NCLEX-RN Practice Quiz Test Bank #9 (75 Questions And Answers)
Document Content and Description Below
NCLEX-RN Practice Quiz Test Bank #9 (75 Questions) NCLEXRN-09-001 Question Tag: room assignments Question Category: Physiological Integrity, Basic Care and Comfort Which roommate would be mo... st suitable for the 6-year-old male with a fractured femur in Russell’s traction? A. 16-year-old female with scoliosis B. 12-year-old male with a fractured femur C. 10-year-old male with sarcoma D. 6-year-old male with osteomyelitis Correct Answer: B. 12-year-old male with a fractured femur The 6-year-old should have a roommate as close to the same age as possible, so the 12-year-old is the best match. A bed is available and the patient gets assigned. There are certain constraints—sex, semi-private versus private, isolation issues, acuity, telemetry and specialty needs. All need to be taken into account to ensure that each patient goes to the right place and receives the proper care. But good capacity management demands that bed assignment be carefully considered and executed. Option A: The client is too old and is female. Bed assignment simply provides the proper location based on specific patient attributes like sex, isolation, telemetry, acuity and specialty needs. Option C: The 10-year-old with sarcoma has cancer and will be treated with chemotherapy that makes him immune suppressed. Bed managers aim at finding an assignment of patients to rooms that strikes a balance between patients’ preferences and comfort on the one hand, and patients’ clinical conditions and the resulting required room facilities on the other. Option D: The 6-year-old with osteomyelitis is infectious. Rooms and beds belong to the critical assets of just any hospital. They account for a considerable part of a hospital’s infrastructure, and a large amount of financial resources are invested in equipping them with medical apparatus to facilitate patient care. Furthermore, they also represent the place where most patients will spend a large part of their stay, as they recover from surgery, wait for examinations to take place, etc. NCLEXRN-09-002 Question Tag: celebrex (Celecoxib) Question Category: Health Promotion and Maintenance A client with osteoarthritis has a prescription for celebrex (Celecoxib). Which instruction should be included in the discharge teaching? A. Take the medication with milk. B. Report chest pain. C. Remain upright after taking for 30 minutes. D. Allow 6 weeks for optimal effects. Correct Answer: B. Report chest pain. Cox II inhibitors have been associated with heart attacks and strokes. Any changes in cardiac status or signs of a stroke should be reported immediately, along with any changes in bowel or bladder habits because bleeding has been linked to use of Cox II inhibitors. Like all NSAIDs, celecoxib carries an FDA boxed warning for cardiovascular risk, including the increased risk of heart attacks and strokes. As a selective COX-2 inhibitor, celecoxib also faces scrutiny for increased cardiovascular risk, since another selective COX-2 inhibitor, rofecoxib, was withdrawn from production in 2004 due to cardiovascular risk concerns. Option A: The medication can be taken with water. Celecoxib is a medication that is taken orally and comes in 50, 100, 200, and 400 mg doses. In rare cases, celecoxib can also be added to customized compounds for topical administration with or without the use of iontophoresis or other topical delivery mechanisms. It is not available via any other route of administration. Option C: The client may remain upright but not necessarily for 30 minutes. Symptoms of celecoxib overdose would likely be similar to overdoses of other NSAIDs, which include lethargy, drowsiness, nausea, vomiting, and epigastric pain. Activated charcoal may be administered for overdose treatment at the discretion of emergency medical providers if the patient presents within 4 hours of known or suspected ingestion of significant amounts of celecoxib. Option D: Allow 6 weeks for optimal effect. In the inpatient setting, as mentioned above, celecoxib is increasingly being used as part of pre-operative and post-operative multimodal pain management algorithms. Research has shown in several small randomized trials that administering celecoxib peri-operatively for elective procedures such as total hip arthroplasties, total knee arthroplasties, and other procedures with some success in reducing pain and improving functionality such as early ambulation. NCLEXRN-09-003 Question Tag: fracture, cast Question Category: Safe and Effective Care Environment,, Safety and Infection Control A client with a fractured tibia has a plaster-of-Paris cast applied to immobilize the fracture. Which action by the nurse indicates an understanding of a plaster-of-Paris cast? The nurse: A. Handles the cast with the fingertips B. Petals the cast C. Dries the cast with a hair dryer D. Allows 24 hours before bearing weight Correct Answer: D. Allows 24 hours before bearing weight A plaster-of-Paris cast takes 24 hours to dry, and the client should not bear weight for 24 hours. After the process of applying the casting material is completed, the material will start to dry in about 10 to 15 minutes. The temperature of the skin might rise as the plaster is drying because of a chemical reaction that occurs. When plaster is used, it can take from 1 to 2 days for the cast to harden completely. Option A: The cast should be handled with the palms, not the fingertips. Use the palm of hand to apply, hold, or move cast and support on pillows after application. Uneven plaster is irritating to the skin and may result in abrasions. Option B: Petaling a cast is covering the end of the cast with cast batting or a sock, to prevent skin irritation and flaking of the skin under the cast. Trim excess plaster from edges of the cast as soon as casting is completed; prevents skin breakdown caused by prolonged moisture trapped under the cast. Option C: The client should be told not to dry the cast with a hair dryer because this causes hot spots and could burn the client. This also causes unequal drying. Promote cast drying by removing bed linen, exposing it to circulating air; pressure can cause ulcerations, necrosis, or nerve palsies. Pad (petal) the edges of the cast with waterproof tape; provides an effective barrier to cast flaking and moisture. Helps prevent the breakdown of cast material at the edges and reduce skin irritation and excoriation. NCLEXRN-09-004 Question Tag: fiberglass cast Question Category: Physiological Integrity, Basic Care and Comfort The teenager with a fiberglass cast asks the nurse if it will be okay to allow his friends to autograph his cast. Which response would be best? A. “It will be alright for your friends to autograph the cast.” B. “Because the cast is made of plaster, autographing can weaken the cast.” C. “If they don’t use chalk to autograph, it is okay.” D. “Autographing or writing on the cast in any form will harm the cast.” Correct Answer: A. “It will be alright for your friends to autograph the cast.” There is no reason that the client’s friends should not be allowed to autograph the cast; it will not harm the cast in any way, so answers B, C, and D are incorrect. Fiberglass has several advantages compared to plaster. It weighs less, so the cast made from it will be lighter. More durable and porous, fiberglass allows air to flow in and out. Fiberglass is the better choice in case the limb must be X-rayed during the healing process. It is also available in a variety of colors. Option B: Plaster costs less than fiberglass and is more malleable (is more easily shaped) than fiberglass in certain cases. Plaster comes in strips or rolls that are moistened and rolled on over the padding. Plaster materials are made from dry muslin that is treated with starch or dextrose and calcium sulfate. Option C: Keep the cast clean and dry. A hair dryer with a cool setting may be used to dry a fiberglass cast if it becomes damp. Call a doctor if the cast does not dry or if the skin under the cast becomes wet. Avoid placing pressure or weight on the cast. If you have a leg injury and have a walking cast, make sure that the cast has hardened completely before you attempt to walk on it. Option D: Like plaster, fiberglass materials come in rolls. Strips are moistened and applied to form the cast. The cast will appear rough after it has dried. Do not place any objects inside the cast. Avoid using lotions or powders on skin underneath the cast. NCLEXRN-09-005 Question Tag: Steinmann pin Question Category: Safe and Effective Care Environment, Management of Care The nurse is assigned to care for the client with a Steinmann pin. During pin care, she notes that the LPN uses sterile gloves and Q-tips to clean the pin. Which action should the nurse take at this time? A. Assisting the LPN with opening sterile packages and peroxide. B. Telling the LPN that clean gloves are allowed. C. Telling the LPN that the registered nurse should perform pin care. D. Asking the LPN to clean the weights and pulleys with peroxide. Correct Answer: A. Assisting the LPN with opening sterile packages and peroxide The nurse is performing the pin care correctly when she uses sterile gloves and Q-tips. All pins and wire sites must be cleaned daily. Basic pin care will be performed once daily by the hospital nursing staff prior to discharge from the hospital. Following discharge, the patient and family will go to the clinic for pin care teaching and instructions. Option B: During pin care, the sterile technique is utilized and sterile gloves are needed. The approach to pin care should occur in a stepwise fashion. If step one is effective there is no need to go further and pins can be wrapped with gauze. If step one is not effective, please continue until effective pin care has been achieved. Option C: A licensed practical nurse can perform pin care. Pin care is recommended during showers, after pool therapy, or swimming in the pool or ocean (ocean saltwater is good for pin sites). Ideally, pin sites are cleaned when the surrounding skin and gauze are soft. This should make removal of gauze and cleaning of pins less painful. Option D: There is no need to clean the weights. The purpose of the cleaning is to prevent the skin from attaching to the pins and wires and to clean and inspect the area to decrease the chance of infection. NCLEXRN-09-006 Question Tag: scoliosis, spica cast Question Category: Physiological Integrity, Reduction of Risk Potential A child with scoliosis has a spica cast applied. Which action specific to the spica cast should be taken? A. Check the bowel sounds B. Assess the blood pressure C. Offer pain medication D. Check for swelling Correct Answer: A. Check the bowel sounds A body cast or spica cast extends from the upper abdomen to the knees or below. Bowel sounds should be checked to ensure that the client is not experiencing a paralytic ileus. Auscultate the abdomen for bowel sounds, if bowel sounds are present, or the patient reports they are passing flatus, clear fluids can commence and aperiments can be administered. Patients must not commence oral fluids if bowel sounds are not present as this finding indicates an ileus. Option B: Checking the blood pressure is a treatment for any client. Routine post anaesthetic observations are a requirement for patient assessment and the recognition of clinical deterioration in post-operative patients; acknowledging that children are at a high risk of complications post anesthetics, surgeries and procedures. Option C: Offering pain medication is inappropriate. Patients who have had a closed reduction usually only require oral analgesia. Patients who have sustained a fracture or who have had open reduction or osteotomy will usually require an opioid infusion and/or epidural. Pain scores, interventions, and evaluation of interventions performed, should be documented in the observation flowsheet. Option D: Checking for swelling isn’t specific to the stem. Evaluate patients’ skin integrity regularly. Observe any redness, irritation or burning sensation. In the acute postoperative period swelling can occur and a tight cast can potentially cause neurovascular compromise. Children who have had an open reduction or osteotomy may have significant swelling in the groin area. Monitor swelling and plaster to ensure the cast is not too tight. NCLEXRN-09-007 Question Tag: fracture, traction Question Category: Safe and Effective Care Environment,, Safety and Infection Control The client with a cervical fracture is placed in traction. Which type of traction will be utilized at the time of discharge? A. Russell’s traction B. Buck’s traction C. Halo traction D. Crutchfield tong traction Correct Answer: C. Halo traction Halo traction will be ordered for the client with a cervical fracture. Halo-gravity traction is a way to pull the head and spine upward carefully, applying a slow stretch to the spine. Doctors do this by attaching a halo (a metal ring that surrounds the head) to a pulley system. Over several weeks, weights are added to the pulley system to slowly pull the head upward. This pulling is called “traction.” Kids stay in the hospital during halo-gravity traction. Option A: According to Oxford Reference, Russell traction is a type of skin traction used to stabilize and align the lower extremities. The patient’s leg is suspended in a sling and attached to pulleys, strings and weights, which serve to gently draw the bones into alignment. Option B: An apparatus for applying longitudinal traction on the leg by contact between the skin and adhesive tape, for maintaining the proper alignment of a leg fracture; friction between the tape and skin permits application of force through a cord over a pulley, suspending a weight; elevation of the foot of the bed allows the body to act as a counterweight; a type of traction in which a non constricting boot with weights is worn by the Pt to maintain proper alignment. Option D: Crutchfield tongs are used while in the hospital and the client is immobile. A traction device whose pins are inserted into the skull to distract and/or immobilize the neck. Crutchfield tongs are used to stabilize fractures of the cervical spine. NCLEXRN-09-008 Question Tag: continuous passive motion device Question Category: Physiological Integrity, Physiological Adaptation A client with a total knee replacement has a CPM (continuous passive motion device) applied during the postoperative period. Which statement made by the nurse indicates an understanding of the CPM machine? A. “Use of the CPM will permit the client to ambulate during the therapy.” B. “The CPM machine controls should be positioned distal to the site.” C. “If the client complains of pain during the therapy, I will turn off the machine and call the doctor.” D. “Use of the CPM machine will alleviate the need for physical therapy after the client is discharged.” Correct Answer: B. “The CPM machine controls should be positioned distal to the site.” The controller for the continuous-passive-motion device should be placed away from the client. Many clients complain of pain while having treatments with the CPM, so they might turn off the machine. The CPM flexes and extends the leg. Continuous passive motion (CPM) is a therapy in which a machine is used to move a joint without the patient having to exert any effort. A motorized device gently bends the joint back and forth to a set number of degrees, and the amount of movement and speed can be adjusted by the physical therapist. CPM machines are most commonly used on knee joints (after some types of knee surgery), but there are versions made for other joints as well. Option A: The client is in the bed during CPM therapy. The use of CPM may begin in the recovery room after surgery or on the day after surgery. Use of the CPM machine may be continuous while you are in the hospital, other than at times when you are receiving other physical therapy or are getting out of bed to use the restroom. Option C: The client will experience pain with the treatment. Recovering normal joint mobility after surgery can be a significant challenge. The stiffness of a joint can be a complication that limits outcomes and causes pain. Because of this, some surgeons use CPM to try to prevent scar tissue formation and improve range of motion. Option D: Use of the CPM does not alleviate the need for physical therapy. It may be recommended after procedures like ACL reconstruction or frozen shoulder surgery, but CPM is most likely to be prescribed after knee replacement or knee cartilage repair surgery. It may also be used after surgery to remove knee tumors in children with osteosarcoma. NCLEXRN-09-009 Question Tag: walker, fracture Question Category: Safe and Effective Care Environment,, Safety and Infection Control A client with a fractured hip is being taught correct use of the walker. The nurse is aware that the correct use of the walker is achieved if the: A. Palms rest lightly on the handles B. Elbows are flexed 0° C. Client walks to the front of the walker D. Client carries the walker Correct Answer: A. Palms rest lightly on the handles The client’s palms should rest lightly on the handles. The elbows should be flexed no more than 30° but should not be extended. Once a model of the walker has been selected, the “fit” of the walker becomes important. When holding on to the walker, the elbows should be bent in a position that feels comfortable and natural. The top of the walker should be even with the crease on the underside of the wrist when the arms are relaxed at the side. Option B: A 0° is not a relaxed angle for the elbows and will not facilitate correct walker use. Walkers that are too low cause the client to stoop over while walking, which impedes proper body mechanics. If the walker is at the wrong height, the client will be prone to aches and pains. Option C: The client should walk to the middle of the walker, not to the front of the walker. To get started, the client should push the walker slightly ahead, then step into the walker. Keep that pattern going—walker slightly ahead, then step into the walker. The walker should never be too far ahead and the client should have excellent posture as he takes steps. Also, the client should not look at feet, rather in front of him. Option D: The client should be taught not to carry the walker because this would not provide stability. If there is trouble gripping the walker, platform walkers are available that may prove to be a better option. The platform allows the client to rest the elbow and forearm, taking stress off the hands. NCLEXRN-09-010 Question Tag: prolapsed cord Question Category: Physiological Integrity, Physiological Adaptation When assessing a laboring client, the nurse finds a prolapsed cord. The nurse should: A. Attempt to replace the cord B. Place the client on her left side C. Elevate the client’s hips D. Cover the cord with a dry, sterile gauze Correct Answer: C. Elevate the client’s hips. The client with a prolapsed cord should be treated by elevating the hips and covering the cord with a moist, sterile