*NURSING > STUDY GUIDE > NUR2790: Professional Nursing III / PN3 Final Exam Study Guide RN 3 | Download To Score An A (All)
NUR2790: Professional Nursing III / PN3 Final Exam Study Guide RN 3 | Download To Score An A
Document Content and Description Below
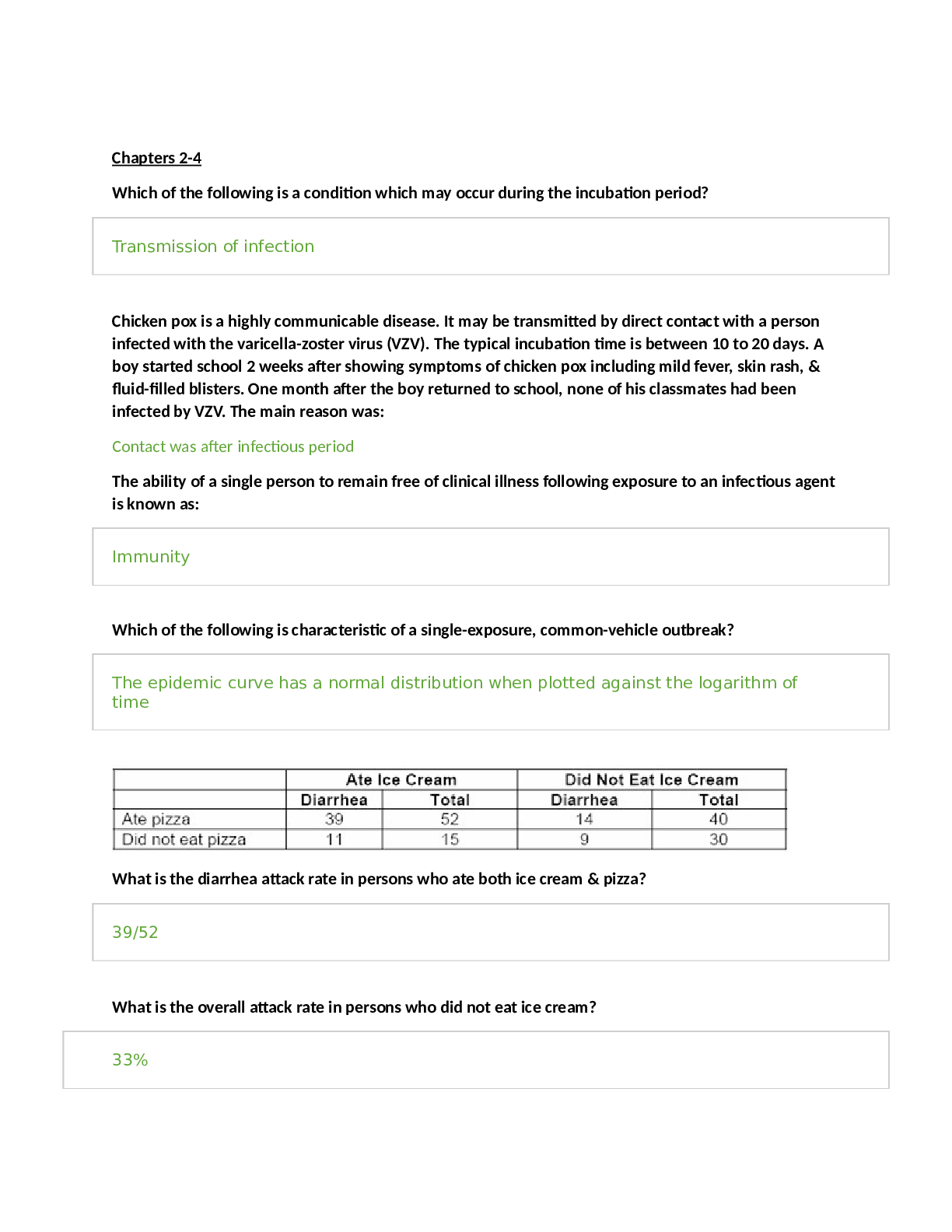
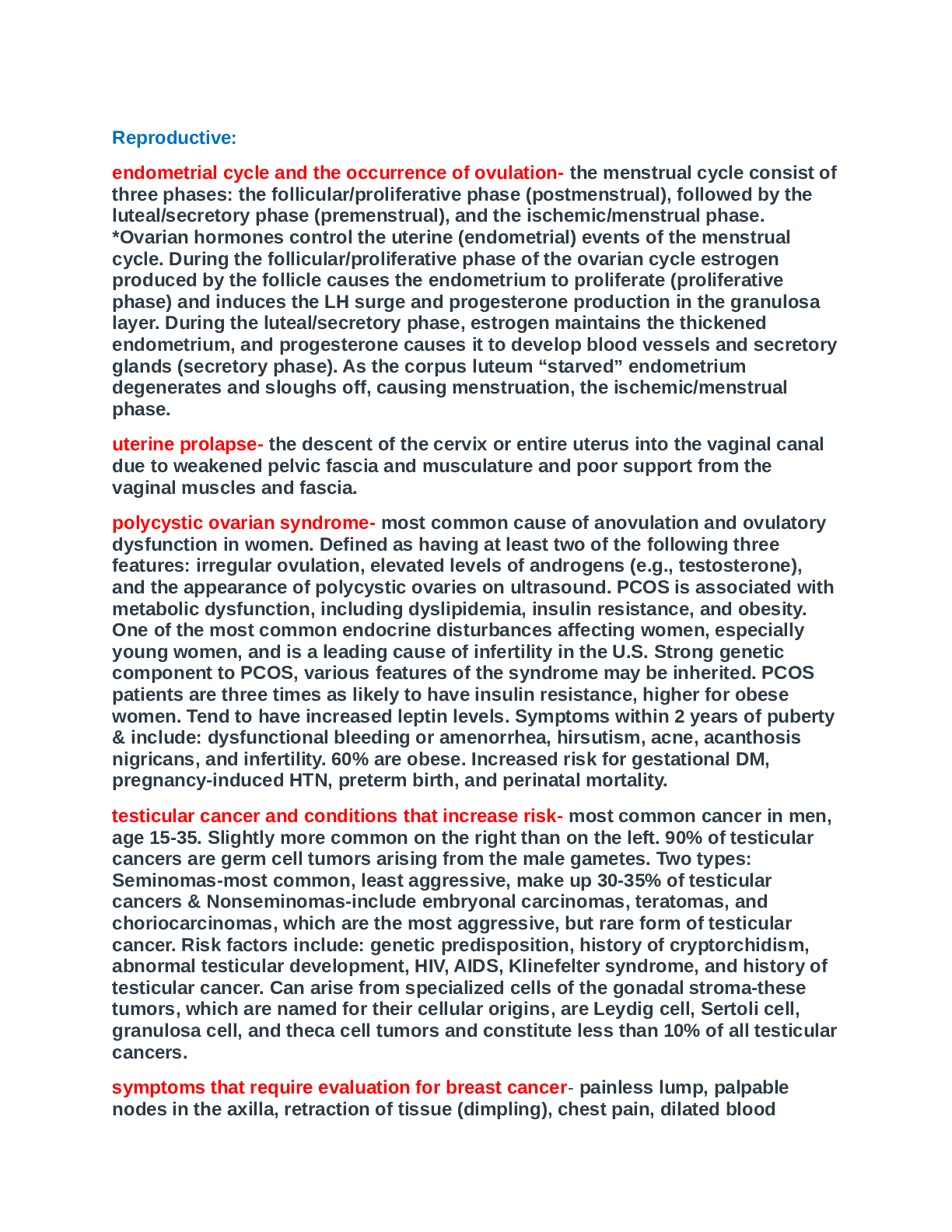
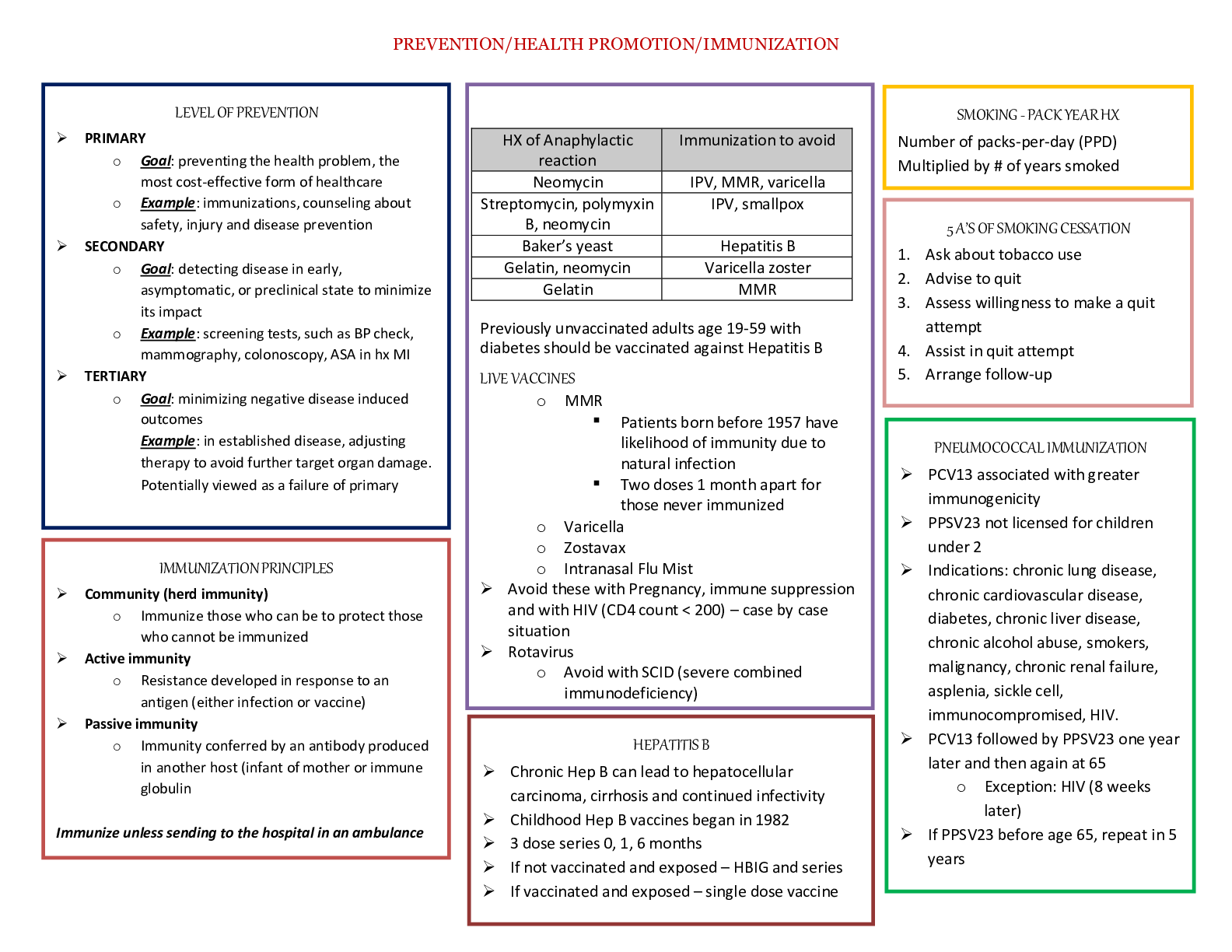
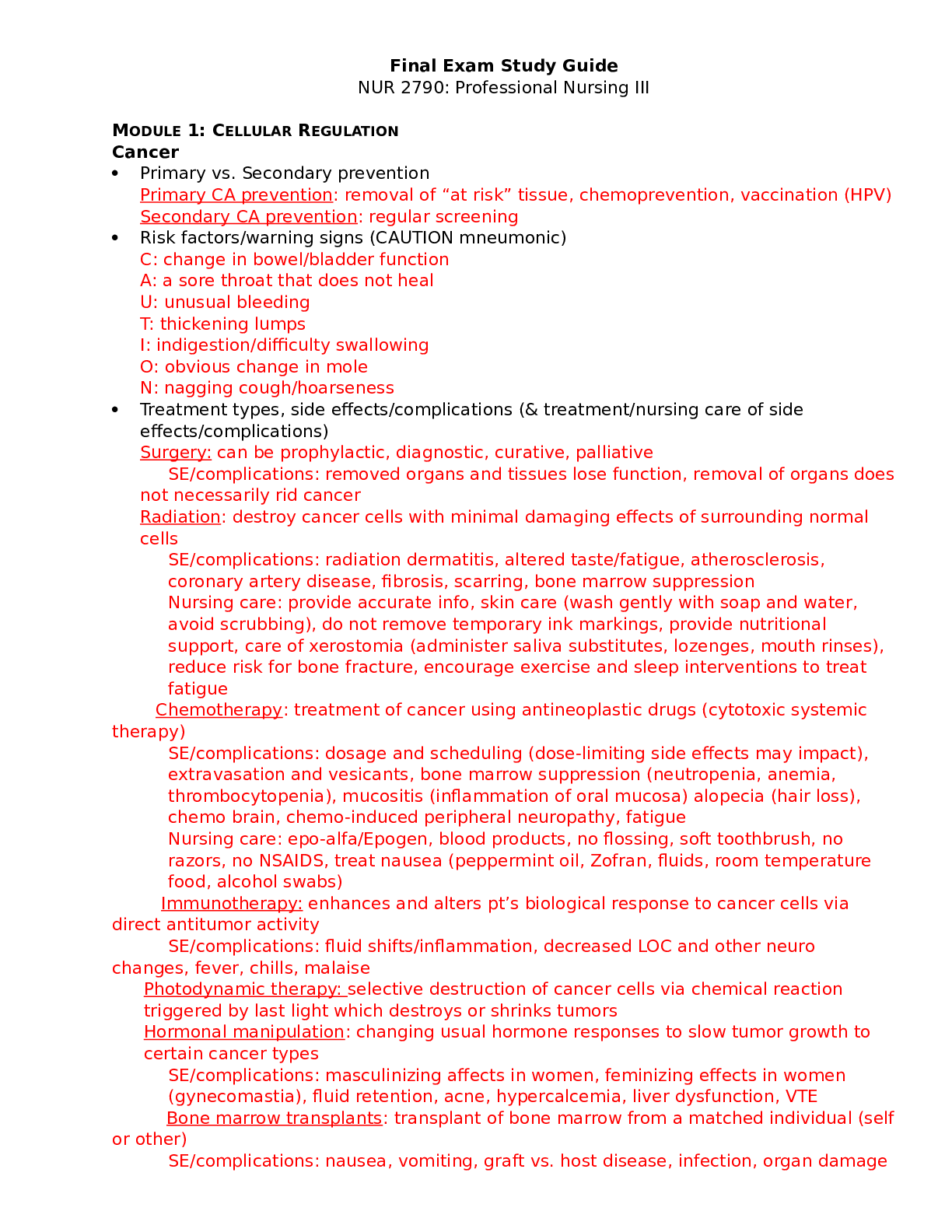
Final Exam Study Guide NUR 2790: Professional Nursing III MODULE 1: CELLULAR REGULATION Cancer • Primary vs. Secondary prevention Primary CA prevention: removal of “at risk” tissue, chemo... prevention, vaccination (HPV) Secondary CA prevention: regular screening • Risk factors/warning signs (CAUTION mneumonic) C: change in bowel/bladder function A: a sore throat that does not heal U: unusual bleeding T: thickening lumps I: indigestion/difficulty swallowing O: obvious change in mole N: nagging cough/hoarseness • Treatment types, side effects/complications (& treatment/nursing care of side effects/complications) Surgery: can be prophylactic, diagnostic, curative, palliative SE/complications: removed organs and tissues lose function, removal of organs does not necessarily rid cancer Radiation: destroy cancer cells with minimal damaging effects of surrounding normal cells SE/complications: radiation dermatitis, altered taste/fatigue, atherosclerosis, coronary artery disease, fibrosis, scarring, bone marrow suppression Nursing care: provide accurate info, skin care (wash gently with soap and water, avoid scrubbing), do not remove temporary ink markings, provide nutritional support, care of xerostomia (administer saliva substitutes, lozenges, mouth rinses), reduce risk for bone fracture, encourage exercise and sleep interventions to treat fatigue Chemotherapy: treatment of cancer using antineoplastic drugs (cytotoxic systemic therapy) SE/complications: dosage and scheduling (dose-limiting side effects may impact), extravasation and vesicants, bone marrow suppression (neutropenia, anemia, thrombocytopenia), mucositis (inflammation of oral mucosa) alopecia (hair loss), chemo brain, chemo-induced peripheral neuropathy, fatigue Nursing care: epo-alfa/Epogen, blood products, no flossing, soft toothbrush, no razors, no NSAIDS, treat nausea (peppermint oil, Zofran, fluids, room temperature food, alcohol swabs) Immunotherapy: enhances and alters pt’s biological response to cancer cells via direct antitumor activity SE/complications: fluid shifts/inflammation, decreased LOC and other neuro changes, fever, chills, malaise Photodynamic therapy: selective destruction of cancer cells via chemical reaction triggered by last light which destroys or shrinks tumors Hormonal manipulation: changing usual hormone responses to slow tumor growth to certain cancer types SE/complications: masculinizing affects in women, feminizing effects in women (gynecomastia), fluid retention, acne, hypercalcemia, liver dysfunction, VTE Bone marrow transplants: transplant of bone marrow from a matched individual (self or other) SE/complications: nausea, vomiting, graft vs. host disease, infection, organ damage Complementary & Alternative Medicine (CAM) • Types of CAM (mind-body therapy, tai chi, chiropractic care, herbal meds, etc.), goals of use, and interactions Mind-body therapies: biofeedback, guided imagery, intercessory prayer, meditation, relaxation exercise Biologically-based therapies: herbal therapies (chamomile, garlic, gingko, ginseng, peppermint, st.john’s wart, vaerin) Manipulative and body-based therapies: acupuncture, acupressure, chiropractic, massage, rolfing, shiatsu, tai chi, yoga Energy therapies: reiki, therapeutic touch Alternative medical systems: homeopathy (tx of disease with minute drug doses to activate and illness that then stimulates the body’s normal defense system to eliminate disease; remedies without chemically active ingredients), naturopathy (the practice of assisting in the health of patients through the application of natural remedies), osteopathy (embracing the full spectrum of medicine, including the use of medications and surgery, in addition to manipulative techniques) MODULE 2: END-OF-LIFE CARE Chapter 10: Principles of Emergency and Disaster Preparedness • Palliative vs. Hospice care (goals of each, differientation) Palliative care: can be any stage of serious or chronic illness, care may be provided concurrently with curative therapies, care not limited by time periods, care provided by PCP with potential follow-up vistis Hospice care: prognosis of less than 6 months to live, initiated when curative tx stops, 60-90 day periods of care, care provided by RNs, social workers, chaplains, and volunteers • Ethical/legal considerations r/t dying (AD’s, living will, euthanasia, etc.) • Durable power of attorney for health care (DPOAHC): makes decisions about pt’s healthcare when MD determines pt does not have capacity to make decisions (pt does not receive info, pt does not evaluate, deliberate and mentally manipulate info, pt does not communicate a tx preference) Living will: discusses CPR or code status (must be initiated unless and DNR order exists, may be violent and painful), intubation/artificial ventilation, artificial nutrition/hydration “Five wishes”: identification of decision maker (DPOAHC), identification of treatments the pt does/does not want, comfort level expectations, how they want to be treated, what the pt wants loved ones to know Active euthanasia: use of medications or tx that purposefully causes pt’s death (physician assisted suicide) Passive euthanasia: discontinuation of one or more therapies that may