*NURSING > STUDY GUIDE > NR 340 Week 3 Exam One (Version 1 & 2) STUDY GUIDE | Download To Score An A (All)
NR 340 Week 3 Exam One (Version 1 & 2) STUDY GUIDE | Download To Score An A
Document Content and Description Below
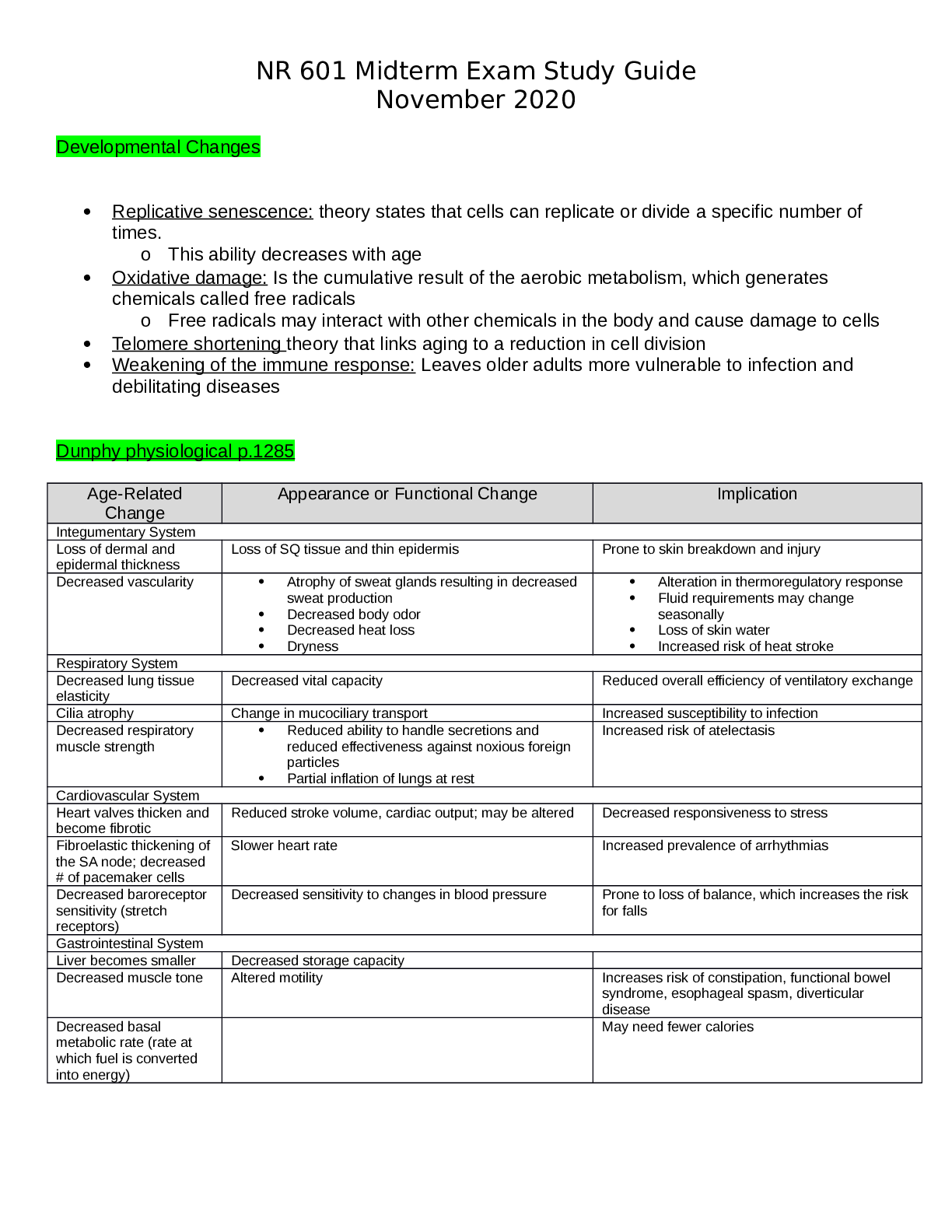
NR 340 Week 3 Exam One (Version 1 & 2) EXAM 1 CRITICAL CARE Critical Care • Direct delivery of medical care within a specialized unit with specialized personnel o Mainly for the treatment ... of life-threatening problems o Levels of Care ▪ I: Most comprehensive, typically a teaching environment • Staffed by specialty Drs & RNs ▪ II: Limited care to specialty patients • burn units ▪ III: Limited availability for comprehensive critical care • med-evac to a more comprehensive facility if out of scope for care o Types of Units ▪ Open Unit • Docs aren't ICU based, so frequent calls out occur • multidisciplinary team is based in ICU • Possible use of an Intensivist for patient management ▪ Closed Unit • Physician collaboration • Multidisciplinary team with an Intensivist • Better patient outcomes than with an open unit o Sentinel Events ▪ actual or potential outcomes that can cause patient harm or death ▪ commonplace in ICUs o Strategies for Error Prevention ▪ Forcing Functions • used to correct errors that can occur within the patient care setting • no mixing of own meds o done at the pharmacy level or hand delivered to the unit ▪ Use patient constraints • allergy bands, fall risk identification, height or weights ▪ Restrict number of hours that can be worked in succession ▪ Use timeouts prior to procedures ▪ simplify processes Ethical Principles • Advocacy o act on behalf of the patient foremost, then the family • Autonomy o patient has the right to determine what, if any medical care they may receive • Beneficence o duty to prevent/remove harm & promote good • Nonmalficence o do no harm • Justice o fair allocation & distribution of health resources to all • Confidentially o respect for the right to control patient information o HIPPA CC Nurse Stressors • Moral distress o providing aggressive care to patients who may not benefit from it powerlessness o unable to find meaning in suffering ▪ doing invasive procedures that will not help in the end o lots of RNs leave ICU environment r/t loss of inability to have compassion for pts • Compassion Fatigue o difficulty separating work from personal life o lowered frustration tolerance o angry outbursts o depression Sources of stress for patients and families • inability to communicate related to tubes, etc • anxiety • sleeplessness • delirium related to environment, lack of sleep • pain Communication with critically ill patients • difficult for patient & RN • sedation results in issues with communication • RN must anticipate what pt needs • use of writing tools may help with communication Pain Management • unpleasant sensory & emotional experience • Predisposing factors for pain o disease, procedures, trauma, nursing care o Influence on pain perceptions ▪ expectations & previous pain experiences ▪ emotional & cognitive state • Assessment Tools o Numerical pain scoring ▪ 0-10, with 0=no pain & 10=worst pain imaginable o Wong-Baker faces ▪ useful in children and those who may not speak English well or at all o Behavioral Pain Scale ▪ Facial expression (1=relaxed up to 4=grimacing) ▪ Upper limbs (1=no movement up to 4=permanently retracted) ▪ Compliance with Vent (1=tolerating movement up to 4=unable to control ventilation) o FLACC ▪ Face ▪ Legs ▪ Activity ▪ Cry & Consolability • Pharmacological Management of Pain o Opioids (CNS)-watch for resp. depression & hypotension ▪ Morphine sulfate • Potent with a rapid onset (~5m) • drug of choice (1st line) • inexpensive • duration ~2h, so can be given PRN ▪ Fentanyl • extremely potent with faster onset than morphine (~1-2m) • use for acute distress or ongoing hemodynamic instability o NSAIDs (PNS)-increases risk for GI bleeds, renal (I) or liver (A) insufficiency; decreases need for opioid medications ▪ Tylenol (Acetominophen) ▪ Motrin (Ibuprofen) ▪ Toradol • good for use as an all-over anti-inflammatory o PCAs (patient controlled analgesia) ▪ Patient must be able to manage pump to be effective ▪ best for patients with • elective surgery • large surgical or traumatic wounds • normal cognitive/motor skills Anxiety • prolonged state of apprehension in