saline gauze. The nurse should use her fingers to push up on the presenting part until a cesarean section can be performed. Cesarean section should be performed before rupture of the membrane or the cord would slide down the vagina. Option A: The nurse should not attempt to replace the cord. Assessment of fetal heart sounds is necessary after rupture of membranes to rule out cord prolapse. If there is already complete dilatation, the physician can deliver the baby to prevent fetal anoxia. Option B: The client should not be turned to the side. The goal in therapeutic management is to relieve cord compression to avoid fetal anoxia that can be achieved through manually lifting the head of the fetal head off the cord through the vagina or placing the woman in a Trendelenburg position. Option D: The cord should be covered with a moist, sterile saline gauze. Once the cord has prolapsed and is exposed to air, drying of the umbilical cord and atrophy of the umbilical vessels would begin. Cover any exposed portion of the cord with a sterile saline compress to avoid drying. NCLEXRN-09-011 Question Tag: rosuvastatin Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The client presents to the clinic with a serum cholesterol of 275 mg/dL and is placed on rosuvastatin (Crestor). Which instruction should be given to the client? A. Report muscle weakness to the physician. B. Allow six months for the drug to take effect. C. Take the medication with fruit juice. D. Ask the doctor to perform a complete blood count before starting the medication. Correct Answer: A. Report muscle weakness to the physician. The client taking antilipidemics should be encouraged to report muscle weakness because this is a sign of rhabdomyolysis. The most common toxic side effect of rosuvastatin is myalgia. If the patient has mild to moderate muscle symptoms, the drug should be discontinued to evaluate for other causes of myalgia. If there is a resolution of the underlying etiology, the patient can restart the original or a lower dose of rosuvastatin; however, if symptoms reoccur for a second time, then discontinue rosuvastatin indefinitely. Switching to a different statin medication at a lower dose may relieve muscle symptoms. Option B: The medication takes effect within 1 month of beginning therapy. Dosing is individualized based on the low-density lipoprotein (LDL) levels at baseline and the goal of therapy. The patient’s response and adherence to medication is an important determinant to therapeutic success. Adjustments should be made at a regular interval of four weeks or more depending on the underlying pathology of the disease and whether the treatment is for primary versus secondary prevention. Option C: The medication should be taken with water because fruit juice, particularly grapefruit, can decrease the effectiveness. The administration of rosuvastatin is via capsule or tablet. The capsule can be administered orally or via a nasogastric tube. The oral route can be taken with or without food, at any time of the day, and should be swallowed whole. The capsule should never be crushed or chewed. If opening the capsule, it is recommended to empty the contents into one teaspoonful of applesauce and then swallow immediately without chewing. Option D: Liver function studies should be checked before beginning the medication, not after the fact, making answer D incorrect. Creatinine phosphokinase (CPK) levels should not be routinely measured; however, the clinician can base special considerations for measuring CPK on family history of statin intolerance, drug-drug interactions leading to increased risk of myopathy, or other clinical presentations that create a high index of suspicion of myopathy. NCLEXRN-09-012 Question Tag: diazoxide, hypertensive crises Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The client is admitted to the hospital with hypertensive crises. Diazoxide (Hyperstat) is ordered. During administration, the nurse should: A. Utilize an infusion pump B. Check the blood glucose level C. Place the client in Trendelenburg position D. Cover the solution with foil Correct Answer: B. Check the blood glucose level Hyperstat is given as an IV push for hypertensive crises, but it often causes hyperglycemia. The glucose level will drop rapidly when stopped. This medication is used to treat very low blood sugar (hypoglycemia). Certain conditions (such as tumor on the pancreas, cancer, leucine sensitivity) can cause the release of too much insulin. Insulin is a natural substance that lowers blood sugar. This drug works by preventing insulin release from the pancreas, helping to return the blood sugar to normal levels. Diazoxide is a thiazide drug, but has no diuretic (“water pill”) effects like other thiazides. Option A: Diazoxide (Hyperstat) is given by IV push. Diazoxide is a potassium channel activator. Its mechanism of action revolves around enhancing cell membrane permeability to potassium ions. This action consequently elicits the relaxation of local smooth muscles. This switches off voltage-gated calcium ion channels which inhibits the generation of an action potential. Option C: The client should be placed in a dorsal recumbent position, not a Trendelenburg position. Diazoxide is used to treat low blood sugar (hypoglycemia) caused by certain cancers or other conditions that can make the pancreas release too much insulin. This medicine is for use in adults and children as young as infants. Option D: This medication does not have to be covered with foil. Store at room temperature away from moisture, heat, and light. Diazoxide is only part of a treatment program that may also include diet. Follow the doctor’s instructions very closely. NCLEXRN-09-013 Question Tag: ventral septal defect, Digitalis Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The 6-month-old client with a ventral septal defect is receiving Digitalis for regulation of his heart rate. Which finding should be reported to the doctor? A. Blood pressure of 126/80 B. Blood glucose of 110 mg/dL C. Heart rate of 60 bpm D. Respiratory rate of 30 per minute Correct Answer: C. Heart rate of 60 bpm A heart rate of 60 in the baby should be reported immediately. The dose should be held if the heart rate is below 100 bpm. Digoxin has vagomimetic effects on the AV node. By stimulating the parasympathetic nervous system, it slows electrical conduction in the atrioventricular node, therefore, decreases the heart rate. The rise in calcium levels leads to prolongation of phase 4, and phase 0 of the cardiac action potential thus increases the refractory period of the AV node. Slower conduction through the AV node carries a decreased ventricular response. Option A: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart. Digoxin induces an increase in intracellular sodium that will drive an influx of calcium in the heart and cause an increase in contractility. Cardiac output increases with a subsequent decrease in ventricular filling pressures. Option B: Electrocardiogram changes seen with digoxin demonstrate a downsloping ST-segment depression, also known as a “reverse check” sign. The ST segments may appear “scooped” without abnormal Q waves or T wave inversions. Regular intake of digoxin results in changes such as a decreased QT interval, prolongation of the PR interval and T wave inversion or flattening. In the case of overdose, the patient should receive digoxin immune fab. Option D: The prescriber needs to check levels with any recent change in medication. The kidneys excrete approximately 70% of digoxin in direct proportion to the patient’s glomerular filtration rate. The physician must request regular electrocardiograms and bloodwork to assess for renal function, and electrolytes require close monitoring. NCLEXRN-09-014 Question Tag: angina, nitroglycerin Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The client admitted with angina is given a prescription for nitroglycerin. The client should be instructed to: A. Replenish his supply every 3 months B. Take one every 15 minutes if pain occurs C. Leave the medication in the brown bottle D. Crush the medication and take with water Correct Answer: C. Leave the medication in the brown bottle Nitroglycerine should be kept in a brown bottle (or even a special air- and water-tight, solid or plated silver or gold container) because of its instability and tendency to become less potent when exposed to air, light, or water. Store nitroglycerin pills in a dark-colored (such as brown), airtight, glass container that you cannot see through. Keep the container tightly closed. Keep nitroglycerin pills and liquid spray away from heat or moisture. Option A: The supply should be replenished every 6 months, not 3 months. Nitroglycerin is most commonly administered as a tablet that is absorbed sublingually. It is given in hospitals as well as prescribed for outpatient use. Patients may be prescribed nitroglycerin to take as prophylaxis for anginal chest pain prior to an event that may provoke anginal symptoms. They must be instructed to allow the nitroglycerin to dissolve in their mouth and allow their oral mucosa to absorb the drug. Option B: One tablet should be taken every 5 minutes until pain subsides. If the pain does not subside, the client should report to the emergency room. There currently are three doses available: 0.3 mg, 0.4 mg, and 0.6 mg. The dose is repeatable every 5 minutes until the achievement of relief. If anginal pain persists after three doses, prompt medical attention is required. After administration, the onset of vasodilatory effects occurs within 1 to 3 minutes, with a max effect occurring within 5 minutes. Option D: The medication should be taken sublingually and should not be crushed. Nitroglycerin is primarily eliminated via metabolism in the liver and has a mean half-life of approximately 2 to 3 minutes. In the event of overdose, monitoring of vital signs may be necessary to monitor the hemodynamic effects of nitroglycerin. Continuous monitoring of blood pressure, heart rate, respiratory rate, and oxygen saturation is recommended. NCLEXRN-09-015 Question Tag: cholesterol Question Category: Physiological Integrity, Basic Care and Comfort The client is instructed regarding foods that are low in fat and cholesterol. Which diet selection is lowest in saturated fats? A. Macaroni and cheese B. Shrimp with rice C. Turkey breast D. Spaghetti Correct Answer: C. Turkey breast Turkey contains the least amount of fats and cholesterol. Both turkey and chicken are rich in high-quality protein. Chicken breast has slightly more protein than turkey breast, but turkey thigh is minimally higher in protein than chicken thigh. The other meat cuts provide equal amounts of protein. Option A: It’s typically high in calories because it’s made with pasta, cheese, cream, and butter, although the calorie content varies significantly between brands, ingredients, and serving size. Mac and cheese contain large amounts of fat and refined carbs, both of which contribute to its high calorie count. Eating more calories than you burn, regardless of which foods they come from, can lead to weight gain. Option B: White rice is highly processed and missing its hull (the hard protective coating), bran (outer layer), and germ (nutrient-rich core). Meanwhile, brown rice only has the hull removed. White rice is considered empty carbs since it loses its main sources of nutrients. Option D: Spaghetti is one of the most popular forms of pasta, and it’s used in dishes all around the world. Most spaghetti is made from durum wheat, so it’s high in complex carbohydrates and includes all the nutrients found in refined white flour. Liver, eggs, beef, cream sauces, shrimp, cheese, and chocolate should be avoided by the client. The client should bake meat rather than frying to avoid adding fat to the meat during cooking. NCLEXRN-09-016 Question Tag: congestive heart failure Question Category: Physiological Integrity, Reduction of Risk Potential The client is admitted with right congestive heart failure. In assessing the client for edema, the nurse should check the: A. Feet B. Neck C. Hands D. Sacrum Correct Answer: B. Neck The jugular veins in the neck should be assessed for distension. Increased blood volume, which can occur with right sided heart failure, or anything that interferes with filling of the right atrium or movement of the blood into the right ventricle, can increase the central venous pressure and the amount of jugular vein distention. Option A: Jugular vein distention is affected by the position of your body. If the height is greater than 3 to 4 centimeters when measured while you are in bed with your head elevated 45 degrees, this may signal vascular or heart disease. Smaller amounts of jugular vein distention can occur in people without heart or vascular disease. Option C: For example, jugular vein distention may be raised by a narrowing or blockage of the superior vena cava, which can interfere with blood return to the heart. Option D: It can also be caused by constrictive pericarditis (infection of the lining that surrounds the heart) and cardiac tamponade (filling of the sac around the heart with blood or other fluid), both of which restrict the volume of the heart. The other parts of the body will be edematous in right-sided congestive heart failure, not left-sided. NCLEXRN-09-017 Question Tag: central venous pressure Question Category: Physiological Integrity, Reduction of Risk Potential The nurse is checking the client’s central venous pressure. The nurse should place the zero of the manometer at the: A. Phlebostatic axis B. PMI C. Erb’s point D. Tail of Spence Correct Answer: A. Phlebostatic axis The phlebostatic axis is located at the fifth intercostal space midaxillary line and is the correct placement of the manometer. Phlebostatic axis is a point located by drawing an imaginary line from the fourth intercostal space at the sternum and finding its intersection with an imaginary line drawn down the center of the chest below the axillae. Option B: The PMI or point of maximal impulse is located at the fifth intercostal space midclavicular line. The point of maximal impulse, known as PMI, is the location at which the cardiac impulse can be best palpated on the chest wall. Frequently, this is at the fifth intercostal space at the midclavicular line. When dilated cardiomyopathy is present, this can be shifted laterally. Option C: Erb’s point is the point at which you can hear the valves close simultaneously. “Erb’s point” is also a term used in head and neck surgery to describe the point on the posterior border of the sternocleidomastoid muscle where the four superficial branches of the cervical plexus—the greater auricular, lesser occipital, transverse cervical, and supraclavicular nerves—emerge from behind the muscle. Option D: The Tail of Spence (the upper outer quadrant) is the area where most breast cancers are located and has nothing to do with the placement of a manometer. The tail of Spence (Spence’s tail, axillary process, axillary tail) is an extension of the tissue of the breast that extends into the axilla. It is actually an extension of the upper lateral quadrant of the breast. It passes into the axilla through an opening in the deep fascia called foramen of Langer. NCLEXRN-09-018 Question Tag: hypertension Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The physician orders lisinopril (Zestril) and furosemide (Lasix) to be administered concomitantly to the client with hypertension. The nurse should: A. Question the order B. Administer the medications C. Administer separately D. Contact the pharmacy Correct Answer: B. Administer the medications Zestril is an ACE inhibitor and is frequently given with a diuretic such as Lasix for hypertension. Studies of hypertension confirm that ACE inhibitors enhance the antihypertensive effects of diuretics, though the interaction appears more additive than synergistic. Combining diuretics with ACE inhibitors appear to be no more effective than combining them with beta blockers. Option A: Diuretics and angiotensin-converting enzyme (ACE) inhibitors are commonly used in combination, both for patients with heart failure and for those with hypertension. Option C: Diuretics activate the renin–angiotensin–aldosterone (RAAS) system that may limit the effects of diuretics on vascular tone and sodium excretion, which in turn, may limit their efficacy in reducing arterial pressure or in improving the symptoms of heart failure. ACE inhibitors can reduce plasma concentrations of angiotensin II and aldosterone, providing a theoretical rationale for use in combination with a diuretic. Option D: The order is accurate. There is no need to question the order, administer the medication separately, or contact the pharmacy. When used in combination, the thiazide diuretics and the angiotensin-converting enzyme inhibitors have been shown to improve blood pressure reduction over either drug used alone. NCLEXRN-09-019 Question Tag: edema Question Category: Physiological Integrity, Physiological Adaptation The best method of evaluating the amount of peripheral edema is: A. Weighing the client daily B. Measuring the extremity C. Measuring the intake and output D. Checking for pitting Correct Answer: B. Measuring the extremity ADVERTISEMENTS The best indicator of peripheral edema is measuring the extremity. A paper tape measure should be used rather than one of plastic or cloth, and the area should be marked with a pen, providing the most objective assessment. The circumferential method is one of the girth measurement techniques. For consistent measurements, each upper extremity or lower extremity is marked with a semi-permanent marker at a certain part with reference to the bony prominences. Option A: Weighing the client will not indicate peripheral edema. The accumulation of fluid occurs when local or systemic conditions disrupt this equilibrium, leading to increased capillary hydrostatic pressure, increased plasma volume, decreased plasma oncotic pressure (hypoalbuminemia), increased capillary permeability, or lymphatic obstruction. Option C: Measuring the intake and output will not indicate peripheral edema. The most commonly used tools to measure edema are: volume measurements (with a water volumeter); girth measurements (with a tape measure); and pitting edema assessment (based on the depth and duration of the indentation). Water displacement and ankle circumference had shown a high inter-examiner agreement (intraclass correlation coefficient 0.93, 0.96 right; 0.97, 0.97 left). Option D: Checking for pitting edema is less reliable than measuring with a paper tape measure. There are two types of edema, pitting and non- pitting edema. Pitting edema is described as an indentation that remains in the edematous area after pressure is applied. Its location, timing, and extent are determined for treatment response. It is mainly assessed on the medial malleolus, the bony portion of the tibia, and the dorsum of the foot. Non-pitting edema is seen in lymphoedema, myxedema, and lipedema. NCLEXRN-09-020 Question Tag: vaginal cancer, radioactive