Health Care > DISCUSSION POST > HSM 410 Week 2 Discussion Question 1 – U.S. Healthcare System Organization (RATED A+) (All)
HSM 410 Week 2 Discussion Question 1 – U.S. Healthcare System Organization (RATED A+)
Document Content and Description Below
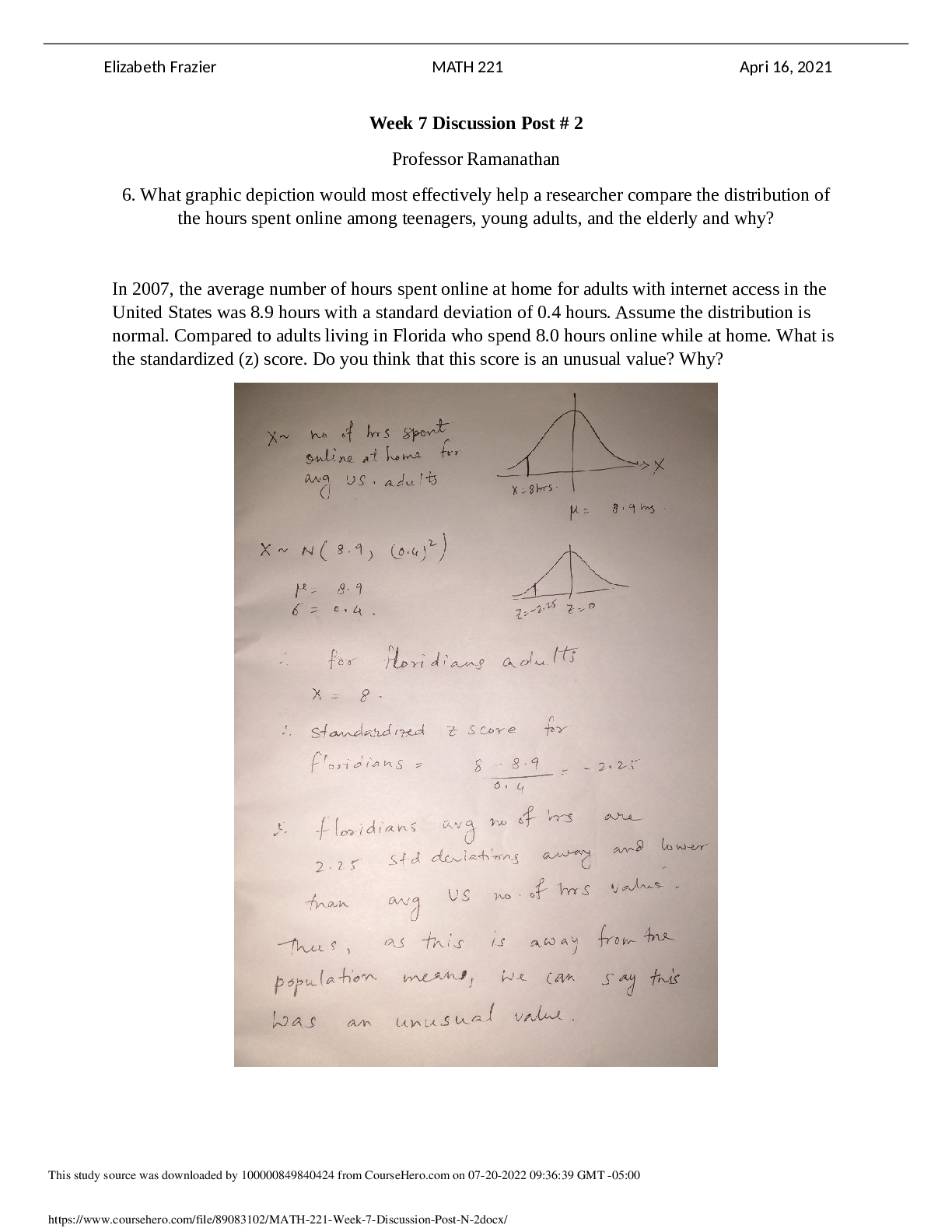
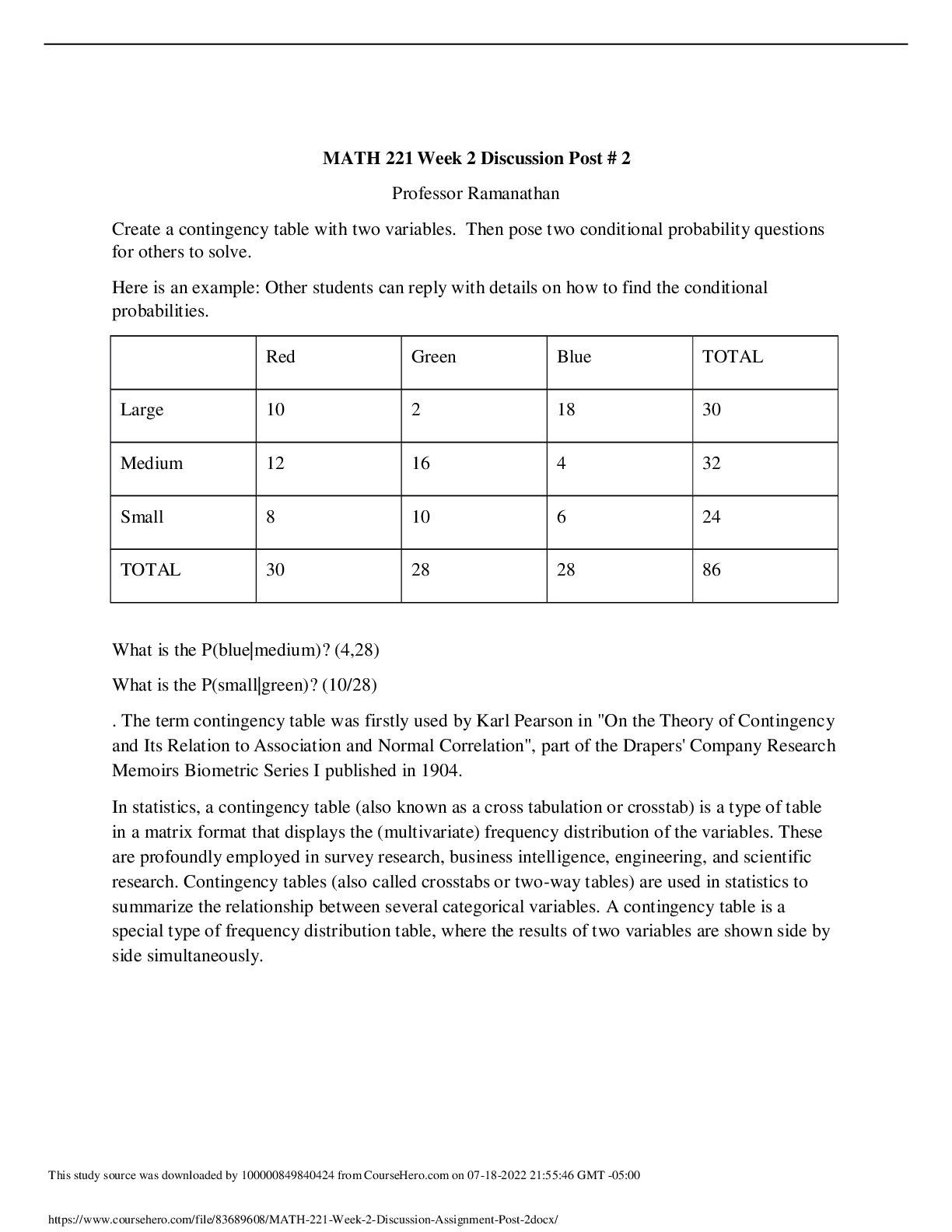
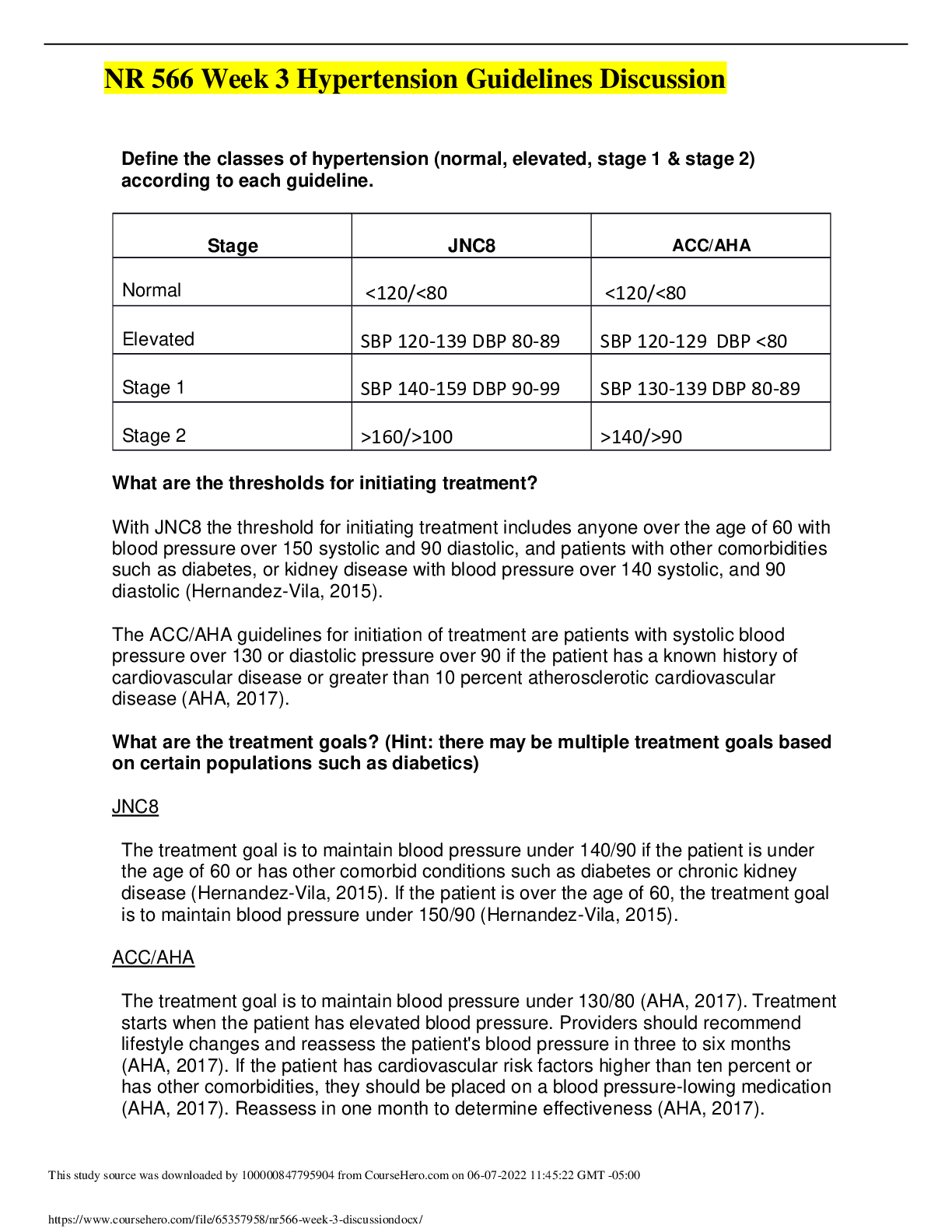
HSM 410 Week 2 Discussion Question 1 – U.S. Healthcare System Organization What have been some of the forces driving the organization of U.S. healthcare? Bodenheimer states that there are sever... al reasons for the forces driving the organization of U.S. healthcare: 1.) The biomedical model - basically in a nutshell, as diseases have grown or developed, like different strains of the flu, cancers, and etc., the needs for more than just family practice has moved to needing more specialty disciplines, plus the 1-year general practice internship was replaced by a 3-year residency program and specialty board certifications. 2.)Financial incentives - to be more exact, financial incentives for physician specialization and hospital expansion began. 3.)Professionalism - The last thing is the nature of control over health planning. "The U.S., unlike other nations, is unique in its relative laxity of public regulation of health care resources." So the professional status that comes with being a physician has given them a special authority to guide the development of the U.S. healthcare system. (Chapter 5, 2012) Bodenheimer states, “People in the United States rightfully take pride in the technological accomplishments of their healthcare system.” (Chapter 5, 2012) The need for Family Practitioners and General Practitioners for the U.S. population has been a subject of debate and legislative concern for a couple of decades. It will reach a critical concern with the Baby Boomers turning senior and healthcare reform. (Chapter 5, 2012) Class, why has the U.S. seen more focus on the specialist versus the general practitioner? The U.S. seen more focus on the specialist versus the general practitioner because the fees are higher for a specialist. The figure shows trends over time in the average income of primary care physicians relative to specialist physicians in the U.S. and in the percentage of graduating medical students in the U.S. planning on entering careers in primary care. The average primary care physician income was about half that of specialist. (chapter 5, 2012) "Generalists earn lower incomes than specialists". Due to education costs more specialized medicine leads a higher salary verses the salary of a generalists. "Generalists appear to practice less resource-intensive style of medicine and generate lower overall healthcare expenditures, including less use of hospital and laboratory services". General practitioners treat acute diseases, the rise of chronic disease in the U.S has raised the demand