response to fear • agitation, autonomic arousal, pain, sleep deprivation, noises in hospital setting • predisposing factors o ET tube o alarms from monitors o inability to move freely o sleep deprivation Delirium: causes and assessment. • acutely changing mental status & inattention o hyperactive-agitated, combative, disoriented, restless ▪ pt may be hard to keep in bed o hypoactive-quiet, depression, withdrawn, flat affect, lethatgic o mixed-fluctuation between hyper/hypo states ▪ sundowning • Assessment o CAM-ICU ▪ worksheet to watch for acute changes in pt o ICDSC ▪ watches for disorganized thinking and decreased alertness • Predisposing factors o polypharmacy o benzodiazepine & narcotic use o infection/sepsis o preexisting dementia & sleep disruptions • Management o medication & environmental control ▪ Sedatives • Haldol (5 mg) • Ativan (2 mg) ▪ calm environment • quiet with limited stressors, i.e. bright lights, loud sounds • provide patient with glasses, hearing aids, etc ▪ review current medications & make changes as needed • decrease or discontinue drugs that cause delirium • titrate all medications to desired sedation level Sedative Agents • given to reduce symptoms • dosage determined by scales o RASS o Ramsey o SAS; Riker • Medications o Sedative-hypnotics ▪ Propofol o Benzodiazepines ▪ Versed (midazolam) • potent, with rapid onset & short duration • short term use, like procedural sedation ▪ Ativan (lorazepam) • less potent, with slow onset & longer duration • longer term use, preferred >48h o Meds can be given around the clock if needed o reach "steady state" where loading dose is given then maintenance doses o decrease medications over time as condition improves (weaning) ▪ decrease doses in elderly & those with renal disorders • Neuromuscular Blockades o used to facilitate treatment or procedures, incl. difficult/emergency intubations, elevated ICP, or improve tolerance to mechanical ventilation o Must provide sedation-no analgesic or sedative properties o monitor with "train of four" ▪ watch for tremors with stimuli • NMB is working with 4x twitch • goal is 2x twitch Nutrition support: assessment; complications of tube feedings; parenteral nutrition: complications • Basic nutrition aids in wound healing, provides basic metabolic needs, tissue repair & immune function o trauma or mechanical ventilation requires an increase in nutritional needs • Assessment data o PMH o malabsorption syndrome o I&O,daily weights o gag reflex, dentition & dysphagia o hydration restrictions • Enteral Nutrition o nourishment via feeding tube placed into GI tract ▪ NG/OG tubes • short term use (<3 mo) • do not use OG if patient is alert & talking, use for intubations ▪ GJ tubes • longer term use (>3 mo) o lower risk of infection o less expensive o contains proteins, vitamins, calories, & minerals needed o Feeding schedules ▪ intermittent • gastric ▪ continuous • small bowel o residual assessment ▪ return all residuals back through tube ▪ 200-250 is a concern ▪ >500 pt is not tolerating feedings o start @ 10 ml/hr & titrate to goals o check tube placement to reduce risk of aspiration pneumonia ▪ air of pH ▪ keep HOB @ 30* minimum • Parenteral Nutrition o infusion of nutrient solutions into the bloodstream ▪ Central Line (TPN) ▪ Peripheral Line (PPN) o Use in patients that can't tolerate enteral feedings ▪ GI obstruction ▪ intractible vomiting/diarrhea ▪ NPO for >1 week o inability to meet nutritional demands with EN only o use of a dedicated PN line is needed o use aseptic technique when dressings/lines are changed o assess site q12h, verify placement with CXR o Complications ▪ gut atrophy ▪ overfeeding ▪ sepsis ▪ hyper/hypoglycemia ▪ F&E imbalances o Evaluation ▪ monitor albumin ▪ H&H ▪ E-, including K, Mg, Phos Mechanisms of Injury in Trauma • Trauma o physical injury or wound caused by external forces ▪ ex. stabbing, GSW • Injury o uncontrolled/acute source of energy makes contact with the body & body can't tolerate exposure ▪ energy sources • mechanical/kinetic • thermal • chemical • electrical • radiate o Types ▪ Blunt force • most common • skin remains intact with widespread injury underlying the area of impact • MVAs, assault, falls from heights, sports • severity depends on kinetic energy involved ▪ Penetrating • open disruption of the skin • lacerations, punctures, amputations Levels of Trauma