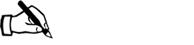
*NURSING > STUDY GUIDE > NR-511 Week 4 Midterm Study Guide Worksheets | COMPLETE GUIDE To Score An A. (All)
NR-511 Week 4 Midterm Study Guide Worksheets | COMPLETE GUIDE To Score An A.
Document Content and Description Below
NR 511 Disease Risk Subjective Finding Objective Findings Diagnostics Treatment Education GI DISORDERS Appendicitis -Most common between 10-30yrs; but can occur at any age; rare in infants and olde... r adults -men more at risk - Diets low in fiber, high in fat, refined sugars, & other carbs at increased risk. - Obstruction of appendix is cause of majority of appendicitis - contributing factors: Intra-abdominal tumors, positive family hx - Recent roundworm infection or viral GI infection -Dx made clinically, based primarily on H&P exam - Classic presentation includes acute onset of mild to severe colicky, epigastric, or periumbilical pain - Pain is vague at first then localizes within 24hrs to RLQ - Pain exacerbated by walking\coughing - Men may feel radiated pain in testes - Abd muscle rigidity, N\V, anorexia - Mildly elevated temp 99-100F common - If RLQ accompanied by shaking chills, perforation should be suspected - Older adults may present with weakness, anorexia, abd distention, mild pain leading to delayed dx and increased morbidity. -May have HTN\tachy proportional to pain\symptoms -When lying flat, may flex R knee to relieve tension in abd muscle -Pain with palpation in abd, diffuse in early stages. Localized to RLQ later -Positive for rebound pain; ask pt to cough to localize pain location -Sudden cessation of pain means perforation and is ER -Labs are not diagnostic and nonspecific -Women should have urine human chorionic gonadotrophin to r\o ectopic pregnancy - +Rovsing’s Sign- deep palpation & release in LLQ causes rebound pain in RLQ - +Psoas Sign- lift R leg against gentle pressure causes pain - +Obturator Sign- flex R hip & knee and slowly rotate internally causes pain - +McBurney’s Sign- pain with pressure applied to point between umbilicus & ilium - x-ray\CT helpful when paired with positive H&P findings -Surgical; preoperative care, NPO, correction of fluid\electrolyte imbalances -Avoid narcotics -Atb with 3rd gen cephalosporin; Ex: ampicillin, gentamycin, flagyl -F\U with surgeon -Ambulation after surgery -Adv diet when bowel sounds return -Return to hosp with s\s of infection -Avoid heavy lifting for at least 2 wks Celiac disease ** (autoimmune disorder caused by an immunologic response to gluten) Mostly diagnosed in adulthood. A family member with celiac disease or dermatitis herpetiformis Type 1 diabetes Many asymptomatic. May complain of diarrhea, gas, dyspepsia, wt loss. Atypical symptoms: fatigue, bone or joint pain, arthritis, osteoporosis, or Muscle wasting (anemia), reduces subcutaneous fat, ataxia, & peripheral neuropathy (vitamin B12 deficiencies) osteoporosis or osteopenia (bone loss) Serologic testing for anti-tTG IgA antibody Total IgA (2% of pts have IgA deficiency and will falsely test negative) duodenal biopsies lifelong adherence to a strict gluten-free diet. Referral to a dietician to help. Some pts may need treatment with immunomodulating teaching related to gluten free diet. Some people with celiac disease have vitamin or nutrient deficiencies that do not cause them to feel ill, such as anemia due to iron Down syndrome or Turner syndrome Autoimmune thyroid disease Microscopic colitis (lymphocytic or collagenous colitis) Addison's disease osteopenia (bone loss) liver and biliary tract disorders (transaminitis, fatty liver, primary sclerosing cholangitis, depression or anxiety peripheral neuropathy seizures or migraines missed menstrual periods infertility or recurrent miscarriage canker sores inside the mouth dermatitis herpetiformis (itchy skin rash) hypothyroidism Pts with dermatitis herpetiformis found to have signs of celiac disease on intestinal biopsy. Test for nutritional deficiencies associated with malabsorption of C.D. (hemoglobin, iron, folate, vit B12, Calcium, and Vitamin D.) agents. deficiency or bone loss due to vitamin D deficiency. However, these deficiencies can cause problems over the long term. Untreated celiac/developing certain types of gastrointestinal cancer. This risk can be reduced by eating a gluten-free diet. Cholelithiasis is the formation of gallstones and is found in 90% of patients with cholecystitis. --Risk factors--2 types of stones (cholesterol and pigmented) a. Cholesterol (most common form): female, obesity, pregnancy, increased age, drug- induced (oral contraceptives and clofibrates: cholesterol lowering agent), cystic fibrosis, rapid weight loss, spinal cord injury, Ileal disease with extensive resection, Diabetes mellitus, sickle cell anemia. b. Pigmented: hemolytic diseases, increasing age, hyperalimentation Patient complaint of indigestion, nausea, vomiting (after consuming meal high in fat), and pain in RUG or epigastrium that may radiate to the middle of the back, infrascapular area or right shoulder. Right side involuntary guarding of abdominal muscles, Positive Murphy's sign, possible palpable gallbladder, Low grade fever between 99-101 degrees. Possible jaundice from common bile duct edema and diminished bowel sounds. Mild elevation of WBC up to 15, 000 Abdominal Xray: Quick, noninvasive, reliable, and cost- effective means of identifying the presence of cholelithiasis. a. Initial management-- begins with definitive diagnosis. When asymptomatic (normally an incidental finding while exploring another problem) require no further treatment except teaching s/sx of "gallbladder attack". Nonsurgical candidate can be treated with dissolution therapy or lithotripsy. Acute includes hydration (IV fluids), antibiotics, analgesics, GI rest. b. Treatment of choice for Acute cholecystitis is early surgical intervention after stabilization. Poor surgical risk may benefit from cholecystectomy operatively or percutaneously. Nonsurgical intervention: weight loss, avoidance of fatty foods to decrease attacks, alternative birth control for persons taking oral contraceptives, menopausal women taking estrogen informed about alternative sources of phytoestrogens (soy products). (artificial supply of nutrients, typically IV), cirrhosis, biliary stasis, chronic biliary infections. Crohn’s ** Ages 15-25 of onset and then again at 50-80. Familial tendency, smoker Carcinoma less common in patients with CD due to treatment sometimes colectomy Mild-Four or fewer loose bowel movements per day, can have small amounts of blood and mucus in the stool, and cramping in the rectum. Moderate-4-6 loose bowel movements per day containing more blood and mucus and other sx such as tachycardia, weight loss, fever, mild edema. Severe- frequent bloody bowel movements (6-10), abd pain and tenderness, sx of anemia, hypovolemia, impaired nutrition. Most common sx are abd cramping/tenderness, fever, anorexia, wt loss, spasm, flatulence, RLQ pain or mass Tenderness in LLQ or across entire abd with guarding and abd distension. DRE performed to look for anal and perianal inflammation, rectal tenderness, and blood in stool. S/Sx of peritonitis and ileus may be found depending on severity of crohns. Tender mass in RLQ, anal fissure, perianal fissure, edematous pale skin tags. Extra intestinal finding may be episcleritis, erythema nodosum, nondeforming peripheral arthritis, and axial arthropathy Stool analysis to r/o bacterial, fungal, or parasitic infection for cause of diarrhea. CBC to check for anemia, eval for hypocalcemia, vit D deficiency., hypoalbuminemia, and steatorrhea. LFT to screen for primary sclerosis cholangitis, and other liver problems assoc with IBD. Check fluid and electrolytes. May have elevated WBC count and sed rate and prolonged prothrombin time. Barium upper GI series, colonoscopy, and CT to determine bowel wall thickening or abscess formation Glucocorticoids, there is no cure for CD and treatment is aimed at suppressing inflammation and symptomatic relief of complications. Initially oral prednisone 40-60 mg/d, tapered over 2-4 months, then can have daily maintenance dose of 5-10mg/d. Sulfasalazine for mild to moderate CD 500 mg BID, increased to 3-4 g/d. Clinical improvement in 3-4 wks, and then tapered to 2-3 g/d for 3-6 months, this medication interferes with folid acid absorption and patient must take supplements. Metronidazole effective in tx perianal disease and in controlling crohns colitis, other ABT’s such as Cipro, Ampicillin, and Tetracycline effective in controlling CD ileitis, and ileocolitis. Immunosuppressive meds when unresponsive to other treatments. Pt educated on disease process, diet and lifestyle changes. Stress reduction, adequate rest to decrease bowel motility and promote healing. Low residue diet when obstructive sx present such as canned fruits, vegetables and white bread Diverticulitis ** -Uncommon under 40yrs; risk rises after -Rare in pediatric; equal in men\women -More common in -25% develop symptoms -LLQ abd pain, worsens after eating -Pain sometimes -LLQ abd tenderness with possible Firm, fixed mass may be identified in area of diverticula -Abd x-ray can reveal free air, ileus, obstruction -Barium studies show sinus tracts, fistulas, -Asymptomatic cases managed with high fiber diet or fiber supplement with psyllium -Mild symptoms managed -Increase fiber in diet to avoid constipation and straining -H2O intake of at developed countries -High in low fiber, high fat\red meat diets -Obesity, chronic constipation, h\o diverticulitis, & number of diverticula which occur in sigmoid colon. relieved with BM or flatus -BM may alternate between diarrhea\ constipation -May present with bleeding w\o pain or discomfort -Fever, chills, tachy; LLQ with anorexia, N\V -Fistula may form causing dysuria, pneumaturia, fecaluria -May have rebound tenderness with guarding\rigidity -Tender rectal exam; stool usually + for occult blood obstruction -Colonoscopy to r\o Ca, but less sensitive than barium for diverticula -CT with contrast outpatient with clear liquid diet and rest -Atb should not be routinely used but can be with diverticula abscess culture -Amoxicillin\clavulanate K (or) flagyl with bactrim -Symptoms usually subside quickly and diet can be advanced slowly -Pain managed with antispasmotics Ex; Levsin, Bentyl, BuSpar -Avoid morphine -NG for ileus or intractable N\V -Pt can be D\C’d from hosp once able to maintain adequate nutrition\ hydration if acute phase resolved -Colon resection may be necessary if no improvement or deterioration after 72hrs of treatment least 8\8oz glasses to promote bowel regularity -Bulk-forming laxative may be needed Ex: psyllium, FiberCon, Metamucil GERD ** -Can occur at any age -Risk increases with age, then decreases after 69yrs -Prevalence equal across gender, ethnic, cultural -Obesity, alcohol, caffeinated beverages, chocolate, fruit, decaf coffee, fatty foods, onions, peppermint\ spearmint, tomato products Anticholinergics, beta- -Heartburn; mild to severe -Regurgitation, water brash, dysphagia, sour taste in AM, belching, coughing, odynophagia (painful swallow), hoarseness or wheezing at night -Substernal\ retrosternal pain -Worsens if reclined after eating, eating large meals, constrictive clothing -H&P usually normal -May be + for occult blood in stool -Usually Hx alone diagnoses -May manifest with atypical symptoms such as adult-onset asthma, chronic cough, chronic laryngitis, sore throat, noncardiac chest pain -If pt fails to respond to 4-8wks PPI, EGD is ordered -EGD warranted over empiric treatment when heartburn & -8wk trial of PPI; weight loss, avoiding triggers -If unresponsive to once daily dosing; can increase to twice daily; if no relief EGD needed -PPI and H2-RA should not be taken together -Pt’s on long term therapy should be re-eval’d q6mos -Weight loss, med compliance and avoidance of triggers -Small frequent meals; main meal mid-day, avoid eating 4hrs before bed, avoid straining, sleep with HOB elevated, smoking cessation, stress mgmt adrenergics, CaChannel blockers, diazepam, Estrogen\ progesterone, Nicotine, Theophylline -May present with dysphagia; dysphagia should only occur with first bite dysphagia, bleeding, anemia, weight loss, or recurrent vomiting -EGD with Barrett’s esophagus q3-5yrs Giardia Can harbor in intestine, protozoan attaches to mucosa of small bowel. In US, risk in adults is oral-anal intercourse, children in daycare. In third world countries, risk of contamination through water sources. Bloating, flatulence, nausea, watery diarrhea, weight loss, anorexia, Malabsorption Stool testing positive for trophozoites 50% of the time. Duodenal aspirate or small bowel biopsy Quinacrine Hydrochloride (Atabrine) 100 mg TID after meals for 5-7 days or Metronidazole (Flagyl) 250 mg TID for 5-7 days Teach good hand washing technique, sanitize surfaces, and avoid swimming in all types of water sources to avoid further contamination. H. Pylori Infection Risks: Increased age, living in crowded conditions, no clean water source (nonfiltered water), smoking Ache or burning pain in abdomen. Abdominal pain that is worse when stomach is empty. Nausea/loss of appetite/unintentional weight loss. Frequent burping/bloating Objective Findings RUQ/LUQ tenderness -Fecal antigen assay -Urea breath Test -Biopsy with histological examination -Serological antibody Standard triple drug therapy is clarithromycin and either amoxicillin or metronidazole with a PPI BID for 14 days. Amoxicillin preferred over metronidazole b/c there are some resistant strands of metronidazole. -Complications (PUD) -Medication side effects Irritable bowel syndrome ** Women more than men, rate 3:1; starts in late adolescence and early adulthood; rare in pts >50 -2 kinds of patients- those with abdominal pain and altered bowel habits, and those with painless diarrhea. -Left lower quadrant pain, sharp and burning with cramping or a diffuse, dull ache, precipitated by eating, The physical exam tenderness in LLQ and over the umbilicus or epigastric area in those with small bowel involvement. Digital rectal exam may reveal tenderness and may exacerbate CBC, ESR, CMP (electrolytes, serum amylase), urinalysis, stools for occult blood, ova and parasites, and cultures. Labs mostly normal and any diagnostic clue as to the cause is Producing IBS include caffeine, legumes (and other fermentable carbohydrates), and artificial sweeteners. alleviate symptoms by eating a lower-fat diet that contains more protein. High fiber diet is good, introduced slowly to avoid Recognize triggers and avoid them. Patients must understand that the goal of treatment is to improve their symptoms, not cure the disease, and that improvement in symptoms can be stress and relieved with a bm or flatus. -The pain does not interfere with sleeping, frequent complaints of abdominal distention, gas, and belching, urgency to defecate, passage of large volumes of mucus within the stool. -frequently associated with psych dg, which presents in the form of anxiety, depression, and somatoform disorders (marital discord, death, or abuse) symptoms. -No weight loss or deterioration in health. -Key to diagnosis is the lack of fever, leukocytosis, or bloody stools. pg579 advanced assessment helpful. If WBC found in the stool = infectious or inflammatory process and not IBS. Rule out food intolerance, lactase deficiency (hydrogen breath test or lactose tolerance test). IBS is often confused with lactose intolerance and can be evaluated by removing lactose from the diet for 2 weeks and monitoring the symptoms. the sensation of bloating, 8 glasses of water per day, probiotic VSL#3 one packet bid, Antidiarrheal medications only temporary. -If diarrhea is severe, episodic use of loperamide (Imodium) 2 mg or diphenoxylate (Lomotil) 2.5–5.0 mg every 6 hours can be used as needed. -Constipation- lactulose or magnesium hydroxide. -Postprandial pain- dicyclomine 10 to 20 mg 3- 4x a day by mouth or hyoscyamine 0.125 to 0.75 mg twice a day. Anticholinergics avoid in glaucoma and bph. Tricyclic antidepressants and ssri in some pt a time-consuming process. Dietary education- fiber intake increase Peptic ulcer disease ** (includes gastric ulcers and duodenal ulcers) 3 major causes: (1) Infection w/ H.Pylori, (2) chronic ingestion of ASA and other NSAIDs, (3) acid hypersecretion such as in Zollinger- Ellison syndrome. Genetics, blood type, personality type, and cigarette smoking may also play a role in the development of PUD. Pts w/ COPD, cirrhosis, renal failure, and renal transplant have higher incidence. Hallmark: c/o burning or gnawing (hunger) sensation or pain (dyspepsia) in epigastrium, often relieved by food or antacids. Pts describe pain episodic pattern of c/o in which the pain tends to cluster and last for minutes, w/ episodes separated by periods of no sx. Almost half w/ NSAID- induced ulcers are asymptomatic. Nocturnal pain: in 2/3 of pts w/ duodenal Pts w/ duodenal ulcers often demonstrate epigastric tenderness 2.5cm to right of midline, but this may also be present in cholecystitis, pancreatitis, non- ulcer dyspepsia, and other GI disorders. Reports of melena or coffee-ground-like emesis usually indicate bleeding ulcer, and perforated ulcer may present w/ abdominal rigidity. Routine lab tests: normal unless significant bleeding or vomiting. Pt actively bleeding à CBC w/ diff. to eval HGB levels is paramount. Most pts w/ upper GI bleeding should have restrictive strategy, defined as transfusing when HGB levels fall below 7 g/dL. Diagnostic standard à upper GI endoscopy. Serology test or direct bacteriological analysis via an esophagogastroduode Aim to relieve pain, heal ulcer, & prevent complication and recurrences. -PPIs: drugs of choice & includes omeprazole, raveprazole, lansoprazole, esomeprazole, dexlansoprazole, pantoprazole. PPIs heal duodenal ulcers in 4 wks therapy and gastric ulcers after 8 wks. -H2-R eceptor Antagonists: Used for mild symptoms with no complication or serious Smoking cessation; avoid foods that precipitate dyspepsia. MUST follow treatment regimen. Educate about side effects such as change in stool color to black with bismuth preparations. If sucralfate with antacid, PPI, H2RA being taken, stress that sucralfate cannot be taken with other meds or ulcers and 1/3 of those w/ gastric ulcers. -Nausea & anorexia sometimes occur in pts w/ gastric ulcers. Vomiting and weight loss indicate more serious complications like gastric malignancy or pyloric obstruction. Pts w/ duodenal ulcers may report a reduction in pain after eating; pts w/ gastric ulcers tend to experience more intense pain after eating. noscopy (EGD) Bx à to check for H. Pylori. EGD is ordered for pts who have failed the standard triple-drug therapy for H. Pylori. A serological antibody (enzyme-linked immunosorbent assay) test can be used detect infection w/ H. Pylori, doesn’t distinguish between active or past (treated) infection and is expensive. Urease is plentiful in pts w/ H.Pylori infection. Breath tests for H. Pylori are based on the production of ammonia from the metabolism of urea by urease à indicate active infection and are noninvasive way of dx H. Pylori. In pts w/ increase in gastric acid secretion is suspected, a fasting serum gastrin level should be drawn. Levels higher than 200 pg/mL should be confirmed on repeat testing and followed by basal and peak acid-output measurements. Zollinger-Ellison syndrome should be suspected in pts disease; treatment for 2 wks. If symptoms persist past 2 weeks, EGD considered. If used for peptic ulcer tx, standard therapy is daily x 6 wks or half the dose bid x 8 weeks (cimetidine, ranitidine, nizatidine, famotidine) -Other agents: antacids were mainstay of ulcer treatment. Do not use antacids with calcium in PUD because calcium causes rebound acid secretion. Sucralfate 1g QID heals duodenal ulcers, bismuth (also has antimicrobial action against H. Pylori), misoprostol (Cytotec) used for prophylactic measure to prevent gastric ulcer formation in pts who use NSAIDs. Triple therapy for H. Pylori is a combination of 2 antibiotics (clarithromycin and either amoxicillin or metronidazole) w/ a PPI BID x 14 days. Amoxicillin preferred over metronidazole due to resistant h. pylori strains. Bismuth subsalicylate & 2 antibiotics is also effective but dosing is QID. with digoxin, ciprofloxacin, phenytoin due to it binding with these meds. whose fasting serum gastrin level is > 600 pg/mL and who have a basal acid output > 15 mmol/hr. Pancreatitis ACUTE\ CHRONIC ACUTE: About 80% of hospital admissions are a result of biliary tract disease (passing gallstones) or alcoholism. --Risk: Infection (mumps), Hyperlipidemia, Metabolic disorders (hyperparathyroidism, hypercalcemia), Drugs (furosemide, valproic acid, sulfonamides, thiazides), Endoscopic retrograde cholangiopancreatograp hy (ERCP), Abn pancreatic duct (stricture, carcinoma, pancreas divisum), Abn Common bile duct and ampullary region, Surgery of stomach and biliary tract, vascular disease (artherosclerosis, severe hypotension), trauma. CHRONIC: Slow progressive process --Risk: alcoholism, diets high in protein combined with high/low fat can further predispose to pancreatic injury from ACUTE: Pain that is intense, abrupt onset deep epigastric pain that last for hours to days. Radiates straight through the back. Pain is often refractory to narcotics. Aggravated by vigorous activity (coughing) and lying supine. Alleviated when seated and leaning forward. Intractable nausea/vomiting. Depending on severity may present with seating, weakness and anxiety. May report ingestion of alcohol or big meal before onset of symptoms. CHRONIC: Patient presents with intractable abdominal pain, weight loss, diarrhea but can be mild (dyspepsia, nausea, vomiting). Abdominal pain normally epigastric/LUQ that may radiate to back or left lumbar region that is described as dull and constant. Pain is aggravated by food or ACUTE: Severe abdominal tenderness over epigastric area accompanied by guarding. Abdominal distension presents in about 20% of patients. Bowel sounds hypoactive or absent if paralytic ileus present. Tachycardia (100-140 b/min) with rapid, shallow respirations. Increased blood pressure due to pain. Temp initially normal but increases to 100.4-102.2. CHRONIC: Mild to Moderate epigastric tenderness without rebound tenderness or guarding. ACUTE: Abdominal Pain Elevated Serum Amylase/Lipase that return to normal after 3-7 days WBC between 12-20, 000 CT of abdomen: provides fast and accurate for definitive diagnosis CHRONIC: CT and /or US of the abdomen to show abnormal size or consistency of pancreas. Evaluation of pancreatic function: Bentiromide Test--collections of normal volume and low in bicarbonate suggest chronic pancreatitis. ACUTE: Management is aimed at limiting severity of pancreatic inflammation, preventing further complications and managing symptoms. Mild symptoms can resolve on its own and managed outpatient conservatively. Fasting is necessary until symptoms have subsided. Maintain fluid status with parenteral fluids Pain medication other than opiates (to prevent pressure within sphincter of Oddi). Introduction of clear fluids implemented once pain free, amylase/lipase levels returned to normal, bowel sounds have returned, Low fat diet as patient tolerates. CHRONIC: Aimed at preventing further pancreatic damage, managing pain and supplementing exocrine and endocrine function. Sustaining from alcohol use. Relief of pain by pancreatic enzymes in some patients and others may need narcotic pain management. Operative ACUTE: Informed the cause of pancreatitis Reduction of dietary intake of fat Abstain from alcohol abuse Drug induced--avoid causing agent Hyperlipidemia-- diet instruction and information on avoidance of factors such as alcohol, estrogens. CHRONIC: Patho of disease and long- term outlook Decrease in frequency in attacks after 5-10 years Medication regimen/Rational for medications (control diarrhea and gain body weight) Pain management if long term narcotic is needed. alcohol, autoimmune disease, genetic mutations, hereditary predisposition, high triglycerides, severe malnutrition, tropical pancreatitis, obstruction caused by stenosis, stones, tumor, cystic fibrosis. alcohol. treatment considered in patients that fail pain management with pancreatic enzymes or analgesics. Malabsorption managed with low-fat diet and oral pancreatic enzymes (Viokase/Cotazym/Pancrea se/Creon/Donnazyme). Salmonella ** One of the major causes of diarrhea worldwide. Three species: S. typhi, S. choleraesuis, and S. enteritidis. Found primarily in chicken, eggs, and livestock, causing 85% of community-acquired Sal monella outbreaks. Individuals must ingest 10,000–1 million organisms to become infected. Duration is 2–5 days; onset is 8–48 hours after ingestion. Patients may become “chronic carriers,” defined as individuals with positive stool cultures 1 year after initial disease. Peak incidence is in summer and fall. Symptoms begin with nausea and vomiting, followed by colicky abdominal pain and bloody or mucoid diarrhea. Enteric fever results from organisms entering the bloodstream via the Present with varying degrees of nausea, vomiting, diarrhea, fever, and abdominal pain and cramping. Symptoms depend on the underlying cause but can also include fatigue, malaise, anorexia, tenesmus, and borborygmus. Individuals with profuse diarrhea may complain of rectal burning and hematochezia from rectal abrasion and bleeding. Patients may complain of symptoms that suggest dysentery, including passage of numerous small- volume stools containing blood and mucus. Reports of voluminous stools are suggestive of a source in the small bowel or proximal colon; small stools accompanied by a sense of urgency suggest a source in the Present with varying degrees of nausea, vomiting, diarrhea, fever, and abdominal pain and cramping. Symptoms depend on the underlying cause but can also include fatigue, malaise, anorexia, tenesmus, and borborygmus. Individuals with profuse diarrhea may complain of rectal burning and hematochezia from rectal abrasion and bleeding. Patients may complain of symptoms that suggest dysentery, including passage of numerous small- volume stools containing blood and mucus. Reports of voluminous stools are suggestive of a source in the small bowel or proximal colon; small stools accompanied by a sense of urgency The physical exam is usually normal except for the aforementioned GI problems. Depending on the degree of dehydration, the skin turgor may be poor, and mucous membranes may be dry. -Vital signs may reflect dehydration, such as a fever with an increased heart rate. Older and very young patients with gastroenteritis m ay show signs of severe dehydration such as orthostatic hypotension and dizziness. Patients who have had prolonged illness and are malnourished may present with edema resulting from hypoalbuminemia. Diagnosis is made by isolation of organism in stool. No treatment Treatment includes trimethoprim- sulfamethoxazole (Bactrim DS) or a quinoline, norfloxacin 400 mg or ofloxacin 400 mg PO twice daily for 7–10 days. Stress proper handling of food, thorough cooking, and good hand washing. bowel lymphatics, causing bacteremia, headache, and myalgias. Tissue abscesses may develop. Stools may be foul smelling. left colon or rectum. Bloody stools suggest mucosal damage and an inflammatory process secondary to invasive pathogens. Frothy stools and flatus suggest a malabsorption problem. suggest a source in the left colon or rectum. Bloody stools suggest mucosal damage and an inflammatory process secondary to invasive pathogens. Frothy stools and flatus suggest a malabsorption problem. is necessary unless associated with fever and systemic disease. Shigella One of the most common causes of bacillary dysentery. Several species: S. sonnei is isolated in 75% of cases in the United States. Because of poor hygiene and overcrowding, it is spread via the fecal–oral route and requires only a small number of organisms to produce disease. Organism causes epithelial invasion of intestinal mucosa. Duration usually 4–7 days and is self-limiting. Incubation period of 1– 2 days after exposure or ingestion of pathogen. See Salmonella See Salmonella Diagnosis is made by