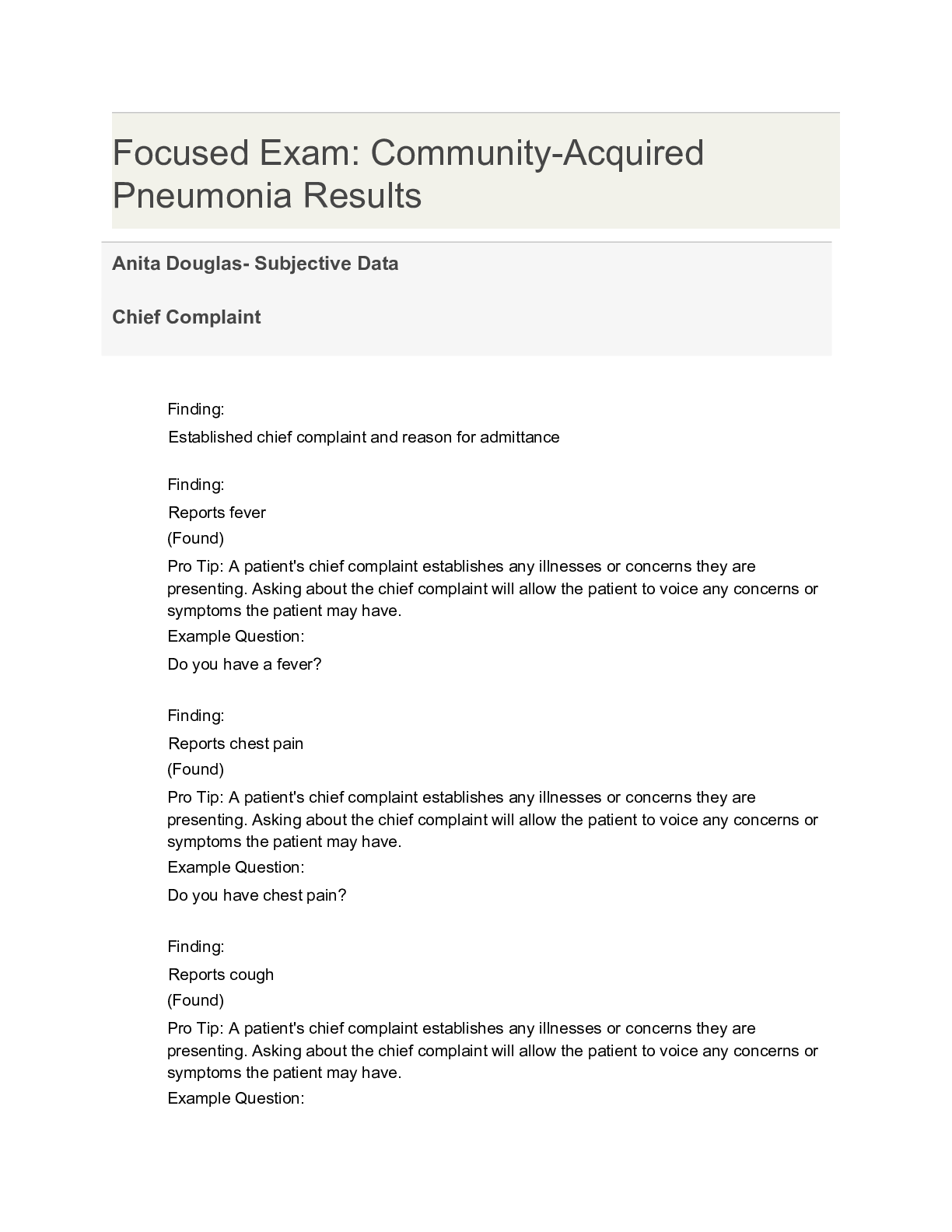
*NURSING > SHADOW HEALTH > Chamberlain College of Nursing NR 509 Chest Pain Documentation Shadow (All)
Chamberlain College of Nursing NR 509 Chest Pain Documentation Shadow
Document Content and Description Below
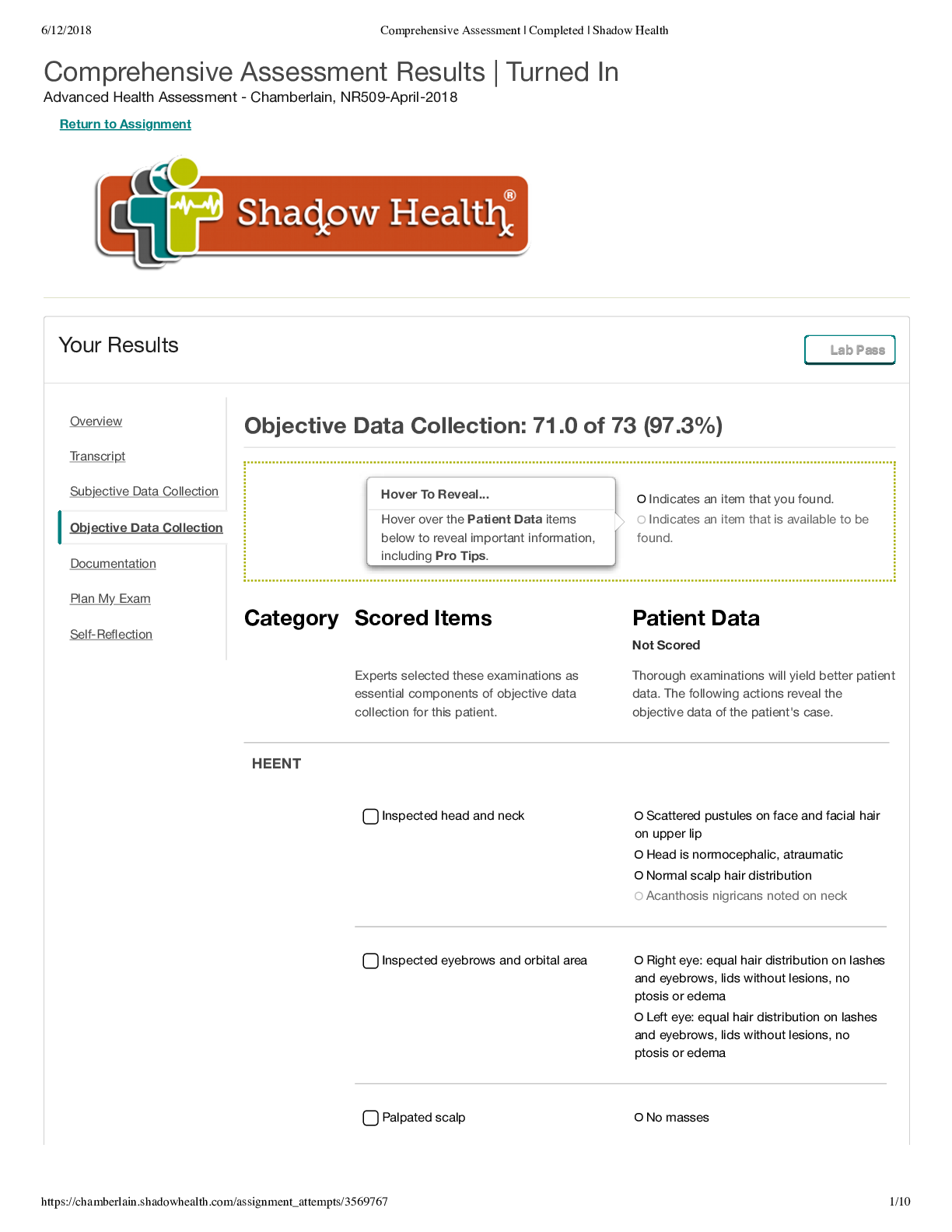
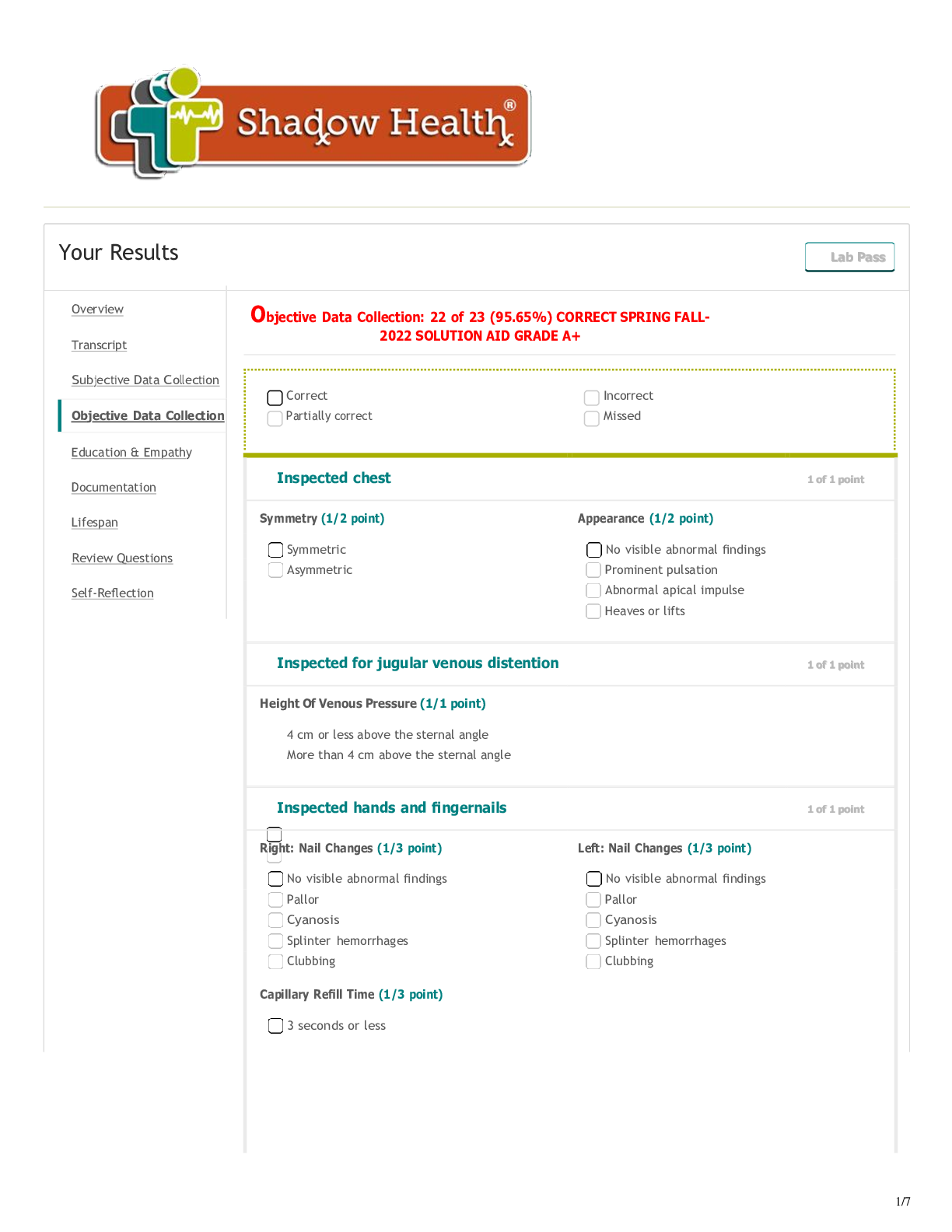
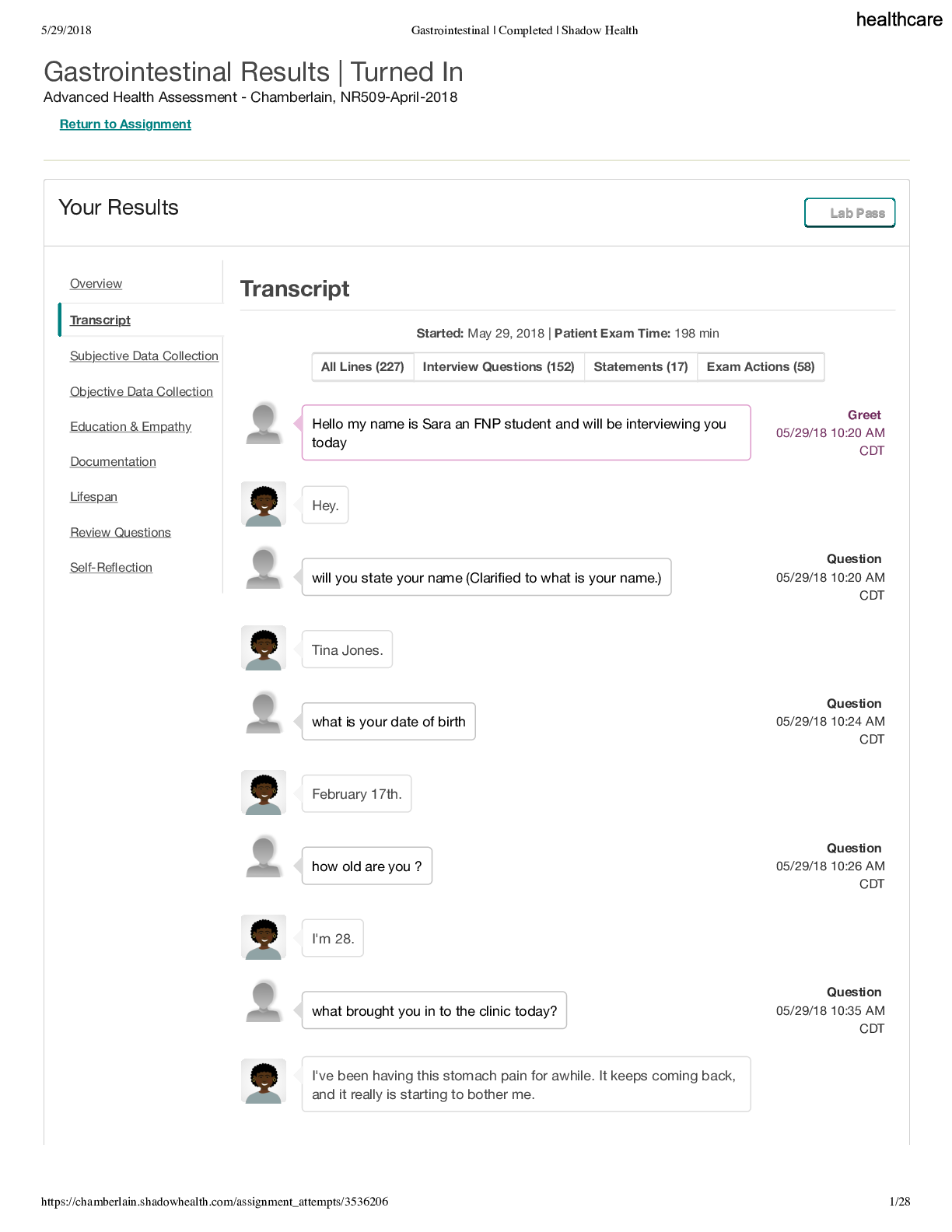
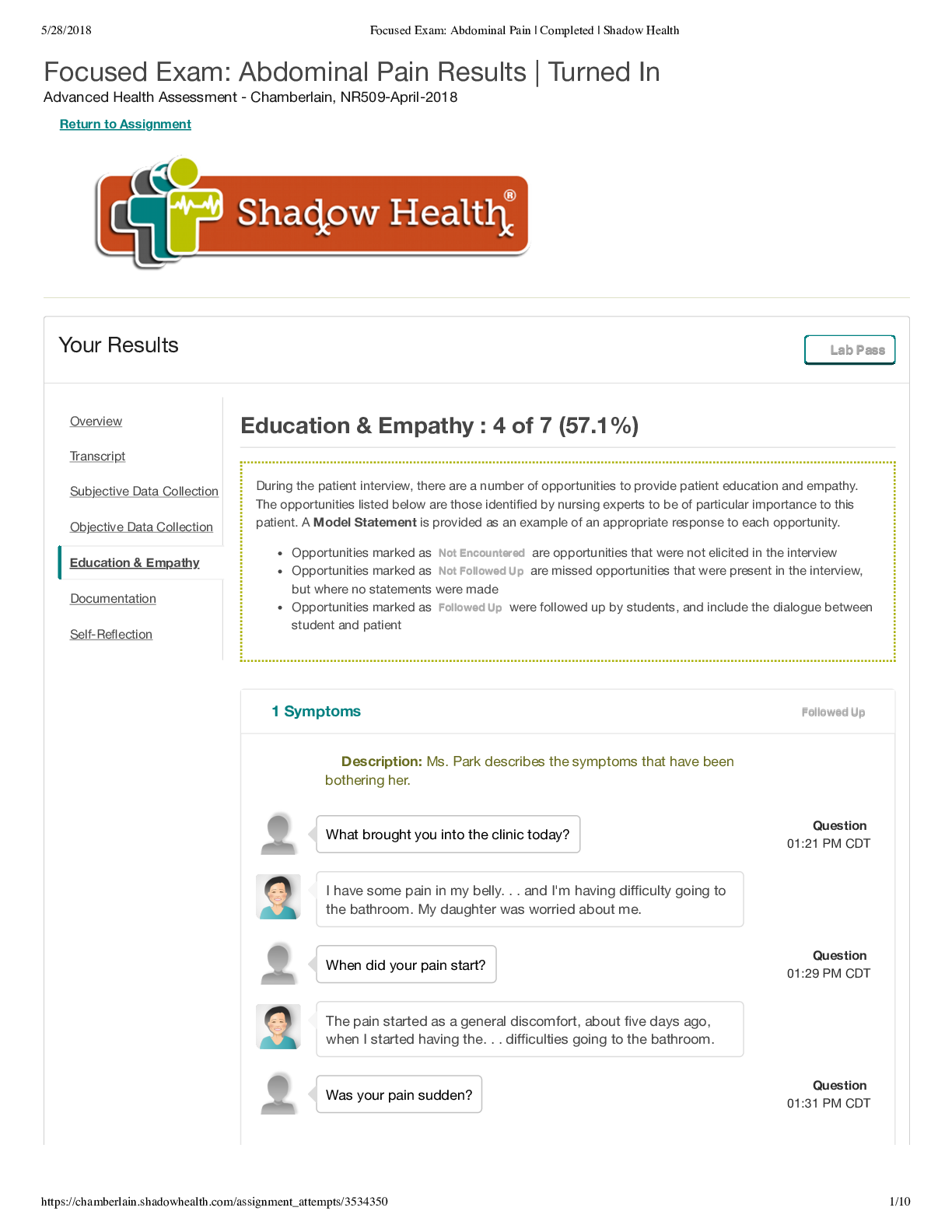
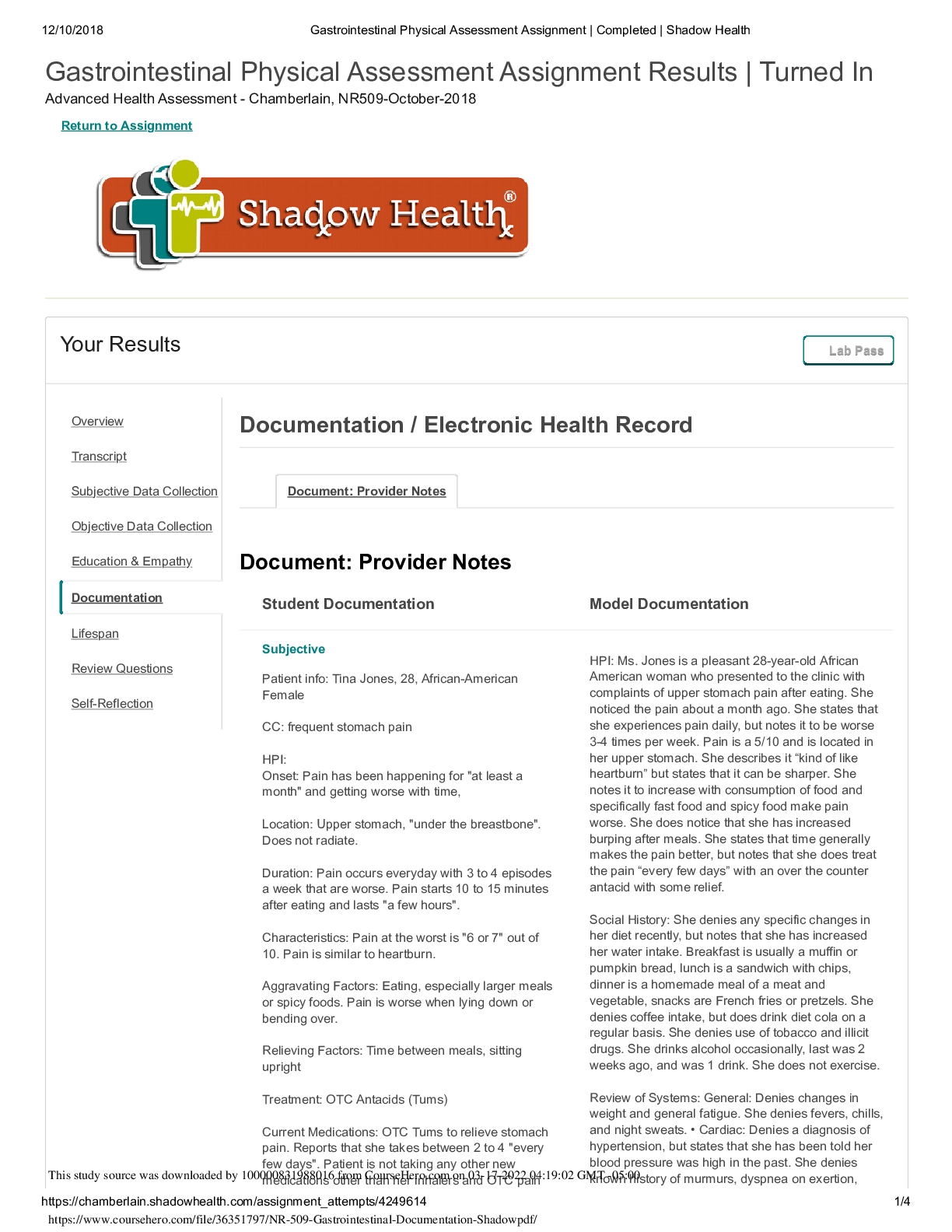
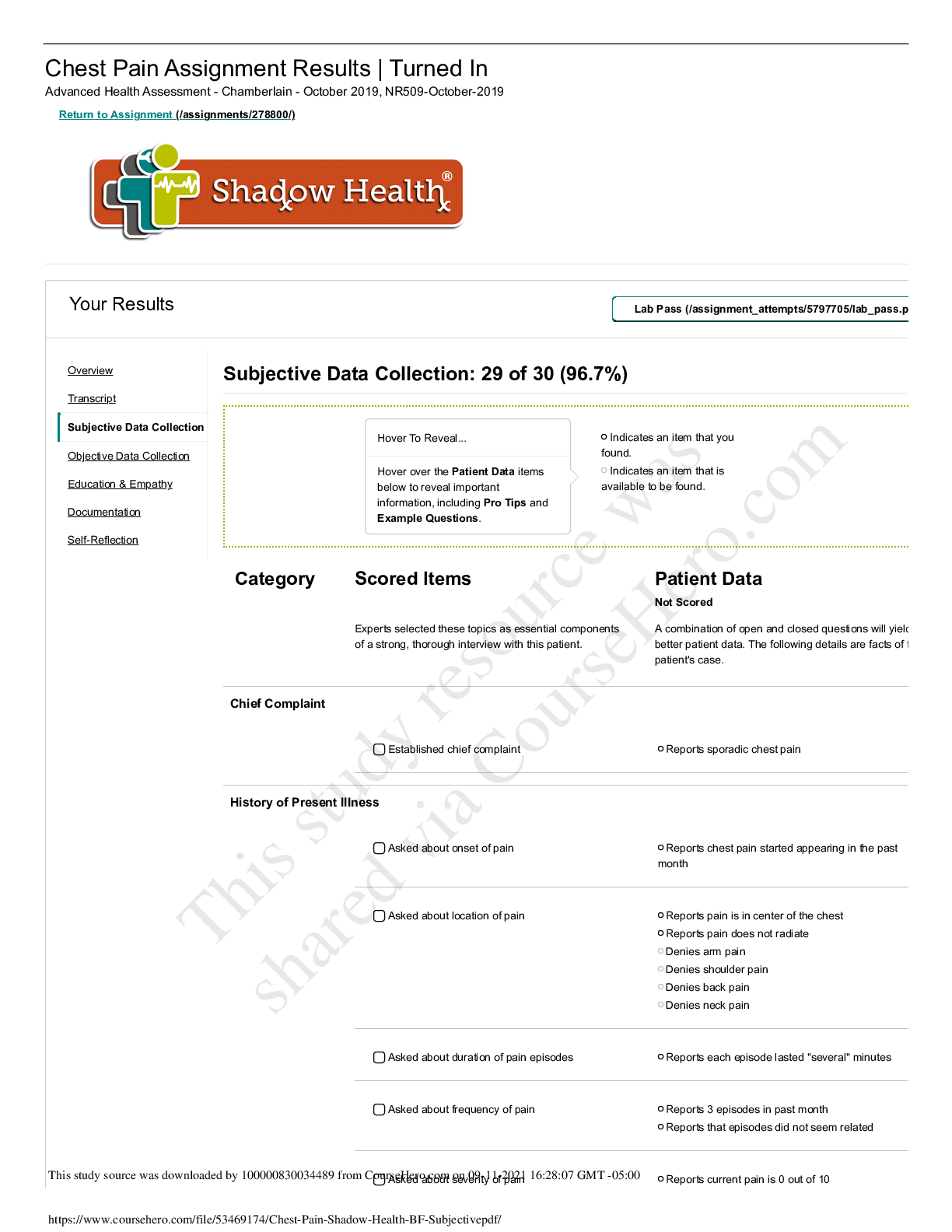
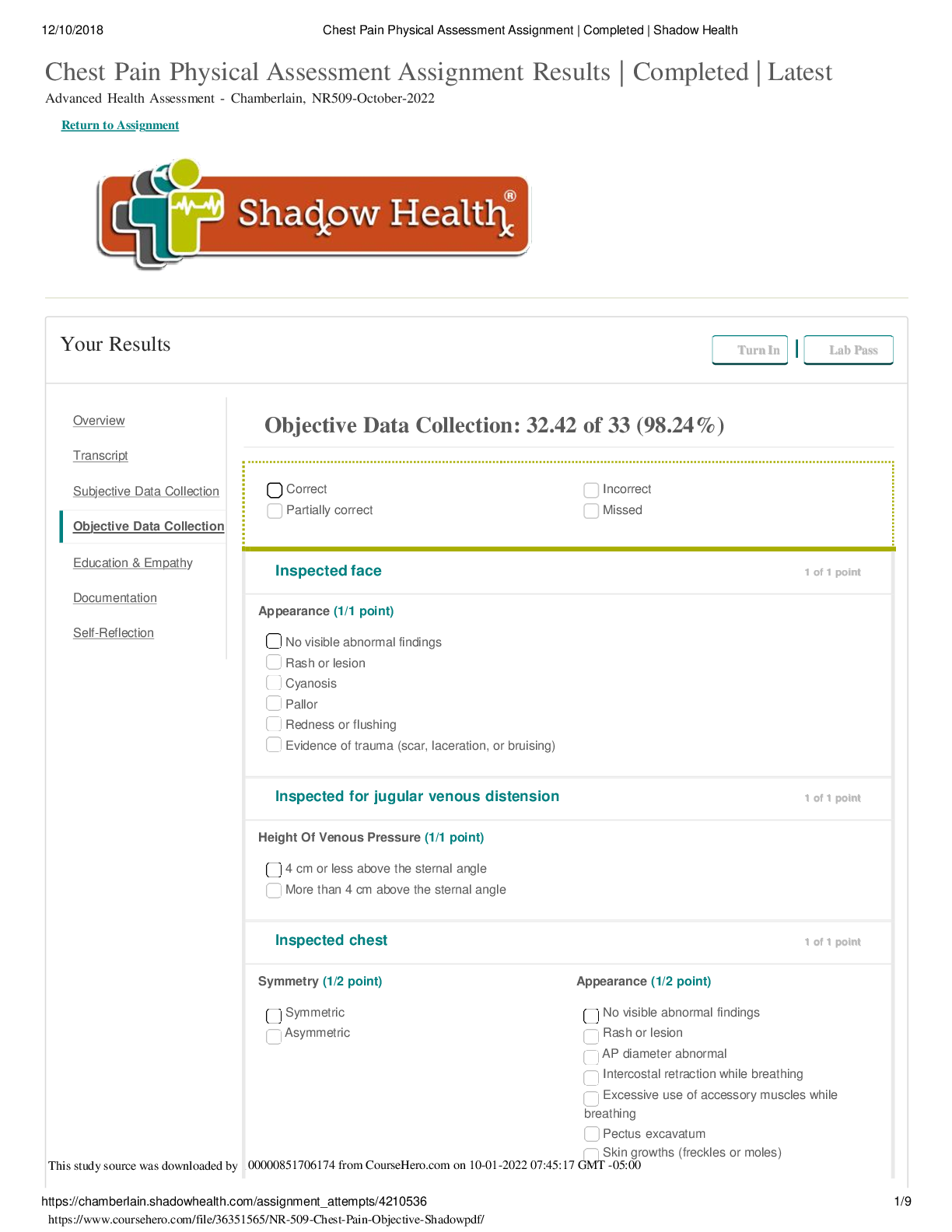
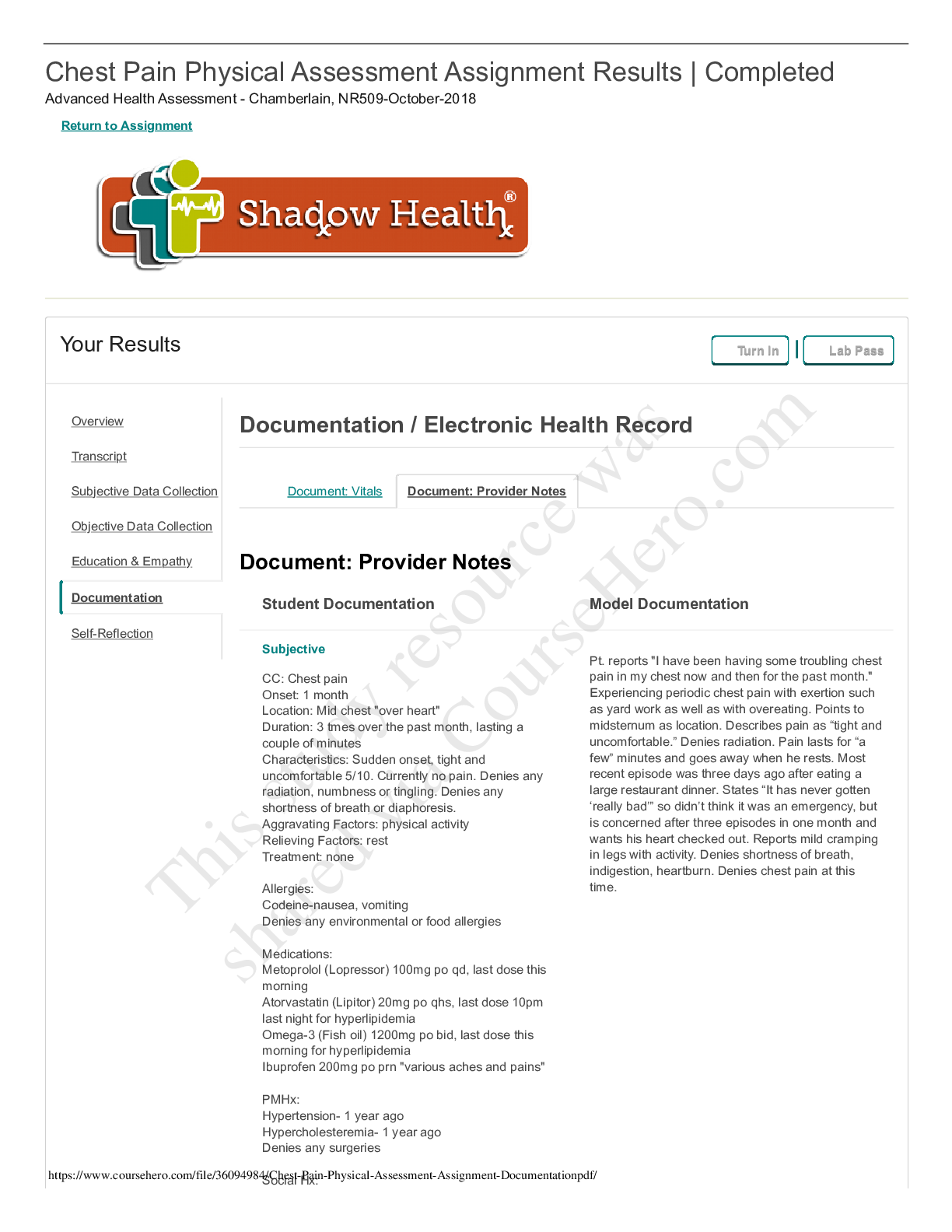
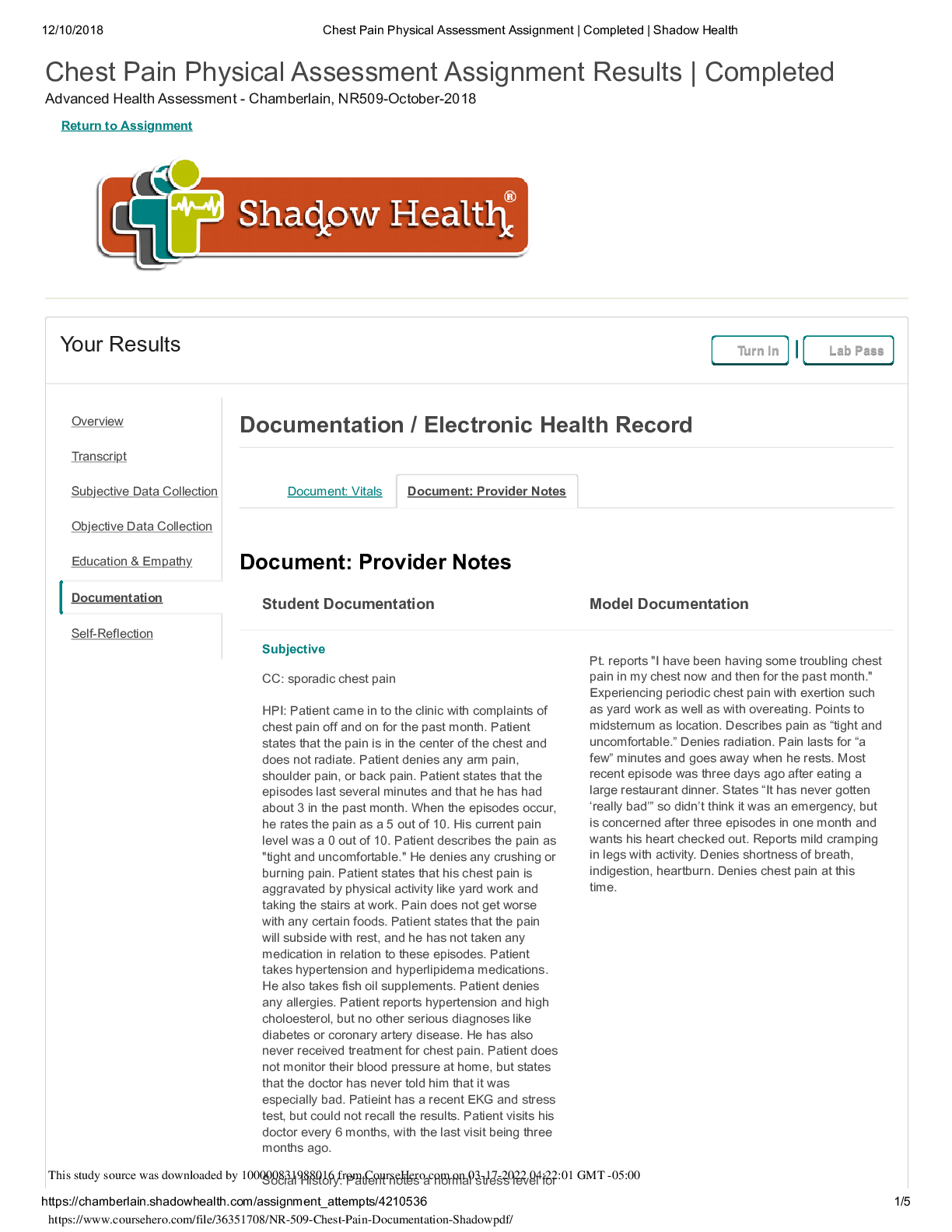