Care • Level 1 o teaching environment o state of the art • Level 2 o care provided for trauma patients & transferred to a level 1 if needed • Level 3 o community hospital where no level 1 or 2 exists • Level 4 o provides advanced trauma life support & transfer Assessment Priorities • Primary assessment-done in 1-2 min o A-airway patency with C-Spine immobile ▪ talking=breathing o B-breathing presence & effectiveness o C-Circulation; presences of pulses or external hemorrhage o D-disability (neuro status) ▪ ANOx_ o E-expose patient/environment control ▪ strip naked & check for other injuries o Treat all life threatening/major injuries before moving on to secondary assessment • Secondary Assessment-after major injuries are stabilized o F-full set of vitals/talk to family o G-give comfort measures (pain control) o H-head to toe assessment & history o I-inspection of posterior surfaces ▪ logroll patient only until spinal injury is ruled out Triage process and levels of care • determine if patient needs to be transferred to a level 1 center for further treatment o made by prehospital personnel (EMS) • Classes o 1-emergent-Red ▪ critical, life threatening ▪ immediate care required ▪ compromised airway, shock, or hemorrhage o 2-urgent-Yellow ▪ major illness or injury ▪ treatment required within 30-120 min ▪ open fracture, chest wound o 3-nonurgent-Green ▪ care can be delayed 2+ hours ▪ minor injuries, walking wounded ▪ closed fracture, sprain, strain o 4-expectant-Black ▪ dead or expected to die ▪ massive head injury, extensive full-thickness burns • Diagnostic tests o ABGs, CBC, T&C o UA, BMP/CMP o ETOH/drug screen o Xray, abdominal US, CT o tetanus shot Facial Fractures • Blunt trauma-MC • Assessment o airway compromise o C-Collar until cleared o hemorrhage/nosebleed o malocclusion of teeth/jaw out of place o CSF leak ▪ nose or ear ▪ complaints of salty taste ▪ halo test • Management o Maintain ABCs ▪ breathe on own or intubation o Maintain C-spine immobilization o maintain SaO2 o IV access ▪ 16 or 18 ga x2 o control bleeding Uncomplicated Rib/Sternal Fractures • Chest wall injuries-MC o MOI-blunt trauma • Assessment o pain localized over site o tenderness/muscle spasm o pain worse with cough, deep breath, motion o chest wall deformity o can show up weeks later due to calcification-may not show up on Xray immediately • Management o splint chest with hands or pillow o pain relief ▪ pain typically subsides in 5-7 days o O2 therapy o IS to encourage lung expansion & prevent pneumonia Flail Chest • two or more ribs broken in 2+ places o piece moved independently from rest of ribcage o fragment can puncture lung ▪ pneumothorax ▪ hemothorax ▪ tension pneumothorax o often a fatal condition o one side of chest rises, other does not ▪ depression of segment on inspiration (opposite of normal) • Assessment o dyspnea o paradoxical motion of chest o severe pain at injury site with breathing o respiratory distress ▪ dyspnea with accessory muscle use & increased WOB ▪ tachypnea with shallow respirations ▪ restlessness r/t hypoxia ▪ absent breath sounds on affected side ▪ respiratory acidosis • can't blow off CO2 due to shallow breaths ▪ pale, cool, moist skin that becomes cyanotic ▪ SQ emphysema • Management o pain control o stabilize flail segment to speed healing o positioning r/t ventilator/oxygenation o ETT with mechanical ventilation Pneumothorax o air enters pleural space & causes loss of negative intrapleural pressure that can create total or partial collapse of lung on affected side Open Pneumothorax • loss of chest wall integrity r/t trauma o MOI-penetrating chest wound • air drawn into pleural space during inspiration o can lead to tension pneumo if not treated quickly or correctly • Assessment o sucking sound o symmetrical chest movement o pain on respiratory movement o absent or diminished breath sounds on affected side o dyspnea o SQ emphysema • Management o cover wound with occlusive dressing to prevent air from entering lung ▪ cough then cover o airway, maintain SaO2 o insert and/or maintain chest tube o pain control Tension Pneumothorax • often accompanies flail chest o MOI-blunt or penetrating injury • chest wall injury allows air leaks into pleural space with each inspiration & is trapped by tissue acting as a one-way pressure valve o pressure build up as air continues to accumulate ▪ lung