plug bowel obstruction. A therapeutic enema is performed with fluoroscopy. The patient is in position and barium is instilled into the colon through the anus for the reduction. What CPT® code is reported by the independent radiologist for the radiological service? b. 74283-26 b. 74283-26 Response Feedback: Rationale: A therapeutic enema was performed with contrast (barium) to reduce the meconium plug (intraluminal obstruction). In the CPT® Index look for Enema/Therapeutic/for Intussusception directing you to 74283. The code description includes therapeutic enema with contrast for intraluminal obstruction. Modifier 26 denotes the professional service. • Question 25 4 out of 4 points A patient is positioned on the scanning table headfirst with arms at the side for an MRI of the thoracic spine and spinal canal. A contrast agent is used to improve the quality of the images. The scan confirms the size and depth of a previously biopsied leiomyosarcoma metastasized to the thoracic spinal cord. What CPT® and ICD-10-CM codes are reported? b. 72147, C79.49 b. 72147, C79.49 Response Feedback: Rationale: In the CPT® Index look for Magnetic Resonance Imaging (MRI)/Diagnostic/Spine/Thoracic for the code range 72146, 72147, 72157. Code 72147 describes an MRI of the thoracic spine with contrast. This is a secondary (metastasized) cancer to the thoracic spinal cord. Look in the ICD-10-CM Alphabetic Index for Leiomyosarcoma which states see also Neoplasm, connective tissue, malignant. In the ICD-10-CM Table of Neoplasms look for Neoplasm, neoplastic/connective tissue NEC/cord (true) (vocal)/spinal (thoracic) and select from the Malignant Secondary (column) you are guided to code C79.49. Sunday, November 19, 2017 9:21:49 AM MST • Question 1 10 out of 10 points The word “pathology” refers to the study of: c. Disease c. Disease Response Feedback: RATIONALE: The root word path means “disease”. The suffix ~logy is “study of”. • Question 2 10 out of 10 points A test determining the presence or absence of a substance is considered what type of test? a. Qualitative a. Qualitative Response Feedback: RATIONALE: A qualitative test determines the presence or absence of the substance. • Question 3 10 out of 10 points Which word describes the study of small life forms? d. Microbiology d. Microbiology Response Feedback: RATIONALE: The root words micro (small) and bio (life) combined with ~logy describe the study of small life forms. • Question 4 10 out of 10 points A woman has identified a lump in her right breast. After examination, the physician decides a biopsy is indicated. A specimen is sent for pathologic examination. The finding is carcinoma of the breast. What diagnosis is assigned for the pathologic examination? c. C50.911 c. C50.911 Response Feedback: RATIONALE: Always code the most specific diagnosis known. When a diagnosis of carcinoma of the breast has been confirmed, it is inappropriate to code a less specific diagnosis, no matter the reason for the original test. In the ICD-10-CM Alphabetic Index look for Carcinoma (malignant) (see also Neoplasm, by site, malignant). Go to the Table of Neoplasms, and look for Neoplasm, neoplastic/breast/Malignant Primary (column) C50.9-. Verification in the Tabular List indicates six characters are needed to complete the code. C50.911 for unspecified site on right breast. • Question 5 10 out of 10 points A patient has a history of prostate cancer with removal of the prostate and has completed radiation therapy with no recurrence for 2 years. A PSA is performed to check for any recurrence. The results show a PSA within normal limits. What diagnosis code(s) describe(s) this test? b. Z08, Z85.46 b. Z08, Z85.46 Response Feedback: RATIONALE: Per ICD-10-CM coding guideline I.C.21.c.8 follow-up codes are used to explain continuing surveillance following completed treatment of a disease, condition, or injury. They imply that the condition has been fully treated and no longer exists. The follow-up code is sequenced first followed by the history code. Look in the ICD-10-CM Alphabetic Index for Examination/follow-up (routine) (following)/radiotherapy NEC/malignant neoplasm directing you to Z08. Once cancer has been excised and there is no further treatment directed toward the cancer site without recurrence, code a personal history of malignancy code. Look for History/personal (of)/malignant neoplasm (of)/prostate directing you to Z85.46. Confirm codes in the Tabular List. According to AHA Coding Clinic (2000 Vol. 17 No.4) screening codes are not used for patients who have any sign or symptom of a suspected condition or history of a condition. • Question 6 10 out of 10 points A patient with rheumatoid arthritis takes Non-steroidal anti-inflammatory drugs (NSAIDs) to manage pain. He also has regular blood tests to verify he has not developed any liver problems due to his use of the NSAIDs. What code(s) describe(s) the need for the test when the results are normal (the patient has no symptoms of liver disease)? b. M06.9, Z79.1, Z51.81 b. M06.9, Z79.1, Z51.81 Response Feedback: RATIONALE: Code both the arthritis and the long-term use of NSAIDs. Look in the ICD-10-CM Alphabetic Index for Arthritis/rheumatoid, directing you to M06.9. For the next code, look for Therapy/drug, long term (current) (prophylactic)/anti-inflammatory directing you to Z79.1. There is an instructional note under category code Z79 to code also any therapeutic drug level monitoring with code Z51.81. This is found in the Alphabetic Index by looking for Monitoring (encounter for)/therapeutic drug level Z51.81. Verify these codes in the Tabular List and read any instructions provided. • Question 7 10 out of 10 points A patient with deep vein thrombosis requires heparin to maintain therapeutic anticoagulation levels. He has regular PTT’s drawn to monitor his level of anticoagulation. What code describes this testing? a. 85730 a. 85730 Response Feedback: RATIONALE: PTT stands for partial thromboplastin time. Look in the CPT® Index for PTT, you are directed to - See Thromboplastin, Partial Time directing you to 85730–85732. Checking the listing, 85730 Thromboplastin time, partial (PTT); plasma or whole blood is the correct code for this test. • Question 8 10 out of 10 points A patient with Acquired Immune Deficiency Syndrome (AIDS) presents for follow up care. A total T-cell count is ordered to evaluate progression of the disease. Choose the code(s) for this study. d. 86359 d. 86359 Response Feedback: RATIONALE: Code 86359 is for total T-cell count. If other studies were performed, they were not ordered and may not be billed, not matter how seemingly appropriate. Look in the CPT® Index for T-Cells/Count directs you to 86359. • Question 9 0 out of 10 points What is the code and any required modifier(s) for dipstick urinalysis, non-automated, without microscopy performed in a physician office for a Medicare patient? b. 81002-26-QW c. 81002 Response Feedback: RATIONALE: 81002 is for dipstick urinalysis. Modifier 26 is not needed in the physician office and QW is not required as this is not a CLIA waived test. Look in the CPT® Index for Urinalysis/Routine. • Question 10 10 out of 10 points A 27-year-old male dies of a gunshot wound. An autopsy is performed to gain evidence for the police investigation and any subsequent trial. What code describes this service? c. 88040 c. 88040 Response Feedback: RATIONALE: Services related to legal investigations and trials are forensic examinations. Look in the CPT® Index for Autopsy/Forensic Exam you are directed to 88040. Read the code to verify this as the correct listing. Sunday, November 19, 2017 9:22:06 AM MST • Question 1 4 out of 4 points A patient presents with worries she is at risk for cancer. She asks for tests to verify whether she has cancer. The test comes back normal. What type of service is this considered? a. Screening services a. Screening services Response Feedback: Rationale: Services performed when there are no symptoms and returning normal results are considered screening services. • Question 2 4 out of 4 points Tests in the Chemistry section of CPT® are what types of tests unless specified otherwise? c. Quantitative c. Quantitative Response Feedback: Rationale: The codes in the Chemistry section (82009-84999) identify how much of a substance is present in the specimen. According to the guidelines, “The examination is quantitative unless specified.” • Question 3 4 out of 4 points The suffix -ology means c. Study of c. Study of Response Feedback: Rationale: -ology means the study of. • Question 4 4 out of 4 points What modifier must always be applied to Medicare claims for tests performed in a site with a CLIA Waived certificate? b. QW b. QW Response Feedback: Rationale: Medicare requires that the QW modifier be applied for all claims for payment of test performed in a site with a CLIA waived certificate. If the location does not have a certificate, the service should not be billed and it should not be performed. Modifier QW is found in the HCPCS Level II codebook. • Question 5 4 out of 4 points HCPCS Level II codes specifically for Pathology and Laboratory services all start with what letter? d. P d. P Response Feedback: Rationale: In the HCPCS codebook, P2028-P9615 report Pathology and Laboratory Services including chemistry, toxicology and microbiology tests, screening Pap procedures and various blood products. • Question 6 4 out of 4 points A patient with AIDS presents for follow up care. The total T-cell count is ordered to evaluate any progression of the disease. What CPT® code(s) is/are reported? c. 86359 c. 86359 Response Feedback: Rationale: Code 86359 is for total T-cell count. If other studies were performed and they were not ordered they may not be billed, no matter how seemingly appropriate. In the CPT® Index, look for T Cells/Count. • Question 7 4 out of 4 points A 35 year-old type II diabetic is feeling weak. The physician performs a stat glucose test in which a finger stick is done placing the drop of blood on a reagent strip. The test indicates the patient is hypoglycemic. The physician gives the patient some glucose supplements and performs another stat glucose test using the same lab test as before 30 minutes later. The second test shows the glucose levels returned to normal. How are the lab tests reported? a. 82948, 82948-91 a. 82948, 82948-91 Response Feedback: Rationale: Look in the CPT® Index for Glucose/Blood Test referring you to codes 82947-82948, 82950. The lab test used a reagent strip for the glucose test reporting code 82948. Modifier 91 is the correct modifier to use when the same laboratory test is repeated on the same day for a subsequent result. • Question 8 0 out of 4 points A patient with abnormal growth had a suppression study that included 4 glucose tests and 4 human growth hormone tests. What CPT® code(s) is/are reported? c. 82947 x 4, 83003 x 4 d. 80430, 82947 Response Feedback: Rationale: Use the Evocative/Suppressive panel codes whenever all of the tests in the panel are performed. If extra tests are performed, these should be coded separately. In the CPT® Index, look for Growth Hormone/Growth Hormone Suppression Panel. Also, in the CPT® Index, look for Glucose/Blood test. Code descriptor for code 80430 indicates this should include Glucose (82947 X 3) and Human growth hormone (HGH) (83003 X 4). • Question 9 4 out of 4 points A patient has a severe traumatic fracture of the humerus. During the open reduction procedure, the surgeon removes several small pieces of bone embedded in the nearby tissue. They are sent to Pathology for examination without microscopic sections. The pathologist finds no evidence of disease. How should the pathologist code for his services? c. 88300 c. 88300 Response Feedback: Rationale: In the CPT® Index, look for Pathology and Laboratory/Surgical pathology/Gross Exam/Level I directing you to 88300. Examination without microscopic sections is coded 88300 for all types of specimens. Code 88304 includes both gross and microscopic exam. • Question 10 4 out of 4 points If the findings on examination of a Pap smear are normal and described as “negative for intraepithelial lesion or malignancy” this is an example of what type of results reporting? d. Bethesda d. Bethesda Response Feedback: Rationale: This is an example of reporting by the Bethesda method. In the CPT® Index, look for Bethesda System referring you to 88164-88167. On the page before this code range, read the Guidelines where it discusses the Bethesda & non-Bethesda reporting of Pap smears. • Question 11 4 out of 4 points A patient presents with right upper quadrant pain, nausea and other symptoms of liver disease as well as complaints of decreased urination. Her physician orders an albumin; bilirubin, both total and direct; alkaline phosphatase; total protein; alanine amino transferase; aspartate amino transferase, and creatinine. What CPT® code(s) is/are reported? a. 80076, 82565 a. 80076, 82565 Response Feedback: Rationale: Code the laboratory panel anytime all of the tests listed in the panel are completed. If additional tests are also performed, they are coded separately. In the CPT® Index, see Blood Tests/Panels/Hepatic Function. Also, see Creatinine/Blood. • Question 12 4 out of 4 points A lab test reveals an excessive level of alcohol in the blood. What ICD-10-CM code is reported? a. R78.0 a. R78.0 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Findings, abnormal, inconclusive, without diagnosis/in blood (of substance not normally found in blood)/alcohol (excessive level) R78.0. Verification in Tabular List confirms R78.0 is for finding of alcohol in blood. • Question 13 4 out of 4 points A patient has a cytopathology study performed by a fine needle aspiration. The results are quite unusual and the slides as well as a copy of pertinent information from the patient’s record are sent to another cytopathologist for consultation. The consulting pathologist reviews the slides and reviews the patient’s chart material. A report is sent back to the original pathologist with the findings. What CPT® code is reported? c. 80502 c. 80502 Response Feedback: Rationale: Pathology consultation with review of the patient’s record is coded 80502. The E/M consultation codes require a face-to-face encounter with the patient. In the CPT® Index, look for Consultation/Clinical Pathology directing you to 80502. • Question 14 4 out of 4 points What is the code and any required modifier(s) for dipstick urinalysis, automated, without microscopy performed in a physician office for a Medicare patient? a. 81003-QW a. 81003-QW Response Feedback: Rationale: 81003 is for dipstick urinalysis, automated, without microscopy. Modifier 26 is not needed in the physician office but QW is required as this is a CLIA waived test. In the CPT® Index, look for Urinalysis/Automated. Modifier QW is found in HCPCS Level II codebook. • Question 15 4 out of 4 points A patient has a cholecystectomy and a soft tissue lipoma removed during the same operative session. Both specimens were sent to pathology in separate containers are examined by the pathologist. What CPT® code(s) are reported? a. 88304 x 2 a. 88304 x 2 Response Feedback: Rationale: In the CPT® Index, look for Pathology and Laboratory/Surgical Pathology/Gross and Micro Exam. Under Gross and Micro Exam, Levels II-VI are