of specialists. Bodenheimer states, “Critics of the US health care system find fault with its “top-heavy” specialist and tertiary care orientation and lack of organizational coherence. Analyses of health care in the United States over the past half century abound with such descriptions as “a nonsystem with millions of independent, uncoordinated, separately motivated moving parts,” “fragmentation, chaos, and disarray,” and “uncontrolled growth and pluralism verging on anarchy.” (Chapter 5, 2012) Class, do you agree? Does this affect the driving forces? I agree, the American health system is a mixture of independent moving parts with individual agendas which is an extensive contributor factor guiding the organization of healthcare within the U.S. The specialist’s oriented and chaotic health care structure has added to the rising cost of care. Moreover, this type of format deteriorates quality of care. For instance, when many hospitals each perform small numbers of surgical procedures such as coronary artery bypass grafts, mortality rates are higher than when such procedures are regionalized in a few higher-volume centers (Bodenheimer & Grumbach, 2012). Some of the driving forces of the organization of U.S. healthcare is from the economy and the patients. The recession has reduced their employment, their benefits, and now other costs for families are rising gas being the most recent. As state and local government frantically reduce services to balance their budgets, health care simply has to deliver more value. The government is trying to focus on better performance and bedside manner from all healthcare professionals and ThDisosctutdoyrsso.urIcfetwhaesydoawrneloaabdeldebtyo10m00e0e0t82t9h9e57s1t2a5nfrdomarCdosurtsheHaetrao.rceomreonqu03i-r0e2d-20t2h2e2n3:t1h7:e2i8rGpMaTy -c0a6:n00increase. This can also be referred to as an incentive to have the health care professionals work harder to manage the proper patient care. Our hospital is always doing the HCAHPS and NCR pickers to see how were doing and what need to be improved. In our office we do Oswestry per and post op scoring which helps with reimbursement for the office. Pay for performance is the wave of the future and honestly the topic of much debate in the health care realm. CMS has initiatives that are directed at not only paying for the services but also basing this payment on patient outcomes. I know from personal experience as an Inpatient case manager for an insurance company CMS has a re-admission policy that if the person is re-admitted for similar symptoms and has not remained in the community for 24 hours post discharge then the hospital will not receive another DRG payment. This was one of the beginning steps to having providers be responsible for positive outcomes. The Affordable Care Act has also addressed many of these areas such as the "Hospital Readmissions Reduction Program and the Hospital-Acquired