isolation of organism in stool or rectal swab. In severe cases sigmoidoscopy shows mucosal hyperemia, friability, and ulceration. Initially patients present with watery diarrhea and high fever. Later colitis- type symptoms develop: Abdominal cramps, tenesmus, urgency, frequent small stools with blood and mucus. Low-grade fever may persist for 2–20 days. Complications can include hemolytic- uremic syndrome and colitis. Treat with Bactrim DS twice daily for 3 days if infection was acquired in the United States. Stress proper handling of food, thorough cooking, and good hand washing. Ulcerative Colitis ** Peak age of onset: 15 to 30 y/o, but may occur at any age. More common Mild: 4 or fewer loose BMs per day associated w/ Tenderness in LLQ or across the entire abdomen, often Digital Rectal Exam: to assess for anal and perianal Initial: nutrition counseling. Parenteral nutrition may be Colonoscopy should be avoided w/ in males. Familial tendency. abdominal cramps relieved w/ defecation, small amounts of blood and mucus in the stool, and sometimes tenesmus Moderate: 4-6 loose BMs per day w/ more blood and mucus. Systemic Sx: tachycardia, mild fever, weight loss and mild edema depending on serum albumin levels Severe: more frequent blood BMs (6-10 per day, abdominal pain and tenderness, Sx of anemia, hypovolemia, and impaired nutrition If Ulcerative Colitis (UC) confined to rectal or sigmoid area, stools can be normal or hard and dry; however, the rectum will continue to dispel mucus containing both RBCs and WBCs. As disease process moves proximally, the stools become looser. Pts may report eating less to decrease BM frequency, which leads to further nutritional deficiencies. accompanied by guarding and abdominal distention. Depending on severity: S/S of ileus and peritonitis may be found. Serological: + for antineutrophil cytoplasmic antibodies (pANCA). Fever & malaise w/ severe disease. Early disease: mucous membrane is granular, friable, and edematous w/ loss of normal vascular pattern. May be scattered areas of hemorrhage that bleed w/ minor trauma. Resulting ulcerations develop after mucosa breaks down, leaving the mucous membranes dotted w/ numerous bleeding and pus- oozing ulcers. Severe disease: Copious amounts of purulent exudate. Periods of remission, sigmoidoscopy always shows some friability and granulation present inflammation, rectal tenderness, and blood in the stool. Dx made by correlating sx w/ hx and physical exam. Stool analysis and Cx are obtained to r/o bacterial, fungal, or parasitic infection (ova & parasites) as cause for diarrhea. Stool is examined for mucus and blood. Contrast radiography and endoscopy primary diagnositic tool to confirm IBD (Irritable Bowel Disease). Sigmoidoscopy, defines the actual extent of the mucosal inflammation. Bx results à chronic inflammation. Colonoscopy to determine the extent of the disease, to avoid perforation, usually reserved for pts who have started tx. necessary w/ severe anorexia or uncontrollable diarrhea. Pts w/ mild-mod diarrhea may benefit from diphenoxylate w/ atropine (Lomotil) 2.5 to 5.0 mg PO BID up to 4x daily, loperamide (Imodium) 2 mg after each BM, or codeine 15 to 30 mg PO Q4-6H. Disease limited to rectosigmoid area: topical steroids or mesalamine. Steroid enemas and foams (hydrocortisone [Cortifoam] 100 mg) nightly x 2 wks. PO formulation of Asacol (5-ASA) med help maintain remission after enemas have been d/c’d More advanced disease: Systemic glucocorticoid in combo w/ sulfasalazine or 5-ASA therapy. Glucocorticoids esp. helpful in controlling extracolonic manifestations à peripheral arthritis, ankylosing spondylitis, erythema nodosum, anterior uveitis, and pyoderma gangrenosum: Oral prednisone (Prelone), up to 40 to 60 mg in single or divided doses, tapered and not d/c’d abruptly. Severe or fulminant: (10 or > bloody stools per day): severe colitis or deep ulcerations because of risk of perforation or development of toxic megacolon. Pts should avoid caffeine, raw fruits, vegetables, and other foods high in fiber à can cause trauma to the already inflamed mucosal surface. Some pts may benefit from lactose-free diet, but not recommended unless a trial produces symptomatic relief. Bland diet high in calories and protein yet low in fat can help to control diarrhea and flatulence and maintain nutrition and weight. Antidiarrheal meds should be avoided in acute phase but can be helpful for pts w/ mild sx. All pts should be informed of disease process, tx options, and expected outcomes. Education about diet and lifestyle abdominal tenderness, fever, colon dilation and tachycardia à require hospitalization, monitor closely for development of toxic megacolon and colonic perforation. If no improvement after 7-10 days; consider surgical intervention. Surgery: Subtotal or total colectomy à prevent perforation of bowel and its complications. Some pts may need fluid/electrolyte management and/or blood transfusions. Most common procedure protocolectomy: Brooke ileostomy, curative and functional procedure. Immunosuppressive agents: azathioprine (Imuran), cyclosporine, and metabolit 6- mercaptopurine (6MP) à used in cases unresponsive to other medical management and in pts who are not surgical candidates. For disease unresponsive to other therapies: anti- tumor necrosis factor (anti-TNF) agents can be used à infliximab (Remicade) 5 mg/kg and adalimumab (Humira) administered SubQ 160 mg @ wk 1, 80 mg @ wk 2, then maintenance of 40 changes. Importance of adequate rest and stress reduction to decrease bowel motility and promote healing. Stress management techniques: guided imagery, referred for counseling if necessary. Provided information and addresses for national organizations à Crohn’s and Colitis Foundation of America: up-to-date info and local support groups. If no S/S of acute attack, they can eat whatever they want or can tolerate. About possibility of parenteral nutrition or oral supplementation during acute attacks. Foods that can cause diarrhea and gas-producing foods should be avoided during acute attacks. Female pts require special guidance and counseling before attempting pregnancy. If pregnancy occurs, mg Q other Wk beginning @ wk 4. Pts w/ toxic megacolon: NG tube placement for intermittent suction, NPO, antidiarrheal meds should be d/c’d. F/E imbalances need corrected: hypokalemia. Total parenteral nutrition may be necessary short term. Daily abdominal x-rays. pt must be followed closely by gastroenterologist Viral gastroenteritis ** Causes of gastroenteritis are numerous; however, bacterial, viral, and parasitic infections are among the most common. Almost all forms of enteric infection manifest with diarrhea. Several different viruses including rotavirus, norovirus, adenovirus, and astroviruses account for most cases of acute viral gastroenteritis. Most are transmitted via the fecal-oral route, including contaminated food and water. Transmission has also been shown to occur via fomites, vomitus, and possibly airborne methods. Peak viral load within the stool is anywhere between 24 to 48 hours after symptomatology. See Salmonella See Salmonella Viral gastroenteritis is a known cause of nausea, vomiting, diarrhea, anorexia, weight loss, and dehydration. Clinical manifestations for viral gastroenteritis are due to the effects that the viruses, along with specific cytotoxins, have on the enterocytes of the intestine. The virus uses the enterocyte to replicate, leading to interference with brush border enzyme production, which in turn leads to malabsorption and osmotic diarrhea [8]. Additionally, viral toxins lead to direct damage and cell lysis of enterocytes and intestinal villa, causing a transudative loss of fluid into the intestine [15]. The Most important goal of treatment is to maintain hydration status and effectively counter fluid and electrolyte losses. Antimotility drugs are the most frequently prescribed and most effective drugs for the treatment of symptomatic gastroenteritis. These agents work by slowing intraluminal peristalsis, thereby slowing the passage of fluids through the lumen, which facilitates absorption. Patients with febrile dysentery should not receive antimotility medications because slowing the intraluminal time may prolong the duration of the disease Prevention of the spread of disease from patients with infectious diarrhea to other individuals. Teaching includes good hand washing and safe disposal of waste products. Any infant or child with infectious diarrhea should not attend day care until the diarrhea has stopped or the child has completed the prescribed course of antibiotics. Good hand washing technique is imperative to prevent household outbreaks of the disease.Patients traveling in high-risk areas should be instructed to consume only safe foods and beverages there and Some studies show viral shedding lasting for several weeks past symptomatology loss of cell function can lead to electrolyte abnormalities which are caused by the loss of transporter functionality. That can lead to acid-base disturbances as well. The virus is then shed through feces, and occasionally in the vomitus. Complete blood counts may reveal a mild leukocytosis in a patient with viral gastroenteritis. Other serum inflammatory markers may also show mild elevation. Patients who are suffering from significant dehydration may demonstrate hemoconcentration on complete blood count testing as well as electrolyte disturbances on chemistry panels. Dehydration may also present as acute kidney injury, evidenced by changes in the BUN and creatinine on chemistry panel. on the airplane leaving the area. HEENT DISORDERS Bacterial conjunctivitis (viral is most contagious) Occurs in fall and winter. More common in children than adults. Discharge is purulent, thick with crusted eyelids shut in the Normal visual acuity. No pupillary abnormalities. No Usually none. Consider culture of exudates for Consider fluorescein staining is corneal abrasion suspected. -Good hand hygiene and eye hygiene. -Use clean Direct contact with secretions or with contaminated objects and surface. morning. Sandy, gritty feeling in eye. Unilateral but usually becomes bilateral due to contamination. photophobia. Lymph nodes NOT palpable. Reddened conjunctiva (both over the eyeball and inside lid) and eyelid swelling. Hallmark symptom of bacterial conjunctivitis is purulent discharge. recurrent conjunctivitis but rarely indicated. Bacterial form is also self- limited. Treatment shortness course if initiated early. Self-limiting in 5-7 days; can delay treatment until third day -Eyedrops or ointment: trimethoprim/polymyxin B (Polytrim), erythromycin, tobramycin, gentamicin, sodium sulfacetamide, or ciprofloxacin, levofloxacin -Contact lens wearers: fluoroquinolones are first line Tobramycin (These medicines include ciprofloxacin (Cipro), gemifloxacin (Factive), levofloxacin (Levaquin), moxifloxacin (Avelox), norfloxacin (Noroxin), and ofloxacin (Floxin) Children: ointment preferred over drops One exception to the rule in regards to the effectiveness of antibiotic drops for all bacterial conjunctivitis cases is gonococcal infections. Gonococcal conjunctivitis is sight threatening because it can affect the cornea, so patients should be sent to the ER immediately. Gonococcal conjunctivitis is associated washcloth each time face is washed. -Change pillowcases daily. -Warm compresses for infectious origin. -do not wear contact lenses until inflammation resolved (1 week); discard current contact lenses. -Discard makeup used. -Symptoms should improve in 2-4 days -Instruct patients to treat the eye that is affected but to start treatment in the other eye if symptoms develop -Bacterial conjunctivitis very contagious; stay home from work or school until 24 hours of antibiotic treatment or as soon as clinical improvement (decreased redness and discharge) with hyper-purulent discharge Corneal abrasion Mechanical or chemical means; Trauma induced by contact lenses, damaged contact lenses, or foreign body. Spontaneous induced and often known as recurrent erosions that stems from a previous injury. More common in young, active patient. Uncommon in older adults. Excessive tearing, severe eye pain and inability to open eye due to foreign body sensation, photophobia, conjunctival hyperemia. Hx of scratching the eye, contact lens irritation, or actual trauma. Patients with recurrent corneal erosion syndrome experience searing pain in the middle of the night. It awakens them, or they feel pain on awakening -Constricted pupil, foreign body, lacrimation. Profuse tearing. -Invert eyelid to r/o foreign body underneath. Stain the eye with fluorescein and use a cobalt blue filter light or slit lamp to inspect the eye for foreign objects or scratches. Areas of epithelial disruption fluoresce green when exposed to a Wood’s lamp. Access visual acuity: should be normal unless abrasion is large. Treatment includes antibiotic eye drops or ointment for 5 – 7 days to prevent bacterial infection. Traumatic/foreign body/recurrent abrasions: Erythromycin ointment OR sulfacetamide Contact lens abrasion: ofloxacin, ciprofloxacin OR tobramycin drops/ointment Oral analgesics for pain Only ophthalmologists should prescribe topical anesthetics due to delayed wound healing and risk of ulceration, scarring, perforation and blindness Tetanus prophylaxis Normal saline to irrigate eye. Patching is not usually necessary. The patient should avoid wearing contact lenses until the abrasion heals. f/u in 24-48 hours if no improvement f/u in 24 hours to assess healing f/u by eye doctor Epiglotittis Common in young children 2-4 years; most common >7 years; may occur in older children and adults. Men > women. Infection with Haemophilus influenzae B (Hib) (most common); streptococci now major pathogen of cause. Odynophagia (pain on swallowing), dyspnea, drooling, stridor. Never use tongue blade or light due to laryngospasm and airway obstruction may occur. Transport to OR for fiberoptic laryngoscope visualization showing that epiglottis is swollen and erythematous (cherry red). Endotracheal tube should be inserted. ER care for adequate airway control. Needs hospitalization for IV antibiotics such cefuroxime (Ceftin), ceftriaxone (Rocephin), or ampicillin/sulbactam (Unasyn). Dexamethasone (Decadron) should also be administered IV and tapered as signs and symptoms resolve. Continuous pulse oximetry and careful monitoring of the patient’s airway are critical. Patients who develop hypoxemia and respiratory distress will require intubation. Eustachian tube disorder Some of the most common causes include conditions causing nasal congestion as is seen with allergic rhinitis, sinusitis, URIs, enlarged adenoids, and pregnancy. Additionally, those who have recently traveled in an airplane or who have been scuba-diving are at risk for ETD. Often people complain of decreased hearing or a fullness in the ears. Hearing may be muffled or diminished. May report an inability to “pop” or “clear” their ears, which normally occurs with changes of barometric pressure. They may have accompanying tinnitus or disequilibrium. Patients may come to you thinking that they have an ear infection due to pain or pressure. They may also be concerned of cerumen impaction if they are experiencing hearing loss. Physical exam findings with ETD depend on precipitating event. Nasopharyngeal examination may reveal findings consistent with allergic rhinitis, sinusitis, or URI. On the affected side, typically you will see a TM that appears retracted or “sucked back.” Diagnosis of ETD is based on the history and physical exam. If pneumatic otoscopy is performed, the affected TM will be immobile. A Weber and Rinne hearing test will reveal conductive hearing loss on the affected side. Key it to treat underlying problem. -If a cold, then nasal saline drops or a neti pot may help. -AOM and sinus infections are treated with antibiotics. -Allergic rhinitis should be treated with nasal steroids and decongestants; however, decongestants are contraindicated in children under 6 years of age. Comfort measures can include acetaminophen or ibuprofen. Patients can be instructed to attempt to relieve pressure by yawning, chewing, or sucking. Holding the nose and blowing out is not recommended due to risk of TM performation. For chronic ETD unresponsive to tx, refer to ENT. Tympanostomy tubes may be placed to equalize pressure. Hyphema (a layer of RBCs - hemorrhage) Usually a result of blunt or penetrating trauma. Vision loss and eye pain; may be Conjunctival injection noted; blood in Based on physical findings but may Possible evacuation of blood by ophthalmologist. Immediate referral to ophthalmologist. May be spontaneous. Spontaneous hyphema is a result of DM, iris melanoma, retinoblastoma, eye tumors, juvenile xanthogranuloma, clotting disorders, sickle cell disease or trait; anticoagulant medications. 70% of cases occur in children; peak between ages 10 and 20. Boys > girls accompanied by nausea/vomiting anterior chamber of eye, visible fluid line in pupil, photophobia, decreased visual acuity include CT, orbital ultrasonography, or US biomicroscopy. Consider hematology studies (like clotting factors) based on history and exam Eye shield; head elevated 30-40 degrees; complete bedrest and dim lighting Pain management, treat n/v; correct coagulopathy; avoid aspirin products, miotics, mydriatics in acute setting Protective eye devices. Control of diabetes and hemophilia. Med education on what to avoid at home. Meniere’s disease Age of onset 30-60; most cases develop in 50’s. Rare in young children and adults >70 years. White Americans of European descent at increased risk. Equally affects men/women. Stress, allergies; high sodium, caffeine, alcohol intake; hormonal changes; changes in barometric pressure; exposure to high noise levels for many years. Inflammatory response of inner ear from insults (blunt trauma, viral infections, allergies, reduced or negative middle ear pressure). Recurrent tinnitus, vertigo, and progressive low- frequency hearing loss or complete hearing loss in severe cases. Acute episode last anywhere from 20min- 3hrs. Attacks rarely last > 4 hrs. Characterized as sudden attacks of nausea, emesis, pallor, diaphoresis, dizziness (spatial disorientation), vertigo, roaring tinnitus, increased pressure, fullness, and hearing loss in affected ear. Rapid movement aggravates symptoms, and possible report of falls or accidents No apparent abnormalities on otoscopic exam unless otitis media present. Dilation of inner ear endolymphatic system present on autopsy. Spontaneous nystagmus is observed after preventing eye fixation by having pt wear 40 diopter glasses (Frenzel Lenses). Is a diagnosis of exclusion; numerous disorders mimic this disease. Careful history, neurologic assessment, and response to empiric therapy. Weber and RInne show sensorineural hearing loss; diagnostic criteria involves 2 episodes of vertigo lasting 20 minutes along with sensorineural hearing loss and either tinnitus or a perception of aural fullness. Audiometry shows low-frequency hearing loss and impaired speech discrimintation. 1st, r/o other cause of symptoms. No proven cure; palliative tx given for reducing symptoms. Acute attacks treated with rest by closing eyes and protection from falling. Vestibular rehab reduces symptoms of unilateral peripheral vestibular dysfunction. Meds: Vestibular sedatives like prochlorperazine for severe n/v; a antihistamine like betahistine to reduce frequency and severity of vertigo attacks. Intratympanic Education on reducing sodium 1g/day, caffeine, and alcohol intake; stop smoking. Manage stress levels. Avoid all ototoxic drugs and polypharmacy. Return if further symptoms worsen or acute episodes increase in frequency. Acute attacks best managed by quiet bedrest and prevention of falls - Familial history. History of migraines, autoimmune conditions (systemic lupus erythematosus), RA, certain thyroid disorders. during episodes. Frequency and severity may decrease over time with hearing improvement post attack, but some episodes may last 24 hours. Cold and warm caloric responses are typically reduced in the affected ear, as demonstrated by electronystagmograp hy or direct patient observation (while wearing 40-diopter Frenzel lenses); the direction of the fast phase of nystagmus is variable. These findings are not diagnostic for Ménière’s disease. dexamethasone used in pts refractory to lifestyle changes. Last resort: Aminoglycosides like streptomycin or gentamicin ablation therapy to reduce unbearable vestibular symptoms. not medicine. Reduce food intake during episodes to avoid n/v. Mononucleosis: primarily caused by EBV Angie RISK -Common: Adolescents, young adults (especially college students) -Rarely: Elderly -Immunocompromised persons. SUBJECTIVE -Gradual onset -Mild to Severe throat pain, but mono tends to be the most painful. -low grade fever -Marked fatigue -Tickle sensation -Head and body aches -swollen lymph nodes in the neck and armpits -swollen liver/spleen or both (less common). -rash -spread through saliva (kissing, sharing drinks/cups. OBJECTIVE -Exudative tonsillitis (50% of cases). -Palatal petechiae -exanthem (rash) maculopapular rash DIAGNOSTIC -VCA (viral capsid antigen Anti-VCA IgM appears early in EBV) -VCA Anti-VCA IgG appears in the acute phase of EBV -Monospot test positive by wk 2-3 (nonspecific heterophile antibody test) and decreases in sensitivity when used at the extremes of age (not recommended for general use). -CBC if viral will show 60% lymphocytes, of which at least 10% show atypical morphology. -fewer normal neutrophils or platelets TREATMENT -No specific treatment for EBV -Relief of symptoms -drink fluids to stay hydrated -get plenty of rest -take OTC medication for pain/fever relief. -No vigorous exercise, sport or heavy lifting -warm salt-water gargle -avoid stress -eat a balanced diet PHARMACOLOGIC: -Acetaminophen for fever, aches, pain--Avoid if elevated liver function. -Ibuprofen: AVOID: -ampicillin or amoxicillin due to increased susceptibility to reaction EDUCATION Instruct patient: -drink plenty of fluids and get plenty of rest. -No vigorous exercise, sports or heavy lifting for 6 wks to avoid rupture spleen. -symptoms may subside in 1-3 wks, but fatigue may last for several more weeks. -perform good hand washing -avoid stress -eat a balanced diet -Contagious for 3 months after symptoms subside and could last as long as 18 mo. -Can be spread -Posterior cervical lymphadenopathy (90%) *OCC. OCCURS -significant tender lymphadenopathy of the draining anterior cervical lymph nodes. -Liver enzymes: abnormal liver function -US-dx splenomegaly -consider rapid strep/throat culture: pharyngitis is similar to presentation of strep. (rash). -Steroids unless severe pharyngeal erythema or tonsillar hypertrophy develops, resulting in obstruction (may prolong illness) -Aspirin (risk of Reye’s syndrome) through saliva, bodily fluids such as blood, sexual contact, organ transplant, cough, sneeze, kissing, sharing food/drinks. Nasal polyps Caused by poorly controlled rhinitis. increases with age, female>male. Associated with cystic fibrosis, Asthma, bronchiectasis, ASA hypersensitivity, chronic sinusitis, primary ciliary dyskinesia (Kartagener syndrome), and laryngopharyngeal reflux. Rhinorrhea, nasal congestion, postnasal drainage, hyposmia (inability to smell), inability to breath through nose, dull headache, facial pain/pressure over middle 3rd of face or No symptoms in some cases. Usually bilateral; if unilateral is reported; check for malignancy Gray-blue to yellow- tan nasal polyps may present with chronic perennial rhinitis If large posterior nasal polyps, examine tympanic membrane for ETD. If unilateral, check for malignancy. Flexible/rigid endoscopy (gold standard of diagnosis) Pale-translucent mass on anterior rhinoscopy. CT scan may help reveal extent of disease and differentiate a polyp from another mass. MRI if neoplasia, mycetoma, or encephalocele suspected. Goal – reduce size or eliminate polyp. Daily intranasal corticosteroid use with saline irrigation 1st-line therapy. Treat for minimal of 12 weeks. Use budesonide, beclomethasone dipropionate, fluticasone, mometasone furoate. Mometasone furoate preferred for children. Short course of oral corticosteroids (14-21 days) and/or doxycycline (21 days) in symptomatic patients despite initial tx. (prednisone, prednisolone, doxycycline) Otitis Externa (AKA swimmer’s ear) ** Common in warmer months. No ethnic predisposition. Men/women equally affected. Those at risk: Immunocompromised pts on corticosteroid therapy or with chronic conditions such as DM. Pseudomonas infection common from excess Acute, often severe otalgia of sudden or gradual onset; may be bilaterally. Pain may be worse at night, more severe when pulling on pinna or earlobes or applying pressure to tragus. Ear canal may be erythematous and edematous; absence or presence of cerumen or accumulation of purulent drainage. Tenderness on traction of pinna and/or pain with Rarely needed if symptoms fits classic pic or otitis externa. Fluid from ear may be cultured and antibiotic sensitivity tested if organisms found. Done for those who Treat pain: local application of heat or ice- pack to outer ear. Nonprescription pain relievers: aspirin or acetaminophen or NSAIDS - 1st line agents. Extreme pain: Acetaminophen/codeine 325mg/5mg 1-2 tabs po Keep ear dry, avoid swimming or submersion of ear during and after acute episodes for 4-6 wks. Use shower caps and ear plugs to shower. Those susceptible to repeated infections, a 2% acetic acid swimming in hot, humid weather, especially in polluted water. Highly chlorinated pool water leads to drying out of ear canal creating potential entry of bacteria and fungi. Inadequate cerumen (a protective barrier). Patients with seborrhea due to excess sebum production. Manual ear picking; forging bodies in auditory canal(like leaving cotton in ear); long use of ear plugs, hearing aids, cotton swabs may lead to local irritation and predispose to infection. Previous ear infections and hx of skin allergies. Chewing may elicit pain. Initially, ear may feel full or obstructed with temporary conductive hearing loss if edema present. May be pruritic. Purulent drainage. Fever/chills. chronic otitis externa may have dryness and pruritus of ear canal. pressure over tragus. May be diffused with complete involvement of auditory canal or localized with focal lesions (pustules or furuncles) along auditory or external ear structures. Sebaceous secretions in those with seborrhea. Fluid may be apparent: Pseudomonas -copious green exudate Staphylococcus infection - yellow crusting with purulent exudate. Fungal infections - fluffy white or black malodorous carpet of growth. Allergic reactions - seen as scaly, cracked, and/or weepy tissue. Frank invasive disease - granulation tissue spreading out from primary site of infection and eroding into temporal bone, do not respond to treatment or those with chronic otitis externa, especially those with purulent exudates indicating bacterial infection. Culture also done for immunocompromised pts. Rule our fungi and mycobacteria in these pts. ESR level may be elevated. CT and MRI used to determine soft tissue or bony involvement in malignant disease. Temporal bone 1st bone affected. q6h OR Acetaminophen/hydrocod one (Vicodin) 325mg/5mg po q8h for 1st 24-48 hours (risk for abuse). To facilitate healing: Clean ear canal to remove Cerumen, exudate, debris with cotton pledget or gentle irrigation using warm water. 