listed. Read these codes to determine the correct code. Both of these specimens (gallbladder and soft tissue lipoma) are coded under 88304. Sometimes it is helpful to know the names of surgical procedure to select the correct pathology code. A cholecystectomy is excision of the gallbladder. • Question 16 4 out of 4 points A physician orders a quantitative FDP. What CPT® code is reported? c. 85379 c. 85379 Response Feedback: Rationale: Check for unfamiliar abbreviations in the Index. Read codes closely to identify whether they are quantitative, semi-quantitative or qualitative. In the CPT® Index, look for FDP, you are directed to See Fibrin Degradation Products, this refers you to See Pathology and Laboratory/Fibrin Degradation Products/Quantitative directing you to 85379. • Question 17 4 out of 4 points What is/are the code(s) for thawing 4 units of fresh frozen plasma? a. 86927 x 4 a. 86927 x 4 Response Feedback: Rationale: In the CPT® Index, look for Plasma/Frozen Preparation and you are directed to 86927. Code 86927 is specifically for plasma rather than whole blood. The code is used per unit with 86927 x 4 as correct. • Question 18 4 out of 4 points The code for sweat collection by iontophoresis can be found in what section of the Pathology Chapter of CPT®? d. Other Procedures d. Other Procedures Response Feedback: Rationale: The Other Procedures section includes codes for a number of miscellaneous procedures. Many of them are for analysis of substances found in other body substances and tissues. There are also a number of tests for specific conditions and diseases. In the CPT® Index, look for Iontophoresis/Sweat Collection referring you to 89230. Code 89230 is under the heading, Other Procedures. • Question 19 4 out of 4 points A patient with AIDS presents for follow up care. An NK (natural killer cell) total count is ordered. What CPT® code(s) is/are reported? d. 86357 d. 86357 Response Feedback: Rationale: Although there are a number of cells that attack viruses and other infectious organisms, NK cells are specifically identified by code 86357. In the CPT® Index, see Natural Killer (NK) Cells count. • Question 20 4 out of 4 points A patient will be undergoing a transplant and needs HLA tissue typing with DR/DQ multiple antigen and lymphocyte mixed culture. How will these services be coded? b. 86817, 86821 b. 86817, 86821 Response Feedback: Rationale: Code 86817 is the correct code to report for HLA tissue typing with DR/DQ. In the CPT® Index look for Tissue/Typing/Human Leukocyte Antigen (HLA)/Antibodies. Code 86821 is reported for the lymphocyte culture. This is indexed under Tissue/Typing/Lymphocyte Culture. Codes 86805 and 86806 are for lymphocytotoxicity, not lymphocyte mixed culture. • Question 21 4 out of 4 points A patient has partial removal of his lung which is sent in for gross and microscopic examination. The pathologist also did gross and microscopic exam on biopsies for several lymph nodes in the patient’s chest which are placed in one container. A consultation is performed on a tissue block of a single specimen intraoperatively by frozen section. The pathologist also performs a trichrome stain. What CPT® codes are reported for the lab tests performed? a. 88309, 88305, 88313, 88331 a. 88309, 88305, 88313, 88331 Response Feedback: Rationale: Separately code for each, the lung gross and microscopic lung examination (88309), the gross and microscopic lymph node biopsies (88305, it is only reported once because all the specimens from the one area is placed in one container), the frozen section pathology consultation on one tissue block and single specimen (88331), and for the special trichrome stain (88313). In the CPT® Index, see Pathology and Laboratory/Surgical Pathology/Level IV and Level VI. Also, see Consultation/Surgical Pathology/Intraoperative directing you to code range 88329-88334. Look in the CPT® Index for Pathology and Laboratory/Surgical Pathology/Staining 88312-88314. This is a trichome stain, so 88313 is reported. • Question 22 0 out of 4 points Esther Glass has a primary cancer located in the intra-hepatic biliary tract and had a cholecystectomy and biopsy of the duodenum done. Two separate specimens (gall bladder, biopsy of duodenum) were sent to the pathologist working at a hospital laboratory. The technician prepared the slides and the pathologist (self-employed) read them. Select the best code or codes for the pathologist’s services. c. 88304, 88305 a. 88304-26, 88305-26 Response Feedback: Rationale: Two different specimens from two different locations were sent to pathology. The first specimen is the gall bladder as evidenced by the documentation for cholecystectomy. Code 88304 is a level III specimen. Code 88305 corresponds to a level IV biopsy of the duodenum. In the CPT® Index, see Pathology and Laboratory/Surgical Pathology/Gross and Micro Exam. Modifier 26 is added to each code because the pathologist was not an employee of the hospital lab and provided the professional component only. • Question 23 4 out of 4 points A patient’s mother and sister have been treated for breast cancer. She has blood drawn for cancer gene analysis with molecular pathology testing. She has previously received genetic counseling. Blood will be tested for full sequence analysis and common duplication or deletion variants (mutations) in BRCA1, BRCA2 (breast cancer 1 and 2). What CPT® code is reported for this molecular pathology procedure? a. 81211 a. 81211 Response Feedback: Rationale: In the CPT® Index, look for Breast/Cancer Gene Analysis/BRCA1 (breast cancer 1) referring you to 81162, 81211-81215. The correct code is 81211. This is a blood test performed to look for any gene mutations affecting the BRCA1 and BRCA2 genes. These human genes are known as tumor suppressors, mutation of these genes has been linked to hereditary breast and/or ovarian cancer. A woman’s risk of developing breast or ovarian cancer is increased if she inherits this harmful mutation. Men with this mutation also have an increased risk of breast cancer. Be sure to read the parenthetical instructions. • Question 24 4 out of 4 points What ICD-10-CM code is reported for an abnormal cervical pap smear? b. R87.619 b. R87.619 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Abnormal, abnormality, abnormalities/Papanicolaou (smear)/cervix R87.619. Verification in the Tabular List confirms R87.619 is for unspecified abnormal cytological findings in specimens from cervix uteri. • Question 25 4 out of 4 points Flow cytometry is performed for DNA analysis. What CPT® code is reported? c. 88182 c. 88182 Response Feedback: Rationale: Flow cytometry is a cytopathologic study. Code 88182 specifies flow cytometry for DNA analysis. Look in the CPT® Index for Flow Cytometry. Sunday, November 19, 2017 9:22:21 AM MST • Question 1 10 out of 10 points John, a 16-year-old male, is admitted by the emergency department physician for observation after an ATV accident. The patient is discharge from observation by another provider the next day. What category or subcategory of evaluation and management codes would be selected for the emergency department physician? d. Initial observation care d. Initial observation care Response Feedback: Rationale: The patient presented to the Emergency Department and was admitted to observation by the ED physician. The guidelines for Initial Observation Care state that all services provided by the admitting physician for the same date of service are included in the initial hospital care, and in this instance the emergency department services would not be coded. If the patient was discharged on the same date of service, a code from Observation or Inpatient Care Services (Including Admission and Discharge Services) would be selected. • Question 2 0 out of 10 points Dr. Hedrick, a neurosurgeon, was asked to assist in a surgery to remove cancer from the spinal cord. He acted as a co-surgeon working with an orthopedic surgeon. Dr. Hedrick followed up with the patient during his rounds at the hospital the next day. From what category or subcategory of evaluation and management services would Dr. Hedrick's follow up visit be reported? b. Inpatient consultation c. Non-billable Response Feedback: Rationale: The follow-up visit from the neurosurgeon the day following surgery bundled in the surgical procedure an not billable. The visit is within the global period of the procedure. • Question 3 10 out of 10 points The patient presents to the clinic today for a follow-up of his hospitalization for pneumonia. He was placed back on Singulair® and has been improving with his breathing since then. He has no complaints today. What is the level of history? a. Problem focused a. Problem focused Response Feedback: Rationale: History HPI Location Severity Timing Modifying Factors Quality Duration Context Assoc Signs & Symptoms Brief (1-3) Brief (1-3) Extended (4 or more) Extended (4 or more) ROS Const GI Integ Hem/lymph Eyes GU Neuro All/Immuno Card/Vasc Musculo Psych All other negative Resp ENT, mouth Endo None Pertinent to problem (1 system) Extended (2-9 systems) Complete PFSH Past history (current meds, past illnesses, operations, injuries, treatments) Family history (a review of medical events in the patient's family) Social history (an age appropriate review of past and current activities) None None Pertinent (1 history area) Complete (2 (est) or 3 (new) history areas) Problem Focused Expanded Problem Focused Detailed Comprehensive CC: Follow-up of hospitalization for pneumonia. HPI: Modifying Factor: He was placed back on Singulair® and has been improving with his breathing since then. ROS: None PFSH: None • Question 4 0 out of 10 points Emergency Department A 47 year-old white male presents to the emergency department after the four-wheeler he was operating struck a ditch and rapidly came to a halt. This threw him against the windshield where he struck the mid part of his face and lower lip. This resulted in lip and chin lacerations. He is evaluated by Dr. Jones and a CT scan suggests a hyper dense abnormality within the brain. A bleed could not be ruled out and an inpatient hospital admission is recommended. His past history includes previous tonsillectomy, previous hospital admission for a syncopal episode associated with pain in the groin area, and hypercholesterolemia. He has no known allergies. His current medications are Zocor® and Accutane®. He is a non-smoker and a moderate drinker of alcohol. The review of systems is negative for nausea, vomiting, blurred vision, or headache. What is the level of history? c. Detailed b. Expanded problem focused Response Feedback: Rationale: History HPI Location Severity Timing Modifying Factors Quality Duration Context Assoc Signs & Symptoms Brief (1-3) Brief (1-3) Extended (4 or more) Extended (4 or more) ROS Const GI Integ Hem/lymph Eyes GU Neuro All/Immuno Card/Vasc Musculo Psych All other negative Resp ENT, mouth Endo None Pertinent to problem (1 system) Extended (2-9 systems) Complete PFSH Past history (current meds, past illnesses, operations, injuries, treatments) Family history (a review of medical events in the patient's family) Social history (an age appropriate review of past and current activities) None None Pertinent (1 history area) Complete (2 (est) or 3 (new) history areas) Problem Focused Expanded Problem Focused Detailed Comprehensive CC: ATV accident HPI: Context - ATV accident Location - Lip and chin lacerations ROS: GI - Negative for nausea and vomiting Eyes - Negative for blurred vision Neuro - Negative for headache PFSH: Past history - surgeries and illnesses reviewed, current meds Social history - Nonsmoker, moderate alcohol Note: Only 2 of 3 PFSH are needed for complete for Emergency Department, but all three are needed for a complete PFSH for a hospital admit. • Question 5 10 out of 10 points Physical Exam: CONSTITUTIONAL: Vital Signs: Pulse: 161. Resp: 30. Temp: 102.4. Oxygen saturation 90% GENERAL APPEARANCE: The patient reveals profound mental retardation. Tracheostomy is in place. EYES: Conjunctivae are slightly anemic. ENT: Oral mucosa is dry. NECK: The neck is supple and the trachea is midline. Range of motion is normal. There are no masses, crepitus or tenderness of the neck. The thyroid gland has no appreciable goiter. RESPIRATORY: The lungs reveal transmitted upper airway signs and bilateral rales, wheezes and rhonchi. CARDIOVASCULAR: The chest wall is normal in appearance. Regular rate and rhythm. No murmurs, rubs or gallops are noted. There is no significant edema to the lower extremities. GASTROINTESTINAL: The abdomen is soft and nondistended. There is no tenderness, rebound or guarding noted. There are no masses. No organomegaly is appreciated. SKIN: The skin is pale and slightly diaphoretic. NEUROLOGIC: Cranial nerves appear intact. The patient moves all 4 extremities symmetrically. No lateralizing signs are noted. Gross sensation is intact to all extremities. LYMPHATIC: There are no palpable pathologic lymph nodes in the neck or axilla. MUSCULOSKELETAL: Gait and station are normal. Strength and tone to the upper and lower extremities are normal for age with no evidence of atrophy. There is no cyanosis, clubbing or edema to the digits. What is the level of exam? d. Comprehensive d. Comprehensive Response Feedback: Rationale: Organ Systems: Constitutional, Eyes, ENMT, Respiratory, Cardiovascular, Gastrointestinal, Integumentary, Neurologic, Lymphatic, Musculoskeletal. Ten organ systems were examined. The level of exam is Comprehensive. • Question 6 0 out of 10 points Physical Exam: GENERAL APPEARANCE: Healthy appearing individual in no distress ABDOMEN: Soft, non-tender, without masses. No CVA tenderness FEMALE EXAM: VULVA/LABIA MAJORA: No erythema, ulcerations, swelling, or lesions seen. BARTHOLIN GLANDS: No cysts, abscesses, induration, discharge, masses, or inflammation noted. SKENE’S: No cysts, abscesses, induration, discharge, masses, or inflammation noted. CLITORIS/LABIA MINORA: Clitoris normal. No atrophy, adhesions, erythema, or vesicles noted. Labia unremarkable. URETHRAL MEATUS: Meatus appears normal in size and location. No masses, lesions or prolapse. URETHRA: No masses, tenderness or scarring. BLADDER: Without fullness, masses or tenderness. VAGINA: Mucosa clear without lesions, Pelvic support normal. No discharge. CERVIX: The cervix is clear, firm and closed. No visible lesions. No abnormal discharge. UTERUS: Uterus non-tender and of normal size, shape and consistency. Position and mobility are normal. ADNEXA/PARAMETRIA: No masses or tenderness noted. Based on the 1995 documentation guidelines, what is the level of exam? d. Detailed c. Comprehensive Response Feedback: Rationale: Organ Systems: The documentation supports a comprehensive/complete single system (Female Genitourinary) exam. The level of exam is Comprehensive. • Question 7 0 out of 10 points ED Visit: Data: BUN 74, creatinine 8.8, K 4.9, HGB 10.8, Troponin 0.01. I reviewed the EKG which shows some LVH but no ST changes. I also reviewed the chest x-ray, which showed moderate pulmonary vascular congestion, but no infiltrate. Impression: New problem of pulmonary edema due to hypervolemia. No evidence of acute MI or unstable angina. The patient also has ESRD which is stable and poorly controlled HTN, which is most likely due to hypervolemia. Plan: I