Condition (HAC) Reduction program" All of this is the beginning of the shift. I know at my company we are discussing metrics and outcome incentives to be implemented and added to our providers. This is not only for the inpatient facilities but for all service providers. References: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNMattersArticles/downloads/MM3389.pdf http://www.medicare.gov/hospitalcompare/linking-quality-to-payment.html?AspxAutoDetectCookieSupport=1 Class, do you feel that the U.S. is a dispersed or regionalized model of care? Why or why not? What does this mean? I feel that the U.S. is a dispersed model of healthcare. I say this because the regionalized healthcare model has all healthcare organizations in the area controlled and maintained under a single organization or agency. All the different private healthcare insurance companies, as well as government insurance like Medicaid, are in no way operated by one entity. They all operate differently, but in accordance to government rules and regulations, of course. Does anyone else have any input? I was fairly unsure of how to answer this as I hadn't really become familiarized with these two terms yet. I feel that the US provides a dispersed model of care sine there are so many different types of insurance carriers to choose from. Now Canada, on the other hand would be considered regionalized due to the government being a single payor. Class, discuss the pros and cons of requiring everyone to enter the healthcare system through a gatekeeper healthcare provider? Some of the pros and cons of requiring everyone to enter the healthcare system through a gatekeeper healthcare provider are; more coverage, a more competitive insurance industry, insurance company would have to accept everyone, cheaper prescriptions for seniors, its reform. Some cons are cuts in medicare, costs, no new incentives for primary care physicians, more taxes. Its beneficial to have reform for us because "We’re in a situation where healthcare is even becoming unaffordable to employers, leaving employees with higher out-of-pocket expenses even if they are ensured." A negative to enter the healthcare system through a gatekeeper healthcare provider "the government has to pay for healthcare reform somehow." This would indicate more taxes. http://www.businesspundit.com/the-pros-and-cons-of-the-new-health-care-reform-bill/ Why have physician reimbursement models changed over the years? Physician reimbursement models have changed because of cost containment. Nobody wants to spend money excessively or unnecessarily. "Private insurers, Medicaid and Medicare replaced fee for payment services, which encouraged use of more services." This placed economic pressure on the physician/hospital to limit the number and costs on their services. Bundling the services shifted the financial risk away from payers and providers onto the