implant Question Category: Physiological Integrity, Physiological Integrity, Reduction of Risk Potential A client with vaginal cancer is being treated with a radioactive vaginal implant. The client’s husband asks the nurse if he can spend the night with his wife. The nurse should explain that: A. Overnight stays by family members are against hospital policy. B. There is no need for him to stay because staffing is adequate. C. His wife will rest much better knowing that he is at home. D. Visitation is limited to 30 minutes when the implant is in place. Correct Answer: D. Visitation is limited to 30 minutes when the implant is in place. Clients with radium implants should have close contact limited to 30 minutes per visit. The general rule is limiting time spent exposed to radium, putting distance between people and the radium source, and using lead to shield against the radium. Teaching family members these principles is extremely important. Internal radiation therapy uses a pill, liquid, implant or temporary source to put radiation inside the body to kill the cancer cells, and may require certain safety precautions for staff and family while the patient is in the hospital or at home, according to the National Cancer Institute Option A: Do not spend any more time in the patient’s room than is necessary to care for the patient. In particular, time at the patient’s bedside should be kept to a minimum. Specific “stay times” will be provided on the patient’s door. Option B: Visitors are allowed provided that: visitors shall be 18 years or older; the patient shall not have pregnant visitors; and visitors should remain at least 6 feet from the patients and should not stay more than 2 hours per day (unless other information is provided). Option C: The most common safety precautions related to preventing unnecessary radiation exposure are limiting time near the patient, maintaining a safe distance of three to six feet from the source of the radiation and using lead shielding to protect family and staff. NCLEXRN-09-021 Question Tag: facial stroke Question Category: Physiological Integrity, Basic Care and Comfort The nurse is caring for a client hospitalized with a facial stroke. Which diet selection would be suited to the client? A. Roast beef sandwich, potato chips, pickle spear, iced tea B. Split pea soup, mashed potatoes, pudding, milk C. Tomato soup, cheese toast, Jello, coffee D. Hamburger, baked beans, fruit cup, iced tea Correct Answer: B. Split pea soup, mashed potatoes, pudding, milk The client with a facial stroke will have difficulty swallowing and chewing, and these food items mentioned provide the least amount of chewing. Consult with a speech therapist to evaluate gag reflexes; assist in teaching alternate swallowing techniques, advise the patient to take smaller boluses of food, and inform the patient of foods that are easier to swallow; provide thicker liquids or pureed diet as indicated. Option A: The patient would have difficulty in chewing meat. Observe the patient for paroxysms of coughing, food dribbling out or pooling in one side of the mouth, food retained for long periods in the mouth, or nasal regurgitation when swallowing liquids. Have the patient sit upright, preferably on a chair, when eating and drinking; advance diet as tolerated. Option C: This group would still require more chewing. Prepare for GI feedings through a tube if indicated; elevate the head of bed during feedings, check tube position before feeding, administer feeding slowly, and ensure that the cuff of the tracheostomy tube is inflated (if applicable); monitor and report excessive retained or residual feeding. Option D: The following food items would require more chewing and, thus, are incorrect. Avoid hard, chewy foods as these can be difficult to prepare, and choose a soft easy chew diet (such as pasta dishes, fish, well-cooked meats, and vegetables). Try smaller mouthfuls as these are easier to control and less likely to spill from the mouth. NCLEXRN-09-022 Question Tag: diabetes mellitus, insulin Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The physician has prescribed Novolog insulin for a client with diabetes mellitus. Which statement indicates that the client knows when the peak action of the insulin occurs? A. “I will make sure I eat breakfast within 10 minutes of taking my insulin.” B. “I will need to carry candy or some form of sugar with me all the time.” C. “I will eat a snack around three o’clock each afternoon.” D. “I can save my dessert from supper for a bedtime snack.” Correct Answer: A. “I will make sure I eat breakfast within 10 minutes of taking my insulin.” NovoLog insulin onsets very quickly, so food should be available within 10–15 minutes of taking the insulin. The onset of action is 1 to 3 hours. Crystalline NPH insulin administration is subcutaneous. Administration is not Intramuscular or intravenous. NPH insulin is available in a two-phase solution, which means that apart from NPH, it has a solvent or a rapid-acting insulin solution. It comes in the form of a subcutaneous suspension or suspension pen-injector. Option B: This does not address a particular type of insulin, so it is incorrect. The abdominal subcutaneous injection causes quicker absorption as compared to arms or thighs. The most significant advantage of NPH is that it can be included in premixed formulation with regular insulin. NPH in premixed formulations does not affect the potency and time-action profile of regular insulin. Exercise, massage, and local heat application increase NPH insulin absorption. Option C: NPH insulin peaks in 8–12 hours, so a snack should be eaten at the expected peak time. It may not be 3 p.m. NPH insulin pen requires adequate mixing to get complete resuspension before injecting it. It may be given once or twice daily. Since the action profile of NPH insulin does not cover 24 hours, a twice-daily dose in the morning and evening or bedtime is the recommended regimen, which applies to the premixed formulations as well. Option D: There is no need to save the dessert until bedtime. NPH insulin has a somewhat higher risk of hypoglycemia. Inadequate resuspension is thought to contribute to the high day to day variability in the pharmacodynamic and pharmacokinetic profile of NPH insulin, leading to hypoglycemia. Patients can adequately resuspend NPH by rotating the vial several times until it is uniformly cloudy. NCLEXRN-09-023 Question Tag: infant care Question Category: Health Promotion and Maintenance The nurse is teaching basic infant care to a group of first-time parents. The nurse should explain that a sponge bath is recommended for the first 2 weeks of life because: A. New parents need time to learn how to hold the baby. B. The umbilical cord needs time to separate. C. Newborn skin is easily traumatized by washing. D. The chance of chilling the baby outweighs the benefits of bathing. Correct Answer: B. The umbilical cord needs time to separate. The umbilical cord needs time to dry and fall off before putting the infant in the tub. The first bath will be a sponge bath. Pick a warm room with a flat surface, like a bathroom or kitchen counter, a changing table, or a bed. Cover the surface with a thick towel. Make sure the room temperature is at least 75 degrees Fahrenheit, because babies chill easily. Option A: Taking the baby away for a bath too soon can interrupt skin-to-skin care, mother-child bonding, and early breastfeeding success. One study showed a 166% increase in hospital breastfeeding success after implementing a 12-hour delay in the baby’s first bath compared to those bathed within the first couple hours. Option C: Gentle sponge baths are perfect for the first few weeks until the umbilical cord falls off, the circumcision heals, and the navel heals completely. Once the umbilical cord falls off, and the circumcision and the navel are completely healed, it’s time to try a tub bath. Option D: Although these statements might be important, they are not the primary answer to the question. The World Health Organization (WHO) recommends delaying a baby’s first bath until 24 hours after birth—or waiting at least 6 hours if a full day isn’t possible for cultural reasons. Babies who get baths right away may be more likely to become cold and develop hypothermia. The minor stress of an early bath can also make some babies more likely to have a drop in blood sugar (hypoglycemia). NCLEXRN-09-024 Question Tag: leukemia Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies A client with leukemia is receiving Trimetrexate. After reviewing the client’s chart, the physician orders Wellcovorin (leucovorin calcium). The rationale for administering leucovorin calcium to a client receiving Trimetrexate is to: A. Treat iron-deficiency anemia caused by chemotherapeutic agents B. Create a synergistic effect that shortens treatment time C. Increase the number of circulating neutrophils D. Reverse drug toxicity and prevent tissue damage Correct Answer: D. Reverse drug toxicity and prevent tissue damage Leucovorin is the antidote for Methotrexate and Trimetrexate which are folic acid antagonists. Leucovorin is a folic acid derivative. Leucovorin is FDA indicated after high dose methotrexate therapy in osteosarcoma, to decrease the toxic effects of methotrexate or to counter the toxic effects of folate antagonists. Leucovorin is also occasionally an alternative agent used in the treatment of megaloblastic anemia when oral intake of folic acid is not possible. Option A: Leucovorin does not treat iron deficiency. Off-label uses include as neoadjuvant treatment in bladder cancer, as a cofactor in methanol toxicity, in the treatment of advanced esophageal cancer, advanced gastric cancer, advanced pancreatic cancer, prevention of hematological toxicity of pyrimethamine in patients with AIDS and the treatment of ectopic pregnancy (along with methotrexate). Option B: Leucovirin does not create a synergistic effect when taken with Trimextrate. When used as a part of chemotherapeutic regimens, leucovorin is not administered along with methotrexate. It is usually administered 24 hours after a course of methotrexate. Tissue toxicity may be permanent if leucovorin therapy gets delayed beyond 40 hours. Option C: An increase in neutrophils is not an effect of Leucovirin. Folic acid in large quantities has been shown to counteract the pharmacological actions of antiepileptics such as primidone, phenobarbital, and phenytoin. When leucovorin has been used concomitantly during the treatment of Pneumocystis jirovecii with trimethoprim-sulfamethoxazole (TMP-SMX), higher rates of treatment failure and morbidity have been reported. NCLEXRN-09-025 Question Tag: immunization Question Category: Health Promotion and Maintenance A 4-month-old is brought to the well-baby clinic for immunization. In addition to the DPT and polio vaccines, the baby should receive: A. HibTITER B. Mumps vaccine C. Hepatitis B vaccine D. MMR Correct Answer: A. HibTITER The Haemophilus influenza vaccine is given at 4 months with the polio vaccine. It protects the child from Hib disease, which can cause lifelong disability and be deadly; protects the child from the most common type of Hib disease, meningitis (an infection of the lining covering the brain and spinal cord); and keeps the child from missing school or child care, and the parents from missing work. Option B: Mumps vaccine is the best way to decrease the risk of getting mumps. It is usually given as part of a combination vaccine that protects against three diseases: measles, mumps, and rubella (MMR). This vaccine is only licensed for use in children who are 12 months through 12 years of age. Option C: Hepatitis B vaccine is given immediately after birth and for children up to 18 years. Hepatitis B vaccine is usually given as 2, 3, or 4 shots. Infants should get their first dose of hepatitis B vaccine at birth and will usually complete the series at 6 months of age (sometimes it will take longer than 6 months to complete the series). Children and adolescents younger than 19 years of age who have not yet gotten the vaccine should also be vaccinated. Option D: MMR stands for measles, mumps and rubella vaccine, which is given at 9 months old. The MMR vaccine is safe and effective. Most children don’t have any side effects from the vaccine. The side effects that do occur are usually very mild, such as a fever or rash. The first dose at 12 through 15 months of age, and the second dose at 4 through 6 years of age. Questions and rationale from Nurseslabs.com Feel free to print or share and link back to us! For more practice questions, please visit our Nursing Test Bank [https://nurseslabs.com/nursing-test-bank] NCLEXRN-09-026 Question Tag: gastritis Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The physician has prescribed esomeprazole (Nexium) for a client with erosive gastritis. The nurse should administer the medication: A. 30 minutes before meals B. With each meal C. In a single dose at bedtime D. 30 minutes after meals Correct Answer: A. 30 minutes before meals. Proton pump inhibitors reduce the production of acid in the stomach. Proton pump inhibitors work best when they are taken 30 minutes before the first meal of the day. Take each dose with a full glass (8 ounces) of water. Esomeprazole is usually given for 4 to 8 weeks only. The doctor may recommend a second course of treatment if the client needs additional healing time. Option B:It should be taken only once every day. Esomeprazole is used to treat symptoms of gastroesophageal reflux disease (GERD) and other conditions involving excessive stomach acid such as Zollinger-Ellison syndrome. Esomeprazole is also used to promote healing of erosive esophagitis (damage to the esophagus caused by stomach acid). Option C: The medicine would not work on its best if taken at bedtime. Use exactly as directed on the label, or as prescribed by the doctor. Swallow the pill whole and do not crush, chew, break, or open it. Esomeprazole is not for immediate relief of heartburn symptoms. Option D: Proton pump inhibitors are best taken before the first meal of the day to an empty stomach. Esomeprazole may also be given to prevent gastric ulcer caused by infection with Helicobacter pylori (H. pylori), or by the use of nonsteroidal anti-inflammatory drugs (NSAIDs). NCLEXRN-09-027 Question Tag: psychiatric unit Question Category: Psychosocial Integrity A client in the psychiatric unit is in an uncontrolled rage and is threatening other clients and staff. What is the most appropriate action for the nurse to take? A. Call security for assistance and prepare to sedate the client. B. Tell the client to calm down and ask him if he would like to play cards. C. Tell the client that if he continues his behavior he will be punished. D. Leave the client alone until he calms down. Correct Answer: A. Call security for assistance and prepare to sedate the client. If the client is a threat to the staff and to other clients the nurse should call for help and prepare to administer a medication such as Haldol to sedate him. Alert staff if a potential for seclusion appears imminent. Usual priority of interventions would be: firmly setting limits; chemical restraints (tranquilizers); and seclusion. If nursing interventions (quiet environment and firm limit setting) and chemical restraints (tranquilizers–e.g., haloperidol [Haldol]) have not helped dampen escalating manic behaviors, then seclusion might be warranted. Option B: Telling the client to calm down will not work. Frequently assess client’s behavior for signs of increased agitation and hyperactivity. Early detection and intervention of escalating mania will prevent the possibility of harm to self or others, and decrease the need for seclusions. Option C: Telling the client that if he continues he will be punished is a threat and may further anger him. Remain neutral as possible; Do not argue with the client. The client can use inconsistencies and value judgments as justification for arguing and escalating mania. Use a calm and firm approach; provide structure and control for a client who is out of control. Option D: If the client is left alone he might harm himself. Decrease environmental stimuli (e.g., by providing a calming environment or assigning a private room); helps decrease escalation of anxiety and manic symptoms. NCLEXRN-09-028 Question Tag: postpartum Question Category: Health Promotion and Maintenance When the nurse checks the fundus of a client on the first postpartum day, she notes that the fundus is firm, is at the level of the umbilicus, and is displaced to the right. The next action the nurse should take is to: A. Check the client for bladder distention B. Assess the blood pressure for hypotension C. Determine whether an oxytocic drug was given D. Check for the expulsion of small clots Correct Answer: A. Check the client for bladder distention If the fundus of the client is displaced to the side, this might indicate a full bladder. The next action by the nurse should be to check for bladder distention and catheterize, if necessary. The uterus continues to contract after delivery, and its size decreases rapidly as estrogen and progesterone levels diminish. Immediately after delivery, the upper portion of the uterus, known as the fundus, is midline and palpable halfway between the symphysis pubis and the umbilicus. Option B: Primary responsibilities of nurses in postpartum settings are to assess postpartum patients, provide care and teaching, and if necessary, report any significant findings. It is imperative for nurses to distinguish between normal and abnormal findings and to have a clear understanding of the nursing care necessary to promote patients’ health and well-being. Option C: By approximately one hour post delivery, the fundus is firm and at the level of the umbilicus. The fundus continues to descend into the pelvis at the rate of approximately one centimeter (finger-breadth) per day and should be nonpalpable by two weeks postpartum. Option D: These are actions that relate to postpartum hemorrhage. After delivery, the endometrial surface of the uterus is shed via the vagina. The shedding endometrium is known as lochia. Menstruation does not typically return until 12 weeks or later. However ovulation can return prior to menses, and it is important for healthcare providers to discuss family planning with patients during the early postpartum period in order to prevent undesired pregnancies. NCLEXRN-09-029 Question Tag: hemoptysis Question Category: Physiological Integrity, Physiological Adaptation A client is admitted to the hospital with a temperature of 99.8°F, complaints of blood-tinged hemoptysis, fatigue, and night sweats. The client’s symptoms are consistent with a diagnosis of: A. Pneumonia B. Reaction to antiviral medication C. Tuberculosis D. Superinfection due to low CD4 count Correct Answer: C. Tuberculosis A low-grade temperature, blood-tinged sputum, fatigue, and night sweats are symptoms consistent with tuberculosis. A chronic cough, hemoptysis, weight loss, low-grade fever, and night sweats are some of the most common physical