on affected side collapses ▪ mediastinal shift away from affected side resulting in possible decreased CO ▪ neck vein distention • Assessment o tacycardia/pnea, hypotension o extreme dyspnea o possible cyanosis o agitation & restlessness r/t hypoxia o tracheal deviation o asymmetric chest with 1 hyperexpanded side o little chest wall movement on affected side o respiratory acidosis ▪ lactic acid builds up • Management o O2 at 100% ▪ non-rebreather mask with 10-15L o convert tension pneumo to open pneumo ▪ needle thoracostomy (decompression) ▪ thoracentesis ▪ chest tube insertion Hemothorax • collection of blood in pleural space from blunt or penetrating trauma • CT & blood drainage usually only treatment required • bleeding subsides with chest tube insertion o monitor amount, color, & hemodynamic reaponse Chest tubes • Care o position below chest o maintain connections o observe for tidaling ▪ water in chamber moving up & down with inspiration/exhalation o excessive bubbling can indicate an air leak somewhere o assess dressing & skin around tube for crepitus o keep tubing connected ▪ do not clamp if tension pneumo • Maintenance o keep clamps & occlusive dressings near bedside o tidaling ▪ will stop when lung is reinflated ▪ will stop if tubing is kinked, occluded or has a break in the system ▪ will stop with bubbling r/t air leak o After removal, a chest Xray is done to verify lung reinflation Hemorrhagic Shock Assessment and treatment • Signs & symptoms o tachycardia, tachypnea o narrowing pulse pressure o falling PaO2 o decreased UO o Increased lactate levels indicate acidosis o falling H&H • Causes o blood loss • Pathophysiology o decreased intravascular volume o decreased venous return & decreased ventricular filling o decreased stroke volume & decreased cardiac output o impaired tissue perfusion o SNS, RAA system-increased AHD • Assessment • Classifications o Class 1-15% blood loss (early) ▪ normal vitals with possible mild anxiety ▪ treat with NS or LR o Class 2-15-30% blood loss ▪ tachycardia ▪ increased UO ▪ anxiety ▪ possible normal SBP with drop in MAP ▪ treat with NS or LR o Class 3-30-40% blood loss (moderate) ▪ tachycardia >120, tachypnea ▪ LOC changes, decreased SBP ▪ treated with LR or NS and probably blood products o Class 4->40% blood loss (emergent) ▪ tachycardia >140, tachypnea ▪ pronounced LOC changes ▪ low SBP & DBP that is difficult to find ▪ pale, cool skin with delayed cap refill ▪ LR/NS and blood products to treat • Management o restore intravascular volume • increases risk of ARDS with rapid fluid replacement ▪ crystalloids ▪ colloids ▪ blood products • women will typically always get O- if of childbearing age; men O+ o Increase preload ▪ give vasopressors o Oxygen Cardiac Tamponade • Caused by a penetrating injury resulting in rapid filling of the pericardial sac with fluid, or blunt injury associated with cardiac contusion o intrapericardial pressure increased o CO impaired r/t decreased venous return o ventricles can't fill properly during diastole o SV decreases resulting in tissue hypoxia • Assessment o dyspnea, tachycardia o increased pericardial pain with expiration and relieved by tripod position o agitation & restlessness r/t hypoxia o increased right atrial pressure o JVD o Beck's Triad ▪ hypotension ▪ muffled heart sounds ▪ elevated CVP o Paradoxical pulses ▪ BP 10 mmHg higher during expiration than on inspiration • Management o pericardialcentesis ▪ removing 40ml can increase SV 40 ml o supplemental O2 Abdominal Trauma (Blunt) • MC cause is MVA • nature & severity are often not immediately apparent so mortality can be high • Velocity o low-velocity: single organ injury o high-velocity: multi organ injury • Solid organs more affected r/t more vasculature and less give o spleen most frequent after blunt trauma to abd r/t left rib fracture (between 9-11) o liver most frequent injury after blunt or penetrating injury Abdominal Trauma (Penetrating) • GSW, stabbing • usually will require surgical repair of tissues o Stab wounds ▪ always have entry wound, may or may not have exit wound ▪ can't easily determine depth or direction o GSW ▪ often will have an exit wound, otherwise must locate the bullet • Assessment o history of injury o look for abdominal abrasions, increasing abd girth, absent bowel sounds ▪ Cullen's sign-bruising around umbilicus ▪ Grey Turner's