spoke with the dialysis unit. We can get him in for an early treatment this afternoon as opposed to having to wait for his usual shift tomorrow. For that reason, it is okay to discharge him from the ED, to go directly to the unit. What is the level of medical decision making? c. Moderate d. High Response Feedback: Rationale: New problem to examiner, additional workup - dialysis (four points); Labs, EKG, and X-ray reviewed (three points); risk is High (chronic illness posing a threat to life). The medical decision making is High. • Question 8 0 out of 10 points IMPRESSION: Right recurrent gynecomastia. PLAN: The patient had a right breast ultrasound on November 17, which showed a hypoechoic area measuring 1.7 x 0.7 x 1.2 cm in the 11 o’clock position of the right breast. There was no Doppler flow, and the transmission suggested that this was a cystic lesion. Follow-up in a month was suggested at that time. Because of this ultrasound and because this is symptomatic, I have recommended a simple mastectomy under general anesthesia. The patient is in agreement. I filled out the prison forms requesting permission, and I described the operation to the patient. What is the level of medical decision making? d. High b. Low Response Feedback: Rationale: Established problem worsening (two points); ultrasound reviewed (one point), risk is moderate (simple mastectomy). The medical decision making is Low. • Question 9 10 out of 10 points A patient is admitted to the hospital for a lung transplant. The admitting physician performs a comprehensive history, a comprehensive exam, and a high level of medical decision making. What CPT® code is the appropriate E/M code for this visit? c. 99223 c. 99223 Response Feedback: Rationale: Initial hospital care codes require all three key components be met to determine a level of visit. In this case, the comprehensive history and exam, and the high level of medical decision making support a 99223. • Question 10 10 out of 10 points An established patient is seen in clinic for allergic rhinitis. A problem focused history, expanded problem focused exam, and a low level of medical decision making are performed. What E/M code is reported for this visit? b. 99213 b. 99213 Response Feedback: Rationale: Established patient codes require two of three key components be met to determine a level of visit. In this case, the expanded problem focused exam and low level of medical decision making support a level 3 established patient office visit 99213. Sunday, November 19, 2017 9:22:37 AM MST • Question 1 10 out of 10 points During a soccer game, Ashley, a 26-year-old female, heard a popping sound in her knee. Her knee has been unstable since the incident and she decided to consult an orthopedist. She visits Dr. Howard, an orthopedist she has not seen before, to evaluate her knee pain. Dr. Howard's diagnosis is a torn ACL. From what category or subcategory of evaluation and management code would be selected for the visit to Dr. Howard? a. Office visit, new patient a. Office visit, new patient Response Feedback: Rationale: Consultations performed at the request of a patient are coded using office visit codes. Because the patient has not seen Dr. Howard before, this would be considered a new patient visit. • Question 2 10 out of 10 points Dr. Hedrick, a neurosurgeon, was asked to assist in a surgery to remove cancer from the spinal cord. He acted as a co-surgeon working with an orthopedic surgeon. Dr. Hedrick followed up with the patient during his rounds at the hospital the next day. From what category or subcategory of evaluation and management services would Dr. Hedrick's follow up visit be reported? c. Non-billable c. Non-billable Response Feedback: Rationale: The follow-up visit from the neurosurgeon the day following surgery bundled in the surgical procedure an not billable. The visit is within the global period of the procedure. • Question 3 0 out of 10 points Established patient CHIEF COMPLAINT: Fever. PRESENT ILLNESS: The patient is a 2 year 3 month-old female with less than 1 day of a high fever with decreased appetite. There has been no vomiting or diarrhea. Parents are unaware of any cough. Tylenol has been given which reduced the fever. PAST MEDICAL HISTORY: Otherwise negative. CURRENT MEDICATIONS; Tylenol® 160 mg q.4 h. per infant Tylenol® drops. ALLERGIES; NONE. IMMUNIZATIONS: Up to date. REVIEW OF SYSTEMS: As per HPI. Rest of review of systems reviewed and negative. PERSONAL, FAMILY, SOCIAL HISTORY: The patient is not exposed to secondhand cigarette smoke. What is the level of history? c. Detailed d. Comprehensive Response Feedback: Rationale: History HPI Location Severity Timing Modifying Factors Quality Duration Context Assoc Signs & Symptoms Brief (1-3) Brief (1-3) Extended (4 or more) Extended (4 or more) ROS Const GI Integ Hem/lymph Eyes GU Neuro All/Immuno Card/Vasc Musculo Psych All other negative Resp ENT, mouth Endo None Pertinent to problem (1 system) Extended (2-9 systems) Complete PFSH Past history (current meds, past illnesses, operations, injuries, treatments) Family history (a review of medical events in the patient's family) Social history (an age appropriate review of past and current activities) None None Pertinent (1 history area) Complete (2 (est) or 3 (new) history areas) Problem Focused Expanded Problem Focused Detailed Comprehensive CC: Fever HPI: Duration - Less than one day Severity - High fever Associated signs and symptoms - Decreased appetite Modifying factor - Tylenol® has been given which reduced the fever. ROS: GI - No vomiting or diarrhea Resp - Parents unaware of any cough Rest of review of systems reviewed and negative: Complete ROS PFSH: Personal history - Current meds Social history - Not exposed to second hand smoke e • Question 4 0 out of 10 points HISTORY OF PRESENT ILLNESS A 73-year-old man who is a veterinarian is seen here for the first time today. He has a history of squamous cell carcinoma on the left arm and a basal cell carcinoma on the right forehead near the temple, both in January 20XX. He says he has had a lesion on his forehead for approximately one year. He is concerned about what it is and thinks it may be another skin cancer. He is also concerned about another lesion that has been present for a while, just lateral to his right eye. He would also like a full skin check today. He uses a hat for sun protection. He has lived in California and has had significant sun exposure in the past. REVIEW OF SYSTEMS: Otherwise well, no other skin complaints. PAST MEDICAL HISTORY Coronary artery disease status post bypass surgery, history of squamous and basal cell carcinomas as noted above, hay fever, and hyperlipidemia. He has had lipomas removed. MEDICATIONS: Tylenol, tramadol, thyroxin, fish oil, flax seed oil, simvastatin, Zyrtec®, 5% saline in eyes. ALLERGIES: No known drug allergies. FAMILY HISTORY: No family history of skin cancer or other skin problems. SOCIAL HISTORY: Patient is a veterinarian. He recently moved to the Rochester area from Pennsylvania. He is married. What is the level of history? c. Detailed b. Expanded problem focused Response Feedback: Rationale: History HPI Location Severity Timing Modifying Factors Quality Duration Context Assoc Signs & Symptoms Brief (1-3) Brief (1-3) Extended (4 or more) Extended (4 or more) ROS Const GI Integ Hem/lymph Eyes GU Neuro All/Immuno Card/Vasc Musculo Psych All other negative Resp ENT, mouth Endo None Pertinent to problem (1 system) Extended (2-9 systems) Complete PFSH Past history (current meds, past illnesses, operations, injuries, treatments) Family history (a review of medical events in the patient’s family) Social history (an age appropriate review of past and current activities) None None Pertinent (1 history area) Complete (2 (est) or 3 (new) history areas) Problem Focused Expanded Problem Focused Detailed Comprehensive CC: Skin lesions HPI: Location – Forehead and lateral to right eye Duration – About a year ROS: Integumentary – No other skin complaints Stated, “Otherwise well”, this is not an indication that all other systems were reviewed. PFSH: Past, Family, and Social all reviewed as it relates to skin. • Question 5 10 out of 10 points Physical Exam: General/Constitutional: No apparent distress. Well nourished and well developed. Ears: TM’s gray. Landmarks normal. Positive light reflex. Nose/Throat: Nose and throat clear; palate intact; no lesions. Lymphatic: No palpable cervical, supraclavicular, or axillary adenopathy. Respiratory: Normal to inspection. Lungs clear to auscultation. Cardiovascular: RRR without murmurs. Abdomen: Non-distended, non-tender. Soft, no organomegaly, no masses. Integumentary: No unusual rashes or lesions. Musculoskeletal: Good strength; no deformities. Full ROM all extremities. Extremities: Extremities appear normal. What is the level of exam? d. Comprehensive d. Comprehensive Response Feedback: Rationale: Organ Systems: Constitutional, ENMT, Lymphatic, Respiratory, Cardiovascular, Gastrointestinal, Skin, Musculoskeletal. There are 8 organ systems examined. The level of exam is Comprehensive. • Question 6 0 out of 10 points Physical Exam: GENERAL: His physical exam shows an intubated male. He is at times somewhat combative. There is a brace on the right shoulder. SKIN: His skin is warm and dry. No rashes, ulcers or lesions. LUNGS: The lungs are diminished breath sounds, though no crackles are noted. CARDIAC: Cardiac exam is tachycardic, no distinct murmurs appreciated. Extremities show no significant edema. ABDOMEN: Abdominal exam is soft. No masses or tenderness. No hepatosplenomegaly. EXTREMITIES: No clubbing or cyanosis. Bilateral lower. No misalignment or tenderness. Based on the 1995 documentation guidelines, what is the level of exam? b. Expanded problem focused c. Detailed Response Feedback: Rationale: Organ Systems: Constitutional, Skin, Respiratory, Cardiovascular, Gastrointestinal, and Musculoskeletal. There are six organ systems examined with detailed documentation. The level of exam is Detailed. • Question 7 10 out of 10 points ED Visit: Data: BUN 74, creatinine 8.8, K 4.9, HGB 10.8, Troponin 0.01. I reviewed the EKG which shows some LVH but no ST changes. I also reviewed the chest x-ray, which showed moderate pulmonary vascular congestion, but no infiltrate. Impression: New problem of pulmonary edema due to hypervolemia. No evidence of acute MI or unstable angina. The patient also has ESRD which is stable and poorly controlled HTN, which is most likely due to hypervolemia. Plan: I spoke with the dialysis unit. We can get him in for an early treatment this afternoon as opposed to having to wait for his usual shift tomorrow. For that reason, it is okay to discharge him from the ED, to go directly to the unit. What is the level of medical decision making? d. High d. High Response Feedback: Rationale: New problem to examiner, additional workup - dialysis (four points); Labs, EKG, and X-ray reviewed (three points); risk is High (chronic illness posing a threat to life). The medical decision making is High. • Question 8 0 out of 10 points Established patient CHIEF COMPLAINT: Gallstones and reflux. HISTORY OF PRESENT ILLNESS: This is a 61 year-old woman who comes back to see me today with a 2-year history of severe gallbladder attacks. Also of note, she has had ongoing reflux problems for many years. Within the last few months, her reflux has worsened. ASSESSMENT/PLAN: This is a 61 year-old woman with likely symptomatic cholelithiasis and reflux. Her number one concern right now is the gallbladder attacks. This sounds like symptomatic cholelithiasis. As a result, we recommended for her to have laparoscopic cholecystectomy with intraoperative cholangiogram. The risks and benefits were explained to the patient who understood and agrees for us to proceed. With regards to her reflux, it is partially controlled by her medication. She also is overweight and might have symptom improvement after weight loss. She is also very hesitant to proceed with the Nissan fundoplication because her husband had the surgery done before and had some problems with vomiting afterwards. She does have objective evidence of reflux as well and is a good candidate for surgery. However, we will let her decide whether she wants to proceed with surgery or not. What is the level of medical decision making? d. High c. Moderate Response Feedback: Rationale: Two problems worsening (4 points). No data reviewed with moderate risk (elective major surgery). The medical decision making is Moderate. • Question 9 10 out of 10 points A patient is admitted to the hospital for a lung transplant. The admitting physician performs a comprehensive history, a comprehensive exam, and a high level of medical decision making. What CPT® code is the appropriate E/M code for this visit? c. 99223 c. 99223 Response Feedback: Rationale: Initial hospital care codes require all three key components be met to determine a level of visit. In this case, the comprehensive history and exam, and the high level of medical decision making support a 99223. • Question 10 10 out of 10 points An established patient is seen in clinic for allergic rhinitis. A problem focused history, expanded problem focused exam, and a low level of medical decision making are performed. What E/M code is reported for this visit? b. 99213 b. 99213 Response Feedback: Rationale: Established patient codes require two of three key components be met to determine a level of visit. In this case, the expanded problem focused exam and low level of medical decision making support a level 3 established patient office visit 99213. Sunday, November 19, 2017 9:22:49 AM MST • Question 1 4 out of 4 points If the pain is sharp, stabbing or dull, what is the component of the History of Present Illness (HPI)? c. Quality c. Quality Response Feedback: Rationale: Quality describes a problem’s characteristics. Sharp, stabbing or dull refer to the characteristics of pain. • Question 2 4 out of 4 points Fred is fishing at the local area lake while on vacation. He gets lightheaded and dizzy and goes to the local hospital Emergency Department. He’s evaluated by the ED provider. This is the first time he has been to this hospital. What subsection is used to report the ED visit? a. Emergency Department Services a. Emergency Department Services Response Feedback: Rationale: No distinction is made between new and established patients in the emergency department. Evaluation and Management services provided in an Emergency Department are reported with codes from the Emergency Department Services Subsection 99281-99285. • Question 3 4 out of 4 points Where are clinical examples for evaluation and management codes found in CPT®? a. Appendix C a. Appendix C Response Feedback: Rationale: Appendix C of CPT® contains clinical examples of evaluation and management codes. The appendix may be used in addition to the E/M code descriptors. • Question 4 4 out of 4 points What modifier is used to report an evaluation and management service mandated by a court order? a. 32 a. 32 Response Feedback: Rationale: Modifier 32 is used for services related to mandated consultation and/or related services by a third party payer, governmental, legislative or regulatory requirements. • Question 5 0 out of 4 points A PCP transfers a patient to a cardiologist for management of the