prolong life Voluntary stopping of eating and drinking (VSED): refusal to eat or drink in order to hasten death by competent pt with terminal illness • S/Sx of end-of-life Lack of heartbeat, absence of spontaneous respirations, irreversible brain dysfunction Weakness, anorexia, changes in cardio function (cool, mottled cyanotic extremities, decreased BP, heart rate will increase-irregular-brady-asystole), dyspnea (cheyne- stokes), changes in GU (incontinence, decreased UO), changes in LOC (sleeping, restless, anxiety, lethargy) MODULE 3: TISSUE INTEGRITY Chapter 10: Principles of Emergency and Disaster Preparedness • Traditional triage vs. Mass Casualty triage Traditional triage: most critical pt’s are seen first(emergent/immediate threat to lfie, urgent/major injuries, nonurgent minor injuries) Mass casualty triage: emergent (red tag) pt’s seen first, urgent (yellow tag), nonurgent (green tag), expectant or allowed to die (black tag) • Internal vs. External events Internal events: power outage, active shooter, explosion External: tornado, volcano, hurricane, wild fires, epidemics Chapter 26: Care of the Patient with Burns • Classifications of burn injury (superficial, partial-thickness, etc.) Superficial-thickness burns (1st degree): least damage; epidermis is only part of skin injured (sun burn, flash exposures) Partial-thickness burns (2nd degree): Superficial partial-thickness: injury to upper third of dermis, pink moist blanchable, blister formation, heals within 10-21 days without scarring Deep partial-thickness: extend deep into the dermis, red dry with slow blanching, no blisters, edema, heal within 2-6 weeks with scarring Full-thickness burns (3rd degree): destruction of entire epidermis and dermis, skin does not regrow, characterized by; eschar, edema, waxy-white, deep-red, yellow, brown, or black appearance, may have no blood supply, reduced/absent sensation, healing takes weeks to months • Rule of 9’s • Phases of burn injury (time periods, priority assessments, etc.) Resuscitative/emergent phase: 24 to 48 hours Goals: secure airway, support circulation (fluids), pain relief, prevent infection, maintain body temp, provide emotional support Assessment: direct airway injury (hoarseness, brassy cough, drool, tachypnea, wheezes, stridor), smoke poisoning, pulmonary edema (SOB, crackles), CO poisoning (cherry-red coloring, headache, nausea, drowsiness, irritiable), thermal airway injury (ulcerations, redness, edema), hypovolemia, decreased CO, decreased BP with increased HR, EKG changes with direct heart damage, fluid shifts, decreased UO, concentrated urine Diagnostics: increased Hgb, Hct, increased BUN, glucose, potassium, decreased sodium, protein and albumin Interventions: maintain airway, fluid resuscitation, manage pain, preventresp distress Acute phase: 36-48 hours Debridement, dressings (biologic, biosynthetic, synthetic), surgical wound management (grafting), minimizing weight loss, support self-esteem Rehabilitative phase: years to lifetime Wound closure, emphasis on; prevention of scars, psychosocial adjustment, resuming pre-burn activity • Immediate burn care (Education for patients) Remove cause of burn, check of breathing, administer CPR if needed, lukewarm water to cool skin around burn unless wound is open, remove any loose debris, remove jewelry, cover burned area with clean dry cotton, raise burned area above level of heart • Parkland formula 2-4mL/kg/%BSA burned (over 1st 24 hours), half of total volume over 1st 8 hours, half over next 16 hours MODULE 4: GAS EXCHANGE Chapter 8: Principles of Emergency and Trauma Nursing • Triage (Definition, How does it work?, Where is it used? Etc.) Triage: an organized system for sorting and classifying pt’s into priority levels, depending on illness or injury severity o Pts with highest acuity need the quickest eval and tx, ED nurses act as the gatekeeper, three-tiered system, disposition of pt’s in the ED o 3 options: admit to hospital, transfer to specialty care center, discharge home Chapter 32: Care of Critically Ill Patients with Respiratory Problems • S/Sx of respiratory distress* Dyspnea, orthopnea, increased RR, decreased SpO2, restlessness, irritability, confusion, increased HR, decreased LOC, headache, weak peripheral pulses • Who is at risk for impaired gas exchange? Pt’s with pulmonary embolism (PE), venous thromboembolism (VTE), acute respiratory failure (ARF), acute respiratory distress syndrome (ARDS), chest trauma • Chest Trauma (pneumothorax, rib fractures, etc.) types & treatment measures Pulmonary contusion: common chest injury caused by rapid deceleration during MVA, may lead to ARDS, asymptomatic at first s/sx: bloody sputum, decreased breath sounds, crackles or wheezes, dullness on percussion tx: may resolve on own, good lung down positioning, maintain oxygenation Rib fractures: often from blunt trauma, risk for deep chest injury, pt often splints chest with breathing tx: maintain adequate gas exchange, splint rib cage when breathing/coughing, analgesics, fractured ribs reunite spontaneously Flail chest: results from fractures of two or more ribs in two or more places causes paradoxical chest wall movement s/sx: chest goes in during inspiration and out during expiration, dyspnea, cyanosis, increased HR, decreased BP tx: intubation with positive-pressure ventilation, analgesics Pneumothorax: air in pleural space (open=exposed to air, closed= spontaneous) s/sx: reduced or absent breath sounds on affected side, hyperresonant percussion, tracheal deviation to unaffected side types: traumatic (r/t trauma), spontaneous (not from trauma) tx: provide