sign-flank bruising o pain on movement ▪ Spleen=LUQ pain • Kehr's sign-pain to left shoulder r/t splenic bleeding ▪ Liver=RUQ pain • rebound tenderness • hypoactive, absent bowel sounds • Abd wall rigidity o Diagnostic testing ▪ FAST (focus assessment with sonography in trauma) ▪ CBC, amylase, liver enzymes, bilirubin ▪ Xray, DPL (peritoneal lavage) • Complications o peritonitis o hypovolemic shock r/t bleeding o abd compartment syndrome ▪ hypertension within organ; surgical emergency ▪ tissue hypoxia=increased lactic acid, more tissue damage & thick sludgy blood ▪ tachycardia • Management o do not remove foreign objects o do not replace abdominal contents, just cover with moist sterile dressing o reverse acidosis with HCO3 o maintain blood volume with colloids/crystalloids o NG tube with low-intermittent suction to relieve distension o FFP, platelets o NPO o pain meds, antibiotics, tetanus shot Kidney Trauma • blunt trauma caused by MVA, lower chest or flank injury • penetrating caused by GSW, stabbing • Check UA fast to check for damage • Assessment • hematuria may or may not be present • flank bruising (Turner's sign) • Abd/flank tenderness • Management • Monitor UO • catheterization or suprapubic catheter • abd distention • watch for hemorrhage, infection Organ Donation Determination • deceased o after confirmation of brain death • circulatory death o life sustaining therapies withdrawn • living donor o donation received from a healthy individual Maintaining Organ Viability • hemodynamically stable o pressors • maintain normal lab parameters • manage hypovolemia o give fluids • watch for DI • respiratory status • manage hypothermia Contraindications to being a transplant recipient • >70 years old • untreated malignancy or cancer within the previous 5 years • active infection, Hepatitis, substance abuse, TB • Confirmed HIV+ • severe COPD • diffuse atherosclerosis or CAD Rejection • Hyperacute o immediate graft necrosis as soon as organ is sewn in o rare • Accelerated o within first week • Acute o within 1st year o cell-mediated response managed with increasing immunosuppressant drugs o fevers may develop, so watch for infections • Chronic o months to years after transplantation o combination of cell-mediated responses ▪ Risk factors: increased donor age/young recipient, black, HTN, increased lipids Immunosuppressive Therapy • Induction o given upon transplantation in the OR o monoclonal antibodies & steroids • Maintenance o given long term for either the duration of recipient life or organ removal o antimetabolites, steroids, calcineurin inhibitors • Antirejection o immunosuppression, ▪ steroids, calcineurin inhibitors Adverse effects of immunosuppression • increased chances of infection r/t immunosuppressant drugs & steroids Signs & symptoms of organ rejection • Renal o elevated BUN/creatinine o weight gain o decreased UO o fever & chills • Lung o hard to tell difference between infection & rejection o dyspnea, fatigue, fever, & cough o infiltrates of pleural effusions on chest Xray • Liver o fever, fatigue, HA o abd swelling & tenderness o decreased appetite o jaundice & dark urine INOROUT during CPR • I-introduce self to the family • N-now explain current patient status • O-outcome that can happen • R-relationship or decision maker • O-options & choices to family • U-understand & assess family comprehension • T-time or take action Determining brain death • Coma o watch for grimace to noxious stimuli • absence of brain stem reflexes o pupils >/= 4mm & unresponsive o NO oculocephalic reflex (Doll's eyes) o NO oculovestibular reflex (Cold Caloric test) • apnea o 8 minutes @ 100% O2 and observe for respiratory movement Issues related to decision to limit care • patient comfort, no pain • provide guidance to family & patient • titrate therapy to remove distress Withdrawing care: terminal weaning • titrate pain medication & sedation o relief of tachypnea, dyspnea, & accessory muscle use • morphine Medications used at EOL • IV morphine for dyspnea & pain • IV benzodiazepines for anxiety (ativan) Family support • give time to make decisions • endure all know & understands prognosis • use chaplain, ethics committee, etc • encourage family to stay with patient RESPIRATORY O2-CO2 exchange • Ventilation-movement of gases in & out of alveoli • diffusion of O2 & CO2 at pulmonary capillaries o