physician/hospital. Now, instead of the provider solely setting fees, "the payment levels are more often determined by payers and providers or by fee schedules determined by payers." I think this way is probably better because it helps to balance out overtreatment or undertreatment and controls costs. Health reform initiatives, such as patient-centered medical homes, ACOs, and bundled payments, are significantly altering the way in which physicians — even those that remain independent — will be paid in coming years. - See more at: http://www.physicianspractice.com/blog/changing-reimbursement-models-challenging-physicians- administrators#sthash.YUoLUnrP.dpuf http://www.physicianspractice.com/blog/changing-reimbursement-models-challenging-physicians-administrators According to Bryant, “the state affairs in healthcare, healthcare reimbursement has changed dramatically and that reimbursement based upon fee-for-service will gradually disappear and will be replaced by models based upon the ability to better manage patient diseases and conditions. This means that reimbursement will be based upon the quality This study source was downloaded by 100000829957125 from CourseHero.com on 03-02-2022 23:17:28 GMT -06:00 of the quality of service delivered by the provider" (Bryant, 2012). Several factors contribute to this; the recent studies showed that more than 50% of healthcare spending in the U.S. is wasted or harmful. "Costs have been rising 7% to 8% per year, healthcare was 18% of GDP in 2012 and was set to double to 30% GDP by 2030" (Bryant, 2012) Bodenheimer says, “During the course of a typical day, some physicians will be involved with four or five distinct types of reimbursement.” (Chapter 4, 2012) The five different types of reimbursements are Fee for service payment, payment by episode of illness, per diem payments to hospitals, capitation payment and payment for all services delivered to all patients within a certain time period. Methods of payment range from the simplest (one fee for one service rendered) to the most complex (Chapter 4, 2012) These include: Fee for service (FFS) Payments by Episode of illness Per diem Capitation Payment for all services Delivered to all patients in a select time frame Managed Care Plans Fee for service with Utilization Review Preferred Provider Organizations (PPO) Class, why is understanding the financial risk involved with a payment method important to providers? To insurance companies? The pros and cons of the five models—fee for service, pay for coordination, pay for performance, episode or bundled payment, and comprehensive care or total cost of care payment. It also offers the work group’s recommendations for how these models might be applied in a reformed health care system. One challenge facing physicians, hospitals, payers, and policy makers is managing the transition to new payment models. Because numerous models and countless