oxygen, relieve pain/anxiety, correct acid-base imbalance, minimize further damage, remove air (needle thoracostomy) Hemothorax: bleeding into the pleural space (simple is less than 1000mL, massive is greater than 1000mL) s/sx: reduced or absent breath sounds on affected side, dull percussion • Mechanical Ventilation (settings, complications, etc.) Support pt until lung function is adequate/episode has passed to improve gas exchange and decrease WOB Controls: o Tidal volume (Vt): volume of air the pt receives with each breath (6-8mL/kg) o Rate (f): ventilator breaths delivered per minute o Positive end-expiratory pressure (PEEP): positive pressure exerted during expiration (prevents atelectasis, usually 5-15cm H2O) o FiO2: oxygen level delivered to pt, ranging between 21-100% o Peak inspiratory pressure (PIP): pressure used by ventilator to deliver a set tidal volume at a given lung compliance, highest pressure reached during inspiration • ETT vs. Tracheostomy (purposes, differentiation, etc.) ETT: intubation with a long PVC tube that is passed through the mouth and into the trachea, most often required for pt’s with hypoxemia and progressive alveolar hypoventilation with resp acidosis, utilized for 10-14 days max, performed by CRNA or RT Tracheostomy: intubation with PVC tube that is surgically placed into the trachea, utilized when pt cannot wean from ETT after 10-14 days to improve comfort and decreased risk for pneumonia MODULE 5: PERFUSION Chapter 33: Cardiac Function and Hemodynamics • Hemodynamic measures (CO, SV, CVP, MAP) Blood pressure (BP): pressure contained within the walls of the arteries Mean arterial pressure (MAP): average pressure contained within the arterial system SBP + 2(DBP) / 3 = MAP Cardiac output (CO): HR x SV = CO Stroke volume: mL of bleed ejected with each heartbeat, affected by contractility, preload and afterload, normal is 60-100 mL • Preload, afterload, & contractility (What affects these? How do we fix alterations?) Preload: the degree of the end-diastolic stretch of myocardial muscle fibers, volume of blood in ventricles just prior to systole, comparable to pt’s fluid volume status, measure central venous pressure (CVP, normal CVP = 3-8 mmHg) Contractility: inotropic state of the muscle, measured by ejection fraction 55-70% (normal) Afterload: resistance left ventricle must overcome to circulate blood, increased in hypertension and vasoconstriction (increased afterload = increased cardiac workload), determined by BP, SVR = 80 x (MAP - CVP) / CO • Vasopressors vs. Vasodilators Vasopressors: epinephrine, norepinephrine (Levophed), phenylephrine (Neo- synephrine), dobutamine, dopamine, vasopressin Epinephrine activates a1, a2, b1, b2 Norepinephrine activates a1, a2, b1 Phenylephrine activates a1 Dopamine activates dopaminergic, b1 Dobutamine activates b1 Vasopressin activates ADH Vasodilators: nitroglycerin, clevidipine/cleviprex Chapter 34: Care of Patients with Dysrhythmias • Cardiac Electrical Anatomy (What are the areas involved? What do they look like on EKG?) SV node: the pacemaker, 60-100 bpm = P wave AV junction: consisted of transitional cell zone, AV ndoe, and bundle of his, lies below right atrium endocardium (AV node is the area in which impulses are slowed or delated before moving to ventricles) = PR segment Purkinje cells: responsible for rapid conduction of electrical impulses through ventricles, which leads to ventricular muscle contraction = QRS complex • Parts of a rhythm (P, QRS, T, U, PR segment, QT interval, etc.) • Rhythms/Dysrhythmias (NSR, SA, ST, SB, SVT, PVC’s, AV-blocks, VT, VF, Paced rhythm, PEA, etc.) o Be able to differentiate between o Nursing interventions and treatment (medications, skills, etc.) NORMAL SINUS RHYTHM (NSR) SINUS ARRHYTHMIA (SA): changes in intrathoracic pressure with breathing, digitalis, morphine causes: exercise/anxiety, pain, fever, anemia, hypoxemia, hyperthyroidism, epinephrine, atropine, caffeine, alcohol, nicotine, cocaine tx: rest, avoid causative substance, stress management SINUS BRADYCARDIA (SB): causes: vagal simulation (bearing down, vomiting, suctioning), pain, hypoxia, inferior MI, beta blockers, calcium channel blockers, digitalis, athleticism, hypothyroidism tx: 0.5mg atropine, IVF administration, apply oxygen, remove causative agent, pacemakers SUPRAVENTRICULAR TACHYCARDIA (SVT): causes: stress, heart failure, hyperthyroidism, caffeine, pregnancy, surgery tx: none needed if stops on it’s own, vagal maneuvers (cough, bear down, carotid massage (MDs only)), adenosine (6 then 12 mg IVP), beta blockers, ca-channel blockers, cardioversion, radiofrequency catheter ablation ATRIAL FIBRILLATION (AF OR A-fib) ATRIAL FLUTTER causes of a-fib and flutter: heart failure, hypertension, coronary artery disease, heart valve disease, diabetes, obesity, elderly tx: cardioversion, left atrial appendage closure with watchman device, radiofrequency catheter ablation, MAZE procedure AV BLOCKS PREMATURE VENTRICULAR COMPLEX (PVC): s/sx: often asymptomatic, palpitations, chest discomfort, diminished or absent peripheral pulses tx: none unless symptomatic, electrolyte replacement VENTRICULAR TACHYCARDIA (VT): causes: MI, cardiomyopathy, electrolyte disturbance, heart failure, drug toxicity, cocaine/illicit drugs, torsades des pointes (usually caused by hypomagnesemia) tx: amiodarone drip (if pt has a pulse), CPR, cardioversion, 1mg epinephrine, 300 mg then 150 mg of amiodarone VENTRICULAR FIBRILLATION (VF): causes: MI, hypokalemia, hypomagnesemia, hemorrhage, rapid SVT, shock tx: CPR, cardioversion, 1mg epinephrine, 300 mg then 150 mg amiodarone,defibrillation