patient’s congestive heart failure. The cardiologist examines the patient, discusses treatment options and schedules a stress test for this new patient. A report is sent to the PCP detailing the findings of the office visit, results of the stress test and intent to manage and treat the congestive heart failure. An E/M code would be selected from what subcategory for the cardiologist? a. Office consultation c. New patient office visit Response Feedback: Rationale: The PCP transferred the patient to the cardiologist to manage/treat the congestive heart failure. The cardiologist accepted the transfer of care of the patient and sent a letter to the PCP with findings of the first visit and stress test. This would be coded as a new patient since the cardiologist accepted the patient and is taking over the care of a specific problem. • Question 6 4 out of 4 points A 75 year-old established patient sees his regular primary care provider for a physical screening prior to joining a group home. He has no new complaints. The patient has an established diagnosis of cerebral palsy and type 2 diabetes and is currently on his meds. A comprehensive history and examination is performed. The provider counsels the patient on the importance of taking his medication and gives him a prescription for refills. Blood work was ordered. PPD was done and flu vaccine given. Patient already had a vision exam. No abnormal historical facts or finding are noted. What CPT® code is reported? d. 99397 d. 99397 Response Feedback: Rationale: According to CPT® guidelines Preventive Medicine Services codes provide a means to report a routine or periodic history and physical examination in asymptomatic individuals. They include only those evaluation and management services related to the age specific history and examination provided by the provider. The patient is here for a preventive service. He did not have any complaints and the provider did not identify any new problems. In the CPT® Index look for Preventive Medicine/Established Patient. You are referred to 99382-99397. The code selection is based on age. Code 99397 is the correct code for a patient who is older than 65 years. • Question 7 4 out of 4 points Mr. Flintstone is seen by his oncologist just two days after undergoing extensive testing for a sudden onset of petechiae, night sweats, swollen glands and weakness. After a brief review of history, Dr. B. Marrow re-examines Mr. Flintstone. The exam is documented as expanded problem focused and the medical decision making of moderate complexity. The oncologist spends an additional 45 minutes discussing Mr. Flintstone’s new diagnosis of Hodgkin’s lymphoma, treatment options and prognosis. What is/are the appropriate procedure code(s) for this visit? b. 99213, 99354 b. 99213, 99354 Response Feedback: Rationale: This is an established patient. Two of the three key elements are required for an established patient. An expanded problem focused exam and moderate MDM meet or exceed the requirement for code 99213. The provider spent an additional 45 minutes with the patient discussing the patient’s new diagnosis. Prolonged Service codes 99354-99357 are used when provider or other qualified heath care professional provides prolonged service involving direct patient contact that is provided beyond the usual service. The codes reported based on the place of service and total time. Codes 99213 and add-on code 99354 are used to report the services. • Question 8 0 out of 4 points A pediatrician is asked to be in the room during the delivery of a baby at risk for complications. The pediatrician is in the room for 45 minutes. The baby is born and is completely healthy, not requiring the services of the pediatrician. What CPT® code(s) is/are reported by the pediatrician? c. 99360 x 2 a. 99360 Response Feedback: Rationale: The physician provider standby services. In the CPT® Index look for Standby Services and you are directed to 99360. 99360 is reported based on time. Each 30 minutes is reported if only the entire 30 minutes is met. 99360 with 1 unit is the correct code choice. • Question 9 4 out of 4 points A new patient visits the internal medicine clinic today for diabetes, chronic constipation, arthritis and a history of cardiac disease. The provider performs a detailed history, comprehensive exam and a medical decision making of moderate complexity. What CPT® code is reported? c. 99203 c. 99203 Response Feedback: Rationale: In the CPT® Index look for Office and/or Other Outpatient Services/Office Visit/New Patient and you are directed to codes 99201-99205. For New Patient visits, all three key components must be met. This service supports a level 3 new patient visit, 99203. • Question 10 4 out of 4 points A 10 year-old girl is scheduled for her yearly physical with her pediatrician. At the time of the visit, the patient complains of watery eyes, scratchy throat and stuffy nose for the past two days. The provider performs the physical. He also performs an expanded problem history and exam and treats the patient for a URI. What CPT® code(s) is/are reported for this visit? c. 99393, 99213-25 c. 99393, 99213-25 Response Feedback: Rationale: The physical exam code is selected from the Preventive Medicine Services and selected based on whether the patient is new or established and by age. The pediatrician also evaluates and treats the URI. The additional work for the URI allows us to report an established patient office visit. Modifier 25 is appended to the office visit to show it is a significant and separately identifiable service from the preventive visit. • Question 11 4 out of 4 points The attending provider at the hospital spent 25 minutes with the patient in the morning and another 15 in the afternoon examining the patient, writing discharge orders and giving discharge instructions to the patient. What CPT® code is reported for the discharge? a. 99239 a. 99239 Response Feedback: Rationale: In the CPT® Index look for Hospital Services/Inpatient Services/Discharge Services and you are directed to code ranges 99238-99239 and 1110F-1111F. Codes 1110F-1111F are Category II supplemental codes used for performance measurement. They may not be used as a substitute for Category I codes. Codes 99238-99239 are based on time. All of the time spent by the discharge provider on the discharge date is included in the time. The provider spent a total of 40 minutes with the patient on the discharge date. 99239 is the correct code choice. • Question 12 4 out of 4 points After moving across country, Ms. Robbins took her 2 year-old daughter to a new pediatric clinic for an annual physical. The provider completed an age / gender appropriate history, exam, and provided anticipatory guidance. He ordered no additional tests or immunizations. What CPT® code is reported? c. 99382 c. 99382 Response Feedback: Rationale: This is a new patient to the pediatric clinic. Look in the CPT® Index for Preventive Medicine/New Patient and you are directed to code range 99381-99387. The code selection is based on age. Code 99382 is for ages 1-4 making it the correct code choice. • Question 13 4 out of 4 points What ICD-10-CM code is reported for vertigo? b. R42 b. R42 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for vertigo. There are many different subentries for the type of vertigo; however, the type of vertigo is not specified. R42 is the default code for vertigo. Verify code selection in the Tabular List. • Question 14 4 out of 4 points A 32 year-old patient sees Dr. Smith for a consult at the request of his PCP, Dr. Long, for an ongoing problem with allergies. The patient has failed Claritin and Alavert and feels his symptoms continue to worsen. Dr. Smith performs an expanded problem focused history and exam and discusses options with the patient on allergy management. The MDM is straightforward. The patient agrees he would like to be tested to possibly gain better control of his allergies. Dr. Smith sends a report to Dr. Long thanking him for the referral and includes the date the patient is scheduled for allergy testing. Dr. Smith also includes his findings from the encounter. What E/M code is reported? c. 99242 c. 99242 Response Feedback: Rationale: The three R’s of consultation are documented (request, render, reply). The consultation code range is 99241-99245 and applies to new or established patients. Consultations require three key components. The documentation states the history and exam were expanded problem focused and the MDM is straightforward. These three key elements meet the requirement for 99242. • Question 15 4 out of 4 points What ICD-10-CM code is reported for angina pectoris with a documented spasm? d. I20.1 d. I20.1 Response Feedback: Rationale: Look in the ICD-10-CM Alphabetic Index for Angina (attack) (cardiac) (chest) (heart) (pectoris) (syndrome) (vasomotor)/with/documented spasm which directs you to I20.1. Verify code selection in the Tabular List. • Question 16 4 out of 4 points A 28 year-old female patient is returning to her provider’s office with complaints of RLQ pain and heartburn with a temperature of 100.2. The provider performs a detailed history, detailed exam and determines the patient has mild appendicitis. The provider prescribes antibiotics to treat the appendicitis in hopes of avoiding an appendectomy. What are the correct CPT® and ICD-10-CM codes for this encounter? a. 99214, K37, R12 a. 99214, K37, R12 Response Feedback: Rationale: This is an established patient E/M level of service due to the indication she returning to her provider for the visit. Code 99214 is appropriate when two of the three key components are met for an established patient. According to the ICD-10-CM guidelines I.B.4., a definitive diagnosis is reported when it has been established. Look in the ICD-10-CM Alphabetic Index for Appendicitis which directs you to K37. Guideline I.B.5 indicates any signs or symptoms that would be an integral part of that definitive diagnosis/disease process would not be separately reported. Heartburn is not a symptom commonly seen with appendicitis so we can report this as an additional code, refer to guideline I.B.6. Look in the Alphabetic Index for Heartburn which directs you to R12. Verification in the Tabular List confirms code selections. • Question 17 0 out of 4 points A 90 year-old female was admitted this morning from observation status for chest pain to r/o angina. A cardiologist performs a comprehensive history and comprehensive exam. Her chest pain has been relieved with the nitroglycerin drip given before admission and she would like to go home. Doctor has written prescriptions to add to her regimen. He had given her Isosorbide, and she is tolerating it well. He will go ahead and send her home. We will follow up with her in a week. Patient was admitted and discharged on the same date of service. What CPT® code is reported? a. 99217 d. 99235 Response Feedback: Rationale: This patient was admitted and discharged on the same date of service from observation status. According to CPT® guidelines for Observation or Inpatient Care Services (Including Admission and Discharge Services), services for a patient admitted and discharged on the same date of service is reported by one code. For a patient admitted and discharged from observation or inpatient status on the same date, codes 99234-99236 is reported as appropriate.” The provider performed a comprehensive history, comprehensive exam and moderate MDM (New problem to the examiner, 0 data points and moderate risk). The correct code is 99235. • Question 18 0 out of 4 points An infant is born six weeks premature in rural Arizona and the pediatrician in attendance intubates the child and administers surfactant in the ET tube while waiting in the ER for the air ambulance. During the 45-minute wait, he continues to bag the critically ill patient on 100 percent oxygen while monitoring VS, ECG, pulse oximetry and temperature. The infant is in a warming unit and an umbilical vein line was placed for fluids and in case of emergent need for medications. How is this coded? c. 99471-25, 94610, 36510 d. 99291-25, 31500, 36510, 94610 Response Feedback: Rationale: When neonatal services are provided in the outpatient setting, Inpatient Neonatal Critical Care guidelines direct the coder to use critical care codes 99291 Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes and 99292 … each additional 30 minutes (List separately in addition to code for primary service). Care is documented as lasting 45 minutes with the physician in constant attendance. The physician also administered intrapulmonary surfactant (94610), placed an umbilical vein line (36510) and intubated the patient (31500). According to CPT® Critical Care Services guidelines these procedures are not included in the critical care codes. Therefore, they can be reported separately in addition to critical care services with modifier 25 appended to code 99291. • Question 19 4 out of 4 points Subjective: 6 year-old girl twisted her arm on the playground. She is seen in the ED complaining of pain in her wrist. Objective: Vital Signs: stable. Wrist: Significant tenderness laterally. X-ray is normal Assessment: Wrist sprain Plan: Over the counter Anaprox. Give twice daily with hot packs. Recheck if no improvement. What is the E/M code for this visit? b. 99281 b. 99281 Response Feedback: Rationale: Emergency Department services must meet or exceed three of the three key components. The provider performed a problem focused history (brief HPI, no ROS, no PFSH), a problem focused exam (one body area is examined) and low MDM (for one new problem to the examiner, one data point for the X-ray, and low level of risk). The problem focused history and exam lead us to select 99281 as the appropriate code. • Question 20 0 out of 4 points An established patient presents to the clinic today for a follow-up of his pneumonia. He was hospitalized for 6 days on IV antibiotics. He was placed back on Singulair and has been doing well with his breathing since then. An expanded problem focused exam was performed. Records were obtained from the hospital and the provider reviewed the labs and X-rays. The patient was told to continue antibiotics for another two weeks to 20 days, and the prescription Keteck was replaced with Zithromax. Patient is to return to the clinic in two weeks for recheck of his breathing and follow up X-ray. What CPT® code is reported? d. 99242 a. 99213 Response Feedback: Rationale: The patient was seen in the clinic which is an outpatient service. The provider performed a problem focused history (brief HPI, no ROS, and pertinent PFSH) + expanded problem focused exam + moderate MDM (new problem to examiner, three data points and acute illness with systemic symptoms and prescription drug management). Established patient office visits require two of three components be met. Code 99213 is the appropriate code for this visit. • Question 21 0 out of 4 points Dr. Inez discharges Mr. Blancos from the pulmonary service after a bout of pneumococcal pneumonia. She spends 45 minutes at the bedside explaining to Mr. Blancos and his wife the medications and IPPB therapy she ordered. Mr. Blancos is a resident of the Shady Valley Nursing Home due to his advanced Alzheimer’s disease and will return to the nursing home after discharge. On the