findings in pulmonary tuberculosis. Secondary tuberculosis differs in clinical presentation from the primary progressive disease. In secondary disease, the tissue reaction and hypersensitivity is more severe, and patients usually form cavities in the upper portion of the lungs. Option A: If the answer had said pneumocystis pneumonia, it would have been consistent with the symptoms given in the stem, but just saying pneumonia isn’t specific enough to diagnose the problem. Tuberculosis (TB) is an ancient human disease caused by Mycobacterium tuberculosis which mainly affects the lungs, making pulmonary disease the most common presentation (K Zaman, 2010). However, TB is a multi-systemic disease with a protean presentation. The organ system most commonly affected include the respiratory system, the gastrointestinal (GI) system, the lymphoreticular system, the skin, the central nervous system, the musculoskeletal system, the reproductive system, and the liver Option B: M. tuberculosis causes tuberculosis. M. tuberculosis is an alcohol and acid-fast bacillus. It is part of a group of organisms classified as the M. tuberculosis complex. Other members of this group are Mycobacterium africanum, Mycobacterium bovis, and Mycobacterium microti. Most other mycobacteria organisms are classified as non-tuberculous or atypical mycobacterial organisms. Option D: They are not directly related to the stem. Pulmonary or systemic dissemination of the tubercles may be seen in active disease, and this may manifest as miliary tuberculosis characterized by millet shaped lesions on chest x-ray. Disseminated tuberculosis may also be seen in the spine, the central nervous system, or the bowel. NCLEXRN-09-030 Question Tag: migraine Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The client is seen in the clinic for treatment of migraine headaches. The drug Imitrex (sumatriptan succinate) is prescribed for the client. Which of the following in the client’s history should be reported to the doctor? A. Diabetes B. Prinzmetal’s angina C. Cancer D. Cluster headaches Correct Answer: B. Prinzmetal’s angina If the client has a history of Prinzmetal’s angina, he should not be prescribed triptan preparations because they cause vasoconstriction and coronary spasms. Tell the doctor if there is or have ever had heart disease; a heart attack; angina (chest pain); irregular heartbeats; stroke or ‘mini-stroke’; or circulation problems such as varicose veins, blood clots in the legs, Raynaud’s disease (problems with blood flow to the fingers, toes, ears, and nose), or ischemic bowel disease (bloody diarrhea and stomach pain caused by decreased blood flow to the intestines). The doctor may advise not to take sumatriptan. Option A: Sumatriptan is used to treat the symptoms of migraine headaches (severe, throbbing headaches that sometimes are accompanied by nausea or sensitivity to sound and light). Sumatriptan is in a class of medications called selective serotonin receptor agonists. It works by narrowing blood vessels in the head, stopping pain signals from being sent to the brain, and blocking the release of certain natural substances that cause pain, nausea, and other symptoms of migraine. Sumatriptan does not prevent migraine attacks or reduce the number of headaches. Option C: Sumatriptan comes as a tablet to take by mouth. It is usually taken at the first sign of a migraine headache.If symptoms improve after taking sumatriptan but return after 2 hours or longer, the client may take a second tablet. However, if symptoms do not improve after taking sumatriptan, do not take a second tablet without calling the doctor. The doctor will advise the maximum number of tablets to be taken in a 24-hour period. Option D: There is no contraindication for taking triptan drugs in clients with diabetes, cancer, or cluster headaches. If the client takes sumatriptan more often or for longer than the recommended period of time, the headaches may get worse or may occur more frequently. The client should not take sumatriptan or any other headache medication for more than 10 days per month. Call a doctor if there is a need to take sumatriptan to treat more than four headaches in a 1-month period. NCLEXRN-09-031 Question Tag: meningitis Question Category: Physiological Integrity, Physiological Adaptation The client with suspected meningitis is admitted to the unit. The doctor is performing an assessment to determine meningeal irritation and spinal nerve root inflammation. A positive Kernig’s sign is charted if the nurse notes: A. Pain on flexion of the hip and knee B. Nuchal rigidity on flexion of the neck C. Pain when the head is turned to the left side D. Dizziness when changing positions Correct Answer: A. Pain on flexion of the hip and knee Kernig’s sign is positive if pain occurs on flexion of the hip and knee. Kernig’s sign is one of the physically demonstrable symptoms of meningitis. Severe stiffness of the hamstrings causes an inability to straighten the leg when the hip is flexed to 90 degrees. Option B: The Brudzinski reflex is positive if pain occurs on flexion of the head and neck onto the chest. Brudzinski’s sign is one of the physically demonstrable symptoms of meningitis. Severe neck stiffness causes a patient’s hips and knees to flex when the neck is flexed. Brudzinski’s sign is used to diagnose meningitis. Option C: A tension headache may cause pain on the left side and behind the eyes, and may be linked to stress. Tension headaches account for up to 42 percent of headaches worldwide. They may occur on one side so could be the cause of a headache on the left side. Option D: Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you’re spinning or that the inside of your head is spinning. BPPV causes brief episodes of mild to intense dizziness. It is usually triggered by specific changes in the head’s position. This might occur when one tips their head up or down, when the client lies down, or when he turns over or sits up in bed. NCLEXRN-09-032 Question Tag: Alzheimer’s disease Question Category: Psychosocial Integrity The client with Alzheimer’s disease is being assisted with activities of daily living when the nurse notes that the client uses her toothbrush to brush her hair. The nurse is aware that the client is exhibiting: A. Agnosia B. Apraxia C. Anomia D. Aphasia Correct Answer: A. Agnosia Agnosia is the term used to describe the loss of the ability to recognize what objects are and what they are used for. For instance, a person with agnosia might try to use a fork instead of a spoon, a shoe instead of a cup or a knife instead of a pencil etc. With regard to people, this might involve failing to recognize who people are, not due to memory loss but rather as a result of the brain not working out the identity of a person on the basis of the information supplied by the eyes. Option B: Apraxia is the term used to describe the failure to carry out voluntary and purposeful movements notwithstanding the fact that muscular power, sensibility, and coordination are intact. In everyday terms, this might involve the inability to tie shoelaces, turn a tap on, fasten buttons or switch on a radio. Option C: Aphasia is the term used to describe a difficulty or loss of the ability to speak or understand spoken, written or sign language as a result of damage to the corresponding nervous center. This can become apparent in a number of ways. It might involve exchanging a word which is linked by meaning (e.g. time instead of clock), using the wrong word but one which sounds alike (e.g. boat instead of coat) or using a totally different word with no apparent connection. When accompanied by echolalia (the involuntary repetition of words or phrases spoken by another person) and the constant repetition of a word or phrase, the result can be a form of speech which is difficult for others to understand or a kind of jargon. Option D: Anomia is a form of aphasia in which the patient is unable to recall the names of everyday objects. Anomic aphasia is a language disorder that leads to trouble naming objects when speaking and writing. Brain damage caused by stroke, traumatic injury, or tumors can lead to anomic aphasia. NCLEXRN-09-033 Question Tag: dementia Question Category: Psychosocial Integrity The client with dementia is experiencing confusion late in the afternoon and before bedtime. The nurse is aware that the client is experiencing what is known as: A. Chronic fatigue syndrome B. Normal aging C. Sundowning D. Delusions Correct Answer: C. Sundowning Increased confusion at night is known as “sundowning” syndrome. This increased confusion occurs when the sun begins to set and continues during the night. The term “sundowning” refers to a state of confusion occurring in the late afternoon and spanning into the night. Sundowning can cause a variety of behaviors, such as confusion, anxiety, aggression or ignoring directions. Sundowning can also lead to pacing or wandering. Option A: Fatigue is not necessarily present. Sundowning isn’t a disease, but a group of symptoms that occur at a specific time of the day that may affect people with dementia, such as Alzheimer’s disease. The exact cause of this behavior is unknown. Option B: Increased confusion at night is not part of normal aging. Some research suggests that a low dose of melatonin — a naturally occurring hormone that induces sleepiness — alone or in combination with exposure to bright light during the day may help ease sundowning. Option D: A delusion is a firm, fixed belief. Delusions are defined as fixed, false beliefs that conflict with reality. Despite contrary evidence, a person in a delusional state can’t let go of their convictions. Delusions are often reinforced by the misinterpretation of events. Many delusions also involve some level of paranoia. For example, someone might contend that the government is controlling our every move via radio waves despite evidence to the contrary. NCLEXRN-09-034 Question Tag: confusion Question Category: Psychosocial Integrity The client with confusion says to the nurse, “I haven’t had anything to eat all day long. When are they going to bring breakfast?” The nurse saw the client in the day room eating breakfast with other clients 30 minutes before this conversation. Which response would be best for the nurse to make? A. “You know you had breakfast 30 minutes ago.” B. “I am so sorry that they didn’t get you breakfast. I’ll report it to the charge nurse.” C. “I’ll get you some juice and toast. Would you like something else?” D. “You will have to wait a while; lunch will be here in a little while.” Correct Answer: C. “I’ll get you some juice and toast. Would you like something else?” The client who is confused might forget that he ate earlier. Don’t argue with the client. Simply get him something to eat that will satisfy him until lunch. Avoid challenging illogical thinking. Challenges to the patient’s thinking can be perceived as threatening and result in a defensive reaction. Maintain normal fluid and electrolyte balance; establish/maintain normal nutrition, body temperature, oxygenation (if patients experience low oxygen saturation treat with supplemental oxygen), blood glucose levels, blood pressure. Option A: Orient patient to surroundings, staff, necessary activities as needed. Present reality concisely and briefly. Avoid challenging illogical thinking—defensive reactions may result. Increased orientation ensures a greater degree of safety for the patient. Option B: This statement is validating the delusion. Encourage family/SO(s) to participate in reorientation as well as providing ongoing input (e.g., current news and family happenings). The confused patient may not completely understand what is happening. The presence of family and significant others may enhance the patient’s level of comfort. Option D: Communicate the patient’s status, cognition, and behavioral manifestations to all necessary providers. Recognize that a patient’s fluctuating cognition and behavior is a hallmark for delirium and is not to be construed as a patient preference for caregivers. NCLEXRN-09-035 Question Tag: Alzheimer’s disease Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The doctor has prescribed Exelon (rivastigmine) for the client with Alzheimer’s disease. Which side effect is most often associated with this drug? A. Urinary incontinence B. Headaches C. Confusion D. Nausea Correct Answer: D. Nausea Nausea and gastrointestinal upset are very common in clients taking acetylcholinesterase inhibitors such as Exelon. Other side effects include liver toxicity, dizziness, unsteadiness, and clumsiness. The main adverse effects associated with the use of rivastigmine are gastrointestinal. The primary symptoms are nausea and vomiting. These acute effects primarily occur during the initial dose-escalation phase of therapy upward dose titration of the drug to achieve a therapeutic dose. These events can be minimized by using a slow titration schedule and taking the medication with food if prescribing an oral formulation. Option A: Toxicity to the drug, while rare, should be carefully monitored. Common manifestations of toxicity include the presence of severe gastrointestinal reactions, allergic cutaneous reactions, as well as central nervous system effects. Classic manifestations of a patient in crisis can be remembered by the mnemonic DUMBELS – diarrhea, urination, miosis, bradycardia, excitability, lacrimation, salivation/excessive sweating prior to treatment. Option B: The client might already be experiencing urinary incontinence or headaches, but they are not necessarily associated. Patients that are experiencing a cholinergic crisis should have atropine followed by pralidoxime to reverse the anticholinergic effects of rivastigmine. While the usual treatment of the crisis involves giving atropine before pralidoxime, a case study done in 2009 showed a successful reversal of cholinergic crisis with just pralidoxime without atropine pretreatment. Option C: The client with Alzheimer’s disease is already confused. With its approval by the FDA, rivastigmine is indicated to treat mild to moderate dementia of the Alzheimer’s type. Its indications also include the treatment of mild to moderate dementia that is associated with Parkinson disease. NCLEXRN-09-036 Question Tag: labor Question Category: Physiological Integrity, Reduction of Risk Potential A client is admitted to the labor and delivery unit in active labor. During examination, the nurse notes a papular lesion on the perineum. Which initial action is most appropriate? A. Document the finding B. Report the finding to the doctor C. Prepare the client for a C-section D. Continue primary care as prescribed Correct Answer: B. Report the finding to the doctor Any lesion should be reported to the doctor. This can indicate a herpes lesion. Clients with open lesions related to herpes are delivered by Cesarean section because there is a possibility of transmission of the infection to the fetus with direct contact to lesions. During pregnancy there is a higher risk of perinatal transmission with primary HSV infection than with recurrent infection. If a primary HSV outbreak is diagnosed in pregnancy, oral antiviral treatment may be administered to help reduce the duration and severity of symptoms and viral shedding. Option A: It is not enough to document the finding. Viral or serologic testing should be performed to confirm suspected HSV infections; the basic groups of tests used are viral and antibody detection techniques. For viral detection, the primary testing techniques are viral culture and HSV antigen detection by polymerase chain reaction. Option C: The physician must make the decision to perform a C-section. Cesarean delivery is recommended to prevent perinatal HSV transmission in women with active genital lesions or prodromal symptoms, but it is not recommended for women with HSV lesions found only on nongenital areas, such as the back, thigh, or buttock. Option D: It is not enough to continue primary care. Antiviral agents commonly used to treat HSV infections are acyclovir (Zovirax), famciclovir (Famvir), and valacyclovir (Valtrex), which are all U.S. Food and Drug Administration pregnancy category B medications. For patients with more severe HSV infection, oral treatment can be used for more than 10 days if the lesions have not healed completely. NCLEXRN-09-037 Question Tag: human papillomavirus Question Category: Physiological Integrity, Physiological Adaptation A client with a diagnosis of HPV is at risk for which of the following? A. Hodgkin’s lymphoma B. Cervical cancer C. Multiple myeloma D. Ovarian cancer Correct Answer: B. Cervical cancer The client with HPV is at higher risk for cervical and vaginal cancer related to this STI. The Human Papillomavirus (HPV) is the initiating force behind multiple epithelial lesions and cancers, predominantly of cutaneous and mucosal surfaces. Today, HPV has been implicated as a cause of laryngeal, oral, lung and anogenital cancer. Subtypes 6 and 11 are low risk and usually present with the formation of condylomata and low-grade precancerous lesions. HPV subtypes 16 and 18 are high risk and are responsible for high-grade intraepithelial lesions that progress to malignancies. ADVERTISEMENTS Option A: It is important to understand that HPV alone does not cause cancer but requires triggers like smoking, folate deficiency, exposure to UV light, immunosuppression and pregnancy. Long term follow up is essential as recurrence of warts is common. In addition, all treatments for warts have side effects that need to be monitored. Option C: The prognosis after an HPV infection is good but recurrences are common. Even though there are many treatments for warts, none works well and most patients require repeated treatments. The HPV infection can also result in vulvar intraepithelial dysplasia, cervical dysplasia, and cervical cancer. Option D: Some women remain at high risk for developing vaginal and anal cancer. The risk of malignant transformation is highest in immunocompromised individuals. Finally, when a patient has been diagnosed with HPV infection, there is a 5-20% risk of also having other STDs like gonorrhea and/or chlamydia. NCLEXRN-09-038 Question Tag: lesion, vulva Question Category: Physiological integrity, Physiological Adaptation During the initial interview, the client reports that she has a lesion on the perineum. Further investigation reveals a small blister on the vulva that is painful to touch. The nurse is aware that the most likely source of the lesion is: A. Syphilis B. Herpes C. Gonorrhea D. Condylomata Correct Answer: B. Herpes A lesion that is painful is most likely a herpetic lesion. Herpes genitalis can be caused by the herpes simplex virus type 1 or type 2 and manifests as either a primary or recurrent infection. Most commonly, viral replication occurs in epithelial tissue and establishes dormancy in sensory neurons, reactivating periodically as localized recurrent lesions. It remains one of the most common sexually transmitted infections (STI) but continues to be underestimated, given the vague presentation of