increased capillary pressure=decreased diffusion o decreased RBCs=decreased O2 transport=hypoxia • Oxygenated blood perfused to tissues • diffusion of gases occurs at cellular levels o CO2 transport to right side of heart o diffusion based on concentration gradient Compliance • stretch of lungs determined by elasticity o elastic recoil & compliance are inversely related • static o measured with no airflow (inpsiratory hold) • dynamic o measured while gases flowing (active breathing) Resistance • opposition to gas flow in airways o airway length o airway diameter o flow rate of gases Ventilation/Perfusion Relationships • V=air that reaches alveoli o normal ~4L/min • Q=circulation of blood through pulmonary capillaries o normal ~5L/min • VQ ratio=0.8 • Distribution of V o bases are better ventilated better than apex of lungs o lower thorax is larger & has most dependant alveoli o less pressure in bases to overcome to exchange gases ▪ (-) intrapleural pressure at apex r/t gravity • Distribution of Q o bases better perfused r/t gravity o intra-alveolar pressure are lower in bases for more perfusion • Shunting o VQ ratio <0.8 o decreased ventilation o little to no air movement • Dead Space o VQ ratio >0.8 o decreased perfusion Calculating Shunt • used to indicate normal gas exchange & how well O2 is moving from alveoli to arterial blood • normal gradient is <20mmHg o FiO2 (as decimal) x (barometric pressure [760]-water vapor [47])-PaCO2/respiratory quotient [0.8] o example: 0.5(760-47)-64/0.8=276.5 • P/F Ratio o PaO2/FiO2 o normal ration 400-500mmHg Lung Measures • Tidal Volume (VT) o normal breath o 500 ml or 5-7 ml/kg • Residual Volume (RV) o amount of air remaining after max expiration o ~1200 ml • Inspiratory reserve volume (IRV) o max amount of gas that can be inspired at end of normal breath (over & above VT) o ~3000 ml • Expiratory reserve volume (ERV) o max amount of gas that can be forcefully expelled at end of normal breath o ~1200 ml • Functional residual capacity (FRC) o volume of gas remaining in lungs at normal resting expiration o RV+ERV o ~2500 ml • Vital Capacity (VC) o max volume of gas forcefully expelled after maximum inspiration o VT+IRV+ERV o ~4600 ml • Total lung capacity (TLC) o max amount of air lungs can physically hold o ~6000 ml Abnormal Breathing Patterns • Cheyne-Stokes-cyclical with 15-20 sec apneic periods • Biots-cluster breathing, irregular • Kussmauls-deep, regular & rapid, hyperventilation • Apneustic-gasping inspirations Breath Sounds • Normal o bronchial-tracheal o bronchovesicular-mid chest o vesicular-all over lungs • Adventitious o crackles-wet, popping ▪ pulmonary edema, CHF, pneumonia o Rhonchi-low pitch rattle ▪ COPD, CHF o Wheezes-high pitch squeals ▪ asthma o Pleural Friction Rub-squeak & grating ▪ PE or pleurisy o Stridor-intense bronchial wheeze ▪ choking, foreign body in airway Oxygenation • PaO2-from ABGs o normal 80-100 mmHg o treat <60 • SaO2-from pulse oximeter o normal 92-100% Oxyhemoglobin Curve Changes • Shift to Right o fever o reduced pH (acidosis) o hypercapnia • Shift to Left o cold o alkalosis o low CO2 ABG interpretation • pH: concentration of hydrogen ions o normal 7.35-7.45 o <7.35=acidosis o >7.45=alkalosis • PaCO2: partial concentration of CO2 in arterial blood o normal 35-45 mmHg o >45=acidosis o <35=alkalosis • HCO3: concentration of sodium bicarbonate in blood o normal 22-26 o <22=acidosis o >26=alkalosis • PO2: normal 80-100 mmHg • Buffers o bicarb/carbonic acid o lungs o kidneys • Compensation o partial: abnormal pH o complete: normal pH Respiratory Acidosis • caused by hypoventilation (COPD, CNS depression) • Assessment o HA, DTRs hypoactive, hypoxia, dyspnea o hyperkalemia o VS & skin color changes • Treatment o TCDB, suction, treat infections, IS o O2 therapy o sodium bicarbonate Metabolic Acidosis • caused by DKA, renal failure, lactic acidosis, diarrhea • Assessment o HA, DTRs hypoactive o hyperkalemia o anion gap 8-16 (Na-Cl-HCO3) • Treatment o sodium bicarbonate Respiratory Alkalosis • caused by hyperventilation • Assessment o neuromuscular irritability/parasthesias, DTRs hyperactive, positive Chovstkek & Trousseaus signs, tetany o syncope • Treatment o CO2-rebreathe or retain Metabolic Alkalosis • caused by loss of GI contents, diuretics, excess intake of HCO3 • Assessment o neuromuscular irritability/parasthesias, DTRs