same day Dr. Inez re-admits Mr. Blancos to the nursing facility. She obtains a detailed interval history, does comprehensive examination and the medical decision making is moderate complexity. What is/are the appropriate evaluation and management code(s) for this visit? d. 99238, 99305 a. 99239, 99304 Response Feedback: Rationale: Hospital discharge is a time-based code. The documentation states that the provider spent 45 minutes discharging the patient. In the CPT® Index look for Hospital Services/Discharge Services. Code 99239 is for 30 minutes or more. Upon discharge the patient was readmitted to a skilled nursing facility (SNF) where he is a resident. CPT® guidelines preceding the Initial Nursing Facility Care codes state when a patient is discharged from the hospital on the same day and readmitted to a nursing facility both the discharge and readmission is reported. Initial nursing facility care codes require the three key components to meet or exceed the requirements. Documentation tells us the physician provided a detailed history, comprehensive exam, and medical decision making was of moderate complexity. Code 99304 states the history and exam can be detailed or comprehensive. Our documentation shows it to be of moderate complexity, which meets the requirements. Because our history is only detailed, the requirements are not met for 99305. • Question 22 4 out of 4 points New Patient History & Physical CHIEF COMPLAINT: Right inguinal hernia. HISTORY OF PRESENT ILLNESS: This 44 year-old athletic man has been aware of a bulge and a pain in his right groin for over a year. He is very active, both aerobically and anaerobically. He has a weight routine which he has modified because of this bulge in his right groin. Usually, he can complete his entire workout. He can swim and work without problems. Several weeks ago in the shower he noticed there was a bulge in the groin and he was able to push on it and make it go away. He has never had a groin operation on either side. The pain is minimal, but it is uncomfortable and it limits his ability to participate in his physical activity routine. In addition, he likes to do a lot of exercise in the back country and his personal provider, Dr. X told him it would be dangerous to have this become incarcerated in the back country. PAST MEDICAL HISTORY: Serious illnesses: Reactive airway disease for which he takes Advair. He is not on steroids and has no other pulmonary complaints. Operations: None. MEDICATIONS: Advair. ALLERGIES: None. REVIEW OF SYSTEMS: He has no weight gain or weight loss. He has excellent exercise tolerance. He denies headaches, back pain, abdominal discomfort, or constipation. PHYSICAL EXAMINATION: VITAL SIGNS: Weight 82 kg, temperature 36.8, pulse 48 and regular, blood pressure 121/69. GENERAL APPEARANCE: He is a very muscular well-built man in no distress. SKIN: Normal. LYMPH NODES: None. HEAD AND NECK: Sclerae are clear. External ocular eye movements are full. Trachea is midline. Thyroid is not felt. CHEST: Clear to auscultation. HEART: Regular rhythm with no murmur. ABDOMEN: Soft. Liver and spleen not felt. He has no abnormality in the left groin. In the right groin I can feel a silk purse sign, but I could not feel an actual mass. I am quite sure he has by history and by physical examination a rather small indirect inguinal hernia. His cord and testicles are normal. IMPRESSION: Right indirect inguinal hernia. PLAN: We discussed observation and repair. He is motivated toward repair and I described the operation in detail. I gave him the scheduling number, and he will call and arrange the operation. What CPT® and ICD-10-CM codes are reported? b. 99203, K40.90 b. 99203, K40.90 Response Feedback: Rationale: This is a new patient office visit which is coded from range 99201-99205. For a new patient office visit, all three key components must be met in order to support the level of visit. We have a detailed history (Extended HPI + Extended ROS + Pertinent History), Comprehensive exam (Const, Skin, Lymphatic, Eyes, Respiratory, Cardiovascular, Gastrointestinal, Genitourinary) and moderate MDM (New problem, no additional work up, no tests, elective surgery). The level of visit is 99203. In the ICD-10-CM Alphabetic Index look for Hernia, hernial/inguinal (indirect). Indirect is a nonessential modifier listed for Hernia, hernial/inguinal. You are directed to K40.90. Verify code in the Tabular List. • Question 23 4 out of 4 points ICU - CC: Multi-system organ failure INTERVAL HISTORY: Patient remains intubated and sedated. Overnight events reviewed. Tolerating tube feeds. Systolic pressures have been running in the low 90s on LEVOPHED. Cultures remain negative. Kidney function has worsened, but patient remains non-oliguric. PHYSICAL EXAM: 96/60, 112, 100.8. Lungs have anterior rhonchi. Heart RRR with no MRGs. Abdomen is soft with positive bowel sounds. Extremities show moderate edema. LABS: BUN 89, creatinine 2.6, HGB 10.2, WBC 22,000. ABG: 7.34/100/42 on 50% FiO2. CXR shows RLL infiltrate. IMPRESSION Hypoxic respiratory failure Community acquired pneumonia Septic shock Non-oliguric acute renal failure PLAN: Continue NS at 75 cc/hr. Decrease ZOSYN to 2.25 grams IV Q 6H Follow cultures. Continue tube feeds. Titrate LEVOPHED to maintain SBP > 90 Usual labs ordered for tomorrow. Critical care time: 35 minutes What CPT® code(s) is/are reported? c. 99291 c. 99291 Response Feedback: Rationale: This patient meets the definition of a critically ill patient as defined by the E/M Guidelines for Critical Care services. A critical illness is one acutely impairing one or more vital organ system with a high probability of imminent or life threatening deterioration in the patient’s condition. The physician documents 35 minutes of critical care time. Critical care for 35 minutes is reported with 99291. • Question 24 4 out of 4 points An established 47 year-old patient presents to the provider’s office after falling last night in her apartment when she slipped in water on the kitchen floor. She is complaining of low back pain and no tingling or numbness. Provider documents that she has full range motion of the spine, with discomfort. Her gait is within normal limits. Straight leg raising is negative. She requested no medication. It is recommended to use heat, such as a hot water bottle. Provider’s Assessment: Lower Back Muscle Strain. What E/M and ICD-10-CM codes are reported for this service? c. 99213, S39.012A, W01.0XXA, Y92.030 c. 99213, S39.012A, W01.0XXA, Y92.030 Response Feedback: Rationale: The patient is an established patient. In the CPT® Index look for Established Patient/Office and/or Other Outpatient/Office Visit. You are referred to 99211-99215. An established patient visit requires 2 of 3 key components. The provider documents an Expanded Problem Focused History (brief HPI, pertinent ROS, and no PFSH), a Problem Focused Exam (1 affected organ system, musculoskeletal) and Low MDM (New Problem to examiner, no additional work-up, 0 data points, and acute complicated injury, e.g., simple sprain). Review codes to choose the appropriate level of service. Code 99213 is the correct code. Lower Back Muscle Strain was the provider’s diagnosis. In the ICD-10-CM Alphabetic Index look for Strain/low back. You are referred to S39.012-. Tabular List shows that a 7th character is reported. A is reported for the initial encounter. Next go to the External Cause of Injuries Index. Look for Slipping (accidental) (on same level) (with fall)/on/surface (slippery) (wet) NEC. You are referred to W01.0-. In the Tabular List placeholders of X are needed for the 5th and 6th characters. The 7th character is reported with A to indicate initial encounter. Next look for Place of occurrence/residence/apartment/kitchen. You are referred to Y92.030. Review the code in Tabular List to verify accuracy. • Question 25 0 out of 4 points 65 year-old was admitted in the hospital two days ago and is being examined today by his primary care physician, who has been seeing him since he has been admitted. Primary care physician is checking for any improvements or if the condition is worsening. CHIEF COMPLAINT: CHF INTERVAL HISTORY: CHF symptoms worsened since yesterday. Now has some resting dyspnea. HTN remains poorly controlled with systolic pressure running in the 160s. Also, I’m concerned about his CKD, which has worsened, most likely due to cardio-renal syndrome. REVIEW OF SYSTEMS: Positive for orthopnea and one episode of PND. Negative for flank pain, obstructive symptoms or documented exposure to nephrotoxins. PHYSICAL EXAMINATION: GENERAL: Mild respiratory distress at rest VITAL SIGNS: BP 168/84, HR 58, temperature 98.1. LUNGS: Worsening bibasilar crackles CARDIOVASCULAR: RRR, no MRGs. EXTREMITIES: Show worsening lower extremity edema. LABS: BUN 56, creatinine 2.1, K 5.2, HGB 12. IMPRESSION: 1. Severe exacerbation of CHF 2. Poorly controlled HTN 3. Worsening ARF due to cardio-renal syndrome PLAN: 1. Increase BUMEX to 2 mg IV Q6. 2. Give 500 mg IV DIURIL times one. 3. Re-check usual labs in a.m. What E/M Category is used for this visit? b. Inpatient Consultation (99251-99255) c. Subsequent Hospital Visit (99231-99233) Response Feedback: Rationale: This is a subsequent hospital visit which is reported with code range 99231-99233; because the patient was admitted in the hospital two days ago and the primary care physician has been seeing the patient since he has been admitted to the hospital. Initial Hospital Visit (99221-99223) is when the physician is admitting the patient to the hospital. Inpatient Consultation (99251-99255) is when the provider requests for another provider to see the patient to recommend care for a specific condition or to accept ongoing management for the patient’s condition. Established Patient Office/Outpatient Visit (99211-99215) is when the patient is being seen in the office setting, not the hospital. Sunday, November 19, 2017 9:23:13 AM MST • Question 1 10 out of 10 points A 35-year-old patient plans to travel to a country with a high incidence of yellow fever. The patient receives the yellow fever immunization. Select the appropriate procedure codes for this service. a. 90717, 90471 a. 90717, 90471 Response Feedback: Rationale: Code for both the vaccine and the administration. Codes 90717 and 90471 describe the yellow fever vaccine and the immunization administration for 1 vaccine. In the CPT® Index look for Vaccines and Toxoids/Yellow Fever and Administration/Immunization One Vaccine/Toxoid. • Question 2 10 out of 10 points An inpatient with ESRD is placed on a regular schedule of hemodialysis treatments. The patient receives dialysis at the hospital and is re-evaluated once by the physician for possible revision of the prescribed treatments. On re-evaluation, the physician determines no change in regimen is needed. Code for the dialysis and physician re-evaluation. a. 90937 a. 90937 Response Feedback: Rationale: Code 90937 describes hemodialysis requiring physician re-evaluation with or without substantial revision of dialysis. In the CPT® Index, look for Hemodialysis/Procedure/ with Evaluation. • Question 3 10 out of 10 points A patient with chronic gastrointestinal disturbances undergoes complete ultrasonic scanning of the intestinal vascular structure to determine if blood flow is adequate. Select the appropriate CPT® code for reporting this service. b. 93975 b. 93975 Response Feedback: Rationale: Code 93975 describes a complete scan of arterial inflow and venous outflow of the abdominal, pelvic, scrotal contents, and/or retroperitoneal organs. In the CPT® Index, look for Duplex Scan/Arterial Studies/Visceral. • Question 4 10 out of 10 points A 4-year-old has not reached the expected developmental milestones for her age group. She was referred by her pediatrician for extensive developmental testing. The psychologist initiated multiple function studies, using standardized instruments and reported the results to the child's pediatrician. Code the psychologist’s service. c. 96111 c. 96111 Response Feedback: Rationale: Code 96111 describes extensive testing for developmental assessment, including interpretation and report. In the CPT® Index, look for Developmental Testing. • Question 5 10 out of 10 points A patient sustained a severe ankle sprain playing basketball. The ankle is stiff and without complete range of motion. The physician refers the patient for physical therapy. Prior to treatment, the therapist evaluates the patient. The therapist docu-ments a brief history and exam of the ankle and determines the sprain as uncomplicated with no other injury to the ankle. The therapist recommends an additional 5 sessions for strength and endurance and no basketball for two weeks. The clinical decision making is of low complexity. The patient has a one-hour therapy session on the same day. What is the correct code(s)? a. 97161-GP, 97110-GP x 4 a. 97161-GP, 97110-GP x 4 Response Feedback: Rationale: The therapist evaluates the patient and problem at the first visit and determines a treatment plan Code 97161 is reported for an uncomplicated injury with low clinical decision making. In the CPT® Index, look for Physical Medicine/Therapy/Occupational Therapy/Evaluation/Physical Therapy. Code 97110 describes exercises performed to develop strength and range of motion, per 15 minutes. For one hour, report four units. In the CPT® Index, look for Physical Medicine/Therapy/Occupational Therapy/Procedures/Therapeutic Exercises. • Question 6 10 out of 10 points An anorexic patient is experiencing signs of severe dietary deficiency and electrolyte imbalance. She will need medical nutrition therapy to treat these symptoms. The provider spends 30 minutes with the patient to discuss the seriousness of her eating disorder and the necessity of nutrition therapy. What is the code for this initial assessment? c. 97802 x 2 c. 97802 x 2 Response Feedback: Rationale: Code 97802 describes the initial medical nutrition assessment interview per 15 minutes of face-to-face time. Report two units for the 30-minute session. In the CPT® Index, look for, Nutrition Therapy/Initial Assessment. • Question 7 10 out of 10 points A patient continues to have low back pain after lifting a heavy bin while cleaning the basement. The chiropractor manipulates both the lumbar and sacral areas. What is the correct code? c. 98940 c. 98940 Response Feedback: Rationale: Code 98940 describes manipulation of 1-2 spinal regions. In the CPT® Index, look for Manipulation/Chiropractic. • Question 8 10 out of 10 points A patient in a rural setting with limited travel resources visits his physician for a physical examination. Lab work is done. The physician advises the patient that if the results are negative, he does not need to return to the office. The nurse emails the patient that the results were negative, and the patient does not need to return for six months unless new symptoms appear. One month later, the patient emails the office with a request to change his current medication to a less-expensive generic version. The nurse answers the email, advising one of his medications could be changed to a generic version and refills will be called to the pharmacy as needed. She also responds to several questions the patient has about his general health conditions. She spends 25 minutes entering this information. What