combinations of them may be employed as alternatives to fee for service, selecting the most appropriate options can be confusing. Cleverley says that “capitation reimbursement reverses the actions that providers must take to ensure financial success. Under all prospective payment methods, the key to provider success is to work harder, increase utilization, and hence increase profits. Under capitation, the key to profitability is to work smarter and decrease utilization.” (Cleverley, Chapter 3) Class, who assumes risk with capitation? How does this affect delivery of healthcare to the patient? Capitation or payments per patient are monthly fixed lump sums of monies paid out by an insurer for each of its enrolled patients to a medical facility to provide medical care. The idea of capitation is to shift the risk from the insurer to the provider. If one patient within the plan requires long lasting extensive care, tests and procedures the expenses could greatly surpass revenues earned from the other patients that required little to no treatment. In this method quality of care may be reduced because it is in the best interest of the hospital to conserve supplies to increase profits (Bodenheimer & Grumbach, 2012). There is also a matter of calculating the risk. Many physicians' practices I have known, signed a contract without calculating the financial risk they incurred by the contract and if those covered lives were young and healthy or older and more prone to illness. They merely wanted to increase their patient base. ThCilsasstusd,ywsohuarcte iwsa‘sadsoswunmloaindegd rbiys1k0?0’0W008h2o99i5n7c12u5rsfrormiskCowuristehHetrho.ecovmaornio0u3-s02p-a20y2m2 2e3n:1t7t:2y8pGeMs:TF-F06S:,00capitation, per diem, etc? Provider groups are taking on risk-based contracts in which healthcare payers offer financial rewards for quality and cost management targets. Risk has its rewards. Capitation Fee for Service Providers assume Risk No or little risk for Providers Withholds or Bonuses/ Risk Sharing Pools Traditional system of payment for Providers Management Center: Manage the spectrum of health care services - financial incentive to keep patient treatment cost low Cost Center: Financial incentive to maximize reasonable patient treatment costs Health/ Preventive Care Sick Care Health maintenance/ Preventative medicine/ Bonus for appropriate and efficient use of resources More income is derived from frequent patient- physician encounters since physicians are paid for each visit. Physicians do not pay for services (including consultations/ tests/ procedures, etc.) out of pre-arranged capitation. More tests ordered/More services rendered/ May possibly mean more $ for physician Outpatient care preferred over inpatient care Oriented to both Inpatient care and Outpatient care Know costs of services provided Charge cost plus profit margin Financial risk to physicians if treatment costs