VENTRICULAR ASYSTOLE (ASYSTOLE) causes: myocardial hypoxia (usually after VT or VF) PULSELESS ELECTRICAL ACTIVITY (PEA) tx: CPR, cardioversion, 1mg epinephrine, 300 mg then 150 mg amiodarone until pulse and BP restored • Defibrillation vs. Cardioversion& CPR basics Defibrillation: asynchronous countershock that depolarizes critical mass of myocardium simultaneously to stop re-entry circuit and allow sinus node to regain control of the heart, resets cardiac electrical activity, DO NOT touch pt, defib patches should not be placed over monitoring electrodes or implanted pacemaker Cardioversion: same therapy technique as defibrillation, except it is done under a controlled, planned environment MODULE 6 – LEADERSHIP AND PERFUSION Chapter 37: Care of Patients with Shock • What is the primary problem in shock? Lack of oxygen due to hypoperfusion • Stages of Shock: Initial, Nonprogressive/Compensatory, Progressive, & Refractory/MODS Initial: HR and RR increase, s/sx subclinical, anerobic metabolism begins, MAP decreased by 10mmHg Non-progressive/compensatory: increased HR and RR, decreased BP and O2, anerobic metabolism progresses to acidosis, hypoxia to non-vital organs (body attempts to maintain homeostasis), MAP decreased 10-15mmHg Progressive: impending doom, rapid weak pulses, decreased BP, cyanosis, anuria, increased lactic acid (normal 0.5-1), increased potassium, acidosis (decreased pH), hypoxia to vital organs, MAP decreased 20+mmHg from baseline Refractory: irreversible, rapid LOC, nonpalpable pulses, slow shallow RR, unable to measure O2, MODS, organ failure • Signs of organ failure Significant decrease in neurologic function, decreased urine output (less than 30mL/hr), nausea, increased HR with decreased BP, shortness of breath • Types of Shock: Hypovolemic, Cardiogenic, Obstructive, Distributive (anaphylactic, septic, & neurogenic) o Causes (volume, pump, vasculature?) o Etiology (what disease processes cause?) o S/Sx specific to shock type o Treatment/Reversal (meds, procedures, nursing care) Hypovolemic * Decreased blood volume in circulation * Hemorrhage, dehydration, chemo, diabetes insipidis * > HR, < MAP, weak/nonpalpablepulsea, < O2, > RR, < urine output * Cool, moist skin, pallor, < LOC, < DTR * Replace lost fluid( IVF, blood products, colloids) * Monitor labs, bedrest, vasopressor (last resort) Cardiogenic * Impaired pumping of the heart * Heart attack, cardiac arrest, heart failure, ventricular dysrhythmias * < cardiac output, > HR, Thread pulse, < BP, Narrow pulse pressure, Orthostatic hypotension, Slow cap refill, Diminished peripheral pulse, Flat neck/hand veins * Dopamine, dobutamine, intra-aortic balloon pump, impella, EMCO * Complication: myocardial infacrtion, heart failure Distributive * Anaphylaxis * Allergic/ hypersensitivity reaction * Widespread loss of blood vessel tone, <BP, < cardiac output * Epinephrine, corticosteroids, beta-agonist(albuterol), Benadryl * Septic * Widespread infection, whole body inflammation * Gram-negative(E.coli, pseudomonas), gram-positive( staph, strep), central line infections(CLABSI) * > HR, vasodilation, capillary leak, >RR, < O2, < urine output, > lactic acid * Early: skin warm, pink, late: mottled, pale, cyanotic * Obtain blood cultures, administer O2, administer IVF/blood products * Abx, corticosteroids, insulin, heparin(DIC), vasopressor( maintain MAP >65 * Complication: systemic inflammatory response syndrome( SIRS), disseminated intravascular coagulation(DIC) * Neurogenic ineffective sympathetic activity (decreases vascular smooth muscle) spinal cord injury (T5 or higher), spinal anesthesia widespread vasodilation Anxiety, Restlessness, Lethargy, Coma, Generalized weakness, Sluggish pupil response, Diminished/absent DTR < BP, <HR – only time you see bradycardia in shock IV fluids, Vasopressor therapy, Supportive care Obstructive * Problems that impair the ability of the heart to pump effectively, heart muscle is normal Cardiac tamponade, pulmonary embolism, pericarditis, tension pneumo, thoracis tumors * Decreased LOC, Confusion, Chest pain, Lightheadedness, >HR, Faint pulse, SOB, Fast shallow breathing, Sweating, <urine output, Clammy skin, Pallor, Cold extremities * Relieve obstruction Pericardiocentesis, thrombectomy, chest tube placement, thoracostomy * Vasopressor, IVF to correct hypotension Leadership: • Delegation to UAP/NA, LPN, and other RN’s Delegation: process of a nursing task or activity to the appropriate, qualified person Supervision: guidance or direction, evaluation, and follow-up to ensure activities have been performed appropriately First step in delegation process is always to evaluate the scope of practice of the person you are delegating to MODULE 7 – CV& COAGULATION INTEGRITY Chapter 38: Care of Patients with Acute Coronary Syndrome • Types of ACS (S/Sx, EKG changes, nursing care, cardiac enzymes, etc.) • Risk factors for ACS & CAD* • Diagnostic tests/procedures • Nitroglycerin (How does it work? Administration & side effects) MODULE 8 – RENAL AND ENDOCRINE Chapter 62: Care of Patients with Pituitary and Adrenal Gland Problems • Pituitary abnormalities (Hypo-/Hyper-pituitism, Cushing’s, DI, SIADH, Adrenal hypo/hyperfunction, pheochromocytoma, etc.) o Diagnosis o S/Sx o Nursing care & Treatment o Hypopituitarism ▪ Diagnosis: • Labs: < thyroid hormones, < PRL • Imaging: Bone Changes (enlargement, erosion, calcifications) ▪ S/Sx: • Loss of secondary sex characterissitcs o Men: facial/body hair loss, < libido o Women: amenorrhea, dyspareunia (painful iintercourse), infertility, decreased libido o Neurologic symptoms: decreased peripheral