is the correct code for this service? d. 98969 d. 98969 Response Feedback: Rationale: Code 98969 describes an on-line medical evaluation with a nonphysician qualified healthcare professional not relating to a management and assessment service within the previous seven days and not leading to the next urgent care appointment. In the CPT® Index, look for Evaluation and Management/Online Services. • Question 9 10 out of 10 points A physician performes a magnified anogenital examination on a young child to determine if assault occurred. What is the correct code for this service? b. 99170 b. 99170 Response Feedback: Rationale: Code 99170 describes a magnified anogenital examination on a child for suspected trauma. In the CPT® Index, look for Anogenital Region – See Perineum. Locate Perineum/Anogenital Examination/with Magnification and Image/Recording. • Question 10 10 out of 10 points A nurse visites a patient in the home to manage infusion of a thrombolytic agent for two hours. What is the correct code for this visit? d. 99601 d. 99601 Response Feedback: Rationale: Code 99601 describes home infusion of a specialty drug per visit, up to two hours. In the CPT® Index, look for Home Services/Home Infusion Procedures. Sunday, November 19, 2017 9:23:29 AM MST • Question 1 4 out of 4 points A 15 year-old underwent placement of a cochlear implant 1 year ago. It now needs to be reprogrammed. What CPT® code is reported for the reprogramming? b. 92604 b. 92604 Response Feedback: Rationale: Cochlear implants differ from hearing aids; they bypass the damaged part of the ear. The use of a cochlear implant involves relearning how to hear and react to sounds. In the CPT® Index look for Cochlear Device/Programming which directs you to codes 92602, 92604. The code selection is based on the age of the patient and whether it is the initial programming or subsequent reprogramming. Code 92604 describes subsequent reprogramming for a patient age 7 or older. • Question 2 4 out of 4 points A child with suspected sleep apnea was given an apnea monitoring device to use over the next month. The device was capable of recording and storing data relative to heart and respiratory rate and pattern. The pediatric pulmonologist reviewed the data and reported to the child’s primary pediatrician. What CPT® code(s) is/are reported for the monitor attachment, download of data, provider review, interpretation and report? d. 94774 d. 94774 Response Feedback: Rationale: In the CPT® Index look for Monitoring/Pediatric Apnea and you are directed to code range 94774-94777. Code selection is based on the components of the test performed. In this case, code 94774 describes the data storage capability, including the provider or other qualified health care professional interpretation and report. The code is to be reported each 30-day period. • Question 3 4 out of 4 points A 5 year-old fell on broken glass and required suturing of a laceration. Due to the age and combative behavior of the patient, the provider utilized moderate sedation while repairing the laceration. The provider gave the child 50 mg of Ketamine IM. A nurse monitored the patient during the procedure which took 30 minutes. What CPT® code is reported for moderate sedation? b. 99152, 99153 b. 99152, 99153 Response Feedback: Rationale: Moderate sedation is often used for pediatric patients in situations not normally requiring sedation. In this case, the provider administered sedation with a nurse assisting in monitoring the patient. In the CPT® Index look for Sedation/Moderate/with Independent Observation and you are directed to code range 99151-99153. Code selection is based on age of the patient and the length of time. Code 99152 describes an encounter using moderate sedation, and the physician or other qualified health care professional rendering the diagnostic or therapeutic service also manages the sedation. This code is specific for the age of the patient and up to 15 minutes of time. Add-on 99153 is for each additional 15 minutes of intraservice time. • Question 4 4 out of 4 points A cardiologist provided an interpretation and report of an EKG. What CPT® code is reported? d. 93010 d. 93010 Response Feedback: Rationale: In the CPT® Index look for EKG and you are directed to see Electrocardiography. For Electrocardiography/Evaluation you are directed to 0178T-0180T, 93000, 93010, 93660. 0178T-0180T are used for EKGs using 64 or more leads and graphic presentation and analysis. 93660 involves a tilt table evaluation. The remaining codes are 93000, 93010. 93000 includes the 12 lead EKG in addition to the interpretation and report. The provider only provided the interpretation and report making 93010 the correct code choice. • Question 5 4 out of 4 points A patient was brought to the emergency department in cardiac arrest. The physician immediately initiated CPR. What CPT® code is reported for CPR? a. 92950 a. 92950 Response Feedback: Rationale: Medical personnel usually begin cardiopulmonary resuscitation (CPR) which provides artificial breathing and chest compressions for a person in cardiac arrest. In the CPT® Index you can look for either CPR or Cardiopulmonary Resuscitation or Resuscitation/Cardiopulmonary. All indexed items direct you to code 92950. • Question 6 4 out of 4 points A 49 year-old female was brought to the emergency department. She was lethargic, but awake. She is four years post liver transplant. Neurology was consulted who determined the patient was encephalopathic with altered mental status. There was some question whether she had a seizure. An EEG and WADA test were performed. What CPT® and ICD-10-CM codes are reported? c. 95958, G93.40, R41.82, Z94.4 c. 95958, G93.40, R41.82, Z94.4 Response Feedback: Rationale: In the CPT® Index look for WADA Activation Test and you are directed to code 95958. You can also see Electroencephalography/Monitoring/with WADA Activation. The WADA activation test is coded as 95958 and includes EEG monitoring. For the diagnoses, look in the ICD-10-CM Alphabetic Index for Encephalopathy and you are directed to G93.40. Next, look for Alteration (of), Altered/mental status directing you to R41.82. The patient is also status post liver transplant, which is found in the Alphabetic Index by looking for Transplant(ed) (status)/liver which directs you to Z94.4. Verification of the codes in the Tabular List confirms code selections. • Question 7 4 out of 4 points A patient with severe atrial fibrillation presents for an EPS study. The cardiologist performs the professional component of a comprehensive EPS study, including right atrial and ventricular pacing/recording, bundle of His recording and induction of atrial fibrillation, and insertion and repositioning of multiple electrode catheters. What CPT® code(s) is/are reported? c. 93620 –26 c. 93620 –26 Response Feedback: Rationale: An EPS study is an electrophysiology study evaluating the electrical system of the heart. In the CPT® Index look for Electrophysiology Procedure and you are directed to code range 93600-93660. It is important to read code descriptions carefully to avoid coding each element separately when there is a code combining all elements performed. 93620 includes all the elements described. Modifier 26 is appropriate to indicate the professional component was performed by the provider. • Question 8 4 out of 4 points A patient diagnosed with amyotrophic lateral sclerosis has increasing muscle weakness in the upper extremities. The provider orders needle electromyography (EMG) to record electrical activity of the muscles. What CPT® and ICD-10-CM codes are reported? c. 95861, G12.21 c. 95861, G12.21 Response Feedback: Rationale: In the CPT® Index look for Electromyography/Needle/Extremities and you are directed to code range 95860-95864. Code selection is based on the number of extremities studied. In this case, two extremities (upper) are studied making 95861 the correct code selection. Amyotrophic lateral sclerosis (ALS) is also known as Lou Gehrig’s disease. In the ICD-10-CM Alphabetic Index, look for Sclerosis/amyotrophic (lateral) which directs you to code G12.21. Verification in the Tabular List confirms code selection. • Question 9 4 out of 4 points A patient sustained a neck strain as a driver in an automobile accident, losing control, hydroplaning and hitting a tree off the highway which caused the car to overturn. He has continued to have neck pain and stiffness. He sees a chiropractor who assesses the patient and manipulates his neck. The diagnosis is neck strain. What CPT® and ICD-10-CM codes are reported for the chiropractor? a. 98940, S16.1XXA, V47.0XXA a. 98940, S16.1XXA, V47.0XXA Response Feedback: Rationale: In the CPT® Index look for Manipulation/Chiropractic directs you to code range 98940-98943. The neck is the cervical spine and code selection is based on the number regions treated. In this case, 1 region is treated making 98940 is the correct code choice. In the ICD-10-CM Alphabetic Index look for Strain/cervical or Strain/neck and you are directed to code S16.1-. The Tabular List shows seven characters are needed to complete the code. X is used as a placeholder for the 5thand 6th characters. A is the 7th character for the initial encounter receiving active treatment. Next, report the external cause. The patient was the driver in a non-collision vehicle accident when he lost control of the car. Look in the ICD-10-CM External Cause of Injuries Index for Accident/car which states to see Accident, transport, car occupant. Look for Accident/transport/car occupant/driver/collision (with)/stationary object/nontraffic. When referring to the Tabular List, subcategory code V47.0 is used and it shows seven characters are needed to complete this code. X is used as the 5th and 6thcharacters and A, initial encounter, is used for the 7thcharacter. • Question 10 4 out of 4 points A 5 week-old infant shows signs of fatigue after eating and has poor weight gain. He is suspected to have a congenital heart defect. The neonatologist ordered a transthoracic echocardiogram (TTE). TTE is showing a shunt between the right and left ventricles. The neonatologist read and interpreted the study and indicated the patient has a ventricular septal defect (VSD). What are the CPT® and ICD-10-CM codes for the TTE read? b. 93303-26, Q21.0 b. 93303-26, Q21.0 Response Feedback: Rationale: In the CPT® Index look for Echocardiography/Transthoracic/Congenital Cardiac Anomalies which directs you to 93303, 93304. Code selection is based on whether it is a complete study, follow up or limited study. This is a complete study therefore code 93303 the correct code choice. Since we are only reporting reading and interpretation of the report, a modifier 26 is appended. In ICD-10-CM Alphabetic Index look for Defect, defective/ventricular septal and you are directed to Q21.0. Verification in the Tabular List confirms code selection. • Question 11 4 out of 4 points What ICD-10-CM code is reported for an anaphylactic reaction to peanuts, initial encounter? b. T78.01XA b. T78.01XA Response Feedback: Rationale: In the ICD-10-CM Alphabetic Index look for Anaphylactic/shock or reaction which states see Shock, anaphylactic. Look for Shock/anaphylactic/due to food (nonpoisonous)/peanuts which directs you to T78.01. In the Tabular List, a 7thcharacter is required. Placeholder X is used for the 6th character. The initial encounter is specified with 7th character A for the initial encounter. • Question 12 4 out of 4 points A patient with chronic myeloid leukemia (CML), BCR/ABL-positive has an implanted access port for delivery of chemotherapy. The device needs to be irrigated before receiving treatment. What ICD-10-CM and CPT® codes are reported for the irrigation? c. 96523, C92.10 c. 96523, C92.10 Response Feedback: Rationale: In the CPT® Index look for Irrigation/Venous Access Device. Report code 96523 for irrigation of an implanted venous access device. In the ICD-10-CM Alphabetic Index look for Leukemia/chronic myeloid, BCR/ABL-positive and you are directed to C92.1-. In the Tabular List the 5th character of 0 is used to indicate there is no mention of having achieved remission. • Question 13 4 out of 4 points A 70 year-old patient with chronic obstructive asthma is brought to the urgent care center with increased wheezing and coughing. The provider initiated an albuterol inhalation treatment, one dose, delivered by nebulizer. After treatment, the patient’s exacerbation was somewhat improved but the provider determined a second treatment was necessary. What codes are reported? a. 94640, 94640-76, J7609 x 2, J44.1 a. 94640, 94640-76, J7609 x 2, J44.1 Response Feedback: Rationale: In the CPT® Index look for Inhalation Treatment/for Airway Obstruction/Pressured or Nonpressured and you are directed 94640. Inhalation treatment was given therapeutically in treating the acute airway obstruction. Two treatments were given so code 94640 is reported twice. Under code 94640 there is a parenthetical instruction stating to use modifier 76 if more than one inhalation treatment is performed on the same date. Because treatment is in the office (urgent care is considered office treatment), the provider will also bill for the medication used. In this case, it is albuterol. In the HCPCS Level II codebook go to the Table of Drugs and Biologicals and look for Albuterol, unit dose form which directs you to J7609, J7613. J7609 is reported for albuterol per dose. Two doses were given reporting J7609 x 2. For the diagnosis in the ICD-10-CM Alphabetic Index look for Asthma/chronic obstructive/with exacerbation (acute) directing you to J44.1. There is no mention of status asthmaticus, but exacerbation is mentioned. The diagnosis code is J44.1. Verification in the Tabular List confirms code selection. • Question 14 4 out of 4 points A patient who has psoriasis vulgaris on his back has not responded to topical applications. He is treated with laser therapy on a total area of 260 sq. cm. d. 96921, L40.0 d. 96921, L40.0 Response Feedback: Rationale: In the CPT® Index look for Psoriasis/Treatment, you are directed to code range 96910-96922. 96910-96913 are for photochemotherapy. 96920-96922 are for laser treatment and code selection is based on the size of the area treated. 