hyperactive, positive Chovstkek & Trousseaus signs, tetany o hypokalemia • Treatment o IV fluids: 0.9% NS o potassium chloride o Diamox/acetazolamide (carbonic anhydrase inhibitor) o calcium gluconate R-O-M-E pH PCO2 HCO3 Metab Acidosis Decreased ---- Decreased Metab Alkalosis Increased --- Increased Resp Acidosis Decreased Increased --- Resp Alkalosis Increased Decreased --- Oxygen supplementation methods • Nasal Cannula o 1-5L/min=FiO2 24-44% o Hi-Flow Nasal Cannula ▪ 60-90% FiO2 • Simple Face Mask o 5-10 L/min=FiO2 30-60% • Mask with Reservoirs o partial rebreather=35-60% fiO2 o nonrebreather=60-80%FiO2 • Venturi Mask (fixed performance) o 4-10 L/min=FiO2 24-50% Endotracheal Tubes • use for 2-3 weeks timeframe • auscultate bilaterally for placement • CXR is gold standard for indication of correct placement • document (in cm) of tube to teeth or to gums for placement, and note any changes in placement • complications o upper airway trauma, tracheal erosion, infection, vocal cord damage Tracheostomy • used for long term mechanical ventilation • avoids vocal cord damage • suction frequently • reduces WOB • decreases dead space • can eat, drink, & talk with it in Ventilator Settings • FiO2: 21% RA • VT: 6-8 ml/kg, typical is 500 • RR: 14-20 initially, but can adjust based on ABGs • I:E ratio of 1:2 (length of inhale vs exhale) • Flow Rate: how quickly VT is delivered • Sensitivity: amount of effort for a breath • High pressure limit: 10-20 cm H20 Ventilator Modes • Pressure support Ventilation (PSV) o 5-10 cm H2O o patient's spontaneous respiratory activity is augmented by delivery of preset amount of inspiratory pressure ▪ no rate is set on vent; patient generates each breath ▪ allows for spontaneous respiration patterns • PEEP (positive pressure end expiration) o 5-20 cm H20 o can cause reduced CO if high and impedes venous return secondary to barotrauma or increased intrathoracic pressure o constant set pressure @ end of expiration ▪ used to prevent alveolar collapse ▪ decreases dead space & shunting • Volume Control (CMV)-mode of controlled venting that only delivers what vent is set at; all breaths are mechanical. PIP varies with patient effort o Assist Control (AC) ▪ set rate & volume ▪ patient has to trigger machine ▪ only will deliver a breath at set VT ▪ when rate decreases below preset limit for control, ventilator will deliver a breath • risk for hyperventilation & resp alkalosis o Synchronized Intermittent Mandatory Ventilation (SIMV) ▪ delivers mandatory/spontaneous breaths ▪ mechanical breaths delivered in synchrony with patient's breaths ▪ set VT rate; any more breaths patient wants are at their own rate & volume ▪ used for weaning & decreasing vent dependency • Pressure Control (PC)-vent allows for set airflow until preset pressure is reached. PIP allows for max pressure on inspiration & is constant o Continuous positive airway pressure (CPAP) ▪ similar to PEEP; during entire respiratory cycle ▪ can be used without a ventilator & patient can be alert ▪ used regularly for patients with sleep apnea, CHF Ventilator Alarms • Hi Peak pressure: coughing or other intra-thoracic pressure, biting tube, ARDS (pressure too high in unit) • Low pressure: low CPAP or PEEP, air leak • Low exhaled tidal volume (LETV): not exhaling properly • Low minute ventilation (LMV): not breathing as often as should be • High exhaled tidal volume (HETV): breathing out to frequently • High minute ventilation (HMV): breathing too fast over machine • apnea: no breathing occurring Complications of Ventilation • baro/volutrauma o can result in pneumothorax, SQ emphysema, tension pneumothorax • ETT slips into right bronchus so only ventilating one lung • unplanned extubation • tracheal/laryngeal tear or damage • aspiration • VAP Weaning • Methods o T-tube ▪ delivers passive O2 over airway to increase time off vent o SIMV o CPAP set at 3-5 cm H2O ▪ trial for weaning; pt does work, but + lung pressure is kept o PSV titrated down to 5-10 cm H2O ▪ decreased pressure increased volume allowing for max O2 distribution & conditioning of diaphragm • Must be hemodynamically stable with adequate CO • no use of accessory muscles • mental readiness for extubation • minimal need for medications such as morphine or fentanyl • Criteria o RR<25/min o VT >/= 3-5 o pH >/= 7.25 o PaO2 >60 o PaCO2 <45 o SaO2 >90 o FiO2 <40 • Stop