1st line agents: Acetic acid/aluminum acetate, acetic acid/hydrocortisone, ciprofloxacin/hydrocortiso ne, ciprofloxacin/dexamethas one, neomycin/polymyxin B/hydrocortisone, and ofloxacin. Liquid ophthalmic preparations of gentamicin and tobramycin may be used otically to cover both P. aeruginosa and S. aureus. Bacterial otitis externa Safe with perforated tympanic membrane (TM): include ciprofoxacin 0.3% and dexamethasone 0.1% (Ciprodex otic); not for 6 months of age. Ofloxacin 0.3% (Floxin otic) 6 months-13 years 5 drops in affected ear daily for 7 days; adults 10 drops in the affected ear for 7 days Not safe with perforated solution may be used prophylactically to acidify ear canal whenever ears get wet. Teach proper method to clean ears using soft cotton pledget NOT swabs, sticks, or agents. Excessive cleaning harmful; small earwax necessary to prevent infection. Cured 7-10 days of treatment. F/U 1 week for uncomplicated pts. If ear wick placed, F/U 2 days for removal and canal cleaning and symptoms should begin to subside in 48h - pt to call if unresolving. F/U daily in hospitalized patients immunocompromis ed on IV therapy. F/U closely in healthy pts with invasive disease. Gallium scans performed to evaluate efficacy outer auricle, or through perforated tympanic membrane. Neck lymphadenopathy not detected. TM: Chloroxylenol 1mg+pramoxine HCL 10 mg + hydrosortisone 10mg/mL (cortone B Aqueous) Colistin 3 mg Neomycin 3.3 mg, hydrocortisone Acetate 10 mg Thonzonium bromide 0.5 mg (Cortisporin-TC Otic) Refractory cases to initial therapy or involve auricular cellulitis required systemic ABX covering both Staphylococcus and Pseudomonas. Given for those immunocompromised or with factors such as DM. 1st -gen cephalosporins or penicillins with narrow coverage, like cephalexin (Keflex) 250 to 500 mg PO four times daily and dicloxacillin 250 to 500 mg PO QID. 2nd-gen cephalosporins with broader-spectrum coverage, like cefuroxime (Ceftin) 250 to 500 mg PO BID or cefdinir (Omnicef) 300 mg PO BID, or beta- lactamase–resistant penicillins like amoxicillin/clavulanate (Augmentin XR) 1,000 mg PO BID based on the amoxicillin component. during follow-up (not CT or MRI). Neomycin, an antibiotic commonly found in otic preparations, is known to cause skin reactions and ototoxicity; limit duration of therapy. Ceftazidime (Ceftaz, Fortaz) 2 g IV q 8-12h or combination of tobramycin (1–1.5 mg/kg IV eq8h, with dosage adjusted by monitoring serum levels and renal function) and ticarcillin (3 g IV Q4H). These regimens carry significant risk of nephrotoxicity, ototoxicity, and bleeding diatheses. Otitis Media More common in infants/young children. Increases in winter months. Native Americans (Navajos and native Alaskans) higher prevalence rate. Americans of European descent. Equal in men/women. Dysfunction in eustachian tube. Genetic conditions such as Down syndrome at risk. Active/passive smoking, crowded or unsanitary living conditions, exposure to wood-burning stoves, family history of OM. AOM risk factors: child in daycare, presence of tobacco smoke in home, and residing in communities where antibiotic-resistance Acute OM: Otalgia, Otorrhea, and fever. Unilateral hearing loss, recent hx of URI. Dizziness, vertigo, tinnitus, vomiting, or nausea possible. Pain subsides with TM rupture and then complain of otic drainage. Recurrent OM: clearance of middle ear effusions between acute episodes of inflammation. Chronic OM: Presents with history of repeated bouts of AOM followed by a period of continuous or intermittent otorrhea lasting for more than 3 months. Pain is rare; hearing AOM: Auralgan otic solution (combination analgesic and anesthetic agent; contra in ruptured TM) may be needed to assess ear. TM may be amber or yellow- orange, or may be infected and pinkish gray to fiery red. T M usually full or bulging in acute cases; absent/ obscured bony landmarks and cone light reflex. Chronic OM: perforated, draining tympanic membrane and possibly granulation tissue. Chronic, foul-smellling otorrhea typical of anaeroobic bacterial infection; a chronic grayish-yellow suppuration may be a cholesteotoma at site Rarely needs if symptoms fit picture of OM. If confirmation is desired, pneumatic otoscopy will demonstrate decreased or absent tympanic membrane mobility in serous, acute, or chronic OME. Tympanometry may be useful if fluid buildup behind middle ear suspected in absence of other clinical signs; a flat tympanogram is consistent with restrictive disease of the middle ear cavity In subacute, recurrent, or chronic cases of OM, cultures and antibiotic Uncomplicated OM may not require specific intervention other than pain and symptomatic relief: Acetaminophen, Ibuprofen. If signs and symptoms of AOM persist for 48 to 72 hours in spite of using systemic analgesics, the child should be reassessed, and antibiotic treatment should be considered. No-day care; no ABX in past 90 days: amoxicillin standard dose Day-care or ABX in past 90 days: amoxicillin high dose. mild PCN allergy: use 2nd generation cephalosporin: cefuroxime axetil (Ceftin), or cefprozil (Cefzil). Severe PCN allergy or cephalosporin allergy: Teach preventive measures: avoid tobacco exposure, exclusive breastfeeding for 1st 6 mths of life or longer, annual influenza 6 months and older, pneumococcal 13 6 weeks of age and older, pneumococcal 23 for high risk children 2 years and older. Demonstrate proper cleaning technique. Bedrest or reduced activity may be suggested in severe cases until fever and pain subside, and the importance of completing the full regimen of all antibiotic therapies should be emphasized. forms of S. pneumoniae are endemic. loss primary concern. OM w/ effusion: absence of s/s of infection. Typically complain of stuffiness, fullness, and loss of auditory acuity in affected ear. May hv pooping, crackling, gurgling sounds when chewing, yawning, blowing the nose. Pain rare. Vertigo rare. Usually afebrile and may have hs of recent viral URI or either allergic or vasomotor rhinitis. of infection. Bullae in rare cased forms between tympanic membrane from M. Pneumoniae or certain viruses. Acute infection: lymphadenopathy of preauricular and posterior cervical nodes common. OME: examination of external ear unremarkable; mucous membranes of nasal and oral cavities may be infected or edematous from recent URI. Decrease tympanic mobility of pneumatic otoscopy. sensitivity testing helpful in guiding alternative treatment. If cultures are obtained, fungi and mycobacteria should be specifically ruled out. sinus x-rays and CT scan to reveal mucosal thickening in middle ear in those with recurrent infection. Weber (sound lateralizes to affected ear) and negative Rinne test (bone conduction superior in duration and volume to air conduction). extended spectrum ABX: Clarithromycin (Biaxin) or a sulfonomide like TMP/SMX; Bactrim Failure of initial AOM tx in Pedi pts with amoxicillin: give Amoxicillin- Clavulanate (Augmentin) Complicated and recurrent OM require tx Avoid swimming until OM clears; immersion in water may lead to otitis externa, complicating the middle ear infection. Keep ear canal dry. T M perforation can be avoided by not using cotton swabs or sharp objects to clean ears. Traumatic injuries to the middle ear should be avoided as well to prevent perforation. All cases, especially with ruptured T M blowing of the nose should be avoided; do gently as possible if needed. Nasal saline used to liquefy nasal secretions and facilitate drainage. Presbycusis (sensorineural hearing loss; not reversible) Affects older adults 50 and >; tinnitus may be associated with presbycusis. Some contributing factors include environmental noise, loss of hair cells, hereditary factors, aging, health, and side effects of medication “difficulty hearing,” hears mumbled or slurred speech, difficult hearing made worse with background noise, men’s voices easier to hear, some sounds seem overly loud, possible tinnitis in one Bilateral hearing loss to high frequencies. Patient unable to hear you clearly at high frequencies. Perform Weber, RInne, and Schwabach tests. For sensorineural hearing loss: Weber (sound in less Revealed by audiometric testing including pure tone and speech testing. Hearing loss irreversible. Education should be provided to avoid further damage such as avoiding loud noises, wearing ear plugs, and hearing aids for hearing. In cases of presbycusis it is important to educate and support the pt so that no further damage will occur; for example, exposure to or both ears affected/unaffected ear is louder). Rinne (air should be 2 as long as bone conduction; but in sensorineural loss, the ratio is equal). excessive noise and ototoxic drugs should be avoided. Rhinosinusitis - viral URI, airplane travel, smoking, air pollution, sneezing with mouth closed, chronic use of decongestants, cold damp weather, dry indoor heat, dental abscesses, swimming in contaminated water, nasal trauma URI, airplane travel, smoking, air pollution, sneezing with mouth closed, chronic use of decongestants, cold damp weather, dry indoor heat, dental abscesses, swimming, nasal trauma. All sinusitis – present with nasal congestion, mucopurulent rhinorrhea, head pressure, maybe cough, maybe sore throat, eye pain, malaise, fatigue. Pain exacerbated by sudden head movements. Frontal sinus pain worsen when lying down; maxillary sinus pain worsen when erect; ethmoid sinusitis associated with retro- orbital pain. Subacute or chronic sinusitis – painless as with some cases of acute sinusitis. Tender sinuses on palpation, nasal congestion, opacification of sinuses on transillumination, red/swollen nasal turbinates Acute sinusitis: total opacification on transillumination On palpation, the affected sinuses may be tender to palpation. Sphenoid sinusitis presents as tenderness over the vertex or mastoids, ethmoid sinusitis as retro-orbital or nasal bridge tenderness, maxillary sinusitis as cheek or dental tenderness, and frontal sinusitis as tenderness of the forehead. In the event of maxillary sinusitis related to a dental abscess, percussion over the affected sinus will produce Noncontrast head CT recommended in more complicated cases, will show sinus opacification, air-fluid level or mucosal thickening Saline nasal flushes, cool- mist humidifier, increase fluid intake, hot shower or compress for facial pain; ibuprofen, tylenol for pain, OTC decongestant (not longer than 4 days r/t rebound congestion); expectorants such as guaifenesin. Prescription drugs: fluticasone (Flonase), mometesone (Nasonex), triamcinocole (Nasocort). Oral antihistamines not indicated unless allergic component is evident. They dry the mucosa, thicken purulent sinus fluid, & slow mucosal drainage. Majority of acute rhinosinusitis cases are caused by viruses rather than bacteria, antibiotics are largely unhelpful Increase fluids to thin nasal secretions, avoid aggravating factors such as smoke, air pollution. Report complications such as peri-orbital swelling, visual impairments, AMS, visual impairments, facial palsy. Avoid OTC decongestants with antihistamine. marked tenderness in the teeth and gums Rhinosinusitis - bacterial Similar to above + persistent blockage of nasociliary sinus drainage, deviated septum, adenoidal hypertrophy nasal polyps, nasal neoplasms, Dx such as immunoglobulin A deficiency, immobile cilia syndrome (Kartagener’s syndrome), cystic fibrosis, HIV, diabetes Similar to above, postnasal and nasal drainage tends to be mucopurulent, yellow/green and pt reports symptoms longer than 7-10 days Similar to above + more mucopurulent drainage Anteroposterior, lateral, and particularly occipitomental sinus x-ray examinations can be done if symptoms show no improvement after 4 to 5 days of pharmacotherapy; Air–fluid levels, mucosal thickening beyond 4 mm, or complete opacification of the sinuses on any of these views is strongly suggestive of sinusitis. Presence of at least 10,000 organisms per mL on Gram stain of sinus aspirates may confirm local sinus infection. No routinely done since nairs have a diverse array of organisms. If allergic disease suspected perform allergy testing. Eosinophilia and elevated total or allergen specific IgE levels. If symptoms last longer than 7-10, antibiotic may be warranted. First-line is Amoxicillin alone or Augmentin 1000 mg/125mg PO BID. May use Bactrim or doxycycline Same as above, in addition to report no signs of improvement with antibiotic Streptococcus Tinnitus Hearing loss Labyrinthitis Meniere’s Disease Otitis media Otitis externa Otosclerosis Ear canal blockage (from cerumen or foreign body) History of high or low BP Head trauma Anemia Hypothyroidism Hyperthyroidism Allergies Chronic exposure to noise damage cilia & auditory hair cells tinnitus Taking certain medications Reversable tinnitus Salicylates Quinine Alcohol Indomethacin Irreversible tinnitus Kanamycin Streptomycin Gentamicin Vancomycin Me: Hearing loss, labyrinthitis, Meniere’s disease, otitis media, otitis externa, otosclerosis, earcanal blockage (from ear wax Significant subjective findings “Sound of escaping air or running water” “buzzing, ringing, or humming noise” Unilateral or bilateral Often not affected by tinnitus until in an usually quiet environment Me: Sound of escaping air, running water, sound heard in seashell, or as ringing, humming, buzzing sound or roaring or musical sound in one or both ears when no environmental noise is present. Subjective tinnitus is more common and heard only by patient. Sound more prevalent and bothersome in quiet environments; less bothersome around noise. May affect sleep, concentration, and cause depression. Significant objective findings Subjective ringing = will not see objective signs of ringing in ears Do orthostatic BP’s Gross hearing tests, Weber & Rinne fork tests Thorough ear exam If unilateral Check for bruit on affected side Palpation of carotid may reveal weak pulse on affected side Consider cardiovascular studies Doppler ultrasound – assess carotids for stenosis EKG – detect changes of atherosclerotic disease Neuro exam Rule out neuro deficits that may suggest a neurologic etiology Me: Objective tinnitus heard with a stethoscope placed over head and neck structures near ear. High blood pressure via orthostatic MRI – diagnostic procedure of choice May reveal ear- related pathology in detail Lab Tests – confirm possible underlying causes of tinnitus CBC – rule out anemia or infection Metabolic studies – rule out thyroid disease, hyperlipidemia, vitamin deficiency, zinc deficiency, electrolyte abnormalities If see drainage in canal culture drainage Me: Lab tests, CBC to r/o anemia or infection. Metabolic studies to r/o thyroid disease, high lipids, vitamin deficiency, zinc deficiency, electrolytes abnormalities. CUlture ear if drainage present. MRI - procedure of choice to evaluate ear pathology or a CT if MRI not possible. Tympanometry to check for presence of 1st line treatment Typically not treated successfully Manage symptoms Treat underlying causative disorder 2nd line treatment Oral antidepressants Effective in reducing symptoms Physical interventions – minimize distress caused by tinnitus Hearing aids Tinnitus-masking devices Eliminate possible offending medications. No successful treatment. No oral meds to help; however, oral antidepressants prove effective in reducing symptoms. Nortriptyline (Elavil), Diazepam (Valium), and Meclizine HCL (Antivert) have been used depending on the reason for tinnitus. If tinnitus due to otitis media, tx with antibiotics or if needed myringotomy. . Find caucaustive factor to Teach coping mechanisms. Avoid excessive noise, wear protective earplugs. Tinnitus-masking devices may help. External white-noise machine. Hearing aids to amplify environmental sounds and suppress tinnitus. Biofeedback for psychological problems may help. Stop smoking, decrease caffeine, chocolate, alcohol, and salt intake. Proper sleep hygiene. Chew gum or swallowing during descent of airplanes. or forign body), cardio disorders, hx of high or low BP, head trauma, anemia, hypothyroidism, hyperthyroidism, or allergies. Chronic exposure to noise. Certain meds w/ reversible effects include salicylates, quinine, alcohol, indomethacin [Indocin], and those w/ irreversible effects include kanamycin, streptomycin, gentamicin, and vancomycin. Strongly associated with aging. Men and Whites have a higher risk. measurements. Perform gross hearing tests, Weber and RInne, otologic exam. Auscultate upper neck proximate to affected ear for possible bruit, and palpate for weak pulse. Cardiovascular studies: carotid doppler to assess for stenosis, EKG to detect atherosclerosis. Neurological exam to r/o other deficits. middle ear fluid, acoustic reflex measurement, or acoustic reflectometry. Screen psychological disorders due to association with depression or as a somatic symptom to acute anxiety help the problem from worsening. Supplement with Vit A, Vit C, cyanocobalamin, and nicotinic acid or with mag or copper. Viral conjunctivitis (highly contagious; usually caused by adenovirus which are associated with URIs or the common cold. Other viruses include HXV, HZV (zoster), and Molluscum contagiosum. 2 types of herpes viruses. HSV-1 typically occurs above the waist, and HSV-2 typically occurs below the waist. HSV conjunctivitis spread by contact with persons who Current respiratory infection (common cold); STDs, hx of contact with infected person Second eye becomes involved within 24- 48h; burning/sandy/gritty feeling; initially unilateral, then bilateral s/s irritation, mild light sensitivity, and swollen lids; foreign sensation. Injected conjunctiva; profuse tearing; mucus discharge; concurrent upper respiratory infections; enlarged or tender preauricular node. If herpetic HSV1 or HSV2, recurrences or vesicles on skin; Corneal infection with the hallmark “dendrite” appearance. If severe viral from Usually none Consider culture of exudates for recurrent conjunctivitis or STD suspected; rarely indicated Immunofluorescence test for herpes simplex or chlamydia Viral swab (10-minute test) for adenovirus is costly, requires 6 passes, and may not be tolerated by children Self-limiting; resolves in a few days to weeks; therapy reduces symptoms. Artificial tears. Antihistamine/decongesta nt drops (naphazoline/pheniramine ) for severe itching Trifluridine (herpes conjunctivitis); or acyclovir po Same as bacterial: hand hygiene Highly contagious; absence from work or school until absence of redness or tearing has resolved. have visible, infected lesions and with persons symptomatically shedding the virus. Meaning, the patient may be experiencing a prodrome of ill- related symptoms such as malaise, low grade fever, pain or tingling near site of the lesions (but the lesions are not yet visible). herpes zoster or simplex: burning sensation, rarely itching; unilateral, herpetic skin vesicles in zoster; palpable preauricular node. Palpable preauricular lymphadenopathy may be present. Hemorrhagic coxsackievirus-related epidemics. DISCHARGE NOT PURULENT which is the difference between bacterial and viral. Allergic conjunctivitis is usually caused by an environmental allergen such as pollen, grass, trees, and so on. Occurrence can be seasonal and can be isolated to the eyes or include upper respiratory allergy symptoms such as rhinitis. Allergies. The hallmark characteristic symptom is itching. Tearing; discharge. There may also be uniquely identifying “bumps” on the conjunctiva which are called follicles and when present are a Hallmark symptom of allergy. Other symptoms can include a diffuse, milky, conjunctival hyperemia; swollen conjunctiva; tearing; and symptoms are almost always bilateral. Treatment is symptomatic. Cool artificial tears, anti- allergy eye drops (either OTC or RX) can be helpful, but prescription drops are very expensive, so start with OTC first. Systemic antihistamines are not very helpful for symptoms. it is important to advise the patient not to scratch as this can result in a corneal abrasion and induces more itching by the inflammatory response. SKIN DISORDERS Acanthosis nigricans: Benign dermatosis May be a sign of hyperinsulinemia and Complain of darkening of the skin or itching. Most often present in posterior neck, flex Obtain fasting blood glucose or HbA1C; Diet and weight loss; d/c offending drugs; treat Encourage diet and exercise. characterized by velvety, hyperpigmented, hyperkeratotic plaques insulin resistance but can be a marker to malignancy. A sign of risk of developing metabolic syndrome. Etiologies include obesity, insulin resistance, genetic syndromes, familial AN, malignant AN, and drug reactions. Most common between 11- 40 and in those with BMI >30; indicator for risk of DM and subclinical atherosclerosis. . URL’s and inter trig IOU’s surfaces (axillae, elbow, inframammary areas, groin and anogenital regions), most often asymptomatic but may cause pruritus. Skin exam: early or mild lesions may appear as a macular discoloration. May have dirty appearance on the affected skin with rough texture. Symmetric hyper- pigmented, hyperkeratotic, velvety to verrucous brown plaques. fasting lipids, thyroid test, electrolytes to r/o DM or other endocrinopathies. Screen for malignancies. Low testosterone levels may be a predictor if AN in male, obese patients. malignancy is associated with malignancy. Tx usually not indicated but Metformin has been shown to reducing AN lesions. It also improves insulin levels and promotes weight loss. Gastric bypass for weight reduction. Acne Acne is a condition that is manageable but not curable. A provider must emphasize this to their patients so there are realistic expectations. Adolescent who has already tried self- treatment for several months Females more likely to verbalize emotional distress over their appearance Some patients’ c/o pain and tenderness if acne is severe Acne can occur at any age, and there are different levels of severity. Acne is classified into three categories mild, moderate, and severe. Facial involvement and other locations such as back, chest, and upper outer arms Mild is a patient with a few papules and some pustules. Lesions are primarily noninflammatory comedones with occasional small papules Moderate acne patients have papules, Adolescent who has already tried self- treatment for several months Females more likely to verbalize emotional distress over their appearance Some patients’ c/o pain and tenderness if acne is severe Diagnosed by its classic location and characteristic lesions. A complete history is crucial to the diagnosis and supplants the importance of most diagnostic tests which are only needed when an underlying predisposing conditions is suspected Good cleanser: benzoil peroxide or salicylic acid Benzoil peroxide can be drying and does tend to bleach towels or sheets, so make sure you educate your patient and parents on these side effects. (first- line therapy) Treating mild acne is best accomplished with a good cleanser and a retinoid with the possibility of a topical antibiotic. For a moderate case of acne, one would prescribe a retinoid, a topical antibiotic, and oral antibiotics. Adapalene is the lowest potency retinoid and good to use Education is a vital component of acne treatment because of the long duration of treatment and potential adverse reactions Wait at least 30 minutes after washing the face before applying topical acne medications (topicals should not be used on sunburned or irritated skin) Sunscreen should be used with all acne medications Avoid oily makeup, pustules, and nodules. Severe acne consists of papules, multiple pustules, and multiple nodules that can be painful. Acne lesions can appear on the face, neck, chest, back, and upper arms. The differential diagnosis should include: rosacea, folliculitis, perioral dermatitis for mild acne. Retin-A Micro is a mid-potency retinoid and good to start with for mild or moderate acne. A patient with moderate acne will need a good cleanser, medium to high potency retinoid, topical antibiotics, and oral antibiotics. For severe acne, treatment includes a good cleanser, topical and oral antibiotics, as well as a medium to high potency retinoid. Medications: Acutane/ Isotrentinoin Used to treat severe acne Derivative of Vitamin A: which is a good option for moderate to severe acne that has failed other treatment options and in whom scarring is a concern. The patient takes the medication for 4 to 6 months and some patients may need a second round of treatment. The medication can cause elevation in triglycerides and liver enzymes. Labs need to be monitored prior to starting medication, at midpoint and at completion. There is a possible risk of developing an inflammatory bowel disorder and a slight increased risk of suicide oily hair conditioners, excessive scrubbing of face, excessive handling of the face from depression (1%). Therefore, patients need to be properly evaluated and advised of this prior to treatment. The most common side effect is chapped lips (which can be really severe) and dryness of skin overall. Accutane will cause serious birth defects if taken during pregnancy so all females who are on Accutane must be tested for pregnancy prior to treatment and started on oral contraceptives. ● Patients should be referred to dermatology for Accutane treatment. Actinic keratosis: Premalignant lesion that can progress to SCC. Most common precancerous skin lesion in light skinned patients, more common in patients 50 years or older (most common in Celtic, Irish, and Scottish descent) Found in sun exposed areas Caused by skin cells that accumulate from repeated sun exposure Continued sun damage from UV radiation damages the DNA in Patient complains of irritated, rough or scaly rash, pruritus, tenderness or stinging sensation Reddened, scaly, rough, or uneven surfaces. Hard or spiny lesion. Sandpaper like texture. Flesh-colored; irregular. Fluorescence using photosensitizing drug (methyl ester of 5- aminolevulinic acid) over area of concern will have a pink fluorescence with the wood’s lamp No evidence to support removal of lesion as most will not turn cancerous however it is standard to REMOVE the lesion(s) Topical Therapy: 5-fluorouracil (5-FU) cream (Efudex, Carac) applied in a thin layer over the lesion BID for 3 weeks, avoid eyelids, lips, and folds of the nose. This treatment causes red, raw, and painful skin in the areas applied which may lead to noncompliance. Exposure to sunlight makes this worse Centered around prevention, avoidance of excessive sun exposure, use of protective clothing, and use of sunscreen. Should teach patients ABCDE mnemonic A= asymmetry B= border irregularity C= color change D= Diameter larger than a pencil eraser epithelial cells Primary lesions: macules or plaques, poorly circumscribed Secondary lesion: erythematous and scaly May feel like sandpaper when touched Not an aggressive form of cancer if/when it changes to squamous cell unless on the lip Imiquimod 5% cream used for face and scalp lesions. Applied 3x weekly for 8 weeks. Diclofenac 3% in 2.5% hyaluranon gell (Solaraza) applied BIF for 60 to 90 days Adapalene 0.1%to 0.3% (topical retinoid)applied daily for 4 weeks and then increased to BID Side effects of these treatments include redness, itching, rash, and dry skin Topical chemotherapy combined with phototherapy with blue or red wavelength have better cosmetic results than cryosurgery. 