260 sq. cm is reported with 96921. In the ICD-10-CM Alphabetic Index, look for Psoriasis/vulgaris referring you to L40.0. Verification in the Tabular List confirms code selection. • Question 15 4 out of 4 points A patient has an open wound on his left lower leg caused by a cat bite. The animal tested negative for rabies, but the wound has failed to heal and became infected by Clostridium perfringens. The patient underwent hyperbaric oxygen therapy attended and supervised by the provider. What CPT® and ICD-10-CM codes are reported? a. 99183, S81.852A, B96.7, W55.01XA a. 99183, S81.852A, B96.7, W55.01XA Response Feedback: Rationale: In the CPT® Index look for Hyperbaric Oxygen Pressurization and you are directed to code 99183. The wound is complicated due to the infection. In the ICD-10-CM Alphabetic Index look for Bite(s) (animal) (human)/leg (lower) and you are directed to S81.85-. Tabular List shows seven characters are needed to complete the code. The 6th character 2 indicates the left leg. 7th character A indicates initial encounter for receiving active treatment. The infectious agent is identified as Clostridium perfringens. Look for Infection/Clostridium/perfringens/as cause of disease classified elsewhere directing you to code B96.7. The external cause is the cat bite. Look in the ICD-10-CM External Cause of Injuries Index for Bite, bitten by/cat which directs you to code W55.01-. Tabular List shows seven characters are needed to complete the code. A placeholder X is assigned to the 6th character and A is assigned for initial encounter for the 7th character. • Question 16 4 out of 4 points A patient with carcinoma of the descending colon presents for chemotherapy administration at the infusion center. The infusion was started with 1000 cc of normal saline. Heparin, 1000 units was added and then Fluorouracil, 800 mg was added and infused over 2 hours. Dexamethasone, 20 mg was administered, IV push. At the end of the 2 hours, the IV was disconnected and the patient was discharged. What codes are reported? c. 96413, 96415, 96375, J9190 x 2, J1100 x 20, J1644, Z51.11, C18.6 c. 96413, 96415, 96375, J9190 x 2, J1100 x 20, J1644, Z51.11, C18.6 Response Feedback: Rationale: In the CPT® Index look for Chemotherapy/Intravenous/Infusion which directs you to 96413, 96415, 96416, 96417. Chemotherapy infusion administration is reported as 96413 for the 1st hour and 96415 for each additional hour. The chemotherapy ran for 2 hours; report 96413 & 96415. Dexamethasone was administered as a push technique. Dexamethasone is not a chemotherapy agent. In the CPT® Index, look for Injection/Intravenous Push referring you to 96374-96376. This is a sequential infusion following the initial service of chemotherapy and is reported as 96375. The chemotherapy drugs are Fluorouracil and Heparin. The Fluorouracil is reported with J9190 (HCPCS Level II). It is listed as 500 mg therefore 2 units are charged for 800 mg administered. Heparin (J1644) is listed as 1,000 units, therefore one unit is reported for the 1000 units given. Dexamethasone is packaged in 1 mg; charge 20 units for the 20 mg administered (J1100). Per ICD-10-CM guideline I.C.2.e.2 a visit for the purpose of chemotherapy is reported with Z51.11 with the primary and the malignancy sequenced second. In the ICD-10-CM Alphabetic Index, look for Chemotherapy(session) (for)/cancer which directs you to Z51.11. Report also the reason for the chemotherapy. In this case, it is carcinoma of the descending colon. Look in the Alphabetic Index for Carcinoma which states see also Neoplasm, by site, malignant. Go to the ICD-10-CM Table of Neoplasms and look for Neoplasm, neoplastic/intestine, intestinal/large/descending and select from the Malignant Primary column which refers you to C18.6. Verification in the Tabular List confirms code selection. • Question 17 4 out of 4 points A therapist in a residential care facility works with a nonverbal autistic child, age 4. In this session the therapist uses drawing paper and washable markers. The therapist sat with the child and began to draw on a sheet of paper. She gave paper and markers to the child and encouraged the child to draw. The psychotherapy session lasted 30 minutes. b. 90832, 90785, F84.0 b. 90832, 90785, F84.0 Response Feedback: Rationale: Psychotherapy session with was performed lasting 30 minutes. In the CPT® Index look for Psychotherapy/Individual Patient/Family Member refers you to 90832-90834, 90836-90838. Review of the codes identify code 90832 is the correct code to report. Art therapy is frequently used when working with children who are unable to verbalize well or not at all. It may give insight to thought processes through the expressions captured in the artwork. Art therapy is considered individual psychotherapy. In the CPT® Index look up Psychotherapy/Interactive Complexity you are directed to code range 90785. Code selection is based on time and whether a medical evaluation and management was performed. Code 90785 is an add-on code and for this case is reported with 90832 per instructions at the beginning of this section. Time is not a factor with 90785. The child is currently autistic and does not communicate verbally. In the ICD-10-CM Alphabetic Index look for Autism, autistic (childhood) (infantile) which directs you to F84.0. Since an autism spectrum is not defined, the correct diagnosis code is F84.0. Verification in the Tabular List confirms code selection. • Question 18 4 out of 4 points A patient with congestive heart failure and chronic respiratory failure with hypoxia is placed on home oxygen. Prescribed treatment is 2L nasal cannula oxygen at all times. A home care nurse visited the patient to assist with his oxygen management. What CPT® and ICD-10-CM codes are reported? b. 99503, I50.9, J96.11 b. 99503, I50.9, J96.11 Response Feedback: Rationale: In the CPT® Index look for Home Services/Respiratory Therapy which directs you to code 99503. In the ICD-10-CM Alphabetic Index look for Failure/heart/congestive and you are directed to I50.9. Then look for Failure, failed/respiration, respiratory/chronic/with/hypoxia which directs you to J96.11. Verification in the Tabular List confirms code selection. • Question 19 4 out of 4 points A qualified genetics counselor is working with a child who has been diagnosed with fragile X syndrome. After extensive research about the condition, she meets with the parents to discuss the features of the disease and the child’s prognosis. The session lasted 45 minutes. What CPT® and ICD-10-CM codes are reported? b. 96040, Q99.2 b. 96040, Q99.2 Response Feedback: Rationale: In the CPT® Index look for Medical Genetics which directs you to 96040. The genetics counseling session is reported as face-to-face time per 30 minutes. Report 1 unit for the first 30 minutes. Since the remaining time is 15 minutes, it is not reported separately per the Medical Genetics and Genetic Counseling Services guidelines. Fragile X syndrome is a congenital chromosomal anomaly that may include mental retardation. In the ICD-10-CM Alphabetic Index look for Syndrome/fragile X. The condition is reported with code Q99.2. Verification in the Tabular List confirms code selection. • Question 20 0 out of 4 points A patient with bilateral sensory hearing loss is fitted with a digital, binaural, behind the ear hearing aid. What HCPCS Level II and ICD-10-CM codes are reported? b. V5140, H90.6 a. V5261, Z46.1, H90.3 Response Feedback: Rationale: In the HCPCS Level II Index look for Hearing aid/Binaural/Digital/BTE referring you to V5261. The purpose of the visit is the fitting of the hearing aid. Look in the ICD-10-CM Alphabetic Index for Fitting (and adjustment) (of)/hearing aid directing you to Z46.1. The condition necessitating the hearing aid is bilateral sensory hearing loss. In the Alphabetic Index, look for Deafness/sensorineural/bilateral which directs you to H90.3. Verification in the Tabular List confirms code selection. • Question 21 4 out of 4 points What ICD-10-CM code(s) is/are reported for a diabetic foot ulcer on the right foot? c. E11.621, L97.519 c. E11.621, L97.519 Response Feedback: Rationale: ICD-10-CM guideline I.C.4.a.2. instructs you to use the default code E11- for type 2 diabetes when the type is not indicated. Look in the ICD-10-CM Alphabetic Index for Diabetes, diabetic/with/foot ulcer which directs you to E11.621. In the Tabular List there is a note to use an additional code to identify the site of the ulcer (L97.4-, L97.5-). Look in the Alphabetic Index for Ulcer/lower limb/foot specified NEC/right which directs the coder to L97.519. The severity of the ulcer is not documented in this scenario. Verification in the Tabular List confirms E11.621 is for type 2 diabetes mellitus with foot ulcer and L97.519 is for non-pressure chronic ulcer of other part of right foot with unspecified severity. • Question 22 0 out of 4 points A 64 year-old patient came to the emergency department complaining of chest pressure. The provider evaluated the patient and ordered a 12 lead EKG. Findings included signs of acute cardiac damage. Appropriate initial management was continued by the ED provider who contacted the cardiologist on call in the hospital. Admission to the cardiac unit was ordered. No beds were available in the cardiac unit and the patient was held in the ED. The cardiologist left the ED after completing the evaluation of the patient. Several hours passed and the patient was still in the ED. During an 80-minute period, the patient experienced acute breathing difficulty, increased chest pain, arrhythmias and cardiac arrest. The patient was managed by the ED provider during this 80-minute period. Included in the provider management were a new 12 lead EKG, endotracheal intubation and efforts to restore the patient’s breathing and circulation for 20 minutes. CPR was unsuccessful, the patient was pronounced dead after a total of 44 minutes critical care time, exclusive of other separately billable services. What CPT® codes are reported by the ED provider? c. 99285-25, 93010 x 2, 31500, 92950 d. 99291-25, 31500, 92950 Response Feedback: Rationale: Only one E&M code is reportable per provider per day. The patient never left the emergency department. The first part of the encounter did not meet critical care, although the second part did meet critical care. In the CPT® Index look for Critical Care Services. Use code 99291 for 44 minutes of critical care. The Critical Care Services guidelines list services that are included in Critical Care time. Additional services performed not included in the listing is reported separately. In the CPT® Index look for Insertion/Endotracheal Tube/Emergency Intubation which directs you to 31500. In the CPT® Index look for CPR. Report cardiopulmonary resuscitation with code 92950. The EKG reading is included in critical care per the guidelines and is not separately billable. • Question 23 4 out of 4 points A 49 year-old patient had several episodes of esophageal reflux and underwent a gastroesophageal reflux test to measure the pH balance (a measure of the degree of acidity or alkalinity). The test was performed with a mucosal attached capsule. The provider provided an interpretation and report. The provider stated the diagnosis as gastroesophageal reflux. What CPT® and ICD-10-CM codes are reported? c. 91035, K21.9 c. 91035, K21.9 Response Feedback: Rationale: In the CPT® Index look for Acid Reflux Test/Esophagus which directs you to 91034-91035, 91037-91038. The provider measured the pH balance and used a mucous capsule, which attaches the electrode to the mucous in the esophagus which is reported with code 91035. Catheter placement of the electrode is becoming rare with the development of the mucous attaching capsule. In the ICD-10-CM Alphabetic Index look for Reflux/gastroesophageal. The diagnosis code for gastroesophageal reflux without esophagitis is K21.9. Reflux is regurgitation of gastric contents into the mouth, caused by incompetence of the lower esophageal sphincter. Verification in the Tabular List confirms code selection. • Question 24 4 out of 4 points A patient with sickle cell anemia with painful sickle crisis received normal saline IV 100 cc per hour to run over 5 hours for hydration in the provider’s office. She will be given Morphine & Phenergan, prn (as needed). What codes are reported? d. 96360, 96361 x 4, J7050 x 2, D57.00 d. 96360, 96361 x 4, J7050 x 2, D57.00 Response Feedback: Rationale: In the CPT® Index look for Hydration/Intravenous and you are directed to codes 96360-96361. The hydration will run 5 hours at 100 cc per hour. Codes are time based. Code the hydration therapy as 96360 for the first hour, and 96361 x 4 for a total infusion time of 5 hours. In the HCPCS Level II look for Saline Solution referring you to codes J7030-J7050. Code for the normal saline with J7050 x 2 units for 500 cc. The type of sickle cell anemia is not identified, but the patient has painful sickle crisis. In the ICD-10-CM Alphabetic Index, look for Disease, diseased/sickle-cell/with crisis directing you to D57.00. Verification in the Tabular List confirms code selection. • Question 25 4 out of 4 points A 54 year-old female with uncontrolled type 1 insulin dependent diabetes and related peripheral vascular disease presents with a deep diabetic ulceration on the bottom of her right foot. The wound reaches into the fascia and appears to be draining. She acknowledges going barefoot frequently and is not certain how or when the wound occurred. After the provider discusses the seriousness of her condition he debrides the wound, using a water jet and surgical scissors. Size of wound is 70 sq. cm. He applied topical ointment and a sterile dressing. He counseled the patient about the need to wear shoes at all times and inspect her feet daily. He advised the patient to wear a water protective covering on her lower leg when taking a shower and to change the dressing daily, using ointment provided. A surgical shoe was provided. Patient is to return weekly until the wound heals and continue her insulin regime. If satisfactory progress does not occur, a graft may be considered. What codes are reported? b. 97597, 97598 x 3, L3260, E10.621, E10.51, L97.513 b. 97597, 97598 x 3, L3260, E10.621, E10.51, L97.513 Response Feedback: Rationale: In the CPT® Index look for Wound/Care/Debridement/Selective and you are directed to code range 97597-97598. Code selection is based on the size of the area debrided. 70 sq. cm were debrided. Code 97597 is reported for the first 20 sq. cm and 97598 is reported 3 times to show the remaining area debrided (20 sq. cm, 20 sq. cm, 10 sq. cm). In the HCPCS Level II codebook look for Boot/Surgical, ambulatory referring you to L3260. The patient has type 1 diabetes and peripheral vascular disease with a diabetic foot ulcer. A cause and effect relationship is stated between diabetes and peripheral vascular disease. The ulcer is also a diabetic complication. In the ICD-10-CM Alphabetic Index look for Diabetes, diabetic (mellitus) (sugar)/type 1/with/foot ulcer and you are directed to E10.621. In the Tabular List there is an instructional note to code from L97.4- or L97.5- for the location and type of ulceration. The ulcer is on the bottom of the right foot. Look in the Alphabetic index for Ulcer, ulcerated, ulcerating, ulceration, ulcerative/lower limb/foot/right/with/muscle necrosis which directs you to L97.513. In the Alphabetic Index look for Diabetes, diabetic (mellitus) (sugar)/type 1/with/peripheral angiopathy and you are directed to E10.51. ICD-10-CM guideline 1.C.4.a. states to assign as many diabetic codes as necessary to describe all complications. Verification in the Tabular List confirms code selection. Long term insulin usage (Z79.4) is not coded with type I diabetes. Sunday, November 19, 2017 9:23:55 AM MST [Show More]
Last updated: 1 year ago
Preview 1 out of 500 pages
 – American Academy of Professional Coders.png)
Reviews( 0 )
Recommended For You
Computer Science> EXAM > AAPC IDC 10. American Academy of Professional Coders. All Exams TEST BANK. (All)
 Test Bank - American Academy of Professional Coders.png)
AAPC IDC 10. American Academy of Professional Coders. All Exams TEST BANK.
AAPC IDC 10 Exam (All Exams) Test Bank - American Academy of Professional Coders Physician Coding for CPC Preparation (Q-S) Review Test Submission: Chapter 1 Quiz Course 2019 Physician Coding...