vision, HA, diplopia, limited eye movement ▪ Nursing Care/Treatment • Hormone replacement • HTN management and blood thinners o w/ estrogen o Hyperpituitarism ▪ Diagnosis • MRI • X-Ray ▪ S/Sx • Chnages in hat, glove, ring size, Backache/joint pain (from bone changes), HA, Vision changes **COMMON**, Decreased libido ▪ Nursing Care/ Treatment • Surgery: Hypophysectomy • Radiation o No immediate effects • Pharmacologic: o Dopamine agonists (parlodel/bromocriptine & Dostinex/cahergoline) o Somatostatin analogs (acteotide/Sandostatin, Somavet/Pegvisomant) o Cushings ▪ Diagnosis • excessive glucocorticoid therapy • pituitary adenoma ▪ S/Sx o DI • Weight gain, Increased appetite, Fatigue, Easy bruising, Osteoporosis, Frequent infections, <Lymphocytes, “Buffalo hump”, Truncal Obesity, “Moon face”, Striae, Acne, increased body hair, Male-pattern balding, Oligomenorrhea (scant or infrequent menses), Edema s/t >Na+/H2O retention, <Muscle mass/weakness, Hyperglycemia, Mood swings, irritability, or confusion, >Blood, urine, & salivary cortisol, >Na+, <Ca+ ▪ Nursing Care/Treatment • Restoring fluid volume balance o Assess for S/Sx of fluid overload o Drugs that <cortisol (Elipten, Metopirone, Signifor) o Water restrictions o 2-4g Na+ restriction o Accurate I/O’s o Daily weights o Tumor removal (adrenal or pituitary) • Surgery: o Adrenalectomy o Hypophysectomy • Preventing injury o Prevent skin breakdown o Lotion o Avoid adhesives o Prevention of falls o Monitor for bleeding o Frequent BG checks • Monitor for S/Sx of infection o infection prevention! • Wean glucocorticoids appropriately! ▪ Diagnosis: • >Plasma Osmolarity • >Na+ • Classifications: o Neurogenic ▪ Primary or secondary o Nephrogenic ▪ Drug-related ▪ S/Sx • Polyuria • Excessive thirst • Symptoms of dehydration • Dilute urine o Low urine specific gravity (<1.005) o Low urine osmolarity & osmolality (50-200 mOsm/kg or L) ▪ Treatment/Nursing Care • Pharmacologic: o Desmopressin (DDAVP)—symthetic vasopressin o IVF replacement • Non-pharmacologic: o Accurate I/O’s o Daily weights o SIADH ▪ Etiology • Cancer • Pulmonary infection • SSRI’s • Trauma • Tumors ▪ S/Sx • Water Retentions , Fluid shifts, Lethargy, HA, Disorientation/Changes in LOC, Hypothermia ▪ Nursing Care/Treatment • Fluid restrictions o 500-1000 mL/day o Saline flushes per GT o Accurate I/O’s o Daily weights • Monitor for S/Sx of Hyponatremia o Neuro changes o Seizures o Muscle twitching and irritability o Coma • Pharmacologic: o Vasopressin-receptor agonists (Vaptans) o Diuretics o Hypertonic saline (3% sodium chloride) o Adrenal Gland Hypofunction ▪ Etiology • Insufficiency of aldosterone, androgen, & cortisol • Acute adrenal insufficiency (Addisonian Crisis): life-threatening event in which the need for cortisol and aldosterone is greater than body’s supply o Usually s/t stressful events, autoimmune conditions, adrenalectomy, pituitary tumors, cessation of long-term steroid therapy ▪ S/Sx • Fatigue, Muscle Weakness, Salt craving, n/v, Hypoglycemia, Fluid depletion, Hyperkalemia, Hyponatremia, Lethargy depressed confused psychotic ▪ Laboratory Tests: • < Cortisol • < Blood glucose • <Na+ • >K+ • >BUN ▪ Nursing Care/ Treatment • Restoring fluid volume balance o Assess for S/Sx of fluid overload o Drugs that <cortisol (Elipten, Metopirone, Signifor) o Water restrictions o 2-4g Na+ restriction o Accurate I/O’s o Daily weights o Tumor removal (adrenal or pituitary) • Surgery: o Adrenalectomy o Hypophysectomy • Preventing injury o Prevent skin breakdown o Lotion • Avoid adhesives • Prevention of falls • Monitor for bleeding • Frequent BG checks o Monitor for S/Sx of infection o Infection prevention! • Wean glucocorticoids appropriately! o Hyperaldosteronism ▪ Etiology • Excessive aldosterone secretion s/t adenoma (Primary) • Excessive aldosterone secretion s/t kidney injury (Secondary) • Results in fluid and electrolyte imbalance ▪ S/Sx • >BP, HA, Fatigue, Muscle Weakness, Dehydration, Polydipsia, Polyuria, Paresthesias, <K+, >Na+, Metabolic alkalosis, Low spec grav ▪ Nursing Care/ Treatment • Surgery: o Adrenalectomy • K+ replacements • K+-sparing diuretics o Spironolactone (Aldactome) • Glucocorticoids o Pheochromocytoma ▪ Etiology • Usually benign, bilateral or unilateral • Produce, store, & release epinephrine & norepinephrine • Common among ages 30-50 with rare inherited disorders o Neurofibromatosis, multiple endocrine neoplasia, von Hippel- Lindau disease ▪ S/Sx • HTN!!, Tachycardia, Severe headaches, Palpitations, Diaphoresis, Flushing, Pallor, Pain, Apprehension, Sense of impending doom, Chest or abdominal pain, Heat intolerance, Weight loss, Tremors, Elevated catecholamine levels ▪ 5 P’s • Pain, pallor, pressure, palpitations, perspiration Chapter 63: Care of Patients with Problems of the Thyroid • Hypo- vs. Hyper-thyroidism (diagnosis, S/Sx, nursing care/treatment) o `Hypothyroidism ▪ Diagnosis: • <T3, T4 • </> TSH ▪ S/Sx • < Metabolism! ▪ Nursing Care/ Treatment • Maintain adequate VS • Warm blankets • Prevent Complications • Medication o Levothyroxine Sodium (synthroid0 o Hyperthyroidism ▪ Diagnosis: • Elevated T3, T4, or TSH (Thyroid-stimulating hormone) • Thyroid scan ▪ S/Sx • >Metabolism ▪ Nursing care/Treatment • VS assessments q4h • Encourage rest • Frequent, high calorie meals • Reduce room temperature • Pharmacologic o Thionamides (methomaole/Tapaxole) o Propylthiouracil (PTU) ▪ >Infection risk • Radioactive Iodine (RAI) Therapy • Surgery: o Thyroidectomy Chapter 68: Care of Patients with AKI & CKD • ARF/AKI vs. CKD o Pathophysiology & Etiology o S/Sx o Nursing Care (diet/fluid restrictions!, what to watch for, etc.) o