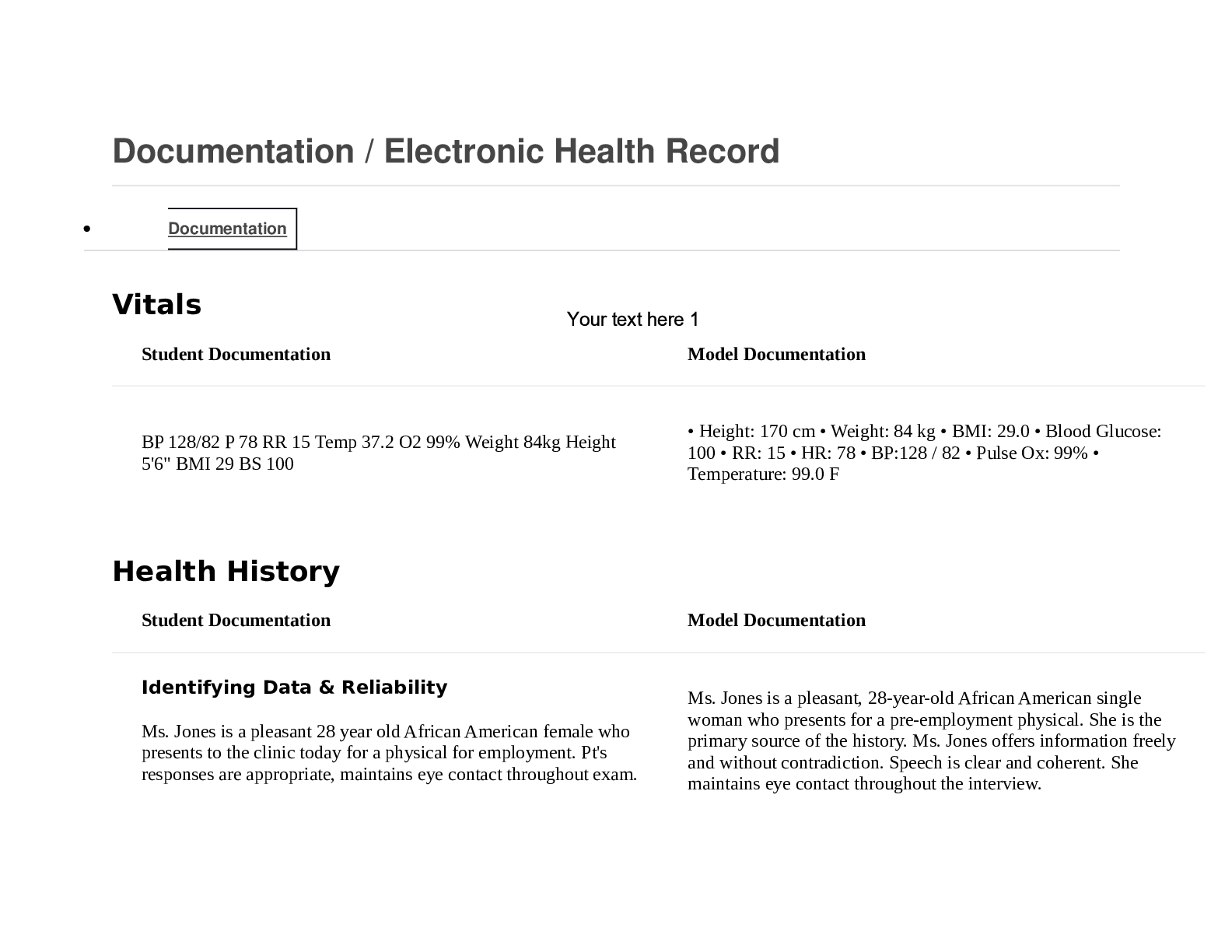
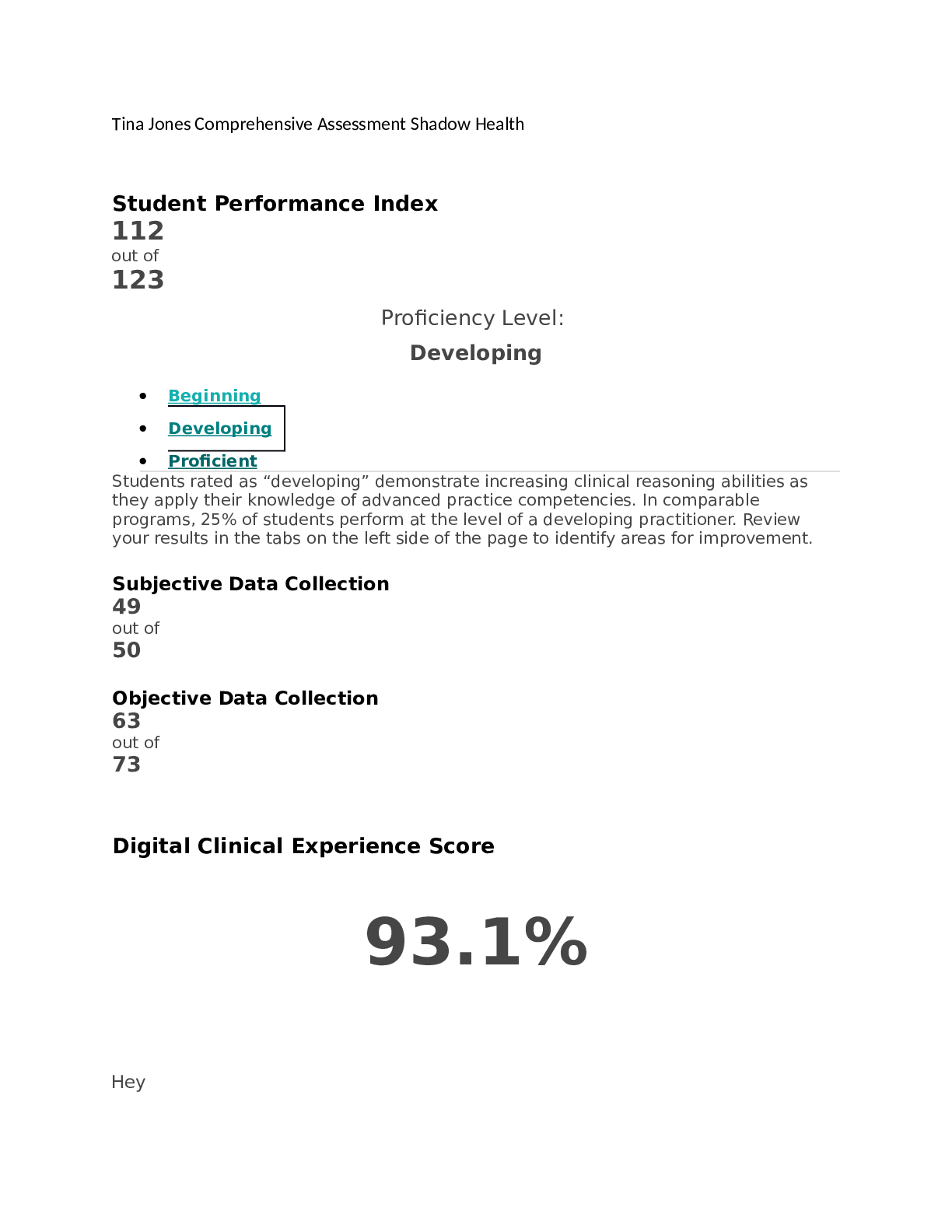
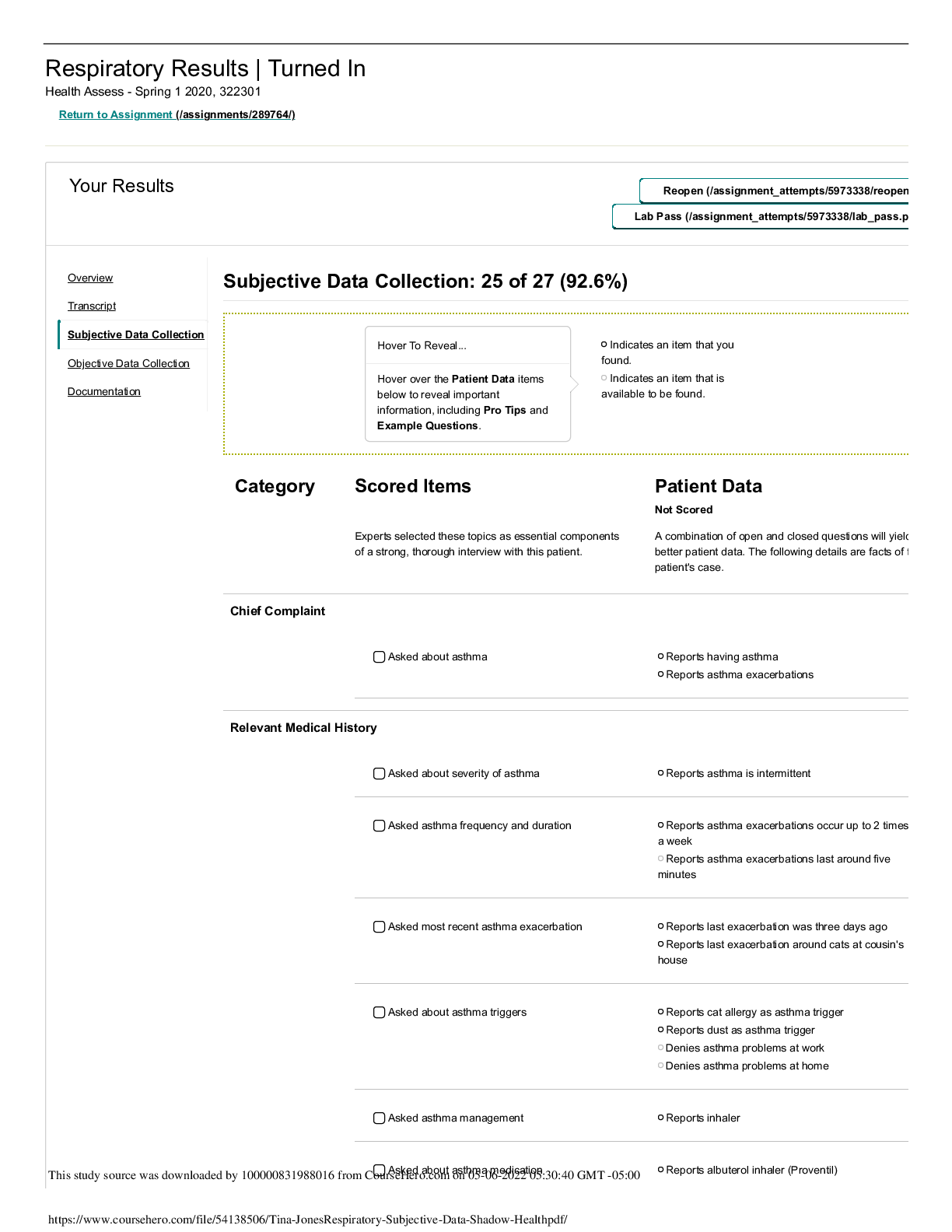
Chest Pain Physical Assessment Assignment Results | Completed Advanced Health Assessment - Chamberlain, NR509-October-2018 Return to Assignment Your Results Turn In Lab Pass Document: Vitals Docum... ent: Provider Notes Document: Provider Notes Student Documentation Model Documentation Subjective CC: sporadic chest pain HPI: Patient came in to the clinic with complaints of chest pain off and on for the past month. Patient states that the pain is in the center of the chest and does not