By Martin Freeman , Uploaded: Nov 16, 2020
$16
Health Care> EXAM > ACES FINAL EXAM PREP | 135 Questions | 100% Correct (All)
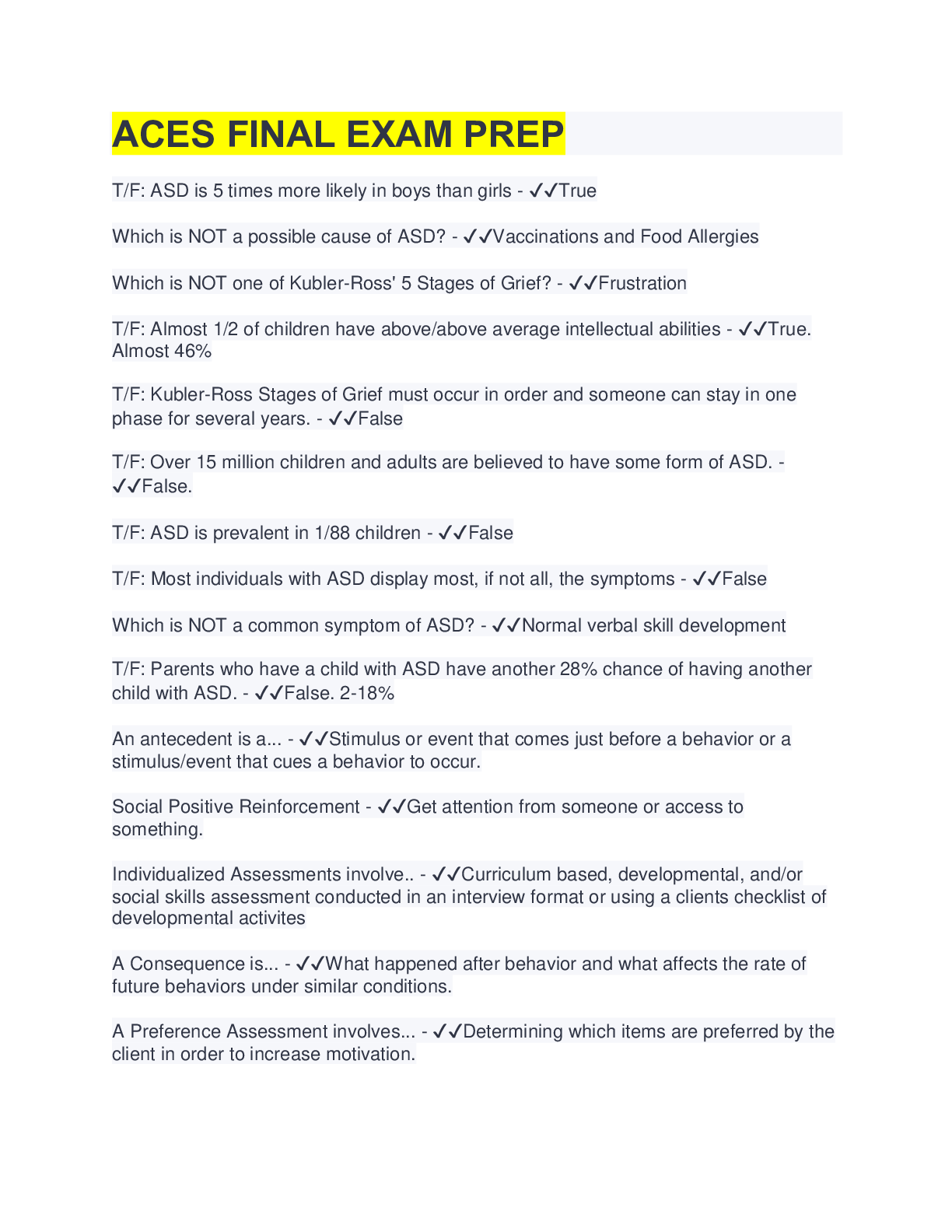
ACES FINAL EXAM PREP | 135 Questions | 100% Correct
T/F: ASD is 5 times more likely in boys than girls - ✔✔True Which is NOT a possible cause of ASD? - ✔✔Vaccinations and Food Allergies Which is NOT one of Kubler-Ross' 5 Stages of Grief? - ✔✔Frustrat...
By Tessa , Uploaded: Aug 12, 2022
$10
Finance> EXAM > 117 CFA Final Exam Prep Questions and Answers (All)
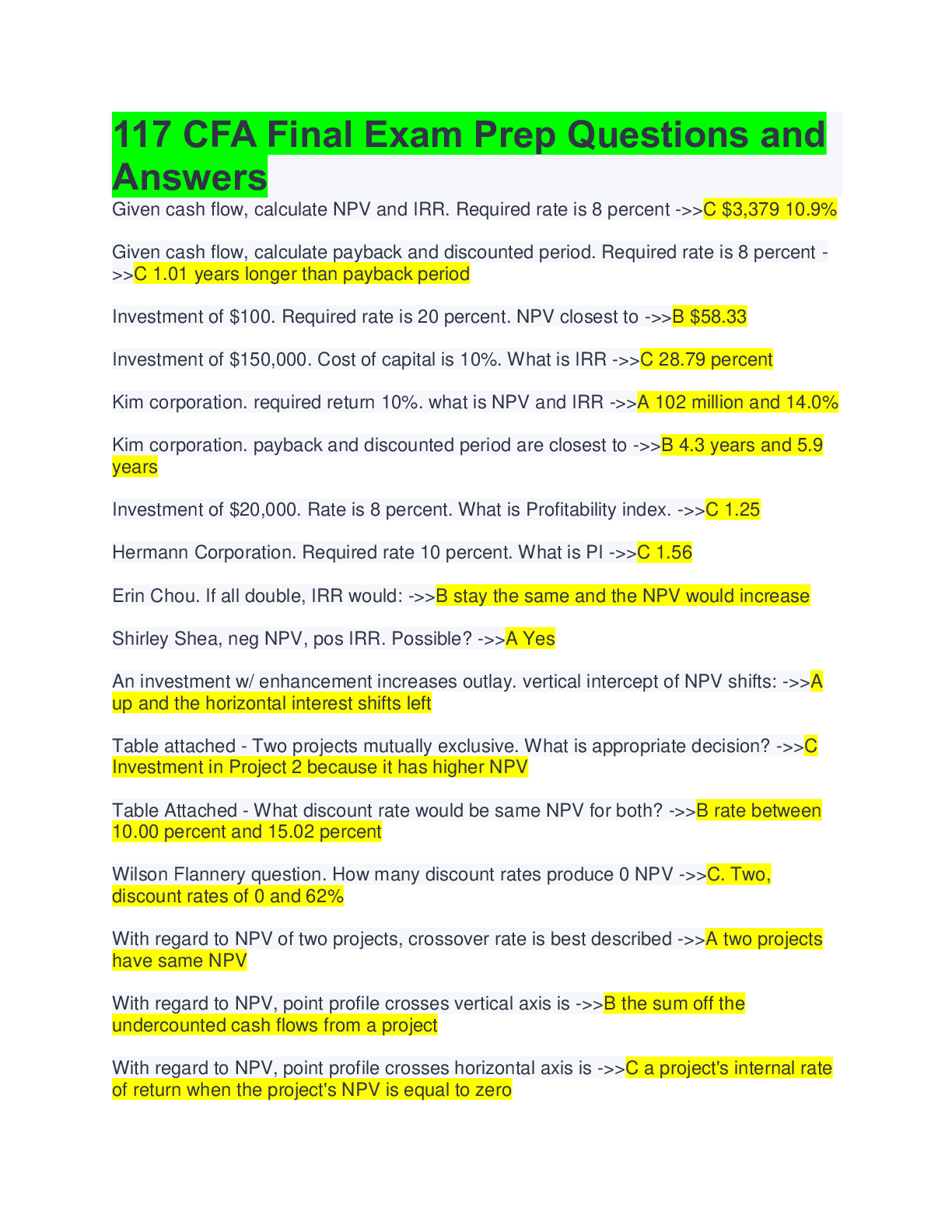
117 CFA Final Exam Prep Questions and Answers
117 CFA Final Exam Prep Questions and Answers Given cash flow, calculate NPV and IRR. Required rate is 8 percent ->>C $3,379 10.9% Given cash flow, calculate payback and discounted period. Requir...
By Professor Lynne , Uploaded: Aug 11, 2022
$9
Medicine> EXAM > AAPC CPC FINAL EXAM QUESTIONS AND AND ANSWERS DOWNLOAD TO SCORE AN A. (All)
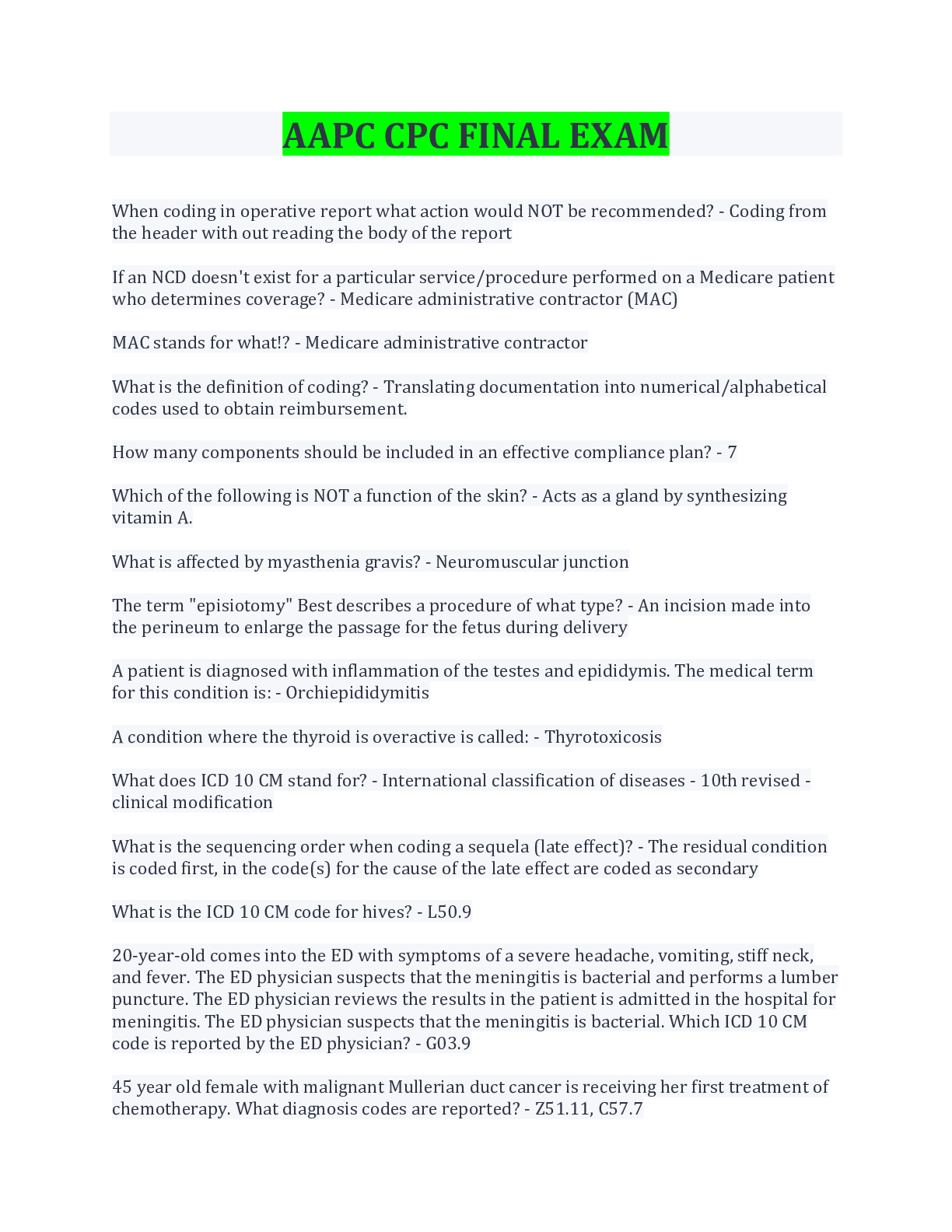
AAPC CPC FINAL EXAM QUESTIONS AND AND ANSWERS DOWNLOAD TO SCORE AN A.
AAPC CPC FINAL EXAM QUESTIONS AND AND ANSWERS DOWNLOAD TO SCORE AN A.
By FallonCarrington , Uploaded: Jul 23, 2022
$11.5
Finance> EXAM > FIN111 Final Exam Prep (All)
FIN111 Final Exam Prep
FIN111 Final Exam Prep Question and Answers 1. The purchase of additional physical facilities such as additional property or a new factory is an example of a capital expenditure Answer: true 2. If...
By Topmentor , Uploaded: Jul 19, 2022
$15
*NURSING> EXAM > CPCO 2017 CPC/; Final Exam Prep Questions And Answers3/TOP SCORE (All)
CPCO 2017 CPC/; Final Exam Prep Questions And Answers3/TOP SCORE
CPCO 2017 CPC Final Exam Prep Questions • • Question 1 10 out of 10 points What form is provided to a patient to indicate a service may not be covered by Medicare and the patient may be responsibl e f...
By BrendaGee , Uploaded: Jul 17, 2022
$10.5
Health Care> EXAM > AAPC CPC FINAL EXAM 2020 | with Complete Solution (All)
AAPC CPC FINAL EXAM 2020 | with Complete Solution
Evaluation and management services are often provided in a standard format such as SOAP notes. What does the acronym SOAP stand for? a. Scope, Observation, Action, Plan b. Standard, Objective, Ac...
By Tessa , Uploaded: Jul 16, 2022
$10
Health Care> EXAM > AAPC CPC FINAL EXAM 2022/2023 QUESTIONS WITH FULL ANSWER KEY & RATIONALE (All)
AAPC CPC FINAL EXAM 2022/2023 QUESTIONS WITH FULL ANSWER KEY & RATIONALE
When coding in operative report what action would NOT be recommended? - Coding from the header with out reading the body of the report If an NCD doesn't exist for a particular service/procedure per...
By professor chue , Uploaded: Jul 15, 2022
$12
Social Sciences> EXAM > Firefighter 2 Final Exam Prep (Latest 2022/2023) 100% Correct (All)

Firefighter 2 Final Exam Prep (Latest 2022/2023) 100% Correct
Firefighter 2 Final Exam Prep (Latest 2022/2023) 100% Correct
By kofee , Uploaded: Jul 12, 2022
$12
*NURSING> EXAM > Firefighter 2 Final Exam Prep Questions And Answers( Complete best Solution Rated A) (All)

Firefighter 2 Final Exam Prep Questions And Answers( Complete best Solution Rated A)
Firefighter 2 Final Exam Prep Divisions of labor... A. Outlines how things are to be done and usually how far a person can go without requesting further guidance B. Relates to the number of people one...
By Jameson , Uploaded: Jun 27, 2022
$11
Document information
Connected school, study & course
About the document
Uploaded On
Nov 16, 2020
Number of pages
500
Written in
Additional information
This document has been written for:
Uploaded
Nov 16, 2020
Downloads
0
Views
492