Treatment (medications, HD, CRRT, PD o Prevention of AKI/CKD • Acute kidney failure/injury – rapid reduction of kidney function – may result in chronic kidney disease o Prerenal ▪ Hypotension, heart attack, burns, dehydration, renal artery stenosis o Intrarenal ▪ Trauma, pyelonephritis, glomerulonephritis, ischemia to renal tissue, chronic NSAID use o Postrenal ▪ Bladder cancer, colon cancer, prostate cancer, nephrolithiasis( kidney stones) o Diagnosis: ▪ Increased creatinine by 0.3 in 48 hours ▪ 1.5x baseline creatinine in 7 days ▪ Urine output <0.5ml/kg/hr x 6 hours o s/sx ▪ oliguriaanuria, azotemia, fluid overload, <BP, < O2, > creatinine, > BUN, < GFR o treatment: ▪ maintain MAP > 80( >65), diuretics, IVF bolus, fluid restrictions, hyperkalemia( kayexalate, insulin&dextrose challenge) ▪ low protein (converts to ureaurea processed by kidneys), ▪ < K, phosphorus and Na ▪ dialysis (continuous, intermittent) • chronic kidney disease – abnormalities in kidney structure or function present for > 3 months – progressive – irreversible o increased creatinine and urea o < K ( applesauce is a good snack), < phosphorus, < Na o Care of access device, fall prevention, bleeding prevention, decrease medication dosages • Hemodialysis vs Peritoneal o HD – requires long-term access( AV grafts, fistulas, AV shunts) o PD – exchanges waste, fluid, and elytes in the peritoneal cavity • things to avoid in AKI/CKD o NSAIDS, vancomycin, gentamycin, contrast dye MODULE 9: INTRACRANIAL REGULATION AND SENSORY PERCEPTION Chapter 45: Care of Critically Ill Patients with Neurologic Problems Stroke o Risk factors-Family History, High BP, tobacco, obesity, not working out, DM, Booze, drug use, high fat diet, atherosclerosis o Diagnostic tests- CT (best), MRI w/ contrast, Ultrasound o S/Sx o Treatment ▪ tepa, (Clot buster) -given within 3.5-4.5 ▪ Contraindications-hemmoragaic stroke, stroke over 4.5 hours ago, active bleeding, recent surgery, s/Sx improving, head trauma, known tumor, high BP (over 185/110), low platelets, on blood thinners, over 80, recent MI, or post op o Stroke prevention measures -good diet, working out, blood thinners, stop smoking, stop drinking, statins, TBI o S/Sx- low BP, Hypoxemia, <LOC, Pupillary changes, Cheyne-Stokes respirations or apnea, Cushing’s triad: (Severe HTN, widened pulse pressure, Bradycardia), Vision loss, HA, seizures, emotional changes, forgetting, suspicious CSF, lower GCS o TX- Maintain ABC’s, VS q 1-2h (at least!), Normal RR, Temperature management, administer oxygen (PRN) to keep PaO2 80-100, Strict I/O’s, Mannitol, Lasix, Analgesics (esp. Opioids) o Teaching- PT/OT, Safety in home, Healthy diet, Refrain from illicit drug & EtOH use, Seizure prevention, reinforce positive behaviors, return to safe job when medically cleared Types of Brain Bleeds • Epidural Hematoma: Bleed into the space between dura mater and inner skull o Commonly caused by fracture • Subdural Hematoma (SDH): Bleed into space between dura mater and arachnoid space o Slow bleed that may not show symptoms for days to weeks after injury • Intracerebral hemorrhage (ICH): Accumulation of blood within the brain tissue o Caused by blows to head, fractures, or brainstem injuries Brain Tumors: • Primary – originate within CNS • Secondary – result from metastasis ▪ S/SX- ▪ Cerebral: HA, Seizure*, N/v, Changes in visual acuity*, Hemiparesis or hemiplegia*, Aphasia*, Personality Changes ▪ Brainstem: Hearing loss, Facial pain, weakness, Dysphagia, Nystagmus, Hoarseness, Ataxia or dysarthria*, Loss of balance, Apnea*, <HR, <BP • Increased intracranial pressure (ICP) o S/Sx -CONFUSION, changes in LOC, agitation, pupil changes, posturing, decreased motor function, HA, seizures, high BP, slurred speech, and vomiting o Treatment-elevate HOB, calm environment, avoid coughing/straining/sneezing, stool softeners, prevent hypoxia, no neck flexion, NIHSS q 15min to 4 hours MODULE 10: METABOLISM & MOBILITY Chapter 51: Care of Patients with MSK Trauma • Fractures o Common causes o Types o S/Sx o Diagnosis o Treatment (medications, casts, splints, traction) ▪ Types of traction ▪ Difference between casting/splinting ▪ Complications of treatment (esp. casting!) o Complications (compartment syndrome, rhabdomyolysis, VTE/PE*, fat embolism*, etc.) ▪ Definitions ▪ S/Sx ▪ Treatment • Other MSK problems (carpal tunnel, rotator cuff injuries, amputations) o Causes/etiology o S/Sx o Treatment& nursing care* Module 10: Metabolism & Mobility Chapter 51: Care of Patients with MSK Trauma • Fractures o Common causes o Fragility Fracture: Occurs with minimal trauma to a bone weakened by disease ▪ AKA Pathologic or Spontaneous fracture (osteoporosis) o Fatigue (Stress) Fracture: Results from excessive strain and stress on the bone (athletic/shin splints) o Compression Fracture: Loading force applied to long axis of cancellous bone (vertebral) o Types o Complete: Break across entire width of bone ▪ Displaced—bone alignment is disrupted/altered o Incomplete: Partial break (doesn’t divide bone in two portions) o Open/Compound: Skin surface is disrupted, resulting in external wound o Closed/Simple: Does not extent through skin; no visible wound o S/Sx o Severe pain, Changes in bone alignment. Ecchymosis, Subcutaneous emphysema (rib fx) o Diagnosis o Laboratory Assessment: ▪ Hgb/Hct ▪ ESR ▪ WBC ▪ Ca++ & Phos ▪ CK & myoglobin o Imaging: ▪ X-ray, CT, or MRI o Treatment (medications, casts, splints, traction) ▪ Treatment and Nursing Care • Maintain ABC’s! • Cut away clothing and remove jewelry • Achieve hemostasis (PRN) • Manage Pain o Opioids, Nonopioids (NSAID’s, Tylenol), & muscle relaxants • Apply