2 day course Cryosurgery tissue is destroyed by freezing using liquid nitrogen. Hypopigmentation may occur at site of previous lesion Surgical curettage or shave excision are not considered first line treatments for actinic E= elevation from a flat lesion to a raised or evolving lesion keratosis Surgical biopsy is the only way to obtain an intact sample to be analyzed as a way to confirm diagnosis If treatment does not work, no matter the choice always refer to dermatologist Alopecia areata, temporary loss of hair (nonscarring alopecia) Associated with autoimmune endocrinopathies such as Addison’s disease and pernicious anemia. Occurred once or may be recurrent. May state they have gone grey overnight because grey hair is not affected and not lost. Well-circumscribed patches of hair loss on scalp or sometimes on the face, in areas such as eyebrows or the beard. Occasionally only 1 patch is seen, but multiple patches can happen. Upon microscopic study of scalp, short, stubby hairs with tapered ends (exclamation point hairs) are seen on the bald spot. Thorough H&P; Finasteride for men but side effects include decreased libido, erectile dysfunction, ejaculatory dysfunction but these may resolved with prolonged treatment. Monitor liver. Less effective >60 Topical Minoxidil men/women; includes Rogaine. Used in those with <5 years of alopecia and younger than 50. Side effects: irritation, dryness, scaling, redness of scalp. Hypertrichosis in women (excessive hair). >50% hair loss: oral corticosteroid, topical immunotherapy, and immunomodulators; however these have side effects with prolonged used. <50% hair loss: intralesional corticosteroid injections, anthralin cream Hair regrowth occurs after several months with new hair that look thinner and finer than the original hair. No cure. Prognosis good if it occurs after puberty. Cases of persistent alopecia areata has occurred and unresponsive to treatment. or ointment, topical minoxidil solution and foam, or topical corticosteroid creams. Topical treatment with a potent corticosteroid is preferred by PCPs because it is not invasive and is simple to use, although it is not as effective as intralesional injections Atopic dermatitis (eczema) is not considered a distinct entity but is a descriptive term for a group of skin disorders characterized by pruritus and inflammation whose distinct cause is unknown. Eczema is a more general term that is often used collectively to describe skin of an erythematous and inflamed appearance Family history of atopic disease Skin infections Stress Temperature extremes Contact with irritating substance (wearing new clothing prior to washing, harsh soaps, skin products with perfumes) With atopic dermatitis it characterized by an extremely low threshold for pruritus and has been called “the itch that rashes” because the itch almost always comes before the rash appears, and scratching the rash worsens it clinically. A cardinal sign of atopic dermatitis is severe pruritus and diagnosis cannot be made without the history of pruritis. The patient may also report a personal or family history of other atopic conditions (asthma, allergic rhinitis). Rash is often reported as better in the warmer months and worse in the fall and Atopic dermatitis usually begins as infantile eczema, with lesions on the cheeks, face, and upper extremities. Erythema is often seen before pruritus and the acute lesion are excoriated, maculopapular, and inflamed. Eczema presents as a group of pinpoint pruritic vesicles and papules on a coin- shaped, erythematous base and usually worsens in winter. In infancy and early childhood, oozing, and crusting usually characterize the erythema. As children become older, the disease can go into remission or change Usually none done Skin biopsy to rule out other skin disorders 80% of patients may have eosinophilia during episodes of disease activity Serum allergy testing available Nonpharmacologic management: Avoid excessive dry skin Use emollient Soak bathes preferred with lukewarm water Pat dry Moisturize liberally after partial drying Avoid fragrance perfumes and bath oils, avoid cosmetics, deodorants, and preservatives Avoid agents that contain alcohol, lactic acid, or other alpha- hydroxy/glycolic acids that would aggravate their condition Humidifiers are helpful at maintain skin hydration Avoid skin trauma: use Sunscreen Bleach baths: 3 times weekly ¼to ½ cup household bleach in a full tub of water; soak 20 minutes. And liberally apply moisturizer Pharmacologic First step in treatment is to avoid known triggers: Liberal use of emollients to prevent dry skin Avoid known precipitating factors (wool clothing, detergent or soaps with fragrance, etc) Keep environment free of dust as possible Use of air purifiers and humidifiers Eliminate carpets; clean bedding weekly, use mattress protectors to reduce dust mites Wash bedding in 120 to 130 degrees F Humidity in the home should be no more that 50 % Education on winter. to flexural distribution occurring in the antecubital fossa and neck area. Flexural eczema last between ages 4 to 10 but can last into adulthood. In adults, eczema presents with symmetrical lesions that are crusting and excoriated. In its early stages, lesions may be erythematous, papulovesicular, edematous, and weeping. Later the rash becomes crusted, scaly, thickened, and lichenified. The classic locations are noted to correspond to areas that are most accessible to rubbing and scratching, flexural areas are involved. management If skin lesions are wet or have exudate wet soaks or compresses with cool tap water, Burrows (aluminum acetate) solution (1:40 dilution), saline (1 tsp per int of water), or silver nitrate solution (1 to 10%) can be used to dry the lesions and provide comfort. Burrows solution can be applied as a compress for 20 to 30 minutes Topical corticosteroids (creams are preferred) are the mainstay therapy (use lowest potency to control symptoms) Antihistamines (oral or topical) for itching Emollients 2 to 3 times per day (Eucerin, Lubriderm, Cetaphil) Oral corticosteroids may be used in severe cases only for short bursts Topical calcineurin inhibitors Elidel cream 1% or Tacrolimus ointments 0.03% and 0.1% maintenance dosing twice a week for 12 months, use moisturizers on other days Dry skin treated with corticosteroid therapy will exhibit minimal response; however, use for 7 days or less may ease symptoms of erythema and pruritus watching for signs and symptoms of secondary bacterial infection and to report them immediately so that oral antibiotics can be prescribed Bleach baths, are helpful at reducing secondary bacterial infections Keep nails clean, smooth, and short to reduce risk of skin trauma Basal Cell carcinoma Chronic accumulated Adult or elderly patient Appears in areas of Suspicious lesions (if Simple excision of area; Avoidance of (most common”): malignant tumor of the skin that originates in the basal cells of the epidermis. It is a slow-growing and locally invasive tumor that rarely metastasizes. sun exposure. Seen more in older adults and elderly. UV light and IVB exposure. Those of Celtic background (Irish, Scottish, English), light skinned, light haired, blue eyed, freckles, and who sunburn easily. Men more at risk. Hx of skin cancer, basal cell nevus syndrome, precancerous lesions including acitinic keratosis, hx of burn scars or areas of skin damaged by chronic inflammation or ulcers and hx of immunosuppression. Environment hx: us radiation (sunlight), exposure to arsenic, polycyclic aromatic hydrocarbons, or radiation. who presents with complaints of a spot or a bump that is getting larger or a sore that is not healing. Often the lesion appears as a thick, rough patch that may bleed if scratched or scraped. Some patients think they are warts with a raised border and crusted surface. The skin lesion may be pruritic or asymptomatic. skin that are chronically exposed to the sun, such as the face, ears, cheeks, nose, and the neck. Nodulo-ulcerative BCC is characterized by elevated papules that have a pearly appearance, with some crusting. When the crusts are removed, a small amount of bleeding ensues. On close examination, telangiectatic blood vessels are seen on the border of the lesion. Borders appear rolled. A central ulceration is seen during the later stages of BCC lesions. BCC lesions may be the same color as the patient’s skin or have areas of variegated color such as blue, black, or brown. Superficial BCC appears similar to dermatitis, with erythema and scaling bordered by a fine rim. The sclerosing, or morpheaform, type of not located on the face) can be biopsied by an experienced primary-care practitioner or referred to a dermatologist. Because BCC rarely metastasizes, staging of the lesions is not necessary. electrodesiccation and curettage; cryosurgery (liquid nitrogen), and laser surgery. Moths microsurgery has highest cure rate. This method involves less scarring and suited for areas of cosmetic important. imiquimod cream (used five times weekly), topical 5-fluorouracil (5-FU), and photodynamic treatment (used for both nodular and superficial forms) utilizing a photosensitizer with blue wavelength phototherapy to create reactive oxygen species. excessive sun exposure is an important factor in preventing these skin cancers. F/u with dermatologist or oncologist for any suspicious skin cancers. Survivors of nonmelanomatous skin cancer should be informed of their increased risk of developing a second lesion or of recurrence of the original lesion. Thus, these patients in particular should be instructed to report any changes in existing moles or the development of new or rapidly growing lesions. Avoid sun exposure from 11am-4pm; wear protective clothing like long sleeves and hats; wear sung glasses; avoid tanning beds; apply sunscreen as directed. Learn the ABCDEs of malignancy BCC is highly aggressive with a high rate of recurrence, presenting as a white plaque with palpable fibrosis and poorly circumscribed margins melanoma. Performed self-skin physical assessment. Contact dermatitis: A common condition categorized as either irritant dermatitis or allergic dermatitis. Allergic dermatitis is from immunologically mediated response and irritant dermatitis is the result of repeated insults to atopic skin by caustic or irritant substances. Stages of contact dermatitis are: Acute: Erythema and edema Clear, fluid filled vesicles or bullae Exudate, clear fluid Distinct margins Subacute: Lessening edema Formation of papules Less distinct margins Chronic: Minimal edema Scaling skin Lichenification Minimal erythema Family history Continued contact with offending substance: plants, chemicals, soaps, fragrances, rubber Topical drugs: neomycin, thimerosal, parabens, glucocorticoid steroids Occupation: hairdresser, nurses, dental personnel, construction worker, chefs, bartenders, farmers, printing industry Cardinal symptom of contact dermatitis is a pruritic erythematous rash. Often patient not aware of previous history. Patient may not be able to identify contributing factors or substances to the appearance of the rash. In contact dermatitis the inflammatory reaction occurs within 6 to 12 hours of re-exposure. However, the response time varies and depends on the length of exposure, and concentration of the offending substance Contact dermatitis presents with inflammation of the epidermis and is manifested by erythema but does not present with smooth intact epidermal surfaces that characterize hives. Contact dermatitis results in rough, reddened patches but without the skin thickening and discrete demarcation of psoriasis. The acute presentation of contact dermatitis is characterized by weeping lesions with numerous tiny vesicles on an erythematous base that is pruritic it has a burin got stinging sensation. None needed if history indicates obvious cause Patch test of offending substance Nonpharmacologic: Avoid contact with offending substance If contact with offending substance occurs wash skin immediately (within 15 minutes) with soap and water and rinse liberally Soak in Burrows solution (aluminum acetate and water 1:40 dilution), saline solution (tsp/pint of water) Colloidal oatmeal baths Soak in cool water for burning and /or irritation Tepid bath may help with pruritus Pharmacologic: For chronic inflammation, emollients to prevent drying Monitor for bacterial secondary infection Corticosteroids: topical, oral, and/or injectable Calamine lotion for itching Moisture barrier: zinc oxide Antihistamine: topical and /or oral Topical or oral antibiotics if secondary infection The provider should teach that patient and family about the disease course, how to recognize triggers( exposure to allergen or irritant 24 to 72 hours before onset of rash) and prevent future contact, the appropriate use of medications and signs of an exacerbation that should prompt the patient to seek care. The mainstay of prevention is helping patients identify the agents causing the dermatitis and teaching them to avoid exposure, to use protective clothing, gloves, and to prevent spread of contact allergens by avoiding scratching, trimming the fingernails and through handwashing. Eczema Atopic dermatitis(eczema) is not considered a distinct entity but is a descriptive term for a group of skin disorders characterized by pruritus and inflammation whose distinct cause is unknown. Eczema is a more general term that is often used collectively to describe skin of an erythematous and inflamed appearance (SEE ATOPIC DERMATITS) Erythema infectiosum (AKA 5th disease or EI); primarily caused by human parvovirus B19 Peak age 4-12 years; male=females affected; no racial favored; occur in late winter to early summer. Local outbreaks may occur every 2-4 years. School related epidemic and non immune household contacts. Highest secondary attack are for daycare providers and school personnel in contact with affected children. Rash, headache, chills and possible cough pharyngitis (sore throat and low grade fever), rhinorrhea, athralgias and arthritis (joint pain that is moderate, spreading, and symmetrical), nausea, GI disturbances, pruritis (more to sole of feet), fever, myalgia and malaise. Then they will have the rash. Women more likely to have joint pain from this disease. Stage 1: 1st gets fever and sore throat for a few days; then develops “Slapped cheek” (hallmark finding) appearance that spares nasolabial fold, forehead, and perioral area. Last 4 days. Stage 2: Then after a few days, a lacy, reticular erythematous macules on extremities and trunk; spare palms and soles. May be itchy at No need for routine labs; disease self- limiting. IgG and IgM in immunocompromised patients. B19 specific DNA polymerase chain reaction (PCR) testing for fetal infection via cord blood or amniotic fluid as well as for patients with chronic infection or those who are imunnocompromised. Screen pregnant patients who have No therapy is usually needed. Cessation of immunosuppressive therapy allows some patients to clear chronic infections. B19 associated anemia in HIV positive patient may resolve with highly active antiretroviral therapy. 1st line meds: anti- inflammatory agents for arthrotic symptoms; antipyretic for fever, but avoid aspirin in children. 2nd line meds: RBC transfusions or aplastic crisis. IV immunoglobulin Avoid heat because it exacerbates rash. Disease spread through respiratory droplets and blood products. Children with the rash are no longer infectious and may attend school. Pregnant women must avoid exposure to patients with active/chronic infections. Increased cell turnover ( hemoglobinopathy, SS, thalassemia) are at increased for TAC. Immunodeficiency (HIV; congenital), 40% of pregnancy women not immune. this stage. Begins 1-4 days after stage 1 and last 1-6 weeks. Stage 3: 2-3 weeks of the body rash. This rash may come and last up to 3 weeks. Rash may be pruritis and recurrent, exacerbated by bathing, exercise, sun exposure, heat, or emotional stress. B19 may manifest as painful pruritic papules and purpura on the hands and feet. Been exposed to b19. for b19 related refractory anemia or PRAC, especially in immunodeficiency states. Intrauterine RBC transfusions reduce mortality in cases of fetal hydrosphere. Joint symptoms subside in weeks (often by 2 weeks but may last months). Full recovery from aplastic crisis in 2-3 weeks. Erythema migrans (bull’s eye rash) associated with Lyme Disease Tick infested area from April through November. Where ixodid ticks are found. These ticks are common on deer. Initially patient may complained of flu-like symptoms, including fever, chills, and myalgia. May report a rash that grew in size. Most patients with Lyme disease don’t remember a tick bite. Later in the coarse, malaise, fatigue, neck pain and stiffness, and generalized pain may occur. When left untreated, it progresses to arthritis or one or more joints. May complain of memory loss, cognitive disturbances, mood Erythema migrans is typically located on parts of the body where the tick selectively feeds, such as the axilla, groin, and waistline. occasionally pruritic and/or burning, may develop central clearing, and is typically greater than 5 cm in size This rash usually diagnostic of LD. Carditis, neurological manifestations, and radiculoneuritis (triad 2 step process EIA and then Western Blot assay. Children 8 years and > and no pregnant adult patients, give single dose of doxycycline 200mg. Alternative agents include amoxicillin (Amoxil), cefuroxime (Ceftin), and erythromycin (E- MycinAlternative agents include amoxicillin (Amoxil), cefuroxime (Ceftin), and erythromycin (E-Mycin). Wear appropriate clothing to prevent tick bites and avoid high risk areas where ticks reside. Wear tick repellant. After removing cloths, inspect Alikhan groin, waistband areas for ay attached ticks or bites. For those already infected, teach treatment action plan with possible residual symptoms. Re-infection possible if in high changes, and peripheral neuropathy in addition to arthritis. known as Bannwarth syndrome). risk area. Folliculitis: a superficial to deep skin infection of the hair follicles. Mainly caused by gram- positive bacteria, occasional by fungus or by gram-negative bacilli. Bacteria infect the hair follicle at a superficial level which leads to the clinical presentation of little pustules or erythema surrounding the base of the hair follicle. Pseudomonas folliculitis presents as follicular erythematous papules, pustules, or vesicles over the back, buttocks, and upper arms. Associated features include pruritus, malaise, low- grade fever, sore throat and eyes, and axillary lymphadenopathy. This type of folliculitis usually resolves spontaneously within 10 days. Common in middle-age (40-60) and children, especially if immunocompromised. Predisposing factors include diabetes, obesity, a chronic carrier of Staphylococci (present in the nares, axillae, or perineum), poor hygiene, hyperimmunoglobulin E (Job’s syndrome, a primary immunodeficiency disorder), exposure to chemicals and solvents (cutting oils), and chronic skin friction. Wet environment, inadequate chlorinated pools. Those on long term, oral ABX like tetracycline for acne or rosacea or older men with seborrhea. Prolonged steroid users. At risk for Candida folliculitis due to antibiotic use which kills normal flora May occur anywhere on Pt shaves, burrowed someone razor, or was recently in a hot tub. Complains of bumpy rash that can appear anywhere on the body. Rash located on hair follicles of face, forehead, back of earlobes, neck, shoulders, buttocks, torso, or extremities. Usually NOT accompanied by itching. No hx of previous skin eruptions or of pertinent hx of diabetes. Lesions can range from minute white- topped pustules in newborns to large, yellow-white tender pustules in adults. NO involvement of surrounding skin. Eyelids, face, scalp, and extremities most common sites. A hair in the center of the pustule sometimes perforates the lesion. This presentation is a hallmark for diagnosis. Pustules resolve into red macules, which fade to leave post inflammatory hyperpigmented scars in susceptible persons. Folliculitis is usually asymptomatic, but it can be very pruritic and is sometimes accompanied by burning Check adjacent lymph nodes for spreading lymphadenitis. H&P; sampling pustule to identify pathogen for gram strain and culture to help differentiate folliculitis from other bacterial infections. Obtain KOH prep to see under microscope in office if a fungal infection is suspected. Topic ABXs: mupirocin (Bactroban), Retapamulin (altabax), Clindamycin, Erythromycin. Antifungal for fungal – ketoconazole (Nizoral) may be in cream, shampoo, or tablet form With deeper forms of folliculitis, especially in the presence of positive blood cultures or systemic symptoms, an ER referral for hospitalization and IV antibiotics are recommended. Clearance of nasal colonization of Staph. Aureus by treatment with mupirocin intranasally BID x 5 days has been shown to significantly reduce the incidence of recurrent folliculitis. Eosinophilic folliculitis treated with anti- inflammatory agents. 1st- line is systemic indomethacin AND topical corticosteroids. Large pustular lesions with necrotic areas should first be cleansed with a weak soap solution, followed by Gentle cleansing by washing the skin twice daily with an antibacterial soap. Hand-hygiene and good hygiene. Avoid shaving during treatment to allow healing. Electric shaver preferred once shaving is resumed. Avoid burrowing or using older razors when shaving infected areas. Avoid tight fitting cloths. Shaving folliculitis is the result of sebaceous follicles which are colonized by gram negative bacteria become infected due to trauma from shaving. “Hot tub” folliculitis is a form of folliculitis that is caused by pseudomonas aeruginosa, which can withstand temperatures of up to 107 degrees F and chlorine levels up to 3mg/L. skin as a result of trauma or damage to hair follicle from chronic irritation or friction soaking of (or the use of compresses on) the affected skin with saline or aluminum subacetate twice daily. When the skin is softened, the clinician can gently open the large pustules and trim away necrotic tissue. Hand Foot and Mouth Disease (HFMD) a contagious virus mostly occurring in young children which is caused by the coxsackievirus A16 and enterovirus 71. Prior to the rash the patient may a have low- grade fever, fatigue, or sore throat 1–2 days prior to rash Vesicles on the hands and feet with mouth sores. Mouth sores are in almost 90% of the cases and are usually the first sign. There can be more than 10 mouth aphthae (sores) anywhere in the oral cavity and frequently are asymptomatic. The hand vesicles appear with erythematous halos and appear mostly on the soles and palms. Vesicles might appear on the legs, buttocks, and face. The lesions do usually resolve The management is symptomatic care for the patient. The patient or the patient’s parents need reassurance that there won’t be scarring and/or that it is not some other rare skin disorder. The patient is considered contagious 4–6 days prior to outbreak and should not return to school or activities until the lesions are scabbed. around 7 days. Keratosis pilaris – benign skin disorder resulting in hyperkeratinization of the hair follicles; Slight female predominance. Worsens during puberty. Affects 80% adolescents and 40% adults. Frequent in obese patients. Autosomal dominant inheritance. Associated with Ichthyosis, xerosis, & atopic dermatitis. Appears as “chicken skin or goosebumps or sandpaper-like”; usually asymptomatic and improves with age 1-2mm keratotic papules localized to hair follicles most often to lateral aspects of arms and thighs. Underlying hair may be found in some of the papules. H&P; clinical findings Dermoscopy may be of assistance if diagnosis if in doubt. Mainstay of tx: Moisturize to prevent excessive drying of the skin. This improves symptoms but is not curative. 1st-line: lactic acid 12% creams/lotions (e.g., ammonium lactate: AmLactin Ultra, Lac- Hydrin) Urea (in 40–50% topical preparations) Second Line Emollient-based topical steroids (e.g., clocortolone [Cloderm], hydrocortisone [Locoid Lipocream]) ADDITIONAL THERAPIES Topical retinoids: tretinoin (Retin- A), adapalene (Differin), ta zarotene (Tazorac) Tacrolimus (Protopic) ointment SURGERY/OTHER PROCEDURES Microdermabrasion, laser (Nd:YAG, pulsed dye) Resolves in adulthood. Use mild soaps and avoid hot showers; use moisturizers. Lichen Planus Jessica Sparks Lichen planus can mimic psoriasis; its cause is unknown. The lesions appear with shiny flat tops that are a red to violaceous color (red- violet tinged). Other Lichen planus is treated with antihistamines, topical and systemic steroids and retinoids, cyclosporine, psoralens with PUVA, and tacrolimus or pimecrolimus topical preparations. The treatment of lichen planus presentations include small, flat-topped papules and a netlike lesion on the buccal mucosa (reticular lichen planus), penis, and external female genitalia. Malignant oral lesions occasionally occur, but oral carcinoma is rare. Lichen planus may have several presentations and locations. Lesions may be generalized, or they may be located on the arms, trunk, mouth, and genitalia. This disease may last for months to years; it does not have a cure and is best managed by a dermatologist. is best managed by dermatologists. Melanoma Age: Risk increases with age. Skin, Eye, Hair Color: light, blue or green eyes, red or blond hair. Personal History: Any type of skin cancer, dysplastic nevi, congenital nevi greater than 20 mm, blistering sunburn before age 20 years, immunosuppression. Usually no symptoms. Some patients present with a pruritic, ulcerated, or bleeding mole. May have a mole that has changed in appearance after having had the mole for many years. Often presents as an asymmetrical lesion Most melanomas appear on sun- exposed areas of skin. The back and neck are the most common sites in men. The legs are a common site in women. Following a full-body skin assessment, suspicious lesions should be biopsied under local anesthesia by a dermatologist. Excisional biopsy is preferred if melanoma is suspected because measurement of thickness can be made along with Four treatments which may be used in combination: Mohs surgery (or other type of excision), chemotherapy, radiation therapy, and biological therapy. If lesion is found early, chance of complete cure with excision is good. Staging of the lesion helps to determine how it will Prevention should start in infancy, especially in individuals with Celtic backgrounds or family history of skin cancer. Early diagnosis improves treatment outcomes. Early detection made easier by ABCDE. Family History: Melanoma Environmental History: Excessive exposure to ultraviolet radiation, exposure to indoor tanning. with an irregular border, notching, and a diameter greater than 6 mm. Often exhibits variegation in color with blue, red, tan, brown, black, and white. Rarely, tumors might be amelanotic. Early nodular tumors are typically flat and may lack typical characteristics of melanoma. There is an increase in thickness which causes elevation into a firm nodule as the tumor advances. Even though there is an emphasis placed on lesions being more than 6 mm, early melanoma can be smaller than 6 mm in diameter. Diagnosis usually requires skin biospy. Nailbed or subungual melanoma may be observed in older patients and is most commonly found on the thumb or great toe. Posterior nailbed involvement, staging, which is useful as a predictor of prognosis and a guide for treatment. Thickness or depth of melanoma is a critical factor in determining both prognosis and choice of therapy. Breslow depth classification system has been used as a prognostic factor and Clark staging system of tumor invasiveness is used. Clark’s Levels: I - confined to dermis II - extends through the basement membrane and into the papillary dermis (upper portion) III- Extends into the papillary dermis IV- Extends into the reticular dermis V- Invades the deep subcutaneous tissue Breslow’s Method: (% = 5-year survival rate) Less than 1 mm = 92%-97% 1.01-2mm = 81%-92% be managed. If melanoma is located on a limb, high-dose chemotherapy via isolated limb perfusion is available. Circulation of the limb is isolated by a tourniquet at the root of the affected limb. High-dose chemotherapy is infused and limited to the affected limb only, minimizing adverse systemic effects. External beam radiation is usually reserved for palliative treatment. For metastatic lesions of the lung, brain, or viscera that cause pressure on tissue, radiation therapy is used to reduce the tumor’s size and provide pain relief. Biological therapy such as high-dose interferon and interleukin-2 in high-risk patients has shown promise with preventing recurrence. Vaccines are currently being developed that stimulate immune function against melanoma tumors. A- Asymmetry B- Border irregularity C- Color change D- Diameter larger than a pencil eraser (6mm) E - Evolving (changing) over time; elevated (raised) lesion. Proper use of sunscreen (risk doubles with more than five sunburns). Should avoid the sun during the hottest part of the day, daily application of high- SPF sunscreen, wear hats to protect scalp and back of neck. Wearing loose fitting clothing provides some protection if all areas of skin are covered. Tanning beds are hazardous and considered a moderate risk (Class II). Survivors of melanoma should be informed of Hutchinson’s sign, is an ominous physical finding associated with advanced disease. 