its symptoms. Option A: A chancre lesion associated with syphilis is not painful. The classic primary syphilis presentation is a solitary non-tender genital chancre in response to invasion by the T. pallidum. However, patients can have multiple non-genital chancres, such as digits, nipples, tonsils, and oral mucosa. These lesions can occur at any site of direct contact with the infected lesion and are accompanied by tender or nontender lymphadenopathy. Option C: Gonorrhea does not present as a lesion, but is exhibited by a yellow discharge. Although many females, more than 50%, will not manifest symptoms of their gonococcal cervix infections, most males, more than 90%, will manifest urogenital gonorrhea symptomatically. The most common clinical manifestations of gonococcal disease in males include penile purulent discharge, dysuria, and testicular discomfort. Option D: Condylomata lesions are painless warts, so answer D is incorrect. Patients will generally be concerned about the appearance of the lesions, as they often cause psychological and psychosexual distress. Condyloma acuminata may also be found incidentally during routine female gynecological examinations. NCLEXRN-09-039 Question Tag: treponema pallidum Question Category: Physiological Integrity, Physiological Adaptation A client visiting a family planning clinic is suspected of having an STI. The best diagnostic test for treponema pallidum is: A. Venereal Disease Research Lab (VDRL) B. Rapid plasma reagin (RPR) C. Fluorescent treponemal antibody (FTA) D. Thayer-Martin culture (TMC) Correct Answer: C. Fluorescent treponemal antibody (FTA) Fluorescent treponemal antibody (FTA) is the test for treponema pallidum. The fluorescent treponemal antibody absorption (FTA-ABS) test is a blood test that checks for the presence of antibodies to Treponema pallidum bacteria. These bacteria cause syphilis. Syphilis is a sexually transmitted infection (STI) that’s spread through direct contact with syphilitic sores. Option A: The venereal disease research laboratory (VDRL) test is designed to assess whether you have syphilis, a sexually transmitted infection (STI). Syphilis is caused by the bacterium Treponema pallidum. The bacterium infects by penetrating into the lining of the mouth or genital area. The VDRL test doesn’t look for the bacteria that cause syphilis. Instead, it checks for the antibodies your body makes in response to antigens produced by cells damaged by the bacteria. Antibodies are a type of protein produced by your immune system to fight off invaders like bacteria or toxins. Testing for these antibodies can let your doctors know whether you have syphilis. Option B: The rapid plasma reagin (RPR) test is a blood test that looks for antibodies to syphilis. Syphilis is a sexually transmitted infection (STI) that first causes symptoms seen with many other illnesses. Early symptoms include rash, fever, swollen glands, muscle aches, and sore throat. The RPR test looks for antibodies that react to syphilis in the blood. This means the test doesn’t detect the actual bacteria that cause syphilis. Instead, it looks for antibodies against substances given off by cells that have been harmed by the bacteria. Option D: The Thayer-Martin culture is done for gonorrhea. It is used for culturing and primarily isolating pathogenic Neisseria bacteria, including Neisseria gonorrhoeae and Neisseria meningitidis, as the medium inhibits the growth of most other microorganisms. NCLEXRN-09-040 Question Tag: HELLP syndrome Question Category: Physiological Integrity, Reduction of Risk Potential A 15-year-old primigravida is admitted with a tentative diagnosis of HELLP syndrome. Which laboratory finding is associated with HELLP syndrome? A. Elevated blood glucose B. Elevated platelet count C. Elevated creatinine clearance D. Elevated hepatic enzymes Correct Answer: D. Elevated hepatic enzymes The criteria for HELLP is hemolysis, elevated liver enzymes, and low platelet count. The syndrome of hemolysis, elevated liver enzymes, and low platelets, otherwise referred to as HELLP syndrome, has historically been classified as a complication or progression of severe preeclampsia. Genetic analysis of the inheritability of predisposition for preeclampsia and/or HELLP syndrome in pregnancy has also been explored. Results show both genetic and immunological factors that play a role in pathogenesis. Option A: An elevated blood glucose level is not associated with HELLP. One of the features of HELLP syndrome is microangiopathic hemolytic anemia. Schistocytes or helmet cells, present on a peripheral blood smear is diagnostic of microangiopathic hemolytic anemia, making peripheral smears useful in the workup for HELLP syndrome. Option B: Platelets are decreased, not elevated, in HELLP syndrome. The coagulation cascade is activated by adhesion of platelets on the activated and damaged endothelium. Platelets release thromboxane A and serotonin, causing vasospasm, platelet aggregation, and further endothelial damage. The cascade only terminates with the delivery of the fetus. This causes the usage of platelets and hence, thrombocytopenia. Option C: The creatinine levels are elevated in renal disease and are not associated with HELLP syndrome. In the liver, intravascular fibrin deposits give rise to sinusoidal obstruction, intrahepatic vascular congestion, increased hepatic pressures leading to hepatic necrosis. This may eventually result in intraparenchymal or subcapsular hemorrhage and capsular rupture. NCLEXRN-09-041 Question Tag: preeclampsia Question Category: Physiological Integrity, Reduction of Risk Potential The nurse is assessing the deep tendon reflexes of a client with preeclampsia. Which method is used to elicit the biceps reflex? A. The nurse places her thumb on the muscle inset in the antecubital space and taps the thumb briskly with the reflex hammer. B. The nurse loosely suspends the client’s arm in an open hand while tapping the back of the client’s elbow. C. The nurse instructs the client to dangle her legs as the nurse strikes the area below the patella with the blunt side of the reflex hammer. D. The nurse instructs the client to place her arms loosely at her side as the nurse strikes the muscle insert just above the wrist. Correct Answer: A. The nurse places her thumb on the muscle inset in the antecubital space and taps the thumb briskly with the reflex hammer. The biceps reflex is elicited by placing your thumb on the biceps tendon and striking the thumb with the reflex hammer and observing the arm movement. Repeat and compare with the other arm. Using a reflex hammer, deep tendon reflexes are elicited in all 4 extremities. Note the extent or power of the reflex, both visually and by palpation of the tendon or muscle in question. Option B: This elicits the triceps reflex. The triceps reflex is measured by striking the triceps tendon directly with the hammer while holding the patient’s arm with your other hand. Repeat and compare to the other arm. The triceps reflex is mediated by the C6 and C7 nerve roots, predominantly by C7. Option C: This elicits the patellar reflex. The patellar reflex is a deep tendon reflex, mediated by the spinal nerves from the levels L2, L3, and L4 in the spinal cord, predominantly in the root L4. The patellar reflex test is performed to determine the integrity of the neurological function, which is accomplished by hitting the patellar tendon below the knee cap with a test hammer Option D: This elicits the radial nerve. For the testing of the brachioradialis reflex, the examiner places the patient in a seated position. From there, the clinician uses his or her forearm to support the patient’s forearm in a slightly pronated position. The physician supports the patient’s forearm rather than asking the patient to maintain the position to achieve relaxation of the muscle. Once in position, the physician delivers a series of quick hits to the area of the styloid process of the radius at the point of brachioradialis insertion. NCLEXRN-09-042 Question Tag: diabetes, primigravida Question Category: Safe and Effective Care Environment,, Safety and Infection Control A primigravida with diabetes is admitted to the labor and delivery unit at 34 weeks gestation. Which doctor’s order should the nurse question? A. Magnesium sulfate 4gm (25%) IV B. Brethine 10 mcg IV C. Stadol 1 mg IV push every 4 hours as needed prn for pain D. Ancef 2gm IVPB every 6 hours Correct Answer: B. Brethine 10 mcg IV Brethine is used cautiously because it raises blood glucose levels. Terbutaline can cause a temporary increase in the baby’s heart rate and blood sugar levels. These side effects usually aren’t serious and are easy to treat after delivery if they occur. There are concerns about long term use of this drug because the incidence of danger to the baby increases. Option A: Magnesium sulfate is indicated to prevent seizures associated with pre-eclampsia, and for control of seizures with eclampsia. Magnesium levels must be monitored frequently by checking serum levels every 6 to 8 hours or clinically by following patellar reflexes or urinary output. If serum concentration levels are low, a proper dose of magnesium sulfate can be given parenterally to replete low serum concentrations with recommended follow up laboratory testing. Option C: Stadol is indicated for labor pain in full-term (37 weeks gestation or more) women without fetal distress in early labor. This medication is used to treat moderate to severe pain, including pain from surgery, muscle pain, and migraine headaches. Butorphanol is an opioid pain reliever similar to morphine. It acts on certain centers in the brain to give pain relief. Option D: Ancef is generally acceptable for pregnant women. Controlled studies in pregnant women show no evidence of fetal risk. Cefazolin is an antibiotic used to treat a wide variety of bacterial infections. It may also be used before and during certain surgeries to help prevent infection. This medication is known as a cephalosporin antibiotic. It works by stopping the growth of bacteria. NCLEXRN-09-043 Question Tag: amniocentesis Question Category: Physiological Integrity, Reduction of Risk Potential A diabetic multigravida is scheduled for an amniocentesis at 32 weeks gestation to determine the L/S ratio and phosphatidylglycerol level. The L/S ratio is 1:1 and the presence of phosphatidylglycerol is noted. The nurse’s assessment of this data is: A. The infant is at low risk for congenital anomalies. B. The infant is at high risk for intrauterine growth retardation. C. The infant is at high risk for respiratory distress syndrome. D. The infant is at high risk for birth trauma. Correct Answer: C. The infant is at high risk for respiratory distress syndrome. When the L/S ratio reaches 2:1, the lungs are considered to be mature. The Lecithin-to-Sphingomyelin Ratio (L/S ratio) is one of several methods for clinicians to assess fetal lung maturation. This biochemical test was first introduced in the 1970s, where a sample of amniotic fluid was collected via amniocentesis to determine the risk of the neonate developing respiratory distress syndrome (RDS). The sample was then evaluated, utilizing thin-layer chromatography to assess the size of lecithin relative to sphingomyelin. Option A: The L/S ratio does not indicate congenital anomalies. Based on new guidelines, these indications no longer warrant testing the L/S ratio or performing other fetal lung testing modalities. One possible exception relates to inaccurate dating of the gestational age. If there is poor dating of the pregnancy and the delivery is to be planned between 32 to 39 weeks gestation, the clinician may consider testing for fetal lung maturity. Option B: The infant is not at risk for intrauterine growth retardation. The main focus of testing the L/S ratio is to determine fetal lung maturity in an effort to decrease the risk of delivering a neonate with respiratory distress syndrome (RDS). RDS predominantly occurs in preterm infants less than 39 weeks gestation with increased risk with lesser gestational age. Option D: The infant will most likely be small for gestational age and will not be at risk for birth trauma. The normal L/S ratio is 2.0 to 2.5 and is significant for appropriate fetal lung development. An L/S ratio of less than 2.0 is significant for immature fetal lung development. For patients who have poorly controlled diabetes, there was a discussion for the L/S ratio to be 3.0 due to elevated maternal glucose impacting the maturity of the developing fetal lungs. NCLEXRN-09-044 Question Tag: diabetes Question Category: Health Promotion and Maintenance Which observation in the newborn of a diabetic mother would require immediate nursing intervention? A. Crying B. Wakefulness C. Jitteriness D. Yawning Correct Answer: C. Jitteriness Jitteriness is a sign of seizure in the neonate. For infants presenting with clinical signs compatible with hypoglycemia, like apnoea, hypotonia, jitteriness, apathy, hypothermia, tremors and seizures, treatment must ensure that blood glucose levels remain above 0.45 g/L (2.5 mmol/L). An IV bolus dose of glucose (150-200 mg/kg) should be administered urgently, followed by a constant rate infusion. Option A: It’s normal for a baby to cry for 2–3 hours a day for the first 6 weeks. During the first 3 months of life, they cry more than at any other time. New parents often are low on sleep and getting used to life with their little one. Option B: Generally, newborns sleep a total of about 8 to 9 hours in the daytime and a total of about 8 hours at night. But because they have a small stomach, they must wake every few hours to eat. Most babies don’t start sleeping through the night (6 to 8 hours) until at least 3 months of age. But this can vary a lot. Some babies don’t sleep through the night until closer to 1 year. Option D: It is also common for newborns to hiccup, sneeze, yawn, spit up, burp, and gurgle. Sometimes newborns cry for no reason at all. If this happens, try comforting the baby by rocking, singing, talking softly, or wrapping him or her in a blanket. NCLEXRN-09-045 Question Tag: magnesium sulfate Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The nurse caring for a client receiving intravenous magnesium sulfate must closely observe for side effects associated with drug therapy. An expected side effect of magnesium sulfate is: A. Decreased urinary output B. Hypersomnolence C. Absence of knee jerk reflex D. Decreased respiratory rate Correct Answer: B. Hypersomnolence The client is expected to become sleepy, have hot flashes, and be lethargic. Patients most commonly complain of minor facial flushing and warmth with the administration; however, symptoms typically resolve spontaneously. In patients with neuromuscular disease, such as in myasthenia gravis, the neuromuscular function may become worse at lower concentrations of medication. Option A: Magnesium levels must be monitored frequently by checking serum levels every 6 to 8 hours or clinically by following patellar reflexes or urinary output. If serum concentration levels are low, a proper dose of magnesium sulfate can be given parenterally to replete low serum concentrations with recommended follow up laboratory testing. Option C: If the patient is on a continuous magnesium sulfate infusion, serum levels must be accounted for as symptoms related to hypermagnesemia may become clinically evident. At supratherapeutic serum concentrations, absent reflexes, abnormal cardiac conduction, and muscle weakness may occur. Option D: Decreased respirations indicate a magnesium sulfate toxicity. If patients exhibit signs and symptoms of hypermagnesemia, the recommendation is to discontinue magnesium sulfate products immediately. If the patient consumed magnesium sulfate orally, then the use of magnesium-free enemas or cathartics can be useful in removing excess magnesium from the GI tract. NCLEXRN-09-046 Question Tag: epidural anesthesia Question Category: Physiological Integrity, Reduction of Risk Potential The client has elected to have epidural anesthesia to relieve labor pain. If the client experiences hypotension, the nurse would: A. Place her in Trendelenburg position B. Decrease the rate of IV infusion C. Administer oxygen per nasal cannula D. Increase the rate of the IV infusion Correct Answer: D. Increase the rate of the IV infusion If the client experiences hypotension after an injection of epidural anesthetic, the nurse should turn her to the left side, apply oxygen by mask, and speed the IV infusion. If the blood pressure does not return to normal, the physician should be contacted. Epinephrine should be kept for emergency administration. Option A: Placing the client in Trendelenburg position (head down) will allow the anesthesia to move up above the respiratory center, thereby decreasing the diaphragm’s ability to move up and down and ventilate the client. Option B: The IV rate should be increased, not decreased. Monitoring the patient’s hemodynamic status during the procedure is very important. The minimum monitors required are pulse oximeter for pulse and oxygen saturation as well as blood pressure cuff and continuous EKG to assess cardiovascular status. Option C: The oxygen should be applied by mask, not cannula. Epidural anesthesia is achievable using either the classic epidural, the combined spinal-epidural (CSE) technique, or dural puncture epidural (DPE). CSE and DPE include an additional step consisting of delivering a spinal dose of LA and co adjuvants (CSE) or only puncturing the dura mater (DPE) using a spinal needle. NCLEXRN-09-047 Question Tag: cancer of the pancreas Question Category: Physiologic Integrity, Physiological Adaptation A client has cancer of the pancreas. The nurse should be most concerned about which nursing diagnosis? A. Alteration in nutrition B. Alteration in bowel elimination C. Alteration in skin integrity D. Ineffective individual coping Correct Answer: A. Alteration in nutrition Cancer of the pancreas frequently leads to severe nausea and vomiting and altered nutrition. Weight loss occurs in about 90% of patients. Abdominal pain occurs in about 75% of patients. Weakness, pruritus from bile salts in the skin, anorexia, palpable, non-tender, distended gallbladder, acholic stools, and dark urine. Option B: Patients with adenocarcinoma of pancreas typically present with painless jaundice (70%) usually due to obstruction of the common bile duct from the pancreatic head tumor. Lab findings will include elevation in liver function tests, direct and total bilirubin levels, elevated amylase and lipase, and elevated pancreatic tumor markers (CA 19-9 and CEA). Option C: Neoadjuvant first approach in resectable pancreatic adenocarcinoma is implemented more and more frequently at high-volume centers nationwide and internationally. The rationale behind neoadjuvant first approach is that the patient is in their best shape to receive chemotherapy and at best odds of completing chemotherapy for 4-6 months. In addition, tissue is thought to be still well-oxygenated having not gone through a large procedure such as the Whipple. Option