exceeds proceeds from capitation payments No or very low financial risk to physicians Capitation check every month Time intensive collection process - Charges plus collection percentage determines income Relationship with MCO’s, other Providers, interactive, communicative oriented, money required to build information structure that is vital to operation of a continuum of care Can be more isolated, emphasizes independence (though consultants are indirectly rewarded and independence is from insurance payor), autonomy "Business case" is defined as a positive return on investment within a reasonable period of time for the parties that invest in these improvements. The authors call for changes in health care payment policies to provide financial rewards to parties who pay for the development and implementation of improvements in health care. http://www.medicalpracticecme.com/Class%201/Articles%20for%20class%201/article_6.htm The risk with capitation is assumed by the medical provider because they are given a monthly payment for each patient on that insurances roster that is assigned to them without regards to the amount of times that the patient will actually be seen or not. For exmple, if a provider has an elderly patient that is on an insurance that pays by capitation and that patient needs to be seen twice a week for 3 weeks due to a fall that they had that left them with an infected skin abrasion on the arm, well the provider still will only recieve that one payment for that patient. Now if a 20 something is on the same insurance and is assigned to the same clinic and has no reason to be seen for the whole year, well the provider will still recieve that monthly payment without having to worry about using time for that patient. That is why some providers might rush, or not do as many follow ups on patients with capitated insurances. The government has attempted to control cost for decades. Many payment plans today use the Bundled Services arrangement. Bundled services have two key features: payment is grouped into a mutually exclusive set of service categories (such as per diem or per case rate), and secondly, the bundled services arrangement may have a fixed fee for Thuins sittuodyf ssoeurrcveicweas(dleownngltohadeodfbsyta10y00ti0m08e29s9a57n12e5gforotimaCteoudrspeHeerrod.cioemmonra0t3e-0.2)-M202e2d2i3c:a17r:e28dGeMveTl-o0p6:e00d a bundled services payment plan for most healthcare providers which has strongly impacted the rest of the industry and had become the standard for many health plans: RBRVS and MS-DRG. (Cleverley, 2011) Class, describe these two payment systems. Who assumes risk with these methods? I think that the two payment systems that pay by bundling services are one payment per illness (diagnosis code) and capitation. In the payment per illness our text states that a lot of insurances will do this for pregnancy diagnosis, so the provider does not