weaning if o RR >35 or <8 o low VT <5 o low SaO2 <90 o HR or BP changes >20% from baseline o ST elevation or dysrhythmia o decreased LOC Acute Respiratory Failure (ARF) • Failure to oxygenate o altered gas exchange ▪ PaO2 <60, SaO2 <90 ▪ PaCO2 >50 ▪ pH<7.3 o hypoventilation o VQ mismatch o Low CO o Low hemoglobin o tissue hypoxia • Failure to ventilate o hypercapnia ▪ >45 o alveolar hypoventilation o VQ ratio <0.8 • Pathophysiology: o 50/50 Rule: PaCO2 >50 or PaO2 <50 ▪ increased pulmonary vascular resistance • Cor Pulmonale: R heart failure & systemic edema • L heart failure & decreased CO r/t backed up lungs ▪ diaphragmatic fatigue r/t increased WOB o BNP for heart failure ▪ normal is <100, 100s level is concern ▪ 900+ is indicative of HF • Assessment o Early: dyspnea, anxiety, HA, fatigue, cool & dry skin, HTN, tachycardia, dysrhythmia o Intermediate: confusion, lethargy, tachypnea, hypotension/vasodilation o Late: cyanosis, diaphoresis, coma, respiratory arrest o decreased PaO2, increased PaCO2, decreased pH (acidotic) o decreased SVO2=impaired tissue oxygenation • Management o establish & maintain airway ▪ artificial ▪ TCBD, suction ▪ bronchodilators, steroids, antibiotics o Maintain oxygenation ▪ increased FiO2 with CPAP or Venturi mask o correct A/B balance ▪ give bicarb o Restore F/E balance ▪ treat hypokalemia • ARF in COPD o VQ mismatch worsens <0.8 o causes acute exacerbations, CHF/pulmonary edema, pneumonia, dehydration , F&E imbalances o correct hypoxemia o bronchodilators, steroids, antibiotics, sedatives with caution ARDS • Initiation o disruption of capillary permeability o cascade effect of cellular mediators ▪ neutrophils, macrophages, platelets o humoral mediators cause further damage • Onset of non-cardiogenic pulmonary edema o Exudate Phase ▪ initial leak of capillary membranes/protein rich fluid fills capillary membranes & decrease gas exchange ▪ increased capillary flow over the next 4 days ▪ flow stays increased for appx 1 week • CXR will show bilateral infiltrates o Proliferation/alveolar collapse ▪ 7-10 days to 1 month ▪ decreased surfactant production ▪ VQ mismatch and hypoxia ▪ increased WOB with decreased lung compliance o Fibrotic/end stage ▪ pulmonary HTN begins ▪ alveolar hypoventilation leads to right ventricular failure ▪ fibrotic changes occur to alveolar capillary membranes ▪ compliance further decreases & worsens the pulmonary HTN ▪ leukocytosis, fever occurs with worsening infiltrates • Causes o Direct: lung tissue damage ▪ pneumonia, drowning o Indirect: inflammatory process ▪ high volume replacement, sepsis • Diagnostic Criteria o PaO2/FiO2 ratio <200 o bilateral infiltrates o hypoxemia & acute respiratory alkalosis • Assessment o dyspnea & tachypnea o hyperventilation o resp alkalosis o increased P&T o Increased PIP on ventilation • Management o antibiotics o monitor respiratory & cardiac function o artificial airway & ventilation o O2 o low VT & use of PEEP o sedation, steroids, albuterol o NMBA o colloids & crystalloid administration • Complications o multi organ dysfunction syndrome (MODS) o renal failure o disseminated vascular coagulation (DIC) o can end up on O2 for life • Treatment o comfort ▪ sedation ▪ pain relief ▪ NMBA o decrease O2 use o proning o F&E balance o nutrition o psychosocial support Pulmonary Embolism • A clot or plug of material that travels from one blood vessel to another smaller vessel and occludes blood flow o affects dead space o brochoconstriction o shunting o pulmonary HTN o HF o decreased CO o Virchow's triad ▪ venous stasis ▪ altered coagulability ▪ damage to vessel walls o VQ mismatch >0.8 • Risk Factors o DVT o atherosclerosis o polycythemia o atrial fibrillation o broken long bones • Assessment o tachycardia & tachypnea o chest pain o dyspnea o hypoxemia o crackles & wheezes • Diagnosis o sense of impending doom o d-dimer assay + o duplex ultrasound o CT angiography o MRI o pulmonary angiogram • Prevention o medication ▪ heparin, lovenox o mechanical ▪ TED hose, SCDs o position changes o treatment of afib o prophylactic long term therapy ▪ coumadin • Treatment o maintain ABCs, O2 o thrombolytics to dissolve clot o heparin o surgery ▪ embolectomy ▪ vena cava umbrella [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 08, 2021
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Sep 08, 2021
Downloads
0
Views
53