D: For patients with metastatic, stage IV, pancreatic cancer, discussions with the patient regarding treatment are essential. One can receive chemotherapy. However, the life prolongation will be at best months, yet affect the toxicity and effects of the chemotherapy. It is important to keep nutrition on the forefront of the patient’s care as nutrition can affect wound healing. NCLEXRN-09-048 Question Tag: ascites Question Category: Physiological Integrity, Reduction of Risk Potential The nurse is caring for a client with ascites. Which is the best method to use for determining early ascites? A. Inspection of the abdomen for enlargement B. Bimanual palpation for hepatomegaly C. Daily measurement of abdominal girth D. Assessment for a fluid wave Correct Answer: C. Daily measurement of abdominal girth Measuring with a paper tape measure and marking the area that is measured is the most objective method of estimating ascites. Ascites is the pathologic accumulation of fluid within the peritoneal cavity. It is the most common complication of cirrhosis and occurs in about 50% of the patients with decompensated cirrhosis in 10 years. The development of ascites denotes the transition from compensated to decompensated cirrhosis. Option A: The initial tests that should be performed on the ascitic fluid include a blood cell count, with both a total nucleated cell count and polymorphonuclear neutrophils (PMN) count, and a bacterial culture by bedside inoculation of blood culture bottles. Ascitic fluid protein and albumin are measured simultaneously with the serum albumin level to calculate the serum-ascites albumin gradient (SAAG). Option B: Palpation of the liver will not determine the amount of ascites. The first abnormality that develops is portal hypertension in the case of cirrhosis. Portal pressure increases above a critical threshold and circulating nitric oxide levels increase, leading to vasodilation. As the state of vasodilatation becomes worse, the plasma levels of vasoconstrictor sodium-retentive hormones elevate, renal function declines, and ascitic fluid forms, resulting in hepatic decompensation. Option D: Inspecting and checking for fluid waves are more subjective. Patients typically report progressive abdominal distension that may be painless or associated with abdominal discomfort, weight gain, early satiety, shortness of breath, and dyspnea resulting from fluid accumulation and increased abdominal pressure. Symptoms such as fever, abdominal tenderness, and confusion can be seen in spontaneous bacterial peritonitis. NCLEXRN-09-049 Question Tag: vehicle accident Question Category: Physiological Integrity, Physiological Adaptation The client arrives in the emergency department after a motor vehicle accident. Nursing assessment findings include BP 80/34, pulse rate 120, and respirations 20. Which is the client’s most appropriate priority nursing diagnosis? A. Alteration in cerebral tissue perfusion B. Fluid volume deficit C. Ineffective airway clearance D. Alteration in sensory perception Correct Answer: B. Fluid volume deficit The vital signs indicate hypovolemic shock. Monitor and document vital signs especially BP and HR. Decrease in circulating blood volume can cause hypotension and tachycardia. Alteration in HR is a compensatory mechanism to maintain cardiac output. Usually, the pulse is weak and may be irregular if electrolyte imbalance also occurs. Hypotension is evident in hypovolemia. Option A: The oxygen and nutrients subsequently diffuse from the blood into the interstitial fluid and then into the body cells. Insufficient arterial blood flow causes decreased nutrition and oxygenation at the cellular level. Decreased tissue perfusion can be temporary, with few or minimal consequences to the health of the patient, or it can be more acute or protracted, with potentially destructive effects on the patient. Option C: Ineffective airway clearance is the inability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. Appropriate management is vital to prevent potentially life-threatening hypovolemic shock. Older patients are more likely to develop fluid imbalances. The goals of management are to treat the underlying disorder and return the extracellular fluid compartment to normal, to restore fluid volume, and to correct any electrolyte imbalances. Option D: Alterations sensory / perceptual (visual, auditory, kinesthetic, gustatory, tactile, olfactory) State in which an individual experiences a change in the amount or type of stimuli received, accompanied by a decrease towards exaggeration or disorder of the response to such stimuli. NCLEXRN-09-050 Question Tag: osteogenesis imperfecta Question Category: Safe and Effective Care Environment,, Safety and Infection Control The home health nurse is visiting an 18-year-old with osteogenesis imperfecta. Which information obtained on the visit would cause the most concern? The client: A. Likes to play football B. Drinks several carbonated drinks per day C. Has two sisters with sickle cell tract D. Is taking acetaminophen to control pain Correct Answer: A. Likes to play football The client with osteogenesis imperfecta is at risk for pathological fractures and is likely to experience these fractures if he participates in contact sports. The client might experience symptoms of hypoxia if he becomes dehydrated or deoxygenated; extreme exercise, especially in warm weather, can exacerbate the condition. Option B: Osteogenesis imperfecta (OI) is a genetic disorder of connective tissues caused by an abnormality in the synthesis or processing of type I collagen. It is also called brittle bone disease. It is characterized by an increased susceptibility to bone fractures and decreased bone density. Other manifestations include blue sclerae, dentinogenesis imperfecta, short stature, as well as deafness in adulthood. There are also reports of valvular insufficiencies and aortic root dilation. Option C: Osteogenesis imperfecta is a rare genetic disease. In the majority of cases, it occurs secondary to mutations in the COL1A1 and COL1A2 genes. More recently, there has been the identification of diverse mutations related to OI. Option D: Milder manifestations include generalized laxity, easy bruising, hernias, and excess sweating. Clinical manifestations range from mild with a nearly asymptomatic form to most severe forms (involving infants presenting with crumpled ribs, fragile cranium, and long bone fractures incompatible with life) resulting in perinatal mortality. Questions and rationale from Nurseslabs.com Feel free to print or share and link back to us! For more practice questions, please visit our Nursing Test Bank [https://nurseslabs.com/nursing-test-bank] NCLEXRN-09-051 Question Tag: white blood cell count Question Category: Physiological Integrity, Reduction of Risk Potential The nurse working the organ transplant unit is caring for a client with a decreased white blood cell count. During evening visitation, a visitor brings a basket of fruit. What action should the nurse take? A. Allow the client to keep the fruit B. Place the fruit next to the bed for easy access by the client C. Offer to wash the fruit for the client D. Tell the family members to take the fruit home Correct Answer: D. Tell the family members to take the fruit home The client with neutropenia should not have fresh fruit because it should be peeled and/or cooked before eating. He should also not eat foods grown on or in the ground or eat from the salad bar. The nurse should remove potted or cut flowers from the room as well. Any source of bacteria should be eliminated, if possible. Option A: Educate clients and SO about appropriate methods for cleaning, disinfecting, and sterilizing items. Knowledge of ways to reduce or eliminate germs reduces the likelihood of transmission. Option B: Perform measures to break the chain of infection and prevent infection. Assist clients in carrying out appropriate skin and oral hygiene. Instruct clients to perform hand hygiene when handling food or eating. Option C: Place the patient in protective isolation if the patient is at high risk of infection. Protective isolation is set when the WBC indicates neutropenia. Wear personal protective equipment (PPE) properly. NCLEXRN-09-052 Question Tag: laryngectomy Question Category: Physiological Integrity, Physiological Adaptation The nurse is caring for the client following a laryngectomy when suddenly the client becomes unresponsive and pale, with a BP of 90/40 systolic. The initial nurse’s action should be to: A. Place the client in Trendelenburg position B. Increase the infusion of Dextrose in normal saline C. Administer atropine intravenously D. Move the emergency cart to the bedside Correct Answer: B. Increase the infusion of Dextrose in normal saline Dextrose in normal saline is indicated as a source of water, electrolytes, and calories. Early complications after total laryngectomy are bleeding, postoperative edema, and airway compromise, these, especially in the immediate postoperative, should be carefully monitored. Option A: In clients who have not had surgery to the face or neck, however, in this situation, this could further interfere with the airway. Increasing the infusion and placing the client in supine position would be better. Option C: Administration of atropine IV is not necessary at this time and could cause hyponatremia and further hypotension. Administration of corticosteroids is recommended to minimize postoperative edema and airway compromise, hematoma or seroma, that should be prompt surgically evacuated, wound infection related to the perioperative exposure of the wound to bacteria, it could be minimized using a broad-spectrum antibiotic coverage and pharyngocutaneous fistula; total laryngectomy patients are at risk for pharyngeal suture line dehiscence with a resultant pharyngocutaneous fistula. Option D: Moving the emergency cart at the bedside is not necessary at this time. The primary goal for the treatment of laryngeal cancer is the control of the disease. Preservation of speech, swallowing functions, and avoidance of the tracheostomy are secondary goals. Traditionally the treatment of laryngeal carcinomas has been radiotherapy or surgery or a combination of both. NCLEXRN-09-053 Question Tag: chest tube Question Category: Physiological Integrity, Reduction of Risk Potential The client admitted 2 days earlier that a lung resection accidentally pulls out the chest tube. Which action by the nurse indicates understanding of the management of chest tubes? A. Order a chest x-ray B. Reinsert the tube C. Cover the insertion site with a Vaseline gauze D. Call the doctor Correct Answer: C. Cover the insertion site with a Vaseline gauze If the client pulls the chest tube out of the chest, the nurse’s first action should be to cover the insertion site with an occlusive dressing. Afterward, the nurse should call the doctor, who will order a chest x-ray and possibly reinsert the tube. A chest tube may be inserted at the bedside, in the procedure room, or in the surgical suite. Health care providers often assist physicians in the insertion and removal of a closed chest tube drainage system. Option A: A chest tube falling out is an emergency. Immediately apply pressure to the chest tube insertion site and apply sterile gauze or place a sterile Jelonet gauze and dry dressing over the insertion site and ensure tight seal. Apply dressing when the patient exhales. If a patient goes into respiratory distress, call a code. Notify primary health care providers to reinsert new chest tube drainage systems. Option B: A chest tube drainage system disconnecting from the chest tube inside the patient is an emergency. Immediately clamp the tube and place the end of the chest tube in sterile water or NS. The two ends will need to be swabbed with alcohol and reconnected. Option D: After initial insertion of a chest tube drainage system, assess the patient every 15 minutes to 1 hour. Once the patient is stable, and depending on the condition of the patient and the amount of drainage, monitoring may be less frequent. If the patient is stable (vital signs within normal limits; drainage amount, colour, or consistency is within normal limits; the patient is not experiencing any respiratory distress or pain), assessment may be completed every 4 hours. Always follow hospital policy for frequency of monitoring a patient with a chest tube. NCLEXRN-09-054 Question Tag: sodium warfarin Question Category: Physiological Integrity, Reduction of Risk Potential A client being treated with sodium warfarin has a Protime of 120 seconds. Which intervention would be most important to include in the nursing care plan? A. Assess for signs of abnormal bleeding B. Anticipate an increase in the Coumadin dosage C. Instruct the client regarding the drug therapy D. Increase the frequency of neurological assessments Correct Answer: A. Assess for signs of abnormal bleeding The normal Protime is 12–20 seconds. A Protime of 120 seconds indicates an extremely prolonged Protime and can result in a spontaneous bleeding episode. Patients receiving treatment with warfarin should have close monitoring to ensure the safety and efficacy of the medication. Periodic blood testing is the recommendation to assess the patient’s prothrombin time (PT) and the international normalized ratio (INR). Option B: The laboratory parameter utilized to monitor warfarin therapy is the PT/INR. The PT is the number of seconds it takes the blood to clot, and the INR allows for the standardization of the PT measurement depending on the thromboplastin reagent used by a laboratory. Therefore, monitoring a patient’s INR while on warfarin is strongly preferable over PT because it allows for a standardized measurement without variations due to different laboratory sites. Option C: When managing warfarin toxicity, the initial step would be to discontinue warfarin and then administer vitamin K (phytonadione). The vitamin K administration can be either via the oral, intravenous, or subcutaneous route. However, the initial administration of oral vitamin K is often preferable in patients without major bleeding or extremely elevated INR. Option D: Patients also require close monitoring for signs and symptoms of active bleeding throughout their treatment. Close monitoring for signs and symptoms of bleeding, such as dark tarry stools, nosebleeds, and hematomas, is necessary. The patient’s hemoglobin and hematocrit level should undergo an assessment before initiating warfarin and approximately every six months while on therapy. NCLEXRN-09-055 Question Tag: calcium Question Category: Health Promotion and Maintenance Which selection would provide the most calcium for the client who is 4 months pregnant? A. A granola bar B. A bran muffin C. A cup of yogurt D. A glass of fruit juice Correct Answer: C. A cup of yogurt The food with the most calcium is the yogurt, which has approximately 400 mg of calcium. A growing baby needs a considerable amount of calcium to develop. If the mother does not consume enough calcium to sustain the needs of the developing baby, the body will take calcium from the bones, decreasing bone mass and putting the mother at risk for osteoporosis. Osteoporosis causes dramatic thinning of the bone, resulting in weak, brittle bones that can easily be broken. Option A: Eat a variety of foods to get all the nutrients you need. Recommended daily servings include 6-11 servings of breads and grains, two to four servings of fruit, four or more servings of vegetables, four servings of dairy products, and three servings of protein sources (meat, poultry, fish, eggs or nuts).Consume fats and sweets sparingly. Option B: Choose foods high in fiber that are enriched, such as whole-grain breads, cereals, beans, pasta and rice, as well as fruits and vegetables. Although it’s best to get fiber from foods, taking a fiber supplement can help get the necessary amount. Option D: A glass of fruit juice is mainly rich in vitamin C and fiber. Choose at least one good source of vitamin C every day, such as oranges, grapefruits, strawberries, honeydew, papaya, broccoli, cauliflower, Brussels sprouts, green peppers, tomatoes, and mustard greens. Pregnant women need 80 – 85 mg of vitamin C a day. NCLEXRN-09-056 Question Tag: preeclampsia, magnesium sulfate Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The client with preeclampsia is admitted to the unit with an order for magnesium sulfate. Which action by the nurse indicates understanding of the possible side effects of magnesium sulfate? A. The nurse places a sign over the bed not to check blood pressure in the right arm. B. The nurse places a padded tongue blade at the bedside. C. The nurse inserts a Foley catheter. D. The nurse darkens the room. Correct Answer: C. The nurse inserts a Foley catheter. The client receiving magnesium sulfate should have a Foley catheter in place, and hourly intake and output should be checked. Strict intake and output will be assessed throughout the magnesium sulfate infusion. Record urinary output at least every 1 hour if Foley catheter is in place. Otherwise, measure and record all voids. Urine output should be at least 30 mL/hour while administering magnesium sulfate. If less, notify the provider of decreased urine output. Option A: There is no need to refrain from checking the blood pressure in the right arm. Before beginning any infusion of magnesium sulfate, the primary RN will obtain baseline vital signs (temperature, pulse, respirations, blood pressure, and O2 saturation). Baseline fetal heart rate (FHR), deep tendon reflexes (DTRs), clonus, bilateral breath sounds, urinary output, and activity will be assessed and documented in the Electronic Health Record (EHR). Option B: A padded tongue blade should be kept in the room at the bedside, just in case of a seizure, but this is not related to the magnesium sulfate infusion. Temperature is assessed every 4 hours, unless rupture of membranes. Once membranes have ruptured, temperature will be assessed every 2 hours. If febrile (≥ 100.4) provider will be notified and temperature will be assessed hourly thereafter. Option D: Darkening the room is unnecessary. Inform staff and visitors of the need to maintain a quiet environment, and avoidance of excessive visitation and environmental stimulation. Include assessment of epigastric pain, visual disturbances, edema, headache, level of consciousness, and lung auscultation prior to start of infusion and every 2 hours throughout infusion or more frequently as condition indicates. NCLEXRN-09-057 Question Tag: blood transfusion Question Category: Safe and Effective Care Environment, Management of Care A 6-year-old client is admitted to the unit with a hemoglobin of 6g/dL. The physician has written an order to transfuse 2 units of whole blood. When discussing the treatment, the child’s mother tells the nurse that she does not believe in having blood transfusions and that she will not allow her child to have the treatment. What nursing action is most appropriate? A. Ask the mother to leave while the blood transfusion is in progress B. Encourage