get paid fee- for-service but a lump sum for a specific diagnosis code. The same would happen like when my husband had to have gallbladder surgery, his surgeon only got paid one specific amount for the surgery and all follow up visits that were needed afterwards. Bodenheimer et al (2012) goes on to state that, "Bundling of services transfers a portion of the risk from the payer to the physician" (Bodenheimer, 02/2012, p. 34). Now with capitation a medical provider will get a monthly payment regardless if their patient needs 0 visits that month or 15 visits for a particular illness. Once again, the risk is moved from the insurance company to the provider. Class, we can anticipate many changes in reimbursement methods. This article is interesting! What do you think? http://www.nejmcareercenter.org/article/physician-compensation-models-big-changes-ahead/ Cleverley notes that, “Under historical cost reimbursement, payers reimburse providers for all costs, a system that provides little incentive to control costs. Facilities will be lavish and amenities plush. Services that may not truly be required might be provided because more services lead to higher costs, which mean higher revenues. Cost-based reimbursement is the least risky for providers because payers more or less ensure that costs will be covered, and hence profits will be earned.” (Cleverley, Chapter 3) Class, are there many payers that pay by cost reimbursement? Why? There are many payers that pay by cost reimbursement. The cost of healthcare is increasing an the quality is not being matched with the high prices, I think that this is to cut down the cost of unnecessary procedures from being performed, and to focus more on the quality than the performance. I can agree that the more payers that pay by cost reimbursement the cost of healthcare is increasing at an quality is not being matched. Focusing on more quality than the performance is a better way to do business anyway. Cost reimbursement is "a cost reimbursable contract (sometimes called a cost plus contract) is one in which the contractor is reimbursed the actual costs they incur in carrying out the works, plus an additional fee." http://www.designingbuildings.co.uk/wiki/Cost_reimbursable_contract Rising costs are harmful to everyone because they make health services and health insurance unaffordable. (Bodenheimer, 02/2012, p. vi) Bodenheimer, T., Grumbach, K. (02/2012). Understanding Health Policy, 6th Edition [VitalSource Bookshelf version]. Retrieved from http://online.vitalsource.com/books/0071802304 The citation provided is a guideline. Please check each citation for accuracy before use. This study source was downloaded by 100000829957125 from CourseHero.com on 03-02-2022 23:17:28 GMT -06:00 [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 03, 2022
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Mar 03, 2022
Downloads
0
Views
66


.png)