splint and immobilize • Bone reduction (surgical vs non-surgical) • PT/OT • Active & passive ROM • Use of walkers, canes, or crutches • Traction • Surgery (ORIF) ▪ Types of traction Traction: Application of a pulling force to a part of the body to provide reduction, alignment, and rest • Classifications: o Running traction: pulling force is in one direction (pt’s body acts as countertraction o Balanced suspension: provides countertraction on its own so the pulling force is not altered by pt or bed movement • Types of Traction (Table 51-1) o Skin Traction (running) “Buck’s Traction” ▪ Involves use of a Velcro boot, belt, or halter secured around the affected leg • Connected to 5-10 lb weight as pulling force ▪ Decreases painful muscle spasms accompanying hip/femur fractures o Skeletal Traction (Balanced suspension) ▪ Involves use of surgically inserted screws • Allows use for longer time and heavier weights (15-30 lbs) ▪ Aids in bone realignment, but decreases mobility • Nursing Care o Skin checks (@ pin sites) q 1-4h ▪ Pin sites must be kept clean & dry o Check proper function q 8-12h o Check weight per MD order o Assess neurovascular status of affected extremity o Assess peripheral perfusion ▪ Difference between casting/splinting ▪ Complications of treatment (esp. casting!) o Complications (compartment syndrome, rhabdomyolysis, VTE/PE*, fat embolism*, etc.) ▪ Definitions ▪ S/Sx ▪ Treatment Compartment Syndrome: Serious, life-threatening condition in which increased pressure within one or more compartments reduces circulation to the area • Compartments: Areas in body in which muscles, blood vessels, and nerves are contained within fascia (inelastic tissue surrounding muscles, blood vessels, & nerves) • Usually s/t casting or other restrictive measures • Pain continues despite receipt of pain medication • Most commonly affected areas: o Lower leg (tibial fractures) o Forearm (ulnar or radial fractures) • 6 Hallmark S/Sx of Compartment Syndrome o Pain (Despite pain medication administration) o Paralysis o Paresthesia o Pressure ▪ Significant edema/swelling o Pulselessness o Pallor • Pathophysiology of Compartment Syndrome • Treatment of Compartment Syndrome o Keep limb at or below level of heart o IVF administration o Analgesics o Fasciotomy Fat Embolism Syndrome (FES): Syndrome in which fat globules are released from yellow bone marrow (long bones) into bloodstream • 12-48h after injury • Fat globules clog small blood vessels and impair perfusion • Highest risk: Hip fracture – and femur fractures • Most common clot site: Lungs (PE!) o S/Sx of PE – feeling of impending doom, SOB, pain with breathing, cyanosis… o Petechiae to chest o Neuro symptoms: Confusion Seizures Bone Infection: Osteomyelitis: Most common with open fractures s/t loss of skin integrity Rhabdomyolysis: Buildup of protein (myoglobin) in blood secondary to traumatic injury, muscle hypoperfusion, strenuous exercise… Common cause of intrarenal AKI. S/S: Anorexia, Weakness, N/v, Oliguria, >HR, <BP, >RR, Myalgias & muscle cramps, Edema, Fatigue, HA Dark, reddish-brown urine, Crackles Treatment: Closely monitor VS, labs Pharmacologic: IVF resuscitation Sodium bicarbonate Mannitol Dialysis Amputations: Removal of a part of the body • Considered only after other interventions have been unsuccessful at maintaining circulation o Traumatic vs. Elective • Causes/Risk factors: o PVD o Cancer o Ateriosclerosis o Complex injuries o DM • Complications of Amputation o Hemorrhage o Infection/Osteomyelitis o Phantom limb pain: Painful sensation felt in amputated part ▪ Burning, curshing, cramping pain o Neuroma: Sensitive tumor consisting of damaged nerve cells o Flexion contractures • Nursing Care & Treatment o Monitor for decreased tissue perfusion o Manage pain ▪ PLP: IV calcitonin, beta-blockers (-olols), antiepileptics (Neurontin, Lyrica), or antispasmodics (baclofen) • Admin meds prior to stump cares! o Promote mobility ▪ PT/OT ▪ ROM ▪ Contracture prevention • Pronation 10-20 mins/day ▪ Leg prosthesis o Provide stump cares: ▪ Per MD order ▪ Wash with soap/water daily and allow to dry fully ▪ Elevate to prevent swelling o Monitor for and prevent infection o Promote self-esteem o Do not massage stump! Carpal Tunnel Syndrome: Common condition in which the median nerve in the wrist becomes compressed s/t swelling, causing pain and numbness • Common causes: o Repetitive stress injury (RSI) ▪ Factory workers, computer operators, jackhammer operators ▪ Athletes (golf, tennis) • Treatment: o NSAIDs o Splinting o Corticosteroid injections weekly-monthly o Surgery: ▪ Endoscopic Carpal Tunnel Release (ECTR) ▪ Open Carpal Tunnel Release (OCTR) Rotator Cuf f Injury • Purpose of Rotator Cuff: Stabilizes the head of the humerus in the glenoid cavity during shoulder abduction o Results in pain, especially with abduction and overhead activities • Common causes: o Falls o Throwing a ball (baseball, basketball) o Heavy lifting o Aging o Repetitive motions • Treatment: o NSAID’s o Steroid injections o PT o Activity limitations o Arthroscopic repair Chapter 59: Care of Patients With Problems of the Biliary System and Pancreas Chapter 59: Care of Patients With Problems of the Biliary System and Pancreas • Problems of biliary system & pancreas (Cholecystitis, acute v. chronic pancreatitis, pancreatic CA, etc.) o Causes/etiology o Diagnostic tests o S/Sx o Treatment o Complications o Prevention Cholecystitis: Inflammation of the gall bladder • Acute vs. Chronic • Etiology: o Familial history o Older age o Female o Race American-Indian and Mexican-American o Excessive cholesterol intake o Sedentary