2.01-4 mm = 70%- 81% More than 4 mm = 53%-70% Diagnosis of melanoma requires excision of melanoma and margins by dermatologist or oncologist. Excisional biopsy is sufficient for removal of atypical nevi. A patient who has dysplastic nevi should receive regular skin surveillance, about every 6 months by dermatologist. Subsequent testing may include a lymph node biopsy via computed tomography (CT) - guided needle aspiration. Lymphatic drainage mapping and sentinel node biopsy have been shown to identify occult metastases by employing a technique that identifies the lymph node specifically draining the area of increased risk of second primary tumor or recurrence of previous lesion. Any change of existing lesion or new pigmented skin lesion should be reported to PCP and dermatologist. Should also report swelling in lymph nodes of neck, axilla, or groin area. the skin that contains the melanoma. This node, called the sentinel node, is excised and examined for melanoma cells. If any cancer cells are present, the remaining nodes in the area are dissected. If biopsy of the sentinel node is negative, metastasis is unlikely and recurrence rates are low. If metastatic disease is suspected, a thorough physical examination, laboratory tests, x-ray studies, and CT scans are done to evaluate for distant metastases. Melasma Butterfly face Pregnancy mask Sun exposure and hormones (e.g. pregnancy, oral contraceptives),; tanning beds. This is seen mostly in women Darkening of skin “hyperpigmentation of certain areas of the skin,” typically on face Clinical impression Skin-bleaching creams (hydroquinone), topical retinoids, laser therapy. Avoid sun exposure,, use sun- screen, wear hats in sun; otherwise a benign condition. Molluscum Most common among -itchy, red, swollen, Tiny pustules which -Thorough H&P; can There is a consensus that -Keep your Contagiosum (viral infection that causes a mild skin rash, wart- like bump); caused by the Poxviridae virus. This virus is encased in a protective sac that prevents the immune system from being triggered. kids between 1 and 12 years old -athletes who have close skin-to-skin contact, such as wrestlers, or athletes who share equipment, such as gymnasts -spread by contact, scratching, autoinoculation, or shaving. -People whose immune systems have been weakened by conditions such as HIV, cancer treatment, or long-term steroid use sore, and infected bump -common placed in children are thighs and arms; -adult presentation is usually in the genital region spread from sexual contact. Soles and palms spared. are 2-5mm, and even have a slight depression in the center of the fles- colored dome. Single or multiple lesions may occur. The rash looks like one or more small growths or wart-like bumps (called mollusca) that are usually pink, white, or skin-colored. The bumps are usually smooth and shiny or pearly-looking, and may have an indented center. Some patients present with erythematous papules and scaling from itching. Due to autoinoculation, the virus can last up to 8 months or longer. be mistaken for genital warts. -Providers often can diagnose the infection by merely looking at the affected area. -A skin scraping viewed under a microscope or a biopsy can confirm the Molluscum Contagiosum treatment should be indicated in patients with extensive disease, secondary complications (bacterial superinfection, molluscum dermatitis, conjunctivitis), or aesthetic Non-prescription over the counter medications for molluscum such as Zymaderm can be used or prescription topical retinoids may be helpful. Oral Cimetidine (Tagamet) 40mg/kg/day for 2 months can also be tried. Cryosurgery with liquid nitrogen; however there may be scaring or hypopigmentation of the skin so educating the parent or patient before this therapy is important. Cryotherapy is an effective treatment Mechanical removal (curettage) of a molluscum contagiosum with a punch tool Chemical methods such as Cantharidin and Potassium hydroxide destroy skin lesions through the inflammatory response youngster from having skin-to-skin contact with another child or adult with molluscum contaglesioniosum . -Good hand hygiene -Don’t scratch or pick at molluscum lesions Exclude patient from activities or sports such as gymnastics or wrestling until they are symptom free or unless they keep lesions covered -Do not share towels, clothing, or other personal items during sports activities avoid sexual activities if legions are private parts they produce. Cantharidin is a topical agent and an inhibitor of phosphodiesterase. Potassium hydroxide is an alkaline compound that dissolves keratin Pediculosis (head lice infestation) Head lice infestations are frequently found in school settings or institutions. Crab lice infestations can be found among sexually active individuals. Body lice infestation can be found in people living in crowded, unsanitary conditions where clothing is infrequently changed or laundered. School children are commonly afflicted, but refugees, urban slums, child labor, jails, orphanages, and fishing communities are vulnerable too itching or scratching in the area of the body where the lice feed. Scratching at the back of the head or around the ears should lead to an examination for head lice eggs (nits) on the hair. Itching around the genital area should lead to an examination for crab lice or their eggs. Scratching can be sufficiently intense to result in secondary bacterial infection in these areas. -The presence of lice on the scalp. -Small red bump on the scalp, neck, and shoulder. -The presence of nits (lice eggs) on shafts of hair Wet combing is a very accurate method to diagnose active head lice infestation. Visual inspection is the method of choice, if one aims to determine the frequency of carriers of eggs or nits. Medicated shampoos or cream rinses containing pyrethrins or permethrin 1% are preferred for treating people with head lice. Products containing pyrethrins, permethrin or malathion 0.5% are available over-the-counter, but those containing lindane 1% or malathion are available only through a physician's prescription.Lindane- based are not recommended for infants, pregnant women, HIV patients, and many other people Avoid physical contact with an infected person Itching may continue for up to 1 wk after successful treatment Soak brushes and combs in rubbing alcohol for 1 hr Do not share personal items: combs, hats, towels, beddings Permethrin should be applied on damp hair and be washed with non- conditioner shampoo. Screen all household members and their close contacts Malathion and pyrethrin should be applied on dry hair completely cover the scalp with medications wash hand after treatment Pityriasis rosea Affects people of both sexes; more common in females, and in 15–30 years age group although also seen commonly in elderly and children The eruption is usually preceded by a prodrome of sore throat, gastrointestinal disturbance, fever, upper respiratory tract infection, viral infection, and arthralgia. Rash can be itchy and patient may have a low-grade fever, headache, and fatigue. 1st a herald patch appears, typically on the trunk. The large lesion is commonly 2 to 10 cm in diameter, ovoid, erythematous, and slightly raised, with a typical collarette of scale at the margin. Collarette scaling is seen typically. 2-3 weeks later, a general rash appears. Resembles shape of Christmas tree on the trunk. Face, Palmar, and sole surfaces usually spared. H&P Management includes antihistamines, and unlike Fifth’s disease the sun could help the rash instead of exacerbate the rash. Acyclovir for 1 week may decrease severity. . Patients may be contagious 7-14 days prior to rash eruption Rash can possible last 1-2 months or even longer. Returning to activities will depend on the patient’s symptoms, by the time the rash has appeared though, the patient is not contagious anymore. Psoriasis Prevalence is highest among Scandinavians, with rates slightly higher in northern rather than southern Sweden, further supporting the role of climate and sunlight exposure in the expression of the disease. Adult men and women are affected with equal frequency. The two peak ages of onset are Patients with psoriasis usually present to the practitioner with concern over “itchy, red, inflamed and dry, scaly plaques that have gotten worse.” Statements about the onset and course of the disease are highly variable among patients. Symptoms usually begin gradually and are confined to Physical examination reveals erythematous plaques surrounded by a thick, silvery scale (which is not easily removed), resembling mica. When these micaceous scales are traumatically removed, multiple small sites of bleeding appear (Auspitz’s sign). In intertriginous areas, maceration and Initial laboratory studies include routine testing with a CBC with differential to assess for infection and a serum chemistry profile with a serum uric acid level. Laboratory tests are generally within normal limits in psoriasis, except for the serum uric acid level, which may be The goal of therapy for psoriasis is to control the disease so that the patient no longer feels physically or psychologically hindered by the skin lesions. For sparse or mild lesions that do not bother the patient, no treatment may be needed. When treatment is indicated, however, the disease is controlled by decreasing epidermal proliferation Psoriasis presents many challenges to both the patient and the health-care provider. For patients with disfiguring and difficult-to-control psoriasis, education and support are central to the treatment process. The patient should be informed of during the late teens to early 20s and in the late 50s to early 60s. Women and adolescent girls tend to have an earlier onset than males, and earlier onset is associated with a more severe disease. There is little to no epidemiological evidence that psoriasis is mediated by infectious agents. Psoriasis has a strong genetic influence, with one-third of patients with psoriasis reporting having a relative with the disease. In family studies, when one parent is affected, 8% of offspring develop psoriasis and tend to have an earlier onset. When both parents have psoriasis, the percentage increases to approximately 40%. The mode of genetic transmission is not yet defined, however. Trauma to normal skin (in patients with preexisting psoriasis) that develops into new psoriatic lesions (Köbner phenomenon) Physical, chemical, electrical, surgical, infective, or inflammatory insults only a few areas (e.g., one or both elbows, the knees, buttocks, or scalp), but psoriasis can also be explosive in onset. Three tools commonly used to assess the severity of psoriasis are as follows: 1. The Psoriasis Area and Severity Index combines the assessment of plaque severity (erythema, induration/thickness, and scaling) and the extent of skin surface area affected; it is the most widely used assessment tool for psoriasis in clinical research and practice settings. 2. The Dermatology Life Quality Index has the patient self-rate the impact of the condition on important aspects of his or her life. 3. Affected body surface area is an assessment of the overall skin area involved by percentage. moisture prevent dry scales from accumulating, but the lesions remain red and sharply defined. Lesions usually are distributed symmetrically over areas of bony prominences such as the elbows and knees. Scaly plaques also occur frequently on the trunk, scalp, intergluteal cleft, and umbilicus. The latter three areas are frequently overlooked by the patient and clinician but are important in making the diagnosis, especially in patients with associated psoriatic arthritis and limited skin lesions. In fact, the nature of such inflammatory arthritis may only become apparent after typical psoriatic skin lesions are recognized. Nail involvement may include stippling or pitting of the nail plate or a yellow to red-brown coloring (“oil-staining”) of the nails (nail psoriasis). elevated (hyperuricemia). In more severe variants of psoriasis, other specific tests may be ordered. Throat culture is appropriate if Streptococcus pyogenes infection is suspected as the precipitating factor (as in guttate psoriasis). Immunoglobulins are generally normal, but selective IgA and IgG deficiencies are observed in some patients. In pustular psoriasis, leukocytosis and hypocalcemia are seen. An elevated erythrocyte sedimentation rate and decreased albumin levels, along with anemia, can be observed in chronic disease. X-ray studies of the hands are sometimes helpful to search for associated psoriatic arthritis in patients who complain of joint pains in their hands. X-ray of patients with psoriatic arthritis will show extensive erosion and luxation of distal and underlying dermal inflammation through the use of topical corticosteroids and other immunomodulatory agents, along with phototherapy in some patients. Systemic agents are reserved for moderate to severe or recalcitrant cases. Topical agents are first-line pharmacotherapeutics for psoriasis that are usually effective. If less than 20% of the body (e.g., no more than the elbows, knees, ears, and scalp) is involved, topical agents are usually sufficient. However, if more than 20% of the body is affected and manifestations are moderate to severe, systemic therapy may be warranted, and referral to a dermatologist is recommended. For stubborn, persistent, and widespread lesions, ultraviolet (UV) light treatment should be strongly considered. Systemic therapy in psoriasis is usually used as a last resort because the significant effectiveness of biological agents must be weighed against their high cost and side-effect available community resources and support groups. Explanation of the disease process and treatment, including potential adverse effects of medications, is helpful. A newly diagnosed patient and his or her family should be reassured that the disease is not contagious or infectious. Patients need to understand that psoriasis may be an added risk for health problems in the future, such as cardiovascular and psychological comorbidities. Overweight and obese patients should also undergo dietary counseling. Although the genetic aspects of psoriasis are complex and incompletely characterized, it may be explained to family members of a patient that if neither of the patient’s parents has psoriasis, the Infections: HIV, Streptococcus Endocrine and metabolic factors: Postpartum period Hypocalcemia (e.g., after dialysis and parathyroidectomy) Weather-related factors: Extreme cold weather Prolonged exposure to sunlight* or hot, humid weather (more exacerbations occur in summer) Medications: Systemic corticosteroids Lithium Beta-adrenergic blockers Antimalarial drugs NSAIDs Psychogenic factors: Stress Mood disorders, e.g., depression Other factors: Fatigue Alcoholism Smoking An accumulation of yellow debris under the nails, simulating a tinea infection (tinea unguium), is seen in some patients. Swelling, redness, and scaling of the paronychial margins occur often and are associated with arthritis of the distal interphalangeal joints. The clinical course of this disease is characterized by chronicity and seasonal fluctuations, with improvement in the summer (due to sun exposure) and worsening in the winter as dry skin leads to epidermal injury. Up to 10% to 20% of patients with psoriasis may also have an inflammatory arthritis known as psoriatic arthritis, although the most common form of arthritis seen in psoriasis patients, as in the general population, is osteoarthritis. interphalangeal or metatarsophalangeal joints bilaterally, with characteristic “pencil- in-cup” erosive abnormalities of the interphalangeal joints. In these abnormalities, the distal head of a bone becomes pointed like a sharp pencil, while the adjacent articular surface becomes rounded, like a cup. Biopsy is seldom necessary because the clinical features of psoriasis are so distinctive. Of note, the sudden onset of psoriasis, in particular erythrodermic forms, may be associated with HIV; thus, the presence of underlying HIV infection should be ruled out in such patients, if unknown. profile. Systemic therapy is reserved for patients with severe incapacitating disease—pustular, guttate, and/or arthritic psoriasis. It is administered only by expert specialists such as rheumatologists or dermatologists who regularly use systemic antimitotic agents, including methotrexate, etretinate, and cyclosporine. Monitoring of blood counts, including platelets, should be done weekly in patients taking methotrexate, followed by monthly testing. Renal and liver function tests (baseline and follow-up studies) should be done. Intermittent liver biopsies may be needed with chronic dosing because hepatic fibrosis may occur with prolonged use. Methotrexate is teratogenic and should not be given to those who are pregnant or who want to become pregnant. Utilization of complementary therapies for psoriasis is growing. Therapies include dietary modifications, herbs and supplements, mind–body therapies (e.g., chances are less than 10% that another child will develop the disease. If one parent is affected, the chance of a child developing psoriasis increases to 15%. If both parents are affected, the chance increases to approximately 60% that one or more children will have the disease. The clinician should educate the patient that there are several ways of remaining in remission, once treatments have taken effect. Patients with psoriasis should avoid skin trauma and should keep the skin relatively dry to decrease pruritus, scratching, and scaling. They should avoid photosensitizing medications such as tetracyclines, sulfa drugs, or phenothiazines. If drugs of these types are necessary, patients should be aromatherapy, yoga, meditation), physical therapy, exercise, acupuncture and tai chi. Much of the evidence supporting the use of complementary therapies for psoriasis and psoriatic arthritis is anecdotal, however, and certain practices such as dietary restrictions may actually be harmful, if key nutrients are removed from the diet. advised to inform the prescribing physician of their psoriasis and to ask for a possible alternative. Although photosensitizing drugs should be avoided, controlled sun exposure during the summer is beneficial, although patients should be advised to use a high-SPF sunscreen to prevent sunburns. Patients should also be informed to seek treatment immediately for streptococcal infections (e.g., skin infections, sore throats), and that other aggravating factors for psoriasis include increased stress and alcohol. The clinician should explain to the patient that dietary manipulations do not appear to play a role in treating psoriasis. However, healthy eating habits support a strong immune system, and nutritionists recommend a low- fat, high-fiber diet for patients. Naturopaths recommend many herbal medicines to improve psoriasis and to control or provide relief from the disturbing effects of these flare-ups (e.g., capsaicin, tea tree oil, turmeric). Although many persons subscribe to these therapies, there is a lack of data from randomized clinical trials to confirm their effectiveness. Rosacea Most common in people 30-60 ears of age who are of Irish, English, Scottish, Welsh, or eastern European descent. Patients sometimes have one or more close relatives with the condition. Women are 3 times more likely to develop rosacea than men, especially cutaneous vascular manifestations leading to erythema of the central face. Triggers: Sun exposure, Patients with rosacea usually do not seek care because they mistakenly think they have acne, a sunburn, or temporary rash. Usually present because they become intolerant of the persistent burning, itching, or stinging sensations on the face, in particular. Patients with ocular rosacea complain of watery, irritated, or bloodshot Initially the patient’s forehead, cheek, nose, or chin may have a rosy hue without comedones. This is the central third of the face and is referred to as the “flush/blush” area. There may be inflammatory papules, pustules, and telangiectasias. Scarring is usually unapparent unless the patient also has concomitant acne. There is no diagnostic test for rosacea; physical assessment is the key to diagnosis. Although there is no cure for rosacea, if treatment is started early, some of the cutaneous manifestations may be prevented. The key to management is early diagnosis and avoidance of triggers because rosacea is a chronic condition with no known cure. Topical treatments should be the mainstay of therapy. Potent topical corticosteroids should be avoided because they may worsen the condition. Metronidazole cream is the mainstay of therapy but it may take up to 6 to Patients should be taught about the events or circumstances that can trigger a rosacea flare-up and learn how to avoid them. Sunscreen with a sun protection factor of at least 15 should be used on all exposed skin surfaces when outdoors. Patients should stay cool on hot or cold weather, wind, overheating during exercise, excessive alcohol ingestion, hot beverages, spicy or aged food products such as cheese, emotional stress, irritating cosmetics, hot baths, saunas, hot tubs, smoking, caffeine, and excessive washing of the face. Inflammation instead of infection seems to be the primary mechanism. eyes. Although the lesions tend to be symmetrical bilaterally, they may appear on only one side. Seborrhea may also be seen. If there has been ocular involvement resulting in blepharoconjunctivitis , there will be redness of the eyelids and conjunctiva. With prerosacea, the clinician will note a rosy-cheeked, ruddy complexion on a patient who never develops the full clinical spectrum of the disease. There is no effective treatment for prerosacea, nor is any needed. Patients should just be observed for signs of developing rosacea and encouraged to use sunscreen. There are four subtypes of rosacea classified by the pattern and grouping of symptoms: • Subtype 1: erythematotelangiect atic rosacea—flushing and persistent 8 weeks for a therapeutic response to be seen. If metronidazole (0.75% or 1%) is not effective, other topical antibiotics may be tried. Topical ointments such as tretinoin and azelaic acid are also recommended. Antibiotics should be reserved for flare-ups or when initiating therapy with topical medications, after which antibiotics should be discontinued. Clinicians should taper the dose as soon as possible; typically patients can readily learn how to taper the dosage at home. Treatment with tetracycline, minocycline, or doxycycline typically delivers a rapid therapeutic response. Antibiotic therapy is usually effective in reducing acneiform lesions, and this helps confirm the diagnosis of rosacea. These antibiotics typically work more as anti-inflammatory agents rather than as anti- infectives. The flushing and flat telangiectasias of rosacea tend to persist and do not respond well to antibiotic therapy. In refractory cases, isotretinoin may succeed hot days and protect their face from cold air and wind by using a scarf. Caution should be used when exercising, and patients should be encouraged to exercise for shorter, more frequent intervals, using a cool towel around the neck and taking frequent water breaks. Gentle cleansing with fragrance-free facial cleansers should be encouraged. Proper use of topical creams and lotions should be stressed, along with the use of minimal antibiotics. redness, which may include visible blood vessels • Subtype 2: papulopustular rosacea—persistent redness with transient bumps and pimples • Subtype 3: phymatous rosacea— skin thickening usually with hyperplasia of the nose, resulting in a large, bumpy, and bulbous appearance • Subtype 4: ocular rosacea—ocular manifestations with dry eye, tearing and burning, erythematous eyelids, recurrent styes, and possible vision loss from corneal damage. when other measures have failed. Electrocautery with a small needle may be used to destroy small telangiectasias. Larger telangiectatic vessels may require laser treatment (intense pulsed light therapy). For men with rhinophyma, surgical reduction may be used to reduce the bulbous appearance of the nose. Roseola Infantum (AKA 6th disease) – caused by the human herpes virus types 6 and 7. Virus is mild and common in children under age 2; spread via saliva. Short lives 3-5 days Symptoms: high fever, irritability, diarrhea, cough, and cervical lymphadenopathy. The skin rash presents with light pink, erythematous macules and papules on the face, neck, and extremities. Rash resolves in 1-3 days. Scabies Poverty, overcrowding, poor hygiene, malnutrition, sexual promiscuity Generalized itching and is occurring in finger webs, flexor surfaces of wrist, Lesions (inflammatory, erythematous, pruritic papules) Easily missed Consider diagnosis in patient of any age with persistent & 1st line treatment Lotions containing scabicides: Permethrin lotion Do not exceed recommended exposure times of medication (wash Occurs mainly in children, young adults, health-care workers, institutionalized persons Hot tropical climates; immunocompromised patients elbows, axillae, buttocks, genitalia, feet, ankles, and spared head/neck in adults Potential contact with infected person. Asymptomatic for 3-4 wks after initial/primary infection commonly found in finger webs, flexor surfaces of wrist, elbows, axillae, buttocks, genitalia, feet, ankles, and spared head/neck in adults Pustules may be from secondary infection Prutitic nodules in covered areas (buttocks, axillae, groin) Crusted scabied (or Norwegian scabies) is a psoriasiform dermatosis occurring with hyperinfestation with thousands/millions of mites (more common in immunosurpressed patients) severe pruritus Burrow Ink Test Rub felt-tip marker over suspected burrow Remove excess ink with alcohol wipe Remaining ink will concentrate in the burrow tunnel Once burrow identified Drop mineral oil over burrow Scrape off burrow with #15 scalpel blade Scrapings onto slide identification of S. Scabiei mite, eggs or fecal matter = + diagnostic Just because no + diagnostic, does not rule out scabies 2nd line treatment Lindane 19% (gamma- benzene hexachloride) Most toxic off lotion as prescribed) Signs of toxicity irritability seizures Secure storage of treatment products (prevent children from ingesting) Itching may last up to 1 week after treatment (due to local irritation) May need to repeat treatment All persons in household & close contact should be treated All environmental reservoirs (bedding, clothing, towels, etc) must be cleaned with HOT water & detergent Spraying pesticides is ineffective & not recommended Trim fingernails (reduce risk of harboring mites) Children in daycare/school can return after treatment Squamous Cell carcinoma: a malignant tumor originating from keratinocytes, can invade the dermis and occasionally men are twice as likely to develop BCC and three times as likely to develop squamous skin cancers compared with women. adult or elderly patient who presents with complaints of a spot or a bump that is getting larger or a sore that is not healing. Found on sun- exposed areas, such as the lips, the tips of ears, the nose, the upper cheeks, the scalp (in bald men), the dorsa of the Suspicious lesions (if not located on the face) can be biopsied by an experienced primary-care practitioner or referred to a Management of nonmelanomatous skin cancers is dependent on several factors: size and depth of the invasion, location, cosmetic concerns, and metastasis Recurrence may occur within 3 years of treatment Avoid sun exposure; wear protective clothing, hats, sunglasses, apply metastasize to distant sites. Smokers are prone to cancerous lesions on the lips and tongue. Immunosuppression, a history of exposure to ionizing radiation, exposure to arsenic and PAHs (paint thinners, organic solvents), treatment with psoralens and UV light (therapy used for psoriasis), and infection with oncogenic HPV. SCC is also seen with increased frequency in areas of skin damage due to chronic inflammation, burns, old scars, or chronic ulcers Often the lesion appears as a thick, rough patch that may bleed if scratched or scraped. Some patients think they are warts with a raised border and crusted surface. The skin lesion may