radiate. Patient denies any arm pain, shoulder pain, or back pain. Patient states that the episodes last several minutes and that he has had about 3 in the past month. When the episodes occur, he rates the pain as a 5 out of 10. His current pain level was a 0 out of 10. Patient describes the pain as "tight and uncomfortable." He denies any crushing or burning pain. Patient states that his chest pain is aggravated by physical activity like yard work and taking the stairs at work. Pain does not get worse with any certain foods. Patient states that the pain will subside with rest, and he has not taken any medication in relation to these episodes. Patient takes hypertension and hyperlipidema medications. He also takes fish oil supplements. Patient denies any allergies. Patient reports hypertension and high choloesterol, but no other serious diagnoses like diabetes or coronary artery disease. He has also never received treatment for chest pain. Patient does not monitor their blood pressure at home, but states that the doctor has never told him that it was especially bad. Patieint has a recent EKG and stress test, but could not recall the results. Patient visits his doctor every 6 months, with the last visit being three months ago. Social History: Patient notes a normal stress level for Pt. reports "I have been having some troubling chest pain in my chest now and then for the past month." Experiencing periodic chest pain with exertion such as yard work as well as with overeating. Points to midsternum as location. Describes pain as “tight and uncomfortable.” Denies radiation. Pain lasts for “a few” minutes and goes away when he rests. Most recent episode was three days ago after eating a large restaurant dinner. States “It has never gotten ‘really bad’” so didn’t think it was an emergency, but is concerned after three episodes in