the mother to reconsider C. Explain the consequences without treatment D. Notify the physician of the mother’s refusal Correct Answer: D. Notify the physician of the mother’s refusal If the client’s mother refuses the blood transfusion, the doctor should be notified. Because the client is a minor, the court might order treatment. Appropriate management of such patients entails understanding of ethical and legal issues involved, providing meticulous medical management, use of prohemostatic agents, essential interventions and techniques to reduce blood loss and hence, reduce the risk of subsequent need for blood transfusion. Option A: It is inappropriate to ask the mother to leave during blood transfusion, especially as she has not consented to it. Respect for a patient’s autonomy and human rights require obtaining informed consent before any medical intervention. This is fundamental to good medical practice. The rejection of blood transfusions causes an ethical dilemma between the patient’s freedom to accept or to reject a medical treatment even unto death (i.e., autonomy), and the physician’s duty to provide optimal treatment. Option B: It is better to discuss with patients the specifics of blood transfusion refusal, if possible. A mentally competent individual has an absolute moral and legal right to refuse or reject the consent for medical treatment or transfusion except when he has diminished decision-making capacity or a legal intervention mandates treatment. Option C: It is the physician’s primary responsibility to explain the consequences to the mother and try to encourage her to consent for the procedure. It is important to convince that every attempt will be made to avoid blood, but also convey that a doctor would not allow a child to die for lack of blood transfusion. In the UK, children under 16 years of age can legally give consent if they can understand the issues involved (Gillick Competence). NCLEXRN-09-058 Question Tag: burns Question Category: Physiological Integrity, Physiological Adaptation A client is admitted to the unit 2 hours after an explosion causes burns to the face. The nurse would be most concerned with the client developing which of the following? A. Hypovolemia B. Laryngeal edema C. Hypernatremia D. Hyperkalemia Correct Answer: B. Laryngeal edema The nurse should be most concerned with laryngeal edema because of the area of burn. For burns classified as severe (> 20% TBSA), fluid resuscitation should be initiated to maintain urine output > 0.5 mL/kg/hour. One commonly used fluid resuscitation formula is the Parkland formula. The total amount of fluid to be given during the initial 24 hours = 4 ml of LR × patient’s weight (kg) × % TBSA. Option A: Severe burns cause not only significant injury at the local burn site but also a systemic response throughout the body. Inflammatory and vasoactive mediators such as histamines, prostaglandins, and cytokines are released causing a systemic capillary leak, intravascular fluid loss, and large fluid shifts. These responses occur mostly over the first 24 hours peaking at around six to eight hours after injury. This response, along with decreased cardiac output and increased vascular resistance, can lead to marked hypovolemia and hypoperfusion called “burn shock.” Option C: Patient’s vital signs, mental status, capillary refill and urine output must be monitored and fluid rates adjusted accordingly. Urine output of 0.5 mL/kg or about 30 – 50 mL/hr in adults and 0.5-1.0 mL/kg/hr in children less than 30kg is a good target for adequate fluid resuscitation. Recent literature has raised concerns about complications from over-resuscitation described as “fluid creep.” Again, adequate fluid resuscitation is the goal. Option D: The primary survey assesses the A.B.C.s for life-threats. In the burn patient, attention should focus on the airway looking for oral burns that might cause swelling and obstruction, breathing problems from smoke inhalation or lung injury, and bleeding or circulation problems by looking for life-threatening bleeding and checking blood pressure, heart rate, and pulses. The next step would be resuscitation and immediate intervention for life-threats. NCLEXRN-09-059 Question Tag: anorexia nervosa Question Category: Health Promotion and Maintenance, Physiological Adaptation The nurse is evaluating nutritional outcomes for a patient with anorexia nervosa. Which data best indicates that the plan of care is effective? A. The client selects a balanced diet from the menu. B. The client’s hemoglobin and hematocrit improve. C. The client’s tissue turgor improves. D. The client gains weight. Correct Answer: D. The client gains weight. The client with anorexia shows the most improvement by weight gain. Expect weight gain of about 1 lb (0.5 kg) per week to see the effectiveness of the treatment regimen. Establish a minimum weight goal and daily nutritional requirements. Malnutrition is a mood-altering condition, leading to depression and agitation and affecting cognitive function and decision making. Improved nutritional status enhances thinking ability, allowing initiation of psychological work. Option A: Selecting a balanced diet does little good if the client will not eat. Make a selective menu available, and allow the patient to control choices as much as possible. Patient who gains confidence in herself and feels in control of the environment is more likely to eat preferred foods. Option B: The hematocrit might improve by several means, such as blood transfusion, but that does not indicate improvement in the anorexic condition. Use a consistent approach. Sit with the patient while eating; present and remove food without persuasion and comment. Promote a pleasant environment and record intake. Patient detects urgency and may react to pressure. Any comment that might be seen as coercion provides focus on food. When staff responds in a consistent manner, the patient can begin to trust staff responses. The single area in which the patient has exercised power and control is food or eating, and he or she may experience guilt or rebellion if forced to eat. Structuring meals and decreasing discussions about food will decrease power struggles with the patient and avoid manipulative games. Option C: The tissue turgor indicates fluid stasis, not an improvement of anorexia. Maintain a regular weighing schedule, such as Monday and Friday before breakfast in the same attire, and graph results. Provides an accurate ongoing record of weight loss or gain. Also diminishes obsessing about changes in weight. NCLEXRN-09-060 Question Tag: fracture, cast application Question Category: Physiological Integrity, Physiological Adaptation The client is admitted following repair of a fractured tibia and cast application. Which nursing assessment should be reported to the doctor? A. Pain beneath the cast B. Warm toes C. Pedal pulses weak and rapid D. Paresthesia of the toes Correct Answer: D. Paresthesia of the toes Paresthesia is not normal and might indicate compartment syndrome. Acute compartment syndrome occurs when there is increased pressure within a closed osteofascial compartment, resulting in impaired local circulation. Acute compartment syndrome is considered a surgical emergency since, without proper treatment, it can lead to ischemia and eventually necrosis. Option A: At this time, pain beneath the cast is normal. Pain is typically severe, out of proportion to the injury. Early on, pain may only be present with passive stretching. However, this symptom may be absent in advanced acute compartment syndrome. In the initial stages, pain may be characterized as a burning sensation or as a deep ache of the involved compartment. Option B: Classically, the presentation of acute compartment syndrome has been remembered by “The Five P’s”: pain, pulselessness, paresthesia, paralysis, and pallor. However, aside from paresthesia, which may occur earlier in the course of the condition, these are typically late findings. Option C: Pulses should be present. Beware that the presence or absence of a palpable arterial pulse may not accurately indicate relative tissue pressure or predict the risk for compartment syndrome. In some patients, a pulse is still present, even in a severely compromised extremity. NCLEXRN-09-061 Question Tag: barbiturates Question Category: Psychosocial Integrity A client with a history of abusing barbiturates abruptly stops taking the medication. The nurse should give priority to assessing the client for: A. Depression and suicidal ideation B. Tachycardia and diarrhea C. Muscle cramping and abdominal pain D. Tachycardia and euphoric mood Correct Answer: B. Tachycardia and diarrhea Barbiturates create a sedative effect. When the client stops taking barbiturates, he will experience tachycardia, diarrhea, and tachypnea. When given in IV anesthetics, barbiturates will produce a reduction in blood pressure and an increase in heart rate. Respiratory depression and apnea may occur. Given the potential for severe adverse events including death, a pharmacist should verify the dosing, and perform a thorough medication reconciliation to ensure there are no drug interactions, in particular, additive CNS depression effects. Option A: Enough depression and suicidal ideation go along with barbiturate use; it is not the priority. Barbiturates cause postsynaptic enhancement of GABA, interacting with alpha and beta subunits of the GABA-A receptor. Barbiturates increase chloride ion flux which results in GABA-induced postsynaptic inhibition. Phenobarbital and pentobarbital affect the GABA-A receptors with a dose-dependent response. Option C: Muscle cramps and abdominal pain are vague symptoms that could be associated with other problems. Barbiturate classification is according to the duration of their action, IV formulations of thiopental and methohexital are in the ultra short-acting class. The short and intermediate-acting have an effect lasting 2 to 6 hours. This classification includes sleeping medications pentobarbital, secobarbital, amobarbital, and butabarbital. Long-acting barbiturates have an effect of longer than 6 hours and include barbital and phenobarbital. Option D: Tachycardia is associated with stopping barbiturates, but euphoria is not. At higher micromolar concentrations associated with anesthetic levels, these drugs directly activate chloride channels. Both barbiturates and benzodiazepines interact with GABA-A receptors, but barbiturates are unique in that they potentiate GABA-A receptors while increasing chloride ion influx even with very low concentrations of the GABA neurotransmitter. NCLEXRN-09-062 Question Tag: labor, FHT Question Category: Physiological Integrity, Physiological Adaptation During the assessment of a laboring client, the nurse notes that the FHT are loudest in the upper-right quadrant. The infant is most likely in which position? A. Right breech presentation B. Right occiput anterior presentation C. Left sacral anterior presentation D. Left occiput transverse presentation Correct Answer: A. Right breech presentation If the fetal heart tones are heard in the right upper abdomen, the infant is in a breech presentation. A breech position is not ideal for delivery. Though the majority of breech babies are born healthy, they may have a higher risk of birth defects or trauma during delivery. This position can also be problematic because it increases the risk of forming a loop in the umbilical cord that could cause injury to the baby if they’re delivered vaginally. Option B: If the infant is positioned in the right occiput anterior presentation, the FHTs will be located in the right lower quadrant, so answer B is incorrect. The baby is head down, with their face facing the mother’s back. The baby’s chin is tucked into their chest and their head is ready to enter the pelvis. The baby is able to flex their head and neck, and tuck their chin into their chest. This is usually referred to as occipito-anterior, or the cephalic presentation. Option C: If the fetus is in the sacral position, the FHTs will be located in the center of the abdomen, so answer C is incorrect. Left Sacrum Anterior (LSA) means the fetal sacrum is closest to the mother’s symphysis and rotated slightly to the mother’s left (clockwise from direct SA). Option D: If the FHTs are heard in the left lower abdomen, the infant is most likely in the left occiput transverse position, making answer D incorrect. This LOT (Left, Occiput, Transverse) position and its’ mirror image, ROT, are common in early labor. As labor progresses and the fetal head descends, the occiput usually rotates anteriorly, converting this LOT to an LOA or OA as the head delivers. NCLEXRN-09-063 Question Tag: asthma Question Category: Physiological Integrity, Physiological Adaptation The primary physiological alteration in the development of asthma is: A. Bronchial inflammation and dyspnea B. Hypersecretion of abnormally viscous mucus C. Infectious processes causing mucosal edema D. Spasm of bronchial smooth muscle Correct Answer: D. Spasm of bronchial smooth muscle Asthma is the presence of bronchial spasms. This spasm can be brought on by allergies or anxiety. Asthma is a condition of acute, fully reversible airway inflammation, often following exposure to an environmental trigger. The pathological process begins with the inhalation of an irritant (e.g., cold air) or an allergen (e.g., pollen), which then, due to bronchial hypersensitivity, leads to airway inflammation and an increase in mucus production. Option A: The primary physiological alteration is not inflammation. Airway obstruction occurs due to the combination of inflammatory cell infiltration; mucus hypersecretion with mucus plug formation; and smooth muscle contraction. Option B: There is the production of abnormally viscous mucus, not a primary alteration. If not corrected rapidly, asthma may become more difficult to treat, as the mucus production prevents the inhaled medication from reaching the mucosa. The inflammation also becomes more edematous. This process is resolved (in theory complete resolution is required in asthma, but in practice, this is not checked or tested) with beta-2 agonists (e.g., salbutamol, salmeterol, albuterol) and can be aided by muscarinic receptor antagonists (e.g., ipratropium bromide), which act to reduce the inflammation and relax the bronchial musculature, as well as reducing mucus production Option C: The infection is not primary to asthma. These irreversible changes may become irreversible over time due to basement membrane thickening, collagen deposition, and epithelial desquamation, and airway remodeling occurs in chronic disease with smooth muscle hypertrophy and hyperplasia. NCLEXRN-09-064 Question Tag: mania Question Category: Physiological Integrity, Basic Care and Comfort ADVERTISEMENTS A client with mania is unable to finish her dinner. To help her maintain sufficient nourishment, the nurse should: A. Serve high-calorie foods she can carry with her B. Encourage her appetite by sending out for her favorite foods C. Serve her small, attractively arranged portions D. Allow her in the unit kitchen for extra food whenever she pleases Correct Answer: A. Serve high-calorie foods she can carry with her The client with mania is seldom sitting long enough to eat and burns many calories for energy. Finger foods or things a client can eat while moving around are the best options to improve nutrition. Decreasing environmental stimulation may assist the client to relax; the nurse must provide a quiet environment without noise, television, and other distractions. Option B: The client should be treated the same as other clients. Frequently remind the client to eat (e.g.,Rob, finish your pancake”, “Sandra, drink this apple juice.”). The manic client is unaware of bodily needs and is easily distracted. Needs supervision to eat. Option C: Small meals are not the correct option for this client. Encourage frequent high-calorie protein drinks and finger foods (e.g., sandwiches, fruit, milkshakes). Constant fluid and calorie replacement are needed. The client might be too active to sit at meals. Finger foods allow “eating on the run”. Option D: Allowing her into the kitchen gives her privileges that other clients do not have and should not be allowed. Monitor intake, output, and vital signs. Ensures adequate fluid and caloric intake; minimizes dehydration and cardiac collapse. NCLEXRN-09-065 Question Tag: Bryant’s traction Question Category: Physiological Integrity, Basic Care and CoMFORT To maintain Bryant’s traction, the nurse must make certain that the child’s: A. Hips are resting on the bed, with the legs suspended at a right angle to the bed B. Hips are slightly elevated above the bed and the legs are suspended at a right angle to the bed C. Hips are elevated above the level of the body on a pillow and the legs are suspended parallel to the bed D. Hips and legs are flat on the bed, with the traction positioned at the foot of the bed Correct Answer: B. Hips are slightly elevated above the bed and the legs are suspended at a right angle to the bed Bryant’s traction is used for fractured femurs and dislocated hips. The hips should be elevated 15° off the bed. Bryant’s traction is used for developmental dislocated hip(s) (DDH). In Bryant’s traction, the child’s body and the weights are used as tension to keep the end of the femur (the large bone that goes from the knee to the hip) in the hip socket. Traction will help position the top of the femur into the hip socket correctly Option A: The hips should not be resting on the bed. Let the weights hang freely. They should not touch the bed. Keep all blankets and sheets away from the traction ropes. In order to have effective traction, make sure to position the patient properly with a correct body alignment in the center of the bed to have good maintenance of the pull. Ropes and weights should be observed and checked regularly to make sure it is moving freely on the pulley. Option C: The hips should not be above the level of the body. The rope knots should be maintained in a right position in order to prevent it from touching the pulley. And the comfort of the patient should be maintained, and making sure he/she is comfortable in his/her position to avoid any further complications. Option D: The hips and legs should not be flat on the bed. With Bryant’s traction, the legs are wrapped with strips of adhesive tape (moleskin) attached to a gauze adhesive elastic bandage (Elastoplast), then more moleskin and Elastoplast, then connected to ropes and weights. The bandage and weights do not hurt the child. NCLEXRN-09-066 Question Tag: herpes zoster Question Category: Physiological Integrity, Reduction of Risk Potential Which action by the nurse indicates understanding of herpes zoster? A. The nurse covers the lesions with a sterile dressing. B. The nurse wears gloves when providing care. C. The nurse administers a prescribed antibiotic. D. The nurse administers oxygen. Correct Answer: B. The nurse wears gloves when providing care. Herpes zoster is shingles. Clients with shingles should be placed in contact