be pruritic or asymptomatic. hands and forearms, and the shins in women. Common presentation is a firm papule with a scaly (keratotic) rough surface with irregular borders. These lesions may even present as cutaneous horns, with columnar hyperkeratosis atop an erythematous base. Later, the surfaces of SCC lesions tend to bleed easily (become friable) with minor trauma and appear eroded with ulcerations. The typical lesion of Bowen’s disease appears as a solitary, slowly enlarging erythematous, red- brown hyperkeratotic plaque that has a slight scaling and minimal crusting. Similar lesions in the anogenital region known as Bowenoid papulosis have been associated with oncogenic HPV strains. dermatologist. to other sites Excisional biopsy at the time of initial diagnosis; this procedure is both diagnostic and curative. Alternative methods for removal of small BCC and SCC lesions include electrodesiccation and curettage, cryosurgery (liquid nitrogen), and laser surgery Mohs microsurgery has the highest cure rate for both BCC and SCC. surgical excision, lymph node dissection and systemic chemotherapy are used to treat large and invasive SCC lesions that have metastasized. External beam radiation is used as the primary treatment on tumors that are large or located in areas of skin that make surgery difficult, or in elderly or debilitated patients who are poor surgical candidates. External beam therapy is also used as adjuvant therapy in lesions with a high risk of recurrence or in cancers that have metastasized. sunscreen SPF at least 15; reapply as needed; avoid tanning beds and sun lamps. Teach pt ABCDEs of malignant melanomas Telogen Effluvium – Can be caused by stress, Has been occurring for Decreased density of Diagnosis of Self-limiting. Correct Ful hair growth in 6 can be a cause of non scarring alopecia. Is excessive shedding of scalp hair that results from an increases number of hair follicles entering the resting stage (telogen). pregnancy, and/or childbirth, extreme weight loss, and general anesthesia. Can be caused by fever and certain drugs. Very Rare in men. Risk factors: infection, trauma, major surgery, thyroid disorder, febrile disorder, malignancy, allergic contact dermatitis, iron deficiency anemia, excess vitamin a, protein calorie restriction, end-stage liver or renal disease, hormone changes (pregnancy, delivery, and estrogen-containing medication); chronic stress, drug induced (BB, anticonvulsants, antidepressants, anticoagulants, retinoids, ACE inhibitors, etc.); immunizations 2-6 months; fear of becoming bald; pts present with bags of hair to emphasize severity of hair loss. hair on scalp, most commonly the crown. Chronic TE may present with hair loss to eyebrows and pubic region (rare). Hair may shed when you run fingers through scalp. Shed hair are telogen hairs which have small bulb of unpigmented or pigmented keratin on the root end. May affect nail growth, resulting in the appearance of Beau lines, which are transverse grooves on the nails of the hands and feet. exclusion. Blood work to r/o possible causes. Initial lab tests: CBC, ferritin; T-SHIRTv; creatinine; hepatic enzymes; consider RPR/VDRL. Hair pul test (unreliable) Hair clip test: <10% of hair shafts of small diameter (negative). >10% of hair shafts small diameter (positive) Scalp biopsy (rarely needed) underlying cause. Oral zinc therapy. Nigella saliva (black cumin) essential oil may be beneficial. months to 1 yr. Tinea versicolor (aka pityriasis versicolor) - Jenna Common in summer time. Tinea versicolor obvious during summer, when tanning exposes hypopigmented macules that do not tan. Common in teens and young adults but can occur at any age. Become noticeable in summer, since the macules do not tan. Asymptomatic with gradual onset. Mild pruritus - rare. People of African descent complain of hypopigmented or Macules that may be round or oval, pink or hypo or hyperpigmented. Asymptomatic. Not associated with pruritus. Will be seen mainly on back, chest, arms, and sometimes Fungal culture not required unless clinical is unsure of diagnosis or if infection not responsive to treatment. Caused by yeast P. orbiculare (which causes round Treated with selenium sulfide lotion (selsun) daily for 7 days from neck to waist with small amounts of water lathered and left for 10 minutes); repeated once a week for 1 month. Treatment will eradicate infection but will not remove the hypopigmented spots from skin which take longer to resolve. Educate on high rate hyperpigmented spots. Will complain of these macules to back, upper chest, arms, and sometimes neck and face. neck. In children, rash common on face or forehead. Sometimes very fine scales are visible, especially if patient has not showered or bathed for several days. Daily bathing usually eradicates the scales. lesions) or Pityrosporum ovale (which produces oval lesions); Clotrimazole 1% cream and solution (Lotrimin) twice daily for 2-8 weeks Terbinafine 1% solution (Lamisil solution) twice daily for 1 week. Education: Do not use on face or mucous membranes; avoid broken or irritated skin. Ciclopirox 0.77% cream, lotion (Loprox) twice daily for 2-4 weeks. Do not use in children younger than 10 years. Avoid occlusion. Ketoconazole 2% shampoo (Nizoral) 1 application applied to damp scalp, leave for 5 minutes and rinse Econazole 1% cream, foam (Spectazole) (Ecoza) once daily for 2 weeks Sulconazole 1% cream, solution (Exelderm) 1-2 daily for 3 weeks Oxiconazole cream, lotion (Oxistat) 1-2 times daily for 2 weeks Fluconazole (diflucan) 150- 300mg single weekly dose for 2-4 weeks of 300mg weekly for 2 weeks Itraconazole 200mg daily for 7 days of recurrence because P. orbiculare (M. furfur) is a normal habitant of the skin. sunlight can speed up resolution of hypopigmented spots. High risk of hepatotoxicity with systemic (oral) antifungals and treatment does not prevent recurrence. Some success with photodynamic therapy Trichotillomania (hair pulling) - jenna Seen more commonly in children and teens. Family hx, age, stress, depression, anxiety, obsessive-compulsive disorders (OCD). Reports balding, sense of pleasure with pulling hair, or pull hair without realizing it. Pull hair due to stress, anxiety, tension. Compulsive hair pulling may be observed. Nonscarring alopecia. Usually on the same side of the dominant hand and may include more than just scap hair (eye lashes, eye brows, and beards) Observation Refer to dermatologist or psychologist. An SSRI for 1st line treatment of OCD in children and adults. Cognitive behavior therapy is another option as a first line management for OCD. Varicella Immune compromised such as AIDS and HIV Risk -No prior history of varicella -No vaccination -Immunocompromised **Patients are contagious for 2 days prior the appearance of the rash and until all lesions have crusted. **infection in adults is more likely to produce serious illnesses subjective -Malaise -Anorexia -Abdominal pain -Headache -fever/chills -arthralgia -Childhood: onset of exanthem Then 1-2 days later, the urticarial (or itching) erythematous macules and papules appear, which quickly turn unto vesicles and pustules. Rash starts on the face and chest then spreads over the entire body. The blisters may even appear in the ear canal or mouth. Lesions dry up within 1 week. Rash with widely distributed papules and vesicular lesions; appear on head and neck area objective rash phase -small erythematous macules appear on the scalp, face, trunk and limbs with rapid progression within 12- 24 hrs to papules, clear vesicles and pustules with central umbilication and form crusts. -vesicles appear on palms, soles, mucous membranes, oropharyngeal area and urogenital areas Diagnostic none indicated unless in pregnant women -tzanck smear -vesicular fluid culture -serology -chest xray if pneumonia suspected -PCR Treatment is symptomatic care with oral antihistamines for itching, NSAIDS, cool compresses, and oatmeal baths. Valacyclovir (Valtrex ) 1 gm po q8h for 7 days or Acyclovir (Zovirax) 800mg po 5 times a day for 7-10 days or Famciclovir (Famvir) 500mg po TID for 7 days plus topical silver sulfadiazine for skin lesions. No evidence of fetal harm if used during pregnancy. treatment *Non pharmacologic -Supportive therapy -good hygiene to prevent bacterial secondary infections -cut fingernails short to prevent scratching in education -Do not immunize pregnant women -In pregnant woman who has never had chicken pox or immunization, avoid contact with recently vaccinated individuals for 6 weeks Prevention includes vaccination. A patient is contagious 2-3 days before rash erupts and may return to school, sports, or work after lesions have scabbed over. A client who has a varicella rash can return to work once all the vesicles are crusted over. younger children -Tepid bath, oatmeal bath for itching *Pharmacologic Skin protectant such as calamine antipyretics: avoid aspirin due to increased risk of Reye’s syndrome with varicella patients -Antiviral agents: consider in adolescents, adults and high-risk patients to decrease viral shedding and duration of fever Acyclovir (2-16 years old) 20mg /kg/dose (max 800 mg /dose, 4 times daily for 5 days Famciclovir (adults): 500 mg 3X daily for 7 days-10 days Valacyclovir (adults) : 1g 3 X daily for 7-10days diphenhydramine, hydroxyzine or other antihistamine for itching Varicella is contagious 48 hours before the onset of the vesicular rash, during the rash formation (usually 4-5 days), and during the several days it takes the vesicles to dry up. The characteristic rash appears 2 to 3 weeks after exposure. Verruca vulgaris (Common warts): p.203 Small, hardened growths of keratinized tissue. Warts usually grow around nails, on fingers, and the backs of hands, but can appear Skin trauma, contact with wart exudate after treatment, immunocompromosed state Patients typically complain of a wart or small “bump” (or group of bumps) that has been present for several weeks to many months and sometimes for years. Some patients report the same wart being treated before and then recurring in the Common wart: rough-surfaced, elevated, flesh- colored papules None needed but if unable to distinguish lesions, small specimen can be sent for identification. Salicylic acid solution/plasters Cryotherapy with liquid nitrogen Surgical excision Studies suggest that one- half of warts resolve without treatment within Avoid contact with wart exudate from self and others by covering wart; avoid skin trauma Can cause scarring, autoinoculation, and nail deformity The clinician should educate the patient anywhere on the body. Common warts (verruca vulgaris) are primarily caused by HPV serotypes 1 to 5, 7, 27, or 29, whereas HPV serotypes 3, 10, 28, and 29 cause flat warts. HPV serotypes 1 to 4, 27, 29, and 57 typically causes plantar warts, whereas HPV serotypes 6 and 11 cause anogenital warts. same area. Many adult patients with common warts attempt self- treatment with over- the-counter (OTC) wart remedies with limited to no success. Warts are usually asymptomatic but may be cosmetically undesirable. Plantar warts may cause discomfort with weight-bearing. 1 year, and two-thirds resolve within 2 years. Therefore, first-line therapy for new warts is watchful waiting with no treatment. Initial management for established warts should be geared toward relieving pain and pressure and minimizing skin trauma and scarring caused by available therapies. It is important to note that several treatments for warts are contraindicated in pregnant women; however, salicylic acid applied to a small area of the skin for a short duration and liquid nitrogen cryotherapy are considered safe during pregnancy. on the prevention of self-inoculation and the routes of transmission for common warts. These measures include limiting shaving of the affected area until warts are eradicated, strategies to control nail biting, and avoidance of scratching and rubbing warts. Wearing protective foot coverings in wet public areas such as showers, locker rooms, and pools and keeping warts dry are additional approaches to prevent infection Vitiligo Presence of other auto- immune diseases Hyperthyroidism Adrenal insufficiency Alopecia areata Pernicious anemia Type 1 diabetes mellitus (NOT type 2) Family history – can be inherited Report loss of skin color – patchy areas Rarely affects entire body Often affects Face, lips, arms, hands, feet “white macules or patches, usually located on sun- exposed areas” Physical Exam Based on family history History of skin trauma, rash or sunburn to affected area Family or personal history of other auto- immune disease Biopsy Confirm absence of melanocytes in 1st line treatment Topical corticosteroids 2nd line treatment Light therapy (UVA and/or UVB light) Topical corticosteroids May cause skin thinning, striae Light therapy May require multiple sessions/treatments May not yield permanent results affected skin BUSINESS ESSENTIALS (jenna) DEFINITION/CHARACTERISTICS Medical coding Is the use of codes to communicate with payers about which procedures were performed and why. Medical billing Is the process of submitting and following up on claims made to a payer in order to receive payment for medical services rendered by a healthcare provider CPT codes Offers the official procedural coding rules and guidelines required when reporting medical services and procedures performed by physician and non-physician providers. Recognized universally and provide a logical means to be able to track healthcare data, trends, and outcomes. Each service or procedure is represented by a five-digit code that is presented in six sections, including evaluation and management; anesthesiology; surgery; radiology; pathology; and medicine. Every CPT code must have a diagnosis code (ICD-10) that corresponds. ICD10 codes Currently in ICD-10 revision. Shorthand for patient’s diagnosis and used to provide payer information on the necessity of the visit or procedure performed. Medicare Part A Covers hospital services Medicare Part B Covers physician/provider and outpatient services. Deductible is $183 per year. Once paid, the patient is charged 20% of the approved Medicare rate for physician office visits and some diagnostic tests. Obtain payments at the beginning of the calendar year since most patients have not met their deductibles yet. Collect before rendering services. Direct patient billing occurs when providing services before collecting payment and this is costly. Medicare Part D Medicare prescription drug benefit Health maintenance organization (HMO) (couldn’t find in text book) HMOs have their own network of doctors, hospitals and other healthcare providers who have agreed to accept payment at a certain level for any services they provide. This allows the HMO to keep costs in check for its members Preferred provider organization (PPO) (couldn’t find in text book) A preferred provider organization (PPO) is a medical care arrangement in which medical professionals and facilities provide services to subscribed clients at reduced rates. PPO medical and healthcare providers are called preferred providers Indemnity insurer (couldn’t find in text book) Part of a 3rd party payer. Also known as fee-for-service plans which is what most health insurance companies offered to insurance consumers before the prevalence of PPO and HMO. Not limited to choices of health service providers in a certain preferred provider list like with PPOs or HMOs. May choose any health-care facility or doctor. (HAV) (HCV) (HDV) Virus (HEV) Transmission Fecal–oral through sewage- contaminated water and shellfish; possibly through blood Percutaneous and permucosal through infected blood and body fluids; sexual transmission Percutaneous through infected blood and body fluids; community, many infected individuals have no known risk factors Percutaneous, but must have co- infection with HBV Fecal–oral Incubation period (days) 15–50 (average 20–37) 25–160 (average 60–110) 42–49 Same as for HBV 10–56 Laboratory tests Anti-HAV IgM (acute); anti-HAV IgG (resolving) HBsAg (confirms), IgM anti- HBs (acute phase), IgG anti- HBs (resolving/immunity), HBeAg, anti-HBe, anti-HBc (persists in carriers) Anti-HCV appears in 6–37 weeks Anti-HDV appears late Anti-HEV IgM detected within 26 days of jaundice; IgG antibody persists Immunity/immunizatio n 45% of United States population has antibodies against HAV; HAV vaccine available 5%–15% of U.S. population has anti-HBs; HBV vaccine available Unknown; no vaccine available People immune to HBV are also protected against HDV Unknown Prevalence Increasing in adults Decreasing in the United States 4% of post- transfusion hepatitis; 50% IV drug users Common in IV drug abusers Rare in United States; endemic in Southeast Asia, India, North Africa, Mexico Course/mortality Does not progress to chronic state; mortality is 0– 0.2% with fulminant hepatitis Chronic liver disease occurs in 1%–5% of adults and 80%–90% in children; mortality rate is 0.3%–1.5% Chronic active hepatitis develops in 70%–90% of cases; 20% develop chronic liver disease; mortality Chronic liver disease develops if present in chronic HBV; mortality rate is 2%–20% for acute icteric Does not progress to chronic liver disease; mortality rate is 1%–2% but as rate is the same as for HBV hepatitis high as 10%– 15% in pregnant women TABLE 15.2 Herpes Simplex Infections Infection Location Commonly Affected Age Group Oral—labial herpes simplex Lips, oral cavity Children age 2–5 years, adults Herpetic keratoconjunctivitis Eyelids, periorbital area, cornea Newborns, adults Herpetic tracheobronchitis Pharynx, trachea, bronchi Older adults Herpes simplex encephalitis Temporal lobe of the brain Any age, primarily immunocompromised adults Herpes gladiatorum Shoulder, neck, knuckles, areas of contact Age 14 years and older (commonly seen in wrestlers) Herpetic whitlow Fingertip Age 1 year and older Lumbosacral herpes Trunk or back Adult Herpes simplex of the buttocks Buttocks Adult women Genital herpes Labia minora, labia majora, vagina, cervix, urethra, penis, rectal area Young and older adults, 1% of pregnant women Eczema herpeticum Face or any area of active or recently healed atopic dermatitis Infants, children, and adults, commonly with a history of atopic dermatitis Erythema multiforme Extremities, palms, soles of feet Age 20–30 years; more commonly seen in men than women Question 1. Treatment for achalasia may include: Balloon dilation of the lower esophageal sphincter. Question 2. Which oral medication might be used to treat a client with chronic cholelithiasis who is a poor candidate for surgery? Ursodiol (Actigall). Question 3. All of the following medications are used for the control of nausea and vomiting. Which medication works by affecting the chemoreceptor trigger zone, thereby stimulating upper gastrointestinal motility and increasing lower esophageal sphincter pressure? Antidopaminergic and cholinergic agents, such as metoclopramide (Reglan). Question 4. Which is the most common presenting symptom of gastric cancer? Weight loss. Question 5. Margie, age 52, has an extremely stressful job and was just given a diagnosis of gastric ulcer. She tells you she is sure it is going to be malignant. How do you respond? “About 95% of gastric ulcers are benign.” Question 6. Marcie just returned from Central America with traveler’s diarrhea. Which is the best treatment? Supportive care. Question 7. Rose has gastroesophageal reflux disease (GERD). You know she misunderstands your teaching when she tells you she will: Have a snack before retiring so that the esophagus and stomach are not empty at bedtime. Question 8. Marty, age 52, notices a bulge in his midline every time he rises from bed in the morning. You tell him that it is a ventral hernia, also known as an: Epigastric hernia. Question 9. You are trying to differentiate between functional (acquired) constipation and Hirschsprung disease in a neonate. Distinguishing features of Hirschsprung disease include which of the following? Small ribbonlike stools. Question 10. You are doing routine teaching with a patient who has a family history of colorectal cancer. You know she misunderstands the teaching when she tells you she will: Increase her fluid intake. Question 11. Bobby, age 6, has constant periumbilical pain shifting to the right lower quadrant, vomiting, a small volume of diarrhea, absence of headache, a mild elevation of the white blood cell count with an early left shift, and white blood cells in the urine. You suspect: Appendicitis. Question 12. Melva, age 63, presents with an acute exacerbation of pancreatitis, and you are going to admit her to the hospital. Which is the most important factor in determining a negative long-term outcome for her? Infection. Question 13. A mother brings in her 4-year-old child, who she states has acute abdominal pain and a rash. Which of the following do you initially rule out? Appendicitis. Question 14. Icterus due to hyperbilirubinemia is seen when the serum level of bilirubin is greater than? 2.5 mg/dL. Question 15. A 45-year-old homeless man presents to your urgent care clinic for evaluation. His chief complaint is diarrhea. The patient states he started to have diarrhea 2-3 days ago, and it is getting progressively worse. He also notes nausea without vomiting, dry mouth, and double vision. On exam you notice his pupillary reflex is absent. The patient states he lives on the street and eats mostly canned goods that he scavenges from a grocery store dumpster. What is the likely cause of the patient’s symptoms? Botulism. Question 16. Hepatitis D is an RNA virus that requires a coinfection with which of the following strains of hepatitis in order to replicate? Hepatitis B. Question 17. Which of the following is not true regarding hepatitis C? If hepatitis is asymptomatic it doesn’t cause cirrhosis or liver cancer. Question 18. A 54-year-old female presents to your primary care office for routine reevaluation for gastroesophageal reflux disease (GERD). She has been treated with diet modifications and 6 weeks of omeprazole without improvement of her symptoms. What is the next step in management of this patient’s GERD? Order an endoscopy. 2. Question 19. A 75-year-old male presents for a routine physical. He is obese and has no abdominal pain or recent injuries or problems. He has no complaints. He lies supine for his abdominal exam. He is nontender to palpation and has a normal exam. When he sits up you see a large mass protrude from his abdomen. It is central to his abdomen and inferior to his rib cage. It disappears when he is sitting up fully. What is the patient’s diagnosis? Umbilical hernia. Question 20. Which gastrointestinal disease below could theoretically be completely eradicated with a total colectomy? Ulcerative colitis. Question 1. You auscultate Julie’s abdomen and hear a peritoneal friction rub. Which condition do you rule out? Irritable bowel syndrome. Question 2. Susan, age 59, has no specific complaints when she comes in for her annual examination. She does, however, have type 2 diabetes mellitus (DM), slight hypertension, dyslipidemia, and central obesity. How would you diagnose her? As having metabolic syndrome. Question 3. Timothy, age 68, complains of an abrupt change in his defecation pattern. You evaluate him for: Colorectal cancer. Question 4. Ruby has a colostomy and complains that her stools are too loose. What food(s) do you suggest to help thicken the stools? Cheese Question 5. Martina, age 34, has AIDS and currently suffers from diarrhea. You suspect she has which protozoal infection of the bowel? Cryptosporidiosis. Question 6. When Sammy asks you what he can do to help his wife, who has dumping syndrome, what do you suggest he encourage her to do? Eat foods with a moderate fat and protein content. Question 7. Lucy, age 49, has pain in both the left and right lower quadrants. What might you suspect? Pelvic inflammatory disease. Question 8. You suspect appendicitis in Andrew, who is 18. With his right hip and knee flexed, you slowly rotate his right leg internally to stretch a muscle. He states that it is painful over his right lower quadrant. Which sign did you elicit? Obturator sign. Rationales Option 1: Rovsing sign is pain elicited with deep palpation over the left lower quadrant (LLQ), with sudden resultant pain in the right lower quadrant (RLQ). This causes tenderness over the RLQ and is considered a positive finding. Option 2: Psoas sign is pain elicited when the patient is instructed to try to lift the right leg against gentle pressure applied by the examiner or when the patient is placed in the left lateral decubitus position, extending the right leg at the hip. An increase in pain is considered positive and is an indication of the inflamed appendix irritating the psoas muscle. Option 3: Obturator sign is elicited when, with the patient’s right hip and knee flexed, the examiner slowly rotates the right leg internally, which stretches the obturator muscle. Pain over the right lower quadrant (RLQ) is considered a positive sign. Option 4: McBurney sign is pain elicited when pressure is applied to McBurney point, which is located halfway between the umbilicus and the anterior spine of the ilium. Question 9. You elicit costovertebral angle tenderness in Gordon, age 29. Which condition do you suspect? Inflammation of the kidney Question 10. Marvin, a known alcoholic with cirrhosis, is frequently admitted for coagulopathies and occasionally receives blood transfusions. His wife asks you why he has bleeding problems. How do you respond? “There is an interruption of the normal clotting mechanism.” Question 11. Olive has an acute exacerbation of Crohn’s disease. Which laboratory test value(s) would you expect to be decreased? Vitamin A, B complex, and C levels. Question 12. You suspect that Harry has a peptic ulcer and tell him that it has been found to be strongly associated with: Infection by Helicobacter pylori. 