one month and wants his heart checked out. Reports mild cramping in legs with activity. Denies shortness of breath, indigestion, heartburn. Denies chest pain at this time. Overview Transcript Subjective Data Collection Objective Data Collection Education & Empathy Documentation Self-Reflection Documentation / Electronic Health Record This study source was downloaded by 100000831988016 from CourseHero.com on 03-17-2022 04:22:01 GMT -05:00 https://www.coursehero.com/file/36351708/NR-509-Chest-Pain-Documentation-Shadowpdf/ 12/10/2018 Chest Pain Physical Assessment Assignment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/4210536 2/5 Student Documentation Model Documentation his lifestyle. He denies regular exercise for the past two years. His food intake is things like sandwhiches and grilled meats and vegetables. He drinks water regularly, but also consumes two cups of coffee a day. Patient does not smoke, do any illicit drugs, and only drinks socially, 2-3 drinks on the weekends. Family History: Patient notes a family history of heart attack, but denies a family history of stroke or pulmonary embolism. ROS: General: Patient denies any fever, denies fatigue, denies any dizziness, and denies any palpitations. Patient notes that they have gained around 20lbs, but attributes it to aging. Cardio: Patient denies any angina, edema, circulation problems, easy bleeding, and easy brusing. Respiratory: Patient denies any cough or difficulty breathing. HEENT: Patient denies any changes in taste and any sore throat. Gastro: Patient denies any nausea, vomiting, bloating, or heartburn. Current medications: Lopressor 100mg once daily and Lipitor 20mg once daily at bedtime [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 17, 2022
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Mar 17, 2022
Downloads
0
Views
59




.png)
.png)