precautions. Wearing gloves during care will prevent transmission of the virus. Use universal precautions in caring for the client to prevent transmission of disease to self or other clients. VZV can be transmitted to others and cause chickenpox in the person who has not previously had the disease. Option A: Covering the lesions with a sterile gauze is not necessary. Suggest the use of gauze to separate the lesions in skin folds. This reduces irritation, itching, and cross-contamination. Teach contact isolation. VZV is spread by contact with fluid from lesions containing viruses. Option C: Antibiotics are not prescribed for herpes zoster. Instruct the client in the use of antiviral medications, as prescribed. Antiviral agents are most effective during the first 72 hours of an outbreak when viruses are proliferating. Drugs of choice are acyclovir, famciclovir, or valacyclovir. Option D: Oxygen is not necessary for shingles. Instruct the client to avoid contact with pregnant women and immunocompromised individuals. Active lesions can be infectious, and immunosuppressed individuals are more susceptible. NCLEXRN-09-067 Question Tag: Vancomycin Question Category: Physiological Integrity, Reduction of Risk Potential The client has an order for a trough to be drawn on the client receiving Vancomycin. The nurse is aware that the nurse should contact the lab for them to collect the blood: A. 15 minutes after the infusion B. 30 minutes before the infusion C. 1 hour after the infusion D. 2 hours after the infusion Correct Answer: B. 30 minutes before the infusion A trough level should be drawn 30 minutes before the third or fourth dose. Draw through specimens immediately before (≤30 min) the next dose. Do not draw specimens until a steady state is achieved (ie, before the fourth dose). Draw peak specimens 1-2 hours after completion of intravenous dosage. Option A: Vancomycin is a glycopeptide antibiotic first isolated in 1953. It is a naturally occurring antimicrobial synthesized by soil bacterium Amycolatopsis Orientalis. Generic vancomycin became available and approved for use in 1958 and quickly became a common antibiotic in treating rapidly growing penicillin-resistant Staphylococcus species. Option C: The emergence of pseudomembranous enterocolitis, coupled with the spread of methicillin-resistant Staphylococcus aureus (MRSA), led to a resurgence in the use of vancomycin. It is used to treat serious, life-threatening infections by gram-positive bacteria that are resistant to less-toxic agents. Option D: General indications for measuring vancomycin trough levels include risk of nephrotoxicity and inadequate therapeutic response. Monitor at regular intervals. Specifically, trough levels should be measured in patients at risk for nephrotoxicity. NCLEXRN-09-068 Question Tag: diaphragm Question Category: Health Promotion and Maintenance The client using a diaphragm should be instructed to: A. Refrain from keeping the diaphragm in longer than 4 hours B. Keep the diaphragm in a cool location C. Have the diaphragm resized if she gains 5 pounds D. Have the diaphragm resized if she has any surgery Correct Answer: B. Keep the diaphragm in a cool location The client using a diaphragm should keep the diaphragm in a cool location. The diaphragm is a birth control (contraceptive) device that prevents sperm from entering the uterus. The diaphragm is a small, reusable rubber or silicone cup with a flexible rim that covers the cervix. Before sex, the diaphragm is inserted deep into the vagina so that part of the rim fits snugly behind the pubic bone. Option A: She should refrain from leaving the diaphragm for longer than 8 hours, not 4 hours. Always use the diaphragm with spermicidal cream, foam or gel. Avoid use of body lotions near the vagina and vaginal medications when using the diaphragm. If using a diaphragm and douche, wait until at least six hours after sex to avoid washing away spermicide. Option C: The traditional dome-shaped diaphragm comes in different sizes, and the woman needs to be fitted for one by her healthcare provider. A newer diaphragm option — the Caya diaphragm — comes in one size. To get either type of diaphragm, the woman needs a prescription from her healthcare provider. Option D: She should have the diaphragm resized when she gains or loses 10 pounds or has abdominal surgery. The woman will require an internal examination to assess what size of diaphragm will be suitable for her. A diaphragm should be replaced at least every 2 years. It should be examined regularly for holes or weak spots, and replaced as needed. She will need to be ‘resized’ for a diaphragm if she lost or gained more than 7 pounds in weight or had a pregnancy. NCLEXRN-09-069 Question Tag: postpartum, breastfeeding Question Category: Health Promotion and Maintenance The nurse is providing postpartum teaching for a mother planning to breastfeed her infant. Which of the client’s statements indicates the need for additional teaching? A. “I’m wearing a support bra.” B. “I’m expressing milk from my breast.” C. “I’m drinking four glasses of fluid during a 24-hour period.” D. “While I’m in the shower, I’ll allow the water to run over my breasts.” Correct Answer: C. “I’m drinking four glasses of fluid during a 24-hour period.” Mothers who plan to breastfeed should drink plenty of liquids, and four glasses are not enough in a 24-hour period. Women need extra support, encouragement, and reassurance while breastfeeding. Although we view breastfeeding as a natural process, it is still a skill that has to be learned. Initially, breastfeeding can seem demanding, as the baby may have a desire to feed/suck frequently. Babies, however, begin to establish their own pattern over time, and the mother will begin to feel more comfortable and at ease. Option A: Wearing a support bra is a good practice for the mother who is breastfeeding as well as the mother who plans to bottle-feed. A comfortable, soft, cotton nursing bra is a good choice for both day and night, and a sports bra style may also make a comfortable bra for nighttime use. Option B: Expressing milk from the breast will stimulate milk production. If it is necessary to express breast milk, show the mother how to do this and show her how to feed expressed breast milk by the cup. You may need to refer her to a trained infant feeding counselor for this. Option D: Allowing the water to run over the breast will also facilitate “letdown,” when the milk begins to be produced; thus, answer D is incorrect. Some women also find that the initial ‘let down’ reflex is very strong which causes them pain or they get strong after-pains as their wombs contract. Reassure them that this will pass. The ‘let down’ reflex may also cause them to leak milk when they have sexual intercourse. Reassure them that this is normal and that they may need to tell their husband or partner that this is normal. NCLEXRN-09-070 Question Tag: cranial nerve VII Question Category: Physiological Integrity, Physiological Adaptation Damage to the VII cranial nerve results in: A. Facial pain B. Absence of ability to smell C. Absence of eye movement D. Tinnitus Correct Answer: A. Facial pain The facial nerve is cranial nerve VII. If damage occurs, the client will experience facial pain. The sensory portion, or intermediate nerve, has the following components: (1) taste to the anterior two-thirds of the tongue; (2) secretory and vasomotor fibers to the lacrimal gland, the mucous membranes of the nose and mouth, and the submandibular and sublingual salivary glands; (3) cutaneous sensory impulses from the external auditory meatus and region back of the ear. Option B: Olfactory nerve controls smell, and it is cranial nerve I. The olfactory nerve is the first cranial nerve and is instrumental in our sense of smell. The olfactory nerve contains only afferent sensory nerve fibers and, like all cranial nerves, is paired. The olfactory nerve is the shortest cranial nerve, and along with the optic nerve is one of the only two cranial nerves that do not converge with the brainstem. Option C: Eye movement is controlled by the Trochlear or C IV. The trochlear nerve is the fourth cranial nerve (CN IV) and one of the ocular motor nerves that controls eye movement. The trochlear nerve, while the smallest of the cranial nerves, has the longest intracranial course as it is the only nerve to have a dorsal exit from the brainstem. It originates in the midbrain and extends laterally and anteriorly to the superior oblique muscle. Option D: The vestibulocochlear nerve or CN VIII is responsible for hearing loss and tinnitus. The vestibulocochlear nerve, also known as cranial nerve eight (CN VIII), consists of the vestibular and cochlear nerves. Each nerve has distinct nuclei within the brainstem. The vestibular nerve is primarily responsible for maintaining body balance and eye movements, while the cochlear nerve is responsible for hearing. NCLEXRN-09-071 Question Tag: urinary tract infection Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies A client is receiving Pyridium (phenazopyridine hydrochloride) for a urinary tract infection. The client should be taught that the medication may: A. Cause diarrhea B. Change the color of her urine C. Cause mental confusion D. Cause changes in taste Correct Answer: B. Change the color of her urine Clients taking Pyridium should be taught that the medication will turn the urine orange or red. Pyridium can also cause a yellowish color to skin and sclera if taken in large doses. Phenazopyridine relieves urinary tract pain, burning, irritation, and discomfort, as well as urgent and frequent urination caused by urinary tract infections, surgery, injury, or examination procedures. However, phenazopyridine is not an antibiotic; it does not cure infections. Option A: It does not cause diarrhea. Phenazopyridine comes as a tablet or capsule to take by mouth. It usually is taken three times a day after meals. Do not chew or crush the tablets as it may cause your teeth to become stained; swallow them whole with a full glass of water. You may stop taking this drug when pain and discomfort completely disappear. Option C: The drug does not cause mental confusion. Phenazopyridine can interfere with laboratory tests, including urine tests for glucose (sugar) and ketones. If you have diabetes, you should use Clinitest rather than Tes-Tape or Clinistix to test your urine for sugar. Urine tests for ketones (Acetest and Ketostix) may give false results. Before you have any tests, tell the laboratory personnel and doctor that you take this medication. Option D: It is not associated with changes in taste. Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom). NCLEXRN-09-072 Question Tag: Accutane Question Category: Physiological Integrity, Reduction of Risk Potential Which of the following tests should be performed before beginning a prescription of Accutane? A. Check the calcium level B. Perform a pregnancy test C. Monitor apical pulse D. Obtain a creatinine level Correct Answer: B. Perform a pregnancy test Accutane is contraindicated for use by pregnant clients because it causes teratogenic effects. Isotretinoin was a pregnancy category X drug under the previous FDA system and is contraindicated in women who are pregnant or who may become pregnant. There have been severe, documented congenital disabilities when pregnant women have taken isotretinoin. Option A: Calcium levels are unnecessary. To prescribe and receive isotretinoin, the Food and Drug Administration requires prescribers and patients to register with the iPLEDGE program. iPLEDGE ensures the fulfillment of appropriate requirements before the distribution of isotretinoin to prevent the use of this medication during pregnancy. Option C: Apical pulse is not necessary. Two negative pregnancy tests are necessary before the initiation of therapy with isotretinoin. The first pregnancy test occurs up to 30 days prior to medication initiation. The second pregnancy test must occur at least 19 days after the first negative pregnancy test and within the first five days of the patient’s menstrual cycle. Each subsequent month the patient must have a recorded negative pregnancy test to continue therapy. After discontinuation of therapy, a final pregnancy test should take place at 30 days following therapy completion. Option D: Liver function tests (LFTs), fasting lipid profile (including triglycerides), blood glucose, creatinine phosphokinase (CPK), and complete blood counts (CBC) with differential should be drawn before initiating therapy with isotretinoin. Screening for mood alteration, psychosis, aggression, suicidal ideation, skin changes, and visual changes should also take place prior to starting therapy. NCLEXRN-09-073 Question Tag: AIDS, acyclovir Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies A client with AIDS is taking Zovirax (acyclovir). Which nursing intervention is most critical during the administration of acyclovir? A. Limit the client’s activity B. Encourage a high-carbohydrate diet C. Utilize an incentive spirometer to improve respiratory function D. Encourage fluids Correct Answer: D. Encourage fluids Clients taking Acyclovir should be encouraged to drink plenty of fluids because renal impairment can occur. Acute kidney injury (AKI) is the most significant side effect of parenteral acyclovir administration. The incidence of AKI is comparable to other nephrotoxic medications such as aminoglycosides. Patients with CKD are at higher risk. Dose adjustment of acyclovir for ideal body weight and baseline renal function is imperative. Option A: Limiting activity is not necessary. Patients should be monitored for adverse effects such as malaise, inflammation or phlebitis at infusion site, nausea, vomiting, rash (including Steven-Johnson syndrome), transaminitis, nausea, vomiting, diarrhea, headache, abdominal pain, aggression/confusion, agitation, alopecia, anaphylaxis, anemia, angioedema, anorexia, ataxia, coma, disseminated intravascular coagulation (DIC), dizziness and fatigue. Option B: Eating a high-carbohydrate diet is unnecessary. When taken orally, acyclovir may be taken with or without food 2 to 5 times a day for 5 to 10 days as well as up to 12 months to prevent outbreaks of genital herpes. For limited mucocutaneous lesions, acyclovir administration can be via the oral route. In cases in which there is disseminated, visceral, or CNS involvement, the acyclovir administration should be intravenous. Option C: Use of an incentive spirometer is not specific to clients taking Acyclovir. A study regarding the pharmacokinetics of acyclovir demonstrated that a patient’s glomerular filtration and tubular secretion contribute to its renal excretion. Appropriate cautions are necessary when administering intravenous acyclovir to such higher-risk patients. NCLEXRN-09-074 Question Tag: MRI Question Category : Physiological Integrity, Reduction of Risk Potential A client is admitted for an MRI. The nurse should question the client regarding: A. Pregnancy B. A titanium hip replacement C. Allergies to antibiotics D. Inability to move his feet Correct Answer: A. Pregnancy Although there is no evidence to suggest MRI scans can pose a risk during pregnancy, it is considered precaution to not perform MRI during pregnancy, particularly in the first three months. This is particularly the case during the first trimester of pregnancy, as organogenesis takes place during this period. The concerns in pregnancy are the same as for MRI in general, but the fetus may be more sensitive to the effects—particularly to heating and to noise. Option B: Clients with a titanium hip replacement can have an MRI. Some other devices and implants might be contraindicated. To ensure patients’ safety, the radiologist and MRI technologist must evaluate the type of device that patients have. Radiologists, referring physicians and MR technologists, need to be able to assess MRI safety, patients’ condition, and compatibility of medical devices to keep patients safe. Option C: No antibiotics are used with this test. MRI contrast agents are gadolinium chelates with different stability, viscosity, and osmolality. Gadolinium is a relatively very safe contrast; however, it rarely might cause allergic reactions in patients. Option D: The client should remain still only when instructed. Patients who are unable to be still or obey breathing instructions in the scanner need special attention. Some patients in pain might move during the procedure, which degrades the quality of the images, restricts the interpretation, and decreases the accuracy of the report. Some MRI sequences need to be obtained while patients hold their breath and lie motionless. NCLEXRN-09-075 Question Tag: Amphotericin B Question Category: Physiological Integrity, Pharmacological and Parenteral Therapies The nurse is caring for the client receiving Amphotericin B. Which of the following indicates that the client has experienced toxicity to this drug? A. Changes in vision B. Nausea C. Urinary frequency D. Changes in skin color Correct Answer: D. Changes in skin color Clients taking Amphotericin B should be monitored for liver, renal, and bone marrow function because this drug is toxic to the kidneys and liver, and causes bone marrow suppression. Jaundice is a sign of liver toxicity and is not specific to the use of Amphotericin B. Due to the similarity of mammalian and fungal membranes, which both contain sterols (the therapeutic target for amphotericin B), amphotericin B can exhibit cellular toxicity. Option A: Changes in vision are not related. Other potential uncommon side effects include demyelinating encephalopathy in patients with bone marrow transplant with total body irradiation or who are receiving cyclosporine. Option B: Nausea is a side effect, not a sign of toxicity. Monitoring is a recommendation to evaluate for the presence of side effects. Initially, a daily electrolyte panel, including potassium and magnesium concentrations until the dose increases to its therapeutic level, and after that, weekly electrolyte concentrations are sufficient. Clinicians should obtain potassium concentrations immediately if the patient presents with any signs of hypokalemia, such as muscle weakness, cramps, drowsiness, or ECG changes of hypokalemia. Option C: Urinary frequency is a side effect. Renal toxicity correlates with conventional amphotericin B use and can lead to renal failure and requirement for dialysis. But the azotemia often stabilizes with therapy and renal damage is reversible after discontinuation of amphotericin B. [Show More]
Last updated: 1 year ago
Preview 1 out of 95 pages
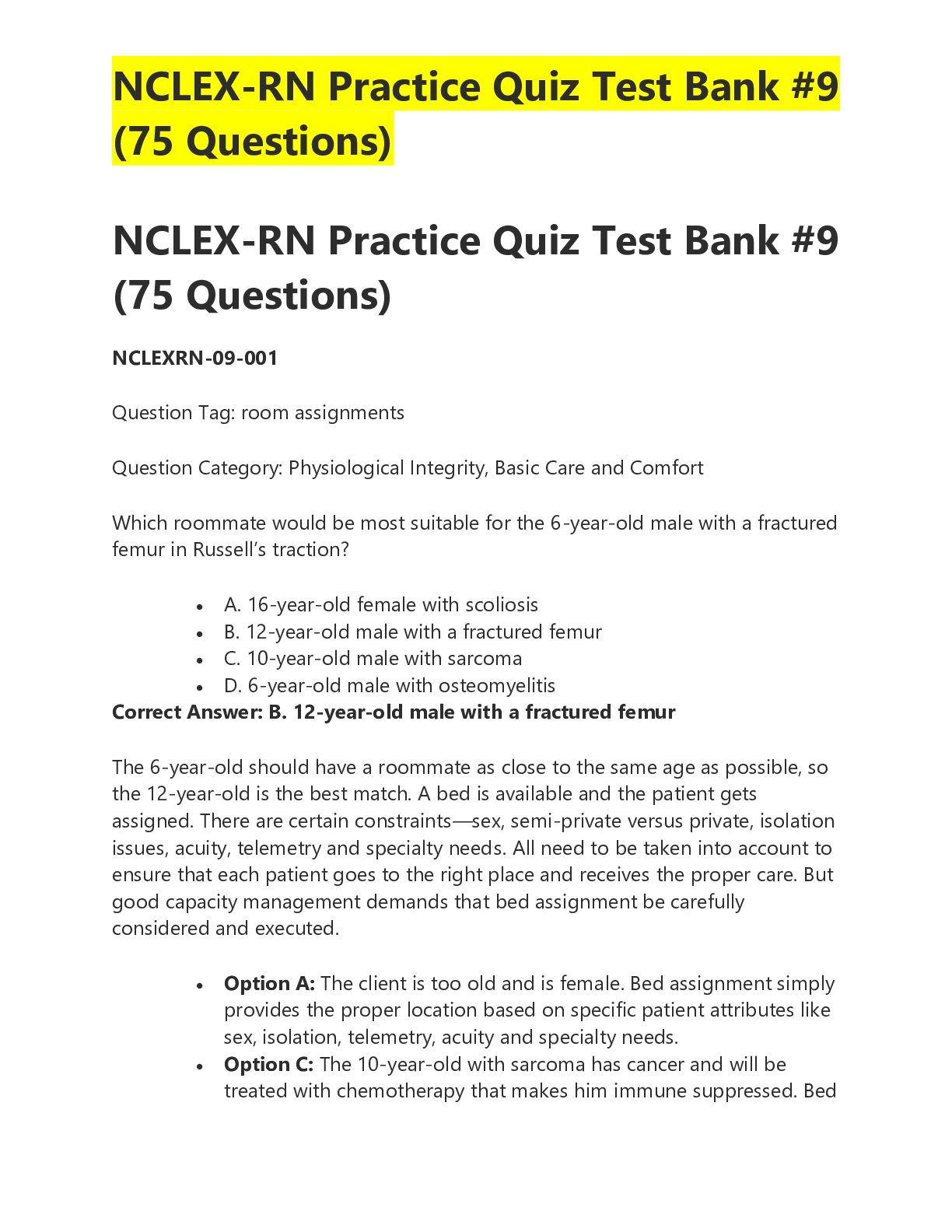
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 21, 2021
Number of pages
95
Written in
Additional information
This document has been written for:
Uploaded
Dec 21, 2021
Downloads
0
Views
271

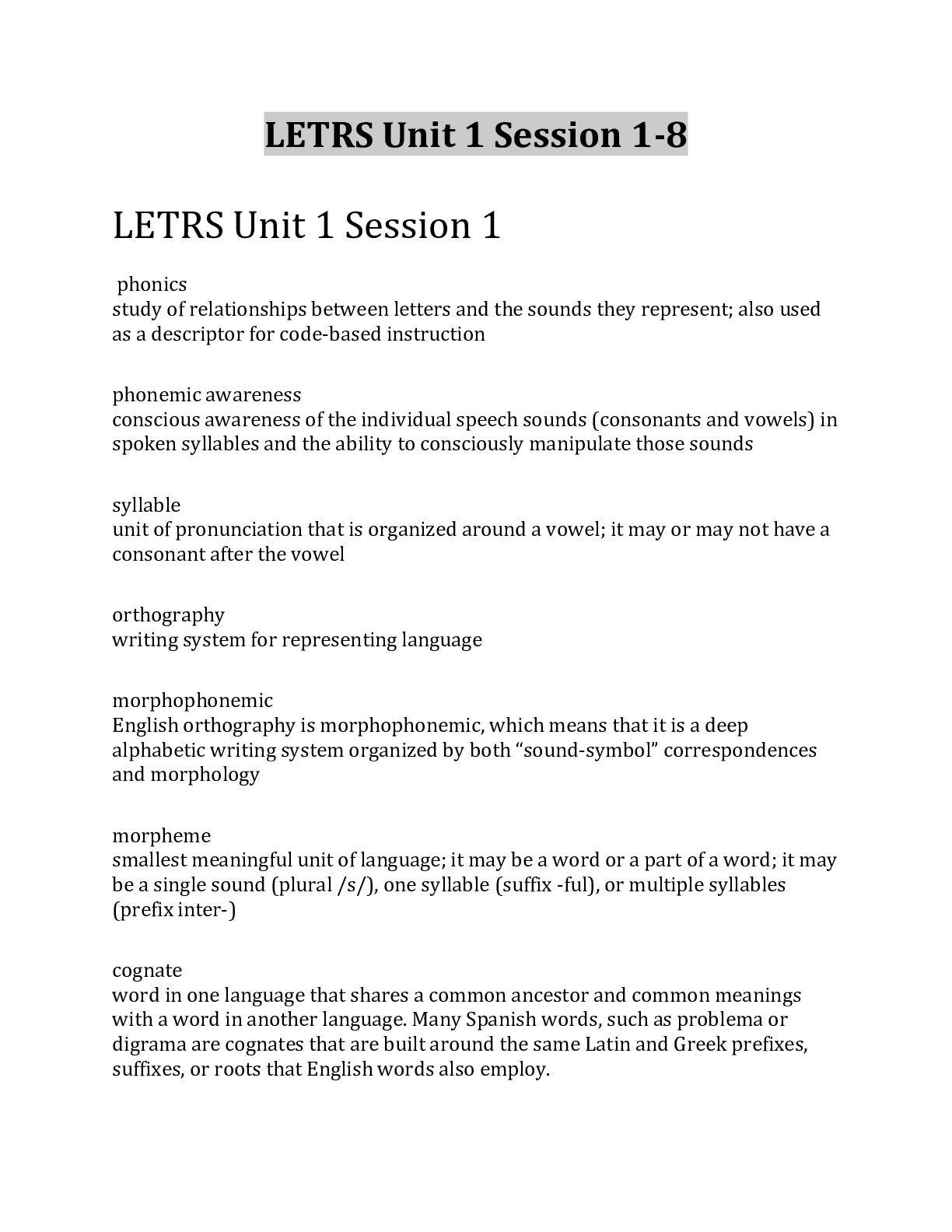

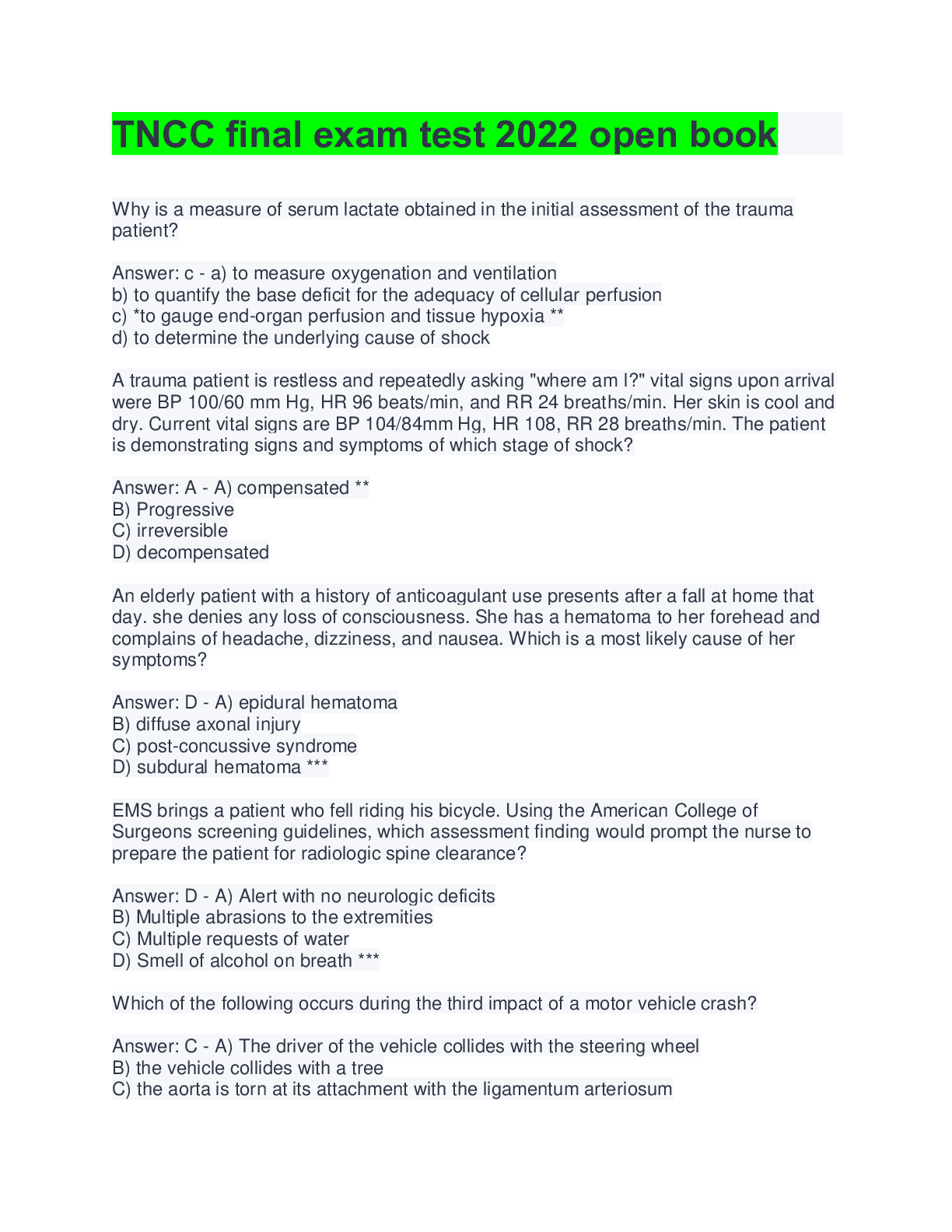
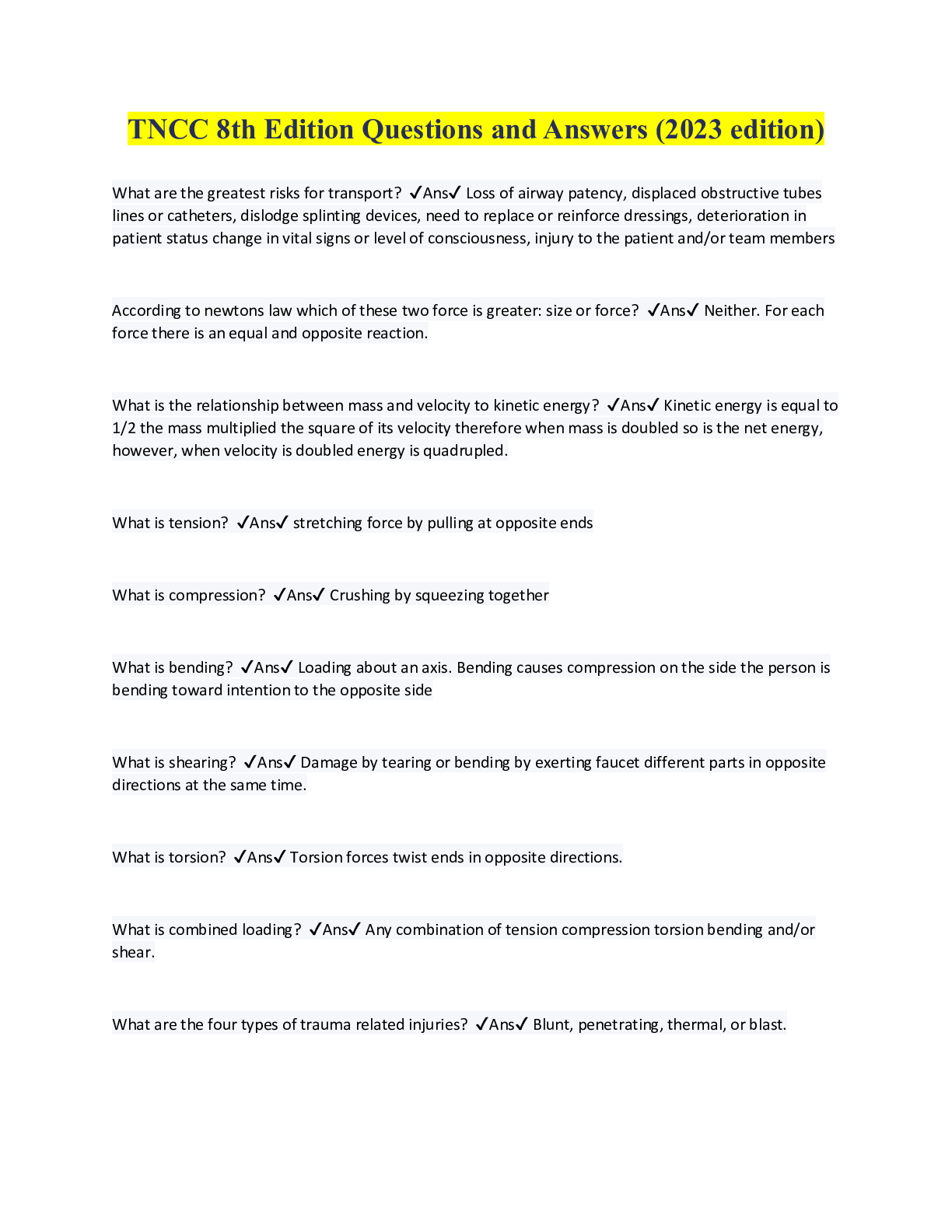
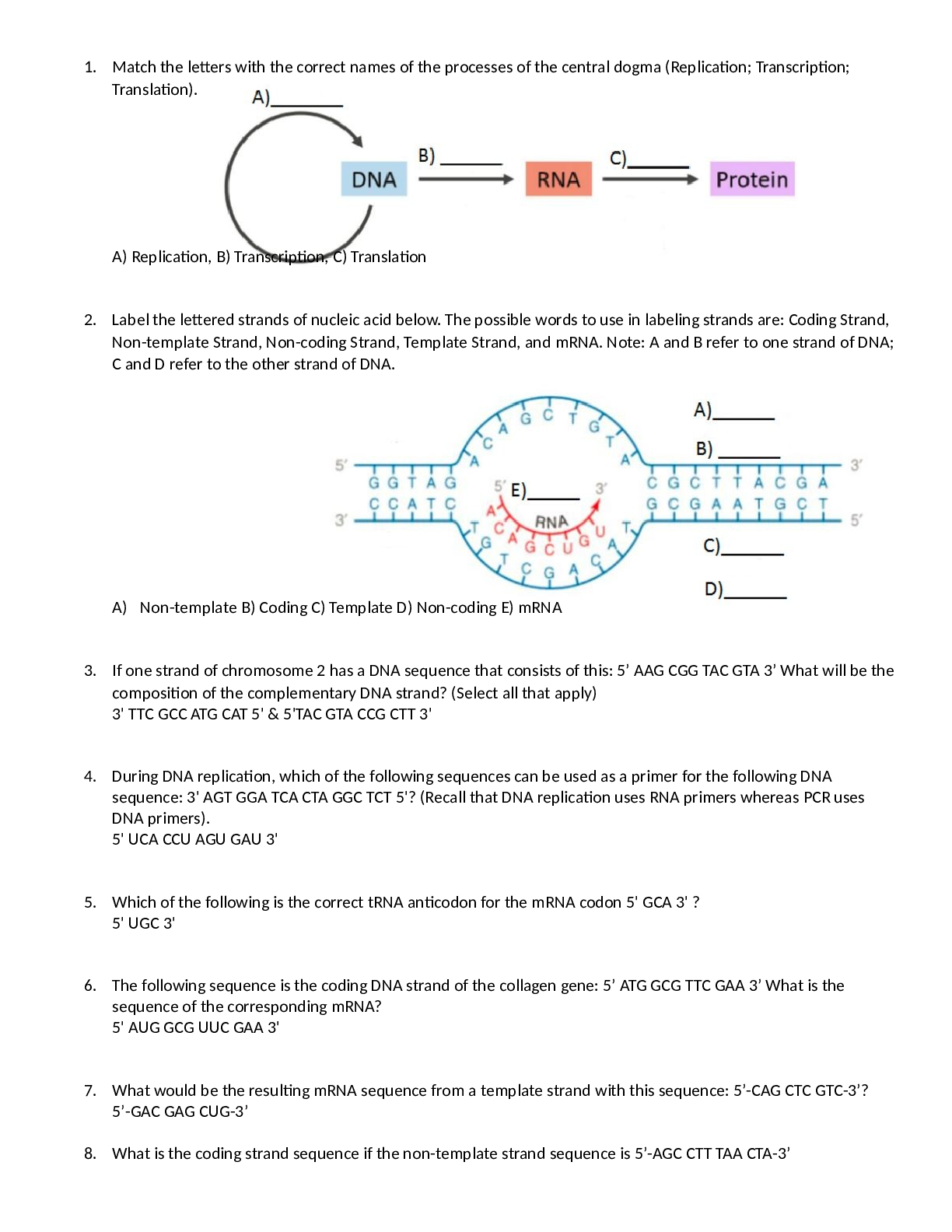
.png)
.png)
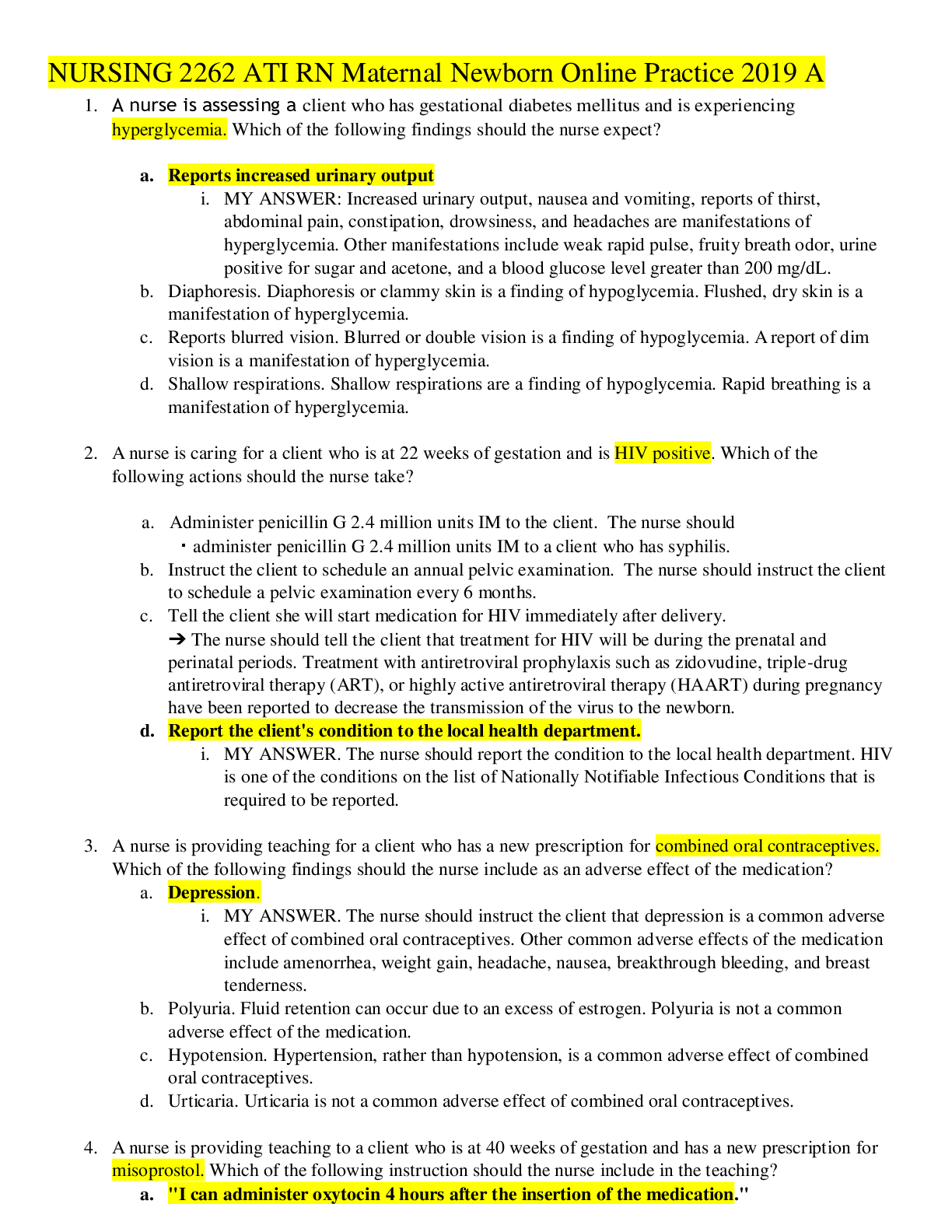
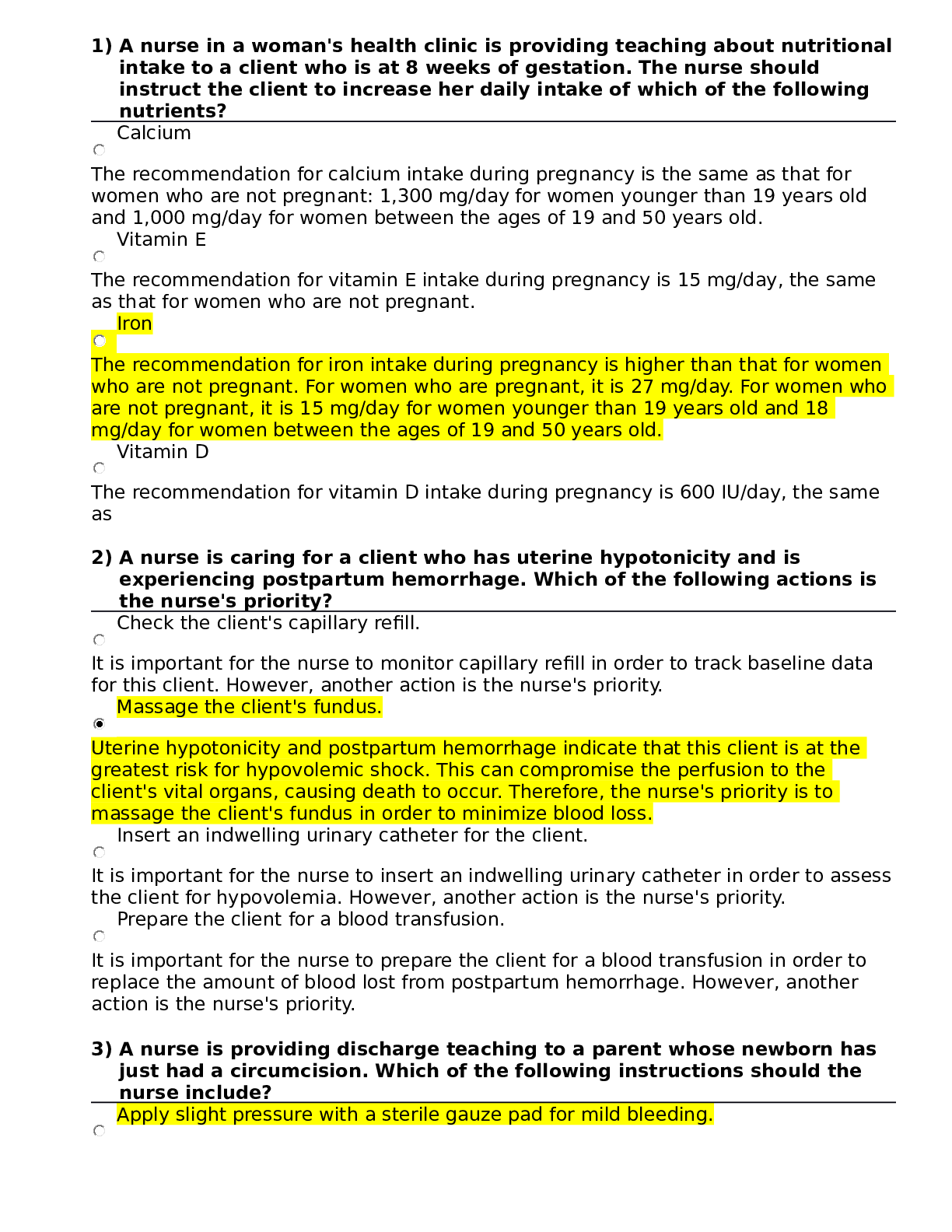
.png)