90% of cases are caused by H. Pylori Question 14. Dottie brings in her infant, who has gastroesophageal reflux. What do you tell her about positioning her infant? “Always position infants on their back to prevent sudden infant death syndrome.” Question 15. To differentiate among the different diagnoses of inflammatory bowel diseases, you look at the client’s histological, culture, and radiological features. Mary has transmural inflammation, granulomas, focal involvement of the colon with some skipped areas, and sparing of the rectal mucosa. What do you suspect? Crohn disease. The key is “skipped areas of mucosal involvement” Question 18. What is the best diagnostic test to confirm the diagnosis of celiac disease? Anti-tTG IgA Question 19. A 50-year-old female presents to the urgent care clinic complaining of left lower quadrant pain. She has associated nausea and vomiting, and her vital signs are as follows: temperature 102.5°F, pulse 110, blood pressure 150/90, pulse oximetry 99% on room air. What is the best test to evaluate this patient? Computed tomography (CT) scan with oral contrast. Question 20. The screening guidelines for colon cancer recommend which of the following for the general population? Colonoscopy starting at age 50 Question 2. Zena just had a hemorrhoidectomy. You know she has not understood your teaching when she tells you she will: . Decrease her dietary fiber for 1 month. Question 3. Simon, age 72, states that he is worried because he has a bowel movement only every third day. You respond: “There is no such thing as a ‘normal’ pattern of defecation.” Question 4. Matt, age 26, recently returned from a camping trip and has gastroenteritis. He says that he has been eating only canned food. Which of the following pathogens do you suspect? Clostridium botulinum Question 7. Anson tells you he thinks his antacids are causing his diarrhea. You respond: “Antacids may contain magnesium, which decreases bowel transit time and may contain poorly absorbed salts that draw fluid into the bowel.” Question 9. Sandy, age 52, presents with jaundice, dark urine, and light-colored stools, stating that she is slightly improved over last week’s symptoms. Which stage of viral hepatitis do you suspect? Icteric. Question 10. Ellie, age 42, has a seizure disorder and has been taking phenytoin (Dilantin) for years. Which supplement should she also be taking if no other problems exist? Folic acid. Question 13. Harvey just came back from Mexico. Which pathogen do you suspect is responsible for his diarrhea? Escherichia coli. Most common cause of travelers diarrhea Question 14. Which of the following medications/drugs are not known to cause heartburn or dyspepsia? Tylenol. Question 17. A 25-year-old male presents complaining of hematochezia. The patient states he has noticed this for 2 days. He states there is a streak of bright blood along his stool every time he has a bowel movement. The patient has no pain with his bowel movements. He admits to eating a poor diet. The patient has no abdominal pain, nausea, or vomiting. On physical exam the patient has a positive fecal occult blood test but has no noticeable rectal bleeding or lesions. What is the likely diagnosis? Internal hemorrhoid. Question 20. Which of the following is the most common cause of acute pancreatitis? Gallstone obstruction of the pancreatic duct and alcoholism. Question 1. The metabolism of which drug is not affected in Marsha, age 74? Alcohol. Question 2. Nausea is difficult to discern in a young child. What question might you ask to determine if a child has nausea? “Are you hungry?” Question 3. Sally, age 21, is to undergo a tonsillectomy. She has heard about permanent taste changes after a tonsillectomy. What do you tell her? “You may notice a slight difference initially, but there are no lasting changes in taste.” Question 7. Cydney has been given a diagnosis of ascariasis. Which symptoms would you expect to see? Low-grade fever, productive cough with blood-tinged sputum, wheezing, and dyspnea. Question 8. Marian, age 52, is obese. She complains of a rapid onset of severe right upper quadrant abdominal cramping pain, nausea, and vomiting. Your differential diagnosis might be: Cholecystitis. Question 9. A 7-year-old male presents with his mother to the urgent care clinic complaining of abdominal pain. He started to complain of pain prior to going to bed; however, it has gotten progressively worse and is now preventing him from sleeping. He is nauseous but hasn’t vomited and didn’t eat dinner due to the pain. The patient appears pale and is complaining of right-sided abdominal pain. His vitals are as follows: blood pressure 130/85, pulse 120, temperature 100.5°F, pulse oximetry 98% on room air. On physical exam he is tender in the right lower quadrant. His complete blood count (CBC) shows a white blood cell count (WBC) of 17.0. What is the patient’s likely diagnosis? Appendicitis. Question 10. What would you expect to see on an abdominal series that would lead toward a diagnosis of small-bowel obstruction? Air-fluid levels. Question 2. What is the most common bacterial pathogen associated with acute otitis media? Streptococcus pneumoniae. Question 4. When the Weber test is performed with a tuning fork to assess hearing and there is no lateralization, the nurse practitioner should document this finding as: A normal finding. Question 6. You are assessing a first grader and find that the tonsils are touching the uvula. How would you grade this finding? Grade 3. Question 1. Which of the following is not a cause of conductive hearing loss? Presbycusis. Question 2. Jill, a 34-year-old bank teller, presents with symptoms of hay fever. She complains of nasal congestion, runny nose with clear mucus, and itchy nose and eyes. On physical assessment, you observe that she has pale nasal turbinates. What is your diagnosis? 1. Allergic rhinitis. Question 3. Mrs. Johnson, a 54-year-old accountant, presents to the office with a painful red eye without discharge. You should suspect: Iritis. Question 4. April, age 50, presents with soft, raised, yellow plaques on her eyelids at the inner canthi. She is concerned that they may be cancerous skin lesions. You tell her that they are probably: Xanthelasmas. Question 5. A 62-year-old woman presents to your clinic with a sudden right-sided headache that is worse in her right eye. She states that her vision seems blurred, and her right pupil is dilated and slow to react. The right conjunctiva is markedly injected, and the eyeball is firm. You screen her vision and find that she is 20/30 OS and 20/30 OD. She most likely has: 2. Angle-closure glaucoma. Rationales Option 1: With open-angle glaucoma, the onset is more insidious. Option 2: In angle-closure glaucoma, the patient presents with a sudden onset of symptoms as described in this case. This client has a visual deficit and pain as well as fullness of the affected eye. This is a medical emergency, and she should be referred immediately because, without intervention, blindness can occur within days. Option 3: Herpetic conjunctivitis is generally associated with a herpetic rash, and the pain is dull in character. Option 4: Diabetic retinopathy is a complication of diabetes that affects both eyes. It is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (ie, the retina). Question 1. A 25-year-old male presents with “bleeding in my eye” for 1 day. He awoke this morning with a dark area of redness in his eye. He has no visual loss or changes. He denies constitutional symptoms, pruritus, drainage, or recent trauma. The redness presents on physical exam as a dark red area in the patient’s sclera of the right eye only and takes up less than 50% of the eye. The patient’s remaining sclera is clear and white. He also notes he was drinking alcohol last night and vomited afterward. What is the best treatment? 3. Reassurance that this lesion will resolve without any treatment in 2 to 4 weeks. Rationales Option 1: This would be the treatment for an infectious process; however, topical steroids need to be used in the eye with care. Option 2: This would be the treatment for a globe rupture or acute angle-closure glaucoma. Option 3: This is the classic presentation of a subconjunctival hemorrhage. It will resolve without treatment in 2 to 4 weeks. Vomiting probably caused his hemorrhage. Option 4: This is the treatment for viral conjunctivitis. Question 2. You prescribe Levaquin (levofloxacin) for a severe sinus infection. What is not a possible adverse reaction to this medication? 4. Stevens-Johnson syndrome. Question 3. A 20-year-old male presents to your primary care clinic. This patient is a college student. He complains of fatigue, sore throat, and low-grade fever for 3 days. On physical exam, he has a temperature of 100.7°F. His ear exam is normal. His nose and throat exam shows mild erythema of the nasal mucosa and edematous, enlarged tonsils bilaterally, with erythema of the pharyngeal wall and tonsillar exudates. He has inflamed posterior cervical lymph nodes. He has a mild nonproductive cough and clear lung exam. What is his most likely diagnosis? Mononucleosis. Rationales Option 1: This presentation could be a viral pharyngitis; however, with posterior cervical lymphadenitis, you would suspect mononucleosis. Option 2: This presentation could be a viral pharyngitis; however, with posterior cervical lymphadenitis, you would suspect mononucleosis. Option 3: You would expect fever and tonsillar exudates without posterior cervical lymphadenitis. Option 4: Upper respiratory infections usually present with cough that may be productive and milder ear, nose, and throat symptoms. Question 4. When you are assessing the internal structure of the eye of your 59-year-old patient, the absence of a red reflex may indicate: A cataract or hemorrhage into the vitreous humor. Rationales Option 1: When assessing the internal structure of the eye, absence of a red reflex may indicate the total opacity of the pupil because of a cataract or hemorrhage into the vitreous humor. It may also be a result of improper positioning of the ophthalmoscope. Option 2: Acute iritis is noted by constriction of the pupil accompanied by pain and circumcorneal redness (ciliary flush). Option 3: The absence of a red reflex is not a normal finding. It may be caused by a cataract or a hemorrhage into the vitreous humor. Option 4: If areas of hemorrhage, exudate, and white patches are present when the internal structure of the eye is assessed, they are usually a result of diabetes or long-standing hypertension. Question 5. What significant finding(s) in a 3-year-old child with otitis media with effusion would prompt more There is a change in the child’s hearing threshold to greater than 25 dB. Rationales Option 1: If a child with otitis media with effusion has a change in the hearing threshold greater than 25 dB and has notable speech and language delays, more aggressive treatment is indicated. When the child’s hearing examination reveals a change in the hearing threshold, it is extremely important that the provider evaluate the child’s achievement of developmental milestones in speech and language. Any abnormal findings warrant referral. Option 2: A child with otitis media with effusion might become irritable during meals. Option 3: A slight delay in language and speech does not warrant aggressive treatment or referral. Option 4: Persistent rhinitis does not warrant aggressive treatment or referral. Question 6. Max, age 35, states that he thinks he has an ear infection because he just flew back from a business trip and feels unusual pressure in his ear. You diagnose barotrauma. What is your next action? Prescribe nasal steroids and oral decongestants. Question 7. Susan is a 19-year-old college student and avid swimmer. She frequently gets swimmer’s ear and asks if there is anything she can do to help prevent it other than wearing earplugs, which do not really work for her. What do you suggest? Start using a cotton-tipped applicator to dry the ears after swimming. Use ear drops made of a solution of equal parts alcohol and vinegar in each ear after swimming. Rationales Option 1: The adage “You shouldn’t put anything smaller than your elbow in your ear” holds true today. Option 2: Using ear drops made of a solution of equal parts alcohol and vinegar in each ear after swimming is effective in drying the ear canal and maintaining an acidic environment, therefore preventing a favorable medium for the growth of bacteria, the cause of swimmer’s ear. Option 3: A hair dryer operated on the lowest setting several inches from the ear may be used to dry the canal. Option 4: There is no reason for the client to stop swimming. Question 8. Mary, age 82, presents with several eye problems. She states that her eyes are always dry and look “sunken in.” What do you suspect? Normal age-related changes. Rationales Option 1: With hyperthyroidism, the eyes appear to bulge out (exophthalmos), but in hypothyroidism, the eyes do not appear any different. Option 2: Dryness of the eyes and the appearance of “sunken” eyes are normal age-related changes. Option 3: A moon face is apparent with Cushing syndrome, and this might make the eyes appear to be sunken in, although on close examination, they are not. Option 4: With a detached retina, the outward appearance is normal, but the client complains of seeing floaters or spots in the visual field and describes the sensation as like a curtain being drawn across the vision. Question 9. Nystatin (Mycostatin) is ordered for Michael, a 56-year-old banker who has an oral fungal infection. What instructions for taking the medication do you give Michael? “Swish and swallow the medication.” Rationales Option 1: The oral medication should not be diluted, as that may compromise the absorption. Option 2: Taking the medication with meals may compromise the absorption. Option 3: When ordering nystatin (Mycostatin) for an oral fungal infection, tell the client to swish the medication in the mouth to coat all the lesions and then to swallow it. Option 4: It is almost impossible to apply this liquid medication to only the lesions; swishing it in the mouth coats all the lesions more effectively. Question 10. The most common cause of a white pupil (leukokoria or leukocoria) in a newborn is: A congenital cataract. Rationales Option 1: The most common cause of a white pupil (leukokoria or leukocoria) in a newborn is a congenital cataract. The incidence may be as high as 1 in every 500 to 1000 live births, and there is usually a family history. Some infants require no treatment; however, in other cases surgery may be performed during the first few weeks of life. Option 2: Retinoblastoma, a common intraocular malignancy, is detected within the first few weeks of life and is the second most common cause of a white pupil. Option 3: Persistent hyperplastic primary vitreous is the third most common cause of a white pupil and is a congenital developmental abnormality. Option 4: Retinal detachment may occur as a result of trauma or disease and only rarely occurs in infancy. Question 11. You diagnose acute epiglottitis in Sally, age 5, and immediately send her to the local emergency room. Which of the following symptoms would indicate that an airway obstruction is imminent? Stridor. Question 12. A 27-year-old female comes in to your primary care office complaining of a perioral rash. The patient noticed burning around her lips a couple days ago that quickly went away. She awoke from sleep yesterday and noticed a group of vesicles with erythematous bases where the burning had been before. There is no burning today. She is afebrile and has no difficulty eating or swallowing. What test would confirm her diagnosis? Tzanck smear. Question 13. Which condition is not included in the atopic triad? Aspirin sensitivity. Question 14. The ABCDEs of melanoma identification include which of the following? Asymmetry: one half does not match the other half. Question 15. Your 24-year-old client whose varicella rash just erupted yesterday asks you when she can go back to work. What do you tell her? “Once all the vesicles are crusted over.” Question 16. Tom, age 50, is complaining of an itchy rash that occurred about a half hour after putting on his leather jacket. He recalls having a slightly similar rash last year when he wore his jacket. The annular lesions are on his neck and both arms. They are erythematous, sharply circumscribed, and both flat and elevated. His voice seems a little raspy, although he states that his breathing is normal. What is your first action? Determine the need for 0.5 mL 1:1000 epinephrine subcutaneously. Question 17. You suspect a platelet abnormality in a 40-year-old woman who presents to your clinic with: Red, flat, nonblanchable petechiae. Question 18. Justin, an obese 42-year-old, cut his right leg 3 days ago while climbing a ladder. Today his right lower leg is warm, reddened, and painful, without a sharply demarcated border. What do you suspect? Cellulitis. Question 19. During a camping trip, Jim, age 35, abruptly developed fever, headache, and joint pain. A few days after the onset of the fever, a blanchable macular rash began on his wrists and ankles and quickly spread to the palms and soles before becoming generalized. The rash is now petechial. You suspect Jim has: Rocky Mountain spotted fever. Question 20. You’re teaching Mitch, age 18, about his tinea pedis. You know he doesn’t understand your directions when he tells you which of the following? “I should wear rubber shoes in the shower to prevent transmission to others.” Question 1. A 75-year-old female presents to your office complaining of dizziness and hearing loss. The patient states she awoke yesterday with dizziness, which she described as feeling the room spinning. She also notes intermittent ringing in her ears. On physical exam, the patient has lateralization of her hearing loss to the unaffected ear. Rinne test shows air conduction lasts longer than bone conduction. What is the next step in helping this patient’s symptoms? Start the patient on a low-salt, low-caffeine diet and give her meclizine for vertigo attacks. Question 3. Which of the following is not recommended for hoarseness? 4. Oral steroids. Question 4. Kevin, a 56-year-old lawyer, has throbbing pain in the left eye, an irregular pupil shape, marked photophobia, and redness around the iris. What is your initial diagnosis? Iritis. Question 5. You are the nurse practitioner caring for Martha, a 47-year-old accountant. You have made a diagnosis of acute sinusitis based on Martha’s history and the fact that she complains of pain behind her eye. Which sinuses are affected? 2. Ethmoid. Question 6. Marlene, a 57-year-old cashier, comes to the clinic because she is unable to differentiate between sharp and dull stimulation on both sides of her face. You suspect: A lesion affecting the trigeminal nerve. Question 7. While doing a face, head, and neck examination on a 16-year-old patient, you note that the palpebral fissures are abnormally narrow. What are you examining? 2. The openings between the margins of the upper and lower eyelids. Question 8. A 44-year-old banker comes to your office for evaluation of a pulsating headache over the left temporal region, and he rates the pain as an 8 on a scale of 1 to 10. The pain has been constant for the past several hours and is accompanied by nausea and sensitivity to light. He has had frequent, though less severe, headaches for many years, and they are usually relieved by over-the-counter medicines. He is unclear as to a precipitating event but notes that he has had visual disturbances before each headache and he has been under a lot of stress in his job. Based on this description, what is the most likely diagnosis of this type of headache? Migraine. Question 9. Your client, a 72-year-old smoker of 50 years, is at the office today for a routine physical. During your inspection of the oral mucosa, you discover a white lesion on the lateral surface of the tongue that you suspect to be cancerous. You document your finding as: A white, painless, firm, ulcerated lesion with indurated borders. Question 10. Which of the following conditions produces sharp, piercing facial pain that lasts for seconds to minutes? 1. Trigeminal neuralgia. Question 11. Mary, age 82, presents with several eye problems. She states that her eyes are always dry and look “sunken in.” What do you suspect? 2. Normal age-related changes. Question 12. A 64-year-old obese woman comes in complaining of difficulty swallowing for the past 3 weeks. She states that “some foods get stuck” and she has been having “heartburn” at night when she lies down, especially if she has had a heavy meal. Occasionally, she awakes at night coughing. She denies weight gain and/or weight loss, vomiting, or change in bowel movements or color of stools. She denies alcohol and tobacco use. There is no pertinent family history or findings on review of systems (ROS). Physical examination is normal, with no abdominal tenderness, and the stool is occult blood (OB) negative. What is the most likely diagnosis? Gastroesophageal reflux disease (GERD). Question 13. Mr. Johnson, age 69, has had Meniere disease for several years. He has some hearing loss but now has persistent vertigo. What treatment might be instituted to relieve the vertigo? A vestibular neurectomy. Question 14. Marjorie, age 37, has asthma and has been told she has nasal polyps. What do you tell her about them? 2. Nasal polyps are benign growths. Cataracts are a common occurrence in patients over 60 years of age. You counsel your patient that the best cure for cataracts is: Corrective lens surgery. In a young child, unilateral purulent rhinitis is most often caused by: A foreign body. Kathleen, age 54, has persistent pruritus of the external auditory canal. External otitis and dermatological conditions, such as seborrheic dermatitis and psoriasis, have been ruled out. What can you advise her to do? Apply mineral oil to counteract dryness. Question 19. At the clinic, you are assessing Kyle, a 4-month-old baby, for the first time and notice that both eyes are turning inward. What is this called? Esotropia. Question 20. Kevin, age 26, has AIDS and presents to the clinic with complaints of a painful tongue covered with what look like creamy white, curdlike patches overlying erythematous mucosa. You are able to scrape off these “curds” with a tongue depressor, which assists you in making which of the following diagnoses? Oral candidiasis. Which of the following patients would not be at risk of Candida infection? 1. A patient with a history of coronary artery disease. Which of the following has/have not been linked to the use of isotretinoin? Pancreatitis. Sophie brings in her husband, Nathan, age 72, who is in a wheelchair. On his sacral area, he has a deep crater with full-thickness skin loss. Subcutaneous tissue is visible but muscle and bone are not. Which pressure ulcer stage is this? Stage III. A Gram stain of a lesion reveals large, square-ended, gram-positive rods that grow easily on blood agar. Which diagnosis does this finding confirm? Anthrax. Question 6. Roy, age 13, was recently diagnosed with epilepsy and prescribed carbamazepine for control of his seizures. He has developed erythematous papules, dusky appearing vesicles, purpura, and target lesions that have erupted rapidly and are more centrally distributed on the face. He has hemorrhagic crusts on his lips. He tells you his skin feels tender and burns. Additionally, he has developed exudative conjunctivitis. These findings are indicative of: Stevens-Johnson syndrome (SJS). Question 8 Which disease usually starts on the cheeks and spreads to the arms and trunk? Erythema infectiosum (fifth disease). Jennifer, age 32, is pregnant and has genital warts (condylomata) and would like to have them treated. What should you order? Trichloroacetic acid. Question 9 Louis, age 52, presents with pruritus with no rash present. He has hypertension, diabetes, and end-stage renal disease (ESRD). Which of the following would be included in the differential diagnosis? Uremia from chronic renal disease. Question 10 Susan states that her fiancé has been frostbitten on the nose while skiing and is fearful that it will happen again. What do you tell her? “Infarction and necrosis of the affected tissue can happen with repeated frostbite.” Question 11 What is the most important thing a person can do to maintain healthy skin and hopefully reduce wrinkles? Avoid smoking. Question 12 Which of the following statements about malignant melanomas is true? The prognosis is directly related to the thickness of the lesion. Lee brings her 13-year-old son to your clinic. He has been complaining of a rash on the buttocks, anterior thighs, and posterolateral aspects of his upper arms. He tells you it is mildly pruritic and looks like “gooseflesh.” On examination, the rash appears as small, pinpoint, follicular papules on a mildly erythematous base. You explain to Lee that the benign condition is likely to resolve by the time her son reaches adulthood, and it is known as: Keratosis pilaris. Question 14. Jim, age 59, presents with recurrent, sharply circumscribed red papules and plaques with powdery white scale on the extensor aspects of his elbows and knees. What do you suspect? Psoriasis. Question 15. Mildred, age 72, presents to the clinic with a blistering rash that is generalized but located mostly in skin folds and on flexural areas. She describes the course of the rash as beginning with pruritic urticarial papules that coalesced into plaques that turned dark red in about 2 weeks, followed by the development of vesicles and bullae. She tells you that the lesions are moderate to severely pruritic. During your exam, you determine the bullae are very tense and do not rupture when pressure is applied. Her daily medications include an angiotensin-converting enzyme (ACE) inhibitor, a loop diuretic, and a nonsteroidal anti-inflammatory drug (NSAID). What is your diagnosis? Bullous pemphigoid. Question 16. Sandra, age 69, is complaining of dry skin. What do you advise her to do? Bathe or shower with lukewarm water and use a mild soap or skin cleanser. Question 17. Caroline has a 13-year-old daughter who has had 2 recent infestations of lice. She asks you what she can do to prevent this. You respond: “Don’t let her share hats, combs, or brushes with anyone.” Question 18. Candidiasis may occur in many parts of the body. James, age 29, has it in the glans of his penis. What is your diagnosis? Balanitis. Question 19. Mr. Swanson, age 67, presents to the clinic for his annual health exam. He asks you if there is anything he can do to prevent the painful, blistering sores that develop on his lip in the summertime when he plays golf. You explain to Mr. Swanson that the way to prevent the development of these lesions is to: Protect the lips from sun exposure with a blocking agent, such as zinc oxide, or a lip balm that contains a broad-spectrum sunscreen. Question 20. A biopsy of a small, yellow-orange papulonodule on the eyelid will probably show: Lipid-laden cells. Question 1. A 75-year-old African American male presents to your family practice office complaining of visual impairment. He has worn corrective lenses for many years but has noticed that his vision has gotten progressively worse the past 6 months. He denies pain. He states his vision is worse in both eyes in the peripheral aspects of his visual field. He also notes trouble driving at night and halos around street lights at night. You test his intraocular pressure, and it is 23 mm Hg. What is his most likely diagnosis? Open-angle glaucoma. Question 2. Which of the following is not a complication of untreated group A streptococcal pharyngitis? Hemolytic anemia. Question 3. The antibiotic of choice for recurrent acute otitis media (AOM) and/or treatment failure in children is: Amoxicillin and potassium clavulanate (Augmentin). Question 4. Mattie, age 64, presents with blurred vision in 1 eye and states that it felt like “a curtain came down over my eye.” She doesn’t have any pain or redness. What do you suspect? Retinal detachment. Question 5. While doing a face, head, and neck examination on a 16-year-old patient, you note that the palpebral fissures are abnormally narrow. What are you examining? The openings between the margins of the upper and lower eyelids. Question 6. Mia, a 27-year-old school teacher, has a 2-day history of severe left ear pain that began after 1 week of upper respiratory infection (URI) symptoms. On physical examination, you find that she has acute otitis media (AOM). She has a severe allergy to penicillin. The most appropriate antimicrobial option for this patient is: Azithromycin (Zithromax). Question 7. Mario, a 17-year-old high school student, came to the office for evaluation. He is complaining of persistent sore throat, fever, and malaise not relieved by the penicillin therapy prescribed recently at the urgent care center. As the nurse practitioner, what would you order next? A Monospot test. Question 8. Cynthia, a 31-year-old woman with a history of depression, is seen in the office today for complaints of headaches. She was recently promoted at her job, and this has caused increased stress. She describes the headache as a tightening (viselike) feeling in the temporal and nuchal areas. The pain is bilateral and tends to wax and wane. It started approximately 2 days ago and is still present. What kind of headache is she describing? Tension headache. Question 9. Ellen, a 56-year-old social worker, is seen by the nurse practitioner for complaints of fever; left-sided facial pain; moderate amounts of purulent, malodorous nasal discharge; and pain and headache when bending forward. The symptoms have been occurring for approximately 6 days. On physical assessment, there is marked redness and swelling of the nasal passages and tenderness/pain on palpation over the cheekbones. The nurse practitioner should suspect: Acute rhinosinusitis Question 10. Sally, age 19, presents with pain and pressure over her cheeks and discolored nasal discharge. You cannot transilluminate the sinuses. You suspect which sinus to be affected? Maxillary sinus Question 11. A 3-year-old patient presents to your pediatric office with her mother. She has recently been started in day care. Her mother noted slight perioral erythema on the right side of the patient’s mouth prior to bed last night. The patient awoke today with 3 