lifestyle o Obesity o DM (Type II) o Dyslipidemia o Insulin resistance o Pregnancy o Hormone replacement therapy • Signs & Symptoms o Flatulence, dyspepsia, or belching after fatty food intake o Anorexia, n/v o RUQ abdominal pain Mild/achy to constant “gallbladder attacks” o Biliary colic o Sausage-shaped mass in RUQ (deep palpation by PCP) o Jaundice & icterus o Clay-colored stools o Dark urineSteatorrhea o Low-grade fever o Tachycardia • Diagnosis: o >WBC o >liver enzymes o >Bilirubin o Gallbladder edema on US o Gallstones on X-ray (Ca++) o HIDA scan o ERCP • Nursing Care/Treatment: o High fiber, low fat diet o Limit gas-producing foods o Small, frequent meals o Manage pain Opioids Toradol (ketorolac) Antiemetics (Zofran) Lithotripsy- waves to break up the stones o Cholecystectomy (lap vs. open) Acute Pancreatitis: Serious, life-threatening inflammation of the pancreas resulting in autodigestion and fibrosis of the pancreas o Digestive enzymes activate in the pancreas • Etiology: Trauma, obstruction, EtOH, tobacco use, gallstones • Signs & Symptoms: common around holidays when not eating properly and drinking o Severe mid-epigastric or LUQ abdominal pain Sudden onset Radiates to back, L) flank, or L) shoulder Worsens when supine or fetal position o n/v, anorexia, weight loss o Jaundice o Gray-blue discoloration of the abdomen, periumbilicus, or flanks o Absent or diminished bowel sounds o Palpable mass o Fever o Tachycardia, hypotension o Lung problems Adventitious lung sounds Dyspnea or orthopnea • Laboratory Assessment: o Elevated pancreatic enzymes (amyplase, lipase, protease/trypsin, & elastase) o >BG o <Ca++ o <Mg++ o >bilirubin o >liver enzymes o >WBCs o <Plts • Imaging: o Abdominal US o CT w/ contrast o Abdominal X-ray o ERCP • Treatment & Nursing Care o Manage Pain NPO w/ isotonic IVF x 24-48h since they cant digest anything Electrolyte replacements Gastric decompression via NGT Opioids (morphine, fentanyl, or dilaudid) • IV vs. PO vs. PCA Zantac or Prilosec Side-lying or fetal position Surgical: ERCP, chole o Oxygen therapy (prn) o Antiemetics prn o Diet: Small, frequent, bland meals, Moderate to High carb, high protein, low fat o Avoid EtOH & tobacco • Complications of Acute Pancreatitis o Pleural effusions, atelectasis, or pneumonia ARDS risk! o MODS o Coagulation defects (DIC) o Shock s/t vasodilation & hypovolemia o Paralytic ileus o DM, pancreatic infection and acute kidney injury Chronic Pancreatitis: Progressive, destructive disease of the pancreas characterized by remissions and flare-ups in which fibrosis and inflammation coexist • Categories: o Chronic calcifying pancreatitis (CCP): most common type, caused by EtOH- ism Men > women o Chronic obstructive pancreatitis: develops s/t inflammation, spasm, & obstruction (cholelithiasis) o Autoimmune pancreatitis: Immunoglobulins invade the pancreas, causing inflammation o Idiopathic/Hereditary Chronic Pancreatitis: Gene mutations result in pancreatitis • Signs & Symptoms o Intense abdominal pain, Often continuous, burning, or gnawing o Abdominal tenderness, Ascites, LUQ mass, Pseudocyst or abscess, Respiratory compromise, Steatorrhea or clay-colored stools, Weight loss, Jaundice, Dark urine, Polyuria, polydipsia, polyphagia • Diagnosis: o ERCP o CT or MRI o US o Elevated amylase & lipase o Elevated liver enzymes & BG • Treatment/Nursing Interventions: o Opioids for pain management o Pancreatic-enzyme replacement therapy (PERT) take with food Pancrelipase PO • Contains amylase, lipase, & protease • Take with antacids, PPI’s, or H2-receptor agonists o Monitor I/O’s (esp. stools!) o Diet: High carb, high protein, high calorie diet (4000-6000 Cals/day!) Bland foods No EtOH o Surgery: Pancreatectomy Pancreas transplant Pancreatic Abscess: Serious complication of necrotizing pancreatitis in which collections of purulent liquefaction form in a necrotic pancreas • Fatal if untreated! • Significant fever (>104 F) • Treatment: Drainage ASAP, Antibiotics Pancreatic Pseudocyst: Encapsulated, saclike structures that form on or surround the pancreas, causing inflammation & fibrosis • May contain Liters of fluid! • Risk factors: Pancreatitis & abdominal trauma • S/Sx: o Epigastric pain radiating to back, Abdominal fullness • Treatment: o Drainage if needed Pancreatic Cancer: Cancer of the pancreas, usually originating from epithelial cells of the pancreatic ductal system o Highly metastatic! o Late diagnosis • Risk factors: Older age, Males>females, Family history, DM, Chronic pancreatitis, Cirrhosis, High red meat intake, Obesity, Smoking • Signs & Symptoms o Often do not exhibit until late, advanced disease! Jaundice *often initial sign*, Clay-colored stool. Dark, frothy urine, Dry, itchy skin, Vague upper abdominal pain radiating to back, N/v, Weight loss, & anorexia, Glucose intolerance, Splenomegaly, Flatulence, GI bleed, Ascites, VTE (PE or DVT), Weakness/fatigue, Elevated pancreatic enzymes, Elevated BG levels • Diagnosis: o ERCP o CT or US o Elevated CEA • Treatment: o Chemotherapy o Radiation o Biliary stents for obstruction o Pancreatectomy Partial: laparoscopic removal of pancreatic tumor • For <3 cm in size Radical (Whipple/pancreatoduodenectomy): Removal of proximal head of pancreas, the duodenum, a portion of the jejunum, the stomach, and the gallbladder • Anastomosis of pancreatic duct, common bile duct, and stomach to jejunum • Splenectomy may also be performed [Show More]
Last updated: 1 year ago
Preview 1 out of 26 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 06, 2022
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Jan 06, 2022
Downloads
0
Views
142