small, superficial, honey-colored vesicles where the erythema was last night. The patient has no surrounding erythema. She had no difficulty eating this morning and is active and energetic and doesn’t appear lethargic or fatigued. She is also afebrile. How would you treat this child? Local debridement and mupirocin for 5 days. Question 12. Sandra, age 32, comes in to the clinic. She has painful joints and a distinctive rash in a butterfly distribution on her face. The rash has red papules and plaques with a fine scale. What do you suspect? Systemic lupus erythematosus. Question 14. The nurse practitioner (NP) tells Samantha, age 52, that she has an acrochordon on her neck. What is the NP referring to? A skin tag. Question 17. Thomas, age 35, uses a high-potency corticosteroid cream for a dermatosis. He also currently has tinea corporis. You tell him the following regarding the cream: “It may exacerbate your concurrent tinea corporis.” Question 19. A mother complains that her newborn infant, while lying on his side, appears red on the dependent side of the body and pale on the upper side. When she picks up the baby, this coloring disappears. You explain to her about which of the following? Harlequin sign. Question 20. Helen, age 39, comes to your clinic for generalized joint pain, especially in the knees and hands. She tells you that the pain is moderate, spreading, and symmetrical. She reports having had a sore throat and low-grade fever for a few days and then developing a rash, described as warm erythema of the cheeks, which lasted about 4 days before disappearing. You ask her if the rash on the cheeks included the nasolabial folds or circumoral skin, and she tells you that it did not cover these areas. Two days later, she developed a nonspecific macular eruption that preceded the joint pain. Her rash faded within 2 weeks, but she tells you that it comes and goes if she bathes in hot water or spends time in the sunlight. Your patient’s symptoms are most consistent with a diagnosis of: Erythema infectiosum. Question 1. Which of the following statements about macular degeneration is not true? Macular degeneration is characterized by gradual loss of peripheral vision. Question 2. A 6-year-old female presents to your pediatric office with her mother complaining of right ear pain for 3 days. This pain resolved with Tylenol. The patient has also had noted fevers of 101.3°F over the last 2 nights. The patient had a nonproductive cough for 7 days prior to the ear pain. On physical exam, the patient has tenderness with tugging on the auricle of the ear. The tympanic membrane is not mobile with pneumatic otoscopy and is erythematous and full. The patient has no drainage from the ear and no mastoid tenderness. What is the next step? Amoxicillin 80 to 90 mg/kg/d. Question 3. What is the most common cause of epistaxis? Digital trauma. Question 4. Mallory brings her 4-week-old infant to the office because she noticed small, yellow- white, glistening bumps on her infant’s gums. She says they look like teeth, but she is worried that they may be cancer. You diagnose these bumps as: Epstein pearls Question 5. Jonathan, age 19, has just been given a diagnosis of mononucleosis. Which of the following statements is true? Jonathan should avoid contact sports and heavy lifting. Question 6. Martin, age 24, presents to the office with an erythematous ear canal and pain on manipulation of the auricle. He is on vacation and has been swimming daily at the resort. What is your diagnosis? External otitis. Question 7. Samantha, age 12, presents with ear pain. When you begin to assess her ear, you tug on her normal-appearing auricle, eliciting severe pain. This leads you to suspect: Otitis externa. Question 8. Which manifestation is noted with carbon monoxide poisoning? Cherry-red lips. Question 9. A 22-year-old African American female presents to your family practice office complaining of progressive skin discoloration. She is adopted and has no known family history of skin problems. The patient notes nonpalpable patches of skin loss and blanching of her forehead and both hands and feet. It has developed over a period of 6 months and appears to have stopped. It is not pruritic, and there is no erythema or sign of infectious etiology. What is the most likely diagnosis? Vitiligo. Question 11. A 16-year-old male presents to your office. He was sent by an orthopedist. He has recently had surgical fixation of a humerus fracture. The patient has been going to physical therapy and has been developing a rash on his arm after therapy that disappears shortly after returning home. He does not have the rash prior to therapy. The patient denies fevers and chills, and his incision is well healed, with no signs of infection. Of note, the patient has been experiencing more hand edema than the average patient and has had edema wraps used at the end of therapy to help with his swelling. The wraps are made of a synthetic plastic material. The rash the patient gets is erythematous and blotchy, not raised; it is on the operative upper extremity. What is the most likely diagnosis? Contact dermatitis. Question 13. Maryann, age 28, presents to the clinic because of a rapid onset of patchy hair loss. The skin within these oval patches of hair loss is very smooth. Tapered hairs that resemble exclamation points are seen at the margin of a patch of hair loss. Based on these findings, you suspect Maryann has: Alopecia areata. Question 14. Which treatment is considered the gold standard in tissue-conserving skin cancer removal? Mohs micrographic surgery (MMS). Question 15. You are examining Barbara, age 27, who presents with multiple dry, dusky red, well- localized plaques with a “stuck-on” appearance. They are 5 to 20 mm in diameter and located on her face, scalp, and external ears. You note there is atrophy, telangiectasia, depigmentation, and follicular plugging present. On examination of the scalp, there are areas of total hair loss. There is depigmented scarring of the concha of the ear. Your most likely diagnosis is: Discoid lupus erythematosus. Question 16. Michael, a 25-year-old military reservist, presents to your clinic for a rash that began on his chest and has since developed into smaller lesions that are more concentrated on the lower abdomen and pubic area. In obtaining a history of the present illness, he reports that he had an upper respiratory infection 1 month before the rash developed. He tells you it started with 1 large oval-shaped lesion on his left chest, and 1 to 2 weeks later he developed numerous smaller lesions on the lower abdomen and groin. It has been 2 weeks since the smaller lesions developed, and he tells you he is concerned that the rash isn’t improving. As you examine the patient, you note that the lesions are salmon-colored and have a thin collarette of scale within them. The original lesion is still present. You suspect Michael has: Pityriasis rose Question 17. Shelby, age 14, has a blister on her arm that is filled with clear fluid. It is the result of contact with a hot iron. How do you document this? Bulla. Question 18. Deanna, age 6, was bitten by a friend’s dog. Her mother asks you if the child needs antirabies treatment. You tell her: “If the dog is a domestic pet that has been vaccinated, the wound should be cleaned and irrigated.” Question 19. Buddy, age 13, presents with annular lesions with scaly borders and central clearing on his trunk. What do you suspect? Tinea corporis. Question 20. Sandy asks what she can do for Dolores, her 90-year-old mother, who takes a bath every day and who has extremely dry skin. You respond: “Your mother does not need a bath every day.” Question 6. Erica, age 39, has a sudden onset of shivering, sweating, headache, aching in the orbits, and general malaise and misery. Her temperature is 102°F. The nurse practitioner diagnosed her with influenza (flu). What is your next course of action? Prescribe rest, fluids, acetaminophen (Tylenol), and possibly a decongestant and an antitussive. Question 7. You diagnose 46-year-old Mabel with viral conjunctivitis. Your treatment should include: Supportive measures and lubricating drops (artificial tears). Question 8. Which presentation is most concerning for skin cancer? Dark pigmentation of 1 solitary nail that has developed quickly and without trauma. Question 9. A 4-year-old male presents to your pediatric clinic with his mother complaining of an itchy rash, mostly between his fingers. This has been going on for multiple days and has been getting worse. The patient recently started at a new day care. On physical exam, the patient is afebrile and has multiple small (1-2 mm) red papules in sets of 3 located in the web spaces between his fingers. He also has signs of excoriation. What is the treatment for this problem? Permethrin lotion for the patient and also his family members. Question 10. Which of the following statements about psoriasis is not true? Psoriatic lesions often occur in the folds of the elbows and behind the knees. Question 11. Eric, age 52, has gout. What do you suggest? Limiting consumption of purine-rich foods. Question 12. Marge, age 36, is planning to go skiing with her fiancé. He has warned her about frostbite, and she is wondering what to do if frostbite should occur. You know she’s misunderstood the directions when she tells you which of the following? “I should rub the area with snow.” Question 13. Which disease usually starts on the cheeks and spreads to the arms and trunk? Erythema infectiosum (fifth disease). Question 15. A dark-field microscopic examination is used to diagnose: Syphilis. Question 16. Which of the following should be used with all acne medications? Sunscreen. Question 18. In a burn trauma, which blood measurement rises as a secondary result of hemoconcentration when fluid shifts from the intravascular compartment? Hematocrit. Question 2. Alexandra, age 34, was treated with oral antibiotics 2 weeks ago for a urinary tract infection. She is seen in the office today for a follow-up visit. On physical examination, the nurse practitioner notices that she has some painless, white, slightly raised patches in her mouth. This is probably caused by: Candidiasis. Question 4. Aaron, age 4, is brought in to the clinic by his father. His tympanic membrane is perforated from otitis media. His father asks about repair of the eardrum. How do you respond? “The eardrum, in most cases, heals within several weeks. Question 5. Sharon, a 47-year-old bank teller, is seen by the nurse practitioner in the office for a red eye. You are trying to decide between a diagnosis of conjunctivitis and iritis. One distinguishing characteristic between the two is: A ciliary flush. Question 7. A 25-year-old client who plays in a band complains that he finds it difficult to understand his fellow musicians at the end of a night of performing, a problem that is compounded by the noisy environment of the club. These symptoms are most characteristic of which of the following? Sensorineural loss. Question 8. Marcia, age 4, is brought in to the office by her mother. She has a sore throat, difficulty swallowing, copious oral secretions, respiratory difficulty, stridor, and a temperature of 102°F but no pharyngeal erythema or cough. What do you suspect? Epiglottitis. Question 9. An 80-year-old woman comes in to the office with complaints of a rash on the left side of her face that is blistered and painful and accompanied by left-sided eye pain. The rash broke out 2 days ago, and she remembers being very tired and feeling feverish for a week before the rash appeared. On examination, the rash follows the trigeminal nerve on the left, and she has some scleral injection and tearing. You suspect herpes zoster ophthalmicus. Based on what you know to be complications of this disease, you explain to her that she needs: Ophthalmological consultation. Question 10. Regular ocular pressure testing is indicated for older adults taking: High-dose inhaled glucocorticoids. Question 14. Client teaching is an integral part of successfully treating pediculosis. Which of the following statements would you incorporate into your teaching plan? “Itching may continue for up to a week after successful treatment.” Question 15. A 70-year-old client with herpes zoster has a vesicle on the tip of the nose. This may indicate: Ophthalmic zoster. Question 16. Which skin cancer that arises from skin cells, characteristically occurs on body areas exposed to the sun, most commonly presents as a pearly nodule with fine telangiectasias over the surface and a border that appears rolled, and is the most common skin cancer? Basal cell carcinoma. Question 17. Ashley, age 6 months, has a Candida infection in the diaper area. What do you suggest to the parent? “Keep the area as dry as possible. Question 18. Danny, age 18, presents with a pruritic rash on his upper trunk and shoulders. You observe flat to slightly elevated brown papules and plaques that scale when they are rubbed. You also note areas of hypopigmentation. What is your initial diagnosis? Tinea versicolor. Question 19. Elizabeth, age 83, presents with a 2-day history of pain and burning in the left forehead. This morning she noticed a rash with erythematous papules at that site. What do you suspect? Herpes zoster. Question 1. A 10-year-old male in 5th grade presents to the pediatric office with his mother complaining of itchy and red eyes for 1 day. The patient complains of watery drainage in both eyes, associated with repetitive itching. On physical exam, he has no fever or constitutional symptoms. His vision is normal, with no decrease in extraocular movements. The patient has a sibling that just started day care recently. He also has bilateral preauricular lymph nodes that are inflamed. What is the patient’s diagnosis? Viral conjunctivitis. Question 2. A 65-year-old man presents complaining of a left-sided, deep, throbbing headache and mild fatigue. On examination, the client has a tender, tortuous temporal artery. You suspect giant cell arteritis (GCA), or temporal arteritis. What is the least invasive procedure to help with diagnosis? Erythrocyte sedimentation rate (ESR). Question 4. Mandy, 44, was given a diagnosis of flu 1 day ago and wants to start on the “new flu medicine” right away. What do you tell her? “I’ll start you on oseltamivir (Tamiflu) today. It may shorten the course of the disease and perhaps lessen the severity of your symptoms.” Question 5. Mr. Clark, age 78, is being treated with timolol maleate (Timoptic) drops for his chronic open-angle glaucoma. While performing a new client history and physical, you note that he is taking other medications. Which medication would you be most concerned about? Atenolol (Tenormin), a beta blocker for high blood pressure. Question 7. How would you describe the cervical lymphadenopathy associated with asymptomatic human immunodeficiency virus (HIV) infection? Nontender, mobile, and firm but not hard lymph nodes. Question 8. A 22-year-old college student presents to your urgent care clinic complaining of a rash. She was recently on spring break and spent every night in the hot tub at her hotel. On physical exam, she has multiple small areas of 1- to 2-mm erythematous pustules that are present mostly where her bathing suit covered her buttocks. What is the most likely pathogen causing these lesions? Pseudomonas aeruginosa. Question 9. Which human papillomavirus serotypes most commonly cause cancer? Serotypes 16 and 18 Question 10. An eczematous skin reaction may result from: Penicillin. Question 11. When palpating the skin over the clavicle of Norman, age 84, you notice tenting, which is: Common in thin older adults. Question 15. You are teaching Harvey, age 55, about the warts on his hands. What is included in your teaching? Warts are caused by the human papillomavirus. Question 16. Jill, age 29, has numerous transient lesions that come and go, and she is diagnosed with urticaria. What do you order? Antihistamines. Question 19. Dan, age 57, has just been given a diagnosis of herpes zoster. He asks you about exposure to others. You tell him: He should stay away from children and pregnant women who have not had chickenpox. Question 20. Martin, age 13, just started taking amoxicillin for otitis media. His mother said that he woke up this morning with a rash on his trunk. What is your first action? . Stop the amoxicillin. Question 1. Which of the following is not a modifiable risk factor? Race. Question 2. Which of the following is not a subjective finding? Respiratory rate. Question 3. What intervention would not be included in the definition of secondary health promotion? Computed tomography (CT) scan of the head for all car accident victims. Question 4. Which of the following refers to an aspect of a patient’s health that can be changed or affected by a health intervention? Modifiable risk factor. Question 5. Which of the following refers to an aspect of a patient’s health that cannot be changed or affected by a health intervention? Nonmodifiable risk factor. Question 6. Which of the following patients is health literate? A 62-year-old female who speaks the language of her provider, has Medicare for insurance, and can drive. Question 7. All of the following statements about the US Preventive Services Task Force (USPSTF) are true except? All of the recommendations made by the USPSTF are strong recommendations. Question 8. Between ages 7 and 18, both boys and girls are immunized against the following diseases: Tetanus, diphtheria, pertussis, meningitis, and human papillomavirus. Question 9. Telehealth has shown a drastic increase in utilization by patients in which of the following fields of medicine? Psychology and psychiatry. Question 10. Eileen, a 42-year-old woman, comes to your office with a chief complaint of fatigue, weight loss, and blurred vision. Eileen has a past medical history that is negative for any chronic medical problems. You obtain a fasting chemistry panel, lipid profile, complete blood count (CBC), and hemoglobin A1c (HbA1c). The results of the blood work show Eileen’s blood sugar elevated at 356 mg/dL, total cholesterol elevated at 255, high-density lipoprotein (HDL) cholesterol low at 28, low-density lipoprotein (LDL) cholesterol elevated at 167, triglycerides 333, and HbA1c 12. On questioning Eileen further, you discover that both her grandmothers had adult-onset diabetes mellitus. You diagnose type 2 diabetes mellitus. Your treatment plan should include a cholesterol-lowering agent, an agent that lowers blood sugar, and which other class of medication? Angiotensin-converting enzyme (ACE) inhibitor. Question 11. A lab value that is commonly decreased in older adults is: Creatinine clearance. Question 12. Dennis, age 62, has benign prostatic hyperplasia (BPH). He tells you that he voids at least 4 times per night and that he has read about a preventive drug called terazosin hydrochloride (Hytrin) that might help him. What do you tell him? “It’s not a preventive drug, but it relaxes smooth muscle in the prostate and bladder neck.” Question 13. You are sharing with your client the idea that he needs to get some counseling to deal with his severe stress because it is affecting his physiological condition. Which of the following hormonal changes occurs during severe stress? . An increase in cortisol. Question 14. Margaret, age 29, is of medium build and 5 ft 4 in tall. You estimate that she should weigh about: 120 lb. Question 15. Martha, age 82, has an asymptomatic carotid bruit on the left side. What do you recommend? No treatment at this time. Question 16. When performing a sports physical exam on Kevin, a healthy 16-year-old boy, which question in the history is important to ask Kevin or his guardian? Did anyone in your family ever have sudden cardiac death? Question 17. If a screening test used on 100 individuals known to be free of breast cancer identified 80 individuals who did not have breast cancer while missing 20 of the individuals, the specificity would be: 80%. Question 18. Harvey, age 55, comes to the office with a blood pressure (BP) of 144/96 mm Hg. He states that he did not know if it was ever elevated before. When you retake his blood pressure at the end of the examination, it remains 144/96. What should your next action be? Try nonpharmacological methods and have him monitor his blood pressure at home. Question 19. Mimi, age 52, asks why she should perform a monthly breast self-examination (BSE) when she has her mammograms on schedule. You respond: “More than 90% of all breast abnormalities are first detected by self-examination.” Question 20. Which of the following individuals should get the shingles (herpes zoster) vaccine? Joe, who has a stressful job. Question 3. As a primary care provider, which of the following topics is not typically important for adults aged 20 to 40? Focusing on increasing lifespan Question 4. As a nurse practitioner, which of the following would not be an example of primary health promotion? Posting health articles on your social media account. Question 5. Which of the following initiatives does not fall under the National Prevention Strategy? Diabetes management. Question 7. The OLD CARTS (onset, location, duration, character, aggravating/alleviating factors, radiation, timing, severity) mnemonic is best used in which part of your chart note? History of present illness. Question 8. A nurse practitioner is practicing based on the rule-based actions he was taught in school and doesn’t understand when/where those rules may be inappropriate. Which following statement best describes this skill level? Novice. Question 9. Mildred, an independent 92-year-old woman, is moving into her daughter’s home. Her daughter comes to see you seeking information to help keep her mother from falling. Which of the following interventions would you suggest she do to help prevent Mildred from falling? Remove all loose rugs from floors and install hand grasps in bathtubs and near toilets. Question 10. Joseph, a 55-year-old man with diabetes, is at your office for his diabetes follow-up. On examining his feet with monofilament, you discover that he has developed decreased sensation in both feet. There are no open areas or signs of infection on his feet. What health teaching should Joseph receive today regarding the care of his feet? “See a podiatrist yearly; wash your feet daily with warm, soapy water and towel dry between the toes; inspect your feet daily for any lesions; and apply lotion to any dry areas.” Question 11. Sandra, a 27-year-old nurse, states that she does not want to get the hepatitis B virus vaccine because of its adverse effects. You tell her that the most common adverse effect is: Pain at the injection site. Question 12. Harry is taking his entire family to Central America and is wondering about protection against bites from malaria-causing mosquitoes. What advice do you give him? Use an insect repellent with diethyltoluamide (DEET) for adults and permethrin for children, and stay inside from dusk to dawn. Question 14. Susie, age 5, comes to the clinic for a well-child visit. She has not been in since she was 2. Her immunizations are up to date. What immunizations would you give her today? Diphtheria, tetanus, and pertussis (DTaP); inactivated polio vaccine (IPV); and measles, mumps, and rubella (MMR). Question 15. Mary, a 70-year-old woman with diabetes, is at your office for her 3-month diabetic checkup. Mary’s list of medications includes metformin (Glucophage XR) 1000 mg daily, an angiotensin-converting enzyme (ACE) inhibitor daily, and 1 baby aspirin (ASA) daily. Mary’s blood work showed a fasting blood sugar (FBS) of 112 and glycosylated hemoglobin (HbA1c) of 6.5. You tell Mary that her blood work shows: That her diabetes is under good control and she should remain on the same medications Question 16. Sandy, a 68-year-old woman, presents to your office for screening for osteoporosis. She states that her grandmother and mother both lost inches in their old age. She has been postmenopausal for the past 15 years and never took any hormone replacement medications. She is Caucasian, weighs 108 lb, and is 5 ft 1 in tall on today’s measurement. When do women lose the greatest amount of bone density? The first 10 years after menopause. Question 18. Julia, age 18, asks you how many calories of fat she is eating when 1 serving has 3 g of fat. You tell her: 27 cal. Question 19. Marian’s husband, Stu, age 72, has temporal arteritis. She tells you that his physician wants to perform a biopsy of the temporal artery. She asks if there is a less invasive diagnostic test. What test do you tell her is less invasive? Color duplex ultrasonography. Question 20. For which patient would you administer the human papillomavirus (HPV) vaccination? Janice, age 17, who had a baby 6 months ago and is breastfeeding. Question 1. Which of the following demonstrates a subjective finding? Pain level. Question 3. Which of the following statements about health promotion is false? Health promotion is a benefit to add to your practice if you have time. Question 4. Which of the following statements defines health literacy? The level to which a patient can understand, gain access to, and make proper medical decisions. Question 5. The study of the way diseases are spread through groups and what causes and helps spread these diseases is called? Epidemiology. Question 6. Which of the following statements does not belong in the past medical history portion of your chart note? Your patient had lab work at their last appointment that was negative. Question 7. An 81-year-old patient presents for a physical. She recently had a fall and now has problems walking up her stairs. The only restroom in the house is on the second floor. She also has a flight of stairs outside her house she has to navigate in order to reach street level, and this is difficult for her. Where does this information belong in your chart note? Functional health patterns. Question 10. Mark, a 56-year-old man, comes to your practice seeking help quitting smoking. You prescribe varenicline (Chantix), a prescription medication, to aid with his attempt. What instructions do you give Mark regarding how to stop smoking with Chantix? Start the Chantix today according to the dosing schedule and then pick a date to stop smoking about 7 days after starting Chantix. Question 11. How do you respond when Jill, age 42, asks you how long she should work out each week? Exercise for at least 30 minutes 5 days per week. Question 12. Marvin is a gay man who is ready to “come out.” What is the last step in the process of coming out? Identity integration and self-disclosure. Question 16. Jan’s mother has Alzheimer disease (AD). Jan tells you that her mother’s recent memory is poor and that she is easily disoriented, incorrectly identifies people, and is lethargic. Jan asks you, “Is this as bad as it gets?” You tell her that her mother is in which stage of the disease? Stage 3. Question 17. Herbert, a 69-year-old man, comes to your office complaining of nocturia. On questioning Herbert, you find that for the past 3 months he has been getting up at least 5 times a night to void. He came in to seek help today because of his wife’s insistence that he be checked out. When you perform the digital rectal exam, you find that his prostate protrudes 3 to 4 cm into the rectum. What grade would you assign to Herbert’s prostate enlargement? Grade 3 [Show More]
Last updated: 1 year ago
Preview 1 out of 111 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 08, 2021
Number of pages
111
Written in
Additional information
This document has been written for:
Uploaded
Dec 08, 2021
Downloads
0
Views
42

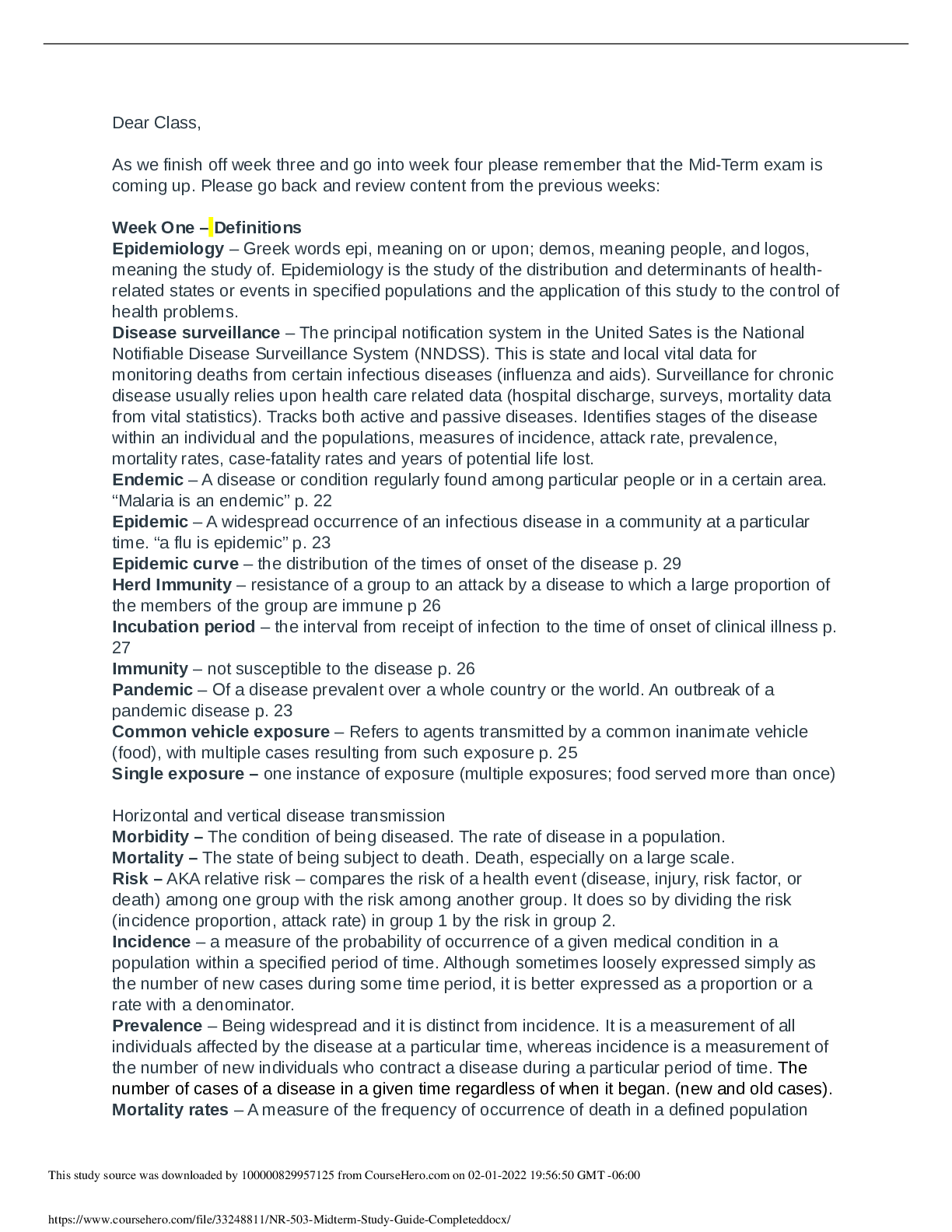
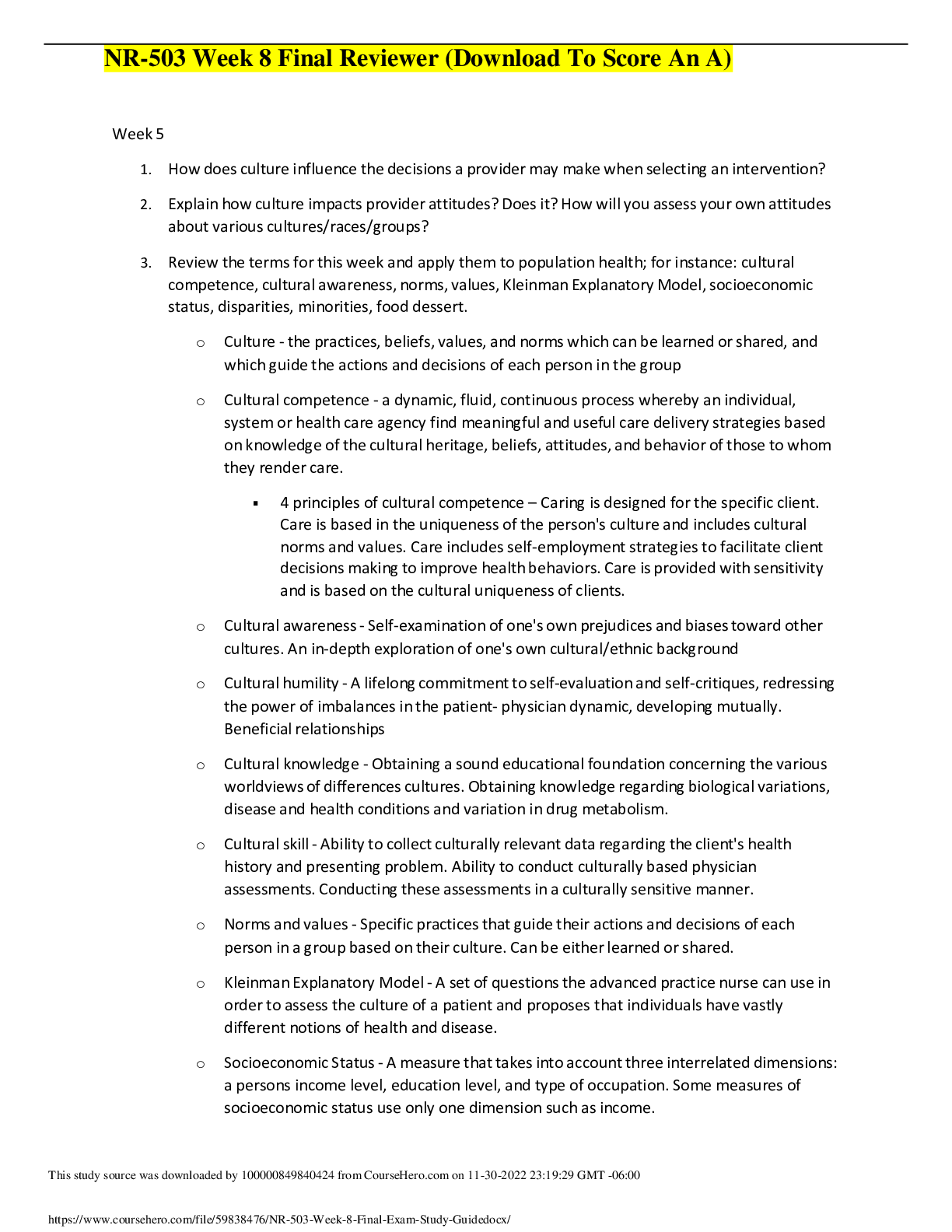
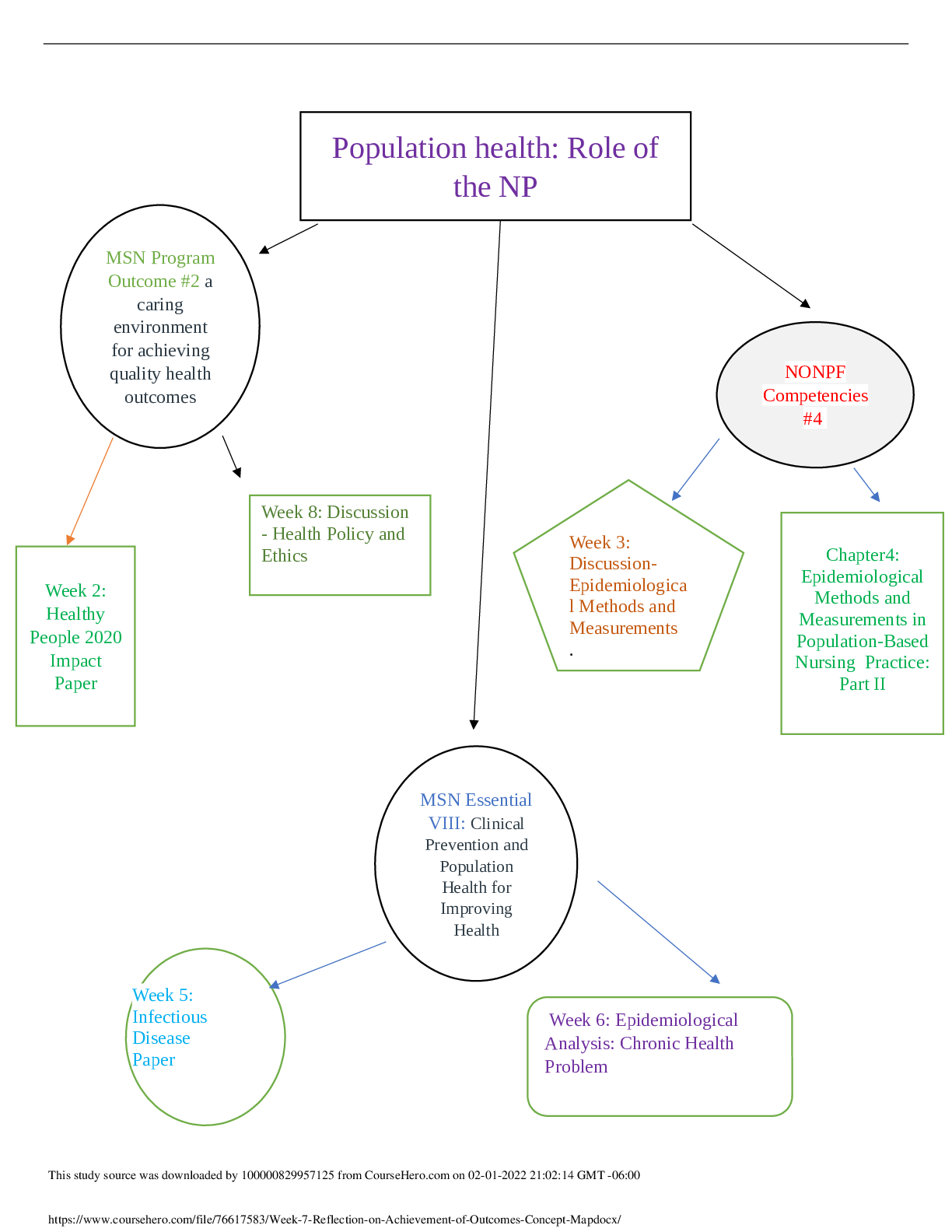
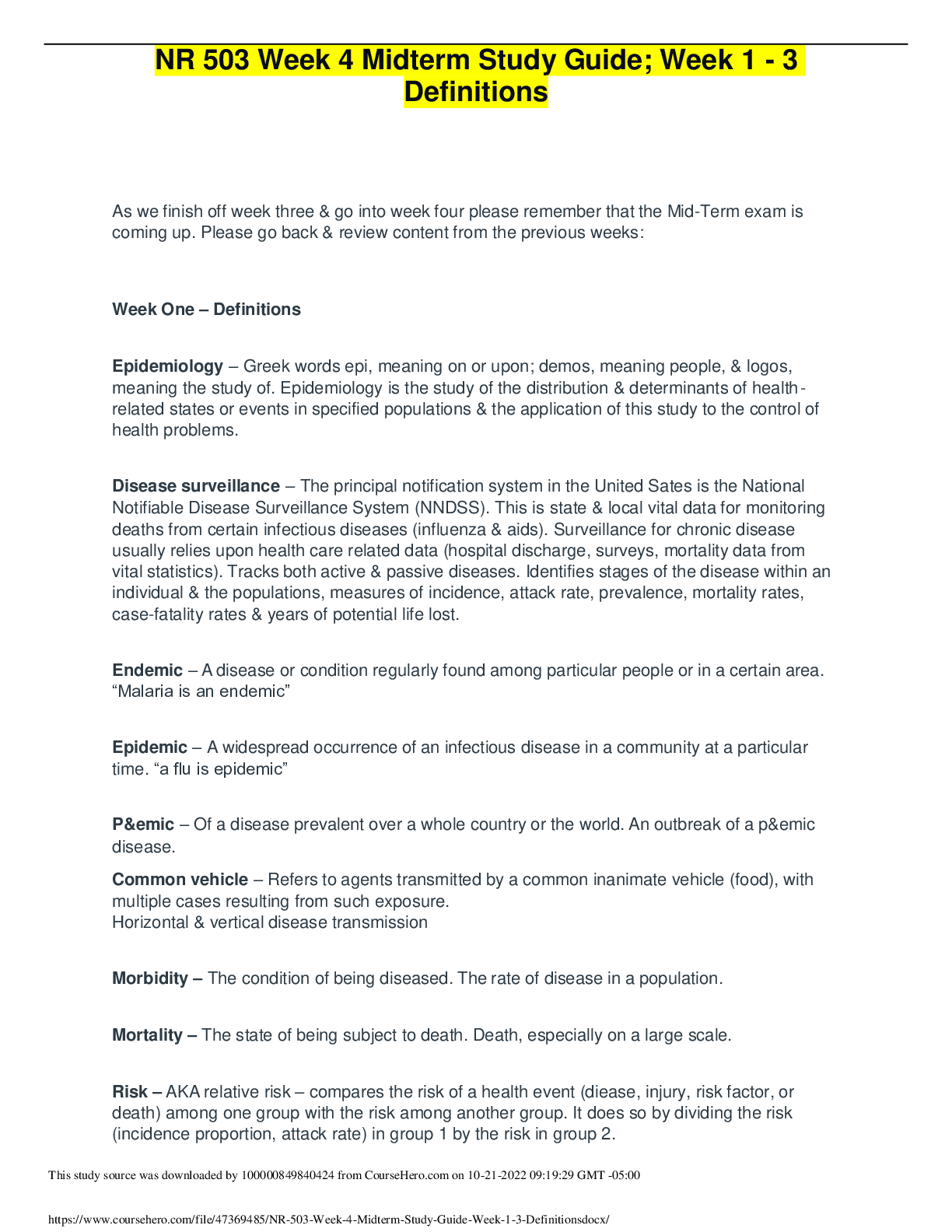
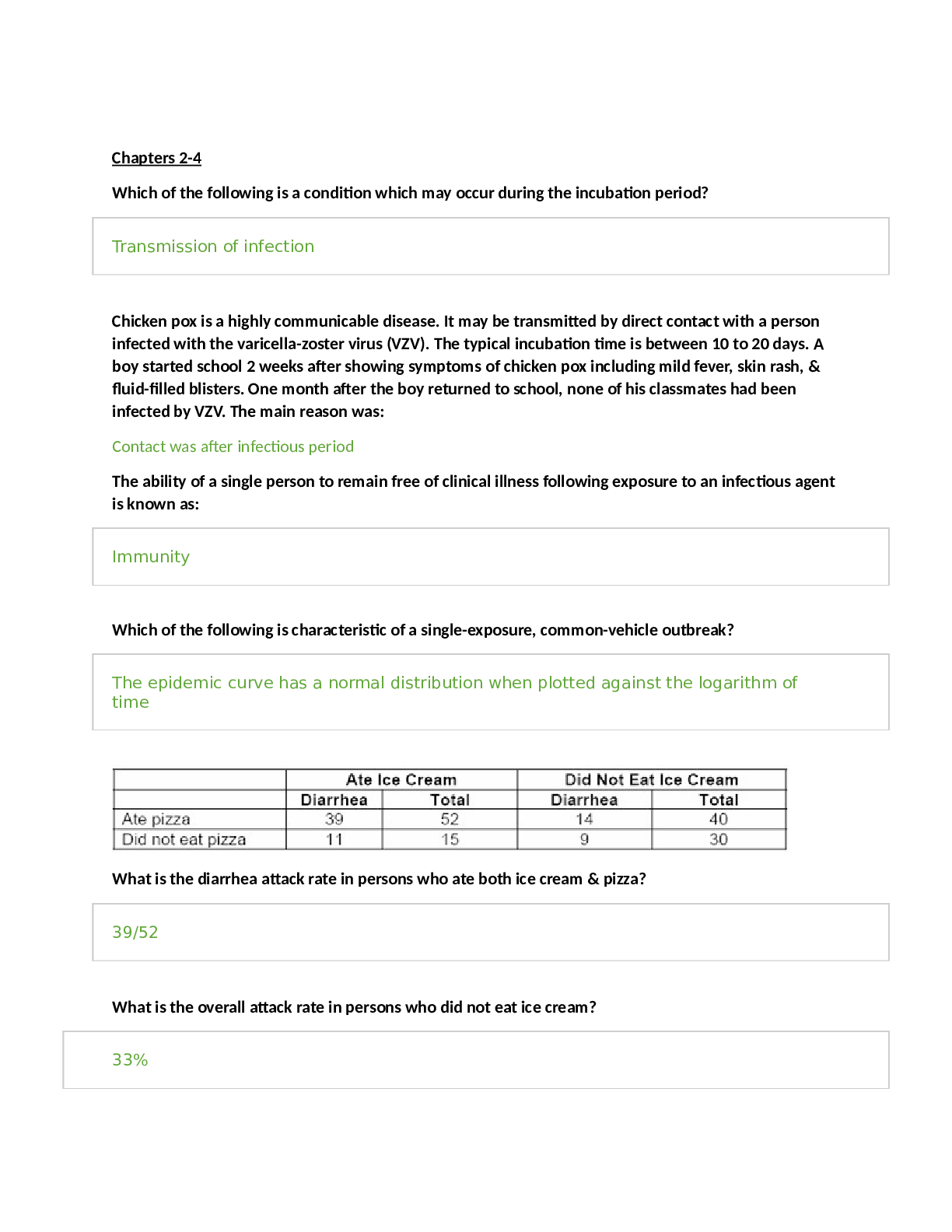
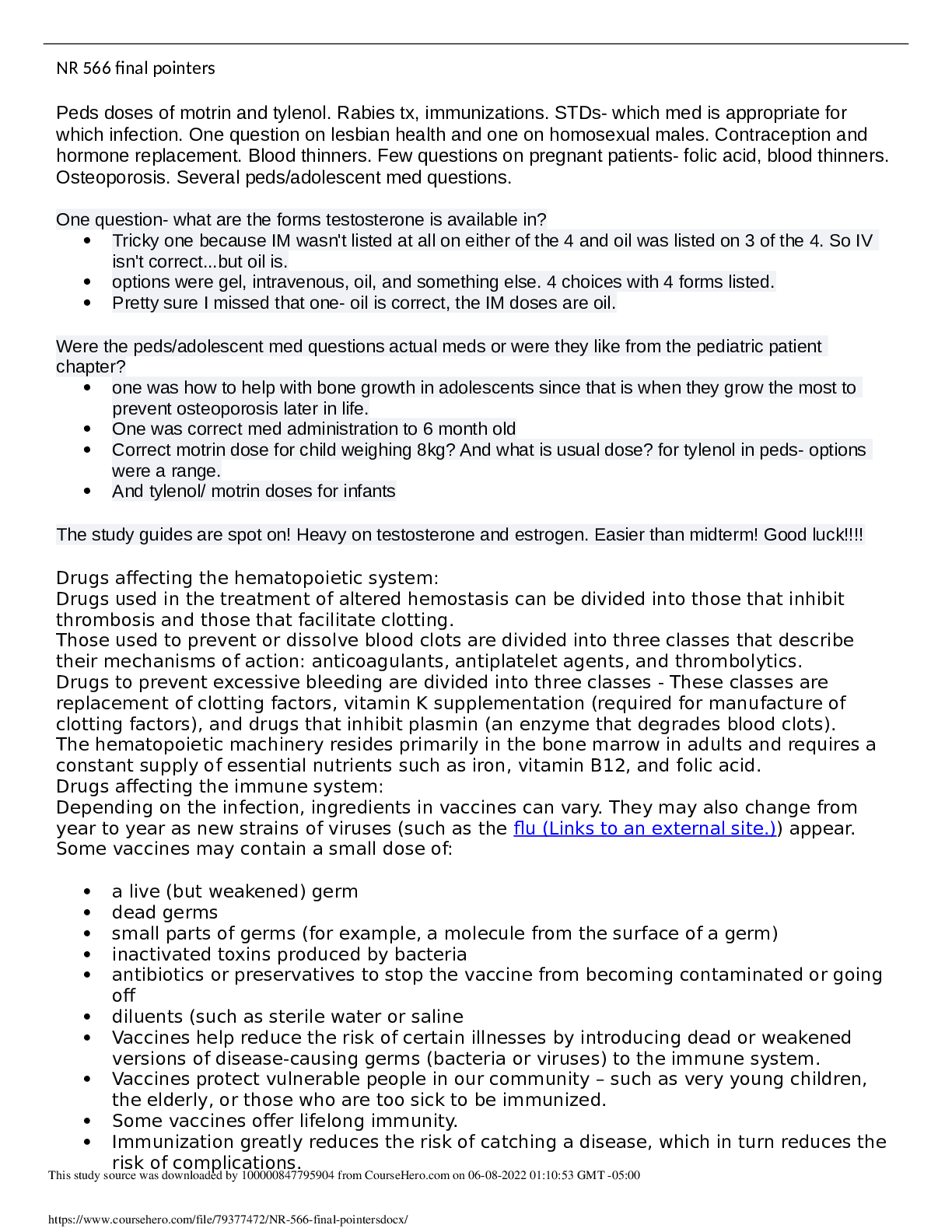
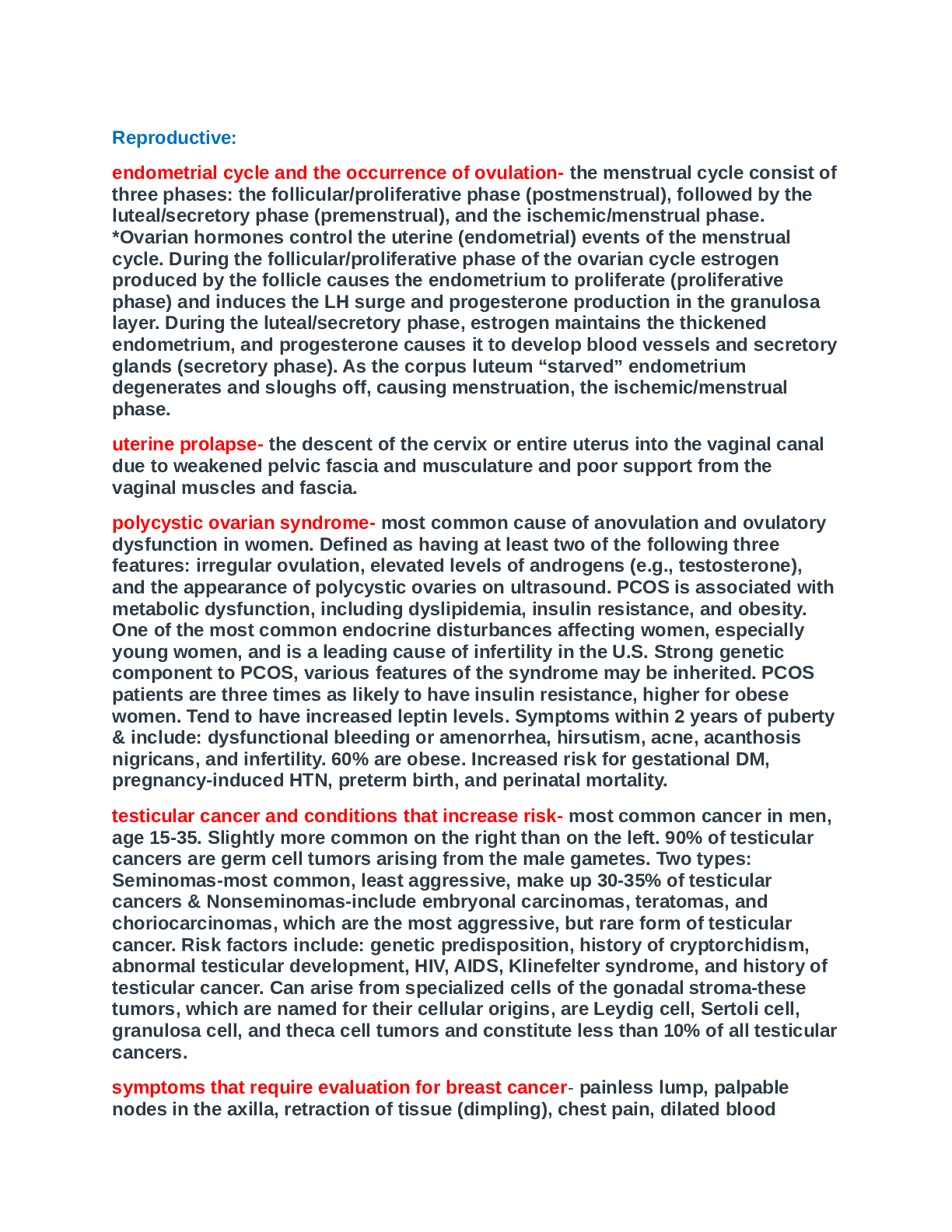
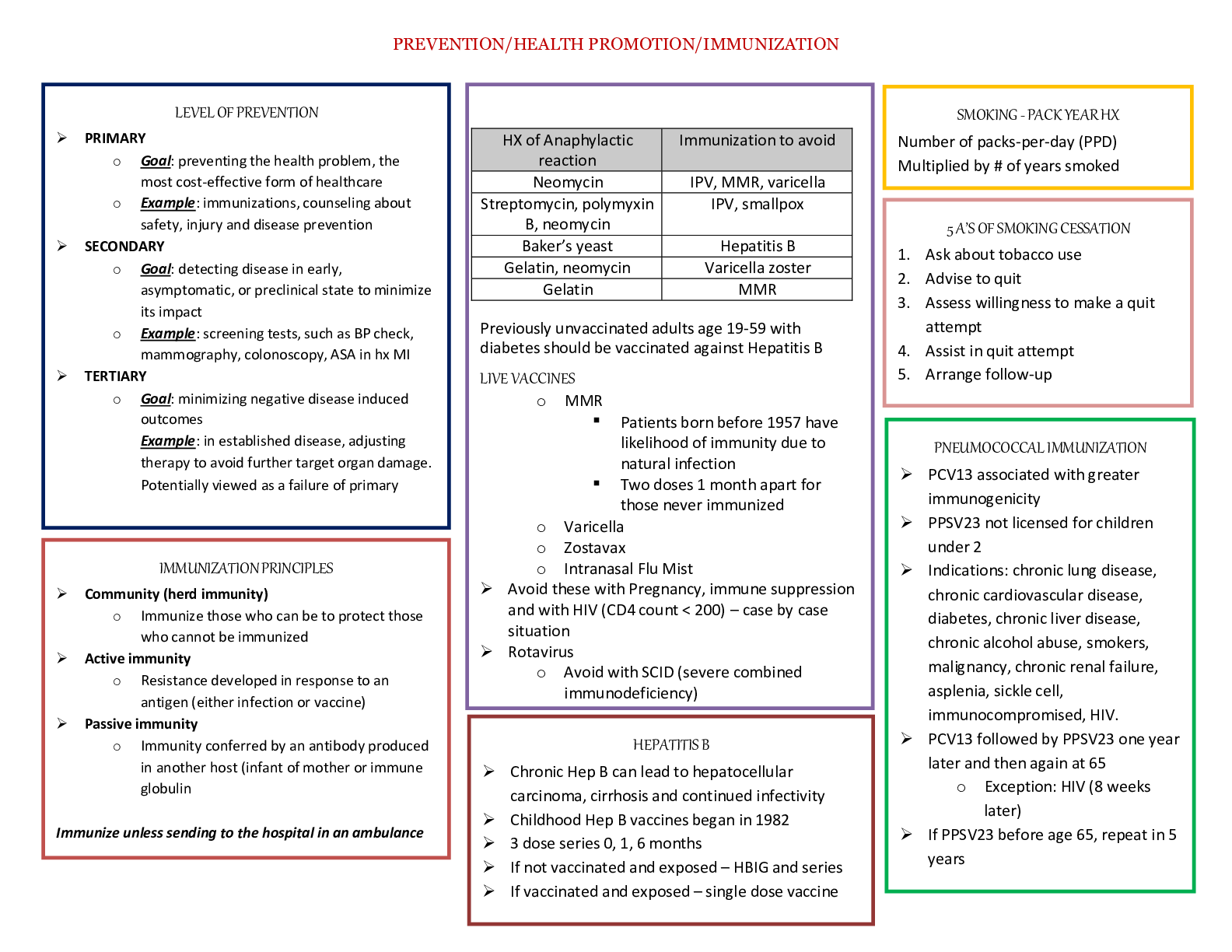
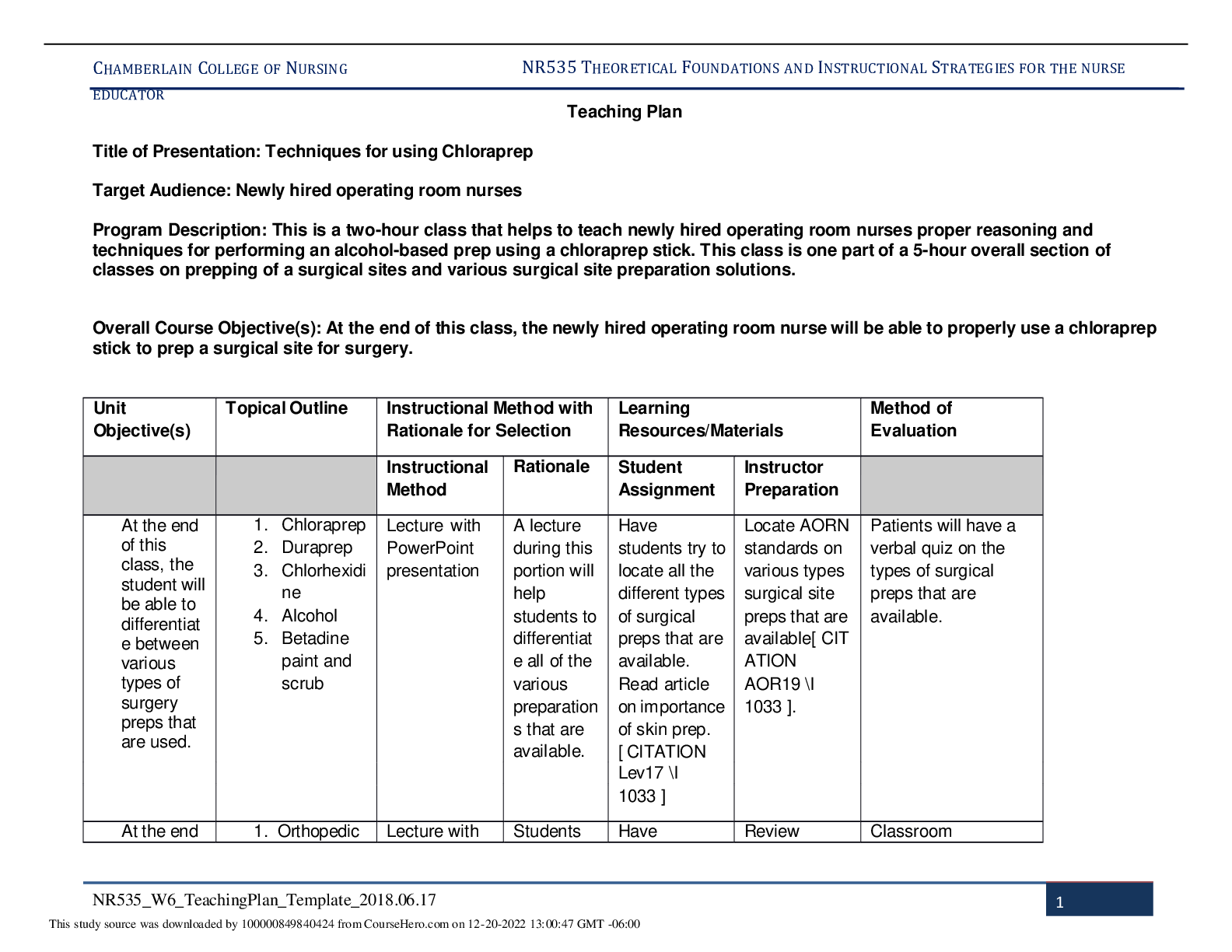
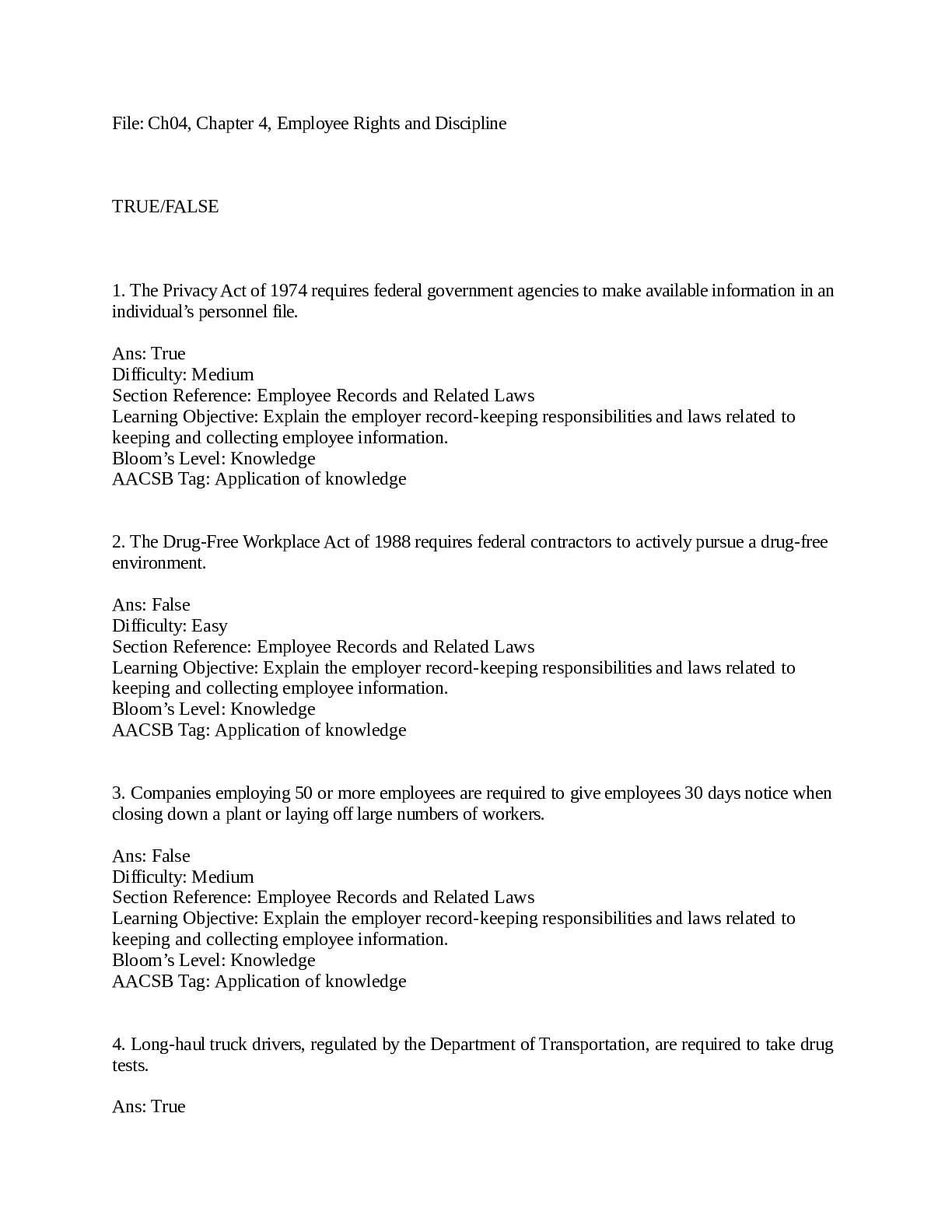

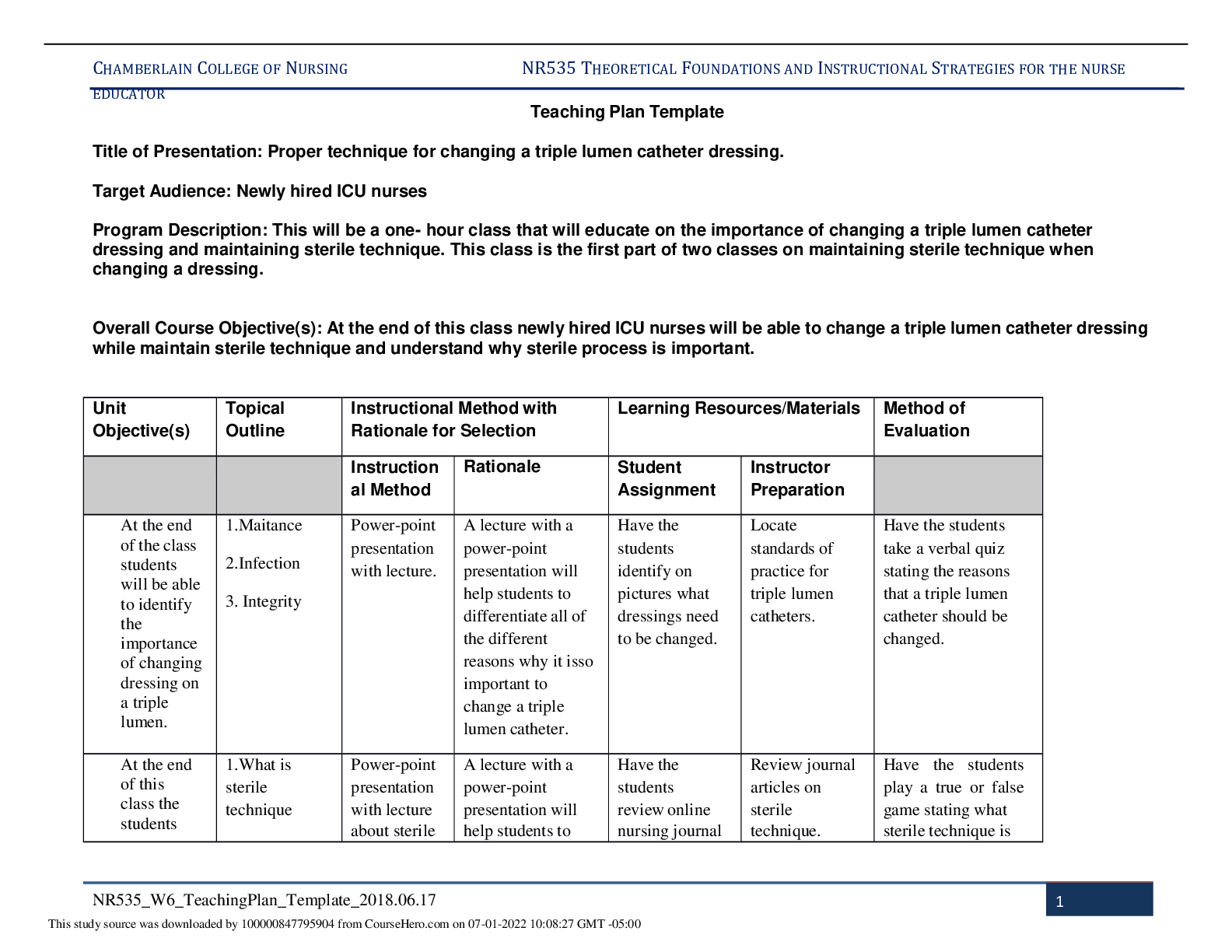
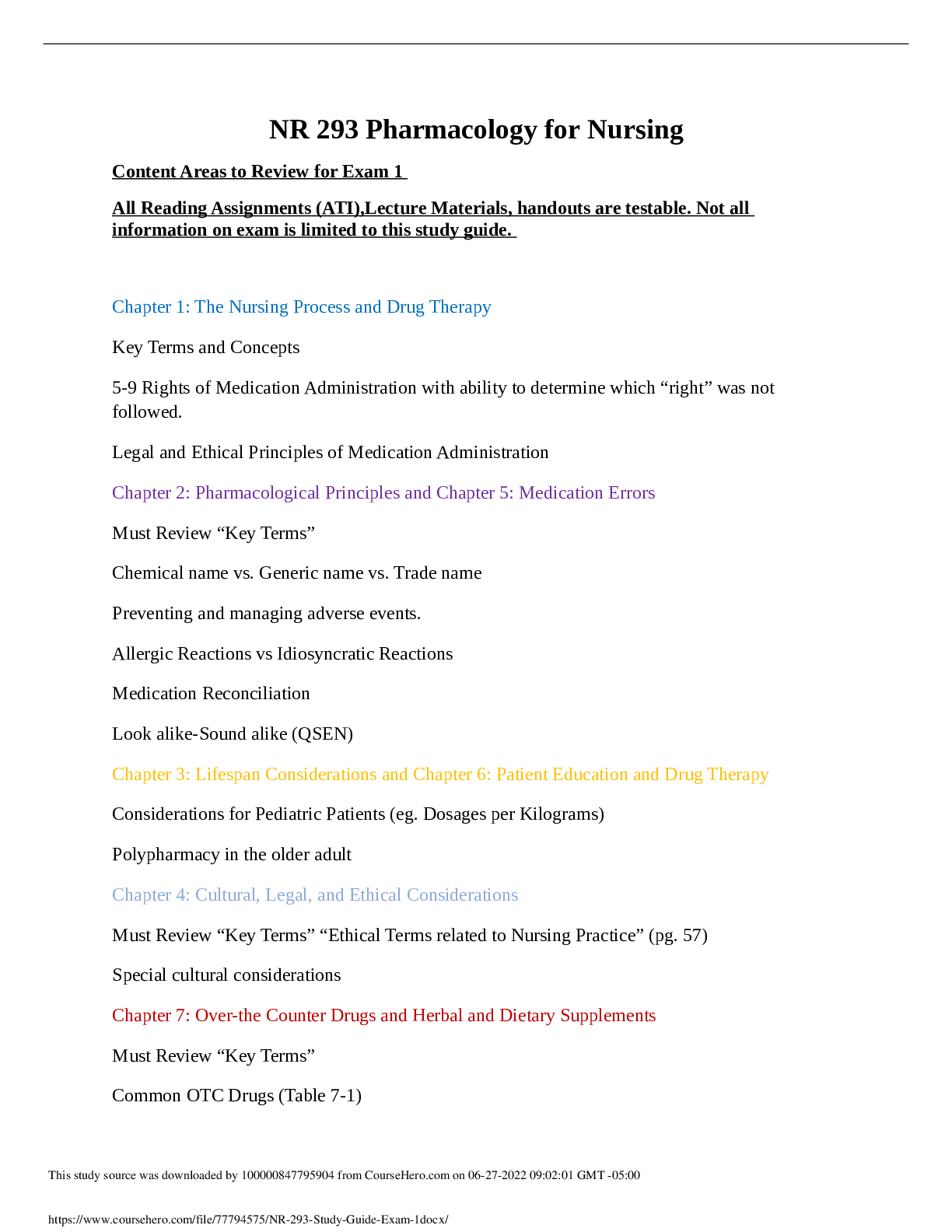

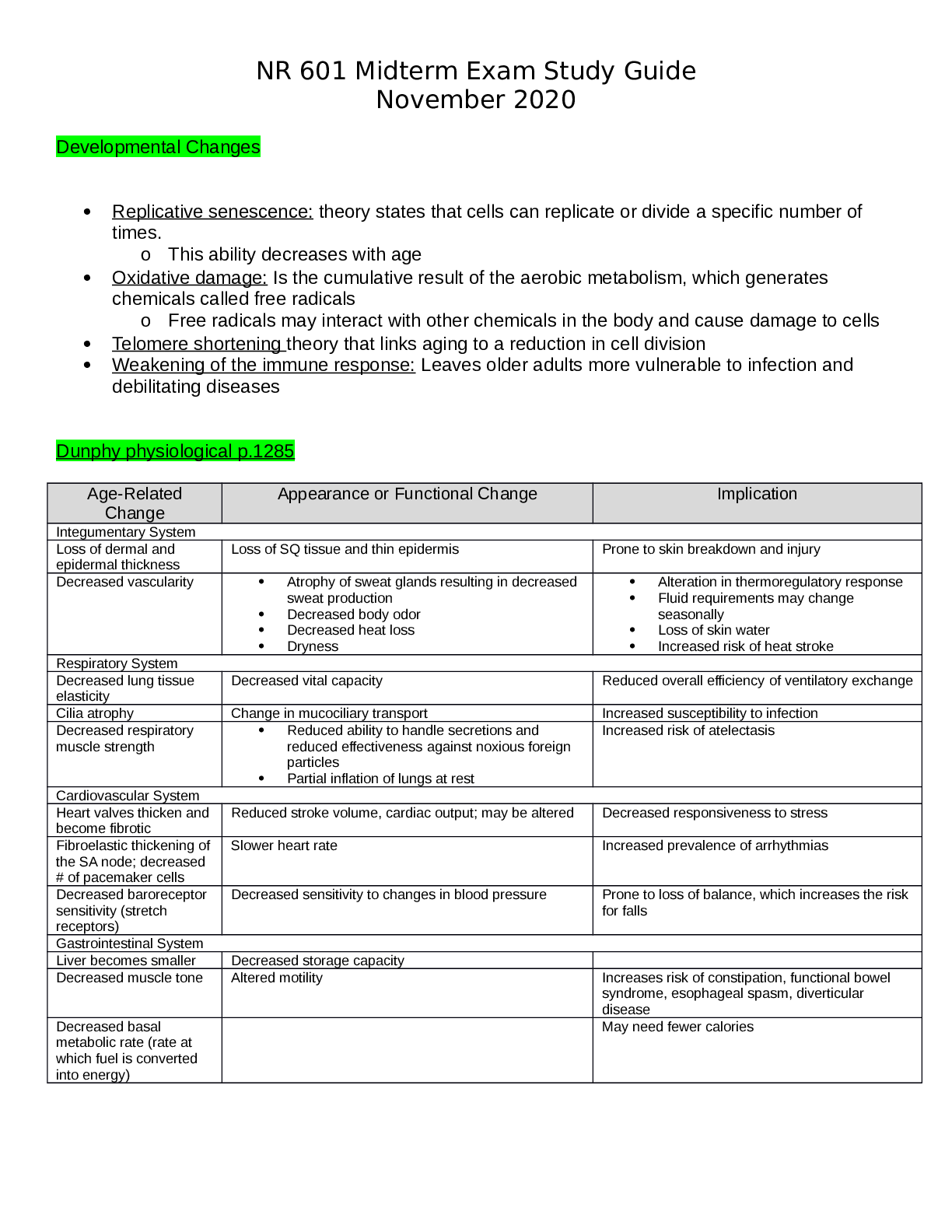
.png)
.png)